A report by The Rt Hon the Baroness Hallett DBE Chair of the UK Covid-19 Inquiry
Presented to Parliament pursuant to section 26 of the Inquiries Act 2005
Ordered by the House of Commons to be printed 18 July 2024
HC 18
| Figure | Description |
|---|---|
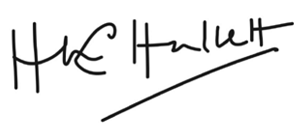
| Figure 1 | Pandemic preparedness and response central government structures in the UK and England - c. August 2019 |
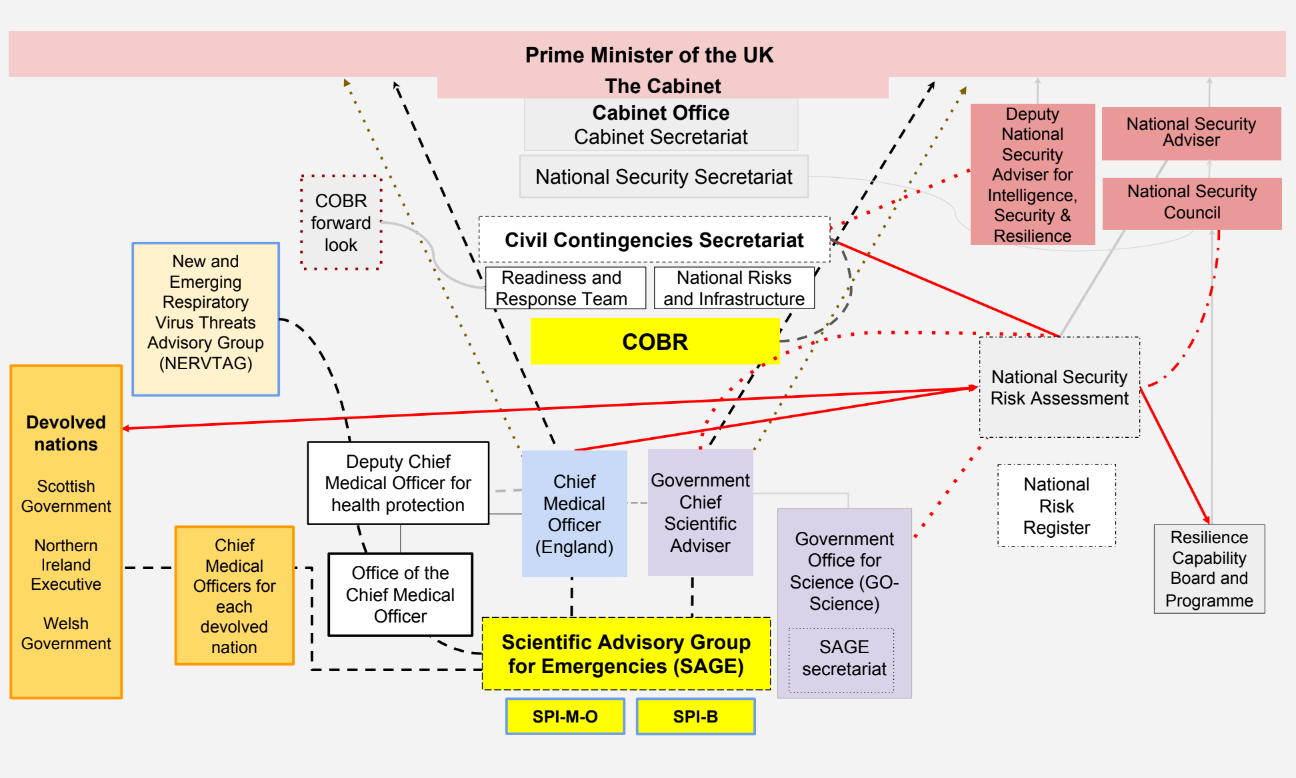
| Figure 2 | Pandemic preparedness and response structures in the UK and England – c. August 2019 |
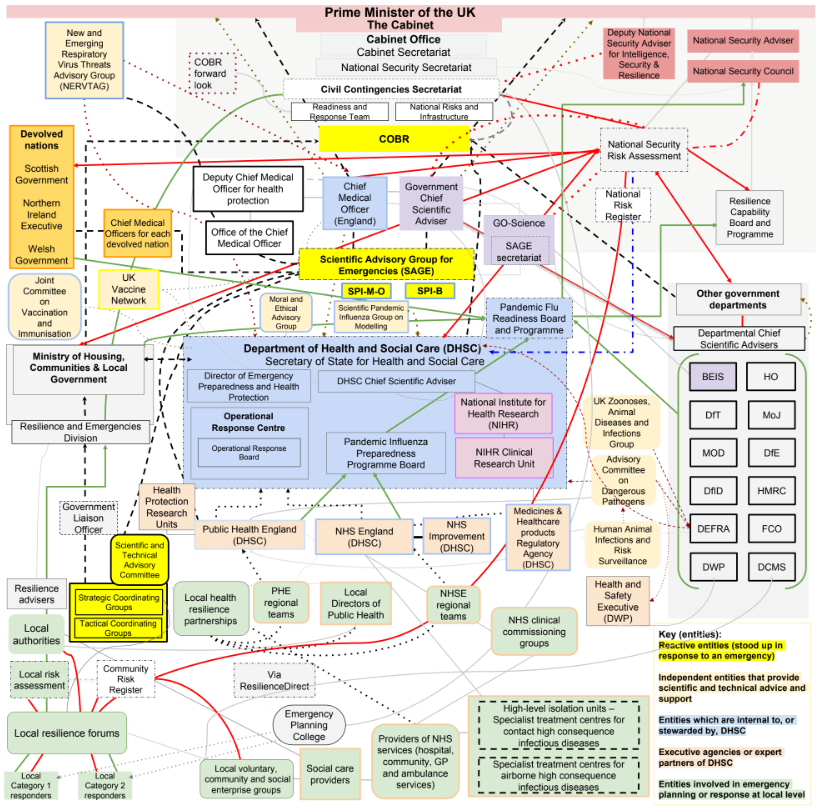
| Figure 3 | Pandemic preparedness and response central government structures in Scotland – c. 2019 |
| Figure 4 | Pandemic preparedness and response structures in Scotland – c. 2019 |
| Figure 5 | Pandemic preparedness and response central government structures in Wales – c. 2019 |
| Figure 6 | Pandemic preparedness and response structures in Wales – c. 2019 |
| Figure 7 | Pandemic preparedness and response central executive structures in Northern Ireland – c. 2019 |
| Figure 8 | Pandemic preparedness and response structures in Northern Ireland – c. 2019 |
| Figure 9 | A timeline of key exercises undertaken between 2003 and 2018 |
| Table | Description |
|---|---|
| Table 1 | Summary of past major epidemics and pandemics |
| Table 2 | Reasonable worst-case scenarios from UK risk assessments in 2014, 2016 and 2019 |
| Table 3 | Module 1 Core Participants |
| Table 4 | Module 1 expert witnesses |
| Table 5 | Module 1 witnesses from whom the Inquiry heard evidence |
| Table 6 | Module 1 Counsel team |
| Table 7 | Key simulation exercises relevant to pandemic preparedness and resilience |
Introduction by The Rt Hon the Baroness Hallett DBE
This is the first report of the UK Covid-19 Inquiry. It examines the state of the UK’s central structures and procedures for pandemic emergency preparedness, resilience and response.
The primary duty of the state is to protect its citizens from harm. It is, therefore, the state’s duty to ensure that the UK is as properly prepared to meet threats from a lethal disease as it is from a hostile force. Both are threats to national security.
In this case, the threat came from a novel and potentially lethal virus. In late December 2019, a cluster of cases of pneumonia of an unknown origin were detected in the city of Wuhan in the Hubei province of China. A new virus, a strain of coronavirus, was subsequently identified and named as severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2). The viral pathogen SARS-CoV-2 and the disease that it caused, Covid-19, spread across the globe.
It killed millions of people worldwide and infected many millions more. As at March 2024, the World Health Organization stated that there had been more than 774 million confirmed cases and over 7 million deaths reported globally, although the true numbers are likely to be far higher. The Covid-19 pandemic caused grief, untold misery and economic turmoil. Its impact will be felt for decades to come.
The impact of the disease did not fall equally. Research suggests that, in the UK, mortality rates were significantly higher among people with a physical or learning disability and people with pre-existing conditions, such as dementia and Alzheimer’s disease, heart disease, high blood pressure and diabetes. People from some ethnic minority groups and those living in deprived areas had a significantly higher risk of being infected by Covid-19 and dying from it.
Beyond the individual tragedy of each and every death, the pandemic placed extraordinary levels of strain on the UK’s health, care, financial and educational systems, as well as on jobs and businesses.
As in many other countries, the UK government and the governments of Scotland, Wales and Northern Ireland were required to take serious and far-reaching decisions about how to contain and respond to the virus. The 23 March 2020 decision to implement a legally enforced ‘stay at home’ order was hitherto unimaginable.
The life of the UK was severely curtailed as the majority of its citizens were confined to home. Almost every area of public life across all four nations was badly affected. The hospitality, retail, travel and tourism, arts and culture, and sport and leisure sectors effectively ceased to operate. Even places of worship closed.
Levels of mental illness, loneliness, deprivation and exposure to violence at home surged. Children missed out on academic learning and on precious social development.
The cost, in human and financial terms, of bringing Covid-19 under control has been immense. Government borrowing and the cost of procurement and of the various job retention, income, loan, sick pay and other support schemes have severely impacted public finances and the UK’s financial health.
The impact on the NHS, its operations, its waiting lists and on elective care has been similarly immense. Millions of patients either did not seek or did not receive treatment and the backlog for treatment has reached historically high levels.
Societal damage has been widespread, with existing inequalities exacerbated and access to opportunity significantly weakened.
Ultimately, the UK was spared worse by the individual efforts and dedication of health and social care workers and the civil and public servants who battled the pandemic; by the scientists, medics and commercial companies who researched valiantly to produce life-saving treatments and ultimately vaccines; by the local authority workers and volunteers who looked after and delivered food and medicine to elderly and vulnerable people, and who vaccinated the population; and by the emergency services, transport workers, teachers, food and medicinal industry workers and other key workers who kept the country going.
Unfortunately, the expert evidence suggests that they will be called upon again. It is not a question of ‘if’ another pandemic will strike but ‘when’. The evidence is overwhelmingly to the effect that another pandemic – potentially one that is even more transmissible and lethal – is likely to occur in the near to medium future. Unless the lessons are learned, and fundamental change is implemented, that effort and cost will have been in vain when it comes to the next pandemic.
There must be radical reform. Never again can a disease be allowed to lead to so many deaths and so much suffering.
It is into these extreme events and consequences that it is my duty to inquire. In May 2021, then Prime Minister Boris Johnson MP announced his decision to establish a statutory inquiry to examine the UK’s preparedness and response to the Covid-19 pandemic and learn lessons for the future. I was appointed Chair of the Inquiry in December 2021.
The extremely broad Terms of Reference for this Inquiry were drawn up following formal consultation between the Prime Minister and the First Ministers of Scotland and Wales and the First Minister and deputy First Minister of Northern Ireland. There was then an extensive public consultation process.
I consulted widely across all four nations, visiting towns and cities in England, Wales, Scotland and Northern Ireland and speaking, in particular, to a number of bereaved people. In parallel, the Inquiry team met with representatives of more than 150 organisations in ‘roundtable’ discussions. In total, the Inquiry received more than 20,000 responses to the consultation.
In light of the views expressed, the Inquiry recommended a number of significant changes to the draft Terms of Reference. These were accepted in full and included explicit acknowledgement of the need to hear about people’s experiences and to consider any disparities in the impact of the pandemic.
The unprecedented width and scope of the Terms of Reference therefore commanded public support.
I also sought an express mandate to publish interim reports so as to ensure that any urgent recommendations could be published and considered in a timely manner. It is plainly in the public interest that effective recommendations are made as quickly as possible to ensure that proper emergency preparedness and resilience structures and systems are in place before the next pandemic or national civil emergency.
The Terms of Reference reflect the unprecedented complexity of this Inquiry. It is not an inquiry limited in scope by a single event, a short passage of time or a single policy or finite course of government or state conduct. It is an inquiry into how the gravest and most multi- layered peacetime emergency struck an entire country (in fact, four countries) and how the UK government and devolved administrations responded, across almost the entire range of their decision-making and public functions. The pandemic and the response spared no part of British life and so there is almost no part of that life excluded from our investigations.
I was determined from the outset that this Inquiry would not drag on for years and produce a report or reports long after they had lost any relevance. The Inquiry has therefore proceeded at great pace.
On 21 July 2022, about five months following the ending of Covid-19 legal restrictions on the population of the UK, the Inquiry was formally opened. I also announced the decision to conduct the Inquiry in modules. The first public hearing, Module 1 (Resilience and preparedness), took place less than a year later, between 13 June and 20 July 2023.
The hearing was preceded by an extensive and complex process of obtaining under compulsion potentially relevant documents from a wide range of sources. This material was then examined by the Inquiry team, and more than 18,000 documents were deemed to be relevant and were disclosed to the Core Participants to assist them in their preparation for the hearing.
The Module 1 Inquiry team obtained more than 200 witness statements and called 68 factual and expert witnesses from the UK government, the devolved administrations, resilience and health structures, civil society groups and groups representing bereaved people.
The public hearing for Module 2 (Core UK decision-making and political governance) then took place between 3 October and 13 December 2023. The analogous public hearings into the core political and administrative decision-making of the Scottish, Welsh and Northern Irish governments took place, respectively, between 16 January and 1 February 2024, 27 February and 14 March 2024, and 30 April and 16 May 2024.
As at the publication date of this Report, Module 3 (Impact of the Covid-19 pandemic on healthcare systems in the four nations of the UK), Module 4 (Vaccines and therapeutics), Module 5 (Procurement), Module 6 (Care sector), Module 7 (Test, trace and isolate), Module 8 (Children and young people) and Module 9 (Economic response) have all been formally opened and are in the course of being prepared for public hearings. There will also be further hearings into the impact that the pandemic and the response had on various aspects of British life.
No inquiry with such a wide scope has ever proceeded with such speed or rigour, or obtained so much relevant documentation in such a relatively limited amount of time. It is right to say that few countries have established formal legal inquiries investigating the many aspects of the Covid-19 pandemic, let alone inquiries of this scale. A number of countries, such as Sweden, Norway, Denmark and Australia, have instead instituted independent commissions led by experts in epidemiology, public health, economics and public policy. Such research commissions may be quicker and cheaper than a UK statutory inquiry, but they are not necessarily legal processes with the force of the law behind them. Most do not have the powers to compel the production of evidence or the giving of sworn testimony by political and administrative leaders; they are not open to public scrutiny in the same way as this Inquiry; they do not allow bereaved people and other interested groups to participate meaningfully in the process as legal core participants; and they do not have anything like the same scope or depth.
It may be thought therefore that a statutory inquiry with extensive powers was the right and only appropriate vehicle for an inquiry considering a national crisis of such scale and intensity, and one involving so much death and suffering. The people of the UK, but especially bereaved people and those who have otherwise suffered harm, need to know whether anything could reasonably have been done better.
If the Inquiry’s recommendations are implemented, the risk of loss and suffering in the future will be reduced, and policy-makers, faced with extraordinarily difficult decisions, will be assisted in responding to a crisis.
I want to express my gratitude to all those who have given so much of their time and resources in providing the Inquiry with the voluminous amount of documentary material, to the many people who have provided their assistance through the provision of written statements and sworn evidence, and to all who have shared their experience of the pandemic with the Inquiry through its listening exercise, Every Story Matters. I would also like to thank the Module 1 team (both secretariat and legal) without whose extraordinarily hard work the Module 1 hearings and this Report would not have been possible.
I am also very grateful to the Core Participants and their legal teams, especially the groups representing bereaved people, for their insightful and conscientious contribution to the Inquiry process. The determination and drive of their clients and representatives, and the skill and experience of their legal teams, continue to be of invaluable assistance to me and to the Inquiry team.
The harrowing testimony of loss and grief given by the bereaved witnesses and others who suffered during the pandemic provided a salutary confirmation of the purpose of this Inquiry.
The Rt Hon the Baroness Hallett DBE
18 July 2024
Voices of those bereaved
Dad was an incredibly popular man, and it was a source of great pain for everybody that knew him that they would not be able to attend his funeral. Only ten people were allowed there on the day, all had to be socially distanced, due to those limitations, and as an illustration of how popular my dad was and the impact that he had on the people around him, over 300 people lined the streets for the procession ... In my dad’s case, we were offered the chance to have a phone call – I say a phone call, a video call with my dad in hospital to say our goodbyes, which is something that I didn’t take the hospital up on, as that’s not how I want to remember my dad. Some of the last photos I had of him are him sitting in his hospital bed wearing his oxygen mask and I would prefer not to remember him like that and instead to remember him how he was in life.”¹
“It was actually five days from the onset of Covid until she died ... in that time the Covid destroyed her lungs, her kidneys, her liver and her pancreas. They tried to give her dialysis, but the Covid had made her blood so thick and sticky that it actually blocked the dialysis machine ... they told her and myself that she wasn’t a candidate for ICU [intensive care unit] and intubation and told us both that she was dying, and there was nothing, sadly, that they could do to help her ... it was the terrible decisions you had to make about who could go and who couldn’t, and of course if someone had been with their loved one at the end, they were often told by some hospitals, ‘You have a choice: you can either come in and be with them at the end or you can go to the funeral, but you can’t do both, because you have to be in isolation.’”²
“Something that was not communicated to us was that once somebody with Covid dies, they are almost treated like toxic waste. They are zipped away and you – nobody told us that you can’t wash them, you can’t dress them, you can’t do any of those things, the funerals, the ceremonies, you just can’t do any of those. You couldn’t sing at a funeral. You know, we’re Welsh, that’s something you have to do ... my dad did not have a good death. Most of our members’ loved ones did not have a good death ... when we left the hospital, my dad – we were given my dad’s stuff in a Tesco carrier bag. Some people were given somebody else’s clothes that were in a pretty awful state. It’s those things like that that don’t often get considered ... there is such a thing as a good death, and I think that was very overlooked during the pandemic ... there is a whole generation, my mum’s generation, who haven’t got the mechanisms like maybe I have to complain and question, and they are heartbroken and really in shock. You know, my mum cries daily and – even though it’s nearly three years ... it’s just – they’re just left with that feeling of nobody cared.”³
“When we took mummy up into the hospital, there was very limited – just a plastic apron on staff, and my sister actually asked about Covid, and we were told not to worry, it would be a flash in the pan and gone by the summer ... I am here to remind everybody of the human cost that we paid as bereaved people. My mummy was not cannon fodder. My mummy was a wonderful wee woman who had the spirit of Goliath, and I know she’s standing here with me today, because she would want me to be here, because she knows that she lived a life, as did all our loved ones, and it’s very important that we remember the human cost, because there are too many people out there now that think Covid has gone away. People are still losing their life to Covid.”⁴
Executive summary
In 2019, it was widely believed, in the UK and abroad, that the UK was not only properly prepared but was one of the best-prepared countries in the world to respond to a pandemic. This Report concludes that, in reality, the UK was ill prepared for dealing with a catastrophic emergency, let alone the coronavirus (Covid-19) pandemic that actually struck.
In 2020, the UK lacked resilience. Going into the pandemic, there had been a slowdown in health improvement, and health inequalities had widened. High pre-existing levels of heart disease, diabetes, respiratory illness and obesity, and general levels of ill-health and health inequalities, meant that the UK was more vulnerable. Public services, particularly health and social care, were running close to, if not beyond, capacity in normal times.
The Inquiry recognises that decisions as to the allocation of resources to prepare for a whole-system civil emergency fall exclusively to elected politicians. They must grapple with competing demands for public money and limited resources. It may be tempting for them to focus on the immediate problem before them rather than dwell on what may or may not happen. Proper preparation for a pandemic costs money. It involves preparing for an event that may never happen. However, the massive financial, economic and human cost of the Covid-19 pandemic is proof that, in the area of preparedness and resilience, money spent on systems for our protection is vital and will be vastly outweighed by the cost of not doing so.
Had the UK been better prepared for and more resilient to the pandemic, some of that financial and human cost may have been avoided. Many of the very difficult decisions policy-makers had to take would have been made in a very different context. Preparedness for and resilience to a whole-system civil emergency must be treated in much the same way as we treat a threat from a hostile state.
The Inquiry found that the system of building preparedness for the pandemic suffered from several significant flaws:
- The UK prepared for the wrong pandemic. The significant risk of an influenza pandemic had long been considered, written about and planned for. However, that preparedness was inadequate for a global pandemic of the kind that struck.
- The institutions and structures responsible for emergency planning were labyrinthine in their complexity.
- There were fatal strategic flaws underpinning the assessment of the risks faced by the UK, how those risks and their consequences could be managed and prevented from worsening, and how they could be responded to.
- The UK government’s sole pandemic strategy, from 2011, was outdated and lacked
adaptability. It was virtually abandoned on its first encounter with the pandemic. It focused on only one type of pandemic, failed adequately to consider prevention or proportionality of response, and paid insufficient attention to the economic and social consequences of pandemic response. - Emergency planning generally failed to account sufficiently for the pre-existing health and societal inequalities and deprivation in society. There was also a failure to appreciate the full extent of the impact of government measures and long-term risks, from both the pandemic and the response, on ethnic minority communities and those with poor health or other vulnerabilities, as well as a failure to engage appropriately with those who know their communities best, such as local authorities, the voluntary sector and community groups.
- There was a failure to learn sufficiently from past civil emergency exercises and outbreaks of disease.
- There was a damaging absence of focus on the measures, interventions and infrastructure required in the event of a pandemic – in particular, a system that could be scaled up to test, trace and isolate in the event of a pandemic. Despite reams of documentation, planning guidance was insufficiently robust and flexible, and policy documentation was outdated, unnecessarily bureaucratic and infected by jargon.
- In the years leading up to the pandemic, there was a lack of adequate leadership, coordination and oversight. Ministers, who are frequently untrained in the specialist field of civil contingencies, were not presented with a broad enough range of scientific opinion and policy options, and failed to challenge sufficiently the advice they did receive from officials and advisers.
- The provision of advice itself could be improved. Advisers and advisory groups did not have sufficient freedom and autonomy to express dissenting views and suffered from a lack of significant external oversight and challenge. The advice was often undermined by ‘groupthink’.
The Inquiry has no hesitation in concluding that the processes, planning and policy of the civil contingency structures within the UK government and devolved administrations and civil services failed their citizens.
The Module 1 Report recommends fundamental reform of the way in which the UK government and the devolved administrations prepare for whole-system civil emergencies. Although each recommendation is important in its own right, all the recommendations must be implemented in concert so as to produce the changes that the Inquiry judges to be necessary.
Later modules will specifically report and make recommendations in relation to the preparedness of three particular aspects of the UK’s preparedness and response structures: test, trace and isolate schemes; government stockpiles and procurement of personal protective equipment (PPE); and vaccine availability.
This first Report recommends, in summary, the following:
- Each government should create a single Cabinet-level or equivalent ministerial committee (including the senior minister responsible for health and social care) responsible for whole-system civil emergency preparedness and resilience, to be chaired by the leader or deputy leader of the relevant government. There should also be a single cross-departmental group of senior officials in each government to oversee and implement policy on civil emergency preparedness and resilience.
- The lead government department model for whole-system civil emergency preparedness and resilience is not appropriate and should be abolished.
- The UK government and devolved administrations should develop a new approach to risk assessment that moves away from reliance on reasonable worst-case scenarios towards an approach that assesses a wider range of scenarios representative of the different risks and the range of each kind of risk. It should also better reflect the circumstances and characteristics particular to England, Scotland, Wales, Northern Ireland and the UK as a whole.
- A new UK-wide whole-system civil emergency strategy should be put in place and it should be subject to a substantive reassessment at least every three years to ensure that it is up to date and effective, and incorporates lessons learned from civil emergency exercises.
- The UK government and devolved administrations should establish new mechanisms for the timely collection, analysis, secure sharing and use of reliable data for informing emergency responses, such as data systems to be tested in pandemic exercises. In addition, a wider range of ‘hibernated’ and other studies should be commissioned that are designed to be rapidly adapted to a new outbreak.
- The UK government and devolved administrations should hold a UK-wide pandemic response exercise at least every three years.
- Each government should publish a report within three months of the completion of each civil emergency exercise summarising the findings, lessons and recommendations, and should publish within six months of the exercise an action plan setting out the specific steps to be taken in response to the report’s findings. All exercise reports, action plans, emergency plans and guidance from across the UK should be kept in a single UK-wide online archive, accessible to all involved in emergency preparedness, resilience and response.
- Each government should produce and publish a report to their respective legislatures on whole-system civil emergency preparedness and resilience at least every three years.
- External ‘red teams’ should be regularly used in the Civil Service of the UK government and devolved administrations to scrutinise and challenge the principles, evidence, policies and advice relating to preparedness for and resilience to whole-system civil emergencies.
- The UK government, in consultation with the devolved administrations, should create a UK-wide independent statutory body for whole-system civil emergency preparedness, resilience and response. The body should provide independent, strategic advice to the UK government and devolved administrations, consult with the voluntary, community and social enterprise sector at a national and local level, as well as with directors of public health, and make recommendations.
Chapter 1: A brief history of epidemics and pandemics
Introduction
| 1.1. | To assess the state of a nation’s preparedness for a pandemic, one must first assess the nature of the risk, the likelihood of its occurring and the impact of the risk if it does occur. This chapter considers a brief history of epidemics and pandemics to put the likelihood and the possible impact into context. |
| 1.2. | Epidemics and pandemics have occurred throughout recorded human history.1 They were and remain a substantial and increasing risk to the safety, security and wellbeing of the UK.2 The coronavirus (Covid-19) pandemic is estimated to have caused approximately 22 million excess deaths globally.3 Official UK figures put the number of deaths involving Covid-19 in the four nations of the UK at over 225,000 in June 2023.4 Nothing on this scale has been seen in more than a century. |
Past major epidemics and pandemics
| 1.3. | There is an inherent uncertainty and unpredictability about disease outbreaks, but the Covid-19 pandemic was not without precedent. As set out in Table 1, major epidemics and pandemics (an epidemic of an infection occurring worldwide or over a very wide area, usually affecting a large number of people) are far from unknown.5 |
| Time period | Pathogen | Disease (colloquial or common name) | Global cases (attack rate) | Global deaths | UK cases | UK deaths | Case fatality ratio* | Route of transmission | Asymptomatic infection widespread? | Probable origin |
|---|---|---|---|---|---|---|---|---|---|---|
| 1889 to 1894 | Uncertain. HCoV-OC43 or influenza | Russian flu | Became endemic (>90%)* | 1m* | Became endemic (>90%) | 132,000 | 0.1–0.28% | Respiratory | Unknown but probable | Central Asia |
| 1918 to 1920 | Influenza: H1N1 | Spanish flu | Became endemic (>90%) | 50m* | Became endemic (>90%) | 228,000 | 2.5–10% | Respiratory | Yes | USA (or, less likely, China/France) |
| 1957 to 1959 | Influenza: H2N2 | Asian flu | Became endemic (>90%)* | 1.1m | Became endemic (>90%)* | 5,000* | 0.017–0.1% | Respiratory | Yes | China |
| 1968 to 1970 | Influenza: H3N2 | Hong Kong flu | Became endemic (>90%) | 2m | Became endemic (>90%) | 37,500* | 0.1–0.2% | Respiratory | Yes | Hong Kong or China |
| 1977 to 1978 | Influenza: H1N1 | Russian flu | Became endemic (>90%) | 700,000 | Became endemic (>90%) | 6,000* | <0.1% | Respiratory | Yes | China or Russia (not zoonotic)* |
| 1981 onwards | Retrovirus: HIV | AIDS | 84.2m cumulative, 38.4m now (0.7%) | 40.1m | 165,338 | 25,296 | ~99% [untreated] | Blood-borne/sexual | Yes | West Central Africa (first detected USA) |
| 2002 to 2003 | Coronavirus: SARS-CoV-1 | SARS | 8,096 (<0.001%) | 774 | 4 | 0 | 9.6% | Respiratory | No | China |
| 2009 to 2010 | Influenza: H1N1 | Swine flu | Became endemic (first wave ~24%) [491,382 official]* | 284,000 [18,449 official] | Became endemic (>90%) [28,456 official]* | 457 [official] | 0.01–0.02% | Respiratory | Yes | Mexico (first detected USA) |
| 2012 onwards | Coronavirus: MERS-CoV | MERS | 2,519 (<0.001%) | 866 | 5 | 3 | 34.3% | Respiratory | Not initially, but more reports over time | Saudi Arabia |
| 2013 to 2016 | Ebola virus: EBOV | Ebola | 28,616 (<0.001%) | 11,310 | 3 | 0 | 62.9% | Contact | No | Guinea |
| 2019 onwards | Coronavirus: SARS-CoV-2 | Covid-19 | Becoming endemic as of 2023 (>90%) | 22m | Becoming endemic (>90%) [22m official] | 225,668 [official] | 0.67–1.18% [infection fatality ratio] | Respiratory | Yes | China |
All figures are approximate. They are estimates derived from published research available before 2020, apart from sources for SARS-CoV-2. Figures may not be strictly comparable and methodological quality varies. Asterisks denote particularly important caveats (see INQ000207453). Further details, including all caveats and references, are in the full table: INQ000207453.
| 1.4. | Two types of zoonotic pathogens are of particular concern when preparing for epidemics and pandemics: virus strains of pandemic influenza and coronaviruses. In addition, there is always the possibility of ‘Disease X’, a hypothetical emerging future pathogen currently not known to cause human disease with the potential to cause a pandemic, whatever its origins.⁶ Covid-19, when it emerged, was a ‘Disease X’.⁷ |
Pandemic influenza
| 1.5. | Pandemic influenza is caused by a novel influenza virus that is different from the usual circulating strains.⁸ It has caused repeated pandemics that have varied in terms of magnitude, severity and impact, and is notoriously difficult to predict.⁹ For example, the ‘Spanish flu’ pandemic of 1918 to 1920, which was caused by an H1N1 influenza strain, is estimated to have killed approximately 50 million people worldwide and 228,000 in the UK.¹⁰ The 2009 to 2010 H1N1 influenza pandemic (‘swine flu’), by contrast, had a significantly smaller impact than typical influenza seasons.¹¹ |
| 1.6. | Prior to the Covid-19 pandemic, the focus of the UK’s pandemic preparedness and resilience was on influenza. This was and remains the single biggest predictable pathogen risk.¹² Although it was understandable for the UK to prioritise pandemic influenza, this should not have been to the effective exclusion of other potential pathogen outbreaks. These too have been increasing in number. |
Coronaviruses
| 1.7. | Coronaviruses in humans were seen only to be a relatively benign group of circulating viruses that caused mild respiratory illnesses (ie common colds) in the majority of people.¹³ It was not until late 2002 that human coronaviruses became a cause for global concern.¹⁴ Severe acute respiratory syndrome (SARS) is thought to have emerged from an animal in a live animal ‘wet market’ in the Guangdong province of China sometime in late 2002.¹⁵ It was the first new severe disease transmissible from person to person to emerge in the 21st century, and caused outbreaks in multiple countries.¹⁶ In June 2012, in Saudi Arabia, Middle East respiratory syndrome coronavirus (MERS-CoV) was first identified following transmission of the infection from camels to humans.¹⁷ In May 2015, a major outbreak of MERS-CoV occurred in healthcare facilities in South Korea when an infected person returned home from the Middle East.¹⁸ |
Outbreaks of disease
| 1.8. | There are a number of ways in which epidemics and pandemics may emerge. In humans, novel infectious diseases are predominantly caused by zoonotic spillover.¹⁹ This generally occurs when humans come into close contact with infected animals or animal products and a pathogen crosses the species barrier from animals to humans.²⁰ The world is teeming with organisms that have not yet found their way into the human population. Globally, there are thought to exist more than 1.5 million undescribed viruses in mammals and birds, of which about 750,000 are thought to have the potential to spill over into humans and cause epidemics.²¹ As of 2020, there were more than 200 known zoonotic pathogens.²² These range in impact from those that are completely harmless to humans to those with pandemic potential and devastating consequences. |
| 1.9. | Professor Jimmy Whitworth and Dr Charlotte Hammer, expert witnesses on infectious disease surveillance (see Appendix 1: The background to this module and the Inquiry’s methodology), explained that the possibility of novel pathogens making the leap from animals to humans had increased in recent decades.²³ This was due to a number of factors, including urbanisation and globalisation, which increase the likelihood of pathogens transmitting from one part of the world to another and the speed with which they will do so.²⁴ |
| 1.10. | The more interconnected the world becomes, the more likely it is that pathogens that emerge in one part of the world will spread to another.²⁵ The more ecological change and development there is at the interface between humans and the natural world, the greater the probability that pathogens will make the leap from animals to humans.²⁶ The more laboratories there are in the world that are involved in biological research, the more chance there is that leaks from laboratories will occur with ramifications for the population at large.²⁷ Increased instability between and within nations increases the biological security threat.²⁸ The risk of new pathogens arising and spreading in the human population is only likely to increase. The key characteristics of pathogens with pandemic potential are high adaptability, high transmissibility and becoming infectious before the host has developed symptoms or in the absence of any symptoms.²⁹ It is on those characteristics, as well as the critically important case fatality ratio, that the UK’s systems of preparedness and resilience should be focused. |
| 1.11. | Laboratory accidents and the malicious use of biological material are less frequent and less likely to be publicly acknowledged than zoonotic spillover, but their consequences may be just as lethal.³⁰ While novel pathogens are not the only potential biological or civil emergency risk faced by the UK, it is clear that the risk of pathogenic outbreaks must be taken very seriously by society and governments, and proper preparations made. |
| 1.12. | While the primary routes of transmission for pandemic influenza and coronaviruses are airborne and respiratory, there are – and will be in the future, including for novel pathogens – other potential routes of transmission.³¹ These may include: oral – through water or food (eg cholera and typhoid); vector-borne – carried by insects or arachnids (eg malaria and Zika virus); and contact – by touch (eg Ebola virus disease).³² Prior to Covid-19, the last major pandemic with significant mortality had been caused by human immunodeficiency virus (HIV), which has killed more than 40 million people worldwide to date and more than 25,000 people in the UK.³³ HIV’s route of transmission is sexual and intravenous. Before the availability of antiretroviral drugs, it had a mortality rate of nearly 100%.³⁴ |
| 1.13. | This puts into context the emergence of severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2, the virus that causes Covid-19) and the Covid-19 pandemic. In the 20th century alone, the threat from epidemics and pandemics did not subside but increased. Novel infectious diseases are part of the landscape for emergency preparedness and resilience. Their emergence ought not to come as a surprise. |
| 1.14. | In the early 21st century, prior to the Covid-19 pandemic, the world had experienced four large outbreaks caused by high consequence human infectious diseases that stopped short of becoming global pandemics – three of which were caused by coronaviruses.³⁵ The UK scientific community had recognised that coronaviruses were a category of viruses that presented a “clear and present danger” that needed to be addressed.³⁶ The international scientific community had also warned of the dangers of emerging zoonotic infectious diseases – which had caused the majority of emerging infectious disease events in the previous six decades – and of the pandemic threat posed by high-impact respiratory pathogens.³⁷ A coronavirus pandemic was described by Professor Whitworth, who provided expert evidence to the Inquiry about infectious disease surveillance, as a “reasonable bet” prior to 2020, with another being “very plausible” in the future.³⁸ |
| 1.15. | Furthermore, it was and is not difficult to contemplate a virus that is more transmissible and more lethal. Covid-19 had a case fatality ratio of between 0.5 and 1%.³⁹ By comparison, the case fatality ratios of SARS and MERS at the beginning of the outbreaks (ie before population immunity or clinical countermeasures) were approximately 10% and 35% respectively.⁴⁰ Professor Mark Woolhouse, Professor of Infectious Disease Epidemiology at the University of Edinburgh, underscored this:
“[O]n the scale of potential pandemics, Covid-19 was not at the top and it was possibly quite far from the top. It may be that next time – and there will be a next time … we are dealing with a virus that is much more deadly and is also much more transmissible … The next pandemic could be far more difficult to handle than Covid-19 was, and we all saw the damage that that pandemic caused us.”⁴¹ |
| 1.16. | In the light of that history, the UK’s resilience to and its preparedness for pandemics are matters of vital importance to the security of the nation. However, it is crucial even following the recent experience of the Covid-19 pandemic not to lose perspective, either on the risk or on what can be done about it. As Professor Whitworth and Dr Hammer told the Inquiry:
“The COVID-19 epidemic was unprecedented in recent times, and it would not be reasonable to expect the UK to be fully prepared for a hypothetical epidemic of this size of a previously unknown pathogen.”⁴² |
| 1.17. | The Inquiry agrees. Even the threat of an outbreak has a significant impact on society’s preparedness – whether an epidemic occurs or not. The potential disruption to social and economic life, and the cost (in real financial terms and opportunity) as the result of a false alarm, may be disproportionate to the burden of an actual epidemic or pandemic. There are proper limits to preparedness and resilience (as there are for security), but improvements, even radical ones, can still be made. It is critical for any government, with the public’s approval, to steer a course between complacency and overreaction.⁴³ |
- Charlotte Hammer 14 June 2023 81/4-12
- Charlotte Hammer 14 June 2023 81/4-12; INQ000196611_0005 para 3. The UK government considers that infectious disease outbreaks are likely to be more frequent up to 2030 and another novel pandemic remains a realistic possibility; see: Global Britain in a Competitive Age, HM Government, March 2021, p31 (https://assets.publishing.service.gov.uk/media/60644e4bd3bf7f0c91eababdGlobal_Britain_in_a_Competitive_Age_the_Integrated_Review_of_Security__Defence__Development_and_Foreign_Policy.pdf; INQ000196501).
- INQ000207453
- INQ000207453. For up-to-date figures, see Deaths Registered Weekly in England and Wales, Provisional, Office for National Statistics, 2024 (https://www.ons.gov.uk/peoplepopulationandcommunity/birthsdeathsandmarriages/deaths/datasets/weeklyprovisionalfiguresondeathsregisteredinenglandandwales).
- INQ000184638_0008 para 1.12
- INQ000196611_0007-0008 paras 8, 13
- INQ000196611_0008-0009 paras 13-15
- INQ000184638_0041 para 5.19
- INQ000184638_0041 para 5.21
- See Table 1 above; INQ000207453_0001; INQ000196611_0007 para 10
- INQ000184638_041 para 5.21
- Christopher Whitty 22 June 2023 93/15-22
- INQ000184638_0043 para 5.28; Richard Horton 13 July 2023 67/15-19
- Richard Horton 13 July 2023 67/15-68/13
- INQ000195846_0007 para 21
- ‘Lessons learned from SARS: The experience of the Health Protection Agency, England’, N.L. Goddard, V.C. Delpech, J.M. Watson, M. Regan and A. Nicoll, Public Health (2006), 120, 27-32 (http://doi.org/10.1016/j.puhe.2005.10.003; INQ000187893-1)
- INQ000195846_0010 paras 36-37
- INQ000195846_0011 para 40
- Sustaining Global Surveillance and Response to Emerging Zoonotic Diseases, Institute of Medicine and National Research Council, 2009, p44 (https://nap.nationalacademies.org/read/12625/chapter/1; INQ000149100); INQ000196611_0006, 0016 paras 7, 33
- INQ000195846_0006 para 16. For example, the original hosts of influenza pandemics are usually wild aquatic birds, with intermediary hosts found among wild birds, livestock and mammals such as pigs (INQ000196611_0007 para 9). The original hosts of coronaviruses are most likely bats, with intermediary hosts in previous outbreaks having been other mammals such as civets, as in SARS, and dromedary camels, as in MERS (INQ000196611_0008 para 11). Close contact may involve consumption, hunting, live animal wet markets, handling or cohabitation (INQ000196611_0006 para 7).
- INQ000196611_0016 para 33. As at June 2024, the World Health Organization’s priority diseases and pathogens include Covid-19, Crimean-Congo haemorrhagic fever, Ebola virus disease and Marburg virus disease, Lassa fever, MERS, SARS, Nipah and henipaviral diseases, Rift Valley fever, Zika virus and ‘Disease X’ (INQ000196611_0008, 0017 paras 13-15, 35).
- INQ000196611_0006 para 6
- INQ000196611_0005-0006, 0006-0007 paras 5, 7
- Charlotte Hammer 14 June 2023 81/22-85/2; INQ000196611_0006 para 7
- INQ000196611_0005 para 3
- INQ000196611_0005-0006 para 5
- INQ000196611_0010-0011 para 19
- INQ000196611_0005-0006 para 5
- INQ000196611_0007 para 8
- INQ000196611_0010 paras 18-21
- INQ000184638_0037-0038, 0040-0041, 0042 paras 5.4, 5.16-5.21, 5.23
- INQ000184638_0037-0038 para 5.4
- See Table 1 above; INQ000207453
- See Table 1 above; INQ000207453; INQ000184638_0038 para 5.5
- These four outbreaks were SARS (2002 to 2003), MERS in Saudi Arabia (2012 onwards), MERS in South Korea (2015) and Ebola (2013–2016).
