Raport pani baronowej Hallett, DBE, przewodniczącej brytyjskiego dochodzenia w sprawie Covid-19
Przedstawione parlamentowi zgodnie z art. 26 ustawy o dochodzeniach z 2005 r
Zamówione przez Izbę Gmin do wydrukowania 18 lipca 2024 r
HC 18
| Postać | Opis |
|---|---|
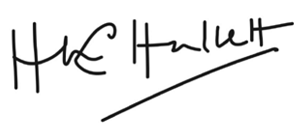
| Rysunek 1 | Gotowość i reagowanie na pandemię Struktury rządu centralnego w Wielkiej Brytanii i Anglii – ok. sierpień 2019 |
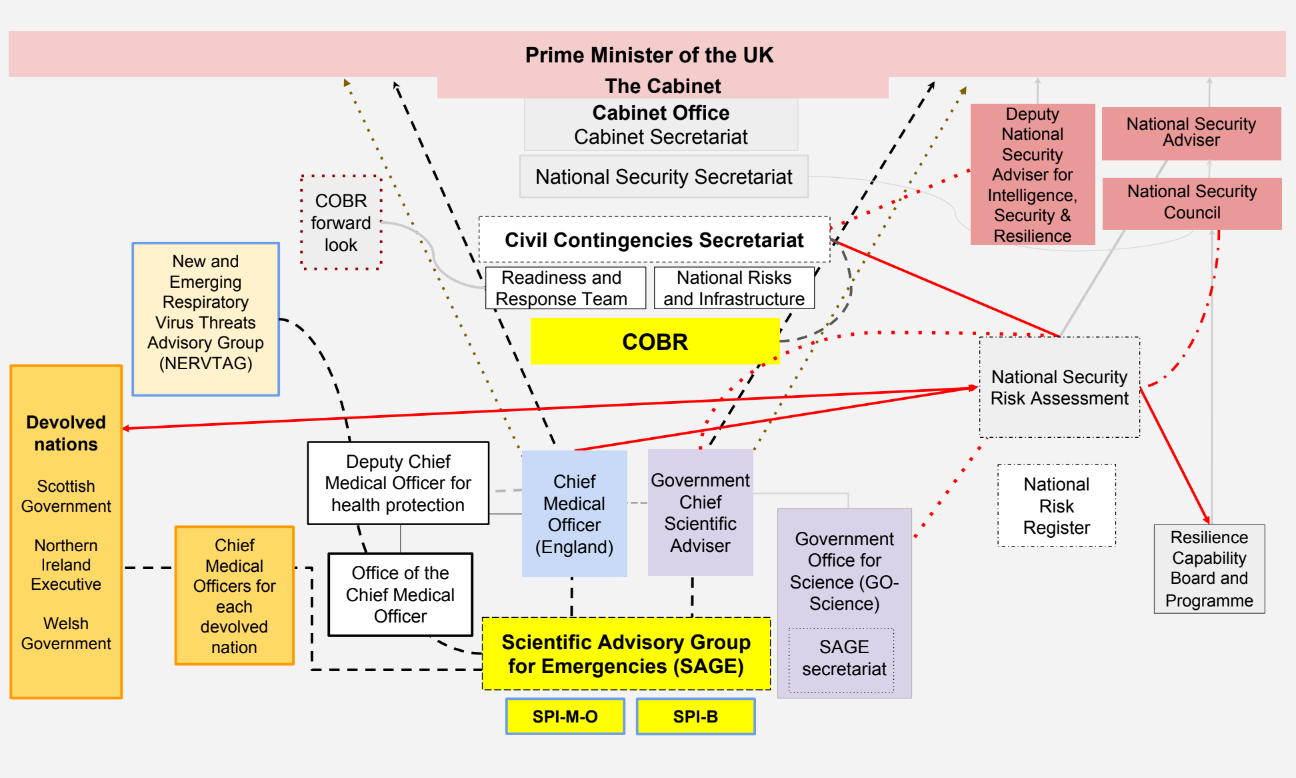
| Rysunek 2 | Struktury gotowości i reagowania na pandemię w Wielkiej Brytanii i Anglii – ok. sierpień 2019 |
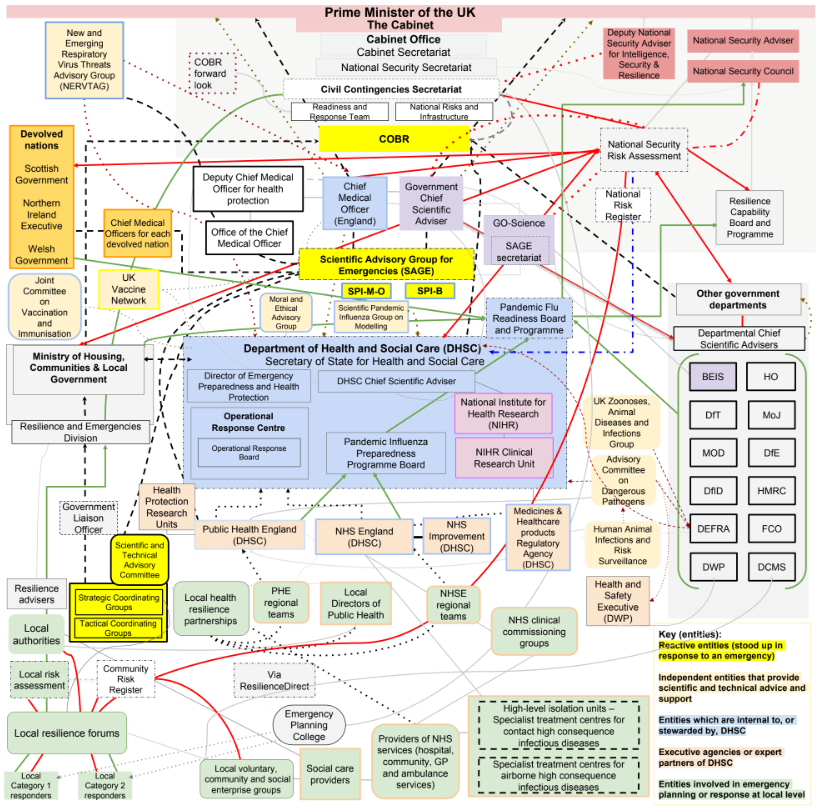
| Rysunek 3 | Gotowość i reagowanie na pandemię Struktury rządu centralnego w Szkocji – ok. 2019 |
| Rysunek 4 | Struktury gotowości i reagowania na pandemię w Szkocji – ok. 2019 |
| Rysunek 5 | Gotowość i reagowanie na pandemię Struktury rządu centralnego w Walii – ok. 2019 |
| Rysunek 6 | Struktury gotowości i reagowania na pandemię w Walii – ok. 2019 |
| Rysunek 7 | Centralne struktury wykonawcze dotyczące gotowości i reagowania na pandemię w Irlandii Północnej – ok. 2019 |
| Cyfra 8 | Struktury gotowości i reagowania na pandemię w Irlandii Północnej – ok. 2019 |
| Rysunek 9 | Kalendarium kluczowych działań przeprowadzonych w latach 2003–2018 |
| Tabela | Opis |
|---|---|
| Tabela 1 | Podsumowanie głównych epidemii i pandemii w przeszłości |
| Tabela 2 | Rozsądne najgorsze scenariusze na podstawie ocen ryzyka Wielkiej Brytanii w latach 2014, 2016 i 2019 |
| Tabela 3 | Uczestnicy Modułu 1 |
| Tabela 4 | Biegli moduł 1 |
| Tabela 5 | Moduł 1 Świadkowie, od których dochodzenie przesłuchało dowody |
| Tabela 6 | Moduł 1 Zespół doradców |
| Tabela 7 | Kluczowe ćwiczenia symulacyjne istotne dla gotowości i odporności na pandemię |
Wprowadzenie przez Rt Hon, baronową Hallett DBE
To pierwszy raport z brytyjskiego dochodzenia w sprawie Covid-19. Bada stan centralnych struktur i procedur Wielkiej Brytanii w zakresie gotowości, odporności i reagowania na wypadek pandemii.
Podstawowym obowiązkiem państwa jest ochrona obywateli przed krzywdą. Dlatego obowiązkiem państwa jest zapewnienie, że Wielka Brytania będzie tak samo dobrze przygotowana na zagrożenie ze strony śmiertelnych chorób, jak i na wypadek wrogich sił. Obydwa stanowią zagrożenie dla bezpieczeństwa narodowego.
W tym przypadku zagrożenie pochodziło ze strony nowego i potencjalnie śmiertelnego wirusa. Pod koniec grudnia 2019 r. w mieście Wuhan w prowincji Hubei w Chinach wykryto grupę przypadków zapalenia płuc nieznanego pochodzenia. Następnie zidentyfikowano nowy wirus, szczep koronaawirusa, i nadano mu nazwę koronawirus 2 ciężkiego ostrego zespołu oddechowego (SARS-CoV-2). Wirusowy patogen SARS-CoV-2 i wywołana przez niego choroba Covid-19 rozprzestrzeniły się po całym świecie.
Zabiła miliony ludzi na całym świecie i zainfekowała wiele milionów kolejnych. Według stanu na marzec 2024 r. Światowa Organizacja Zdrowia na całym świecie odnotowano ponad 774 miliony potwierdzonych przypadków i ponad 7 milionów zgonów, chociaż prawdziwe liczby są prawdopodobnie znacznie wyższe. Pandemia Covid-19 spowodowała smutek, niewypowiedzianą nędzę i zawirowania gospodarcze. Jego skutki będą odczuwalne przez dziesięciolecia.
Wpływ choroby nie spadł jednakowo. Badania sugerują, że w Wielkiej Brytanii współczynnik umieralności był znacznie wyższy wśród osób z niepełnosprawnością fizyczną lub trudnościami w uczeniu się oraz osób z istniejącymi wcześniej schorzeniami, takimi jak demencja i choroba Alzheimera, choroby serca, wysokie ciśnienie krwi i cukrzyca. W przypadku osób z niektórych mniejszości etnicznych oraz osób zamieszkujących obszary ubogie ryzyko zarażenia się Covid-19 i śmierci z jego powodu było znacznie wyższe.
Oprócz indywidualnej tragedii każdej śmierci, pandemia spowodowała niezwykłe obciążenie dla brytyjskich systemów opieki zdrowotnej, opieki, finansów i edukacji, a także dla miejsc pracy i przedsiębiorstw.
Podobnie jak w wielu innych krajach, rząd Wielkiej Brytanii oraz rządy Szkocji, Walii i Irlandii Północnej musiały podjąć poważne i dalekosiężne decyzje dotyczące sposobu powstrzymania wirusa i reagowania na niego. Decyzja z 23 marca 2020 r. o wykonaniu prawnie egzekwowanego nakazu pozostania w domu była dotychczas niewyobrażalna.
Życie Wielkiej Brytanii zostało poważnie ograniczone, ponieważ większość jej obywateli przebywała w domach. Prawie każda dziedzina życia publicznego we wszystkich czterech krajach została poważnie dotknięta. Sektory hotelarstwa, handlu detalicznego, podróży i turystyki, sztuki i kultury oraz sportu i rekreacji faktycznie przestały działać. Zamknięto nawet miejsca kultu.
Wzrósł poziom chorób psychicznych, samotności, deprywacji i narażenia na przemoc w domu. Dzieciom ominęła nauka akademicka i cenny rozwój społeczny.
Koszty ludzkie i finansowe opanowania Covid-19 są ogromne. Pożyczki rządowe oraz koszty zamówień publicznych, a także różnych programów utrzymania pracy, dochodów, pożyczek, zasiłków chorobowych i innych programów wsparcia poważnie wpłynęły na finanse publiczne i kondycję finansową Wielkiej Brytanii.
Wpływ na NHS, jej działalność, listy oczekujących i opiekę planową był równie ogromny. Miliony pacjentów albo nie ubiegały się o leczenie, albo nie otrzymały go, a zaległości w leczeniu osiągnęły historycznie wysoki poziom.
Szkody społeczne są powszechne, pogłębiają się istniejące nierówności i znacznie osłabiają dostęp do możliwości.
Ostatecznie Wielkiej Brytanii oszczędziły indywidualne wysiłki i poświęcenie pracowników służby zdrowia i opieki społecznej oraz urzędników służby cywilnej i publicznej, którzy walczyli z pandemią; przez naukowców, lekarzy i firmy komercyjne, które odważnie prowadziły badania w celu opracowania leków ratujących życie, a ostatecznie szczepionek; przez pracowników i wolontariuszy władz lokalnych, którzy opiekowali się i dostarczali żywność i lekarstwa osobom starszym i bezbronnym, a także szczepili ludność; oraz przez służby ratunkowe, pracowników transportu, nauczycieli, pracowników przemysłu spożywczego i leczniczego oraz innych kluczowych pracowników, dzięki którym kraj mógł funkcjonować.
Niestety, z opinii biegłych wynika, że zostaną oni wezwani ponownie. Nie chodzi o to, „czy” uderzy kolejna pandemia, ale „kiedy”. Dowody w przeważającej mierze wskazują, że w najbliższej lub średniej przyszłości prawdopodobnie pojawi się kolejna pandemia – potencjalnie jeszcze bardziej zaraźliwa i śmiertelna. Jeśli nie wyciągniemy wniosków i nie wdrożymy fundamentalnych zmian, ten wysiłek i koszty pójdą na marne, jeśli chodzi o kolejną pandemię.
Musi nastąpić radykalna reforma. Nigdy więcej nie można pozwolić, aby choroba doprowadziła do tak wielu zgonów i tak wielkiego cierpienia.
Moim obowiązkiem jest zadać pytanie tym ekstremalnym wydarzeniom i ich konsekwencjom. W maju 2021 r. ówczesny premier Boris Johnson, poseł do parlamentu, ogłosił swoją decyzję o wszczęciu ustawowego dochodzenia w celu zbadania gotowości Wielkiej Brytanii i reakcji na pandemię Covid-19 oraz wyciągnięcia wniosków na przyszłość. Zostałem mianowany przewodniczącym śledztwa w grudniu 2021 r.
Niezwykle szeroki zakres zadań i obowiązków niniejszego dochodzenia został sporządzony po formalnych konsultacjach pomiędzy Premierem i Pierwszymi Ministrami Szkocji i Walii oraz Pierwszym Ministrem i Zastępcą Pierwszego Ministra Irlandii Północnej. Następnie przeprowadzono szeroko zakrojony proces konsultacji społecznych.
Konsultowałem się szeroko we wszystkich czterech krajach, odwiedzając miasta w Anglii, Walii, Szkocji i Irlandii Północnej oraz rozmawiając w szczególności z wieloma osobami pogrążonymi w żałobie. Równolegle zespół badawczy spotkał się z przedstawicielami ponad 150 organizacji w ramach dyskusji przy okrągłym stole. W sumie w ramach zapytania w ramach konsultacji otrzymano ponad 20 000 odpowiedzi.
W świetle wyrażonych poglądów Zapytanie zaleciło wprowadzenie szeregu istotnych zmian do projektu SIWZ. Zostały one zaakceptowane w całości i obejmowały wyraźne uznanie potrzeby wysłuchania ludzkich doświadczeń i uwzględnienia wszelkich rozbieżności w skutkach pandemii.
Bezprecedensowa szerokość i zakres zakresu wymagań i obowiązków wzbudziły zatem poparcie społeczne.
Zwracałem się także o wyraźne upoważnienie do publikowania sprawozdań okresowych, aby zapewnić możliwość publikacji i rozpatrzenia wszelkich pilnych zaleceń w odpowiednim czasie. W oczywistym interesie publicznym leży jak najszybsze wydanie skutecznych zaleceń w celu zapewnienia istnienia odpowiednich struktur i systemów gotowości na wypadek sytuacji nadzwyczajnych oraz odporności przed następną pandemią lub krajowym stanem nadzwyczajnym.
Regulamin odzwierciedla bezprecedensową złożoność niniejszego Zapytania. Nie jest to dochodzenie ograniczone w zakresie pojedynczym wydarzeniem, krótkim upływem czasu, pojedynczą polityką lub skończonym sposobem postępowania rządu lub państwa. Jest to badanie tego, jak najpoważniejsza i najbardziej wielowarstwowa sytuacja nadzwyczajna w czasie pokoju dotknęła cały kraj (właściwie cztery kraje) oraz jak zareagował rząd Wielkiej Brytanii i zdecentralizowane administracje, w niemal całym zakresie swoich procesów decyzyjnych i funkcji publicznych. Pandemia i reakcja na nią nie oszczędziły żadnej części życia Brytyjczyków, dlatego prawie żadna część tego życia nie została wykluczona z naszych badań.
Od początku byłem zdecydowany, że to dochodzenie nie będzie ciągnąć się latami i nie sporządzić raportu lub raportów długo po tym, jak stracą one jakiekolwiek znaczenie. Dochodzenie postępowało zatem w ogromnym tempie.
W dniu 21 lipca 2022 r., około pięć miesięcy po zakończeniu ograniczeń prawnych Covid-19 nałożonych na ludność Wielkiej Brytanii, formalnie wszczęto dochodzenie. Ogłosiłem także decyzję o przeprowadzeniu Zapytania w modułach. Pierwsze wysłuchanie publiczne, Moduł 1 (Odporność i gotowość), odbyło się niecały rok później, między 13 czerwca a 20 lipca 2023 r.
Rozprawa została poprzedzona rozległym i skomplikowanym procesem pozyskiwania pod przymusem potencjalnie istotnych dokumentów z szerokiego zakresu źródeł. Materiał ten został następnie zbadany przez zespół dochodzeniowy i ponad 18 000 dokumentów uznano za istotne i ujawniono głównym uczestnikom, aby pomóc im w przygotowaniach do przesłuchania.
Zespół dochodzeniowy modułu 1 uzyskał ponad 200 zeznań świadków i wezwał 68 świadków rzeczowych i biegłych reprezentujących rząd Wielkiej Brytanii, zdecentralizowane administracje, struktury ds. odporności i zdrowia, grupy społeczeństwa obywatelskiego oraz grupy reprezentujące osoby pogrążone w żałobie.
Następnie w dniach od 3 października do 13 grudnia 2023 r. odbyło się wysłuchanie publiczne dotyczące modułu 2 (podstawowe podejmowanie decyzji i zarządzanie polityczne w Wielkiej Brytanii). Odbyły się analogiczne przesłuchania publiczne dotyczące podstawowych procesów decyzyjnych politycznych i administracyjnych w rządzie Szkocji, Walii i Irlandii Północnej. miejsce odpowiednio w dniach 16 stycznia – 1 lutego 2024 r., 27 lutego i 14 marca 2024 r. oraz 30 kwietnia i 16 maja 2024 r.
Na dzień publikacji niniejszego Raportu Moduł 3 (Wpływ pandemii Covid-19 na systemy opieki zdrowotnej w czterech krajach Wielkiej Brytanii), Moduł 4 (Szczepionki i produkty lecznicze), Moduł 5 (Zamówienia), Moduł 6 (Sektor opieki ), moduł 7 (testowanie, śledzenie i izolowanie), moduł 8 (dzieci i młodzież) oraz moduł 9 (reagowanie gospodarcze) zostały formalnie otwarte i są w trakcie przygotowań do przesłuchań publicznych. Odbędą się również dalsze przesłuchania w sprawie wpływu pandemii i reakcji na różne aspekty życia Brytyjczyków.
Żadne dochodzenie o tak szerokim zakresie nigdy nie było prowadzone z taką szybkością i rygorystycznością ani nie uzyskało tak dużej ilości istotnej dokumentacji w tak stosunkowo krótkim czasie. Słuszne jest stwierdzenie, że niewiele krajów wszczęło formalne dochodzenia prawne badające wiele aspektów pandemii Covid-19, nie mówiąc już o dochodzeniach na taką skalę. Zamiast tego szereg krajów, takich jak Szwecja, Norwegia, Dania i Australia, powołało niezależne komisje, na których czele stoją eksperci w dziedzinie epidemiologii, zdrowia publicznego, ekonomii i porządku publicznego. Takie komisje badawcze mogą być szybsze i tańsze niż dochodzenie ustawowe w Wielkiej Brytanii, ale niekoniecznie są to procesy prawne, za którymi stoi moc prawa. Większość z nich nie ma uprawnień pozwalających na wymuszenie przedstawienia dowodów lub złożenia zeznań pod przysięgą przez przywódców politycznych i administracyjnych; nie podlegają one publicznej kontroli w taki sam sposób, jak niniejsze dochodzenie; nie pozwalają osobom pogrążonym w żałobie ani innym zainteresowanym grupom na znaczący udział w procesie jako główni uczestnicy prawni; i nie mają czegoś podobnego do tego samego zakresu i głębokości.
Można zatem pomyśleć, że ustawowe dochodzenie posiadające szerokie uprawnienia było właściwym i jedynym właściwym narzędziem dochodzenia, biorąc pod uwagę kryzys narodowy o takiej skali i intensywności, który wiązał się z tak dużą ilością śmierci i cierpienia. Mieszkańcy Wielkiej Brytanii, a w szczególności osoby pogrążone w żałobie i osoby, które w inny sposób doznały krzywdy, muszą wiedzieć, czy można było w rozsądny sposób zrobić coś lepiej.
Jeśli zalecenia Badania zostaną wdrożone, ryzyko strat i cierpień w przyszłości zostanie zmniejszone, a decydenci, stojący przed niezwykle trudnymi decyzjami, otrzymają pomoc w reakcji na kryzys.
Pragnę wyrazić moją wdzięczność wszystkim, którzy poświęcili tak wiele czasu i zasobów, aby dostarczyć Dochodzeniu tak dużą ilość materiału dokumentacyjnego, wielu osobom, które udzieliły pomocy poprzez złożenie pisemnych oświadczeń i zeznań pod przysięgą, oraz wszystkim, którzy podzielili się z Inquiry swoimi doświadczeniami związanymi z pandemią podczas słuchania „Każda historia ma znaczenie”. Chciałbym także podziękować zespołowi ds. modułu 1 (zarówno sekretariatowi, jak i prawnemu), bez którego niezwykle ciężkiej pracy przesłuchania w ramach modułu 1 i niniejsze sprawozdanie nie byłyby możliwe.
Jestem także bardzo wdzięczny Głównym Uczestnikom i ich zespołom prawnym, zwłaszcza grupom reprezentującym osoby pogrążone w żałobie, za ich wnikliwy i sumienny wkład w proces Dochodzenia. Determinacja i determinacja ich klientów i przedstawicieli, a także umiejętności i doświadczenie ich zespołów prawnych w dalszym ciągu są nieocenioną pomocą dla mnie i zespołu dochodzeniowego.
Wstrząsające świadectwo straty i żalu złożone przez pogrążonych w żałobie świadków i inne osoby, które ucierpiały podczas pandemii, stanowiło zbawienne potwierdzenie celu tego dochodzenia.
Rt Hon, baronowa Hallett DBE
18 lipca 2024 r
Głosy osób pogrążonych w żałobie
Tata był niezwykle popularnym człowiekiem i dla wszystkich, którzy go znali, przyczyną wielkiego bólu była niemożność wzięcia udziału w jego pogrzebie. Tego dnia mogło tam przebywać tylko dziesięć osób, a ze względu na te ograniczenia wszyscy musieli zachować dystans społeczny. Aby pokazać, jak popularny był mój tata i wpływ, jaki wywarł na otaczających go ludzi, na ulicach stało ponad 300 osób na procesję… W przypadku mojego taty zaoferowano nam możliwość odbycia rozmowy telefonicznej – mówię rozmowę telefoniczną, rozmowę wideo z tatą w szpitalu, aby się pożegnać, z czego nie skorzystałem szpital, bo nie tak chcę pamiętać mojego tatę. Niektóre z ostatnich jego zdjęć, jakie mam, przedstawiają go siedzącego na szpitalnym łóżku w masce tlenowej. Wolałabym go takiego nie pamiętać, ale zamiast tego pamiętać, jaki był za życia”.
„Właściwie minęło pięć dni od zachorowania na Covid do jej śmierci… w tym czasie Covid zniszczył jej płuca, nerki, wątrobę i trzustkę. Próbowali poddać ją dializie, ale Covid sprawił, że jej krew była tak gęsta i lepka, że właściwie zablokowała aparat do dializy… powiedzieli jej i mnie, że nie nadaje się na OIOM [oddział intensywnej terapii], intubację i powiedziała nam obojgu, że umiera i niestety nie mogą nic zrobić, aby jej pomóc… to były okropne decyzje, które trzeba było podjąć w sprawie tego, kto może jechać, a kto nie, i oczywiście, czy ktoś byli z ukochaną osobą na końcu, w niektórych szpitalach często mówiono im: „Masz wybór: możesz albo przyjść i być przy nich na końcu, albo możesz iść na pogrzeb, ale nie możesz zrobić obu rzeczy” , bo trzeba być w izolacji.””²
„Nie poinformowano nas o tym, że gdy ktoś chory na Covid umrze, traktuje się go prawie jak odpady toksyczne. Są zapięte, a ty – nikt nam nie powiedział, że nie możesz ich prać, nie możesz ich ubierać, nie możesz robić żadnej z tych rzeczy, pogrzebów, ceremonii, po prostu nie możesz robić żadnej z tych rzeczy . Nie można było śpiewać na pogrzebie. Wiesz, jesteśmy Walijczykami, to coś, co musisz zrobić… mój tata nie miał dobrej śmierci. Większość bliskich naszych członków nie miała dobrej śmierci… Kiedy wychodziliśmy ze szpitala, mój tata – dostaliśmy rzeczy mojego taty w torbie Tesco. Niektórzy otrzymali cudze ubrania, które były w dość okropnym stanie. Właśnie takie rzeczy nie są często brane pod uwagę… istnieje coś takiego jak dobra śmierć i myślę, że zostało to bardzo przeoczone podczas pandemii… jest całe pokolenie, pokolenie mojej mamy, które nie Nie mam mechanizmów, jakbym musiał narzekać i zadawać pytania, a oni są załamani i naprawdę w szoku. Wiesz, moja mama płacze codziennie i – mimo że minęły już prawie trzy lata… to po prostu – pozostaje z poczuciem, że nikogo to nie obchodzi.”3
„Kiedy zawieźliśmy mamę do szpitala, było tam bardzo mało miejsc – tylko plastikowy fartuch dla personelu, a moja siostra zapytała o Covid i powiedziano nam, żebyśmy się nie martwili, to będzie błyskawiczna sprawa i minie lato... Jestem tutaj, aby przypomnieć wszystkim o kosztach ludzkich, jakie ponieśliśmy jako osoby pogrążone w żałobie. Moja mamusia nie była mięsem armatnim. Moja mamusia była cudowną małą kobietką, która miała ducha Goliata i wiem, że stoi tu dzisiaj ze mną, ponieważ chciała, abym tu był, ponieważ wie, że żyła życiem, tak jak wszyscy nasi bliscy, i bardzo ważne jest, abyśmy pamiętali o kosztach ludzkich, ponieważ obecnie zbyt wielu ludzi uważa, że Covid już zniknął. Ludzie nadal tracą życie z powodu Covida.”⁴
Podsumowanie wykonawcze
W 2019 r. w Wielkiej Brytanii i za granicą panowało powszechne przekonanie, że Wielka Brytania jest nie tylko odpowiednio przygotowana, ale jest jednym z najlepiej przygotowanych krajów na świecie do reakcji na pandemię. W niniejszym raporcie stwierdza się, że w rzeczywistości Wielka Brytania była źle przygotowana na radzenie sobie z katastrofalną sytuacją nadzwyczajną, nie mówiąc już o pandemii wirusa Covid-19, która faktycznie wybuchła.
W 2020 r. Wielkiej Brytanii brakowało odporności. W momencie wybuchu pandemii poprawa stanu zdrowia uległa spowolnieniu, a nierówności w zdrowiu pogłębiły się. Wysoki poziom istniejących wcześniej chorób serca, cukrzycy, chorób układu oddechowego i otyłości, a także ogólny poziom złego stanu zdrowia i nierówności zdrowotnych oznaczały, że Wielka Brytania była bardziej bezbronna. Usługi publiczne, w szczególności opieka zdrowotna i społeczna, w normalnych czasach były bliskie, jeśli nie przekraczały swoich możliwości.
W dochodzeniu uznano, że decyzje dotyczące alokacji zasobów w celu przygotowania się na sytuację nadzwyczajną cywilną obejmującą cały system należą wyłącznie do wybranych polityków. Muszą stawić czoła konkurencyjnemu żądaniu publicznych pieniędzy i ograniczonych zasobów. Może ich kusić skupienie się na bezpośrednim problemie, przed którym stoją, zamiast rozwodzić się nad tym, co może się wydarzyć, a co nie. Odpowiednie przygotowanie na pandemię kosztuje. Polega na przygotowaniu się na wydarzenie, które może nigdy nie nastąpić. Ogromne koszty finansowe, gospodarcze i ludzkie pandemii Covid-19 są jednak dowodem na to, że w obszarze gotowości i odporności pieniądze wydane na systemy zapewniające naszą ochronę mają kluczowe znaczenie i znacznie przewyższą koszty niezastosowania się do tych działań.
Gdyby Wielka Brytania była lepiej przygotowana na pandemię i odporniejsza na nią, można byłoby uniknąć części tych kosztów finansowych i ludzkich. Wiele z bardzo trudnych decyzji, jakie musieli podjąć decydenci, zostałoby podjętych w zupełnie innym kontekście. Gotowość i odporność na kryzys cywilny obejmujący cały system należy traktować w podobny sposób, w jaki traktujemy zagrożenie ze strony wrogiego państwa.
Dochodzenie wykazało, że system budowania gotowości na pandemię ma kilka istotnych wad:
- Wielka Brytania przygotowała się na niewłaściwą pandemię. Znaczące ryzyko pandemii grypy było rozważane, pisane i planowane od dawna. Jednak ta gotowość była niewystarczająca w przypadku globalnej pandemii tego rodzaju, która uderzyła.
- Instytucje i struktury odpowiedzialne za planowanie na wypadek sytuacji nadzwyczajnych były labiryntem w swojej złożoności.
- Ocena ryzyka, na jakie narażona jest Wielka Brytania, a także tego, w jaki sposób można zarządzać tym ryzykiem i jego konsekwencjami i zapobiegać ich pogorszeniu oraz w jaki sposób można na nie zareagować, zawierał fatalne błędy strategiczne.
- Jedyna strategia brytyjskiego rządu na wypadek pandemii z 2011 r. była przestarzała i brakowało jej
zdolność adaptacji. Został praktycznie opuszczony już po pierwszym spotkaniu z pandemią. Skoncentrował się tylko na jednym rodzaju pandemii, nie uwzględnił odpowiednio zapobiegania lub proporcjonalności reakcji i nie poświęcił wystarczającej uwagi gospodarczym i społecznym konsekwencjom reakcji na pandemię. - W planowaniu na wypadek sytuacji nadzwyczajnych zasadniczo nie uwzględniono w wystarczającym stopniu istniejących wcześniej nierówności w zakresie zdrowia i społeczeństwa oraz ubóstwa w społeczeństwie. Nie doceniono także pełnego zakresu wpływu środków rządowych i długoterminowego ryzyka, zarówno wynikającego z pandemii, jak i reakcji, na społeczności mniejszości etnicznych oraz osoby o złym stanie zdrowia lub innych bezbronnościach, a także brak zaangażowania odpowiednio z tymi, którzy najlepiej znają swoje społeczności, takimi jak władze lokalne, sektor wolontariatu i grupy społeczne.
- Nie wyciągnięto wystarczających wniosków z wcześniejszych ćwiczeń w zakresie sytuacji nadzwyczajnych i wybuchów chorób.
- Wystąpił szkodliwy brak skupienia się na środkach, interwencjach i infrastrukturze wymaganych w przypadku pandemii – w szczególności na systemie, który można skalować w celu testowania, śledzenia i izolowania w przypadku pandemii. Pomimo dużej ilości dokumentacji wytyczne dotyczące planowania nie były wystarczająco solidne i elastyczne, a dokumentacja dotycząca polityki była przestarzała, niepotrzebnie biurokratyczna i zainfekowana żargonem.
- W latach poprzedzających pandemię brakowało odpowiedniego przywództwa, koordynacji i nadzoru. Ministrom, którzy często nie są przeszkoleni w specjalistycznej dziedzinie nieprzewidzianych wypadków cywilnych, nie przedstawiono wystarczająco szerokiego zakresu opinii naukowych i opcji politycznych, a także nie zakwestionowano w wystarczającym stopniu rad, które otrzymali od urzędników i doradców.
- Można by ulepszyć samo świadczenie porad. Doradcy i grupy doradcze nie mieli wystarczającej swobody i autonomii, aby wyrażać odrębne poglądy, a także cierpieli z powodu braku znaczącego nadzoru zewnętrznego i wyzwań. Rada ta była często podważana przez „myślenie grupowe”.
Dochodzenie bez wahania stwierdza, że procesy, planowanie i polityka cywilnych struktur awaryjnych w rządzie Wielkiej Brytanii oraz zdecentralizowanych administracjach i służbach cywilnych zawiodły swoich obywateli.
Raport Modułu 1 zaleca fundamentalną reformę sposobu, w jaki rząd Wielkiej Brytanii i zdecentralizowane administracje przygotowują się na cywilne sytuacje kryzysowe obejmujące cały system. Chociaż każde zalecenie jest ważne samo w sobie, wszystkie zalecenia muszą zostać wdrożone wspólnie, aby wprowadzić zmiany, które w Dochodzeniu uznają za konieczne.
Późniejsze moduły będą szczegółowo przedstawiać sprawozdania i formułować zalecenia dotyczące gotowości trzech konkretnych aspektów brytyjskich struktur gotowości i reagowania: schematów testowania, śledzenia i izolowania; zapasy rządowe i zamówienia środków ochrony indywidualnej (ŚOI); i dostępność szczepionek.
W pierwszym Raporcie zaleca się w skrócie, co następuje:
- Każdy rząd powinien utworzyć jedną komisję ministerialną na szczeblu gabinetu lub równoważną komisję ministerialną (w tym starszego ministra odpowiedzialnego za zdrowie i opiekę społeczną) odpowiedzialną za gotowość i odporność ludności na sytuacje kryzysowe całego systemu, której przewodniczyć będzie przywódca lub zastępca przywódcy odpowiedniego rządu. W każdym rządzie powinna także istnieć jedna międzyresortowa grupa urzędników wyższego szczebla, która będzie nadzorować i wdrażać politykę dotyczącą gotowości i odporności cywilnej na sytuacje kryzysowe.
- Model głównego departamentu rządowego dotyczący gotowości i odporności cywilnej całego systemu na sytuacje kryzysowe jest nieodpowiedni i powinien zostać zniesiony.
- Rząd Wielkiej Brytanii i zdecentralizowane administracje powinny opracować nowe podejście do oceny ryzyka, które odejdzie od polegania na rozsądnych najgorszych scenariuszach w stronę podejścia oceniającego szerszy zakres scenariuszy reprezentatywnych dla różnych ryzyk i zakresu każdego rodzaju ryzyka. Powinien także lepiej odzwierciedlać okoliczności i cechy charakterystyczne Anglii, Szkocji, Walii, Irlandii Północnej i Wielkiej Brytanii jako całości.
- Należy wdrożyć nową, obejmującą cały system strategię dotyczącą sytuacji nadzwyczajnych w Wielkiej Brytanii, która powinna podlegać ponownej merytorycznej ocenie co najmniej co trzy lata, aby zapewnić, że jest aktualna i skuteczna oraz uwzględnia wnioski wyciągnięte z ćwiczeń w sytuacjach nadzwyczajnych.
- Rząd Wielkiej Brytanii i zdecentralizowane administracje powinny ustanowić nowe mechanizmy terminowego gromadzenia, analizowania, bezpiecznego udostępniania i wykorzystywania wiarygodnych danych na potrzeby reagowania w sytuacjach kryzysowych, takich jak systemy danych, które będą testowane podczas ćwiczeń związanych z pandemią. Ponadto należy zlecić szerszy zakres badań „hibernowanych” i innych, zaprojektowanych z myślą o szybkim dostosowaniu do nowego ogniska choroby.
- Rząd Wielkiej Brytanii i zdecentralizowane administracje powinny organizować ogólnokrajowe ćwiczenia w zakresie reagowania na pandemię co najmniej co trzy lata.
- Każdy rząd powinien opublikować raport w ciągu trzech miesięcy od zakończenia każdego ćwiczenia w zakresie stanu nadzwyczajnego, podsumowujący ustalenia, wnioski i zalecenia, a także powinien opublikować w ciągu sześciu miesięcy od ćwiczenia plan działania określający konkretne kroki, jakie należy podjąć w odpowiedzi na zalecenia zawarte w raporcie Wyniki. Wszystkie sprawozdania z ćwiczeń, plany działania, plany awaryjne i wytyczne z całej Wielkiej Brytanii powinny być przechowywane w jednym ogólnokrajowym archiwum internetowym, dostępnym dla wszystkich osób zaangażowanych w gotowość, odporność i reagowanie na sytuacje kryzysowe.
- Każdy rząd powinien co najmniej raz na trzy lata sporządzać i publikować dla swoich odpowiednich organów ustawodawczych raport na temat gotowości i odporności cywilnej całego systemu na sytuacje kryzysowe.
- W służbie cywilnej rządu Wielkiej Brytanii i zdecentralizowanych administracji należy regularnie wykorzystywać zewnętrzne „zespoły czerwone”, aby badać i kwestionować zasady, dowody, polityki i porady dotyczące gotowości i odporności na cywilne sytuacje kryzysowe w całym systemie.
- Rząd Wielkiej Brytanii, w porozumieniu ze zdecentralizowanymi administracjami, powinien utworzyć ogólnokrajowy niezależny organ ustawowy zajmujący się gotowością, odpornością i reagowaniem na sytuacje cywilne w całym systemie. Organ powinien zapewniać niezależne, strategiczne doradztwo rządowi Wielkiej Brytanii i zdecentralizowanym administracjom, konsultować się z sektorem wolontariatu, społecznościami i przedsiębiorstwami społecznymi na poziomie krajowym i lokalnym, a także z dyrektorami ds. zdrowia publicznego oraz wydawać zalecenia.
Rozdział 1: Krótka historia epidemii i pandemii
Wstęp
| 1.1. | Aby ocenić stan gotowości narodu na pandemię, należy najpierw ocenić charakter ryzyka, prawdopodobieństwo jego wystąpienia oraz skutki ryzyka, jeśli wystąpi. W tym rozdziale omówiono krótką historię epidemii i pandemii, aby umieścić prawdopodobieństwo i możliwy wpływ w odpowiednim kontekście. |
| 1.2. | Epidemie i pandemie zdarzały się w całej zapisanej historii ludzkości.1 Stanowili i pozostają istotnym i rosnącym zagrożeniem dla bezpieczeństwa, ochrony i dobrostanu Wielkiej Brytanii.2 Szacuje się, że pandemia wirusa Covid-19 spowodowała na całym świecie około 22 miliony dodatkowych zgonów.3 Oficjalne dane brytyjskie podają, że liczba zgonów z powodu Covid-19 w czterech krajach Wielkiej Brytanii w czerwcu 2023 r. wyniosła ponad 225 000.4 Nic na taką skalę nie widziano od ponad stulecia. |
Główne epidemie i pandemie w przeszłości
| 1.3. | Wybuch chorób jest nieodłącznie związany z niepewnością i nieprzewidywalnością, ale pandemia Covid-19 nie była bez precedensu. Jak przedstawiono w Tabeli 1, poważne epidemie i pandemie (epidemia infekcji występująca na całym świecie lub na bardzo dużym obszarze i zwykle dotykająca dużą liczbę osób) nie są nieznane.5 |
| Okres czasu | Patogen | Choroba (nazwa potoczna lub potoczna) | Przypadki globalne (wskaźnik ataków) | Globalne zgony | Sprawy brytyjskie | zgonów w Wielkiej Brytanii | Wskaźnik śmiertelności przypadków* | Droga transmisji | Powszechna infekcja bezobjawowa? | Prawdopodobne pochodzenie |
|---|---|---|---|---|---|---|---|---|---|---|
| 1889 do 1894 | Niepewny. HCoV-OC43 lub grypa | Rosyjska grypa | Stał się endemiczny (>90%)* | 1m* | Stał się endemiczny (> 90%) | 132,000 | 0,1–0,28% | Oddechowy | Nieznane, ale prawdopodobne | Azja centralna |
| 1918 do 1920 | Grypa: H1N1 | Hiszpańska grypa | Stał się endemiczny (> 90%) | 50m* | Stał się endemiczny (> 90%) | 228,000 | 2,5–10% | Oddechowy | Tak | USA (lub, co mniej prawdopodobne, Chiny/Francja) |
| 1957 do 1959 | Grypa: H2N2 | Grypa azjatycka | Stał się endemiczny (>90%)* | 1,1 m | Stał się endemiczny (>90%)* | 5,000* | 0,017–0,1% | Oddechowy | Tak | Chiny |
| 1968 do 1970 | Grypa: H3N2 | Grypa Hongkong | Stał się endemiczny (> 90%) | 2 m | Stał się endemiczny (> 90%) | 37,500* | 0,1–0,2% | Oddechowy | Tak | Hongkong czy Chiny |
| 1977 do 1978 | Grypa: H1N1 | Rosyjska grypa | Stał się endemiczny (> 90%) | 700,000 | Stał się endemiczny (> 90%) | 6,000* | <0,1% | Oddechowy | Tak | Chiny lub Rosja (nie odzwierzęca)* |
| Od 1981 r | Retrowirus: HIV | AIDS | 84,2 mln łącznie, obecnie 38,4 mln (0,7%) | 40,1 m | 165,338 | 25,296 | ~99% [nieleczony] | Przenoszone przez krew/seksualne | Tak | Afryka Środkowo-Zachodnia (po raz pierwszy wykryto USA) |
| 2002 do 2003 | Koronawirus: SARS-CoV-1 | SARS | 8096 (<0,001%) | 774 | 4 | 0 | 9.6% | Oddechowy | NIE | Chiny |
| 2009 do 2010 | Grypa: H1N1 | Świńska grypa | Stał się endemiczny (pierwsza fala ~ 24%) [491 382 oficjalne]* | 284,000 [18 449 oficjalnych] | Stał się endemiczny (> 90%) [28 456 oficjalnych]* | 457 [urzędnik] | 0,01–0,02% | Oddechowy | Tak | Meksyk (po raz pierwszy wykryto USA) |
| Od 2012 roku | Koronawirus: MERS-CoV | MERS | 2519 (<0,001%) | 866 | 5 | 3 | 34.3% | Oddechowy | Na początku nie, ale z biegiem czasu będzie coraz więcej raportów | Arabia Saudyjska |
| 2013 do 2016 | Wirus Ebola: EBOV | Ebola | 28616 (<0,001%) | 11,310 | 3 | 0 | 62.9% | Kontakt | NIE | Gwinea |
| Od 2019 r | Koronawirus: SARS-CoV-2 | COVID-19 | Staje się endemiczny od 2023 r. (> 90%) | 22 m | Staje się endemiczny (>90%) [oficjalne 22 miliony] | 225,668 [urzędnik] | 0,67–1,18% [wskaźnik śmiertelności infekcji] | Oddechowy | Tak | Chiny |
Wszystkie liczby są przybliżone. Są to szacunki pochodzące z opublikowanych badań dostępnych przed 2020 rokiem, z wyłączeniem źródeł dotyczących SARS-CoV-2. Dane mogą nie być całkowicie porównywalne, a jakość metodologiczna jest różna. Gwiazdki oznaczają szczególnie ważne zastrzeżenia (patrz INQ000207453). Dalsze szczegóły, w tym wszystkie zastrzeżenia i odniesienia, znajdują się w pełnej tabeli: INQ000207453.
| 1.4. | Dwa typy patogenów odzwierzęcych budzą szczególne obawy podczas przygotowań na epidemie i pandemie: szczepy wirusa grypy pandemicznej i koronawirusy. Ponadto zawsze istnieje możliwość wystąpienia „choroby X” – hipotetycznego, powstającego przyszłego patogenu, obecnie o którym nie wiadomo, że powoduje chorobę u ludzi i który może wywołać pandemię, niezależnie od jej pochodzenia.⁶ Covid-19 w momencie pojawienia się był „chorobą” Choroba X'.⁷ |
Pandemia grypy
| 1.5. | Grypa pandemiczna jest wywoływana przez nowy wirus grypy, który różni się od zwykle krążących szczepów.⁸ Wywołuje powtarzające się pandemie, które różnią się pod względem skali, dotkliwości i skutków, a przy tym są niezwykle trudne do przewidzenia.⁹ Na przykład „hiszpański wirus grypy” Szacuje się, że pandemia grypy w latach 1918–1920 spowodowana szczepem grypy H1N1 spowodowała śmierć około 50 milionów ludzi na całym świecie i 228 000 w Wielkiej Brytanii.¹⁰ Dla kontrastu pandemia grypy H1N1 („świńska grypa”) w latach 2009–2010 , miał znacznie mniejszy wpływ niż typowe sezony grypowe.¹¹ |
| 1.6. | Przed pandemią Covid-19 przygotowanie i odporność Wielkiej Brytanii na pandemię skupiały się na grypie. Było to i pozostaje największym pojedynczym przewidywalnym ryzykiem związanym z patogenami.¹² Chociaż dla Wielkiej Brytanii zrozumiałe było nadanie priorytetu grypie pandemicznej, nie powinno to prowadzić do skutecznego wykluczenia innych potencjalnych ognisk patogenów. Ich liczba także wzrasta. |
Koronawirusy
| 1.7. | Koronawirusy u ludzi były postrzegane jedynie jako stosunkowo łagodna grupa krążących wirusów, które u większości ludzi powodowały łagodne choroby układu oddechowego (tj. przeziębienie).¹³ Dopiero pod koniec 2002 r. ludzkie koronawirusy stały się powodem do niepokoju na całym świecie¹⁴ Ciężkie. Uważa się, że ostry zespół oddechowy (SARS) rozwinął się od zwierzęcia zebranego na „mokrym targu” żywych zwierząt w prowincji Guangdong w Chinach pod koniec 2002 r.¹⁵ Była to pierwsza nowa ciężka choroba przenoszona z człowieka na człowieka, która pojawiła się na XXI wieku i spowodował epidemie w wielu krajach¹⁶ W czerwcu 2012 r. w Arabii Saudyjskiej po raz pierwszy zidentyfikowano koronaawirusa bliskowschodniego zespołu oddechowego (MERS-CoV) po przeniesieniu infekcji z wielbłądów na ludzi.¹⁷ W maju 2015 r. miała miejsce poważna epidemia MERS-CoV wystąpiło w placówkach opieki zdrowotnej w Korei Południowej, gdy zarażona osoba wróciła do domu z Bliskiego Wschodu¹⁸ |
Wybuchy chorób
| 1.8. | Epidemie i pandemie mogą pojawiać się na wiele sposobów. U ludzi nowe choroby zakaźne są spowodowane głównie przeniesieniem chorób odzwierzęcych.¹⁹ Dzieje się tak zazwyczaj, gdy ludzie wchodzą w bliski kontakt z zakażonymi zwierzętami lub produktami pochodzenia zwierzęcego, a patogen przekracza barierę gatunkową łączącą zwierzęta z ludźmi.²⁰ Świat jest pełen organizmów, które mają nie przedostały się jeszcze do populacji ludzkiej. Uważa się, że na całym świecie występuje ponad 1,5 miliona nieopisanych wirusów u ssaków i ptaków, z których około 750 000 może przedostać się do ludzi i wywołać epidemie.²¹ W 2020 r. znanych było ponad 200 patogenów odzwierzęcych .²² Ich wpływ sięga od całkowicie nieszkodliwych dla ludzi po te, które mogą wywołać pandemię i mieć niszczycielskie skutki. |
| 1.9. | Profesor Jimmy Whitworth i dr Charlotte Hammer, biegli w zakresie nadzoru nad chorobami zakaźnymi (zob Załącznik 1: Informacje o tym module i metodologia badania) wyjaśnił, że w ostatnich dziesięcioleciach wzrosło prawdopodobieństwo przedostania się nowych patogenów ze zwierząt na ludzi²3. Było to spowodowane wieloma czynnikami, w tym urbanizacją i globalizacją, które zwiększają prawdopodobieństwo przeniesienia patogenów z jednej części świata do drugiego i szybkość, z jaką to zrobią.²⁴ |
| 1.10. | Im bardziej świat jest ze sobą połączony, tym większe jest prawdopodobieństwo, że patogeny pojawiające się w jednej części świata rozprzestrzenią się na inną²⁵. Im więcej zmian i rozwoju ekologicznego ma miejsce na styku człowieka ze światem przyrody, tym większe prawdopodobieństwo że patogeny przeniosą się ze zwierząt na ludzi.²⁶ Im więcej laboratoriów na świecie zaangażowanych w badania biologiczne, tym większe jest ryzyko, że nastąpi wyciek z laboratoriów, co będzie miało konsekwencje dla całej populacji.²⁷ Zwiększona niestabilność między a w obrębie narodów zwiększa zagrożenie bezpieczeństwa biologicznego²⁸ Ryzyko pojawienia się i rozprzestrzeniania nowych patogenów w populacji ludzkiej prawdopodobnie tylko wzrośnie. Kluczowymi cechami patogenów o potencjale pandemicznym są wysoka zdolność adaptacji, wysoka zdolność przenoszenia się oraz zakaźność, zanim u żywiciela wystąpią objawy lub w przypadku braku jakichkolwiek objawów.²⁹ To właśnie na tych cechach, a także na niezwykle ważnym współczynniku śmiertelności przypadków, decyduje się Należy skoncentrować brytyjskie systemy gotowości i odporności. |
| 1.11. | Wypadki laboratoryjne i złośliwe wykorzystanie materiału biologicznego są rzadsze i rzadziej są ujawniane publicznie niż rozprzestrzenianie się chorób odzwierzęcych, ale ich konsekwencje mogą być równie śmiertelne.³⁰ Chociaż nowe patogeny nie są jedynym potencjalnym zagrożeniem biologicznym lub cywilnym, na jakie napotyka Wielka Brytania jasne jest, że społeczeństwo i rządy muszą bardzo poważnie potraktować ryzyko wybuchu epidemii patogenów oraz poczynić odpowiednie przygotowania. |
| 1.12. | Chociaż główne drogi przenoszenia grypy pandemicznej i koronawirusów przenoszą się przez powietrze i drogi oddechowe, istnieją – i będą w przyszłości, także w przypadku nowych patogenów – – inne potencjalne drogi przenoszenia.³¹ Mogą one obejmować: drogą pokarmową – przez wodę lub żywność (np. cholera i dur brzuszny); wektory – przenoszone przez owady lub pajęczaki (np. malarię i wirusa Zika); i kontakt – dotyk (np. choroba wywołana wirusem Ebola).³² Przed Covid-19 ostatnią poważną pandemię ze znaczną śmiertelnością wywoływał ludzki wirus niedoboru odporności (HIV), który do tej pory zabił ponad 40 milionów ludzi na całym świecie, a a nawet więcej ponad 25 000 osób w Wielkiej Brytanii.³³ HIV przenosi się drogą płciową i dożylną. Przed udostępnieniem leków przeciwretrowirusowych śmiertelność wynosiła prawie 100%.³⁴ |
| 1.13. | To stawia w kontekście pojawienie się koronaawirusa 2 ciężkiego ostrego zespołu oddechowego (SARS-CoV-2, wirusa wywołującego Covid-19) i pandemii Covid-19. Tylko w XX wieku zagrożenie epidemiami i pandemiami nie ustąpiło, ale wzrosło. Nowe choroby zakaźne stanowią część krajobrazu gotowości i odporności na sytuacje kryzysowe. Ich pojawienie się nie powinno być zaskoczeniem. |
| 1.14. | Na początku XXI wieku, przed pandemią Covid-19, na świecie wystąpiły cztery duże epidemie spowodowane poważnymi chorobami zakaźnymi u ludzi, które nie przerodziły się w globalne pandemie – z których trzy były spowodowane przez koronawirusy.³⁵ Brytyjska społeczność naukowa uznało, że koronawirusy to kategoria wirusów stanowiących „wyraźne i aktualne niebezpieczeństwo”, którym należy się zająć.³⁶ Międzynarodowa społeczność naukowa ostrzegła również przed niebezpieczeństwami wynikającymi z pojawiających się chorób zakaźnych odzwierzęcych, które były przyczyną większości pojawiających się chorób zakaźnych w ciągu ostatnich sześciu dekad – oraz zagrożenia pandemią stwarzanego przez patogeny układu oddechowego o dużym wpływie.³⁷ Profesor Whitworth, który przedstawił ekspertyzy w ramach dochodzenia w sprawie nadzoru nad chorobami zakaźnymi, opisał pandemię koronaawirusa jako „rozsądne założenie” przed rokiem 2020 , a inny oznacza „bardzo prawdopodobną” przyszłość.³⁸ |
| 1.15. | Co więcej, nietrudno było i nie jest trudno wyobrazić sobie wirusa, który jest bardziej zaraźliwy i bardziej śmiercionośny. Wskaźnik śmiertelności w przypadku Covid-19 wynosił od 0,5 do 1%.³⁹ Dla porównania, współczynnik śmiertelności SARS i MERS na początku epidemii (tj. przed odpornością populacji lub wprowadzeniem klinicznych środków zaradczych) wynosił odpowiednio około 10% i 35%.⁴⁰ Profesor Mark Woolhouse, profesor epidemiologii chorób zakaźnych na Uniwersytecie w Edynburgu, podkreślił to:
„[O]W skali potencjalnych pandemii Covid-19 nie znajdował się na szczycie i być może był dość daleko od czołówki. Może tak być następnym razem – i będzie następny raz… mamy do czynienia z wirusem, który jest znacznie bardziej śmiercionośny, a jednocześnie znacznie bardziej zaraźliwy… Następna pandemia może być znacznie trudniejsza do opanowania niż Covid-19, a wszyscy widzieliśmy szkody, jakie wyrządziła nam ta pandemia.”⁴¹ |
| 1.16. | W świetle tej historii odporność Wielkiej Brytanii na pandemie i jej przygotowanie na nie mają kluczowe znaczenie dla bezpieczeństwa narodu. Jednak nawet po niedawnych doświadczeniach związanych z pandemią Covid-19 niezwykle ważne jest, aby nie stracić perspektywy ani co do ryzyka, ani tego, co można z nim zrobić. Jak powiedzieli profesor Whitworth i dr Hammer w dochodzeniu:
„Epidemia Covid-19 była w ostatnim czasie bezprecedensowa i nierozsądne byłoby oczekiwać, że Wielka Brytania będzie w pełni przygotowana na hipotetyczną epidemię tej wielkości wywołaną wcześniej nieznanym patogenem.”⁴² |
| 1.17. | Zapytanie zgadza się. Nawet groźba wybuchu epidemii ma znaczący wpływ na gotowość społeczeństwa – niezależnie od tego, czy epidemia wystąpi, czy nie. Potencjalne zakłócenia w życiu społecznym i gospodarczym oraz koszt (w realnych warunkach finansowych i możliwościach) w wyniku fałszywego alarmu mogą być nieproporcjonalne do ciężaru rzeczywistej epidemii lub pandemii. Istnieją odpowiednie granice gotowości i odporności (podobnie jak w przypadku bezpieczeństwa), ale nadal można wprowadzić ulepszenia, nawet radykalne. Dla każdego rządu, za zgodą społeczeństwa, niezwykle ważne jest obranie kursu pomiędzy samozadowoleniem a nadmierną reakcją.⁴³ |
- Charlotte Hammer 14 czerwca 2023 81/4-12
- Charlotte Hammer 14 czerwca 2023 81/4-12; INQ000196611_0005 ust. 3. Rząd Wielkiej Brytanii uważa, że ogniska chorób zakaźnych będą prawdopodobnie częstsze do 2030 r., a kolejna nowa pandemia pozostaje realistyczną możliwością; patrz: Global Britain in a Competitive Age, HM Government, marzec 2021, s. 31 (https://assets.publishing.service.gov.uk/media/60644e4bd3bf7f0c91eababdGlobal_Britain_in_a_Competitive_Age_the_Integrated_Review_of_Security__Defence__Development_and_Foreign_Policy.pdf; INQ000196501).
- INQ000207453
- INQ000207453. Aktualne dane można znaleźć w dokumencie Deaths Register Weekly in England and Wales, Provisional, Office for National Statistics, 2024 (https://www.ons.gov.uk/peoplepopulationandcommunity/birthsdeathsandmarriages/deaths/datasets/weeklyprovisionalfiguresondeathsregisteredinenglandandwales).
- INQ000184638_0008 ust. 1.12
- INQ000196611_0007-0008 ust. 8, 13
- INQ000196611_0008-0009 pkt 13-15
- INQ000184638_0041 ust. 5.19
- INQ000184638_0041 ust. 5.21
- Patrz tabela 1 powyżej; INQ000207453_0001; INQ000196611_0007 ust. 10
- INQ000184638_041 ust. 5.21
- Christopher Whitty 22 czerwca 2023 r. 93/15–22
- INQ000184638_0043 ust. 5.28; Richard Horton 13 lipca 2023 67/15-19
- Richard Horton 13 lipca 2023 67.15-68.13
- INQ000195846_0007 ust. 21
- „Wnioski wyciągnięte z SARS: doświadczenie Agencji Ochrony Zdrowia, Anglia”, NL Goddard, VC Delpech, JM Watson, M. Regan i A. Nicoll, Public Health (2006), 120, 27-32 (http://doi.org/10.1016/j.puhe.2005.10.003; INQ000187893-1)
- INQ000195846_0010 pkt 36–37
- INQ000195846_0011 paragraf 40
- Sustaining Global Surveillance and Response to Emerging Zoonotic Diseases, Instytut Medycyny i Krajowa Rada ds. Badań, 2009, s. 44 (https://nap.nationalacademies.org/read/12625/chapter/1; INQ000149100); INQ000196611_0006, 0016 ust. 7, 33
- INQ000195846_0006 ust. 16. Na przykład pierwotnymi żywicielami pandemii grypy są zwykle dzikie ptaki wodne, a żywicielami pośrednimi są dzikie ptaki, zwierzęta gospodarskie i ssaki, takie jak świnie (INQ000196611_0007 ust. 9). Pierwotnymi żywicielami koronawirusów są najprawdopodobniej nietoperze, a żywicielami pośrednimi w poprzednich ogniskach były inne ssaki, takie jak cywety, jak w przypadku SARS, i wielbłądy dromaderowe, jak w przypadku MERS (INQ000196611_0008 ust. 11). Bliski kontakt może obejmować konsumpcję, polowanie, targi żywych zwierząt na mokro, obchodzenie się z nimi lub wspólne pożycie (INQ000196611_0006 ust. 7).
- INQ000196611_0016 para 33. Według stanu na czerwiec 2024 r. do priorytetowych chorób i patogenów Światowej Organizacji Zdrowia należą: Covid-19, gorączka krwotoczna krymsko-kongijska, choroba wirusowa Ebola i choroba wirusowa Marburg, gorączka Lassa, MERS, SARS, Nipah i choroby henipawirusowe, gorączka doliny Rift , wirus Zika i „choroba X” (INQ000196611_0008, 0017 pkt 13-15, 35).
- INQ000196611_0006 ust. 6
- INQ000196611_0005-0006, 0006-0007 ust. 5, 7
- Charlotte Hammer 14 czerwca 2023 81/22-85/2; INQ000196611_0006 ust. 7
- INQ000196611_0005 ust. 3
- INQ000196611_0005-0006 ust. 5
- INQ000196611_0010-0011 ust. 19
- INQ000196611_0005-0006 ust. 5
- INQ000196611_0007 ust. 8
- INQ000196611_0010 pkt 18–21
- INQ000184638_0037-0038, 0040-0041, 0042 pkt 5.4, 5.16-5.21, 5.23
- INQ000184638_0037-0038 ust. 5.4
- Patrz tabela 1 powyżej; INQ000207453
- Patrz tabela 1 powyżej; INQ000207453; INQ000184638_0038 ust. 5.5
- Te cztery epidemie to SARS (2002–2003), MERS w Arabii Saudyjskiej (od 2012 r.), MERS w Korei Południowej (2015) i Ebola (2013–2016).
- Mark Woolhouse 5 lipca 2023 r. 115/7-117/1; Zobacz też INQ000149116_0002
- Sustaining Global Surveillance and Response to Emerging Zoonotic Diseases, Instytut Medycyny i Krajowa Rada ds. Badań, 2009, s. 1–4 (https://nap.nationalacademies.org/read/12625/chapter/1; INQ000149100); Charlotte Hammer 14 czerwca 2023 81/22-82/22; Gotowość na pandemię patogenów układu oddechowego o dużym wpływie, Johns Hopkins Center for Health Security, wrzesień 2019 r., s. 19–20 (https://www.gpmb.org/reports/m/item/preparedness-for-a-high-impact-respiratory-pathogen-pandemic; INQ000198916)
- Jimmy Whitworth 14 czerwca 2023 r. 104/3-10
- INQ000195846_0008 ust. 25
- INQ000195846_0008 ust. 25
- Mark Woolhouse 5 lipca 2023 r. 148/5-22
- INQ000196611_0034 paragraf 86
- INQ000196611_0011-0012 ust. 22
Rozdział 2: System — instytucje, struktury i przywództwo
Wstęp
| 2.1. | W Wielkiej Brytanii (w tym w krajach zdecentralizowanych: Szkocji, Walii i Irlandii Północnej) istnieje wiele instytucji, struktur i systemów odpowiedzialnych za gotowość, odporność i reagowanie na pandemię. |
| 2.2. | W dochodzeniu wskazano główne organy oraz sposoby ich powiązania w szereg organogramów, zwanych w trakcie przesłuchań w ramach Modułu 1 „diagramami spaghetti”. Pokazują one złożony system, który rozwijał się przez wiele dziesięcioleci, rzekomo w celu zapewnienia rządowi Wielkiej Brytanii i zdecentralizowanej administracji spójnego i skutecznego podejścia do przygotowań na pandemię.¹ |
| 2.3. | W tym rozdziale omówiono kluczowe instytucje, struktury i systemy. Skuteczny system gotowości i odporności na sytuacje kryzysowe powinien był być wspólnym przedsięwzięciem rządu Wielkiej Brytanii i zdecentralizowanych administracji. System miał być prosty, przejrzysty i celowy. Należało ją zorganizować w racjonalnej i spójnej formie, aby zapewnić przygotowanie rządu Wielkiej Brytanii i zdecentralizowanej administracji na pandemię. W tym rozdziale rozważono także skuteczność modelu wiodącego departamentu rządowego w Wielkiej Brytanii w zakresie budowania gotowości i odporności na cywilne sytuacje kryzysowe obejmujące cały system. |
Międzynarodowy system bezpieczeństwa biologicznego
| 2.4. | Głównym celem bezpieczeństwa biologicznego (ogólne określenie przygotowań, polityk i działań mających na celu ochronę zdrowia ludzi, zwierząt i środowiska przed zagrożeniami biologicznymi) jest ochrona społeczeństwa przed szkodliwymi skutkami wybuchów chorób zakaźnych.² Należy zachować równowagę. pomiędzy nadmierną reakcją a nadmierną ostrożnością. Niewielka grupa infekcji może, ale nie musi, zadomowić się w populacji. Dlatego też we wczesnych stadiach epidemii prawdopodobne obciążenie zdrowia publicznego jest dość nieprzewidywalne – może wahać się od błahego po wyniszczające.³ Co więcej, w przypadku lepszego nadzoru nad pojawiającymi się infekcjami, w naturalny sposób będzie ich więcej „”fałszywe alarmy„”.⁴ Zatem inwigilacja sama w sobie niesie ze sobą ryzyko „płaczącego wilka”. Społeczeństwo nadmiernie zastraszone nie jest odporne. Jeżeli alarm zostanie wszczęty bez uzasadnionej przyczyny, cynizm dotyczący zagrożeń, jakie stwarzają poważniejsze ogniska choroby, podważy zaufanie społeczeństwa do bezpieczeństwa biologicznego.⁵ |
| 2.5. | Kluczowe znaczenie dla skutecznego systemu ostrzegania ma przejrzystość i przepływ informacji, zarówno w Wielkiej Brytanii, jak i za granicą. Międzynarodowy system bezpieczeństwa biologicznego opiera się na współpracy między narodami za pośrednictwem organizacji i struktur, w tym:
|
| 2.6. | Obecnie kraje nie mają zachęty – a wręcz przeciwnie – do zgłaszania ognisk choroby na swoim terytorium lub nie mają jej wcale. Konsekwencje takiego postępowania obejmują potencjalne szkody gospodarcze i pewien poziom napiętnowania. Pouczające są niedawne przykłady niechęci do zgłaszania ognisk choroby. Należą do nich ujawnienie przez Arabię Saudyjską wybuchu bliskowschodniego zespołu oddechowego (MERS) oraz ujawnienie przez chiński rząd przypadków ciężkiego ostrego zespołu oddechowego (SARS).⁹ |
| 2.7. | Globalny krajobraz koordynacji nadzoru nad chorobami zakaźnymi podlega obecnie ciągłym zmianom w miarę wprowadzania zmian na kilku poziomach, w tym wyjścia Wielkiej Brytanii z UE, negocjacji w sprawie traktatu pandemicznego, który może zastąpić obecne przepisy oraz utworzenia we wrześniu 2021 r. Organ Komisji ds. gotowości i reagowania na sytuacje kryzysowe w zakresie zdrowia publicznego. Jest zbyt wcześnie, aby ocenić wpływ tych zmian.¹⁰ |
| 2.8. | Chociaż wymagany jest pewien poziom realizmu, kultura społeczności międzynarodowej powinna przekształcić się w kulturę szczerości między narodami i otwartości wobec społeczeństwa w zakresie zgłaszania ognisk nowych patogenów. Rząd Wielkiej Brytanii mógłby przyczynić się do budowania takiej kultury poprzez dalsze zaangażowanie w prace instytucji globalnych, takich jak Światowa Organizacja Zdrowia, oraz wiele regionalnych i międzynarodowych systemów nadzoru i reagowania. Im więcej informacji można uzyskać i udostępnić oraz im mądrzej można je przesłuchać, tym lepiej przygotowana będzie Wielka Brytania i inne kraje. |
Wielka Brytania
| 2.9. | W literaturze rządowej wiele uwagi poświęca się zagadnieniu sytuacji kryzysowych cywilnych „całego systemu”. Są to zdarzenia lub sytuacje, które grożą poważnymi szkodami dla dobrostanu ludzi, środowiska lub bezpieczeństwa Wielkiej Brytanii.¹¹ Generalnie klasyfikuje się je jako zagrożenie (ryzyko o przyczynie innej niż szkodliwa) lub zagrożenie (ryzyko, które ma złośliwa przyczyna).¹² |
| 2.10. | To, czy stan nadzwyczajny jest kryzysem cywilnym obejmującym cały system, jest głównie kwestią skali. Sytuacje nadzwyczajne na małą skalę dotykają mniej osób i angażują mniej decydentów w kwestie gotowości, odporności i reagowania. Na przykład wypadek kolejowy jest głównie problemem związanym z transportem, a powódź jest w dużej mierze problemem środowiskowym. W związku z tym za gotowość, odporność i reagowanie odpowiadają na poziomie krajowym odpowiednie specjalistyczne departamenty – Departament Transportu i Departament Środowiska, Żywności i Spraw Wiejskich lub odpowiadające im dyrekcje lub departamenty w zdecentralizowanych administracjach.¹³ Są to bardziej „normalne” działania ”sytuacje kryzysowe.¹⁴ |
| 2.11. | Inne sytuacje nadzwyczajne mają znacznie szersze i głębsze skutki i wymagają znacznie większej liczby decydentów w odniesieniu do wszystkich aspektów gotowości, odporności i reagowania. Najbardziej złożone sytuacje kryzysowe angażują cały system władz centralnych, regionalnych i lokalnych w Wielkiej Brytanii oraz całe społeczeństwo.¹⁵ Katastrofy cywilne o charakterze ogólnosystemowym mają wpływ na całe społeczeństwo Wielkiej Brytanii i wymagają podejścia międzyresortowego zarówno wewnątrz, jak i na szczeblu lokalnym. pomiędzy rządem Wielkiej Brytanii a administracją zdecentralizowaną. |
| 2.12. | Obecnie pomiędzy rządem Wielkiej Brytanii a zdecentralizowanymi administracjami nie ma uzgodnionej definicji tego, co stanowi stan nadzwyczajny dla całego systemu. Należy to naprawić. Należy stworzyć jedną definicję, opartą na powyższym, i stosować ją do określenia struktur potrzebnych do reagowania, oceny ryzyka i projektowania strategii. Jedno jest jednak jasne: pandemia, która zabija ludzi, jest stanem nadzwyczajnym obejmującym cały system. Ryzyko pandemii wymaga zatem dokładnej oceny, planowania i reakcji. |
| 2.13. | Wielka Brytania sama w sobie jest złożona i ma odrębne systemy prawne oraz zróżnicowane ramy decentralizacji, które w różny sposób przekazują władzę Szkocji, Walii i Irlandii Północnej. Chociaż istnieją różnice w poszczególnych ustaleniach dotyczących decentralizacji, od 1999 r. w Szkocji, Walii i Irlandii Północnej zdrowie jest przede wszystkim kwestią zdecentralizowaną. |
| 2.14. | Jednakże ustawa Civil Contingency Act z 2004 r. oraz powiązane przepisy i wytyczne określają ramy ochrony ludności w sytuacjach nadzwyczajnych w całej Wielkiej Brytanii, biorąc pod uwagę decentralizację uprawnień.¹⁶ Ustawa dzieli lokalne służby ratownicze – przedstawicieli służb publicznych, w tym służb ratunkowych, władze lokalne, NHS i Health and Safety Executive – na dwie kategorie, nakładając na każdą inny zestaw obowiązków. Jest poparte wytycznymi ustawowymi, Gotowość na wypadek sytuacji awaryjnychoraz pakiet wytycznych pozaustawowych, w tym Reagowanie kryzysowe i odzyskiwanie.¹⁷ W czasie pandemii wirusa koronaawirusa (Covid-19) ramy prawne i powiązane wytyczne krajowe brzmiały: „Powszechnie uznawane [przez specjalistów i praktyków w dziedzinie zdrowia publicznego] jako przestarzałe i nieodnoszące się do współczesnych struktur, ról i obowiązków.¹⁸ Jak bada się w kolejnych modułach Zapytania, nie był on wykorzystywany. |
| 2.15. | Powinna istnieć współpraca między rządem Wielkiej Brytanii a zdecentralizowanymi administracjami na wszystkich poziomach. Najlepszą obroną przed rozprzestrzenianiem się patogenów były i pozostają silne krajowe mechanizmy nadzoru i wykrywania – na których ostatecznie opierają się wszystkie systemy międzynarodowe – oraz skuteczna współpraca między różnymi poziomami odpowiedzialności¹⁹. |
| 2.16. | W Wielkiej Brytanii nadzór obejmuje ciągłe, systematyczne gromadzenie, zestawianie, analizę i interpretację danych oraz rozpowszechnianie informacji wśród osób, które ich potrzebują (w tym na poziomie lokalnym); zajmuje się tym głównie Brytyjska Agencja Bezpieczeństwa Zdrowia²⁰ Dr Charlotte Hammer, biegły ds. nadzoru nad chorobami zakaźnymi (zob. Załącznik 1: Informacje o tym module i metodologia badania) zwrócił uwagę na znaczenie wczesnego ostrzegania:
„Im wcześniej otrzymasz alert, tym większe prawdopodobieństwo, że faktycznie na niego zareagujesz, ponieważ reakcja będzie znacznie, znacznie mniejsza, a znacznie mniejszą odpowiedź można montować częściej.”²¹ |
Rząd Wielkiej Brytanii i organizacje wspierające w Anglii
Rysunek 1: Gotowość i reagowanie na pandemię Struktury rządu centralnego w Wielkiej Brytanii i Anglii – ok. sierpień 2019
Źródło: wyciąg z INQ000204014
Rysunek 2: Struktury gotowości i reagowania na pandemię w Wielkiej Brytanii i Anglii – ok. sierpień 2019
Źródło: wyciąg z INQ000204014
Biuro Rady Ministrów
| 2.17. | Gabinet Rady Ministrów to departament rządu Wielkiej Brytanii odpowiedzialny za wspieranie Premiera, Rady Ministrów i szerzej rozumianego funkcjonowania rządu. |
| 2.18. | Sekretariat ds. Zagrożeń Cywilnych działał w ramach Sekretariatu Bezpieczeństwa Narodowego Urzędu Rady Ministrów²². Pełnił szereg ról, w tym:
|
| 2.19. | Katharine Hammond, dyrektor Sekretariatu ds. Zagrożeń Cywilnych od sierpnia 2016 r. do sierpnia 2020 r., powiedziała w dochodzeniu, że był to głównie „koordynowanie„organ zajmujący się ogólnosystemowym planowaniem cywilnym, reagowaniem i odbudową w sytuacjach kryzysowych²⁶ Chociaż znajdował się w centrum rządu, nie przewodził ani nie był odpowiedzialny za gotowość i odporność innych departamentów rządowych. Każdy departament rządowy był odpowiedzialny za zarządzanie ryzykiem wchodzącym w zakres jego kompetencji²⁷ |
| 2.20. | W centrum rządów tkwił problem historyczny: różnica między ilością czasu i zasobów przeznaczonych na rozważenie zagrożeń i niebezpieczeństw. Pani Hammond zasugerowała, że odzwierciedla to pogląd, że złośliwe zagrożenia ze swej natury mogą wydawać się bardziej niepokojące i można im raczej zapobiec.²⁸ Podczas swojej kadencji na stanowisku dyrektora Sekretariatu ds. Zagrożeń Cywilnych do zadań pani Hammond należało dbanie o to, aby nie doszło do -złośliwe ryzyko – zwane zagrożeniami, a nie zagrożeniami – otrzymało odpowiednią uwagę i uwagę wszystkich departamentów rządowych²⁹ |
Nadzór ministerialny
| 2.21. | David Cameron, poseł do parlamentu, premier od maja 2010 r. do lipca 2016 r., za jeden z celów swojego rządu uznał stworzenie architektury radzenia sobie z nieprzewidzianymi sytuacjami cywilnymi i bezpieczeństwem narodowym „bardziej strategiczne”.³⁰ Celem było umożliwienie rządowi Wielkiej Brytanii przyjęcia długoterminowej perspektywy na pojawiające się na horyzoncie zagrożenia dla bezpieczeństwa Wielkiej Brytanii.³¹ Jednym z pierwszych posunięć Camerona w rządzie było powołanie Rady Bezpieczeństwa Narodowego jako komitetu gabinetowego, wspierany przez Sekretariat ds. Bezpieczeństwa Narodowego i Doradcę ds. Bezpieczeństwa Narodowego.³² Rada Bezpieczeństwa Narodowego była głównym forum dyskusji ministerialnej na temat celów rządu Wielkiej Brytanii w zakresie bezpieczeństwa narodowego, w tym odporności.³³ Koncentrowała się na złośliwych zagrożeniach.³⁴ |
| 2.22. | Ponadto utworzono podkomisję Rady Bezpieczeństwa Narodowego (zagrożenia, zagrożenia, odporność i nieprzewidziane zdarzenia), której zadaniem jest skupienie się na planowaniu i gotowości na wypadek sytuacji kryzysowych, co obejmuje zagrożenia inne niż złośliwe.³⁵ Sir Oliver Letwin, poseł do parlamentu, minister polityki rządu od maja 2010 r. do lipca 2016 r. i kanclerzem Księstwa Lancaster od lipca 2014 r. do lipca 2016 r., został odpowiedzialny za podkomisję ds. zagrożeń, niebezpieczeństw, odporności i nieprzewidywalnych sytuacji i miał jej przewodniczyć pod nieobecność Camerona. Został opisany jako „pod wieloma względami ministrem ds. odporności”.³⁶ Cameron powiedział śledczym, że posiadanie silnego ministra w rządzie z „ucho premiera” na tym stanowisku było właściwym podejściem, ponieważ jedynie premier jest w stanie obarczyć swoimi decyzjami całą wagę rządu.³⁷ |
| 2.23. | Podkomisja ds. Zagrożeń, Niebezpieczeństw, Odporności i nieprzewidywalnych sytuacji przedstawiła Premierowi przegląd potencjalnych zakłócających wyzwań cywilnych na szczeblu krajowym, przed którymi może stanąć Wielka Brytania w ciągu następnych 6 miesięcy (w odróżnieniu od pięcioletnich ram czasowych Krajowego Rejestru Ryzyka i Krajowego Rejestru Ryzyka 20-letni harmonogram oceny ryzyka bezpieczeństwa).³⁸ W 2016 r., po wybuchu epidemii wirusa Ebola w 2013 r., rząd Wielkiej Brytanii utworzył specjalistyczną jednostkę badającą horyzonty wirusów, które mogą mieć wpływ na Wielką Brytanię, co zostało uwzględnione w raporcie ds. zagrożeń, zagrożeń i odporności oraz Podkomisja ds. nieprzewidzianych sytuacji.³⁹ |
| 2.24. | Podkomitet ds. zagrożeń, niebezpieczeństw, odporności i sytuacji awaryjnych odegrał ważną rolę we wdrażaniu Strategia gotowości na wypadek pandemii grypy w Wielkiej Brytanii w 2011 r (strategia z 2011 r.):
„składający się z ministrów ze wszystkich departamentów rządu centralnego i [administracja zdecentralizowana], nadzoruje i koordynuje krajowe przygotowania na wypadek wszystkich kluczowych zagrożeń w Wielkiej Brytanii, w tym pandemii grypy”.⁴⁰ Podkomisja położyła nacisk na Radę Ministrów i Premiera za ważne działania w zakresie gotowości. Cameron i sir Oliver Letwin powiedzieli uczestnikom dochodzenia, że jest to konieczne, aby zapewnić podjęcie działań w ważnych kwestiach.⁴¹ |
| 2.25. | Ostatnie posiedzenie Podkomisji ds. Zagrożeń, Niebezpieczeństwa, Odporności i Sytuacji Nieprzewidzianych miało miejsce w lutym 2017 r. (zob. Rozdział 5: Uczenie się na doświadczeniach).⁴² W lipcu 2019 r. podkomisja została formalnie „usunięty ze struktury komisji”.⁴³ Pani Hammond zasugerowała, że mogłoby to być „w razie potrzeby zwoływane ponownie”, ale zaakceptował fakt, że został on faktycznie zniesiony.⁴⁴ W rezultacie bezpośrednio przed pandemią nie było międzyrządowego nadzoru ministerialnego nad sprawami, które wcześniej należały do kompetencji podkomisji. |
Departament Zdrowia i Opieki Społecznej⁴⁵
| 2.26. | Większość sytuacji kryzysowych w Wielkiej Brytanii jest obsługiwana lokalnie przez służby ratunkowe. Jeżeli jednak skala lub złożoność sytuacji nadzwyczajnej jest taka, że wymaga koordynacji lub wsparcia rządu Wielkiej Brytanii, za ogólne zarządzanie planowaniem i reagowaniem odpowiada wyznaczony główny departament rządowy.⁴⁶ Departament Zdrowia i Opieki Społecznej był rządem wiodącym brytyjskiego rządu departament odpowiedzialny za gotowość, reagowanie i odbudowę na wypadek pandemii.⁴⁷ |
| 2.27. | W 2007 roku Departament Zdrowia ustanowił Program gotowości na pandemię grypy.⁴⁸ Program ten skupiał się na zarządzaniu gotowością na pandemię grypy w systemie opieki zdrowotnej i społecznej w Anglii. W skład jej zarządu wchodzili urzędnicy z Departamentu Zdrowia, Gabinetu Rady Ministrów, NHS England i Public Health England.⁴⁹ Jak omówiono w dalszej części niniejszego Raportu, dokonana przez brytyjski rząd ocena ryzyka pandemii i jego strategie radzenia sobie z tym ryzykiem ucierpiały, ponieważ skupiały się niemal całkowicie na grypę jako najbardziej prawdopodobną przyczynę pandemii. Przyczyną pandemii Covid-19 był oczywiście koronawirus. |
| 2.28. | Istniała również Rada ds. Gotowości na Pandemię Grypy, powołana w marcu 2017 r. przez Podkomisję ds. Zagrożeń, Zagrożeń, Odporności i Nieprzewidzianych Warunków⁵⁰ Jej zadaniem było koordynowanie planowania w całej Wielkiej Brytanii poprzez zaangażowanie zdecentralizowanych administracji i 14 odpowiednich departamentów rządowych Wielkiej Brytanii. ⁵¹ Od lutego 2018 r. Radzie ds. gotowości na pandemię grypy współprzewodniczy pani Hammond w imieniu Gabinetu Rady Ministrów oraz Emma Reed, dyrektor ds. gotowości na wypadek sytuacji kryzysowych i ochrony zdrowia w Departamencie Zdrowia i Opieki Społecznej.⁵² Ponownie ta rada zajmowała się jedynie przygotowaniami na pandemię grypy. Co więcej, jego prace pokrywały się z pracami w ramach Programu gotowości na wypadek pandemii grypy. |
| 2.29. | W 2021 r., najwyraźniej w uznaniu swoich podstawowych wad strukturalnych, Rada ds. Gotowości na Pandemię Grypy została zastąpiona przez podmiot zwany Radą ds. Zdolności ds. Chorób Pandemicznych. Uwzględniałoby to gotowość na szeroki zakres pandemii, w tym między innymi grypę pandemiczną, i skupiałoby się na praktycznych zdolnościach niezbędnych do reagowania na pandemie.⁵³ |
Zdrowie Publiczne Anglia
| 2.30. | Przed pandemią Covid-19 główna odpowiedzialność za zarządzanie epidemiami chorób zakaźnych o poważnych konsekwencjach spoczywała na Public Health England. Organ ten powstał w 2013 roku jako agencja wykonawcza Departamentu Zdrowia, której zadaniem jest ochrona i poprawa zdrowia i dobrostanu oraz zmniejszanie nierówności zdrowotnych. Obejmował głównie Anglię, z ograniczonymi obowiązkami obejmującymi całe Zjednoczone Królestwo.⁵⁴ |
| 2.31. | Funkcje Public Health England w zakresie gotowości i odporności na pandemię obejmowały:
|
| 2.32. | Duncan Selbie, dyrektor naczelny Public Health England od lipca 2012 r. do sierpnia 2020 r., opisał to w następujący sposób:
„dobrze przygotowany do doraźnej pracy w zakresie ochrony zdrowia, której zlecił [Departament Zdrowia i Opieki Społecznej] wykonać… ale… nie w pełni przygotowany na radzenie sobie ze skalą i wielkością pandemii niewiadomego pochodzenia, z którą świat stanął w styczniu 2020 r..⁶⁰ |
| 2.33. | W takim przypadku organizacja Public Health England została skutecznie zlikwidowana przez rząd Wielkiej Brytanii po rozpoczęciu pandemii. Od 2021 r. brytyjska Agencja Bezpieczeństwa Zdrowia połączyła personel i możliwości NHS Test and Trace z elementami ochrony zdrowia Public Health England.⁶¹ Sir Christopher Wormald, stały sekretarz Departamentu Zdrowia i Opieki Społecznej od maja 2016 r., opisał Brytyjska Agencja Bezpieczeństwa Zdrowia jako zapewniająca „stałą zdolność do przygotowania się na zagrożenia zdrowia, zapobiegania im i reagowania na nie”.⁶² Jego utworzenie w tym celu pokazało, że przed pandemią nie było tak efektywnej, stałej zdolności do stałego pobytu. |
Fachowe porady medyczne i naukowe
| 2.34. | Dyrektor medyczny w Anglii jest lekarzem, liderem w dziedzinie zdrowia publicznego i urzędnikiem publicznym, a także głównym doradcą medycznym rządu Wielkiej Brytanii. Biuro Naczelnego Lekarza składa się z mniej niż 20 osób, w tym Naczelnego Lekarza i Zastępcy Naczelnego Lekarza.⁶³ Obowiązki Naczelnego Lekarza obejmują zasadniczo trzy obszary: zapewnianie niezależnych porad naukowych ministrom całego brytyjskiego rządu w kwestiach medycznych i publicznych problemy zdrowotne; informowanie społeczeństwa o kwestiach zdrowotnych w sytuacjach nadzwyczajnych; oraz pełnienie funkcji zbiorowego przywództwa specjalistów w dziedzinie medycyny i zdrowia publicznego.⁶⁴ Połączone role dyrektora medycznego w Anglii i głównego doradcy medycznego rządu brytyjskiego działają równolegle do systemu głównych doradców naukowych. |
| 2.35. | System udzielania porad naukowych decydentom obejmował cały rząd Wielkiej Brytanii. Każdy departament i organizacje go wspierające miały własną metodę dostarczania decydentom informacji naukowych, porad i analiz.⁶⁵ Rządowi Wielkiej Brytanii doradzała także duża liczba naukowych grup doradczych, komitetów i podmiotów zajmujących się chorobami zakaźnymi u ludzi i gotowość na wypadek pandemii. Grupy te były w dużej mierze, choć nie wyłącznie, sponsorowane przez Departament Zdrowia i Opieki Społecznej jako główny departament rządowy ds. ryzyka chorób zakaźnych u ludzi. Zwykle przekazywali swoje porady bezpośrednio urzędnikom. |
| 2.36. | Każda z tych grup miała odrębne zadania i specjalizację. Kluczowymi naukowymi grupami doradczymi dotyczącymi ryzyka chorób zakaźnych u ludzi były:
|
| 2.37. | Większość departamentów rządowych Wielkiej Brytanii miała także głównego doradcę naukowego na szczeblu departamentu.⁷⁵ Byli oni odpowiedzialni za zapewnienie istnienia mechanizmów zapewniających doradztwo decydentom i ministrom, zarówno w obrębie ich departamentów, jak i w całym rządzie Wielkiej Brytanii.⁷⁶ System głównych doradców naukowych na poszczególnych wydziałach był jednym z kluczowych sposobów wypełnienia luki pomiędzy decentralizacją doradztwa naukowego w każdym departamencie rządu Wielkiej Brytanii a wprowadzeniem spójnego i konsekwentnego systemu doradztwa naukowego w całym rządzie Wielkiej Brytanii.⁷⁷ |
| 2.38. | W centrum systemu doradztwa naukowego rządu Wielkiej Brytanii znajdował się Główny Doradca Naukowy Rządu, wspierany przez Rządowe Biuro ds. Nauki (znane również jako GO-Science).⁷⁸ Byli oni odpowiedzialni za zapewnianie porad naukowych Premierowi i członkom Rady Ministrów, doradzanie rządowi Wielkiej Brytanii w kwestiach związanych z nauką na potrzeby polityki (w przeciwieństwie do samej polityki naukowej) oraz poprawa jakości i wykorzystania dowodów naukowych oraz doradztwa w rządzie.⁷⁹ Jedno z głównych forów dyskusyjnych za wymianę informacji odpowiadała Sieć Głównych Doradców Naukowych, składająca się z Głównego Doradcy Naukowego Rządu i głównych doradców naukowych na wydziałach, która spotykała się zwykle raz w tygodniu.⁸⁰ |
| 2.39. | System eksperckiego doradztwa medycznego i naukowego rządu brytyjskiego miał dwie główne zalety. Po pierwsze, stosunkowo niewiele sytuacji kryzysowych dotyczyło tylko jednego wydziału, a sieć obejmująca cały rząd umożliwiała szybkie przekazywanie informacji technicznych do departamentów, które ich potrzebowały.⁸¹ Po drugie, każdy doradca naukowy mógł zwrócić się do specjalistów ze swojego wydziału.⁸² Profesor Sir Christopher Whitty, dyrektor medyczny Anglii od października 2019 r., powiedział w dochodzeniu, że „Brytyjski system doradztwa naukowego jest złożony i niedoskonały, ale uważany jest za jeden z silniejszych na arenie międzynarodowej”.⁸³ Sir Jeremy Farrar, główny naukowiec Światowej Organizacji Zdrowia od maja 2023 r. i dyrektor Wellcome Trust w latach 2013–2023, zgodził się z tym.⁸⁴ |
Koordynowanie działań regionalnych i lokalnych w Anglii i Walii
| 2.40. | Lokalne fora dotyczące odporności to w Anglii i Walii główny mechanizm gotowości na wypadek sytuacji kryzysowych i współpracy między agencjami. Ich głównym celem jest zapewnienie lokalnym służbom ratowniczym możliwości skutecznego działania w zakresie obowiązków nałożonych na nich na mocy ustawy o nieprzewidzianych zdarzeniach cywilnych z 2004 r.⁸⁵ |
| 2.41. | Ministerstwo Mieszkalnictwa, Społeczności i Samorządów Lokalnych (poprzez swój Wydział ds. Odporności i Sytuacji Nadzwyczajnych, obecnie przemianowany na Dyrekcję ds. Odporności i Odbudowy) wspólnie z Gabinetem Rady Ministrów odpowiadało za odporność lokalną w Anglii.⁸⁶ Rola Wydziału ds. Odporności i Sytuacji Nadzwyczajnych (poprzez zespoły doradcy ds. odporności) miało przede wszystkim pomóc ratownikom w samodzielnym określeniu ryzyka, na jakie narażają się, oraz sposobach jego ograniczenia, a także zarządzaniu skutkami, które się zmaterializowały. Działałby jak „krytyczny przyjaciel”, kwestionowałby przesłanki, sugerował alternatywy, dzielił się dobrymi praktykami i wspierał działania związane z planowaniem lokalnym. Wnosił swój wkład, doradzał, ułatwiał i uczestniczył.⁸⁷ Rolą Wydziału ds. Odporności i Sytuacji Kryzysowych nie było jednak zapewnianie przywództwa ani zapewnianie, że lokalne służby ratownicze wypełniały swoje ustawowe obowiązki.⁸⁸ |
| 2.42. | Mark Lloyd, dyrektor naczelny Stowarzyszenia Samorządów Lokalnych od listopada 2015 r., określił powiązania między Ministerstwem Mieszkalnictwa, Społeczności i Samorządu Lokalnego a forami na rzecz odporności lokalnej jako „silne”.⁸⁹ Jednakże pod innymi względami opisał „fragmentację”, ponieważ podczas gdy Biuro Rady Ministrów koordynowało działania dotyczące incydentów o zasięgu ogólnokrajowym, Departament Zdrowia i Opieki Społecznej ponosił szczególną odpowiedzialność za pandemie. Lloyd stwierdził, że w rezultacie urzędnicy Ministerstwa Mieszkalnictwa, Społeczności i Samorządu Lokalnego stanęli przed „dużym wyzwaniem” w zarządzaniu interfejsem między władzami centralnymi i lokalnymi.⁹⁰ Brakowało ważnych powiązań między władzami lokalnymi i krajowymi. |
| 2.43. | Kiedy w ramach ustawy Civil Contingency Act z 2004 r. opracowywano wytyczne krajowe, na szczeblu rządu Wielkiej Brytanii brakowało również zrozumienia wzajemnych powiązań między podmiotami na poziomie lokalnym.⁹¹ |
| 2.44. | Struktury lokalne nie są wyrównane. Na przykład lokalne fora dotyczące odporności są zdefiniowane geograficznie według obszarów policji, ale lokalne partnerstwa na rzecz odporności zdrowotnej (fora strategiczne dla organizacji lokalnego sektora zdrowia) podążają za granicami geograficznymi zintegrowanego systemu opieki. Oznacza to, że obszary geograficzne, którymi zajmują się dyrektorzy ds. zdrowia publicznego, nie zawsze pokrywają się z obszarami, którymi zajmują się lokalne fora na rzecz odporności lub lokalne partnerstwa na rzecz odporności zdrowotnej.⁹² Ta wada strukturalna, za którą ostatecznie odpowiedzialny był Urząd Rady Ministrów, jest potencjalną receptą na zamieszanie i powielanie działań. Profesor Jim McManus, prezes Stowarzyszenia Dyrektorów Zdrowia Publicznego od października 2021 r. do października 2023 r., powiedział w dochodzeniu, że może to być „uporządkowany.⁹³ |
| 2.45. | Inną kluczową kwestią było to, że choć dyrektorzy ds. zdrowia publicznego (specjaliści odpowiedzialni za wypełnianie obowiązków władz lokalnych w zakresie zdrowia publicznego) współprzewodniczyli lokalnym partnerstwom na rzecz odporności zdrowotnej, nie zasiadali rutynowo na lokalnych forach poświęconych odporności, ponieważ nie byli do tego zapraszani Pod względem strukturalnym stworzyło to lukę w reagowaniu na sytuacje kryzysowe w zakresie zdrowia publicznego, w której specjaliści zajmujący się kryzysowymi sytuacjami cywilnymi i zdrowiem publicznym nie byli odpowiednio połączeni. Dyrektorzy ds. zdrowia publicznego, pracownicy zdrowia publicznego i władze lokalne mają do wniesienia kluczowy wkład w gotowość i odporność na pandemię. Ich wiedza i umiejętności stanowią ważny zasób lokalny i krajowy, z którego można korzystać w ramach gotowości i odporności cywilnej na wypadek sytuacji kryzysowych całego systemu.⁹⁵ Są oni w regularnym kontakcie z lokalną ludnością i dlatego odgrywają ważną rolę w komunikowaniu swoich potrzeb instytucjom, za które odpowiadają ma ono przygotować się na sytuacje kryzysowe cywilne obejmujące cały system i budować odporność na nie.⁹⁶ W opracowywaniu tych planów powinno być znacznie większe zaangażowanie dyrektorów ds. zdrowia publicznego i lokalnych zespołów ds. zdrowia publicznego. |
| 2.46. | Dr Claas Kirchhelle, biegły w ramach dochodzenia w sprawie struktur zdrowia publicznego (zob Załącznik 1: Informacje o tym module i metodologia badania) opisał długi cykl centralizacji i fragmentacji, w wyniku którego: „niewspółosiowość” w brytyjskich strukturach i systemach opieki zdrowotnej, opieki społecznej oraz gotowości na wypadek pandemii.⁹⁷ Kwestie ciągłej reorganizacji i rebrandingu trafiają na szczyt instytucji odpowiedzialnych za gotowość i odporność w Wielkiej Brytanii. Na przykład we wrześniu 2022 r. Sekretariat ds. Zagrożeń Cywilnych został podzielony na Dyrekcję ds. Odporności i oddzielną Jednostkę COBR. Miało to najwyraźniej wpłynąć na zmianę „zamiar" I "centrum” i „nieco inna oprawa”.⁹⁸ Jednakże liczba pracowników pozostała bardzo podobna i nie wydawało się, aby istniała zasadnicza różnica między starym a nowym systemem.⁹⁹ |
Szkocja
Rząd Szkocji i organizacje wspierające
Rysunek 3: Gotowość i reagowanie na pandemię Struktury rządu centralnego w Szkocji – ok. 2019
Źródło: wyciąg z INQ000204014
Rysunek 4: Struktury gotowości i reagowania na pandemię w Szkocji – ok. 2019
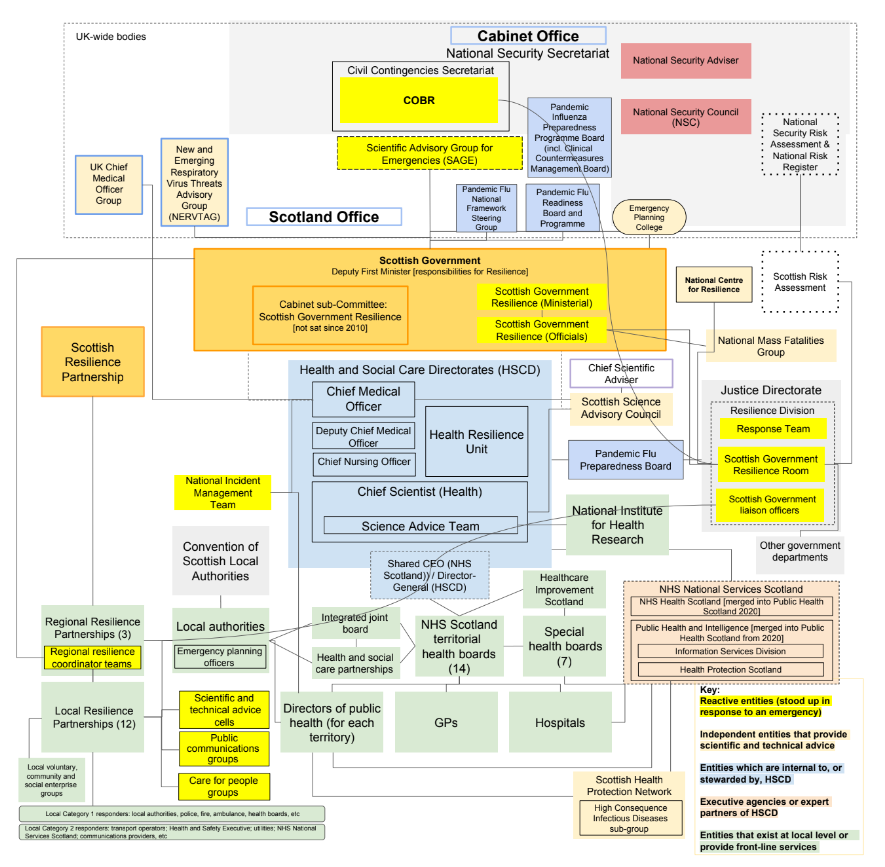
Źródło: wyciąg z INQ000204014_0006
| 2.47. | John Swinney MSP był wicepierwszym ministrem w rządzie Szkocji od listopada 2014 r. do marca 2023 r. Jako wicepierwszy minister Swinney był odpowiedzialny ministerialnie za odporność. Obowiązki te pełni obecnie Sekretarz Gabinetu ds. Sprawiedliwości i Spraw Wewnętrznych¹⁰⁰ Pan Swinney określił swoje stanowisko jako „udział w funkcji Resilience rządu szkockiego i ostatecznie przewodzenie jej”.¹⁰¹ |
| 2.48. | W Szkocji Podkomisja Rządu Szkockiego ds. Odporności zapewniła ministerialny nadzór nad polityką strategiczną i wytycznymi w kontekście odporności w Szkocji¹⁰² Jej ostatnie posiedzenie odbyło się w kwietniu 2010 r. i, jak wynika z protokołów, dysponowała pełnym programem działań pracy.¹⁰³ Prace te zostały podjęte przez Scottish Resilience Partnership, które było bezpośrednio zaangażowane na szczeblu ministerialnym w celu zapewnienia „strategiczny kierunek ministerialny”.¹⁰⁴ Ponieważ wszyscy obecni byli członkami Rady Ministrów, w razie potrzeby kwestie można było poruszać na tym forum.¹⁰⁵ Gillian Russell, dyrektor ds. bezpieczniejszych społeczności w okresie od czerwca 2015 r. do marca 2020 r., stwierdziła, że z jej doświadczenia wynika, że szkocki gabinet podjął decyzje w sprawie odporności, zamiast pracować za pośrednictwem podkomisji.¹⁰⁶ Niemniej jednak pan Swinney powiedział w dochodzeniu:
"[T]może zaistnieć potrzeba, aby określone forum okresowo, formalnie, w formie zarejestrowanej sprawdzało, na jakim etapie są przygotowania.”¹⁰⁷ |
| 2.49. | Odporność została skupiona w rządzie Szkocji wokół modelu „piasty i szprych”. W centrum modelu – piasta – znajdowała się Przygotowanie Szkocji.¹⁰⁸ Był to zestaw krajowych dokumentów zawierających wytyczne dotyczące sytuacji kryzysowych dla ludności, które określały:
„jak Szkocja jest przygotowana. Identyfikuje struktury oraz pomaga w planowaniu, reagowaniu i wychodzeniu z sytuacji awaryjnych. Nie jest to podręcznik operacyjny. Jest to raczej wytyczne dla ratowników, które mają im pomóc w ocenie, planowaniu, reagowaniu i powrocie do zdrowia.”¹⁰⁹ |
| 2.50. | Wydział ds. Odporności w rządzie Szkocji odpowiadał za planowanie sytuacji nadzwyczajnych, reagowanie i odbudowę, a także strategię, wytyczne i program prac na rzecz poprawy odporności podstawowych usług w Szkocji i Przygotowanie Szkocji wytyczne.¹¹⁰ Jego szerokie kompetencje obejmowały nadzorowanie zdolności i potencjału na poziomie krajowym, regionalnym i lokalnym w zakresie przygotowania i reagowania na sytuacje kryzysowe dla ludności, w tym pandemię grypy.¹¹¹ Odpowiadał także za Pomieszczenie ds. odporności rządu szkockiego. Oznaczało to, że podmiot odpowiedzialny za gotowość i odporność został zintegrowany z podmiotem odpowiedzialnym za reagowanie.¹¹² |
| 2.51. | Przed pandemią Covid-19 Dział ds. Odporności został przeniesiony z dyrekcji w Dyrekcji Generalnej ds. Konstytucji i Spraw Zewnętrznych do dyrekcji w Dyrekcji Generalnej ds. Edukacji i Sprawiedliwości.¹¹³ Później, w kwietniu 2021 r., został przeniesiony z powrotem do dyrekcji w Dyrekcji Generalnej ds. Strategii i Spraw Zagranicznych, której nazwa została obecnie przemianowana.¹¹⁴ W dochodzeniu zauważono, że podmioty odpowiedzialne za odporność zbyt często podlegają reorganizacji w Szkocji, podobnie jak ma to miejsce w innych zdecentralizowanych administracjach i w rządzie Wielkiej Brytanii . Istnieje jednak pewien stopień ciągłości, ponieważ służba cywilna w Szkocji nie ma departamentów wzorowanych na modelu Whitehall, lecz ma bardziej elastyczną i ujednoliconą strukturę obejmującą dyrekcje i agencje wykonawcze.¹¹⁵ Swinney zachował także przywództwo polityczne w celu zapewnienia odporności ma znaczenie we wszystkich zmianach poprzedzających jego rezygnację ze stanowiska wicepierwszego ministra w marcu 2023 r.¹¹⁶ |
| 2.52. | Dalej od centrum władzy struktury były bardziej rozproszone, a w konsekwencji bardziej zagmatwane. Rząd Szkocji miał własną Radę ds. Gotowości na Pandemię Grypy¹¹⁷ Health Protection Scotland (która była częścią NHS National Services Scotland, ale ponosiła także wspólną odpowiedzialność przed rządem Szkocji i Konwencją Szkockich Władz Lokalnych) była odpowiedzialna za zapewnienie krajowego przywództwa w zakresie ochrony szkockiego społeczeństwa przed chorobami zakaźnymi i przygotowaniem na epidemie.¹¹⁸ W Dyrekcji ds. Zdrowia Ludności oraz w Wydziale Gotowości i Reagowania na Kryzysy (w Dyrekcji Dyrektora Operacyjnego) funkcjonowało również kilka wydziałów zdrowia publicznego.¹¹⁹ 1 kwietnia 2020 r. , funkcje Health Protection Scotland zostały przeniesione do nowego organu, Public Health Scotland, którego plany zostały szybko zmienione ze względu na pandemię Covid-19.¹²⁰ |
Fachowe porady medyczne i naukowe
| 2.53. | W Szkocji dyrektor medyczny odgrywał jedynie ograniczoną rolę w zakresie gotowości i odporności na pandemię.¹²¹ Główny doradca naukowy rządu szkockiego nie ponosił głównej odpowiedzialności za doradztwo w zakresie zdrowia publicznego, nauk związanych ze zdrowiem publicznym i epidemiologii.¹²² Główny naukowiec (Zdrowie) w Szkocji podobnie nie odegrało żadnej roli w przygotowaniu na wypadek pandemii.¹²³ Szkocja w dużej mierze polegała, jeśli chodzi o fachowe porady medyczne i naukowe, na „Wywiad Wielkiej Brytanii.¹²⁴ |
Koordynowanie działań regionalnych i lokalnych
| 2.54. | Koordynacją działań służb ratowniczych zajmowały się trzy regionalne partnerstwa na rzecz odporności, składające się z przedstawicieli służb ratowniczych kategorii 1 i kategorii 2 oraz innych osób, jeśli uznano to za konieczne.¹²⁵ W każdym regionie Obszar Partnerstwa na rzecz Odporności obejmuje kilka Lokalnych Partnerstw na rzecz Odporności¹²⁶ Partnerstwa regionalne i lokalne obejmowały zarówno gotowość, jak i reagowanie.¹²⁷ Rząd Szkocji koordynował działania z tymi partnerstwami za pośrednictwem wbudowanych zespołów koordynatorów¹²⁸ |
| 2.55. | Scottish Resilience Partnership zgromadziło także główną grupę urzędników szkockiego rządu, ratowników kategorii 1 i przedstawicieli Stowarzyszenia Dyrektorów Zarządzających Władz Lokalnych, a także 12 szkockich Lokalnych Partnerstw na rzecz Odporności. Spotkałoby się to „okresowo nadzorować przygotowanie do działań resilience”.¹²⁹ Pan Swinney powiedział, że ministrowie również byli obecni „dość często" Do "wyznaczać kierunek myślenia ministerialnego.¹³⁰ |
Walia
Rząd walijski i organizacje wspierające
Rysunek 5: Gotowość i reagowanie na pandemię Struktury rządu centralnego w Walii – ok. 2019
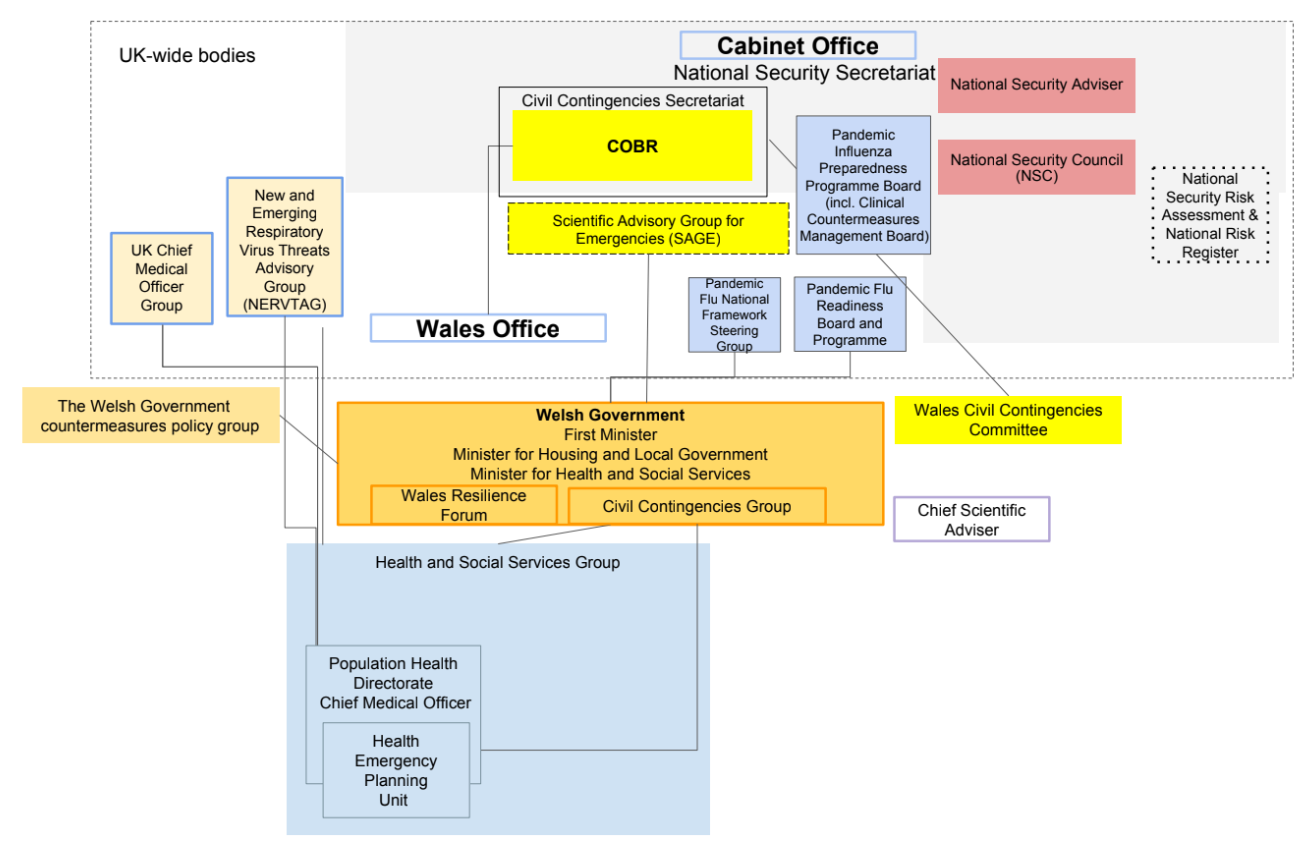
Źródło: wyciąg z INQ000204014
Rysunek 6: Struktury gotowości i reagowania na pandemię w Walii – ok. 2019
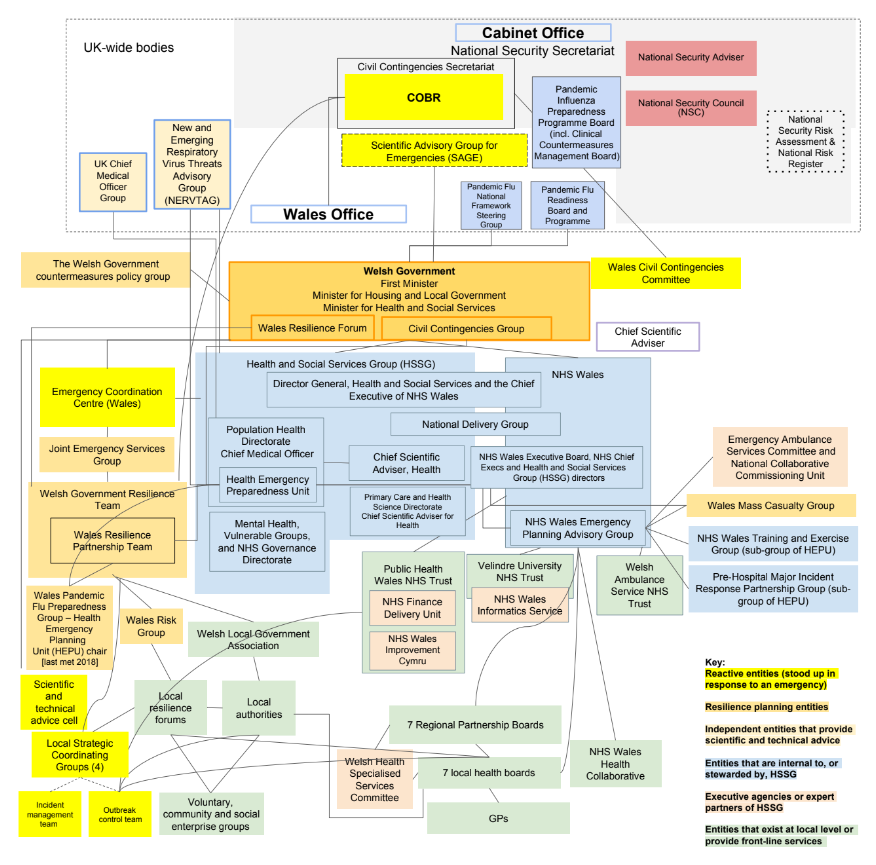
Źródło: wyciąg z INQ000204014
| 2.56. | Pierwszy Minister ponosił ogólną odpowiedzialność za nieprzewidziane sytuacje cywilne i odporność rządu walijskiego131. Stanowiło to znaczące uznanie jego znaczenia. Pod rządami Pierwszego Ministra istniał bardzo skomplikowany zestaw komitetów, zespołów, grup i podgrup, co wskazuje, że rząd walijski nie był tak „kompaktowy” administracja zgodnie z sugestią wynikającą z dochodzenia dr Andrew Goodalla, stałego sekretarza rządu walijskiego od września 2021 r.¹³² |
| 2.57. | W gotowość i odporność zaangażowanych było wiele podmiotów, podzielonych na kilka organów¹³³. Obejmowały one:
|
| 2.58. | Przed pandemią Covid-19 zespół ds. odporności rządu walijskiego znajdował się w Wydziale Bezpieczeństwa Społeczności. Obydwoje byli regularnie przenoszeni w ramach rządu walijskiego: pierwotnie pracowali w Grupie ds. Zasobów Ludzkich, a następnie w 2011 r. zostali przeniesieni do Grupy ds. Samorządu Lokalnego i Społeczności, a następnie w 2017 r. do Grupy ds. Edukacji i Usług Publicznych.¹⁴³ Zespół ds. odporności rządu walijskiego od czasu pandemii została ponownie zreorganizowana. W 2021 r. został rozszerzony i stał się samodzielnym wydziałem obejmującym sprawy cywilne, bezpieczeństwo narodowe i odporność cybernetyczną, znanym jako Wydział ds. nieprzewidywalnych sytuacji cywilnych i bezpieczeństwa narodowego¹⁴⁴. W 2022 r. został ponownie zreorganizowany. Tym razem Wydział ds. Zagrożeń Cywilnych i Bezpieczeństwa Narodowego został połączony z Wydziałem Bezpieczeństwa Społecznego oraz Wydziałem Odzyskiwania i Ponownego Uruchamiania Covid, tworząc nową Dyrekcję ds. Ryzyka, Odporności i Bezpieczeństwa Społeczności¹⁴⁵. W jej skład wchodziła Wales Pandemic Flu Readiness Group, która została utworzona w celu wdrożyć prace określone przez brytyjską Radę ds. Gotowości na Pandemię Grypy¹⁴⁶ Ten ciągły ruch nie poprawia odporności. |
| 2.59. | Opieka zdrowotna jest prawie w całości zdecentralizowana w Walii.¹⁴⁷ Jednakże w odniesieniu do sytuacji nadzwyczajnych dla ludności konkordat między rządami Wielkiej Brytanii i Walii z 2011 r. w sprawie ustawy o nieprzewidzianych zdarzeniach cywilnych z 2004 r. zapewnił szerokie zasady działania władz nadzwyczajnych w Walii. Podkreśliła współpracę i konsultacje między rządami Wielkiej Brytanii i Walii w sprawie planowania i reagowania w sytuacjach awaryjnych¹⁴⁸ |
| 2.60. | Niezależnie od zakresu podmiotów w Walii rzekomo odpowiedzialnych za gotowość, Sir Frank Atherton, dyrektor medyczny Walii od sierpnia 2016 r., powołał w maju 2018 r. Komitet Doradczy ds. Ochrony Zdrowia. Miał on zgromadzić szereg organizacji zaangażowanych w kwestie ochrony zdrowia. Jego celem była pomoc w zrozumieniu szerokiego spektrum zagrożeń wynikających z chorób zakaźnych – nie powołano wcześniej żadnej innej komisji, która zajmowałaby się takimi zagrożeniami lub zajmowała się kwestiami ochrony zdrowia¹⁴⁹. |
| 2.61. | Dla administracji, która szczyciła się efektywnością działań ze względu na względny brak skali i która opisywała siebie jako działającą skutecznie, „pod jednym dachem”, rzeczywistość nie pasowała do retoryki.¹⁵⁰ System był labiryntowy. Dochodzenie nie zostało przekonane przez złagodzenie zaproponowane przez dr Goodalla, że ma ono większy sens dla osób w systemie niż dla tych poza nim.¹⁵¹ Możliwość stworzenia spójnego, a zatem dynamicznego systemu w Walii została utrudniona przez nadmierną złożoność. |
Fachowe porady medyczne i naukowe
| 2.62. | Rolą dyrektora medycznego Walii było doradzanie rządowi walijskiemu w sprawie polityki zdrowia publicznego. Byli także odpowiedzialni za nadzorowanie Jednostki Planowania na wypadek Sytuacji Zdrowotnych, która odpowiadała za przygotowanie na wypadek pandemii i planowanie awaryjne w ramach Grupy ds. Opieki Zdrowotnej i Usług Społecznych w Walii¹⁵². |
| 2.63. | Główny doradca naukowy w Walii i główny doradca naukowy ds. zdrowia w Walii nie odegrali kluczowej roli w przygotowaniu i odporności na pandemię¹⁵³. |
Koordynowanie działań regionalnych i lokalnych
| 2.64. | Powyżej omówiono różne lokalne struktury ds. awaryjnych rozwiązań cywilnych w Walii. Na wysokim poziomie obejmowały one Wales Resilience Forum, walijskie lokalne fora dotyczące odporności oraz Wales Resilience Team Team.¹⁵⁴ |
| 2.65. | Walijskie lokalne fora ds. odporności skupiają służby ratownicze kategorii 1 i 2 i stanowią główne mechanizmy planowania wieloagencyjnego i współpracy na poziomie lokalnym¹⁵⁵ Podobnie jak w Anglii, cztery lokalne fora ds. odporności w Walii opierają się na obszarach służb policyjnych¹⁵⁶ Lokalne Grupa Koordynatorów Forum Odporności zapewnia również wsparcie i dzieli się wiedzą na lokalnych forach poświęconych odporności.¹⁵⁷ |
| 2.66. | Zespół Partnerstwa Walii na rzecz Odporności to grupa działająca pod Forum ds. Odporności Walii. Wspiera je, zapewniając usługi sekretariatu i polityki oraz operacjonalizację niektórych działań omawianych na Wales Resilience Forum¹⁵⁸ |
| 2.67. | Rząd walijski kieruje koordynacją obejmującą całą Walię i pełni rolę wspierającą lokalne fora na rzecz odporności.¹⁵⁹ Wales Resilience Forum to struktura w ramach Rząd walijski, któremu przewodniczy Pierwszy Minister i obejmuje reprezentację wszystkich partnerów wieloagencyjnych, w tym lokalnych forów na rzecz odporności, Walijskiego Stowarzyszenia Samorządów Lokalnych, Stowarzyszenia Dyrektorów Generalnych Władz Lokalnych (Solace) Cymru i Public Health Wales.¹⁶⁰ Wales Resilience Forum zapewnia strategiczne wytyczne i porady sektorom publicznym i lokalnym forom dotyczącym odporności w kwestiach nie ograniczających się do zdrowia i jest organem doradczym, a nie strategicznym decyzyjnym.¹⁶¹ |
| 2.68. | Chris Llewelyn, dyrektor naczelny Walijskiego Stowarzyszenia Samorządów Lokalnych od stycznia 2019 r., powiedział w dochodzeniu, że opisane powyżej struktury istnieją i działają skutecznie, ale podczas pandemii Covid-19 należy je uzupełnić innymi rozwiązaniami.¹⁶² Zdaniem Llewelyna zaistniała potrzeba zaangażowania wszystkich partnerów w reformę całego systemu lub przeprojektowanie ustaleń.¹⁶³ |
| 2.69. | W raporcie Wales Audit Office z grudnia 2012 r. na temat nieprzewidzianych wypadków cywilnych w Walii stwierdzono:
|
| 2.70. | Obserwacje te sprawdziły się zarówno w 2020 r., kiedy pandemia Covid-19 nawiedziła Walię, jak i w momencie pisania raportu w 2012 r. W międzyczasie rząd walijski niewiele zrobił, aby uprościć, usprawnić i zracjonalizować podmioty odpowiedzialne za kierowanie i administrowanie gotowością na wypadek sytuacji kryzysowych w Walii. |
Irlandia Północna
Władze Irlandii Północnej i organizacje wspierające
Rysunek 7: Centralne struktury wykonawcze dotyczące gotowości i reagowania na pandemię w Irlandii Północnej – ok. 2019
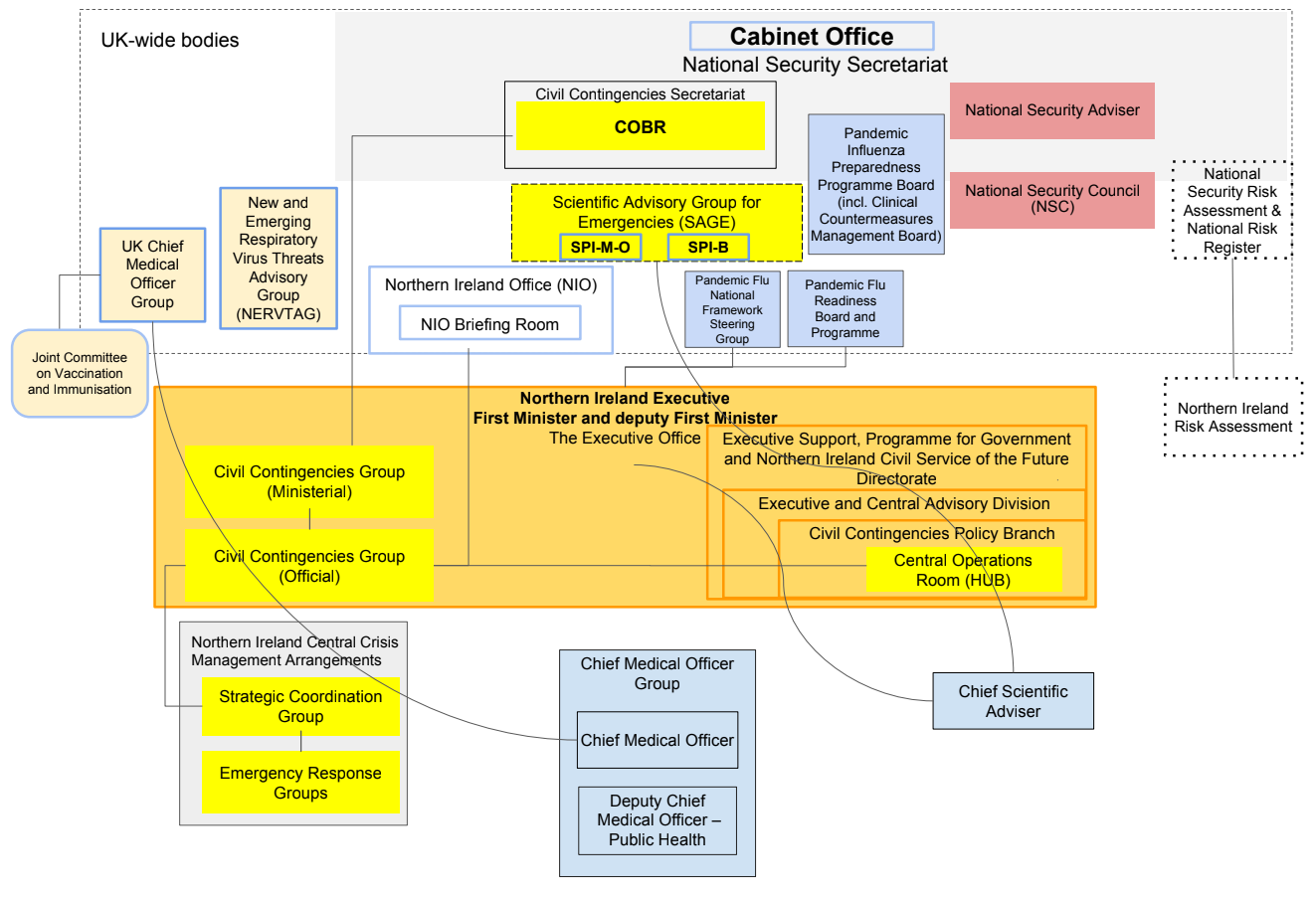
Źródło: wyciąg z INQ000204014
Rysunek 8: Struktury gotowości i reagowania na pandemię w Irlandii Północnej – ok. 2019
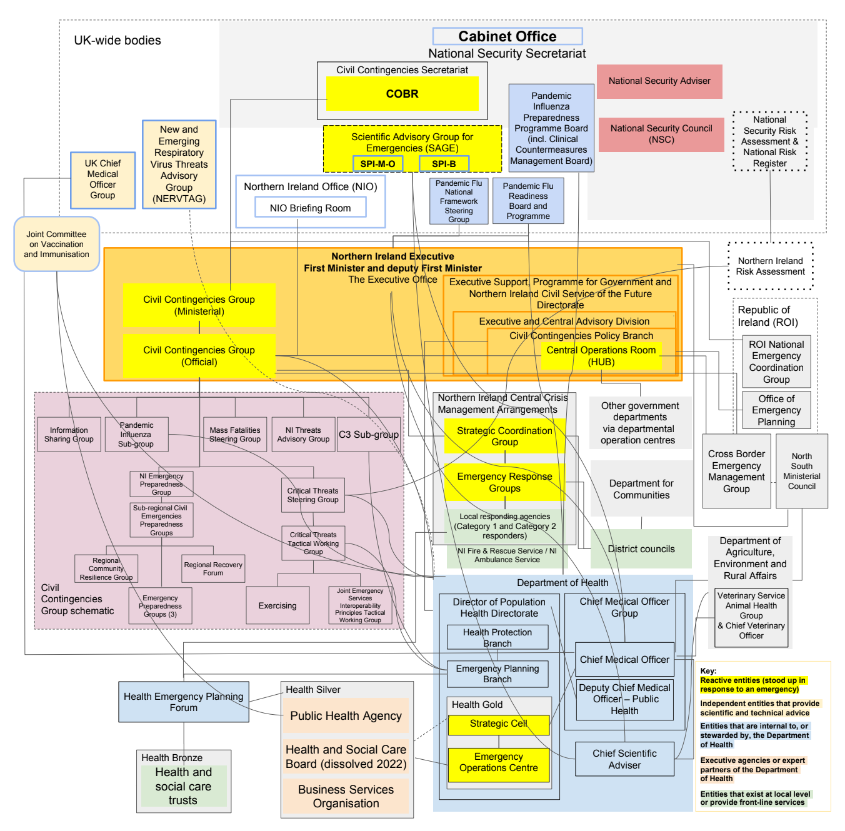
Źródło: wyciąg z INQ000204014
| 2.71. | Polityka i ustawodawstwo dotyczące nieprzewidzianych sytuacji cywilnych oraz ich realizacja w Irlandii Północnej są na ogół sprawami zdecentralizowanymi¹⁶⁷ Zwyczaje i praktyka w Irlandii Północnej miały pozostać w szerokim zakresie zgodne z polityką i najlepszymi praktykami pozostałej części Wielkiej Brytanii.¹⁶⁸ Ustawa o nieprzewidzianych sytuacjach cywilnych Rok 2004 ma zastosowanie tylko częściowo do Irlandii Północnej.¹⁶⁹ Opieka zdrowotna i społeczna to kwestie przekazane, za które odpowiedzialność ponosi władza wykonawcza Irlandii Północnej.¹⁷⁰ |
| 2.72. | Biuro Wykonawcze (którego nadrzędnym celem jest wspieranie Urzędu Wykonawczego Irlandii Północnej) stanowiło serce rządu Irlandii Północnej i ponosiło główną odpowiedzialność polityczną za nieprzewidziane sytuacje cywilne.¹⁷¹ Nie ma jednak uprawnień do kierowania ani kierowania kontrolować wszelkie inne departamenty lub ich agencje.¹⁷² Pod tym względem Biuro Wykonawcze jest cechą unikalnych ustaleń konstytucyjnych Irlandii Północnej. Jego rolą była koordynacja działań pomiędzy departamentami władz wykonawczych Irlandii Północnej. Irlandia Północna również postępowała zgodnie z modelem wiodących departamentów rządowych, przy czym Departament Zdrowia (Irlandia Północna) odpowiadał za przygotowanie na wypadek pandemii¹⁷³. |
| 2.73. | Dwa organy ponoszące główną odpowiedzialność za planowanie pandemii w Irlandii Północnej to:
|
| 2.74. | Istniało jednak wiele innych grup, podgrup, szczebli i podgrup, a także reorganizacji i rebrandingu.¹⁷⁶ W rezultacie system w Irlandii Północnej stał się nadmiernie skomplikowany.¹⁷⁷ |
| 2.75. | W latach 2015–2020 struktury rezerw cywilnych przeszły poważną reformę. W Irlandii Północnej nadal występowało coraz więcej podmiotów.¹⁷⁸ Należą do nich:
|
| 2.76. | Dr Denis McMahon, stały sekretarz Biura Wykonawczego Irlandii Północnej od lipca 2021 r., utrzymywał w trakcie dochodzenia, że pomimo pozornego pozoru złożoności, sytuacja była prostsza w praktyce:
„Jednym z wyzwań i zalet Irlandii Północnej jest to, że wszyscy się znają, to małe miejsce, więc można wszystkich zaprosić do sali w tym samym czasie.”¹⁸² |
| 2.77. | Na pytanie, czy system, choć może być skomplikowany, był skuteczny, dr McMahon przedstawił w dochodzeniu następujące dowody: „ogólnie to zadziałało dobrze”, ale przypisał to w pewnym stopniu „osobiste przywództwo.¹⁸³ Przestrzegał przed radykalnymi reformami w Irlandii Północnej, gdyż obawiał się, że nie zniweczy „lata warunkowania” osób pracujących przy planowaniu sytuacji awaryjnych.¹⁸⁴ The Inquiry wykazuje dla tego większe zrozumienie w Irlandii Północnej niż gdziekolwiek indziej w Wielkiej Brytanii, ale nie oznacza to, że system nie powinien podlegać uproszczeniu i racjonalizacji. |
| 2.78. | Profesor Sir Michael McBride, dyrektor medyczny Irlandii Północnej od września 2006 r., nie wierzył, że to złożoność struktur jest przyczyną nieskuteczności osób pracujących w ramach przygotowania na wypadek sytuacji kryzysowych i planowania. Chodziło, jak stwierdził, bardziej o „funkcjonować" - tj "dla osób pracujących w systemie, które muszą wiedzieć, jak działają te struktury, wiemy, jak te struktury działają i jak są ze sobą powiązane”.¹⁸⁵ Niemniej jednak należy preferować prostotę – która tworzy bardzo jasne granice odpowiedzialności – zamiast rozproszenia wielu grup i ryzyka niemożności zlokalizowania osób odpowiedzialnych za wykonanie pracy. W dochodzeniu zauważono również, że w następstwie przeglądu struktury Grupy Dyrektora Medycznego w 2021 r. utworzono samodzielną Dyrekcję ds. Gotowości, Odporności i Reagowania na sytuacje kryzysowe, co nadało jej pracy większe znaczenie i znaczenie¹⁸⁶. |
Fachowe porady medyczne i naukowe
| 2.79. | Rolą dyrektora medycznego Irlandii Północnej było udzielanie niezależnych, profesjonalnych porad medycznych zarówno Ministrowi Zdrowia, jak i Stałemu Sekretarzowi. Za pośrednictwem Dyrekcji ds. Zdrowia Ludności w Grupie Dyrektorów Medycznych dyrektor ds. medycznych w Irlandii Północnej (wyjątkowo w Wielkiej Brytanii) był odpowiedzialny za planowanie i przygotowanie na skutki zdrowotne sytuacji kryzysowych, w tym wybuchy chorób zakaźnych i pandemie¹⁸⁷. |
| 2.80. | W Irlandii Północnej było dwóch głównych doradców naukowych (jeden w Departamencie Zdrowia (Irlandia Północna), a drugi w Departamencie Rolnictwa, Środowiska i Spraw Wiejskich), ale wcześniej nie było głównego głównego doradcy ds. naukowych Zarządu Irlandii Północnej. na pandemię.¹⁸⁸ Profesor McBride uznał to za „wrodzoną słabość” systemu¹⁸⁹ W dochodzeniu powiedziano, że Biuro Wykonawcze Irlandii Północnej stara się wypełnić tę lukę.¹⁹⁰ |
Zawieszenie ustaleń dotyczących podziału władzy
| 2.81. | Ustalenia dotyczące zarządzania Irlandią Północną zawarte są w ustawie o Irlandii Północnej z 1998 r. Ustawa ta wprowadza w życie ustalenia konstytucyjne zawarte w Porozumieniu z Belfastu z 1998 r. (znanym jako Porozumienie Wielkopiątkowe). Zapewnia wybrane zgromadzenie posiadające władzę ustawodawczą i wykonawczą w sprawach zdecentralizowanych. Władzę wykonawczą sprawują w imieniu Zgromadzenia Irlandii Północnej Pierwszy Minister, Zastępca Pierwszego Ministra i ministrowie pełniący obowiązki departamentalne. Stanowiska ministerialne przydzielane są zgodnie z siłą partii w Zgromadzeniu Irlandii Północnej. Ministrowie stanowią Komitet Wykonawczy. W przypadku braku ustaleń dotyczących podziału władzy za codzienne funkcjonowanie rządu w Irlandii Północnej odpowiadają wyżsi urzędnicy służby cywilnej w Irlandii Północnej. Jednakże istnieją w tym istotne ograniczenia. Na przykład w przypadku braku funkcjonującego Zgromadzenia Irlandii Północnej departamenty nie mogą proponować ustawodawstwa pierwotnego ani funkcji udzielających absolutorium powierzonych specjalnie ministrom. Tak było w okresie od stycznia 2017 r. do stycznia 2020 r.191 |
| 2.82. | Sir David Sterling, szef służby cywilnej Irlandii Północnej i stały sekretarz biura Irlandii Północnej w latach 2017–2020, powiedział w trakcie dochodzenia, że brak funkcjonującego rządu ma trzy główne skutki dla służby cywilnej w Irlandii Północnej.192 Były to następujące:
Pogląd ten podzielał dr McMahon, następca Sir Davida Sterlinga od lipca 2021 r., a także Robin Swann MLA, minister zdrowia Irlandii Północnej w okresie od stycznia 2020 r. do października 2022 r.196 Profesor McBride powiedział, że „istniejeabsolutnie bez wątpienia”, że nieobecność ministrów „znaczący wpływ” na temat zdolności Irlandii Północnej do inicjowania lub rozwijania nowej polityki.197 |
| 2.83. | Trzyletnia przerwa nastąpiła wkrótce po opublikowaniu w 2016 r. dwóch sprawozdań w sprawie znaczących reform systemów opieki zdrowotnej i społecznej w Irlandii Północnej opracowanych przez panel ekspertów i Departament Zdrowia (Irlandia Północna).198 Bez funkcjonującego rządu nie można byłoby zastosować się do zaleceń zawartych w tych raportach.199 Ponadto ograniczona została możliwość podejmowania jakichkolwiek długoterminowych decyzji strategicznych, ponieważ finansowanie ustalano w oparciu o jednoroczny budżet powtarzalny.200 Pan Swann powiedział w dochodzeniu, że „możliwości… zostały zdecydowanie utracone" w tym okresie.201 |
| 2.84. | Oczywiste jest, że problemy strukturalne w Irlandii Północnej w zakresie przygotowań na pandemię Covid-19 zaostrzyły się w wyniku zawieszenia ustaleń dotyczących podziału władzy. W dochodzeniu rozważa się długoterminowy wpływ zawieszenia podziału władzy na reakcję Irlandii Północnej na pandemię w module 2C. Jest to jednak ważny kontekst dla rozważenia gotowości i odporności instytucji w Irlandii Północnej. |
Irlandia Północna i Republika Irlandii
| 2.85. | Ponieważ Irlandia Północna i Republika Irlandii dzielą wyspę i granicę lądową, pod względem epidemiologicznym uważa się je za jedną całość.202 W ramach ustaleń dotyczących wspólnego obszaru podróżowania istnieje swobodny przepływ osób między Irlandią Północną, Wielką Brytanią i Republiką Irlandii.203 Kiedy wybuchła pandemia, liczba przypadków i ich rozprzestrzenianie się w Irlandii Północnej często bardziej odpowiadały Republice Irlandii niż pozostałej części Wielkiej Brytanii.204 Uznaje się zatem znaczenie współpracy między rządami i urzędnikami Wielkiej Brytanii, Irlandii Północnej i Republiki Irlandii.205 |
| 2.86. | Istnieje szereg organów ułatwiających tę współpracę, w tym: Rada Ministerialna Północ Południe, w której skład wchodzą ministrowie władzy wykonawczej Irlandii Północnej i rządu irlandzkiego; Wspólny Sekretariat, w którym pracują urzędnicy z Biura Wykonawczego i irlandzkiej służby cywilnej; oraz Transgraniczna Grupa ds. Zarządzania Kryzysowego dla służb ratowniczych.206 Ze względu na zawieszenie ustaleń dotyczących podziału władzy w latach 2017–2020 nie odbyło się około 46 posiedzeń Rady Ministerialnej Północ-Południe.207 Wspólny Sekretariat i Transgraniczna Grupa ds. Zarządzania Kryzysowego w dalszym ciągu funkcjonowały w tym okresie, ale nie można było podjąć żadnych obszarów wymagających decyzji ministerialnych – na przykład w odniesieniu do finansowania.208 |
| 2.87. | Podkreśla to znaczenie współpracy między rządami i urzędnikami Wielkiej Brytanii, Irlandii Północnej i Republiki Irlandii.209 Kwestia ta jest szerzej rozważana w module 2C zapytania. |
Usprawnienie systemu gotowości i odporności
| 2.88. | Liczba organizacji w Wielkiej Brytanii odpowiedzialnych za gotowość na wypadek pandemii wzrosła z biegiem czasu, stając się niepotrzebnie liczna i złożona. Obowiązki w rządzie Wielkiej Brytanii i zdecentralizowane administracje i organizacje je wspierające powielały się, były rozproszone i delegowane na zbyt dużą odległość od ministrów i urzędników wyższego szczebla, aby umożliwić ich skuteczny nadzór. Nikt, kto składał zeznania w dochodzeniu, nie był w stanie przedstawić merytorycznego uzasadnienia systemu, który był nadmiernie złożony i labiryntowy. Jedyną obroną przed taką złożonością był fakt, że system był ogólnie dobrze zrozumiany przez tych, którzy musieli w nim pracować.210 Złożoność spowodowała jednak szereg problemów. |
| 2.89. | Po pierwsze, system był nieefektywny. Zbyt wiele podmiotów, grup, podgrup, komitetów i podkomitetów zaangażowanych w kwestię gotowości i odporności. Prace wykonywało jednocześnie kilka podmiotów. Jak wynika z „diagramów spaghetti” i podmiotów opisanych powyżej, istniała duża liczba instytucji, struktur i systemów, które miały rządzić i działać w celu przygotowania i budowania odporności w całej Wielkiej Brytanii, a mimo to ich role pokrywały się oraz brak jasności co do podziału obowiązków. |
| 2.90. | Po drugie, pojawiły się zasadnicze luki, które nie zostały zidentyfikowane przez rządy, urzędników wyższego szczebla i organizacje wspierające. System miał skłonność do działania w silosach. Nie dokonano przeglądu całości systemu i w niewystarczającym stopniu poświęcono zasypaniu luki między grupami odpowiedzialnymi za program dotyczący chorób zakaźnych o poważnych konsekwencjach a grupami rozważającymi pandemię grypy, aby sprawdzić, czy pewne aspekty programu będą przydatne w kontrolowaniu rozprzestrzeniania się wirusa potencjalna pandemia.211 Jako przykład systemowego problemu działania w silosach pani Reed podała w dochodzeniu, że do jej kompetencji należy ochrona zdrowia, bezpieczeństwo zdrowotne i gotowość na wypadek pandemii. Chociaż było to szerokie portfolio w odniesieniu do gotowości na wypadek pandemii, powiedziała:
„Nie było ze mną dyskusji na temat kwarantanny… Nie było ze mną dyskusji na temat śledzenia i śledzenia.”212 |
| 2.91. | Zapytana, czy w ogóle toczyła się debata na temat możliwej konieczności zamknięcia granic, samoizolacji lub indywidualnych, masowych lub obowiązkowych kwarantann – czy w ogóle czegokolwiek w tym rodzaju – pani Reed powiedziała w dochodzeniu, że nie jest jej świadoma „żadnych rozmów na temat tych obszarów łagodzenia”.213 Ten brak integracji był symptomatyczny dla systemu, który ostatecznie stał się zbyt złożony i chaotyczny. |
| 2.92. | Po trzecie zabrakło koncentracji. Wynikało to z braku jasnego przywództwa i nadzoru zarówno ze strony ministrów, jak i urzędników. W Wielkiej Brytanii systemy stały się nadmiernie biurokratyczne. Zamiast skupiać się na umiejętnościach, technologii i infrastrukturze, skupiono się na tworzeniu grup, podgrup i dokumentów. W wyniku rozwiązania Podkomisji ds. Zagrożeń, Niebezpieczeństw, Odporności i Sytuacji Nieprzewidzianych, jeden z najważniejszych ryzyk w Wielkiej Brytanii nie sprawował stałego nadzoru ministerialnego.214 Skutek był taki, że gotowość i odporność nie były sprawdzane na najwyższych szczeblach władzy. |
| 2.93. | Weźmy jeden przykład: Public Health England miało własny Departament Reagowania Kryzysowego, który podlegał Dyrekcji Ochrony Zdrowia. Istniały zespoły, które wspierały prace przygotowawcze Public Health England. Należą do nich zespół starszych doradców medycznych, zespół ds. odporności korporacyjnej, zespół szkoleniowy, zespół ćwiczący, zespół zajmujący się obliczeniami naukowymi, zespół ds. nauk behawioralnych i analiz behawioralnych, zespół ds. systemów informacji geograficznej, zespół ds. modelowania matematycznego i zespół ds. chorób przenoszonych przez wektory zagrożeń i zespół entomologii medycznej.215 Zespoły te stanowiły uzupełnienie Rady Programowej ds. Gotowości na Pandemię Grypy i Rady ds. Gotowości na Pandemię Grypy. Pomimo liczby tych zespołów, grup i podgrup Departament Zdrowia i Opieki Społecznej nie zapewnił, że zbiorowo lub indywidualnie wykazywały stałą zdolność do przygotowania się na katastrofy zdrowotne na dużą skalę, zapobiegania im i reagowania na nie. Osiągnięto to dopiero dzięki utworzeniu brytyjskiej Agencji Bezpieczeństwa Zdrowia w październiku 2021 r.216 |
| 2.94. | Właściwą gotowość i odporność mogą zapewnić jedynie systemy (na szczeblu Wielkiej Brytanii oraz w każdym rządzie lub administracji), które są usprawnione, lepiej zintegrowane i bardziej skoncentrowane na celach, które należy osiągnąć. Systemy należy uprościć i ponownie skalibrować, aby lepiej odpowiadały potrzebom osób niezbędnych do przygotowania się na sytuacje kryzysowe i reagowania na nie, a osoby za nie odpowiedzialne muszą być bardziej odpowiedzialne. Instytucje powinny zadbać o to, aby ich części składowe komunikowały się skuteczniej, aby identyfikowano wady i uzupełniano luki oraz aby osoby udzielające pomocy nie były przytłoczone niepotrzebną biurokracją i skomplikowaną polityką. Ogólnie rzecz biorąc, powinno być mniej podmiotów, które ściślej ze sobą współpracują i w ramach jaśniej określonych ról. |
| 2.95. | Ministrowie i urzędnicy powinni zapewnić skuteczniejsze przywództwo i nadzór. Przed pandemią Covid-19 w rządzie Wielkiej Brytanii ani w zdecentralizowanych administracjach nie było kierownictwa ministerialnego, które mogłoby rozważać strategię, kierować polityką i podejmować decyzje w całym rządzie w celu przygotowania się na sytuacje kryzysowe cywilne obejmujące cały system i budowania odporności na nie. Nie istniała żadna brytyjska ani równoważna komisja ds. gotowości i odporności na sytuacje kryzysowe, która kierowałaby, nadzorowała i koordynowała system. |
| 2.96. | Potrzebna jest stała grupa ministrów w rządzie Wielkiej Brytanii i każdej ze zdecentralizowanych administracji, skupiona na gotowości i odporności na cywilne sytuacje kryzysowe obejmujące cały system. Pojedyncza komisja ministerialna na szczeblu gabinetu i jedna międzyresortowa grupa urzędników wyższego szczebla powinny tworzyć podstawową strukturę kierowniczą w całej Wielkiej Brytanii. Należy powołać międzyresortową grupę urzędników wyższego szczebla, aby po pierwsze przeprowadziła przegląd w celu uproszczenia obecnego systemu, a następnie, po drugie, nadzorowała wdrażanie polityki w ramach uproszczonej struktury i zapewniała jej przywództwo. Ustalenia konstytucyjne w Irlandii Północnej nie pozwalają Biuru Wykonawczemu kierować pracą innych departamentów, a rekomendowanie zmian w tych ustaleniach wykracza poza kompetencje niniejszego Dochodzenia. Jednakże ogólny cel, jakim jest utrzymanie pełnego przeglądu gotowości na wypadek pandemii, ma zastosowanie zarówno w Irlandii Północnej, jak i w pozostałej części Wielkiej Brytanii. |
| 2.97. | W grudniu 2022 r. wraz z publikacją Ramy odporności rządu Wielkiej Brytaniirząd Wielkiej Brytanii ogłosił, że częścią rozwiązania problemu braku przywództwa będzie utworzenie podkomitetu Ministrów Bezpieczeństwa Narodowego (odporność).217 Kieruje nim Kanclerz Księstwa Lancaster (stanowisko na szczeblu gabinetu w Urzędzie Rady Ministrów), a w jej skład wchodzą: Kanclerz Skarbu; Sekretarze Stanu ds. Departamentu Spraw Wewnętrznych, Obrony i Wyrównania, Mieszkalnictwa i Społeczności; Minister ds. Stosunków Międzyrządowych; oraz Minister Gabinetu i Generalny Płatnik.218 Jednak obecnie nie obejmuje Sekretarza Stanu ds. Zdrowia i Opieki Społecznej. W dochodzeniu zalecono, aby Sekretarz Stanu ds. Zdrowia i Opieki Społecznej został mianowany stałym członkiem, ponieważ jest prawdopodobne, że jakakolwiek sytuacja nadzwyczajna w całym systemie będzie miała konsekwencje dla zdrowia i opieki społecznej. Według posła Olivera Dowdena, sekretarza parlamentarnego w Gabinecie Rady Ministrów od stycznia 2018 r. do lipca 2019 r. i ministra ds. Gabinetu od lipca 2019 r. do lutego 2020 r., Podkomisja ds. Odporności jest w stanie podejmować decyzje w całym rządzie. Różnica między nieistniejącym już Podkomitetem ds. Zagrożeń, Niebezpieczeństw, Odporności i Sytuacji Nieprzewidzianych a Podkomitetem ds. Odporności polega na tym, że ta ostatnia ma obecnie rozważyć, w pierwszej kolejności, w jaki sposób zapobiegać materializacji ryzyka.219 |
| 2.98. | Reorganizacje mogą potencjalnie osłabić gotowość i odporność, jeżeli wiążą się z częstym przemieszczaniem grup ministrów i urzędników wokół istniejących instytucji. Dochodzenie niechętnie zaleca zatem kolejną zmianę. Utworzenie podstawowej struktury przywództwa i nadzoru powinno jednak spowodować zmiany w systemach gotowości i odporności, które prowadzą do trwałych, a nie tylko przejściowych ulepszeń. Po pierwsze, jednym z głównych celów takiej podstawowej struktury powinna być racjonalizacja i usprawnienie liczby grup i komitetów odpowiedzialnych za gotowość i odporność cywilną na wypadek sytuacji kryzysowych całego systemu – powinny pozostać tylko te, które mają jasno określony cel. Po drugie, to podstawowe struktury będą ostatecznie odpowiedzialne za zapewnienie skuteczności i gotowości systemów gotowości i odporności na następną pandemię. Powinno to zachować powagę i skupić się na znaczeniu ich ról i obowiązków. |
Zalecenie 1: Uproszczona struktura gotowości i odporności cywilnej całego systemu na wypadek sytuacji kryzysowych
Rządy Wielkiej Brytanii, Szkocji, Walii i Irlandii Północnej powinny uprościć i zmniejszyć liczbę struktur odpowiedzialnych za przygotowanie i budowanie odporności na cywilne sytuacje kryzysowe obejmujące cały system.
Podstawowe struktury powinny być:
- pojedynczy komitet ministerialny na szczeblu gabinetu lub równoważny komitet ministerialny (w tym starszy minister odpowiedzialny za zdrowie i opiekę społeczną) odpowiedzialny za gotowość i odporność cywilną całego systemu na wypadek sytuacji kryzysowych w przypadku każdego rządu, który spotyka się regularnie i któremu przewodniczy lider lub zastępca lidera odpowiedniego rząd; I
- pojedyncza międzyresortowa grupa urzędników wyższego szczebla w każdym rządzie (która regularnie składa sprawozdania Radzie Ministrów lub równoważnej komisji ministerialnej) w celu nadzorowania i wdrażania polityki w zakresie gotowości i odporności cywilnej na sytuacje kryzysowe.
Należy to wdrożyć w ciągu 12 miesięcy od opublikowania niniejszego Sprawozdania.
W ciągu 6 miesięcy od utworzenia grupy urzędników wyższego szczebla powinna ona zakończyć przegląd mający na celu uproszczenie i zmniejszenie liczby struktur odpowiedzialnych za ogólnosystemową gotowość i odporność cywilną na sytuacje kryzysowe.
Następnie, w ciągu 24 miesięcy od publikacji niniejszego Raportu, komisja ministerialna powinna zracjonalizować i usprawnić podległe lub wspierające grupy i komitety odpowiedzialne za gotowość i odporność cywilną całego systemu. Wszelkie grupy i komitety powołane lub utworzone w celu wspierania tej podstawowej struktury powinny mieć jasny cel i powinny regularnie składać sprawozdania na temat postępów w realizacji powierzonych im zadań i ich zakończenia.
Wiodący model departamentu rządowego zajmujący się cywilnymi sytuacjami kryzysowymi w całym systemie
| 2.99. | Kiedy wybuchła pandemia Covid-19, w praktyce to premier, 10 Downing Street i Gabinet przejęli kierownictwo nad całym brytyjskim rządem, koordynując reakcję kryzysową między departamentami i agencjami rządowymi.220 Uznaje się, że Gabinet Rady Ministrów, posiadający władzę premiera, ma uprawnienia do kierowania innymi departamentami rządowymi i organizacjami wspierającymi, aby współpracowały w odpowiedzi na cywilne sytuacje kryzysowe obejmujące cały system. Jednakże to Departament Zdrowia i Opieki Społecznej – który oczywiście ma znaczący udział w każdej sytuacji zagrożenia zdrowia – był i pozostaje głównym departamentem rządowym ds. gotowości i odporności na pandemię w Anglii. |
| 2.100. | Obecne podejście wiąże się z wieloma istotnymi problemami. |
| 2.101. | Po pierwsze, ryzyko jest przydzielane poszczególnym departamentom rządowym, niezależnie od tego, czy może ono spowodować sytuację nadzwyczajną w całym systemie. Istnieją w tym zakresie wyraźne ograniczenia. Chociaż za pandemie odpowiada Departament Zdrowia i Opieki Społecznej, jasne jest, że mogą one wywołać kryzysy społeczne i gospodarcze, które wymagają szerszej reakcji ze strony większej liczby instytucji na szczeblu krajowym, regionalnym i lokalnym – wymagają zdolności całego systemu rządów. Sir Oliver Letwin uważał, że pojedynczy departament rządowy nie może „władać” ryzykiem cywilnym związanym z całym systemem.221 Zapytanie zgadza się. |
| 2.102. | Po drugie, sytuacja nadzwyczajna cywilna obejmująca cały system, taka jak pandemia, z definicji wymaga podejścia międzyresortowego. Skala koordynacji, kierowania i przewodzenia w zakresie gotowości i odporności we wszystkich departamentach rządu Wielkiej Brytanii jest tak szeroka, a zadanie tak złożone, że trudno sobie wyobrazić, aby jakikolwiek pojedynczy departament był w stanie samodzielnie sobie z tym poradzić, zwłaszcza w połączeniu z obowiązkami którymi departamenty dysponują do codziennego zarządzania. |
| 2.103. | Po trzecie, w ramach przygotowań na sytuacje nadzwyczajne dla ludności obejmujące cały system, w przeciwieństwie do innych sytuacji nadzwyczajnych dla ludności, każda polityka i decyzja wiąże się ze znacznymi kompromisami i kompromisy. Na przykład, gdyby Departament Zdrowia i Opieki Społecznej uznał, że skuteczną polityką poprawy gotowości na wypadek pandemii byłaby budowa infrastruktury bezpieczeństwa zdrowotnego na granicy, musiałby skierować to do Ministerstwa Spraw Wewnętrznych. Inne departamenty, takie jak Ministerstwo Spraw Zagranicznych, Wspólnoty Narodów i Rozwoju oraz Departament Biznesu i Handlu, mogą przyjąć inny, ale nadal rozsądny pogląd na temat celów i możliwych wyników polityki. Podobnie, jeśli Departament Zdrowia i Opieki Społecznej uzna, że skuteczna polityka gotowości na wypadek pandemii wymaga znacznego wsparcia ekonomicznego dla osób fizycznych i przedsiębiorstw w Wielkiej Brytanii, Ministerstwo Skarbu może mieć uzasadnione obawy fiskalne. Ministerstwo Zdrowia i Opieki Społecznej nie jest w stanie rozwiązać tych problemów. |
| 2.104. | Po czwarte, budowanie gotowości i odporności na sytuacje kryzysowe cywilne obejmujące cały system wymaga współpracy między rządami, departamentami rządowymi i dyrekcjami w całej Wielkiej Brytanii. Dzieje się tak dlatego, że mają one miejsce poza granicami wewnętrznymi Wielkiej Brytanii. Dlatego też w ramach przygotowań na wydarzenia takie jak pandemia konieczne jest, aby departament w centrum brytyjskiego rządu, który jest w stanie koordynować działania ze zdecentralizowanymi administracjami, był odpowiedzialny za gotowość i odporność. |
| 2.105. | Z dochodzenia wynika, że model wiodących departamentów rządowych zasadniczo nie nadaje się do przygotowywania się na sytuacje kryzysowe dla ludności obejmujące cały system, takie jak pandemie, i budowania odporności na nie. Wymogi ostrych kryzysów, które jednocześnie stawiają wymagania całemu brytyjskiemu rządowi i zdecentralizowanej administracji, wymagają innego podejścia. Dlatego konieczne jest powierzenie obowiązków jedynemu departamentowi rządowemu, który ma władzę i uprawnienia niezbędne do przejęcia przywództwa – Gabinetowi Rady Ministrów. Posiada władzę decyzyjną Prezesa Rady Ministrów oraz nadzór i zdolność koordynowania działań całego rządu. |
| 2.106. | Rząd Wielkiej Brytanii przyznał, że model wiodących departamentów rządowych ma swoje ograniczenia:
|
| 2.107. | Proponowane obecnie rozwiązania nie idą wystarczająco daleko, ponieważ poszczególne departamenty rządowe w dalszym ciągu odpowiadają za gotowość i odporność na przypisane im ryzyka. Konieczna jest radykalna zmiana systemu. |
| 2.108. | Należy uznać ograniczenia możliwości departamentów, takich jak Departament Zdrowia i Opieki Społecznej, w zakresie koordynowania i kierowania polityką w całym rządzie. Należy znieść model wiodącego departamentu rządowego w zakresie przygotowania i budowania odporności na cywilne sytuacje kryzysowe w całym systemie. |
| 2.109. | Biuro Rady Ministrów powinno w imieniu rządu Wielkiej Brytanii przejąć wiodącą rolę w monitorowaniu gotowości i odporności innych departamentów, wspieraniu departamentów w rozwiązywaniu problemów i przekazywaniu problemów komisji na szczeblu gabinetu Wielkiej Brytanii oraz grupie urzędników wyższego szczebla, zgodnie z zaleceniami zawartymi w niniejszym Raporcie . W przypadku tego typu sytuacji nadzwyczajnych komisja na szczeblu gabinetu i grupa urzędników wyższego szczebla powinni następnie zapewnić międzyrządowe podejście do zagrożeń, które prawdopodobnie będą miały największy wpływ na Wielką Brytanię. |
| 2.110. | Celem powinna być współpraca wszystkich departamentów rządowych w celu przygotowania się na cywilne sytuacje kryzysowe obejmujące cały system w taki sam sposób, w jaki mają one współpracować w przypadku reagowania. W obecnym systemie nie da się tego osiągnąć. |
Zalecenie 2: Kierowanie Gabinetem Rady Ministrów w przypadku katastrof cywilnych obejmujących cały system w Wielkiej Brytanii
Rząd Wielkiej Brytanii powinien:
- znieść model wiodących departamentów rządowych w zakresie gotowości i odporności cywilnej całego systemu na wypadek sytuacji kryzysowych; I
- wymagać od Gabinetu Rady Ministrów kierowania przygotowaniami i budowaniem odporności na sytuacje kryzysowe cywilne w całym systemie we wszystkich departamentach rządu Wielkiej Brytanii, w tym monitorowaniem gotowości i odporności innych departamentów, wspieraniem departamentów w rozwiązywaniu problemów oraz eskalacją problemów do komisji ministerialnej na szczeblu gabinetu Wielkiej Brytanii oraz grupa urzędników wyższego szczebla w Zaleceniu 1.
| 2.111. | Model wiodących departamentów rządowych ma zastosowanie również w Irlandii Północnej. Biorąc pod uwagę uregulowanie konstytucyjne w Irlandii Północnej, dochodzenie nie zaleciło formalnej zmiany ustaleń, niemniej jednak należy rozważyć wprowadzenie w życie tego zalecenia w świetle kwestii zidentyfikowanych w niniejszym Raporcie. |
- INQ000204014
- INQ000196611_0005 ust. 1
- INQ000196611_0011 ust. 22
- INQ000196611_0012 ust. 22
- INQ000196611_0011-0012 ust. 22
- INQ000196611_0024, 0031 pkt 60, 78
- INQ000196611_0029-0030 paragraf 74
- INQ000196611_0028-0029 pkt 69–71
- David Heymann 15 czerwca 2023 r. 39.07.-41.15; INQ000195846_0009 ust. 31
- INQ000196611_0032 ust. 83; INQ000195846_0039-0040, 0046 pkt 192–194, 232
- Zobacz definicję „sytuacji nadzwyczajnej” w sekcji 1 ustawy o nieprzewidzianych zdarzeniach cywilnych z 2004 r. (https://www.legislation.gov.uk/ukpga/2004/36/contents)
- INQ000145733_0002 ust. 2.2; INQ000182612_0029 pkt 3.71–3.72; Ramy odporności rządu Wielkiej Brytanii, Rząd Jej Królewskiej Mości, grudzień 2022 r., s. 81–83 (https://www.gov.uk/government/publications/the-uk-government-resilience-framework; INQ000097685)
- Krajowy Rejestr Ryzyka, Rząd Jej Królewskiej Mości, 2023, s. 75–76, 150–155 (https://assets.publishing.service.gov.uk/media/64ca1dfe19f5622669f3c1b1/2023_NATIONAL_RISK_REGISTER_NRR.pdf; INQ000357285); INQ000376140_0010, 0015; Bruce Mann 15 czerwca 2023 155/11-14; Oliver Letwin 20 czerwca 2023 54/2-19
- INQ000177810_0005-0007 pkt 17–18, 20, 22
- Oliver Letwin 20 czerwca 2023 54/19-22
- Ustawa o nieprzewidzianych zdarzeniach cywilnych z 2004 r. (https://www.legislation.gov.uk/ukpga/2004/36/contents); INQ000196532
- INQ000377435; INQ000377436
- INQ000148405_0004 ust. 14
- David Heymann 15 czerwca 2023 42.14-16
- INQ000196611_0024-0027 pkt 62–67; Zobacz też INQ000196611_0022-0024 pkt 50–61
- Charlotte Hammer 14 czerwca 2023 r. 115/12-15
- Na czele Sekretariatu Bezpieczeństwa Narodowego stoi Doradca ds. Bezpieczeństwa Narodowego, który jest starszym doradcą Premiera ds. bezpieczeństwa narodowego (zob. Katharine Hammond 16 czerwca 2023 81/8-20).
- INQ000099517_0010 ust. 2.22
- INQ000145733_0002 ust. 2.2; INQ000099517_0010 ust. 2.22
- INQ000099517_0010 ust. 2.22
- Katharine Hammond 16 czerwca 2023 r. 77/19-78/23; INQ000145733_0010 ust. 2.27
- Katharine Hammond 16 czerwca 2023 r. 20.20-93.13
- INQ000145733 _0011 pkt 3.1-3.2
- INQ000145733_0011 ust. 3.1
- INQ000177808_0002 ust. 4iii
- INQ000177808_0002 ust. 4iii
- INQ000177808_0002 ust. 5
- INQ000145733_0002 ust. 2.2
- Katharine Hammond 16 czerwca 2023 81.17-84.10; INQ000194051_0022 paragraf 93
- Katharine Hammond 16 czerwca 2023 81.17-84.10; INQ000194051_0023 paragraf 95
- INQ000177808_0004 ust. 15
- INQ000177808_0004-0005 pkt 14–22
- INQ000177808_0004 ust. 15
- INQ000177808_0004 ust. 16
- Brytyjska strategia gotowości na pandemię grypy 2011, Departament Zdrowia, listopad 2011 r., pkt 3.27 (https://assets.publishing.service.gov.uk media/5a7c4767e5274a2041cf2ee3/dh_131040.pdf; INQ000102974)
- INQ000177808_0004-0006 pkt 15, 21-23; INQ000177810_0012 paragraf 41
- INQ000128057
- Katharine Hammond 16 czerwca 2023 84/11-85/8; Zobacz też INQ000195845_0013 pkt 3.36
- Katharine Hammond 16 czerwca 2023 85/1-8
- Przed styczniem 2018 r. Departament Zdrowia i Opieki Społecznej nosił nazwę Departamentu Zdrowia. W niniejszym raporcie użyto prawidłowej nazwy departamentu i jego Sekretarza Stanu, zgodnie z odpowiednim okresem. W przypadku odniesień obejmujących okres przed i po styczniu 2018 r. w Raporcie używana jest obecna nazwa.
- Główny Departament Rządu i jego rola – wytyczne i najlepsze praktyki, Gabinet Rady Ministrów, marzec 2004, s. 4, ust. 1 (https://assets.publishing.service.gov.uk/media/5a79b2fded915d07d35b772a/lead-government-departments-role.pdf; INQ000022687)
- INQ000184643_0021 paragraf 101
- INQ000184643_0022 ust. 104
- INQ000184643_0022 ust. 104
- INQ000195847_0004 ust. 21; INQ000184643_0061 paragraf 325
- INQ000145733_0021-0025 pkt 3.33–3.42. Dotyczyło to na przykład Ministerstwa Spraw Wewnętrznych, Skarbu Państwa, Ministerstwa Obrony, Departamentu Edukacji oraz Biura Spraw Zagranicznych, Wspólnoty Narodów i Rozwoju (INQ000184643_0032 pkt 178).
- INQ000195847_0004 ust. 21
- INQ000057649_0001 ust. 1-2
- INQ000148429_0006 ust. 22
- INQ000192268_0012 ust. 44
- INQ000090332_0001
- INQ000192268_0011 paragraf 41
- INQ000090332_0001
- INQ000192268_0011 ust. 43
- INQ000192268_0004 ust. 15
- INQ000148429_0007 ust. 23
- INQ000184643_0022 ust. 106
- INQ000184638_0014 ust. 3.1
- INQ000184638_0011 pkt 2.7-2.8, 2.10
- INQ000148407_0009-0010 ust. 20, 22
- INQ000184643_0025-0026 pkt 122–128; INQ000196611_0020 ust. 45; INQ000184638_0018 ust. 3.14; INQ000207293_0003-0007 pkt 2.1-2.13; INQ000147707_0024 ust. 56; INQ000148429_0064-0065 pkt 256–257. Projekt NERVTAG był poprzedzony przez Naukowy Komitet Doradczy ds. Pandemii Grypy w latach 2008–2014, który z kolei był poprzedzony zarówno Krajowym Panelem Ekspertów ds. Nowych i Pojawiających się Zakażeń w latach 2003–2008, jak i Naukową Grupą Doradczą ds. Pandemii Grypy w latach 2005–2008.
- INQ000184643_0026-0027 pkt 129–132; INQ000196611_0021 ust. 47; INQ000184638_0018 ust. 3.15; INQ000184639_0007 pkt 3.14-3.15; INQ000148429_0063 pkt 250–251
- INQ000184643_0027 pkt 133–137; INQ000196611_0020-0021 ust. 46; INQ000184638_0019 ust. 3.16; INQ000148429_0063-0064 pkt 252–255
- INQ000184643_0027-0028 pkt 138–143; INQ000184638_0019 ust. 3.17
- INQ000184643_0029-0030 pkt 148–159; INQ000184638_0016 pkt 3.9-3.10
- INQ000184643_0030 pkt 160–162; INQ000184638_0017 ust. 3.11
- INQ000184643_0030 pkt 163–165; INQ000184638_0056-0057 pkt 6.33–6.36
- INQ000184643_0030-0031 pkt 166–172; INQ000184638_0019 ust. 3.18
- INQ000184643_0031-0032 pkt 173–176; INQ000184638_0016 pkt 3.7–3.8; INQ000148429_0065 paragraf 258
- INQ000148407_0010 ust. 25
- INQ000148407_0010-0011 pkt 23–24, 28; INQ000147810_0004 ust. 10
- INQ000147810_0004 ust. 7, 9-10
- INQ000148407_0007 pkt 14-17
- INQ000148407_0007 ust. 14; INQ000147810_0003 ust. 5-6
- INQ000148407_0014 pkt 33–35
- INQ000184639_0018 pkt 6.2-6.4
- INQ000184639_0018 pkt 6.2-6.4
- INQ000184639_0018 ust. 6.1
- Jeremy Farrar 29 czerwca 2023 1.11-12.15
- INQ000145733_0007 ust. 2.17
- Od maja 2006 r. do stycznia 2018 r. obecny Departament Wyrównania, Mieszkalnictwa i Społeczności nosił nazwę Departamentu Społeczności i Samorządu Lokalnego. Od stycznia 2018 r. do września 2021 r. funkcjonowało pod nazwą Ministerstwo Mieszkalnictwa, Gmin i Samorządu Terytorialnego. We wrześniu 2021 r. przemianowano go na Departament Wyrównywania Poziomów, Mieszkalnictwa i Społeczności. W raporcie tym użyto prawidłowej nazwy działu zgodnie z odpowiednim okresem czasu. W przypadku odniesień obejmujących okres przed i po wrześniu 2021 r. w Raporcie używana jest obecna nazwa.