- Mark Woolhouse 5 July 2023 115/7-117/1; see also INQ000149116_0002
- Sustaining Global Surveillance and Response to Emerging Zoonotic Diseases, Institute of Medicine and National Research Council, 2009, pp1-4 (https://nap.nationalacademies.org/read/12625/chapter/1; INQ000149100); Charlotte Hammer 14 June 2023 81/22-82/22; Preparedness for a High-Impact Respiratory Pathogen Pandemic, Johns Hopkins Center for Health Security, September 2019, pp19-20 (https://www.gpmb.org/reports/m/item/preparedness-for-a-high-impact-respiratory-pathogen-pandemic; INQ000198916)
- Jimmy Whitworth 14 June 2023 104/3-10
- INQ000195846_0008 para 25
- INQ000195846_0008 para 25
- Mark Woolhouse 5 July 2023 148/5-22
- INQ000196611_0034 para 86
- INQ000196611_0011-0012 para 22
Chapter 2: The system — institutions, structures and leadership
Introduction
| 2.1. | In the UK (including in the devolved nations: Scotland, Wales and Northern Ireland), there are a multitude of institutions, structures and systems responsible for pandemic preparedness, resilience and response. |
| 2.2. | The Inquiry set out the principal bodies and the ways in which they were linked in a series of organograms, referred to in the course of the Module 1 hearings as the ‘spaghetti diagrams’. These show a complex system that had grown over many decades, ostensibly to provide the UK government and devolved administrations with a coherent and effective approach to preparing for a pandemic.¹ |
| 2.3. | This chapter examines the key institutions, structures and systems. An effective emergency preparedness and resilience system ought to have been the shared endeavour of the UK government and devolved administrations. The system ought to have been simple, clear and purposeful. It should have been organised in a rational and coherent form to ensure that the UK government and devolved administrations were prepared for a pandemic. This chapter also considers the effectiveness of the lead government department model in the UK for building preparedness for and resilience to whole-system civil emergencies. |
The international system of biosecurity
| 2.4. | The principal aim of biosecurity (an umbrella term for the preparation, policies and actions to protect human, animal and environmental health against biological threats) is the protection of society from the harmful effects of infectious disease outbreaks.² There is a balance to be struck between overreaction and being excessively cautious. A small cluster of infections may or may not become established in the population. In the early stages of an outbreak, therefore, the likely public health burden is quite unpredictable – it could range from the trivial to the devastating.³ Furthermore, when there is greater surveillance for emerging infections, there will naturally be more “‘false alarms’”.⁴ Thus, surveillance itself carries the risk of ‘crying wolf’. A society that is unduly frightened is not a resilient one. If the alarm is sounded without due cause, cynicism about the risks posed by more serious outbreaks will undermine society’s trust in biosecurity.⁵ |
| 2.5. | Critical to an effective alert system are transparency and the flow of information, both within the UK and internationally. The international system of biosecurity is based on cooperation between nations through organisations and frameworks, including:
|
| 2.6. | At present, there is little or no incentive – and much disincentive – for countries to report outbreaks of disease within their borders. The ramifications for doing so include potential economic damage and a certain level of stigma. Recent examples that demonstrate hesitancy to report outbreaks are instructive. They include Saudi Arabia’s disclosure of the Middle East respiratory syndrome (MERS) outbreak and the Chinese government’s disclosure of severe acute respiratory syndrome (SARS).⁹ |
| 2.7. | The global landscape of surveillance coordination for infectious diseases is currently in flux as changes are being made at several levels, including the UK’s exit from the EU, negotiations about a pandemic treaty that may replace the current regulations and the creation in September 2021 of the European Commission’s Health Emergency Preparedness and Response Authority. It is too early to assess the impact of these changes.¹⁰ |
| 2.8. | While a certain level of realism is required, the culture among the international community should develop into one of candour between nations and openness with the public about the reporting of novel pathogen outbreaks. The UK government could contribute towards building such a culture by engaging further with the work of global institutions, such as the World Health Organization, and the many regional and international systems of surveillance and response. The more information that can be obtained and shared, and the more intelligently it can be interrogated, the more prepared the UK and other countries will be. |
The United Kingdom
| 2.9. | Much attention is directed in government literature to the issue of ‘whole-system’ civil emergencies. These are events or situations that threaten serious damage to human welfare, the environment or the security of the UK.¹¹ They are generally categorised either as a hazard (a risk with a non-malicious cause) or a threat (a risk that does have a malicious cause).¹² |
| 2.10. | Whether or not a civil emergency is a whole-system civil emergency is principally a question of scale. Civil emergencies on a small scale impact fewer people and involve fewer decision-makers in preparedness, resilience and response. For example, a rail accident is principally a transport-related issue and flooding is largely an environmental issue. Consequently, preparedness, resilience and response are led at a national level by relevant specialist departments – the Department for Transport and the Department for Environment, Food and Rural Affairs, or their equivalent directorates or departments in the devolved administrations.¹³ These are more “normal” civil emergencies.¹⁴ |
| 2.11. | Other civil emergencies have much broader and deeper impacts and require significantly more decision-makers for all aspects of preparedness, resilience and response. The most complex civil emergencies engage the whole system of central, regional and local government across the UK and the whole of society.¹⁵ Whole- system civil emergencies impact on the whole society of the UK and require a cross- departmental approach within, as well as between, the UK government and devolved administrations. |
| 2.12. | There is, at present, no agreed definition between the UK government and devolved administrations about what amounts to a whole-system civil emergency. This should be rectified. A single definition, based on the above, should be created and used to determine the structures needed in the response, the assessment of risk and the design of strategy. One thing is clear, however: a pandemic that kills human beings is a whole-system civil emergency. The risk of a pandemic therefore demands careful assessment, planning and response. |
| 2.13. | The UK is itself complex and has distinct legal systems and varied devolution frameworks that devolve power differently to Scotland, Wales and Northern Ireland. Although there are differences in each devolution settlement, health has been a primarily devolved matter in Scotland, Wales and Northern Ireland since 1999. |
| 2.14. | However, the Civil Contingencies Act 2004 and associated regulations and guidance set out the framework for civil protection in an emergency across the UK, taking into account the devolution of powers.¹⁶ The Act divides local responders – representatives from public services including the emergency services, local authorities, the NHS and the Health and Safety Executive – into two categories, imposing a different set of duties on each. It is supported by statutory guidance, Emergency Preparedness, and a suite of non-statutory guidance, including Emergency Response and Recovery.¹⁷ At the time of the coronavirus (Covid-19) pandemic, the legislative framework and associated national guidance was “widely acknowledged [by public health specialists and practitioners] as being outdated and did not relate to contemporary structures, roles and responsibilities”.¹⁸ As is being examined in subsequent modules of the Inquiry, it was not utilised. |
| 2.15. | There should be cooperation between the UK government and devolved administrations at all levels. The best defence against the spread of pathogens was and remains strong national surveillance and detection mechanisms – as all international systems are ultimately built upon these – and effective collaboration between the various levels of responsibility.¹⁹ |
| 2.16. | Within the UK, surveillance involves the ongoing, systematic collection, collation, analysis and interpretation of data, with dissemination of information to those that need it (including those at the local level); this is primarily undertaken by the UK Health Security Agency.²⁰ Dr Charlotte Hammer, expert witness on infectious disease surveillance (see Appendix 1: The background to this module and the Inquiry’s methodology), noted the importance of an early alert:
“The earlier your alert, the more likely you can actually respond to it, because the response will be much, much smaller, and a much smaller response can be mounted more often.”²¹ |
The UK government and supporting organisations in England
Figure 1: Pandemic preparedness and response central government structures in the UK and England – c. August 2019
Source: Extract from INQ000204014
Figure 2: Pandemic preparedness and response structures in the UK and England – c. August 2019
Source: Extract from INQ000204014
The Cabinet Office
| 2.17. | The Cabinet Office is the UK government department responsible for supporting the Prime Minister, the Cabinet and the functioning of government more broadly. |
| 2.18. | The Civil Contingencies Secretariat sat within the National Security Secretariat of the Cabinet Office.²² It had a number of roles, including:
|
| 2.19. | Katharine Hammond, Director of the Civil Contingencies Secretariat from August 2016 to August 2020, told the Inquiry that it was principally a “co-ordinating” body for whole-system civil emergency planning, response and recovery.²⁶ Although it was located at the centre of government, it did not lead and was not in charge of the preparedness and resilience of other government departments. Each government department was in charge of managing the risks that fell within its remit.²⁷ |
| 2.20. | There was a historical problem at the centre of government: a difference between the amount of time and resources dedicated to considering threats and hazards. Ms Hammond suggested that this reflected the view that malicious threats could, by their nature, seem more alarming and were more likely to be preventable.²⁸ During her tenure as Director of the Civil Contingencies Secretariat, part of Ms Hammond’s role was to ensure that non-malicious risks – known as hazards as opposed to threats – received adequate attention and focus from all government departments.²⁹ |
Ministerial oversight
| 2.21. | David Cameron MP, Prime Minister from May 2010 to July 2016, made it one of the aims of his government to make the architecture of dealing with civil contingencies and national security “more strategic”.³⁰ The purpose was to enable the UK government to take a longer-term view of the risks on the horizon regarding the UK’s security.³¹ One of Mr Cameron’s first acts in government was to establish a National Security Council as a Cabinet Committee, supported by a National Security Secretariat and a National Security Adviser.³² The National Security Council was the main forum for ministerial discussion of the UK government’s objectives for national security, including resilience.³³ It focused on malicious threats.³⁴ |
| 2.22. | In addition, the National Security Council (Threats, Hazards, Resilience and Contingencies) sub-Committee was created with a focus on emergency planning and preparedness, which included non-malicious hazards.³⁵ Sir Oliver Letwin MP, Minister for Government Policy from May 2010 to July 2016 and Chancellor of the Duchy of Lancaster from July 2014 to July 2016, was placed in charge of the Threats, Hazards, Resilience and Contingencies sub-Committee and would chair it in Mr Cameron’s absence. He was described as “in many ways, the Resilience Minister”.³⁶ Mr Cameron told the Inquiry that having a strong Cabinet minister with “the ear of the Prime Minister” in this position was the right approach because only the Prime Minister is in the position to put the full weight of government behind their decisions.³⁷ |
| 2.23. | The Threats, Hazards, Resilience and Contingencies sub-Committee provided the Prime Minister with an overview of the potential civil domestic disruptive challenges that the UK might face over the next 6 months (as distinct from the National Risk Register’s 5-year timeframe and the National Security Risk Assessment’s 20-year timeline).³⁸ In 2016, following the outbreak of Ebola virus disease in 2013, the UK government established a specialist horizon-scanning unit for viruses that might affect the UK, which fed into the Threats, Hazards, Resilience and Contingencies sub-Committee.³⁹ |
| 2.24. | The Threats, Hazards, Resilience and Contingencies sub-Committee was important to the implementation of the UK Influenza Pandemic Preparedness Strategy 2011 (the 2011 Strategy):
“comprising Ministers from across Central Government departments and the [devolved administrations], oversees and coordinates national preparations for all key UK risks including pandemic influenza”.⁴⁰ The sub-Committee put the weight of the Cabinet and the Prime Minister behind important activities of preparedness. The Inquiry was told by Mr Cameron and Sir Oliver Letwin that this was necessary to ensure that important issues were acted upon.⁴¹ |
| 2.25. | The last occasion on which the Threats, Hazards, Resilience and Contingencies sub-Committee met was in February 2017 (see Chapter 5: Learning from experience).⁴² In July 2019, the sub-Committee was formally “taken out of the committee structure”.⁴³ Ms Hammond suggested that it could be “reconvened if needed” but accepted that it was, in effect, abolished.⁴⁴ As a result, immediately prior to the pandemic, there was no cross-government ministerial oversight of the matters that were previously within the sub-Committee’s remit. |
The Department of Health and Social Care⁴⁵
| 2.26. | Most emergencies in the UK are handled locally by emergency services. However, where the emergency’s scale or complexity is such that it requires UK government coordination or support, a designated lead government department is responsible for the overall management of the planning and response.⁴⁶ The Department of Health and Social Care was the UK government’s lead government department responsible for pandemic preparedness, response and recovery.⁴⁷ |
| 2.27. | In 2007, the Department of Health established the Pandemic Influenza Preparedness Programme.⁴⁸ This programme was focused on the management of pandemic influenza preparedness within the health and social care system in England. Its board comprised officials from the Department of Health, the Cabinet Office, NHS England and Public Health England.⁴⁹ As discussed later in this Report, the UK government’s assessment of pandemic risk and its strategies for dealing with that risk both suffered because they focused almost entirely on influenza as the most likely cause of a pandemic. The Covid-19 pandemic was, of course, caused by a coronavirus. |
| 2.28. | There was also the Pandemic Flu Readiness Board, which was established in March 2017 by the Threats, Hazards, Resilience and Contingencies sub-Committee.⁵⁰ It was intended to coordinate planning across the UK by involving the devolved administrations and 14 relevant UK government departments.⁵¹ From February 2018, the Pandemic Flu Readiness Board was co-chaired by Ms Hammond, on behalf of the Cabinet Office, and Emma Reed, Director of Emergency Preparedness and Health Protection in the Department of Health and Social Care.⁵² Again, this board was concerned only with preparing for an influenza pandemic. Moreover, its work overlapped with the work of the Pandemic Influenza Preparedness Programme. |
| 2.29. | In 2021, apparently in acknowledgement of its fundamental structural flaws, the Pandemic Flu Readiness Board was replaced by an entity called the Pandemic Diseases Capabilities Board. This would consider preparedness for a broad range of pandemics, including but not limited to pandemic influenza, and would focus on the practical capabilities needed to respond to pandemics.⁵³ |
Public Health England
| 2.30. | Before the Covid-19 pandemic, the principal responsibility for managing high consequence infectious disease outbreaks lay with Public Health England. This body was established in 2013 as an executive agency of the Department of Health, to protect and improve health and wellbeing and reduce health inequalities. It primarily covered England, with limited UK-wide responsibilities.⁵⁴ |
| 2.31. | Public Health England’s functions for pandemic preparedness and resilience included:
|
| 2.32. | Duncan Selbie, Chief Executive of Public Health England from July 2012 to August 2020, described it as:
“well prepared for the emergency health protection work that it was commissioned by [the Department of Health and Social Care] to perform … but … not fully prepared to deal with the scale and magnitude of the pandemic of unknown origin that the world faced in January 2020”.⁶⁰ |
| 2.33. | In the event, Public Health England was effectively abolished by the UK government following the commencement of the pandemic. From 2021, the UK Health Security Agency brought together the staff and capabilities of NHS Test and Trace and the health protection elements of Public Health England.⁶¹ Sir Christopher Wormald, Permanent Secretary to the Department of Health and Social Care from May 2016, described the UK Health Security Agency as providing “permanent standing capacity to prepare for, prevent and respond to threats to health”.⁶² Its creation to fulfil this purpose demonstrated that there was no such effective permanent standing capacity prior to the pandemic. |
Expert medical and scientific advice
| 2.34. | The Chief Medical Officer for England is a doctor, public health leader and public official, as well as the Chief Medical Adviser to the UK government. The Office of the Chief Medical Officer comprises fewer than 20 people, including the Chief Medical Officer and Deputy Chief Medical Officers.⁶³ The Chief Medical Officer’s responsibilities fall broadly into three areas: providing independent scientific advice to ministers across the UK government on medical and public health issues; communicating to the public on health matters in times of emergency; and serving as part of the collective leadership of the medical and public health professions.⁶⁴ The combined roles of Chief Medical Officer for England and Chief Medical Adviser to the UK government run parallel to the system of chief scientific advisers. |
| 2.35. | The system for providing scientific advice to decision-makers spanned the whole UK government. Each department and its supporting organisations had their own method by which scientific information, advice and analysis were provided to decision-makers.⁶⁵ The UK government was also advised by a large number of scientific advisory groups, committees and entities relevant to human infectious diseases and pandemic preparedness. These groups were largely, but not exclusively, sponsored by the Department of Health and Social Care as the lead government department for human infectious disease risks. They generally reported their advice directly to its officials. |
| 2.36. | Each of these groups had a separate remit and specialisation. The key scientific advisory groups relevant to human infectious disease risks were:
|
| 2.37. | Most UK government departments also had a departmental chief scientific adviser.⁷⁵ They were responsible for ensuring mechanisms were in place to provide advice to policy-makers and ministers, both within their departments and across the UK government.⁷⁶ The system of departmental chief scientific advisers was one of the key means of bridging the gap between the decentralisation of scientific advice in each UK government department and embedding a coherent and consistent scientific advice system across the UK government as a whole.⁷⁷ |
| 2.38. | At the centre of the UK government scientific advice system was the Government Chief Scientific Adviser supported by the Government Office for Science (also known as GO-Science).⁷⁸ They were responsible for providing scientific advice to the Prime Minister and members of the Cabinet, advising the UK government on aspects of science for policy (as opposed to science policy itself) and improving the quality and use of scientific evidence and advice in government.⁷⁹ One of the main forums for the sharing of information was the Chief Scientific Adviser Network, which consisted of the Government Chief Scientific Adviser and departmental chief scientific advisers and which usually met on a weekly basis.⁸⁰ |
| 2.39. | The UK government’s expert medical and scientific advice system had two main strengths. Firstly, relatively few emergencies involved only a single department and the network across government allowed for the rapid transmission of technical information to the departments that needed it.⁸¹ Secondly, each scientific adviser could call on the specialist capabilities from within their own department.⁸² Professor Sir Christopher Whitty, Chief Medical Officer for England from October 2019, told the Inquiry that the “UK science advisory system is complex and not perfect but is considered to be one of the stronger ones internationally”.⁸³ Sir Jeremy Farrar, Chief Scientist at the World Health Organization from May 2023 and Director of the Wellcome Trust from 2013 to 2023, agreed.⁸⁴ |
Coordinating regional and local activities in England and Wales
| 2.40. | Local resilience forums are the principal mechanism in England and in Wales for emergency preparedness and cooperation between agencies. Their main purpose is to ensure that local responders are able effectively to act on the duties imposed upon them under the Civil Contingencies Act 2004.⁸⁵ |
| 2.41. | The Ministry of Housing, Communities and Local Governments (through its Resilience and Emergencies Division, now renamed the Resilience and Recovery Directorate) shared responsibility for local resilience in England with the Cabinet Office.⁸⁶ The role of the Resilience and Emergencies Division (through teams of resilience advisers) was principally to help responders identify for themselves the risks they faced and how to mitigate those risks, and to manage the impact of risks that materialised. It would act akin to a ‘critical friend’, question rationales, suggest alternatives, share good practice and support local planning activities. It contributed, advised, facilitated and participated.⁸⁷ However, it was not the role of the Resilience and Emergencies Division to provide leadership and it did not ensure that local responders fulfilled their statutory duties.⁸⁸ |
| 2.42. | Mark Lloyd, Chief Executive of the Local Government Association from November 2015, described the link between the Ministry of Housing, Communities and Local Government and local resilience forums as “strong”.⁸⁹ However, in other respects, he described a “fragmentation” because, while the Cabinet Office coordinated activity on national incidents, the Department of Health and Social Care had specific responsibility for pandemics. Mr Lloyd said that, as a result, officials in the Ministry of Housing, Communities and Local Government had a “big challenge” in managing the interface between central and local government.⁹⁰ Important links between local and national governments were missing. |
| 2.43. | When national guidance was developed under the Civil Contingencies Act 2004, there was also a lack of understanding at the UK government level about the inter-relationships between entities at the local level.⁹¹ |
| 2.44. | Local structures are not aligned. For example, local resilience forums are geographically defined by police force areas, but local health resilience partnerships (strategic forums for organisations in the local health sector) follow the geographical boundaries of the integrated care system. This means that the geographical areas covered by directors of public health do not always match those of local resilience forums or local health resilience partnerships.⁹² This structural flaw, for which the Cabinet Office was ultimately responsible, is potentially a recipe for confusion and duplication. Professor Jim McManus, President of the Association of the Directors of Public Health from October 2021 to October 2023, told the Inquiry that this could be “tidied up”.⁹³ |
| 2.45. | Another key issue was that, while directors of public health (specialists accountable for the delivery of their local authority’s public health duties) co-chaired local health resilience partnerships, they did not routinely sit on local resilience forums because they were not invited to do so.⁹⁴ Structurally, this created a gap when it came to addressing a public health emergency, with professionals in civil contingencies and public health not appropriately connected. The directors of public health, the public health workforce and local government have a critical contribution to make to pandemic preparedness and resilience. Their knowledge and skills are an important local and national resource to be drawn upon in whole-system civil emergency preparedness and resilience.⁹⁵ They are in regular contact with the local population and therefore have an important role in communicating their needs to the institutions whose responsibility it is to prepare for and build resilience to whole-system civil emergencies.⁹⁶ There should be far greater involvement of directors of public health and local public health teams in developing those plans. |
| 2.46. | Dr Claas Kirchhelle, expert witness to the Inquiry on public health structures (see Appendix 1: The background to this module and the Inquiry’s methodology), described a lengthy cycle of centralisation and fragmentation resulting in a “misalignment” in the UK’s health, social care and pandemic preparedness structures and systems.⁹⁷ The issues of constant reorganisation and rebranding go to the top of the institutions responsible for preparedness and resilience in the UK. For example, in September 2022, the Civil Contingencies Secretariat was subject to a split into a Resilience Directorate and a separate COBR Unit. This was apparently to give effect to a change in “purpose” and “focus” and a “slightly different framing”.⁹⁸ However, the headcount remained very similar and there did not appear to be a substantive difference between the old system and the new.⁹⁹ |
Scotland
Scottish Government and supporting organisations
Figure 3: Pandemic preparedness and response central government structures in Scotland – c. 2019
Source: Extract from INQ000204014
Figure 4: Pandemic preparedness and response structures in Scotland – c. 2019
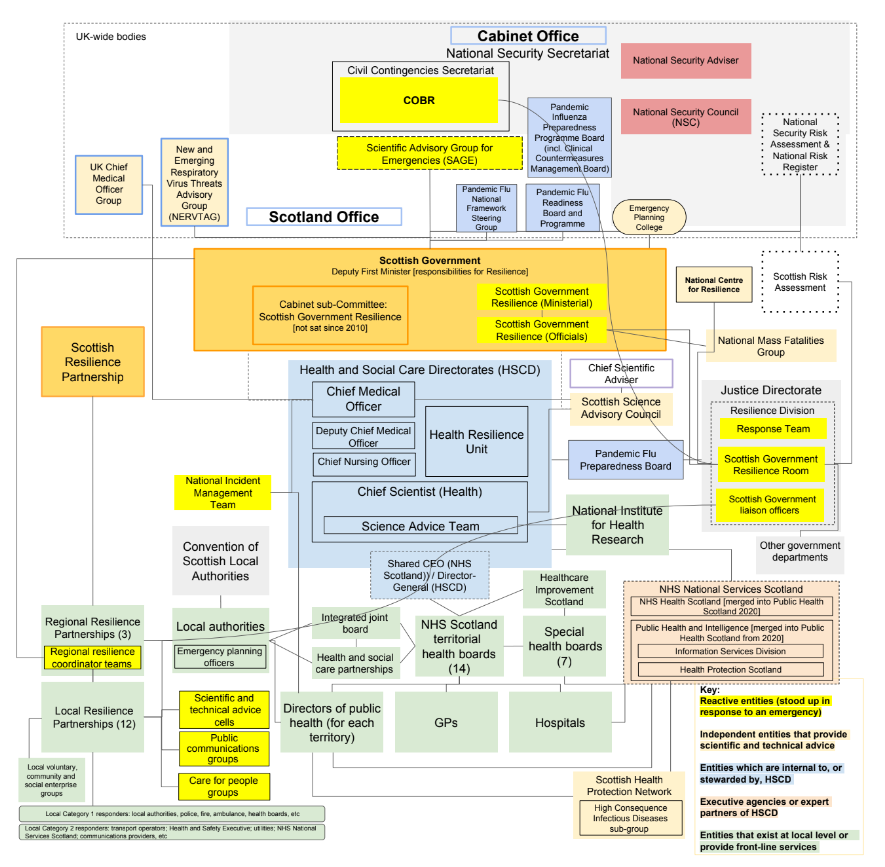
Source: Extract from INQ000204014_0006
| 2.47. | John Swinney MSP was the Deputy First Minister in the Scottish Government from November 2014 to March 2023. As Deputy First Minister, Mr Swinney held ministerial responsibility for resilience. Those responsibilities are now held by the Cabinet Secretary for Justice and Home Affairs.¹⁰⁰ Mr Swinney described his position as “participating in, and ultimately leading, the Resilience function of the Scottish Government”.¹⁰¹ |
| 2.48. | In Scotland, the Cabinet Sub-Committee Scottish Government Resilience provided ministerial oversight to strategic policy and guidance in the context of resilience in Scotland.¹⁰² Its last meeting took place in April 2010, when, according to the minutes, it had a full programme of work.¹⁰³ This work was taken up by the Scottish Resilience Partnership, which had direct ministerial involvement in order to provide “strategic ministerial direction”.¹⁰⁴ As those attending were all members of the Cabinet, if necessary, issues could be taken up in that forum.¹⁰⁵ Gillian Russell, Director of Safer Communities from June 2015 to March 2020, said that, in her experience, the Scottish Cabinet took decisions on resilience rather than working through a sub-committee.¹⁰⁶ Nonetheless, Mr Swinney told the Inquiry:
“[T]here may well be the need for a particular forum to look periodically, formally, in a recorded fashion, to take stock about where preparations happen to be.”¹⁰⁷ |
| 2.49. | Resilience was centralised in the Scottish Government around a ‘hub and spokes’ model. At the centre of the model – the hub – was Preparing Scotland.¹⁰⁸ This was a set of national guidance documents for civil emergencies, which set out:
“how Scotland is prepared. It identifies structures, and assists in planning, responding and recovering from emergencies. It is not intended to be an operations manual. Rather, it is guidance to responders to assist them to assess, plan, respond and recover.”¹⁰⁹ |
| 2.50. | The Resilience Division in the Scottish Government led on emergency planning, response and recovery, as well as on the strategy, guidance and work programme for improving the resilience of essential services in Scotland and the Preparing Scotland guidance.¹¹⁰ Its wide remit included overseeing the capability and capacity at national, regional and local levels to prepare for and respond to civil emergencies, including pandemic influenza.¹¹¹ It was also responsible for the Scottish Government Resilience Room. This meant that the entity responsible for preparedness and resilience was integrated with the entity responsible for response.¹¹² |
| 2.51. | Prior to the Covid-19 pandemic, the Resilience Division was relocated from a directorate in the Directorate-General Constitution and External Affairs to a directorate in the Directorate-General Education and Justice.¹¹³ Later, in April 2021, it was moved back to a directorate in the now renamed Directorate-General Strategy and External Affairs.¹¹⁴ The Inquiry notes that entities responsible for resilience are too often the subject of reorganisation in Scotland, as they are in the other devolved administrations and the UK government. However, there is some degree of continuity in that the Civil Service in Scotland does not have departments based on the Whitehall model, but instead has a more flexible and unified structure, comprising directorates and executive agencies.¹¹⁵ Mr Swinney also retained political leadership for resilience matters throughout all of the changes prior to his resignation as Deputy First Minister in March 2023.¹¹⁶ |
| 2.52. | Further from the centre of government, structures were more diffuse and, as a consequence, more confusing. The Scottish Government had its own Pandemic Flu Preparedness Board.¹¹⁷ Health Protection Scotland (which was part of NHS National Services Scotland but also had joint accountability to the Scottish Government and the Convention of Scottish Local Authorities) was responsible for providing national leadership to protect the Scottish public from infectious diseases and for preparing for outbreaks.¹¹⁸ There were also several public health divisions based within the Directorate of Population Health and the Emergency Preparedness Resilience and Response Division (within the Directorate of the Chief Operating Officer).¹¹⁹ On 1 April 2020, functions of Health Protection Scotland were transferred to a new body, Public Health Scotland, plans for which were rapidly revised for the Covid-19 pandemic.¹²⁰ |
Expert medical and scientific advice
| 2.53. | In Scotland, the Chief Medical Officer had only a limited role in pandemic preparedness and resilience.¹²¹ The Chief Scientific Adviser to the Scottish Government did not hold primary responsibility for advice on public health, public health-related science and epidemiology.¹²² The Chief Scientist (Health) in Scotland similarly did not have a role in pandemic preparedness.¹²³ Scotland substantially relied, in terms of expert medical and scientific advice, on “UK intelligence”.¹²⁴ |
Coordinating regional and local activities
| 2.54. | Coordination between emergency responders was undertaken by three Regional Resilience Partnerships, composed of representatives from Category 1 and Category 2 responders and others as deemed necessary.¹²⁵ Within each Regional Resilience Partnership area are several Local Resilience Partnerships.¹²⁶ The regional and local partnerships covered both preparedness and response.¹²⁷ The Scottish Government coordinated with those partnerships through embedded teams of coordinators.¹²⁸ |
| 2.55. | The Scottish Resilience Partnership also brought together a core group of Scottish Government officials, Category 1 responders and representatives from the Society of Local Authority Chief Executives, as well as Scotland’s 12 Local Resilience Partnerships. It would meet “on a periodic basis to supervise the preparation for resilience activity”.¹²⁹ Mr Swinney said that ministers also attended “quite frequently” to “provide the direction of ministerial thinking”.¹³⁰ |
Wales
Welsh Government and supporting organisations
Figure 5: Pandemic preparedness and response central government structures in Wales – c. 2019
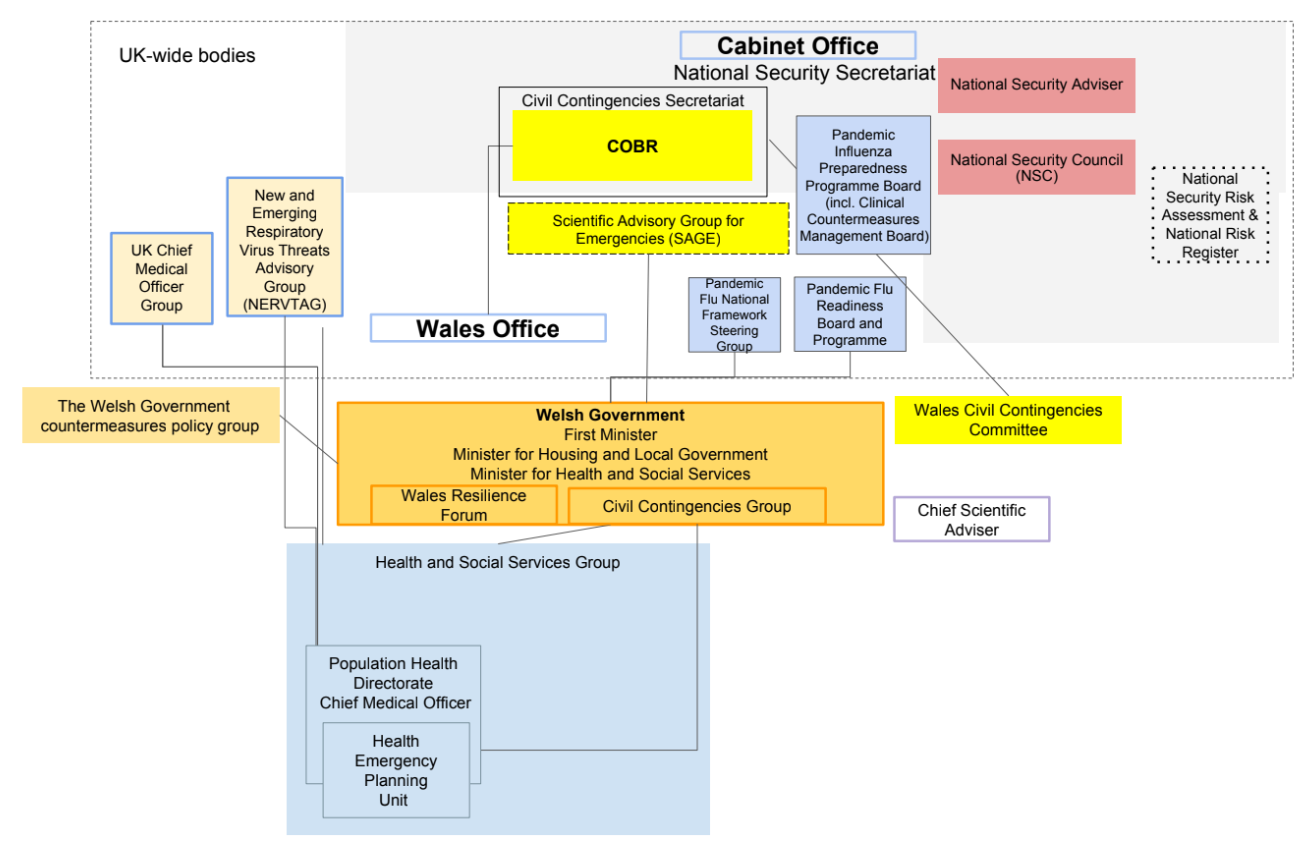
Source: Extract from INQ000204014
Figure 6: Pandemic preparedness and response structures in Wales – c. 2019
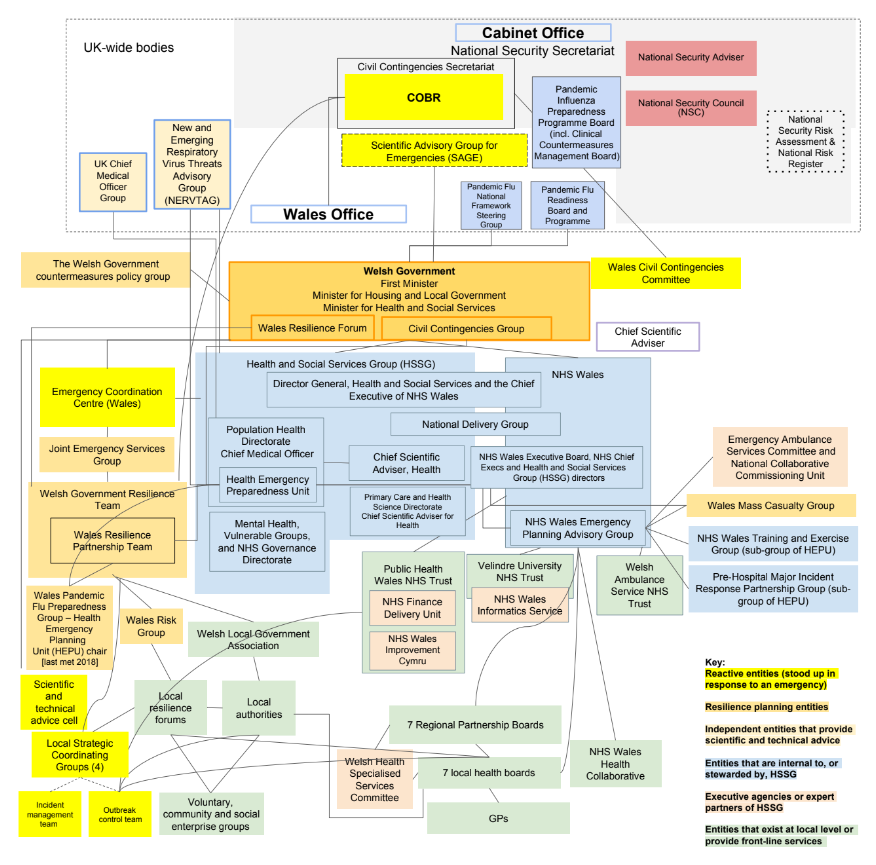
Source: Extract from INQ000204014
| 2.56. | The First Minister had overall responsibility for civil contingencies and resilience within the Welsh Government.¹³¹ This gave significant recognition to its importance. There existed beneath the First Minister a very complicated array of committees, teams, groups and sub-groups, which indicates that the Welsh Government was not as “compact” an administration as suggested to the Inquiry by Dr Andrew Goodall, Permanent Secretary to the Welsh Government from September 2021.¹³² |
| 2.57. | There were multiple entities involved in preparedness and resilience, split across several bodies.¹³³ They included:
|
| 2.58. | The Welsh Government Resilience Team was located within the Community Safety Division before the Covid-19 pandemic. Both had been moved around regularly within the Welsh Government: they were originally located within the Human Resources Group, before transferring to the Local Government and Communities Group in 2011 and then to the Education and Public Services Group in 2017.¹⁴³ The Welsh Government Resilience Team has been reorganised again since the pandemic. In 2021, it was expanded to become a self-standing division that included civil contingencies, national security and cyber resilience, known as the Civil Contingencies and National Security Division.¹⁴⁴ In 2022, it was reorganised again. This time, the Civil Contingencies and National Security Division was merged with the Community Safety Division and the Covid Recovery and Restart Division to form a new Risk, Resilience and Community Safety Directorate.¹⁴⁵ This included the Wales Pandemic Flu Preparedness Group, which was established to implement work set by the UK’s Pandemic Flu Readiness Board.¹⁴⁶ This constant flux does not improve resilience. |
| 2.59. | Health services are almost entirely devolved in Wales.¹⁴⁷ However, in relation to civil emergencies, the 2011 concordat between the UK and Welsh governments for the Civil Contingencies Act 2004 provided a broad principle for the operation of emergency powers in Wales. It emphasised cooperation and consultation between the UK and Welsh governments on emergency planning and response.¹⁴⁸ |
| 2.60. | Notwithstanding the range of entities in Wales ostensibly charged with preparedness, Sir Frank Atherton, Chief Medical Officer for Wales from August 2016, established the Health Protection Advisory Committee in May 2018. This was to bring together a range of organisations involved in health protection issues. Its purpose was to help understand the broad sweep of threats from infectious diseases – no other committee had previously been convened to address such threats or to look at health protection issues.¹⁴⁹ |
| 2.61. | For an administration that prided itself on its efficiency of movement because of its relative lack of scale, and which had described itself as operating, effectively, “under one roof”, the reality did not match the rhetoric.¹⁵⁰ The system was labyrinthine. The Inquiry was not persuaded by the mitigation offered by Dr Goodall that it made more sense to those within the system than those outside of it.¹⁵¹ An opportunity to create a coherent and, therefore, dynamic system in Wales had been hampered by undue complexity. |
Expert medical and scientific advice
| 2.62. | The role of the Chief Medical Officer for Wales was to provide advice to the Welsh Government on public health policy. They were also responsible for overseeing the Health Emergency Planning Unit, which led on pandemic preparedness and civil contingency planning within the Health and Social Services Group in Wales.¹⁵² |
| 2.63. | The Chief Scientific Adviser for Wales and the Chief Scientific Adviser for Health in Wales were not central to pandemic preparedness and resilience.¹⁵³ |
Coordinating regional and local activities
| 2.64. | The various local civil contingencies structures in Wales have been dealt with above. At a high level, these included the Wales Resilience Forum, Welsh local resilience forums and the Wales Resilience Partnership Team.¹⁵⁴ |
| 2.65. | Welsh local resilience forums bring together Category 1 and 2 responders and are the principal mechanisms for multi-agency planning and cooperation at a local level.¹⁵⁵ As with England, the four local resilience forums in Wales are based on police force areas.¹⁵⁶ The Local Resilience Forum Co-ordinators Group also provides support and shared knowledge across the local resilience forums.¹⁵⁷ |
| 2.66. | The Wales Resilience Partnership Team is a group that sits underneath the Wales Resilience Forum. It supports them by providing secretariat and policy services and operationalisation of some of the activities discussed at the Wales Resilience Forum.¹⁵⁸ |
| 2.67. | The Welsh Government leads on all-Wales coordination and has a support role for local resilience forums.¹⁵⁹ The Wales Resilience Forum is a structure within the Welsh Government that is chaired by the First Minister and includes representation from all multi-agency partners, including from the local resilience forums, the Welsh Local Government Association, the Society of Local Authority Chief Executives (Solace) Cymru and Public Health Wales.¹⁶⁰ The Wales Resilience Forum provides strategic guidance and advice to public sectors and local resilience forums on issues not confined to health, and is an advisory rather than a strategic decision-making body.¹⁶¹ |
| 2.68. | Chris Llewelyn, Chief Executive of the Welsh Local Government Association from January 2019, told the Inquiry that the structures described above were in place and operated effectively but needed to be supplemented with other arrangements during the Covid-19 pandemic.¹⁶² Mr Llewelyn’s view was that there was a need for the engagement of all partners in a whole-system reform or redesign of the arrangements.¹⁶³ |
| 2.69. | A December 2012 report by the Wales Audit Office on civil contingencies in Wales concluded:
|
| 2.70. | These observations were as true in 2020, as the Covid-19 pandemic struck Wales, as they were when the report was written in 2012. Not much had been done in the meantime by the Welsh Government to simplify, streamline and rationalise the entities charged with leading and administering emergency preparedness in Wales. |
Northern Ireland
The Northern Ireland Executive and supporting organisations
Figure 7: Pandemic preparedness and response central executive structures in Northern Ireland – c. 2019
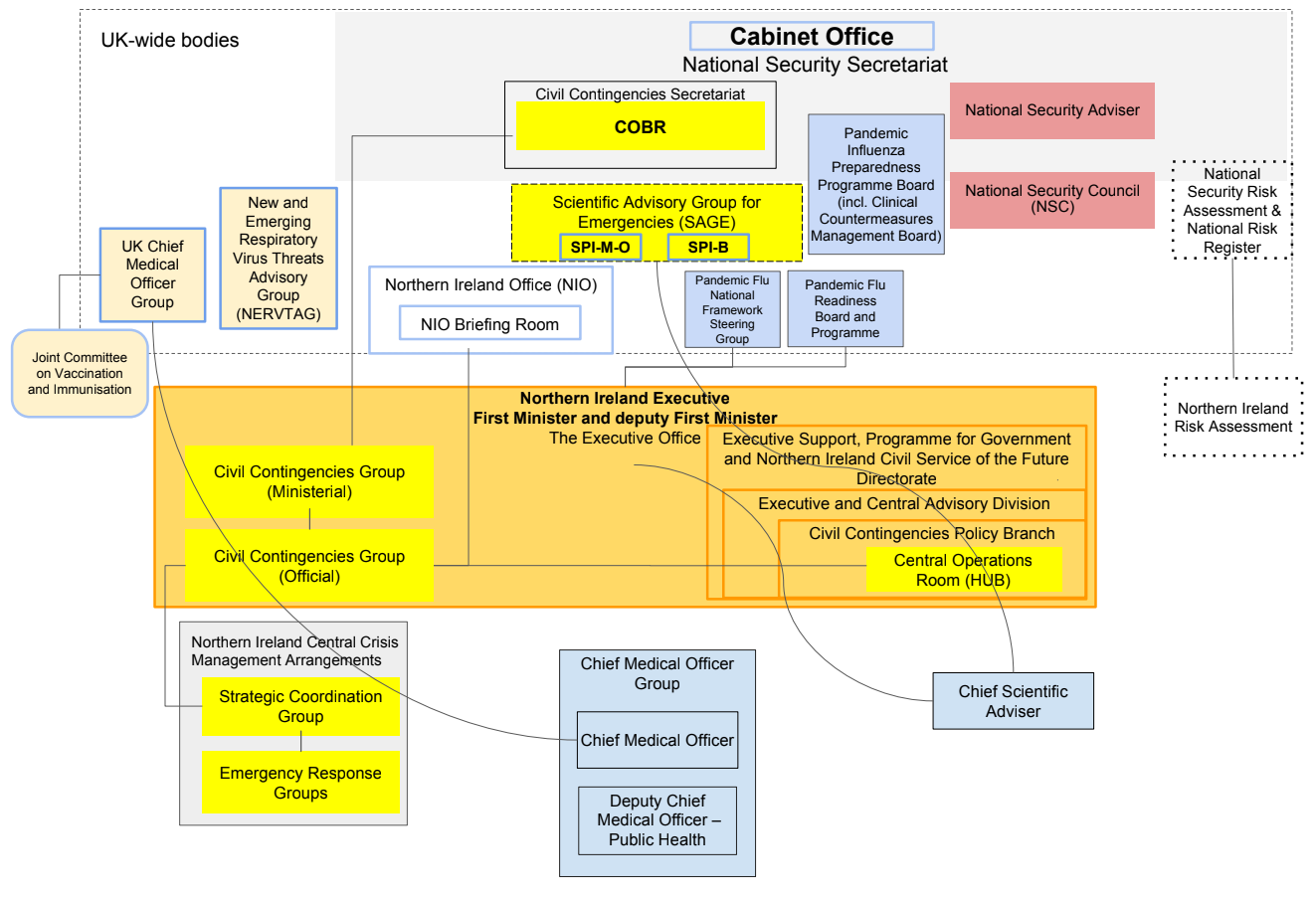
Source: Extract from INQ000204014
Figure 8: Pandemic preparedness and response structures in Northern Ireland – c. 2019
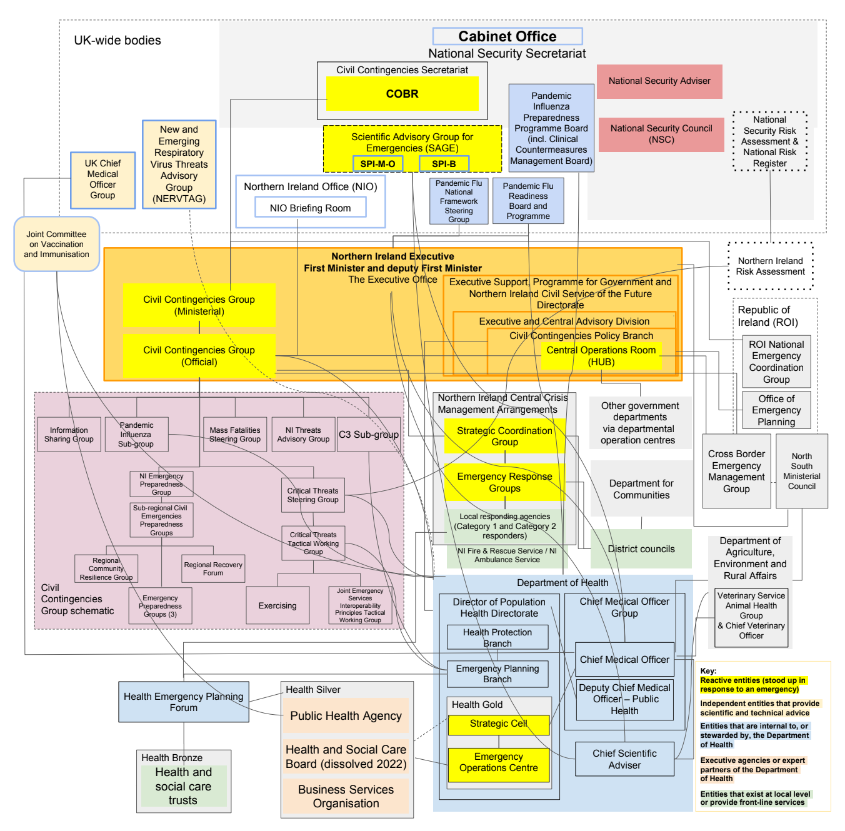
Source: Extract from INQ000204014
| 2.71. | Civil contingencies policy and legislation, and their delivery, in Northern Ireland are generally devolved matters.¹⁶⁷ The custom and practice in Northern Ireland was to remain in broad alignment with the policy and best practice of the rest of the UK.¹⁶⁸ The Civil Contingencies Act 2004 applies only partially to Northern Ireland.¹⁶⁹ Health and social care are transferred matters for which the Northern Ireland Executive has responsibility.¹⁷⁰ |
| 2.72. | The Executive Office (the overarching purpose of which is to support the Northern Ireland Executive) was at the heart of the government of Northern Ireland and had principal policy responsibility for civil contingencies matters.¹⁷¹ It does not, however, have the power to direct or control any other departments or their agencies.¹⁷² In this respect, The Executive Office is a feature of the unique constitutional arrangements for Northern Ireland. Its role was one of coordination across the departments of the Northern Ireland Executive. Northern Ireland also followed the lead government department model, with the Department of Health (Northern Ireland) leading pandemic preparedness.¹⁷³ |
| 2.73. | The two bodies with principal responsibility for pandemic planning in Northern Ireland were:
|
| 2.74. | There were, however, a number of other groups, sub-groups, tiers and sub-tiers, as well as reorganisations and rebrandings.¹⁷⁶ As a result, the system in Northern Ireland had become unduly complex.¹⁷⁷ |
| 2.75. | Between 2015 and 2020, its civil contingencies structures underwent major reform. There remained a proliferation of entities in Northern Ireland.¹⁷⁸ These included:
|
| 2.76. | Dr Denis McMahon, Permanent Secretary to The Executive Office of Northern Ireland from July 2021, maintained to the Inquiry that, notwithstanding its outward appearance of complexity, the situation was more straightforward in practice:
“One of the both challenges and advantages of Northern Ireland is that everybody knows everybody else, it’s a small place, so you can get everybody into the room at the same time.”¹⁸² |
| 2.77. | When asked if the system, complex though it may be, was effective, Dr McMahon’s evidence to the Inquiry was that “overall it has worked well”, but he attributed that in some measure to “personal leadership”.¹⁸³ He cautioned against radical reform in Northern Ireland, as he was concerned not to undo the “years of conditioning” of people working in emergency planning.¹⁸⁴ The Inquiry has greater understanding for this in Northern Ireland than elsewhere in the UK, but that does not mean the system ought not to be subject to simplification and rationalisation. |
| 2.78. | Professor Sir Michael McBride, Chief Medical Officer for Northern Ireland from September 2006, did not believe that it was the complexity of the structures that caused those working in emergency preparedness and planning to be ineffective. It was, he said, more about “function” – ie “for those working in the system, who need to know how those structures work, we know how those structures work and how they interrelate”.¹⁸⁵ Nonetheless, simplicity – which creates very clear lines of accountability – is to be preferred to the diffusion of numerous groups and the risk of an inability to locate those who are responsible for getting the work done. The Inquiry also notes that, following a review of the structure of the Chief Medical Officer Group in 2021, a standalone emergency preparedness, resilience and response directorate had been established, giving its work greater prominence and importance.¹⁸⁶ |
Expert medical and scientific advice
| 2.79. | The role of Chief Medical Officer for Northern Ireland was to provide independent, professional medical advice to both the Minister of Health and the Permanent Secretary. Through the Population Health Directorate in the Chief Medical Officer Group, the Chief Medical Officer for Northern Ireland (uniquely in the UK) held responsibility for planning and preparedness for the health consequences of civil emergencies, including infectious disease outbreaks and pandemics.¹⁸⁷ |
| 2.80. | In Northern Ireland, there were two Chief Scientific Advisers (one within the Department of Health (Northern Ireland) and the other within the Department of Agriculture, Environment and Rural Affairs), but there was no general chief scientific adviser for the Northern Ireland Executive prior to the pandemic.¹⁸⁸ This was recognised by Professor McBride to be an “inherent weakness” in the system.¹⁸⁹ The Inquiry was told that The Executive Office of Northern Ireland was seeking to fill this gap.¹⁹⁰ |
The suspension of the power-sharing arrangements
| 2.81. | The arrangements for the governance of Northern Ireland are contained in the Northern Ireland Act 1998. That Act gives effect to the constitutional settlement contained in the Belfast Agreement of 1998 (known as the Good Friday Agreement). It provides for an elected assembly, with legislative and executive authority in respect of devolved matters. Executive authority is discharged on behalf of the Northern Ireland Assembly by a First Minister, a deputy First Minister and ministers with departmental responsibilities. Ministerial posts are allocated in accordance with party strength in the Northern Ireland Assembly. Ministers constitute the Executive Committee. When these power-sharing arrangements are not in place, senior civil servants in Northern Ireland are responsible for the day-to-day operation of government in Northern Ireland. However, there are important limits to this. For example, in the absence of a functioning Northern Ireland Assembly, departments cannot bring forward primary legislation or discharge functions specifically vested in ministers. This was the case between January 2017 and January 2020.191 |
| 2.82. | Sir David Sterling, Head of the Northern Ireland Civil Service and Permanent Secretary to the Northern Ireland Office from 2017 to 2020, told the Inquiry that there were three major effects of the absence of a functioning government on the Civil Service in Northern Ireland.192 These were as follows:
This view was echoed by Dr McMahon, Sir David Sterling’s successor from July 2021, and also by Robin Swann MLA, Minister of Health in Northern Ireland from January 2020 to October 2022.196 Professor McBride said that there was “absolutely no doubt” that the absence of ministers had “a significant impact” on Northern Ireland’s ability to initiate or develop new policy.197 |
| 2.83. | The three-year hiatus occurred shortly after the publication in 2016 of two reports on significant reforms to the health and social care systems in Northern Ireland produced by an expert panel and the Department of Health (Northern Ireland).198 The recommendations of these reports could not be acted upon in the absence of a functioning government.199 Furthermore, the ability to take any long-term strategic decisions was inhibited, as funding was fixed on a one-year recurring budget.200 Mr Swann told the Inquiry that “opportunities … were firmly missed” in this period.201 |
| 2.84. | It is clear that the structural problems in Northern Ireland, in its preparedness for the Covid-19 pandemic, were exacerbated by the suspension of the power-sharing arrangements. The Inquiry is considering the longer-term impact that the suspension in power-sharing had on Northern Ireland’s response to the pandemic in Module 2C. It is, however, important context for the consideration of the preparedness and resilience of the institutions in Northern Ireland. |
Northern Ireland and the Republic of Ireland
| 2.85. | As Northern Ireland and the Republic of Ireland share an island and a land border, they are considered epidemiologically to be a single unit.202 As part of the Common Travel Area arrangements, there is free movement of people between Northern Ireland, the UK and the Republic of Ireland.203 When the pandemic struck, case rates and spread in Northern Ireland often more closely matched the Republic of Ireland than the rest of the UK.204 The importance of cooperation between the governments and officials of the UK, Northern Ireland and the Republic of Ireland is, therefore, recognised.205 |
| 2.86. | There are a number of bodies to facilitate this cooperation, including: the North South Ministerial Council, which brings together ministers from the Northern Ireland Executive and the Irish government; the Joint Secretariat, staffed by officials from The Executive Office and the Irish Civil Service; and the Cross Border Emergency Management Group for the emergency services.206 Due to the suspension of the power-sharing arrangements, approximately 46 meetings of the North South Ministerial Council did not take place between 2017 and 2020.207 The Joint Secretariat and Cross Border Emergency Management Group continued to function during this period, but any areas that required ministerial decisions – for example, in relation to funding – could not be taken.208 |
| 2.87. | This underlines the importance of cooperation between the governments and officials of the UK, Northern Ireland and the Republic of Ireland.209 This is being considered further in Module 2C of the Inquiry. |
Streamlining the system of preparedness and resilience
| 2.88. | The number of organisations across the UK with responsibility for pandemic preparedness had multiplied over time to become unnecessarily numerous and complex. The responsibilities within the UK government and devolved administrations, and their supporting organisations, were duplicative, diffuse and delegated too far from ministers and senior officials to allow them to be effectively overseen. No one who gave evidence to the Inquiry was able to offer a substantive rationale for a system that was unduly complex and labyrinthine. The only defence offered for such complexity was that the system was generally well understood by those who had to work within it.210 The complexity, however, resulted in a number of problems. |
| 2.89. | Firstly, the system was inefficient. There were too many entities, groups, sub-groups, committees and sub-committees involved with preparedness and resilience. Work was being done by multiple entities at the same time. As is apparent from the ‘spaghetti diagrams’ and the entities described above, there were a large number of institutions, structures and systems that purported to govern and operate to prepare and build resilience across the UK, and yet there was an overlap between their roles and an absence of clarity about the division of responsibilities. |
| 2.90. | Secondly, fundamental gaps had opened up which had not been identified by the governments, senior officials and supporting organisations. The system was prone to operating in silos. The entirety of the system was not reviewed and inadequate consideration was given to bridging the gap between the groups that were responsible for the High Consequence Infectious Diseases Programme and those considering pandemic influenza to see if aspects of the programme would be useful for controlling the spread of a potential pandemic.211 As an example of this systemic issue of operating in silos, Ms Reed told the Inquiry that her remit included health protection, health security and pandemic preparedness. Although this was a broad portfolio with respect to pandemic preparedness, she said:
“There was no discussion with me about quarantining … There was no discussion with me about track and trace.”212 |
| 2.91. | Asked whether there was any debate at all about the possible necessity of border closures, self-isolation, or individual, mass or mandatory quarantines – or, indeed, anything of that kind – Ms Reed told the Inquiry that she was not aware of “any conversations on those areas of mitigation”.213 This lack of integration was symptomatic of a system that had ultimately grown to become too complex and disjointed. |
| 2.92. | Thirdly, there was a lack of focus. This was created by a lack of clear leadership and oversight by both ministers and officials. Across the UK, systems had grown to be overly bureaucratic. Instead of focusing on skills, technology and infrastructure, they were focused on creating groups, sub-groups and documents. As a result of the abolition of the Threats, Hazards, Resilience and Contingencies sub-Committee, there was no ongoing ministerial oversight of one of the UK’s most significant risks.214 The effect was that preparedness and resilience were not being scrutinised at the highest levels of government. |
| 2.93. | To take one example, Public Health England had its own Emergency Response Department, which sat within its Health Protection Directorate. There were teams that supported Public Health England’s preparedness work. These included a team of senior medical advisers, a corporate resilience team, a training team, an exercising team, a scientific computing service, a behavioural science and insights team, a geographic information systems team, a mathematical modelling team and a vector-borne disease threats and medical entomology team.215 These teams were in addition to the Pandemic Influenza Preparedness Programme Board and the Pandemic Flu Readiness Board. Despite the number of these teams, groups and sub-groups, the Department of Health and Social Care had not ensured that they collectively or individually amounted to a permanent standing capacity to prepare for, prevent and respond to health emergencies at scale. This was only achieved with the creation of the UK Health Security Agency in October 2021.216 |
| 2.94. | Proper preparedness and resilience can only come from systems (at the UK level and in each government or administration) that are streamlined, better integrated and more focused on what is to be achieved. The systems should be simplified and recalibrated so that they better meet the needs of those required to prepare for and respond to emergencies, and those in charge of them must be more accountable. The institutions should ensure that their component parts communicate more efficiently, that flaws are identified and gaps are filled, and that responders are not overwhelmed by needless bureaucracy and complicated policy. Overall, there should be fewer entities, working more closely with each other and within more clearly defined roles. |
| 2.95. | There should have been more effective leadership and oversight from ministers and officials. Prior to the Covid-19 pandemic, there was no ministerial leadership within the UK government and devolved administrations that could consider strategy, direct policy and make decisions across the whole of government to prepare for and build resilience to whole-system civil emergencies. There was no UK or equivalent emergency preparedness and resilience committee leading, overseeing and coordinating the system. |
| 2.96. | What is needed is a standing group of ministers, in the UK government and in each of the devolved administrations, focused on preparedness for and resilience to whole-system civil emergencies. A single Cabinet-level ministerial committee and a single cross-departmental group of senior officials should form the core leadership structure across the UK. The cross-departmental group of senior officials should be put in place to, firstly, conduct a review to simplify the current system and then, secondly, oversee and provide leadership to the implementation of policy within the simplified structure. The constitutional arrangements in Northern Ireland do not lend themselves to The Executive Office directing the work of other departments, and it is beyond this Inquiry’s remit to recommend changes to those arrangements. However, the overall aim of maintaining a complete overview of pandemic preparedness applies equally in Northern Ireland as in the rest of the UK. |
| 2.97. | In December 2022, with the publication of The UK Government Resilience Framework, the UK government announced part of its solution to the problem of an absence of leadership to be the establishment of the National Security Ministers (Resilience) sub-Committee.217 This is chaired by the Chancellor of the Duchy of Lancaster (a Cabinet-level post in the Cabinet Office) and comprises: the Chancellor of the Exchequer; the Secretaries of State for the Home Department, Defence, and Levelling Up, Housing and Communities; the Minister for Intergovernmental Relations; and the Minister for the Cabinet Office and Paymaster General.218 However, it does not currently include the Secretary of State for Health and Social Care. The Inquiry recommends that the Secretary of State for Health and Social Care be made a standing member, as it is likely that any whole-system civil emergency will have implications for health and social care. According to Oliver Dowden MP, Parliamentary Secretary to the Cabinet Office from January 2018 to July 2019 and Minister for the Cabinet Office from July 2019 to February 2020, the Resilience sub-Committee is capable of making decisions across government. The difference between the now-defunct Threats, Hazards, Resilience and Contingencies sub-Committee and the Resilience sub-Committee is that the latter is now intended to consider how to prevent risks materialising in the first place.219 |
| 2.98. | Reorganisations have the potential to undermine preparedness and resilience when they involve the frequent movement of groups of ministers and officials around existing institutions. The Inquiry is therefore reluctant to recommend yet another change. However, the creation of a core structure of leadership and oversight should bring about changes to the preparedness and resilience systems that lead to permanent, and not just transient, improvements. Firstly, one of the primary aims of such a core structure should be to rationalise and streamline the number of groups and committees responsible for whole-system civil emergency preparedness and resilience – only those with a clearly defined purpose should remain. Secondly, it is the core structures that will ultimately be accountable for ensuring that the systems of preparedness and resilience are effective and ready for the next pandemic. This should bring seriousness and focus to the importance of their roles and responsibilities. |
Recommendation 1: A simplified structure for whole-system civil emergency preparedness and resilience
The governments of the UK, Scotland, Wales and Northern Ireland should each simplify and reduce the number of structures with responsibility for preparing for and building resilience to whole-system civil emergencies.