- 87 INQ000065107_0012-0013 pkt 33
- Katarzyna Frances 29 czerwca 2023 127/15-132/9
- Mark Lloyd 12 lipca 2023 r. 79/3-7
- Mark Lloyd 12 lipca 2023 r. 79/8-16
- Jim McManus 5 lipca 2023 r. 46/9-14
- Jim McManus 5 lipca 2023 46/15-48/4
- Jim McManus 5 lipca 2023 47/25-48/4
- INQ000183419_0036 paragraf 201
- INQ000183419_0040-0041 pkt 225–230
- Widzieć Kevin Fenton 5 lipca 2023 r. 89/25-90/7; INQ000183419_0017, 0021, 0040-0041 pkt 107–108, 125–126, 225–230; Jim McManus 5 lipca 2023 r. 57/7-58/1; INQ000183419_0019, 0040 paragrafy 118, 225. W Anglii jest około 151 dyrektorów ds. zdrowia publicznego zatrudnionych przez władze lokalne. W Szkocji i Walii odpowiednio 8 i 7 dyrektorów ds. zdrowia publicznego jest zatrudnionych w komisjach ds. zdrowia NHS. W Irlandii Północnej jest tylko jeden dyrektor ds. zdrowia publicznego, który jest zatrudniony przez Agencję Zdrowia Publicznego (patrz Jim McManus 5 lipca 2023 r. 36.16-38.09).
- INQ000205178_0098 paragraf 146
- Roger Hargreaves 22 czerwca 2023 44/2-5
- Oliver Dowden 21 czerwca 2023 134/20-137/2
- INQ000184894_0017 paragraf 61
- INQ000185352_0002 ust. 6
- Przygotowanie Szkocji: Scottish Guidance on Resilience, Rząd Szkocji, 2017, s. 24 (https://ready.scot/sites/default/files/2020-09/preparing scotland-hub-updated-published-version-may-2019-new-hs-diagram.pdf; INQ000102938)
- INQ000102935
- John Swinney 29 czerwca 2023 82/10
- John Swinney 29 czerwca 2023 81.17-83.22
- Gillian Russell 28 czerwca 2023 r., 33/6–14
- John Swinney 29 czerwca 2023 83.12-15
- Przygotowanie Szkocji: Scottish Guidance on Resilience, Rząd Szkocji, 2017 (https://ready.scot/sites/default/files/2020-09/przygotowywanie-scotland-hub-updated-published-version-may-2019-new-hs-diagram.pdf; INQ000102938)
- INQ000184894_0018 paragraf 64
- INQ000185343_0003 ust. 7; INQ000184894_0014, 0018-0019 pkt 49–50, 64
- INQ000185343_0003 ust. 9
- INQ000185343_0006 ust. 19
- INQ000239420_0001-0002, 0006 ust. 4, 6, 29; INQ000184894_0017, 0019 pkt 61, 66
- INQ000239420_0006 ust. 29
- INQ000184894_0006-007 ust. 22
- INQ000185343_0002 ust. 5; INQ000239420_0002 ust. 6; INQ000184894_0017 paragraf 61
- INQ000185343_0007-0008 pkt 24-25
- Jim McMenamin 22 czerwca 2023 174/6-24. W dochodzeniu powiedziano, że wspólna odpowiedzialność wynika z faktu, że zdrowie ludności na poziomie lokalnym było głównym przedmiotem wysiłków Szkocji w zakresie ochrony zdrowia (Jim McMenamin 22 czerwca 2023 178/18-22).
- INQ000184897_0002 ust. 4
- INQ000183410_0015 pkt 1.4.16-1.4.17
- INQ000184897_0003 ust. 6
- INQ000183412_0003 ust. 7-8
- INQ000185342_0002 ust. 4
- INQ000184897_0003 ust. 7
- INQ000184894_0012 paragraf 40
- INQ000184894_0013 paragraf 42
- INQ000184894_0012-0013 pkt 40-43
- INQ000184894_0019 paragraf 69
- INQ000185352_0003 ust. 9
- John Swinney 29 czerwca 2023 84/21-85/25
- INQ000130469_0032-0033 pkt 134
- 132 INQ000130469_0003 ust. 11; zobacz także pkt 80–83; INQ000204014_0009-0012
- Frank Atherton 3 lipca 2023 r., 13.07-12.13
- Quentin Sandifer 4 lipca 2023 r. 67/11-18
- Frank Atherton 3 lipca 2023 r. 40/24-41/9
- INQ000130469_0051 paragraf 193
- INQ000190662_0007 ust. 24; INQ000128975; INQ000130469_0054 paragraf 204
- INQ000107114_0001; INQ000130469_0035, 0054 pkt 144, 204
- INQ000130469_0032 paragraf 133
- INQ000130469_0053-0054 pkt 201–203
- INQ000107116
- INQ000130469_0046 ust. 181; INQ000107115
- INQ000130469_0051 ust. 195; INQ000190662_0008 ust. 27
- INQ000130469_0052 ust. 199; INQ000190662_0023-0024 pkt 84–85
- INQ000130469_0052–0053 ust. 200; INQ000190662_0023-0024 pkt 84–85
- Frank Atherton 3 lipca 2023 r. 40/24-41/9
- INQ000184901_0003 ust. 9
- INQ000107106_0003 ust. 17
- Frank Atherton 3 lipca 2023 r. 54/10-56/7
- INQ000130469_0003 ust. 11
- Andrew Goodall 3 lipca 2023 r. 92/14-16
- INQ000184902_0002-0003 ust. 5-9
- Andrew Goodall 4 lipca 2023 r. 57/8-58/3
- Chris Llewelyn 12 lipca 2023 73/4-9
- INQ000177802_0011 ust. 27
- INQ000203349_0048 paragraf 126
- INQ000130469_0048 paragraf 188
- INQ000177802_0011 ust. 30; Zobacz też Quentin Sandifer 4 lipca 2023 r. 70/14-18
- Sytuacje nadzwyczajne w Walii, Wales Audit Office, 2012, s. 8, pkt 8 (https://www.audit.wales/sites/default/files Civi__Emergency_in_Wales_English_2012_14.pdf; INQ000107113)
- INQ000177802_0009 ust. 20; Zobacz też Quentin Sandifer 4 lipca 2023 r. 70/5-11
- INQ000177802_0009 ust. 21; Zobacz też Quentin Sandifer 4 lipca 2023 r. 70/5-11; INQ000130469_0045 paragraf 179
- Chris Llewelyn 12 lipca 2023 74/8-11
- Chris Llewelyn 12 lipca 2023 r. 74/17-75/17
- Sytuacje nadzwyczajne w Walii, Wales Audit Office, 2012, s. 10, pkt 17 (https://www.audit.wales/sites/default/files/Civi__Emergencies_in_Wales_English_2012_14.pdf; INQ000107113)
- Sytuacje nadzwyczajne w Walii, Wales Audit Office, 2012, s. 10, pkt 17 (https://www.audit.wales/sites/default/files/Civi__Emergencies_in_Wales_English_2012_14.pdf; INQ000107113)
- Sytuacje nadzwyczajne w Walii, Wales Audit Office, 2012, s. 10, pkt 18 (https://www.audit.wales/sites/default/files/Civi__Emergencies_in_Wales_English_2012_14.pdf; INQ000107113)
- INQ000187620_0024 paragraf 93
- INQ000185350_0003 ust. 10; INQ000195848_0001-0002 ust. 4
- INQ000187620_0024 ust. 93; Zobacz też INQ000187620_0037-0038 pkt 153–155
- INQ000187620_0006 ust. 20
- INQ000187620_0010, 0016, 0024 pkt 30, 55, 94
- INQ000187620_0024 paragraf 94
- Zdrowie i opieka społeczna Irlandii Północnej dotyczące gotowości i reagowania na pandemię grypy, Departament Zdrowia, Opieki Społecznej i Bezpieczeństwa Publicznego, styczeń 2013, s. 11 (http://www.niassembly.gov.uk/globalassets/documents/raise/deposited-papers/2013/dp1089.pdf; INQ000001191); Richard Pengelly 11 lipca 2023 68/24-69/2. Uwaga: W dniu 9 maja 2016 r. Departament Zdrowia, Opieki Społecznej i Bezpieczeństwa Publicznego w Irlandii Północnej stał się Departamentem Zdrowia i w niniejszym Raporcie nazywany jest Departamentem Zdrowia (Irlandia Północna), chyba że przed majem 2016 r. W przypadku odniesień obejmujących okres przed i po maju 2016 r. w Raporcie używana jest obecna nazwa.
- INQ000215123_0003-0004 ust. 10, 12
- INQ000215123_0005-0006 pkt 16–23
- Widzieć INQ000187620_0024, 0026-0029, 0037-0040 pkt 94, 101–112, 151–152, 156–160
- Zobacz też INQ000187620_0042 paragraf 169 dotyczący innych grup w ramach Grupy ds. Nagłych Wypadków Cywilnych (Irlandia Północna)
- Istniała także: Grupa Nadzoru nad Pandemią Grypy w Irlandii Północnej, która odpowiadała za przygotowanie i reagowanie w zakresie opieki zdrowotnej i społecznej (INQ000215123_0026-0027 pkt 97–99); Forum Planowania na wypadek Sytuacji Zdrowotnych, które wymieniało informacje pomiędzy Ministerstwem Zdrowia a organizacjami zajmującymi się zdrowiem i opieką społeczną (INQ000215123_0016-0017 ust. 60); Grupę Sterującą ds. Gotowości na Krytyczne Zagrożenia, aby zrozumieć obraz krytycznych zagrożeń dla Irlandii Północnej (INQ000215123_0017 ust. 61); Wspólną Radę Planowania Kryzysowego, aby zapewnić gotowość opieki zdrowotnej i społecznej (INQ000215123_0017 ust. 62); oraz Wspólny Zespół Planowania Kryzysowego, który wspierał Wspólną Radę Planowania Kryzysowego (INQ000215123_0017-0018 pkt 63).
- INQ000184642_0002-0006 pkt 2.1-2.13; INQ000174824
- INQ000215123_0026 pkt 94–96
- INQ000184642_0005 ust. 2.9
- Denis McMahon 6 lipca 2023 r. 47/17-48/2
- Denis McMahon 6 lipca 2023 r. 38.14-39.17
- Denis McMahon 6 lipca 2023 r. 56/18-25
- Michael McBride 10 lipca 2023 r. 125/22-127/22
- Michael McBride 10 lipca 2023 r. 115/21-117/13
- INQ000187306_0003 ust. 7-14
- Michael McBride 10 lipca 2023 155/20-156/2
- Michael McBride 10 lipca 2023 156/1-2
- Patrick Vallance 22 czerwca 2023 148/4-5; Michael McBride 10 lipca 2023 155/20-21; Arlene Foster 11 lipca 2023 41/20-25; Denis McMahon 6 lipca 2023 r. 94/3-11
- Widzieć INQ000187620_0004-0013 pkt 7-42
- INQ000187620_0013 pkt 43–44
- INQ000185350_0006 ust. 22
- INQ000185350_0006 ust. 22
- INQ000185350_0006-0008 pkt 23-25
- Denis McMahon 6 lipca 2023 13.10-19; Robin Swann 6 lipca 2023 159/9-160/25; INQ000192270_0015 ust. 45
- Michael McBride 10 lipca 2023 129/4-15
- Systemy, a nie struktury: zmiana zdrowia i opieki społecznej, Panel Ekspertów, 2016 (https://www.health-ni.gov.uk/sites/default/files/publications/health/expert-panel-full-report.pdf; INQ000205179); Zdrowie i dobre samopoczucie 2026: Wspólna realizacja, Departament Zdrowia, 2016 (https://www.healthni.gov.uk/sites/default/files/publications/health/health-and-wellbeing-2026-delivering-together.pdf; INQ000185457)
- Michael McBride 10 lipca 2023 131/6-133/14
- INQ000192270_005-006, 0015-0016 pkt 10–11, 45–47
- Robin Swann 6 lipca 2023 159/14-160/4
- Michael McBride 10 lipca 2023 r. 152/15-24
- Michael McBride 10 lipca 2023 r. 151/7-9
- Raport techniczny na temat pandemii COVID-19 w Wielkiej Brytanii, Departament Zdrowia i Opieki Społecznej, 1 grudnia 2022 r., s. 127, 176 (https://assets.publishing.service.gov.uk/media/63bd35b78fa8f55e3ac750c4/Technical-report-on-the-COVID-19-pandemic-in-the-UK-PRINT.pdf; INQ000101642)
- Widzieć INQ000203352_0016-0017 pkt 46–48; Michael McBride 10 lipca 2023 147/25-155/1; Arlene Foster 11 lipca 2023 r., 38.03.-39.24; Michelle O'Neill 12 lipca 2023 19.05-46.11
- INQ000187620_0021-0023 pkt 81–92; Denis McMahon 6 lipca 2023 57/6-62/4
- Denis McMahon 6 lipca 2023 r. 22.24–23.13; INQ000187620_0022 paragraf 84
- INQ000187620_0022 ust. 85; INQ000214130_0004-0005
- Michael McBride 10 lipca 2023 147/25-155/1; Arlene Foster 11 lipca 2023 r., 38.03.-39.24; Michelle O'Neill 12 lipca 2023 19.05-46.11; INQ000203352_0016-0017 pkt 46–48
- Zobacz na przykład Denis McMahon 6 lipca 2023 r. 56/2-25; Oświadczenie końcowe w imieniu Gabinetu Rady Ministrów 19 lipca 2023 r. 89/6-23; Mark Drakeford 4 lipca 2023 163/9-164/2, 165/16-166/4; Katharine Hammond 16 czerwca 2023 104/5-108/10
- Christopher Wormald 19 czerwca 2023 110/6-111/19, 118/23-122/9
- Emma Reed 26 czerwca 2023 r., 10/10–18
- Emma Reed 26 czerwca 2023 r., 17/18–23
- Katharine Hammond 16 czerwca 2023 84/11-85/8
- INQ000148429_0042-0044 pkt 153–164
- INQ000184643_0022 pkt 106-107
- INQ000377437_0003
- INQ000377438_0004
- Oliver Dowden 21 czerwca 2023 78/3-17
- Katharine Hammond 16 czerwca 2023 r. 77.12-78.23
- Oliver Letwin 20 czerwca 2023 55/10-12
- INQ000056240_0011-0012 ust. 14
- The UK Government Resilience Framework, Rząd Jej Królewskiej Mości, grudzień 2022 r., s. 13, pkt 25–26 (https://www.gov.uk/government/publications/the-uk-government-resilience-framework; INQ000097685)
- Brytyjska strategia bezpieczeństwa biologicznego, rząd Jej Królewskiej Mości, czerwiec 2023 r., s. 56–58 (https://assets.publishing.service.gov.uk/media/64c0ded51e10bf000e17ceba/UK_Biological_Security_Strategy.pdf; INQ000208910)
Rozdział 3: Ocena ryzyka
Wstęp
| 3.1. | Ryzyko jest istotną częścią naszego życia. Jest to możliwość wystąpienia złych rzeczy i niepewność przewidzenia, jakie mogą to być złe rzeczy. Ocena i zarządzanie ryzykiem to zadanie, z którym każdy z nas jest wrodzony. |
| 3.2. | Jak zaobserwowano w Ramy odporności rządu Wielkiej Brytanii opublikowanym w grudniu 2022 r., punktem wyjścia dla odporności (podstawowej zdolności społeczeństwa do przeciwstawiania się kryzysom i zdolności dostosowywania się do przełomowych wydarzeń) jest zrozumienie ryzyka.1 Jeśli ryzyko nie zostanie odpowiednio przewidywane i rozumiane, trudno jest przygotować się na katastrofalne zdarzenia i ich skutki lub zbudować odporność na nie. |
| 3.3. | Istnieje kilka prostych, ale ważnych pytań, które stanowią podstawę oceny ryzyka. Zawierają:
|
| 3.4. | Planując zdarzenia katastrofalne, należy zatem najpierw zidentyfikować ryzyko, a następnie opracować strategię jego przeciwdziałania. Strategia powinna z wyprzedzeniem ocenić, co można, a czego nie można zrobić w związku z tym ryzykiem, czy można mu zapobiec, a jeśli nie, czy można ograniczyć lub złagodzić jego szkodliwe skutki.2 W tym rozdziale przeanalizowano systemy oceny ryzyka w zakresie gotowości na wypadek pandemii w Wielkiej Brytanii. |
Ocena ryzyka przeprowadzona przez rząd Wielkiej Brytanii i zdecentralizowane administracje
| 3.5. | W brytyjskich ocenach ryzyka od 2005 r. do przedednia pandemii wirusa Covid-19 grypa pandemiczna była konsekwentnie opisywana jako najważniejsze ryzyko cywilne, na jakie narażona jest Wielka Brytania.3 Odprawę „pierwszego dnia” otrzymaną przez posła Matta Hancocka, Sekretarza Stanu ds. Zdrowia i Opieki Społecznej od lipca 2018 r. do czerwca 2021 r., wygłosił Sir Christopher Wormald, stały sekretarz Departamentu Zdrowia (i Opieki Społecznej) od maja 2016 r.4 Towarzyszył mu szereg dokumentów informacyjnych.5 Obejmowały one notatkę od Clary Swinson, dyrektor generalnej ds. zdrowia globalnego i publicznego na tym wydziale, z listopada 2016 r., w której stwierdzono:
„Pandemia grypa stanowi najwyższe ryzyko dla rządu (w krajowym rejestrze ryzyka Urzędu Rady Ministrów). W każdym roku szacujemy prawdopodobieństwo wystąpienia pandemii na 3% w oparciu o 3 pandemie w XX wieku, a wpływ „rozsądnego najgorszego scenariusza” na 750 tys. zgonów. Mamy plany awaryjne i program prac, dzięki którym będziemy je aktualizować i uzupełniać. Możemy przekazać Ci dalsze informacje na temat bieżącego zagrożenia i naszej pracy w odpowiedzi na nie.”6 (podkreślenie w oryginale) |
W całej Wielkiej Brytanii
| 3.6. | W latach poprzedzających pandemię Covid-19 Sekretariat ds. Zagrożeń Cywilnych w Urzędzie Rady Ministrów był odpowiedzialny za przygotowanie się do poważnych sytuacji kryzysowych, reagowanie na nie i wyciąganie wniosków z nich.7 Opracowano oceny ryzyka obejmujące całą Wielką Brytanię, które posłużyły do planowania na poziomie krajowym i lokalnym. Podejście zdecentralizowanych administracji nie różniło się istotnie od podejścia rządu Wielkiej Brytanii do oceny ryzyka. |
| 3.7. | Przed 2019 r. Sekretariat ds. Zagrożeń Cywilnych opracował, we współpracy z innymi departamentami rządowymi, agencjami i zdecentralizowanymi administracjami, dwie oddzielne oceny ryzyka obejmujące całą Wielką Brytanię.8 Krajowa Ocena Ryzyka była „narzędzie strategicznego planowania średnioterminowego” na wypadek sytuacji kryzysowych w kraju w perspektywie pięcioletniej, opracowanej w celu zapewnienia podstawy planowania awaryjnego na poziomie krajowym i lokalnym.9 Ocena ryzyka bezpieczeństwa narodowego skupiała się na szerszych zagrożeniach dla bezpieczeństwa narodowego (w tym ryzykach międzynarodowych mających wpływ na interesy Wielkiej Brytanii) w perspektywie 20 lat.10 Ogólnie rzecz biorąc, ryzyko chorób zakaźnych u ludzi zostało odnotowane w Krajowej Ocenie Ryzyka. W 2019 r. Sekretariat ds. Zagrożeń Cywilnych połączył dwie oceny ryzyka obejmujące całą Wielką Brytanię w jedną ocenę ryzyka dla bezpieczeństwa narodowego, aby stworzyć ujednolicone ramy.11 |
| 3.8. | Ponadto od 2008 r. Sekretariat ds. Zagrożeń Cywilnych publikował Krajowy Rejestr Ryzyka jako udostępnioną publicznie wersję Krajowej Oceny Ryzyka i Oceny Ryzyka Bezpieczeństwa Narodowego, które były i pozostają niejawne.12 Każdy dokument był kilkakrotnie aktualizowany przed wybuchem pandemii Covid-19.13 |
Zdecentralizowane narody
| 3.9. | Na zewnątrz oceny ryzyka przeprowadzone przez zdecentralizowane administracje były ich własnymi dokumentami, ale ich metoda po prostu skopiowała ocenę rządu Wielkiej Brytanii. Ograniczało to ich użyteczność jako narzędzia oceny ryzyka, ponieważ nie oceniało, w jaki sposób poszczególne zagrożenia wpłyną na populację poszczególnych narodów i nie uwzględniało w wystarczającym stopniu lub w ogóle podstawowych warunków zdrowotnych, społecznych i ekonomicznych każdej populacji. Oceny ryzyka specyficzne dla każdej zdecentralizowanej administracji (i Anglii) zasygnalizowałyby przed pandemią, w jaki sposób dostosować reakcję do potrzeb każdej populacji. |
Szkocja
| 3.10. | W styczniu 2015 r. John Swinney MSP, zastępca pierwszego ministra w rządzie Szkocji od listopada 2014 r. do marca 2023 r., zlecił opracowanie szkockiej oceny ryzyka, której pierwsze i jedyne wydanie ukazało się w 2018 r.14 Miało ono uzupełnić oceny obejmujące całą Wielką Brytanię, zapewniając szkocki kontekst dla zagrożeń, w przypadku których Szkocja byłaby dotknięta inaczej niż reszta Wielkiej Brytanii, a także informacje pomocne w planowaniu przez lokalne służby ratownicze.15 |
| 3.11. | Chociaż opracowano odrębny dokument, Gillian Russell, dyrektor ds. bezpieczniejszych społeczności w rządzie Szkocji od czerwca 2015 r. do marca 2020 r., powiedziała w dochodzeniu: „[W]kapelusz, który zrobiliśmy, to to wzięliśmy [Wielka Brytania] Krajowa ocena ryzyka, a następnie spójrz, jak na tej podstawie powinna wyglądać szkocka ocena ryzyka.”16 Krótko mówiąc, dane dotyczące populacji zawarte w ogólnobrytyjskiej krajowej ocenie ryzyka zastąpiono danymi dotyczącymi populacji Szkocji. Nie przeprowadzono oddzielnej analizy dla Szkocji, która odpowiednio uwzględniłaby konkretne czynniki, które mogłyby szczególnie wpłynąć na populację Szkocji.17 |
Walia
| 3.12. | Rząd walijski oparł się na poziomie oceny ryzyka obejmującym całą Wielką Brytanię.18 Nie rozdzielono w nim materiału obejmującego całą Wielką Brytanię na ocenę, w jaki sposób zagrożenia cywilne, na jakie napotyka Wielka Brytania, mogą konkretnie wpłynąć na populację Walii.19 Mark Drakeford MS, pierwszy minister Walii od grudnia 2018 r. do marca 2024 r., powiedział w dochodzeniu, że w pewnych celach „z walijskiego punktu widzenia rozsądne jest poleganie na wiedzy specjalistycznej i możliwościach” rządu brytyjskiego.20 Przed pandemią nie istniał zatem walijski krajowy rejestr ryzyka, który uwzględniałby szczególne okoliczności w Walii. |
| 3.13. | 2023 Przegląd sytuacji awaryjnych w Walii zalecił utworzenie walijskiego rejestru ryzyka.21 Doktor Andrew Goodall, stały sekretarz rządu walijskiego od września 2021 r., powiedział w dochodzeniu, że Walia „wprowadzenie„walijski krajowy rejestr ryzyka.22 Pan Drakeford przyznał, że „współczesne myślenie opiera się na tym średniozaawansowanym poziomie walijskim [oceny ryzyka] może wymagać wzmocnienia”.23 Reg Kilpatrick, dyrektor generalny ds. koordynacji Covid w rządzie walijskim od września 2020 r., poinformował dochodzenie, że istniało „bardzo duża perspektywa, jeśli nie pewność”, żeby tak się stało.24 Według stanu na czerwiec 2024 r. nie było to jeszcze obowiązujące. |
| 3.14. | Chociaż rząd walijski nie opracował walijskiego rejestru ryzyka w celu oceny, w jaki sposób ryzyko związane z sytuacjami cywilnymi może wpłynąć na ludność Walii, prowadził on rejestry ryzyka korporacyjnego, ale jedynie identyfikowały one zagrożenia dla jego zdolności do wykonywania swoich obowiązków. W rejestrze ryzyka korporacyjnego z 2014 roku ryzyko grypy pandemicznej zidentyfikowano jako jeden z zaledwie pięciu przykładów „pełen zakres zagrożeń i zagrożeń narodowych” skierowaną do Walii, ale w kategoriach ogólnych i pozbawionych informacji, jeśli chodzi o szczegóły dotyczące gotowości na wypadek pandemii, odporności i reagowania.25 W rejestrze ryzyka korporacyjnego za 2019 r. w ogóle nie uwzględniono grypy pandemicznej jako ryzyka, a zatem nie rozważono szczegółowo środków zaradczych, jakie można temu zaradzić. Zamiast tego starano się ująć wpływ wszystkich rodzajów sytuacji kryzysowych za pomocą terminu „wydarzenie zakłócające”.26 Podobnie, chociaż ryzyko grypy pandemicznej zostało ujęte w departamentalnym rejestrze ryzyka Grupy ds. Zdrowia i Opieki Społecznej rządu walijskiego, nie wydaje się, aby zostało uznane za ważną kwestię międzyrządową.27 Co więcej, wyniki zarejestrowane w odniesieniu do ryzyka w rejestrze ryzyka korporacyjnego rządu walijskiego wskazywały, że rząd walijski uważa, że jego zdolność do łagodzenia skutków pandemii poprawiła się.28 Jak przyznał dr Goodall, ryzyko „były zbyt uogólnione, co prawdopodobnie dawało niewłaściwą pewność" I "z perspektywy czasu„Oceny ryzyka powinny być wyższe.29 Oceny ryzyka nie odzwierciedlały rzeczywistości w terenie. |
Irlandia Północna
| 3.15. | Przed pandemią Irlandia Północna „zasadniczo… zastosował podejście brytyjskie”do oceny ryzyka.30 Ocenę ryzyka Irlandii Północnej przygotowano w latach 2009 i 2013.31 Przyjęto podejście zastosowane w ocenach ryzyka obejmującego całą Wielką Brytanię i zastosowano je do Irlandii Północnej.32 Odniesienia do ryzyka chorób zakaźnych u ludzi dostarczyły niewiele dalszych informacji wykraczających poza te zawarte w ocenach ryzyka obejmujących całą Wielką Brytanię.33 W okresie od 2013 r. do stycznia 2020 r. nie dokonano żadnych aktualizacji oceny ryzyka Irlandii Północnej.34 Kolejny, Rejestr Ryzyka Irlandii Północnej, powstał podczas pandemii Covid-19 w lipcu 2022 r.35 |
| 3.16. | Władze Irlandii Północnej prowadziły jednak rejestry ryzyka korporacyjnego. W departamentalnym rejestrze ryzyka Departamentu Zdrowia (Irlandia Północna) na rok 2018/2019 ostrzegł:
„Sektor zdrowia i opieki społecznej może nie być w stanie zareagować na sytuację zdrowotną Przed pandemią nie podjęto wystarczających działań w związku z tym kluczowym ostrzeżeniem. Dochodzenie zostało poinformowane, że było to spowodowane brakiem wystarczających zasobów Departamentu Zdrowia (Irlandia Północna).37 |
Kluczowe błędy w ocenach ryzyka
| 3.17. | W podejściu do oceny ryzyka w Wielkiej Brytanii wystąpiło pięć głównych błędów, które miały istotny wpływ na gotowość i odporność na sytuacje kryzysowe cywilne obejmujące cały system, takie jak pandemie:
|
| 3.18. | W wyniku przyjęcia przez zdecentralizowane administracje podejścia do ryzyka brytyjskiego rządu, wady te przeniosły się na ich systemy cywilne na wypadek nieprzewidzianych wypadków. |
| 3.19. | W styczniu 2021 r. Sekretariat ds. Zagrożeń Cywilnych zlecił Królewskiej Akademii Inżynierii przeprowadzenie pierwszego zewnętrznego przeglądu oceny ryzyka bezpieczeństwa narodowego.38 Jej raport końcowy został przedłożony Sekretariatowi ds. Zagrożeń Cywilnych we wrześniu 2021 r.39 Rząd Wielkiej Brytanii uwzględnił części raportu i opracował nową edycję oceny ryzyka bezpieczeństwa narodowego w 2022 r. oraz zaktualizowany krajowy rejestr ryzyka w sierpniu 2023 r.40 Poniżej zbadano, w jakim stopniu zalecenia dotyczące pięciu powyższych obszarów zostały uwzględnione przez rząd Wielkiej Brytanii. |
Wada 1: Poleganie na jednym scenariuszu
| 3.20. | Scenariusze są ustaloną częścią praktyki oceny ryzyka. Polegają one na „opracowywanie modeli tego, co może się wydarzyć w przyszłości" I "może pomóc zidentyfikować ryzyko i zbadać niepewność, konsekwencje i współzależności”.41 Są przydatne, ale mają swoje ograniczenia. |
| 3.21. | Oceny ryzyka obejmujące całą Wielką Brytanię celowo nie uwzględniły wszystkich zagrożeń, z jakimi może się zmierzyć Wielka Brytania. Każdy zestaw ryzyk został zgrupowany wokół jednego „uzasadniony najgorszy scenariusz”.42 Miało to na celu:
„ilustrują przejawy ryzyka w [Ocena ryzyka bezpieczeństwa narodowego] poprzez przedstawienie kontekstu, opisanie przebiegu zdarzenia oraz ilościowe określenie wpływu i prawdopodobieństwa takiego zdarzenia. [Rozsądne najgorsze scenariusze] należy je czytać jako scenariusz, a nie prognozę, i często są obarczone znaczną niepewnością.”43 |
| 3.22. | W przeglądzie z 2010 r. dotyczącym reakcji Wielkiej Brytanii na pandemię grypy H1N1 („świńskiej grypy”) w latach 2009–2010) Dame Deirdre Hine wyraziła zaniepokojenie stosowaniem rozsądnych najgorszych scenariuszy ze względu na możliwość ich interpretacji raczej jako przewidywania niż tylko jeden scenariusz, według którego należy planować.44 Zapytanie zgadza się. Ustalenie wielu scenariuszy, aż do rozsądnego najgorszego przypadku i poza nim, powinno skutkować bardziej wyrafinowanym planowaniem i większym zakresem możliwych reakcji. |
| 3.23. | Rozsądne najgorsze scenariusze miały być „stanowiący wyzwanie, ale prawdopodobny przejaw ryzyka”.45 Zostały one ujęte na liście scenariuszy ryzyka tylko wtedy, gdy spełniły określone kryteria.46 Należą do nich:
|
| 3.24. | Przed pandemią Covid-19 w ogólnokrajowym procesie oceny ryzyka konsekwentnie identyfikowano tylko dwa rozsądne, najgorsze scenariusze dotyczące chorób zakaźnych u ludzi. One były:
(Choroba zakaźna o poważnych konsekwencjach to taka, która zazwyczaj charakteryzuje się wysokim współczynnikiem śmiertelności, może być trudna do rozpoznania i szybkiego wykrycia, może przenosić się w społeczeństwie i może nie mieć skutecznych środków zapobiegania lub leczenia. Wymaga ulepszonej, specjalistycznej opieki odpowiedź.)51 |
| 3.25. | Różnicę między tymi dwoma scenariuszami odzwierciedla Tabela 2, która podsumowuje rozsądne najgorsze scenariusze z ocen ryzyka z lat 2014, 2016 i 2019. W każdej iteracji przewidywano, że liczba ofiar śmiertelnych i ofiar (tj. szkód bliskich śmierci) będzie znacznie wyższa w scenariuszu pandemii grypy niż w scenariuszu dotyczącym pojawiających się chorób zakaźnych innych niż grypa. |
| Grypa pandemiczna: założenia | Pojawiające się choroby zakaźne: założenia | |
|---|---|---|
| 2014 | Ofiary śmiertelne: 750,000
Ofiary wypadku: 50% populacji (Widzieć INQ000176765_0001, 0003, 0006-0007) |
Ofiary śmiertelne: 200
Ofiary wypadku: 2,000 (Widzieć INQ000176766_0001, 0004-0005) |
| 2016 | Ofiary śmiertelne: 750,000
Ofiary wypadku: 50% populacji, 30 milionów ludzi (Widzieć INQ000176770_0001-0002, 0005-0006) |
Ofiary śmiertelne: 101 do 1000
Ofiary wypadku: 2000 do 10 000 (Widzieć INQ000176771_0004) |
| 2019 | Ofiary śmiertelne: 820,000
Ofiary wypadku: 50% populacji, 32,8 miliona ludzi (Widzieć INQ000176776_0001, 0006-0007) |
Ofiary śmiertelne: 200
Ofiary wypadku: 2,000 (Widzieć INQ000185135_0008) |
| 3.26. | Przygotowania Wielkiej Brytanii na wypadek pandemii skupiały się na grypie jako jedynym rozsądnym najgorszym scenariuszu na skalę pandemii.52 Założono, że taki scenariusz będzie wystarczająco reprezentatywny dla wszystkich pandemii.53 Jednak do tego pojedynczego scenariusza przywiązano zbyt dużą wagę. Pozostawiło to poważną lukę w ocenie ryzyka w Wielkiej Brytanii, co będzie miało konsekwencje dla całej gotowości Wielkiej Brytanii na wypadek pandemii. Zasygnalizował systemowi gotowości i odporności na sytuacje nadzwyczajne w Wielkiej Brytanii, że nie ma konieczności odrębnych przygotowań na pojawienie się choroby zakaźnej (innej niż grypa), która może osiągnąć skalę pandemii. W rezultacie w niewystarczającym stopniu uwzględniono różne umiejętności, infrastrukturę, technologię i zasoby, które mogą być potrzebne w takim przypadku (zob. Rozdział 5: Uczenie się na doświadczeniach). |
| 3.27. | Rozsądne najgorsze scenariusze zawarte w krajowych ocenach ryzyka z 2014 r. i 2016 r. oparto na opinii Komitetu Doradczego ds. Niebezpiecznych Patogenów (komitetu ekspertów Departamentu Zdrowia) z lutego 2013 r.54 W ocenie ryzyka bezpieczeństwa narodowego z 2019 r. utrzymano rozsądny najgorszy scenariusz dotyczący nowo pojawiających się chorób zakaźnych i grypy pandemicznej, z podobną liczbą ofiar śmiertelnych i ofiar, jak w krajowych ocenach ryzyka z 2014 r. i 2016 r.55 Eksperci z całego świata zachodniego poinformowali, że pandemia grypy stanowi najpoważniejsze zagrożenie dla zdrowia na dużą skalę.56 Grypa pandemiczna była – i pozostaje – największym ryzykiem, ale inne formy pandemii również były i są ryzykiem. Scenariusz pojawienia się choroby zakaźnej oparto na danych z lat 2002–2003 dotyczących wybuchu ostrego zespołu oddechowego (SARS).57 Zostało ono opisane przez Komitet Doradczy ds. Niebezpiecznych Patogenów jako wydarzenie, które „prawdopodobnie" I "prawdopodobny”, ale z ważnym zastrzeżeniem, że „poza tym na tym etapie nie można zaproponować żadnego oszacowania prawdopodobieństwa ani wpływu”.58 |
| 3.28. | Pomimo tej uwagi dotyczącej prawdopodobieństwa i skutków pojawienia się choroby zakaźnej układu oddechowego, Departament Zdrowia i Opieki Społecznej popełnił znaczący błąd, przyjmując SARS jako jedyną podstawę rozsądnego najgorszego scenariusza. W ten sposób wysłał sygnał, że planowanie dotyczące patogenu innego niż grypa powinno skupiać się na pojawiającej się chorobie zakaźnej, która nie byłaby wystarczająco przenośna, aby spowodować pandemię. |
| 3.29. | W ogólnokrajowych ocenach ryzyka z lat 2008–2019 wielokrotnie stwierdzono, że Departament Zdrowia i Opieki Społecznej opracował krajowy plan awaryjny na wypadek SARS.59 Ich zdaniem zapewni to podstawę do postępowania w przypadku każdej przyszłej epidemii SARS i opiera się na ogólnych reakcjach na ogniska chorób zakaźnych oraz wnioskach wyciągniętych podczas wybuchu SARS w latach 2002–2003. Wygląda na to, że było to fałszywe zapewnienie. Pomimo próśb płynących z dochodzenia, rząd brytyjski nie ujawnił żadnego planu awaryjnego obejmującego całą Wielką Brytanię w przypadku SARS, bliskowschodniego zespołu oddechowego (MERS) ani żadnej innej choroby zakaźnej o poważnych konsekwencjach. Dochodzenie nie wykazało zatem, czy takie plany kiedykolwiek istniały. |
| 3.30. | Jedynymi planami awaryjnymi dotyczącymi SARS lub MERS, jakie otrzymano w ramach dochodzenia, są plany tymczasowe będące w posiadaniu odpowiednio Agencji Ochrony Zdrowia i Zdrowia Publicznego Anglii. Plan przejściowy SARS z grudnia 2003 roku opisywał się jako „plan awaryjny obejmujący skoordynowaną reakcję Agencji Ochrony Zdrowia” i taki, który został zaprojektowany do stosowania w połączeniu z planami SARS brytyjskich departamentów zdrowia i NHS.60 W planie przejściowym MERS na 2014 r. wyraźnie stwierdzono, że „dokument wewnętrzny” do użytku przez Public Health England i że było to „nieprzeznaczone do użytku poza organizacją”.61 Nie wydaje się, aby istniał odrębny plan dokumentujący konkretną, ogólnokrajową strategię reagowania na epidemię SARS, MERS lub jakiejkolwiek innej choroby zakaźnej o poważnych konsekwencjach i określający wpływ na zdrowie, opiekę społeczną i systemy zdrowia publicznego i szerszego społeczeństwa, lub interwencje niefarmaceutyczne, takie jak obowiązkowa kwarantanna, ustalanie kontaktów zakaźnych lub kontrole graniczne. |
| 3.31. | Królewska Akademia Inżynierska zarekomendowała rządowi Wielkiej Brytanii we wrześniu 2021 r.:
„Dla każdego ryzyka należy wygenerować szereg scenariuszy, aby zbadać niepewność i dodatkowe wymagania dotyczące planowania, poprawić wyniki i zapewnić maksymalną wartość z całego procesu.”62 W swoich zeznaniach złożonych w dochodzeniu wielu naukowców zgodziło się z tą opinią. Byli wśród nich profesor Sir Mark Walport (główny doradca naukowy rządu od kwietnia 2013 r. do września 2017 r.), profesor Sir Patrick Vallance (główny doradca naukowy rządu od kwietnia 2018 r. do marca 2023 r.), profesor John Edmunds (profesor modelowania chorób zakaźnych w London School of Higiena i medycyna tropikalna) oraz profesor Sir Christopher Whitty (od października 2019 r. dyrektor medyczny w Anglii).63 Każdy rodzaj choroby ma swój własny profil i sposoby przenoszenia, ale – jak jasno stwierdzili świadkowie – gotowość na pandemie i odporność na nie powinna uwzględniać możliwość przenoszenia wszystkimi potencjalnymi drogami zakażenia.64 |
| 3.32. | Katharine Hammond, dyrektor Sekretariatu ds. Zagrożeń Cywilnych od sierpnia 2016 r. do sierpnia 2020 r., powiedziała w dochodzeniu, że przewidywanie i planowanie wszystkiego, co może się wydarzyć, nie jest rozsądne. System brytyjski został zbudowany w oparciu o dobrą ocenę ryzyka w celu określenia możliwości i posiadanie środków umożliwiających ich szybkie dostosowanie w obliczu wydarzeń.65 Pani Hammond wyraziła obawę, że wykorzystanie wielu scenariuszy pandemii wymagałoby zbyt dużych zasobów, a Sekretariat ds. Zagrożeń Cywilnych „w rzeczywistości nie miał takich możliwości”.66 W rezultacie planowanie wielu scenariuszy w ramach oceny ryzyka narodowego z 2016 r. i oceny ryzyka bezpieczeństwa narodowego z 2019 r. było bardzo ograniczone.67 |
| 3.33. | Oprócz wpływu drugim czynnikiem oceny ryzyka jest prawdopodobieństwo jego wystąpienia. Jednakże, jak zaleciła Królewska Akademia Inżynierii rządowi Wielkiej Brytanii w 2021 r.:
„[L]podobieństwo nie powinno być głównym czynnikiem wpływającym na ustalanie priorytetów, ponieważ może być trudno ocenić to z dużą pewnością w odniesieniu do wszystkich rodzajów ryzyka. Podejmowanie decyzji powinno opierać się na wpływie i gotowości powiązanej ze zdolnościami w zakresie zapobiegania, łagodzenia, reagowania i odbudowy.”68 Zapytanie zgadza się. Mniejszą wagę należy przywiązywać do prawdopodobieństwa, ponieważ należy planować także zdarzenia mało prawdopodobne. Sir Oliver Letwin, poseł do parlamentu, minister polityki rządu od maja 2010 r. do lipca 2016 r. i kanclerz księstwa Lancaster od lipca 2014 r. do lipca 2016 r., uznał, że skupienie się na prawdopodobieństwie było błędem”ponieważ zdarzenia o ogromnych skutkach, które są bardzo mało prawdopodobne i mogą nie wystąpić przez wiele lat, jeśli wystąpią, będą jednak miały ogromne skutki”.69 Doradcy naukowi, w tym profesorowie Walport i Vallance, powiedzieli w dochodzeniu, że skupianie się na prawdopodobieństwie było błędem.70 |
| 3.34. | Wielu świadków i departamentów rządowych starało się scharakteryzować pandemię Covid-19 jako na tyle nieprawdopodobną, że można ją nazwać wydarzeniem „czarnego łabędzia”.71 Jest to wydarzenie katastrofalne, ale bezprecedensowe, wykraczające poza doświadczenie i rozsądną kontemplację, a zatem nieprzewidywalne.72 Koncepcja ta nie jest powszechnie akceptowana i nie budzi kontrowersji w dziedzinie nieprzewidzianych wypadków cywilnych. Na przykład profesor David Alexander i Bruce Mann, eksperci w dziedzinie zarządzania ryzykiem i odporności (zob Załącznik 1: Informacje o tym module i metodologia badania) stwierdził, że większość zagrożeń cywilnych można przewidzieć w jakiejś formie lub formie.73 Niemniej jednak żaden rząd nie jest w stanie przewidzieć wszystkiego. Jak powiedział sir Oliver Letwin w dochodzeniu:
"[N]o zakres planowania odporności lub analizy horyzontu będzie wystarczający, aby zapewnić, że rząd zawsze będzie skutecznie reagował na pojawiające się sytuacje kryzysowe. Wcześniejsza wiedza nigdy nie jest pełna: zdarzają się niespodzianki.”74 |
| 3.35. | W świetle rad wielu ekspertów racjonalne było, aby oceny ryzyka obejmujące całą Wielką Brytanię zawierały scenariusze zarówno pandemii grypy, jak i choroby zakaźnej o poważnych konsekwencjach na mniejszą skalę, takiej jak SARS, ale nie powinno to dotyczyć wykluczenie innych możliwości. Niedawne doświadczenia SARS i MERS sprawiły, że można było przewidzieć kolejną epidemię koronaawirusa na skalę pandemii. To nie było wydarzenie czarnego łabędzia. Brak takiego scenariusza w ocenach ryzyka był zasadniczym błędem Departamentu Zdrowia i Opieki Społecznej oraz Sekretariatu ds. Zagrożeń Cywilnych. Rząd Wielkiej Brytanii i zdecentralizowane administracje mogły i powinny były ocenić ryzyko związane z nowym patogenem, który mógłby osiągnąć skalę pandemii. |
| 3.36. | Ocena ryzyka bezpieczeństwa narodowego z 2022 r. uwzględniła bardziej ogólne scenariusze pandemii i pojawiających się chorób zakaźnych75. Sprostowanie jest mile widziane, ale podkreśla błąd występujący przed pandemią Covid-19. Wydaje się, że prace nad udoskonaleniami są nadal w toku. Rząd Wielkiej Brytanii będzie musiał także dopilnować, aby wybór wielu scenariuszy dla różnych ryzyk odzwierciedlał reprezentatywny zakres tego, co może pójść nie tak i aby wybór ten nie był oparty głównie na prawdopodobieństwie tych scenariuszy. Nie wyjaśniła jeszcze w jasny sposób, w jaki sposób proponuje pełniej wdrożyć zalecenia Królewskiej Akademii Inżynierii, aby ustrzec się przed opisanymi powyżej problemami.76 |
Wada 2: Zapobieganie sytuacji awaryjnej
| 3.37. | Wielkiej Brytanii nie udało się zaplanować zapobiegania powszechnym chorobom i śmierci przewidzianym w najgorszym możliwym scenariuszu pandemii grypy. Hancock powiedział, że Krajowy Rejestr Ryzyka:
„jednoznacznie zakładano, że w przypadku pandemii zachoruje duża liczba ludzi. Nie wspomniała o działaniach, które można podjąć, aby temu zapobiec.”77 Założenie, że ryzyka nie da się złagodzić, odniósł się do fundamentalnego niepowodzenia „doktryna”.78 |
| 3.38. | Zgodził się z tym poseł Jeremy Hunt, sekretarz stanu ds. zdrowia (i opieki społecznej) od września 2012 r. do lipca 2018 r.79 Profesor Whitty”połowa” zgodził się, stwierdzając:
„[W]Nie zastanowiliśmy się wystarczająco nad tym, co moglibyśmy zrobić, aby zatrzymać pandemię na skalę Covida lub jakiegokolwiek innego patogenu, który realnie mógłby tam dotrzeć.”80 Profesor Whitty uznał, że rozsądne jest także posiadanie praktycznego planu działania, gdy wszystko inne zawiedzie.81 Profesor Edmunds przypisał tę porażkę doktryny faktowi, że rozsądny najgorszy scenariusz pandemii grypy był w dużej mierze scenariuszem niełagodzonym.82 |
| 3.39. | Ocena ryzyka bezpieczeństwa narodowego z 2019 r. zawierała wyraźne zastrzeżenie dotyczące pandemii:
„Rozsądny najgorszy scenariusz nie uwzględnia wprowadzonych przez nas środków zaradczych, ponieważ wpływ środków zaradczych w przypadku jakiejkolwiek pandemii jest trudny do przewidzenia, ponieważ będzie zależał od charakteru wirusa.”83 Stwierdzono to również w Krajowych Ocenach Ryzyka z 2014 i 2016 roku.84 |
| 3.40. | Z kolei w rozsądnym, najgorszym scenariuszu dotyczącym pojawiających się chorób zakaźnych, zawartym w ocenie ryzyka bezpieczeństwa narodowego z 2019 r., faktycznie zakładano, że środki kontroli infekcji polegające na podstawowym ustalaniu kontaktów zakaźnych pozwolą opanować epidemię.85 Scenariusz o Nie uwzględniono pojawiającej się choroby zakaźnej osiągającej skalę pandemii i wymagającej podobnego systemu śledzenia kontaktów jako pierwszego kroku w celu kontrolowania rozprzestrzeniania się. |
| 3.41. | Podejścia do oceny ryzyka wiązały się z dwoma problemami. Po pierwsze, oceny ryzyka nie zawsze wyraźnie określały lub wyjaśniały środki łagodzące przyjęte w scenariuszach ryzyka.86 Przyszłe oceny ryzyka muszą jaśniej i spójnie wyjaśniać leżące u ich podstaw założenia. Po drugie, w ocenie ryzyka bezpieczeństwa narodowego i w jej poprzednikach nie uwzględniono należycie środków zapobiegawczych i łagodzących. W rezultacie nie uwzględniono odpowiednio technologii, umiejętności, infrastruktury i zasobów, które byłyby potrzebne do złagodzenia skutków sytuacji nadzwyczajnej lub zapobiegania jej (zob. Rozdział 5: Uczenie się na doświadczeniach). |
| 3.42. | To nie była nowa kwestia. W październiku 2013 r. profesor Walport napisał do posła Davida Camerona, premiera od maja 2010 r. do lipca 2016 r., zalecając zatwierdzenie Krajowej Oceny Ryzyka z 2013 r. i wskazując szereg obszarów, w których można ją wzmocnić, w tym:
"[A] dobry rejestr ryzyka powinien skłaniać do myślenia o tym, w jaki sposób można zapobiegać zagrożeniom, je łagodzić, postępować w przypadku ich wystąpienia, a następnie je wyjaśniać. The [Krajowa Ocena Ryzyka] jest dość skutecznie wykorzystywany do obsługi i oczyszczania, ale w różny sposób do podejmowania decyzji dotyczących zapobiegania i łagodzenia skutków.”87 Profesor Walport wyraził podobne poglądy urzędnikom Gabinetu w czerwcu 2014 r. i ponownie w październiku 2014 r.88 W śledztwie powiedział, że „byłzaczyna brzmieć jak zdarta płyta" w tej sprawie.89 Zapytany w ramach dochodzenia, czy jego zdaniem wykorzystanie krajowej oceny ryzyka w zakresie zapobiegania i łagodzenia poprawiło się podczas jego urzędowania, powiedział: „Myślę, że była to praca w toku i myślę, że nadal jest to praca w toku.”90 |
| 3.43. | W 2014 r. Sekretariat ds. Zagrożeń Cywilnych był gospodarzem warsztatów, w których zalecono „[g]skupiamy się na tym, „czemu chcemy zapobiec”.„” i lepsze zrozumienie „skalowalność zdolności i zasobów (aby pomóc zidentyfikować luki w gotowości)”.91 |
| 3.44. | Wygląda na to, że Gabinet Rady Ministrów uznał potrzebę ulepszeń w tym obszarze w ramach swoich prac nad rozporządzeniem Strategia Bezpieczeństwa Narodowego oraz Strategiczny Przegląd Obrony i Bezpieczeństwa 2015. W części „Zapobieganie” Trybunał zauważył:
„Oznacza to skupienie się na zarządzaniu ryzykiem, tam gdzie to możliwe, na jego łagodzeniu, a nie tylko na przygotowywaniu się na sytuacje awaryjne.”92 |
| 3.45. | W marcu 2017 r. Sekretariat ds. Zagrożeń Cywilnych powołał Radę Sterującą ds. Oceny Ryzyka. Jego celem było nadzorowanie podejścia do oceny ryzyka bezpieczeństwa narodowego z 2019 r. W protokole z pierwszego posiedzenia zapisano:
„Zarząd uznał, że chociaż sporządzenie oceny ryzyka, która wspierała decyzje dotyczące zapobiegania ryzyku, a także przygotowania ryzyka i reagowania na nie, było godne podziwu, nie powinno to ograniczać elastyczności dokumentu.”93 Nie uwzględniono odpowiednio roli zapobiegania przy ocenie ryzyka. Była to stracona szansa, ponieważ przed wystąpieniem stanu nadzwyczajnego nie uwzględniono możliwości jego zapobiegania lub łagodzenia. |
Wada 3: Powiązane zagrożenia i efekt domina
| 3.46. | Wiele sytuacji awaryjnych może oddziaływać na siebie, tworząc łączną awarię gorszą, niż gdyby wystąpiły pojedynczo. Pojedyncza sytuacja nadzwyczajna może wywołać efekt domina, w którym, gdy coś pójdzie nie tak, inne rzeczy również pójdą nie tak.94 Profesor Alexander opisał je odpowiednio jako „ryzyko złożone" I "ryzyko kaskadowe”.95 Reakcja na zdarzenie może również wiązać się z ryzykiem. Dotyczy to szczególnie sytuacji kryzysowych obejmujących cały system, w których rząd może interweniować na znaczną skalę. Używając analogii profesora Walporta, lekarstwo na konkretny przypadek może mieć szkodliwe skutki uboczne.96 |
| 3.47. | Zdarzenia takie jak pandemia zasadniczo różnią się od innych izolowanych sytuacji kryzysowych, ponieważ angażują cały system reagowania. Ryzykiem może być początek pandemii (zagrożenie dla zdrowia), w wyniku której rząd podejmuje szereg interwencji mających na celu ochronę ludności (przynosząc korzyści, ale także koszty dla osób bezbronnych), co skutkuje zaciągnięciem pożyczek w celu zapewnienia nadzwyczajnego wsparcia finansowego (program ryzyko gospodarcze), co samo w sobie skutkuje brakiem możliwości zapewnienia przez rząd opieki zdrowotnej osobom jej potrzebującym w czasie pandemii i po niej (kolejne ryzyko dla zdrowia). Podobnie niepilne podjęcie działań w związku z niezwykle niebezpieczną epidemią patogenów może mieć katastrofalne skutki, powodując załamanie społeczne i gospodarcze. Nie jest łatwo osiągnąć równowagę. W przypadku takich zdarzeń „całościowych” ryzyko spirali kryzysowej, w tym w wyniku reakcji, jest znacznie większe. Należy je traktować w kategorii zupełnie innej niż pozostałe zagrożenia. Zarządzanie tymi kwestiami w odpowiedzi na pandemię Covid-19 jest analizowane w późniejszych modułach niniejszego zapytania. Jasne jest jednak, że w obu scenariuszach ryzyko poważnych szkód gospodarczych oznacza, że Skarb Państwa odgrywa kluczową rolę w ocenie ryzyka. Oznacza to również, że należy wziąć pod uwagę wpływ na społeczeństwo i osoby, które mogą zostać najbardziej dotknięte. Różne reakcje na różne sytuacje kryzysowe będą miały szereg skutków ubocznych w całym społeczeństwie. Podstawowym aspektem każdej oceny ryzyka powinno być uwzględnienie potencjalnego wpływu na społeczeństwo i gospodarkę. |
| 3.48. | Ocena ryzyka narodowego i ocena ryzyka bezpieczeństwa narodowego skupiały się zasadniczo na pojedynczych sytuacjach kryzysowych.97 Od 2016 roku podejmowano próby pobudzania myślenia o ryzyku wystąpienia opisanego powyżej efektu domina.98 Jednakże, jak zauważyła Królewska Akademia Inżynierii, w rządzie Wielkiej Brytanii uznano, że wszechstronne myślenie o wzajemnie powiązanych ryzykach jest „kluczowym elementem, którego brakuje w obecnej metodologii”.99 |
| 3.49. | Na te ograniczenia zwrócono uwagę jeszcze przed pandemią. W lipcu 2019 r. profesor Vallance napisał do pani Hammond, w którym zauważył:
„Wiele ryzyk jest ze sobą powiązanych i może przyczyniać się do powstania innych zagrożeń lub je umożliwiać. To z kolei może zwiększyć pewne ryzyko. Zagadnienie to nie jest obecnie dostatecznie dobrze ujęte w art [Ocena ryzyka bezpieczeństwa narodowego] metodologia.”100 W swojej odpowiedzi pani Hammond zgodziła się, że należy zbadać tę kwestię.101 Kiedy jednak wybuchła pandemia, było już oczywiście za późno. |
| 3.50. | Jeżeli przed pandemią nie zostaną rozważone środki zaradcze w postaci interwencji niefarmaceutycznych, ich potencjalne skutki uboczne nie zostaną z wyprzedzeniem poddane rygorystycznej analizie. Rząd Wielkiej Brytanii przyznał się do tej słabości, ale dopiero od czasu pandemii. W kwietniu 2022 r. nowa ogólnobrytyjska Rada ds. Zdolności ds. Chorób Pandemicznych zauważyła, że obecne oceny:
„nie obejmują pełnej oceny ryzyka stosowania [interwencje niefarmaceutyczne]. Biorąc pod uwagę, że nałożenie izolacji częściowo spowodowało spadek PKB o 25% w okresie od lutego do kwietnia 2020 r., co stanowi największy spadek w historii, a także liczne skutki wtórne i trzeciorzędne dla wszystkich sektorów, stanowi to znaczna luka w brytyjskiej ocenie ryzyka pandemii.”102 (podkreślenie w oryginale) Rada zaleciła prowadzenie dalszych prac w celu sporządzenia dodatkowej oceny ryzyka oceniającej wpływ zmian w zachowaniach społeczeństwa, których oczekiwano podczas pandemii w różnych sektorach.103 Zaleciła także aktualizację oceny ryzyka gospodarczego przeprowadzonej przez rząd Wielkiej Brytanii w celu uwzględnienia szerszego zakresu skutków, w tym znaczącego potencjalnego wpływu |
| 3.51. | W dochodzeniu zgadza się, że była to słabość w procesie oceny ryzyka. Odpowiedzialność za to spoczywa na całym rządzie Wielkiej Brytanii:
|
| 3.52. | Królewska Akademia Inżynierii uznała, że podejście rządu Wielkiej Brytanii do wzajemnie powiązanych ryzyk wymaga innego sposobu myślenia niż w przypadku ryzyk indywidualnych.108 Te same obserwacje odnoszą się w równym stopniu do administracji zdecentralizowanej. W tym świetle we wrześniu 2021 r. Królewska Akademia Inżynierii zaleciła rządowi Wielkiej Brytanii konieczność przeprowadzenia wspólnego badania międzyrządowego w celu zmapowania wzajemnie powiązanych zagrożeń i planowania zdolności.109 |
| 3.53. | Analiza powiązań ryzyka może być zarówno trudna, jak i wymagać dużych zasobów.110 Chociaż w dochodzeniu uznano, że naprawienie tego niedociągnięcia w ocenie ryzyka nie jest łatwe, nie umniejsza to wagi tego działania. Odniesienia do tej kwestii w ramach odporności z grudnia 2022 r. oraz inicjatywa dotycząca programu pilotażowego Urzędu Rady Ministrów stanowią mile widzianą oznakę zaangażowania rządu Wielkiej Brytanii w realizację tego zalecenia.111 Wydaje się jednak, że ocena ryzyka bezpieczeństwa narodowego z 2022 r. nie zawiera żadnego odniesienia do wzajemnie powiązanych zagrożeń, a ramy czasowe poprawy zdolności w tym obszarze są niejasne.112 Nie ma dowodów na postęp w opublikowanej przez rząd Wielkiej Brytanii aktualizacji dotyczącej wdrażania ram odporności z grudnia 2023 r.113 |
Wada 4: Ryzyko długoterminowe i bezbronni ludzie
| 3.54. | Odporność zależy od posiadania odpornej populacji. Istnienie i utrzymywanie się bezbronności wśród ludności stanowi długoterminowe ryzyko dla Wielkiej Brytanii. Ryzyko długoterminowe różni się od ryzyka ostrego, ponieważ z biegiem czasu stopniowo wpływa na odporność.114 Szczególnej uwagi wymagają długoterminowe zagrożenia dla bezbronnych osób w społeczeństwie. Jak wyjaśnił profesor Walport, ryzyko to połączenie samego zagrożenia, narażenia na niebezpieczeństwo i podatności ludzi na niebezpieczeństwo.115 Najwyraźniejszym przykładem długoterminowego ryzyka, które pandemia uwidoczniła lub pogłębiła, jest podstawowy stan zdrowia populacji Wielkiej Brytanii przed 2020 r. W przypadku populacji niezdrowej ryzyko wystąpienia poważnych chorób i śmierci jest znacznie wyższe w wyniku choroba zakaźna. Jeżeli poziom złego stanu zdrowia nie będzie kontrolowany przez dłuższy czas, nieuniknioną konsekwencją będzie to, że najbardziej ucierpią osoby bezbronne z powodu złego stanu zdrowia. |
| 3.55. | Kiedy wybuchła pandemia, wiele osób, które ucierpiały, i wiele osób, które zmarły, było już bezbronnych. Z dowodów przedstawionych przez kilka organizacji wolontariackich, społecznych i przedsiębiorstw społecznych wynika, że zarówno choroba, jak i reakcja na sytuację nadzwyczajną miały nieproporcjonalny wpływ na osoby bezbronne.116 Profesor Vallance wyjaśnił:
"[T]oto straszna, straszna prawda, nad którą wszyscy musimy się zastanowić, a mianowicie, że wszystkie pandemie karmią się nierównością i ją napędzają. … To tragedia, którą należy zrozumieć.”117 |
| 3.56. | Jednak gdy Wielka Brytania przystąpiła do pandemii Covid-19, „[s]znaczne systematyczne nierówności w zdrowiu ze względu na status społeczno-ekonomiczny, pochodzenie etniczne, deprywację na poziomie obszaru, region, mniejszości wykluczone społecznie i grupy zdrowia włączające”.118 Profesorowie Clare Bambra i Sir Michael Marmot, eksperci ds. nierówności zdrowotnych (zob Załącznik 1: Informacje o tym module i metodologia badania) stwierdził, że katastrofalne wstrząsy spowodowane sytuacjami nadzwyczajnymi, takimi jak pandemie, uwidaczniają i pogłębiają istniejące nierówności w zdrowiu.119 Covid-19 nie był „wirus równych szans”.120 Skutkowało to większym prawdopodobieństwem zachorowań i śmierci wśród osób najbardziej bezbronnych w społeczeństwie.121 Profesorowie Bambra i Marmot byli zdania, że:
„Krótko mówiąc, Wielka Brytania weszła w pandemię z wyczerpaniem usług publicznych, zatrzymaniem poprawy stanu zdrowia, zwiększeniem nierówności w zdrowiu i pogorszeniem się stanu zdrowia najbiedniejszych ludzi.”122 |
| 3.57. | W ocenie ryzyka bezpieczeństwa narodowego z 2019 r. utrwalił się problem niewystarczającego uwzględnienia ryzyka dla osób bezbronnych.123 System oceny ryzyka nadzorowany przez Sekretariat ds. Zagrożeń Cywilnych oraz Departament Zdrowia i Opieki Społecznej nie uwzględnił w wystarczającym stopniu czynników – poza wiekiem i podatnością kliniczną – które mogą sprawić, że określone grupy populacji będą szczególnie podatne na epidemię patogenu.124 Pełna ocena scenariusza pandemii choroby grypopodobnej obejmowała jedynie krótką sekcję dotyczącą „wpływ na grupy wrażliwe”.125 Został on sformułowany zbyt wąsko iw zbyt ograniczonym stopniu skupiał się na wpływie na usługi publiczne i potencjał kadrowy. |
| 3.58. | W Krajowym Rejestrze Ryzyka na rok 2020 rzeczywiście znalazły się konkretne odniesienia do grup szczególnie wrażliwych i zagrożonych. Jednakże jego wytyczne dotyczące tego, jak osoby zaangażowane w gotowość i odporność powinny zająć się tymi kwestiami, były zbyt niejasne, aby były pomocne:
„[W]Podczas planowania i reagowania na te zagrożenia planiści z władz krajowych, samorządów lokalnych i grup społecznych mają do odegrania ważną rolę w łagodzeniu nieproporcjonalnego wpływu na te osoby.”126 |
| 3.59. | Gotowość na wypadek sytuacji awaryjnych (wytyczne ustawowe rządu Wielkiej Brytanii, opublikowane po raz pierwszy w 2006 r., a ostatnio zaktualizowane w 2012 r.) określają ogólne ramy ochrony ludności na mocy ustawy o nieprzewidzianych zdarzeniach cywilnych z 2004 r. i potwierdzają, że osoby bezbronne są „jedna grupa ludzi, których wszystkie plany awaryjne muszą uwzględniać”.127 Nie zapewnia jednak praktycznego zrozumienia podatności na zagrożenia do celów zapewnienia gotowości.128 Definicja podatności na zagrożenia w zakresie gotowości na wypadek sytuacji kryzysowych brzmi: „podatność osób lub społeczności, usług lub infrastruktury na szkody powstałe w wyniku sytuacji nadzwyczajnej lub innego zdarzenia”.129 Do celów planowania za osoby wymagające szczególnego traktowania uznaje się osoby mające problemy z poruszaniem się, problemy ze zdrowiem psychicznym, dzieci i kobiety w ciąży.130 Podobnie specjalne, nieustawowe wytyczne – Identyfikacja osób, które są podatne na zagrożenia w sytuacji kryzysowej z 2008 r. – definiują podatność na zagrożenia jako „które w sytuacji zagrożenia nie są w stanie same sobie pomóc”.131 |
| 3.60. | W momencie wejścia w pandemię większość planów nie definiowała grup osób bezbronnych, a te, które to zrobiły, przyjęły wąską definicję podatności na zagrożenia opartą wyłącznie na warunkach klinicznych.132 Michael Adamson, dyrektor naczelny Brytyjskiego Czerwonego Krzyża od listopada 2014 r., powiedział, że przy ocenie podatności na zagrożenia zbyt duży nacisk kładziono na podatność kliniczną, a za mało na szersze czynniki społeczne i ekonomiczne.133 |
| 3.61. | Definicje podatności na zagrożenia zawarte zarówno w ustawowych, jak i pozaustawowych wytycznych opracowanych przez Biuro Rady Ministrów były zbyt niejasne, aby mogły mieć jakąkolwiek użyteczność. Biuro Rady Ministrów nie korzystało z wiedzy specjalistycznej dostępnej w swoim własnym departamencie ani na zewnątrz, aby dowiedzieć się, jak identyfikować i chronić osoby bezbronne.134 Podobnie, chociaż organ Departamentu Zdrowia i Opieki Społecznej zajmujący się przygotowaniem na pandemię (Rada ds. gotowości na pandemię grypy) uznał w lutym 2018 r., że należy wyjaśnić znaczenie w przypadku pandemii słów „osoby bezbronne”, nie podjęto wystarczających działań.135 Planowanie na wypadek sytuacji nadzwyczajnej w Wielkiej Brytanii przed pandemią nie uwzględniało odpowiednio zakresu podatności na zagrożenia ani wpływu nierówności na osoby, które mogą być szczególnie dotknięte sytuacją nadzwyczajną lub reakcją na nią.136 |
| 3.62. | Ocena ryzyka bezpieczeństwa narodowego z 2022 r. zawierała nową sekcję zatytułowaną „Wytyczne dla grup szczególnie wrażliwych”.137 Zwróciła się do osób pełniących wiodącą rolę w zakresie ryzyka, aby podczas opracowywania scenariuszy rozważyły nieproporcjonalny wpływ, jaki ryzyko może mieć na grupy szczególnie wrażliwe. Jest to pozytywne zjawisko. Jednak nie idzie to wystarczająco daleko. Uwzględnia jedynie podstawowe skutki, które mogą wyniknąć z sytuacji awaryjnej. Sugeruje, że departamenty rządowe powinny wziąć pod uwagę inne skutki – na przykład skutki uboczne danej reakcji – ale nie określa, jakie mogą to być skutki ani w jaki sposób można je złagodzić (patrz powyżej w odniesieniu do wady 3). Znacznie większą wagę należy przywiązywać do skutków społecznych i gospodarczych. Należy odejść od przyczyn zagrożeń w kierunku minimalizacji ich skutków, szczególnie w przypadku osób najbardziej bezbronnych.138 |
| 3.63. | Jednym ze sposobów osiągnięcia tego celu jest lokalna ocena ryzyka. Mark Lloyd, dyrektor naczelny Stowarzyszenia Samorządów Lokalnych od listopada 2015 r., powiedział w dochodzeniu, że należy przeprowadzić dokładniejszą ocenę ryzyka na poziomie lokalnym.139 Zapytanie zgadza się. Pozwoliłoby to na skuteczniejsze uwzględnienie osób bezbronnych w bliższej ich sytuacji osobistej. Odzwierciedlałoby to również znaczenie lepszej oceny ryzyka na poziomie zdecentralizowanych administracji, aby uwzględnić indywidualne profile ich populacji. Gdyby tak się stało, ocena ryzyka w większym stopniu uwzględniałaby zakres podatności na zagrożenia oraz to, jak objawia się to na różne sposoby w populacji Wielkiej Brytanii. Ocena ryzyka powinna być wspólnym wysiłkiem, mającym zastosowanie do rządu centralnego, ale także na poziomie zdecentralizowanym, regionalnym i lokalnym.140 |
| 3.64. | Ponadto w dochodzeniu uznano, że powinna istnieć jedna definicja podatności na zagrożenia dla rządu Wielkiej Brytanii i zdecentralizowanych administracji. Powinno to uwzględniać cechy chronione na mocy ustawy o równości z 2010 r., ale także być wystarczająco szerokie i umożliwiać dostosowanie do okoliczności poważnej sytuacji nadzwyczajnej, w miarę gromadzenia informacji o jej potencjalnym szerszym wpływie. Należy wziąć pod uwagę wpływ, jaki zarówno działanie, jak i brak działania może mieć na osoby najbardziej narażone na krzywdę i cierpienie. Gdyby takie podejście zastosowano do wszystkich aspektów gotowości i odporności, ryzyko cierpienia i szkód – nie tylko w wyniku pandemii, ale w wyniku reakcji – zostałoby zmniejszone. |
| 3.65. | W swoich ramach dotyczących odporności z grudnia 2022 r. rząd Wielkiej Brytanii wskazał, że zbada nowy proces identyfikacji i oceny ryzyka długoterminowego, w tym jego wpływu na osoby bezbronne.141 W aktualizacji dotyczącej wdrożenia z 2023 r. sugeruje się, że ustanowiono nowy proces identyfikacji i oceny tego rodzaju długoterminowych wyzwań, ale obiecuje jedynie, że: „Więcej szczegółów na temat tych prac będzie dostępnych w 2024 r.”142 Prace nad tą sprawą są w dalszym ciągu prowadzone w Gabinecie Rady Ministrów – prawie trzy lata po zewnętrznej ocenie Królewskiej Akademii Inżynierskiej. |
Wada 5: Możliwości i pojemność
| 3.66. | Niezwykle istotne jest, aby ocena ryzyka była powiązana z praktycznymi możliwościami i możliwościami, a mianowicie z tym, co faktycznie można zrobić w reakcji na sytuację nadzwyczajną. W ten sposób ocenę ryzyka należy powiązać ze strategią i planowaniem, które muszą uwzględniać rzeczywistość pod względem gotowości i odporności w terenie. Jeśli ocena ryzyka nie uwzględnia tego, co jest, a co nie jest praktycznie wykonalne, jest to ćwiczenie akademickie odległe od tych, na których ostatecznie będzie miało wpływ. To właśnie wydarzyło się w Wielkiej Brytanii. |
| 3.67. | W dochodzeniu uznano, że lepszym podejściem do oceny ryzyka byłoby kontynuacja oceny ryzyka. Po pierwsze, zidentyfikuj ryzyko i zbuduj możliwości niezbędne do zapobiegania mu lub reagowania na nie. Po drugie, cofnij się od możliwości, które obecnie istnieją lub których istnienia można zasadnie oczekiwać, aby obliczyć ryzyko. Na przykład, gdyby Wielka Brytania miała możliwość testowania, śledzenia i izolowania na dużą skalę oraz przy zachowaniu elastycznego poziomu zdolności w systemie opieki zdrowotnej i społecznej, wpływ pandemii na populację – a tym samym ryzyko – prawdopodobnie zostanie zmniejszony . Podobnie, jeśli finanse publiczne będą w dobrej kondycji, rządy będą w stanie zapewnić wsparcie gospodarcze podczas pandemii, co zmniejszy ryzyko, że sytuacja nadzwyczajna zdrowotna stanie się nadzwyczajną sytuacją gospodarczą. |
| 3.68. | Konieczność podejmowania decyzji „opierają się na wpływie i gotowości powiązanej ze zdolnościami w zakresie zapobiegania, łagodzenia, reagowania i odbudowy” było jednym z kluczowych zaleceń Królewskiej Akademii Inżynierii i powracającym tematem w jej raporcie.143 Nie jest jasne, jakie dokładnie prace podejmuje rząd Wielkiej Brytanii w celu wdrożenia tego zalecenia.144 |
Doskonalenie oceny ryzyka
| 3.69. | W rządzie Wielkiej Brytanii i administracjach zdecentralizowanych konieczna jest fundamentalna i trwała poprawa oceny ryzyka, zarówno w przypadku pandemii, jak i innych katastrof cywilnych obejmujących cały system. Rząd Wielkiej Brytanii i zdecentralizowane administracje powinny przeprowadzić oceny ryzyka, które odzwierciedlają okoliczności i cechy charakterystyczne Anglii, Walii, Szkocji, Irlandii Północnej i Wielkiej Brytanii jako całości, takie jak ich demografia i położenie geograficzne. |
| 3.70. | Powinny one uwzględniać wszystkie pięć wad zbadanych w tym rozdziale, aby oceny ryzyka:
|
| 3.71. | Jeżeli ocena ryzyka nie zostanie przeprowadzona prawidłowo, całe podejście do gotowości i odporności zaczyna się w niewłaściwym miejscu. Ponieważ ocena ryzyka stanowi podstawę całego systemu gotowości i odporności – pod względem strategii, struktur, doradztwa oraz umiejętności, technologii i infrastruktury niezbędnych do skutecznego reagowania – należy ją pilnie ulepszyć. Chociaż ocena ryzyka stanowi dziedzinę wiedzy technicznej, należy ją powiązać z rzeczywistymi możliwościami i możliwościami Wielkiej Brytanii, a także mieć na uwadze konsekwencje dla osób szczególnie dotkniętych katastrofami cywilnymi obejmującymi cały system, takimi jak pandemie. W dochodzeniu zalecono zatem ogólną poprawę podejścia. |
Zalecenie 3: Lepsze podejście do oceny ryzyka
Rząd Wielkiej Brytanii i zdecentralizowane administracje powinny współpracować nad opracowaniem nowego podejścia do oceny ryzyka, które odejdzie od polegania na pojedynczych rozsądnych najgorszych scenariuszach w stronę podejścia, które:
- ocenia szerszy zakres scenariuszy reprezentatywnych dla różnych ryzyk i zakres każdego rodzaju ryzyka;
- oprócz radzenia sobie z jej konsekwencjami uwzględnia zapobieganie sytuacjom nadzwyczajnym i łagodzenie ich skutków;
- zapewnia pełną analizę sposobów, w jakie połączone skutki różnych zagrożeń mogą skomplikować lub pogorszyć sytuację nadzwyczajną;
- oprócz krótkoterminowych ocenia ryzyko długoterminowe i rozważa, w jaki sposób mogą one na siebie oddziaływać;
- dokonuje oceny wpływu każdego ryzyka na osoby bezbronne; I
- uwzględnia potencjał i możliwości Wielkiej Brytanii.
Czyniąc to, rząd Wielkiej Brytanii i zdecentralizowane administracje powinny przeprowadzić oceny ryzyka, które odzwierciedlają okoliczności i cechy charakterystyczne Anglii, Walii, Szkocji, Irlandii Północnej i Wielkiej Brytanii jako całości.
- Ramy odporności rządu Wielkiej Brytanii, Rząd Jej Królewskiej Mości, grudzień 2022 r., pkt 14 (https://www.gov.uk/government/publications/the-uk-government-resilience-framework; INQ000097685)
- Zobacz na przykład Denis McMahon 6 lipca 2023 r. 28/23–29/4
- INQ000181825_0003 ust. 11-13; INQ000145912_0012-0030, 0072-0073 pkt 6,15-6,18, 6,22-6,24, 6,28, 6,33-6,36, 6,40-6,41, 6,43, 6,45-6,46, 6,50-6,52, 6,55-6,58, 6,62-6,63, 6,66-6,68, 6,71-6,72, 6,74-6,75, 6,82 -6,86, 9,5-9,6, 9,9
- INQ000181825_0006 ust. 23
- INQ000183334
- INQ000183334_0011 ust. 10
- INQ000145912_0005 ust. 5.1.3
- INQ000145733_0008-0009 ust. 2.22; INQ000145912_0007-0008 pkt 6.3, 6.5
- INQ000147769_0007; INQ000147771_0006; INQ000145912_0007 ust. 6.3; INQ000182612_0013 ust. 3.7
- 10 INQ000147769_0007; INQ000147771_0006; INQ000145912_0007 ust. 6.3; INQ000182612_0013 ust. 3.7
- INQ000147771_0006; INQ000145912_0007 ust. 6.3; INQ000182612_0013, 0023 pkt 3.9, 3.43
- INQ000145912_0007, 0011-0012, 0073 pkt 6.1.1, 6.3, 6.12, 9.9; INQ000182612_0012 pkt 3.3, 3.5
- Krajową ocenę ryzyka opracowano po raz pierwszy w 2005 r., z corocznymi zmianami w latach 2006–2014, a ostateczną wersję w 2016 r. (zob. INQ000145912_0014-0019, 0021-0022, 0024-0027, 0072-0073 pkt 6,22–6,32, 6,40–6,44, 6,50–6,54, 6,62–6,65, 6,71–6,73, 9,5–9,6, 9,9; INQ000182612_0015-0016, 0019-0021 pkt 3.18–3.19, 3.27–3.30, 3.33–3.37; INQ000147769_0007). Ocenę ryzyka bezpieczeństwa narodowego opracowano po raz pierwszy w 2010 r., a zmiany w latach 2012 i 2015, a ostateczną wersję opracowano w 2017 r. (zob. INQ000182612_0014-0022 pkt 3.14–3.17, 3.20–3.26, 3.31–3.32, 3.38–3.42). Nową, połączoną ocenę ryzyka bezpieczeństwa narodowego po raz pierwszy opracowano w 2019 r., a aktualną wersję w 2022 r. (zob. INQ000145912_0029-0030 pkt 6.82–6.86; INQ000182612_0023-0024 pkt 3.43-3.48). Krajowy Rejestr Ryzyka powstał po raz pierwszy w 2008 r., a następnie został zweryfikowany w latach 2010, 2012, 2013, 2015, 2017 i 2020; aktualna wersja jest datowana na rok 2023 (INQ000145912_0012-0013, 0017-0018, 0019-0021, 0022-0024, 0025-0026, 0028-0029, 0030_0031, 0073 pkt 6,15–6,21, 6,33–6,39, 6,45–6,49, 6,55–6,61, 6,66–6,70, 6,74–6,81, 6,87–6,90, 9,9).
- INQ000020678_0003; INQ000185352_0005 ust. 16; INQ000185343_0003 ust. 10
- INQ000184894_0021 ust. 75; INQ000185352_0005 ust. 16; INQ000102940_0003
- Gillian Russell 28 czerwca 2023 r. 40/17–19
- Gillian Russell 28 czerwca 2023 51/25-60/3; Caroline Lamb 28 czerwca 2023 109/18-110/8
- INQ000130469_0038 ust. 154; INQ000190662_0025-0026 pkt 90–91
- Andrew Goodall 4 lipca 2023 r., 7.1-7.07
- Mark Drakeford 4 lipca 2023 r. 170/11-173/21
- INQ000187580_0026, 0032 Zalecenie 2
- Andrew Goodall 4 lipca 2023 3/6-4/3, 6/15-7/7
- Mark Drakeford 4 lipca 2023 r. 179/3-4
- Reg Kilpatrick 6 lipca 2023 r. 132/9-13; Zobacz też INQ000190662_0025-0026 pkt 90–91
- INQ000128968_0006-0008
- INQ000215558
- INQ000130469_0041 paragraf 162
- INQ000128968_0006; INQ000215558; Andrew Goodall 4 lipca 2023 r. 18.05-19.05
- Andrew Goodall 4 lipca 2023 r. 19.20-22.05
- Denis McMahon 6 lipca 2023 63/20-21
- INQ000187620_0044 ust. 177; INQ000086936; INQ000086937
- INQ000086936_0020-0022 ust. 4-10
- INQ000086936_0014, 0022, 0027; INQ000086937_0014
- Denis McMahon 6 lipca 2023 r. 22.02-21.10
- INQ000187620_0045 ust. 182; INQ000217257
- INQ000185379_0006, 0024-0025
- Richard Pengelly 11 lipca 2023 84/14-88/4
- INQ000068403_0006; INQ000145912_0111 ust. 10.2.2; INQ000182612_0023-0024 pkt 3.47
- INQ000185338_0004 ust. 17
- INQ000145912_0117-0121 pkt 10.7-10.8; INQ000182612_0023-0024 pkt 3.47–3.48; Krajowy Rejestr Ryzyka, Rząd Jej Królewskiej Mości, 2023 (https://assets.publishing.service.gov.uk/media/64ca1dfe19f5622669f3c1b1/2023_NATIONAL_RISK_REGISTER_NRR.pdf; INQ000357285)
- INQ000068403_0053 sekcja 7.1
- INQ000147770_0004-0006; INQ000147768_0007-0009; Katharine Hammond 16 czerwca 2023 148/25-149/12
- INQ000068403_0053 sekcja 7.1
- The 2009 Influenza Pandemic: Niezależny przegląd reakcji Wielkiej Brytanii na pandemię grypy w 2009 r., Dame Deirdre Hine, lipiec 2010 r., pkt 4.50–4.55, zalecenie 11 (https://assets.publishing.service.gov.uk/media/5a7975f1ed915d0422068a10/the2009influenzapandemic-review.pdf; INQ000022705)
- INQ000147775_0004 przypis 3; INQ000147768_0009; INQ000147770_0005
- INQ000147775_0004; INQ000147768_0008-0009; INQ000147770_0004-0005
- W przypadku krajowych ocen ryzyka z 2014 r. i 2016 r. wykluczono ryzyko, jeśli prawdopodobieństwo jego wystąpienia przynajmniej raz w ciągu najbliższych pięciu lat wynosi mniej niż 1 na 20 000: INQ000147775_0004 przypis 4; INQ000147768_0008. W ocenie ryzyka bezpieczeństwa narodowego na rok 2019 wykluczono ryzyko, jeśli prawdopodobieństwo jego wystąpienia w ciągu najbliższego roku do dwóch lat wynosi mniej niż 1 na 100 000 (INQ000147770_0004).
- INQ000147775_0004 przypis 5; INQ000147768_0008; INQ000147770_0004; Zobacz też INQ000182612_0013, 0026 ust. 3.7, 3.55
- W krajowej ocenie ryzyka z 2014 r. określana jako „H23 (DH)… choroba grypowa (pandemia)” (INQ000176765_0001), „Pandemia grypy H23 (DH)” w Krajowej ocenie ryzyka z 2016 r. (INQ000147769_0047; INQ000176770_0001) oraz „Pandemia choroby grypopodobnej R95-DHSC” w ocenie ryzyka bezpieczeństwa narodowego z 2019 r. (INQ000147771_0138; INQ000176776_0001).
- W krajowej ocenie ryzyka z 2014 r. określane jako „H24 (DH)… pojawiające się choroby zakaźne” (INQ000176766_0001), „Pojawiające się choroby zakaźne H24 (DH)” w krajowej ocenie ryzyka z 2016 r. (INQ000147769_0048; INQ000176771_0001) oraz „Pojawiająca się choroba zakaźna… (R97-DHSC)” w ocenie ryzyka bezpieczeństwa narodowego z 2019 r. (INQ000147771_0140; INQ000185135_0001).
- INQ000196611_0009 przypis 2; INQ000148429_0059 paragraf 234
- Katharine Hammond 16 czerwca 2023 116/11-14; INQ000145733_0032 pkt 5.10-5.11
- Christopher Wormald 19 czerwca 2023 106/1-10, 108/1-109/9
- INQ000176766_0003; INQ000176771_0003; INQ000013824_0003-0004 ust. 5.1; INQ000148360_0010
- INQ000145912_0029-0030 pkt 6.82-6.85
- Christopher Whitty, 22 czerwca 2023 r., 93.11-22; Sally Davies, 20 czerwca 2023 r., 146/8-18
- INQ000176766_0003; INQ000176771 _0004
- INQ000013824_0004 pkt 5.3.2-5.3.3
- INQ000145912_0018, 0020, 0023-0024, 0026, pkt 6.39.1, 6.46.5, 6.49.1, 6.61, 6.71.1
- INQ000179082_0003, 0006
- INQ000001332_0004 trzeci akapit
- INQ000068403_0095 sekcja 11.4
- INQ000147707_0048 pkt 143, 145; Mark Walport 21 czerwca 2023 r. 24.05-36.21, 56/6-22; INQ000147810_0009 ust. 26; INQ000148419_0011-0012 pkt 5.2-5.3; Christopher Whitty 22 czerwca 2023 r. 100/16-101/5
- Widzieć Christopher Whitty 22 czerwca 2023 111/15-19
- INQ000145733_0033 ust. 5.14
- INQ000145733_0033 ust. 5.13
- INQ000176770_0009; INQ000176771_0006-0007; INQ000176776_0005-0006; INQ000185135_0004-0007
- INQ000068403_0097 sekcja 11.5
- Oliver Letwin 20 czerwca 2023 20.01-21.15
- Mark Walport 21 czerwca 2023 46/5-24; Patrick Vallance 22 czerwca 2023 158/13-25
- Zobacz np. zgłoszenia w imieniu Departamentu Zdrowia (Irlandia Północna) 13 czerwca 2023 r. 142/3; zgłoszenia w imieniu Biura Rządu ds. Nauki 14 czerwca 2023 r. 10/18; zgłoszenia w imieniu Departamentu Zdrowia i Opieki Społecznej 14 czerwca 2023 20.14-16; Matt Hancock 27 czerwca 2023 30/3-5, 101/9-16
- Pomysłodawcą wydarzenia „czarnego łabędzia” był Nassim Nicholas Taleb. Zobacz: Czarny łabędź: wpływ wysoce nieprawdopodobnego, Random House, 2007 (INQ000369660_xvii-xviii).
- David Alexander 15 czerwca 2023 23.105-106.13; Bruce Mann 15 czerwca 2023 108/10-13
- INQ000177810_0004 ust. 15
- INQ000147772_0121-0123; INQ000145912_0118 pkt 10.8.7-10.8.8
- INQ000145912_0118 pkt 10.8.7-10.8.10
- INQ000181825_0008 ust. 30
- INQ000181825_0013 pkt 52–54
- Jeremy Hunt 21 czerwca 2023 r. 168/6-14
- Christopher Whitty 22 czerwca 2023 102/3-7
- Christopher Whitty 22 czerwca 2023 102/8-16
- INQ000148419_0012-0013 ust. 5.5
- INQ000176776_0002
- INQ000176765_0005-0006; INQ000147767_0027; INQ000147769_0047; INQ000176770_0001
- INQ000185135_0002. Chociaż w krajowych ocenach ryzyka z 2014 r. i 2016 r. nie było wyraźnego odniesienia do środków kontroli zakażeń, podobna liczba ofiar śmiertelnych i ofiar przewidziana w uzasadnionych najgorszych scenariuszach dotyczących pojawiających się chorób zakaźnych stanowczo wskazuje na to, że przyjęły one podobne podejście.
- INQ000068403_0022 sekcja 4.2.1
- INQ000142113_0001
- INQ000142145_0001; INQ000142120_0001
- Mark Walport 21 czerwca 2023 42/8-9
- Mark Walport 21 czerwca 2023 30/25-31/1; Zobacz też Mark Walport 21 czerwca 2023 42/13-14
- INQ000186622_0009-0010
- INQ000127915_0006 ust. 23
- INQ000187355_0004 ust. 8 lit. d)
- David Alexander 15 czerwca 2023 96/3-97/2; Mark Walport 21 czerwca 2023 33/2-15
- INQ000203349_0016 przypisy 30 i 31. Techniczne wyjaśnienie ryzyk „współbieżnych”, „złożonych”, „kaskadowych” i „współzależności” można znaleźć w: INQ000068403_0023-0024, 0035-0036, 0146-0147 sekcje 4.2.3, 6.1-6.1.2, załącznik G; INQ000203349_0016 pkt 20 lit. d), przypisy 30–31.
- INQ000147707_0033 paragraf 86
- INQ000147769_0019; INQ000147768_0010; INQ000147770_0013
- INQ000147769_0019; INQ000147768_0010; INQ000147770_0013
- INQ000068403_0023 sekcja 4.2.3
- INQ000213808_0001
- INQ000213809_0001
- INQ000087205_0004 paragraf 16. Rada ds. Zdolności ds. Chorób Pandemicznych była międzyrządową grupą obejmującą całą Wielką Brytanię utworzoną w lipcu 2021 r. w celu pracy nad przygotowaniem na szeroki zakres pandemii, w tym między innymi grypę pandemiczną (INQ000057649_0001 ust. 1-2). Zastąpiła Radę ds. gotowości na pandemię grypy.
- INQ000087205_0004-0005 zalecenia 2, 2.1
- INQ000087205_0005 ust. 20
- INQ000145912_0007-0008 pkt 6.3, 6.5, 6.6; INQ000182612_0013 pkt 3.8-3.9; INQ000203351_0009-0012 pkt 33–45
- INQ000184643_0051, 0076 pkt 274, 398; INQ000203351_0009-0012 pkt 33–45
- INQ000182612_0028-0029 ust. 3.70
- INQ000068403_0023 sekcja 4.2.3
- INQ000068403_0093 sekcja 11.3
- INQ000068403_0036-0038, 0094 sekcje 6.2.1, 11.3.2
- The UK Government Resilience Framework, Rząd Jej Królewskiej Mości, grudzień 2022, s. 9, 66 (Załącznik B) (https://www.gov.uk/government/publications/the-uk-government-resilience-framework; INQ000097685); INQ000145912_0118 pkt 10.8.5-10.8.6
- The UK Government Resilience Framework, Rząd Jej Królewskiej Mości, grudzień 2022, s. 9, 66 (Załącznik B) (https://www.gov.uk/government/publications/the-uk-government-resilience-framework; INQ000097685); INQ000145912_0118 pkt 10.8.5-10.8.6
- Ramy dotyczące odporności rządu Wielkiej Brytanii: aktualizacja wdrożenia z 2023 r., Gabinet Rady Ministrów, 4 grudnia 2023 r., pkt 9–10 (https://assets.publishing.service.gov.uk/media/656def711104cf0013fa7498/The_UK_Government_Resilience_Framework_2023_Implementation_Update.pdf; INQ000372824)
- Zobacz dyskusje na temat długoterminowych ryzyk „chronicznych”, krótkoterminowych „ostrych” ryzyk i podatności na zagrożenia w INQ000068403_0146-0147 Załącznik G; INQ000147772_0005, 0010
- Mark Walport 21 czerwca 2023 41/3-6
- Należą do nich Age UK (INQ000106031_0009-0011, 0013-0014, 0022 pkt 29–35, 41–44, 71–72), Brytyjskie Stowarzyszenie Medyczne (INQ000205177_0009-0012, 0016 pkt 28–29, 34–35, 40–41, 42(f)), Rodziny w trudnej sytuacji klinicznej (INQ000137308_0002, 0012-0015 pkt 5, 18–20), Coram (INQ000108530_0013-0016, 0018, 0019 pkt 33-36, 40-42, 44, 50, 53), Disability Rights UK (INQ000185333_0002-0006 pkt 6, 8, 10-23), Doctors of the World UK (INQ000148404_0002-0008 pkt 7-22, 24), Federacja Organizacji Mniejszości Etnicznych Opieki Zdrowotnej (INQ000174832_0001-0003, 0004 ust. 3, 7-8, 11-12), Fundacja Zdrowia (INQ000183420_0008-0009, 0014 pkt 24, 42), Wspólna Rada ds. Opieki nad Imigrantami (INQ000184644_0004-0006, 0010-0013, 0015, 0018 pkt 15–21, 38, 41–46, 56, 65), Medact (INQ000148410_0004, 0006-0007 pkt 11–12, 18–19, 21), Konfederacja NHS (INQ000147815_0017, 0021 pkt 61–62, 77), Runnymede Trust (INQ000195842_0001-0006 pkt 1, 3, 6-15), Pomoc dla Kobiet Solace (INQ000108557_0003, 0006-0009 pkt 10–11, 20, 25–29), Southall Black Sisters (INQ000108571_0003-0008, 0011-0013, 0016-0017 pkt 11-16, 18-19, 22-23, 32, 36, 43), WinVisible (kobiety z widoczną i niewidoczną niepełnosprawnością) (INQ000191132_0003, 0005-0007 pkt 6-7, 17, 20, 22-25).
- Patrick Vallance 22 czerwca 2023 165/5-9
- INQ000195843_0029 paragraf 58
- INQ000195843_0074 paragraf 179
- Richard Horton 13 lipca 2023 74/11
- INQ000195843_0075 paragraf 181
- INQ000195843_0029 paragraf 58
- INQ000147771_0138, 0140
- Christopher Wormald 19 czerwca 2023 151/19-25
- INQ000176776_0004-0005
- Krajowy Rejestr Ryzyka, Rząd Jej Królewskiej Mości, 2020, s. 21 (https://assets.publishing.service.gov.uk/media/6001b2688fa8f55f6978561a/6.6920_CO_CCS_s_National_Risk_Register_2020_11-1-21-FINAL.pdf; INQ000055874)
- Gotowość na wypadek sytuacji nadzwyczajnych, Gabinet Rady Ministrów, rozdział 5, poprawiony w październiku 2011 r., pkt 5.98 (https://assets.publishing.service.gov.uk/media/5a789f9140f0b62b22cbb78e/Emergency_Preparedness_chapter5_amends_21112011.pdf; INQ000080807_0039)
- Gotowość na wypadek sytuacji nadzwyczajnych, Gabinet Rady Ministrów, rozdział 5, poprawiony w październiku 2011 r., pkt 5.99 (https://assets.publishing.service.gov.uk/media/5a789f9140f0b62b22cbb78e/Emergency_Preparedness_chapter5_amends_21112011.pdf; INQ000080807_0039)
- Gotowość na wypadek sytuacji nadzwyczajnych, Gabinet Rady Ministrów, Glosariusz, wersja poprawiona z marca 2012 r. (https://assets.publishing.service.gov.uk/media/5a75afda40f0b67f59fced2b/EP_Glossary_amends_18042012_0.pdf; INQ000080808_0029); INQ000195843_0004 ust. 2
- Gotowość na wypadek sytuacji kryzysowych, Gabinet Rady Ministrów, rozdział 5, poprawiony w październiku 2011 r., pkt 5.103 (https://assets.publishing.service.gov.uk/media/5a789f9140f0b62b22cbb78e/Emergency_Preparedness_chapter5_amends_21112011.pdf; INQ000080807_0040)
- INQ000097681_0004 ust. 4; Identyfikacja osób, które są podatne na zagrożenia w sytuacjach kryzysowych, Sekretariat ds. nieprzewidywalnych sytuacji cywilnych, Biuro Rady Ministrów, luty 2008 r., s. 4 ust. 4 (https://assets.publishing.service.gov.uk/media/5a799f0ded915d0422069d24/vulnerable_guidance.pdf; INQ000080825); INQ000195843_0061 pkt 146.1.3
- INQ000195843_0059 ust. 145.6.4; INQ000147709_0010 ust. 38; INQ000137505_0010
- INQ000182613_0013-0014 ust. 54
- Marcus Bell 13 lipca 2023 20.07-8.02; Melanie Field 13 lipca 2023 25.08-26.15
- INQ000022908_0004 ust. 4.2. W 2017 r. powołano Radę ds. gotowości na pandemię grypy, pod wspólnym przewodnictwem Gabinetu Rady Ministrów i Departamentu Zdrowia, w celu realizacji międzyrządowego i obejmującego całą Wielką Brytanię programu prac skupiającego się na gotowości na pandemię grypy. Omówiono to szczegółowo w Rozdziale 5: Uczenie się na podstawie doświadczeń. Profesor Bambra potwierdziła podczas dochodzenia, że w 40 dokumentach, które sprawdziła, nie ma wspólnej definicji osób bezbronnych lub osób cierpiących z powodu nierówności zdrowotnych, w tym dokumentów odnoszących się do ustawy o nieprzewidzianych zdarzeniach cywilnych z 2004 r. i ustawy o grypie pandemicznej (2019): Clare Bambra 16 czerwca 2023 r. 46/7-23 (INQ000195843_0061-0063 pkt 146–146.4).
- INQ000182613_0013-0014 ust. 54
- INQ000147807_0102-0103
- Oliver Letwin 20 czerwca 2023 20/2-11
- INQ000177803_0041 paragraf 150
- 1INQ000068403_0093 sekcja 11.3; David Alexander 15 czerwca 2023 147/1-6
- Ramy odporności rządu Wielkiej Brytanii, Rząd Jej Królewskiej Mości, grudzień 2022 r., pkt 14–20 (https://www.gov.uk/government/publications/the-uk-government-resilience-framework; INQ000097685)
- Ramy dotyczące odporności rządu Wielkiej Brytanii: aktualizacja wdrożenia z 2023 r., Gabinet Rady Ministrów, grudzień 2023 r., s. 14 (https://assets.publishing.service.gov.uk/media/656def711104cf0013fa7498 The_UK_Government_Resilience_Framework_2023_Implementation_Update.pdf; INQ000372824)
- INQ000068403_0009, 0080, 0097-0098
- INQ000145912_0118 pkt 10.8.9-10.8.10
Rozdział 4: Skuteczna strategia
Wstęp
| 4.1. | Strategia opiera się na ocenie ryzyka. Chociaż podejście do ryzyka polega na technicznej ocenie tego, co może się wydarzyć, skuteczna strategia to inna i odrębna ocena tego, jak najlepiej złagodzić ryzyko lub jego wpływ. Strategia powinna umożliwiać planowanie najważniejszych kwestii w warunkach niepewności. W przypadku gotowości na wypadek pandemii strategia powinna dotyczyć najlepszego sposobu reagowania na ogólnosystemową sytuację nadzwyczajną spowodowaną wybuchem choroby i wyjścia z niej. |
| 4.2. | W tym rozdziale zbadano skuteczność jedynej strategii na skalę pandemii obowiązującej w Wielkiej Brytanii w momencie wybuchu pandemii wirusa Covid-19 – strategii Strategia gotowości na wypadek pandemii grypy w Wielkiej Brytanii w 2011 r (strategia z 2011 r.).¹ Rozważa, co powinna obejmować skuteczna strategia na wypadek sytuacji kryzysowych dla ludności obejmujących cały system, takich jak pandemie, oraz w jaki sposób można ją ulepszyć za pomocą danych i badań. |
| 4.3. | Ponieważ zdrowie jest jedną z kwestii powierzonych rządom Szkocji, Walii i Irlandii Północnej, każdy zdecentralizowany kraj mógł przyjąć inne podejście. Każdy z nich zdecydował się przyjąć strategię z 2011 r. Na przykład w Szkocji nie było dyskusji na temat dostosowania strategii z 2011 r., aby uczynić ją bardziej skoncentrowaną na Szkocji². Założeniem kluczowych wytycznych zarówno w Walii, jak i Irlandii Północnej była strategia z 2011 r.³ Ocena przeprowadzona w ramach dochodzenia dotycząca strategii z 2011 r. Strategia ma zatem takie samo zastosowanie do poszczególnych krajów zdecentralizowanych, jak i do całej Wielkiej Brytanii. Wszystkie rządy Wielkiej Brytanii uznały, że gotowość na wypadek pandemii jest, przynajmniej w zasadzie, kwestią wymagającą koordynacji w całej Wielkiej Brytanii. Gdyby istniały fundamentalne wady, miałoby to – i miało – wpływ na cały system gotowości w Wielkiej Brytanii. |
Strategia na rok 2011
| 4.4. | Strategia z 2011 r. była strategią Wielkiej Brytanii dotyczącą reagowania w sytuacjach kryzysowych, mającą na celu przygotowanie się na pandemię i reagowanie na nią. Chociaż stwierdzono, że jest to strategia na wypadek pandemii grypy, miała być wystarczająco elastyczna i łatwa do dostosowania do zastosowania w przypadku innych pandemii.⁴ Została opublikowana w listopadzie 2011 r. przez Ministerstwo Zdrowia po przeglądzie przeprowadzonym w 2010 r. przez Dame Deirdre Zwróćmy uwagę na reakcję Wielkiej Brytanii na pandemię grypy H1N1 („świńska grypa”) w latach 2009–2010.⁵ Nie została ona zaktualizowana przed pandemią Covid-19 i od tego czasu pozostaje niezmieniona.⁶ |
| 4.5. | Odpowiedzialność za Strategię na rok 2011 przed pandemią Covid-19 została przedłużona na kadencję trzech Sekretarzy Stanu ds. Zdrowia (Zdrowie i Opieka Społeczna od stycznia 2018 r.): poseł Andrew Lansley (od maja 2010 r. do września 2012 r.), poseł Jeremy Hunt (od wrzesień 2012 r. – lipiec 2018 r.) i poseł Matt Hancock (od lipca 2018 r. do czerwca 2021 r.). |
Mocne strony Strategii 2011
| 4.6. | Celem Strategii na rok 2011 było:
|
| 4.7. | Miały one zostać osiągnięte poprzez odniesienie do trzech kluczowych zasad:
|
| 4.8. | W strategii z 2011 r. uznano, że przygotowania na pandemię polegają nie tylko na minimalizowaniu jej potencjalnego i natychmiastowego wpływu na zdrowie ludności, ale także na minimalizowaniu potencjalnego wpływu pandemii i reakcji rządów na społeczeństwo i gospodarkę jako całość. |
| 4.9. | Pandemia to tylko jedno z wielu wyzwań i sytuacji nadzwyczajnych, przed którymi może stanąć kraj. Dzisiejszy rząd jest odpowiedzialny za krótko-, średnio- i długoterminowe interesy Wielkiej Brytanii. W samych celach Strategii na rok 2011 nie było nic złego. Zaprosili przywódców politycznych, aby w przypadku pandemii zrównoważyli priorytety i rozważyli kompromisy między konkurującymi interesami. Gdyby przed wybuchem pandemii wzięto pod uwagę różne, czasem konkurencyjne interesy, Wielka Brytania w naturalny sposób miałaby lepszą bazę dla swojej strategii i reakcji na pandemię. Do zainteresowań tych zaliczać się będą np.:
|
| 4.10. | W strategii z 2011 r. słusznie wskazano, że wpływ pandemii na populację i szersze społeczeństwo będzie zależał od trzech czynników:
|
| 4.11. | Te aspekty strategii na rok 2011 zasługują na pochwałę. Jednak w wielu istotnych aspektach zawierał także błędy. |
Kluczowe błędy Strategii z 2011 roku
| 4.12. | Główne wady strategii na 2011 r. zidentyfikowane w toku dochodzenia to:
|
Wada 1: Niewłaściwe uwzględnienie profilaktyki
| 4.13. | Zgodnie z założeniami planistycznymi Strategii z 2011 r. Wielka Brytania planowała pandemię grypy, podczas której objawy miałyby 50% populacji, z czego 2,5% umrze, przy założeniu braku skutecznego leczenia.¹⁰ Od 1% do 4% objawowych pacjenci wymagaliby opieki szpitalnej, w zależności od ciężkości choroby wywołanej wirusem.¹¹ Przyjęto, że prawdopodobnie nastąpi zwiększone zapotrzebowanie na usługi intensywnej terapii.¹² Podobnie przewidywano, że opieka zdrowotna i społeczna zostanie umieszczona w kategorii „większe napięcie” – służby intensywnej terapii mogą być zagrożone „przytłoczony” i byłoby „szczególne wyzwania” w utrzymaniu usług opieki społecznej.¹³ |
| 4.14. | Odnosząc założenia do populacji Wielkiej Brytanii w 2020 r. wynoszącej około 67 mln osób, w praktyce oznaczało to, że umrze aż 837 500 osób.¹⁴ Strategia z 2011 r. stwierdzała, że już w ciągu pierwszych 15 tygodni pandemii celem było „radzić sobie z” 210 000–315 000 dodatkowych zgonów, z czego być może połowa miała miejsce w ciągu zaledwie trzech tygodni w szczytowym momencie epidemii.¹⁵ Kiedy mówiono, że Wielka Brytania była dobrze przygotowana przed pandemią Covid-19, oznaczało to wówczas, że Wielka Brytania powinna była być w stanie zaradzić śmierci takiej liczby osób – nie dlatego, że była przygotowana, aby im zapobiec. |
| 4.15. | Strategie mające na celu uniknięcie tego rodzaju całkowitej epidemii są szczegółowo badane w module 2 niniejszego badania i można je podzielić na łagodzenie i tłumienie. Chociaż jasne definicje każdej strategii nie są powszechnie uzgodnione, można je opisać w następujący sposób:
|
| 4.16. | Obydwa podejścia mają ograniczenia, a ich skutki zależą całkowicie od charakterystyki patogenu oraz dostępności skutecznych leków i szczepionek. Jednak w strategii z 2011 r. nie uwzględniono w odpowiedni sposób kroków, które można podjąć w celu złagodzenia lub powstrzymania wybuchu nowej choroby zakaźnej. Ta wada miała konsekwencje dla całego systemu gotowości na wypadek pandemii w Wielkiej Brytanii. |
| 4.17. | Strategia z 2011 r. opierała się na założeniu, że prawie na pewno „nie będzie możliwe powstrzymanie lub wyeliminowanie nowego wirusa w kraju pochodzenia lub po przybyciu do Wielkiej Brytanii”.¹⁶ Oczekiwano, że wirus nieuchronnie się rozprzestrzeni i że wszelkie lokalne środki podjęte w celu przerwania lub ograniczenia tego rozprzestrzeniania się prawdopodobnie odniosą bardzo ograniczony lub częściowy sukces na poziomie krajowym. Nie można powoływać się na takie środki jako sposób na „”kupić czas'” .¹⁷ |
| 4.18. | Niezależnie od tego, jak zauważono powyżej, od lipca 2018 r. był Sekretarzem Stanu ds. Zdrowia i Opieki Społecznej, w swoich zeznaniach złożonych w dochodzeniu Hancock w sposób znaczący skrytykował strategię z 2011 r. Stwierdził, że podstawą tego jest „błędną doktrynę.¹⁸ W efekcie:
„zamiast strategii zapobiegania katastrofalnym skutkom pandemii – to [był] strategię poradzenia sobie z katastrofalnymi skutkami pandemii.¹⁹ Utrzymywał także, że „błąd błędnej doktryny był znacznie większy niż błąd polegający na celowaniu w grypę, a nie pandemię koronaawirusa.²⁰ |
| 4.19. | Skuteczność łagodzenia jako podejścia została opisana w Strategii 2011 w ramach założeń planistycznych gotowości na wypadek pandemii jako „niepewny”.²¹ Nie było w ogóle odniesienia do strategii tłumienia. Jeżeli realizowano strategię łagodzenia lub tłumienia – tak jak miało to miejsce podczas pandemii Covid-19 – przed styczniem 2020 r. jej konsekwencje były nie tylko nieznane, ale nawet właściwie nie przemyślane. W strategii z 2011 r. nie omówiono odpowiednio, w jaki sposób w przypadku braku klinicznych środków zaradczych, takich jak leki i szczepionki, można zapobiec rozprzestrzenianiu się choroby.²² |
| 4.20. | Jedną z potencjalnych odpowiedzi były „interwencje niefarmaceutyczne”. Obejmowały one porady dotyczące regularnego mycia rąk, aż po, w najbardziej skrajnym przypadku, tak zwane „blokady” (tj. prawne zakazy działań, które w innym przypadku byłyby zgodne z prawem, mające na celu ograniczenie rozprzestrzeniania się wirusa). Te ostatnie zostały uosobione w ogłoszonym 23 marca 2020 r. nakazie „pozostania w domu”.²³ Chociaż strategia z 2011 r. rzeczywiście przewidywała skorzystanie z pewnych interwencji (w tym zalecenia dotyczące pozostania w domu, minimalizowania bliskich kontaktów oraz stosowania praktyk higieny dróg oddechowych i rąk). , powstrzymało się znacznie od izolacji lub zasugerowania, że ograniczenia wolności będą przedmiotem nałożonych nakazów prawnych²⁴ Zamiast tego w strategii z 2011 r. stwierdzono:
"[T]Rząd będzie zachęcał osoby zdrowe do kontynuowania normalnego życia tak długo i tak dalece, jak to możliwe, przy jednoczesnym zachowaniu podstawowych środków ostrożności w celu ochrony przed infekcją i zmniejszenia ryzyka przeniesienia grypy na inne osoby… Zakłada się, że rząd będzie polegał na dobrowolnym stosowaniu się do zaleceń krajowych.”²⁵ |
| 4.21. | W Strategii z 2011 r. nie wykluczono całkowicie przymusu prawnego, istniało jednak silne założenie przeciwko niemu – zastrzeżonemu jedynie dla „istotne zagrożenie" Lub "ekstremalne okoliczności”lub używany jako„Ostatnia deska ratunku.²⁶ Ze względu na niepewność wyniku i ingerencję w wolność, uprawnienia nadzwyczajne musiały zostać „ograniczają się w swoim zakresie do bezpośredniego łagodzenia skutków sytuacji nadzwyczajnej”.²⁷ Zamiast tego rząd Wielkiej Brytanii opowiadał się za udzielaniem porad obywatelom i ufaniem im, że ocenią ryzyko i zastosują takie środki ostrożności, jakie uznają za stosowne. Hancock potwierdził, że nie był to przypadek, ale konkretna i długotrwała decyzja polityczna, potwierdzona ostatnio w 2017 r., kiedy Hunt był sekretarzem stanu²⁸. |
| 4.22. | W dochodzeniu przyjmuje się, że nałożenie blokady (której cechy i konsekwencje zostały szczegółowo omówione w module 2) powinno być środkiem ostatecznym. Rzeczywiście są tacy, którzy twierdzą, że blokady nigdy nie należy wprowadzać. Jednakże dopóki istnieje taka możliwość, należy odpowiednio rozważyć wprowadzenie blokad przed wybuchem nowej choroby zakaźnej. Należy rozważyć interwencje, które można i należy zastosować, aby zapobiec izolacji, ale także okoliczności, w których blokada może okazać się konieczna. Należy odpowiednio zaplanować, jakie aspekty przymusu prawnego w celu ochrony społeczeństwa można zastosować, a także zapewnić przejrzystość co do tego, co rząd zamierza zrobić w przypadku zagrożenia zdrowia. Jest to temat, który jest przedmiotem Zapytania w kolejnych modułach. |
Wada 2: Skoncentruj się tylko na jednym typie pandemii
| 4.23. | W świetle strategii z 2011 r. oczywiste jest, że Wielka Brytania poświęciła swoje wysiłki przygotowaniom na pandemię grypy. Profesor Dame Sally Davies, dyrektor medyczny Anglii od czerwca 2010 r. do października 2019 r., nie przypomina sobie debaty na temat uwzględnienia pandemii innych niż grypa w strategii na rok 2011.²⁹ Profesor Isabel Oliver, od października tymczasowa dyrektor ds. nauki brytyjskiej Agencji Bezpieczeństwa Zdrowia 2021 r. wyjaśnił, że „jedynym patogenem, dla którego przygotowano szczegółowe plany na skalę pandemii, była grypa”.³⁰ Emma Reed, dyrektor ds. gotowości na wypadek sytuacji kryzysowych i ochrony zdrowia w Departamencie Zdrowia i Opieki Społecznej od lutego 2018 r. stwierdziła, że Strategia na 2011 r. była jedyną strategią pandemiczną prowadzoną centralnie przez ten departament.³¹ |
| 4.24. | Clara Swinson, dyrektor generalna ds. zdrowia globalnego i publicznego w Departamencie Zdrowia i Opieki Społecznej od 2016 r., która przewodniczyła Radzie Programowej ds. Gotowości na Pandemię Grypy w latach 2017–2022, powiedziała, że jedyny obowiązujący w Wielkiej Brytanii plan lub strategia dotyczy grypy pandemicznej , chociaż inne organizacje miały własne plany.³² To był błąd. Powiedziała także śledczemu:
„Tam, gdzie są niewiadome, chodzi o badania i rozwój, o elastyczne zasoby, o doradztwo naukowe i tak dalej… Spoglądając wstecz, można śmiało powiedzieć, że obecnie chcielibyśmy, aby ten zakres był szerszy.”³³ Pani Swinson powiedziała, że od czasu pandemii Covid-19 i uznając tę wadę, Departament Zdrowia i Opieki Społecznej zamierza skoncentrować się na „system, który nie opiera się na planach, ale na kluczowych możliwościach i odporności”.³⁴ Powinno to oznaczać, że podstawowy zestaw umiejętności, technologii i infrastruktury będzie gotowy do użycia w przypadku kolejnej pandemii. Będzie musiał wykazywać wystarczające zdolności adaptacyjne, aby reagować na grypę, ale także na szereg pandemii. |
| 4.25. | Uznano, że strategię z 2011 r. można dostosować w przypadku innych chorób układu oddechowego; opisano to jako „gotowy na grypę, gotowy na wszystko”.³⁵ Mogłoby to, co możliwe, być w zasadzie prawdą. Profesor Mark Woolhouse, profesor epidemiologii chorób zakaźnych na Uniwersytecie w Edynburgu, stwierdził:
„Chociaż słusznie obawialiśmy się grypy (i zagrożenie to pozostaje), powinniśmy byli być przygotowani na większą różnorodność zagrożeń związanych z pandemią. Założenie w zakresie planowania, że reakcja odpowiednia w przypadku grypy będzie również odpowiednia w przypadku innego wirusa oddechowego, nie sprawdziło się w praktyce. W tym przypadku grypa okazała się niedoskonałym modelem dla Covid-19.”³⁶ |
| 4.26. | Zgodnie ze Strategią z 2011 r. „plany można dostosować i wdrożyć w przypadku scenariuszy takich jak wybuch innej choroby zakaźnej, np. ciężkiego ostrego zespołu oddechowego (SARS).³⁷ Uznał:
„Pandemie grypy są z natury nieprzewidywalne. Plany reagowania na przyszłą pandemię powinny zatem być elastyczne i można je dostosować do szerokiego zakresu scenariuszy, a nie tylko „rozsądnie najgorszego przypadku”.”³⁸ Powinna istnieć wystarczająca elastyczność i zdolność adaptacji, aby poradzić sobie z pandemią, która uderzyła, ale tak się nie stało. Świadczy o tym faktyczne odejście od Strategii z 2011 r. w reakcji na pandemię Covid-19, o czym mowa poniżej. |
| 4.27. | Gdyby głębiej zastanowić się, co oznaczałaby w praktyce gotowość na szereg patogenów, w strategii na rok 2011 zaczerpnięto by z programu NHS England dotyczącego chorób zakaźnych o poważnych konsekwencjach (omówionego dalej w Rozdział 5: Uczenie się na doświadczeniach).³⁹ Dla Dochodzenia nie jest jasne, dlaczego strategie dotyczące chorób zakaźnych i pandemii o poważnych konsekwencjach były tak różne i niepowiązane ze sobą. Należało je rozważyć łącznie. Gdyby tak było, systemy rutynowo stosowane w przypadku chorób zakaźnych o poważnych konsekwencjach (takie jak testy, śledzenie i izolowanie) byłyby skalowalne i gotowe do kontrolowania rozprzestrzeniania się nowego wirusa o potencjale pandemicznym. Podział na te dwie kategorie przymykał oczy na rząd i tych, którzy wdrażali politykę rządu. Między planowaniem obu scenariuszy istniała rozbieżność. Mimo że obie koncepcje dotyczyły potencjalnego wybuchu i rozprzestrzeniania się katastrofalnej choroby, pozostały one odrzucone, pozostawiając poważną lukę w planach strategicznych Wielkiej Brytanii. |
| 4.28. | Według Sir Christophera Wormalda, stałego sekretarza Departamentu Zdrowia i Opieki Społecznej od maja 2016 r., strategia na wypadek pandemii i Program Chorób Zakaźnych Poważnych Konsekwencji brzmiały: „równolegle”.⁴⁰ Jeśli jednak porzucono strategię po uderzeniu Covid-19, w rzeczywistości nie było żadnej strategii. Powiedział, że Departament Zdrowia i Opieki Społecznej zmienił swoje podejście do niektórych z tych kwestii:⁴¹
„Moim zdaniem za bardzo polegaliśmy na planach i kropka. Nasze myślenie skupia się teraz bardziej w kategoriach: jakie są elastyczne możliwości, które pozwalają przygotować właściwy rodzaj reakcji, biorąc pod uwagę rodzaj choroby, z którą się spotykasz?”⁴² |
| 4.29. | Ważne jest, aby nie narzucać zbyt wielu norm w kwestii technologii, umiejętności, infrastruktury i zasobów, które będą wymagane w przypadku przyszłej pandemii. Profesor Sir Christopher Whitty, dyrektor medyczny Anglii od października 2019 r., uznał, że częścią rozwiązania kwestii gotowości na wypadek pandemii jest „elementy składowe wielu różnych możliwości”.⁴³ Powtórzył to profesor Sir Patrick Vallance, główny doradca naukowy rządu w okresie od kwietnia 2018 r. do marca 2023 r., który powiedział w dochodzeniu:
"[I]Nie chodzi o to, żeby mieć w tylnej kieszeni bardzo konkretne odpowiedzi, przygotowane na każdą ewentualność. To nie jest możliwe. Istnieją jednak ogólne możliwości, które są ważne w całym utworze.”⁴⁴ |
| 4.30. | Wystąpiła strategiczna luka pomiędzy epidemią lub wybuchem nowej choroby zakaźnej na skalę pandemii (w tym choroby zaklasyfikowanej jako choroba zakaźna o poważnych konsekwencjach) a grypą pandemiczną. Tak się złożyło, że Covid-19 znalazł się w tej luce, podobnie jak możliwości kontroli granicznej, poddawania kwarantannie i ustalania kontaktów zakaźnych – w każdym przypadku na dużą skalę – pod kątem potencjalnego wybuchu pandemii. Szersza i kompleksowa strategia, która oceniałaby szereg potencjalnych typów patogenów i obejmowała szereg zmierzonych potencjalnych środków zaradczych, byłaby w stanie skuteczniej zapobiegać rozprzestrzenianiu się niebezpiecznej choroby niż łagodzić jej skutki. Dochodzenie nie otrzymało żadnego odpowiedniego wyjaśnienia, dlaczego istniała ta oczywista luka. |
Wada 3: Brak odpowiedniego rozważenia proporcjonalności reakcji
| 4.31. | W przypadku wybuchu nowej choroby zakaźnej rząd powinien mieć na uwadze szereg potencjalnych reakcji, od niepodejmowania działań na jednym końcu spektrum, aż po znaczące ograniczenia swobód w celu zapobiegania przenoszeniu choroby na drugim końcu spektrum. |
| 4.32. | W wiodącym zaleceniu z przeglądu z 2010 r., który doprowadził do powstania strategii, Dame Deirdre Hine zaleciła:
„Ministrowie powinni określić na początku pandemii, w jaki sposób zapewnią, że reakcja będzie proporcjonalna do postrzeganego poziomu ryzyka i jak będzie to wpływać na proces decyzyjny.”⁴⁵ |
| 4.33. | Jednakże tak samo jak w strategii z 2011 r. nie uwzględniono łagodzenia ani tłumienia skutków, tak też nie uwzględniono z wyprzedzeniem w odpowiedni sposób proporcjonalności potencjalnych reakcji na pandemię. Określiła to podejście w następujący sposób:
„Proporcjonalność: reakcja na pandemię nie powinna być większa i nie mniejsza niż konieczna w stosunku do znanych zagrożeń. Należy zatem wdrożyć plany nie tylko na wypadek pandemii o poważnych skutkach, ale także na łagodniejsze scenariusze, z możliwością ich dostosowywania w miarę pojawiania się nowych dowodów.”⁴⁶ |
| 4.34. | Najbliżej uwzględnienia proporcjonalności w praktyce w strategii z 2011 r. znalazła się tabela zatytułowana „Proporcjonalna reakcja na pandemię grypy”.⁴⁷ Było to jednak niewystarczające z dwóch głównych powodów. Nie uwzględniono w nim szczegółowo różnych potencjalnych reakcji na pandemię, natomiast rozważono potencjalne skutki ognisk o łagodnym, umiarkowanym i silnym wpływie w kategoriach zbyt niejasnych, aby były przydatne. |
| 4.35. | Na przykład w strategii z 2011 r. stwierdzono, że w przypadku powszechnej choroby w Wielkiej Brytanii szpitale będą mogły świadczyć jedynie usługi w nagłych przypadkach i udzielane będą porady dotyczące minimalizacji ryzyka przeniesienia.⁴⁸ Było to wyraźnie nieodpowiednie w przypadku takich ważny dokument strategiczny. Poinformował podmioty zaangażowane w gotowość, odporność i reagowanie, czego się spodziewać, a nie tego, co w praktyce może lub powinno zostać zrobione i przez kogo. Ta porażka najprawdopodobniej dotknęła osoby bezbronne, ponieważ to właśnie oni byli nieproporcjonalnie narażeni na ryzyko, że dotknie ją zarówno sama sytuacja nadzwyczajna, jak i próby jej zapobiegania.⁴⁹ |
| 4.36. | W strategii z 2011 r. należało określić szeroką gamę scenariuszy epidemii patogenów, od mniejszej do większej dotkliwości i o różnych skutkach dla całej populacji. Gdyby tak zrobiło, osoby odpowiedzialne za planowanie pandemii mogłyby ocenić, które reakcje polityczne – na przykład porady dla społeczeństwa, łagodzenie i tłumienie – były proporcjonalne do problemu, jeszcze przed nadejściem jakiejkolwiek pandemii. Wymagane było podejście systematyczne, aby:
|
| 4.37. | Gdyby ocena proporcjonalności znalazła się w centrum strategii z 2011 r., mogłaby przedstawić rozważania, a następnie przedstawić – z wyprzedzeniem – szereg reakcji politycznych na pandemie, przy współczynniku śmiertelności wynoszącym na przykład 0,011. TP3T do 10% i więcej. Strategia z 2011 r. – zamiast nakazywać systemowi gotowości, aby planował uwzględnienie szeregu rodzajów i poziomów dotkliwości ognisk chorób i w ten sposób zwracać się do departamentów rządowych o opracowanie z wyprzedzeniem reakcji politycznych dostosowanych do tego zakresu – zamiast tego nakazywała systemowi być przygotowanym jedynie na zarządzanie jeden wynik dla chorych i umierających. Całkowicie brakowało jakichkolwiek środków oceny całkowitego wpływu danej reakcji. |
| 4.38. | W przypadku strategii niezwykle istotne jest uwzględnienie szeregu scenariuszy w kontekście sytuacji nadzwyczajnej cywilnej obejmującej cały system, takiej jak pandemia. W przypadku braku skutecznej strategii, w której decyzje są przemyślane z wyprzedzeniem, system reagowania kryzysowego naraża się na ryzyko nadmiernej lub niedostatecznej reakcji na sytuację nadzwyczajną, nie dysponując mechanizmem pozwalającym zorientować się, że tak się dzieje. Spójna strategia musi zatem umożliwiać reakcję na zaistniałą sytuację nadzwyczajną, ale także zapobiegać jej eskalacji poza kontrolą rządu. Wyjaśnił to profesor Davies:
„ministrowie potrzebują równowagi w zakresie wkładu biomedycznego… i spojrzenia na sytuację kryzysową/pandemię zdrowotną z perspektywy gospodarki i dobrostanu społeczeństwa”.⁵⁰ |
| 4.39. | Zasadniczą słabością strategii z 2011 r. był brak jasnego określenia, co może, a co nie, być proporcjonalną reakcją na szereg pandemii o potencjalnym zakresie skutków dla zdrowia. |
| 4.40. | W przyszłości w nowej strategii należy szczegółowo rozważyć kwestię oceny proporcjonalności środków mających na celu ograniczenie lub powstrzymanie przenoszenia. Należy tego dokonać poprzez określenie w strategii:
|
| 4.41. | Strategia powinna jasno określać zakres środków, które można zastosować, rozwiązania prawne, medyczne i ekonomiczne, które mogą być wymagane, a także zakres, w jakim te zdolności istnieją lub będą wymagały zwiększenia w przypadku sytuacji nadzwyczajnej, a także pozytywne i negatywne skutki każdego środka. W takiej sytuacji do rządów należałaby decyzja, kierując się danymi i odpowiednimi poradami, jakie środki – w tym te, które można określić jako „ostateczność” – wdrożyć i kiedy. Rozważając łagodzenie i tłumienie, a także to, w jaki sposób i w jakich okolicznościach należy stosować takie środki, rządy powinny również wziąć pod uwagę doświadczenia brytyjskie i międzynarodowe. |
Wada 4: Brak skutecznej strategii gospodarczej
| 4.42. | Skarb Państwa jest wyjątkowy wśród departamentów rządowych, ponieważ odpowiada za ich finansowanie, a także zapewnia podstawowe bezpieczeństwo ekonomiczne, na którym polegają zarówno one, jak i Wielka Brytania jako całość. Szacuje się, że całkowity koszt wydatków rządowych w wyniku Covid-19 przekroczy 376 miliardów funtów.⁵¹ Jest prawdopodobne, że koszty katastrof cywilnych obejmujących cały system, takich jak pandemie, poniosą następne pokolenia – stąd znaczenie myślenia długoterminowego. Ma konsekwencje daleko wykraczające poza bezpośrednią sytuację nadzwyczajną – w tym dla możliwości finansowania opieki zdrowotnej i społecznej. |
| 4.43. | George Osborne, poseł do parlamentu, kanclerz skarbu od maja 2010 r. do lipca 2016 r., powiedział w trakcie dochodzenia, że Ministerstwo Skarbu planowało na wypadek sytuacji nadzwyczajnych finansowych lub gospodarczych tylko wtedy, gdy było głównym departamentem rządowym.⁵² Ministerstwo Skarbu było zaangażowane jedynie w przygotowanie cywilne na wypadek sytuacji kryzysowych przez inne departamenty poprzez ogólne zarządzanie gospodarką oraz poprzez ustalanie budżetów i stosowanie kontroli wydatków w ramach codziennych działań rządu.⁵³ W związku z tym nie opracował strategii gospodarczej specjalnie na wypadek pandemii ani potencjalnych reakcji na pandemię.⁵⁴ analiza ekonomiczna przeprowadzona po poprzednich epidemiach grypy nie stworzyła „plan”, „projekt" Lub "podręcznik zabaw„konkretnych reakcji gospodarczych na pandemię”.⁵⁵ Zdaniem Catherine Little, drugiej stałej sekretarz skarbu od października 2022 r., stało się tak, ponieważ:
"[D]różne zagrożenia dla zdrowia i gospodarki wymagają różnych reakcji politycznych, w zależności od charakteru ryzyka i panującego kontekstu. Niepewny charakter obu sytuacji oznacza, że opracowanie z wyprzedzeniem konkretnych i szczegółowych planów reagowania na wszystkie możliwe sytuacje awaryjne – w tym przypadku na gospodarcze i fiskalne konsekwencje globalnej pandemii – byłoby niemożliwe, biorąc pod uwagę dostępne zasoby w całym departamencie.”⁵⁶ |
| 4.44. | Pan Osborne stwierdził:
"[T]Ministerstwo Skarbu Wielkiej Brytanii ani, o ile mi wiadomo, żaden zachodni skarb państwa nie planowało proszenia całej populacji o pozostanie w domu przez wiele miesięcy.”⁵⁷ Powiedział, że nikt nie przypuszczał, że możliwa jest reakcja polityczna obejmująca blokady włącznie, dopóki Chiny nie rozpoczną takiej reakcji w 2020 r., w związku z czym nie ma powodu, aby Ministerstwo Skarbu planowało taką reakcję.⁵⁸ Osborne powiedział w dochodzeniu, że jeśli opinia publiczna finanse nie zostałyby postawione na równi, kraj nie byłby w stanie utrzymać siebie i gospodarki w taki sposób, jak to robił, pożyczając i wydając duże sumy pieniędzy:⁵⁹ "[T]nie ma sensu mieć planu awaryjnego, za który nie można zapłacić, a absolutnie kluczowa w tym wszystkim jest zdolność gospodarki i finansów publicznych do elastyczności w obliczu kryzysu.”⁶⁰ |
| 4.45. | Z pewnością jest tak, że planowanie gospodarcze i finansowe musi być wystarczająco elastyczne, aby można było dostosować się do szeregu scenariuszy. Jednakże tak samo, jak istotne jest, aby z góry jasno określić, jakie interwencje w zakresie zdrowia publicznego są dostępne dla polityków, muszą również istnieć plany interwencji gospodarczych zarówno na poziomie mikro, jak i makro. Oprócz wstrząsów czysto ekonomicznych należało zobowiązać skarb państwa do planowania specjalnie na wypadek wstrząsów pozaekonomicznych. Z dochodzenia nie wynika, że Ministerstwo Skarbu powinno było stworzyć plan nakazowy, ponieważ miałby on ograniczone zastosowanie, ale mogło stworzyć taki plan w ściślejszej współpracy z ekspertami z Departamentu Zdrowia i Opieki Społecznej, którzy z wyprzedzeniem zidentyfikowali: szeroki zakres scenariuszy pandemii i, podobnie, szereg głównych opcji polityki gospodarczej, które można zastosować w przypadku pandemii określonego rodzaju i dotkliwości. |
| 4.46. | Chociaż w dochodzeniu przyznano, że modelowanie ekonomiczne będzie obarczone niepewnością, szczególnie w dłuższej perspektywie, samo to nie oznacza, że nie należało tego robić. Biuro ds. Odpowiedzialności Budżetowej, utworzone w 2011 r. jako oficjalny niezależny prognostyk gospodarczy i budżetowy rządu Wielkiej Brytanii, w swoich Ryzyka fiskalne i zrównoważony rozwój informuje o wydarzeniach wykraczających poza tradycyjną analizę ekonomiczną, ale które mogą mieć poważne implikacje gospodarcze i fiskalne.⁶¹ Jej przewodniczący, Richard Hughes, stwierdził:
„Chociaż przewidzenie, kiedy zmaterializuje się ryzyko katastrofalne, może być trudne, można przewidzieć jego szerokie skutki, jeśli tak się stanie. Ryzyko globalnej pandemii znajdowało się na szczycie rządowych rejestrów ryzyka przez dziesięć lat przed pojawieniem się wirusa, jednak przyciągało stosunkowo niewielką (a z perspektywy czasu zdecydowanie zbyt małą) uwagę społeczności gospodarczej.”⁶² (Zagadnienie to zostało omówione w dalszej części Rozdział 3: Ocena ryzyka.) |
| 4.47. | Strategia gospodarcza powinna znajdować się w centrum planowania następnej pandemii. Obok Urzędu Rady Ministrów i Departamentu Zdrowia i Opieki Społecznej Skarb Państwa powinien odgrywać wiodącą rolę w planowaniu scenariuszy dotyczących skutków dla gospodarki różnych rodzajów reakcji na szeroki zakres cywilnych sytuacji kryzysowych obejmujących cały system, w tym pandemie. Umożliwiłoby to rządowi Wielkiej Brytanii rozważenie, które reakcje gospodarcze spowodują najmniejsze szkody w perspektywie krótko-, średnio- i długoterminowej. Tylko wtedy społeczeństwo będzie mogło rozważyć, jaką cenę jest w stanie zapłacić, aby uchronić się przed kolejnym kryzysem. |
Aktualizacja Strategii na 2011 rok
| 4.48. | Od chwili publikacji Strategia na rok 2011 nie była aktualizowana ani poddawana przeglądowi. Oznaczało to, że przez prawie dekadę podstawowy dokument dotyczący jednego z głównych zagrożeń dla Wielkiej Brytanii pozostawał w zastoju. Profesor Davies powiedział:
„Byłoby pomocne, gdybyśmy na nowo spojrzeli na podstawowe zasady np. czy pozwalamy grypie przejść przez populację? Rząd powinien był także dokonać przeglądu stanu wiedzy w zakresie diagnostyki i wykorzystania danych itp., aktualizując praktyki w miarę postępu technologii i praktyki.”⁶³ |
| 4.49. | W listopadzie 2018 r. uznano, że jest taka potrzeba "odświeżać" strategii z 2011 r.64. W listopadzie 2019 r. ponownie odnotowano, że strategia z 2011 r. wymagała "odświeżać" w ciągu najbliższych sześciu miesięcy.⁶⁵ Można było pomyśleć, że „odświeżenie” oznaczałoby, że niektóre z podstawowych błędów zostaną poddane analizie. Jak jednak wykazało dochodzenie, „odświeżenie” było eufemizmem określającym aktualizację, która była niewielka i miała ograniczony zakres.⁶⁶ Zatem żadna zmiana nie miałaby istotnego wpływu na gotowość Wielkiej Brytanii na wypadek pandemii.⁶⁷ Jest mało prawdopodobne, aby taka przegląd uwzględniałby podstawowe błędy strategii z 2011 r. lub jej realizacji. W każdym razie interweniowała pandemia Covid-19. |
| 4.50. | Brak aktualizacji strategii z 2011 r. oznaczał w szczególności, że nie uwzględniła ona żadnych wniosków wyciągniętych z międzynarodowych doświadczeń związanych z chorobą wirusową Ebola, bliskowschodnim zespołem oddechowym (MERS) czy ogniskami SARS, a także nie uwzględniła wniosków płynących z wszelkie ćwiczenia, które miały miejsce po 2011 roku (por Rozdział 5: Uczenie się na doświadczeniach). |
| 4.51. | Hunt stwierdził, że nie przypomina sobie, aby kiedykolwiek poinformowano go o konieczności aktualizacji strategii z 2011 r.⁶⁸ Hancock powiedział, że "brak pomysłu" dlaczego w strategii z 2011 r. nie uwzględniono podejścia przyjętego przez kraje dotknięte SARS, tak aby można było wyciągnąć wnioski dla Wielkiej Brytanii.⁶⁹ |
| 4.52. | Dokumenty, które w efekcie stanowią podstawę całego systemu gotowości i odporności na cywilne sytuacje kryzysowe w całym systemie, należy okresowo rozpatrywać całkowicie od nowa. Nie mniej dotyczy to strategii pandemicznej. Profesor Vallance stwierdził, że w takich krytycznych dokumentach należy podać datę ważności, aby mieć pewność, że nadal są pozytywne "pozostały", po czym zostaną poddane bardziej zasadniczemu przeglądowi.⁷⁰ Dochodzenie potwierdza tę opinię. |
| 4.53. | Wydaje się, że nie istniał żaden formalny system ani bezpośredni nadzór ministerialny zapewniający poddanie tego rodzaju przeglądowi dokumentu tak ważnego jak strategia z 2011 r. Potrzebna jest rygorystyczna kontrola, krytyczne podejście i systematyczne ponowne rozważenie podstawowych zasad, w ramach których ministrowie, eksperci i urzędnicy są gotowi rzucić wyzwanie każdemu prezentowanemu im podejściu doktrynalnemu. |
Rezygnacja ze Strategii z 2011 roku
| 4.54. | Jak zbadano w module 2 niniejszego dochodzenia, strategia z 2011 r. w rzeczywistości nigdy nie została właściwie przetestowana. Kiedy wybuchła pandemia, rząd Wielkiej Brytanii nie dostosował strategii z 2011 roku. Doktryna leżąca u jej podstaw (tzn. reagowanie na sytuację nadzwyczajną, a nie zapobieganie jej wystąpieniu) została skutecznie porzucona, podobnie jak sama Strategia z 2011 roku. Hancock wyjaśnił, że dzieje się tak, ponieważ, jego słowami, „żałośnie niewystarczające”.⁷¹ |
| 4.55. | Zamiast tego, w obliczu pandemii Covid-19, rząd Wielkiej Brytanii i zdecentralizowane administracje przyjęły nowe, nieprzetestowane podejście do pojawiającego się kryzysu. Profesor Woolhouse powiedział śledczym:
„Blokada była doraźną interwencją w zakresie zdrowia publicznego opracowaną w czasie rzeczywistym w obliczu szybko zmieniającego się stanu zagrożenia zdrowia publicznego. Nie planowaliśmy wprowadzenia izolacji… nie było wytycznych co do tego, kiedy należy ją wdrożyć, ani jasnych oczekiwań co do efektów, jakie przyniesie.”⁷² |
| 4.56. | Nowa ogólnosystemowa strategia na wypadek sytuacji nadzwyczajnych, która uwzględnia pandemie, powinna zapewnić zmniejszenie ryzyka przebywania na nieznanym terytorium podczas poważnego kryzysu. Oczywiście niemożliwe będzie zaprojektowanie strategii na każdą ewentualność, powinna ona jednak wyznaczać jasne cele i możliwości niezbędne do ich osiągnięcia, a także starać się przewidywać i zapewniać wytyczne dla szerokiego zakresu scenariuszy, tak aby jak najwięcej myślenia, planowania strategii i planowanie, o ile to możliwe, odbywa się przed wystąpieniem sytuacji awaryjnej. |
| 4.57. | Strategia z 2011 r. była obarczona poważnymi błędami, które każdy mógł dostrzec. Zamiast traktować ocenę ryzyka jako przewidywanie tego, co może się wydarzyć, a następnie zalecić kroki mające na celu zapobieżenie skutkom lub ich ograniczenie, przyjęto założenie, że wynik jest nieunikniony. Wysłało to zły sygnał do systemów gotowości i odporności w Wielkiej Brytanii (w tym w krajach zdecentralizowanych). Sekretarze stanu ds. zdrowia oraz ds. zdrowia i opieki społecznej, którzy zastosowali się do strategii, eksperci i urzędnicy, którzy im to doradzili, a także rządy krajów zdecentralizowanych, które ją przyjęły, ponoszą odpowiedzialność za nieprzeprowadzenie analizy tych błędów i poprawione. Dotyczy to między innymi Hancocka, który porzucił tę strategię, gdy wybuchła pandemia, kiedy było już za późno, aby wywrzeć jakikolwiek wpływ na gotowość i odporność. |
| 4.58. | Rząd Wielkiej Brytanii mógł mieć pewność, że Wielka Brytania jest dobrze przygotowana – na przykład przez Światową Organizację Zdrowia lub ranking Wielkiej Brytanii w Globalnym Indeksie Bezpieczeństwa Zdrowotnego za rok 2019.⁷³ Jednakże, gdyby zapytano go „przygotowany na co?”, rząd Wielkiej Brytanii mógłby uzyskać pewność, że jedyną odpowiedzią byłoby „przygotowanie do wdrożenia strategii z 2011 r.” – ze wszystkimi jej podstawowymi wadami i konsekwencjami. Ujawniłoby to, że głównym celem strategii nie było zapobieganie sytuacji nadzwyczajnej ani jej łagodzenie, ale zarządzanie ofiarami śmiertelnymi, które z niej wynikną. |
Rozwój sytuacji po pandemii Covid-19
| 4.59. | Od czasu pandemii Covid-19 rząd Wielkiej Brytanii przeprowadził szereg przeglądów w celu przeanalizowania adekwatności swoich systemów i struktur pod kątem gotowości i odporności na sytuacje nadzwyczajne dla ludności. |
| 4.60. | Mówi się, że planem dotyczącym odporności rządu Wielkiej Brytanii na rok 2022 jest taki plan „wzmocnić podstawowe systemy, które zapewniają naszą odporność na wszelkie ryzyko”, z „szerokim i wymiernym zestawem działań”, co było „pierwszy krok w naszym zaangażowaniu w opracowanie szerokiego i strategicznego podejścia do odporności”.⁷⁴ Mówiono też, że tak „tylko punkt wyjścia dla ambicji rządu Wielkiej Brytanii w zakresie odporności”.⁷⁵ Jednakże ze względu na długo oczekiwaną kulminację licznych przeglądów i prawie 20 lat doświadczeń od uchwalenia ustawy o nieprzewidzianych sytuacjach cywilnych z 2004 r. brakowało konkretnych zobowiązań niezbędnych do poprawy gotowości i odporności Wielkiej Brytanii. |
| 4.61. | The Ramy odporności rządu Wielkiej Brytanii zawodzi z kilku powodów:
Dokument nie zawiera zestawu wystarczająco jasnych propozycji, które należy pilnie wdrożyć, przy wsparciu niezbędnych zasobów. |
| 4.62. | Brytyjska strategia bezpieczeństwa biologicznego z 2018 r. została zaktualizowana w 2023 r. w następstwie pandemii Covid-19.⁸¹ W dokumencie z 2023 r. opisano „cztery filary naszej reakcji na zagrożenia biologiczne” Jak:
|
| 4.63. | Opisuje reakcję Wielkiej Brytanii jako opartą na „trzy przekrojowe czynniki umożliwiające [Który] przebiegają przez wszystkie cztery filary i są wyciągane oddzielnie”.83 Są to:
|
| 4.64. | Główne ulepszenia między strategiami na lata 2018 i 2023 to zobowiązania do:
|
Nowa ogólnosystemowa strategia na wypadek sytuacji kryzysowych
| 4.65. | Zmienione plany określone w 2022 r Ramy dotyczące odporności rządu Wielkiej Brytanii i brytyjska strategia bezpieczeństwa biologicznego na rok 2023 należy ich powitać. Na przykład powołanie głównego ministra i wyższego urzędnika nadzorującego wdrażanie oraz grupy głównych doradców naukowych, którzy kwestionują politykę, to pozytywne kroki⁸⁶ Jednakże zazwyczaj nie przedstawiają one problemów ani rozwiązań w sposób jasny i dokładny. W strategii 2023 brakuje terminów, w jakich należy podjąć działania i według których można by mierzyć postęp rządu. Opinia publiczna nie może wiedzieć, czy rząd poniósł porażkę, jeśli sam rząd nie chce lub nie jest w stanie opisać i ustalić obiektywnych kryteriów pomiaru jego działań, ani też urzędnicy, których zadaniem jest wdrażanie takiej strategii, nie mogą się dowiedzieć. |
| 4.66. | Ważne jest, aby myślenie o różnych sposobach, w jakie rząd Wielkiej Brytanii i zdecentralizowane administracje mogą skutecznie zareagować na kolejną pandemię, zostało podjęte jak najszybciej i aby stanowiło integralną część nowej strategii pandemicznej. W następstwie pandemii Covid-19 w Wielkiej Brytanii i na całym świecie dostępna jest obecnie ogromna ilość danych na temat:
|
| 4.67. | Chociaż strategia nie powinna mieć charakteru normatywnego (ponieważ następna pandemia może nie być taka sama lub nawet podobna do poprzedniej), ogólne zasady, którymi przywódcy polityczni mają się kierować przy podejmowaniu decyzji dotyczących kompromisów w stosowaniu różnych aspektów strategii, powinny zostać określone możliwie najdokładniej. Powinien na przykład określać rodzaje infrastruktury, technologii i umiejętności, które byłyby potrzebne i można je dostosować, dostępne środki ochrony zdrowia (takie jak udzielanie porad społeczeństwu, dystans społeczny, zamykanie szkół i obowiązkowa kwarantanna) oraz prawdopodobne skutki społeczne i gospodarcze w krótkim, średnim i długim okresie ich stosowania. W ramach dochodzenia szczegółowo bada się skuteczność takich środków w kolejnych modułach. |
Zalecenie 4: Ogólnounijna strategia na wypadek sytuacji kryzysowych obejmująca cały system
Rząd Wielkiej Brytanii i zdecentralizowane administracje powinny wspólnie wprowadzić ogólnokrajową, całościową strategię cywilną na wypadek sytuacji nadzwyczajnych (która obejmuje pandemie), aby zapobiec każdej sytuacji nadzwyczajnej, a także ograniczyć, kontrolować i łagodzić jej skutki.
Strategia powinna co najmniej:
- być elastycznym;
- zawierać sekcje poświęcone każdej potencjalnej sytuacji nadzwyczajnej cywilnej obejmującej cały system – na przykład sekcję dotyczącą pandemii, z jasnym wyjaśnieniem ról i obowiązków rządu Wielkiej Brytanii, zdecentralizowanych administracji i ich departamentów/dyrekcji, a także lokalnych służb ratowniczych;
- rozważyć szeroki zakres potencjalnych scenariuszy dla każdego rodzaju sytuacji awaryjnej;
- zidentyfikować kluczowe problemy i określić zakres potencjalnych reakcji;
- określić, w jaki sposób należy zastosować strategię, aby zapewnić, że wszelkie potencjalne reakcje będą proporcjonalne do konkretnych okoliczności sytuacji nadzwyczajnej;
- obejmować ocenę krótko-, średnio- i długoterminową, opartą na opublikowanych modelach, potencjalnych skutków zdrowotnych, społecznych i gospodarczych sytuacji nadzwyczajnej oraz potencjalnych reakcji na sytuację nadzwyczajną dla ludności, a w szczególności osób bezbronnych; I
- obejmować ocenę infrastruktury, technologii i umiejętności, których Wielka Brytania potrzebuje, aby skutecznie reagować na sytuację nadzwyczajną, oraz ocenę tego, jak te potrzeby mogą się zmienić w zależności od różnych scenariuszy.
Strategia powinna podlegać ponownej merytorycznej ocenie co najmniej co trzy lata, aby zapewnić jej aktualność i skuteczność oraz uwzględniać wnioski wyciągnięte pomiędzy ponownymi ocenami.
Udoskonalanie strategii za pomocą danych i badań
Dane
| 4.68. | Dane dobrej jakości i szeroki zakres typów danych mają kluczowe znaczenie w reagowaniu na pandemie i inne sytuacje kryzysowe cywilne obejmujące cały system, ponieważ wnioski wyciągnięte z danych na temat pojawiającego się kryzysu określą, która część strategii powinna być realizowana i kiedy należy ją realizować oraz czy należy zmienić obrany kurs. Dane są niezbędne do opracowania strategii, która może być elastyczna i dostosowywalna w miarę gromadzenia i analizowania informacji o sytuacji nadzwyczajnej. |
| 4.69. | Istnieją ograniczenia co do tego, co można zrobić z danymi przed wystąpieniem stanu nadzwyczajnego, takiego jak pandemia. Tam, gdzie to możliwe, należy zapewnić decydentom rzetelny dostęp do aktualnych danych już od najwcześniejszych momentów kryzysu, co umożliwi tym decydentom lepszą kontrolę w miarę rozwoju wydarzeń. Jeśli dostępne są jedynie dane historyczne, z których można ekstrapolować przyszłość, ograniczenia w projektowaniu strategii są oczywiste. Są one uznawane przez Gabinet Rady Ministrów co najmniej od 2014 r., a ostatnio przez Królewską Akademię Inżynierską we wrześniu 2021 r.⁸⁷ |
| 4.70. | W momencie wybuchu pandemii kluczowy jest dostęp do aktualnych, kompleksowych danych na temat:
|
| 4.71. | Dostęp do takich danych wymaga, aby Wielka Brytania posiadała odpowiednie systemy i możliwości gromadzenia danych przed wystąpieniem sytuacji nadzwyczajnej. Istotne są zarówno dane administracyjne (takie jak aktualna liczba dostępnych łóżek szpitalnych czy liczba pociągów, które mogą kursować), jak i dane generowane i analizowane w drodze badań naukowych (takie jak skuteczność lub brak środków zaradczych). |
| 4.72. | Decyzje podjęte na początku pandemii Covid-19 opierały się na konieczności posiadania „szybkie i niezawodne dane”.⁸⁸ Jeśli decydenci i doradcy nie mają dostępu do takich danych, to tak jest „zasadniczo jazda w ciemności”.⁸⁹ Im lepsze dostępne dane, tym dokładniejsze decyzje można podjąć. Bez dobrych danych podejmowanie decyzji w oparciu o dowody staje się znacznie trudniejsze ze względu na niepewność, z jaką muszą się borykać decydenci. |
| 4.73. | Znaczenie tego zostało docenione przed pandemią Covid-19. W latach 2013–2018 profesor Sir Mark Walport, główny doradca naukowy rządu od kwietnia 2013 r. do września 2017 r., zamówił szczegółowe wytyczne na ten temat.⁹⁰ Miały one pomóc głównemu doradcy naukowemu rządu oraz Naukowej Grupie Doradczej ds. Sytuacji Nadzwyczajnych (SAGE) w celu zapewnienia doradztwa naukowego COBR (krajowemu centrum zarządzania kryzysowego rządu brytyjskiego zajmującemu się reagowaniem na cywilne sytuacje kryzysowe obejmujące cały system) w przypadku sytuacji nadzwyczajnej. Jeden z tych dokumentów zawierał wytyczne dotyczące ryzyka pojawienia się chorób zakaźnych, przedstawiając pomocną listę pytań otwartych, na które należy odpowiedzieć w ramach odpowiedzi, jakie dane będą potrzebne, aby odpowiedzieć na te pytania, kiedy dane te będą potrzebne oraz jakie były źródła takich danych⁹¹ Jednak do czasu pandemii Covid-19 profesor Vallance opisał, że istniały „niedobór danych”, co oznaczało, że rząd Wielkiej Brytanii i zdecentralizowane administracje „lecieliśmy bardziej na ślepo, niż byś sobie tego życzył”.⁹² |
| 4.74. | Potwierdził to profesor Sir Ian Diamond, brytyjski statystyk narodowy od października 2019 r „nie istniały żadne formalne struktury ONS [Urząd Statystyki Krajowej] bezpośrednie przyczynianie się do gotowości i reagowania na sytuacje kryzysowe cywilne poza komisjami ad hoc i prośbami o wsparcie”.⁹³ Zasugerował, że przed pandemią Covid-19 takie zaangażowanie w rzeczywistości nie istniało.⁹⁴ |
| 4.75. | Ponadto należy przyjąć bardziej spójne podejście do kompatybilności systemów danych we wszystkich czterech krajach Wielkiej Brytanii. w Raport techniczny w sprawie pandemii COVID-19 w Wielkiej Brytanii dyrektorzy medyczni i główni doradcy naukowi czterech krajów podkreślili znaczenie zarówno badań, jak i danych.⁹⁵ Zauważyli jednak również:
„Systemy danych i systemy opieki zdrowotnej różnią się w poszczególnych 4 krajach, dlatego przy projektowaniu wspólnego systemu testowania konieczne było uwzględnienie pełnego zakresu okoliczności”.⁹⁶ Oznacza to, że chociaż Anglia, Walia, Szkocja i Irlandia Północna były zagrożone tym samym zagrożeniem zdrowotnym, dane i systemy opieki zdrowotnej były tak różne, że stanowiły przeszkodę w skutecznej gotowości. |
| 4.76. | Profesor Whitty opisał dane jako "absolutnie niezbędna" i w dużej mierze „pytanie o zasoby i umiejętności”.⁹⁷ Systemy danych muszą zostać uruchomione przed pandemią. Muszą być zautomatyzowane i zintegrowane, aby zapewnić spostrzeżenia, na podstawie których można podjąć działania w wymaganych ramach czasowych.⁹⁸ Jakakolwiek przyszła strategia dotycząca cywilnych sytuacji kryzysowych obejmujących cały system, w tym pandemii, będzie musiała opierać się na ustanowieniu „wielkoskalowe platformy cyfrowe”.⁹⁹ W przypadku pandemii konieczne będzie „platforma cyfrowa umożliwiająca zarządzanie kontaktami, szybkie raportowanie danych epidemiologicznych” I „mechanizmy nadzoru” aby uchwycić i zrozumieć epidemiologię patogenu.¹⁰⁰ Wszystko to będzie wymagało publicznej debaty i ostatecznie zgody.¹⁰¹ Ważne jest, aby ta rozmowa rozpoczęła się teraz. |
| 4.77. | W tej dziedzinie nastąpiły pozytywne zmiany. W październiku 2021 r. Gabinet Rady Ministrów utworzył Krajowe Centrum Sytuacyjne, którego zadaniem jest gromadzenie i wykorzystywanie danych do monitorowania zagrożeń i reagowania na sytuacje kryzysowe w całym systemie, które wpływają jednocześnie na wiele obszarów usług publicznych.¹⁰² Urząd Statystyczny jest teraz podłączony do Krajowe Centrum Sytuacyjne, umieszczając swoje dane i analizy w centrum podejścia rządu Wielkiej Brytanii do gotowości i reagowania.¹⁰³ Częścią funkcji brytyjskiego Komitetu Ochrony Zdrowia, utworzonego w 2021 r., jest lepsze zapewnienie możliwości udostępniania danych w całym kraju UK.¹⁰⁴ W 2022 r. powołano Wspólne Centrum Danych i Analiz, skupiające wszystkie zespoły ds. danych i analiz zlokalizowane w Biurze Rady Ministrów.¹⁰⁵ |
Badania
| 4.78. | Przedstawione powyżej problemy z danymi dotyczą w równym stopniu rutynowo gromadzonych danych administracyjnych, jak i danych gromadzonych w drodze badań naukowych. Jednak właściwe zaprojektowanie i wykorzystanie metod badawczych, które umożliwiają odpowiednią analizę bardziej złożonych danych i przekształcenie informacji w użyteczny dowód, stanowi dodatkowe wyzwanie dla gotowości i reagowania na pandemię. Należy to zaplanować, jeśli zastosowanie strategii ma być oparte na dowodach i skuteczne. Dzieje się tak zwłaszcza w przypadku nowego patogenu, w przypadku którego dokładna charakterystyka choroby nie jest z góry znana („choroba X” omówiona w pkt. Rozdział 1: Krótka historia epidemii i pandemii). Badania dostarczają dowodów niezbędnych do przejścia od tępych, a nawet destrukcyjnych narzędzi (takich jak stosowanie odległości i barier fizycznych w celu zapobiegania przenoszeniu) na bardziej ukierunkowane reakcje, takie jak skuteczne szczepionki i środki lecznicze.¹⁰⁶ Mogą one również dostarczyć informacji na temat niemal każdego innego aspektu gotowości na wypadek pandemii lub odpowiedź: dokładność i rzetelność testu; skuteczność środków ochrony indywidualnej przed przenoszeniem chorób; zakres bezobjawowego przeniesienia; reakcja behawioralna społeczeństwa na patogen; oraz pomiar i łagodzenie niepożądanych skutków interwencji niefarmaceutycznych. |
| 4.79. | Co ważne, podczas szybko rozprzestrzeniającej się fali infekcji badania należy rozpocząć jak najszybciej, aby mieć pewność, że możliwości zbadania patogenu i interwencji zastosowanych w celu jego zwalczania nie zostaną utracone przed zakończeniem tej fali. Zdolność do szybkiego przeprowadzenia wysokiej jakości badań w odpowiedzi na pojawiającą się pandemię zależy zatem od tego, czy naukowcy byli w stanie z dużym wyprzedzeniem przygotować podwaliny pod te badania. Bez opracowania istniejących ram, w ramach których naukowcy mogliby podejmować tak szybkie badania, Wielka Brytania mogłaby zostać pozbawiona przewagi w zakresie wiedzy naukowej, która mogłaby ratować życie i chronić społeczeństwo. Zapewnienie Wielkiej Brytanii najlepszych szans na zapewnienie sobie przewagi wymaga przemyślenia i zasobów. |
| 4.80. | Oczywiste jest, że przed przyszłymi pandemiami należy zrobić więcej w zakresie badań, aby zapewnić lepsze przygotowanie Wielkiej Brytanii. Profesor Whitty powiedział, że w odpowiedzi na pandemię Covid-19 Wielka Brytania uruchomiła lub uruchomiła wiele badań badawczych oraz „położyć większy nacisk na badania naukowe niż większość porównywalnych krajów”.¹⁰⁷ Jednym z kluczowych przykładów było badanie dotyczące infekcji koronawirusem (Covid-19) przeprowadzone przez Urząd Statystyczny, które, jak zauważył profesor Vallance, „zaczęło być podziwiane na całym świecie jako badanie poziomu populacji, które pozwoliło nam zrozumieć wzorce chorób w Wielkiej Brytanii”.¹⁰⁸ W czasie pandemii Covid-19 badanie trzeba było rozpocząć od zera; Profesor Vallance powiedział to w przyszłości „Byłoby bardzo, bardzo ważne jest, aby skonfigurować te rzeczy wcześniej”.¹⁰⁹ |
| 4.81. | Podobnie można było przeprowadzić więcej badań w celu ulepszenia bazy danych dotyczących różnych środków w zakresie zdrowia publicznego. Profesor Walport zauważył, że stworzenie bazy dowodowej, na podstawie której można podejmować bardziej świadome decyzje dotyczące interwencji niefarmaceutycznych, takich jak noszenie masek na poziomie populacji, środki dotyczące dystansu społecznego lub zamykanie szkół, jest „znacznie trudniejsza propozycja” niż inne kwestie naukowe istotne dla gotowości na pandemię.¹¹⁰ Podobnie profesor Vallance zaobserwował ograniczenia dostępnych w Wielkiej Brytanii badań dotyczących interwencji niefarmaceutycznych, zauważając, że:
„trudność w uzyskaniu dobrej jakości danych na temat skutków interwencji niefarmaceutycznych. Jest to z natury trudny obszar, ponieważ istnieje tak wiele zmiennych, tak dużo „szumu”, że trudno jest wiarygodnie wyodrębnić wpływ dowolnego środka.”¹¹¹ |
| 4.82. | Z kolei profesor John Edmunds, profesor modelowania chorób zakaźnych w London School of Hygiene & Tropical Medicine, stwierdził, że „Należało przeprowadzić randomizowane, kontrolowane badania kliniczne, aby zapewnić najwyższą jakość dostępnych dowodów”.¹¹² Chociaż zasugerowano to podczas pandemii Covid-19, po kilku próbach przeprowadzonych w trakcie i po niej, powiedział:
„[I]Zaskakujące jest, jak ograniczone były nasze ambicje w tym zakresie. Ta stracona szansa na wyciągnięcie wniosków z pandemii sprawi, że będziemy podobnie nieprzygotowani na następną”.¹¹³ |
| 4.83. | W dochodzeniu przyznano, że ulepszenie bazy dowodowej w zakresie takich środków w zakresie zdrowia publicznego nie jest proste i wymaga znacznie więcej przemyśleń w środowisku naukowym. Pokazuje to jednak, jak ważne jest stworzenie lepszych podstaw w tym zakresie przed kolejną pandemią. Kluczowe będzie określenie, które grupy osób bezbronnych prawdopodobnie najbardziej ucierpią na skutek pandemii i jakie są tego przyczyny. Szczególnym przedmiotem badań powinny być przyczyny większych nierówności w wynikach, ze szczególnym uwzględnieniem nierówności w zdrowiu.¹¹⁴ |
| 4.84. | Departament Zdrowia i Opieki Społecznej zleca niezależne badania za pośrednictwem Narodowego Instytutu Badań nad Zdrowiem i Opieką, jednego z głównych brytyjskich fundatorów badań nad zdrowiem i opieką, wydającego ponad 1 miliard funtów rocznie.¹¹⁵ Inwestycja ta obejmuje badania nad gotowością na wypadek pandemii, infrastrukturę badań klinicznych i, co ważne, projekty badawcze „hibernowane” lub „uśpione” – elastyczne projekty protokołów, które są projektowane z wyprzedzeniem, a następnie utrzymywane w stanie gotowości, aby można je było rozpocząć natychmiast po pojawieniu się nowego wybuchy epidemii chorób zakaźnych.¹¹⁶ Od 2009 r. do stycznia 2020 r. na łącznie dziewięć kontraktów badawczych w ramach hibernacji w zakresie gotowości na wypadek pandemii przeznaczono łącznie zaledwie około 3,8 miliona funtów.¹¹⁷ Odpowiada to średnio zaledwie 380 000 funtów rocznie. |
| 4.85. | Biorąc pod uwagę znaczenie badań dla gotowości na wypadek pandemii oraz użyteczność projektów badawczych w stanie hibernacji, w dochodzeniu uznano, że potrzebny jest ambitniejszy, szeroko zakrojony i lepiej finansowany program badań w trybie hibernacji, powiązany z nową strategią gotowości na wypadek pandemii. Program ten musi stanowić część zmiany sposobu myślenia, w ramach której znaczenie badań, podobnie jak danych, powinno stanowić centralny punkt nowej, obejmującej cały system strategii na wypadek sytuacji cywilnych. W ten sposób wymagania strategii mogą zidentyfikować niepewności wymagające lepszych badań, podczas gdy niezależny rozwój badań może lepiej wpłynąć na strategię. |
| 4.86. | Profesor Jimmy Whitworth i dr Charlotte Hammer, biegli w zakresie nadzoru nad chorobami zakaźnymi (zob Załącznik 1: Informacje o tym module i metodologia badania), opowiadał się za podejściem do bezpieczeństwa biologicznego „Jedno zdrowie”, obejmującym badania w ramach specjalistycznych dziedzin nauki i pomiędzy nimi, odporne systemy opieki zdrowotnej oraz koordynację globalnego zarządzania zdrowiem. Gotowość, odporność i reagowanie na sytuacje kryzysowe zostaną następnie rozważone łącznie we wszystkich obszarach¹¹⁸ Zalecili także zmiany w środkach niezbędnych do poprawy bezpieczeństwa biologicznego. Obejmowałoby to lepsze przywództwo w zakresie międzynarodowych systemów ostrzegania, inwestycje w zdolność Wielkiej Brytanii do szybkiego zwiększenia jej zdolności do reagowania na pandemie oraz poprawę w zakresie gromadzenia zapasów i odporności Wielkiej Brytanii na łańcuch dostaw. Gdyby połączyć to poza pandemią ze znacznymi inwestycjami publicznymi i prywatnymi w badania i rozwój skalowalnych klinicznych środków zaradczych, Wielka Brytania byłaby lepiej przygotowana na pandemię w przyszłości¹¹⁹ |
Zalecenie 5: Dane i badania dotyczące przyszłych pandemii
Rząd Wielkiej Brytanii, współpracując z zdecentralizowanymi administracjami, powinien ustanowić mechanizmy terminowego gromadzenia, analizowania, bezpiecznego udostępniania i wykorzystywania wiarygodnych danych na potrzeby reagowania w sytuacjach kryzysowych przed przyszłymi pandemiami. Systemy danych należy przetestować w ćwiczeniach związanych z pandemią.
Rząd Wielkiej Brytanii powinien także zlecić szerszy zakres projektów badawczych, gotowych do rozpoczęcia w przypadku przyszłej pandemii. Mogą to być badania „hibernowane” lub istniejące badania, które zaprojektowano tak, aby można je było szybko dostosować do nowej epidemii. Należy zachęcać do lepszej współpracy z partnerami międzynarodowymi. Powinno to obejmować projekty mające na celu:
- zrozumieć powszechność występowania nowego wirusa;
- mierzyć skuteczność szeregu różnych środków w zakresie zdrowia publicznego; I
- określić, które grupy osób bezbronnych są najbardziej dotknięte pandemią i dlaczego.