The core structures should be:
- a single Cabinet-level or equivalent ministerial committee (including the senior minister responsible for health and social care) responsible for whole-system civil emergency preparedness and resilience for each government, which meets regularly and is chaired by the leader or deputy leader of the relevant government; and
- a single cross-departmental group of senior officials in each government (which reports regularly to the Cabinet-level or equivalent ministerial committee) to oversee and implement policy on civil emergency preparedness and resilience.
This should be put in place within 12 months of the publication of this Report.
Within 6 months of the creation of the group of senior officials, it should complete a review to simplify and reduce the number of structures responsible for whole- system civil emergency preparedness and resilience.
Subsequently, within 24 months of the publication of this Report, the ministerial committee should rationalise and streamline subordinate or supporting groups and committees responsible for whole-system civil emergency preparedness and resilience. Any groups and committees retained or created to support this core structure should have a clear purpose and should report regularly about progress with, and completion of, tasks assigned to them.
The lead government department model for whole- system civil emergencies
| 2.99. | When the Covid-19 pandemic took hold, it was, in practice, the Prime Minister, 10 Downing Street and the Cabinet Office that took the lead for the whole of the UK government by coordinating the emergency response between government departments and agencies.220 As it has the authority of the Prime Minister behind it, the Cabinet Office is deemed to have the power to direct other government departments and supporting organisations to work together in response to whole-system civil emergencies. However, it is the Department of Health and Social Care – which of course has a significant stake in any health emergency – that was and remains the lead government department for pandemic preparedness and resilience in England. |
| 2.100. | There are a number of significant problems with the current approach. |
| 2.101. | Firstly, risks are allocated to individual government departments, irrespective of whether they may cause a whole-system civil emergency. There are clear limitations to this. While pandemics are the responsibility of the Department of Health and Social Care, it is clear that they have the potential to trigger social and economic crises that require a wider response from a greater range of institutions at the national, regional and local levels of government – they require the capabilities of the whole system of government. Sir Oliver Letwin considered that whole-system civil emergency risks cannot be “owned” by a single government department.221 The Inquiry agrees. |
| 2.102. | Secondly, a whole-system civil emergency such as a pandemic requires, by definition, a cross-departmental approach. The scale of coordinating, directing and leading on preparedness and resilience across all UK government departments is so wide-ranging and the task so complex that it is difficult to envisage any single department being able to manage on its own, especially when combined with the responsibilities that departments have for day-to-day governance. |
| 2.103. | Thirdly, in preparing for whole-system civil emergencies, as opposed to other civil emergencies, every policy and decision involves significant trade-offs and compromises. For example, if the Department of Health and Social Care considered that an effective policy to improve pandemic preparedness would be to build health security infrastructure at the border, it would have to direct the Home Office to do so. Other departments, such as the Foreign, Commonwealth and Development Office and the Department for Business and Trade, might take a different but still reasonable view about the objectives and possible outcomes of the policy. Similarly, if the Department of Health and Social Care considered that an effective pandemic preparedness policy required significant economic support to individuals and businesses in the UK, the Treasury may have reasonable fiscal concerns. These issues are not capable of being resolved by the Department of Health and Social Care. |
| 2.104. | Fourthly, building preparedness for and resilience to whole-system civil emergencies requires collaboration between governments, government departments and directorates across the UK. This is because they occur across the UK’s internal borders. It is therefore necessary in preparing for events such as a pandemic that a department at the centre of the UK government that is capable of coordinating with the devolved administrations is put in charge of preparedness and resilience. |
| 2.105. | The Inquiry concludes that the lead government department model is fundamentally unsuited to preparing for and building resilience to whole-system civil emergencies such as pandemics. The requirements of acute crises that place demands on the whole of the UK government and devolved administrations at once requires a different approach. It is therefore necessary to place in charge the only government department that has the power and authority necessary to take the lead – the Cabinet Office. It has the decision-making power of the Prime Minister and the oversight and ability to coordinate the activities of the whole government. |
| 2.106. | The UK government has acknowledged that the lead government department model has its limitations:
|
| 2.107. | The solutions currently proposed do not go far enough, as individual government departments remain in charge of preparedness for and resilience to the risks allocated to them. A radical change to the system is required. |
| 2.108. | The limitations on the ability of departments, such as the Department of Health and Social Care, to coordinate and direct policy across government should be recognised. The lead government department model for preparing for and building resilience to whole-system civil emergencies should be abolished. |
| 2.109. | The Cabinet Office should take the lead, on behalf of the UK government, on monitoring the preparedness and resilience of other departments, supporting departments to correct problems and escalating issues to the UK Cabinet-level committee and group of senior officials as recommended in this Report. For these types of emergencies, the Cabinet-level committee and group of senior officials should then ensure that there is a cross-government approach to risks that are likely to have the greatest impact on the UK. |
| 2.110. | The aim should be for all government departments to work together to prepare for whole-system civil emergencies in the same way that they are required to work together in response. This cannot be achieved under the current system. |
Recommendation 2: Cabinet Office leadership for whole-system civil emergencies in the UK
The UK government should:
- abolish the lead government department model for whole-system civil emergency preparedness and resilience; and
- require the Cabinet Office to lead on preparing for and building resilience to whole-system civil emergencies across UK government departments, including monitoring the preparedness and resilience of other departments, supporting departments to correct problems, and escalating issues to the UK Cabinet-level ministerial committee and group of senior officials in Recommendation 1.
| 2.111. | The lead government department model also applies in Northern Ireland. Given the constitutional settlement in Northern Ireland, the Inquiry has not recommended a formal change to its arrangements, but, nonetheless, there should be consideration of giving effect to this recommendation in light of the issues identified in this Report. |
- INQ000204014
- INQ000196611_0005 para 1
- INQ000196611_0011 para 22
- INQ000196611_0012 para 22
- INQ000196611_0011-0012 para 22
- INQ000196611_0024, 0031 paras 60, 78
- INQ000196611_0029-0030 para 74
- INQ000196611_0028-0029 paras 69-71
- David Heymann 15 June 2023 39/7-41/15; INQ000195846_0009 para 31
- INQ000196611_0032 para 83; INQ000195846_0039-0040, 0046 paras 192-194, 232
- See the definition of an ‘emergency’ in section 1 of the Civil Contingencies Act 2004 (https://www.legislation.gov.uk/ukpga/2004/36/contents)
- INQ000145733_0002 para 2.2; INQ000182612_0029 paras 3.71-3.72; The UK Government Resilience Framework, HM Government, December 2022, pp81-83 (https://www.gov.uk/government/publications/the-uk-government-resilience-framework; INQ000097685)
- National Risk Register, HM Government, 2023, pp75-76, 150-155 (https://assets.publishing.service.gov.uk/ media/64ca1dfe19f5622669f3c1b1/2023_NATIONAL_RISK_REGISTER_NRR.pdf; INQ000357285); INQ000376140_0010, 0015; Bruce Mann 15 June 2023 155/11-14; Oliver Letwin 20 June 2023 54/2-19
- INQ000177810_0005-0007 paras 17-18, 20, 22
- Oliver Letwin 20 June 2023 54/19-22
- Civil Contingencies Act 2004 (https://www.legislation.gov.uk/ukpga/2004/36/contents); INQ000196532
- INQ000377435; INQ000377436
- INQ000148405_0004 para 14
- David Heymann 15 June 2023 42/14-16
- INQ000196611_0024-0027 paras 62-67; see also INQ000196611_0022-0024 paras 50-61
- Charlotte Hammer 14 June 2023 115/12-15
- The National Security Secretariat is headed by the National Security Adviser, who is the Prime Minister’s senior adviser on national security issues (see Katharine Hammond 16 June 2023 81/8-20).
- INQ000099517_0010 para 2.22
- INQ000145733_0002 para 2.2; INQ000099517_0010 para 2.22
- INQ000099517_0010 para 2.22
- Katharine Hammond 16 June 2023 77/19-78/23; INQ000145733_0010 para 2.27
- Katharine Hammond 16 June 2023 92/20-93/13
- INQ000145733 _0011 paras 3.1-3.2
- INQ000145733_0011 para 3.1
- INQ000177808_0002 para 4iii
- INQ000177808_0002 para 4iii
- INQ000177808_0002 para 5
- INQ000145733_0002 para 2.2
- Katharine Hammond 16 June 2023 81/17-84/10; INQ000194051_0022 para 93
- Katharine Hammond 16 June 2023 81/17-84/10; INQ000194051_0023 para 95
- INQ000177808_0004 para 15
- INQ000177808_0004-0005 paras 14-22
- INQ000177808_0004 para 15
- INQ000177808_0004 para 16
- UK Influenza Pandemic Preparedness Strategy 2011, Department of Health, November 2011, para 3.27 (https://assets.publishing.service.gov.uk media/5a7c4767e5274a2041cf2ee3/dh_131040.pdf; INQ000102974)
- INQ000177808_0004-0006 paras 15, 21-23; INQ000177810_0012 para 41
- INQ000128057
- Katharine Hammond 16 June 2023 84/11-85/8; see also INQ000195845_0013 para 3.36
- Katharine Hammond 16 June 2023 85/1-8
- Prior to January 2018, the Department of Health and Social Care was called the Department of Health. This Report uses the correct name for the department and its Secretary of State according to the relevant time period. For references that span both before and after January 2018, the Report uses the current name.
- The Lead Government Department and Its Role – Guidance and Best Practice, Cabinet Office, March 2004, p4, para 1 (https://assets.publishing.service.gov.uk/media/5a79b2fded915d07d35b772a/lead-government-departments-role.pdf; INQ000022687)
- INQ000184643_0021 para 101
- INQ000184643_0022 para 104
- INQ000184643_0022 para 104
- INQ000195847_0004 para 21; INQ000184643_0061 para 325
- INQ000145733_0021-0025 paras 3.33-3.42. This included, for example, the Home Office, the Treasury, the Ministry of Defence, the Department for Education, and the Foreign, Commonwealth and Development Office (INQ000184643_0032 para 178).
- INQ000195847_0004 para 21
- INQ000057649_0001 paras 1-2
- INQ000148429_0006 para 22
- INQ000192268_0012 para 44
- INQ000090332_0001
- INQ000192268_0011 para 41
- INQ000090332_0001
- INQ000192268_0011 para 43
- INQ000192268_0004 para 15
- INQ000148429_0007 para 23
- INQ000184643_0022 para 106
- INQ000184638_0014 para 3.1
- INQ000184638_0011 paras 2.7-2.8, 2.10
- INQ000148407_0009-0010 paras 20, 22
- INQ000184643_0025-0026 paras 122-128; INQ000196611_0020 para 45; INQ000184638_0018 para 3.14; INQ000207293_0003-0007 paras 2.1-2.13; INQ000147707_0024 para 56; INQ000148429_0064-0065 paras 256-257. NERVTAG was preceded by the Scientific Pandemic Influenza Advisory Committee from 2008 to 2014, which in turn was preceded by both the National Expert Panel on New and Emerging Infections between 2003 and 2008 and the Scientific Advisory Group on Pandemic Influenza between 2005 and 2008.
- INQ000184643_0026-0027 paras 129-132; INQ000196611_0021 para 47; INQ000184638_0018 para 3.15; INQ000184639_0007 paras 3.14-3.15; INQ000148429_0063 paras 250-251
- INQ000184643_0027 paras 133-137; INQ000196611_0020-0021 para 46; INQ000184638_0019 para 3.16; INQ000148429_0063-0064 paras 252-255
- INQ000184643_0027-0028 paras 138-143; INQ000184638_0019 para 3.17
- INQ000184643_0029-0030 paras 148-159; INQ000184638_0016 paras 3.9-3.10
- INQ000184643_0030 paras 160-162; INQ000184638_0017 para 3.11
- INQ000184643_0030 paras 163-165; INQ000184638_0056-0057 paras 6.33-6.36
- INQ000184643_0030-0031 paras 166-172; INQ000184638_0019 para 3.18
- INQ000184643_0031-0032 paras 173-176; INQ000184638_0016 paras 3.7-3.8; INQ000148429_0065 para 258
- INQ000148407_0010 para 25
- INQ000148407_0010-0011 paras 23-24, 28; INQ000147810_0004 para 10
- INQ000147810_0004 paras 7, 9-10
- INQ000148407_0007 paras 14-17
- INQ000148407_0007 para 14; INQ000147810_0003 paras 5-6
- INQ000148407_0014 paras 33-35
- INQ000184639_0018 paras 6.2-6.4
- INQ000184639_0018 paras 6.2-6.4
- INQ000184639_0018 para 6.1
- Jeremy Farrar 29 June 2023 11/1-12/15
- INQ000145733_0007 para 2.17
- From May 2006 to January 2018, what is now the Department for Levelling Up, Housing and Communities was called the Department for Communities and Local Government. From January 2018 to September 2021, it was known as the Ministry of Housing, Communities and Local Government. In September 2021, it was renamed the Department for Levelling Up, Housing and Communities. This Report uses the correct name for the department according to the relevant time period. For references that span both before and after September 2021, the Report uses the current name.
- 87 INQ000065107_0012-0013 para 33
- Catherine Frances 29 June 2023 127/15-132/9
- Mark Lloyd 12 July 2023 79/3-7
- Mark Lloyd 12 July 2023 79/8-16
- Jim McManus 5 July 2023 46/9-14
- Jim McManus 5 July 2023 46/15-48/4
- Jim McManus 5 July 2023 47/25-48/4
- INQ000183419_0036 para 201
- INQ000183419_0040-0041 paras 225-230
- See Kevin Fenton 5 July 2023 89/25-90/7; INQ000183419_0017, 0021, 0040-0041 paras 107-108, 125-126, 225-230; Jim McManus 5 July 2023 57/7-58/1; INQ000183419_0019, 0040 paras 118, 225. There are about 151 directors of public health in England, who are employed by local authorities. In Scotland and Wales, the 8 and 7 directors of public health, respectively, are employed by NHS health boards. In Northern Ireland, there is only one director of public health, who is employed by the Public Health Agency (see Jim McManus 5 July 2023 36/16-38/9).
- INQ000205178_0098 para 146
- Roger Hargreaves 22 June 2023 44/2-5
- Oliver Dowden 21 June 2023 134/20-137/2
- INQ000184894_0017 para 61
- INQ000185352_0002 para 6
- Preparing Scotland: Scottish Guidance on Resilience, Scottish Government, 2017, p24 (https://ready.scot/sites/default/ files/2020-09/preparing scotland-hub-updated-published-version-may-2019-new-h-s-diagram.pdf; INQ000102938)
- INQ000102935
- John Swinney 29 June 2023 82/10
- John Swinney 29 June 2023 81/17-83/22
- Gillian Russell 28 June 2023 33/6-14
- John Swinney 29 June 2023 83/12-15
- Preparing Scotland: Scottish Guidance on Resilience, Scottish Government, 2017 (https://ready.scot/sites/default/files/2020-09/ preparing-scotland-hub-updated-published-version-may-2019-new-h-s-diagram.pdf; INQ000102938)
- INQ000184894_0018 para 64
- INQ000185343_0003 para 7; INQ000184894_0014, 0018-0019 paras 49-50, 64
- INQ000185343_0003 para 9
- INQ000185343_0006 para 19
- INQ000239420_0001-0002, 0006 paras 4, 6, 29; INQ000184894_0017, 0019 paras 61, 66
- INQ000239420_0006 para 29
- INQ000184894_0006-007 para 22
- INQ000185343_0002 para 5; INQ000239420_0002 para 6; INQ000184894_0017 para 61
- INQ000185343_0007-0008 paras 24-25
- Jim McMenamin 22 June 2023 174/6-24. The Inquiry was told that the joint accountability was because the health of the population, at the local level, was the focus of Health Protection Scotland’s efforts (Jim McMenamin 22 June 2023 178/18-22).
- INQ000184897_0002 para 4
- INQ000183410_0015 paras 1.4.16-1.4.17
- INQ000184897_0003 para 6
- INQ000183412_0003 paras 7-8
- INQ000185342_0002 para 4
- INQ000184897_0003 para 7
- INQ000184894_0012 para 40
- INQ000184894_0013 para 42
- INQ000184894_0012-0013 paras 40-43
- INQ000184894_0019 para 69
- INQ000185352_0003 para 9
- John Swinney 29 June 2023 84/21-85/25
- INQ000130469_0032-0033 para 134
- 132 INQ000130469_0003 para 11; see also paras 80-83; INQ000204014_0009-0012
- Frank Atherton 3 July 2023 7/13-12/13
- Quentin Sandifer 4 July 2023 67/11-18
- Frank Atherton 3 July 2023 40/24-41/9
- INQ000130469_0051 para 193
- INQ000190662_0007 para 24; INQ000128975; INQ000130469_0054 para 204
- INQ000107114_0001; INQ000130469_0035, 0054 paras 144, 204
- INQ000130469_0032 para 133
- INQ000130469_0053-0054 paras 201-203
- INQ000107116
- INQ000130469_0046 para 181; INQ000107115
- INQ000130469_0051 para 195; INQ000190662_0008 para 27
- INQ000130469_0052 para 199; INQ000190662_0023-0024 paras 84-85
- INQ000130469_0052–0053 para 200; INQ000190662_0023-0024 paras 84-85
- Frank Atherton 3 July 2023 40/24-41/9
- INQ000184901_0003 para 9
- INQ000107106_0003 para 17
- Frank Atherton 3 July 2023 54/10-56/7
- INQ000130469_0003 para 11
- Andrew Goodall 3 July 2023 92/14-16
- INQ000184902_0002-0003 paras 5-9
- Andrew Goodall 4 July 2023 57/8-58/3
- Chris Llewelyn 12 July 2023 73/4-9
- INQ000177802_0011 para 27
- INQ000203349_0048 para 126
- INQ000130469_0048 para 188
- INQ000177802_0011 para 30; see also Quentin Sandifer 4 July 2023 70/14-18
- Civil Emergencies in Wales, Wales Audit Office, 2012, p8, para 8 (https://www.audit.wales/sites/default/files Civi__Emergencies_in_Wales_English_2012_14.pdf; INQ000107113)
- INQ000177802_0009 para 20; see also Quentin Sandifer 4 July 2023 70/5-11
- INQ000177802_0009 para 21; see also Quentin Sandifer 4 July 2023 70/5-11; INQ000130469_0045 para 179
- Chris Llewelyn 12 July 2023 74/8-11
- Chris Llewelyn 12 July 2023 74/17-75/17
- Civil Emergencies in Wales, Wales Audit Office, 2012, p10, para 17 (https://www.audit.wales/sites/default/files/Civi__Emergencies_in_Wales_English_2012_14.pdf; INQ000107113)
- Civil Emergencies in Wales, Wales Audit Office, 2012, p10, para 17 (https://www.audit.wales/sites/default/files/Civi__Emergencies_in_Wales_English_2012_14.pdf; INQ000107113)
- Civil Emergencies in Wales, Wales Audit Office, 2012, p10, para 18 (https://www.audit.wales/sites/default/files/Civi__Emergencies_in_Wales_English_2012_14.pdf; INQ000107113)
- INQ000187620_0024 para 93
- INQ000185350_0003 para 10; INQ000195848_0001-0002 para 4
- INQ000187620_0024 para 93; see also INQ000187620_0037-0038 paras 153-155
- INQ000187620_0006 para 20
- INQ000187620_0010, 0016, 0024 paras 30, 55, 94
- INQ000187620_0024 para 94
- Northern Ireland Health and Social Care Influenza Pandemic Preparedness and Response Guidance, Department of Health, Social Services and Public Safety, January 2013, p11 (http://www.niassembly.gov.uk/globalassets/documents/raise/deposited-papers/2013/dp1089.pdf; INQ000001191); Richard Pengelly 11 July 2023 68/24-69/2. Note: On 9 May 2016, the Department of Health, Social Services and Public Safety in Northern Ireland became the Department of Health, and it is referred to in this Report as the Department of Health (Northern Ireland) unless referring specifically to before May 2016. For references that span both before and after May 2016, the Report uses the current name.
- INQ000215123_0003-0004 paras 10, 12
- INQ000215123_0005-0006 paras 16-23
- See INQ000187620_0024, 0026-0029, 0037-0040 paras 94, 101-112, 151-152, 156-160
- See also INQ000187620_0042 para 169 regarding other groups within the Civil Contingencies Group (Northern Ireland)
- There was also: the Northern Ireland Pandemic Flu Oversight Group, which led on health and social care preparedness and response (INQ000215123_0026-0027 paras 97-99); the Health Emergency Planning Forum, which shared information between the Department of Health and health and social care organisations (INQ000215123_0016-0017 para 60); the Critical Threats Preparedness Steering Group, to understand the critical threats picture for Northern Ireland (INQ000215123_0017 para 61); the Joint Emergency Planning Board, to assure health and social care preparedness (INQ000215123_0017 para 62); and the Joint Emergency Planning Team, which supported the Joint Emergency Planning Board (INQ000215123_0017-0018 para 63).
- INQ000184642_0002-0006 paras 2.1-2.13; INQ000174824
- INQ000215123_0026 paras 94-96
- INQ000184642_0005 para 2.9
- Denis McMahon 6 July 2023 47/17-48/2
- Denis McMahon 6 July 2023 38/14-39/17
- Denis McMahon 6 July 2023 56/18-25
- Michael McBride 10 July 2023 125/22-127/22
- Michael McBride 10 July 2023 115/21-117/13
- INQ000187306_0003 paras 7-14
- Michael McBride 10 July 2023 155/20-156/2
- Michael McBride 10 July 2023 156/1-2
- Patrick Vallance 22 June 2023 148/4-5; Michael McBride 10 July 2023 155/20-21; Arlene Foster 11 July 2023 41/20-25; Denis McMahon 6 July 2023 94/3-11
- See INQ000187620_0004-0013 paras 7-42
- INQ000187620_0013 paras 43-44
- INQ000185350_0006 para 22
- INQ000185350_0006 para 22
- INQ000185350_0006-0008 paras 23-25
- Denis McMahon 6 July 2023 13/10-19; Robin Swann 6 July 2023 159/9-160/25; INQ000192270_0015 para 45
- Michael McBride 10 July 2023 129/4-15
- Systems, Not Structures: Changing Health & Social Care, Expert Panel, 2016 (https://www.health-ni.gov.uk/sites/default/files/publications/health/expert-panel-full-report.pdf; INQ000205179); Health and Wellbeing 2026: Delivering Together, Department of Health, 2016 (https://www.healthni.gov.uk/sites/default/files/publications/health/health-and-wellbeing-2026-delivering-together.pdf; INQ000185457)
- Michael McBride 10 July 2023 131/6-133/14
- INQ000192270_005-006, 0015-0016 paras 10-11, 45-47
- Robin Swann 6 July 2023 159/14-160/4
- Michael McBride 10 July 2023 152/15-24
- Michael McBride 10 July 2023 151/7-9
- Technical Report on the COVID-19 Pandemic in the UK, Department of Health and Social Care, 1 December 2022, pp127, 176 (https://assets.publishing.service.gov.uk/media/63bd35b78fa8f55e3ac750c4/Technical-report-on-the-COVID-19-pandemic-in-the-UK-PRINT.pdf; INQ000101642)
- See INQ000203352_0016-0017 paras 46-48; Michael McBride 10 July 2023 147/25-155/1; Arlene Foster 11 July 2023 38/3-39/24; Michelle O’Neill 12 July 2023 45/19-46/11
- INQ000187620_0021-0023 paras 81-92; Denis McMahon 6 July 2023 57/6-62/4
- Denis McMahon 6 July 2023 22/24-23/13; INQ000187620_0022 para 84
- INQ000187620_0022 para 85; INQ000214130_0004-0005
- Michael McBride 10 July 2023 147/25-155/1; Arlene Foster 11 July 2023 38/3-39/24; Michelle O’Neill 12 July 2023 45/19-46/11; INQ000203352_0016-0017 paras 46-48
- See, for example, Denis McMahon 6 July 2023 56/2-25; Closing statement on behalf of the Cabinet Office 19 July 2023 89/6-23; Mark Drakeford 4 July 2023 163/9-164/2, 165/16-166/4; Katharine Hammond 16 June 2023 104/5-108/10
- Christopher Wormald 19 June 2023 110/6-111/19, 118/23-122/9
- Emma Reed 26 June 2023 10/10-18
- Emma Reed 26 June 2023 17/18-23
- Katharine Hammond 16 June 2023 84/11-85/8
- INQ000148429_0042-0044 paras 153-164
- INQ000184643_0022 paras 106-107
- INQ000377437_0003
- INQ000377438_0004
- Oliver Dowden 21 June 2023 78/3-17
- Katharine Hammond 16 June 2023 77/12-78/23
- Oliver Letwin 20 June 2023 55/10-12
- INQ000056240_0011-0012 para 14
- The UK Government Resilience Framework, HM Government, December 2022, p13, paras 25-26 (https://www.gov.uk/government/publications/the-uk-government-resilience-framework; INQ000097685)
- UK Biological Security Strategy, HM Government, June 2023, pp56-58 (https://assets.publishing.service.gov.uk/media/64c0ded51e10bf000e17ceba/UK_Biological_Security_Strategy.pdf; INQ000208910)
Chapter 3: The assessment of risk
Introduction
| 3.1. | Risk is an essential part of all our lives. It is the possibility of bad things happening and the uncertainty of predicting what those bad things might be. The assessment and management of risk is a task with which each of us becomes innately familiar. |
| 3.2. | As observed in The UK Government Resilience Framework published in December 2022, the starting point for resilience (the underlying ability of society to withstand crises and the ability to adapt to disruptive events) is understanding risk.1 If risks are not adequately anticipated and understood, it is difficult to prepare for or build resilience to catastrophic events and their effects. |
| 3.3. | There are some simple but important questions that underpin risk assessment. They include:
|
| 3.4. | In planning for catastrophic events, one should therefore first identify the risk and then develop a strategy to address it. The strategy should assess what can, and cannot, be done about that risk in advance, whether it can be prevented from occurring or, if it cannot, whether its harmful effects can be reduced or mitigated.2 This chapter examines the risk assessment systems for pandemic preparedness across the UK. |
Risk assessment by the UK government and devolved administrations
| 3.5. | Pandemic influenza was consistently described as the most significant civil emergency risk facing the UK in the UK’s risk assessments from 2005 until the eve of the coronavirus (Covid-19) pandemic.3 The ‘day one’ briefing received by Matt Hancock MP, Secretary of State for Health and Social Care from July 2018 to June 2021, was given by Sir Christopher Wormald, Permanent Secretary to the Department of Health (and Social Care) from May 2016.4 It was accompanied by a number of briefing documents.5 These included a note from Clara Swinson, Director General for Global and Public Health at the department from November 2016, which stated:
“Pandemic flu is the government’s highest risk (on the Cabinet Office’s national risk register). In any given year we estimate the likelihood of a pandemic to be 3%, based on 3 pandemics in the 20th century, and the impact of a ‘reasonable worst case scenario’ to be 750k deaths. We have contingency plans and a work programme to keep this up to date and supplement it. We can brief you further on the current threat and our work in response.”6 (emphasis in original) |
Across the United Kingdom
| 3.6. | In the years leading up to the Covid-19 pandemic, the Civil Contingencies Secretariat within the Cabinet Office was responsible for preparing for, responding to and learning lessons from major emergencies.7 It produced UK-wide risk assessments to inform planning at national and local levels. The approach of the devolved administrations did not materially differ from the UK government’s approach to the assessment of risk. |
| 3.7. | Before 2019, the Civil Contingencies Secretariat produced, in coordination with other government departments, agencies and devolved administrations, two separate UK-wide risk assessments.8 The National Risk Assessment was a “strategic medium term planning tool” for domestic emergencies over a five-year timescale, designed to provide a basis for contingency planning at national and local levels.9 The National Security Risk Assessment focused on broader national security risks (including international risks impacting UK interests) over a 20-year timescale.10 Generally, human infectious disease risks were recorded on the National Risk Assessment. In 2019, the Civil Contingencies Secretariat combined the two UK-wide risk assessments into a single National Security Risk Assessment to create a unified framework.11 |
| 3.8. | In addition, from 2008, the Civil Contingencies Secretariat published the National Risk Register as a public-facing version of the National Risk Assessment and the National Security Risk Assessment, which were and remain classified.12 Each document was revised several times before the start of the Covid-19 pandemic.13 |
The devolved nations
| 3.9. | In outward appearance, the risk assessments by the devolved administrations were their own documents, but their method simply copied that of the UK government. This limited their utility as a risk assessment tool because they did not assess how particular risks would affect the population of the individual nations and failed to take into account sufficiently, or at all, the underlying health, social and economic circumstances of each population. Risk assessments specific to each devolved administration (and to England) would have signalled, in advance of the pandemic, how to tailor the response to the needs of each population. |
Scotland
| 3.10. | In January 2015, John Swinney MSP, Deputy First Minister in the Scottish Government from November 2014 to March 2023, commissioned the development of a Scottish Risk Assessment, the first and only edition of which was published in 2018.14 It was intended to complement the UK-wide assessments, providing a Scottish context for risks where Scotland would be affected differently from the rest of the UK, as well as information to assist planning by local responders.15 |
| 3.11. | Although a separate document was created, Gillian Russell, Director of Safer Communities in the Scottish Government from June 2015 to March 2020, told the Inquiry: “[W]hat we did do was take that [UK] National Risk Assessment and then look at what a Scottish risk assessment should look like on the back of that.”16 In short, the population figures in the UK-wide National Risk Assessment were replaced with those for the Scottish population. There was no separate analysis for Scotland that adequately took into account specific factors that might particularly affect the population of Scotland.17 |
Wales
| 3.12. | The Welsh Government relied on the UK-wide level of risk assessment.18 It did not separate the UK-wide material into an assessment of how civil emergency risks faced by the UK might specifically impact the population of Wales.19 Mark Drakeford MS, First Minister of Wales from December 2018 to March 2024, told the Inquiry that, for certain purposes, it was “sensible from a Welsh perspective … to rely on the expertise and the capacity” of the UK government.20 Prior to the pandemic, there was therefore no Welsh national risk register to take into account the specific circumstances in Wales. |
| 3.13. | A 2023 Review of Civil Contingencies in Wales recommended the creation of a Welsh risk register.21 Dr Andrew Goodall, Permanent Secretary to the Welsh Government from September 2021, told the Inquiry that Wales was “introducing” a Welsh national risk register.22 Mr Drakeford acknowledged that “contemporary thinking is that that intermediate Welsh level [of risk assessment] may need strengthening”.23 Reg Kilpatrick, Director General for Covid Coordination in the Welsh Government from September 2020, informed the Inquiry that there was a “very strong prospect, if not a certainty” that it would be done.24 As of June 2024, this was not yet in place. |
| 3.14. | While the Welsh Government did not develop a Welsh risk register to assess how civil emergency risks might affect the people of Wales, it did maintain corporate risk registers, but these only identified risks to its ability to carry out its responsibilities. The 2014 corporate risk register identified the risk of pandemic influenza as one of just five examples of the “full range of national hazards and threats” facing Wales, but in terms that were broad and uninformative as to the detail of pandemic preparedness, resilience and response.25 The 2019 corporate risk register gave no specific consideration at all to pandemic influenza as a risk and, therefore, no specific consideration of the countermeasures to meet it. Instead, the impact of all types of civil emergencies were sought to be captured by the term “disruption event”.26 Similarly, although the risk of pandemic influenza was included in the departmental risk register of the Welsh Government’s Health and Social Services Group, it does not appear to have been identified as an important cross-government issue.27 Moreover, the scores recorded against the risk in the Welsh Government’s corporate risk register indicated that the Welsh Government believed its ability to mitigate the impact of a pandemic had improved.28 As Dr Goodall admitted, the risks “were too generalised, and that probably gave some inappropriate assurance” and “in hindsight” the risk scores should have been higher.29 The risk assessments did not reflect the reality on the ground. |
Northern Ireland
| 3.15. | Prior to the pandemic, Northern Ireland “fundamentally … followed the UK approach” to risk assessment.30 A Northern Ireland Risk Assessment was prepared in 2009 and 2013.31 This took the approach of the UK-wide risk assessments and applied it to Northern Ireland.32 The references to human infectious disease risks provided little further information beyond what was contained in the UK-wide risk assessments.33 There were no updates to the Northern Ireland Risk Assessment between 2013 and January 2020.34 The next, the Northern Ireland Risk Register, was produced during the Covid-19 pandemic in July 2022.35 |
| 3.16. | The Northern Ireland Executive did, however, maintain corporate risk registers. The 2018/2019 Department of Health (Northern Ireland) Departmental Risk Register warned:
“The health and social care sector may be unable to respond to the health Insufficient action was taken on this crucial warning in advance of the pandemic. The Inquiry was informed that this was because the Department of Health (Northern Ireland) did not have sufficient resources.37 |
The key flaws in risk assessments
| 3.17. | There were five major flaws in the approach to risk assessment in the UK that had a material impact on preparedness for and resilience to whole-system civil emergencies such as pandemics:
|
| 3.18. | As a result of the devolved administrations adopting the UK government’s approach to risk, these flaws flowed through to their civil contingencies systems. |
| 3.19. | In January 2021, the Civil Contingencies Secretariat commissioned the Royal Academy of Engineering to carry out the first external review of the National Security Risk Assessment.38 Its final report was submitted to the Civil Contingencies Secretariat in September 2021.39 The UK government took into account parts of the report and produced a new edition of the National Security Risk Assessment in 2022 and an updated National Risk Register in August 2023.40 The extent to which recommendations on the five areas above have been taken into account by the UK government is examined below. |
Flaw 1: Reliance on a single scenario
| 3.20. | Scenarios are an established part of risk assessment practice. They involve “developing models of what might happen in the future” and “can help identify risk and explore uncertainty, consequences, and interdependencies”.41 They are useful but they have their limitations. |
| 3.21. | The UK-wide risk assessments deliberately did not capture every risk that the UK could face. Each set of risks was grouped together around a single “reasonable worst case scenario”.42 This was in order to:
“illustrate a manifestation of the risks in the [National Security Risk Assessment] by providing context, describing how the incident would play out, and quantifying the impact and likelihood of such an occurrence. [Reasonable worst-case scenarios] are intended to be read as a scenario, not a prediction, and are often subject to significant uncertainty.”43 |
| 3.22. | In the 2010 review into the UK’s response to the 2009 to 2010 H1N1 influenza pandemic (‘swine flu’), Dame Deirdre Hine recorded unease about the use of reasonable worst-case scenarios because of the potential for them to be interpreted as a prediction rather than as just one scenario against which to plan.44 The Inquiry agrees. Setting out multiple scenarios, up to and beyond the reasonable worst case, should result in more sophisticated planning and a greater range of possible responses. |
| 3.23. | Reasonable worst-case scenarios were intended to be “a challenging yet plausible manifestation of the risk”.45 They were only included within the list of risk scenarios if they met certain criteria.46 These included:
|
| 3.24. | Prior to the Covid-19 pandemic, the UK-wide risk assessment process consistently identified only two reasonable worst-case scenarios for human infectious diseases. These were:
(A high consequence infectious disease is one that typically has a high case fatality ratio, may be difficult to recognise and detect rapidly, can transmit in the community, and may not have an effective means of prevention or treatment. It requires an enhanced, specialist response.)51 |
| 3.25. | The difference between the two scenarios is reflected in Table 2, which summarises the reasonable worst-case scenarios from the 2014, 2016 and 2019 risk assessments. In each iteration, the numbers of fatalities and casualties (ie harm falling short of death) were envisaged to be much higher in the pandemic influenza scenario than in the scenario for emerging infectious diseases other than influenza. |
| Pandemic influenza: assumptions | Emerging infectious disease: assumptions | |
|---|---|---|
| 2014 | Fatalities: 750,000
Casualties: 50% of the population (See INQ000176765_0001, 0003, 0006-0007) |
Fatalities: 200
Casualties: 2,000 (See INQ000176766_0001, 0004-0005) |
| 2016 | Fatalities: 750,000
Casualties: 50% of the population, 30 million people (See INQ000176770_0001-0002, 0005-0006) |
Fatalities: 101 to 1,000
Casualties: 2,000 to 10,000 (See INQ000176771_0004) |
| 2019 | Fatalities: 820,000
Casualties: 50% of the population, 32.8 million people (See INQ000176776_0001, 0006-0007) |
Fatalities: 200
Casualties: 2,000 (See INQ000185135_0008) |
| 3.26. | The UK’s pandemic preparedness was focused on influenza as the only pandemic-scale reasonable worst-case scenario.52 It was assumed that this scenario would be sufficiently representative of all pandemics.53 However, too much weight was placed on this single scenario. This left a major gap in the UK’s assessment of risk, with ramifications for the entirety of the UK’s pandemic preparedness. It signalled to the system of preparedness for and resilience to civil emergencies in the UK that it was not necessary to prepare separately for an emerging infectious disease (other than influenza) that might reach the scale of a pandemic. As a result, there was inadequate consideration of the different skills, infrastructure, technology and resources that might be needed in such an event (see Chapter 5: Learning from experience). |
| 3.27. | The reasonable worst-case scenarios in the 2014 and 2016 National Risk Assessments were based on the February 2013 advice of the Advisory Committee on Dangerous Pathogens (an expert committee of the Department of Health).54 The 2019 National Security Risk Assessment retained a reasonable worst-case scenario for emerging infectious diseases and pandemic influenza with a similar number of fatalities and casualties as the 2014 and 2016 National Risk Assessments.55 Experts throughout the Western world advised that pandemic influenza represented the greatest large-scale health emergency.56 Pandemic influenza was – and remains – the greatest risk, but other forms of pandemic were, and are, also a risk. The scenario for an emerging infectious disease was based on data from the 2002 to 2003 severe acute respiratory syndrome (SARS) outbreak.57 It was described by the Advisory Committee on Dangerous Pathogens as an event that was “likely” and “probable”, but with the important caveat that “beyond that no estimate of likelihood or impact could at this stage be suggested”.58 |
| 3.28. | Despite this note of caution about the likelihood and impact of a respiratory emerging infectious disease, the Department of Health and Social Care made a significant error in adopting SARS as the sole basis for the reasonable worst-case scenario. In doing so, it sent the message that planning for a non-influenza pathogen should focus on an emerging infectious disease that would not be sufficiently transmissible to result in a pandemic. |
| 3.29. | The UK-wide risk assessments between 2008 and 2019 repeatedly asserted that the Department of Health and Social Care had developed a national contingency plan for dealing with SARS.59 This, they said, would provide the basis for dealing with any future SARS outbreak and was built on generic responses to outbreaks of infectious diseases and lessons learned during the 2002 to 2003 SARS outbreak. This appears to have been a false assurance. Despite requests from the Inquiry, no UK-wide contingency plan for SARS, Middle East respiratory syndrome (MERS) or any other high consequence infectious disease has been disclosed by the UK government. The Inquiry is not therefore satisfied that such plans ever existed. |
| 3.30. | The only SARS or MERS-specific contingency plans received in evidence by the Inquiry are interim plans held by the Health Protection Agency and Public Health England respectively. The SARS interim plan, dated December 2003, described itself as “a contingency plan for a co-ordinated response from the Health Protection Agency” and one that was designed to be used in conjunction with plans for SARS of UK health departments and the NHS.60 The 2014 MERS interim plan expressly stated that it was “an internal document” for use by Public Health England and that it was “not intended for use outside of the organisation”.61 There does not appear to have been a separate plan that documents a specific UK-wide strategy for responding to an outbreak of SARS, MERS or any other high consequence infectious disease and that sets out the impacts on the health, social care and public health systems and wider society, or non-pharmaceutical interventions such as mandated quarantining, contact tracing or border controls. |
| 3.31. | The Royal Academy of Engineering recommended to the UK government in September 2021:
“For each risk, a range of scenarios should be generated to explore uncertainty and additional planning requirements, improve the output, and deliver maximum value from the overall process.”62 In their evidence to the Inquiry, a number of scientists agreed. They included Professor Sir Mark Walport (Government Chief Scientific Adviser from April 2013 to September 2017), Professor Sir Patrick Vallance (Government Chief Scientific Adviser from April 2018 to March 2023), Professor John Edmunds (Professor of Infectious Disease Modelling at the London School of Hygiene & Tropical Medicine) and Professor Sir Christopher Whitty (Chief Medical Officer for England from October 2019).63 Each type of disease has its own profile and means of transmission but, as these witnesses made clear, preparedness for and resilience to pandemics should include consideration of transmission through all potential routes of infection.64 |
| 3.32. | Katharine Hammond, Director of the Civil Contingencies Secretariat from August 2016 to August 2020, told the Inquiry that it was not reasonable to anticipate and plan for everything that could happen. The UK’s system was built on using good risk assessment to identify the capabilities and having a means of rapidly adapting these in the face of events.65 Ms Hammond expressed the concern that the use of multiple pandemic scenarios would have been too resource-intensive and the Civil Contingencies Secretariat “did not realistically have the capacity”.66 As a result, there was only very limited multiple scenario planning within the 2016 National Risk Assessment and the 2019 National Security Risk Assessment.67 |
| 3.33. | In addition to impact, the second factor in the assessment of risk is the likelihood of occurrence. However, as the Royal Academy of Engineering recommended to the UK government in 2021:
“[L]ikelihood should not be the main driver for prioritisation as this can be difficult to assess with a high degree of confidence across all risks. Decision-making should be driven by impact and preparedness linked to capability across prevention, mitigation, response, and recovery.”68 The Inquiry agrees. Less weight should be given to likelihood, since there should be planning for unlikely events too. Sir Oliver Letwin MP, Minister for Government Policy from May 2010 to July 2016 and Chancellor of the Duchy of Lancaster from July 2014 to July 2016, considered that a focus on likelihood was a mistake “because events with huge impacts that are very unlikely and may not occur for many years, if they do occur, will nevertheless have huge impacts”.69 Scientific advisers including Professors Walport and Vallance told the Inquiry that focusing on likelihood was an error.70 |
| 3.34. | A number of witnesses and government departments sought to characterise the Covid-19 pandemic as so unlikely that it was a ‘black swan’ event.71 This is an event that is catastrophic but is unprecedented, beyond experience or reasonable contemplation and, therefore, unforeseeable.72 The concept is not universally accepted or without controversy within the field of civil contingencies. For instance, Professor David Alexander and Bruce Mann, expert witnesses on risk management and resilience (see Appendix 1: The background to this module and the Inquiry’s methodology), said that most civil emergency risks are foreseeable in some shape or form.73 Nevertheless, no government can foresee everything. As Sir Oliver Letwin told the Inquiry:
“[N]o amount of resilience-planning or horizon-scanning will be sufficient to ensure that government always responds in an effective way to emergencies as they occur. Fore-knowledge is never complete: surprises occur.”74 |
| 3.35. | In the light of the advice from many experts, it was therefore rational for the UK-wide risk assessments to contain scenarios for both an influenza pandemic and a smaller- scale high consequence infectious disease such as SARS, but this should not have been to the exclusion of other possibilities. The recent experiences of SARS and MERS meant that another coronavirus outbreak at pandemic scale was foreseeable. It was not a black swan event. The absence of such a scenario from the risk assessments was a fundamental error of the Department of Health and Social Care and the Civil Contingencies Secretariat. The UK government and devolved administrations could and should have assessed the risk of a novel pathogen with the potential to reach pandemic scale. |
| 3.36. | The 2022 National Security Risk Assessment has incorporated more generic pandemic and emerging infectious disease scenarios.75 The rectification is welcome but underlines the flaw prior to the Covid-19 pandemic. The improvements appear still to be a work in progress. The UK government will also need to ensure that the selection of multiple scenarios for different risks reflects a representative range of what could go wrong, and that this is not mainly driven by the likelihood of these scenarios. It has not yet explained in clear terms how it proposes to implement the Royal Academy of Engineering’s recommendations more fully to guard against the problems described above.76 |
Flaw 2: Preventing the emergency
| 3.37. | The UK failed to plan to prevent the widespread illness and death envisaged by the reasonable worst-case scenario for pandemic influenza. Mr Hancock said that the National Risk Register:
“explicitly assumed that in the event of a pandemic large numbers of people would fall ill. It did not mention action that might be taken to prevent this from happening.”77 He referred to the assumption that the risk could not be mitigated as a fundamental failure of “doctrine”.78 |
| 3.38. | Jeremy Hunt MP, Secretary of State for Health (and Social Care) from September 2012 to July 2018, agreed.79 Professor Whitty “half” agreed, stating:
“[W]e did not give sufficient thought to what we could do to stop in its tracks a pandemic on the scale of Covid or indeed any other pathogen that could realistically go there.”80 Professor Whitty considered that it was also sensible to have a practical plan for what to do when all else fails.81 Professor Edmunds attributed this failure of doctrine to the fact that the reasonable worst-case scenario for pandemic influenza was a largely unmitigated scenario.82 |
| 3.39. | The 2019 National Security Risk Assessment contained an express caveat for pandemics:
“The reasonable worst case scenario does not take into account the response measures we put in place as the impact of the countermeasures in any given pandemic is difficult to predict as it will depend on the nature of the virus.”83 This was also stated in the 2014 and 2016 National Risk Assessments.84 |
| 3.40. | By contrast, the reasonable worst-case scenario for emerging infectious diseases in the 2019 National Security Risk Assessment did assume that infection control measures by basic contact tracing would control the outbreak.85 The scenario of an emerging infectious disease reaching pandemic scale and requiring a similar system of contact tracing as a first step to controlling the spread was not considered. |
| 3.41. | There were two problems to the approaches to risk assessment. Firstly, the risk assessments did not always explicitly state or explain the mitigation assumed in the risk scenarios.86 Future risk assessments need to explain more clearly and consistently the assumptions that lie behind them. Secondly, the National Security Risk Assessment and its predecessors failed properly to consider prevention and mitigation. As a consequence, the technology, skills, infrastructure and resources that would be needed to mitigate or prevent the emergency were not adequately considered (see Chapter 5: Learning from experience). |
| 3.42. | This was not a new issue. In October 2013, Professor Walport wrote to David Cameron MP, Prime Minister from May 2010 to July 2016, recommending the approval of the 2013 National Risk Assessment and identifying a number of areas in which it could be strengthened, including:
“[A] good risk register should drive thinking about how risks can be prevented, mitigated, handled if they transpire and to clear up afterwards. The [National Risk Assessment] is used fairly effectively for the handling and clear-up, but variably to drive decisions about prevention and mitigation.”87 Professor Walport expressed similar views to Cabinet Office officials in June 2014 and again in October 2014.88 He told the Inquiry that he was “beginning to sound like a broken record” on the issue.89 When asked by the Inquiry whether he considered that the use of the National Risk Assessment in prevention and mitigation had improved during his time in office, he said: “I think it was a work in progress, and I think it’s still a work in progress.”90 |
| 3.43. | The Civil Contingencies Secretariat hosted workshops in 2014 that recommended a “[g]reater focus on ‘what do we want to prevent’” and better understanding of the “scalability of capabilities and resources (to help identify gaps in preparedness)”.91 |
| 3.44. | The Cabinet Office appeared to have acknowledged the need for improvement in this area as part of its work on the National Security Strategy and Strategic Defence and Security Review 2015. It observed, under ‘Prevention’:
“This means focusing risk management onto mitigation where possible, not just preparing for emergencies.”92 |
| 3.45. | In March 2017, the Civil Contingencies Secretariat convened a Risk Assessment Steering Board. Its purpose was to oversee the approach to what became the 2019 National Security Risk Assessment. The minutes of its first meeting recorded:
“The board felt that whilst it was admirable to produce a risk assessment that supported decisions about risk prevention as well as risk preparation and response, this should not reduce the agility of the document.”93 It failed to consider adequately the role of prevention when assessing risk. It was a missed opportunity as it failed to consider, in advance of a civil emergency, its prevention or mitigation. |
Flaw 3: Interconnected risks and the domino effect
| 3.46. | Multiple emergencies may interact with each other to produce a worse aggregate emergency than if they occurred individually. A single emergency may create a domino effect in which, when one thing goes wrong, other things go wrong as well.94 Professor Alexander described these, respectively, as “compound risk” and “cascading risk”.95 The response to an event may also carry risks. This is particularly the case with whole-system civil emergencies, where the government may intervene on a significant scale. To use Professor Walport’s analogy, the cure for a specific emergency can have harmful side effects.96 |
| 3.47. | Events such as pandemics are fundamentally different from other isolated emergencies because they engage the whole system of response. A risk could be the onset of a pandemic (a health risk), which results in a series of interventions by the government to protect the population (with benefits but also costs to vulnerable people), resulting in borrowing to provide emergency financial support (an economic risk), itself resulting in the government being unable to provide healthcare to those who need it during the pandemic and beyond (a further health risk). Equally, failing to address an extremely dangerous pathogen outbreak with sufficient urgency may have catastrophic consequences by causing societal and economic collapse. It is not an easy balance to strike. For such ‘whole-system’ events, the risk of the emergency spiralling, including as a result of the response, is much greater. They ought to be treated in a wholly different category from other risks. The management of these issues in the response to the Covid-19 pandemic is being examined in later modules of this Inquiry. However, it is clear that, in both scenarios, the risk of severe economic damage means that the Treasury has a critical role in the assessment of risk. It also means that the impact on society and those likely to be the worst affected should be considered. Different responses to different civil emergencies will have a range of side effects across society. It should be a fundamental aspect of all risk assessment that the potential impacts on society and the economy are taken into account. |
| 3.48. | The National Risk Assessment and National Security Risk Assessment were essentially focused on single emergencies.97 From 2016 onwards, there were some attempts to stimulate thinking about the risk of the domino effect described above.98 However, as the Royal Academy of Engineering noted, the recognition within the UK government was that comprehensive thinking about interconnected risks was “a key element that is missing from the current methodology”.99 |
| 3.49. | These limitations were highlighted prior to the pandemic. In July 2019, Professor Vallance wrote to Ms Hammond, noting:
“Many risks are interconnected and can act as contributors or enablers of other risks. This in turn can amplify certain risks. This issue is not currently captured sufficiently well in the [National Security Risk Assessment] methodology.”100 In her reply, Ms Hammond agreed that this was something to be explored.101 But by the time the pandemic struck, it was, of course, too late. |
| 3.50. | If countermeasures in the form of non-pharmaceutical interventions are not considered in advance of a pandemic, their potential side effects will not be subject, in advance, to rigorous scrutiny. This weakness has been acknowledged by the UK government, but only since the pandemic. In April 2022, the new UK-wide Pandemic Diseases Capabilities Board noted that the current assessments:
“do not include a full risk assessment for the use of [non-pharmaceutical interventions]. Given that the imposition of lockdown in part accounted for a 25% drop in GDP between February and April 2020, the largest drop on record, and numerous secondary and tertiary impacts on all sectors, this represents a significant gap in the UK’s assessment of pandemic risk.”102 (emphasis in original) The board recommended that further work be carried out to produce a supplementary risk assessment assessing the impacts of the changes in public behaviour that were expected during a pandemic in various sectors.103 It also recommended updating the UK government’s economic risk assessment to include a broader range of impacts, including the significant potential impacts |
| 3.51. | The Inquiry agrees that this was a weakness in the risk assessment process. Responsibility for this is shared across the UK government:
|
| 3.52. | The Royal Academy of Engineering considered that the UK government’s approach to interconnected risks required a different mindset from that for individual risks.108 The same observations apply equally to the devolved administrations. In that light, in September 2021 the Royal Academy of Engineering recommended to the UK government that a collaborative cross-government study was needed to map interconnected risks and capability planning.109 |
| 3.53. | An analysis of how risks are connected may well be both challenging and resource- intensive.110 While the Inquiry recognises that this deficiency in risk assessment is not straightforward to rectify, this does not detract from the importance of doing so. References to this issue in the December 2022 Resilience Framework, and the initiative of a Cabinet Office pilot scheme, are a welcome indication of the UK government’s commitment to meeting this recommendation.111 However, the 2022 National Security Risk Assessment did not appear to include any reference to interconnected risks, and the timeframe for improving capabilities in this area is unclear.112 There is no evidence of progress in the UK government’s December 2023 Resilience Framework Implementation Update.113 |
Flaw 4: Long-term risks and vulnerable people
| 3.54. | Resilience depends on having a resilient population. The existence and persistence of vulnerability in the population is a long-term risk to the UK. Long-term risks are different from acute risks because they gradually affect resilience over time.114 The long-term risks to vulnerable people in society require special attention. As Professor Walport explained, a risk is a combination of the hazard itself, the exposure to the hazard and the vulnerability of people to the hazard.115 The clearest example of a long-term risk that was exposed or aggravated by the pandemic is the underlying health of the UK population prior to 2020. An unhealthy population is at significantly greater risk of experiencing higher rates of serious illness and death as the result of an infectious disease. If levels of poor health are left unchecked over an extensive period of time, the inevitable consequence will be that those who are vulnerable due to poor health will be the hardest hit. |
| 3.55. | When the pandemic struck, many of those who suffered and many of those who died were already vulnerable. The evidence from several voluntary, community and social enterprise organisations was that both the disease and the response to the emergency had a disproportionate impact on vulnerable people.116 Professor Vallance explained:
“[T]here is a terrible, terrible truth, and it’s something that we all need to reflect on, which is that all pandemics feed off inequality and drive inequality. … That is a tragedy that needs to be understood.”117 |
| 3.56. | Yet, as the UK entered the Covid-19 pandemic, there were “[s]ubstantial systematic health inequalities by socio-economic status, ethnicity, area-level deprivation, region, socially excluded minority groups and inclusion health groups”.118 Professors Clare Bambra and Sir Michael Marmot, expert witnesses on health inequalities (see Appendix 1: The background to this module and the Inquiry’s methodology), stated that catastrophic shocks brought about by emergencies such as pandemics expose and amplify pre-existing health inequalities.119 Covid-19 was not an “equal opportunity virus”.120 It resulted in a higher likelihood of sickness and death for people who were most vulnerable in society.121 It was the view of Professors Bambra and Marmot that:
“In short, the UK entered the pandemic with its public services depleted, health improvement stalled, health inequalities increased and health among the poorest people in a state of decline.”122 |
| 3.57. | The 2019 National Security Risk Assessment perpetuated the problem of not adequately accounting for the risk to people who are vulnerable.123 The risk assessment system overseen by the Civil Contingencies Secretariat and the Department of Health and Social Care did not sufficiently take into account factors – beyond age and clinical vulnerability – that might make particular sections of the population especially susceptible to a pathogen outbreak.124 The full scenario assessment for an influenza-type disease pandemic included only a short section on the “impact on vulnerable groups”.125 It was too narrowly drawn and had too limited focus on the impact on public services and staff capacity. |
| 3.58. | The 2020 National Risk Register did make specific reference to vulnerable and at-risk groups. However, its guidance about how these matters ought to be addressed by those involved in preparedness and resilience was too vague to be helpful:
“[W]hen planning for and responding to these risks, planners from national government, local government and community groups all have an important role to play in mitigating the disproportionate impacts on these individuals.”126 |
| 3.59. | Emergency Preparedness (the UK government’s statutory guidance, first published in 2006 and updated most recently in 2012) sets out the generic framework for civil protection under the Civil Contingencies Act 2004 and acknowledges that vulnerable people are “one set of people to whom all emergency plans must have regard”.127 However, it fails to provide a practical understanding of vulnerability for the purposes of preparedness.128 The definition of vulnerability in Emergency Preparedness is “the susceptibility of individuals or a community, services or infrastructure to damage or harm arising from an emergency or other incident”.129 The only recognition of vulnerable people for planning purposes are those with mobility issues, mental health issues, children and pregnant women.130 Similarly, the dedicated, non-statutory guidance – Identifying People Who Are Vulnerable in a Crisis, from 2008 – defines vulnerability as those “that are less able to help themselves in the circumstances of an emergency”.131 |
| 3.60. | On entering the pandemic, most plans did not define groups of vulnerable people, and those that did took a narrow definition of vulnerability based only on clinical conditions.132 Michael Adamson, Chief Executive of the British Red Cross from November 2014, said that, when making assessments of vulnerability, there was too much focus on clinical vulnerability and not enough on wider social and economic factors.133 |
| 3.61. | The definitions of vulnerability in both the statutory and non-statutory guidance produced by the Cabinet Office were too vague to have any utility. The Cabinet Office did not call on the expertise available in its own department, or externally, on how to identify and protect vulnerable people.134 Similarly, although a body of the Department of Health and Social Care that focused on pandemic preparedness (the Pandemic Flu Readiness Board) recognised in February 2018 that there should be a clarification of the meaning in a pandemic of “vulnerable individuals”, this was not sufficiently acted upon.135 UK emergency planning prior to the pandemic did not adequately account for the breadth of vulnerability or the impact of inequality on those likely to be particularly affected by an emergency or the response to it.136 |
| 3.62. | The 2022 National Security Risk Assessment contained a new section entitled “Vulnerable Groups Guidance”.137 It invited those charged with a leadership role on risk, when developing scenarios, to consider the disproportionate impact the risk may have on vulnerable groups. This is a positive development. However, it does not go far enough. It considers only the primary impacts that might result from an emergency. It suggests that government departments should take account of other impacts – for example, the side effects of any given response – but does not set out what those impacts might be or how they could be mitigated (see above in relation to Flaw 3). The social and economic impacts ought to be given significantly more weight. There needs to be a move away from the causes of risks towards minimising their impact, particularly for people who are the most vulnerable.138 |
| 3.63. | One way in which this may be achieved is through local risk assessment. Mark Lloyd, Chief Executive of the Local Government Association from November 2015, told the Inquiry that there ought to be a closer assessment of risk at the local level.139 The Inquiry agrees. This would allow for more effective consideration of vulnerable people in closer proximity to their personal circumstances. It would also reflect the importance of better risk assessment at the level of the devolved administrations to take into account the individual profiles of their populations. If this were done, the assessment of risk would then take better account of the range of vulnerability and how this manifests itself in different ways across the population of the UK. Risk assessment ought to be a collaborative effort, applying to central government but also at the devolved, regional and local levels.140 |
| 3.64. | In addition, the Inquiry considers that there should be a single definition of vulnerability for the UK government and devolved administrations. This should take into account the protected characteristics under the Equality Act 2010 but also be sufficiently broad and capable of adaptation to the circumstances of a major emergency as information about its potential wider impact is gathered. There should be consideration of the effect that both action and inaction may have on those most at risk of harm and suffering. If this approach were taken to all aspects of preparedness and resilience, the risk of suffering and harm – not only from a pandemic but from the response – would be reduced. |
| 3.65. | The UK government indicated in its December 2022 Resilience Framework that it would explore a new process for identifying and assessing long-term risks, including their impact on people who are vulnerable.141 Its 2023 Implementation Update suggests that it has established a new process for identifying and assessing these kinds of longer-term challenges but promises only that: “More detail will be available on this work in 2024.”142 This continues to be a work in progress for the Cabinet Office – almost three years after the Royal Academy of Engineering’s external review. |
Flaw 5: Capabilities and capacity
| 3.66. | It is critical that the assessment of risk is connected to practical capabilities and capacity – namely, what can actually be done in response to an emergency. In this way, risk assessment should be connected to strategy and planning, which have to take account of the reality in terms of preparedness and resilience on the ground. If risk assessment does not take into account what is and is not practically feasible, it is an academic exercise distant from those on whom it will ultimately have an impact. This is what happened in the UK. |
| 3.67. | The Inquiry considers that a better approach to risk assessment would be to work forwards from the risk assessment. Firstly, identify the risk and build the capabilities needed to prevent or respond to it. Secondly, work backwards from the capabilities as they currently exist or are reasonably anticipated to exist, to calculate the risk. For example, if the UK had the ability to test, trace and isolate at scale and a level of flexible capacity in the health and social care system, the impact of a pandemic on the population – and therefore the risk – is likely to be reduced. Similarly, if public finances are sound, governments would have the capacity to provide economic support during a pandemic – this would reduce the risk of a health emergency becoming an economic emergency. |
| 3.68. | The need for decision-making to be “driven by impact and preparedness linked to capability across prevention, mitigation, response, and recovery” was one of the key recommendations made by the Royal Academy of Engineering and was a recurrent theme in their report.143 It is not clear exactly what work is being undertaken to implement this recommendation by the UK government.144 |
Improving the assessment of risk
| 3.69. | In the UK government and devolved administrations, a fundamental and permanent improvement is needed in the assessment of risk, both for pandemics and for other whole-system civil emergencies. The UK government and devolved administrations should perform risk assessments that reflect the circumstances and characteristics particular to England, Wales, Scotland, Northern Ireland and the UK as a whole, such as their demography and geography. |
| 3.70. | These should address all five flaws examined in this chapter, in order that risk assessments:
|
| 3.71. | If the assessment of risk is not undertaken properly, the whole approach to preparedness and resilience begins in the wrong place. As the assessment of risk underpins the entire system of preparedness and resilience – in terms of strategy, structures, advice and the skills, technology and infrastructure that are needed to respond effectively – it should be improved as a matter of urgency. While assessing risk is an area of technical expertise, it should be connected to the real-world capacity and capabilities of the UK, and mindful of the consequences for those particularly impacted by whole-system civil emergencies such as pandemics. The Inquiry is therefore recommending an overall improvement in approach. |
Recommendation 3: A better approach to risk assessment
The UK government and devolved administrations should work together on developing a new approach to risk assessment that moves away from a reliance on single reasonable worst-case scenarios towards an approach that:
- assesses a wider range of scenarios representative of the different risks and the range of each kind of risk;
- considers the prevention and mitigation of an emergency in addition to dealing with its consequences;
- provides a full analysis of the ways in which the combined impacts of different risks may complicate or worsen an emergency;
- assesses long-term risks in addition to short-term risks and considers how they may interact with each other;
- undertakes an assessment of the impact of each risk on vulnerable people; and
- takes into account the capacity and capabilities of the UK.
In doing so, the UK government and devolved administrations should perform risk assessments that reflect the circumstances and characteristics particular to England, Wales, Scotland, Northern Ireland and the UK as a whole.
- The UK Government Resilience Framework, HM Government, December 2022, para 14 (https://www.gov.uk/government/publications/the-uk-government-resilience-framework; INQ000097685)
- See, for example, Denis McMahon 6 July 2023 28/23-29/4
- INQ000181825_0003 paras 11-13; INQ000145912_0012-0030, 0072-0073 paras 6.15-6.18, 6.22-6.24, 6.28, 6.33-6.36, 6.40-6.41,6.43, 6.45-6.46, 6.50-6.52, 6.55-6.58, 6.62-6.63, 6.66-6.68, 6.71-6.72, 6.74-6.75, 6.82-6.86, 9.5-9.6, 9.9
- INQ000181825_0006 para 23
- INQ000183334
- INQ000183334_0011 para 10
- INQ000145912_0005 para 5.1.3
- INQ000145733_0008-0009 para 2.22; INQ000145912_0007-0008 paras 6.3, 6.5
- INQ000147769_0007; INQ000147771_0006; INQ000145912_0007 para 6.3; INQ000182612_0013 para 3.7
- 10 INQ000147769_0007; INQ000147771_0006; INQ000145912_0007 para 6.3; INQ000182612_0013 para 3.7
- INQ000147771_0006; INQ000145912_0007 para 6.3; INQ000182612_0013, 0023 paras 3.9, 3.43
- INQ000145912_0007, 0011-0012, 0073 paras 6.1.1, 6.3, 6.12, 9.9; INQ000182612_0012 paras 3.3, 3.5
- The National Risk Assessment was first produced in 2005, with annual revisions between 2006 and 2014, before the final version in 2016 (see INQ000145912_0014-0019, 0021-0022, 0024-0027, 0072-0073 paras 6.22-6.32, 6.40-6.44, 6.50-6.54, 6.62-6.65, 6.71-6.73, 9.5-9.6, 9.9; INQ000182612_0015-0016, 0019-0021 paras 3.18-3.19, 3.27-3.30, 3.33-3.37; INQ000147769_0007). The National Security Risk Assessment was first produced in 2010, with revisions in 2012 and 2015, before the final version was produced in 2017 (see INQ000182612_0014-0022 paras 3.14-3.17, 3.20-3.26, 3.31-3.32, 3.38-3.42). A new combined National Security Risk Assessment was first produced in 2019, with the current version in 2022 (see INQ000145912_0029-0030 paras 6.82-6.86; INQ000182612_0023-0024 paras 3.43-3.48). The National Risk Register was first produced in 2008, then revised in 2010, 2012, 2013, 2015, 2017 and 2020; the current version is dated 2023 (INQ000145912_0012-0013, 0017-0018, 0019-0021, 0022-0024, 0025-0026, 0028-0029, 0030_0031, 0073 paras 6.15-6.21, 6.33-6.39, 6.45-6.49, 6.55-6.61, 6.66-6.70, 6.74-6.81, 6.87-6.90, 9.9).
- INQ000020678_0003; INQ000185352_0005 para 16; INQ000185343_0003 para 10
- INQ000184894_0021 para 75; INQ000185352_0005 para 16; INQ000102940_0003
- Gillian Russell 28 June 2023 40/17-19
- Gillian Russell 28 June 2023 51/25-60/3; Caroline Lamb 28 June 2023 109/18-110/8
- INQ000130469_0038 para 154; INQ000190662_0025-0026 paras 90-91
- Andrew Goodall 4 July 2023 1/7-7/7
- Mark Drakeford 4 July 2023 170/11-173/21
- INQ000187580_0026, 0032 Recommendation 2
- Andrew Goodall 4 July 2023 3/6-4/3, 6/15-7/7
- Mark Drakeford 4 July 2023 179/3-4
- Reg Kilpatrick 6 July 2023 132/9-13; see also INQ000190662_0025-0026 paras 90-91
- INQ000128968_0006-0008
- INQ000215558
- INQ000130469_0041 para 162
- INQ000128968_0006; INQ000215558; Andrew Goodall 4 July 2023 18/5-19/5
- Andrew Goodall 4 July 2023 19/20-22/5
- Denis McMahon 6 July 2023 63/20-21
- INQ000187620_0044 para 177; INQ000086936; INQ000086937
- INQ000086936_0020-0022 paras 4-10
- INQ000086936_0014, 0022, 0027; INQ000086937_0014
- Denis McMahon 6 July 2023 20/22-21/10
- INQ000187620_0045 para 182; INQ000217257
- INQ000185379_0006, 0024-0025
- Richard Pengelly 11 July 2023 84/14-88/4
- INQ000068403_0006; INQ000145912_0111 para 10.2.2; INQ000182612_0023-0024 para 3.47
- INQ000185338_0004 para 17
- INQ000145912_0117-0121 paras 10.7-10.8; INQ000182612_0023-0024 paras 3.47-3.48; National Risk Register, HM Government, 2023 (https://assets.publishing.service.gov.uk/media/64ca1dfe19f5622669f3c1b1/2023_NATIONAL_RISK_REGISTER_NRR.pdf; INQ000357285)
- INQ000068403_0053 section 7.1
- INQ000147770_0004-0006; INQ000147768_0007-0009; Katharine Hammond 16 June 2023 148/25-149/12
- INQ000068403_0053 section 7.1
- The 2009 Influenza Pandemic: An independent review of the UK response to the 2009 influenza pandemic, Dame Deirdre Hine, July 2010, paras 4.50-4.55, Recommendation 11 (https://assets.publishing.service.gov.uk/media/5a7975f1ed915d0422068a10/the2009influenzapandemic-review.pdf; INQ000022705)
- INQ000147775_0004 footnote 3; INQ000147768_0009; INQ000147770_0005
- INQ000147775_0004; INQ000147768_0008-0009; INQ000147770_0004-0005
- For the 2014 and 2016 National Risk Assessments, risks were excluded if they had less than a 1 in 20,000 chance of occurring at least once in the next five years: INQ000147775_0004 footnote 4; INQ000147768_0008. For the 2019 National Security Risk Assessment, risks were excluded if they had less than a 1 in 100,000 chance of occurring over the next one to two years (INQ000147770_0004).
- INQ000147775_0004 footnote 5; INQ000147768_0008; INQ000147770_0004; see also INQ000182612_0013, 0026 paras 3.7, 3.55
- Referred to as “H23 (DH) … Influenza type disease (pandemic)” in the 2014 National Risk Assessment (INQ000176765_0001), “Pandemic Influenza H23 (DH)” in the 2016 National Risk Assessment (INQ000147769_0047; INQ000176770_0001) and “Influenza-type Disease Pandemic R95-DHSC” in the 2019 National Security Risk Assessment (INQ000147771_0138; INQ000176776_0001).
- Referred to as “H24 (DH) … Emerging infectious diseases” in the 2014 National Risk Assessment (INQ000176766_0001), “Emerging Infectious Diseases H24 (DH)” in the 2016 National Risk Assessment (INQ000147769_0048; INQ000176771_0001) and “Emerging infectious disease … (R97-DHSC) ” in the 2019 National Security Risk Assessment (INQ000147771_0140; INQ000185135_0001).
- INQ000196611_0009 footnote 2; INQ000148429_0059 para 234
- Katharine Hammond 16 June 2023 116/11-14; INQ000145733_0032 paras 5.10-5.11
- Christopher Wormald 19 June 2023 106/1-10, 108/1-109/9
- INQ000176766_0003; INQ000176771_0003; INQ000013824_0003-0004 para 5.1; INQ000148360_0010
- INQ000145912_0029-0030 paras 6.82-6.85
- Christopher Whitty 22 June 2023 93/11-22; Sally Davies 20 June 2023 146/8-18
- INQ000176766_0003; INQ000176771 _0004
- INQ000013824_0004 paras 5.3.2-5.3.3
- INQ000145912_0018, 0020, 0023-0024, 0026, paras 6.39.1, 6.46.5, 6.49.1, 6.61, 6.71.1
- INQ000179082_0003, 0006
- INQ000001332_0004 third para
- INQ000068403_0095 section 11.4
- INQ000147707_0048 para 143, 145; Mark Walport 21 June 2023 35/24-36/21, 56/6-22; INQ000147810_0009 para 26; INQ000148419_0011-0012 paras 5.2-5.3; Christopher Whitty 22 June 2023 100/16-101/5
- See Christopher Whitty 22 June 2023 111/15-19
- INQ000145733_0033 para 5.14
- INQ000145733_0033 para 5.13
- INQ000176770_0009; INQ000176771_0006-0007; INQ000176776_0005-0006; INQ000185135_0004-0007
- INQ000068403_0097 section 11.5
- Oliver Letwin 20 June 2023 20/21-21/15
- Mark Walport 21 June 2023 46/5-24; Patrick Vallance 22 June 2023 158/13-25
- See, eg, submissions on behalf of the Department of Health (Northern Ireland) 13 June 2023 142/3; submissions on behalf of the Government Office for Science 14 June 2023 10/18; submissions on behalf of the Department of Health and Social Care 14 June 2023 20/14-16; Matt Hancock 27 June 2023 30/3-5, 101/9-16
- The concept of a ‘black swan’ event was conceived by Nassim Nicholas Taleb. See: The Black Swan: The Impact of the Highly Improbable, Random House, 2007 (INQ000369660_xvii-xviii).
- David Alexander 15 June 2023 105/23-106/13; Bruce Mann 15 June 2023 108/10-13
- INQ000177810_0004 para 15
- INQ000147772_0121-0123; INQ000145912_0118 paras 10.8.7-10.8.8
- INQ000145912_0118 paras 10.8.7-10.8.10
- INQ000181825_0008 para 30
- INQ000181825_0013 paras 52-54
- Jeremy Hunt 21 June 2023 168/6-14
- Christopher Whitty 22 June 2023 102/3-7
- Christopher Whitty 22 June 2023 102/8-16
- INQ000148419_0012-0013 para 5.5
- INQ000176776_0002
- INQ000176765_0005-0006; INQ000147767_0027; INQ000147769_0047; INQ000176770_0001
- INQ000185135_0002. While there was no express reference to infection control measures in the 2014 and 2016 National Risk Assessments, the similar numbers of fatalities and casualties envisaged by the reasonable worst-case scenarios for emerging infectious diseases provides a strong inference that they adopted a similar approach.
- INQ000068403_0022 section 4.2.1
- INQ000142113_0001
- INQ000142145_0001; INQ000142120_0001
- Mark Walport 21 June 2023 42/8-9
- Mark Walport 21 June 2023 30/25-31/1; see also Mark Walport 21 June 2023 42/13-14
- INQ000186622_0009-0010
- INQ000127915_0006 para 23
- INQ000187355_0004 para 8(d)
- David Alexander 15 June 2023 96/3-97/2; Mark Walport 21 June 2023 33/2-15
- INQ000203349_0016 footnotes 30 and 31. For a technical account of ‘concurrent’, ‘compound’, ‘cascading’ risks and ‘interdependencies’, see: INQ000068403_0023-0024, 0035-0036, 0146-0147 sections 4.2.3, 6.1-6.1.2, Annex G; INQ000203349_0016 paras 20(d), footnotes 30-31.
- INQ000147707_0033 para 86
- INQ000147769_0019; INQ000147768_0010; INQ000147770_0013
- INQ000147769_0019; INQ000147768_0010; INQ000147770_0013
- INQ000068403_0023 section 4.2.3
- INQ000213808_0001
- INQ000213809_0001
- INQ000087205_0004 para 16. The Pandemic Diseases Capabilities Board was a cross-government, UK-wide group established in July 2021 to work on preparedness for a broad range of pandemics, including but not limited to pandemic influenza (INQ000057649_0001 paras 1-2). It replaced the Pandemic Flu Readiness Board.
- INQ000087205_0004-0005 recommendations 2, 2.1
- INQ000087205_0005 para 20
- INQ000145912_0007-0008 paras 6.3, 6.5, 6.6; INQ000182612_0013 paras 3.8-3.9; INQ000203351_0009-0012 paras 33-45
- INQ000184643_0051, 0076 paras 274, 398; INQ000203351_0009-0012 paras 33-45
- INQ000182612_0028-0029 para 3.70
- INQ000068403_0023 section 4.2.3
- INQ000068403_0093 section 11.3
- INQ000068403_0036-0038, 0094 sections 6.2.1, 11.3.2
- The UK Government Resilience Framework, HM Government, December 2022, pp9, 66 (Annex B) (https://www.gov.uk/government/publications/the-uk-government-resilience-framework; INQ000097685); INQ000145912_0118 paras 10.8.5-10.8.6
- The UK Government Resilience Framework, HM Government, December 2022, pp9, 66 (Annex B) (https://www.gov.uk/government/publications/the-uk-government-resilience-framework; INQ000097685); INQ000145912_0118 paras 10.8.5-10.8.6
- The UK Government Resilience Framework: 2023 Implementation Update, Cabinet Office, 4 December 2023, paras 9-10 (https://assets.publishing.service.gov.uk/media/656def711104cf0013fa7498/The_UK_Government_Resilience_Framework_2023_Implementation_Update.pdf; INQ000372824)
- See the discussions of long-term ‘chronic’ risks, short-term ‘acute’ risks and vulnerabilities in INQ000068403_0146-0147 Annex G; INQ000147772_0005, 0010
- Mark Walport 21 June 2023 41/3-6
- These included Age UK (INQ000106031_0009-0011, 0013-0014, 0022 paras 29-35, 41-44, 71-72), the British Medical Association (INQ000205177_0009-0012, 0016 paras 28-29, 34-35, 40-41, 42(f)), Clinically Vulnerable Families (INQ000137308_0002, 0012-0015 paras 5, 18-20), Coram (INQ000108530_0013-0016, 0018, 0019 paras 33-36, 40-42, 44, 50, 53), Disability Rights UK (INQ000185333_0002-0006 paras 6, 8, 10-23), Doctors of the World UK (INQ000148404_0002-0008 paras 7-22, 24), the Federation of Ethnic Minority Healthcare Organisations (INQ000174832_0001-0003, 0004 paras 3, 7-8, 11-12), The Health Foundation (INQ000183420_0008-0009, 0014 paras 24, 42), the Joint Council for the Welfare of Immigrants (INQ000184644_0004-0006, 0010-0013, 0015, 0018 paras 15-21, 38, 41-46, 56, 65), Medact (INQ000148410_0004, 0006-0007 paras 11-12, 18-19, 21), the NHS Confederation (INQ000147815_0017, 0021 paras 61-62, 77), the Runnymede Trust (INQ000195842_0001-0006 paras 1, 3, 6-15), Solace Women’s Aid (INQ000108557_0003, 0006-0009 paras 10-11, 20, 25-29), Southall Black Sisters (INQ000108571_0003-0008, 0011-0013, 0016-0017 paras 11-16, 18-19, 22-23, 32, 36, 43), WinVisible (women with visible and invisible disabilities) (INQ000191132_0003, 0005-0007 paras 6-7, 17, 20, 22-25).
- Patrick Vallance 22 June 2023 165/5-9
- INQ000195843_0029 para 58
- INQ000195843_0074 para 179
- Richard Horton 13 July 2023 74/11
- INQ000195843_0075 para 181
- INQ000195843_0029 para 58
- INQ000147771_0138, 0140
- Christopher Wormald 19 June 2023 151/19-25
- INQ000176776_0004-0005
- National Risk Register, HM Government, 2020, p21 (https://assets.publishing.service.gov.uk/media/6001b2688fa8f55f6978561a/6.6920_CO_CCS_s_National_Risk_Register_2020_11-1-21-FINAL.pdf; INQ000055874)
- Emergency Preparedness, Cabinet Office, Chapter 5, revised October 2011, para 5.98 (https://assets.publishing.service.gov.uk/media/5a789f9140f0b62b22cbb78e/Emergency_Preparedness_chapter5_amends_21112011.pdf; INQ000080807_0039)
- Emergency Preparedness, Cabinet Office, Chapter 5, revised October 2011, para 5.99 (https://assets.publishing.service.gov.uk/media/5a789f9140f0b62b22cbb78e/Emergency_Preparedness_chapter5_amends_21112011.pdf; INQ000080807_0039)
- Emergency Preparedness, Cabinet Office, Glossary, revised March 2012 (https://assets.publishing.service.gov.uk/media/5a75afda40f0b67f59fced2b/EP_Glossary_amends_18042012_0.pdf; INQ000080808_0029); INQ000195843_0004 para 2
- Emergency Preparedness, Cabinet Office, Chapter 5, revised October 2011, para 5.103 (https://assets.publishing.service.gov.uk/media/5a789f9140f0b62b22cbb78e/Emergency_Preparedness_chapter5_amends_21112011.pdf; INQ000080807_0040)
- INQ000097681_0004 para 4; Identifying People Who Are Vulnerable in a Crisis, Civil Contingencies Secretariat, Cabinet Office, February 2008, p4 para 4 (https://assets.publishing.service.gov.uk/media/5a799f0ded915d0422069d24/vulnerable_guidance.pdf; INQ000080825); INQ000195843_0061 para 146.1.3
- INQ000195843_0059 para 145.6.4; INQ000147709_0010 para 38; INQ000137505_0010
- INQ000182613_0013-0014 para 54
- Marcus Bell 13 July 2023 7/20-8/2; Melanie Field 13 July 2023 25/8-26/15
- INQ000022908_0004 para 4.2. The Pandemic Flu Readiness Board was established in 2017, jointly chaired by the Cabinet Office and the Department of Health, to deliver a cross-government and UK-wide programme of work focused on preparedness for pandemic influenza. This is examined further in Chapter 5: Learning from experience. Professor Bambra confirmed to the Inquiry that there was no common definition of vulnerability or those suffering from health inequalities in the 40 documents that she had reviewed, including those that related to the Civil Contingencies Act 2004 and the Pandemic Influenza Bill (2019): Clare Bambra 16 June 2023 46/7-23 (INQ000195843_0061-0063 paras 146-146.4).