- Strategia gotowości na wypadek pandemii grypy w Wielkiej Brytanii 2011, Departament Zdrowia, listopad 2011 r. (https://assets.publishing.service.gov.uk/media/5a7c4767e5274a2041cf2ee3/dh_131040.pdf; INQ000102974)
- Widzieć Jeane Freeman 28 czerwca 2023 r. 130/19-132/23; Caroline Lamb 28 czerwca 2023 100/14-101/1; Catherine Calderwood 5 lipca 2023 8/10–15
- Andrew Goodall 4 lipca 2023 r. 22.11-25.04; Frank Atherton 3 lipca 2023 22.18-27.10, 28.4-33.08; Michael McBride 10 lipca 2023 145/2-147/24
- Brytyjska strategia gotowości na pandemię grypy 2011, Departament Zdrowia, listopad 2011 r., pkt 2.21 (https://assets.publishing.service.gov.uk/media/5a7c4767e5274a2041cf2ee3/dh_131040.pdf; INQ000102974)
- INQ000184643_0059-0060 ust. 316; INQ000184638_0052-0053 ust. 6.13; Pandemia grypy 2009: Niezależny przegląd reakcji Wielkiej Brytanii na pandemię grypy w 2009 r., Dame Deirdre Hine, lipiec 2010 r. (https://assets.publishing.service.gov.uk/media/5a7975f1ed915d0422068a10/the2009influenzapandemic-review.pdf; INQ000022705); Brytyjska strategia gotowości na pandemię grypy 2011, Departament Zdrowia, listopad 2011 r., pkt 1.7–1.8 (https://assets.publishing.service.gov.uk/media/5a7c4767e5274a2041cf2ee3/dh_131040.pdf; INQ000102974)
- INQ000184638_0053 ust. 6.14
- Brytyjska strategia gotowości na pandemię grypy 2011, Departament Zdrowia, listopad 2011, pkt 3.1 (https://assets.publishing.service.gov.uk/media/5a7c4767e5274a2041cf2ee3/dh_131040.pdf; INQ000102974)
- Strategia gotowości na pandemię grypy Wielkiej Brytanii 2011, Departament Zdrowia, listopad 2011, pkt 3.2 (https://assets.publishing.service.gov.uk/media/5a7c4767e5274a2041cf2ee3/dh_131040.pdf; INQ000102974)
- Brytyjska strategia gotowości na pandemię grypy 2011, Departament Zdrowia, listopad 2011 r., pkt 2.13 (https://assets.publishing.service.gov.uk/media/5a7c4767e5274a2041cf2ee3/dh_131040.pdf; INQ000102974)
- Brytyjska strategia gotowości na pandemię grypy 2011, Departament Zdrowia, listopad 2011 r., pkt 2.19–2.20 (https://assets.publishing.service.gov.uk/media/5a7c4767e5274a2041cf2ee3/dh_131040.pdf; INQ000102974)
- Brytyjska strategia gotowości na pandemię grypy 2011, Departament Zdrowia, listopad 2011, s. 16 (https://assets.publishing.service.gov.uk/media/5a7c4767e5274a2041cf2ee3/dh_131040.pdf; INQ000102974)
- Brytyjska strategia gotowości na pandemię grypy 2011, Departament Zdrowia, listopad 2011, s. 16 (https://assets.publishing.service.gov.uk/media/5a7c4767e5274a2041cf2ee3/dh_131040.pdf; INQ000102974)
- Brytyjska strategia gotowości na pandemię grypy 2011, Departament Zdrowia, listopad 2011 r., pkt 6.1–6.5 (https://assets.publishing.service.gov.uk/media/5a7c4767e5274a2041cf2ee3/dh_131040.pdf; INQ000102974)
- W momencie sporządzania oceny ryzyka bezpieczeństwa narodowego na rok 2019 – na krótko przed pandemią Covid-19 – rozsądny najgorszy scenariusz w przypadku pandemii grypy podobnie przewidywał współczynnik śmiertelności na poziomie 2,5%, co oznaczałoby 820 000 ofiar śmiertelnych, na podstawie ówczesnych Liczba ludności w Wielkiej Brytanii: INQ000176776_0001-0002, 0006-0007
- Brytyjska strategia gotowości na pandemię grypy 2011, Departament Zdrowia, listopad 2011, s. 17, akapit pierwszy (https://assets.publishing.service.gov.uk/media/5a7c4767e5274a2041cf2ee3/dh_131040.pdf; INQ000102974)
- Brytyjska strategia gotowości na pandemię grypy 2011, Departament Zdrowia, listopad 2011, pkt 2.12 (https://assets.publishing.service.gov.uk/media/5a7c4767e5274a2041cf2ee3/dh_131040.pdf; INQ000102974)
- Brytyjska strategia gotowości na pandemię grypy 2011, Departament Zdrowia, listopad 2011, pkt 2.12 (https://assets.publishing.service.gov.uk/media/5a7c4767e5274a2041cf2ee3/dh_131040.pdf; INQ000102974)
- INQ000181825_0013-0014 pkt 52–56; Zobacz też INQ000181825_0008, 0013-0016 pkt 30–31, 52–67; Matt Hancock 27 czerwca 2023 r. 20.02-34.02
- INQ000181825_0008 ust. 31
- Matt Hancock 27 czerwca 2023 79/19-22
- Brytyjska strategia gotowości na pandemię grypy 2011, Departament Zdrowia, listopad 2011, s. 17, akapit pierwszy (https://assets.publishing.service.gov.uk/media/5a7c4767e5274a2041cf2ee3/dh_131040.PDF; INQ000102974)
- Brytyjska strategia gotowości na pandemię grypy 2011, Departament Zdrowia, listopad 2011 r., pkt 4.26 (https://assets.publishing.service.gov.uk/media/5a7c4767e5274a2041cf2ee3/dh_131040.pdf; INQ000102974)
- Oświadczenie Premiera w związku z koronawirusem (COVID-19): 23 marca 2020 r., GOV.UK, 23 marca 2020 r. (https://www.gov.uk/government/speeches/pm-address-to-the-nation-on-coronavirus-23-march-2020)
- Brytyjska strategia gotowości na pandemię grypy 2011, Departament Zdrowia, listopad 2011 r., pkt 4.10–4.25 (https://assets.publishing.service.gov.uk/media/5a7c4767e5274a2041cf2ee3/dh_131040.pdf; INQ000102974)
- Brytyjska strategia gotowości na pandemię grypy 2011, Departament Zdrowia, listopad 2011 r., pkt 7.4, 7.25 (https://assets.publishing.service.gov.uk/media/5a7c4767e5274a2041cf2ee3/dh_131040.pdf; INQ000102974)
- Brytyjska strategia gotowości na pandemię grypy 2011, Departament Zdrowia, listopad 2011 r., pkt 7.26–7.29 (https://assets.publishing.service.gov.uk/media/5a7c4767e5274a2041cf2ee3/dh_131040.pdf; INQ000102974)
- Brytyjska strategia gotowości na pandemię grypy 2011, Departament Zdrowia, listopad 2011, pkt 7.30 (https://assets.publishing.service.gov.uk/media/5a7c4767e5274a2041cf2ee3/dh_131040.pdf; INQ000102974)
- Matt Hancock 27 czerwca 2023 72.11-21
- Sally Davies 20 czerwca 2023 154/22-155/16
- INQ000194054_0040 paragraf 157
- Emma Reed 26 czerwca 2023 13.14-17, 16.14-18
- Clara Swinson 19 czerwca 2023 161/17-162/4
- Clara Swinson 19 czerwca 2023 173/10-18; Zobacz też INQ000023017_0001
- INQ000182608_0022 paragraf 52
- Christopher Wormald 19 czerwca 2023 106/1-15, 122/1-9, 124/22-125/6, 154/13-17
- INQ000182616_0004 ust. 13
- Brytyjska strategia gotowości na pandemię grypy 2011, Departament Zdrowia, listopad 2011, s. 15, pierwszy akapit tekstu w ramce (https://assets.publishing.service.gov.uk/media/5a7c4767e5274a2041cf2ee3/dh_131040.pdf; INQ000102974)
- Brytyjska strategia gotowości na pandemię grypy 2011, Departament Zdrowia, listopad 2011 r., pkt 2.21, podpunkt czwarty (https://assets.publishing.service.gov.uk/media/5a7c4767e5274a2041cf2ee3/dh_131040.pdf; INQ000102974)
- INQ000184893_0004 pkt 8-9. Jak wyjaśniono w Rozdziale 3: Ocena ryzyka, choroba zakaźna o poważnych konsekwencjach to taka, która zazwyczaj charakteryzuje się wysokim współczynnikiem śmiertelności, może być trudna do szybkiego rozpoznania i wykrycia, może przenosić się w społeczeństwie i może nie mieć skutecznych środków zapobiegania lub leczenie. Wymaga wzmocnionej, specjalistycznej reakcji (zob INQ000184643_0005-0006, 0010-0012 pkt 20d, 41-55; INQ000196611_0009 przypis 2).
- Christopher Wormald 19 czerwca 2023 r. 110/6-15
- Christopher Wormald 19 czerwca 2023 123/8-14
- Christopher Wormald 19 czerwca 2023 125/22-126/1
- Christopher Whitty 22 czerwca 2023 r. 100/6-15
- Patrick Vallance 22 czerwca 2023 160/3-7
- Pandemia grypy 2009: Niezależny przegląd reakcji Wielkiej Brytanii na pandemię grypy w 2009 r., Dame Deirdre Hine, lipiec 2010, s. 5, 50, Zalecenie 1 (https://assets.publishing.service.gov.uk/media/5a7975f1ed915d0422068a10/the2009influenzapandemic-review.pdf; INQ000022705)
- Brytyjska strategia gotowości na pandemię grypy 2011, Departament Zdrowia, listopad 2011 r., pkt 3.2, podpunkt drugi (https://assets.publishing.service.gov.uk/media/5a7c4767e5274a2041cf2ee3/dh_131040.pdf; INQ000102974)
- Brytyjska strategia gotowości na pandemię grypy 2011, Departament Zdrowia, listopad 2011, s. 21–25 (https://assets.publishing.service.gov.uk/media/5a7c4767e5274a2041cf2ee3/dh_131040.pdf; INQ000102974)
- Brytyjska strategia gotowości na pandemię grypy 2011, Departament Zdrowia, listopad 2011, s. 25 (https://assets.publishing.service.gov.uk/media/5a7c4767e5274a2041cf2ee3/dh_131040.pdf; INQ000102974)
- INQ000195843_0043, 0075-0076 pkt 108, 181
- INQ000184637_0010 ust. 7.7
- Brytyjska strategia bezpieczeństwa biologicznego, rząd Jej Królewskiej Mości, czerwiec 2023 r., s. 14 (https://assets.publishing.service.gov.uk/media/64c0ded51e10bf000e17ceba/UK_Biological_Security_Strategy.pdf; INQ000208910)
- INQ000187308_0009 ust. 22; Zobacz też INQ000099516_0006 ust. 16
- INQ000187308_0008 ust. 20; Zobacz też George Osborne 20 czerwca 2023 61/6-23
- George Osborne 20 czerwca 2023 65.19-67.25, 75.12, 80.4-8; INQ000099516_0056-0057 pkt 242–243
- INQ000099516_0056-0057 pkt 242–243
- INQ000099516_0017 paragraf 65
- George Osborne 20 czerwca 2023 65/19-22
- George Osborne 20 czerwca 2023 r. 77/2-78/9
- George Osborne 20 czerwca 2023 71/8-72/1, 92/23-93/9, 96/25-97/3, 117/19-118/7
- George Osborne 20 czerwca 2023 r. 82/17-20
- INQ000130270_0007-0008 ust. 7; Fiscal Risks and Sustainability, Biuro Odpowiedzialności Budżetowej, lipiec 2022 r., s. 31–32 (https://obr.uk/docs/dlm_uploads/Fiscal_risks_and_sustainability_2022-1.pdf; INQ000119290)
- INQ000130270_0005 ust. 6d
- INQ000184637_0013 pkt 7.22
- INQ000184638_0053 ust. 6.14
- INQ000023131_0005
- Christopher Whitty 22 czerwca 2023 91/25
- Christopher Whitty 22 czerwca 2023 r. 24.11-93.22
- Jeremy Hunt 21 czerwca 2023 r. 161/4-8
- INQ000181825_0014 ust. 56
- Patrick Vallance 22 czerwca 2023 136/7-12
- INQ000181825_0014 ust. 56
- INQ000182616_0003 ust. 10-11
- Globalny wskaźnik bezpieczeństwa zdrowia: budowanie zbiorowych działań i odpowiedzialności, inicjatywa na rzecz zagrożenia nuklearnego/Johns Hopkins Bloomberg School of Public Health, 2019, s. 26 (https://www.nti.org/analysis/articles/global-health-security-index/; INQ000149103); Matt Hancock 27 czerwca 2023 r. 17.19-21
- Ramy odporności rządu Wielkiej Brytanii, Rząd Jej Królewskiej Mości, grudzień 2022 r., s. 7 (https://assets.publishing.service.gov.uk/media/63cff056e90e071ba7b41d54/UKG_Resilience_Framework_FINAL_v2.pdf; INQ000097685)
- Ramy odporności rządu Wielkiej Brytanii, Rząd Jej Królewskiej Mości, grudzień 2022 r., ust. 5 (https://assets.publishing.service.gov.uk/media/63cff056e90e071ba7b41d54/UKG_Resilience_Framework_FINAL_v2.pdf; INQ000097685)
- Ramy dotyczące odporności rządu Wielkiej Brytanii, Rząd Jej Królewskiej Mości, grudzień 2022 r., pkt 60 (https://assets.publishing.service.gov.uk/media/63cff056e90e071ba7b41d54/UKG_Resilience_Framework_FINAL_v2.pdf; INQ000097685); Roger Hargreaves 22 czerwca 2023 r. 14.00-51.15
- Ramy odporności rządu Wielkiej Brytanii, Rząd Jej Królewskiej Mości, grudzień 2022 r., s. 15 (https://assets.publishing.service.gov.uk/media/63cff056e90e071ba7b41d54/UKG_Resilience_Framework_FINAL_v2.pdf; INQ000097685). Podobnie było w przypadku podziału Sekretariatu ds. Zagrożeń Cywilnych na Jednostkę COBR i Dyrekcję ds. Odporności (zob. Roger Hargreaves 22 czerwca 2023 24.11-25, 22.08-44.08; Oliver Dowden 21 czerwca 2023 134/20-137/2).
- Ramy odporności rządu Wielkiej Brytanii, Rząd Jej Królewskiej Mości, grudzień 2022 r., s. 72–74 (https://assets.publishing.service.gov.uk/media/63cff056e90e071ba7b41d54/UKG_Resilience_Framework_FINAL_v2.pdf; INQ000097685)
- Roger Hargreaves 22 czerwca 2023 48/20-49/5
- Roger Hargreaves 22 czerwca 2023 r. 52.11-12
- Brytyjska strategia bezpieczeństwa biologicznego, rząd Jej Królewskiej Mości, czerwiec 2023 r. (https://assets.publishing.service.gov.uk/media/64c0ded51e10bf000e17ceba/UK_Biological_Security_Strategy.pdf; INQ000208910)
- Brytyjska strategia bezpieczeństwa biologicznego, rząd Jej Królewskiej Mości, czerwiec 2023 r., s. 8 (https://assets.publishing.service.gov.uk/media/64c0ded51e10bf000e17ceba/UK_Biological_Security_Strategy.pdf; INQ000208910)
- Brytyjska strategia bezpieczeństwa biologicznego, rząd Jej Królewskiej Mości, czerwiec 2023 r., s. 8 (https://assets.publishing.service.gov.uk/media/64c0ded51e10bf000e17ceba/UK_Biological_Security_Strategy.pdf; INQ000208910)
- Brytyjska strategia bezpieczeństwa biologicznego, rząd Jej Królewskiej Mości, czerwiec 2023 r., s. 8–9 (https://assets.publishing.service.gov.uk/media/64c0ded51e10bf000e17ceba/UK_Biological_Security_Strategy.pdf; INQ000208910)
- Brytyjska strategia bezpieczeństwa biologicznego, rząd Jej Królewskiej Mości, czerwiec 2023 r., s. 6 (https://assets.publishing.service.gov.uk/media/64c0ded51e10bf000e17ceba/UK_Biological_Security_Strategy.pdf; INQ000208910)
- Brytyjska strategia bezpieczeństwa biologicznego, rząd Jej Królewskiej Mości, czerwiec 2023 r., s. 56–59 (https://assets.publishing.service.gov.uk/media/64c0ded51e10bf000e17ceba/UK_Biological_Security_Strategy.pdf; INQ000208910)
- INQ000186622_0007-0009; INQ000068403_0021-0023, 0074 sekcje 4.2, 4.2.1, 4.2.2
- Christopher Whitty 22 czerwca 2023 112/9-10
- Christopher Whitty 22 czerwca 2023 112/13
- INQ000147707_0022 ust. 49
- INQ000142139
- Patrick Vallance 22 czerwca 2023 167/22-24
- INQ000176062_0022 paragraf 111
- INQ000176062_0019-0022 pkt 103–110
- INQ000087225, patrz szczególnie strony 106-168
- INQ000087225_0206 drugi akapit
- Christopher Whitty 22 czerwca 2023 114/4-5
- Raport techniczny na temat pandemii COVID-19 w Wielkiej Brytanii, Departament Zdrowia i Opieki Społecznej, 1 grudnia 2022 r., s. 159 (https://www.gov.uk/government/publications/technical-report-on-the-covid-19-pandemic-in-the-uk; INQ000130955)
- Raport techniczny na temat pandemii COVID-19 w Wielkiej Brytanii, Departament Zdrowia i Opieki Społecznej, 1 grudnia 2022 r., s. 228 (https://www.gov.uk/government/publications/technical-report-on-the-covid-19-pandemic-in-the-uk; INQ000130955)
- Raport techniczny na temat pandemii COVID-19 w Wielkiej Brytanii, Departament Zdrowia i Opieki Społecznej, 1 grudnia 2022 r., s. 39, 229 (https://www.gov.uk/government/publications/technical-report-on-the-covid-19-pandemic-in-the-uk; INQ000130955)
- Christopher Whitty 22 czerwca 2023 113/24-114/19
- INQ000145912_0128 pkt 10.26-10.27
- INQ000176062_0034 paragraf 166
- INQ000145912_0109-0110 pkt 9.157–9.159
- INQ000145912_0122 ust. 10.11.10
- Raport techniczny na temat pandemii COVID-19 w Wielkiej Brytanii, Departament Zdrowia i Opieki Społecznej, 1 grudnia 2022 r., akapit czwarty (https://www.gov.uk/government/publications/technical-report-on-the-covid-19-pandemic-in-the-uk; INQ000130955)
- INQ000184639_0026 ust. 8.10
- INQ000147810_0029 ust. 90; Zobacz też INQ000184639_0026 ust. 8.11; INQ000183421_0003 ust. 1.1.4
- Patrick Vallance 22 czerwca 2023 168/12-13
- INQ000147707_0026 paragraf 62
- INQ000147810_0035 paragraf 110
- INQ000148419_0014 ust. 5.10
- INQ000148419_0014 ust. 5.10
- INQ000195843_0082-0083 pkt 199.2, 199.6
- Widzieć INQ000184643_0024-0025, 0051 pkt 116–120, 277
- Widzieć INQ000184643_0051-0052 pkt 277, 284–285; INQ000148418_0006, 0029, 0031, 0033 pkt 2.13, 3.15–3.18, 3.22, 3.26(3)
- INQ000184643_0052 pkt 284–285
- INQ000196611_0012 pkt 23. Poparł to m.in. profesor David Heymann, biegły epidemiologiczny (por Załącznik 1: Informacje o tym module i metodologia badania) (INQ000195846_0057 ust. 268; David Heymann 15 czerwca 2023 65/12-14), Sir Jeremy Farrar, główny naukowiec Światowej Organizacji Zdrowia od maja 2023 r. i dyrektor Wellcome Trust od 2013 r. do 2023 r. (INQ000182610_0024) i dr Richard Horton, redaktor naczelny The Lancet od 1995 r. (Richard Horton 13 lipca 2023 78/21-79/3)
- INQ000196611_0012 pkt 25–30; Zobacz też INQ000195846_0043 paragraf 220
Rozdział 5: Uczenie się na doświadczeniach
Wstęp
| 5.1. | Uczenie się na podstawie doświadczeń stanowi podstawę prawidłowego planowania: powinno obejmować uczenie się, co się sprawdziło, a co nie, rozpoznawanie luk w systemie i naprawianie wszelkich wad. Jednym ze sposobów zdobywania takiej wiedzy są ćwiczenia symulacyjne. Są cennym narzędziem. |
| 5.2. | Celem ćwiczeń symulacyjnych jest możliwie przybliżenie okoliczności, w jakich powstają zdarzenia takie jak pandemia oraz sprawdzenie zdolności instytucji, struktur i systemów do reagowania na sytuację kryzysową. Wdrożone na dużą skalę mogą również stanowić okazję do zbadania odporności.1 To właśnie poprzez szczegółowe badanie sposobu reagowania na zagrożenie cywilne obejmujące cały system, system jest poddawany testom warunków skrajnych, co pozwala wykryć luki i wady w planowaniu. |
| 5.3. | W związku z tym rząd Wielkiej Brytanii i zdecentralizowane administracje od wielu lat przeprowadzają ćwiczenia w zakresie gotowości na wypadek pandemii. Na podstawie takich ćwiczeń oraz doświadczeń tego i innych krajów w radzeniu sobie z niedawnymi epidemiami Wielka Brytania powinna była zbudować „zbiorową pamięć” na temat tego, co oznacza gotowość na pandemię, i być dobrze przygotowana na Covid-19. W tym rozdziale zbadano, czy wyciągnięto wnioski, posłuchano ostrzeżeń i odpowiednio wzięto pod uwagę międzynarodową praktykę i doświadczenie. Bada także skuteczność systemu gotowości i odporności na sytuacje nadzwyczajne dla ludności w zakresie rozpoznawania własnych wad i eliminowania ich, jak wykazały ćwiczenia. Na koniec rozważono, w jaki sposób w przyszłości gotowość i odporność na cywilne sytuacje nadzwyczajne w całym systemie mogą zostać lepiej poddane testom warunków skrajnych, bardziej otwarte na kontrolę publiczną i skupione na podejmowaniu działań. |
Doświadczenia międzynarodowe i krajowe
| 5.4. | W latach 2017 i 2018 Światowa Organizacja Zdrowia przeprowadziła roczny przegląd chorób, którym jej zdaniem należy nadać priorytet ze względu na stwarzane przez nie ryzyko. Celem ćwiczenia było zidentyfikowanie luk w badaniach i rozwoju. Nie uwzględniono patogenów, które były dobrze znane i na które istniały już szczepionki, takie jak grypa. W przeglądzie z 2017 r. na listę patogenów, w przypadku których istniała pilna potrzeba badań i rozwoju, wpisano koronawirus zespołu oddechowego Bliskiego Wschodu (MERS-CoV) i koronawirus zespołu ostrej niewydolności oddechowej 1 (SARS-CoV-1).2 Takie samo stanowisko było w 2018 r., kiedy połączono je w jedną kategorię blisko spokrewnionych koronawirusów. Dodano także „chorobę X” jako znacznik potwierdzający, że następna pandemia może być spowodowana nową, wcześniej nieznaną, wysoce zjadliwą infekcją.3 |
Lekcje z SARS-CoV-1
| 5.5. | Ciężki ostry zespół oddechowy (SARS) wywołany przez SARS-CoV-1 był pierwszą poważną nowo pojawiającą się chorobą zakaźną przenoszoną z człowieka na człowieka w XXI wieku.4 Postęp wiedzy na temat koronawirusów w momencie ich pojawienia się spowodował, że stały się one tematem poważnego globalnego zainteresowania.5 Chociaż SARS-CoV-1 spowodował epidemie w wielu krajach, Wielka Brytania została w dużej mierze oszczędzona. W Wielkiej Brytanii było 368 podejrzanych przypadków, ale tylko jedna potwierdzona infekcja, bez dalszego przenoszenia i bez zgonów.6 |
| 5.6. | Epidemia SARS w latach 2002–2003 była pierwszym poważnym testem gotowości Wielkiej Brytanii na wypadek pandemii w tym stuleciu. Doktor Philip Mortimer, były kierownik działu wirusologii w Laboratorium Zdrowia Publicznego, napisał w 2003 roku:
"[I]nie należy zakładać, że ponowne wystąpienie SARS jest… mało prawdopodobne lub że dalszą epidemię można będzie kontrolować… Jeżeli występują słabe strony lub braki, nie należy sądzić, że można je lub należy naprawić za pomocą szybkich rozwiązań za każdym razem, gdy zmaterializuje się poważne zagrożenie . Takie wydatki nie pozwalają na zbudowanie infrastruktury niezbędnej do utrzymania kompleksowej zdolności do szybkiego i odpowiedniego technologicznie reagowania na nowe patogeny.”7 |
| 5.7. | Dr Mortimer poinformował, że Wielka Brytania potrzebuje zintegrowanej infrastruktury laboratoryjnej zdrowia publicznego, wydajności lokalnych laboratoriów, znaczników kontaktów i łóżek izolacyjnych. Przestrzegł przed nadmiernym poleganiem na matematycznym modelowaniu chorób i danych wywiadowczych dotyczących epidemii zamiast tego, co jego zdaniem jest naprawdę ważne, czyli wystarczającej podstawowej infrastruktury.8 |
| 5.8. | Ćwiczenia Shipshape odbyły się 6 czerwca 2003 r. po potwierdzeniu pierwszego przypadku SARS w Wielkiej Brytanii.9 Ćwiczenie to dostarczyło ważnych ostrzeżeń na temat stanu gotowości Anglii i Walii w tamtym czasie na radzenie sobie z epidemiami chorób zakaźnych o poważnych konsekwencjach, takich jak SARS. Obejmowały one obserwacje dotyczące znaczenia:
|
| 5.9. | Ćwiczenie Bennachie, które odbyło się w grudniu 2004 r., doprowadziło do podobnych wniosków w przypadku Szkocji, ale zawierało także obserwacje dotyczące potrzeby usprawnienia, racjonalizacji i aktualizacji dużej liczby planów w zakresie chorób zakaźnych.11 |
| 5.10. | Ćwiczenia Goliat, które odbyły się w grudniu 2003 r., sprawdzały reakcję Irlandii Północnej. Stwierdziła potrzebę szerszej dyskusji na temat zapobiegania początkowemu rozprzestrzenianiu się wirusa (a nie tylko radzenia sobie z jego skutkami).12 |
| 5.11. | W 2005 r. raport Agencji Ochrony Zdrowia formalnie udokumentował wnioski wyciągnięte z epidemii SARS, w tym następujące:
|
| 5.12. | Międzynarodowe doświadczenia związane z epidemią SARS w latach 2002–2003 oraz następujące po nich ćwiczenia krajowe ujawniły szereg ważnych wniosków. Gdyby wnioski te zostały wzięte pod uwagę i zastosowane w kontekście krajowym, Wielka Brytania byłaby lepiej przygotowana na pandemię wirusa Covid-19, która uderzyła w styczniu 2020 r. |
Lekcje z wirusa H1N1 („świńska grypa”)
| 5.13. | Kolejnym ważnym testem gotowości Wielkiej Brytanii na wypadek pandemii była pandemia grypy H1N1 („świńskiej grypy”) w latach 2009–2010. Na szczęście była to stosunkowo łagodna choroba dla większości dotkniętych nią osób i wiele z zapasów szczepionek i środków ochrony osobistej nie zostało wykorzystanych.16 |
| 5.14. | W przeglądzie Dame Deirdre Hine z 2010 r. dotyczącym reakcji Wielkiej Brytanii na pandemię grypy H1N1 zauważono, że „proporcjonalne i skuteczne”, z wieloma dobrymi praktykami, na których można budować.17 Zauważyła jednak:
"[I]w przypadku poważniejszej pandemii pracownicy służby zdrowia prawdopodobnie byliby przytłoczeni szybciej, a zasoby zostałyby wykorzystane do leczenia przypadków zamiast wdrażania środków ograniczających rozprzestrzenianie się wirusa.”18 |
| 5.15. | Zdecentralizowane administracje przeprowadziły także inne przeglądy wewnętrzne. Na przykład w artykule opracowanym przez rząd Szkocji opisano Szkocję jako „uważaną przez resztę Wielkiej Brytanii za stojącą w awangardzie walki z wirusem”.19 Stwierdzono:
"[H]chociaż wirus był poważniejszy lub trwał dłużej, spowodowałoby to znaczne zakłócenia normalnego funkcjonowania NHS.”20 |
| 5.16. | W Walii podobną obserwację poczyniono w raporcie z ćwiczenia Taliesin z 2009 r. Pandemia grypy H1N1 nie wystawiła w pełni na próbę planów reagowania Walii, ponieważ dotkliwość pandemii spadła znacznie poniżej oczekiwań.21 |
| 5.17. | W pewnym stopniu pandemia grypy H1N1 uśpiła rząd Wielkiej Brytanii i zdecentralizowane administracje w fałszywym poczuciu bezpieczeństwa.22 Chociaż znaki ostrzegawcze były obecne, były one ukryte za wybuchem znacznie łagodniejszego patogenu, niż oczekiwano. |
Lekcje z Eboli
| 5.18. | Wybuch epidemii wirusa Ebola w Afryce Zachodniej w latach 2013–2016 był największym wystąpieniem tego wirusa od czasu jego pierwszego odkrycia w 1976 r. Do czasu, gdy w sierpniu 2014 r. Światowa Organizacja Zdrowia ogłosiła go stanem nadzwyczajnym w zakresie zdrowia publicznego o zasięgu międzynarodowym, importowano do kilku krajów, w tym do Włoch, Hiszpanii, Wielkiej Brytanii i USA.23 |
| 5.19. | Środki podjęte w Wielkiej Brytanii w odpowiedzi na epidemię wirusa Ebola obejmowały badanie przesiewowe objawów w portach wejścia, śledzenie kontaktów w przypadku pozytywnych przypadków oraz utworzenie programu w zakresie chorób zakaźnych o poważnych konsekwencjach, który obejmował nadzór.24 Utworzono także brytyjską sieć szczepień.25 Public Health England zapewniło badania przesiewowe na wejściu podróżnym przybywającym z krajów wysokiego ryzyka. Zespoły sprawdzające skupiły się na londyńskich lotniskach Heathrow i Gatwick oraz w Birmingham i Manchesterze, gdzie do Wielkiej Brytanii przybyło ponad 97% odpowiednich pasażerów, w tym wszyscy zidentyfikowani pracownicy podwyższonego ryzyka.26 W Wielkiej Brytanii odnotowano tylko trzy przypadki wirusa Ebola, bez dalszego rozprzestrzeniania się.27 |
| 5.20. | Wspólny raport Departamentu Zdrowia, NHS England i Public Health England z lipca 2013 r., Wyciągnięcie wniosków z reakcji na wirusa Ebola, zalecił przegląd uprawnień prawnych, aby umożliwić bardziej systematyczne podejście do kontroli portowych i granicznych.28 Stwierdzono:
„Obecnie istnieją różne kontrole i uprawnienia w zakresie zarządzania chorobami, które nie są stosowane systematycznie w przypadku różnych rodzajów portów wprowadzenia lub w przypadku różnych grup chorób. Istnieje możliwość przeglądu i dostosowania wszystkich odpowiednich uprawnień, aby umożliwić logiczne, stopniowane interwencje od portu do społeczności. O ile to możliwe, wymagania operacyjne należy uwzględniać obok kwestii politycznych i prawnych, chociaż nie zawsze będzie to proste.”29 |
| 5.21. | Przed spotkaniem szefów rządów G7 w 2015 r. poseł David Cameron, premier od maja 2010 r. do lipca 2016 r., powiedział:
„Niedawna epidemia wirusa Ebola w szokujący sposób przypomniała o zagrożeniu, przed jakim stoimy wszyscy w wyniku wybuchu choroby… Jednak rzeczywistość jest taka, że ponownie staniemy w obliczu epidemii takiej jak Ebola, a wirus ten może być bardziej agresywny i trudniejszy do powstrzymania. Najwyższy czas obudzić się i zdać sobie sprawę z tego zagrożenia.”30 |
| 5.22. | W marcu 2015 r. w Anglii przeprowadzono ćwiczenia w zakresie gotowości na wypadek wirusa Ebola. Jego celem było przetestowanie wydajności i odporności szpitali i agencji zdrowia w warunkach skrajnych poprzez rozważenie ustaleń w czterech wyznaczonych ośrodkach NHS w Anglii w celu zareagowania na nową chorobę zakaźną o poważnych konsekwencjach (liczne pozytywne przypadki wirusa Ebola).31 Chociaż ośrodki miały pewność, że poradzą sobie ze skutkami posiadania jednego pacjenta z wirusem Ebola, podniesiono poważne kwestie dotyczące wyzwań związanych z leczeniem wielu pacjentów jednocześnie.32 |
| 5.23. | Wkrótce po ćwiczeniach utworzono Program Chorób Zakaźnych Poważnych Konsekwencji. Jego celem było opracowanie uzgodnionej metody postępowania z podejrzanymi i potwierdzonymi chorobami zakaźnymi o poważnych konsekwencjach oraz utworzenie dodatkowych specjalistycznych placówek, w których można by leczyć pacjentów z chorobami wysoce zakaźnymi lub zakaźnymi.33 Doktor Michael Prentice w imieniu NHS England powiedział śledczym:
„Głównym powodem powołania Programu było utrzymujące się zagrożenie chorobami „przenoszonymi drogą powietrzną”, takimi jak MERS, SARS i ptasia grypa.”34 Program miał jednak dotyczyć wyłącznie „małe liczby”pacjentów.35 W całej Anglii uruchomiono cztery nowe ośrodki leczenia HCID przenoszonych drogą powietrzną (w celu całkowitego ograniczenia wszelkich chorób zakaźnych o poważnych konsekwencjach przenoszonych drogą powietrzną, przy czym każdy ośrodek rutynowo zapewnia dwa łóżka) |
| 5.24. | Reakcja Wielkiej Brytanii na wirusa Ebola i rozwój Programu chorób zakaźnych o poważnych konsekwencjach były znaczącymi sukcesami w zakresie przygotowania Wielkiej Brytanii na niewielki wybuch choroby zakaźnej o poważnych konsekwencjach. Jednakże rząd Wielkiej Brytanii, zdecentralizowane administracje i agencje zdrowia publicznego nie rozważyły odpowiednio, czy Wielka Brytania jest przygotowana na radzenie sobie z epidemią lub wybuchem nowej choroby zakaźnej na skalę pandemiczną (w tym choroby zaklasyfikowanej jako choroba zakaźna o poważnych konsekwencjach). |
Lekcje z MERS
| 5.25. | MERS to wysoce śmiertelna choroba zakaźna o poważnych konsekwencjach, wywoływana przez koronaawirusa MERS-CoV.38 W lutym 2016 r. w Londynie przeprowadzono ćwiczenia Alice, których celem było zbadanie wyzwań, jakie może wiązać się z epidemią MERS na dużą skalę w Anglii.39 Jego celem nie było sprawdzenie gotowości na wypadek sytuacji nadzwyczajnej cywilnej całego systemu na skalę pandemii, ale raczej ocena gotowości Wielkiej Brytanii na „na dużą skalę”wybuch MERS.40 Symulowany scenariusz rozpoczął się od przyjęcia do szpitala trzech „pacjentów” z objawami infekcji. Rozwinęło się w 50 „potwierdzonych” laboratoryjnie przypadków MERS z łączną liczbą możliwych kontaktów 650.41 |
| 5.26. | Z ćwiczenia jasno wynikało, że na najwcześniejszych etapach takiej epidemii kluczową rolę odgrywali odpowiednio przeszkoleni specjaliści z dostępem do wystarczających ilości środków ochrony indywidualnej, wystarczającą liczbą łóżek i specjalistycznym sprzętem klinicznym.42 Zaobserwowano, że chociaż wnioski dotyczące wirusa Ebola poprawiły kontrolę infekcji, nadal nie zostało to uwzględnione w systemie.43 |
| 5.27. | Uczestnicy ćwiczenia (w tym przedstawiciele NHS England, Public Health England, Departamentu Zdrowia i obserwatorzy ze zdecentralizowanych organów administracji Walii i Szkocji) pytali o zarządzanie w przypadku wybuchu epidemii MERS w Korei Południowej w 2015 r.44 Ważne były trzy aspekty doświadczeń Korei Południowej: objęcie kwarantanną około 17 000 osób, dowody na późniejsze przeniesienie wirusa oraz znaczenie bezpieczeństwa granic w postaci kontroli temperatury.45 |
| 5.28. | Odbyła się znacząca dyskusja na temat ograniczenia przemieszczania się pacjentów z objawami, narażonymi i bezobjawowymi. Dyskutowano, czy izolacja ta powinna być dobrowolna (samoizolacja), czy wymuszona (kwarantanna). Jedną z omawianych opcji było, wzorując się na modelu południowokoreańskim, wykorzystanie hoteli do izolacji. Innym było korzystanie z wyznaczonych miejsc, w których znajdowały się stanowiska do szczepień oddechowych i diagnostyki, w celu zapewnienia zakwaterowania ludziom. Dyskutowano także na temat prawa do ograniczenia przemieszczania się. Zasugerowano, że pragmatycznym rozwiązaniem byłoby doradzanie i namawianie osób do samoizolacji w domu pod aktywnym nadzorem zdrowotnym, udzielanie im informacji i oferowanie codziennego kontaktu ze specjalistami ochrony zdrowia.46 |
| 5.29. | W ćwiczeniu określono 12 działań. Należą do nich:
|
| 5.30. | Jako organizacja zlecająca, Departament Zdrowia i Opieki Społecznej był odpowiedzialny za przydział działań wynikających z Ćwiczeń Alicja i „osadzanie uczenia się”.50 Działania te pozostały jednak nieprzydzielone.51 |
| 5.31. | Sir Christopher Wormald, stały sekretarz Departamentu Zdrowia i Opieki Społecznej od maja 2016 r., zapytany w ramach dochodzenia, czy departament podjął jakiekolwiek działania wynikające z ćwiczeń Alice, powiedział, że niektóre „były częściowo, ale masz rację, że nie wszystkie były w całości”.52 Zalecenia, które nie zostały zrealizowane, obejmowały sporządzenie dokumentu informacyjnego na temat doświadczeń Korei Południowej i planowanie kwarantanny do samoizolacji.53 |
| 5.32. | W raporcie „wyciągniętych wniosków” z września 2020 r. Departament Zdrowia i Opieki Społecznej stwierdził, że:
„skorzystalibyśmy na pełniejszym zrozumieniu reakcji krajów azjatyckich… na wcześniejszym etapie planowania, co mogłoby umożliwić nam wcześniejsze rozpoczęcie tworzenia systemów testowych”.54 Wielu świadków zgodziło się, że pomocne byłoby rozważenie reakcji w Azji Wschodniej na SARS i MERS przed przybyciem Covid-19 do Wielkiej Brytanii.55 |
| 5.33. | W Korei Południowej reakcja na MERS obejmowała zwiększenie liczby łóżek na potrzeby hospitalizacji i izolacji, udostępnienie sal wyposażonych w urządzenia do dializy nerek i wentylacji, a także zaawansowaną sieć laboratoriów publicznych i prywatnych, aby umożliwić szybkie zwiększenie skali testów. W styczniu 2020 r. Korei Południowej udało się wykryć przypadki Covid-19 i szybko wdrożono reakcję, co doprowadziło do szybkiej identyfikacji i izolacji potencjalnie zakaźnych nosicieli.56 |
| 5.34. | Bazując na swoich doświadczeniach z SARS, Tajwan był w podobny sposób w stanie szybko zwiększyć skalę testów, aby w ciągu kilku dni zidentyfikować osoby, które mogły być narażone na Covid-19; musieli odbyć kwarantannę. Wczesna identyfikacja źródła infekcji w połączeniu z wczesnymi ograniczeniami w podróżach międzynarodowych skutecznie ograniczyła rozprzestrzenianie się Covid-19.57 |
| 5.35. | Jedna z najbardziej uderzających różnic między podejściami stosowanymi w Wielkiej Brytanii i Azji Wschodniej polegała na tym, że w tym drugim przypadku panowało przekonanie, że przy odpowiedniej infrastrukturze można powstrzymać rozprzestrzenianie się wirusa. Byłoby to wykorzystanie tego, co profesor David Heymann, biegły epidemiologiczny (por Załącznik 1: Informacje o tym module i metodologia badania), opisany jako "dobra podstawowa epidemiologia i kontrola epidemii”.58 W dochodzeniu powiedziano, że można wyciągnąć wnioski z doświadczeń Korei Południowej i Tajwanu oraz że połączenie wczesnych ograniczeń granicznych, lokalnych blokad, rygorystycznych testów, ustalania kontaktów zakaźnych i poddania kwarantannie rozprzestrzenianie się koronaawirusa takiego jak Covid -19 można było opanować, zanim wynaleziono szczepionkę.59 |
| 5.36. | Brak dokładnego zbadania takich środków przed pandemią Covid-19 oznaczał, że Wielka Brytania była narażona na ryzyko konieczności tworzenia polityki w czasie stanu nadzwyczajnego, a nie przed wystąpieniem stanu nadzwyczajnego. |
Testowanie warunków skrajnych brytyjskich systemów gotowości na wypadek pandemii
Rysunek 9: Kalendarium kluczowych działań przeprowadzonych w latach 2003–2018
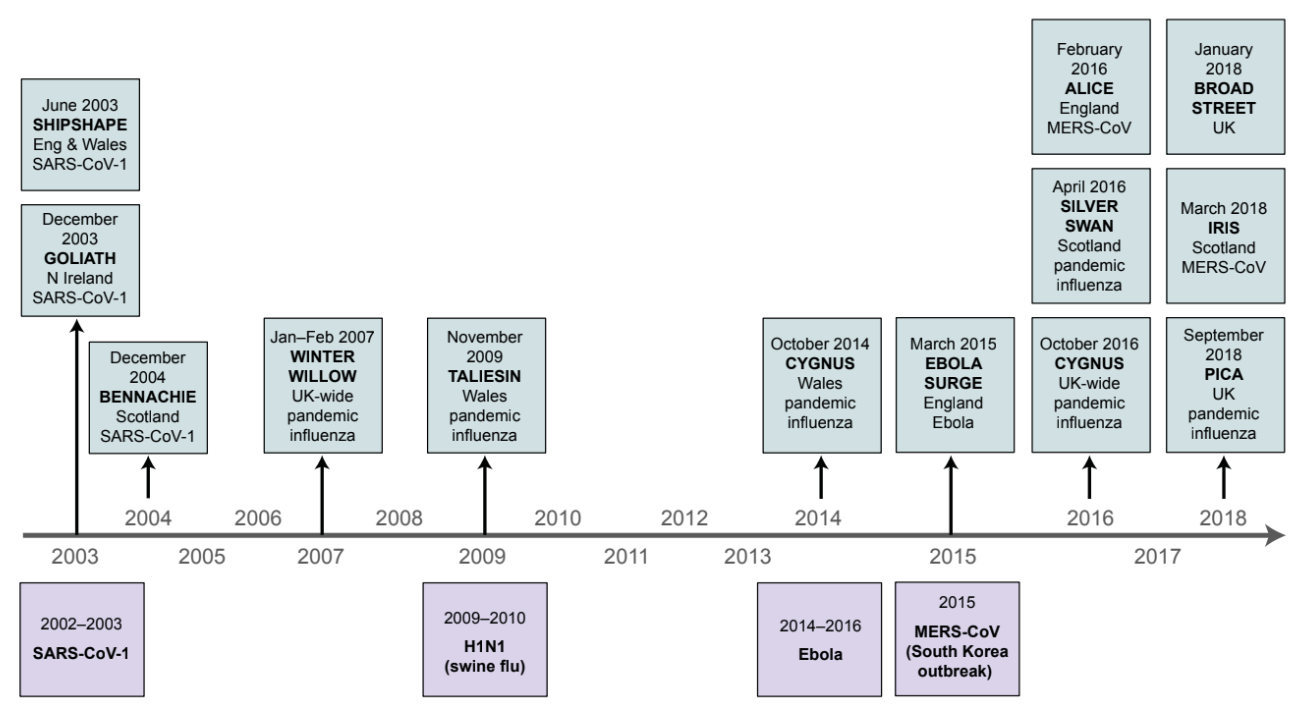
| 5.37. | Oprócz ćwiczeń i raportów określonych powyżej w kontekście ognisk poszczególnych wirusów, w czterech krajach Wielkiej Brytanii przeprowadzono dalsze ćwiczenia.60 Chociaż istniały pewne różnice w tematyce i dokładnym zakresie każdego ćwiczenia, zidentyfikowane problemy w znacznym stopniu się pokrywały. |
Ćwicz Łabędzia
| 5.38. | Ćwiczenia Cygnus były głównymi, trzydniowymi ćwiczeniami międzyrządowymi, które odbyły się w październiku 2016 r. Zasługują na szczególną uwagę, ponieważ ich ustalenia i zalecenia w ostry sposób przypominały o stanie Wielkiej Brytanii w zakresie gotowości i odporności na pandemię w ciągu trzech lat poprzedzające pandemię Covid-19. |
| 5.39. | Opierało się ono na czterech symulowanych spotkaniach COBR (krajowego centrum zarządzania kryzysowego rządu Wielkiej Brytanii zajmującego się reagowaniem na cywilne sytuacje kryzysowe w całym systemie) i miało na celu ocenę gotowości Wielkiej Brytanii i reakcji na epidemię grypy pandemicznej. Ćwiczenia przeprowadzono w siódmym tygodniu pandemii, która dotknęła do 50% populacji Wielkiej Brytanii i spowodowała śmierć od 200 000 do 400 000 dodatkowych osób. Ponad 950 przedstawicieli krajów zdecentralizowanych, Departament Zdrowia i 12 innych departamentów rządowych, NHS Wales, NHS England, Public Health England, osiem lokalnych forów na rzecz odporności (partnerstwa wieloagencyjne składające się z przedstawicieli lokalnych służb publicznych) i sześć więzień wziął udział w ćwiczeniu.61 |
| 5.40. | Z ćwiczenia wynikały 4 kluczowe „efekty uczenia się” i 22 szczegółowe wnioski, w tym:
|
| 5.41. | Jednym z kluczowych efektów uczenia się Ćwiczenia Cygnus było:
"[T]Gotowość i reakcja Wielkiej Brytanii pod względem planów, polityk i możliwości są obecnie niewystarczające, aby sprostać ekstremalnym wymaganiom związanym z poważną pandemią, która będzie miała ogólnokrajowy wpływ we wszystkich sektorach.”68 |
| 5.42. | W lutym 2017 r., po ćwiczeniach Cygnus, posłanka Theresa May (premier od lipca 2016 r. do lipca 2019 r.) zauważyła na posiedzeniu podkomisji Rady Bezpieczeństwa Narodowego (zagrożenia, zagrożenia, odporność i nieprzewidziane zdarzenia), że pandemia grypy stanowi największe ryzyko, na jakie naraża się przez Wielką Brytanię.69 |
| 5.43. | Na tym posiedzeniu poruszono wiele ważnych spraw. Uzgodniono, że:
Jednakże na tym spotkaniu nie odniesiono się do zasadniczego wniosku z ćwiczeń Cygnus – że plany, polityka i możliwości reagowania Wielkiej Brytanii na wypadek pandemii nie były wystarczające, aby sprostać ekstremalnym wymaganiom związanym z poważną pandemią.73 Samo ćwiczenie Cygnus miało także zasadniczą wadę: nie uwzględniało w nim niczego szerszego niż pandemia grypy i przedstawiony scenariusz.74 |
Rada ds. gotowości na pandemię grypy
| 5.44. | W odpowiedzi na ćwiczenia Cygnus w marcu 2017 r. na wniosek Podkomisji ds. Zagrożeń, Niebezpieczeństw, Odporności i Sytuacji Nieprzewidzianych powołano Radę ds. Gotowości na Pandemię Grypy.75 Współprzewodniczyli mu urzędnicy z Urzędu Rady Ministrów i Ministerstwa Zdrowia.76 Zarząd składał sprawozdania Podkomisji ds. Zagrożeń, Niebezpieczeństw, Odporności i Sytuacji Nieprzewidzianych za pośrednictwem Sekretarza Stanu ds. Zdrowia i Ministra Gabinetu.77 |
| 5.45. | Zarys planu pracy zarządu z kwietnia 2017 r. obejmował:
|
| 5.46. | Plan prac nie obejmował trzech kluczowych kwestii zidentyfikowanych podczas posiedzenia Podkomitetu ds. Zagrożeń, Niebezpieczeństw, Odporności i Sytuacji Nieprzewidzianych w lutym 2017 r. Obejmowały one rozważenie ograniczenia przepływu pracowników, którzy nie są niezbędni, różne scenariusze planowania pandemii, które uwzględniały potencjalną charakterystykę pandemii, oraz inne bardziej radykalne środki kontroli przenoszenia (jak omówiono powyżej).79 Były to istotne zaniedbania ze strony Urzędu Rady Ministrów i Departament Zdrowia. |
| 5.47. | W sierpniu 2017 r. Katharine Hammond, dyrektor Sekretariatu ds. Zagrożeń Cywilnych od sierpnia 2016 r. do sierpnia 2020 r., napisała do Marka Sedwilla, doradcy ds. bezpieczeństwa narodowego na lata 2017–2020. Stwierdziła:
„Obecnie kluczowym ryzykiem dla dostaw jest znaczna presja na zasoby w ramach [Departament Zdrowia] …w dalszym ciągu brakuje zasobów przeznaczonych na program.”80 |
| 5.48. | W kwietniu 2018 r. poseł Jeremy Hunt (sekretarz stanu ds. zdrowia i opieki społecznej od września 2012 r. do lipca 2018 r.) i poseł David Lidington (minister gabinetu i kanclerz Księstwa Lancaster od stycznia 2018 r. do lipca 2019 r.) napisali do członków podkomisji ds. zagrożeń, zagrożeń, odporności i nieprzewidywalnych sytuacji w celu przedstawienia aktualnych informacji na temat prac Rady ds. gotowości na pandemię grypy. Stwierdzili, że „[a] wiele osiągnięto, ale pozostaje jeszcze wiele do zrobienia, aby utrzymać i zwiększyć gotowość do akceptowalnego poziomu”.81 Określili proponowane działania na następne 12 miesięcy i zobowiązali się do zapewnienia „dalsze informacje na temat postępów… na początku 2019 r”.82 Było to opóźnienie o rok w stosunku do pierwotnego terminu „początek 2018 roku”, który został ustawiony na „ukończenie wszystkich dostaw”.83 |
| 5.49. | Matt Hancock, poseł do parlamentu, sekretarz stanu ds. zdrowia i opieki społecznej od lipca 2018 r. do czerwca 2021 r., powiedział w dochodzeniu, że został poinformowany o ćwiczeniach Cygnus i roli Rady ds. gotowości na pandemię grypy. Powiedział:
„Uznałem to za uspokajające. Zapewniono mnie, że zasadniczo wszystko jest pod ręką, ponieważ istnieje struktura, struktura posiadająca zasoby, która umożliwia to urzeczywistnienie.”84 |
| 5.50. | Jednakże po posiedzeniu Podkomitetu ds. Zagrożeń, Niebezpieczeństwa, Odporności i Sytuacji Nieprzewidzianych, o którym mowa powyżej, w lutym 2017 r., nie zebrał się on jednak ponownie. Podobnie Rada ds. gotowości na pandemię grypy nie spotykała się przez rok od listopada 2018 r. do listopada 2019 r. Po rocznej przerwie uznano, że istnieje potrzeba „ponownie ożywić Zarząd” i do „ustalaj priorytety i ponownie energetyzuj strumienie pracy oraz [Tablica]".85 Priorytetem rządu Wielkiej Brytanii nigdy nie było powrót do gotowości na wypadek pandemii. Rada ds. gotowości na pandemię grypy zebrała się ponownie dopiero 23 stycznia 2020 r.86 |
Ograniczenia ćwiczeń
| 5.51. | Wartość ćwiczeń została podważona przez ich ograniczenia. |
| 5.52. | Po pierwsze, w żadnym z czterech krajów nie przeprowadzono ćwiczeń, podczas których sprawdzano wybuch epidemii lub wybuchu nowej choroby zakaźnej na skalę pandemii (w tym choroby zaklasyfikowanej jako choroba zakaźna o poważnych konsekwencjach). Oznaczało to, że przed pandemią Covid-19 nie stosowano takich środków, jak masowe testy, śledzenie masowych kontaktów, obowiązkowe dystansowanie społeczne czy blokady. |
| 5.53. | Po drugie, ćwiczenie Cygnus nie dało uczestnikom możliwości przetestowania ich zdolności do zatrzymania lub powstrzymania przenoszenia wirusa w początkowej fazie reakcji na pandemię grypy. |
| 5.54. | Po trzecie, pytania „co by było, gdyby” zadawane były rzadko, jeśli w ogóle, i udzielane na nie odpowiedzi. Na przykład nikt w Departamencie Zdrowia i Opieki Społecznej ani w Ministerstwie Zdrowia Publicznego Anglii nie zapoznał się z ćwiczeniami Alice dotyczącymi chorób zakaźnych o poważnych konsekwencjach i ćwiczeniami Cygnus dotyczącymi grypy pandemicznej i nie zapytał, w jaki sposób Wielka Brytania może spowolnić lub zatrzymać przenoszenie nowej i istotnej choroby, która może może wywołać pandemię.87 |
| 5.55. | Po czwarte, rola władz lokalnych, lokalnych służb ratowniczych oraz sektora wolontariatu, społeczności i przedsiębiorstw społecznych w ćwiczeniach nie została odpowiednio uwzględniona. Są one absolutnie niezbędne w planowaniu pandemii, a jednak ćwiczenia zbadane w ramach dochodzenia nie obejmowały odpowiednio osób działających w terenie. Dla przykładu Mark Lloyd, dyrektor naczelny Stowarzyszenia Samorządów Lokalnych od listopada 2015 r., powiedział, że tylko 8 z 42 lokalnych forów dotyczących odporności wzięło udział w ćwiczeniu Cygnus.88 |
| 5.56. | Po piąte, brakowało otwartości w odniesieniu do wyników ćwiczeń. Związek Samorządowy nie dostrzegł wniosków z ćwiczeń Cygnus. Mimo że raport z ćwiczenia Cygnus umieścił na swojej liście dystrybucyjnej wszystkie lokalne fora dotyczące odporności i miał zostać opublikowany w serwisie ResilienceDirect, Stowarzyszenie Samorządów Lokalnych uzyskało ujawnienie raportu dopiero w wyniku postępowania sądowego wszczętego przez inny organ w 2020 r.89 Nie była świadoma istnienia ćwiczenia Alice aż do jesieni 2022 r., kiedy o jego istnieniu dowiedziała się w wyniku niniejszego dochodzenia.90 Władze lokalne nie były zaangażowane w ćwiczenia Alice, nie udostępniono też ich raportów ani zaleceń.91 Pan Lloyd powiedział w dochodzeniu, że gdyby Stowarzyszenie Samorządów Lokalnych wiedziało o takich kwestiach, jak potencjalne znaczenie kwarantanny w planowaniu, „zmieniłoby to, co robiliśmy w naszym planowaniu lokalnym”.92 Wiele innych osób żywo zainteresowanych wynikami ćwiczeń Cygnus, w tym Royal College of Nursing i podmioty świadczące prywatne domy opieki, nie było w stanie wyciągnąć z nich wniosków ani wnieść wkładu do dyskusji na temat sposobów ulepszenia systemów gotowości.93 Raporty powinny były być udostępniane rządom i kluczowym organizacjom, a także społeczeństwu. |
| 5.57. | Po szóste, chociaż poprzednie pandemie uwidoczniły i pogłębiły nierówności w zdrowiu, ćwiczenia nie zajmowały się rutynowo tym problemem.94 W dochodzeniu zwrócono się do profesor Clare Bambra i profesora Sir Michaela Marmota, biegłych w dziedzinie nierówności zdrowotnych (zob. Załącznik 1: Informacje o tym module i metodologia badania), aby rozważyć materiał dotyczący próbki 12 ćwiczeń. Nie znaleźli żadnej wzmianki o szczególnych potrzebach osób bezbronnych.95 Profesor Isabel Oliver, tymczasowa dyrektor ds. nauki w brytyjskiej Agencji Bezpieczeństwa Zdrowia od października 2021 r., poinformowała w toku dochodzenia, że przed pandemią Covid-19 potencjalny wpływ nierówności zdrowotnych nie był rutynowo uwzględniany w ćwiczeniach jako szczegółowy cel ćwiczeń.96 |
| 5.58. | Pomimo znacznej liczby przeprowadzonych ćwiczeń i raportów na temat gotowości na wypadek pandemii opracowanych przez rząd Wielkiej Brytanii, zdecentralizowane administracje i agencje zdrowia publicznego, wnioski wyniesione z nich nie zostały dostatecznie udostępnione i przedyskutowane. W wielu przypadkach wnioski i zalecenia, choć nominalnie zapisane w dokumentacji, po prostu nie zostały zastosowane lub zostały zapomniane. Wprowadzenie w październiku 2022 r. przez Gabinet Rady Ministrów do Podsumowanie lekcji dotyczących odporności w Wielkiej Brytanii pomoc w rozwiązaniu niektórych z tych problemów jest pozytywną zmianą, ale pozostaje jeszcze wiele do zrobienia.97 |
| 5.59. | Podejście do ćwiczeń stało się biurokratyczne i nieskuteczne. Rząd Wielkiej Brytanii i zdecentralizowane administracje były nadmiernie skupione na przeprowadzaniu ćwiczeń i sporządzaniu raportów, zamiast na wyciąganiu wniosków i wdrażaniu swoich zaleceń. Sprawozdania nie spowodowały istotnej poprawy gotowości ani nie pomogły w pociągnięciu do odpowiedzialności odpowiednich agencji i przywódców politycznych. Stały się celem samym w sobie, a nie sposobem na wyciągnięcie wniosków na przyszłość. Jak stwierdził dr Claas Kirchhelle, biegły ds. struktur zdrowia publicznego (zob Załącznik 1: Informacje o tym module i metodologia badania), stwierdził:
„Jednym z najbardziej niepokojących spostrzeżeń… jest to, jak dobrze znane były strukturalne słabości brytyjskich zdolności reagowania na pandemię do czasu pandemii Covid-19… W wyniku selektywnego oficjalnego przechwytywania pamięci nie podjęto żadnych działań po ostrzeżeniach.”98 |
| 5.60. | Cały system gotowości i odporności na pandemię powinien był również podlegać bardziej rygorystycznym, regularnym i zbiorowym testom warunków skrajnych, aby zapewnić jego skuteczność w przypadku sytuacji nadzwyczajnej. Sir Oliver Letwin, poseł do parlamentu, minister polityki rządowej od maja 2010 r. do lipca 2016 r. i kanclerz księstwa Lancaster od lipca 2014 r. do lipca 2016 r., zasugerował, że Wielka Brytania powinna włożyć więcej wysiłku niż dotychczas w wielokrotne przeprowadzanie ćwiczeń na dużą skalę w celu przetestować jego odporność na różne formy katastrof cywilnych obejmujących cały system, w tym pandemie.99 Dochodzenie z zadowoleniem przyjmuje zaangażowanie Gabinetu Rady Ministrów w przywrócenie Krajowego Programu Ćwiczeń.100 |
Zidentyfikowano kluczowe wnioski
| 5.61. | Ćwiczenia przeprowadzone w Wielkiej Brytanii oraz inne informacje dostępne rządowi Wielkiej Brytanii i zdecentralizowanej administracji uwydatniły szereg działań, które można i należało podjąć w celu przygotowania się na wybuch epidemii lub wybuchu nowej choroby zakaźnej na skalę pandemii (w tym choroby zaklasyfikowanej jako choroba zakaźna) choroba zakaźna o poważnych konsekwencjach). Polegały one zasadniczo na stworzeniu solidnych epidemiologicznie i skutecznych środków kontroli infekcji, w tym:
|
Testowanie i śledzenie kontaktów
| 5.62. | Po wybuchu epidemii wirusa Ebola w Afryce Zachodniej w latach 2013–2016 wprowadzono system śledzenia kontaktów, tak aby w przypadku pozytywnego przypadku wirusa Ebola lekarze szpitalni informowali lokalny zespół ds. ochrony zdrowia, który następnie monitorował wszystkie kontakty.101 Działo się to jednak tylko na małą skalę. |
| 5.63. | Jeśli chodzi o możliwości przeprowadzania testów, prawdopodobny wpływ ograniczonej wydajności laboratoriów na diagnozę i dane podczas pandemii został uznany na posiedzeniu Naukowej Grupy ds. Modelowania Pandemii Grypy przy Departamencie Zdrowia (zwanej SPI-M) w styczniu 2017 r. Public Health England przyznało, że w przyszłości mogą wystąpić problemy z wydajnością laboratoriów, w zależności od charakteru epidemii. Stwierdziła również, że ma pewność, że zrobiono wszystko, co można było zrobić, aby złagodzić te problemy. Jest mało prawdopodobne, aby zwrócić się do sektora prywatnego w celu zwiększenia mocy produkcyjnych, ale nie wykluczono takiej opcji.102 |
| 5.64. | Duncan Selbie, dyrektor naczelny Public Health England od lipca 2012 r. do sierpnia 2020 r., powiedział w trakcie dochodzenia, że przed pandemią Covid-19 nie podjęto żadnych kroków w celu „zwiększenia” wydajności laboratoriów103. Hancock powiedział w dochodzeniu:
„Na testach, [Zdrowie Publiczne Anglia] odmówił zaangażowania sektora prywatnego w możliwości przeprowadzania testów, mimo że było oczywiste, że konieczna jest masowa rozbudowa testów, a istniejące możliwości nie były skalowalne.”104 |
| 5.65. | Według pana Selbiego obowiązkiem Public Health England było wiedzieć jedynie, co przechodzi przez systemy nadzoru, opracować niezbędny test (w razie potrzeby dostosowany), a następnie przesłać go do laboratoriów, głównie w ramach NHS. Powiedział, że w przypadku chorób zakaźnych o poważnych konsekwencjach liczby te sięgają kilkuset (co Public Health England określiło mianem „na dużą skalę”). Jednakże Public Health England nigdy nie planowało przeprowadzania masowych testów ani masowego śledzenia kontaktów kontaktowych. Rozumiał, że Public Health England nie będzie testować 50% populacji, ale jedynie do celów nadzoru i badań.105 |
| 5.66. | Podobnie przed pandemią w Szkocji, Walii i Irlandii Północnej nie istniał skalowalny system testów i śledzenia kontaktów.106 |
| 5.67. | Całość brytyjskiego systemu testów i ustalania kontaktów zakaźnych zaprojektowano zatem tak, aby obejmowała jedynie niewielką liczbę przypadków nowo pojawiających się chorób zakaźnych, w przeciwieństwie do masowych testów lub śledzenia kontaktów zakaźnych. Podczas pandemii Covid-19 trzeba było szybko i od podstaw zbudować zdolność do zwiększenia skali testów i śledzenia.107 |
| 5.68. | Rząd Wielkiej Brytanii i zdecentralizowane administracje mogły i powinny były zainwestować w tę infrastrukturę przed pandemią Covid-19, ale tego nie zrobiły.108 Chociaż decyzje polityczne dotyczące alokacji zasobów ostatecznie należą do wybieranych polityków, a taka inwestycja byłaby znacząca, w dochodzeniu uznano, że byłaby ona w oczywisty sposób opłacalna, biorąc pod uwagę zniszczenia spowodowane początkowym brakiem skutecznej kontroli infekcji i ogromne koszty do narodu budującego od podstaw systemy testowe i śledzenia. Należy utrzymać elementy składowe i zasadniczą strukturę systemów testowania i śledzenia ustanowionych przez rząd Wielkiej Brytanii i zdecentralizowane administracje podczas pandemii, aby można było szybko przywrócić te systemy i dostosować je do użytku w przypadku wybuchu epidemii w przyszłości. |
Izolacja
| 5.69. | Prace nad kwarantanną były omawiane na posiedzeniu Zarządu Wydziału Departamentu Zdrowia w dniu 29 września 2016 r. Podczas spotkania uznano, że „Gdyby konieczne stało się śledzenie lub poddanie kwarantannie tysięcy ludzi, pojawiłyby się poważne problemy”.109 Prace podjęte w celu zbadania metod kwarantanny w Azji Wschodniej zostały wstrzymane w ramach departamentalnego „ćwiczenie ustalania priorytetów obciążenia pracą” przez Ministerstwo Zdrowia.110 |
| 5.70. | Sir Christopher Wormald przyznał, że do 2020 r. nie toczyła się żadna debata na temat poddania kwarantannie lub izolacji znacznej liczby ludności w kontekście pandemii.111 Strumień pracy pozostał wstrzymany. Powiedział:
„Słusznie więc odbyło się wiele dyskusji na temat niektórych krajów, które wyjątkowo dobrze poradziły sobie z Covidem, takich jak Korea Południowa. W rzeczywistości dysponowali znacznie wyższym progiem powstrzymywania [choroba zakaźna o poważnych konsekwencjach] niż byliśmy w stanie zrobić i to była kluczowa różnica.”112 |
| 5.71. | Podobnie przed pandemią nie istniał system izolacji w Szkocji, Walii i Irlandii Północnej.113 |
| 5.72. | O ile brak myślenia o masowej kwarantannie można częściowo wytłumaczyć rozbieżnością pomiędzy planowaniem na wypadek pandemii grypy a epidemią lub wybuchem na skalę pandemiczną nowo powstającej choroby zakaźnej (w tym zakwalifikowanej jako choroba zakaźna o poważnych konsekwencjach), o której mowa w art. Rozdział 4: Skuteczna strategia, potrzeba wprowadzenia systemu masowej kwarantanny była także lekcją, którą uwypukliły epidemie MERS i Ebola oraz ćwiczenia, w związku z którymi nie podjęto żadnych działań. |
Kontrole graniczne
| 5.73. | Istnieje szeroki zakres środków bezpieczeństwa zdrowotnego, które można zastosować w celu zmniejszenia ryzyka importu infekcji z zagranicy podczas globalnej epidemii. Ich wykorzystanie jest rozważane w ramach innych modułów niniejszego Zapytania. Środki te obejmują:
|
| 5.74. | Kontrole portowe i graniczne zostały opisane przez profesor Dame Jenny Harries, dyrektor naczelną brytyjskiej Agencji Bezpieczeństwa Zdrowia od kwietnia 2021 r., jako należące do kategorii „niegodziwe kwestie”, którego Public Health England nie było w stanie rozwiązać samodzielnie. Zdrowie publiczne w Anglii podjęło „dość dużo pracy” w sprawie kontroli bezpieczeństwa w porcie wejścia, ale wiązało się to z konsekwencjami prawnymi i wymagało wsparcia ze strony „prawie wszyscy”w rządzie.114 |
| 5.75. | Postępowanie w przypadku epidemii wirusa Ebola w latach 2013–2016 było pouczające, jeśli chodzi o to, w jaki sposób ograniczenia graniczne mogą być skuteczne, jako część pakietu środków, w hamowaniu rozprzestrzeniania się choroby zakaźnej o poważnych konsekwencjach. Kontrole graniczne były również skutecznie stosowane przez Koreę Południową w ramach szeregu środków mających na celu ograniczenie przenoszenia wirusa na początku wybuchu epidemii MERS w 2015 r. (omówione powyżej). W ramach reakcji Wielkiej Brytanii na epidemię wirusa Zika w 2016 r. i incydent radiologiczny w Fukushimie w 2011 r. przeprowadzono badania przesiewowe w porcie wejścia.115 |
| 5.76. | Poseł Michael Gove (kanclerz księstwa Lancaster od lipca 2019 r. do września 2021 r. i minister gabinetu od lutego 2020 r. do września 2021 r.) powiedział w trakcie dochodzenia, że chociaż zamknięcie granic nieuchronnie pociąga za sobą koszty gospodarcze i społeczne, „mogą być bardzo potężnymi narzędziami zapobiegania lub spowalniania rozprzestrzeniania się choroby”.116 Profesor Dame Sally Davies, dyrektor medyczny Anglii od czerwca 2010 r. do października 2019 r., zgodziła się:
"[T]Są chwile, kiedy trzeba zrobić rzeczy, które mogą nie wydawać się opłacalne, ponieważ naród ich potrzebuje.”117 |
| 5.77. | W 2017 r. przedsiębiorstwo Public Health England przeprowadziło przegląd swoich usług zdrowia publicznego w portach, w którym wzięto pod uwagę potrzebę szybkiego reagowania na sytuacje nadzwyczajne dotyczące zdrowia publicznego o zasięgu międzynarodowym, w tym na przykład poprzez świadczenie usług kontroli bezpieczeństwa w porcie wejścia.118 W przeglądzie tym podkreślono, że chociaż obowiązki w zakresie zdrowia na granicach przypadły szeregowi różnych organizacji (na przykład Public Health England, Agencji Zdrowia Zwierząt i Roślin, Straży Granicznej, władzom lokalnym i NHS), nie istniał dokument opisujący, w jaki sposób te agencje powinny współpracować. Public Health England wraz z innymi podmiotami podjęło systematyczną pracę w celu opracowania opisu zakresu ról i obowiązków.119 Powinno to doprowadzić do porozumienia w sprawie bliższej współpracy, zwłaszcza w sytuacjach nadzwyczajnych. |
| 5.78. | W listopadzie 2019 r. Departament Zdrowia i Opieki Społecznej zgodził się na wspólny program prac zaproponowany przez Public Health England w celu poprawy podstawowych zdolności w zakresie zdrowia publicznego w portach. Program prac obejmował wprowadzenie planów awaryjnych we wszystkich znaczących portach, organizację ćwiczeń w celu przetestowania tych planów oraz udostępnienie w portach miejsc do kwarantanny. Do czasu wybuchu pandemii Covid-19 działania te nie zostały zakończone.120 |
| 5.79. | Pan Hancock powiedział w dochodzeniu, że:
"[T]nie było w ogóle przygotowania na fakt, że na granicy mogą być potrzebne środki zdrowotne w celu ochrony ludności.”121 Wyjaśnił dalej, że środki graniczne zostały podważone przez coś, co określił jako „błąd” w ustawie o zdrowiu publicznym (kontroli chorób) z 1984 r.122 Chociaż granica Wielkiej Brytanii wyraźnie leży w gestii rządu Wielkiej Brytanii, środki zdrowotne są zdecentralizowane, co powoduje zamieszanie i komplikacje. Jego zdaniem należy zmienić ustawodawstwo, aby w sposób jednoznaczny uczynić środki zdrowotne na granicy obowiązkiem rządu Wielkiej Brytanii.123 Dochodzenie nie otrzymało żadnych dowodów na to, że problem został rozwiązany. |
| 5.80. | W związku z tym w styczniu 2020 r. nie istniały kompleksowe ramy umożliwiające rządowi Wielkiej Brytanii lub zdecentralizowanym administracjom ocenę względnych kosztów i korzyści wielu różnych dostępnych dla nich interwencji na granicy. Chociaż w dochodzeniu rozumie się złożoność i trudności związane z wprowadzeniem takich ram, rząd brytyjski miał obowiązek przyjrzeć się tej kwestii. Nie udało się tego zrobić przed nadejściem pandemii. |
Zwiększenie potencjału opieki zdrowotnej i społecznej
| 5.81. | Na posiedzeniu zarządu Departamentu Zdrowia w dniu 29 września 2016 r., o którym mowa powyżej, wyrażono obawy co do odporności rozdrobnionego systemu opieki zdrowotnej i społecznej, zwłaszcza w świetle historycznych lub potencjalnych przyszłych cięć w finansowaniu.124 |
| 5.82. | Profesor Davies powiedział śledczym: „[T]Od ponad dziesięciu lat NHS jest znana z tego, że każdej zimy „pracuje na pełnych obrotach”, czyli pracuje na pełnych obrotach.”125 W dochodzeniu wykazano również, że występowały poważne niedobory personelu i że znaczna część infrastruktury szpitalnej w Anglii nie była dostosowana do potrzeb.126 Sektor opieki społecznej w Anglii borykał się z podobnymi problemami.127 Ta kombinacja czynników miała bezpośrednio negatywny wpływ na środki kontroli infekcji oraz na zdolność NHS i sektora opieki do „zwiększenia” wydajności podczas pandemii.128 |
| 5.83. | Służba zdrowia i opieka społeczna w Walii i Szkocji stanęła przed podobnymi wyzwaniami jak Anglia.129 W Irlandii Północnej system opieki zdrowotnej i społecznej ucierpiał w szczególności z powodu braku dyrektora w latach 2017–2020. Profesor Sir Michael McBride, dyrektor ds. medycznych w Irlandii Północnej od września 2006 r., powiedział w dochodzeniu, że służba zdrowia w 2020 r. nie był nawet tak odporny jak w 2009 r.130 |
| 5.84. | Kwestie finansowania to decyzje polityczne, które właściwie należą do wybieranych polityków.131 Nie zmienia to jednak faktu, że rosnąca zdolność systemów zdrowia publicznego i opieki zdrowotnej czterech krajów do reagowania na pandemię była ograniczona przez ich finansowanie. Wydajność i odporność systemów opieki zdrowotnej i społecznej zostaną rozważone w ramach dochodzenia w kolejnych modułach. |
Sprzęt ochrony osobistej
| 5.85. | Znaczenie środków ochrony indywidualnej było kwestią, która pojawiała się wielokrotnie podczas ćwiczeń, w tym ćwiczeń Silver Swan w 2016 r. (pandemia grypy w Szkocji) i Iris (epidemia MERS-CoV w Szkocji), a także w okresie poprzedzającym Cygnus.132 |
| 5.86. | Było jasne, że środki ochrony indywidualnej należy zgromadzić przed pandemią w wystarczających ilościach, przetestować pod kątem dopasowania i podłączyć do skutecznej sieci dystrybucji. Sir Christopher Wormald powiedział w dochodzeniu, że „[w]W całym kraju nigdy nie zabrakło środków ochrony osobistej", ale to "w poszczególnych miejscach brakowało środków ochrony osobistej i ludzie musieli używać niewłaściwych środków ochrony indywidualnej”.133 Hancock powiedział, że wystąpiły trudności logistyczne w szybkim uzyskaniu dostępu do zapasów.134 Dochodzenie będzie dokładniej badać tę kwestię oraz ŚOI w kolejnych modułach. |
Ochrona osób bezbronnych
| 5.87. | Obszarem, który nie został dostatecznie uwzględniony w ćwiczeniach i dlatego nie podjęto w nim działań, był najlepszy sposób ochrony osób bezbronnych. Wystąpiła awaria (jak omówiono powyżej i w Załącznik 2: Ćwiczenia):
|
| 5.88. | Te niepowodzenia naraziły najbardziej bezbronne osoby w społeczeństwie na skutki pandemii. Aby zapobiec takim sytuacjom w przyszłości, należy za pomocą ćwiczeń zbadać skutki ogólnosystemowego stanu nadzwyczajnego dla osób bezbronnych, a kroki mające na celu złagodzenie tego zjawiska powinny zostać poddane większej kontroli publicznej poprzez uwzględnienie ich w opublikowanym raporcie, Jak opisano poniżej. |
Wartość ćwiczeń pandemicznych
| 5.89. | Lekcje te podkreślają wyraźną wartość regularnych, odpowiednio skonstruowanych i dokładnych ćwiczeń, nawet jeśli mają one swoje ograniczenia. W dochodzeniu uznano, że zaprojektowanie i przeprowadzenie ćwiczeń jest trudne i kosztowne, a także nieuchronnie wiąże się z wyborem do symulacji pewnych rodzajów ryzyka zamiast innych, co może nie odzwierciedlać dokładnych okoliczności, które mają miejsce. Grozi to także odwróceniem uwagi ministrów i urzędników od pilniejszych spraw bieżących. Jednak potencjalne zalety prowadzenia dużych ćwiczeń okresowych przeważają nad wadami. |
| 5.90. | W dochodzeniu zaleca się organizowanie regularnych ćwiczeń na wypadek pandemii, w tym co trzy lata ogólnokrajowych ćwiczeń na wypadek pandemii, przeprowadzanych w atmosferze ciekawości i otwartości i mających na celu sprawdzenie reakcji na pandemię na wszystkich etapach – od początkowej epidemii po długi okres -reakcja terminowa, z wieloma falami na przestrzeni wielu lat. Zapewni to również odpowiednie uwzględnienie potencjalnych skutków reakcji na każdym etapie. W ćwiczeniach powinni brać udział ministrowie i wyżsi urzędnicy ze zdecentralizowanych administracji, a także liderzy NHS, opieki społecznej i zdrowia publicznego, przedstawiciele lokalnych forów na rzecz odporności, wolontariuszy, przedsiębiorstw społecznych i społecznych oraz dyrektorzy ds. zdrowia publicznego. |
| 5.91. | Planowanie ćwiczeń powinno być przedmiotem kontroli zewnętrznego „czerwonego zespołu” złożonego z pozarządowych ekspertów posiadających doświadczenie w różnych odpowiednich dziedzinach, w tym w dyscyplinach naukowych, gospodarczych i społecznych. Zachęcałoby to do rozważenia praktycznych konsekwencji w świecie rzeczywistym oraz do zadawania pytań i odpowiadania na pytania „co by było, gdyby”. Użycie czerwonych drużyn zostało omówione w dalszej części Rozdział 6: Nowe podejście. |
| 5.92. | Powinien być większy nadzór ministerialny. Ministrowie w departamentach rządowych są niezwykle zajęci. Nie zawsze można je dostrzec w wynikach każdego raportu. Jednakże ministrowie ponoszą ostateczną odpowiedzialność za dopilnowanie, aby ich departamenty wdrożyły wnioski wyciągnięte ze sprawozdań w celu poprawy gotowości. Biorąc pod uwagę znaczenie ćwiczeń dla identyfikacji znaczących luk w planowaniu oraz praktyczną zdolność reagowania w sytuacjach awaryjnych w terenie, ministerstwo powinno było w większym stopniu zaangażować się w ćwiczenia i nadzorować je. Ministrowie i ich wyżsi urzędnicy muszą zatem w przyszłości przyjąć bardziej aktywne podejście, aby dopilnować, aby wnioski nie zostały po prostu powtórzone i rozważone ponownie podczas następnego ćwiczenia. |
| 5.93. | Gdyby system ten obowiązywał w 2019 r. oraz gdyby działania, zalecenia i wnioski wyciągnięte z poprzednich działań zostały właściwie wdrożone, Wielka Brytania byłaby znacznie lepiej przygotowana na pandemię Covid-19, która po niej nastąpiła. |
Zalecenie 6: Regularne ćwiczenia w zakresie reagowania na pandemię w całej Wielkiej Brytanii
Rząd Wielkiej Brytanii i zdecentralizowane administracje powinny wspólnie przeprowadzać ogólnokrajowe ćwiczenia w zakresie reagowania na pandemię co najmniej co trzy lata.
Ćwiczenie powinno:
- przetestować ogólnokrajową, międzyrządową, krajową i lokalną reakcję na pandemię na wszystkich etapach, od początkowej epidemii po liczne fale na przestrzeni kilku lat;
- obejmować szeroki zakres osób zaangażowanych w przygotowanie i reagowanie na pandemię; I
- rozważyć, w jaki sposób w przypadku pandemii zostanie udzielona pomoc szerokiemu gronu bezbronnych osób.