- INQ000182613_0013-0014 para 54
- INQ000147807_0102-0103
- Oliver Letwin 20 June 2023 20/2-11
- INQ000177803_0041 para 150
- 1INQ000068403_0093 section 11.3; David Alexander 15 June 2023 147/1-6
- The UK Government Resilience Framework, HM Government, December 2022, paras 14-20 (https://www.gov.uk/government/publications/the-uk-government-resilience-framework; INQ000097685)
- The UK Government Resilience Framework: 2023 Implementation Update, Cabinet Office, December 2023, p14 (https://assets.publishing.service.gov.uk/media/656def711104cf0013fa7498 The_UK_Government_Resilience_Framework_2023_Implementation_Update.pdf; INQ000372824)
- INQ000068403_0009, 0080, 0097-0098
- INQ000145912_0118 paras 10.8.9-10.8.10
Chapter 4: An effective strategy
Introduction
| 4.1. | Strategy builds on risk assessment. While the approach to risk is a technical assessment of what could happen, an effective strategy is a different and separate judgement as to how best to mitigate the risk or its impact. A strategy should enable plans to be made for major issues in conditions of uncertainty. In the case of pandemic preparedness, a strategy should address how best to respond to and recover from a whole-system civil emergency caused by the outbreak of a disease. |
| 4.2. | This chapter examines the effectiveness of the only UK-wide pandemic-scale strategy in place at the time the coronavirus (Covid-19) pandemic struck – the UK Influenza Pandemic Preparedness Strategy 2011 (the 2011 Strategy).¹ It considers what an effective strategy for whole-system civil emergencies such as pandemics should comprise and how it may be improved by data and research. |
| 4.3. | As health is one of the matters devolved to the governments of Scotland, Wales and Northern Ireland, it was open to each devolved nation to take a different approach. Each chose to adopt the 2011 Strategy. In Scotland, for instance, there was no discussion of adapting the 2011 Strategy to make it more Scotland-centric.² The key guidance in both Wales and Northern Ireland had, as its premise, the 2011 Strategy.³ The Inquiry’s assessment of the 2011 Strategy is, therefore, of equal application to the devolved nations individually as it is to the whole of the UK. Pandemic preparedness was considered by all of the governments in the UK to be, at least in principle, a matter that required UK-wide coordination. If there were fundamental flaws, it would – and did – have an effect on the whole system of preparedness in the UK. |
The 2011 Strategy
| 4.4. | The 2011 Strategy was the UK’s emergency response strategy for preparing for and responding to a pandemic. Although it stated that it was a strategy for an influenza pandemic, it was intended to be sufficiently flexible and adaptable for use in the event of other pandemics.⁴ It was published in November 2011 by the Department of Health following the 2010 review by Dame Deirdre Hine into the UK’s response to the 2009 to 2010 H1N1 influenza pandemic (‘swine flu’).⁵ It was not updated prior to the Covid-19 pandemic and remains unchanged since.⁶ |
| 4.5. | Responsibility for the 2011 Strategy prior to the Covid-19 pandemic extended over the tenures of three Secretaries of State of Health (Health and Social Care from January 2018): Andrew Lansley MP (from May 2010 to September 2012), Jeremy Hunt MP (from September 2012 to July 2018) and Matt Hancock MP (from July 2018 to June 2021). |
Strengths of the 2011 Strategy
| 4.6. | The objectives of the 2011 Strategy were to:
|
| 4.7. | These were to be achieved by reference to three key principles:
|
| 4.8. | The 2011 Strategy recognised that preparing for a pandemic was not only about minimising its potential and immediate effect on the health of the population, but also about minimising the potential impact of a pandemic and governments’ responses on society and the economy as a whole. |
| 4.9. | A pandemic is only one of the many challenges and emergencies that a country may face. The government of the day has a responsibility for the short, medium and long-term interests of the UK. There was nothing wrong with the objectives of the 2011 Strategy in themselves. They invited political leaders to balance priorities and consider the trade-offs between competing interests in the event of a pandemic. If differing, sometimes competing, interests were considered prior to the onset of a pandemic, the UK would naturally have a better base for its pandemic strategy and response. These interests would include, for example:
|
| 4.10. | The 2011 Strategy correctly identified that the impact a pandemic would have on the population and wider society would be determined by three factors:
|
| 4.11. | These aspects of the 2011 Strategy are to be commended. However, it was also flawed in a number of important respects. |
Key flaws in the 2011 Strategy
| 4.12. | The major flaws in the 2011 Strategy identified by the Inquiry were:
|
Flaw 1: Failure adequately to consider prevention
| 4.13. | According to the planning assumptions of the 2011 Strategy, the UK was planning for an influenza pandemic in which 50% of the population would have symptoms, of whom 2.5% would die, assuming that no effective treatment was available.¹⁰ Between 1% and 4% of symptomatic patients would require hospital care, depending on the severity of the disease caused by the virus.¹¹ It was accepted that there would likely be increased demand for intensive care services.¹² It was similarly anticipated that health and social care would be placed under “greater strain” – critical care services may be at risk of being “overwhelmed” and there would be “particular challenges” in maintaining social care services.¹³ |
| 4.14. | Applying the assumptions to the UK population in 2020 of approximately 67 million people, this meant in practice that up to 837,500 people would die.¹⁴ The 2011 Strategy stated that, in as little as the first 15 weeks of a pandemic, the aim was to “cope with” 210,000 to 315,000 additional deaths, with perhaps half of these occurring over just three weeks at the height of the outbreak.¹⁵ When it was said that the UK was well prepared before the Covid-19 pandemic, this meant at the time that the UK should have been able to manage the deaths of this number of people – not that it was prepared to prevent them. |
| 4.15. | The strategies that aim to avoid this kind of unmitigated epidemic are being examined further in Module 2 of this Inquiry and may be categorised into mitigation or suppression. While clear definitions of each strategy are not widely agreed, they may be described in the following terms:
|
| 4.16. | Both approaches have limitations, and their effects depend entirely on the characteristics of the pathogen and the availability of effective medicines and vaccines. But the 2011 Strategy failed adequately to consider the steps that could be taken to either mitigate or suppress the outbreak of a novel infectious disease. This flaw had ramifications for the entire system of pandemic preparedness in the UK. |
| 4.17. | The 2011 Strategy had as its premise that it would almost certainly “not be possible to contain or eradicate a new virus in its country of origin or on arrival in the UK”.¹⁶ The expectation was that the virus would inevitably spread and that any local measures taken to disrupt or reduce this spread were likely to have very limited or partial success at a national level. Such measures could not be relied upon as a way to “‘buy time’” .¹⁷ |
| 4.18. | Notwithstanding that, as noted above, he had been Secretary of State for Health and Social Care from July 2018, Mr Hancock made considerable criticism of the 2011 Strategy in his evidence to the Inquiry. He said that it was underpinned by a “flawed doctrine”.¹⁸ As a result:
“instead of a strategy for preventing a pandemic having a disastrous effect, it [was] a strategy for dealing with the disastrous effect of a pandemic”.¹⁹ He also maintained that “the error of the flawed doctrine was significantly bigger than the error of targeting a flu rather than a coronavirus pandemic”.²⁰ |
| 4.19. | The effectiveness of mitigation as an approach was described in the 2011 Strategy under the planning assumptions for pandemic preparedness as “not certain”.²¹ There was no reference at all to a suppression strategy. If a strategy of mitigation or suppression were pursued – as it was during the Covid-19 pandemic – its consequences were not only unknown but not even properly thought about prior to January 2020. The 2011 Strategy did not address adequately how, in the absence of clinical countermeasures such as therapeutics and vaccines, the spread of a disease could be prevented.²² |
| 4.20. | One of the potential answers was ‘non-pharmaceutical interventions’. These ranged from advice to wash hands regularly to, at the most extreme, what are now widely referred to as ‘lockdowns’ (ie legal prohibitions against what otherwise would be lawful activity for the purpose of limiting the spread of the virus). The latter were epitomised in the order announced on 23 March 2020 to ‘stay at home’.²³ While the 2011 Strategy did include recourse to certain interventions (including advice to stay at home, minimise close contacts, and adopt respiratory and hand hygiene practices), it stopped far short of a lockdown or suggesting that restrictions on liberty would be the subject of imposed legal mandates.²⁴ Instead the 2011 Strategy stated:
“[T]he Government will encourage those who are well to carry on with their normal daily lives for as long and as far as that is possible, whilst taking basic precautions to protect themselves from infection and lessen the risk of spreading influenza to others … The presumption is that the Government will rely on voluntary compliance with national advice.”²⁵ |
| 4.21. | Legal coercion was not ruled out entirely in the 2011 Strategy, but there was a strong presumption against it – being reserved only for “a substantial threat” or “extreme circumstances”, or used as a “last resort”.²⁶ Due to the uncertainty of outcome and interference with liberty, emergency powers had to be “limited in their scope to the direct amelioration of the effects of the emergency”.²⁷ Instead, the UK government favoured providing advice to citizens and trusting them to assess the risk and take such precautionary measures as they deemed fit. Mr Hancock confirmed that this was not an accident but a specific and longstanding policy decision affirmed, most recently, in 2017 when Mr Hunt was Secretary of State.²⁸ |
| 4.22. | The Inquiry accepts that the imposition of a lockdown (the features and consequences of which are being addressed in detail in Module 2) should be a measure of last resort. Indeed, there are those who would argue that a lockdown should never be imposed. However, for as long as they remain a possibility, lockdowns should be considered properly in advance of a novel infectious disease outbreak. There should be consideration of the interventions that can and should be deployed to prevent a lockdown but also of the circumstances in which a lockdown may become necessary. There should be adequate planning as to which aspects of legal coercion to protect the public may be used and transparency about what the government intends to do in the event of a health emergency. This is a subject the Inquiry is examining in subsequent modules. |
Flaw 2: Focus only on one type of pandemic
| 4.23. | It is obvious, on the face of the 2011 Strategy, that the UK had devoted its efforts to preparing for an influenza pandemic. Professor Dame Sally Davies, Chief Medical Officer for England from June 2010 to October 2019, could not recall a debate about including non-influenza pandemics in the 2011 Strategy.²⁹ Professor Isabel Oliver, Interim Chief Scientific Officer of the UK Health Security Agency from October 2021, explained that the “only pathogen for which specific pandemic-scale plans were in place was influenza”.³⁰ Emma Reed, Director of Emergency Preparedness and Health Protection in the Department of Health and Social Care from February 2018, stated that the 2011 Strategy was the only pandemic strategy centrally run by the department.³¹ |
| 4.24. | Clara Swinson, Director General for Global and Public Health at the Department of Health and Social Care from 2016, who chaired the Pandemic Influenza Preparedness Programme Board from 2017 to 2022, said that the only UK-wide plan or strategy in place was for pandemic influenza, although other organisations had their own plans.³² This was an error. She also told the Inquiry:
“Where there are unknowns, that’s about research and development, that’s about having flexible resources, it’s about scientific advice, all of those things … it is fair to say, looking back, that we now wish that scope to be wider.”³³ Ms Swinson said that, since the Covid-19 pandemic and in recognition of this flaw, the Department of Health and Social Care was going to focus on “a system that is not based around plans but around core capabilities and resilience”.³⁴ This ought to mean that a core set of skills, technology and infrastructure will be in place ready to be deployed in the event of the next pandemic. It will need to be sufficiently adaptable to respond to influenza but also to a range of pandemics. |
| 4.25. | The 2011 Strategy was thought to be adaptable to deal with other respiratory diseases; this was described as “ready for flu, ready for anything”.³⁵ That might, conceivably, have been true in principle. Professor Mark Woolhouse, Professor of Infectious Disease Epidemiology at the University of Edinburgh, stated:
“Though it is right that we were concerned about influenza (and that threat remains), we should have been prepared for a wider diversity of pandemic threats. The planning assumption that a response appropriate for influenza would also be appropriate for a different respiratory virus did not work out well in practice. In the event, influenza proved an imperfect model for Covid-19.”³⁶ |
| 4.26. | According to the 2011 Strategy, “the plans could be adapted and deployed for scenarios such as an outbreak of another infectious disease, eg Severe Acute Respiratory Syndrome (SARS)”.³⁷ It recognised:
“Influenza pandemics are intrinsically unpredictable. Plans for responding to a future pandemic should therefore be flexible and adaptable for a wide range of scenarios, not just the ‘reasonable worst case’.”³⁸ There should have been sufficient flexibility and adaptability to cope with the pandemic that struck, but there was not. This is evident from the virtual abandonment of the 2011 Strategy in the response to the Covid-19 pandemic, as discussed below. |
| 4.27. | If deeper thought had been given to what being ready for a range of pathogens would mean in practice, the 2011 Strategy would have borrowed from NHS England’s High Consequence Infectious Diseases Programme (discussed further in Chapter 5: Learning from experience).³⁹ It is not apparent to the Inquiry why the strategies for high consequence infectious diseases and pandemics were so different and disconnected from each other. They ought to have been considered together. If they had, then systems that were routine for high consequence infectious diseases (such as test, trace and isolate) would have been scalable and ready to control the spread of a novel virus with pandemic potential. The division between the two categories placed blinkers on the government and those who implemented government policy. There was a chasm between planning for the two scenarios. Despite both concepts being concerned with the potential outbreak and spread of a catastrophic disease, they remained in silos, leaving a major gap in the UK’s strategic plans. |
| 4.28. | According to Sir Christopher Wormald, Permanent Secretary to the Department of Health and Social Care from May 2016, the strategy for a pandemic and the High Consequence Infectious Diseases Programme ran “in parallel”.⁴⁰ However, if the strategy was abandoned as Covid-19 struck, then there was in reality no strategy at all. He said that the Department of Health and Social Care had changed its approach to some of these issues:⁴¹
“My view is we were overreliant on plans, period. Our thinking now is much more in terms of: what are the flexible capabilities that allow you to put together the correct type of response, given the type of disease that happens to be in front of you?”⁴² |
| 4.29. | It is important not to be too prescriptive about the technology, skills, infrastructure and resources that will be required in a future pandemic. Professor Sir Christopher Whitty, Chief Medical Officer for England from October 2019, considered that part of the solution to pandemic preparedness was having “the building blocks of lots of different capabilities”.⁴³ This was echoed by Professor Sir Patrick Vallance, Government Chief Scientific Adviser from April 2018 to March 2023, who told the Inquiry:
“[I]t’s not about trying to end up with highly specific responses in the back pocket all ready for every single eventuality. That’s not possible. But there are generic capabilities which are important across the piece.”⁴⁴ |
| 4.30. | There was a strategic gap between an epidemic or pandemic-scale outbreak of an emerging infectious disease (including one categorised as a high consequence infectious disease) and pandemic influenza. As it happened, Covid-19 fell into this gap, as did the possibilities of border screening, quarantining and contact tracing – each at scale – for a potential pandemic outbreak. A more broadly based and comprehensive strategy, which assessed a range of potential types of pathogen and had a range of measured potential countermeasures, would have been more capable of preventing the spread of a dangerous disease rather than mitigating its effects. The Inquiry did not receive any adequate explanation as to why this obvious gap existed. |
Flaw 3: Failure adequately to consider proportionality of response
| 4.31. | When there is a novel infectious disease outbreak, the government should have a range of potential responses in mind, from doing nothing at one end of the spectrum, to significant restrictions on liberties with the aim of preventing transmission at the other. |
| 4.32. | In the leading recommendation of the 2010 review that led to the strategy, Dame Deirdre Hine recommended:
“Ministers should determine early in a pandemic how they will ensure that the response is proportionate to the perceived level of risk and how this will guide decision-making.”⁴⁵ |
| 4.33. | However, just as the 2011 Strategy did not consider mitigation or suppression, it also did not adequately consider, in advance, the proportionality of potential responses to a pandemic. It set out the approach in the following terms:
“Proportionality: the response to a pandemic should be no more and no less than that necessary in relation to the known risks. Plans therefore need to be in place not only for high impact pandemics, but also for milder scenarios, with the ability to adapt them as new evidence emerges.”⁴⁶ |
| 4.34. | The closest that the 2011 Strategy came to considering proportionality in practice was in a table headed “Proportionate response to pandemic influenza”.⁴⁷ However, this was inadequate for two principal reasons. It did not consider, in depth, the different potential responses to a pandemic, and it considered the potential effects of mild, moderate and high-impact outbreaks in terms that were too vague to be useful. |
| 4.35. | For example, the 2011 Strategy stated that, in the event of a widespread disease in the UK, hospitals would only be able to provide emergency services and advice would be given about how to minimise the risks of transmission.⁴⁸ This was clearly inadequate for such an important strategic document. It told those involved in preparedness, resilience and response what to expect rather than what, in practice, could or should be done and by whom. The people whom this failure was most likely to affect were vulnerable people, because it is they who were disproportionately at risk of being affected both by the emergency itself and by attempts to prevent it.⁴⁹ |
| 4.36. | The 2011 Strategy should have set out a wide variety and range of pathogen outbreak scenarios, ranging from lesser to greater severity and with different impacts across the population. If it had done this, those responsible for pandemic planning could have assessed which policy responses – for instance, advice to the public, mitigation and suppression – were proportionate to the problem, before the arrival of any pandemic. A systematic approach was required to:
|
| 4.37. | If the assessment of proportionality had been at the heart of the 2011 Strategy, it would have been able to set out the considerations and then provide – in advance – a range of policy responses to pandemics with case fatality ratios ranging from, for example, 0.01% to 10% and beyond. The 2011 Strategy – rather than telling the preparedness system to plan for a range of types and severity levels of disease outbreaks, and thus asking government departments to devise policy responses in advance to match this range – instead told the system to be prepared only to manage one outcome for the sick and dying. Any means of assessing the total impact of any given response was completely lacking. |
| 4.38. | It is critical for a strategy to consider a range of scenarios in the context of a whole- system civil emergency, such as a pandemic. In the absence of an effective strategy in which decisions are thought through in advance, the emergency response system lays itself open to the risk of overreacting or underreacting to the emergency, without having a mechanism in place for realising that it is doing so. A coherent strategy must therefore enable a response to the emergency at hand, but also prevent it from escalating out of the government’s control. This was explained by Professor Davies:
“ministers need a balance to the biomedical input … and to look at the health emergency/pandemic from the perspective of the economy and well-being of society”.⁵⁰ |
| 4.39. | A fundamental weakness of the 2011 Strategy was its failure to identify clearly what may and may not be a proportionate response to a range of pandemics with a potential range of impacts on health. |
| 4.40. | In future, the issue of how to assess the proportionality of measures to mitigate or suppress transmission must be specifically considered in a new strategy. This should be done by setting out in the strategy:
|
| 4.41. | The strategy should set out clearly the range of measures that might be utilised, the legal, medical and economic responses that may be required, and the extent to which those capabilities exist or will require scaling up in the event of an emergency, as well as the positive and negative effects of each measure. It would then be a matter for governments, guided by data and appropriate advice, to decide which measures – including those that might be described as a ‘last resort’ – to deploy at which time. Governments should also take into account UK and international experience when considering mitigation and suppression as well as how and in what circumstances such measures should be applied. |
Flaw 4: Lack of an effective economic strategy
| 4.42. | The Treasury is unique among government departments because it is responsible for funding them and also provides the underlying economic security upon which they, and the UK as a whole, rely. It is estimated that the total cost of government spending as a result of Covid-19 will exceed £376 billion.⁵¹ It is likely that the costs of whole-system civil emergencies, such as pandemics, will be borne by the generations that follow – hence the importance of thinking in the long term. It has consequences far beyond the immediate emergency – including for the ability to fund health and social care. |
| 4.43. | George Osborne MP, Chancellor of the Exchequer from May 2010 to July 2016, told the Inquiry that the Treasury only planned for financial or economic emergencies where it was the lead government department.⁵² The Treasury was only involved in the civil emergency preparedness of other departments by the overall management of the economy and by setting budgets and applying spending controls as part of the day-to-day business of government.⁵³ It therefore did not produce an economic strategy specifically for pandemics or the potential responses to a pandemic.⁵⁴ Its economic analysis following previous influenza outbreaks did not form a “plan”, “blueprint” or “playbook” of specific economic responses to a pandemic.⁵⁵ According to Catherine Little, Second Permanent Secretary to the Treasury from October 2022, this was because:
“[D]ifferent health and economic risks demand different policy responses, based upon the nature of the risk and the prevailing context. The uncertain nature of both means that the development of specific and detailed response plans ahead of time for all possible contingencies – in this instance, to the economic and fiscal consequences of a global pandemic – would be impossible given the available resources across the department.”⁵⁶ |
| 4.44. | Mr Osborne stated:
“[T]here was no planning done by the UK Treasury or indeed, as far as I’m aware, any western treasury for asking the entire population to stay at home for months and months on end.”⁵⁷ He said that no one had thought that a policy response up to and including lockdowns was possible until China had commenced one in 2020, and so there was no reason for the Treasury to plan for it.⁵⁸ Mr Osborne told the Inquiry that, if public finances had not been placed on an even keel, the country would not have been able to support itself and the economy as it did by borrowing and spending large sums of money:⁵⁹ “[T]here’s no point having a contingency plan you can’t pay for, and absolutely central to all of this is the ability of your economy and your public finances to flex in a crisis.”⁶⁰ |
| 4.45. | It is certainly the case that economic and financial planning must be flexible enough to adapt to a range of scenarios. However, in the same way that it is essential to be clear in advance about what public health interventions are open to politicians, there must also be plans for economic interventions at both micro and macro levels. The Treasury should have been required to plan specifically for non-economic shocks, in addition to purely economic ones. The Inquiry does not suggest that the Treasury ought to have created a prescriptive plan, as this would have been of limited use, but it could have created one working more closely with experts in the Department of Health and Social Care that identified, in advance, a wide range of pandemic scenarios and, similarly, a range of the major economic policy options that could be deployed in the event of a pandemic of a particular type and severity. |
| 4.46. | While the Inquiry accepts that there will be uncertainty in economic modelling, particularly over the longer term, this alone does not mean that it should not have been done. The Office for Budget Responsibility, established in 2011 as the UK government’s official independent economic and fiscal forecaster, explores in its Fiscal Risks and Sustainability reports events beyond the realm of traditional economic analysis but which could have major economic and fiscal implications.⁶¹ Its Chair, Richard Hughes, stated:
“While it may be difficult to predict when catastrophic risks will materialise, it is possible to anticipate their broad effects if they do. The risk of a global pandemic was at the top of government risk registers for a decade before coronavirus arrived but attracted relatively little (and in hindsight far too little) attention from the economic community.”⁶² (This issue is discussed further in Chapter 3: The assessment of risk.) |
| 4.47. | An economic strategy should be at the heart of planning for the next pandemic. Alongside the Cabinet Office and the Department of Health and Social Care, the Treasury should be at the forefront of scenario planning for the effects on the economy of different types of responses to a wide range of whole-system civil emergencies, including pandemics. This would enable the UK government to consider which economic responses will cause the least harm in the short, medium and long term. Only then will society be able to consider what price it is willing to pay to protect itself from the next crisis. |
Updating the 2011 Strategy
| 4.48. | The 2011 Strategy had not been updated or reviewed since its publication. This meant that, for a period of nearly a decade, a core document relating to one of the principal risks to the UK remained in stasis. Professor Davies said:
“It would have been helpful had we looked at the basic principles afresh e.g. do we let flu pass through the population? The Government should also have reviewed the state of the art of diagnostics and use of data etc, updating practices as required as technology and practice moved on.”⁶³ |
| 4.49. | In November 2018, it was recognised that there was a need to “refresh” the 2011 Strategy.64 In November 2019, it was again recorded that the 2011 Strategy needed a “refresh” within the next six months.⁶⁵ It might have been thought that a ‘refresh’ would have meant that some of the underlying flaws would have been subject to scrutiny. However, as the Inquiry learned, ‘refresh’ was a euphemism for an update that was only minor and limited in scope.⁶⁶ Thus, any change would not have had a material effect on the UK’s pandemic preparedness.⁶⁷ It is unlikely that any such review would have considered the underlying flaws in the 2011 Strategy or its implementation. In any event, the Covid-19 pandemic intervened. |
| 4.50. | The absence of an update to the 2011 Strategy meant, in particular, that it did not incorporate any learning from the international experiences of the Ebola virus disease, Middle East respiratory syndrome (MERS) or SARS outbreaks, and did not take into account lessons from any exercises that took place after 2011 (see Chapter 5: Learning from experience). |
| 4.51. | Mr Hunt said that he did not ever recall being advised that the 2011 Strategy needed to be updated.⁶⁸ Mr Hancock said that he had “no idea” why the 2011 Strategy did not consider the approach taken by countries affected by SARS so that the lessons could have been learned for the UK.⁶⁹ |
| 4.52. | Documents that, in effect, underpin the entire system of preparedness for and resilience to whole-system civil emergencies should be considered completely afresh on a periodic basis. This is no less true for a pandemic strategy. Professor Vallance said that critical documents such as this ought to state an expiry date to ensure that they are still positively “extant”, after which they are subject to a more fundamental review.⁷⁰ The Inquiry agrees. |
| 4.53. | There appears not to have been any formal system, nor any direct ministerial oversight, for ensuring that a document as important as the 2011 Strategy was subject to this sort of review. What is needed is rigorous scrutiny, a critical approach and a systematic reconsideration from first principles in which ministers, experts and officials are prepared to challenge any doctrinal approaches presented to them. |
Abandonment of the 2011 Strategy
| 4.54. | As is being examined in Module 2 of this Inquiry, the 2011 Strategy was never in fact properly tested. When the pandemic struck, the UK government did not adapt the 2011 Strategy. The doctrine that underpinned it (ie to respond to the emergency as opposed to prevent it from happening) was effectively abandoned, as was the 2011 Strategy itself. Mr Hancock explained this was because it was, in his words, “woefully inadequate”.⁷¹ |
| 4.55. | Instead, when faced with the Covid-19 pandemic, the UK government and devolved administrations took a new, untested approach to the emerging crisis. Professor Woolhouse told the Inquiry:
“Lockdown was an ad hoc public health intervention contrived in real time in the face of a fast-moving public health emergency. We had not planned to introduce lockdown … there were no guidelines for when a lockdown should be implemented and no clear expectations as to what it would achieve.”⁷² |
| 4.56. | A new whole-system civil emergency strategy, which addresses pandemics, should ensure that the risk of being in unknown territory during a major crisis is reduced. It will, of course, be impossible to design a strategy for every eventuality, but it should set clear objectives and the capabilities needed to achieve them, and seek to anticipate and provide guidance for a wide range of scenarios so that as much thinking, strategising and planning as possible are done in advance of an emergency. |
| 4.57. | The 2011 Strategy was beset by major flaws, which were there for everyone to see. Instead of taking the risk assessment as a prediction of what could happen and then recommending steps to prevent or limit the impact, it proceeded on the basis that the outcome was inevitable. This sent the wrong signal to the systems of preparedness and resilience across the UK (including in the devolved nations). The Secretaries of State for Health and for Health and Social Care who adhered to the strategy, the experts and officials who advised them to do so, and the governments of the devolved nations that adopted it, all bear responsibility for failing to have these flaws examined and rectified. This includes Mr Hancock, who abandoned the strategy when the pandemic struck, by which time it was too late to have any effect on preparedness and resilience. |
| 4.58. | The UK government might have been assured that the UK was well prepared – for example, by the World Health Organization or the UK’s ranking on the 2019 Global Health Security Index.⁷³ However, if it had been asked ‘prepared for what?’, the only answer would have been ‘prepared to implement the 2011 Strategy’ – with all its underlying flaws and consequences. This would have revealed that the primary aim of the strategy was not to prevent or mitigate the emergency but to manage the casualties and fatalities that would result. |
Developments following the Covid-19 pandemic
| 4.59. | Since the Covid-19 pandemic, the UK government has undertaken a number of reviews to analyse the adequacy of its systems and structures for preparedness for and resilience to civil emergencies. |
| 4.60. | The 2022 UK Government Resilience Framework was said to be a plan to “strengthen the underpinning systems that provide our resilience to all risks”, with a “broad and tangible set of actions”, which was “the first step in our commitment to develop a wide and strategic approach to resilience”.⁷⁴ It was also said to be “just the starting point for the UK Government’s ambitions on resilience”.⁷⁵ However, as the long-awaited culmination of multiple reviews, and nearly 20 years of experience since the Civil Contingencies Act 2004, it lacked concrete commitments necessary to improve preparedness and resilience in the UK. |
| 4.61. | The UK Government Resilience Framework fails on a number of grounds:
The document does not offer a set of sufficiently clear proposals to be implemented with urgency, supported by the necessary resources. |
| 4.62. | The 2018 UK Biological Security Strategy was updated in 2023, in the wake of the Covid-19 pandemic.⁸¹ The 2023 document describes “the four pillars of our response to biological risks” as:
|
| 4.63. | It describes the UK’s response as being based on “three crosscutting enablers [which] run through all four pillars and are drawn out separately”.83 These are:
|
| 4.64. | The principal improvements between the 2018 and 2023 strategies are commitments to:
|
A new whole-system civil emergency strategy
| 4.65. | The revised plans set out in the 2022 UK Government Resilience Framework and the 2023 UK Biological Security Strategy are to be welcomed. For example, the establishment of a lead minister and senior official to oversee implementation and a group of chief scientific advisers to challenge policy are positive steps.⁸⁶ However, they generally fail to articulate problems or solutions clearly and in accurate terms. The 2023 Strategy lacks deadlines by which actions should occur and by which the government’s progress could be measured. The public cannot know if the government has failed if the government itself is unwilling or unable to describe and set objective tests by which its actions can be measured, nor can the officials whose job it is to implement such a strategy. |
| 4.66. | It is important that the thinking about the different ways in which the UK government and devolved administrations may respond effectively to the next pandemic is done as soon as possible – and that it forms an integral part of a new pandemic strategy. Following the Covid-19 pandemic, a vast quantity of data is now available in the UK and from around the world about:
|
| 4.67. | While a strategy should not be prescriptive (because the next pandemic may not be the same or even similar to the last), the general principles to guide political leaders in their decision-making about the trade-offs in applying different aspects of the strategy should be set out as fully as possible. It should, for example, set out the kinds of infrastructure, technology and skills that would be needed and could be adapted, the health protection measures that are available (such as providing advice to the public, social distancing, closing schools and mandatory quarantining), and the likely social and economic consequences in the short, medium and long term of applying them. The Inquiry is examining the efficacy of such measures in detail in subsequent modules. |
Recommendation 4: A UK-wide whole-system civil emergency strategy
The UK government and devolved administrations should together introduce a UK-wide whole-system civil emergency strategy (which includes pandemics) to prevent each emergency and also to reduce, control and mitigate its effects.
As a minimum, the strategy should:
- be adaptable;
- include sections dedicated to each potential whole-system civil emergency – for example, one on pandemics with a clear explanation of the roles and responsibilities of the UK government, devolved administrations and their departments/directorates as well as local responders;
- consider a wide range of potential scenarios for each type of emergency;
- identify the key issues and set out a range of potential responses;
- identify how the strategy is to be applied to ensure that any potential responses are proportionate to the particular circumstances of the emergency;
- include an assessment in the short, medium and long term, based on published modelling, of the potential health, social and economic impacts of the emergency and of potential responses to the emergency on the population and, in particular, on vulnerable people; and
- include an assessment of the infrastructure, technology and skills the UK needs to respond effectively to the emergency and how those needs might change for different scenarios.
The strategy should be subject to a substantive reassessment at least every three years to ensure that it is up to date and effective, incorporating lessons learned between reassessments.
Improving strategy with data and research
Data
| 4.68. | Good-quality data and a broad range of data types are critical for responding to pandemics and other whole-system civil emergencies because the conclusions drawn from data about an emerging crisis will determine which part of the strategy should be pursued, when it should be pursued, and if the course pursued should be changed. Data are essential to guiding a strategy that can be flexible and adaptable as information about the emergency is gathered and analysed. |
| 4.69. | There are limits to what can be done with data in advance of a civil emergency such as a pandemic. Where possible, it should be ensured that there is a reliable feed of live data for decision-makers from the very earliest moments of a crisis – this will enable those decision-makers to have a firmer grip as events unfold. If all that is available are historical data from which to extrapolate about the future, the limitations for designing strategies are obvious. They have been recognised by the Cabinet Office since at least 2014 and, more recently, by the Royal Academy of Engineering in September 2021.⁸⁷ |
| 4.70. | It is crucial when a pandemic starts to emerge to have access to up-to-date, comprehensive data about:
|
| 4.71. | Access to such data requires the UK to have adequate data-gathering systems and capabilities in advance of an emergency. Administrative data (such as the current number of available hospital beds or the number of trains that are able to run) and data generated and analysed by scientific research (such as the effectiveness or otherwise of countermeasures) are both essential. |
| 4.72. | The decisions that were taken early in the Covid-19 pandemic rested on having “fast and reliable data”.⁸⁸ If decision-makers and advisers lack access to such data, they are “essentially driving in the dark”.⁸⁹ The better the data available, the more exact the decisions that can be made. Without good data, evidence-based decision- making becomes much more difficult due to the uncertainties with which decision- makers must grapple. |
| 4.73. | The importance of this was acknowledged before the Covid-19 pandemic. At some time between 2013 and 2018, Professor Sir Mark Walport, Government Chief Scientific Adviser from April 2013 to September 2017, commissioned specific guidance documents on this topic.⁹⁰ They were intended to assist the Government Chief Scientific Adviser and the Scientific Advisory Group for Emergencies (SAGE) to provide scientific advice to COBR (the UK government’s national crisis management centre for responding to whole-system civil emergencies) in the event of an emergency. One of these documents provided guidance about the risk of emerging infectious diseases, outlining a helpful list of open questions that would need to be answered as part of the response, what data would be needed to answer those questions, when these data would be needed and what sources there were for such data.⁹¹ However, by the time of the Covid-19 pandemic, Professor Vallance described there being “a paucity of data”, which meant that the UK government and devolved administrations “were flying more blind than you would wish to”.⁹² |
| 4.74. | Professor Sir Ian Diamond, the UK National Statistician from October 2019, confirmed that “no formal structures existed for the ONS [Office for National Statistics] to directly contribute to civil emergency preparedness and responses outside of ad hoc commissions and requests for support”.⁹³ He suggested that such engagement was effectively non-existent prior to the Covid-19 pandemic.⁹⁴ |
| 4.75. | Furthermore, a more consistent approach needs to be taken to the compatibility of data systems across all four nations of the UK. In the Technical Report on the COVID-19 Pandemic in the UK, the Chief Medical Officers and Chief Scientific Advisers of the four nations underlined the importance of both research and data.⁹⁵ However, they also noted:
“Data systems and health systems differ across the 4 nations, and there was a need to consider the full range of circumstances when designing a shared testing system.”⁹⁶ This means that, despite England, Wales, Scotland and Northern Ireland being at risk of the same health emergency, the data and health systems were so different that they were a barrier to effective preparedness. |
| 4.76. | Professor Whitty described data as “absolutely essential” and largely “a resource and skillset question”.⁹⁷ Data systems have to be in place in advance of the pandemic. They have to be automated and integrated, to provide insights that can be acted upon within the required timeframe.⁹⁸ Any future strategy for whole-system civil emergencies, including for pandemics, will need to be based upon the establishment of “large-scale digital platforms”.⁹⁹ There will need to be, in the case of a pandemic, “a digital platform enabling contact management, rapid epidemiological data reporting” and “surveillance mechanisms” to capture and understand the epidemiology of the pathogen.¹⁰⁰ These will all require public debate and, ultimately, consent.¹⁰¹ It is important that this conversation commences now. |
| 4.77. | There have been positive developments in this area. In October 2021, the Cabinet Office created the National Situation Centre to gather and use data to both monitor risks and respond to whole-system civil emergencies that affect multiple public service areas at the same time.¹⁰² The Office for National Statistics is now connected to the National Situation Centre, placing its data and analysis at the centre of the UK government’s approach to preparedness and response.¹⁰³ Part of the function of the UK Health Protection Committee, created in 2021, is to better ensure that data may be shared across the UK.¹⁰⁴ In 2022, the Joint Data and Analysis Centre was established, bringing together all data and analytics teams located in the Cabinet Office.¹⁰⁵ |
Research
| 4.78. | The problems with data outlined above apply equally to routinely gathered administrative data and to data gathered through scientific research. However, the proper design and use of research methods that can appropriately analyse more complex data and turn the information into useful evidence adds an additional challenge to pandemic preparedness and response. This must be planned for if the application of the strategy is to be evidence based and effective. This is particularly the case in the event of a novel pathogen where the exact characteristics of the disease are not known in advance (‘Disease X’, discussed in Chapter 1: A brief history of epidemics and pandemics). Research provides the evidence necessary to shift from blunt and even disruptive tools (such as using distance and physical barriers to prevent transmission) towards more targeted responses, such as effective vaccines and therapeutics.¹⁰⁶ It can also inform almost any other aspect of pandemic preparedness or response: the accuracy and reliability of a test; the effectiveness of personal protective equipment against disease transmission; the extent of asymptomatic transmission; the public’s behavioural response to the pathogen; and the measurement and mitigation of the adverse effects of non-pharmaceutical interventions. |
| 4.79. | Importantly, during a fast-moving wave of infection, research must begin as soon as possible to ensure that the opportunities to study the pathogen and the interventions used to tackle it are not lost before the wave is over. The ability to conduct high- quality research quickly in response to an emerging pandemic therefore depends on scientists having been able to lay the groundwork for that research well in advance. Without having developed pre-existing frameworks within which scientists can undertake such rapid research, the UK could be deprived of a head start in scientific understanding that could save lives and protect society. Providing the UK with the best chances of securing that head start requires thought and resources. |
| 4.80. | It is clear that more needs to be done in terms of research in advance of future pandemics to ensure that the UK is better prepared. Professor Whitty said that, in response to the Covid-19 pandemic, the UK set up or activated multiple research studies and “put more early emphasis on research than most comparable nations”.¹⁰⁷ One key example was the Office for National Statistics Coronavirus (Covid-19) Infection Survey which, as Professor Vallance noted, “came to be admired around the world as a population level survey that allowed us to understand disease patterns across the UK”.¹⁰⁸ During the Covid-19 pandemic, the survey had to be started from scratch; Professor Vallance said that in the future “it would be very, very important to get those things set up early”.¹⁰⁹ |
| 4.81. | Similarly, more research could have been done to improve the evidence base for different public health measures. Professor Walport noted that establishing an evidence base on which to take more informed decisions about non-pharmaceutical interventions, such as the wearing of masks at a population level, social distancing measures or school closures, is a “much tougher proposition” than other scientific issues relevant to pandemic preparedness.¹¹⁰ Similarly, Professor Vallance observed the limitations in the UK’s available research for non-pharmaceutical interventions, noting that there is:
“difficulty in obtaining good quality data about the effects of non-pharmaceutical interventions. This is an inherently difficult area as there are so many variables, so much ‘noise’, that it is difficult to reliably isolate the effect of any given measure.”¹¹¹ |
| 4.82. | By contrast, Professor John Edmunds, Professor of Infectious Disease Modelling at the London School of Hygiene & Tropical Medicine, considered that “randomised controlled trials should have been conducted to give the highest quality of evidence available”.¹¹² While this was suggested during the Covid-19 pandemic, with a few trials undertaken during and afterwards, he said:
“[I]t is surprising how limited our ambitions were in this regard. This lost opportunity to learn from the pandemic will leave us similarly unprepared for the next one.”¹¹³ |
| 4.83. | The Inquiry acknowledges that improving the evidence base for such public health measures is not straightforward and requires much more thought within the scientific community. However, this demonstrates the importance of laying better groundwork for this in advance of the next pandemic. It will be critical to identify which groups of vulnerable people are likely to be hardest hit by a pandemic and the reasons why. The causes of greater inequality in outcomes, with a focus on health inequality, should be a particular subject of research.¹¹⁴ |
| 4.84. | The Department of Health and Social Care commissions independent research through the National Institute for Health and Care Research, one of the UK’s major funders of health and care research, spending more than £1 billion per year.¹¹⁵ This investment includes pandemic preparedness research, clinical research infrastructure and, importantly, ‘hibernated’ or ‘sleeping’ research projects – flexible draft protocols that are designed in advance, then maintained in a state of readiness so they can be initiated as soon as a new infectious disease outbreak strikes.¹¹⁶ From 2009 to January 2020, only approximately £3.8 million was committed to a total of nine hibernated research contracts for pandemic preparedness.¹¹⁷ That equates to an average of only £380,000 per year. |
| 4.85. | Given the importance of research to pandemic preparedness and the utility of hibernated research projects, the Inquiry considers that there needs to be a more ambitious, widespread and better-funded programme of hibernated research studies linked to a new pandemic preparedness strategy. That programme needs to be part of a change in mindset where the importance of research, as with data, needs to be a central consideration within a new whole-system civil emergency strategy. In this way, the demands of the strategy can identify uncertainties in need of better research, while independent developments in research can better inform the strategy. |
| 4.86. | Professor Jimmy Whitworth and Dr Charlotte Hammer, expert witnesses on infectious disease surveillance (see Appendix 1: The background to this module and the Inquiry’s methodology), advocated for a ‘One Health’ approach to biosecurity, involving research within and between specialist fields of science, resilient health systems, and coordination of global health governance. Emergency preparedness, resilience and response would then be considered together across these areas.¹¹⁸ They also recommended changes in the measures that are needed to improve biosecurity. This would include better leadership of international alert systems, investment in the UK’s ability to rapidly scale up its ability to respond to pandemics, and improvements in the UK’s stockpiling and supply chain resilience. If this were combined, outside of a pandemic, with significant public and private investment in research and development for scalable clinical countermeasures, the UK would be better prepared for a pandemic in the future.¹¹⁹ |
Recommendation 5: Data and research for future pandemics
The UK government, working with the devolved administrations, should establish mechanisms for the timely collection, analysis, secure sharing and use of reliable data for informing emergency responses, in advance of future pandemics. Data systems should be tested in pandemic exercises.
The UK government should also commission a wider range of research projects ready to commence in the event of a future pandemic. These could be ‘hibernated’ studies or existing studies that are designed to be rapidly adapted to a new outbreak. Better working with international partners should be encouraged. This should include projects to:
- understand the prevalence of a new virus;
- measure the effectiveness of a range of different public health measures; and
- identify which groups of vulnerable people are hardest hit by the pandemic and why.
- UK Influenza Pandemic Preparedness Strategy 2011, Department of Health, November 2011 (https://assets.publishing.service.gov.uk/media/5a7c4767e5274a2041cf2ee3/dh_131040.pdf; INQ000102974)
- See Jeane Freeman 28 June 2023 130/19-132/23; Caroline Lamb 28 June 2023 100/14-101/1; Catherine Calderwood 5 July 2023 8/10-15
- Andrew Goodall 4 July 2023 22/11-25/4; Frank Atherton 3 July 2023 22/18-27/10, 28/4-33/8; Michael McBride 10 July 2023 145/2-147/24
- UK Influenza Pandemic Preparedness Strategy 2011, Department of Health, November 2011, para 2.21 (https://assets.publishing.service.gov.uk/media/5a7c4767e5274a2041cf2ee3/dh_131040.pdf; INQ000102974)
- INQ000184643_0059-0060 para 316; INQ000184638_0052-0053 para 6.13; The 2009 Influenza Pandemic: An independent review of the UK response to the 2009 influenza pandemic, Dame Deirdre Hine, July 2010 (https://assets.publishing.service.gov.uk/media/5a7975f1ed915d0422068a10/the2009influenzapandemic-review.pdf; INQ000022705); UK Influenza Pandemic Preparedness Strategy 2011, Department of Health, November 2011, paras 1.7-1.8 (https://assets.publishing.service.gov.uk/ media/5a7c4767e5274a2041cf2ee3/dh_131040.pdf; INQ000102974)
- INQ000184638_0053 para 6.14
- UK Influenza Pandemic Preparedness Strategy 2011, Department of Health, November 2011, para 3.1 (https://assets.publishing.service.gov.uk/media/5a7c4767e5274a2041cf2ee3/dh_131040.pdf; INQ000102974)
- UK Influenza Pandemic Preparedness Strategy 2011, Department of Health, November 2011, para 3.2 (https://assets.publishing.service.gov.uk/media/5a7c4767e5274a2041cf2ee3/dh_131040.pdf; INQ000102974)
- UK Influenza Pandemic Preparedness Strategy 2011, Department of Health, November 2011, para 2.13 (https://assets.publishing.service.gov.uk/media/5a7c4767e5274a2041cf2ee3/dh_131040.pdf; INQ000102974)
- UK Influenza Pandemic Preparedness Strategy 2011, Department of Health, November 2011, paras 2.19-2.20 (https://assets.publishing.service.gov.uk/media/5a7c4767e5274a2041cf2ee3/dh_131040.pdf; INQ000102974)
- UK Influenza Pandemic Preparedness Strategy 2011, Department of Health, November 2011, p16 (https://assets.publishing.service.gov.uk/media/5a7c4767e5274a2041cf2ee3/dh_131040.pdf; INQ000102974)
- UK Influenza Pandemic Preparedness Strategy 2011, Department of Health, November 2011, p16 (https://assets.publishing.service.gov.uk/media/5a7c4767e5274a2041cf2ee3/dh_131040.pdf; INQ000102974)
- UK Influenza Pandemic Preparedness Strategy 2011, Department of Health, November 2011, paras 6.1-6.5 (https://assets.publishing.service.gov.uk/media/5a7c4767e5274a2041cf2ee3/dh_131040.pdf; INQ000102974)
- At the time that the 2019 National Security Risk Assessment was produced – shortly before the Covid-19 pandemic – the reasonable worst-case scenario for an influenza pandemic similarly envisaged a case fatality ratio of 2.5%, resulting in 820,000 fatalities, based on the then UK population numbers: INQ000176776_0001-0002, 0006-0007
- UK Influenza Pandemic Preparedness Strategy 2011, Department of Health, November 2011, p17, first para (https://assets.publishing.service.gov.uk/media/5a7c4767e5274a2041cf2ee3/dh_131040.pdf; INQ000102974)
- UK Influenza Pandemic Preparedness Strategy 2011, Department of Health, November 2011, para 2.12 (https://assets.publishing.service.gov.uk/media/5a7c4767e5274a2041cf2ee3/dh_131040.pdf; INQ000102974)
- UK Influenza Pandemic Preparedness Strategy 2011, Department of Health, November 2011, para 2.12 (https://assets.publishing.service.gov.uk/media/5a7c4767e5274a2041cf2ee3/dh_131040.pdf; INQ000102974)
- INQ000181825_0013-0014 paras 52-56; see also INQ000181825_0008, 0013-0016 paras 30-31, 52-67; Matt Hancock 27 June 2023 30/20-34/2
- INQ000181825_0008 para 31
- Matt Hancock 27 June 2023 79/19-22
- UK Influenza Pandemic Preparedness Strategy 2011, Department of Health, November 2011, p17, first para (https://assets.publishing.service.gov.uk/media/5a7c4767e5274a2041cf2ee3/dh_131040.pdf; INQ000102974)
- UK Influenza Pandemic Preparedness Strategy 2011, Department of Health, November 2011, para 4.26 (https://assets.publishing.service.gov.uk/media/5a7c4767e5274a2041cf2ee3/dh_131040.pdf; INQ000102974)
- Prime Minister’s statement on coronavirus (COVID-19): 23 March 2020, GOV.UK, 23 March 2020 (https://www.gov.uk/government/speeches/pm-address-to-the-nation-on-coronavirus-23-march-2020)
- UK Influenza Pandemic Preparedness Strategy 2011, Department of Health, November 2011, paras 4.10-4.25 (https://assets.publishing.service.gov.uk/media/5a7c4767e5274a2041cf2ee3/dh_131040.pdf; INQ000102974)
- UK Influenza Pandemic Preparedness Strategy 2011, Department of Health, November 2011, paras 7.4, 7.25 (https://assets.publishing.service.gov.uk/media/5a7c4767e5274a2041cf2ee3/dh_131040.pdf; INQ000102974)
- UK Influenza Pandemic Preparedness Strategy 2011, Department of Health, November 2011, paras 7.26-7.29 (https://assets.publishing.service.gov.uk/media/5a7c4767e5274a2041cf2ee3/dh_131040.pdf; INQ000102974)
- UK Influenza Pandemic Preparedness Strategy 2011, Department of Health, November 2011, para 7.30 (https://assets.publishing.service.gov.uk/media/5a7c4767e5274a2041cf2ee3/dh_131040.pdf; INQ000102974)
- Matt Hancock 27 June 2023 72/11-21
- Sally Davies 20 June 2023 154/22-155/16
- INQ000194054_0040 para 157
- Emma Reed 26 June 2023 13/14-17, 14/16-18
- Clara Swinson 19 June 2023 161/17-162/4
- Clara Swinson 19 June 2023 173/10-18; see also INQ000023017_0001
- INQ000182608_0022 para 52
- Christopher Wormald 19 June 2023 106/1-15, 122/1-9, 124/22-125/6, 154/13-17
- INQ000182616_0004 para 13
- UK Influenza Pandemic Preparedness Strategy 2011, Department of Health, November 2011, p15, first para of boxed text (https://assets.publishing.service.gov.uk/media/5a7c4767e5274a2041cf2ee3/dh_131040.pdf; INQ000102974)
- UK Influenza Pandemic Preparedness Strategy 2011, Department of Health, November 2011, para 2.21, fourth bullet point (https://assets.publishing.service.gov.uk/media/5a7c4767e5274a2041cf2ee3/dh_131040.pdf; INQ000102974)
- INQ000184893_0004 paras 8-9. As explained in Chapter 3: The assessment of risk, a high consequence infectious disease is one that typically has a high case fatality ratio, may be difficult to recognise and detect rapidly, can transmit in the community and may not have an effective means of prevention or treatment. It requires an enhanced, specialist response (see INQ000184643_0005-0006, 0010-0012 paras 20d, 41-55; INQ000196611_0009 footnote 2).