Brak działania
| 5.94. | Wszystkie cztery narody z opóźnieniem wdrażały ważne i niezbędne przygotowania na pandemię. |
| 5.95. | W ramach dochodzenia wskazano powyżej szereg obszarów, w których nie wdrożono lub nie wypełniono zaleceń wynikających z ćwiczeń symulacyjnych. Niestety, różne rady i grupy utworzone w celu nadzorowania tych prac okazały się w dużej mierze nieskuteczne. |
| 5.96. | W Anglii do stycznia 2020 r. (trzy lata po ćwiczeniach Cygnus):
|
| 5.97. | Wszystkie kraje zdecentralizowane były zaangażowane w programy pracy wynikające z ćwiczeń Cygnus. |
| 5.98. | W 2018 r. profesor McBride powołał Grupę Nadzoru nad Pandemią Grypy w Irlandii Północnej.136 W 2019 r. w Departamencie Zdrowia (Irlandia Północna) utworzono także „grupę zadaniową i zakończeniową”, której zadania obejmowały przegląd i aktualizację wytycznych dotyczących wzrostu pandemii grypy w opiece zdrowotnej i społecznej.137 Prace te zostały wstrzymane w celu przekierowania do operacji Yellowhammer na cały 2019 r. Nie zostały wznowione przed pojawieniem się Covid-19 w styczniu 2020 r.138 Niedostateczne zasoby Wydziału ds. Polityki Zagrożeń Cywilnych Biura Wykonawczego Irlandii Północnej były problemem od dawna. W listopadzie 2019 r. w wewnętrznym e-mailu napisano:
„Ogólna sytuacja jest fatalna. Doszło do systemowych niepowodzeń w zakresie inwestowania środków i zasobów [Wydział Polityki ds. nieprzewidzianych wypadków cywilnych] przez wiele lat, a obecna sytuacja jest taka, że w momencie, w którym się skupiamy, brak inwestycji, z przykrością muszę Państwu powiedzieć, sprawił, że nie nadawał się on do zamierzonego celu.”139 Dlatego w Irlandii Północnej nie ukończono kluczowych prac niezbędnych do przygotowania sektora opieki zdrowotnej i społecznej na pandemię. |
| 5.99. | Podobnie Walia Rada ds. gotowości na pandemię grypy nie zakończyła swoich prac. Wydaje się, że przyjęto pogląd, że nie należy nic robić, dopóki brytyjska Rada ds. Gotowości na Pandemię Grypy po raz pierwszy nie zaktualizuje strategii z 2011 roku.140 Doktor Andrew Goodall, stały sekretarz rządu walijskiego od września 2021 r., powiedział w trakcie dochodzenia, że być może najbardziej znaczącym obszarem obaw jest zdolność sektora opieki nad osobami dorosłymi do sprostania wymaganiom pandemii. Stało się tak, ponieważ dotyczył bezpośrednio spraw życia i śmierci w sektorze domów opieki. Dla władz lokalnych stanowiło to poważny problem w wykonywaniu swoich obowiązków.141 |
| 5.100. | Szkocka Rada ds. Gotowości na Pandemię Grypy została powołana w 2017 r. i spotykała się co dwa miesiące do listopada 2018 r. W okresie od listopada 2018 r. do czerwca 2019 r. nie zebrała się ona w ogóle – jej posiedzenia zostały odwołane lub przełożone ze względu na niedostępność urzędników lub sprzeczne priorytety Operacja Yellowhammer (lub obie).142 Gillian Russell, dyrektor ds. bezpieczniejszych społeczności w rządzie Szkocji od czerwca 2015 r. do marca 2020 r., wyjaśniła, że chociaż niektóre prace zostały ukończone (np. dotyczące nadmiernej liczby zgonów), inne prace zostały wstrzymane, ponieważ „priorytet postawiono na inne rzeczy”.143 Do czasu wybuchu pandemii Covid-19 8 z 22 zaleceń wynikających z ćwiczeń Cygnus było w Szkocji niekompletnych. Obejmowały one odświeżenie strategii na rok 2011, sprawdzenie dopasowania ŚOI, zwiększenie potencjału opieki społecznej i aktualizację wytycznych dotyczących pandemii.144 |
| 5.101. | System nastawiony na działanie w oparciu o ustalenia badaczy mógłby coś z tym zrobić. Rządy Wielkiej Brytanii, Szkocji, Walii i Irlandii Północnej nie podjęły jednak wystarczająco pilnych działań lub w ogóle nie podjęły takich działań.145 Jak podkreśla konkretny przykład ćwiczenia Cygnus, nie wyciągnięto wniosków, których można było i należało się nauczyć. Pozostało je odkryć na nowo w następnym ćwiczeniu lub, jak się okazało, gdy wybuchła pandemia Covid-19. |
Przyczyny bierności
Zasoby i priorytetyzacja
| 5.102. | Niektórzy świadkowie dochodzenia opisali ustalanie priorytetów i zmianę priorytetów ograniczonych zasobów jako przyczynę bezczynności. Był to temat często powracający w materiałach dowodowych. |
| 5.103. | Nie zostało to lepiej podkreślone niż sytuacja, gdy kilku świadków z brytyjskiego rządu i zdecentralizowanych administracji powiedziało dochodzeniu, że szereg prac związanych z przygotowaniem na wypadek pandemii zostało wstrzymanych ze względu na realokację zasobów na rzecz operacji Yellowhammer.146 |
| 5.104. | Na posiedzeniu Rady ds. gotowości na pandemię grypy w listopadzie 2018 r. pani Hammond powiedziała radzie, że planowanie awaryjne na wypadek wyjścia z Unii Europejskiej bez porozumienia znacznie wzrosło w ciągu ostatnich kilku miesięcy i oczekuje się, że będzie kontynuowane. Przewodniczący przypomniał radzie, że nadanie priorytetów nie powinno oznaczać pozbawienia priorytetów innych obszarów.147 Tabela przedstawiająca postęp we wdrażaniu zaleceń wynikających z ćwiczenia Cygnus wykazała, że według stanu na czerwiec 2020 r. 14 z 22 lekcji zidentyfikowanych przez Cygnusa w Wielkiej Brytanii pozostało niekompletnych.148 W szczególności opieka społeczna była konsekwentnie sygnalizowana jako problem, lecz nie została poruszona. Zatem rzeczywistość była taka, że prace Rady ds. gotowości na pandemię grypy, polegające na wdrażaniu zaleceń ćwiczeń Cygnus – które powtarzały wiele z tych samych lekcji z poprzedniej dekady ćwiczeń – nie przebiegały daleko od zakończenia w terminie wyznaczonym na 2018 r. zostać ukończone na czas, niezależnie od interwencji Operacji Yellowhammer, czy nie. |
| 5.105. | Szereg spotkań informacyjnych prowadzonych w 2019 r. z posłem Oliverem Dowdenem (sekretarzem parlamentarnym w Kancelarii Rady Ministrów od stycznia 2018 r. do lipca 2019 r. i ministrem ds. Gabinetu od lipca 2019 r. do lutego 2020 r.) odnosił się do tzw.ponowne ustalenie priorytetów”.149 W styczniu 2019 r. Sekretariat ds. Zagrożeń Cywilnych został „od tej chwili priorytetem będzie brak przygotowań do zawarcia umowy” i kontynuował:
„niewielką liczbę niezbędnych działań obok przygotowań do braku porozumienia, ale wstrzymano wszystkie inne działania, aby umożliwić wystarczające skupienie się na przygotowaniach do opuszczenia UE bez porozumienia”.150 |
| 5.106. | Roger Hargreaves, dyrektor jednostki COBR od lipca 2022 r., opisał obciążenie zasobów kadrowych spowodowane przygotowaniem się na kryzysy, reagowaniem na nie i wychodzeniem z kryzysu. Oczywistą konsekwencją było podjęcie decyzji o priorytetowym traktowaniu zasobów przeznaczonych do reagowania na bezpośrednie, nadchodzące lub pojawiające się zagrożenia w stosunku do pracy nad mniej bezpośrednimi problemami.151 Podobnie pan Dowden odniósł się do normalnej sytuacji zmiany priorytetów, która ma miejsce w rządzie.152 Twierdził, że istnieje „zawsze flex” w zasobach potrzebnych do reagowania na pojawiające się wyzwania.153 Jednak nawet on zdawał sobie sprawę, że operacja Yellowhammer była, jak to ujął, „na samym końcu wykorzystania tych zasobów” i na „skrajny koniec zmiany priorytetów”.154 |
| 5.107. | W rzeczywistości materiał dowodowy zgromadzony przed dochodzeniem pokazuje, że zmiana priorytetów konkurencyjnych żądań nie była rzadkością. Hargreaves zauważył, że od 2009 r. co najmniej 32 zdarzenia nadzwyczajne o charakterze cywilnym, w które Gabinet Rady Ministrów był bezpośrednio zaangażowany, zmieniły priorytety wobec sprzecznych żądań.155 Pani Hammond zauważyła, że seria sytuacji nadzwyczajnych, które miały miejsce od 2016 r., ich liczba i utrzymujący się charakter nadwyrężyły dość niewielki stały zespół reagowania w Sekretariacie ds. Zagrożeń Cywilnych. Jak to ujęła, w przypadku dużej liczby sytuacji kryzysowych „z konieczności część pracy zostaje odłożona na bokw innych, mniej pilnych sprawach.156 Pani Hammond opisała operację Yellowhammer jako „naprawdę głównym konsumentem zasobów”.157 Sekretariat ds. Zagrożeń Cywilnych i Biuro Rady Ministrów musiały – używając ponownie tego wyrażenia – „odłożyć na bok„pewne strumienie pracy, o których wiedzieli, że powinni wykonywać.158 |
| 5.108. | Pozytywną stroną jest to, że pomimo ogólnego obciążenia w zakresie zasobów Dowden powiedział w dochodzeniu, że w rzeczywistości operacja Yellowhammer sprawiła, że Wielka Brytania „Pasuje do siebie„, aby uporać się z pandemią Covid-19.159 Powiedział, że stało się tak dlatego, że rząd Wielkiej Brytanii zatrudnił około 15 000 dodatkowych pracowników, których można następnie przesunąć w celu zwiększenia gotowości lub wniesienia wkładu w działania związane z reagowaniem na pandemię.160 Pan Gove zgodził się.161 W dochodzeniu zebrano dowody na to, że w wyniku operacji Yellowhammer rząd Wielkiej Brytanii poprawił swoją wiedzę na temat podstawowych łańcuchów dostaw i znaczenia silniejszych relacji z przemysłem, zwiększył zapasy kluczowych leków i dostęp do produktów medycznych.162 |
| 5.109. | Faktem pozostaje jednak, że system gotowości i odporności rządu brytyjskiego znajdował się, co całkiem oczywiste, pod ciągłym obciążeniem. Polegało to na przerwaniu prac nad przygotowaniem się na jedną potencjalną sytuację kryzysową, aby skoncentrować się na innej. Tendencja jest taka, że ryzyko jest bardziej złożone i współbieżne. Powyższe dowody sugerują, że istniały i nadal istnieją rzeczywiste ograniczenia zdolności państwa do radzenia sobie z rosnącą tendencją do występowania wielu złożonych sytuacji kryzysowych w tym samym czasie. |
Biurokracja
| 5.110. | Drugą przyczyną bierności był wzrost biurokracji. |
| 5.111. | Podczas ćwiczeń symulacyjnych, które odbyły się w latach 2003–2016, wielokrotnie pojawiały się te same krytyczne kwestie dotyczące ogólnej nieadekwatności rządu Wielkiej Brytanii i stanu gotowości zdecentralizowanych administracji. Często zwiększano liczbę testów, śledzenie, izolację, wzrost wydajności opieki zdrowotnej i społecznej oraz kontrole graniczne. To mogło i powinno posłużyć jako ostrzeżenie o tym, co należy zrobić. To nie mialo miejsca. |
| 5.112. | Instytucjom nie udało się zidentyfikować i dokładnie opisać podstawowych problemów, co spotęgowało użycie żargonu i eufemizmów w celu ukrycia na przykład niezakończonych zadań. Sytuację spotęgował niepowodzenie we wdrażaniu rozwiązań przez kierownictwo, czego dowodem było mnożenie się długich dokumentów, planów i wytycznych (które w każdym razie często nie były aktualizowane), a nie infrastruktury umożliwiającej radzenie sobie z epidemią patogenów. W Dochodzeniu zaczęto tworzyć procesy rozwiązywania problemów, a nie samo rozwiązywanie problemów (patrz Rozdział 6: Nowe podejście). |
| 5.113. | Ponadto ogólna złożoność systemu gotowości i odporności (zob Rozdział 2: System – instytucje, struktury i przywództwo) doprowadziło do braku wyraźnych granic odpowiedzialności, rozmycia odpowiedzialności, powielania wysiłków i, w ostatecznym rozrachunku, nieefektywności. |
Pamięć instytucjonalna
| 5.114. | Trzecią przyczyną bierności był brak pamięci instytucjonalnej. Często jest to spowodowane częstymi i szybkimi zmianami kadrowymi, a w konsekwencji utratą doświadczenia i wiedzy. Nie jest to problem wyłącznie rządu – jest to problem, przed którym stoją wszystkie najważniejsze instytucje. |
| 5.115. | Pamięć instytucjonalna obejmuje wiedzę wewnętrzną, wyciągnięte wnioski, udane strategie i błędy z przeszłości oraz umożliwia skuteczną kontynuację działalności rządu lub innej organizacji przez kolejne administracje. Istotne jest, aby istniał prosty i dostępny system gromadzenia i udostępniania wiedzy.163 Jest to szczególnie ważne w sytuacji dużej rotacji urzędników i ministrów – „poruszyć się w systemie” lub „drzwi obrotowe”ministrów.164 Skuteczny system pamięci instytucjonalnej wymaga środków przechowywania i dostępu do raportów z ćwiczeń, planów działania, planowania kryzysowego i wytycznych. Umożliwia to pełną i otwartą dyskusję na temat tego, co się sprawdziło, a co nie, a także zachęca do kultury debaty i wyzwań. |
| 5.116. | Zrozumienie lekcji z przeszłości i zachowanie wiedzy o przeszłych niepowodzeniach przyczynia się do skuteczniejszego podejmowania decyzji w przyszłości i pomaga zapobiegać powtarzaniu się podobnych błędów. Sprzyja także innowacjom i ma kluczowe znaczenie dla ciągłego doskonalenia i budowania odporności. Ma to na celu poprawę gotowości, nawet jeśli stopniowo, z biegiem czasu. |
| 5.117. | Wszystkim osobom zaangażowanym w przygotowanie i reagowanie na pandemię w Wielkiej Brytanii powinien zapewnić otwarty dostęp do zachowanych informacji instytucjonalnych. Szybki dostęp do wcześniejszych rozwiązań i najlepszych praktyk również zwiększa wydajność. Zapobiega to konieczności „wynajdywania koła na nowo” i marnotrawstwu procesów równoległych. W dochodzeniu zaleca się zatem utworzenie centralnego, obejmującego całą Wielką Brytanię, internetowego repozytorium informacji odnoszących się do ćwiczeń w sytuacjach nadzwyczajnych, które powinno zawierać wszystkie sprawozdania z ćwiczeń i wytyczne dotyczące sytuacji awaryjnych. Repozytorium to powinno być dostępne między innymi dla zdecentralizowanych organów administracji, władz lokalnych i regionalnych oraz osób z sektora wolontariatu i społeczności. |
Zalecenie 7: Publikacja wniosków i wniosków z ćwiczeń w sytuacjach zagrożenia cywilnego
W przypadku wszystkich ćwiczeń cywilnych w sytuacjach nadzwyczajnych rządy Wielkiej Brytanii, Szkocji, Walii i Irlandii Północnej powinny (chyba że względy bezpieczeństwa narodowego tego nie robią):
- publikuje sprawozdanie z ćwiczenia podsumowujące ustalenia, wnioski i zalecenia w ciągu trzech miesięcy od zakończenia ćwiczenia;
- publikuje plan działania określający konkretne kroki, które zostaną podjęte w odpowiedzi na ustalenia zawarte w raporcie oraz określający podmiot, w terminie sześciu miesięcy od zakończenia działania; I
- przechowuj raporty z ćwiczeń, plany działania oraz plany i wytyczne na wypadek sytuacji nadzwyczajnej z całej Wielkiej Brytanii w jednym, ogólnokrajowym archiwum internetowym, dostępnym dla wszystkich zaangażowanych w gotowość, odporność i reagowanie na sytuacje kryzysowe.
Kontrola parlamentarna
| 5.118. | Wreszcie możliwą przyczyną bierności był brak otwartości. Ćwiczenia nie były prowadzone w sposób wystarczająco otwarty i dlatego nie podlegały wymaganemu poziomowi niezależnej kontroli. Gdyby wyniki ćwiczeń opublikowano szerzej, mogłoby to wywołać komentarze i reakcje innych osób. W dochodzeniu zalecono powyżej sposoby udostępniania wyników ćwiczeń symulacyjnych i udostępniania ich do publicznej kontroli. |
| 5.119. | Jednakże jedną z najskuteczniejszych form kontroli publicznej jest kontrola parlamentarna. W dochodzeniu uznano, że większy nadzór nad ministrami, instytucjami i urzędnikami odpowiedzialnymi za gotowość i odporność cywilną całego systemu przez Parlament i zdecentralizowane ciała ustawodawcze pomoże rozwiązać problemy związane z nieodpowiednimi działaniami zidentyfikowane w niniejszym Raporcie. |
| 5.120. | W swoich ramach odporności na 2022 r. rząd Wielkiej Brytanii zobowiązał się do przedstawiania parlamentowi corocznego oświadczenia na temat swojej wiedzy na temat obecnego obrazu ryzyka, wyników w zakresie odporności oraz obecnego stanu gotowości na wypadek zagrożeń cywilnych.165 Miało to na celu zwiększenie odpowiedzialności publicznej. W grudniu 2023 r. Dowden przedstawił parlamentowi i Gabinetowi pierwsze roczne oświadczenie w sprawie odporności opublikowane Ramy dotyczące odporności rządu Wielkiej Brytanii: aktualizacja wdrożenia z 2023 r.166 Jak dotąd nie podjęto jednak zobowiązania dotyczącego pełnej, opublikowanej analizy zawierającej zalecenia mające na celu poprawę gotowości i odporności; brak analizy kosztów przejęcia ryzyka w porównaniu z korzyściami wynikającymi z podjęcia działań ograniczających ryzyko; i nie ma szczególnego znaczenia, w jaki sposób osoby bezbronne będą chronione. Nie ma planu wdrożenia ani terminów, według których można obiektywnie ocenić wyniki. |
| 5.121. | W celu poprawy dalszej kontroli i odpowiedzialności publicznej, dochodzenie zaleca, aby rząd Wielkiej Brytanii, rząd Szkocji, rząd walijski i Biuro Wykonawcze Irlandii Północnej co najmniej co trzy lata sporządzały i publikowały dla swoich odpowiednich organów ustawodawczych sprawozdania na temat swojego podejścia do całościowych gotowość i odporność systemu na sytuacje kryzysowe. Każdy rząd powinien:
W ten sposób rządy i ich przywódcy polityczni będą mogli być regularnie pociągani do odpowiedzialności za stan systemów gotowości i odporności. |
Zalecenie 8: Opublikowane raporty na temat gotowości i odporności cywilnej całego systemu na sytuacje kryzysowe
Rządy Wielkiej Brytanii, Szkocji, Walii i Irlandii Północnej powinny co najmniej co trzy lata sporządzać i publikować dla swoich odpowiednich organów ustawodawczych sprawozdania na temat gotowości i odporności cywilnej całego systemu na sytuacje kryzysowe.
Raporty powinny zawierać co najmniej:
- ryzyko zidentyfikowane przez każdy rząd prawdopodobnie doprowadzi do katastrof cywilnych w całym systemie;
- zalecenia wydane każdemu rządowi w celu ograniczenia tego ryzyka oraz informację, czy zalecenia te zostały przyjęte, czy odrzucone;
- analizę kosztów i korzyści określającą koszty gospodarcze i społeczne akceptacji ryzyka w porównaniu z podjęciem działań mających na celu jego złagodzenie;
- kto może być narażony na ryzyko i jakie kroki podejmuje się w celu ograniczenia tego ryzyka;
- plan określający harmonogram wdrożenia przyjętych zaleceń; I
- aktualizację dotyczącą postępów we wdrażaniu wcześniej przyjętych zaleceń.
- Richard Horton 13 lipca 2023 71.14-20
- INQ000149108_0013
- Mark Woolhouse 5 lipca 2023 r. 121/2-122/12; „The WHO R&D Blueprint: przegląd pojawiających się chorób zakaźnych z 2018 r. wymagających pilnych wysiłków badawczo-rozwojowych”, M. Si Mehand, F. Al-Shorbaji, P. Millett i B. Murgue, Antiviral Research (2018), 159, 63-67 , s. 66 (https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7113760/pdf/main.pdf; INQ000149109)
- „Wnioski wyciągnięte z SARS: doświadczenie Agencji Ochrony Zdrowia, Anglia”, NL Goddard, VC Delpech, JM Watson, M. Regan i A. Nicoll, Public Health (2006) 120, 27-32, s. 27 (https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7118739/pdf/main.pdf; INQ000187893)
- Richard Horton 13 lipca 2023 68/7-13
- INQ000194054_0049 ust. 198; INQ000205178_0057 ust. 81; patrz także Tabela 1: Podsumowanie głównych epidemii i pandemii w przeszłości w Rozdziale 1: Krótka historia epidemii i pandemii
- INQ000205178_0058-0059 paragraf 83
- „Giants on Clay Feet: COVID-19, kontrola infekcji i sieci laboratoriów zdrowia publicznego w Anglii, USA i (zachodnich) Niemczech (1945–2020)”, C. Kirchhelle, Social History of Medicine (2022), 35(3) ), 703-748, s.736 (https://www.ncbi.nlm.nih.gov/pmc/articles/PMC9384317/pdf/hkac019.pdf; INQ000207449)
- INQ000235216_0001, 0009
- INQ000235217_0005-0011
- INQ000187903_0001-0002
- INQ000206664_0013
- „Wnioski wyciągnięte z SARS: doświadczenie Agencji Ochrony Zdrowia, Anglia”, NL Goddard, VC Delpech, JM Watson, M. Regan i A. Nicoll, Public Health (2006) 120, 27-32, s. 30 (https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7118739/pdf/main.pdf; INQ000187893)
- „Wnioski wyciągnięte z SARS: doświadczenie Agencji Ochrony Zdrowia, Anglia”, NL Goddard, VC Delpech, JM Watson, M. Regan i A. Nicoll, Public Health (2006) 120, 27-32, s. 31 (https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7118739/pdf/main.pdf; INQ000187893)
- „Wnioski wyciągnięte z SARS: doświadczenie Agencji Ochrony Zdrowia, Anglia”, NL Goddard, VC Delpech, JM Watson, M. Regan i A. Nicoll, Public Health (2006) 120, 27-32, s. 32 (https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7118739/pdf/main.pdf; INQ000187893)
- Pandemia grypy 2009: Niezależny przegląd reakcji Wielkiej Brytanii na pandemię grypy w 2009 r., Dame Deirdre Hine, lipiec 2010 r., pkt 1–2 (https://assets.publishing.service.gov.uk/media/5a7975f1ed915d0422068a10/the2009influenzapandemic-review. pdf; INQ000022705)
- Pandemia grypy 2009: Niezależny przegląd reakcji Wielkiej Brytanii na pandemię grypy w 2009 r., Dame Deirdre Hine, lipiec 2010 r., pkt 5 (https://assets.publishing.service.gov.uk/media/5a7975f1ed915d0422068a10/the2009influenzapandemic-review.pdf; INQ000022705)
- Pandemia grypy 2009: Niezależny przegląd reakcji Wielkiej Brytanii na pandemię grypy w 2009 r., Dame Deirdre Hine, lipiec 2010 r., pkt 5.41 (https://assets.publishing.service.gov.uk/media/5a7975f1ed915d0422068a10/the2009influenzapandemic-review.pdf; INQ000022705)
- INQ000102936_0002 ust. 5
- INQ000102936_0002 ust. 6
- INQ000128976_0013 ust. 1-2
- INQ000182610_0015 ust. 1b
- INQ000184643_0069 pkt 362–363
- INQ000184643_0070-0071 pkt 369–373
- INQ000177796_0004 ust. 15
- INQ000022723_0001 ust. 8
- INQ000184643_0069 paragraf 363
- INQ000022723_0014
- INQ000022723_0014 wpisy 16-17
- INQ000177808_0010-0011 ust. 44
- INQ000184643_0067 paragraf 354c
- INQ000090428_0014-0016
- INQ000184893_0009 ust. 36; patrz także INQ000148417_0009 pkt 3.10
- INQ000184893_0010 ust. 37
- INQ000184893_0017 paragraf 61
- INQ000184893_0019–0020 pkt 70, 74
- INQ000184893_0017 paragraf 61
- INQ000185135_0002; INQ000195846_0008 ust. 25; INQ000148429_0059 paragraf 235
- INQ000090431
- INQ000184643_0066 pkt 351–352; Christopher Wormald 19 czerwca 2023 137/10-12
- INQ000090431_0005-0006
- INQ000090431_0009
- INQ000090431_0009
- INQ000090431_0004, 0011
- INQ000090431_0011
- INQ000090431_0012
- INQ000090431_0010
- INQ000090431_0011
- INQ000090431_0013
- INQ000148429_0097 paragraf 380
- Widzieć INQ000090431_0016
- Christopher Wormald 19 czerwca 2023 137/5-12
- INQ000212312_0025 paragraf 100
- INQ000087227_0008 ust. 6.6
- Zob. na przykład poseł Jeremy Hunt, sekretarz stanu ds. zdrowia i opieki społecznej od września 2012 r. do lipca 2018 r. (INQ000177796_0010-0011 pkt 39–45); David Heymann 15 czerwca 2023 54.3-60.25, 61/17-25; Richard Horton 13 lipca 2023 90/5-92/4; Profesor Dame Sally Davies, dyrektor medyczny Anglii od czerwca 2010 r. do października 2019 r. (INQ000184637_0008 paragrafy 6.1-6.3)
- INQ000177796_0010 paragraf 40
- INQ000177796_0010 paragraf 41
- David Heymann 15 czerwca 2023 55/8-9
- INQ000177796_0010-0011 pkt 40–47
- Widzieć Załącznik 2: Ćwiczenia zawierające więcej szczegółów na temat kluczowych ćwiczeń przeprowadzonych w Wielkiej Brytanii i krajach zdecentralizowanych w latach 2002–2008
- Raport Cygnusa z ćwiczeń: Dowództwo pierwszego stopnia po ćwiczeniach Pandemic Influenza – 18–21 października 2016 r., Public Health England, 2017, s. 5–6 (https://www.gov.uk/government/publications/uk-pandemic-preparedness/exercise-cygnus-report-accessible-report; INQ000022792)
- Raport Cygnusa z ćwiczeń: Dowództwo pierwszego stopnia po ćwiczeniach Pandemic Influenza – 18–21 października 2016 r., Public Health England, 2017, s. 8–9 (https://www.gov.uk/government/publications/uk-pandemic-preparedness/exercise-cygnus-report-accessible-report; INQ000022792)
- Raport Cygnusa z ćwiczeń: Dowództwo pierwszego poziomu po ćwiczeniach Pandemic Influenza – 18–21 października 2016 r., Public Health England, 2017, s. 6 (https://www.gov.uk/government/publications/uk-pandemic-preparedness/exercise-cygnus-report-accessible-report; INQ000022792)
- Raport Cygnusa z ćwiczeń: Dowództwo pierwszego poziomu po ćwiczeniach Pandemic Influenza – 18–21 października 2016 r., Public Health England, 2017, s. 6 (https://www.gov.uk/government/publications/uk-pandemic-preparedness/exercise-cygnus-report-accessible-report; INQ000022792)
- Raport Cygnusa z ćwiczeń: Dowództwo pierwszego poziomu po ćwiczeniach Pandemic Influenza – 18–21 października 2016 r., Public Health England, 2017, s. 7 (https://www.gov.uk/government/publications/uk-pandemic-preparedness/exercise-cygnus-report-accessible-report; INQ000022792)
- Raport Cygnusa z ćwiczeń: Dowództwo pierwszego poziomu po ćwiczeniach Pandemic Influenza – 18–21 października 2016 r., Public Health England, 2017, s. 6 (https://www.gov.uk/government/publications/uk-pandemic-preparedness/exercise-cygnus-report-accessible-report; INQ000022792)
- Raport Cygnusa z ćwiczeń: Dowództwo pierwszego stopnia po ćwiczeniach Pandemic Influenza – 18–21 października 2016 r., Public Health England, 2017, s. 9 (https://www.gov.uk/government/publications/uk-pandemic-preparedness/exercise-cygnus-report-accessible-report; INQ000022792). Podobne kwestie zostały poruszone w części ćwiczeń Cygnus, które odbyły się w Walii w 2014 roku (INQ000128979). Najbardziej znaczącym uchybieniem zidentyfikowanym w trakcie tego działania była zdolność sektora opieki nad osobami dorosłymi do sprostania wymogom pandemii (Andrew Goodall 4 lipca 2023 r., 34/9-20).
- Raport Cygnusa z ćwiczeń: Dowództwo pierwszego poziomu po ćwiczeniach Pandemic Influenza – 18–21 października 2016 r., Public Health England, 2017, s. 6 (https://www.gov.uk/government/publications/uk-pandemic-preparedness/exercise-cygnus-report-accessible-report; INQ000022792)
- INQ000128057_0005 pierwszy akapit
- INQ000128057_0007 trzeci punkt
- INQ000128057_0007 punkt szósty
- INQ000128057_0009 pierwszy punkt
- INQ000128057_0005-0006
- INQ000177796_0007 ust. 25
- INQ000128057_0009 pierwszy punkt
- INQ000195847_0004 pkt 21. Zobacz też INQ000145733_0021 ust. 3.33
- INQ000022743_0002 ust. 6
- INQ000022748
- INQ000128057_0007 podpunkt trzeci i szósty, INQ000128057_0009 pierwszy punkt
- INQ000045034_0001-0002 ust. 4-5
- INQ000022921_0002
- INQ000022921_0002
- INQ000022748 ust. 1
- Matt Hancock 27 czerwca 2023 37/5-7, 52/4-24
- INQ000047302_0002 ust. 3
- INQ000131543_0003 pkt 10, 11, 13, 14
- INQ000090431; Raport Cygnusa z ćwiczeń: Dowództwo pierwszego stopnia po ćwiczeniach Pandemic Influenza – 18–21 października 2016 r., Public Health England, 2017 (https://www.gov.uk/government/publications/uk-pandemic-preparedness/exercise-cygnus-report-accessible-raport; INQ000022792); Clara Swinson 19 czerwca 2023 164/16-166/14
- Mark Lloyd 12 lipca 2023 r. 100/1-13
- Raport Cygnusa z ćwiczeń: Dowództwo pierwszego poziomu po ćwiczeniach Pandemic Influenza – 18–21 października 2016 r., Public Health England, 2017, s. 56 (https://www.gov.uk/government/publications/uk-pandemic-preparedness/exercise-cygnus-report-accessible-report; INQ000022792); INQ000006861_0001 ust. 2; Mark Lloyd 12 lipca 2023 r. 102/10-19
- Mark Lloyd 12 lipca 2023 r. 104/1-17; Zobacz też INQ000177803_0059-0060 pkt 233–234
- Mark Lloyd 12 lipca 2023 r. 107/18-108/2
- Mark Lloyd 12 lipca 2023 104/20-21
- INQ000177809_0015 ust. 39
- INQ000195843_0065 ust. 150; INQ000194054_0065 paragraf 256
- Zbadano dokumentację w odniesieniu do: Ćwiczeń Winter Willow (2007); Ćwiczenie Taliesin (2009); Ćwiczenia Valverde (2015); Ćwiczenia w zakresie gotowości na wypadek wirusa Ebola (2015); Ćwiczenie Srebrny Łabędź (2016); Ćwiczenie Alicja (2016); Ćwiczenie zorzy polarnej (2016); Ćwiczenie Łabędź (2016); Ćwiczenie Tyfon (2017); Ćwiczenie Broad Street (2018); Ćwiczenie Cerberus (2018); i Ćwiczenie Pica (2018) (INQ000195843_0038, 0044, 0052-0055, 0064 pkt 82-84, 113, 133-142, 149).
- INQ000194054_0065 paragraf 256
- INQ000092634_0005; INQ000177803_0059 paragraf 232
- INQ000205178_0103 paragraf 148.2
- INQ000177810_0008 ust. 25
- INQ000145912_0131 pkt 10.36
- INQ000184643_0071 paragraf 372
- INQ000006429_0002-0003 ust. 5
- Duncan Selbie 27 czerwca 2023_152/20-155/1
- INQ000181825_0017 paragraf 73
- Duncan Selbie 27 czerwca 2023 136/15-137/5, 139/13-140/12
- Dla Szkocji, zob Jeane Freeman 28 czerwca 2023 r. 137/15-138/12, Nicola Sturgeon 29 czerwca 2023 42.13-43.07, 46.14-47.16, 62.21-64.15, Catherine Calderwood 5 lipca 2023 r. 18.01-19.04; dla Walii, zob Frank Atherton 3 lipca 2023 26.02-11, 32.13-33.1, 65/4-67/3; dla Irlandii Północnej, zob Denis McMahon 6 lipca 2023 r. 66/1-20, Michael McBride 10 lipca 2023 147/11-24, 162/25-165/3, Richard Pengelly 11 lipca 2023 78/22-79/7, 24-111/3 110/3
- INQ000181825_0017 paragraf 72
- INQ000184639_0017 ust. 5.10
- INQ000057271_0006 ust. 25
- INQ000057281_0001-0002 dot. pozycji HCIDPB 16/46
- Christopher Wormald 19 czerwca 2023 96/13-97/8
- Christopher Wormald 19 czerwca 2023 122/14-19
- Dla Szkocji, zob Nicola Sturgeon 29 czerwca 2023 42.13-43.07; dla Walii, zob Frank Atherton 3 lipca 2023 r. 32.13-33.1; dla Irlandii Północnej, zob Arlene Foster 11 lipca 2023 r. 49/9-50/5, Richard Pengelly 11 lipca 2023 78/22-79/7
- Jenny Harries 26 czerwca 2023 177/13-178/11, 180/24-25/206/3-12
- INQ000194054_0027-0028 paragraf 108
- Michael Gove 13 lipca 2023 r. 158/7-8
- Sally Davies 20 czerwca 2023 r. 160/3-5
- INQ000194054_0027-0028 paragraf 108
- INQ000148429_0040 paragraf 144
- INQ000148429_0040 ust. 144; INQ000194054_0028 paragraf 110
- INQ000181825_0020 paragraf 88
- INQ000181825_0020 paragraf 89
- INQ000181825_0020-0021 paragraf 89
- INQ000057271_0006 ust. 26
- INQ000184637_0005-0006 ust. 4.2
- INQ000177809_0017 ust. 45; Nigel Edwards 13 lipca 2023 51/20-21
- Widzieć INQ000183420_0006 ust. 17; INQ000177809_0017 ust. 45
- INQ000147815_0005, 0006 ust. 19, 23
- INQ000177807_0012 pkt 42–44; INQ000177807_0015 pkt 53 (Walia); INQ000180759_0005 pkt 18–20 (Szkocja)
- Michael McBride 10 lipca 2023 180/14-18
- INQ000184637_0006 ust. 4.6
- INQ000147883_0017; INQ000147839_0008-0009; Raport Cygnusa z ćwiczeń: Dowództwo pierwszego poziomu po ćwiczeniach Pandemic Influenza – 18–21 października 2016 r., Public Health England, 2017, s. 33 (https://www.gov.uk/government/publications/uk-pandemic-preparedness/exercise-cygnus-report-accessible-report; INQ000022792)
- Christopher Wormald 19 czerwca 2023 133/3-134/2
- Matt Hancock 27 czerwca 2023 21/18-22, 94/17-95/2
- Katharine Hammond 16 czerwca 2023 183/24-184/12
- Michael McBride 10 lipca 2023 r. 121/18-122/24
- Michael McBride 10 lipca 2023 123/5-15
- INQ000203352_0012-0013 ust. 38
- INQ000183597 pierwszy akapit
- Frank Atherton 3 lipca 2023 44.22-45.10
- Andrew Goodall 4 lipca 2023 r., 34/9-20
- Gillian Russell 28 czerwca 2023 r. 76/25–78/25
- Gillian Russell 28 czerwca 2023 71/10
- INQ000182606_0006 ust. 20; Caroline Lamb 28 czerwca 2023 118/7-22; Jeane Freeman 28 czerwca 2023 r. 135/25-136/5
- Profesor David Alexander i Bruce Mann, eksperci w dziedzinie zarządzania ryzykiem i odporności (zob Załącznik 1: Informacje o tym module i metodologia badania) zauważył: „W przeciwieństwie do rządu Wielkiej Brytanii warto zauważyć, że zdecentralizowane administracje [w Szkocji i Walii] rzeczywiście dążyły do przygotowania na wypadek pandemii [w latach 2012–2016]” (INQ000203349_0166 ust. 490; zobacz ogólnie INQ000203349_0164-0168 pkt 482–494)
- np Mark Drakeford 4 lipca 2023 r. 192/3-25
- INQ000022069_0002, 0004 ust. 2, 11
- INQ000057522_0002
- Widzieć Oliver Dowden 21 czerwca 2023 90/8-91/1, 95/6-96/4, 105/11-107/20
- INQ000205310_0002 pierwszy i drugi punktor
- INQ000182612_0068-0069 pkt 5.8-5.10
- Oliver Dowden 21 czerwca 2023 95/22-23
- Oliver Dowden 21 czerwca 2023 96/1-4
- Oliver Dowden 21 czerwca 2023 98/16-17, 106/3-4
- INQ000182612_0069-0070 ust. 5.12
- Katharine Hammond 16 czerwca 2023 118/9-119/9
- Katharine Hammond 16 czerwca 2023 r. 119/15-16
- Katharine Hammond 16 czerwca 2023 119/10-16
- Oliver Dowden 21 czerwca 2023 93/17
- Oliver Dowden 21 czerwca 2023 93/13-94/2
- Michael Gove 13 lipca 2023 r. 108/24-109/9
- INQ000184643_0079-0080 ust. 416; Matt Hancock 27 czerwca 2023 64/12-65/2; Michael Gove 13 lipca 2023 148/16-151/22; Zobacz też Mark Drakeford 4 lipca 2023 r. 192/3-25
- Patrick Vallance 22 czerwca 2023 134/21-135/6
- Jenny Harries 26 czerwca 2023 206/19-21; Oliver Letwin 20 czerwca 2023 16.07-8
- Ramy odporności rządu Wielkiej Brytanii, Rząd Jej Królewskiej Mości, grudzień 2022 r. (https://assets.publishing.service.gov.uk/media/63cff056e90e071ba7b41d54/UKG_Resilience_Framework_FINAL_v2.pdf; INQ000097685)
- Ramy dotyczące odporności rządu Wielkiej Brytanii: aktualizacja wdrożenia z 2023 r., Gabinet Rady Ministrów, 4 grudnia 2023 r. (https://assets.publishing.service.gov.uk/media/656def711104cf0013fa7498/The_UK_Government_Resilience_Framework_2023_Implementation_Update.pdf; INQ000372824)
Rozdział 6: Nowe podejście
Wstęp
| 6.1. | Podstawą gotowości na wypadek pandemii jest zapewnienie porad ekspertów. Wielka Brytania ma szczęście, że dysponuje wieloma światowej klasy ekspertami, gotowymi zaoferować swoje usługi. Jednakże w wyniku dochodzenia stwierdzono, że system udzielania porad można i należy ulepszyć. To z kolei doprowadziłoby do bardziej świadomego i usprawnionego podejmowania decyzji. W niniejszym rozdziale rozważono najskuteczniejsze sposoby zapewnienia ministrom dostępu do doradztwa w odpowiednim czasie oraz odpowiedniego przedstawienia im szeregu opinii naukowych i opcji politycznych, które pomogą im lepiej przygotować się na ogólnosystemowe wyzwania cywilne i zbudować odporność na nie. sytuacje awaryjne. Zaleca nowe podejście. |
Rady dla ministrów
| 6.2. | Ministrom rzadko oferuje się doskonałe rozwiązania polityczne. Zwykle muszą równoważyć trudne kompromisy między konkurencyjnymi opcjami. To oni, a nie ich doradcy, są ostatecznie odpowiedzialni za podejmowanie decyzji dotyczących polityki i tego, gdzie należy dokonać kompromisu, ale polegają na doradztwie. |
| 6.3. | Ministrowie rozpoczynają swoją pracę, na ogół, jako amatorzy i często nie są przeszkoleni zawodowo w obszarach polityki swoich departamentów. Wymaga się od nich uczenia się w pracy.1 Muszą jednak zapewniać przywództwo swojemu wydziałowi i decydować o złożonych kwestiach politycznych, co jest nie mniej prawdziwe w dziedzinie gotowości i odporności na sytuacje kryzysowe. |
| 6.4. | Powinni zatem kwestionować porady otrzymywane zarówno od ekspertów, jak i urzędników. Jakość procesu decyzyjnego ministrów będzie tak dobra, jak głębokość i zakres otrzymywanych przez nich rad, a także sprawdzania tych rad. Poseł Michael Gove, kanclerz księstwa Lancaster od lipca 2019 r. do września 2021 r. i minister gabinetu od lutego 2020 r. do września 2021 r., powiedział śledczym:
„[W]to, co wnosimy, to możliwość zadania pytania „głupi chłopcze” i czasami dopiero gdy ktoś zadaje takie pytanie, dowiadujemy się, że cesarz nie ma ubrania lub plan gotowości na wypadek pandemii ma ogromną dziurę pośrodku.”² |
| 6.5. | Sir Oliver Letwin, poseł do parlamentu, minister polityki rządu od maja 2010 r. do lipca 2016 r. i kanclerz księstwa Lancaster od lipca 2014 r. do lipca 2016 r., stwierdził, że ze względu na brak wiedzy specjalistycznej absurdem jest przypuszczenie, że mógłby przeciwdziałać lub uchylić porady naukowców ekspertów.³ Jednakże ministrowie mogli i powinni zadać szersze pytania:
„Myślę, że z perspektywy czasu powinienem był sobie zadać pytanie: «Czy wszyscy ci eksperci się mylą?». ale: „Czy zadali właściwe pytania?” Bo to jest coś, co może zrobić amator. Być może tylko amator może to zrobić. Myślę, że w pewnym sensie trzeba być poza systemem, aby móc zadać to pytanie”. |
| 6.6. | Znaczenie przywództwa i perspektywy zapewnianej przez ministrów podkreślił dr Denis McMahon, stały sekretarz Biura Wykonawczego Irlandii Północnej od lipca 2021 r., który powiedział, że ministrowie:
„widzieć rzeczy z punktu widzenia osoby na miejscu… z mojego doświadczenia wynika, że duchowni nadają rzeczom realność, wnoszą poczucie celu, ponieważ po prostu łączą nas z powrotem ze wspólnotą”.⁵ |
| 6.7. | Profesor Sir Mark Walport, główny doradca naukowy rządu od kwietnia 2013 r. do września 2017 r., wyjaśnił prowadzącym dochodzenie, że z jego doświadczenia wynika, że ministrowie w rządzie przeglądali „trzy soczewki” przy podejmowaniu decyzji:
|
| 6.8. | Kluczem do poinformowania pierwszych dwóch z tych „soczewek” w kontekście planowania pandemii były porady ekspertów. Profesor Sir Patrick Vallance, główny doradca naukowy rządu od kwietnia 2018 r. do marca 2023 r., wyjaśnił, że wiązało się to z czterema pytaniami do doradcy:
|
| 6.9. | Istotne jest również, aby zlecać, udzielać i rozważać porady ekspertów dotyczące poszczególnych wariantów przed wystąpieniem sytuacji nadzwyczajnej, kiedy jest czas na odpowiednią analizę i rozważenie możliwych konsekwencji poszczególnych wariantów strategicznych. Profesor Walport zauważył:
„Każda sytuacja nadzwyczajna w kraju wywiera wpływ na życie obywateli wykraczający poza bezpośredni wpływ samej sytuacji nadzwyczajnej – i zawsze istnieje możliwość, że „lekarstwo” na konkretną sytuację nadzwyczajną w postaci polityki i działań mających na celu powstrzymanie pierwotnych szkód powoduje szkodliwe skutki „skutki uboczne”… Jednak tylko sami decydenci mogą ostatecznie zdecydować, w jaki sposób dokonać niezwykle trudnego wyboru pomiędzy – jako konkretnym i raczej wymownym przykładem – ochroną zdrowia i życia osób starszych i bezbronnych za pomocą środków, które są może zaszkodzić gospodarce i zakłócić edukację młodych ludzi.”¹² |
Poprawa świadczenia doradztwa naukowego
| 6.10. | Porady ekspertów były zamawiane przez ministrów, departamenty i organy publiczne. W dochodzeniu wysłuchano dowodów od szeregu naukowców na temat sposobu, w jaki tego dokonano. Ogólnie rzecz biorąc, osiem wad było widocznych:
|
Role ekspertów-doradców rządu Wielkiej Brytanii i zdecentralizowanej administracji
| 6.11. | Obowiązki głównego doradcy naukowego i dyrektora medycznego w zdecentralizowanych administracjach różnią się od obowiązków ich odpowiedników w rządzie Wielkiej Brytanii oraz od siebie nawzajem (zob. Rozdział 2: System – instytucje, struktury i przywództwo). Chociaż praca systemu głównych doradców naukowych i dyrektora medycznego Anglii skupiała się przede wszystkim na kwestiach istotnych dla Anglii, pełnili oni także znaczącą rolę w odniesieniu do kwestii mających wpływ na zdecentralizowane administracje¹³. Podobnie było w przypadku głównego doradcy naukowego rządu Wielkiej Brytanii.¹⁴ W dochodzeniu uznano, że przygotowanie się na sytuacje kryzysowe cywilne w całym systemie i budowanie odporności na nie wymaga, aby rządy zdecentralizowanych administracji miały dyrektora medycznego i głównego doradcę naukowego o szerszych obowiązkach, porównywalne z uprawnieniami dyrektora medycznego Anglii i głównego doradcy naukowego rządu Wielkiej Brytanii. Należy zatem zapewnić równość między głównymi lekarzami i głównymi doradcami naukowymi Wielkiej Brytanii a doradcami zdecentralizowanych administracji pod względem dostępu i wkładu w debaty na temat gotowości i odporności. Jeżeli zostanie przyjęte takie podejście, rząd Wielkiej Brytanii i zdecentralizowane administracje będą w lepszej sytuacji, aby sformułować jedno nadrzędne podejście do cywilnych sytuacji kryzysowych obejmujących cały system, dostosowując je jednocześnie do warunków każdej populacji. |
Zapewnienie ekspertom swobody doradzania
| 6.12. | Doradcy naukowi zazwyczaj odpowiadali na konkretne prośby o poradę. Profesor John Edmunds, profesor modelowania chorób zakaźnych w London School of Hygiene & Tropical Medicine – który był członkiem wielu naukowych grup doradczych – zauważył, że komitety te zajmowały się praktycznymi, codziennymi kwestiami w przypadku wystąpienia sytuacji kryzysowych, a nie szerszych kwestii strategicznych przed wystąpieniem sytuacji nadzwyczajnej.¹⁵ Profesor Thomas Evans, przewodniczący Komitetu Doradczego ds. Niebezpiecznych Patogenów od 2016 r., zauważył, że rady tego komitetu skupiały się na chorobach zakaźnych o poważnych konsekwencjach, a nie na ogólnej gotowości na wypadek pandemii.¹⁶ Profesor Sir Andrew Pollard, przewodniczący Wspólnej Komisji ds. Szczepień i Szczepień od 2013 r., powiedział, że o ile mu wiadomo, Departament Zdrowia i Opieki Społecznej nie zwracał się do tej komisji o rozważenie planowania na wypadek pandemii innych niż grypa ani o doradzanie w sprawie szczepionek oraz gromadzenie zapasów na wypadek innych chorób zakaźnych – mimo że mieściło się to w jego możliwościach i wiedzy specjalistycznej¹⁷ |
| 6.13. | Profesor Sir Peter Horby, członek Grupy Doradczej ds. Nowych i Pojawiających się Zagrożeń Wirusami Układu Oddechowego (NERVTAG) od 2014 r. i przewodniczący od maja 2018 r., powiedział ankietowanym:
„Treść spotkań była w dużej mierze zlecona przez [Departament Zdrowia i Opieki Społecznej] … nie było żadnych oczekiwań ani wyraźnej zachęty do rozważenia kwestii wykraczających poza konkretne komisje.”¹⁸ |
| 6.14. | Profesor Walport wyjaśnił, jak istotne jest, aby doradcy naukowi nie tylko odpowiadali na pytania, ale także zapewniali „spontaniczna rada” w kwestiach, które uznali za istotne, aby rząd mógł w pełni wykorzystać ich wiedzę fachową.¹⁹ Pogląd ten poparli profesor Vallance i dr Jim McMenamin, dyrektor działu ds. infekcji i dyrektor ds. incydentów strategicznych w Public Health Scotland.²⁰ |
| 6.15. | Profesor Wendy Barclay, kierownik ds. badań wirusologicznych w Action Medical Research w Imperial College w Londynie i członkini NERVTAG od 2014 r., wyjaśniła ankietowanym, że powodem niedostatecznego przemyślenia przez członków stowarzyszenia było „na zewnątrz pudełka”przed pandemią wynikało podobnie z faktu, że ich programy były „wypełniony” z zadaniami wyznaczonymi przez ministrów i urzędników²¹. W konsekwencji nie mieli czasu na rozważenie „niespodziewane”.²² Dotyczy to wirusów innych niż grypa oraz pełnego zakresu potencjalnych reakcji²³ |
| 6.16. | Z kolei profesor Sir Jonathan Van-Tam, przewodniczący NERVTAG w latach 2014–2017 i zastępca dyrektora ds. medycznych w okresie od października 2017 r. do marca 2022 r., uznał, że porady powinny być bardziej rygorystyczne i zorientowane na zadania oraz odpowiadać na prośby²⁴. Zachęcał departamenty rządowe do dokładniejszego przemyślenia kompetencji grup ekspertów i pytań do nich kierowanych. Profesor Van-Tam powiedział śledczym: „NERVTAG nie określa swoich własnych kompetencji, odpowiada na prośby i ogranicza się do dostarczonych wskazówek. Tak powinien działać rządowy komitet doradczy. Jeżeli nie odpowiada bezpośrednio na kierowane do niego prośby, to nie spełnia swojego celu.”²⁵ |
| 6.17. | Profesor Sir Christopher Whitty, dyrektor medyczny Anglii od października 2019 r., opisał „Zasada 80/20”, gdzie większość czasu (80%) należy przeznaczyć na sprawy, o które pytał rząd, ale znaczną mniejszość (20%) należy przeznaczyć na sprawy, o które rząd nie pytał.²⁶ Powiedział w dochodzeniu, że dokładna linia losowanie powinno zależeć od uznania niezależnych przewodniczących, ale należy zachować swobodę. W przeciwnym razie grupy ekspertów i komitety staną się przedłużeniem rządu²⁷ Dochodzenie potwierdza tę opinię. Oprócz odpowiadania na pytania zlecone specjalnie przez ministrów i urzędników, doradcy powinni mieć swobodę rozważenia szerszego kontekstu, w którym zwrócono się o ich poradę.²⁸ Należy zachować równowagę pomiędzy poradami zlecanymi od góry do dołu a poradami udzielanymi spontanicznie przez dół do góry. Doradcy naukowi powinni być „”licencjonowanych dysydentów'”, którego ogólnym zadaniem jest przedstawianie opinii naukowych i kwestionowanie całego systemu.²⁹ |
| 6.18. | Kolejnym problemem jest to, że osoby składające prośby mogą nie wiedzieć dokładnie, jak powinny być sformułowane. Niepotrzebnie ograniczało to grupy ekspertów. Często ich kompetencje były zbyt wąskie, zlecanie doradztwa było zbyt sztywne i nie było wystarczającej ilości czasu na głębsze przemyślenie rozwiązania problemów, o rozpatrzenie których poproszono.³⁰ W rezultacie nie byli w stanie działać z wystarczającą autonomią. The Inquiry zgadza się z profesorem Whitty, że elastyczność ma kluczowe znaczenie. Istnieją bardzo mocne argumenty za tym, aby niezależne grupy ekspertów posiadały mandat do myślenia szerszego i strategicznego. Mogliby wtedy pomyśleć o ogólnej gotowości na wypadek pandemii, a nie tylko o reagowaniu na komisje.³¹ |
Znaczenie informacji zwrotnej
| 6.19. | Okazało się również, że przed pandemią nie panowała kultura rutynowego informowania ekspertów naukowych o tym, jak rząd zastosował się do ich porad. Niektórzy doradcy mieli ograniczoną wiedzę na temat zakresu, w jakim ich rady zostały uwzględnione, jeśli w ogóle.³² |
| 6.20. | W dochodzeniu uznano, że opinie naukowe dotyczące gotowości i odporności powinny rutynowo zachęcać do dwustronnej dyskusji między ministrami i ekspertami. Powinien istnieć system zachęcający do wymiany informacji między doradcami naukowymi a decydentami.³3 Poprawiłoby to jakość zarówno zadawanych pytań, jak i udzielanych porad – pętla pozytywnego sprzężenia zwrotnego. Znacząco usprawniłoby to obecny system.³⁴ |
Zakres specjalizacji
| 6.21. | Wszystkie cywilne sytuacje nadzwyczajne obejmujące cały system mają głębokie skutki gospodarcze i społeczne, podobnie jak środki podjęte w odpowiedzi przez rządy. Skuteczne i długoterminowe podejście do gotowości i odporności powinno zatem umożliwiać rządowi korzystanie z porad obejmujących szereg specjalizacji – od wiedzy naukowej po ekonomiczną – a także od ekspertów rozumiejących wpływ na osoby fizyczne, przedsiębiorstwa i społeczeństwo. W przypadku gotowości na wypadek pandemii doradztwo naukowe będzie w naturalny sposób skupiać się na naukach biomedycznych, ale ze względu na sytuację nadzwyczajną cywilną obejmującą cały system nie może to wykluczać innej wiedzy specjalistycznej. |
| 6.22. | Jednak komitety ekspertów doradzające rządom w zakresie gotowości na wypadek pandemii dopuściły się poważnych zaniedbań. Opinia była ukierunkowana na porady biomedyczne i nie obejmowała porad społeczno-ekonomicznych od porównywalnych ekspertów. Punktem odniesienia dla profesora Whitty'ego była Naukowa Grupa Doradcza ds. Nagłych Wypadków (SAGE) (zbierana w nagłych przypadkach), ale odnosiło się to również do szeregu grup ekspertów doradzających w zakresie gotowości:
„Nie sądzę, aby ludzie z SAGE, w tym ja, mieli kompetencje, aby zapewnić rząd, że rozważyli problem gospodarczy i mogą teraz przedstawić ogólny pogląd na ten temat. Myślę, że trzeba to zrobić osobno.”³⁵ Ta ważna kwestia jest analizowana w module 2. |
| 6.23. | Naukowcy, którzy złożyli zeznania w dochodzeniu, utrzymywali, że mogą doradzić rządowi tylko w jednym aspekcie gotowości: środków zaradczych mających na celu natychmiastową ochronę życia. Nie mogli wyjść poza swoją wiedzę specjalistyczną i dokonać oceny uwzględniającej szerszy wpływ społeczny – była to kwestia wybranych przywódców, kierujących się ich wartościami i osądem.³⁶ Jest to oczywiście słuszne. Jednakże obecnie nie ma instytucji, która mogłaby doradzić ministrom, w jaki sposób najlepiej rozwiązać te problemy. Celem nie jest pozbawienie przywódców politycznych ich odpowiedzialności, ale wsparcie ich w stosowaniu się do oceny ważnego zadania, jakim jest budowanie gotowości i odporności w długoterminowych interesach Wielkiej Brytanii (w tym krajów zdecentralizowanych). |
| 6.24. | Profesor Dame Sally Davies, dyrektor medyczny Anglii od czerwca 2010 r. do października 2019 r., stwierdziła potrzebę „zrównoważyć model biomedyczny”, tak aby decydentom rządowym zaprezentowano porady z szerszego zakresu perspektyw. Może to obejmować na przykład wpływ na gospodarkę, dobrobyt społeczny oraz edukację dzieci i młodych ludzi.³⁷ Jak opisała, powinno być „ramy instytucjonalne zapewniające pełen zakres opinii z każdej dyscypliny”.³⁸ Profesor Edmunds zaobserwował potrzebę większej interakcji między ekonomistami i epidemiologami w celu poprawy ilości i jakości ocen ekonomicznych dotyczących pandemii.³⁹ |
| 6.25. | Profesor Walport podkreślił znaczenie równoważenia doradztwa naukowego z innymi, potencjalnie konkurencyjnymi czynnikami:
"[I]t niezwykle ważne jest, aby decydenci otrzymali porady na temat potencjalnych negatywnych konsekwencji, na przykład blokad, dla przedsiębiorstw, |
| 6.26. | Jak powiedział profesor Vallance w dochodzeniu, zakres wiedzy specjalistycznej, z której można skorzystać, może obejmować: „wiele dyscyplin naukowych, inżynieria, nauki społeczne, modelowanie matematyczne, ekonomia itp. Będą one również powiązane z przemysłem, zarówno małym, jak i dużym.”⁴¹ Rząd Wielkiej Brytanii i zdecentralizowane administracje skorzystałyby na tej wiedzy specjalistycznej, gromadząc się w celu systematycznego doradzania swoim rządom. Jak powiedział profesor Vallance: „[T]tutaj jest coś o zgromadzeniu masy krytycznej ludzi, którzy zajmują się tym samym ogólnym problemem.”⁴² Przyniesie wyzwanie, niezależność i przewidywanie. W zapytaniu stwierdzono, że możliwość uwzględnienia tego zakresu poszczególnych dyscyplin eksperckich „zacząłby dostarczać wglądu w to, jak możesz myśleć o rodzaju trudnych kompromisów, które tam występują”.⁴³ |
| 6.27. | Zapewniłoby to lepsze oparcie doradztwa strategicznego na poprawie potencjału i możliwości rządu Wielkiej Brytanii i zdecentralizowanych administracji. Jak określono w Rozdział 4: Skuteczna strategia I Rozdział 5: Uczenie się na doświadczeniachumiejętności, technologia i infrastruktura na potrzeby gotowości na wypadek pandemii powinny skupiać się przede wszystkim na skalowalnych systemach testowania, śledzenia, izolacji, kontroli granicznych i zwiększaniu potencjału opieki zdrowotnej i społecznej. |
Koordynacja porad
| 6.28. | Nie było podmiotu, który nadzorowałby system eksperckiego doradztwa naukowego, aby był on szeroko zakrojony, zintegrowany i skoordynowany. Naukowe komitety doradcze doradzające w zakresie gotowości i odporności na pandemię powinny stanowić część całego systemu, który „szeroko współpracuje, aby zapewnić doradztwo uwzględniające szerszy system nauki oraz zintegrowane i skoordynowane z innymi jego częściami”.⁴⁴ |
| 6.29. | Profesor Jimmy Whitworth, biegły w dziedzinie nadzoru nad chorobami zakaźnymi (patrz Załącznik 1: Kontekst tego modułu i metodologia badania), uznał, że przydatne byłoby, gdyby grupy ekspertów skupiały się na obszarach, w których leży ich wiedza specjalistyczna. Chciał jednak, aby ich zalecenia zostały skoordynowane i zsyntetyzowane w rządzie, aby uzyskać całościowy obraz zagrożeń⁴⁵ Brakowało takiego wspólnego myślenia. |
| 6.30. | Wielu ekspertów-doradców pracujących w ramach tego systemu stwierdziło, że jest to skomplikowany obraz. Profesor David Salisbury, dyrektor ds. szczepień w Departamencie Zdrowia w latach 2007–2013, zauważył: „eksplozja komitetów” w tej dziedzinie.⁴⁶ Kwestionował skuteczność, skuteczność i wpływ „w proces doradczy zaangażowane są tysiące osób” w stosunku do czasu i zasobów, jakie każdy z nich zużył.⁴⁷ Profesor Horby powiedział w dochodzeniu, że „[t]Struktura zarządzania, w której mieścił się NERVTAG, była dość skomplikowana”, przy braku jasności co do struktur raportowania i pytaniach dotyczących tego, kto przed kim jest odpowiedzialny, pomiędzy NERVTAG, innymi naukowymi grupami doradczymi oraz Departamentem Zdrowia i Opieki Społecznej.⁴⁸ |
| 6.31. | Profesor Barclay podał przykłady dobrej współpracy NERVTAG z innymi naukowymi grupami doradczymi, zauważając: „[T]w pewnym stopniu kompetencje tych komisji(-ów) pokrywają się, a wspólne spotkania umożliwiły połączenie określonej wiedzy specjalistycznej.”⁴⁹ Jednakże profesor Horby zasugerował, że jest to raczej wyjątek niż reguła: „NERVTAG był samodzielnym komitetem utworzonym jako komitet zadaniowy odpowiadający konkretnym komisjom [Departament Zdrowia i Opieki Społecznej]”.⁵⁰ Oznaczało to, że „zakres pracy z innymi grupami był stosunkowo ograniczony”.⁵¹ Profesor Barclay powiedział także:
„Z perspektywy czasu zdaję sobie sprawę, że zakładałem, ale nie wiedziałem, czy inne grupy omawiały… sprawy gdzie indziej. Wiedzieliśmy, o co nas proszono, w jaki sposób działały komisje, ale nie rozumiałem, jak to pasuje do szerszego obrazu całości planu reakcji na pandemię.”⁵² |
| 6.32. | Na przykład każdy z poniższych organów skupiał się na nieco innych obszarach, bez odpowiedniego procesu, dzięki któremu można by koordynować ich pracę poza sytuacją nadzwyczajną:
|
| 6.33. | W sytuacjach awaryjnych SAGE pracowała jako „dyrygent orkiestry” naukowców; jednakże w okresie pomiędzy sytuacjami nadzwyczajnymi nie istniała równoważna jednostka.⁵⁸ Profesor Horby stwierdził, że coroczne wspólne spotkanie przewodniczących naukowych grup doradczych i urzędników wyższego szczebla:
„Mogło przydać się dokonanie przeglądu działań każdego komitetu, ocena ogólnego stanu gotowości i upewnienie się, że prace komisji uwzględniły wszystkie podstawy doradztwa naukowego na temat gotowości na wypadek pandemii”.⁵⁹ |
| 6.34. | SAGE w najściślejszym tego słowa znaczeniu jest „podmiotem odpowiedzi”. Zapewnia COBR (krajowemu rządowi brytyjskiego centrum zarządzania kryzysowego odpowiedzialnemu za reagowanie na cywilne sytuacje kryzysowe obejmujące cały system) doradztwo naukowe na poziomie Wielkiej Brytanii i interpretuje złożone lub niepewne dowody naukowe w formie nietechnicznej.⁶⁰ Posiedzenia są zwykle zwoływane wyłącznie w odpowiedzi na konkretna sytuacja awaryjna. Nie było równoważnego mechanizmu ułatwiającego rygorystyczną debatę naukową na temat najlepszego przygotowania się na takie sytuacje kryzysowe i budowania odporności. Nie istniał żaden podmiot koordynujący doradztwo naukowe i inne dotyczące gotowości i odporności pomiędzy sytuacjami kryzysowymi. |
| 6.35. | Kodeks postępowania z grudnia 2021 r. dla Naukowe Komitety Doradcze i Rady mogą stanowić część rozwiązania służącego zbudowaniu skutecznego systemu doradztwa naukowego, czyli:
„taki, który szeroko współpracuje w celu dostarczania porad uwzględniających szerszy system nauki oraz zintegrowanych i skoordynowanych z innymi jego częściami. |
Termin udzielania porad
| 6.36. | Obecny system nie był zorganizowany w taki sposób, aby kluczowe polityki były rozważane przed pandemią (jak omówiono w Rozdział 4: Skuteczna strategia). Jest to potwierdzenie istnienia poważnej wady brytyjskiej architektury gotowości. Profesor Whitty powiedział śledczym:
„Pomyślałem, że byłoby bardzo zaskakujące, gdyby nie wniosek ze strony wyższego rangą polityka lub kogoś podobnego, aby komitet naukowy zaryzykował: |
| 6.37. | Istniała zasadnicza różnica pomiędzy środowiskiem, w którym politycy szukali porady ekspertów w czasie sytuacji nadzwyczajnej, a środowiskiem pomiędzy sytuacjami kryzysowymi. Profesor Whitty wyraził frustrację związaną z koniecznością zainteresowania decydentów pomiędzy sytuacjami kryzysowymi:
„W sytuacji awaryjnej wszyscy domagają się porad naukowych… Pomiędzy sytuacjami kryzysowymi trzeba w pewnym sensie przepychać się łokciem. Dlatego też uważam, że dużym ryzykiem jest możliwość faktycznego zaangażowania się w cały system pomiędzy sytuacjami awaryjnymi.”⁶³ |
| 6.38. | W dochodzeniu przyznano, że jest to ryzyko. Ministrom należy zapewnić odpowiedni zakres porad ekspertów na temat gotowości, odporności i potencjalnych reakcji, które należy rozważyć przed wystąpieniem sytuacji nadzwyczajnej, gdy mają więcej czasu na właściwe rozważenie. Umożliwiłoby to decydentom lepszą analizę i kwestionowanie porad i możliwych opcji. |
„Myślenie grupowe”
| 6.39. | Poproszeni o wskazanie, co mogło być przyczyną niektórych błędnych sposobów myślenia związanych z planowaniem i przygotowaniem Wielkiej Brytanii na wypadek pandemii, a co za tym idzie także udzielonych porad, wielu świadków składających zeznania w dochodzeniu obwiniało „myślenie grupowe”. Jest to zjawisko polegające na tym, że ludzie w grupie mają tendencję do myślenia o tych samych rzeczach w ten sam sposób. |
| 6.40. | Byli świadkowie, którzy wyraźnie przypisali przynajmniej część winy za brak gotowości Wielkiej Brytanii na wypadek pandemii „myśleniu grupowemu”. Byli wśród nich: poseł David Cameron (premier od maja 2010 r. do lipca 2016 r.), Clara Swinson (dyrektor generalny ds. zdrowia globalnego i publicznego w Departamencie Zdrowia i Opieki Społecznej od listopada 2016 r. oraz przewodnicząca Rady Programowej ds. gotowości na wypadek grypy pandemicznej od 2017 r. do 2022), Sir Oliver Letwin, poseł George Osborne (kanclerz skarbu od maja 2010 r. do lipca 2016 r.), profesor Davies, poseł Jeremy Hunt (sekretarz stanu ds. zdrowia i opieki społecznej od września 2012 r. do lipca 2018 r.), profesor Whitty, Rosemary Gallagher (kierownik ds. zapobiegania i kontroli infekcji w Royal College of Nursing od lipca 2009 r.), dr Richard Horton (redaktor naczelny Nazwa naukowego czasopisma medycznego od 1995 r.) oraz Instytut Ochrony Ludności i Zarządzania Kryzysowego.⁶⁴ |
| 6.41. | Inni, choć nie przypisywali wyraźnie winy „myśleniu grupowemu”, zgodzili się jednak, że jest to ryzyko, które należy ograniczyć. Należeli do nich dr Stuart Wainwright (dyrektor Rządowego Biura ds. Nauki od grudnia 2019 r. do czerwca 2023 r.), profesor Walport, profesor Vallance i pan Gove.⁶⁵ |
| 6.42. | Dwóch świadków, profesor Dame Jenny Harries (dyrektor naczelny brytyjskiej Agencji Bezpieczeństwa Zdrowia od kwietnia 2021 r.) i dr Claas Kirchhelle, biegły ds. struktur zdrowia publicznego (zob. Załącznik 1: Informacje o tym module i metodologia badania), wyraźnie odrzucił pogląd, że „myślenie grupowe” jest zjawiskiem, które negatywnie wpływa na gotowość Wielkiej Brytanii na wypadek pandemii.⁶⁶ |
| 6.43. | Samo „myślenie grupowe” jest po prostu opisem wyniku. Konieczne jest zrozumienie, jak i dlaczego tak się dzieje oraz co można zrobić, aby temu zaradzić. Dynamika bycia częścią grupy może w sposób wyraźny lub ukryty zachęcać do konsensusu i zniechęcać do wewnętrznego kwestionowania rozważenia alternatyw. Może to skutkować irracjonalnym lub złym podejmowaniem decyzji. Jednakże konsensus sam w sobie niekoniecznie jest czymś złym, pod warunkiem, że przed osiągnięciem konsensusu odbędzie się odpowiednia dyskusja i pod warunkiem, że będzie on otwarty na kwestionowanie. |
| 6.44. | Rok 2018 Brytyjska strategia bezpieczeństwa biologicznego, opublikowany przez rząd Wielkiej Brytanii i odnoszący się do prac rządu Wielkiej Brytanii i zdecentralizowanych administracji, określa, w jaki sposób Wielka Brytania była chroniona przed znaczącymi zagrożeniami biologicznymi.⁶⁷ Stwierdzono w niej, że Wielka Brytania „światowej sławy” za jakość swojego planowania gotowości i stwierdził, że Wielka Brytania „wiodące na świecie możliwości”, aby zaradzić znaczącym zagrożeniom biologicznym, takim jak ogniska chorób.⁶⁸ Podkreślono, że reakcja rządu Wielkiej Brytanii na wybuch choroby musi opierać się na „możliwości i możliwości naukowe” i stwierdził, że Wielka Brytania jest „dobrze podane”przez A „szybki, skalowalny i kompleksowy system reagowania, który jest elastyczny w stosunku do zagrożeń i jest w stanie poradzić sobie z nowymi zagrożeniami w miarę ich pojawiania się”.⁶⁹ |
| 6.45. | Globalny Indeks Bezpieczeństwa Zdrowotnego został stworzony przez Uniwersytet Harvarda i przyjęty przez Światową Organizację Zdrowia.⁷⁰ W Globalnym Indeksie Bezpieczeństwa Zdrowotnego za 2019 r. Wielka Brytania zajęła drugie miejsce w klasyfikacji generalnej i pierwsze w kategorii „Szybkie reagowanie i łagodzenie rozprzestrzeniania się epidemii”.⁷¹ Profesor Mark Woolhouse, profesor epidemiologii chorób zakaźnych na Uniwersytecie w Edynburgu, stwierdził na temat tego wskaźnika, że istnieje ryzyko popadnięcia w samozadowolenie i że „okazał się bardzo słabym wskaźnikiem wyników w obliczu faktycznej pandemii”.⁷² Chociaż takie globalne wskaźniki mogą być pomocne, mogą również dać krajom błędną pewność, że są obiektywnie lub porównywalnie dobrze przygotowane, a zatem mniej podatne na ogniska chorób zakaźnych. |
| 6.46. | Dokumenty te mogą jednak wyjaśniać część zapewnień, jakie otrzymał poseł Matt Hancock, sekretarz stanu ds. zdrowia i opieki społecznej od lipca 2018 r. do czerwca 2021 r. Powiedział śledczym, że tak „zapewniliśmy, że Wielka Brytania jest jednym z krajów na świecie najlepiej przygotowanych do reagowania na pandemię”.⁷³ Wielka Brytania została uznana za jednego ze światowych liderów w zakresie gotowości na wypadek pandemii, w tym przez Światową Organizację Zdrowia, co Hancock (między innymi) uważał za „wiarygodne źródło”.⁷⁴ |
| 6.47. | Ponownie, kiedy po raz pierwszy pojawił się koronawirus (Covid-19), pan Hancock był „wielokrotnie zapewniany” przez Public Health England, że ryzyko dla populacji Wielkiej Brytanii zostało ocenione jako bardzo niskie i „nie martwić się”.⁷⁵ Nawet pod koniec 2020 r. Public Health England zapewnił go, że Wielka Brytania „dobrze przygotowane" i to "diagnozowanie, prowadzenie i zajmowanie się przypadkiem znalezienia, a następnie leczenia i ośrodków specjalistycznych [był] wszystko ustawione”.⁷⁶ Jednakże na rady oferowane ministrom i organom międzynarodowym mógł mieć wpływ pewien stopień „myślenia grupowego” w sprawie gotowości na wypadek pandemii. |
| 6.48. | Dochodzenie wykazało, że w trzech ważnych obszarach osiągnięto konsensus pomiędzy Gabinetem Rady Ministrów, Ministerstwem Zdrowia i Opieki Społecznej oraz zdecentralizowaną administracją – a mimo to konsensus był błędny. Tymi obszarami były:
|
| 6.49. | Jak zbadano wcześniej w niniejszym Raporcie, poczyniono przygotowania w tym sensie, że istniał Program Chorób Zakaźnych o Wysokich Konsekwencjach, ale dotyczył on jedynie wybuchu epidemii na małą skalę (jak omówiono w Rozdział 5: Uczenie się na doświadczeniach). Duncan Selbie, dyrektor naczelny Public Health England od lipca 2012 r. do sierpnia 2020 r., wyjaśnił, że Public Health England planowało zawsze jedynie liczby rzędu kilkuset i że nigdy nie było żadnych dyskusji z Sekretarzem Stanu ani kimkolwiek innym na temat potrzeby masowa reakcja przed pandemią Covid-19.⁷⁷ Stało się tak pomimo tego, że Public Health England zgodnie z deklaracją pełniło funkcję krajowej agencji ekspertów ds. zdrowia publicznego, której pierwszą funkcją było wypełnianie obowiązków Sekretarza Stanu ds. Zdrowia i Opieki Społecznej w zakresie ochrony społeczeństwa przed chorobami zakaźnymi i odpowiadać za zapewnienie krajowej infrastruktury ochrony zdrowia, w tym za badanie ognisk chorób zakaźnych i zarządzanie nimi.⁷⁸ |
| 6.50. | Dochodzenie wydaje się, że brak odpowiedniego przemyślenia tych kwestii przed pandemią jest, przynajmniej częściowo, wynikiem „myślenia grupowego”. Albo nikt o nich nie pomyślał, albo nikt nie był w stanie sprawić, aby wystarczająca liczba innych osób w systemie pomyślała i coś z nimi zrobiła – połączenie „myślenia grupowego” i braku proaktywnego kwestionowania konsensusu. |
| 6.51. | Ważne jest, aby nie lokalizować tego „myślenia grupowego” wyłącznie w obrębie grup ekspertów, które doradzały rządowi Wielkiej Brytanii w sprawie gotowości lub z nich nie pochodzić. To był błąd systemowy. Nie oznacza to, że nikt nie ponosi odpowiedzialności: dotyczyło to zarówno urzędników, ekspertów, jak i ministrów. Każda osoba zaangażowana w gotowość na wypadek pandemii ponosi pewną odpowiedzialność, ale winni są głównie ci, którzy przewodzili organizacjom odpowiedzialnym za gotowość, odporność i reagowanie na sytuacje kryzysowe. |
Zrozumienie i ambitne rady
| 6.52. | Opinia naukowa otrzymana przez rząd Wielkiej Brytanii – a w konsekwencji także zdecentralizowane administracje, które w przerwach między sytuacjami nadzwyczajnymi polegały na tych samych opiniach – nie była przedmiotem wystarczającego zewnętrznego sprzeciwu ani ze strony ministrów, ani urzędników. Nie istniała instytucjonalna ochrona przed ryzykiem utrwalenia się konwencjonalnej wiedzy w instytucjach odpowiedzialnych za gotowość i odporność na sytuacje kryzysowe. Ministrowie i urzędnicy zajmujący się gotowością, odpornością i reagowaniem na sytuacje kryzysowe powinni lepiej rozumieć tę specjalistyczną dziedzinę, nie tylko w sytuacjach kryzysowych, ale także pomiędzy nimi.⁷⁹ Muszą zanurzyć się w temacie, zrozumieć go i zadawać pytania na jego temat. Wielu ministrów mogło zrobić więcej, zadając pytania. Pan Hunt zgodził się, że „wspólnie nie włożyliśmy w to nic takiego, jak czas, wysiłek i energia” w zrozumienie zagrożeń związanych z patogenami lub podważenie konsensusu.⁸⁰ Dochodzenie potwierdza tę opinię. |
| 6.53. | Hunt dostarczył jednak doskonały przykład wartości wyzwań ministerialnych. Opowiedział o swoim zaangażowaniu w ćwiczenia Cygnus – międzyrządowe ćwiczenia przeprowadzone w 2016 r. mające na celu sprawdzenie reakcji Wielkiej Brytanii na poważną pandemię grypy. Hunt pamięta, że w trakcie ćwiczeń poproszono go o zatwierdzenie opróżnienia wszystkich łóżek na oddziałach intensywnej terapii w kraju, aby, jak twierdzono, uratować więcej istnień ludzkich.⁸¹ Nazywało się to „segregacja populacji”.⁸² Powiedział: „Słusznie czy nie… Nie byłem na to przygotowany.”⁸³ W wyniku jego decyzji opracowano całkowicie nowe protokoły określające, w jaki sposób należy podejmować te decyzje.⁸⁴ Ten skrajny przykład pokazuje, jak poprzez przedstawienie ministrowi realiów gotowości, odporności i reagowania na sytuacje kryzysowe uzyskano zupełnie nową perspektywę zdobyte. Stało się tak raczej z powodu, a nie pomimo braku wiedzy specjalistycznej. Hunt mógłby przedstawić nową perspektywę i rozważyć przeciwstawną opinię, a mianowicie swój pogląd, że Sekretarz Stanu ds. Zdrowia i Opieki Społecznej zwykle nie jest w najlepszej sytuacji, aby podjąć taką decyzję.⁸⁵ |
| 6.54. | Ministrowie powinni także zdawać sobie sprawę, że może spotkać ich niepewność, a eksperci powinni być przygotowani na jej przedstawienie. Integralną częścią każdej porady jest nieodłączna niepewność. Rady ekspertów nie różnią się. Jeżeli minister ma skutecznie rzucić wyzwanie, ci, którzy doradzają ministrom, powinni zadbać o to, aby zakomunikowali tę niepewność. Nie ma jednego, standardowego sposobu wyrażenia tego podczas przedstawiania dowodów lub porad decydentom i społeczeństwu.⁸⁶ Wiele naukowych grup doradczych udzielało porad decydentom w ramach „zgoda⁸⁷ Zarówno profesorowie Vallance, jak i Whitty zasugerowali w odniesieniu do SAGE, że decydentom zazwyczaj przedstawiano konsensus, który wyrażał szereg możliwości i opisywał niepewności.⁸⁸ Profesor Whitty powiedział w dochodzeniu, że decydenci muszą się ze sobą skonfrontować z kilkoma, konkurencyjnymi poglądami naukowymi, spośród których oczekuje się, że wybiorą „w gorącej sytuacji awaryjnej”, byłoby nieprzydatne.⁸⁹ |
| 6.55. | Może to mieć miejsce w sytuacji nadzwyczajnej, ale celem zachowania gotowości jest umożliwienie decydentom rozważenia i sprawdzenia polityk z wyprzedzeniem. Celem przedstawienia ministrom przed pandemią szeregu opcji, z których każda opiera się na dowodach naukowych i niepewności o różnym stopniu, jest umożliwienie im wyboru najwłaściwszej reakcji w przypadku wystąpienia kryzysu. Jest to z konieczności ocena wartościująca – podkreślająca znaczenie podejmowania ostatecznych decyzji przez przywódców politycznych. Nie oznacza to, że system przygotuje się tylko na jedną reakcję, wykluczając inne, ale powoduje, że osoby w nim pracujące zastanawiają się i wypracowują przed wystąpieniem sytuacji awaryjnej, które opcje są poparte najlepszymi dowodami. |
| 6.56. | Gove zauważył, że politycy poszukują pewności tam, gdzie w przeciwnym razie mogłaby ona nie istnieć, i że konieczna jest szersza dyskusja na temat różnorodności opinii:
„[W]Poszukujemy pewności, ale często jest ona nieuchwytna i byłoby lepiej, gdyby politycy i decydenci powiedzieli: „Opowiedz mi o debacie, jaka jest wiodąca opcja w społeczności akademickiej, ale jakie są także alternatywy?” ⁹⁰ |
| 6.57. | Pan Hunt podobnie powiedział dochodzeniu:
„Kiedy byłem ministrem spraw zagranicznych, odkryłem, że mój poprzednik William Hague poinstruował swoich urzędników, jako ministra spraw zagranicznych, że za każdym razem, gdy pojawia się spór… chciał, żeby go poinformowano o sporze”. |
| 6.58. | W opinii Dochodzenia „opowiedz mi o debacie” powinno znajdować się w centrum pytań, o które ministrowie zwracają się do doradców przy ustalaniu polityki w zakresie gotowości i odporności. Obowiązkiem ministra jest zapoznanie się z radą i dotarcie do sedna kwestii przed podjęciem świadomej decyzji. |
| 6.59. | Celem powinno być położenie kresu kulturze konsensusu, w której zakorzeniona jest ortodoksja. Ministrowie powinni mieć dostęp do pełnego zakresu opinii lub być narażeni na niejasności w wydawanych opiniach oraz powinni zadawać ważne pytania. System gotowości i odporności powinien instytucjonalnie podlegać kwestiom. |
Użycie czerwonych drużyn
| 6.60. | Zasadniczym antidotum na „myślenie grupowe” jest kontrola zewnętrzna, nadzór i rzucanie wyzwanie dominującym instytucjom zaangażowanym w przygotowanie na wypadek pandemii. Jednym ze sposobów włączenia perspektywy zewnętrznej do doradztwa i procesu decyzyjnego w rządzie są „czerwone zespoły”, rozwiązanie, które spotkało się z uznaniem wielu świadków.⁹² Czerwone zespoły to grupy osób spoza zaangażowanych struktur doradczych i decyzyjnych w opracowywaniu polityk, strategii i planów.⁹³ |
| 6.61. | Są cennymi narzędziami z dwóch głównych powodów.⁹⁴ Po pierwsze, ich niezależność od struktur instytucjonalnych zapewnia im świeżą perspektywę, umożliwiając im obiektywną ocenę sposobu myślenia innych i identyfikację błędów poznawczych, które mogą prowadzić do błędów w ocenie.⁹⁵ Są mniej podatni na wszelkie „myślenie grupowe”, nastawienie optymistyczne, zdobytą wiedzę lub zakładaną ortodoksję, które z czasem mogą narastać w tych instytucjach. Po drugie, ich niezależność pozwala im lepiej zadawać trudne pytania i kwestionować uprzedzenia, bez defensywnej postawy lub strachu przed konsekwencjami osobistymi lub zawodowymi, które mogą wystąpić wśród kolegów pracujących w tej samej instytucji.⁹⁶ |
| 6.62. | Wyraźna struktura niezależnych czerwonych zespołów sprawia, że dobrze nadają się do pełnienia wielu różnych ról, które pomagają usprawnić proces podejmowania decyzji, takich jak:
|
| 6.63. | Ogólnie zaleca się, aby w skład czerwonych zespołów wchodzili różni eksperci i osoby niebędące ekspertami.⁹⁸ Zespół czerwony będzie potrzebował kilku członków, którzy są ekspertami w danej dziedzinie, aby zrozumieć materiał. Jednakże ważne jest również włączenie do dyskusji członków niebędących ekspertami, którzy nie znają szczegółowo konkretnego tematu, ale ogólnie posiadają umiejętność analitycznego i krytycznego myślenia. Zapewnia to możliwie najszersze i najostrzejsze zakwestionowanie analizowanych porad lub procesów decyzyjnych, a także chroni przed ryzykiem błędów poznawczych, nawet w samej drużynie czerwonych. |
| 6.64. | Czerwone zespoły nie są nowym pomysłem w rządzie ani w przemyśle. Są one prawdopodobnie najbardziej ugruntowane jako narzędzie w wojsku i obronności, a Ministerstwo Obrony opublikowało wytyczne dotyczące czerwonych drużyn już w 2010 r.⁹⁹ Zalecono je również jako pomocną technikę w bardziej ogólnym zarządzaniu ryzykiem w badaniu z 2011 r. Przegląd Blacketta dotyczący ryzyk o dużym wpływie i niskim prawdopodobieństwie, przegląd prowadzony przez głównego doradcę naukowego rządu, w którym rozważono, w jaki sposób rząd Wielkiej Brytanii mógłby najlepiej identyfikować, oceniać, komunikować i określać ilościowo nieodłączną niepewność w przypadku ryzyk o dużym wpływie i niskim prawdopodobieństwie¹⁰⁰ Grupy ekspertów przypominające niektóre cechy czerwonych zespołów byli zaangażowani w opracowanie Krajowych Ocen Ryzyka za lata 2014 i 2016 oraz Oceny Ryzyka Bezpieczeństwa Narodowego za rok 2019.¹⁰¹ Rzeczywiście, niektóre dokumenty dotyczące oceny ryzyka wyraźnie określają je jako „grupy wyzwań”.¹⁰² Jednakże istniały również dowody na to, że niektóre z tych grup, takie jak Grupa Ekspertów ds. Nauk Behawioralnych, miały wąskie uprawnienia w zakresie zlecania i że jej członkowie mieli niewiele do powiedzenia na temat tego, co badali.¹⁰³ Sugerowałoby to, że mogły cierpieć na omówione już powyżej problemy zlecania w odniesieniu do naukowych grup doradczych. Niewiele było również dowodów sugerujących, że czerwone zespoły były regularnie używane w pełnym zakresie działań rządu Wielkiej Brytanii w zakresie gotowości na wypadek sytuacji kryzysowych, poza oceną ryzyka, lub w ogóle przez zdecentralizowane administracje. |
| 6.65. | Dochodzenie ma świadomość, że Ramy odporności rządu Wielkiej Brytanii od grudnia 2022 r. wyraził ambicję stworzenia procesu oceny ryzyka”który chętnie rzuca zewnętrzne wyzwania ze strony ekspertów, środowiska akademickiego, przemysłu i międzynarodowej społeczności zajmującej się ryzykiem” oraz że w aktualizacji wdrożenia z grudnia 2023 r. ogłoszono „systematyczny program doradztwa eksperckiego”, aby zapewnić konstruktywne wyzwanie w procesie oceny ryzyka ze strony „możliwie najszerszy zasób zewnętrznej wiedzy specjalistycznej.¹⁰⁴ Sugeruje to, że rząd Wielkiej Brytanii zidentyfikował problem wymagający rozwiązania. Jest to jednak nadal zbyt wąskie podejście, ograniczające się do oceny ryzyka, a nie innych aspektów gotowości na wypadek sytuacji kryzysowych, w szczególności strategii, planowania i zapewniania doradztwa. |
| 6.66. | Zespoły czerwone powinny być wykorzystywane znacznie częściej i systematycznie w rządowych strukturach doradczych i decyzyjnych w zakresie gotowości na wypadek sytuacji kryzysowych oraz przekazywania ich poglądów ministrom. W ten sposób ministrowie, a nie wewnętrzny konsensus, określą politykę gotowości, odporności i reagowania na sytuacje kryzysowe. Rządy i ich instytucje powinny być otwarte na potencjalnie niekonwencjonalne myślenie. Korzystanie z czerwonych zespołów powinno również stymulować zmianę kultury, ponieważ będzie wiadomo, że decyzje mogą wymagać uzasadnienia w ramach ćwiczenia „czerwonych zespołów”. Dostęp do szerokiego zakresu wysokiej jakości, konkurencyjnych porad oraz regularnego, zewnętrznego, niezależnego wkładu sprawi, że system będzie lepiej przygotowany do przygotowania się na pandemię i budowania odporności na nią w przyszłości¹⁰⁵ Czerwone zespoły powinny stać się integralną częścią architektury budowanie odporności w Wielkiej Brytanii. |
Zalecenie 9: Regularne używanie czerwonych drużyn
Rządy Wielkiej Brytanii, Szkocji, Walii i Irlandii Północnej powinny wprowadzić w służbie cywilnej wykorzystanie czerwonych zespołów w celu kontrolowania i kwestionowania zasad, dowodów, polityk i porad dotyczących gotowości i odporności na cywilne sytuacje kryzysowe w całym systemie. Czerwone drużyny należy sprowadzić spoza rządu i służby cywilnej.
Nowe podejście
| 6.67. | We wcześniejszych rozdziałach niniejszego Raportu ujawniono wiele powodów, dla których zawiodły systemy gotowości, odporności i reagowania rządu brytyjskiego i zdecentralizowanych administracji. Sposoby oceny ryzyka, opracowania strategii i udzielania porad były błędne. Instytucje, struktury i systemy Wielkiej Brytanii odpowiedzialne za gotowość i odporność były zbyt złożone i niewystarczająco ukierunkowane. Nie wzięto pod uwagę wniosków wyciągniętych z poprzednich epidemii i ćwiczeń, a działania nie zostały wdrożone. Zaangażowanie sektora wolontariatu w gotowość i odporność było zróżnicowane w całej Wielkiej Brytanii. Chociaż Walia wypadła pod tym względem lepiej niż gdziekolwiek indziej w Wielkiej Brytanii, ogólnie rzecz biorąc, zaangażowanie lokalnych organów i urzędników, takich jak dyrektorzy ds. zdrowia publicznego i grupy z sektora wolontariatu, w proces planowania było zbyt małe.106 |
| 6.68. | Nie było jednego, stałego organu, który byłby odpowiedzialny za identyfikację tych wad i „zgromadzenie masy krytycznej ludzi zaniepokojonych tym samym ogólnym problemem, jakim jest pandemia[S] … zapewnić wyzwanie, niezależność i przewidywanie systemowi”.107 |
| 6.69. | Z dochodzenia wynika, że konieczne jest zasadniczo nowe podejście do gotowości i odporności cywilnej na wypadek pandemii i całego systemu. |
Jedno forum dotyczące gotowości i odporności
| 6.70. | W dochodzeniu uznano, że rozwiązaniem wielu zidentyfikowanych problemów jest utworzenie jednego forum lub instytucji, która wyróżniałaby się na tle licznych eksperckich grup doradczych i zapewniałaby rządowi Wielkiej Brytanii i zdecentralizowanej administracji dostęp do skonsolidowanego zasobu doradztwa strategicznego, który jest rozumiane i kwestionowane w stosownych przypadkach. |
| 6.71. | To forum lub instytucja skupiałaby szerokie obszary wiedzy technicznej i specjalistycznej zaangażowane w przygotowanie Wielkiej Brytanii, jej instytucji i systemów na liczne i różnorodne wyzwania związane z pandemiami i sytuacjami kryzysowymi dla ludności w całym systemie. Zapewniłoby to w ten sposób spójne zrozumienie i analizę danego ryzyka, zakresu potencjalnych reakcji, opracowanie odpowiednich planów i ich skuteczną realizację. W raporcie okresowym niezależnego Stałego Komitetu ds. Gotowości na Pandemię powołanego przez rząd Szkocji jednym z kluczowych zaleceń było utworzenie Centrum Gotowości na Pandemię w Szkocji.108 Powinno to stanowić część przedsięwzięcia obejmującego całą Wielką Brytanię. |
| 6.72. | Jak profesor Whitty powiedział śledczym:
„Integracja różnych aspektów doradztwa technicznego jest jednym z bardziej złożonych w rządzie… Nie należy to jednak do kompetencji ani nie jest rolą [różni naukowcy] udzielanie porad w szerszych kwestiach społecznych, gospodarczych, fiskalnych i politycznych, które wybrani przywódcy polityczni muszą zachować równowagę.”109 Przyznał, że trudno jest być bardziej „rodnik”, chyba że cały system działałby razem, ale zdarzało się to tylko w sytuacjach awaryjnych – wtedy było już za późno.110 |
| 6.73. | Podczas reagowania na sytuację awaryjną firma SAGE była odpowiedzialna za „bardziej radykalne myślenie niż miało to miejsce pomiędzy sytuacjami kryzysowymi”, ale pomiędzy sytuacjami kryzysowymi nie było podmiotu, który rozważałby, czy zwracano się o właściwą poradę do właściwych źródeł lub co ta porada oznaczała w całości.111 System po prostu nie został zaprojektowany tak, aby „zaszczepić radykalizm„w politykę.112 Utworzenie Centrum Gotowości Pandemicznej przy Brytyjskiej Agencji Bezpieczeństwa Zdrowia nie rozwiązuje tych kwestii – skupia się jednak wyłącznie na systemie ochrony zdrowia.113 |
| 6.74. | Nowy organ mógłby być również odpowiedzialny za niezależną ocenę brytyjskiego systemu gotowości i odporności na sytuacje kryzysowe. Obecnie funkcjonuje w modelu samooceny. W rządzie Wielkiej Brytanii ani na zewnątrz niego nie istnieje organ centralny ani zdecentralizowane administracje odpowiedzialne za ocenę, czy spełnione są standardy gotowości i odporności (zob. Rozdział 2: System – instytucje, struktury i przywództwo). |
| 6.75. | Sekretariat ds. Zagrożeń Cywilnych podjął szeroki zakres działań mających na celu zrozumienie i zwiększenie gotowości.114 Odpowiadała za opracowanie wytycznych towarzyszących ustawie o nieprzewidzianych zdarzeniach cywilnych z 2004 r.115 Nie pełniła jednak roli równoważnej inspekcji lub innej ocenie zakresu gotowości i odporności.116 W rzeczywistości nie znała stanu gotowości i odporności departamentów rządu Wielkiej Brytanii. |
| 6.76. | Sekretariat ds. Zagrożeń Cywilnych wydał szereg dokumentów zawierających wytyczne dla lokalnych służb ratowniczych, w tym: Krajowe standardy odporności dla lokalnych forów dotyczących odporności i odpowiednich lokalnych organizacji reagujących, opublikowana po raz pierwszy w lipcu 2018 r. i zaktualizowana w grudniu 2019 r. i ponownie w sierpniu 2020 r.117 Jednakże przestrzeganie tych standardów było jedynie dobrowolne i niekompletne.118 Normy dotyczące konkretnie grypy pandemicznej zostały po raz pierwszy opublikowane dopiero w grudniu 2019 r.119 Było już dla nich za późno, aby wprowadzić jakąkolwiek praktyczną zmianę w zakresie gotowości i odporności na pandemię Covid-19. Normy nie były aktualizowane od sierpnia 2020 r. i nadal odnoszą się wyłącznie do grypy pandemicznej, a nie do pandemii bardziej ogólnie.120 |
| 6.77. | Po 2017 r. przerwano badanie National Resilience Capabilities Survey dla Anglii, ponieważ nie spełniło ono zamierzonego celu.121 Sekretariat ds. nieprzewidywalnych sytuacji cywilnych nie zastąpił go jednak wyraźnym następcą.122 Oznacza to, że wiedza rządu Wielkiej Brytanii ograniczała się zasadniczo do dobrowolnej samooceny lokalnych służb ratowniczych, niepotwierdzonych informacji i doświadczeń udostępnionych przez lokalne służby ratownicze w trakcie pracy z Sekretariatem ds. Zagrożeń Cywilnych oraz Wydziałem ds. Odporności i Sytuacji Nadzwyczajnych Ministerstwa Mieszkalnictwa, Społeczności i Samorząd Lokalny.123 |
| 6.78. | Podobny system samooceny oraz brak obowiązkowych standardów istniał w Szkocji, Walii i Irlandii Północnej, zarówno na szczeblu lokalnych służb ratowniczych, jak i na szczeblu rządu centralnego.124 W rzeczywistości zdecentralizowane administracje nie znały obiektywnie stanu swojej gotowości i odporności. Ani w Wielkiej Brytanii, ani w administracji zdecentralizowanej nie posiadał takich informacji żaden organ centralny. |
| 6.79. | Poseł Oliver Dowden, sekretarz parlamentarny w Kancelarii Rady Ministrów od stycznia 2018 r. do lipca 2019 r. i minister ds. Gabinetu od lipca 2019 r. do lutego 2020 r., powiedział w trakcie dochodzenia, że jednym z wyzwań stojących przed Gabinetem Rady Ministrów była wiedza „gdzie wytyczyć granicę pomiędzy pojedynczym departamentem rządowym a działaniami międzyrządowymi”.125 On dodał:
„To, co nie jest dla nas dobrym wykorzystaniem zasobów, to ciągłe zastanawianie się nad kwestiami, które są wyraźnie przydzielone poszczególnym departamentom rządowym.”126 |
| 6.80. | Ryzyka organizacji”zaznaczanie własnej pracy domowej” wynikały z uchybień w przygotowaniu, jak opisano w niniejszym Raporcie.127 Dla dochodzenia jasne jest, że samoocena była modelem nieadekwatnym. |
| 6.81. | Dochodzenie nie jest przekonane, czy system gotowości i odporności został w następstwie pandemii zreformowany lub czy jest w stanie samodzielnie przeprowadzić niezbędne reformy. Dzieje się tak z trzech powodów. |
| 6.82. | Po pierwsze, wiele osób – w tym osoby pełniące ważne role w systemie gotowości i odporności – albo nie było w stanie zidentyfikować i opisać wad w jednoznaczny sposób, albo opisało wady, które były oczywiste, ale w związku z którymi nie podjęto (w ogóle lub wystarczających) działań przed pandemia. W ramach dochodzenia przedstawiono szereg przykładów, a niektóre z nich omówiono wcześniej w niniejszym Raporcie:
|
| 6.83. | Taka niemożność – nawet po pandemii – jasnego wyrażenia tego, co się wydarzyło lub tego, co się nie wydarzyło, sugeruje dochodzeniu, że system zapewniania gotowości był i pozostaje poważnie nieodpowiedni. System albo jest nieświadomy, albo nie chce przyznać się do niektórych swoich wad. Problemami tymi należy się zająć – jeśli nie można ich właściwie zdefiniować, wyrazić i zaakceptować, nie można ich rozwiązać. |
| 6.84. | Po drugie, instytucje odpowiedzialne za gotowość i odporność opracowały znaczną liczbę wytycznych i dokumentów dotyczących planowania. Jednakże często były one obszerne, niezaktualizowane i zawierały odniesienia do mnóstwa innych obszernych dokumentów, które również nie zostały zaktualizowane:
|
| 6.85. | Sir Oliver Letwin powiedział śledczym, że im dłuższy dokument, tym mniej był przydatny. Jak to ujął: „Objętość jest zwykle odwrotnie proporcjonalna do skuteczności.”140 Zapytanie zgadza się. |
| 6.86. | Dwa ważne dokumenty powstałe po pandemii – dokument 2022 Ramy odporności rządu Wielkiej Brytanii i 2023 Brytyjska strategia bezpieczeństwa biologicznego – nie są pewni, w jaki sposób w przyszłości poprawi się gotowość i odporność. Rok 2022 Ramy odporności rządu Wielkiej Brytanii zobowiązał się – ale tylko w niejasnych słowach – rząd Wielkiej Brytanii do:
|
| 6.87. | Rok 2023 Brytyjska strategia bezpieczeństwa biologicznego zawiera żargon i język kierownictwa, który zbyt często przenika do tego rodzaju dokumentów rządowych. Jej język jest nieprzejrzysty i w niewielkim stopniu oświeca czytelnika. Jest on pełen odniesień do „zakres/zakres' (10 razy), 'ułatwiać/ułatwiać' (9 razy), 'rozwijający się' (26 razy) i 'dostarczać / dostarczać(29 razy).142 Na przykład w swoim „Plan wdrożenia strategii wysokiego szczebla", tam jest "zobowiązanie" Do:
„Określ zakres nowego, elastycznego mechanizmu zamówień publicznych do uruchomienia [nauka i technologia] ze środowiska akademickiego i przemysłu Wielkiej Brytanii, stosując uproszczone procesy w celu stymulowania innowacji.”143 Taki język raczej utrudnia komunikację niż oświeca czytelnika. |
| 6.88. | Język jest ważny i nie należy lekceważyć jego wpływu na gotowość i odporność. Dokumenty te powinny jasno określać, co się wydarzy i kiedy. W przeciwnym razie nie można ocenić, czy rząd osiągnął to, co założył. |
| 6.89. | Dokumenty powinny być jasne, precyzyjne i zwięzłe, aby umożliwić ich odczytanie i zrozumienie przez wszystkie osoby zaangażowane w gotowość i odporność. Jednym z zadań zapewnienia jest sprawdzenie, czy tak się dzieje. Brak uproszczenia i skonsolidowania dokumentów dotyczących planowania, wytycznych i strategii jest symptomatyczny dla podstawowego problemu instytucji w Wielkiej Brytanii, które zachowują odpowiedzialność za katastrofy cywilne obejmujące cały system. Świadczą o tym zarówno materiały dokumentacyjne, jak i dowody zawarte w dochodzeniu, opisane powyżej. |
| 6.90. | Sir Oliver Letwin powiedział w dochodzeniu, że nawet przepisanie tego rodzaju dokumentów nie wystarczy, aby ulepszyć system:
"[I]jeśli stanie się to bez dobrze zorganizowanego zespołu centralnego, pod przewodnictwem szefa ds. odporności, który ma bezpośredni dostęp do Premiera i jest równoległy do Doradcy ds. Bezpieczeństwa Narodowego, będzie to wysiłek zmarnowany, ponieważ rozproszy się na niekończące się konsultacje i komitety dookoła Whitehalla, a ćwiczenie polegające na uproszczeniu stanie się ćwiczeniem powodującym komplikacje.”144 |
| 6.91. | Po trzecie, żadna osoba ani organ – na szczeblu ministerialnym ani wśród urzędników i doradców – nie była odpowiedzialna za niezależną ocenę adekwatności, wydajności i skuteczności struktur decyzyjnych i doradczych w Wielkiej Brytanii, zadając pytanie, co wszyscy zrobili i czy robią właściwe rzeczy. |
| 6.92. | Nikt nie zadał pytania, czy są jakieś luki, czy przeprowadzono odpowiednią ocenę ryzyka lub opracowano skuteczną strategię, czy istnieje zbyt wiele długich i nieaktualnych dokumentów oraz, co najważniejsze, czy umiejętności, technologia i infrastruktura były wystarczające. wprowadzenie rozwiązania, które sprawiłoby, że rząd Wielkiej Brytanii i zdecentralizowane administracje byłyby praktycznie przygotowane na cywilną sytuację nadzwyczajną obejmującą cały system. W rezultacie nikt tak naprawdę nie znał z góry poziomu gotowości Wielkiej Brytanii ani odporności na tego rodzaju pandemię, która miała miejsce w styczniu 2020 r. |
Rola nowego ciała
| 6.93. | W dochodzeniu uznano, że jedyną odpowiedzią na rozległe problemy w podejściu rządu Wielkiej Brytanii i zdecentralizowanych administracji do gotowości i odporności jest utworzenie niezależnego organu posiadającego wiedzę fachową w zakresie cywilnych sytuacji kryzysowych obejmujących cały system. Rolą nowego organu będzie:
|
| 6.94. | Nowy organ, który będzie w stanie zgromadzić różne rodzaje porad dotyczących gotowości i odporności, pomoże przywódcom politycznym myśleć o rozwiązywaniu problemów w sposób strategiczny i długoterminowy. Przywódcy polityczni znajdują się w wyjątkowej sytuacji, jeśli chcą, aby wnieść krytyczne myślenie i świeże spojrzenie na problem, a także są dobrze przygotowani do zadawania trudnych pytań ekspertom w imieniu społeczeństwa, któremu służą.145 |
| 6.95. | Przed pandemią pytania te mogły obejmować na przykład: Jaka jest proporcjonalna reakcja na chorobę, która może zabić 100 członków populacji Wielkiej Brytanii? A co by było, gdyby było to 1000, 10 000, 100 000 lub 1 milion ludzi? Czy istnieje punkt zwrotny, w którym pewne interwencje niefarmaceutyczne stają się nieuniknione? Jeśli tak, jaki jest ten punkt krytyczny? Co się stanie, jeśli choroba dotyka tylko określonej części populacji? Czy istnieje moment, w którym skutki uboczne interwencji mogą nie być warte swojej ceny, ponieważ nie udaje się uratować wystarczającej liczby istnień ludzkich w porównaniu ze społecznymi i gospodarczymi kosztami interwencji? |
| 6.96. | To trudne pytania. W dochodzeniu nie uwzględniono przywódców politycznych w rządzie Wielkiej Brytanii, a zdecentralizowane administracje są obecnie odpowiednio poinformowane o tym, jak należy na nie odpowiedzieć w perspektywie długoterminowej. Granice obecnego systemu są jasne. |
| 6.97. | Profesor David Alexander i Bruce Mann, eksperci w dziedzinie zarządzania ryzykiem i odporności (zob Załącznik 1: Informacje o tym module i metodologia badania) zasugerował, że powinno istnieć „jednolity, zintegrowany i profesjonalny system ochrony ludności, zdolny zapewnić skuteczną reakcję całego systemu, całego społeczeństwa na sytuacje kryzysowe o katastrofalnej skali”.146 |
| 6.98. | W dochodzeniu zgodzono się z tym i uznano, że organ ten powinien doradzać ministrom w zakresie strategii długoterminowej w szeregu obszarów polityki istotnych dla gotowości i odporności. Powinno to połączyć się w celu zbudowania spójnego obrazu, który stawia decydentów w najlepszej możliwej pozycji, aby jasno widzieć dowody na poparcie i wykonalność polityki oraz stosować oceny wartościujące podczas podejmowania decyzji. |
| 6.99. | Powinien istnieć sposób, za pomocą którego osoby, które – jak można zasadnie przewidywać – zostaną zaangażowane w SAGE i inne grupy ekspertów na rzecz przyszłej pandemii – lub które brały udział w wybuchu choroby w przeszłości – będą mogły systematycznie dzielić się swoimi doświadczeniami oraz przemyśleć i przyczynić się do gotowości na wypadek pandemii jeszcze przed wystąpieniem sytuacji nadzwyczajnej. Można to następnie rozważyć w połączeniu z szerszą polityką dotyczącą gotowości na wypadek sytuacji nadzwyczajnych, taką jak strategia gospodarcza, wpływ na osoby bezbronne i praktyczne możliwości systemu. |
| 6.100. | W związku z tym dochodzenie zaleca utworzenie wyspecjalizowanego, niezależnego, obejmującego całą Wielką Brytanię organu ds. sytuacji kryzysowych dla ludności, zajmującego się zarówno gotowością, jak i odpornością, odpowiedzialnego przed ministrami odpowiedzialnymi za cywilne sytuacje kryzysowe w całym systemie. Nowy organ powinien zapewniać rządowi Wielkiej Brytanii i zdecentralizowanym administracjom specjalistyczne porady strategiczne dotyczące najlepszych sposobów przygotowania się na sytuacje nadzwyczajne dla ludności obejmujące cały system i budowania odporności na nie, a także potencjalnych reakcji. Umożliwi to władzom wykonawczym skupienie się na zapewnieniu infrastruktury umożliwiającej realizację planów w przypadku wystąpienia sytuacji nadzwyczajnej. |
| 6.101. | W dochodzeniu uznano, że nowy organ powinien zostać ustanowiony na mocy statutu i mieć uprawnienia obejmujące całą Wielką Brytanię, aby zapewnić mu niezależność. Ma to na celu umożliwienie jej wycofania się i przedstawienia przywódcom politycznym krytycznej, obiektywnej i bezstronnej opinii na temat stanu gotowości i odporności oraz możliwości jego poprawy. Przywódcy polityczni będą potrzebować odwagi, aby strategicznie myśleć o tym, jak najlepiej podejść do zagrożeń, przed którymi stanie Wielka Brytania w przyszłości. To nowe ciało miało im pomóc w tym dążeniu. |
| 6.102. | Organ powinien być sponsorowany wspólnie przez odpowiednich ministrów w rządzie Wielkiej Brytanii i każdą z zdecentralizowanych administracji, aby zapewnić mu uprawnienia i dostęp niezbędny do rozpatrywania kwestii w skali Wielkiej Brytanii. Każdy z tych ministrów powinien być uprawniony do zlecania nowemu organowi doradztwa w zakresie wszelkich aspektów planowania na wypadek sytuacji nadzwyczajnych, gotowości i odporności w ramach swoich kompetencji ministerialnych. W zarządzie nowego organu powinni także znajdować się dyrektorzy niewykonawczy reprezentujący każdy ze zdecentralizowanych krajów, a ich powołanie powinno wymagać zgody ministra-finansującego w odpowiedniej zdecentralizowanej administracji. W dochodzeniu wierzy się, że dzięki temu regularne myślenie strategiczne dotyczące gotowości i odporności na sytuacje kryzysowe cywilne znajdzie się w centrum rządu. |
| 6.103. | Wreszcie nowy organ mógłby pomóc w zapewnieniu konsultacji ze społeczeństwem, zaangażowania go i informowania go o tym, jak rządy zamierzają zareagować w przypadku sytuacji nadzwyczajnej. W wyniku sytuacji nadzwyczajnej obejmującej cały system oraz w wyniku reakcji na nią ucierpią obywatele. Jeśli społeczeństwo będzie lepiej poinformowane o ryzyku, a także o potencjalnych konsekwencjach braku jego ograniczenia, z większym prawdopodobieństwem zaakceptuje alokację cennych zasobów w ramach odpowiedniej „polisy ubezpieczeniowej”. |
| 6.104. | Większość społeczeństwa rozumie znaczenie obrony militarnej i bezpieczeństwa kraju. Doświadczywszy niszczycielskich konsekwencji pandemii Covid-19, powinni teraz również zrozumieć znaczenie budowania odporności i gotowości na cywilne sytuacje kryzysowe obejmujące cały system, w tym pandemie. Jak stwierdził profesor Vallance:
„Potrzebujesz armii w kraju, a nie odwracasz się po 20 latach i nie mówisz: „Co to była za strata pieniędzy, nie mieliśmy wojny”„.”147 Profesor Vallance uważał, że tak samo jest z bezpieczeństwem zdrowotnym. Zapytanie zgadza się. |
Zalecenie 10: Niezależny organ ustawowy działający w całej Wielkiej Brytanii zajmujący się gotowością i odpornością całego systemu na sytuacje kryzysowe
Rząd Wielkiej Brytanii powinien, w porozumieniu ze zdecentralizowanymi administracjami, utworzyć ustawowy niezależny organ odpowiedzialny za gotowość i odporność cywilną całego systemu na wypadek sytuacji kryzysowych.
Nowemu organowi należy powierzyć odpowiedzialność za:
- zapewnianie niezależnych, strategicznych porad rządowi Wielkiej Brytanii i zdecentralizowanym administracjom w zakresie planowania, gotowości i budowania odporności na sytuacje kryzysowe cywilne obejmujące cały system;
- konsultacje z sektorem wolontariatu, społeczności i przedsiębiorstw społecznych na poziomie krajowym i lokalnym oraz dyrektorami ds. zdrowia publicznego w sprawie ochrony osób bezbronnych w sytuacjach kryzysowych obejmujących cały system;
- ocena stanu planowania, gotowości i odporności na sytuacje kryzysowe cywilne obejmujące cały system w Wielkiej Brytanii; I
- formułowanie zaleceń dotyczących zdolności i zdolności, które będą wymagane w celu przygotowania się na sytuacje nadzwyczajne cywilne obejmujące cały system i budowania odporności na nie.
Jako środek tymczasowy należy ustanowić nowy organ na zasadach nieustawowych w ciągu 12 miesięcy od wydania niniejszego sprawozdania, aby mógł rozpocząć pracę przed przyjęciem przepisów.
- Widzieć Oliver Letwin 20 czerwca 2023 8/20-24; Michael Gove 13 lipca 2023 r. 114/18-19
- Michael Gove 13 lipca 2023 r. 114/19-25
- Oliver Letwin 20 czerwca 2023 10.12-13.11
- Oliver Letwin 20 czerwca 2023 15.13-21
- Denis McMahon 6 lipca 2023 r. 103/6-13
- Mark Walport 21 czerwca 2023 r., 10/1–21
- INQ000147810_0008 ust. 22; Zobacz też Patrick Vallance 22 czerwca 2023 137/20-21
- INQ000147810_0008 ust. 22; Patrick Vallance 22 czerwca 2023 137/22-138/1
- INQ000147810_0008 ust. 22; Patrick Vallance 22 czerwca 2023 138/2-8
- INQ000147810_0008 ust. 22; Patrick Vallance 22 czerwca 2023 138/9-11
- Patricka Vallance’a 22 czerwca 2023 138/11-13
- INQ000147707_0033 pkt 86, 88
- INQ000184638_0011-0012 ust. 2.12
- INQ000147810_0005 ust. 12
- INQ000148419_0007 ust. 3.17
- INQ000183413_0003 ust. 8
- INQ000184636_0009-0010
- INQ000184851_0008 ust. 28
- Mark Walport 21 czerwca 2023 r. 20/25–21/22
- Patrick Vallance 22 czerwca 2023 136/23-137/3; Jim McMenamin 22 czerwca 2023 193/14-18
- INQ000119020_0008 ust. 28
- INQ000119020_0008 ust. 28
- INQ000119020_0008 ust. 31
- INQ000142125_0005
- INQ000207293_0005 ust. 2.7
- Christopher Whitty 22 czerwca 2023 r. 21.72-73.10
- Christopher Whitty, 22 czerwca 2023 r., 73.11-24; Patrick Vallance 22 czerwca 2023 139/2-19
- INQ000119020_0009 ust. 33
- INQ000147810_0005 ust. 11
- INQ000184851_0004, 0019 pkt 13-14, 80; INQ000148419_0005, 0007 pkt 3.11-3.12, 3.17
- INQ000184851_0019 paragraf 80
- INQ000148419_0007 ust. 3.17; INQ000119020_0007 ust. 24; INQ000184851_0011-0012 ust. 45
- Mark Walport 21 czerwca 2023 r. 21/7–22
- INQ000062443_0004 ust. 24
- Christopher Whitty 22 czerwca 2023 r. 89.18-90.17
- INQ000184638_0026 ust. 3.50
- INQ000184637_0010, 0011 pkt 7.6-7.7, 7.12; Sally Davies 20 czerwca 2023 168/20-169/9
- INQ000184637_0010 ust. 7.7; Zobacz też INQ000148419_0010, 0013 pkt 4.4 lit. f), 5.8
- INQ000148419_0010, 0013 pkt 4.4 lit. f), 5.8
- INQ000147707_0033 paragraf 88
- INQ000147810_0033-0034 ust. 105
- Patrick Vallance 22 czerwca 2023 151/5-9
- Patrick Vallance 22 czerwca 2023 151/16-152/2; Zobacz też INQ000148419_0010 paragraf 4.4(f)
- Kodeks postępowania dla naukowych komitetów i rad doradczych: CoPSAC 2021, Rządowe Biuro ds. Nauki, aktualizacja 14 grudnia 2021 r., sekcja 2.4.1 (https://www.gov.uk/government/publications/scientific-advisory-committees-code-of-practice/code-of-practice-for-scientific-advisory-committees-and-councils-copsac-2021; INQ000101646)
- Jimmy Whitworth 14 czerwca 2023 r. 137/12-20
- INQ000147710_0011 ust. 9.6
- INQ000147710_0011 ust. 9.6
- INQ000184851_0014 ust. 57
- INQ000119020_0005 ust. 17
- INQ000184851_0015 paragraf 60
- INQ000184851_0015 paragraf 60
- INQ000119020_0007 ust. 24
- Jimmy Whitworth 14 czerwca 2023 137/23-138/1
- INQ000207293_0004 ust. 2.6
- Jimmy Whitworth 14 czerwca 2023 r. 138/2-4
- Jimmy Whitworth 14 czerwca 2023 r. 138/5-6
- INQ000196611_0021 ust. 48
- Christopher Whitty 22 czerwca 2023 81.13-15
- INQ000184851_0016 paragraf 63
- INQ000099517_0010 ust. 2.22
- Kodeks postępowania dla naukowych komitetów i rad doradczych: CoPSAC 2021, Rządowe Biuro ds. Nauki, aktualizacja 14 grudnia 2021 r., sekcja 2.4.1 (https://www.gov.uk/government/publications/scientific-advisory-committees-code-of-practice/kodeks postępowania dla komitetów-doradczych-naukowych-i-rad-copsac-2021; INQ000101646)
- Christopher Whitty 22 czerwca 2023 83/8-13
- Christopher Whitty 22 czerwca 2023 117/10-16
- David Cameron 19 czerwca 2023 23.07, 22.03., 56.02; Clara Swinson 19 czerwca 2023 166/25-168/16; Oliver Letwin 20 czerwca 2023 17.11-36.01; INQ000177810_0003, 0014 pkt 8, 47-48; George Osborne 20 czerwca 2023 r. 67/18–25; Sally Davies 20 czerwca 2023 146/8-18, 157/2-9; Jeremy Hunt 21 czerwca 2023 165/22-170/1; INQ000177796_0007-0009, 0015 pkt 25–29, 38, 70; Christopher Whitty 22 czerwca 2023 77/5-21; Rosemary Gallagher 26 czerwca 2023 71/9-20; Richard Horton 13 lipca 2023 68.19-69.12, 88.13-25; INQ000148421_0002 ust. 5; INQ000187305_0008, 0013 pkt 39, 65, 69
- INQ000148406_0014 ust. 21; Mark Walport 21 czerwca 2023 r. 24.03.-25.02; INQ000147810_0020-0023 pkt 63–72; Michael Gove 13 lipca 2023 r. 116/13-117/10
- Jenny Harries 26 czerwca 2023 169/4-21; Claas Kirchhelle 10 lipca 2023 100/12-102/14
- Brytyjska strategia bezpieczeństwa biologicznego, rząd Jej Królewskiej Mości, lipiec 2018 r., s. 15 (https://assets.publishing.service.gov.uk/media/5b5b3ce5e5274a3fe478c3bf/2018_UK_Biological_Security_Strategy.pdf; INQ000142130); Mark Walport 21 czerwca 2023 r. 61/4-62/18
- Brytyjska strategia bezpieczeństwa biologicznego, rząd Jej Królewskiej Mości, lipiec 2018 r., s. 13 (https://assets.publishing.service.gov.uk/media/5b5b3ce5e5274a3fe478c3bf/2018_UK_Biological_Security_Strategy.pdf; INQ000142130)
- Brytyjska strategia bezpieczeństwa biologicznego, rząd Jej Królewskiej Mości, lipiec 2018 r., s. 7, 26 (https://assets.publishing.service.gov.uk/media/5b5b3ce5e5274a3fe478c3bf/2018_UK_Biological_Security_Strategy.pdf; INQ000142130)
- Jimmy Whitworth 14 czerwca 2023 r. 128/8–15
- Globalny indeks bezpieczeństwa zdrowotnego: budowanie zbiorowych działań i odpowiedzialności, inicjatywa na rzecz zagrożenia nuklearnego/Johns Hopkins Bloomberg School of Public Health, 2019 (https://www.nti.org/analysis/articles/global-health-security-index/; INQ000149103). Wielka Brytania gorzej wypadła w innych kategoriach Globalnego Indeksu Bezpieczeństwa Zdrowia. Na przykład zajął 11. miejsce w kategorii „Wystarczający i solidny system opieki zdrowotnej do leczenia chorych i ochrony pracowników służby zdrowia” oraz 26. w kategorii „Ogólne ryzyko środowiskowe i podatność kraju na zagrożenia biologiczne”.
- INQ000182616_0003 ust. 8
- Matt Hancock 27 czerwca 2023 17.19-19
- INQ000181825_0006-0008 pkt 23-30
- INQ000181825_0008 ust. 32
- INQ000181825_0008 ust. 32
- Duncan Selbie 27 czerwca 2023 136/15-137/5; Zobacz też INQ000184639_0016 pkt 5.4-5.5
- INQ000090333_0001 ust. 1
- Michael Gove 13 lipca 2023 r. 113/21-116/12
- Jeremy Hunt 21 czerwca 2023 166/18-167/2
- Jeremy Hunt 21 czerwca 2023 146/18-147/1
- Jeremy Hunt 21 czerwca 2023 149/11
- Jeremy Hunt 21 czerwca 2023 r. 147/8-12
- Jeremy Hunt 21 czerwca 2023 r. 147/16-25
- Jeremy Hunt 21 czerwca 2023 r. 148/1-24
- INQ000147810_0026 paragraf 78
- INQ000184643_0029, 0049-0050 pkt 151, 265; INQ000184638_0016, 0032 ust. 3.10, 3.78; Christopher Whitty 22 czerwca 2023 89/3-14
- INQ000147810_0026 ust. 80; INQ000184639_0019 ust. 6.5
- INQ000184639_0019 ust. 6.5
- Michael Gove 13 lipca 2023 r. 137/11-16
- Jeremy Hunt 21 czerwca 2023 r. 180/6-12
- David Cameron 19 czerwca 2023 r. 21.01-22.09; INQ000177810_0003, 0014 pkt 9, 47; Oliver Letwin 20 czerwca 2023 22.13-14.01, 33.21-36.1; INQ000177796_0015-0016 ust. 70; Jeremy Hunt, 21 czerwca 2023 r., 176/9-14; Christopher Whitty 22 czerwca 2023 88/9-20; Matt Hancock 27 czerwca 2023 88/10-13; Jeremy Farrar 29 czerwca 2023 r. 14.14–18.07; Michael Gove 13 lipca 2023 r. 116/13-117/10; INQ000148402_0019 ust. 80; INQ000099516_0046 ust. 190; INQ000185337_0041-0042 pkt 171–172
- INQ000372823_0014 ust. 1.3
- Zobacz ogólnie INQ000068403_0063 ust. 7.2.2; INQ000372823_0013-0019 pkt 1.1-1.16
- „Myślenie grupowe” jest jednym z przykładów błędu poznawczego, który można opisać bardziej ogólnie jako „systematyczny błąd w myśleniu, który pojawia się, gdy jednostki (i zespoły) szukają, przetwarzają i interpretują informacje, i który wpływa na decyzje i osądy podejmowane na podstawie podstawie tych informacji” (INQ000372823_0018-0019 pkt 1.15).
- Oliver Letwin 20 czerwca 2023 33.21-34.12
- Widzieć INQ000068403_0063, pkt 7.2.2; INQ000372823_0015 ust. 1.5
- INQ000068403_0063, pkt 7.2.2; INQ000372823_0071 pkt 7.5-7.6
- Pierwsze wydanie ukazało się w lutym 2010 r., drugie wydanie w marcu 2013 r., a najnowsze, trzecie wydanie ukazało się w październiku 2021 r. (zob. INQ000372823).
- Blackett Review of High Impact Low Probability Risks, Rządowe Biuro ds. Nauki, 2011, s. 11 (https://assets.publishing.service. gov.uk/media/5a7c901540f0b62aff6c28c0/12-519-blackett-review-high-impact-low-probability-risks.pdf; INQ000055868)
- INQ000147777_0010; INQ000147769_0006; INQ000147768_0005-0006; INQ000147770_0005-0006
- INQ000147769_0006
- INQ000148418_0014 ust. 2.40
- Ramy odporności rządu Wielkiej Brytanii, Rząd Jej Królewskiej Mości, grudzień 2022 r., pkt 20 (https://assets.publishing.service.gov.uk/media/63cff056e90e071ba7b41d54/UKG_Resilience_Framework_FINAL_v2.pdf; INQ000097685); Ramy dotyczące odporności rządu Wielkiej Brytanii: aktualizacja wdrożenia z 2023 r., Gabinet Rady Ministrów, 4 grudnia 2023 r. (https://assets.publishing.service.gov.uk/media/656def711104cf0013fa7498/The_UK_Government_Resilience_Framework_2023_Implementation_Update.pdf; INQ000372824)
- INQ000177810_0003 pkt 8-9
- W sprawie braku uznania i zrozumienia potencjalnego znaczenia i roli lokalnych pracowników zdrowia publicznego, w szczególności dyrektorów ds. zdrowia publicznego, zarówno przed, jak i we wczesnym reagowaniu na pandemię Covid-19, zob.: INQ000183419_0017, 0019, 0021, 0040-0041 pkt 107–109, 118, 125–126, 223–230 i J.im McManus 5 lipca 2023 r. 55/12-59/9. W Anglii jest około 150 dyrektorów ds. zdrowia publicznego zatrudnionych przez władze lokalne. W Szkocji zarządy NHS zatrudniają ośmiu dyrektorów ds. zdrowia publicznego. W Walii jest siedmiu dyrektorów ds. zdrowia publicznego zatrudnionych przez lokalne rady ds. zdrowia. W Irlandii Północnej jest tylko jeden dyrektor ds. zdrowia publicznego, który jest zatrudniony przez Agencję Zdrowia Publicznego (patrz Jim McManus 5 lipca 2023 r. 36.16-38.09). Na temat ogólnego braku uznania i zrozumienia potencjalnego znaczenia i roli sektora wolontariatu zob INQ000182613_0018 ust. 64; Kevin Fenton 5 lipca 2023 r. 89.21-90.25. Dla Walii, zobacz INQ000066503_0013-0014 ust. 10–17; INQ000130469_0100-0101 pkt 394–397.
- Patrick Vallance 22 czerwca 2023 151/5-9
- INQ000103004_0004 p2
- INQ000184638_0027-0028 pkt 3.56, 3.59
- Christopher Whitty 22 czerwca 2023 63.11-17
- Christopher Whitty 22 czerwca 2023 63.15-17, 81.24-82.3
- Christopher Whitty 22 czerwca 2023 77/5-9
- INQ000148429_0159-0160 pkt 638–639
- INQ000182612_0007 ust. 2.10
- INQ000145912_0042-0044 pkt 8.27-8.33
- INQ000145733_0007 ust. 2.19; INQ000182612_0007 ust. 2.10; INQ000148402_0014 ust. 56
- INQ000022975; INQ000047333; INQ000023122; zobacz ogólnie INQ000182612_0053-0055 pkt 4.72–4.81; INQ000203349_0082-0084 pkt 215-220
- INQ000203349_0084-0085 pkt 221–223
- Widzieć Katharine Hammond 16 czerwca 2023 131/25-135/7
- INQ000023122_0034–0035
- INQ000203349_0087 pkt 230–234; INQ000188715_0005 ust. 7–9; INQ000188716_0004-0006 pkt 13-17
- Katharine Hammond 16 czerwca 2023 137/16-138/14
- Zob. na przykład raport z przeglądu po wdrożeniu ustawy Civil Contingency Act (2004) (Planowanie awaryjne) Regulacje z 2005 r., HM Government, s. 7–8, marzec 2017 r., pkt 15, 19 (https://assets.publishing.service.gov.uk/media/5a82c15340f0b6230269c879/post_implementation_review_civil_contingencies_act__print.pdf; INQ000056230); INQ000182612_0037 ust. 4.14
- Zobacz dla Anglii, Szkocji i Walii: INQ000203349_0082-0095 pkt 214–251; oraz dla Irlandii Północnej: Denis McMahon 6 lipca 2023 r. 16.07-20.16
- Oliver Dowden 21 czerwca 2023 119/6-8
- Oliver Dowden 21 czerwca 2023 121/22-25. Zobacz także dowody Rogera Hargreavesa, że jest to złożona kwestia oceny, której nie można znaleźć w samej „doktrynie”: INQ000182612_0008-0010 pkt 2.12-2.18.
- INQ000203349_0093 paragraf 247(f)
- Emma Reed 26 czerwca 2023 40/24-41/2, 41/11-42/9
- Christopher Wormald 19 czerwca 2023 127/19-21
- INQ000184638_0033 ust. 4.1; INQ000023131_0005
- Caroline Lamb 28 czerwca 2023 118/17-22
- Andrew Goodall 3 lipca 2023 r., 24.03-95.16; Andrew Goodall 4 lipca 2023 38.25-40.25, 42.3-43.17
- Andrew Goodall 3 lipca 2023 r., 24.03-95.16; Andrew Goodall 4 lipca 2023 38.25-40.25, 42.3-43.17
- INQ000047302_0002 ust. 3
- Katharine Hammond 16 czerwca 2023 84/11-85/8
- 136 Katharine Hammond 16 czerwca 2023 104/9-108/16, 117/15-118/10; Koncepcja Operacyjna, Gabinet Rady Ministrów, aktualizacja: kwiecień 2013 r. (https://assets.publishing.service.gov.uk/media/5a7a44b0ed915d1fb3cd6a5f/CONOPs_incl_revised_chapter_24_Apr-13.pdf; INQ000036475); INQ000055887
- Jim McMenamin 22 czerwca 2023 181/16-21; INQ000101052; INQ000148759; Caroline Lamb 28 czerwca 2023 118/17-22; Jeane Freeman 28 czerwca 2023 r. 135/25-136/5
- INQ000089575; Quentin Sandifer 4 lipca 2023 r. 96/4-8
- Wytyczne dotyczące gotowości i reagowania na pandemię grypy w Irlandii Północnej, Departament Zdrowia, Opieki Społecznej i Bezpieczeństwa Publicznego, styczeń 2013 r. (http://www.niassembly.gov.uk/globalassets/documents/raise/deposited-papers/2013/dp1089.pdf; INQ000183431); INQ000188750
- Oliver Letwin 20 czerwca 2023 36/5-6
- Ramy odporności rządu Wielkiej Brytanii, Rząd Jej Królewskiej Mości, grudzień 2022 r., pkt 98–100 (https://www.gov.uk/government/publications/the-uk-government-resilience-framework; INQ000097685)
- Zob. na przykład brytyjska strategia bezpieczeństwa biologicznego, rząd Jej Królewskiej Mości, czerwiec 2023 r., s. 31, 46, 54, pkt 41, 86, 107 (https://assets.publishing.service.gov.uk/media/64c0ded51e10bf000e17ceba/UK_Biological_Security_Strategy.pdf; INQ000208910)
- Brytyjska strategia bezpieczeństwa biologicznego, rząd Jej Królewskiej Mości, czerwiec 2023 r., s. 10 (https://assets.publishing.service.gov.uk/media/64c0ded51e10bf000e17ceba/UK_Biological_Security_Strategy.pdf; INQ000208910)
- Oliver Letwin 20 czerwca 2023 38.22-39.04
- Zobacz Oliver Letwin 20 czerwca 2023 15/13-21
- INQ000203349_0097 paragraf 256
- Patrick Vallance 22 czerwca 2023 r. 159/21-24
Załącznik 1: Kontekst tego modułu i metodologia badania
Tło
| A1.1. | Wielmożny poseł Boris Johnson, premier od lipca 2019 r. do września 2022 r., formalnie powołał brytyjskie dochodzenie w sprawie Covid-19 w czerwcu 2022 r. w celu zbadania przygotowań do pandemii koronawirusa (Covid-19) i reakcji na nią w Wielkiej Brytanii oraz wyciągnięcia wniosków dla przyszłość. W grudniu 2021 r. na Przewodniczącą Sądu Apelacyjnego mianował Wielmożną Baronową Hallett DBE, emerytowaną sędzię Sądu Apelacyjnego. |
| A1.2. | Wiosną 2022 r. w ramach dochodzenia przeprowadzono konsultacje społeczne w sprawie projektu zakresu zadań. Zespół dochodzenia spotkał się z ponad 150 rodzinami pogrążonymi w żałobie w całej Wielkiej Brytanii oraz przedstawicielami wielu różnych sektorów, takich jak organizacje charytatywne, związki zawodowe, grupy wyznaniowe, edukacja i opieka zdrowotna. W sumie otrzymano ponad 20 000 odpowiedzi. Informacje te ukształtowały zalecenia baronowej Hallett skierowane do premiera w sprawie zakresu zadań. |
| A1.3. | W dniu 28 czerwca 2022 r. Premier wydał ostateczny Regulamin Dochodzenia, ustalając go na podstawie ustawy o zapytaniach z 2005 r.1 |
| A1.4. | Dochodzenie formalnie wszczęto w dniu 21 lipca 2022 r. w celu „zbadanie, rozważenie i złożenie sprawozdania na temat przygotowań i reakcji na pandemię w Anglii, Walii, Szkocji i Irlandii Północnej, do formalnej daty rozpoczęcia dochodzenia włącznie, czyli do dnia 28 czerwca 2022 r.”.2 Pełny zakres obowiązków obejmuje:
„1. Zbadaj reakcję na COVID-19 i wpływ pandemii w Anglii, Walii, Szkocji i Irlandii Północnej oraz sporządź rzeczową relację, w tym:
|
| A1.5. | Dochodzenie bada sposób postępowania z pandemią w Anglii, Walii, Szkocji i Irlandii Północnej, co obejmuje kwestie zastrzeżone i zdecentralizowane. W Szkocji prowadzone jest odrębne dochodzenie, w ramach którego ocenione zostaną obszary, w których polityka została przekazana rządowi Szkocji, zgodnie z jego zakresem zadań. Zapytanie brytyjskie współpracuje z zapytaniem szkockim, aby tam, gdzie to możliwe, uniknąć powielania pracy. |
| A1.6. | Aby zapewnić pełne i ukierunkowane badanie szerokiego zakresu zagadnień objętych zakresem zadań oraz sporządzać regularne raporty, dochodzenie w ramach Dochodzenia zostało podzielone na sekcje lub „moduły”. Moduły są ogłaszane, a następnie kolejno otwierane, po czym rozpoczyna się gromadzenie materiału dowodowego i rozpatrywanie wniosków Uczestników Podstawowych. W każdym module odbywają się rozprawy wstępne (na których zapadają decyzje dotyczące trybu przeprowadzania przesłuchań publicznych) oraz przesłuchania publiczne pełne, podczas których przeprowadzane są dowody. Szczegóły przesłuchań publicznych publikowane są w Inkwizycji.4 |
| A1.7. | Aktualnie aktywne moduły Zapytania to:
Wszelkie dalsze dochodzenia zostaną ogłoszone w odpowiednim czasie przez Dochodzenie. |
| A1.8. | Jak określono w Zakresie obowiązków, Zapytanie uważa również, że niezwykle istotne w jego pracy jest wysłuchanie i uważne rozważenie doświadczeń rodzin pogrążonych w żałobie i innych osób, które doświadczyły trudności lub strat w wyniku pandemii. Dochodzenie będzie to robić na wiele różnych sposobów, w tym poprzez „ćwiczenie ze słuchania” „Każda historia ma znaczenie”.15 Osoby, które ukończyły 18 rok życia, proszone są o podzielenie się tak dużą lub małą ilością informacji, jak tylko mogą, bez konieczności składania zeznań lub uczestniczenia w przesłuchaniu publicznym. Dzielenie się doświadczeniami z Zapytaniem pomoże w zrozumieniu wydarzeń i ich wpływu oraz w opracowaniu zaleceń, które mogłyby zmniejszyć cierpienie w przyszłości. Doświadczenia zdobyte w ramach dochodzenia zostaną przeanalizowane i opracowane zostaną raporty podkreślające wyłaniające się tematy. Inquiry realizuje również dostosowany do indywidualnych potrzeb i ukierunkowany projekt badawczy, wysłuchując bezpośrednio niektórych dzieci i młodych ludzi najbardziej dotkniętych pandemią, aby pomóc w sformułowaniu wniosków i zaleceń.16 |
Moduł 1
| A1.9. | Niniejsze sprawozdanie dotyczy modułu 1, którego otwarcie nastąpiło 21 lipca 2022 r. i w którym w ramach dochodzenia zbadano kwestie gotowości i odporności. Celem Modułu 1 była ocena, czy istniało odpowiednie planowanie na wypadek pandemii i odporność na pandemię. Zbadano cały system sytuacji kryzysowych, w tym zasoby, zarządzanie ryzykiem i gotowość na wypadek pandemii. |
| A1.10. | Jak określono w Zarysie zakresu, w module 1 uwzględniono:
|
| A1.11. | Moduł 1 skupiał się przede wszystkim, choć nie wyłącznie, na okresie od 11 czerwca 2009 r. do 21 stycznia 2020 r., jak określono w Liście zagadnień.18 Podsumowując, zbadane kwestie dotyczyły:
|
| A1.12. | Zgodnie z zasadą 5 Regulaminu ankiety z 2006 r. i Protokołem głównego uczestnika ankiety, Przewodniczący wyznacza w każdym module pewną liczbę głównych uczestników – osób, organizacji lub instytucji o określonych zainteresowaniach.19 Uczestnicy główni mają zwiększone prawa w procesie dochodzenia, w tym do otrzymywania ujawnień dokumentów, bycia reprezentowanym, składania oświadczeń prawnych i sugerowania kierunków dochodzenia. Mogą również ubiegać się o dofinansowanie na pokrycie kosztów prawnych i innych kosztów. W ramach Modułu 1 do Zapytania wpłynęło ponad 100 wniosków o nadanie statusu Uczestnika Podstawowego, a Przewodniczący wyznaczył 28 Uczestników Podstawowych. |
| Nazwa organizacji/osoby | Uznany przedstawiciel prawny (w momencie publikacji) | Data wyznaczenia |
|---|---|---|
| Stowarzyszenie Dyrektorów Zdrowia Publicznego | Henry Bermingham (ciężarowcy) | 7 września 2022 r |
| Kanclerz Księstwa Lancaster | Sharanjeet Sidhu (rządowy departament prawny) | 7 września 2022 r |
| Rodziny pogrążone w żałobie w związku z Covid-19 na rzecz sprawiedliwości Cymru | Craig Court (Harding Evans) | 7 września 2022 r |
| Rodziny pogrążone w żałobie w związku z Covid-19 w imię sprawiedliwości | Elkan Abrahamson (Broudie Jackson Canter) | 7 września 2022 r |
| Departament Biznesu i Handlu (dawniej Departament Biznesu, Energii i Strategii Przemysłowej) | Rebecca Torsello (rządowy dział prawny) | 7 września 2022 r |
| Sekretarz stanu ds. zdrowia i opieki społecznej | Sarah Wise (rządowy dział prawny) | 7 września 2022 r |
| Biuro Wykonawcze Irlandii Północnej | Joan MacElhatton (wydziałowe biuro radcy prawnego) | 7 września 2022 r |
| Rządowe Biuro ds. Nauki | Amir Mughal (rządowy departament prawny) | 7 września 2022 r |
| Skarb Państwa | Michael Cockings (rządowy departament prawny) | 7 września 2022 r |
| Imperial College w Londynie | Paul Ridge (Bindmans) | 7 września 2022 r |
| Stowarzyszenie Samorządowe | Thelma Stober (Stowarzyszenie Samorządów Lokalnych) | 7 września 2022 r |
| Krajowa Rada Komendantów Policji | Sarah Winfield (Dyrekcja Usług Prawnych MPS) | 7 września 2022 r |
| Departament Zdrowia (Irlandia Północna) | Sara Erwin (wydziałowa kancelaria prawna) | 7 września 2022 r |
| NHS Anglia | Alistair Robertson (DAC Beachcroft) | 7 września 2022 r |
| Służby Narodowe NHS w Szkocji | Morag Shepherd (NHS National Services Scotland) | 7 września 2022 r |
| Irlandia Północna Rodziny pogrążone w żałobie w związku z Covid-19 na rzecz sprawiedliwości | Conal McGarrity (PA Duffy & Co) | 7 września 2022 r |
| Gabinet Naczelnego Lekarza | Warrick Olsen (rządowy departament prawny) | 7 września 2022 r |
| Zdrowie Publiczne w Szkocji | Stefano Rinaldi (Centralne Biuro Prawne) | 7 września 2022 r |
| Zdrowie publiczne Walia | Paul Veysey (NHS Wales Partnerstwo ds. usług wspólnych, dział prawny i usługi związane z ryzykiem) | 7 września 2022 r |
| Szkocki Covid pogrążony w żałobie | Aamer Anwar (Aamer Anwar & Co) | 7 września 2022 r |
| Szkoccy ministrowie | Caroline Beattie (Dyrekcja Prawna Rządu Szkocji) | 7 września 2022 r |
| Sekretarz stanu ds. środowiska, żywności i spraw wiejskich | Luke Chattaway (rządowy dział prawny) | 7 września 2022 r |
| Sekretarz stanu w Departamencie Spraw Wewnętrznych | Warrick Olsen (rządowy departament prawny) | 7 września 2022 r |
| Brytyjska Agencja Bezpieczeństwa Zdrowia | Katrina McCrory (Mills i Reeve) | 7 września 2022 r |
| Rząd walijski | Stephanie McGarry jako Browne Jacobson | 7 września 2022 r |
| Walijskie Stowarzyszenie Samorządów Lokalnych | Thelma Stober (Stowarzyszenie Samorządów Lokalnych) | 7 września 2022 r |
| Brytyjskie Stowarzyszenie Medyczne | Brian Stanton (prawo Innovo) | 28 września 2022 r |
| Kongres Związków Zawodowych | Harry Thompson (radcy prawni Thompsons) | 28 września 2022 r |
| A1.13. | Zgodnie z jego publicznym charakterem i zobowiązaniem przewodniczącego do prowadzenia dochodzenia w sposób jak najbardziej otwarty i przejrzysty, poczyniono ustalenia, aby przesłuchania były dostępne dla wszystkich, którzy chcieli w nich uczestniczyć. Przesłuchania były transmitowane na żywo w witrynie internetowej Inquiry lub na jego kanale YouTube (gdzie są one dostępne), a obywatele mogli osobiście oglądać przesłuchania.20 |
| A1.14. | Podejście Dochodzenia do dokumentów zostało określone w Protokole w sprawie dokumentów, który wyjaśnia kluczowe zasady dostarczania dokumentów do Dochodzenia, w tym wnioski o dokumenty lub zeznania świadków zgodnie z zasadą 9 Regulaminu dochodzeń z 2006 r.21 Należy to czytać wraz z Protokołem Zapytania w sprawie redagowania dokumentów, który szczegółowo opisuje podejście do redagowania dokumentów zarówno w celu ujawnienia Głównym Uczestnikom, jak i publikacji.22 W ramach tego modułu Śledztwo wystosowało ponad 200 wniosków dowodowych. Otrzymała i rozpatrzyła ponad 200 zeznań świadków i 100 000 dokumentów zawierających ponad 1 milion stron. Spośród tych dokumentów ponad 18 000 zostało ujawnionych głównym uczestnikom. Odpowiednie materiały są publikowane na stronie internetowej Zapytania.23 |
| A1.15. | Zgodnie z art. 18 ustawy o dochodzeniach z 2005 r. Przewodniczący podejmuje uzasadnione kroki w celu zapewnienia obywatelom możliwości wglądu do dokumentów dostarczonych w związku z dochodzeniem i uczestniczenia w przesłuchaniach w ramach dochodzenia.24 Wszystkie zeznania świadków i dokumenty stanowiące dowód w toku przesłuchań zostały opublikowane na stronie internetowej Prokuratury.25 Mogą jednak zaistnieć przypadki, w których dowody (lub ich części) dostarczone na potrzeby dochodzenia powinny zostać wyłączone z publicznego ujawnienia w celu ochrony przed ryzykiem wyrządzenia szkody i wyrządzenia szkody interesowi publicznemu. Co do zasady Dochodzenie ujawnia Uczestnikom Głównym wszystkie zeznania świadków i dokumenty, które uzna za istotne i do których nie mają zastosowania ograniczenia, przed przesłuchaniami publicznymi Dochodzenia. Dokumenty wykorzystane podczas przesłuchań publicznych Dochodzenia lub w inny sposób złożone w dowodach zostaną opublikowane na stronie internetowej Dochodzenia.26 W przypadku istnienia uzasadnionego powodu sprzeciwu wobec ujawnienia lub publikacji takich odpowiednich materiałów, do przewodniczącego można złożyć wniosek o wydanie nakazu ograniczenia zgodnie z art. 19 ustawy o dochodzeniach z 2005 r. i zgodnie z Protokołem dochodzenia w sprawie wniosków o Nakazy ograniczające.27 W module 1 przewodniczący wydał zarządzenie ograniczające z dnia 14 grudnia 2023 r. dotyczące zredagowanych materiałów.28 |
| A1.16. | Aby pomóc w dochodzeniu, powołano grupy ekspertów naukowych i innych, zajmujących się szeregiem różnych tematów i poglądów. Obejmowały one, w module 1, ekspertów w dziedzinie nierówności w zdrowiu, epidemiologii chorób zakaźnych, zarządzania ryzykiem i odporności, nadzoru nad chorobami zakaźnymi i struktur zdrowia publicznego. |
| Temat | Wyznaczono eksperta | Raport eksperta |
|---|---|---|
| Nierówności zdrowotne | Profesor Clare Bambra (profesor zdrowia publicznego na Uniwersytecie w Newcastle) Profesor Sir Michael Marmot (profesor epidemiologii i zdrowia publicznego na University College London) |
INQ000195843 |
| Epidemiologia chorób zakaźnych | Profesor David Heymann (profesor epidemiologii chorób zakaźnych w London School of Hygiene & Tropical Medicine) | INQ000195846 |
| Zarządzanie ryzykiem i odporność | Profesor David Alexander (profesor ds. ograniczania ryzyka i katastrof na University College London) Bruce Mann (dyrektor Sekretariatu ds. Zagrożeń Cywilnych od 2004 do 2009) |
INQ000203349 |
| Nadzór nad chorobami zakaźnymi | Profesor Jimmy Whitworth (emerytowany profesor London School of Hygiene & Tropical Medicine) Dr Charlotte Hammer (pracownik Everitt Butterfield Research w Downing College na Uniwersytecie Cambridge) |
INQ000196611 |
| Struktury zdrowia publicznego | Dr Claas Kirchhelle (adiunkt historii na University College Dublin od 2020 r.) | INQ000205178 |
| A1.17. | W ramach dochodzenia świadkowie proszeni są o złożenie zeznań, jeżeli posiadają dowody istotne dla konkretnego modułu. Składają zeznania pod przysięgą i są przesłuchiwani przez Doradcę prowadzącego dochodzenie, a doradca głównych uczestników również może zadawać pytania za zgodą Przewodniczącego. Podczas przesłuchań publicznych dotyczących modułu 1, które rozpoczęły się w dniu 13 czerwca 2023 r. i zakończyły się w dniu 19 lipca 2023 r., w ramach dochodzenia przesłuchano 68 świadków reprezentujących rząd Wielkiej Brytanii, zdecentralizowane administracje, ekspertów w dziedzinie epidemiologii, struktur odporności i zdrowia, grup społeczeństwa obywatelskiego i ludzie pogrążeni w żałobie. |
| Świadek (rola/organizacja) | Data dowodu |
|---|---|
| Profesor Jimmy Whitworth (emerytowany profesor London School of Hygiene & Tropical Medicine) Dr Charlotte Hammer (pracownik Everitt Butterfield Research w Downing College na Uniwersytecie Cambridge) |
14 czerwca 2023 r |
| Profesor David Heymann (profesor epidemiologii chorób zakaźnych w London School of Hygiene & Tropical Medicine) | 15 czerwca 2023 r |
| Profesor David Alexander (profesor ds. ograniczania ryzyka i katastrof na University College London) Bruce Mann (dyrektor Sekretariatu ds. Zagrożeń Cywilnych od 2004 do 2009) |
15 czerwca 2023 r |
| Profesor Clare Bambra (profesor zdrowia publicznego na Uniwersytecie w Newcastle) Profesor Sir Michael Marmot (profesor epidemiologii i zdrowia publicznego na University College London) |
16 czerwca 2023 r |
| Katharine Hammond (dyrektor Sekretariatu ds. Zagrożeń Cywilnych od sierpnia 2016 r. do sierpnia 2020 r.) | 16 czerwca 2023 r |
| Poseł David Cameron (premier od maja 2010 r. do lipca 2016 r.) | 19 czerwca 2023 r |
| Sir Christopher Wormald (Stały Sekretarz Departamentu Zdrowia i Opieki Społecznej od maja 2016 r.) | 19 czerwca 2023 r |
| Clara Swinson (dyrektor generalny ds. zdrowia globalnego i publicznego w Departamencie Zdrowia i Opieki Społecznej od listopada 2016 r. oraz przewodnicząca Rady Programowej ds. gotowości na wypadek pandemii grypy na lata 2017–2022) | 19 czerwca 2023 r |
| Rt Hon Sir Oliver Letwin MP (Minister ds. Polityki Rządu od maja 2010 r. do lipca 2016 r. i Kanclerz Księstwa Lancaster od lipca 2014 r. do lipca 2016 r.) | 20 czerwca 2023 r |
| Rt Hon George Osborne MP (kanclerz skarbu od maja 2010 do lipca 2016) | 20 czerwca 2023 r |
| Profesor Dame Sally Davies (dyrektor medyczny w Anglii od czerwca 2010 r. do października 2019 r.) | 20 czerwca 2023 r |
| Profesor Sir Mark Walport (główny doradca naukowy rządu od kwietnia 2013 r. do września 2017 r.) | 21 czerwca 2023 r |
| Poseł Oliver Dowden (sekretarz parlamentarny w Urzędzie Rady Ministrów od stycznia 2018 r. do lipca 2019 r.; Minister ds. Gabinetu od lipca 2019 r. do lutego 2020 r.; Minister bez teki w Urzędzie Rady Ministrów od września 2021 r. do czerwca 2022 r.; Kanclerz Księstwa Lancaster od października 2022 r.; Sekretarz Stanu w Kancelarii Rady Ministrów od lutego 2023 r.) | 21 czerwca 2023 r |
| Poseł Rt Hon Jeremy Hunt (Sekretarz Stanu ds. Zdrowia i Opieki Społecznej od września 2012 r. do lipca 2018 r.) | 21 czerwca 2023 r |
| Roger Hargreaves (dyrektor jednostki COBR od lipca 2022 r.) | 22 czerwca 2023 r |
| Profesor Sir Christopher Whitty (główny doradca naukowy Departamentu Zdrowia i Opieki Społecznej od stycznia 2016 r. do sierpnia 2021 r., główny doradca naukowy rządu tymczasowego od 2017 r. do 2018 r., dyrektor ds. medycznych w Anglii od października 2019 r.) | 22 czerwca 2023 r |
| Profesor Sir Patrick Vallance (główny doradca naukowy rządu od kwietnia 2018 r. do marca 2023 r.) | 22 czerwca 2023 r |
| Dr Jim McMenamin (kierownik działu ds. zakażeń i dyrektor ds. incydentów strategicznych w Public Health Scotland) | 22 czerwca 2023 r |
| Emma Reed (dyrektor ds. gotowości na wypadek sytuacji kryzysowych i ochrony zdrowia w Departamencie Zdrowia i Opieki Społecznej od lutego 2018 r.) | 26 czerwca 2023 r |
| Rosemary Gallagher (kierownik ds. zapobiegania i kontroli infekcji w Royal College of Nursing od lipca 2009 r.) | 26 czerwca 2023 r |
| Profesor Dame Jenny Harries (dyrektor naczelny brytyjskiej Agencji Bezpieczeństwa Zdrowia od kwietnia 2021 r.) | 26 czerwca 2023 r |
| Poseł Rt Hon Matt Hancock (sekretarz stanu ds. zdrowia i opieki społecznej od lipca 2018 r. do czerwca 2021 r.) | 27 czerwca 2023 r |
| Duncan Selbie (dyrektor naczelny Public Health England od lipca 2012 r. do sierpnia 2020 r.) | 27 czerwca 2023 r |
| Gillian Russell (dyrektor ds. bezpieczniejszych społeczności w rządzie Szkocji od czerwca 2015 r. do marca 2020 r.) | 28 czerwca 2023 r |
| Caroline Lamb (dyrektor generalny ds. zdrowia i opieki społecznej w rządzie Szkocji oraz dyrektor naczelny NHS Scotland od stycznia 2021 r.) | 28 czerwca 2023 r |
| Jeane Freeman (sekretarz gabinetu ds. zdrowia i sportu w rządzie Szkocji od czerwca 2018 r. do maja 2021 r.) | 28 czerwca 2023 r |
| Sir Jeremy Farrar (główny naukowiec Światowej Organizacji Zdrowia od maja 2023 r. i dyrektor Wellcome Trust od 2013 r. do 2023 r.) | 29 czerwca 2023 r |
| Rt Hon Nicola Sturgeon MSP (pierwszy minister Szkocji od listopada 2014 r. do marca 2023 r.) | 29 czerwca 2023 r |
| John Swinney MSP (wicepierwszy minister w rządzie Szkocji od listopada 2014 r. do marca 2023 r.) | 29 czerwca 2023 r |
| Catherine Frances (dyrektor generalny ds. samorządu lokalnego, odporności i społeczności w Departamencie ds. Wyrównania Poziomu, Mieszkalnictwa i Społeczności od kwietnia 2019 r.) | 29 czerwca 2023 r |
| Sir Frank Atherton (od sierpnia 2016 r. dyrektor medyczny Walii) | 3 lipca 2023 r |
| Dr Andrew Goodall (stały sekretarz rządu walijskiego od września 2021 r.) | 3 lipca 2023 r 4 lipca 2023 r |
| Dr Quentin Sandifer (dyrektor wykonawczy ds. usług zdrowia publicznego i dyrektor medyczny w Public Health Wales od października 2012 r. do grudnia 2020 r.) | 4 lipca 2023 r |
| Rt Hon Vaughan Gething MS (minister zdrowia i usług społecznych w rządzie walijskim od maja 2016 r. do maja 2021 r.) | 4 lipca 2023 r |
| Rt Hon Mark Drakeford MS (pierwszy minister Walii od grudnia 2018 r. do marca 2024 r.) | 4 lipca 2023 r |
| Dr Catherine Calderwood (dyrektor medyczny w Szkocji od kwietnia 2015 r. do kwietnia 2020 r.) | 5 lipca 2023 r |
| Profesor Jim McManus (Prezes Stowarzyszenia Dyrektorów Zdrowia Publicznego od października 2021 r. do października 2023 r.) | 5 lipca 2023 r |
| Profesor Kevin Fenton (Od lipca 2022 r. Przewodniczący Wydziału Zdrowia Publicznego) | 5 lipca 2023 r |
| Profesor Mark Woolhouse (profesor epidemiologii chorób zakaźnych na Uniwersytecie w Edynburgu) | 5 lipca 2023 r |
| Dr Denis McMahon (stały sekretarz Biura Wykonawczego Irlandii Północnej od lipca 2021 r.) | 6 lipca 2023 r |
| Reg Kilpatrick (dyrektor generalny ds. koordynacji Covid-19 w rządzie walijskim od września 2020 r.) | 6 lipca 2023 r |
| Robin Swann MLA (Minister Zdrowia Irlandii Północnej od stycznia 2020 r. do października 2022 r.) | 6 lipca 2023 r |
| Dr Claas Kirchhelle (adiunkt historii na University College Dublin od 2020 r.) | 10 lipca 2023 r |
| Profesor Sir Michael McBride (od września 2006 r. dyrektor medyczny Irlandii Północnej) | 10 lipca 2023 r |
| Rt Hon Arlene Foster, Baronowa Foster of Aghadrumsee DBE (pierwsza minister Irlandii Północnej od stycznia 2016 r. do stycznia 2017 r.) | 11 lipca 2023 r |
| Richard Pengelly (stały sekretarz Departamentu Zdrowia (Irlandia Północna) od lipca 2014 r. do kwietnia 2022 r.) | 11 lipca 2023 r |
| Michelle O'Neill MLA (wicepierwsza minister Irlandii Północnej od stycznia 2020 r. do lutego 2022 r.) | 12 lipca 2023 r |
| Mark Lloyd (dyrektor naczelny Związku Samorządów Lokalnych od listopada 2015 r.) | 12 lipca 2023 r |
| Alison Allen (dyrektor naczelny Stowarzyszenia Władz Lokalnych Irlandii Północnej od lutego 2022 r.) | 12 lipca 2023 r |
| Aidan Dawson (dyrektor naczelny Agencji Zdrowia Publicznego w Irlandii Północnej od lipca 2021 r.) | 12 lipca 2023 r |
| Marcus Bell (dyrektor Centrum Równości od września 2020 r.) | 13 lipca 2023 r |
| Melanie Field (dyrektor ds. strategii i polityki Komisji ds. Równości i Praw Człowieka od 2015 r.) | 13 lipca 2023 r |
| Nigel Edwards (dyrektor naczelny Nuffield Trust od 2014 r.) | 13 lipca 2023 r |
| Dr Richard Horton (redaktor naczelny The Lancet od 1995) | 13 lipca 2023 r |
| poseł Michael Gove (kanclerz księstwa Lancaster od lipca 2019 r. do września 2021 r., minister gabinetu od lutego 2020 r. do września 2021 r. oraz sekretarz stanu ds. wyrównywania poziomu, mieszkalnictwa i społeczności od września 2021 r. do lipca 2022 r. oraz od października 2022 r.) | 13 lipca 2023 r |
| Kate Bell (zastępca sekretarza generalnego Kongresu Związków Zawodowych od grudnia 2022 r.) | 17 lipca 2023 r |
| Gerry Murphy (zastępca sekretarza generalnego Irlandzkiego Kongresu Związków Zawodowych od grudnia 2022 r.) | 17 lipca 2023 r |
| Profesor Philip Banfield (przewodniczący brytyjskiej rady Brytyjskiego Stowarzyszenia Medycznego od lipca 2022 r.) | 17 lipca 2023 r |
| Dr Jennifer Dixon (dyrektor naczelny Fundacji Zdrowia od 2013 r.) | 17 lipca 2023 r |
| Michael Adamson (dyrektor naczelny Brytyjskiego Czerwonego Krzyża od listopada 2014 r.) | 17 lipca 2023 r |
| Matt Fowler (współzałożyciel organizacji Covid-19 Bereaved Families for Justice) | 18 lipca 2023 r |
| Jane Morrison (główna członkini Scottish Covid Bereaved) | 18 lipca 2023 r |
| Anna-Louise Marsh-Rees (współprzewodnicząca organizacji Covid-19 Bereaved Families for Justice Cymru) | 18 lipca 2023 r |
| Brenda Doherty (jedna z liderek grupy Northern Ireland Covid-19 Bereaved Families for Justice) | 18 lipca 2023 r |
| A1.18. | W celu zbadania faktów i ustalenia, co dokładnie się wydarzyło, wszczyna się dochodzenie publiczne. Jest to proces inkwizycyjny, a nie kontradyktoryjny. Wnioski i zalecenia zawarte w niniejszym Raporcie opierają się na obiektywnej ocenie całości materiału dowodowego otrzymanego w ramach Dochodzenia. |
| A1.19. | Zasada 13(3) Regulaminu dochodzeń z 2006 roku zabrania umieszczania jakichkolwiek „wyraźna lub znacząca krytyka” dowolnej osoby wymienionej w niniejszym Raporcie, chyba że wysłano pismo z ostrzeżeniem, a odpowiednia osoba otrzymała odpowiednią możliwość udzielenia odpowiedzi.29 Fraza "wyraźna lub znacząca krytyka” zostało zinterpretowane hojnie, aby zapewnić każdemu, kogo zachowanie mogłoby zostać uznane za przedmiot krytyki w niniejszym Raporcie, możliwość ustosunkowania się. Do osób objętych zasadą 13 wysłano pisma z ostrzeżeniami, a Przewodniczący rozważył odpowiedzi na te pisma przed sfinalizowaniem niniejszego Raportu. |
| A1.20. | Celem dochodzenia przeprowadzonego w niniejszym Raporcie dotyczącym Modułu 1 było sprawdzenie, czy stworzono podstawy umożliwiające rządowi Wielkiej Brytanii i zdecentralizowanym administracjom podjęcie niezbędnych decyzji w przypadku wybuchu pandemii Covid-19. W module 2 (Podstawowe podejmowanie decyzji i zarządzanie polityczne w Wielkiej Brytanii) w dochodzeniu rozważa się, czy polityka prowadzona przez te rządy w odpowiedzi na pandemię Covid-19 była właściwa, tj. czy była proporcjonalna do ryzyka. |
| A1.21. | W module 1 przewodniczącemu bardzo pomagał zespół dochodzeniowy składający się z radców prawnych, radców prawnych, asystentów prawnych i innych członków Sekretariatu. |
| Rola | Nazwa |
|---|---|
| Główny doradca | Hugo Keith KC, Kate Blackwell KC |
| Młodszy radca prawny | Jamie Sharma, Bo-Eun Jung, Joshua Cainer, Zeenat Islam |
Terminologia i odniesienia
| A1.22. | Charakter przedmiotu oznacza, że materiał dowodowy rozpatrywany w Dochodzeniu zawiera znaczący język techniczny i specjalistyczny, który w Dochodzeniu starano się zminimalizować w niniejszym Raporcie. W wielu świadkach i dokumentach używano także szeregu skrótów i akronimów. Terminy te są w pełni wyjaśnione w Załącznik 3: Glosariusz, jednak aby uniknąć nieporozumień i pomóc czytelnikowi, w Dochodzeniu podano w całości nazwy i inne kluczowe wyrażenia w niniejszym Raporcie. |
| A1.23. | Dla ułatwienia poniżej wymieniono niektóre terminy, które są szczególnie kluczowe dla zrozumienia niniejszego Raportu. |
Kluczowa terminologia
| A1.24. | Wirus wywołujący chorobę koronawirusową znaną jako Covid-19 to SARS-CoV-2. Jeżeli jednak ta specyfika nie jest konieczna, zgodnie z praktyką Światowej Organizacji Zdrowia, w dochodzeniu termin „Covid-19” odnosi się zarówno do wirusa, jak i do choroby. |
| A1.25. | Pandemia Covid-19 wymagała działań zarówno ze strony rządów krajowych, jak i zdecentralizowanych. Walia, Szkocja i Irlandia Północna mają władzę ustawodawczą i wykonawczą wybieraną przez własne elektoraty (zwane w niniejszym Raporcie „administracją zdecentralizowaną”). Chociaż każde porozumienie w sprawie decentralizacji jest inne, każda administracja jest odpowiedzialna za szereg zagadnień, w tym zdrowie, edukację i transport. Anglia nie ma własnego ciała ustawodawczego, zamiast tego parlament Wielkiej Brytanii stanowi prawo w „zastrzeżonych” (tj. nie zdecentralizowanych) w całej Wielkiej Brytanii kwestiach, takich jak obrona i sprawy zagraniczne, oraz stanowi prawo dla Anglii w kwestiach powierzonych innym krajom. Parlament Wielkiej Brytanii czasami stanowi także prawa dla innych ugrupowań – na przykład w Anglii i Walii w kwestiach związanych z wymiarem sprawiedliwości. |
| A1.26. | Rząd Wielkiej Brytanii jest odpowiedzialny za wszystkie aspekty polityki rządu w Anglii. W czasie pandemii Covid-19 Departament Zdrowia i Opieki Społecznej był odpowiedzialny za politykę w zakresie zdrowia i opieki społecznej dla dorosłych w Anglii (oraz za ogólnokrajowej podstawy dla kilku elementów tych samych spraw, które nie zostałyby w inny sposób przekazane). Przed styczniem 2018 r. Departament Zdrowia i Opieki Społecznej nosił nazwę Departamentu Zdrowia. W niniejszym raporcie użyto prawidłowej nazwy departamentu i jego Sekretarza Stanu, zgodnie z odpowiednim okresem. W przypadku odniesień obejmujących okres zarówno przed styczniem 2018 r., jak i po nim, w Raporcie używana jest obecna nazwa. |
| A1.27. | Najbardziej złożone sytuacje kryzysowe mają wiele potencjalnych skutków, dlatego angażują „cały system” władzy, a nawet „całe społeczeństwo”. Tam, gdzie w niniejszym Raporcie znajdują się ustalenia i zalecenia dotyczące złożonych sytuacji kryzysowych dla ludności, dochodzenie odnosi się do „sytuacji kryzysowych obejmujących cały system”, które wymagają międzyresortowego podejścia do gotowości i reagowania ze strony rządów. Niektóre dotyczą wyłącznie pandemii. |
Bibliografia
| A1.28. | Odniesienia takie jak „Clare Bambra 16 czerwca 2023 46/18-23' Lub 'INQ000087205_0005' w przypisach do niniejszego Raportu odnoszą się do materiałów dostępnych na stronie internetowej Zapytania.30 |
| A1.29. | W transkrypcjach przesłuchań w ramach dochodzenia podaje się osobę, datę przesłuchania oraz numery stron wewnętrznych i wierszy. Na przykład, 'Clare Bambra 16 czerwca 2023 46/18-23odnosi się do zeznań profesor Clare Bambra z dnia 16 czerwca 2023 r., s. 46, wiersze 18–23. |
| A1.30. | Do dowodów z dokumentów odwołuje się numer dokumentu oraz, w stosownych przypadkach, numery stron i akapitów. Na przykład, 'INQ000087205_0005 ust. 20” odnosi się do dokumentu INQ000087205, s. 5, akapit 20. |
| A1.31. | Dokumenty dostępne publicznie wymieniono w przypisach, wraz z łączami do szerszego Internetu i do stron internetowych Zapytań. Na przykład: Ramy odporności rządu Wielkiej Brytanii, Rząd Jej Królewskiej Mości, grudzień 2022 r., pkt 14 (https://www.gov.uk/government/publications/the-uk-government-resilience-framework; INQ000097685). |
- Widzieć https://covid19.public-inquiry.uk/documents/terms-of-reference/, które obejmuje tłumaczenia Zakresu obowiązków Zapytania; Ustawa o dochodzeniach z 2005 r., zob https://www.legislation.gov.uk/ukpga/2005/12/contents.
- https://covid19.public-inquiry.uk/documents/terms-of-reference
- https://covid19.public-inquiry.uk/documents/terms-of-reference
- Widzieć https://covid19.public-inquiry.uk/structure-of-the-inquiry w celu uzyskania dalszych informacji.
- https://covid19.public-inquiry.uk/modules/resilience-and-preparedness/
- https://covid19.public-inquiry.uk/modules/core-uk-decision-making-and-political-governance-module-2/
- https://covid19.public-inquiry.uk/modules/core-uk-decision-making-and-political-governance-scotland-module-2a/
- https://covid19.public-inquiry.uk/modules/core-uk-decision-making-and-political-governance-wales-module-2b/
- https://covid19.public-inquiry.uk/modules/core-uk-decision-making-and-political-governance-northern-ireland-module-2c/
- https://covid19.public-inquiry.uk/modules/impact-of-covid-19-pandemic-on-healthcare-systems-in-the-4-nations-of-the-uk/
- https://covid19.public-inquiry.uk/modules/vaccines-and-therapeutics-module-4/
- https://covid19.public-inquiry.uk/modules/procurement-module-5/
- https://covid19.public-inquiry.uk/modules/care-sector-module-6/
- https://covid19.public-inquiry.uk/modules/test-trace-and-isolate-module-7/
- https://covid19.public-inquiry.uk/every-story-matters/
- Widzieć https://covid19.public-inquiry.uk/news/hundreds-of-children-and-young-people-set-to-tell-the-inquiry-how-the-pandemic-affected-them/ w celu uzyskania dalszych informacji.
- https://covid19.public-inquiry.uk/wp-content/uploads/2023/05/Module-1-Outline-of-Scope.pdf
- https://covid19.public-inquiry.uk/wp-content/uploads/2023/05/Module-1-List-of-Issues-dated-06-April-2023.pdf
- Regulamin dochodzeń z 2006 r. zob https://www.legislation.gov.uk/uksi/2006/1838/contents/made; dla Protokołu Podstawowego Uczestnika, zob https://covid19.public-inquiry.uk/wp-content/uploads/2023/05/Core-Participant-Protocol.docx-1.pdf.
- https://covid19.public-inquiry.uk/hearings/resilience-and-preparedness/; https://www.youtube.com/@UKCovid-19Inquiry/videos
- https://covid19.public-inquiry.uk/wp-content/uploads/2022/11/2022-11-15-Protocol-on-Documents.pdf; https://www.legislation.gov.uk/uksi/2006/1838/article/9/made
- https://covid19.public-inquiry.uk/wp-content/uploads/2023/05/2022-10-04-Inquiry-Protocol-on-the-Redaction-of-Documents.pdf
- https://covid19.public-inquiry.uk/documents/
- https://www.legislation.gov.uk/ukpga/2005/12/contents
- https://covid19.public-inquiry.uk/documents/
- https://covid19.public-inquiry.uk/documents/
- Ustawa o dochodzeniach z 2005 r. zob https://www.legislation.gov.uk/ukpga/2005/12/section/19; Protokół w sprawie wniosków o wydanie nakazów ograniczenia zob https://covid19.public-inquiry.uk/wp-content/uploads/2022/11/2022-10-11-Inquiry-Protocol-on-Applications-for-Restriction-Orders-.pdf.