- Christopher Wormald 19 June 2023 110/6-15
- Christopher Wormald 19 June 2023 123/8-14
- Christopher Wormald 19 June 2023 125/22-126/1
- Christopher Whitty 22 June 2023 100/6-15
- Patrick Vallance 22 June 2023 160/3-7
- The 2009 Influenza Pandemic: An independent review of the UK response to the 2009 influenza pandemic, Dame Deirdre Hine, July 2010, pp5, 50, Recommendation 1 (https://assets.publishing.service.gov.uk/media/5a7975f1ed915d0422068a10/the2009influenzapandemic-review.pdf; INQ000022705)
- UK Influenza Pandemic Preparedness Strategy 2011, Department of Health, November 2011, para 3.2, second bullet point (https://assets.publishing.service.gov.uk/media/5a7c4767e5274a2041cf2ee3/dh_131040.pdf; INQ000102974)
- UK Influenza Pandemic Preparedness Strategy 2011, Department of Health, November 2011, pp21-25 (https://assets.publishing.service.gov.uk/media/5a7c4767e5274a2041cf2ee3/dh_131040.pdf; INQ000102974)
- UK Influenza Pandemic Preparedness Strategy 2011, Department of Health, November 2011, p25 (https://assets.publishing.service.gov.uk/media/5a7c4767e5274a2041cf2ee3/dh_131040.pdf; INQ000102974)
- INQ000195843_0043, 0075-0076 paras 108, 181
- INQ000184637_0010 para 7.7
- UK Biological Security Strategy, HM Government, June 2023, p14 (https://assets.publishing.service.gov.uk/media/64c0ded51e10bf000e17ceba/UK_Biological_Security_Strategy.pdf; INQ000208910)
- INQ000187308_0009 para 22; see also INQ000099516_0006 para 16
- INQ000187308_0008 para 20; see also George Osborne 20 June 2023 61/6-23
- George Osborne 20 June 2023 65/19-67/25, 75/12, 80/4-8; INQ000099516_0056-0057 paras 242-243
- INQ000099516_0056-0057 paras 242-243
- INQ000099516_0017 para 65
- George Osborne 20 June 2023 65/19-22
- George Osborne 20 June 2023 77/2-78/9
- George Osborne 20 June 2023 71/8-72/1, 92/23-93/9, 96/25-97/3, 117/19-118/7
- George Osborne 20 June 2023 82/17-20
- INQ000130270_0007-0008 para 7; Fiscal Risks and Sustainability, Office for Budget Responsibility, July 2022, pp31-32 (https://obr.uk/docs/dlm_uploads/Fiscal_risks_and_sustainability_2022-1.pdf; INQ000119290)
- INQ000130270_0005 para 6d
- INQ000184637_0013 para 7.22
- INQ000184638_0053 para 6.14
- INQ000023131_0005
- Christopher Whitty 22 June 2023 91/25
- Christopher Whitty 22 June 2023 91/24-93/22
- Jeremy Hunt 21 June 2023 161/4-8
- INQ000181825_0014 para 56
- Patrick Vallance 22 June 2023 136/7-12
- INQ000181825_0014 para 56
- INQ000182616_0003 paras 10-11
- Global Health Security Index: Building Collective Action and Accountability, Nuclear Threat Initiative/Johns Hopkins Bloomberg School of Public Health, 2019, p26 (https://www.nti.org/analysis/articles/global-health-security-index/; INQ000149103); Matt Hancock 27 June 2023 19/17-21
- The UK Government Resilience Framework, HM Government, December 2022, p7 (https://assets.publishing.service.gov.uk/media/63cff056e90e071ba7b41d54/UKG_Resilience_Framework_FINAL_v2.pdf; INQ000097685)
- The UK Government Resilience Framework, HM Government, December 2022, para 5 (https://assets.publishing.service.gov.uk/media/63cff056e90e071ba7b41d54/UKG_Resilience_Framework_FINAL_v2.pdf; INQ000097685)
- The UK Government Resilience Framework, HM Government, December 2022, para 60 (https://assets.publishing.service.gov.uk/media/63cff056e90e071ba7b41d54/UKG_Resilience_Framework_FINAL_v2.pdf; INQ000097685); Roger Hargreaves 22 June 2023 50/14-51/15
- The UK Government Resilience Framework, HM Government, December 2022, p15 (https://assets.publishing.service.gov.uk/media/63cff056e90e071ba7b41d54/UKG_Resilience_Framework_FINAL_v2.pdf; INQ000097685). It was similarly true in the splitting of the Civil Contingencies Secretariat into a COBR Unit and Resilience Directorate (see Roger Hargreaves 22 June 2023 41/24-25, 42/22-44/8; Oliver Dowden 21 June 2023 134/20-137/2).
- The UK Government Resilience Framework, HM Government, December 2022, pp72-74 (https://assets.publishing.service.gov.uk/media/63cff056e90e071ba7b41d54/UKG_Resilience_Framework_FINAL_v2.pdf; INQ000097685)
- Roger Hargreaves 22 June 2023 48/20-49/5
- Roger Hargreaves 22 June 2023 52/11-12
- UK Biological Security Strategy, HM Government, June 2023 (https://assets.publishing.service.gov.uk/media/64c0ded51e10bf000e17ceba/UK_Biological_Security_Strategy.pdf; INQ000208910)
- UK Biological Security Strategy, HM Government, June 2023, p8 (https://assets.publishing.service.gov.uk/media/64c0ded51e10bf000e17ceba/UK_Biological_Security_Strategy.pdf; INQ000208910)
- UK Biological Security Strategy, HM Government, June 2023, p8 (https://assets.publishing.service.gov.uk/media/64c0ded51e10bf000e17ceba/UK_Biological_Security_Strategy.pdf; INQ000208910)
- UK Biological Security Strategy, HM Government, June 2023, pp8-9 (https://assets.publishing.service.gov.uk/media/64c0ded51e10bf000e17ceba/UK_Biological_Security_Strategy.pdf; INQ000208910)
- UK Biological Security Strategy, HM Government, June 2023, p6 (https://assets.publishing.service.gov.uk/media/64c0ded51e10bf000e17ceba/UK_Biological_Security_Strategy.pdf; INQ000208910)
- UK Biological Security Strategy, HM Government, June 2023, pp56-59 (https://assets.publishing.service.gov.uk/media/64c0ded51e10bf000e17ceba/UK_Biological_Security_Strategy.pdf; INQ000208910)
- INQ000186622_0007-0009; INQ000068403_0021-0023, 0074 sections 4.2, 4.2.1, 4.2.2
- Christopher Whitty 22 June 2023 112/9-10
- Christopher Whitty 22 June 2023 112/13
- INQ000147707_0022 para 49
- INQ000142139
- Patrick Vallance 22 June 2023 167/22-24
- INQ000176062_0022 para 111
- INQ000176062_0019-0022 paras 103-110
- INQ000087225, see particularly pp106-168
- INQ000087225_0206 second para
- Christopher Whitty 22 June 2023 114/4-5
- Technical Report on the COVID-19 Pandemic in the UK, Department of Health and Social Care, 1 December 2022, p159 (https://www.gov.uk/government/publications/technical-report-on-the-covid-19-pandemic-in-the-uk; INQ000130955)
- Technical Report on the COVID-19 Pandemic in the UK, Department of Health and Social Care, 1 December 2022, p228 (https://www.gov.uk/government/publications/technical-report-on-the-covid-19-pandemic-in-the-uk; INQ000130955)
- Technical Report on the COVID-19 Pandemic in the UK, Department of Health and Social Care, 1 December 2022, pp39, 229 (https://www.gov.uk/government/publications/technical-report-on-the-covid-19-pandemic-in-the-uk; INQ000130955)
- Christopher Whitty 22 June 2023 113/24-114/19
- INQ000145912_0128 paras 10.26-10.27
- INQ000176062_0034 para 166
- INQ000145912_0109-0110 paras 9.157-9.159
- INQ000145912_0122 para 10.11.10
- Technical Report on the COVID-19 Pandemic in the UK, Department of Health and Social Care, 1 December 2022, fourth para (https://www.gov.uk/government/publications/technical-report-on-the-covid-19-pandemic-in-the-uk; INQ000130955)
- INQ000184639_0026 para 8.10
- INQ000147810_0029 para 90; see also INQ000184639_0026 para 8.11; INQ000183421_0003 para 1.1.4
- Patrick Vallance 22 June 2023 168/12-13
- INQ000147707_0026 para 62
- INQ000147810_0035 para 110
- INQ000148419_0014 para 5.10
- INQ000148419_0014 para 5.10
- INQ000195843_0082-0083 paras 199.2, 199.6
- See INQ000184643_0024-0025, 0051 paras 116-120, 277
- See INQ000184643_0051-0052 paras 277, 284-285; INQ000148418_0006, 0029, 0031, 0033 paras 2.13, 3.15-3.18, 3.22, 3.26(3)
- INQ000184643_0052 paras 284-285
- INQ000196611_0012 para 23. This was supported by, for example, Professor David Heymann, expert witness on epidemiology (see Appendix 1: The background to this module and the Inquiry’s methodology) (INQ000195846_0057 para 268; David Heymann 15 June 2023 65/12-14), Sir Jeremy Farrar, Chief Scientist at the World Health Organization from May 2023, and Director of the Wellcome Trust from 2013 to 2023 (INQ000182610_0024) and Dr Richard Horton, Editor-in-Chief of The Lancet from 1995 (Richard Horton 13 July 2023 78/21-79/3)
- INQ000196611_0012 paras 25-30; see also INQ000195846_0043 para 220
Chapter 5: Learning from experience
Introduction
| 5.1. | Learning from experience underpins proper planning: it should include learning what has worked and what has not worked in the past, recognising gaps in the system and remedying any flaws. Simulation exercises are one way in which such learning can be acquired. They are a valuable tool. |
| 5.2. | The aim of simulation exercises is to approximate, as far as is possible, the circumstances in which events such as a pandemic arise and to test the ability of institutions, structures and systems to respond to the emergency. When executed at scale, they may also provide an opportunity to scrutinise resilience.1 It is by examining the detail of how to respond to a whole-system civil emergency that the system is stress-tested, and gaps and flaws in planning may be discovered. |
| 5.3. | The UK government and devolved administrations have accordingly carried out pandemic preparedness exercises for many years. From such exercises, and from the experience of this country and others in dealing with recent epidemics, the UK should have built up a ‘collective memory’ of what preparedness for a pandemic entails and been well prepared for Covid-19. This chapter explores whether lessons were learned, warnings were heeded, and international practice and experience adequately considered. It also examines how effective the preparedness and resilience system for civil emergencies was at recognising and addressing its own flaws, as revealed by the exercises. Finally, it considers how, in the future, preparedness for and resilience to whole-system civil emergencies may be better stress-tested, more open to public scrutiny and focused on taking action. |
International and domestic experience
| 5.4. | In 2017 and 2018, the World Health Organization produced an annual review of diseases that, in its opinion, needed to be prioritised because of the risks they posed. The aim of the exercise was to identify gaps in research and development. Pathogens that were well known and for which vaccines already existed, such as influenza, were not included. In the 2017 review, Middle East respiratory syndrome coronavirus (MERS-CoV) and severe acute respiratory syndrome coronavirus 1 (SARS-CoV-1) were included on the list of pathogens for which there was an urgent need for research and development.2 The position was the same in 2018 when they were combined into one category of closely related coronaviruses. ‘Disease X’ was also added as a marker to acknowledge that the next pandemic might be caused by a new, previously unknown, highly pathogenic infection.3 |
Lessons from SARS-CoV-1
| 5.5. | Severe acute respiratory syndrome (SARS) caused by SARS-CoV-1 was the first severe emerging infectious disease transmissible from person to person of the 21st century.4 The advance in knowledge of coronaviruses when it emerged caused them to become a topic of major global concern.5 While SARS-CoV-1 caused outbreaks in many countries, the UK was largely spared. There were 368 suspected cases in the UK but only one confirmed infection, with no onward transmission and no deaths.6 |
| 5.6. | The 2002 to 2003 SARS epidemic was the first major test of the UK’s pandemic preparedness this century. Dr Philip Mortimer, former Head of Virology at the Public Health Laboratory Service, wrote in 2003:
“[I]t should not be assumed that a recurrence of SARS is … unlikely, or that a further outbreak would be controllable … If there are weaknesses or deficiencies it should not be thought that they can or should be repaired by quick fixes each time an acute threat materialises. Such expenditures fail to build the infrastructure needed to maintain a comprehensive capacity for rapid and technologically appropriate response to new pathogens.”7 |
| 5.7. | Dr Mortimer advised that the UK required an integrated public health laboratory infrastructure, local laboratory capacity, contact tracers and isolation beds. He cautioned against an excessive reliance on mathematical disease modelling and epidemic intelligence in lieu of what he said was really important – namely, sufficient underlying infrastructure.8 |
| 5.8. | Exercise Shipshape took place on 6 June 2003, following confirmation of the first SARS case in the UK.9 This exercise provided important warnings about the state of preparedness in England and Wales at that time for dealing with outbreaks of high consequence infectious diseases such as SARS. These included observations on the importance of:
|
| 5.9. | Exercise Bennachie, held in December 2004, reached similar conclusions for Scotland, but also included observations on the need to streamline, rationalise and update the large number of communicable disease plans.11 |
| 5.10. | Exercise Goliath, held in December 2003, tested Northern Ireland’s response. It identified the need for more discussion on preventing the initial spread of the virus (as opposed to only dealing with its impact).12 |
| 5.11. | In 2005, a report by the Health Protection Agency formally documented the lessons learned from the SARS epidemic, including the following:
|
| 5.12. | The international experience of the 2002 to 2003 SARS epidemic, and the domestic exercises that followed, revealed a number of important lessons. If these lessons had been heeded, and put into the domestic context, the UK would have been better prepared for the coronavirus (Covid-19) pandemic when it struck in January 2020. |
Lessons from H1N1 (‘swine flu’)
| 5.13. | The next major test of the UK’s pandemic preparedness was the 2009 to 2010 H1N1 influenza pandemic (‘swine flu’). This was, fortunately, a relatively mild illness for most of those affected and many of the stockpiles of vaccines and PPE were not called upon.16 |
| 5.14. | Dame Deirdre Hine’s 2010 review of the UK’s response to the H1N1 influenza pandemic observed that it was “proportionate and effective”, with much good practice upon which to build.17 However, she noted:
“[I]n a more severe pandemic, public health professionals would probably have been overwhelmed more quickly, and resources would have been deployed to treat cases instead of implementing containment measures.”18 |
| 5.15. | Other internal reviews were also conducted by the devolved administrations. A paper produced by the Scottish Government, for example, described Scotland as being “regarded by the rest of the UK as being at the vanguard of the fight against the virus”.19 It stated:
“[H]ad the virus been more severe, or lasted for a longer period, this would have resulted in considerable disruption to the normal function of the NHS.”20 |
| 5.16. | In Wales, a similar observation was made in the 2009 Exercise Taliesin report. The H1N1 influenza pandemic did not fully test Wales’s response plans, because the severity of the pandemic fell significantly below what had been expected.21 |
| 5.17. | To some extent, the H1N1 influenza pandemic lulled the UK government and the devolved administrations into a false sense of security.22 Although the warning signs were present, they were hidden behind the outbreak of a significantly milder pathogen than had been expected. |
Lessons from Ebola
| 5.18. | The 2013 to 2016 outbreak of Ebola virus disease in West Africa was the largest occurrence of the virus since it was first discovered in 1976. By the time it was declared a Public Health Emergency of International Concern by the World Health Organization in August 2014, it had been imported to several countries, including Italy, Spain, the UK and the USA.23 |
| 5.19. | The measures taken in the UK in response to the Ebola outbreak included symptom screening at ports of entry, contact tracing for positive cases and setting up the High Consequence Infectious Diseases Programme which included surveillance.24 A UK Vaccine Network was also established.25 Public Health England provided port-of-entry screening to travellers arriving from high-risk countries. Screening teams were focused on London’s Heathrow and Gatwick airports and Birmingham and Manchester airports, where more than 97% of relevant passengers entered the UK, including all identified higher-risk workers.26 There were only three Ebola cases in the UK, with no onward spread.27 |
| 5.20. | A joint report by the Department of Health, NHS England and Public Health England in July 2013, Learning Lessons from the Ebola Response, recommended a review of legal powers to allow for a more systematic approach to port and border controls.28 It concluded:
“There are currently different disease management controls and powers that are not systematic in approach at different types of ports of entry, or for different disease groups. There is an opportunity to review and align all relevant powers to allow logical stepped interventions from port through to community. As far as possible, operational demands should be addressed alongside policy and legal issues, although this will not always be straightforward.”29 |
| 5.21. | Ahead of a meeting of the G7 heads of government in 2015, David Cameron MP, Prime Minister from May 2010 to July 2016, said:
“The recent Ebola outbreak was a shocking reminder of the threat we all face from a disease outbreak … But the reality is that we will face an outbreak like Ebola again and that virus could be more aggressive and more difficult to contain. It is time to wake up to that threat.”30 |
| 5.22. | In March 2015, an Ebola Preparedness Surge Capacity Exercise was conducted in England. Its purpose was to stress-test the surge capacity and resilience of hospitals and health agencies by considering arrangements at the four designated NHS surge centres in England to respond to a novel high consequence infectious disease (multiple positive cases of Ebola).31 Although the centres were confident that they could absorb the impact of having one Ebola patient, serious issues were raised about the challenges of treating multiple patients at the same time.32 |
| 5.23. | Shortly after the exercise, the High Consequence Infectious Diseases Programme was created. Its objective was to develop an agreed method for managing suspected and confirmed high consequence infectious diseases and to put in place additional specialist facilities where patients with highly infectious or transmissible diseases could be treated.33 Dr Michael Prentice, on behalf of NHS England, told the Inquiry:
“The primary reason for establishing the Programme was the continuing threat of ‘airborne’ diseases such as MERS, SARS and Avian influenza.”34 However, the programme was only intended to deal with “small numbers” of patients.35 Four new Airborne HCID Treatment Centres (for the complete containment of any airborne high consequence infectious diseases (or HCIDs)) were commissioned across England, with each centre routinely providing two beds |
| 5.24. | The UK’s response to Ebola and the development of the High Consequence Infectious Diseases Programme were notable successes in the UK’s preparedness for a small outbreak of a high consequence infectious disease. However, the UK government, devolved administrations and public health agencies did not consider adequately whether the UK was prepared to deal with an epidemic or pandemic- scale outbreak of an emerging infectious disease (including one categorised as a high consequence infectious disease). |
Lessons from MERS
| 5.25. | MERS is a highly deadly high consequence infectious disease caused by the coronavirus MERS-CoV.38 In February 2016, Exercise Alice was conducted in London to explore the challenges that a large-scale outbreak of MERS could present in England.39 It was not intended to test preparedness for a whole-system civil emergency at the scale of a pandemic, but rather to assess the UK’s readiness for a “large-scale” outbreak of MERS.40 The simulated scenario commenced with three ‘patients’ being admitted to hospital with symptoms of infection. It developed into 50 laboratory ‘confirmed’ cases of MERS with possible contacts totalling 650.41 |
| 5.26. | It was plain from the exercise that, at the earliest stages of such an outbreak, suitably trained professionals, with access to PPE in sufficient quantities, sufficient bed capacity and specialised clinical equipment, were key.42 It was observed that, while what had been learned from Ebola had improved infection control, this was still not embedded within the system.43 |
| 5.27. | The participants in the exercise (including representatives from NHS England, Public Health England, the Department of Health and observers from the devolved administrations of Wales and Scotland) asked about the management of the 2015 outbreak of MERS in South Korea.44 Three aspects of the South Korean experience were important: the quarantining of about 17,000 people, the evidence about subsequent transmission and the importance of border security in the form of temperature screening.45 |
| 5.28. | There was a significant level of discussion about restricting the movement of symptomatic, exposed and asymptomatic patients. There was debate as to whether this isolation ought to be voluntary (self-isolation) or enforced (quarantine). One of the options discussed was, following the South Korean model, the use of hotels for isolation. Another was the use of designated sites with respiratory immunisation and diagnosis units to house people. There were also discussions about the legal right to restrict movement. It was suggested that a pragmatic solution would be to advise and request people to self-isolate at home under active health surveillance, provide them with information and offer daily contact with specialists in health protection.46 |
| 5.29. | The exercise set out 12 actions. These included:
|
| 5.30. | As the commissioning organisation, the Department of Health and Social Care was responsible for allocating actions arising from Exercise Alice and “embedding learning”.50 The actions were, however, left unallocated.51 |
| 5.31. | Sir Christopher Wormald, Permanent Secretary to the Department of Health and Social Care from May 2016, when asked by the Inquiry whether or not any of the actions arising out of Exercise Alice had been pursued by the department, said that some “were partially, but you are correct that not all of them were completely”.52 The recommendations that were not completed included producing the briefing paper on the South Korean experience and planning for quarantine as opposed to self-isolation.53 |
| 5.32. | In a ‘lessons learned’ report in September 2020, the Department of Health and Social Care recognised that it:
“would have benefitted from a fuller understanding of the response by Asian countries … earlier in our planning, which might have enabled us to start to build testing systems earlier”.54 A number of witnesses agreed that it would have been helpful to have considered the response in East Asia to SARS and MERS prior to the arrival in the UK of Covid-19.55 |
| 5.33. | In South Korea, the response to MERS included the development of excess bed capacity for hospitalisation and isolation, rooms with renal dialysis and ventilation capacity, and a sophisticated network of public and private laboratories to enable the rapid scale-up of testing. In January 2020, South Korea was able to detect cases of Covid-19 and a response was quickly put in place, leading to rapid identification and isolation of potentially contagious carriers.56 |
| 5.34. | Following its experience of SARS, Taiwan was similarly able rapidly to scale up testing to identify, within a few days, those who may have been exposed to Covid-19; they were required to quarantine. Early identification of the source of infections, combined with early restrictions on international travel, effectively limited the spread of Covid-19.57 |
| 5.35. | One of the most striking differences between the approaches in the UK and East Asia was that, in the latter, they believed that, with the right infrastructure, the spread of a virus could be halted. This would be using what Professor David Heymann, expert witness on epidemiology (see Appendix 1: The background to this module and the Inquiry’s methodology), described as “good basic epidemiology and outbreak control”.58 The Inquiry was told that there may be lessons to be learned from the experiences of South Korea and Taiwan and that, by a combination of early border restrictions, localised lockdowns, strict testing, contact tracing and quarantining, the spread of a coronavirus such as Covid-19 could be contained before a vaccine was found.59 |
| 5.36. | The failure to examine such measures thoroughly in advance of the Covid-19 pandemic meant that the UK was exposed to the risk of having to create policy during the emergency rather than before the emergency. |
Stress-testing the UK’s pandemic preparedness systems
Figure 9: A timeline of key exercises undertaken between 2003 and 2018
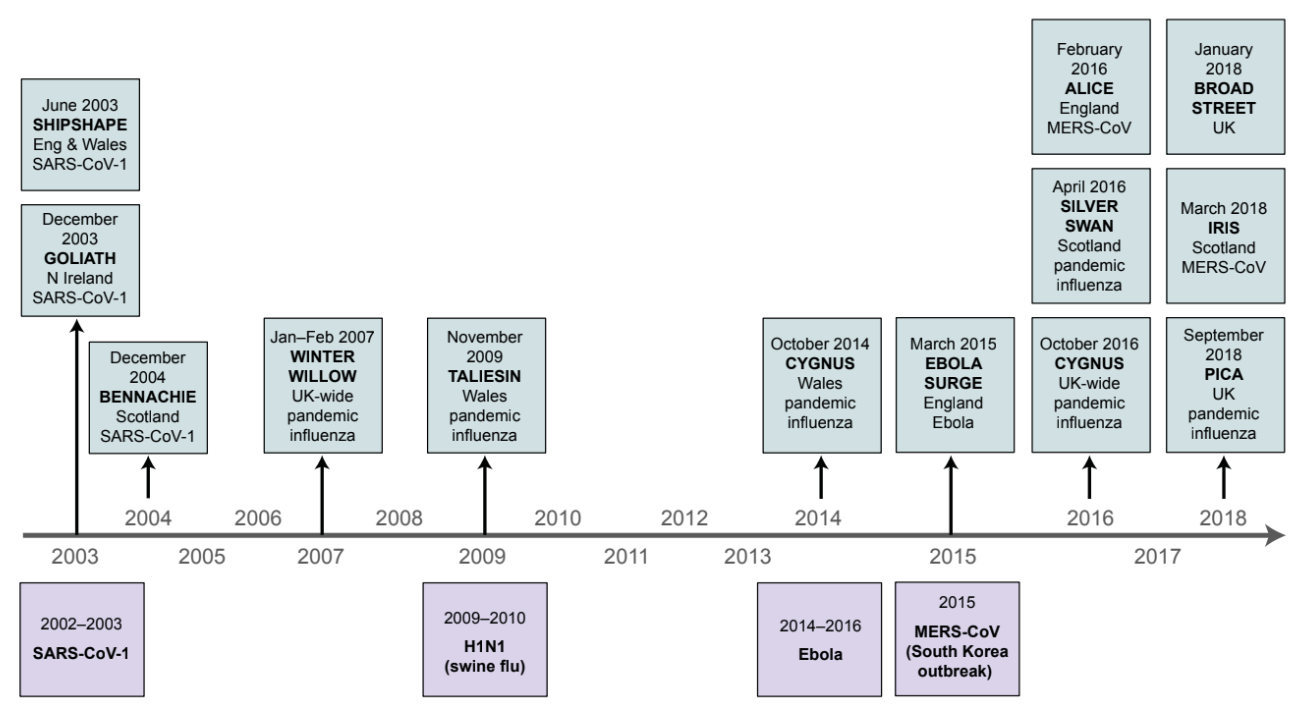
| 5.37. | In addition to the exercises and reports set out above in the context of outbreaks of particular viruses, further exercises were conducted in the four nations of the UK.60 Although there was some variation in the subjects and precise scope of each exercise, there was significant overlap in the issues that were identified. |
Exercise Cygnus
| 5.38. | Exercise Cygnus was a major, three-day, cross-government exercise which took place in October 2016. It warrants particular attention because its findings and recommendations were stark reminders of the state of the UK’s preparedness for and resilience to a pandemic in the three years leading up to the Covid-19 pandemic. |
| 5.39. | It was based on four simulated meetings of COBR (the UK government’s national crisis management centre for responding to whole-system civil emergencies) and was designed to assess the UK’s preparedness and response to a pandemic influenza outbreak. The exercise was set in the seventh week of a pandemic affecting up to 50% of the UK’s population and causing 200,000 to 400,000 excess deaths. More than 950 representatives from the devolved nations, the Department of Health and 12 other government departments, NHS Wales, NHS England, Public Health England, eight local resilience forums (multi-agency partnerships made up of representatives from local public services) and six prisons took part in the exercise.61 |
| 5.40. | There were 4 key ‘learning outcomes’ and 22 detailed lessons from the exercise, including:
|
| 5.41. | One of Exercise Cygnus’s key learning outcomes was:
“[T]he UK’s preparedness and response, in terms of its plans, policies and capability, is currently not sufficient to cope with the extreme demands of a severe pandemic that will have a nation-wide impact across all sectors.”68 |
| 5.42. | In February 2017, following Exercise Cygnus, Theresa May MP (Prime Minister from July 2016 to July 2019) noted at a meeting of the National Security Council (Threats, Hazards, Resilience and Contingencies) sub-Committee that pandemic influenza was the greatest risk faced by the UK.69 |
| 5.43. | A number of important matters were raised at this meeting. It was agreed that:
However, no reference was made at this meeting to the fundamental conclusion of Exercise Cygnus – that the UK’s pandemic plans, policies and response capabilities were not sufficient to cope with the extreme demands of a severe pandemic.73 There was also a fundamental flaw in Exercise Cygnus itself: it did not consider anything wider than pandemic influenza and the scenario presented.74 |
The Pandemic Flu Readiness Board
| 5.44. | In response to Exercise Cygnus, in March 2017 a Pandemic Flu Readiness Board was established at the request of the Threats, Hazards, Resilience and Contingencies sub-Committee.75 It was co-chaired by officials from the Cabinet Office and the Department of Health.76 The board reported to the Threats, Hazards, Resilience and Contingencies sub-Committee via the Secretary of State for Health and the Minister for the Cabinet Office.77 |
| 5.45. | The board’s outline work plan, dated April 2017, included:
|
| 5.46. | The work plan did not include three key issues identified during the February 2017 Threats, Hazards, Resilience and Contingencies sub-Committee meeting. These were consideration of the restriction of movement of non-essential workers, different scenarios in pandemic planning that looked at the potential characteristics of pandemics, and other more radical measures to control transmission (as discussed above).79 These were important omissions by the Cabinet Office and the Department of Health. |
| 5.47. | In August 2017, Katharine Hammond, Director of the Civil Contingencies Secretariat from August 2016 to August 2020, wrote to Mark Sedwill, National Security Adviser from 2017 to 2020. She stated:
“The current key risk to delivery is the notable resource pressures within the [Department of Health] … there remains a lack of resource committed to the programme.”80 |
| 5.48. | In April 2018, Jeremy Hunt MP (Secretary of State for Health and Social Care from September 2012 to July 2018) and David Lidington MP (Minister for the Cabinet Office and Chancellor of the Duchy of Lancaster from January 2018 to July 2019) wrote to members of the Threats, Hazards, Resilience and Contingencies sub- Committee to provide an update on the work of the Pandemic Flu Readiness Board. They stated that “[a] lot has been achieved, but there is more to do to both maintain and enhance preparedness to an acceptable level”.81 They set out the proposed actions for the next 12 months and committed to providing a “further update on progress … in early 2019”.82 This was a delay of one year from the initial deadline of “early 2018”, which had been set for “completion of all deliverables”.83 |
| 5.49. | Matt Hancock MP, Secretary of State for Health and Social Care from July 2018 to June 2021, told the Inquiry that he was informed about Exercise Cygnus and the role of the Pandemic Flu Readiness Board. He said:
“I found that reassuring. I’d been reassured that essentially everything was in hand because there was a structure, a resourced structure to make it happen.”84 |
| 5.50. | However, following the February 2017 meeting of the Threats, Hazards, Resilience and Contingencies sub-Committee referred to above, it did not meet again. Similarly, the Pandemic Flu Readiness Board did not meet for a year between November 2018 and November 2019. Following the year-long hiatus, it was recognised that there was a need to “re-invigorate the Board” and to “prioritize and re-energize work streams and the [Board]”.85 The UK government’s priority did not ever move back to pandemic preparedness. The Pandemic Flu Readiness Board did not meet again until 23 January 2020.86 |
Limitations of the exercises
| 5.51. | The value of the exercises was undermined by their limitations. |
| 5.52. | Firstly, there were no exercises, in any of the four nations, that tested an epidemic or pandemic-scale outbreak of an emerging infectious disease (including one categorised as a high consequence infectious disease). This meant that, prior to the Covid-19 pandemic, there was no exercising of measures such as mass testing, mass contact tracing, mandated social distancing or lockdowns. |
| 5.53. | Secondly, Exercise Cygnus did not provide an opportunity for the participants to test their ability to stop or suppress transmission of the virus during the initial response to an influenza pandemic. |
| 5.54. | Thirdly, ‘what if’ questions were rarely, if ever, asked and answered. For example, no one in the Department of Health and Social Care or Public Health England looked at Exercise Alice on high consequence infectious diseases and Exercise Cygnus on pandemic influenza and asked how the UK might slow or halt the transmission of a novel and significant disease that could cause a pandemic.87 |
| 5.55. | Fourthly, the role of local authorities, local responders, and the voluntary, community and social enterprise sectors in the exercises was not adequately considered. They are absolutely essential to pandemic planning – and yet, the exercises examined by the Inquiry did not adequately involve those who operate on the ground. To give one example, Mark Lloyd, Chief Executive of the Local Government Association from November 2015, said that only 8 out of 42 local resilience forums took part in Exercise Cygnus.88 |
| 5.56. | Fifthly, there was a lack of openness about the outcome of the exercises. The Local Government Association was not sighted on the conclusions of Exercise Cygnus. Although the Exercise Cygnus report included all local resilience forums on its distribution list and it was to be published on ResilienceDirect, the Local Government Association only obtained disclosure of the report as a result of legal proceedings brought by another body in 2020.89 It was not aware of Exercise Alice until the autumn of 2022, when its existence became known through the work of this Inquiry.90 There was no local government involvement in Exercise Alice, nor were its report or recommendations shared.91 Mr Lloyd told the Inquiry that, had the Local Government Association known about issues such as the potential importance of quarantining in planning, it “would have changed what we were doing in our local planning”.92 Many others with an acute interest in the outcome of Exercise Cygnus, including the Royal College of Nursing and private care home providers, were unable to learn from it or contribute to the discussion about how the systems of preparedness could be improved.93 Reports should have been shared between governments and key organisations, as well as with the public. |
| 5.57. | Sixthly, although previous pandemics had exposed and exacerbated health inequalities, exercises did not routinely address this issue.94 The Inquiry asked Professor Clare Bambra and Professor Sir Michael Marmot, expert witnesses on health inequalities (see Appendix 1: The background to this module and the Inquiry’s methodology), to consider the material relating to a sample of 12 exercises. They did not find any mention of the particular needs of vulnerable people.95 Professor Isabel Oliver, Interim Chief Scientific Officer at the UK Health Security Agency from October 2021, informed the Inquiry that, prior to the Covid-19 pandemic, the potential effect of health inequalities had not been routinely included in exercises as a specific exercise objective.96 |
| 5.58. | Despite the significant number of exercises held and reports produced on pandemic preparedness by the UK government, devolved administrations and public health agencies, the lessons that were learned from them were not sufficiently shared and debated. In many cases, learning and recommendations, while nominally recorded in documentation, were simply not acted upon or were forgotten. The introduction in October 2022 by the Cabinet Office to the UK Resilience Lessons Digest to help resolve some of these issues is a positive development but there is more to be done.97 |
| 5.59. | The approach to exercises had been allowed to become bureaucratic and ineffective. The UK government and devolved administrations were overly focused on conducting exercises and producing reports, rather than on learning the lessons and implementing their recommendations. Reports did not result in a material improvement of preparedness, nor did they assist in holding the relevant agencies and political leaders to account. They became an end in themselves rather than a means of learning lessons for the future. As Dr Claas Kirchhelle, expert witness on public health structures (see Appendix 1: The background to this module and the Inquiry’s methodology), stated:
“One of the most worrying insights … is how well-known structural weaknesses of UK pandemic response capabilities were by the time of the COVID-19 pandemic … warnings were not acted on as a result of selective official memory capture.”98 |
| 5.60. | The whole system of pandemic preparedness and resilience should also have been subject to more rigorous, more regular and collective stress-testing, in order to ensure that it would be effective in the event of an emergency. Sir Oliver Letwin MP, Minister for Government Policy from May 2010 to July 2016 and Chancellor of the Duchy of Lancaster from July 2014 to July 2016, suggested that the UK should put more effort than it has yet done into repeatedly performing large-scale exercises to test its resilience to various forms of whole-system civil emergencies, including pandemics.99 The Inquiry welcomes the commitment of the Cabinet Office to re-establish the National Exercising Programme.100 |
Key lessons identified
| 5.61. | The exercises undertaken across the UK and other information available to the UK government and devolved administrations highlighted a number of actions that could and should have been taken to prepare for an epidemic or pandemic-scale outbreak of an emerging infectious disease (including one categorised as a high consequence infectious disease). These essentially consisted of the building of epidemiologically sound and effective infection control measures, including:
|
Testing and contact tracing
| 5.62. | Following the 2013 to 2016 Ebola outbreak in West Africa, a contact tracing system was set up so that, in the event of a positive case of Ebola, hospital clinicians would inform the local health protection team, which would then follow up on all contacts.101 However, this was only on a small scale. |
| 5.63. | As far as testing capacity was concerned, the likely impact of limited laboratory capacity on diagnosis and data during a pandemic was recognised at a meeting of the Department of Health’s Scientific Pandemic Influenza Group on Modelling (referred to as SPI-M) in January 2017. Public Health England acknowledged that there may be laboratory capacity issues in the future, depending on the nature of any outbreak. It also said that it was confident everything that could be done to mitigate these issues had been done. It was unlikely to go to the private sector to boost capacity, but did not rule it out as an option.102 |
| 5.64. | Duncan Selbie, Chief Executive of Public Health England from July 2012 to August 2020, told the Inquiry that no steps had been taken prior to the Covid-19 pandemic to ‘surge’ laboratory capacity.103 Mr Hancock told the Inquiry:
“On testing, [Public Health England] refused to engage private sector testing capacity, despite it being obvious that a massive expansion of testing was necessary, and that the existing capacity was not scalable.”104 |
| 5.65. | It was, according to Mr Selbie, Public Health England’s responsibility to know only what was coming through the surveillance systems, to develop the necessary test (adapted, if necessary) and then to send that to laboratories, principally within the NHS. He said that, with high consequence infectious diseases, the numbers were in the few hundreds (what Public Health England called ‘large scale’). It was never, however, the plan for Public Health England to be carrying out mass testing or mass contact tracing. His understanding was that Public Health England would not be testing 50% of the population, but testing only for surveillance and research purposes.105 |
| 5.66. | There was, similarly, no scalable test and contact tracing system prior to the pandemic in Scotland, Wales and Northern Ireland.106 |
| 5.67. | The entirety of the UK’s testing and contact tracing system was therefore designed to deal only with small numbers of cases of emerging infectious diseases, as opposed to mass testing or contact tracing. During the Covid-19 pandemic, the capacity to scale up testing and tracing had to be rapidly built from scratch.107 |
| 5.68. | The UK government and devolved administrations could and should have invested in this infrastructure in advance of the Covid-19 pandemic, but had not done so.108 While policy decisions on the allocation of resources are ultimately a matter for elected politicians, and such investment would have been significant, the Inquiry believes it would plainly have been worthwhile, given the devastation wrought by the initial absence of effective infection control and the massive cost to the nation of building test and trace systems from scratch. The building blocks and essential structure of the test and trace systems established by the UK government and devolved administrations during the pandemic should be maintained so that these systems can be rapidly restored and adapted for use in the event of a future outbreak. |
Isolation
| 5.69. | Work on quarantining was discussed at a meeting of the Department of Health’s Departmental Board on 29 September 2016. It was recognised during the meeting that “there would be significant issues if it became necessary to track or quarantine thousands of people”.109 The workstream set up to investigate methods of quarantining in East Asia had been put on hold as part of a departmental “workload prioritisation exercise” by the Department of Health.110 |
| 5.70. | Sir Christopher Wormald accepted that, by 2020, there had not been any debate about quarantining or isolating significant numbers of the population in the context of a pandemic.111 The workstream had remained on hold. He said:
“So there has been a lot of discussion, rightly, of some of the countries that handled Covid extremely well, such as South Korea. Effectively what they had was a much higher threshold of containment for [high consequence infectious disease] than we were able to do, and that was the key difference.”112 |
| 5.71. | There was, similarly, no system of isolation prior to the pandemic in Scotland, Wales and Northern Ireland.113 |
| 5.72. | While the lack of thinking about mass quarantining could be partially explained by the gap between planning for pandemic influenza and an epidemic or pandemic- scale outbreak of an emerging infectious disease (including one categorised as a high consequence infectious disease), referred to in Chapter 4: An effective strategy, the need for a system of mass quarantining was also a lesson highlighted by the MERS and Ebola outbreaks and exercises that was not acted upon. |
Border controls
| 5.73. | There is a wide range of health security measures that can be used to reduce the risk of importing infections from abroad during a global outbreak. Their use is being considered as part of other modules of this Inquiry. These measures include:
|
| 5.74. | Port and border controls were described by Professor Dame Jenny Harries, Chief Executive of the UK Health Security Agency from April 2021, as being within a category of “wicked issues” that Public Health England was unable to resolve alone. Public Health England had undertaken “quite a lot of work” on port-of-entry screening but there were legal implications and it needed support from “almost everybody” in government.114 |
| 5.75. | The handling of the 2013 to 2016 Ebola outbreak was instructive as to how border restrictions could be effective, as part of a package of measures, in suppressing the spread of a high consequence infectious disease. Border controls were also used effectively by South Korea as part of a series of measures to reduce transmission early on in the MERS outbreak in 2015 (discussed above). Port-of-entry screening was used as part of the UK’s response to the Zika virus outbreak in 2016 and the Fukushima radiological incident in 2011.115 |
| 5.76. | Michael Gove MP (Chancellor of the Duchy of Lancaster from July 2019 to September 2021 and Minister for the Cabinet Office from February 2020 to September 2021) told the Inquiry that, while border closures inevitably impose economic and social costs, “they can be very powerful tools in preventing or slowing the spread of a disease”.116 Professor Dame Sally Davies, Chief Medical Officer for England from June 2010 to October 2019, agreed:
“[T]here are times when you have to do things that may not look cost-effective because the nation needs them.”117 |
| 5.77. | In 2017, Public Health England conducted a review of its public health services at ports, which considered the need to respond rapidly to public health emergencies of international concern, including, for example, by the provision of a port-of-entry screening service.118 This review highlighted that, while health responsibilities at the borders fell to a number of different organisations (for example, Public Health England, the Animal and Plant Health Agency, Border Force, local authorities and the NHS), there was no document describing how these agencies should work together. Public Health England undertook a systematic piece of work, with others, to produce a description of the range of roles and responsibilities.119 This should have led to agreements for closer collaboration, especially in emergency situations. |
| 5.78. | In November 2019, the Department of Health and Social Care agreed to the joint work programme that was proposed by Public Health England in order to improve the public health core capacities at ports. The programme of work included putting in place emergency contingency plans at all significant ports, organising exercises to test these plans and making quarantine facilities available in ports. These actions were not completed by the time the Covid-19 pandemic hit.120 |
| 5.79. | Mr Hancock told the Inquiry that:
“[T]here was no preparedness at all for the fact that health measures at the border may be needed to protect the population.”121 He further explained that border measures were undermined by what he described as an “error” in the Public Health (Control of Disease) Act 1984.122 While the UK border is clearly a UK government responsibility, health measures are devolved, and this created confusion and complications. His view was that legislation needed to change to make health measures at the border unambiguously a UK government responsibility.123 The Inquiry did not receive any evidence that this issue has been resolved. |
| 5.80. | Thus, in January 2020, there was no comprehensive framework that allowed the UK government or the devolved administrations to weigh up the relative costs and benefits of the many different border interventions open to them. While the Inquiry understands the complexities and difficulties involved in putting such a framework in place, the UK government had a responsibility to look into this issue. It failed to do so before the pandemic arrived. |
Surge capacity in health and social care
| 5.81. | At the meeting of the Department of Health’s board on 29 September 2016 referred to above, concerns were raised about how resilient the fragmented health and social care system would be, especially in light of historical or potential future funding cuts.124 |
| 5.82. | Professor Davies told the Inquiry: “[T]he NHS has been known for more than a decade to ‘run hot’, i.e. at full capacity, every winter.”125 The Inquiry also heard that there were severe staff shortages and that a significant amount of the hospital infrastructure in England was not fit for purpose.126 England’s social care sector faced similar issues.127 This combination of factors had a directly negative impact on infection control measures and on the ability of the NHS and the care sector to ‘surge up’ capacity during a pandemic.128 |
| 5.83. | The health and social care services in Wales and Scotland confronted similar challenges to England.129 In Northern Ireland, the health and social care system suffered, in particular, from the lack of an Executive between 2017 and 2020. Professor Sir Michael McBride, Chief Medical Officer for Northern Ireland from September 2006, told the Inquiry that the health service in 2020 was not even as resilient as it had been in 2009.130 |
| 5.84. | Issues of funding are political decisions that properly fall to elected politicians.131 However, it remains the case that the surge capacity of the four nations’ public health and healthcare systems to respond to a pandemic was constrained by their funding. The capacity and resilience of the health and social care systems will be considered by the Inquiry in subsequent modules. |
Personal protective equipment
| 5.85. | The importance of PPE was an issue that arose repeatedly in the exercises, including the 2016 exercises Silver Swan (pandemic influenza in Scotland) and Iris (a MERS-CoV outbreak in Scotland), and in the lead-up to Cygnus.132 |
| 5.86. | It was clear that PPE needed to be stockpiled in advance of a pandemic, in sufficient quantities, fit-tested and connected to an effective distribution network. Sir Christopher Wormald told the Inquiry that “[w]e never nationally ran out of PPE”, but that “in individual places there were shortages of PPE and people having to use not the right PPE”.133 Mr Hancock said that there were logistical difficulties in getting access to stockpiles quickly.134 The Inquiry will be examining this and PPE more fully in subsequent modules. |
The protection of vulnerable people
| 5.87. | An area not sufficiently considered in the exercises, and therefore not acted upon, was how best to protect vulnerable people. There was a failure (as discussed above and in Appendix 2: Exercises):
|
| 5.88. | These failures left the most vulnerable people in society exposed to the effects of a pandemic. To ensure that this does not happen in the future, the effects of a whole-system civil emergency on vulnerable people should be examined through exercises, and the steps to mitigate it should be subject to greater public scrutiny by including them in a published report, as described below. |
The value of pandemic exercises
| 5.89. | These lessons underline the clear value of regular, properly constructed and thorough exercises, even though they have their limitations. The Inquiry recognises that exercises are difficult and costly to design and run, and inevitably involve selecting certain risks over others for simulation, which may not reflect the precise circumstances that materialise. They also risk distracting ministers and officials from more urgent matters of the day. However, the potential advantages of conducting major periodic exercises outweigh the disadvantages. |
| 5.90. | The Inquiry recommends that there should be regular pandemic exercises, including a UK-wide pandemic exercise every three years, conducted in an environment of curiosity and openness and designed to test the response to a pandemic at all stages – from the initial outbreak to a long-term response, with multiple waves over many years. This will also ensure that the potential effects of the response, at every stage, are adequately considered. Exercises should involve ministers and senior officials from the devolved administrations, as well as the NHS, social care and public health leaders, representatives of local resilience forums, voluntary, community and social enterprises, and directors of public health. |
| 5.91. | The planning of exercises ought to be subject to challenge by an external ‘red team’ of non-governmental experts with experience in a range of relevant backgrounds, including scientific, economic and social disciplines. This would encourage consideration of practical, real-world consequences and the asking and answering of ‘what if’ questions. The use of red teams is discussed further in Chapter 6: A new approach. |
| 5.92. | There should be greater ministerial oversight. Ministers in government departments are extremely busy. They cannot always be sighted on the outcome of every report. However, ministers are ultimately responsible for ensuring that their departments implement the lessons identified in the reports to improve preparedness. Given the importance of the exercises in identifying significant gaps in planning, and the practical capacity to respond to an emergency on the ground, there ought to have been more ministerial involvement in and oversight of the exercises. Ministers and their senior officials must therefore take a more active approach in the future to ensure that lessons are not simply rolled over to be considered again at the next exercise. |
| 5.93. | Had this system been in place in 2019, and had the actions, recommendations and learning from past exercises been properly implemented, the UK would have been far better prepared for the Covid-19 pandemic that ensued. |
Recommendation 6: A regular UK-wide pandemic response exercise
The UK government and devolved administrations should together hold a UK-wide pandemic response exercise at least every three years.