- https://covid19.public-inquiry.uk/wp-content/uploads/2023/12/15164756/2023-12-14-Module-1-General-Restriction-Order.pdf
- https://www.legislation.gov.uk/uksi/2006/1838/made
- https://covid19.public-inquiry.uk/hearings/resilience-and-preparedness/
Załącznik 2: Ćwiczenia
| A2.1. | W niniejszym dodatku szczegółowo opisano kluczowe ćwiczenia symulacyjne dotyczące gotowości i odporności na pandemię, które przeprowadzono w Wielkiej Brytanii i krajach zdecentralizowanych w latach 2002–2018. Istnieją cztery rodzaje ćwiczeń symulacyjnych:
|
| Przegląd | Kluczowe cele i uczestnicy | Kluczowe wnioski/obawy | Kluczowe zalecenia |
|---|---|---|---|
| Ćwicz Shipshape 6 czerwca 2003 Anglia i Walia Ćwiczenia na stole na zlecenie Agencji Ochrony Zdrowia dotyczące ciężkiego ostrego zespołu oddechowego (SARS) INQ000235217 |
Zbadanie zdolności lokalnych systemów opieki zdrowotnej w południowo-zachodniej Anglii i Walii do radzenia sobie z rosnącą liczbą przypadków SARS. Zbadanie innych kwestii istotnych dla reakcji na pandemię, w tym ustaleń dotyczących ustalania kontaktów zakaźnych, procedur izolacji i wymogów w zakresie zasobów (INQ000235216_0002). Wśród uczestników znalazło się Ministerstwo Zdrowia, Agencja Ochrony Zdrowia, fundusze powiernicze NHS, Biuro Rady Ministrów, Szkocka władza wykonawcza i inne departamenty rządowe (INQ000235216_0014-0015). |
Pojemność
|
Pojemność
|
| Ćwicz Goliat 9 grudnia 2003 Irlandia Północna Ćwiczenia na żywo zlecone przez Departament Zdrowia, Opieki Społecznej i Bezpieczeństwa Publicznego dotyczące SARS INQ000206664_0001 |
Aby przetestować reakcję społeczności zdrowotnej w przypadku wybuchu epidemii SARS w Irlandii Północnej. Udział wzięły Ministerstwo Zdrowia, Opieki Społecznej i Bezpieczeństwa Publicznego oraz Agencja Ochrony Zdrowia. Obecni byli także obserwatorzy (w tym inne zarządy, trusty, departamenty rządowe i jurysdykcje) (INQ000206664_0002). | Pojemność
|
Pojemność
|
| Ćwicz Bennachiego 2 grudnia 2004 r Szkocja Odważne ćwiczenie przeprowadzone przez Health Protection Scotland dotyczące SARS INQ000187903_0001 |
Aby sprawdzić ogólną gotowość Szkocji do radzenia sobie z SARS (i podobnymi infekcjami, które mogą spowodować poważne rozprzestrzenianie się i wpływ na społeczeństwo). Format ćwiczeń opierał się na syndykatach obejmujących kluczowych przedstawicieli zaangażowanych w reakcję. Pojedynczo i wspólnie zbadali szereg kwestii i pytań związanych z epidemią SARS. Ćwiczenie opracowano w czterech fazach obejmujących hipotetyczny scenariusz 10-tygodniowy (INQ000187903_0001). W spotkaniu uczestniczyli przedstawiciele funduszy NHS, Scottish Ambulance Service, władz lokalnych, Regionalnego Komitetu ds. Nagłych Przypadków Grampian – Grupy Strategicznej, Health Protection Scotland i władz szkockich (INQ000187903_0001). |
Pojemność
|
Planowanie
|
| Ćwicz wierzbę zimową styczeń – luty 2007 w całej Wielkiej Brytanii Ćwiczenia na stole i na żywo na zlecenie Agencji Ochrony Zdrowia i Gabinetu Rady Ministrów dotyczące pandemii grypy INQ000128977 |
Aby sprawdzić przygotowanie na najważniejsze, zakłócające wyzwania, jakie może przynieść pandemia grypy. Ćwiczenie Winter Willow przeprowadzono w dwóch etapach. Etap 1 odbył się 30 stycznia 2007 r. i obejmował ćwiczenia praktyczne na szczeblu krajowym. Etap 2, trwający od 16 do 21 lutego 2007 r., był kontynuacją decyzji podjętych podczas etapu 1 i obejmował kilkudniowe ogólnokrajowe ćwiczenia. Miało to na celu przetestowanie reakcji Wielkiej Brytanii na poziomie lokalnym, regionalnym i krajowym podczas brytyjskiego poziomu alarmowego 4 (powszechne przypadki w Wielkiej Brytanii) (INQ000128977_0004). W spotkaniu wzięło udział ponad 5000 osób z wielu brytyjskich organizacji reprezentujących rząd, przemysł i sektor wolontariatu (INQ000128977_0003). |
Komunikacja
|
Komunikacja
|
| Ćwicz Taliesin 18 listopada 2009 Walia Ćwiczenia na żywo zlecone przez rząd walijski (Wales Resilience Partnership Team) dotyczące grypy pandemicznej INQ000128976 |
Aby przetestować ogólnowalyjski plan reagowania i plany dotyczące pandemii grypy, za pomocą ćwiczeń na żywo w całej Walii. Ćwiczenie stanowiło część prac Gabinetu Rady Ministrów nad rozwijaniem odporności na pandemię grypy. W tym celu Biuro Rady Ministrów sfinansowało serię ćwiczeń „Złotego Standardu” w regionach Anglii i Walii. W Anglii ćwiczenie przeprowadzono na jednym obszarze lokalnego forum ds. odporności w każdym regionie, natomiast w Walii przeprowadzono je jednocześnie na wszystkich czterech obszarach lokalnego forum ds. odporności w ramach ćwiczenia Taliesin (INQ000128976_0003). W sumie w warsztatach zgodziło się wziąć udział 62 uczestników z całej Walii. Wysłano zaproszenia do lokalnych forów dotyczących odporności i poszczególnych agencji, aby osiągnąć równowagę geograficzną i organizacyjną (INQ000128976_0005). |
Planowanie
|
Planowanie
|
| Ćwiczenie Cygnus (Walia) Październik 2014 Walia Ćwiczenia na żywo rządu walijskiego dotyczące grypy pandemicznej INQ000128979 INQ000107136 |
Wdrożenie Ogólnowalyjskiego Planu Reagowania na wypadek pandemii grypy w celu realizacji strategicznych procesów decyzyjnych zarówno na poziomie lokalnym, jak i krajowym w Walii. Ćwiczenie miało się odbyć w trzech etapach: warsztaty na temat planowania i reagowania w zakresie opieki zdrowotnej, które odbędą się w maju 2014 r.; ćwiczenie główne od 13 do 16 października 2014 r.; i ćwiczenie regeneracyjne, które należy wykonać. Zaangażowano rząd walijski, Walię ds. zdrowia publicznego i lokalne fora na rzecz odporności, a także Walijską Komisję ds. nieprzewidzianych sytuacji cywilnych (INQ000107136_0001). |
Pojemność
|
Pojemność
|
| Ćwiczenia w zakresie gotowości na wypadek wirusa Ebola 10 marca 2015 r Anglia Ćwiczenie seminaryjne zlecone przez NHS England dotyczące choroby wywołanej wirusem Ebola INQ000090428 |
Aby przetestować wzrost wydajności i odporności brytyjskich szpitali i agencji zdrowia w odpowiedzi na nową chorobę zakaźną o poważnych konsekwencjach (Ebola). Ćwiczenie zdolności wzrostowej było jednodniowym wydarzeniem w Londynie. Ćwiczenie składało się z moderowanych dyskusji i ustrukturyzowanego omówienia wymaganych reakcji w przypadku scenariusza(ów). W badaniu uczestniczyli starsi urzędnicy ds. zdrowia i komunikacji z NHS England, Public Health England, czterech ośrodków NHS, dyrektorzy ds. zdrowia publicznego i cztery odpowiednie fundusze pogotowia ratunkowego. Dostępny był również panel ekspertów merytorycznych, którzy mogli wnieść swój wkład i odpowiedzieć na wszelkie poruszone kwestie (INQ000090428_0007). |
Pojemność
|
Pojemność
|
| Ćwicz Valverde 25 maja 2015 r Anglia Ćwiczenia na stanowisku dowodzenia przeprowadzone przez Public Health England na zlecenie grupy zadaniowej ds. udostępniania próbek Global Health Security Initiative w związku z nowym koronawirusem – udostępnianie próbek INQ000022722 |
Przetestowanie istniejących ustaleń dotyczących szybkiego udostępniania próbek laboratoryjnych patogenów innych niż grypa i próbek pokrewnych podczas stanu zagrożenia zdrowia publicznego. Były to międzynarodowe ćwiczenia symulujące wybuch nowego wirusa koronowego w fikcyjnym kraju Valverde w Ameryce Południowej, który staje się stanem nadzwyczajnym w zakresie zdrowia publicznego o zasięgu międzynarodowym. W ćwiczeniu uczestniczyli przedstawiciele krajów członkowskich i organizacji wchodzących w skład Grupy Zadaniowej ds. Wymiany Próbek Globalnej Inicjatywy na rzecz Bezpieczeństwa Zdrowia, ministerstwa zdrowia, wyznaczone laboratoria na poziomie krajowym oraz inne odpowiednie zainteresowane strony i departamenty rządowe zaangażowane w proces udostępniania próbek ponad granicami międzynarodowymi. Komisja Europejska również uczestniczyła w ćwiczeniu w roli wspierającej (INQ000022722_0004). |
Szkolenie
|
Szkolenie
|
| Ćwicz Alicja 15 lutego 2016 r Anglia Ćwiczenia na stole zlecone przez Departament Zdrowia dotyczące koronaawirusa bliskowschodniego zespołu oddechowego (MERS-CoV) INQ000090431 |
Zbadanie zasad, reakcji i problemów związanych z epidemią w Anglii. Ćwiczenie to zostało zlecone przez Departament Zdrowia w odpowiedzi na obawy wyrażone przez dyrektora medycznego dotyczące planowania i odporności w odpowiedzi na epidemię MERS-CoV na dużą skalę w Anglii. W badaniu wzięły udział NHS England, Public Health England i Departament Zdrowia. Ćwiczenie obserwowało Biuro Rady Ministrów, zdecentralizowane administracje i Rządowe Biuro ds. Nauki (INQ000090431). |
Pojemność
|
Pojemność
|
| Ćwicz Srebrnego Łabędzia kwiecień 2016 Szkocja Seria ćwiczeń symulacyjnych prowadzonych przez rząd Szkocji (Wydział Odporności) na temat grypy pandemicznej INQ000103012 |
Ocena gotowości i reakcji lokalnych i krajowych rozwiązań Szkocji na epidemię grypy pandemicznej w dłuższym okresie. Było to nowe podejście do ćwiczeń krajowych. Jednym z najbardziej udanych aspektów tego podejścia było to, że w wydarzeniach wzięło udział ponad 600 osób, w tym uczestnicy z NHS i władz lokalnych (INQ000103012_0008). |
Pojemność
|
Pojemność
|
| Ćwicz Łabędzia 18-20 października 2016 r w całej Wielkiej Brytanii Ćwiczenia na żywo zlecone przez Ministerstwo Zdrowia dotyczące grypy pandemicznej INQ000022792 |
Ocena gotowości Wielkiej Brytanii i reakcji na epidemię grypy pandemicznej (INQ000022792_0003). Opiera się na czterech symulowanych spotkaniach COBR. Akcja rozgrywa się w siódmym tygodniu pandemii, która dotyka do 50% populacji Wielkiej Brytanii i powoduje od 200 000 do 400 000 dodatkowych zgonów. W ćwiczeniu wzięło udział ponad 950 przedstawicieli zdecentralizowanych administracji, Departamentu Zdrowia i 12 innych departamentów rządowych, NHS Wales, NHS England, Public Health England, ośmiu lokalnych forów na rzecz odporności i sześciu więzień (INQ000022792_0005). |
Pojemność
|
Pojemność
|
| Ćwicz na ulicy Szerokiej 29 stycznia 2018 r Anglia Oparte na dyskusji ćwiczenie zlecone przez Radę Programową ds. Chorób Zakaźnych Wysokich Konsekwencji dotyczące przyszłej, ostatecznej choroby zakaźnej o poważnych konsekwencjach (HCID) INQ000090442 |
Rozważenie przyszłej ostatecznej usługi HCID w Anglii oraz wyzwań, jakie incydent związany z HCID może postawić przed profesjonalnymi partnerami w zakresie proponowanej usługi HCID w Anglii (INQ000090442_0005). W dniu 29 stycznia 2018 r. to ćwiczenie oparte na dyskusji odbyło się w Londynie. Uczestnicy pochodzili z Public Health England i NHS England. Dodatkowo obecny był obserwator z Departamentu Zdrowia i Opieki Społecznej (INQ000090442_0008). |
Zdolność
|
Zdolność
|
| Ćwicz Iris 12 marca 2018 r Szkocja Ćwiczenie na stole przeprowadzone przez Wydział Ochrony Zdrowia Rządu Szkocji dotyczące MERS-CoV INQ000147839 |
Ocena reakcji NHS Scotland na podejrzenie wybuchu MERS-CoV. W dniu 12 marca 2018 r. w Szkocji przeprowadzono ćwiczenia praktyczne, aby zbadać wyzwania, przed którymi staną zarządy NHS Scotland w przypadku podejrzeń – a później potwierdzonych – przypadków MERS-CoV w jednym lub większej liczbie obszarów zarządu. Uczestnicy ćwiczenia reprezentowali zarządy NHS Scotland, rady krajowe, w tym NHS 24 i Health Protection Scotland, a także szkockie pogotowie ratunkowe (INQ000147839_0004). |
Pojemność
|
Pojemność
|
| Ćwicz Picę 5 września 2018 r Anglia Ćwiczenie na stole zlecone przez NHS England dotyczące grypy pandemicznej INQ000023034 |
Przegląd i ocena gotowości i reakcji na pandemię grypy w ramach podstawowej opieki zdrowotnej, poprzez umożliwienie zbadania istniejących procesów i ustaleń. Jego celem było zebranie wniosków na temat reakcji podstawowej opieki zdrowotnej NHS na grypę pandemiczną na trzech kluczowych etapach: wykrycie i ocena (pierwsze dni/tygodnie); leczyć i eskalować (szczyt pandemii w 6. i 7. tygodniu); i powrót do zdrowia (miesiące później). Był wspierany przez NHS England i Public Health England. Wśród uczestników znalazły się fundusze powiernicze NHS, Brytyjskie Stowarzyszenie Stomatologiczne, Komisja Lekarzy Rodzinnych Brytyjskiego Stowarzyszenia Medycznego, College of Optometrists, Komisja ds. Jakości Opieki i Królewskie Towarzystwo Farmaceutyczne (INQ000023034_0005). |
Pojemność
|
Pojemność
|
- Przewodnik dla planistów ćwiczeń, Home Office, 1998 (https://assets.publishing.service.gov.uk/media/5a74b983ed915d4d83b5e717/the-exercise-planners-guide.pdf)
- Katharine Hammond 16 czerwca 2023 178/2-7
- Przewodnik dla planistów ćwiczeń, Home Office, 1998 (https://assets.publishing.service.gov.uk/media/5a74b983ed915d4d83b5e717/the-exercise-planners-guide.pdf)
- Katharine Hammond 16 czerwca 2023 178/2-7
- Przewodnik dla planistów ćwiczeń, Home Office, 1998 (https://assets.publishing.service.gov.uk/media/5a74b983ed915d4d83b5e717/the-exercise-planners-guide.pdf)
- Przewodnik dla planistów ćwiczeń, Home Office, 1998 (https://assets.publishing.service.gov.uk/media/5a74b983ed915d4d83b5e717/the-exercise-planners-guide.pdf)
Załącznik 3: Glosariusz
| Termin (akronim) | Opis |
|---|---|
| 10 Downing Street | Biuro Premiera, które wspiera Premiera w ustalaniu i realizacji ogólnej strategii i priorytetów politycznych rządu Wielkiej Brytanii oraz w komunikowaniu polityki rządu Wielkiej Brytanii Parlamentowi, społeczeństwu i publiczności międzynarodowej. |
| Komitet Doradczy ds. Niebezpiecznych Patogenów | Naukowy komitet doradczy Departamentu Zdrowia i Opieki Społecznej. Jej praca obejmuje zapewnianie rządowi Wielkiej Brytanii niezależnych porad naukowych na temat ryzyka narażenia na patogeny. |
| Transmisja lotnicza | Przenoszenie następuje na krótkie lub duże odległości drogą powietrzną z bardzo małych kropelek oddechowych zawierających wirusa, wytwarzanych przez zakażoną osobę. |
| Antybiotyki | Leki stosowane w leczeniu lub zapobieganiu zakażeniom bakteryjnym. |
| Leki przeciwwirusowe | Leki stosowane w leczeniu lub zapobieganiu infekcjom wirusowym. |
| Stowarzyszenie Dyrektorów Zdrowia Publicznego | Reprezentatywna organizacja dyrektorów ds. zdrowia publicznego. |
| Bezobjawowy | Ma infekcję, ale nie wykazuje żadnych objawów. |
| Ptasia grypa | Rodzaj wirusa grypy przystosowany do populacji ptaków. Ptasia grypa może również przenieść się na inne zwierzęta, w tym ludzi, i może rozwinąć się zdolność skutecznego przenoszenia się z człowieka na człowieka. |
| Nauka behawioralna | Naukowe badanie zachowań ludzi i zwierząt, obejmujące takie dyscypliny jak psychologia, antropologia i socjologia. |
| Bezpieczeństwo biologiczne | Przygotowanie, polityki i działania podejmowane w celu ochrony zdrowia ludzi, zwierząt i środowiska przed zagrożeniami biologicznymi. |
| Wydarzenie „Czarny łabędź”. | Katastrofalny scenariusz, który z góry jest bezprecedensowy, wykracza poza nasze pole doświadczenia, poza nasze możliwości rozsądnego rozważenia, a zatem jest tak pozornie nieprawdopodobny, że jest nieprzewidywalny. |
| Brytyjskie Stowarzyszenie Medyczne | Związek zawodowy i organizacja zawodowa lekarzy i studentów medycyny w Wielkiej Brytanii. |
| Gabinet | Zespół składający się z ministrów wyższego szczebla, wybranych do kierowania określonymi obszarami polityki. |
| Biuro Rady Ministrów | Ministerialny departament rządowy Wielkiej Brytanii, wspierany przez 28 agencji i organów publicznych. Wspiera premiera, zapewnia skuteczne funkcjonowanie rządu i przejmuje wiodącą rolę w niektórych kluczowych obszarach polityki. |
| Wskaźnik śmiertelności przypadków | Odsetek osób, u których zdiagnozowano chorobę, i które umierają z jej powodu. |
| Respondenci kategorii 1 i 2 | Zgodnie z ustawą o nieprzewidzianych zdarzeniach cywilnych z 2004 r.: Służby ratownicze kategorii 1 to te organizacje (służby ratunkowe, władze lokalne i organy NHS), które odgrywają kluczową rolę w reagowaniu na większość sytuacji kryzysowych i które podlegają pełnemu zestawowi obowiązków w zakresie ochrony ludności. Służby ratownicze kategorii 2 to organizacje (Inspekcja ds. Zdrowia i Bezpieczeństwa, przedsiębiorstwa transportowe i użyteczności publicznej), które są w dużym stopniu zaangażowane w zdarzenia mające wpływ na ich poszczególne sektory, ale z mniejszym prawdopodobieństwem angażują się w prace związane z planowaniem. Mają mniejszy zestaw obowiązków: współpracę i dzielenie się istotnymi informacjami z innymi ratownikami kategorii 1 i 2. |
| Kanclerz Księstwa Lancaster | Starszy minister gabinetu i członek gabinetu zarządzający majątkami i czynszami Księstwa Lancaster. Odpowiedzialny za nadzorowanie całej polityki Gabinetu, sytuacji awaryjnych, odporności i bezpieczeństwa narodowego. |
| Kanclerz Skarbu | Główny minister finansów brytyjskiego rządu, ponoszący ogólną odpowiedzialność za skarb państwa. |
| Główny Lekarz | Wykwalifikowany lekarz, najwyższy rangą doradca rządowy ds. zdrowia oraz zawodowy szef wszystkich dyrektorów ds. zdrowia publicznego w samorządach terytorialnych i lekarzy w rządzie. Dla Anglii, Walii, Szkocji i Irlandii Północnej istnieje oddzielny dyrektor medyczny. Dyrektor medyczny w Anglii jest głównym doradcą medycznym brytyjskiego rządu. |
| Główni doradcy naukowi | Starsi doradcy ds. nauki, pracujący w większości departamentów rządowych, którzy zapewniają nadzór i zapewnienie potencjału i działań naukowych. |
| Ustawa o nieprzewidzianych zdarzeniach cywilnych z 2004 r | Ustawodawstwo zapewniające ramy ochrony ludności w Wielkiej Brytanii. Umożliwia także tworzenie tymczasowych przepisów specjalnych (przepisów nadzwyczajnych), które pomogą uporać się z najpoważniejszymi sytuacjami kryzysowymi. |
| Grupa ds. nieprzewidzianych wypadków cywilnych (Irlandia Północna) | Główny organ ds. strategicznej gotowości na wypadek zagrożeń cywilnych w sektorze publicznym w Irlandii Północnej, odpowiedzialny za zapewnianie strategicznego przywództwa w zakresie gotowości na wypadek nieprzewidzianych wypadków cywilnych poprzez uzgadnianie polityki i strategii w kwestiach przekrojowych. Zwykle przewodniczy mu starszy urzędnik służby cywilnej, ale alternatywnie może mu przewodniczyć Pierwszy Minister i WicePierwszy Minister działający wspólnie, lub inny minister nominowany wspólnie przez Pierwszego Ministra i WicePierwszego Ministra. Biorą w nim udział m.in. przedstawiciele wszystkich departamentów rządowych Irlandii Północnej, Biura Irlandii Północnej, a także władz lokalnych i służb ratunkowych. |
| Grupa ds. Zagrożeń Cywilnych (Walia) | Grupa wyższych urzędników ds. polityki, utworzona około 2006 r., która spotyka się w celu omówienia strategii gotowości na wypadek sytuacji kryzysowych w Walii, rozważenia pojawiających się zagrożeń i określenia odpowiedniego planowania, reagowania i naprawy we wszystkich departamentach rządowych. Zarządza również wewnętrzną reakcją rządu walijskiego na sytuacje kryzysowe. W przypadku ustalenia, że konieczna jest szersza obecność interesariuszy zewnętrznych, grupa zostaje formalnie ponownie ukonstytuowana jako Wales Civil Warency Committee, zgodnie z warunkami Ogólnowalyjskiego Planu Reagowania. |
| Sekretariat ds. Zagrożeń Cywilnych | Specjalna jednostka w Urzędzie Rady Ministrów, która zarządzała gotowością rządu Wielkiej Brytanii i reagowaniem na ważne wydarzenia o zasięgu ogólnokrajowym. Współpracował z departamentami rządowymi w celu określenia ryzyka i zarządzania nim oraz koordynowania ustaleń dotyczących sytuacji nadzwyczajnych, doradzał Premierowi w zakresie sytuacji nadzwyczajnych, prowadził COBR, współpracował z zdecentralizowaną administracją i lokalnymi służbami ratowniczymi, aby zapewnić wdrożenie planów i zdolności, oraz nadzorował działania na wysokim szczeblu ćwiczenia lub testy systemu gotowości i reagowania. Zastąpiony przez Jednostkę COBR i Dyrekcję ds. Odporności w lipcu 2022 r. |
| COBR | Krajowe centrum zarządzania kryzysowego rządu Wielkiej Brytanii odpowiedzialne za reagowanie na cywilne sytuacje kryzysowe obejmujące cały system. Zapewnia mechanizm koordynacji, dzięki któremu rząd Wielkiej Brytanii szybko reaguje na sytuacje kryzysowe wymagające pilnego podjęcia decyzji. Jego nazwa wywodzi się pierwotnie od lokalizacji w salach posiedzeń Urzędu Rady Ministrów. |
| Transmisja wspólnotowa | Kiedy choroba rozprzestrzenia się w społeczeństwie, a jej konkretne źródło jest nieznane (na przykład nie można jej powiązać z podróżującym z zagranicy). |
| Koncepcja Operacji (rząd Wielkiej Brytanii) | Dokument określający ustalenia Wielkiej Brytanii dotyczące reagowania i usuwania skutków sytuacji kryzysowych. |
| Kontakt | Osoba, która była blisko osoby, która uzyskała pozytywny wynik testu na obecność infekcji. |
| Śledzenie kontaktów | Identyfikacja źródła i kontaktów powiązanych z potwierdzonym przypadkiem choroby zakaźnej. Środek w zakresie zdrowia publicznego mający na celu powstrzymanie rozprzestrzeniania się infekcji. |
| Powstrzymanie | Strategia kontroli choroby mająca na celu zapobieganie przenoszeniu choroby w społeczności, na przykład poprzez śledzenie kontaktów osób zakażonych. |
| Planowanie awaryjne | Planowanie gotowości do skutecznego reagowania w sytuacjach awaryjnych. |
| Koronawirusy | Rodzina wirusów powodujących choroby układu oddechowego u ludzi. |
| Środki zaradcze | Środki podjęte w celu złagodzenia lub powstrzymania skutków pandemii, takie jak śledzenie kontaktów zakaźnych, środki lecznicze i szczepionki. |
| COVID-19 | Choroba wywołana przez koronaawirusa SARS-CoV-2. |
| Rodziny pogrążone w żałobie w związku z Covid-19 w imię sprawiedliwości | Ogólnobrytyjska grupa kampanii reprezentująca interesy pogrążonych w żałobie członków rodzin osób, które zmarły na Covid-19. |
| Rodziny pogrążone w żałobie w związku z Covid-19 na rzecz sprawiedliwości Cymru | Grupa skupiająca się na Walii, której celem jest prowadzenie kampanii na rzecz osób pogrążonych w żałobie z powodu Covid-19 w Walii i udzielanie im głosu. |
| Gorączka krwotoczna krymsko-kongijska | Wirusowa gorączka krwotoczna, wywoływana głównie przez ukąszenia kleszczy. |
| Departament Biznesu i Handlu | Ministerialny departament rządowy Wielkiej Brytanii, wspierany przez 19 agencji i organów publicznych, odpowiedzialny za wzrost gospodarczy i handel międzynarodowy. |
| Departament Wyrównywania Poziomów, Mieszkalnictwa i Społeczności | Ministerialny departament rządowy Wielkiej Brytanii, wspierany przez 15 agencji i organów publicznych, odpowiedzialny za mieszkalnictwo, społeczności, samorząd lokalny i politykę wyrównywania szans. Od maja 2006 r. do stycznia 2018 r. funkcjonował jako Departament ds. Społeczności i Samorządu Terytorialnego, a od stycznia 2018 r. do września 2021 r. jako Ministerstwo Mieszkalnictwa, Gmin i Samorządu Terytorialnego. Określana w niniejszym Raporcie poprawną nazwą dla odpowiedniego okresu lub, w przypadku odniesień obejmujących okres przed i po wrześniu 2021 r., pod obecną nazwą. |
| Departament Zdrowia i Opieki Społecznej/Departament Zdrowia | Ministerialny departament rządowy Wielkiej Brytanii ponoszący ogólną odpowiedzialność za usługi zdrowotne i opiekuńcze. Ustala strategię oraz finansuje i nadzoruje system opieki zdrowotnej i opieki w Anglii wraz z jego odpowiednikami w krajach zdecentralizowanych. Znany przed styczniem 2018 r. jako Departament Zdrowia. Określana w niniejszym Raporcie pod nazwą, jaką nosiła w danym okresie, lub, w przypadku odniesień obejmujących oba okresy, pod obecną nazwą. |
| Departament Zdrowia (Irlandia Północna) | Zdecentralizowany departament rządowy w władzach wykonawczych Irlandii Północnej, którego ustawowy obowiązek obejmuje promowanie zdrowia fizycznego i psychicznego oraz dobrostanu społecznego mieszkańców Irlandii Północnej oraz zapobieganie, diagnozowanie i leczenie chorób. Do dnia 9 maja 2016 r. departament ten nosił nazwę Departament Zdrowia, Opieki Społecznej i Bezpieczeństwa Publicznego, ale w niniejszym Raporcie nazywany jest Departamentem Zdrowia (Irlandia Północna), chyba że zostało to wyraźnie określone przed majem 2016 r. |
| Zastępca Naczelnego Lekarza | Naczelnego Lekarza Medycznego wspierają trzej Zastępcy Naczelnego Lekarza. |
| Zastępca pierwszego ministra w rządzie Irlandii Północnej | Wspólne przewodniczący (wraz z Pierwszym Ministrem) władz wykonawczych Irlandii Północnej. Wszystkie funkcje ustawowe przypisane wicepremierowi (i pierwszemu ministrowi) na mocy ustawy o Irlandii Północnej z 1998 r. muszą być wykonywane łącznie. |
| Zastępca pierwszego ministra rządu Szkocji | Sekretarz gabinetu w rządzie Szkocji, wspierający pracę Pierwszego Ministra. Do 2023 r. wicepierwszy minister odpowiadał za funkcję odpornościową rządu Szkocji. |
| Test diagnostyczny | Test, który może potwierdzić, czy dana osoba jest chora. |
| Dyrektorzy zdrowia publicznego | W Anglii specjaliści zatrudnieni przez wszystkie władze lokalne odpowiedzialne za zdrowie publiczne, którzy ponoszą główną odpowiedzialność za zdrowie swoich społeczności i są odpowiedzialni za realizację obowiązków swoich władz w zakresie zdrowia publicznego. W Szkocji i Walii są oni zatrudniani przez komisje ds. zdrowia NHS, a w Irlandii Północnej jedyny dyrektor ds. zdrowia publicznego odpowiada przed dyrektorem medycznym. |
| „Choroba X” | Choroba zakaźna, która obecnie nie powoduje zakażenia ludzi, ale może spowodować poważną epidemię lub pandemię. |
| DNA | Kwas dezoksyrybonukleinowy, cząsteczka zawierająca instrukcje genetyczne dotyczące wzrostu i funkcjonowania wszystkich znanych organizmów i wielu wirusów. |
| Ebola | Może odnosić się do wirusa Ebola lub choroby, którą powoduje. Wirus przenoszony jest ze zwierząt (takich jak nietoperze lub naczelne inne niż ludzie) na ludzi i może przenosić się z człowieka na człowieka poprzez płyny ustrojowe. Wywołuje ciężką i często śmiertelną gorączkę krwotoczną. |
| Ćwiczenia w zakresie gotowości na wypadek wirusa Ebola | Ćwiczenie z marca 2015 r. zlecone przez NHS England w celu oceny możliwości i zasobów NHS i Public Health England w zakresie zarządzania wieloma przypadkami wirusa Ebola w Anglii. |
| Skuteczność | Omawiając lek, taki jak leczenie lub szczepionka, odnosi się to do tego, jak dobrze lek osiąga zamierzony efekt, gdy jest stosowany w rzeczywistych warunkach. |
| Skuteczność | Stopień, w jakim lek działa zgodnie z zamierzeniami, gdy jest testowany w idealnych okolicznościach, np. w kontrolowanym badaniu naukowym. |
| Grupy gotowości na wypadek sytuacji kryzysowych | Grupy wieloagencyjne w Irlandii Północnej zostały utworzone w celu zapewnienia odpowiedniego przygotowania umożliwiającego skuteczne reagowanie na sytuacje kryzysowe. |
| Gotowość, odporność i reagowanie na sytuacje kryzysowe | W ramach departamentu rządowego funkcja gotowości, odporności i reagowania na sytuacje kryzysowe odpowiada za planowanie i reagowanie na wszystkie zdarzenia, w których istnieje potencjalne ryzyko dla zdrowia publicznego. |
| Departament Reagowania Kryzysowego | Departament zdrowia publicznego w Anglii, który pracował nad poprawą odporności zdrowia publicznego poprzez zapewnienie gotowości na wypadek sytuacji kryzysowych, odporności i usług reagowania w oparciu o badania naukowe i medyczne oparte na dowodach. |
| Choroba endemiczna | Choroba, która utrzymuje się na stałym, przewidywalnym poziomie zapadalności w danym regionie geograficznym. |
| Epidemia | Nagły wzrost częstości występowania choroby, który jest wyższy niż oczekiwano w danym regionie geograficznym. |
| Epidemiologia | Badanie rozmieszczenia, wzorców i determinantów warunków zdrowotnych i chorobowych w określonej populacji. |
| Likwidacja | Całkowita redukcja wszystkich przypadków chorób na świecie do zera, bez ciągłej potrzeby interwencji. |
| Europejskie Centrum Zapobiegania i Kontroli Chorób | Agencja Unii Europejskiej zajmująca się nadzorem nad chorobami zakaźnymi, reagowaniem i gotowością. |
| Nadmiar zgonów | Liczba dodatkowych zgonów w danym okresie jest wyższa, niż można by się tego spodziewać na podstawie ostatnich lat. |
| Biuro Wykonawcze, Irlandia Północna | Zdecentralizowany departament rządowy Irlandii Północnej w władzach wykonawczych Irlandii Północnej, którego główna odpowiedzialność polityczna jest związana z nieprzewidzianymi sytuacjami cywilnymi. Ministrowie ponoszący ogólną odpowiedzialność za departament to Pierwszy Minister i Zastępca Pierwszego Ministra. |
| Ćwicz Alicja | Ćwiczenie z lutego 2016 r. mające na celu ocenę wyzwań związanych z epidemią na dużą skalę bliskowschodniego zespołu oddechowego (MERS-CoV) w Anglii. |
| Ćwicz Bennachiego | Jednodniowe ćwiczenie symulacyjne przeprowadzone w grudniu 2004 r., którego celem było sprawdzenie ogólnego przygotowania do postępowania w przypadku ciężkiego ostrego zespołu oddechowego (SARS). |
| Ćwicz na ulicy Szerokiej | W styczniu 2018 r. przeprowadzono ćwiczenie mające na celu opracowanie uzgodnionego podejścia do zarządzania kompleksową ścieżką pacjenta w przypadku znanych i nieznanych chorób zakaźnych o poważnych konsekwencjach oraz zapewnienie trwałej reakcji. |
| Ćwicz Cerbera | Wewnętrzna ocena gotowości organizacyjnej Public Health England i reakcji na sytuacje kryzysowe dotyczące zdrowia publicznego z lutego 2018 r. |
| Ćwicz Łabędzia | Ćwiczenie z października 2016 r. oceniające gotowość Wielkiej Brytanii i reakcję na wybuch pandemii grypy. |
| Ćwicz Goliat | Test reakcji na epidemię ciężkiego ostrego zespołu oddechowego (SARS) w Irlandii Północnej z grudnia 2003 r. |
| Ćwicz Iris | Ćwiczenia z marca 2018 r. mające na celu ocenę reakcji Szkocji na epidemię bliskowschodniego zespołu oddechowego (MERS-CoV). |
| Ćwicz Picę | Test gotowości i możliwości reagowania podstawowej opieki zdrowotnej NHS na pandemię grypy, przeprowadzony we wrześniu 2018 r. |
| Ćwicz Shipshape | Ćwiczenia z czerwca 2003 r. przeprowadzone po potwierdzeniu pierwszego przypadku ciężkiego ostrego zespołu oddechowego (SARS) w Wielkiej Brytanii. |
| Ćwicz Srebrnego Łabędzia | Seria ćwiczeń przeprowadzonych w całej Szkocji w kwietniu 2016 r. w celu oceny gotowości i reakcji lokalnych i krajowych ustaleń Szkocji na epidemię grypy pandemicznej w dłuższym okresie. |
| Ćwicz Taliesin | Ćwiczenie z listopada 2009 r. mające na celu ocenę planu reagowania dla całej Walii i lokalnych planów dotyczących grypy pandemicznej w całej Walii. |
| Ćwicz Tyfon | Test z lutego 2017 r. mający na celu ocenę zdolności Public Health England do reagowania i zarządzania dwoma równoległymi incydentami na poziomie podwyższonym (poważnym incydentem chemicznym i potwierdzonym pozytywnym przypadkiem wirusowej gorączki krwotocznej). |
| Ćwicz wierzbę zimową | Ćwiczenie przeprowadzone w styczniu i lutym 2007 r. mające na celu ocenę przygotowań na pandemię grypy. |
| Ćwicz Valverde | Ćwiczenie Globalnej Inicjatywy na rzecz Bezpieczeństwa Zdrowia z maja 2015 r. mające na celu przetestowanie projektów ustaleń krajów członkowskich dotyczących udostępniania próbek laboratoryjnych patogenów innych niż grypa podczas stanu zagrożenia zdrowia publicznego. |
| Rozprzestrzenianie się wykładnicze | Infekcja może rozprzestrzeniać się wykładniczo (tzn. przyspieszać w czasie), gdy patogen przedostanie się do populacji z niewielką odpornością lub bez niej. |
| Pierwszy Minister, władza wykonawcza Irlandii Północnej | Wspólne przewodniczący (wraz z wicepremierem) władz wykonawczych Irlandii Północnej. Wszystkie funkcje ustawowe przypisane Pierwszemu Ministrowi (i zastępcy Pierwszego Ministra) na mocy Ustawy o Irlandii Północnej z 1998 r. muszą być wykonywane łącznie. |
| Pierwszy minister Szkocji | Szef rządu Szkocji odpowiedzialny za ogólny rozwój, wdrażanie i prezentację polityki administracji oraz za promocję i reprezentowanie Szkocji w kraju i za granicą. |
| Pierwszy minister Walii | Szef rządu walijskiego odpowiedzialny za ogólny rozwój i koordynację polityki rządu walijskiego. |
| Biuro Spraw Zagranicznych, Wspólnoty Narodów i Rozwoju | Ministerialny departament rządowy, wspierany przez 12 agencji i organów publicznych. |
| Cztery narody | Cztery narody Wielkiej Brytanii: Anglia, Walia, Szkocja i Irlandia Północna. |
| Incydent radiologiczny w Fukushimie | Awaria nuklearna w 2011 r. związana z wyciekami promieniowania w elektrowni jądrowej Fukushima Daiichi w Japonii. |
| G7 | Grupa Siedmiu (G7) to nieformalne forum międzyrządowe składające się z Wielkiej Brytanii, USA, Kanady, Francji, Niemiec, Włoch i Japonii. Obecni są także przedstawiciele Unii Europejskiej. |
| Globalna sieć ostrzegania i reagowania na epidemie, Światowa Organizacja Zdrowia | Sieć instytucji technicznych i sieci Światowej Organizacji Zdrowia na całym świecie, które reagują na ostre zdarzenia związane ze zdrowiem publicznym, wysyłając personel i zasoby do dotkniętych krajów. |
| Główny doradca naukowy rządu | Główny Doradca Naukowy zapewnia doradztwo naukowe Premierowi i członkom Gabinetu oraz koordynuje sieć głównych doradców naukowych. |
| Rządowe Biuro ds. Nauki (GO-Science) | Biuro naukowe doradzające Premierowi i członkom Rady Ministrów w celu zapewnienia, że polityka i decyzje rządu opierają się na najlepszych dowodach naukowych i strategicznym myśleniu długoterminowym. |
| Myślenie grupowe | Biuro naukowe doradzające Premierowi i członkom Rady Ministrów w celu zapewnienia, że polityka i decyzje rządu opierają się na najlepszych dowodach naukowych i strategicznym myśleniu długoterminowym. |
| Myślenie grupowe | Zjawisko, w wyniku którego ludzie w grupie mają tendencję do myślenia o tych samych rzeczach w ten sam sposób. |
| Urząd ds. Gotowości i Reagowania na Kryzysy Zdrowotne, Komisja Europejska | Wspiera projekty wzmacniające gotowość i zdolności reagowania w dziedzinie zdrowia. |
| Agencja Ochrony Zdrowia | Były pozaresortowy organ publiczny, sponsorowany przez Departament Zdrowia i Opieki Społecznej, który stał się częścią Public Health England w 2013 r. Jego rolą było zapewnianie zintegrowanego podejścia do ochrony zdrowia publicznego w Wielkiej Brytanii poprzez zapewnianie wsparcia i porad pracownikom NHS, władze lokalne, służby ratunkowe oraz Departament Zdrowia i Opieki Społecznej i inne agencje. |
| Zespoły ochrony zdrowia | Część brytyjskiej Agencji Bezpieczeństwa Zdrowia. Składają się z profesjonalnie wykwalifikowanych konsultantów ochrony zdrowia, którzy zapewniają specjalistyczne porady w zakresie zdrowia publicznego oraz wsparcie operacyjne dla NHS, władz lokalnych i innych agencji. |
| Choroby Henipawirusowe | Umiarkowane do ciężkich choroby neurologiczne i układu oddechowego wywoływane przez rodzaj wirusów, których głównym naturalnym rezerwuarem są nietoperze owocożerne. Przypadki wirusa Hendra powiązano z bliskim kontaktem z zakażonymi końmi w Australii, a w kilku krajach Azji Południowo-Wschodniej wystąpiły większe epidemie wirusa Nipah, w wyniku których wirus przeniósł się ze świń i nietoperzy, a także zgłoszono przypadki przenoszenia wirusa z człowieka na człowieka. |
| Choroba zakaźna o poważnych konsekwencjach | Ostra choroba zakaźna, która:
|
| Program dotyczący chorób zakaźnych o poważnych konsekwencjach | Program stworzony przez Public Health England i NHS England w 2015 r. w celu opracowania uzgodnionej metody postępowania w przypadku podejrzeń i potwierdzonych przypadków chorób zakaźnych o poważnych konsekwencjach oraz stworzenia dodatkowych specjalistycznych placówek, w których można by leczyć pacjentów cierpiących na te choroby. |
| Domowe biuro | Departament rządu Wielkiej Brytanii, wspierany przez 29 agencji i organów publicznych. Główny departament rządowy ds. imigracji i paszportów, polityki narkotykowej, przestępczości, pożarów, zwalczania terroryzmu i policji. |
| Zakażenia zwierząt ludzkich i nadzór nad ryzykiem | Wieloagencyjna, międzyrządowa grupa badająca horyzonty i oceniająca ryzyko, która bierze pod uwagę pojawiające się i potencjalnie odzwierzęce infekcje. |
| Ludzki wirus niedoboru odporności (HIV) | Wirus przenoszony przez krew lub drogą płciową, który nieleczony powoduje zespół nabytego niedoboru odporności (AIDS) – potencjalnie śmiertelną chorobę wieloukładową. |
| Immunizacja | Kiedy dana osoba staje się chroniona przed chorobą w wyniku naturalnej infekcji lub szczepienia. |
| Odporność | Zdolność do obrony organizmu przed infekcją patogenem. Odporność nabyta opisuje, w jaki sposób organizm buduje pamięć immunologiczną – tak, że jeśli dana osoba zostanie ponownie narażona na tę samą infekcję, reakcja organizmu zostanie wzmocniona. Jest to podstawa do uodporniania się szczepionkami. |
| Zakres | Liczba nowych przypadków choroby w populacji w określonym przedziale czasu. Obliczanie współczynników zapadalności może wskazać, jak szybko choroba zakaźna pojawia się w populacji. |
| Wskaźnik śmiertelności infekcji | Odsetek osób chorych (zdiagnozowanych lub niezdiagnozowanych), które umierają z ich powodu. |
| Grypa (grypa) | Wirusowa infekcja dróg oddechowych, która zakaża ludzi na całym świecie i kilka innych gatunków żywicieli. Powoduje zarówno sezonowe, endemiczne fale infekcji, jak i, gdy pojawiają się nowe szczepy, na które populacja ma słabszą odporność, powoduje poważniejsze epidemie lub pandemie. |
| Oddział intensywnej terapii | Rodzaj oddziału szpitalnego, który zapewnia specjalistyczną opiekę nad krytycznie chorymi pacjentami, na przykład wentylację mechaniczną w przypadku niewydolności oddechowej. |
| Międzynarodowe przepisy zdrowotne | Prawnie wiążący instrument zapewniający nadrzędne ramy prawne dla obowiązków i obowiązków państw w obliczu zdarzenia lub sytuacji nadzwyczajnej dotyczącej zdrowia publicznego, które mogą mieć konsekwencje międzynarodowe. Sygnatariuszami jest 196 państw, w tym 194 państwa członkowskie Światowej Organizacji Zdrowia. |
| Interwencje | Wszelkie działania podejmowane w celu poprawy zdrowia ludzkiego poprzez zapobieganie chorobom, leczenie lub zmniejszanie ciężkości lub czasu trwania istniejącej choroby lub przywrócenie funkcji utraconych w wyniku choroby lub urazu. |
| Wspólny Komitet ds. Szczepień i Szczepień | Komitet naukowy doradzający brytyjskim departamentom zdrowia w zakresie szczepień. |
| W samą porę | Metoda kontroli zapasów, która kładzie nacisk na utrzymywanie zapasów na minimalnym poziomie i stosowanie krótkoterminowych, elastycznych umów, które można szybko dostosować do zmian popytu. |
| Gorączka Lassy | Wirusowa gorączka krwotoczna wywoływana przez wirusa Lassa. Choroba jest na ogół mniej dotkliwa niż wirus Ebola i jest przenoszona głównie przez wdychanie kurzu zanieczyszczonego odchodami szczurów lub kontakt z zakażonymi płynami ustrojowymi. |
| Główny departament rządowy | Departament rządowy odpowiedzialny za kierowanie pracami mającymi na celu identyfikację poszczególnych ryzyk i zapewnienie wdrożenia właściwych rozwiązań w zakresie planowania, reagowania i naprawy. |
| Stowarzyszenie Samorządowe | Krajowy organ członkowski władz lokalnych w Anglii i Walii. |
| Lokalne partnerstwa na rzecz odporności zdrowotnej | Lokalne partnerstwa na rzecz odporności zdrowotnej skupiają lokalne organizacje zajmujące się zdrowiem, regionalnych przedstawicieli Public Health England – a następnie brytyjską Agencję Bezpieczeństwa Zdrowia – i innych lokalnych interesariuszy. Są odpowiedzialni za identyfikację zagrożeń i opracowywanie planów związanych z gotowością, odpornością i reagowaniem w zakresie zdrowia i sytuacji kryzysowych, a także za współpracę z lokalnymi forami poświęconymi odporności. |
| Lokalne fora dotyczące odporności | Partnerstwa wieloagencyjne w Anglii i Walii składające się z lokalnych służb ratowniczych. Główny mechanizm w Anglii i Walii zapewniający gotowość na wypadek sytuacji kryzysowych i współpracę między agencjami. Ich głównym celem jest zapewnienie lokalnym służbom ratowniczym możliwości skutecznego działania w zakresie obowiązków nałożonych na nich na mocy ustawy o nieprzewidzianych zdarzeniach cywilnych z 2004 r. |
| Lokalni respondenci | Przedstawiciele lokalnych służb publicznych, w tym służb ratunkowych, władz lokalnych, NHS, Urzędu ds. Zdrowia i Bezpieczeństwa oraz innych organizacji zaangażowanych w przygotowanie na wypadek sytuacji kryzysowych. |
| Izolacja | Obowiązkowy nakaz pozostania w domu, prawny zakaz nakładania ogólnych ograniczeń na całą populację (poza określonymi czynnościami) w celu ograniczenia rozprzestrzeniania się choroby. |
| Malaria | Choroba pasożytnicza przenoszona na ludzi w endemicznych obszarach tropikalnych przez komary. |
| Choroba wirusowa Marburg | Choroba podobna do wirusa Ebola, która powoduje ciężką gorączkę krwotoczną i może przenosić się z osoby na osobę poprzez płyny ustrojowe. |
| Testowanie masowe | Stosowanie testów na dużej liczbie bezobjawowych osób w celu wykrycia osób zarażonych. |
| Bliskowschodni zespół oddechowy (MERS) | Choroba wywoływana przez MERS-CoV. |
| Koronawirus bliskowschodniego zespołu oddechowego (MERS-CoV) | Wirus układu oddechowego mający rezerwuar w wielbłądach dromaderach, który może również przenosić się z człowieka na człowieka. |
| Łagodzenie | Strategia mająca na celu zastosowanie ograniczonych, ale skutecznych interwencji w celu opóźnienia i zminimalizowania szczytu fal infekcji oraz zmniejszenia ich rozmiarów. Celem jest przede wszystkim rozłożenie presji na system opieki zdrowotnej na dłuższy okres, przy jednoczesnym zaakceptowaniu faktu, że w końcu zarażona zostanie podobna liczba osób. |
| Grupa Doradców Moralnych i Etycznych | Grupa doradcza zapewniająca rządowi Wielkiej Brytanii niezależne porady dotyczące kwestii moralnych, etycznych i wiary w kwestiach związanych ze zdrowiem i opieką społeczną. Zamknięte w październiku 2022 r. |
| Wskaźnik śmiertelności | Wyrażenie liczby zgonów z danej przyczyny podzielonej przez całą populację. |
| Narodowy Instytut Standardów i Kontroli Biologicznych | Agencja rządowa Wielkiej Brytanii zajmująca się ochroną i poprawą zdrowia publicznego poprzez zapewnienie jakości leków biologicznych. |
| Narodowy Instytut Badań nad Zdrowiem i Opieką (NIHR) | Jeden z głównych brytyjskich fundatorów badań nad zdrowiem i opieką, inwestujący w badania nad gotowością na pandemię, infrastrukturę badań klinicznych i projekty badawcze w stanie hibernacji. Do 2022 roku funkcjonował jako Narodowy Instytut Badań nad Zdrowiem. |
| Krajowe standardy odporności | Nieustawowe wytyczne dla lokalnych służb ratowniczych wydane przez Sekretariat ds. Zagrożeń Cywilnych. |
| Krajowa Ocena Ryzyka | Główne narzędzie rządu Wielkiej Brytanii umożliwiające identyfikację i ocenę najpoważniejszych sytuacji kryzysowych w kraju, przed którymi stoi Wielka Brytania w perspektywie pięciu lat. W 2019 r. zostało ono połączone z Oceną Ryzyka Bezpieczeństwa Narodowego. |
| Krajowy Rejestr Ryzyka | Dostępna publicznie wersja Oceny Ryzyka Bezpieczeństwa Narodowego, mająca na celu dostarczenie szczegółowych informacji osobom posiadającym formalne obowiązki w zakresie planowania awaryjnego na poziomie krajowym i lokalnym. |
| Doradca ds. Bezpieczeństwa Narodowego | Centralny koordynator i doradca Premiera oraz członków Rady Ministrów ds. bezpieczeństwa, wywiadu, obrony i niektórych spraw polityki zagranicznej. Kieruje Sekretariatem Bezpieczeństwa Narodowego. |
| Rada Bezpieczeństwa Narodowego | Główne forum zbiorowej dyskusji na temat celów rządu Wielkiej Brytanii w zakresie bezpieczeństwa narodowego. |
| Rada Bezpieczeństwa Narodowego (Odporność) | Podkomitet Rady Bezpieczeństwa Narodowego, który wspiera strategiczne i ściśle skoordynowane międzyrządowe podejście do zagrożeń i możliwości stojących przed Wielką Brytanią, ze szczególnym naciskiem na odporność. |
| Rada Bezpieczeństwa Narodowego (zagrożenia, niebezpieczeństwa, odporność i nieprzewidziane zdarzenia) | Podkomitet Rady Bezpieczeństwa Narodowego, który rozpatrywał kwestie związane z zagrożeniami bezpieczeństwa, zagrożeniami, odpornością i nieprzewidzianymi zdarzeniami cywilnymi. Skutecznie zniesione w lipcu 2019 r. |
| Ocena ryzyka bezpieczeństwa narodowego | Główne narzędzie oceny najpoważniejszych zagrożeń cywilnych stojących przed Wielką Brytanią. Ocenia, porównuje i ustala priorytety najważniejszych ryzyk na szczeblu krajowym, koncentrując się zarówno na prawdopodobieństwie wystąpienia ryzyka, jak i jego wpływie. |
| Sekretariat Bezpieczeństwa Narodowego | Zespół zapewniający koordynację kwestii bezpieczeństwa i wywiadu o strategicznym znaczeniu w całym rządzie. Doradza Radzie Bezpieczeństwa Narodowego, a na jej czele stoi Doradca ds. Bezpieczeństwa Narodowego. |
| Grupa doradcza ds. nowych i pojawiających się zagrożeń wirusami układu oddechowego (NERVTAG) | Ekspercki komitet naukowy Departamentu Zdrowia i Opieki Społecznej, który doradza dyrektorowi medycznemu, a za jego pośrednictwem rządowi Wielkiej Brytanii. Zapewnia naukową ocenę ryzyka i doradztwo w zakresie łagodzenia zagrożeń stwarzanych przez nowe i pojawiające się wirusy układu oddechowego oraz możliwości zarządzania nimi. |
| NHS Anglia | Wykonawczy pozaresortowy organ publiczny, sponsorowany przez Departament Zdrowia i Opieki Społecznej, który kieruje i nadzoruje NHS w Anglii. |
| (NHS) Testowanie i śledzenie | Usługa utworzona w maju 2020 r. w ramach Departamentu Zdrowia i Opieki Społecznej w celu przeprowadzania testów na obecność Covid-19 i ustalania kontaktów zakaźnych. Współpracując z władzami lokalnymi, skontaktował się z osobami, które uzyskały pozytywny wynik testu, oraz z ich niedawnymi kontaktami, aby zalecić im izolację, a także zapewnił monitorowanie telefoniczne i wsparcie. |
| Nipa | Może odnosić się do wirusa Nipah lub choroby, którą powoduje. Jej objawy mogą obejmować umiarkowane lub ciężkie choroby neurologiczne i oddechowe. Jego głównym naturalnym rezerwuarem są nietoperze owocożerne. W kilku krajach Azji Południowo-Wschodniej wystąpiły ogniska choroby, przenoszone przez świnie i nietoperze, a także w niektórych przypadkach z osoby na osobę. |
| Interwencje niefarmaceutyczne | Nielekowe środki ograniczające przenoszenie chorób zakaźnych. Mogą to być środki na poziomie indywidualnym, takie jak dystans fizyczny, stosowanie masek i osłon na twarz oraz ulepszone środki higieny. Mogą to być również środki ograniczające działalność, takie jak zamknięcie różnych obiektów, w tym obiektów sportowych, pubów czy sklepów. |
| Irlandia Północna Rodziny pogrążone w żałobie w związku z Covid-19 na rzecz sprawiedliwości | Oddział ogólnobrytyjskiej organizacji Rodziny pogrążone w żałobie w związku z Covid-19 na rzecz sprawiedliwości. Reprezentuje pogrążonych w żałobie członków rodzin osób, które zmarły na Covid-19 w Irlandii Północnej. |
| Dyrektor Irlandii Północnej | Władza wykonawcza Irlandii Północnej jest organem administracyjnym Zgromadzenia Irlandii Północnej, zdecentralizowanej władzy ustawodawczej Irlandii Północnej. Odpowiada za kwestie obejmujące przedsiębiorczość, handel i inwestycje, rolnictwo i rozwój obszarów wiejskich, edukację, zdrowie, policję i wymiar sprawiedliwości, środowisko i rozwój regionalny. |
| Grupa nadzorująca pandemię grypy w Irlandii Północnej | Założona w 2018 r. jednostka odpowiada za gotowość i reagowanie w zakresie opieki zdrowotnej i społecznej, a także nadzoruje opracowywanie wytycznych w zakresie nagłych zachorowań i segregacji w systemie opieki zdrowotnej i społecznej w Irlandii Północnej. Przewodniczy Dyrektor Zdrowia Publicznego. |
| Biuro Odpowiedzialności Budżetowej | Wykonawczy pozaresortowy organ publiczny, sponsorowany przez Skarb Państwa, który zapewnia niezależną analizę finansów publicznych Wielkiej Brytanii. |
| Urząd Statystyczny Krajowy | Największy w Wielkiej Brytanii niezależny producent oficjalnych statystyk i uznany krajowy instytut statystyczny Wielkiej Brytanii. |
| Operacja Yellowhammer | Plan awaryjny brytyjskiego rządu na wypadek wyjścia z Unii Europejskiej bez porozumienia. |
| Wybuch | Występowanie przypadków choroby w liczbie przekraczającej normalnie oczekiwaną w określonej społeczności, obszarze geograficznym lub sezonie. |
| Pandemia | Epidemia występująca na całym świecie lub na bardzo dużym obszarze, przekraczająca granice międzynarodowe i zwykle dotykająca dużą liczbę osób. |
| Rada ds. możliwości w zakresie chorób pandemicznych | Międzyrządowa rada, która pracowała nad zwiększeniem gotowości na szeroki zakres scenariuszy chorób pandemicznych. Zastąpił Radę ds. gotowości na pandemię grypy w lipcu 2021 r. |
| Rada ds. gotowości na pandemię grypy | Międzyrządowa rada powołana w celu nadzorowania gotowości na wypadek pandemii grypy w świetle wniosków wyciągniętych z ćwiczeń Cygnus. |
| Program gotowości na wypadek pandemii grypy | Ustanowiony przez Ministerstwo Zdrowia w 2007 r. jako program parasolowy obejmujący wszystkie działania mające na celu przygotowanie się na pandemię grypy i reagowanie na nią w systemie opieki zdrowotnej i społecznej |
| Patogeny | Organizmy zakaźne, takie jak wirusy, bakterie lub pasożyty, które mogą wywołać chorobę. |
| Generalny płatnik | Minister rządu oficjalnie odpowiedzialny za dokonywanie płatności rządowych. |
| Stała sekretarka | Starszy urzędnik służby cywilnej odpowiedzialny za bieżące zarządzanie departamentem rządowym. W rządzie Wielkiej Brytanii i Irlandii Północnej każdy departament rządowy ma stałego sekretarza. Każdy z rządów Szkocji i Walii ma jednego stałego sekretarza. |
| Sprzęt ochrony osobistej (ŚOI) | Sprzęt minimalizujący narażenie na zagrożenia. W opiece zdrowotnej i społecznej rozciąga się od artykułów podstawowych, takich jak fartuchy, fartuchy i rękawiczki jednorazowe, po artykuły specjalistyczne, takie jak przyłbice i maski oddechowe. |
| Gotowość i odporność | Stopień, w jakim rząd Wielkiej Brytanii i zdecentralizowane administracje były gotowe na sytuację nadzwyczajną, taką jak pandemia wirusa Covid-19, mogła wytrzymać ją i przystosować się do niej. |
| Rozpowszechnienie | Miara wyrażająca odsetek osób chorych w danym okresie lub w jego trakcie. Wskaźniki chorobowości oblicza się, dzieląc liczbę przypadków przez całkowitą liczbę osób w próbie. |
| Premier Wielkiej Brytanii | Lider rządu Wielkiej Brytanii, ostatecznie odpowiedzialny za politykę i decyzje rządu Wielkiej Brytanii. |
| Zdrowie publiczne | Nauka i sztuka zapobiegania chorobom, przedłużania życia i promocji zdrowia poprzez zorganizowane wysiłki społeczeństwa. |
| Stan nadzwyczajny zdrowia publicznego o zasięgu międzynarodowym | Formalne oznaczenie zadeklarowane przez Światową Organizację Zdrowia, nadające specjalny status w przypadku sytuacji nadzwyczajnej spowodowanej wybuchem choroby zakaźnej. Międzynarodowe przepisy zdrowotne określają, że jest to poważna, nagła, nietypowa lub nieoczekiwana epidemia, która niesie konsekwencje dla zdrowia publicznego poza granicami państwa dotkniętego chorobą i która może wymagać natychmiastowych działań międzynarodowych. |
| Zdrowie Publiczne Anglia | Agencja wykonawcza Departamentu Zdrowia i Opieki Społecznej do czasu jej zastąpienia przez brytyjską Agencję Bezpieczeństwa Zdrowia oraz Biuro ds. Poprawy Zdrowia i Rozbieżności w Zdrowiu w październiku 2021 r. Była odpowiedzialna za wszystkie aspekty zdrowia publicznego. |
| Służba Laboratorium Zdrowia Publicznego | Założona wraz z NHS w 1948 roku i nadzorowała sieć laboratoriów lokalnych, regionalnych i krajowych. Zniesiony w 2003 r., kiedy jego funkcje przejęła Agencja Ochrony Zdrowia. |
| Zdrowie Publiczne w Szkocji | Szkocki krajowy organ ds. zdrowia publicznego, którego zadaniem jest zapobieganie chorobom, przedłużanie zdrowego życia oraz promowanie zdrowia i dobrego samopoczucia. |
| Zdrowie publiczne Walia | Fundusz NHS, którego celem jest ochrona i poprawa zdrowia i dobrostanu oraz zmniejszanie nierówności zdrowotnych w Walii. |
| Kwarantanna | Okres izolacji mający na celu zmniejszenie ryzyka przeniesienia chorób zakaźnych przez przybywających podróżnych. Kwarantanna różni się od izolacji medycznej, podczas której izolowane są osoby z potwierdzonym przypadkiem choroby lub ich kontaktami. Te dwa terminy są często używane zamiennie. |
| Rozsądny najgorszy scenariusz | Narzędzie wykorzystywane do celów planowania w celu zilustrowania najgorszego przejawu ryzyka, którego potencjalnego wystąpienia można racjonalnie oczekiwać w oparciu o aktualne informacje i dane. |
| Regionalne partnerstwa na rzecz odporności/Lokalne partnerstwa na rzecz odporności | Kluczowe organy planowania i gotowości działające w Szkocji. Regionalne partnerstwa na rzecz odporności wspierają koordynację wielu agencji na poziomie regionalnym i składają się z kilku Lokalnych partnerstw na rzecz odporności, które wspierają lokalne ustalenia robocze i utrzymują lokalne kontakty. |
| Wydział Odporności i Sytuacji Nadzwyczajnych (obecnie nazywany Dyrekcją ds. Odporności i Odbudowy), Departament Wyrównywania Poziomów, Mieszkalnictwa i Społeczności | Pomógł ratownikom samodzielnie zidentyfikować ryzyko, na jakie się naraża, jak je złagodzić i jak zarządzać skutkami zaistniałego ryzyka. |
| Transmisja oddechowa | Zakażenie następuje przez usta lub nos z kropelek zawierających wirusa dowolnej wielkości. Przenoszenie przez drogi oddechowe czasami dzieli się na większe kropelki, które szybciej opadają na ziemię, oraz mniejsze kropelki, zwane aerozolami, które mogą pozostawać zawieszone w powietrzu przez dłuższy czas. |
| Gorączka Doliny Rift | Infekcja wirusowa, która może powodować łagodne lub poważniejsze objawy, w tym gorączkę krwotoczną. Zakażenie jest zwykle przenoszone przez kontakt z zakażonymi tuszami zwierząt lub przez ukąszenia komarów. Nie zgłoszono bezpośredniego przeniesienia wirusa z osoby na osobę. Wywołała epidemie w Afryce i na Półwyspie Arabskim. |
| Ryzyko | Możliwość wystąpienia szkodliwego zdarzenia. W kontekście gotowości i odporności cywilnej na sytuacje kryzysowe: zdarzenie, osoba lub przedmiot, które mogą spowodować utratę życia lub obrażenia, szkody w infrastrukturze, zakłócenia społeczne i gospodarcze lub degradację środowiska. |
| Ocena ryzyka | Systematyczny proces oceny prawdopodobieństwa wystąpienia potencjalnego ryzyka i potencjalnego wpływu, jaki miałoby ono, gdyby miało wystąpić. |
| Królewska Akademia Inżynierii | Organizacja charytatywna pełniąca funkcję krajowej Akademii Inżynierii i stowarzyszenia, które zapewnia przywództwo w dziedzinie inżynierii i technologii oraz przywództwo techniczne dla szerszego społeczeństwa. |
| Królewska Szkoła Pielęgniarstwa | Związek pielęgniarski i organizacja zawodowa. |
| Scenariusze | Narzędzie do oceny ryzyka polegające na opracowywaniu modeli tego, co może się wydarzyć w przyszłości, identyfikowaniu ryzyka oraz badaniu niepewności, konsekwencji i współzależności. |
| Naukowa Grupa Doradcza ds. Sytuacji Nadzwyczajnych (SAGE) | Grupa doradcza powołana w celu zapewnienia niezależnego doradztwa naukowego w celu wsparcia procesu decyzyjnego w COBR w przypadku stanu nadzwyczajnego w kraju. |
| Naukowa Grupa ds. Infekcji Pandemicznych ds. Modelowania (SPI-M) | Grupa doradcza Departamentu Zdrowia i Opieki Społecznej, która zapewnia rządowi Wielkiej Brytanii porady eksperckie w oparciu o modelowanie chorób zakaźnych i epidemiologię. Do 2022 roku była to Naukowa Grupa ds. Modelowania Grypy Pandemicznej. |
| Naukowa Grupa ds. Modelowania Zakażeń Pandemicznych, podgrupa operacyjna (SPI-MO) | Podgrupa operacyjna Naukowej Grupy ds. Modelowania Infekcji Pandemicznych, która spotyka się częściej w przypadku wystąpienia pandemii. Została utworzona podczas pandemii grypy H1N1 („świńskiej grypy”) w latach 2009–2010 i została ponownie uruchomiona podczas pandemii Covid-19. |
| Grupa Naukowych Analiz Pandemicznych ds. Zachowań (SPI-B) | Grupa ekspertów zapewniająca niezależne porady eksperckie z zakresu nauk społecznych i behawioralnych Naukowej Grupie Doradczej ds. Nagłych Wypadków (SAGE). |
| Szkocki Covid pogrążony w żałobie | Grupa reprezentująca pogrążonych w żałobie krewnych osób, które zmarły na Covid-19 w Szkocji. |
| Rząd Szkocji | Zdecentralizowana administracja Szkocji. |
| Szkockie partnerstwo na rzecz odporności | Grupa najstarszych ustawowych ratowników i kluczowych partnerów zajmujących się zwiększaniem odporności w Szkocji. Zapewnia zbiorowe gwarancje szkockim ministrom i ustawowym służbom ratowniczym oraz doradza społeczności zajmującej się odpornością, w jaki sposób najlepiej zapewnić Szkocji gotowość do skutecznego reagowania na poważne sytuacje kryzysowe. |
| sekretarz stanu | Minister gabinetu odpowiedzialny za departament rządowy. |
| Samoizolacja | Pozostanie w domu lub unikanie innych osób ze względu na podejrzenie lub potwierdzoną infekcję. |
| Wrażliwość | Prawdopodobieństwo, że osoba chora uzyska pozytywny wynik testu diagnostycznego. |
| Ciężki ostry zespół oddechowy (SARS) | Choroba wywołana przez SARS-CoV-1. |
| Koronawirus 1 ciężkiego ostrego zespołu oddechowego (SARS-CoV-1) | Koronawirus powodujący ciężki ostry zespół oddechowy. Uważa się, że pojawił się w 2002 r. na mokrym rynku w prowincji Guangdong w Chinach. Ściśle powiązany z SARS-CoV-2. |
| Koronawirus 2 ciężkiego ostrego zespołu oddechowego (SARS-CoV-2) | Koronawirus wywołujący chorobę Covid-19 (inną niż ciężki ostry zespół oddechowy (SARS)). |
| Zastawianie | Interwencja wprowadzona w celu wsparcia osób wyjątkowo bezbronnych klinicznie i w związku z tym uważanych za najbardziej narażone na poważną chorobę, na przykład Covid-19. |
| Skutki uboczne | Niepożądane skutki występujące podczas stosowania leku lub szczepionki, takie jak ból w miejscu wstrzyknięcia szczepionki. |
| Dystans społeczny | Środki mające na celu ograniczenie wzajemnych kontaktów, które mogą obejmować tymczasowe ograniczenie kontaktów towarzyskich w miejscach publicznych, takich jak wydarzenia rozrywkowe lub sportowe, ograniczenie korzystania z nieistotnego transportu publicznego lub zalecenie większej liczby pracy w domu. |
| Przedsiębiorstwo społeczne | Firma o celach głównie społecznych, której nadwyżki są głównie ponownie inwestowane w tym celu w firmę lub społeczność, a nie kieruje się potrzebą maksymalizacji zysku dla akcjonariuszy i właścicieli. |
| Stowarzyszenie Dyrektorów Władz Lokalnych (Solace) Cymru | Walijski oddział stowarzyszenia dyrektorów naczelnych i menedżerów wyższego szczebla władz lokalnych, sieci członkowskiej skupiającej specjalistów z sektora publicznego i władz lokalnych. |
| Hiszpańska grypa | Największa odnotowana pandemia grypy, która rozpoczęła się w 1918 r. |
| Tłumienie | Bardziej ekstremalna forma łagodzenia, na wzór blokady, której celem jest całkowite powstrzymanie transmisji. |
| Pojemność udarowa | Zdolność systemu opieki zdrowotnej do zarządzania nieprzewidywalnym i nagłym wzrostem zapotrzebowania na usługi zdrowotne i reagowania na nie. |
| Świńska grypa | Stosunkowo łagodna pandemia grypy, która rozpoczęła się w 2009 r. |
| Objawowy | Wykazuje objawy po infekcji. |
| Lecznictwo | Lek stosowany raczej w leczeniu niż zapobieganiu chorobie. |
| Kongres Związków Zawodowych | Federacja związków zawodowych w Anglii i Walii. |
| Przenośność | Zdolność patogenu, takiego jak wirus, do przenoszenia się z jednej osoby na drugą. |
| Przenoszenie | Proces, w wyniku którego patogen, taki jak wirus, przenosi się z jednej zakażonej osoby na drugą. |
| Skarb Państwa (HM Treasury) | Ministerialny departament rządowy pełniący funkcję ministerstwa gospodarki i finansów, utrzymujący kontrolę nad wydatkami publicznymi i wyznaczający kierunek polityki gospodarczej Wielkiej Brytanii. |
| Rząd Wielkiej Brytanii | Rząd centralny Wielkiej Brytanii, na którego czele stoi premier. Rząd Wielkiej Brytanii jest odpowiedzialny za niezdecentralizowane kwestie polityczne w całej Wielkiej Brytanii. (Rządy Szkocji, Rządu Walii i Wykonawcy Irlandii Północnej są odrębne od rządu Wielkiej Brytanii i są odpowiedzialne za zdecentralizowane kwestie polityczne w swoich krajach.) |
| Brytyjska Agencja Bezpieczeństwa Zdrowia | Agencja wykonawcza utworzona w kwietniu 2021 r. i sponsorowana przez Departament Zdrowia i Opieki Społecznej, odpowiedzialna za ochronę zdrowia publicznego i zdolność do zwalczania chorób zakaźnych. |
| Strategia gotowości na wypadek pandemii grypy w Wielkiej Brytanii w 2011 r | Strategia reagowania kryzysowego Wielkiej Brytanii w obliczu pandemii grypy. |
| Statystyk narodowy Wielkiej Brytanii | Główny doradca rządu Wielkiej Brytanii ds. statystyk oficjalnych. |
| Brytyjska sieć szczepionek | Sieć przedstawicieli przemysłu, środowisk akademickich i odpowiednich organów finansujących doradzająca Departamentowi Zdrowia i Opieki Społecznej w zakresie inwestycji badawczo-rozwojowych związanych z chorobami zakaźnymi, które mogą wywołać epidemię w krajach o niskich i średnich dochodach. |
| Brytyjska Grupa ds. Zoonoz, Chorób Zwierzęcych i Zakażeń | Niezależny komitet składający się z ekspertów z departamentów rolnictwa i zdrowia publicznego, który zapewnia strategiczny przegląd zapewniający ogólną koordynację zdrowia publicznego. |
| Szczepionka | Ochrona osób przed chorobą poprzez leczenie ich szczepionką. |
| Szczepionka | Szczepionki uczą układ odpornościowy rozpoznawania patogenu i obrony organizmu przed nim podczas następnego spotkania. |
| Wentylacja | Proces wprowadzania świeżego powietrza do pomieszczeń wewnętrznych z jednoczesnym usuwaniem zużytego powietrza. |
| Wentylator | Urządzenie podtrzymujące życie służące do mechanicznego wspomagania oddychania poprzez pompowanie powietrza do płuc pacjenta. |
| Wirusologia | Dyscyplina naukowo-medyczna zajmująca się zrozumieniem biologii wirusów i chorób wirusowych, ich leczeniem i zapobieganiem. |
| Wirus | Pasożytniczy czynnik zakaźny, który replikuje się wyłącznie wewnątrz komórek organizmu. |
| Mokry rynek | Targ, na którym sprzedaje się żywe zwierzęta. |
| Sytuacje kryzysowe w całym systemie | Najbardziej złożone sytuacje kryzysowe, które wymagają międzyresortowego podejścia rządu do zapewnienia gotowości i reagowania. |
| Światowa Organizacja Zdrowia | Wyspecjalizowana agencja Organizacji Narodów Zjednoczonych odpowiedzialna za międzynarodowe zdrowie publiczne. |
| Zika | Może odnosić się do wirusa Zika lub choroby, którą powoduje. Wirus przenoszony przez komary, który u większości zarażonych osób powoduje bardzo łagodną chorobę, jednak u kobiet w ciąży może prowadzić do poważnych wad mózgu u nienarodzonego dziecka. |
| Choroba odzwierzęca (zoonoza) | Choroby wywołane przez patogeny pochodzące od zwierząt innych niż ludzie. |
| Skutki odzwierzęce | Proces przenoszenia patogenu ze zwierząt na ludzi. |
Załącznik 4: Lista rekomendacji zawartych w niniejszym Raporcie
| A4.1. | W niniejszym raporcie dotyczącym modułu 1 dochodzenie przedstawia 10 zaleceń dotyczących odporności i gotowości Wielkiej Brytanii. |
Zalecenie 1: Uproszczona struktura gotowości i odporności cywilnej całego systemu na wypadek sytuacji kryzysowych
Rządy Wielkiej Brytanii, Szkocji, Walii i Irlandii Północnej powinny uprościć i zmniejszyć liczbę struktur odpowiedzialnych za przygotowanie i budowanie odporności na cywilne sytuacje kryzysowe obejmujące cały system.
Podstawowe struktury powinny być:
- pojedynczy komitet ministerialny na szczeblu gabinetu lub równoważny komitet ministerialny (w tym starszy minister odpowiedzialny za zdrowie i opiekę społeczną) odpowiedzialny za gotowość i odporność cywilną całego systemu na wypadek sytuacji kryzysowych w przypadku każdego rządu, który spotyka się regularnie i któremu przewodniczy lider lub zastępca lidera odpowiedniego rząd; I
- pojedyncza międzyresortowa grupa urzędników wyższego szczebla w każdym rządzie (która regularnie składa sprawozdania Radzie Ministrów lub równoważnej komisji ministerialnej) w celu nadzorowania i wdrażania polityki w zakresie gotowości i odporności cywilnej na sytuacje kryzysowe.
Należy to wdrożyć w ciągu 12 miesięcy od opublikowania niniejszego Sprawozdania.
W ciągu 6 miesięcy od utworzenia grupy urzędników wyższego szczebla powinna ona zakończyć przegląd mający na celu uproszczenie i zmniejszenie liczby struktur odpowiedzialnych za ogólnosystemową gotowość i odporność cywilną na sytuacje kryzysowe.
Następnie, w ciągu 24 miesięcy od publikacji niniejszego Raportu, komisja ministerialna powinna zracjonalizować i usprawnić podległe lub wspierające grupy i komitety odpowiedzialne za gotowość i odporność cywilną całego systemu. Wszelkie grupy i komitety powołane lub utworzone w celu wspierania tej podstawowej struktury powinny mieć jasny cel i powinny regularnie składać sprawozdania na temat postępów w realizacji powierzonych im zadań i ich zakończenia.
Zalecenie 2: Kierowanie Gabinetem Rady Ministrów w przypadku katastrof cywilnych obejmujących cały system w Wielkiej Brytanii
Rząd Wielkiej Brytanii powinien:
- znieść model wiodących departamentów rządowych w zakresie gotowości i odporności cywilnej całego systemu na wypadek sytuacji kryzysowych; I
- wymagać od Gabinetu Rady Ministrów kierowania przygotowaniami i budowaniem odporności na sytuacje kryzysowe cywilne w całym systemie we wszystkich departamentach rządu Wielkiej Brytanii, w tym monitorowaniem gotowości i odporności innych departamentów, wspieraniem departamentów w rozwiązywaniu problemów oraz eskalacją problemów do komisji ministerialnej na szczeblu gabinetu Wielkiej Brytanii oraz grupa urzędników wyższego szczebla w Zaleceniu 1.
Zalecenie 3: Lepsze podejście do oceny ryzyka
Rząd Wielkiej Brytanii i zdecentralizowane administracje powinny współpracować nad opracowaniem nowego podejścia do oceny ryzyka, które odejdzie od polegania na pojedynczych rozsądnych najgorszych scenariuszach w stronę podejścia, które:
- ocenia szerszy zakres scenariuszy reprezentatywnych dla różnych ryzyk i zakres każdego rodzaju ryzyka;
- oprócz radzenia sobie z jej konsekwencjami uwzględnia zapobieganie sytuacjom nadzwyczajnym i łagodzenie ich skutków;
- zapewnia pełną analizę sposobów, w jakie połączone skutki różnych zagrożeń mogą skomplikować lub pogorszyć sytuację nadzwyczajną;
- oprócz krótkoterminowych ocenia ryzyko długoterminowe i rozważa, w jaki sposób mogą one na siebie oddziaływać;
- dokonuje oceny wpływu każdego ryzyka na osoby bezbronne; I
- uwzględnia potencjał i możliwości Wielkiej Brytanii.
Czyniąc to, rząd Wielkiej Brytanii i zdecentralizowane administracje powinny przeprowadzić oceny ryzyka, które odzwierciedlają okoliczności i cechy charakterystyczne Anglii, Walii, Szkocji, Irlandii Północnej i Wielkiej Brytanii jako całości.
Zalecenie 4: Ogólnounijna strategia na wypadek sytuacji kryzysowych obejmująca cały system
Rząd Wielkiej Brytanii i zdecentralizowane administracje powinny wspólnie wprowadzić ogólnokrajową, całościową strategię cywilną na wypadek sytuacji nadzwyczajnych (która obejmuje pandemie), aby zapobiec każdej sytuacji nadzwyczajnej, a także ograniczyć, kontrolować i łagodzić jej skutki.
Strategia powinna co najmniej:
- być elastycznym;
- zawierać sekcje poświęcone każdej potencjalnej sytuacji nadzwyczajnej cywilnej obejmującej cały system – na przykład sekcję dotyczącą pandemii, z jasnym wyjaśnieniem ról i obowiązków rządu Wielkiej Brytanii, zdecentralizowanych administracji i ich departamentów/dyrekcji, a także lokalnych służb ratowniczych;
- rozważyć szeroki zakres potencjalnych scenariuszy dla każdego rodzaju sytuacji awaryjnej;
- zidentyfikować kluczowe problemy i określić zakres potencjalnych reakcji;
- określić, w jaki sposób należy zastosować strategię, aby zapewnić, że wszelkie potencjalne reakcje będą proporcjonalne do konkretnych okoliczności sytuacji nadzwyczajnej;
- obejmować ocenę krótko-, średnio- i długoterminową, opartą na opublikowanych modelach, potencjalnych skutków zdrowotnych, społecznych i gospodarczych sytuacji nadzwyczajnej oraz potencjalnych reakcji na sytuację nadzwyczajną dla ludności, a w szczególności osób bezbronnych; I
- obejmować ocenę infrastruktury, technologii i umiejętności, których Wielka Brytania potrzebuje, aby skutecznie reagować na sytuację nadzwyczajną, oraz ocenę tego, jak te potrzeby mogą się zmienić w zależności od różnych scenariuszy.
Strategia powinna podlegać ponownej merytorycznej ocenie co najmniej co trzy lata, aby zapewnić jej aktualność i skuteczność oraz uwzględniać wnioski wyciągnięte pomiędzy ponownymi ocenami.
Zalecenie 5: Dane i badania dotyczące przyszłych pandemii
Rząd Wielkiej Brytanii, współpracując z zdecentralizowanymi administracjami, powinien ustanowić mechanizmy terminowego gromadzenia, analizowania, bezpiecznego udostępniania i wykorzystywania wiarygodnych danych na potrzeby reagowania w sytuacjach kryzysowych przed przyszłymi pandemiami. Systemy danych należy przetestować w ćwiczeniach związanych z pandemią.
Rząd Wielkiej Brytanii powinien także zlecić szerszy zakres projektów badawczych, gotowych do rozpoczęcia w przypadku przyszłej pandemii. Mogą to być badania „hibernowane” lub istniejące badania, które zaprojektowano tak, aby można je było szybko dostosować do nowej epidemii. Należy zachęcać do lepszej współpracy z partnerami międzynarodowymi. Powinno to obejmować projekty mające na celu:
- zrozumieć powszechność występowania nowego wirusa;
- mierzyć skuteczność szeregu różnych środków w zakresie zdrowia publicznego; I
- określić, które grupy osób bezbronnych są najbardziej dotknięte pandemią i dlaczego.
Zalecenie 6: Regularne ćwiczenia w zakresie reagowania na pandemię w całej Wielkiej Brytanii
Rząd Wielkiej Brytanii i zdecentralizowane administracje powinny wspólnie przeprowadzać ogólnokrajowe ćwiczenia w zakresie reagowania na pandemię co najmniej co trzy lata.
Ćwiczenie powinno:
- przetestować ogólnokrajową, międzyrządową, krajową i lokalną reakcję na pandemię na wszystkich etapach, od początkowej epidemii po liczne fale na przestrzeni kilku lat;
- obejmować szeroki zakres osób zaangażowanych w przygotowanie i reagowanie na pandemię; I
- rozważyć, w jaki sposób w przypadku pandemii zostanie udzielona pomoc szerokiemu gronu bezbronnych osób.
Zalecenie 7: Publikacja wniosków i wniosków z ćwiczeń w sytuacjach zagrożenia cywilnego
W przypadku wszystkich ćwiczeń cywilnych w sytuacjach nadzwyczajnych rządy Wielkiej Brytanii, Szkocji, Walii i Irlandii Północnej powinny (chyba że względy bezpieczeństwa narodowego tego nie robią):
- publikuje sprawozdanie z ćwiczenia podsumowujące ustalenia, wnioski i zalecenia w ciągu trzech miesięcy od zakończenia ćwiczenia;
- publikuje plan działania określający konkretne kroki, które zostaną podjęte w odpowiedzi na ustalenia zawarte w raporcie oraz określający podmiot, w terminie sześciu miesięcy od zakończenia działania; I
- przechowuj raporty z ćwiczeń, plany działania oraz plany i wytyczne na wypadek sytuacji nadzwyczajnej z całej Wielkiej Brytanii w jednym, ogólnokrajowym archiwum internetowym, dostępnym dla wszystkich zaangażowanych w gotowość, odporność i reagowanie na sytuacje kryzysowe.
Zalecenie 8: Opublikowane raporty na temat gotowości i odporności cywilnej całego systemu na sytuacje kryzysowe
Rządy Wielkiej Brytanii, Szkocji, Walii i Irlandii Północnej powinny co najmniej co trzy lata sporządzać i publikować dla swoich odpowiednich organów ustawodawczych sprawozdania na temat gotowości i odporności cywilnej całego systemu na sytuacje kryzysowe.
Raporty powinny zawierać co najmniej:
- ryzyko zidentyfikowane przez każdy rząd prawdopodobnie doprowadzi do katastrof cywilnych w całym systemie;
- zalecenia wydane każdemu rządowi w celu ograniczenia tego ryzyka oraz informację, czy zalecenia te zostały przyjęte, czy odrzucone;
- analizę kosztów i korzyści określającą koszty gospodarcze i społeczne akceptacji ryzyka w porównaniu z podjęciem działań mających na celu jego złagodzenie;
- kto może być narażony na ryzyko i jakie kroki podejmuje się w celu ograniczenia tego ryzyka;
- plan określający harmonogram wdrożenia przyjętych zaleceń; I
- aktualizację dotyczącą postępów we wdrażaniu wcześniej przyjętych zaleceń.
Zalecenie 9: Regularne używanie czerwonych drużyn
Rządy Wielkiej Brytanii, Szkocji, Walii i Irlandii Północnej powinny wprowadzić w służbie cywilnej wykorzystanie czerwonych zespołów w celu kontrolowania i kwestionowania zasad, dowodów, polityk i porad dotyczących gotowości i odporności na cywilne sytuacje kryzysowe w całym systemie. Czerwone drużyny należy sprowadzić spoza rządu i służby cywilnej.
Zalecenie 10: Niezależny organ ustawowy działający w całej Wielkiej Brytanii zajmujący się gotowością i odpornością całego systemu na sytuacje kryzysowe
Rząd Wielkiej Brytanii powinien, w porozumieniu ze zdecentralizowanymi administracjami, utworzyć ustawowy niezależny organ odpowiedzialny za gotowość i odporność cywilną całego systemu na wypadek sytuacji kryzysowych.
Nowemu organowi należy powierzyć odpowiedzialność za:
- zapewnianie niezależnych, strategicznych porad rządowi Wielkiej Brytanii i zdecentralizowanym administracjom w zakresie planowania, gotowości i budowania odporności na sytuacje kryzysowe cywilne obejmujące cały system;
- konsultacje z sektorem wolontariatu, społeczności i przedsiębiorstw społecznych na poziomie krajowym i lokalnym oraz dyrektorami ds. zdrowia publicznego w sprawie ochrony osób bezbronnych w sytuacjach kryzysowych obejmujących cały system;
- ocena stanu planowania, gotowości i odporności na sytuacje kryzysowe cywilne obejmujące cały system w Wielkiej Brytanii; I
- formułowanie zaleceń dotyczących zdolności i zdolności, które będą wymagane w celu przygotowania się na sytuacje nadzwyczajne cywilne obejmujące cały system i budowania odporności na nie.
Jako środek tymczasowy należy ustanowić nowy organ na zasadach nieustawowych w ciągu 12 miesięcy od wydania niniejszego sprawozdania, aby mógł rozpocząć pracę przed przyjęciem przepisów.
E03069239
Alternatywne formaty
Raport ten jest również dostępny w wielu innych formatach.