The exercise should:
- test the UK-wide, cross-government, national and local response to a pandemic at all stages, from the initial outbreak to multiple waves over a number of years;
- include a broad range of those involved in pandemic preparedness and response; and
- consider how a broad range of vulnerable people will be helped in the event of a pandemic.
A lack of action
| 5.94. | All four nations were slow to implement what were important and necessary preparations for a pandemic. |
| 5.95. | The Inquiry has noted above a number of areas where there was a failure to implement or complete recommendations from simulation exercises. Unfortunately, the various boards and groups set up to oversee this work proved to be largely ineffective. |
| 5.96. | In England, by January 2020 (three years after Exercise Cygnus):
|
| 5.97. | All the devolved nations were involved in programmes of work arising out of Exercise Cygnus. |
| 5.98. | In 2018, Professor McBride established the Northern Ireland Pandemic Flu Oversight Group.136 A ‘task and finish group’ was also formed in 2019 in the Department of Health (Northern Ireland), and its functions included reviewing and updating health and social care influenza pandemic surge guidance.137 This work was paused to redirect to Operation Yellowhammer throughout 2019. It was not resumed prior to the emergence of Covid-19 in January 2020.138 The under-resourcing of the Civil Contingencies Policy Branch of the Executive Office of Northern Ireland had been a longstanding issue. In November 2019, an internal email stated:
“The overall position is dire. There has been systemic failure to invest funding and resources in [the Civil Contingencies Policy Branch] over a number of years and the current position is that at a time of focus, the lack of investment I regret to advise you has left it not fit for purpose.”139 Therefore, in Northern Ireland, the crucial work required to prepare the health and social care sector for a pandemic was not completed. |
| 5.99. | Similarly, the Wales Pandemic Flu Readiness Board did not complete its work. The view appears to have been taken that nothing ought to be done until the UK Pandemic Flu Readiness Board had first updated the 2011 Strategy.140 Dr Andrew Goodall, Permanent Secretary to the Welsh Government from September 2021, told the Inquiry that perhaps the most significant area of concern was the capacity of the adult care sector to cope with the demands of a pandemic. This was because it went directly to matters of life and death in the care home sector. It was a serious issue for local authorities in the discharge of their responsibilities.141 |
| 5.100. | The Scottish Pandemic Flu Preparedness Board was established in 2017 and met every two months until November 2018. It did not meet at all between November 2018 and June 2019 – its meetings were cancelled or postponed due to either the unavailability of officials or the competing priorities of Operation Yellowhammer (or both).142 Gillian Russell, Director of Safer Communities in the Scottish Government from June 2015 to March 2020, explained that, while some work had been completed (eg on excess deaths), other work was paused because “priority was given to other things”.143 By the time the Covid-19 pandemic struck, 8 out of 22 recommendations from Exercise Cygnus were incomplete in Scotland. These included refreshing the 2011 Strategy, fit-testing of PPE, expanding of social care capacity and updating pandemic guidance.144 |
| 5.101. | A system that was geared towards acting upon its findings would have done something about this. However, the governments of the UK, Scotland, Wales and Northern Ireland did not act with sufficient urgency, or at all.145 As the specific example of Exercise Cygnus underlines, lessons that could and should have been learned were not learned. They were left to be discovered afresh in the next exercise or, as it transpired, when the Covid-19 pandemic struck. |
Causes of inaction
Resources and prioritisation
| 5.102. | Some witnesses to the Inquiry described the prioritisation and reprioritisation of limited resources as a cause of inaction. This was a widely recurring theme in the evidence. |
| 5.103. | This was no better highlighted than when several witnesses from the UK government and devolved administrations told the Inquiry that a number of workstreams for pandemic preparedness were paused due to a reallocation of resources to Operation Yellowhammer.146 |
| 5.104. | At a Pandemic Flu Readiness Board meeting in November 2018, Ms Hammond told the board that contingency planning for a ‘no deal’ exit from the European Union had increased significantly over the previous few months and was expected to continue. The Chair reminded the board that prioritisation should not mean that other areas were deprioritised.147 A table charting progress in implementing recommendations made from Exercise Cygnus showed that, as at June 2020, 14 of the 22 lessons identified by Cygnus remained incomplete in the UK.148 Social care, in particular, had been flagged consistently as an issue but had not been addressed. Therefore, the reality was that, far from being completed by its deadline of 2018, the work of the Pandemic Flu Readiness Board in implementing the recommendations from Exercise Cygnus – which repeated many of the same lessons of the previous decade of exercises – was not going to be completed on time, whether Operation Yellowhammer intervened or not. |
| 5.105. | A number of briefings in 2019 to Oliver Dowden MP (Parliamentary Secretary to the Cabinet Office from January 2018 to July 2019 and Minister for the Cabinet Office from July 2019 to February 2020) referred to what was called “re-prioritisation”.149 In January 2019, the Civil Contingencies Secretariat was “prioritising no deal preparations from now on” and was continuing:
“a small number of essential activities alongside no deal preparations but have paused all other activity to enable sufficient focus on preparations for leaving the EU without a deal”.150 |
| 5.106. | Roger Hargreaves, Director of the COBR Unit from July 2022, described the strain on staffing resources caused by preparing for, responding to and recovering from crises. The obvious consequence was that decisions would have to be made to prioritise resources for responding to immediate, upcoming or emerging risks over work on less imminent concerns.151 Mr Dowden, similarly, referred to the normality of reprioritisation that happens within government.152 He claimed that there was “always a flex” in resources needed to respond to challenges as they arise.153 However, even he recognised that Operation Yellowhammer was, as he put it, “at the extreme end of flexing those resources” and at the “extreme end of re-prioritisation”.154 |
| 5.107. | In fact, the evidence before the Inquiry shows that reprioritising competing demands was far from uncommon. Mr Hargreaves noted that at least 32 civil contingencies events in which the Cabinet Office had been directly involved had reprioritised competing demands since 2009.155 Ms Hammond observed that the series of civil emergencies from 2016 onwards, their number and sustained nature, strained the fairly small standing response team within the Civil Contingencies Secretariat. As she put it, when there are a large number of emergencies, “of necessity some of the work is set aside” on other, less urgent matters.156 Ms Hammond described Operation Yellowhammer as a “really major consumer of resources”.157 The Civil Contingencies Secretariat and the Cabinet Office had – to use the expression again – to “set aside” certain streams of work that they knew they ought to be doing.158 |
| 5.108. | On the positive side, despite the general strain on resourcing, Mr Dowden told the Inquiry that, in fact, Operation Yellowhammer made the UK “match fit” to deal with the Covid-19 pandemic.159 He said that this was because the UK government had recruited about 15,000 extra staff who could then be redeployed to increase preparedness or contribute to the pandemic response effort.160 Mr Gove agreed.161 The Inquiry heard evidence that, as a result of Operation Yellowhammer, the UK government had improved its understanding of essential supply chains and the importance of stronger relationships with industry, increased stockpiles of critical medicines and access to medical products.162 |
| 5.109. | The fact, however, remains that the UK government’s preparedness and resilience system was, quite evidently, under constant strain. It was reliant on stopping work on preparing for one potential emergency to concentrate on another. The trend is for there to be more complex and concurrent risks. The evidence above suggests that there were, and remain, real limits on the state’s capacity to cope with an increasing trend of multiple, complex civil emergencies happening at the same time. |
Bureaucracy
| 5.110. | A second cause of inaction was the growth of bureaucracy. |
| 5.111. | In the simulation exercises that took place between 2003 and 2016, the same critical issues concerning the general inadequacy of the UK government and devolved administrations’ state of preparedness reappeared time and again. Testing, tracing, isolation, health and social care surge capacity, and border controls were raised frequently. This could and should have served as a warning of what needed to be done. It did not. |
| 5.112. | There was a failure of the institutions to identify and accurately describe the underlying problems, compounded by the use of jargon and euphemism to disguise, for example, tasks that had not been completed. This was compounded by a failure of leadership to implement solutions, demonstrated by the proliferation of lengthy documents, plans and guidance (which, in any event, were often not updated) rather than the infrastructure to deal with a pathogen outbreak. The Inquiry saw the creation of processes to solve problems rather than the solving of the problems themselves (see Chapter 6: A new approach). |
| 5.113. | Further, the complexity of the preparedness and resilience system overall (see Chapter 2: The system – institutions, structures and leadership) resulted in an absence of clear lines of accountability, a blurring of responsibilities, the duplication of effort and, ultimately, inefficiency. |
Institutional memory
| 5.114. | A third cause of inaction was the lack of institutional memory. This is often caused by frequent and rapid changes in personnel and, as a consequence, a loss of experience and knowledge. It is not a problem unique to government – it is a problem faced by all major institutions. |
| 5.115. | Institutional memory includes internal knowledge, lessons learned, successful strategies and past mistakes, and enables the business of government or some other organisation to continue effectively across successive administrations. It is crucial that there is a simple and accessible system for knowledge to be captured and shared.163 This is especially important when there is a high turnover of officials and ministers – “churn in the system” or a “revolving door” of ministers.164 An effective system of institutional memory requires a means of storing and accessing exercise reports, action plans, emergency planning and guidance. This enables a full and open discussion of what worked well and what did not, and the encouragement of a culture of debate and challenge. |
| 5.116. | Understanding lessons of the past and retaining knowledge about past failures contributes to more effective decision-making in the future and help to prevent the repetition of similar mistakes. It also fosters innovation and is crucial for continuous improvement and building resilience. This is so that preparedness improves, even if incrementally, over time. |
| 5.117. | There should be open access – for all those involved in pandemic preparedness and response throughout the UK – to preserved, institutional information. Having quick access to past solutions and best practices also enhances efficiency. It prevents the need to ‘reinvent the wheel’ and for wasteful parallel processes. The Inquiry is therefore recommending the creation of a central, UK-wide online repository of information relating to civil emergency exercises, which should include all exercise reports and emergency guidance. This repository should be accessible to, among others, the devolved administrations, local and regional tiers of government, and those in the voluntary and community sectors. |
Recommendation 7: Publication of findings and lessons from civil emergency exercises
For all civil emergency exercises, the governments of the UK, Scotland, Wales and Northern Ireland should each (unless there are reasons of national security for not doing so):
- publish an exercise report summarising the findings, lessons and recommendations, within three months of the conclusion of the exercise;
- publish an action plan setting out the specific steps that will be taken in response to the report’s findings, and by which entity, within six months of the conclusion of the exercise; and
- keep exercise reports, action plans, and emergency plans and guidance from across the UK in a single, UK-wide online archive, accessible to all involved in emergency preparedness, resilience and response.
Parliamentary scrutiny
| 5.118. | Finally, a possible cause of inaction was a lack of openness. Exercises were not conducted in a sufficiently open manner and therefore were not subject to the level of independent scrutiny required. Had the results of the exercises been published more widely, this may have triggered comment and response from others. The Inquiry has recommended above ways in which the results of simulation exercises should be shared and open to public scrutiny. |
| 5.119. | However, one of the most effective forms of public scrutiny is parliamentary scrutiny. The Inquiry considers that greater oversight of the ministers, institutions and officials with responsibility for whole-system civil emergency preparedness and resilience by Parliament and the devolved legislatures will help to solve the problems of inadequate action identified in this Report. |
| 5.120. | In its 2022 Resilience Framework, the UK government committed to delivering an annual statement to Parliament on its understanding of the current risk picture, performance on resilience and the current state of preparedness of civil contingencies.165 This was intended to increase public accountability. In December 2023, Mr Dowden delivered the first Annual Resilience Statement to Parliament and the Cabinet Office published The UK Government Resilience Framework: 2023 Implementation Update.166 However, there is, as yet, no commitment to a full, published analysis setting out recommendations to improve preparedness and resilience; no analysis of the costs of assuming the risks as against the benefits of taking steps to mitigate the risks; and no particular regard to how vulnerable people will be protected. There is no implementation plan and there are no deadlines against which performance may be objectively judged. |
| 5.121. | In order to improve further scrutiny and public accountability, the Inquiry recommends that the UK government, Scottish Government, Welsh Government and Executive Office of Northern Ireland should each produce and publish reports to their respective legislatures at least every three years on their approaches to whole- system civil emergency preparedness and resilience. Each government should:
In this way, governments and their political leaders may be properly held to account on a regular basis for the condition of the systems of preparedness and resilience. |
Recommendation 8: Published reports on whole-system civil emergency preparedness and resilience
The governments of the UK, Scotland, Wales and Northern Ireland should each produce and publish reports to their respective legislatures at least every three years on whole-system civil emergency preparedness and resilience.
The reports should include as a minimum:
- the risks that each government has identified are likely to result in whole-system civil emergencies;
- the recommendations that have been made to each government to mitigate those risks, and whether these recommendations have been accepted or rejected;
- a cost–benefit analysis setting out the economic and social costs of accepting the risks as against taking action to mitigate the risks;
- who may be vulnerable to the risks and what steps are being taken to mitigate those risks;
- a plan setting out the timescales for implementing the recommendations that have been accepted; and
- an update on the progress that has been made on implementing previously accepted recommendations.
- Richard Horton 13 July 2023 71/14-20
- INQ000149108_0013
- Mark Woolhouse 5 July 2023 121/2-122/12; ‘The WHO R&D Blueprint: 2018 review of emerging infectious diseases requiring urgent research and development efforts’, M. Si Mehand, F. Al-Shorbaji, P. Millett and B. Murgue, Antiviral Research (2018), 159, 63-67, p66 (https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7113760/pdf/main.pdf; INQ000149109)
- ‘Lessons learned from SARS: The experience of the Health Protection Agency, England’, N.L. Goddard, V.C. Delpech, J.M. Watson, M. Regan and A. Nicoll, Public Health (2006) 120, 27-32, p27 (https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7118739/pdf/main.pdf; INQ000187893)
- Richard Horton 13 July 2023 68/7-13
- INQ000194054_0049 para 198; INQ000205178_0057 para 81; see also Table 1: Summary of past major epidemics and pandemics in Chapter 1: A brief history of epidemics and pandemics
- INQ000205178_0058-0059 para 83
- ‘Giants on Clay Feet: COVID-19, infection control and public health laboratory networks in England, the USA and (West-) Germany (1945–2020)’, C. Kirchhelle, Social History of Medicine (2022), 35(3), 703-748, p736 (https://www.ncbi.nlm.nih.gov/pmc/articles/PMC9384317/pdf/hkac019.pdf; INQ000207449)
- INQ000235216_0001, 0009
- INQ000235217_0005-0011
- INQ000187903_0001-0002
- INQ000206664_0013
- ‘Lessons learned from SARS: The experience of the Health Protection Agency, England’, N.L. Goddard, V.C. Delpech, J.M. Watson, M. Regan and A. Nicoll, Public Health (2006) 120, 27-32, p30 (https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7118739/pdf/main.pdf; INQ000187893)
- ‘Lessons learned from SARS: The experience of the Health Protection Agency, England’, N.L. Goddard, V.C. Delpech, J.M. Watson, M. Regan and A. Nicoll, Public Health (2006) 120, 27-32, p31 (https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7118739/pdf/main.pdf; INQ000187893)
- ‘Lessons learned from SARS: The experience of the Health Protection Agency, England’, N.L. Goddard, V.C. Delpech, J.M. Watson, M. Regan and A. Nicoll, Public Health (2006) 120, 27-32, p32 (https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7118739/pdf/main.pdf; INQ000187893)
- The 2009 Influenza Pandemic: An independent review of the UK response to the 2009 influenza pandemic, Dame Deirdre Hine, July 2010, paras 1-2 (https://assets.publishing.service.gov.uk/media/5a7975f1ed915d0422068a10/the2009influenzapandemic-review. pdf; INQ000022705)
- The 2009 Influenza Pandemic: An independent review of the UK response to the 2009 influenza pandemic, Dame Deirdre Hine, July 2010, para 5 (https://assets.publishing.service.gov.uk/media/5a7975f1ed915d0422068a10/the2009influenzapandemic-review.pdf; INQ000022705)
- The 2009 Influenza Pandemic: An independent review of the UK response to the 2009 influenza pandemic, Dame Deirdre Hine, July 2010, para 5.41 (https://assets.publishing.service.gov.uk/media/5a7975f1ed915d0422068a10/the2009influenzapandemic-review.pdf; INQ000022705)
- INQ000102936_0002 para 5
- INQ000102936_0002 para 6
- INQ000128976_0013 paras 1-2
- INQ000182610_0015 para 1b
- INQ000184643_0069 paras 362-363
- INQ000184643_0070-0071 paras 369-373
- INQ000177796_0004 para 15
- INQ000022723_0001 para 8
- INQ000184643_0069 para 363
- INQ000022723_0014
- INQ000022723_0014 entries 16-17
- INQ000177808_0010-0011 para 44
- INQ000184643_0067 para 354c
- INQ000090428_0014-0016
- INQ000184893_0009 para 36; see also INQ000148417_0009 para 3.10
- INQ000184893_0010 para 37
- INQ000184893_0017 para 61
- INQ000184893_0019–0020 paras 70, 74
- INQ000184893_0017 para 61
- INQ000185135_0002; INQ000195846_0008 para 25; INQ000148429_0059 para 235
- INQ000090431
- INQ000184643_0066 paras 351-352; Christopher Wormald 19 June 2023 137/10-12
- INQ000090431_0005-0006
- INQ000090431_0009
- INQ000090431_0009
- INQ000090431_0004, 0011
- INQ000090431_0011
- INQ000090431_0012
- INQ000090431_0010
- INQ000090431_0011
- INQ000090431_0013
- INQ000148429_0097 para 380
- See INQ000090431_0016
- Christopher Wormald 19 June 2023 137/5-12
- INQ000212312_0025 para 100
- INQ000087227_0008 para 6.6
- See, for example, Jeremy Hunt MP, Secretary of State for Health and Social Care from September 2012 to July 2018 (INQ000177796_0010-0011 paras 39-45); David Heymann 15 June 2023 54/3-60/25, 61/17-25; Richard Horton 13 July 2023 90/5-92/4; Professor Dame Sally Davies, Chief Medical Officer for England from June 2010 to October 2019 (INQ000184637_0008 paras 6.1-6.3)
- INQ000177796_0010 para 40
- INQ000177796_0010 para 41
- David Heymann 15 June 2023 55/8-9
- INQ000177796_0010-0011 paras 40-47
- See Appendix 2: Exercises for more detail on the key exercises conducted in the UK and the devolved nations between 2002 and 2008
- Exercise Cygnus Report: Tier One Command Post Exercise Pandemic Influenza – 18 to 21 October 2016, Public Health England, 2017, pp5-6 (https://www.gov.uk/government/publications/uk-pandemic-preparedness/exercise-cygnus-report-accessible-report; INQ000022792)
- Exercise Cygnus Report: Tier One Command Post Exercise Pandemic Influenza – 18 to 21 October 2016, Public Health England, 2017, pp8-9 (https://www.gov.uk/government/publications/uk-pandemic-preparedness/exercise-cygnus-report-accessible-report; INQ000022792)
- Exercise Cygnus Report: Tier One Command Post Exercise Pandemic Influenza – 18 to 21 October 2016, Public Health England, 2017, p6 (https://www.gov.uk/government/publications/uk-pandemic-preparedness/exercise-cygnus-report-accessible-report; INQ000022792)
- Exercise Cygnus Report: Tier One Command Post Exercise Pandemic Influenza – 18 to 21 October 2016, Public Health England, 2017, p6 (https://www.gov.uk/government/publications/uk-pandemic-preparedness/exercise-cygnus-report-accessible-report; INQ000022792)
- Exercise Cygnus Report: Tier One Command Post Exercise Pandemic Influenza – 18 to 21 October 2016, Public Health England, 2017, p7 (https://www.gov.uk/government/publications/uk-pandemic-preparedness/exercise-cygnus-report-accessible-report; INQ000022792)
- Exercise Cygnus Report: Tier One Command Post Exercise Pandemic Influenza – 18 to 21 October 2016, Public Health England, 2017, p6 (https://www.gov.uk/government/publications/uk-pandemic-preparedness/exercise-cygnus-report-accessible-report; INQ000022792)
- Exercise Cygnus Report: Tier One Command Post Exercise Pandemic Influenza – 18 to 21 October 2016, Public Health England, 2017, p9 (https://www.gov.uk/government/publications/uk-pandemic-preparedness/exercise-cygnus-report-accessible-report; INQ000022792). Similar issues were raised in a part of Exercise Cygnus that took place in Wales in 2014 (INQ000128979). The most significant failing identified through that exercise was the capacity of the adult care sector to cope with the demands of a pandemic (Andrew Goodall 4 July 2023 34/9-20).
- Exercise Cygnus Report: Tier One Command Post Exercise Pandemic Influenza – 18 to 21 October 2016, Public Health England, 2017, p6 (https://www.gov.uk/government/publications/uk-pandemic-preparedness/exercise-cygnus-report-accessible-report; INQ000022792)
- INQ000128057_0005 first para
- INQ000128057_0007 third bullet point
- INQ000128057_0007 sixth bullet point
- INQ000128057_0009 first bullet point
- INQ000128057_0005-0006
- INQ000177796_0007 para 25
- INQ000128057_0009 first bullet point
- INQ000195847_0004 para 21. See also INQ000145733_0021 para 3.33
- INQ000022743_0002 para 6
- INQ000022748
- INQ000128057_0007 third and sixth bullet points, INQ000128057_0009 first bullet point
- INQ000045034_0001-0002 paras 4-5
- INQ000022921_0002
- INQ000022921_0002
- INQ000022748 para 1
- Matt Hancock 27 June 2023 37/5-7, 52/4-24
- INQ000047302_0002 para 3
- INQ000131543_0003 paras 10, 11, 13, 14
- INQ000090431; Exercise Cygnus Report: Tier One Command Post Exercise Pandemic Influenza – 18 to 21 October 2016, Public Health England, 2017 (https://www.gov.uk/government/publications/uk-pandemic-preparedness/exercise-cygnus-report-accessible-report; INQ000022792); Clara Swinson 19 June 2023 164/16-166/14
- Mark Lloyd 12 July 2023 100/1-13
- Exercise Cygnus Report: Tier One Command Post Exercise Pandemic Influenza – 18 to 21 October 2016, Public Health England, 2017, p56 (https://www.gov.uk/government/publications/uk-pandemic-preparedness/exercise-cygnus-report-accessible-report; INQ000022792); INQ000006861_0001 para 2; Mark Lloyd 12 July 2023 102/10-19
- Mark Lloyd 12 July 2023 104/1-17; see also INQ000177803_0059-0060 paras 233-234
- Mark Lloyd 12 July 2023 107/18-108/2
- Mark Lloyd 12 July 2023 104/20-21
- INQ000177809_0015 para 39
- INQ000195843_0065 para 150; INQ000194054_0065 para 256
- Documentation was examined in relation to: Exercise Winter Willow (2007); Exercise Taliesin (2009); Exercise Valverde (2015); Ebola Preparedness Surge Capacity Exercise (2015); Exercise Silver Swan (2016); Exercise Alice (2016); Exercise Northern Light (2016); Exercise Cygnus (2016); Exercise Typhon (2017); Exercise Broad Street (2018); Exercise Cerberus (2018); and Exercise Pica (2018) (INQ000195843_0038, 0044, 0052-0055, 0064 paras 82-84, 113, 133-142, 149).
- INQ000194054_0065 para 256
- INQ000092634_0005; INQ000177803_0059 para 232
- INQ000205178_0103 para 148.2
- INQ000177810_0008 para 25
- INQ000145912_0131 para 10.36
- INQ000184643_0071 para 372
- INQ000006429_0002-0003 para 5
- Duncan Selbie 27 June 2023_152/20-155/1
- INQ000181825_0017 para 73
- Duncan Selbie 27 June 2023 136/15-137/5, 139/13-140/12
- For Scotland, see Jeane Freeman 28 June 2023 137/15-138/12, Nicola Sturgeon 29 June 2023 42/13-43/7, 46/14-47/16, 62/21-64/15, Catherine Calderwood 5 July 2023 18/1-19/4; for Wales, see Frank Atherton 3 July 2023 26/2-11, 32/13-33/1, 65/4-67/3; for Northern Ireland, see Denis McMahon 6 July 2023 66/1-20, Michael McBride 10 July 2023 147/11-24, 162/25-165/3, Richard Pengelly 11 July 2023 78/22-79/7, 110/24-111/3
- INQ000181825_0017 para 72
- INQ000184639_0017 para 5.10
- INQ000057271_0006 para 25
- INQ000057281_0001-0002 re item HCIDPB 16/46
- Christopher Wormald 19 June 2023 96/13-97/8
- Christopher Wormald 19 June 2023 122/14-19
- For Scotland, see Nicola Sturgeon 29 June 2023 42/13-43/7; for Wales, see Frank Atherton 3 July 2023 32/13-33/1; for Northern Ireland, see Arlene Foster 11 July 2023 49/9-50/5, Richard Pengelly 11 July 2023 78/22-79/7
- Jenny Harries 26 June 2023 177/13-178/11, 180/24-25/206/3-12
- INQ000194054_0027-0028 para 108
- Michael Gove 13 July 2023 158/7-8
- Sally Davies 20 June 2023 160/3-5
- INQ000194054_0027-0028 para 108
- INQ000148429_0040 para 144
- INQ000148429_0040 para 144; INQ000194054_0028 para 110
- INQ000181825_0020 para 88
- INQ000181825_0020 para 89
- INQ000181825_0020-0021 para 89
- INQ000057271_0006 para 26
- INQ000184637_0005-0006 para 4.2
- INQ000177809_0017 para 45; Nigel Edwards 13 July 2023 51/20-21
- See INQ000183420_0006 para 17; INQ000177809_0017 para 45
- INQ000147815_0005, 0006 paras 19, 23
- INQ000177807_0012 paras 42-44; INQ000177807_0015 para 53 (Wales); INQ000180759_0005 paras 18-20 (Scotland)
- Michael McBride 10 July 2023 180/14-18
- INQ000184637_0006 para 4.6
- INQ000147883_0017; INQ000147839_0008-0009; Exercise Cygnus Report: Tier One Command Post Exercise Pandemic Influenza – 18 to 21 October 2016, Public Health England, 2017, p33 (https://www.gov.uk/government/publications/uk-pandemic-preparedness/exercise-cygnus-report-accessible-report; INQ000022792)
- Christopher Wormald 19 June 2023 133/3-134/2
- Matt Hancock 27 June 2023 21/18-22, 94/17-95/2
- Katharine Hammond 16 June 2023 183/24-184/12
- Michael McBride 10 July 2023 121/18-122/24
- Michael McBride 10 July 2023 123/5-15
- INQ000203352_0012-0013 para 38
- INQ000183597 first para
- Frank Atherton 3 July 2023 44/22-45/10
- Andrew Goodall 4 July 2023 34/9-20
- Gillian Russell 28 June 2023 76/25-78/25
- Gillian Russell 28 June 2023 71/10
- INQ000182606_0006 para 20; Caroline Lamb 28 June 2023 118/7-22; Jeane Freeman 28 June 2023 135/25-136/5
- Professor David Alexander and Bruce Mann, expert witnesses on risk management and resilience (see Appendix 1: The background to this module and the Inquiry’s methodology), observed: “By contrast [to the UK government], it is notable that the devolved administrations [in Scotland and Wales] did pursue pandemic preparedness [between 2012 and 2016]” (INQ000203349_0166 para 490; see generally INQ000203349_0164-0168 paras 482-494)
- eg Mark Drakeford 4 July 2023 192/3-25
- INQ000022069_0002, 0004 paras 2, 11
- INQ000057522_0002
- See Oliver Dowden 21 June 2023 90/8-91/1, 95/6-96/4, 105/11-107/20
- INQ000205310_0002 first and second bullet points
- INQ000182612_0068-0069 paras 5.8-5.10
- Oliver Dowden 21 June 2023 95/22-23
- Oliver Dowden 21 June 2023 96/1-4
- Oliver Dowden 21 June 2023 98/16-17, 106/3-4
- INQ000182612_0069-0070 para 5.12
- Katharine Hammond 16 June 2023 118/9-119/9
- Katharine Hammond 16 June 2023 119/15-16
- Katharine Hammond 16 June 2023 119/10-16
- Oliver Dowden 21 June 2023 93/17
- Oliver Dowden 21 June 2023 93/13-94/2
- Michael Gove 13 July 2023 108/24-109/9
- INQ000184643_0079-0080 para 416; Matt Hancock 27 June 2023 64/12-65/2; Michael Gove 13 July 2023 148/16-151/22; see also Mark Drakeford 4 July 2023 192/3-25
- Patrick Vallance 22 June 2023 134/21-135/6
- Jenny Harries 26 June 2023 206/19-21; Oliver Letwin 20 June 2023 16/7-8
- The UK Government Resilience Framework, HM Government, December 2022 (https://assets.publishing.service.gov.uk/media/63cff056e90e071ba7b41d54/UKG_Resilience_Framework_FINAL_v2.pdf; INQ000097685)
- The UK Government Resilience Framework: 2023 Implementation Update, Cabinet Office, 4 December 2023 (https://assets.publishing.service.gov.uk/media/656def711104cf0013fa7498/The_UK_Government_Resilience_Framework_2023_Implementation_Update.pdf; INQ000372824)
Chapter 6: A new approach
Introduction
| 6.1. | At the heart of pandemic preparedness is the provision of expert advice. The UK is fortunate to have at its disposal many world-class experts prepared to offer their services. However, the Inquiry has concluded that the system for providing advice could and should be improved. This, in turn, would lead to better-informed and improved decision-making. This chapter considers the most effective means of ensuring that ministers have access to advice at an appropriate time, and that they are properly presented with a range of scientific opinion and policy options that help them to better prepare for and build resilience to whole-system civil emergencies. It recommends a new approach. |
Advice to ministers
| 6.2. | Ministers are rarely offered perfect policy solutions. They must usually balance difficult trade-offs between competing options. They, not their advisers, are ultimately responsible for deciding policy and where those trade-offs lie, but they rely on advice. |
| 6.3. | Ministers commence their role, by and large, as amateurs, and are often not professionally trained in the policy areas of their departments. They are required to learn on the job.¹ They must, nonetheless, provide leadership to their department and decide complex matters of policy, and that is no less true in the field of emergency preparedness and resilience. |
| 6.4. | They should, therefore, challenge the advice they receive from both experts and officials. The quality of the decision-making of ministers will only be as good as the depth and range of advice they receive, as well as their interrogation of that advice. Michael Gove MP, Chancellor of the Duchy of Lancaster from July 2019 to September 2021 and Minister for the Cabinet Office from February 2020 to September 2021, told the Inquiry:
“[W]hat we bring is the capacity to ask the ‘daft laddie’ question, and sometimes it is only when someone asks that question that we find out that the Emperor has no clothes or the pandemic preparedness plan has a huge hole in the middle.”² |
| 6.5. | Sir Oliver Letwin MP, Minister for Government Policy from May 2010 to July 2016 and Chancellor of the Duchy of Lancaster from July 2014 to July 2016, said that his lack of expertise made it absurd to suppose that he could counteract or overrule the advice of scientific experts.³ However, there were wider questions ministers could and should usefully ask:
“I think that I should have said to myself, in retrospect, not, ‘Are all these experts wrong?’ but, ‘Have they asked the right questions?’ Because that is something an amateur can do. Perhaps only an amateur can do that. In a sense you have to be outside to the system, I think, to a degree, to be able to ask that question.”⁴ |
| 6.6. | The importance of the leadership and perspective that is provided by ministers was underscored by Dr Denis McMahon, Permanent Secretary to The Executive Office of Northern Ireland from July 2021, who said that ministers:
“see things from the point of view of the person on the ground … in my experience ministers bring a reality to things, they bring a sense of purpose, because they just connect us back to the community”.⁵ |
| 6.7. | Professor Sir Mark Walport, Government Chief Scientific Adviser from April 2013 to September 2017, explained to the Inquiry that, in his experience, ministers in government looked through “three lenses” when making decisions:
|
| 6.8. | Key to informing the first two of these ‘lenses’ in the context of pandemic planning was expert advice. Professor Sir Patrick Vallance, Government Chief Scientific Adviser from April 2018 to March 2023, explained that this involved four questions for the adviser:
|
| 6.9. | It is also essential that the expert advice on the options is commissioned, provided and considered before an emergency, when there is time properly to analyse it and to consider the possible consequences of the policy options. Professor Walport observed:
“Every national emergency has knock on effects on citizens lives beyond the immediate impact of the emergency itself – and there is always the possibility that the ‘cure’ for the specific emergency in terms of the policies and actions directed at stemming the primary damage causes harmful ‘side effects’ … But it is only the policy makers themselves who can ultimately decide on how to make the exceedingly difficult choices between, as a specific and rather pointed example, preservation of the health and lives of the elderly and vulnerable by measures that are likely to damage the economy and disrupt the education of young people.”¹² |
Improving the provision of scientific advice
| 6.10. | Advice from experts was commissioned by government ministers, departments and public bodies. The Inquiry heard evidence from a range of scientists about the way this was done. Broadly, eight defects were apparent:
|
Roles of expert advisers to the UK government and devolved administrations
| 6.11. | The responsibilities of the chief scientific adviser and chief medical officer roles in the devolved administrations differed from their UK government counterparts and from each other (see Chapter 2: The system – institutions, structures and leadership). While the work of the system of chief scientific advisers and the Chief Medical Officer for England was primarily focused on issues relevant to England, they also had prominent roles in relation to issues that affected the devolved administrations.¹³ This was similarly true for the UK Government Chief Scientific Adviser.¹⁴ The Inquiry considers that preparing for and building resilience to whole-system civil emergencies requires the governments of the devolved administrations to have a chief medical officer and a chief scientific adviser with broader responsibilities, comparable to those of the Chief Medical Officer for England and the UK Government Chief Scientific Adviser. There ought then to be parity between the chief medical officers and chief scientific advisers of the UK and those of the devolved administrations in terms of their access and contribution to the debates on preparedness and resilience. If this approach is taken, the UK government and devolved administrations would be in a better position to formulate a single overarching approach to whole-system civil emergencies, while tailoring it to the circumstances of each population. |
Allowing experts the freedom to advise
| 6.12. | Scientific advisers generally responded to specific requests for advice. Professor John Edmunds, Professor of Infectious Disease Modelling at the London School of Hygiene & Tropical Medicine – who had been a member of a number of scientific advisory groups – observed that these committees dealt with practical, day-to-day issues as emergencies arose, not with broader strategic issues prior to the occurrence of an emergency.¹⁵ Professor Thomas Evans, Chair of the Advisory Committee on Dangerous Pathogens from 2016, observed that this committee’s advice was focused on high consequence infectious diseases rather than overall pandemic preparedness.¹⁶ Professor Sir Andrew Pollard, Chair of the Joint Committee on Vaccination and Immunisation from 2013, said that, as far as he knew, the Department of Health and Social Care did not ask that committee to consider planning for pandemics other than influenza, or to advise on vaccines and stockpiling for other infectious diseases – this was despite it being within its capability and expertise.¹⁷ |
| 6.13. | Professor Sir Peter Horby, a member of the New and Emerging Respiratory Virus Threats Advisory Group (NERVTAG) from 2014, and Chair from May 2018, told the Inquiry:
“The content of the meetings was very much commissioned by [the Department of Health and Social Care] … there was no expectation or explicit encouragement to consider issues beyond the specific commissions.”¹⁸ |
| 6.14. | Professor Walport explained the critical importance of scientific advisers not only responding to questions but also providing “spontaneous advice” on matters they considered to be relevant so that the government would be getting the most out of their expertise.¹⁹ This view was supported by Professor Vallance and Dr Jim McMenamin, Head of Infections Service and Strategic Incident Director at Public Health Scotland.²⁰ |
| 6.15. | Professor Wendy Barclay, Action Medical Research Chair of Virology at Imperial College London and a member of NERVTAG from 2014, explained to the Inquiry that the reason that its members had not thought sufficiently “outside the box” prior to the pandemic was similarly due to the fact that their agendas were “filled” with tasks set by ministers and officials.²¹ As a consequence, they did not have the time to consider “the unexpected”.²² This included viruses that were not influenza and also the full range of potential responses.²³ |
| 6.16. | By contrast, Professor Sir Jonathan Van-Tam, Chair of NERVTAG from 2014 to 2017 and Deputy Chief Medical Officer from October 2017 to March 2022, considered that advice should be more rigid and task-oriented, responding to requests.²⁴ He encouraged government departments to think more carefully about the remits of, and questions put to, the expert groups. Professor Van-Tam told the Inquiry: “NERVTAG does not define its own remit, it responds to requests and will confine its advice to the brief provided. That is how a government advisory committee should operate. If it is not directly responding to the requests put to it, then it is not fulfilling its purpose.”²⁵ |
| 6.17. | Professor Sir Christopher Whitty, Chief Medical Officer for England from October 2019, described an “80/20 rule”, where most of the time (80%) should be spent on things the government has asked about, but a significant minority (20%) should be spent on things the government has not asked about.²⁶ He told the Inquiry that the precise line to be drawn ought to be at the discretion of the independent chairs, but that there should be latitude. Otherwise, the expert groups and committees become an extension of government.²⁷ The Inquiry agrees. In addition to answering questions specifically commissioned by ministers and officials, advisers ought to be free to consider the wider context in which their advice is sought.²⁸ There should be a balance between advice commissioned from the top downwards and advice being given, spontaneously, from the bottom upwards. Scientific advisers ought to be “‘licensed dissidents’” with a general remit to provide scientific opinion and challenge throughout the system.²⁹ |
| 6.18. | There is a further problem in that those making the requests may not know exactly how they should be framed. This unnecessarily constrained the expert groups. Often their remit was set too narrowly, the commissioning of advice was too rigid and there was insufficient time for deeper thought to be given to solving the problems they were asked to consider.³⁰ As a result, they were unable to act with sufficient autonomy. The Inquiry agrees with Professor Whitty that flexibility is critical. There is a very strong case for independent expert groups having a mandate to think more broadly and strategically. They could then think about overall pandemic preparedness rather than only responding to commissions.³¹ |
The importance of feedback
| 6.19. | It also appeared that, prior to the pandemic, there was not a culture of routinely informing scientific experts of how their advice had been applied by the government. Some advisers had limited knowledge of the extent to which their advice was acted upon, if at all.³² |
| 6.20. | The Inquiry considers that scientific advice on preparedness and resilience ought routinely to encourage a two-way discussion between ministers and experts. There should be a system that invites a back-and-forth between scientific advisers and decision-makers.³³ This would enhance the quality of both the questions asked and the advice provided – a positive feedback loop. It would significantly improve the current system.³⁴ |
Range of expertise
| 6.21. | All whole-system civil emergencies have profound economic and social impacts, as do the measures taken by governments in response. An effective and long-term approach to preparedness and resilience should therefore include a way for government to have advice available to it, covering a range of specialisms – from scientific to economic expertise – as well as from experts who understand the impact on individuals, businesses and society. In the case of pandemic preparedness, scientific advice will naturally be weighted towards the biomedical sciences, but, as a whole-system civil emergency, this must not be to the exclusion of other expertise. |
| 6.22. | Yet, there were major omissions from the expert committees advising governments on pandemic preparedness. The advice was biased towards biomedical advice and did not include socio-economic advice from comparable experts. Professor Whitty’s frame of reference was the Scientific Advisory Group for Emergencies (SAGE) (convened in an emergency), but it was equally true of the range of expert groups advising on preparedness:
“I don’t think SAGE people, including myself, have the competence to assure government that they’ve considered the economic problem and they can now give a central view on it. I think that would have to be done separately.”³⁵ This important issue is being explored in Module 2. |
| 6.23. | The scientists who gave evidence to the Inquiry maintained that they could only advise the government on one aspect of preparedness: the countermeasures to immediately protect life. They could not go beyond their expertise and make a judgement call that took into account wider societal impact – that was a matter for elected leaders, applying their values and judgement.³⁶ This is, of course, right. However, there is not currently an institution that can advise ministers, in the round, on how best to go about solving these problems. The purpose is not to supplant political leaders of their responsibility but to support them in applying their judgement to the important task of building preparedness and resilience in the long-term interests of the UK (including the devolved nations). |
| 6.24. | Professor Dame Sally Davies, Chief Medical Officer for England from June 2010 to October 2019, identified a need to “balance the biomedical model” so that government decision-makers were presented with advice from a wider range of perspectives. This might include, for example, impacts on the economy, social wellbeing, and children and young people in education.³⁷ As she described, there should be “an institutional framework to ensure that there are a full range of opinions from each discipline”.³⁸ Professor Edmunds observed the need for greater interaction between economists and epidemiologists to improve the quantity and quality of economic assessments for pandemics.³⁹ |
| 6.25. | The balancing of scientific advice with other, potentially competing, factors was emphasised by Professor Walport:
“[I]t is extremely important that the policy makers receive advice on what are the potential adverse consequences of, for example lockdowns, on businesses, |
| 6.26. | The range of expertise to be drawn on might include, as Professor Vallance told the Inquiry, “many scientific disciplines, engineering, social science, mathematical modelling, economics etc. They would also link to industry, both small and large.”⁴¹ The UK government and devolved administrations would benefit from this expertise coming together to advise their governments systematically. As Professor Vallance said: “[T]here’s something about bringing together a critical mass of people who are concerned with the same overall problem.”⁴² It will bring challenge, independence and foresight. The Inquiry agrees that being able to consider this range of individual expert disciplines “would begin to provide an insight into how you might think about the sort of difficult trade-offs that occur there”.⁴³ |
| 6.27. | This would ensure that strategic advice is better grounded in improvements to the capacity and capabilities of the UK government and devolved administrations. As set out in Chapter 4: An effective strategy and Chapter 5: Learning from experience, the skills, technology and infrastructure for pandemic preparedness should focus first on scalable systems of testing, tracing, isolation, border controls and surge capacity in health and social care. |
Coordination of advice
| 6.28. | There was no entity that oversaw the system of expert scientific advice to ensure that it was broad-based, integrated and coordinated. The scientific advisory committees advising on pandemic preparedness and resilience should be part of a whole system that “collaborates widely to deliver advice that takes account of the wider science system and is integrated and coordinated with other parts of it”.⁴⁴ |
| 6.29. | Professor Jimmy Whitworth, expert witness on infectious disease surveillance (see Appendix 1: The background to this module and the Inquiry’s methodology), thought it was useful for expert groups to be focused on the areas where their expertise lay. However, he wanted to see their recommendations being coordinated and synthesised within the government to get an overarching view of the risks.⁴⁵ Such joined-up thinking has been absent. |
| 6.30. | A number of expert advisers working within this system found it a complex picture to navigate. Professor David Salisbury, Director of Immunisation at the Department of Health from 2007 to 2013, remarked on the “explosion of committees” in this field.⁴⁶ He questioned the efficiency, effectiveness and impact of “casts of thousands being involved across the advisory process”, relative to the time and resources they each consumed.⁴⁷ Professor Horby told the Inquiry that “[t]he governance structure that NERVTAG sat within was quite complicated”, with a lack of clarity about reporting structures and questions about who was accountable to whom between NERVTAG, other scientific advisory groups and the Department of Health and Social Care.⁴⁸ |
| 6.31. | Professor Barclay provided instances of NERVTAG working well with other scientific advisory groups, noting: “[T]here is some overlap in remit of these committee[s] and joint meetings allowed merging of specific expertise.”⁴⁹ However, Professor Horby suggested that this was the exception rather than the rule: “NERVTAG was a standalone committee set up to be a task-oriented committee responding to specific commissions from [the Department of Health and Social Care]”.⁵⁰ This meant that its “scope to work with other groups was relatively limited”.⁵¹ Professor Barclay also said:
“With hindsight, I realise I had assumed, did not know, whether other groups were discussing … matters elsewhere. The way the committees were run we knew what we had been asked but I did not understand how this fitted in the wider picture of the totality of the pandemic response plan.”⁵² |
| 6.32. | For example, each of the following bodies focused on slightly different areas, without a suitable process by which their work could be coordinated outside an emergency:
|
| 6.33. | During an emergency, SAGE worked as the “conductor of the orchestra” of scientists; however, there was no equivalent entity in the period between emergencies.⁵⁸ Professor Horby reflected that an annual joint meeting between the chairs of scientific advisory groups and senior officials:
“may have been useful to review the activities of each committee, assess the overall preparedness landscape and to make sure all the bases with respect to science advice on pandemic preparedness were covered by the work of the committees”.⁵⁹ |
| 6.34. | SAGE, in the strictest sense, is a ‘response entity’. It provides COBR (the UK government’s national crisis management centre for responding to whole-system civil emergencies) with scientific advice at the UK level and interprets complex or uncertain scientific evidence in a non-technical form.⁶⁰ It is usually convened only in response to a specific emergency. There was no equivalent mechanism for facilitating rigorous scientific debate about how best to prepare for, and build resilience to, such emergencies. There was no entity that coordinated scientific and other advice on preparedness and resilience in between emergencies. |
| 6.35. | The December 2021 Code of Practice for Scientific Advisory Committees and Councils may provide part of the solution to build an effective scientific advisory system, that is:
“one that collaborates widely to deliver advice that takes account of the wider science system and is integrated and coordinated with other parts of it. |
Timing of advice
| 6.36. | The current system was not organised so that key policies were considered in advance of a pandemic (as discussed in Chapter 4: An effective strategy). This is an acknowledgement of a major flaw in the UK’s architecture of preparedness. Professor Whitty told the Inquiry:
“I would have thought it would be very surprising, without this being requested by a senior politician, or similar, that a scientific committee would venture, |
| 6.37. | There was a fundamental difference between the environment in which politicians sought expert advice during an emergency, and the environment in between emergencies. Professor Whitty expressed frustration with the need to catch the interest of decision-makers in between emergencies:
“In an emergency everybody is clamouring for science advice … Between emergencies you have to kind of elbow your way in. So it’s the ability to actually engage all the way through the system between emergencies, that I think is the big risk.”⁶³ |
| 6.38. | The Inquiry agrees that this is a risk. An appropriate range of expert advice on preparedness, resilience and potential responses should be provided to and considered by ministers before emergencies, when they have more time for proper consideration. This would allow the advice and the possible options for decision-makers to be better scrutinised and challenged. |
‘Groupthink’
| 6.39. | When asked to identify what might have caused some of the flawed thinking behind the UK’s pandemic planning and preparedness, and therefore the advice offered, many witnesses who gave evidence to the Inquiry blamed ‘groupthink’. This is a phenomenon by which people in a group tend to think about the same things in the same way. |
| 6.40. | There were witnesses who explicitly attributed at least some blame for the UK’s lack of pandemic preparedness on ‘groupthink’. They included: David Cameron MP (Prime Minister from May 2010 to July 2016), Clara Swinson (Director General for Global and Public Health at the Department of Health and Social Care from November 2016 and Chair of the Pandemic Influenza Preparedness Programme Board from 2017 to 2022), Sir Oliver Letwin, George Osborne MP (Chancellor of the Exchequer from May 2010 to July 2016), Professor Davies, Jeremy Hunt MP (Secretary of State for Health and Social Care from September 2012 to July 2018), Professor Whitty, Rosemary Gallagher (Professional Lead for Infection Prevention and Control at the Royal College of Nursing from July 2009), Dr Richard Horton (Editor-in-Chief of The Lancet from 1995) and the Institute of Civil Protection and Emergency Management.⁶⁴ |
| 6.41. | Others, while not explicitly attributing blame to ‘groupthink’, nonetheless agreed that it was a risk that needed to be mitigated. These included Dr Stuart Wainwright (Director of the Government Office for Science from December 2019 to June 2023), Professor Walport, Professor Vallance and Mr Gove.⁶⁵ |
| 6.42. | Two witnesses, Professor Dame Jenny Harries (Chief Executive of the UK Health Security Agency from April 2021) and Dr Claas Kirchhelle, expert witness on public health structures (see Appendix 1: The background to this module and the Inquiry’s methodology), explicitly rejected the idea that ‘groupthink’ was a phenomenon that negatively impacted upon the UK’s pandemic preparedness.⁶⁶ |
| 6.43. | On its own, ‘groupthink’ is simply a description of an outcome. It is necessary to understand how and why it happens and what can be done to remedy it. The dynamics of being part of a group may explicitly or implicitly encourage consensus and discourage internal challenge to consider alternatives. This may result in irrational or poor decision-making. However, consensus by itself is not necessarily a bad thing, provided there is adequate discussion before a consensus is reached and provided it remains open to being challenged. |
| 6.44. | The 2018 UK Biological Security Strategy, published by the UK government and referring to work by the UK government and devolved administrations, set out how the UK was protected from significant biological risks.⁶⁷ It asserted that the UK was “globally renowned” for the quality of its preparedness planning and stated that the UK had “world-leading capabilities” to address significant biological risks, such as disease outbreaks.⁶⁸ It emphasised that the UK government’s response to a disease outbreak had to be underpinned by “scientific capabilities and capacity” and stated that the UK was “well served” by a “swift, scalable and comprehensive response system that is flexible between risks and able to cope with new risks as they emerge”.⁶⁹ |
| 6.45. | The Global Health Security Index was created by Harvard University and adopted by the World Health Organization.⁷⁰ In the 2019 Global Health Security Index, the UK came second overall and first in the category of “Rapid Response to and mitigation of the spread of an epidemic”.⁷¹ Professor Mark Woolhouse, Professor of Infectious Disease Epidemiology at the University of Edinburgh, said of this index that there was a risk of complacency and that “it proved a very poor indicator of outcomes in the face of an actual pandemic”.⁷² While global indexes such as this can be helpful, they also have the potential to give countries a misplaced confidence that they are objectively or comparatively well prepared and therefore less vulnerable to infectious disease outbreaks. |
| 6.46. | These documents may explain, however, some of the assurances that Matt Hancock MP, Secretary of State for Health and Social Care from July 2018 to June 2021, received. He told the Inquiry that he was “assured that the UK was one of the best placed countries in the world for responding to a pandemic”.⁷³ The UK had been acknowledged as being among the global leaders in pandemic preparedness, including by the World Health Organization, which Mr Hancock (among others) regarded as an “authoritative source”.⁷⁴ |
| 6.47. | Again, when coronavirus (Covid-19) first emerged, Mr Hancock was “repeatedly reassured” by Public Health England that the risk to the UK population was assessed as very low and he was “not to worry”.⁷⁵ Even at the end of 2020, Public Health England reassured him that the UK was “well prepared” and that “diagnosing, handling and dealing with the case of finding and then the treatment and the specialist centres [was] all set up”.⁷⁶ However, the advice offered to ministers and international bodies may well have been affected by a degree of ‘groupthink’ on pandemic preparedness. |
| 6.48. | There were three important areas on which it appeared to the Inquiry that a consensus had been reached between the Cabinet Office, the Department of Health and Social Care and the devolved administrations – and yet the consensus was wrong. These areas were:
|
| 6.49. | As has been explored earlier in this Report, preparations had been made in the sense that there was a High Consequence Infectious Diseases Programme, but this was only for an outbreak on a small scale (as discussed in Chapter 5: Learning from experience). Duncan Selbie, Chief Executive of Public Health England from July 2012 to August 2020, explained that Public Health England only ever planned for numbers in the few hundreds and that there had never been any discussion with the Secretary of State or anyone else about the need for a mass response before the Covid-19 pandemic.⁷⁷ This was notwithstanding that it was Public Health England’s stated remit to be the expert national public health agency whose first function was to fulfil the Secretary of State for Health and Social Care’s duty to protect the public from infectious diseases and to be responsible for providing the national infrastructure for health protection, including the investigation and management of outbreaks of infectious diseases.⁷⁸ |
| 6.50. | The failure to think adequately about these issues, in advance of the pandemic, does appear to the Inquiry to be, at least in part, the result of ‘groupthink’. Either no one had thought about them, or no one was able to cause a sufficient number of others within the system to think and do something about them – a combination of ‘groupthink’ and a failure to challenge the consensus proactively. |
| 6.51. | It is important not to locate this ‘groupthink’ exclusively within, or emanating from, the expert groups that advised the UK government about preparedness. This was a systemic flaw. That is not to say that no one bears responsibility: it applied to officials, experts and ministers alike. Everyone involved with pandemic preparedness bears some responsibility, but it is principally those who led the organisations responsible for emergency preparedness, resilience and response who were at fault. |
Understanding and challenging advice
| 6.52. | The scientific advice received by the UK government – and consequently by the devolved administrations which relied, in between emergencies, on the same advice – was not subject to sufficient external challenge by either ministers or officials. There was no institutional guard against the risks of conventional wisdom becoming embedded in the institutions responsible for emergency preparedness and resilience. Ministers and officials concerned with emergency preparedness, resilience and response should have a better understanding of this specialist field, not just during emergencies but also in between them.⁷⁹ They must immerse themselves in the topic, understand it and ask questions about it. There were a great number of ministers who could have done more by asking questions. Mr Hunt accepted that “collectively we didn’t put anything like the time and effort and energy” into understanding the dangers of pathogens or challenging the consensus.⁸⁰ The Inquiry agrees. |
| 6.53. | Mr Hunt did, however, provide an excellent example of the value of ministerial challenge. He gave an account of his involvement in Exercise Cygnus, a 2016 cross- government exercise to test the UK’s response to a serious influenza pandemic. Mr Hunt recalled being asked, during the course of the exercise, to sanction the emptying of all intensive care beds in the country in order, it was said, to save more lives.⁸¹ This was called “population triage”.⁸² He said: “Rightly or wrongly … I wasn’t prepared to do it.”⁸³ As a result of his decision, entirely new protocols were developed on how those decisions ought to be made.⁸⁴ This extreme example demonstrates how, by exposing a minister to the realities of emergency preparedness, resilience and response, an entirely fresh perspective was gained. This was by virtue of, rather than in spite of, his lack of expertise. Mr Hunt could bring a new perspective and consider a countervailing opinion – namely, his view that the Secretary of State for Health and Social Care was not usually in the best position to make such a decision.⁸⁵ |
| 6.54. | Ministers should also be aware of the fact that they may be presented with uncertainty, and experts should be prepared to present it. An integral part of any advice is its inherent uncertainty. The advice of experts is no different. If a minister is to challenge effectively, those who provide advice to ministers should ensure that they communicate this uncertainty. There is no single, standard way to express this when presenting evidence or advice to policy-makers and the public.⁸⁶ Many of the scientific advisory groups provided advice to decision-makers as a “consensus” view.⁸⁷ Both Professors Vallance and Whitty suggested in respect of SAGE that the policy-makers were usually presented with a consensus view that articulated a range of possibilities and described uncertainties.⁸⁸ Professor Whitty told the Inquiry that for policy-makers to be confronted with several, competing scientific views, from which they are expected to choose “in the heat of an emergency”, would be unhelpful.⁸⁹ |
| 6.55. | This may be true during an emergency, but the purpose of preparedness is to allow policy-makers to consider and interrogate policies in advance. The purpose of presenting ministers in advance of a pandemic with a range of options, each with scientific evidence and uncertainty of varying degrees, is to allow them to choose the most appropriate response when the crisis happens. This is necessarily a value judgement – underlining the importance of political leaders making the ultimate decisions. That is not to say that the system will prepare for only one response to the exclusion of others, but it does cause those within the system to think and work out, prior to an emergency, which options are backed up by the best evidence. |
| 6.56. | Mr Gove noted that politicians sought certainty where it otherwise might not exist, and that there needed to be greater discussion about diversity of opinion:
“[W]e seek certainty but it’s often elusive, and it would be better if politicians and decision-makers were to say, ‘Tell me about the debate, what is the lead option within the academic community here, but what also are the alternatives?’”⁹⁰ |
| 6.57. | Mr Hunt similarly told the Inquiry:
“When I was Foreign Secretary I discovered that my predecessor William Hague had instructed his officials, as Foreign Secretary, that any time there was a disagreement … he wanted to be told about the disagreement.”⁹¹ |
| 6.58. | It is the Inquiry’s view that ‘tell me about the debate’ should be at the heart of what ministers ask of advisers when determining policy on preparedness and resilience. It is a minister’s duty to interrogate the advice and get to the bottom of issues before making an informed decision. |
| 6.59. | The aim should be to end the culture of consensus in which orthodoxy becomes entrenched. Ministers should have access to the full range of opinion or exposure to the uncertainties in the opinions that they are given, and they should ask the important questions. The system of preparedness and resilience should be institutionally subject to challenge. |
The use of red teams
| 6.60. | The essential antidote to ‘groupthink’ is external scrutiny, oversight and challenge to the prevailing institutions involved with pandemic preparedness. One solution to injecting an external perspective into advice and decision-making within government is by way of ‘red teams’, a solution that found favour with many witnesses.⁹² Red teams are groups of people external to the advisory and decision-making structures involved in developing policies, strategies and plans.⁹³ |
| 6.61. | They are valuable tools for two main reasons.⁹⁴ Firstly, their independence from those institutional structures affords them a fresh perspective, enabling them objectively to review the thinking of others and identify cognitive biases that can lead to errors of judgement.⁹⁵ They are less susceptible to any ‘groupthink’, optimism bias, received wisdom or assumed orthodoxy that can grow within those institutions over time. Secondly, their independence makes them better placed to ask difficult questions and challenge biases, without the defensiveness or fear of personal or professional repercussions that can exist among colleagues working within the same institution.⁹⁶ |
| 6.62. | The distinct structure of independent red teams makes them well suited to carrying out a number of different roles to help improve decision-making, such as:
|
| 6.63. | It is generally recommended practice that red teams include a diverse membership of experts and non-experts.⁹⁸ A red team will need some members who are experts in the subject matter being considered in order to understand the material. However, it is also important to include non-expert members who do not know the specific topic in any detail but who are skilled at analytical and critical thinking more generally. This ensures that as broad and incisive a challenge as possible can be made to the advice or decision-making under scrutiny and also guards against the risk of cognitive biases, even within the red team itself. |
| 6.64. | Red teams are not a new idea within government or industry. They are perhaps most well established as a tool within the military and defence establishment, with the Ministry of Defence having published guidance on red teams as far back as 2010.⁹⁹ They were also recommended as a helpful technique for more general risk management in the 2011 Blackett Review of High Impact Low Probability Risks, a review led by the Government Chief Scientific Adviser, which considered how the UK government could best identify, assess, communicate and quantify the inherent uncertainty in high-impact, low-probability risks.¹⁰⁰ Expert groups resembling some of the attributes of red teams were involved in the development of the 2014 and 2016 National Risk Assessments and the 2019 National Security Risk Assessment.¹⁰¹ Indeed, some of the risk assessment documents expressly refer to them as “challenge groups”.¹⁰² However, there was also evidence that some of these groups, such as the Behavioural Science Expert Group, had a narrow commissioning remit and that its members had little say in what they examined.¹⁰³ This would suggest that they may have suffered from the problems of commissioning already examined above in relation to scientific advisory groups. There was also little evidence to suggest that red teams were in regular use across the full range of emergency preparedness activity by the UK government, beyond risk assessment, or at all by the devolved administrations. |
| 6.65. | The Inquiry is aware that The UK Government Resilience Framework from December 2022 expressed an ambition to create a risk assessment process “which readily invites external challenge from experts, academia, industry and the international risk community”, and that its December 2023 Implementation Update announced a “systematic expert advisory programme” to ensure constructive challenge within the risk assessment process from “the widest possible pool of external expertise”.¹⁰⁴ This suggests that the UK government has identified the problem that needs to be solved. However, this is still too narrow an approach, restricted to risk assessment and not other aspects of emergency preparedness, particularly strategy, planning and the provision of advice. |
| 6.66. | Red teams should be used far more regularly and systematically across government advisory and decision-making structures relating to emergency preparedness and their views conveyed to ministers. In this way, ministers, rather than an internal consensus, will determine emergency preparedness, resilience and response policy. Governments and their institutions should be open to potentially unconventional thinking. The use of red teams should also stimulate a change in culture, as it will be known that decisions may have to be justified in a ‘red teaming’ exercise. Access to a wide range of high-quality, competing advice and regular, external, independent input will make the system better equipped to prepare for and build resilience to a pandemic in the future.¹⁰⁵ Red teams should become an integral part of the architecture of building resilience in the UK. |
Recommendation 9: Regular use of red teams
The governments of the UK, Scotland, Wales and Northern Ireland should each introduce the use of red teams in the Civil Service to scrutinise and challenge the principles, evidence, policies and advice relating to preparedness for and resilience to whole-system civil emergencies. The red teams should be brought in from outside of government and the Civil Service.
A new approach
| 6.67. | The earlier chapters of this Report reveal the many ways in which the UK government and devolved administrations’ systems of emergency preparedness, resilience and response failed. The ways in which risk was assessed, strategy designed and advice provided were flawed. The institutions, structures and systems of the UK that were in charge of preparedness and resilience were overly complex and not properly focused. Lessons from past epidemics and exercises were not properly heeded and actions were not implemented. The involvement of the voluntary sector in preparedness and resilience varied across the UK. Although Wales fared better in this respect than elsewhere in the UK, there was generally too little involvement in the planning process of local bodies and officials, such as directors of public health and groups from the voluntary sector.106 |
| 6.68. | There was no single, permanent body that was responsible for identifying these flaws and “bringing together a critical mass of people who are concerned with the same overall problem, of pandemic[s] … to provide the challenge and the independence and the foresight into the system”.107 |
| 6.69. | The Inquiry concludes that there must be a fundamentally new approach to pandemic and whole-system civil emergency preparedness and resilience. |
A single forum for preparedness and resilience
| 6.70. | The Inquiry considers that the solution to many of the problems identified is the creation of a single forum or institution that stands back from the numerous expert advisory groups and ensures that the UK government and devolved administrations have access to a consolidated resource of strategic advice that is understood and challenged where appropriate. |
| 6.71. | This forum or institution would bring together the wide-ranging areas of technical and specialist expertise involved in preparing the UK, its institutions and systems for the many and varied challenges of pandemics and whole-system civil emergencies. This would thereby produce a coherent understanding and analysis of any given risks, the range of potential responses, the development of appropriate plans and their effective implementation. The interim report of the independent Standing Committee on Pandemic Preparedness established by the Scottish Government included, as one of its key recommendations, the creation of a Centre of Pandemic Preparedness in Scotland.108 This should be part of a UK-wide endeavour. |
| 6.72. | As Professor Whitty told the Inquiry:
“The integration of different aspects of technical advice is one of the more complex in Government … It is, however, not within the expertise, nor is it the role, of [various scientists] to give advice on the wider social, economic, fiscal and political issues elected political leaders need to balance.”109 He acknowledged that it was difficult to be more “radical” unless the whole system was operating together, but this only occurred during emergencies – by which time it was too late.110 |
| 6.73. | During the response to an emergency, SAGE was responsible for “more radical thinking than occurred between emergencies”, but between emergencies there was no entity that considered whether the right advice was being sought from the right sources, or what the advice meant in its totality.111 The system was simply not designed to “inject radicalism” into policy.112 The establishment of the UK Health Security Agency’s Centre for Pandemic Preparedness does not address these issues – focused, as it is, only on the health protection system.113 |
| 6.74. | A new body could also be responsible for an independent assessment of the UK’s system of emergency preparedness and resilience. It currently operates under a model of self-assessment. There is no central authority within or external to the UK government and devolved administrations responsible for assessing whether standards of preparedness and resilience are met (see Chapter 2: The system – institutions, structures and leadership). |
| 6.75. | The Civil Contingencies Secretariat undertook a wide range of activities aimed at understanding and enhancing preparedness.114 It was responsible for producing guidance to accompany the Civil Contingencies Act 2004.115 It did not, however, have a role equivalent to inspecting or otherwise assessing the extent of preparedness and resilience.116 It did not, in fact, know the state of preparedness and resilience of UK government departments. |
| 6.76. | The Civil Contingencies Secretariat issued a number of guidance documents for local responders, including the National Resilience Standards for local resilience forums and relevant local responder organisations, first published in July 2018, and updated in December 2019 and again in August 2020.117 However, compliance with these standards was only voluntary and they were incomplete.118 Standards relating specifically to pandemic influenza were first published only in December 2019.119 This was too late for them to make any practical difference to preparedness for and resilience to the Covid-19 pandemic. The standards have not been updated since August 2020 and still only refer to pandemic influenza as opposed to pandemics more generally.120 |
| 6.77. | A National Resilience Capabilities Survey for England was discontinued after 2017 because it did not serve its intended purpose.121 However, the Civil Contingencies Secretariat did not replace it with a clear successor.122 This means that the UK government’s knowledge was generally limited to local responders’ voluntary self- assessment, anecdotal information and the experience shared by local responders in the course of working with the Civil Contingencies Secretariat and the Resilience and Emergencies Division of the Ministry of Housing, Communities and Local Government.123 |
| 6.78. | A similar system of self-assessment and an absence of compulsory standards existed in Scotland, Wales and Northern Ireland at both a local responder and central government level.124 The devolved administrations did not, in fact, objectively know the state of their preparedness and resilience. There was no central authority in either the UK or devolved administrations that had this information. |
| 6.79. | Oliver Dowden MP, Parliamentary Secretary to the Cabinet Office from January 2018 to July 2019 and Minister for the Cabinet Office from July 2019 to February 2020, told the Inquiry that one of the challenges for the Cabinet Office was to know “where to delineate the line between the individual government department and cross-government action”.125 He added:
“What is not a good use of resource for us is to constantly second-guess things that are clearly allocated to individual government departments.”126 |
| 6.80. | The risks of organisations “marking their own homework” were borne out by flaws in preparedness, as described in this Report.127 It is clear to the Inquiry that self-assessment was an inadequate model. |
| 6.81. | The Inquiry is not persuaded that the system of preparedness and resilience has, following the pandemic, been reformed or is capable of the necessary reform on its own. This is for three reasons. |
| 6.82. | Firstly, many – including those with important roles within the system of preparedness and resilience – either were unable to identify and describe the flaws in unambiguous terms or described flaws that were apparent but had not been acted upon (at all or sufficiently) prior to the pandemic. The Inquiry received a number of examples, some of which have been discussed earlier in this Report:
|
| 6.83. | Such an inability – even after the pandemic – to articulate in clear terms either what had happened or what had failed to happen suggests to the Inquiry that the system of assuring preparedness was, and remains, seriously inadequate. The system is either oblivious to or unwilling to admit some of its own flaws. These problems need to be addressed – if the problems cannot be properly defined, articulated and accepted, they cannot be solved. |
| 6.84. | Secondly, a significant quantity of guidance and planning documents were produced by the institutions responsible for preparedness and resilience. However, they were often lengthy, not updated, and cross-referred to a profusion of other lengthy documents that had also not been updated:
|
| 6.85. | Sir Oliver Letwin told the Inquiry that the longer the document, the less useful it was. As he put it, “Volume is usually in inverse proportion to effectiveness.”140 The Inquiry agrees. |
| 6.86. | Two important documents created after the pandemic – the 2022 The UK Government Resilience Framework and the 2023 UK Biological Security Strategy – are unclear about how preparedness and resilience will be improved in the future. The 2022 The UK Government Resilience Framework committed – but only in vague terms – the UK government to:
|
| 6.87. | The 2023 UK Biological Security Strategy contains jargon and management speak, which too often infiltrates government documents of this kind. Its language is opaque and does little to enlighten the reader. It is replete with references to ‘scope/scoping’ (10 times), ‘facilitate/facilitating’ (9 times), ‘developing’ (26 times) and ‘deliver/ delivering’ (29 times).142 For example, in its “High Level Strategy Implementation Plan”, there is a “commitment” to:
“Scope a new, agile procurement mechanism for commissioning [science and technology] from UK academia and industry, using simplified processes to stimulate innovation.”143 Language such as this obscures communication rather than enlightens the reader. |
| 6.88. | Language is important and its impact on preparedness and resilience should not be underestimated. These documents should set out in clear terms what is going to happen and by when. Otherwise, there is no means of assessing whether the government has achieved what it has set out to do. |
| 6.89. | Documents should be made clear, precise and concise so that they are capable of being read and understood by all involved in preparedness and resilience. One of the tasks of assurance is to check that this is being done. The failure to simplify and consolidate planning, guidance and strategy documents is symptomatic of a fundamental problem with the institutions in the UK that retain responsibility for whole-system civil emergencies. This is demonstrated by both the documentary material and the evidence to the Inquiry, described above. |
| 6.90. | Sir Oliver Letwin told the Inquiry that even rewriting these kinds of documents was not enough to improve the system:
“[I]f it happens without a well organised central team, under a head of resilience who has direct access to the Prime Minister and is parallel to the National Security Adviser, it will be wasted effort, because it will just dissipate through endless consultations and committees all round Whitehall and the simplification exercise will become a complication exercise.”144 |
| 6.91. | Thirdly, no one person or body – at ministerial level or among officials and advisers – was responsible for independently assessing the adequacy, efficiency and effectiveness of the decision-making and advisory structures across the UK, asking what they all did and whether they were doing the right things. |
| 6.92. | No one asked whether there were any gaps, whether there was an adequate assessment of risk or the design of an effective strategy, whether there were too many long and out-of-date documents and, critically, whether the skills, technology and infrastructure were in place that would make the UK government and devolved administrations practically prepared for a whole-system civil emergency. As a consequence, no one really knew, in advance, the UK’s levels of preparedness for or resilience to the kind of pandemic that struck in January 2020. |
The role of the new body
| 6.93. | The Inquiry considers that the only answer to the extensive problems in the approach of the UK government and devolved administrations to preparedness and resilience is to create an independent body with expertise in whole-system civil emergencies. The role of the new body would be to:
|
| 6.94. | A new body that is able to bring together the various types of advice on preparedness and resilience will help political leaders to think about solving problems strategically and for the long term. Political leaders are in a unique position, if they choose, to bring critical thinking and a fresh perspective to a problem, and are well placed to ask difficult questions of the experts on behalf of the public they serve.145 |
| 6.95. | In advance of the pandemic, these questions might have included, for example: What is the proportionate response to a disease that is likely to kill 100 members of the UK population? What if it were 1,000, 10,000, 100,000 or 1 million people? Is there a tipping point at which certain non-pharmaceutical interventions become an inevitability? If so, what is that tipping point? What happens if the disease affects only a particular section of the population? Is there a point at which the collateral impact of interventions may not be worth the price, because not enough lives are saved compared with the societal and economic costs of the interventions? |
| 6.96. | These are difficult questions to answer. The Inquiry does not consider the political leaders in the UK government and devolved administrations are adequately served at present on how they should be answered for the long term. The limits of the current system are plain. |
| 6.97. | Professor David Alexander and Bruce Mann, expert witnesses on risk management and resilience (see Appendix 1: The background to this module and the Inquiry’s methodology), suggested that there should be a “single, integrated and professional civil protection system capable of providing an effective whole system, whole of society response to emergencies on a catastrophic scale”.146 |
| 6.98. | The Inquiry agrees and considers that ministers should be advised by this body on strategy, across a range of policy areas relevant to preparedness and resilience, for the long term. This should coalesce to build a coherent picture that puts decision- makers in the best possible position to see clearly the evidence for, and practicability of, policy and to apply value judgements when making decisions. |
| 6.99. | There ought to be a means by which those who, it is reasonably anticipated, would be involved in SAGE and other expert groups for a future pandemic – or who have been involved in a past disease outbreak – can systematically share their experience and think about and contribute to pandemic preparedness in advance of the emergency. This could then be considered alongside broader policy on emergency preparedness, such as economic strategy, the impact on vulnerable people and the practical capabilities within the system. |
| 6.100. | The Inquiry therefore recommends the creation of a specialised, independent, UK-wide body for civil emergencies, dealing with both preparedness and resilience, and accountable to the ministers responsible for whole-system civil emergencies. The new body should provide the UK government and devolved administrations with expert strategic advice on how best to prepare for and build resilience to whole-system civil emergencies and on potential responses. This will enable the executive branches of government to focus on ensuring that the infrastructure is in place to make the plans effective when an emergency arises. |
| 6.101. | The Inquiry considers that the new body should be established in statute with a UK-wide remit to give it independence. This is so that it can stand back and provide political leaders with a critical, objective and impartial opinion on the state of preparedness and resilience and how this may be improved. Political leaders will require courage to think strategically about how best to approach the risks that the UK will face in the future. This new body would help them in that pursuit. |
| 6.102. | The body should be sponsored jointly by the relevant ministers in the UK government and each of the devolved administrations, to ensure that it has the authority and access necessary to consider issues on a UK-wide basis. Each of these ministers should be empowered to commission advice from the new body on any aspects of emergency planning, preparedness and resilience within their ministerial competence. The new body’s management board should also include non-executive directors to represent each of the devolved nations and their appointment should require the consent of the sponsoring minister in the relevant devolved administration. The Inquiry believes that this will bring regular strategic thinking on preparedness for and resilience to civil emergencies to the centre of government. |
| 6.103. | Finally, the new body could assist in ensuring that the public is consulted, engaged with and informed about how governments intend to respond in the event of an emergency. Members of the public are the ones who will suffer in a whole-system civil emergency and as a result of the response to it. If the public is better informed about what the risks are, as well as the potential consequences of not mitigating the risks, it will more likely accept the allocation of precious resources on an appropriate ‘insurance policy’. |
| 6.104. | Most members of the public understand the importance of military defence and security to the country. Having experienced the devastating consequences of the Covid-19 pandemic, they should also now understand the importance of building resilience to and preparedness for whole-system civil emergencies, including pandemics. As put by Professor Vallance:
“You need an army in a country and you don’t turn round after 20 years and say, ‘What a waste of money that was, we haven’t had a war’.”147 Professor Vallance considered it to be the same with health security. The Inquiry agrees. |
Recommendation 10: A UK-wide independent statutory body for whole-system civil emergency preparedness and resilience
The UK government should, in consultation with the devolved administrations, create a statutory independent body for whole-system civil emergency preparedness and resilience.
The new body should be given responsibility for:
- providing independent, strategic advice to the UK government and devolved administrations on their planning for, preparedness for and building resilience to whole-system civil emergencies;
- consulting with the voluntary, community and social enterprise sector at a national and local level and directors of public health on the protection of vulnerable people in whole-system civil emergencies;
- assessing the state of planning for, preparedness for and resilience to whole-system civil emergencies across the UK; and
- making recommendations on the capacity and capabilities that will be required to prepare for and build resilience to whole-system civil emergencies.
As an interim measure, the new body should be established on a non-statutory basis within 12 months of this Report, so that it may begin its work in advance of legislation being passed.
- See Oliver Letwin 20 June 2023 8/20-24; Michael Gove 13 July 2023 114/18-19
- Michael Gove 13 July 2023 114/19-25
- Oliver Letwin 20 June 2023 12/10-13/11
- Oliver Letwin 20 June 2023 13/15-21
- Denis McMahon 6 July 2023 103/6-13
- Mark Walport 21 June 2023 10/1-21
- INQ000147810_0008 para 22; see also Patrick Vallance 22 June 2023 137/20-21
- INQ000147810_0008 para 22; Patrick Vallance 22 June 2023 137/22-138/1
- INQ000147810_0008 para 22; Patrick Vallance 22 June 2023 138/2-8
- INQ000147810_0008 para 22; Patrick Vallance 22 June 2023 138/9-11
- Patrick Vallance 22 June 2023 138/11-13
- INQ000147707_0033 paras 86, 88
- INQ000184638_0011-0012 para 2.12
- INQ000147810_0005 para 12
- INQ000148419_0007 para 3.17
- INQ000183413_0003 para 8
- INQ000184636_0009-0010
- INQ000184851_0008 para 28
- Mark Walport 21 June 2023 20/25-21/22
- Patrick Vallance 22 June 2023 136/23-137/3; Jim McMenamin 22 June 2023 193/14-18
- INQ000119020_0008 para 28
- INQ000119020_0008 para 28
- INQ000119020_0008 para 31
- INQ000142125_0005
- INQ000207293_0005 para 2.7
- Christopher Whitty 22 June 2023 72/21-73/10
- Christopher Whitty 22 June 2023 73/11-24; Patrick Vallance 22 June 2023 139/2-19
- INQ000119020_0009 para 33
- INQ000147810_0005 para 11
- INQ000184851_0004, 0019 paras 13-14, 80; INQ000148419_0005, 0007 paras 3.11-3.12, 3.17
- INQ000184851_0019 para 80
- INQ000148419_0007 para 3.17; INQ000119020_0007 para 24; INQ000184851_0011-0012 para 45
- Mark Walport 21 June 2023 21/7-22
- INQ000062443_0004 para 24
- Christopher Whitty 22 June 2023 89/18-90/17
- INQ000184638_0026 para 3.50
- INQ000184637_0010, 0011 paras 7.6-7.7, 7.12; Sally Davies 20 June 2023 168/20-169/9
- INQ000184637_0010 para 7.7; see also INQ000148419_0010, 0013 paras 4.4(f), 5.8
- INQ000148419_0010, 0013 paras 4.4(f), 5.8
- INQ000147707_0033 para 88
- INQ000147810_0033-0034 para 105
- Patrick Vallance 22 June 2023 151/5-9
- Patrick Vallance 22 June 2023 151/16-152/2; see also INQ000148419_0010 para 4.4(f)
- Code of Practice for Scientific Advisory Committees and Councils: CoPSAC 2021, Government Office for Science, Updated 14 December 2021, section 2.4.1 (https://www.gov.uk/government/publications/scientific-advisory-committees-code-of-practice/code-of-practice-for-scientific-advisory-committees-and-councils-copsac-2021; INQ000101646)
- Jimmy Whitworth 14 June 2023 137/12-20
- INQ000147710_0011 para 9.6
- INQ000147710_0011 para 9.6
- INQ000184851_0014 para 57
- INQ000119020_0005 para 17
- INQ000184851_0015 para 60
- INQ000184851_0015 para 60
- INQ000119020_0007 para 24
- Jimmy Whitworth 14 June 2023 137/23-138/1
- INQ000207293_0004 para 2.6
- Jimmy Whitworth 14 June 2023 138/2-4
- Jimmy Whitworth 14 June 2023 138/5-6
- INQ000196611_0021 para 48
- Christopher Whitty 22 June 2023 81/13-15
- INQ000184851_0016 para 63
- INQ000099517_0010 para 2.22
- Code of Practice for Scientific Advisory Committees and Councils: CoPSAC 2021, Government Office for Science, updated 14 December 2021, section 2.4.1 (https://www.gov.uk/government/publications/scientific-advisory-committees-code-of-practice/code-of-practice-for-scientific-advisory-committees-and-councils-copsac-2021; INQ000101646)
- Christopher Whitty 22 June 2023 83/8-13
- Christopher Whitty 22 June 2023 117/10-16
- David Cameron 19 June 2023 7/23, 22/2-3, 56/2; Clara Swinson 19 June 2023 166/25-168/16; Oliver Letwin 20 June 2023 31/17-36/1; INQ000177810_0003, 0014 paras 8, 47-48; George Osborne 20 June 2023 67/18-25; Sally Davies 20 June 2023 146/8-18, 157/2-9; Jeremy Hunt 21 June 2023 165/22-170/1; INQ000177796_0007-0009, 0015 paras 25-29, 38, 70; Christopher Whitty 22 June 2023 77/5-21; Rosemary Gallagher 26 June 2023 71/9-20; Richard Horton 13 July 2023 68/19-69/12, 88/13-25; INQ000148421_0002 para 5; INQ000187305_0008, 0013 paras 39, 65, 69
- INQ000148406_0014 para 21; Mark Walport 21 June 2023 24/3-25/2; INQ000147810_0020-0023 paras 63-72; Michael Gove 13 July 2023 116/13-117/10
- Jenny Harries 26 June 2023 169/4-21; Claas Kirchhelle 10 July 2023 100/12-102/14
- UK Biological Security Strategy, HM Government, July 2018, p15 (https://assets.publishing.service.gov.uk/media/5b5b3ce5e5274a3fe478c3bf/2018_UK_Biological_Security_Strategy.pdf; INQ000142130); Mark Walport 21 June 2023 61/4-62/18
- UK Biological Security Strategy, HM Government, July 2018, p13 (https://assets.publishing.service.gov.uk/media/5b5b3ce5e5274a3fe478c3bf/2018_UK_Biological_Security_Strategy.pdf; INQ000142130)
- UK Biological Security Strategy, HM Government, July 2018, pp7, 26 (https://assets.publishing.service.gov.uk/media/5b5b3ce5e5274a3fe478c3bf/2018_UK_Biological_Security_Strategy.pdf; INQ000142130)
- Jimmy Whitworth 14 June 2023 128/8-15
- Global Health Security Index: Building Collective Action and Accountability, Nuclear Threat Initiative/Johns Hopkins Bloomberg School of Public Health, 2019 (https://www.nti.org/analysis/articles/global-health-security-index/; INQ000149103). The UK did less well in other categories of the Global Health Security Index. For example, it came 11th in ‘Sufficient and robust health system to treat the sick and protect health workers’ and 26th in ‘Overall risk environment and country vulnerability to biological threats’.
- INQ000182616_0003 para 8
- Matt Hancock 27 June 2023 19/17-19
- INQ000181825_0006-0008 paras 23-30
- INQ000181825_0008 para 32
- INQ000181825_0008 para 32
- Duncan Selbie 27 June 2023 136/15-137/5; see also INQ000184639_0016 paras 5.4-5.5
- INQ000090333_0001 para 1
- Michael Gove 13 July 2023 113/21-116/12
- Jeremy Hunt 21 June 2023 166/18-167/2
- Jeremy Hunt 21 June 2023 146/18-147/1
- Jeremy Hunt 21 June 2023 149/11
- Jeremy Hunt 21 June 2023 147/8-12
- Jeremy Hunt 21 June 2023 147/16-25
- Jeremy Hunt 21 June 2023 148/1-24
- INQ000147810_0026 para 78
- INQ000184643_0029, 0049-0050 paras 151, 265; INQ000184638_0016, 0032 paras 3.10, 3.78; Christopher Whitty 22 June 2023 89/3-14
- INQ000147810_0026 para 80; INQ000184639_0019 para 6.5
- INQ000184639_0019 para 6.5
- Michael Gove 13 July 2023 137/11-16
- Jeremy Hunt 21 June 2023 180/6-12
- David Cameron 19 June 2023 21/21-22/9; INQ000177810_0003, 0014 paras 9, 47; Oliver Letwin 20 June 2023 13/22-14/1, 33/21-36/1; INQ000177796_0015-0016 para 70; Jeremy Hunt 21 June 2023 176/9-14; Christopher Whitty 22 June 2023 88/9-20; Matt Hancock 27 June 2023 88/10-13; Jeremy Farrar 29 June 2023 14/14-18/7; Michael Gove 13 July 2023 116/13-117/10; INQ000148402_0019 para 80; INQ000099516_0046 para 190; INQ000185337_0041-0042 paras 171-172
- INQ000372823_0014 para 1.3
- See generally INQ000068403_0063 para 7.2.2; INQ000372823_0013-0019 paras 1.1-1.16
- ‘Groupthink’ is one example of a cognitive bias, which can be described more generally as “a systematic error in thinking that occurs when individuals (and teams) are searching for, processing and interpreting information and which affects the decisions and judgements made on the basis of this information” (INQ000372823_0018-0019 para 1.15).
- Oliver Letwin 20 June 2023 33/21-34/12
- See INQ000068403_0063, para 7.2.2; INQ000372823_0015 para 1.5
- INQ000068403_0063, para 7.2.2; INQ000372823_0071 paras 7.5-7.6
- The first edition was published in February 2010, the second edition was published in March 2013 and the most recent, third, edition was published in October 2021 (see INQ000372823).
- Blackett Review of High Impact Low Probability Risks, Government Office for Science, 2011, p11 (https://assets.publishing.service. gov.uk/media/5a7c901540f0b62aff6c28c0/12-519-blackett-review-high-impact-low-probability-risks.pdf; INQ000055868)
- INQ000147777_0010; INQ000147769_0006; INQ000147768_0005-0006; INQ000147770_0005-0006
- INQ000147769_0006
- INQ000148418_0014 para 2.40
- The UK Government Resilience Framework, HM Government, December 2022, para 20 (https://assets.publishing.service.gov.uk/media/63cff056e90e071ba7b41d54/UKG_Resilience_Framework_FINAL_v2.pdf; INQ000097685); The UK Government Resilience Framework: 2023 Implementation Update, Cabinet Office, 4 December 2023 (https://assets.publishing.service.gov.uk/media/656def711104cf0013fa7498/The_UK_Government_Resilience_Framework_2023_Implementation_Update.pdf; INQ000372824)
- INQ000177810_0003 paras 8-9
- For the lack of recognition and understanding of the potential importance and role of local public health workers, particularly directors of public health, both before and in the early response to the Covid-19 pandemic, see: INQ000183419_0017, 0019, 0021, 0040-0041 paras 107-109, 118, 125-126, 223-230 and Jim McManus 5 July 2023 55/12-59/9. There are approximately 150 directors of public health in England, who are employed by local authorities. In Scotland, there are eight directors of public health, employed by NHS boards. In Wales, there are seven directors of public health, employed by local health boards. In Northern Ireland, there is only one director of public health, who is employed by the Public Health Agency (see Jim McManus 5 July 2023 36/16-38/9). For the general lack of recognition and understanding of the potential importance and role of the voluntary sector, see INQ000182613_0018 para 64; Kevin Fenton 5 July 2023 89/21-90/25. For Wales, see INQ000066503_0013-0014 paras 10-17; INQ000130469_0100-0101 paras 394-397.
- Patrick Vallance 22 June 2023 151/5-9
- INQ000103004_0004 p2
- INQ000184638_0027-0028 paras 3.56, 3.59
- Christopher Whitty 22 June 2023 63/11-17
- Christopher Whitty 22 June 2023 63/15-17, 81/24-82/3
- Christopher Whitty 22 June 2023 77/5-9
- INQ000148429_0159-0160 paras 638-639
- INQ000182612_0007 para 2.10
- INQ000145912_0042-0044 paras 8.27-8.33
- INQ000145733_0007 para 2.19; INQ000182612_0007 para 2.10; INQ000148402_0014 para 56
- INQ000022975; INQ000047333; INQ000023122; see generally INQ000182612_0053-0055 paras 4.72-4.81; INQ000203349_0082-0084 paras 215-220
- INQ000203349_0084-0085 paras 221-223
- See Katharine Hammond 16 June 2023 131/25-135/7
- INQ000023122_0034–0035
- INQ000203349_0087 paras 230-234; INQ000188715_0005 paras 7-9; INQ000188716_0004-0006 paras 13-17
- Katharine Hammond 16 June 2023 137/16-138/14
- See, for example, Report of the Post Implementation Review of the Civil Contingencies Act (2004) (Contingency Planning) Regulations 2005, HM Government, pp7-8, March 2017, paras 15, 19 (https://assets.publishing.service.gov.uk/media/5a82c15340f0b6230269c879/post_implementation_review_civil_contingencies_act__print.pdf; INQ000056230); INQ000182612_0037 para 4.14
- See, for England, Scotland and Wales: INQ000203349_0082-0095 paras 214-251; and for Northern Ireland: Denis McMahon 6 July 2023 16/7-20/16
- Oliver Dowden 21 June 2023 119/6-8
- Oliver Dowden 21 June 2023 121/22-25. See also the evidence of Roger Hargreaves that this is a complex matter of judgement that cannot be found in ‘doctrine’ alone: INQ000182612_0008-0010 paras 2.12-2.18.
- INQ000203349_0093 para 247(f)
- Emma Reed 26 June 2023 40/24-41/2, 41/11-42/9
- Christopher Wormald 19 June 2023 127/19-21
- INQ000184638_0033 para 4.1; INQ000023131_0005
- Caroline Lamb 28 June 2023 118/17-22
- Andrew Goodall 3 July 2023 93/24-95/16; Andrew Goodall 4 July 2023 38/25-40/25, 42/3-43/17
- Andrew Goodall 3 July 2023 93/24-95/16; Andrew Goodall 4 July 2023 38/25-40/25, 42/3-43/17
- INQ000047302_0002 para 3
- Katharine Hammond 16 June 2023 84/11-85/8
- 136 Katharine Hammond 16 June 2023 104/9-108/16, 117/15-118/10; Concept of Operations, Cabinet Office, updated April 2013 (https://assets.publishing.service.gov.uk/media/5a7a44b0ed915d1fb3cd6a5f/CONOPs_incl_revised_chapter_24_Apr-13.pdf; INQ000036475); INQ000055887
- Jim McMenamin 22 June 2023 181/16-21; INQ000101052; INQ000148759; Caroline Lamb 28 June 2023 118/17-22; Jeane Freeman 28 June 2023 135/25-136/5
- INQ000089575; Quentin Sandifer 4 July 2023 96/4-8
- Northern Ireland Health and Social Care Influenza Pandemic Preparedness and Response Guidance, Department of Health, Social Services and Public Safety, January 2013 (http://www.niassembly.gov.uk/globalassets/documents/raise/deposited-papers/2013/dp1089.pdf; INQ000183431); INQ000188750
- Oliver Letwin 20 June 2023 36/5-6
- The UK Government Resilience Framework, HM Government, December 2022, paras 98-100 (https://www.gov.uk/government/publications/the-uk-government-resilience-framework; INQ000097685)
- See, for example, UK Biological Security Strategy, HM Government, June 2023, pp31, 46, 54, paras 41, 86, 107 (https://assets.publishing.service.gov.uk/media/64c0ded51e10bf000e17ceba/UK_Biological_Security_Strategy.pdf; INQ000208910)
- UK Biological Security Strategy, HM Government, June 2023, p10 (https://assets.publishing.service.gov.uk/media/64c0ded51e10bf000e17ceba/UK_Biological_Security_Strategy.pdf; INQ000208910)
- Oliver Letwin 20 June 2023 38/22-39/4
- See Oliver Letwin 20 June 2023 13/15-21
- INQ000203349_0097 para 256
- Patrick Vallance 22 June 2023 159/21-24
Appendix 1: The background to this module and the methodology of the Inquiry
Background
| A1.1. | The Right Honourable Boris Johnson MP, Prime Minister from July 2019 to September 2022, formally established the UK Covid-19 Inquiry in June 2022 to examine preparations for and response to the coronavirus (Covid-19) pandemic in the UK and to learn lessons for the future. In December 2021, he had appointed The Right Honourable the Baroness Hallett DBE, a retired judge of the Court of Appeal, as its Chair. |
| A1.2. | The Inquiry held a public consultation on its draft Terms of Reference in spring 2022. The Inquiry team met over 150 bereaved families across the UK and representatives from many different sectors, such as charities, unions, faith groups, education and healthcare. In total, more than 20,000 responses were received. This feedback shaped Baroness Hallett’s recommendations to the Prime Minister on the Terms of Reference. |
| A1.3. | On 28 June 2022, the Prime Minister issued the final Terms of Reference for the Inquiry, establishing it under the Inquiries Act 2005.1 |
| A1.4. | The Inquiry formally opened on 21 July 2022 to “examine, consider and report on preparations and the response to the pandemic in England, Wales, Scotland and Northern Ireland, up to and including the Inquiry’s formal setting-up date, 28 June 2022”.2 Its Terms of Reference in full are to:
“1. Examine the COVID-19 response and the impact of the pandemic in England, Wales, Scotland and Northern Ireland, and produce a factual narrative account, including:
|
| A1.5. | The Inquiry is investigating the handling of the pandemic in England, Wales, Scotland and Northern Ireland, and this includes reserved and devolved matters. A separate Inquiry is taking place in Scotland, which will evaluate areas where policy was devolved to the Scottish Government, as set out in its Terms of Reference. The UK Inquiry works with the Scottish Inquiry to avoid duplication of work where possible. |
| A1.6. | To ensure a full and focused examination of the wide range of issues covered in the Terms of Reference and to produce regular reports, the Inquiry’s investigation has been divided into sections or ‘modules’. Modules are announced and then opened in sequence, after which gathering of evidence commences and Core Participant applications are considered. Each module has preliminary hearings (at which decisions about the procedure for the conduct of its public hearings are made) and full public hearings where evidence is heard. Details of public hearings are published by the Inquiry.4 |
| A1.7. | The Inquiry’s current active modules are:
Any further investigations will be announced by the Inquiry in due course. |
| A1.8. | As set out in the Terms of Reference, the Inquiry also regards it as critical to its work to listen to and carefully consider the experiences of bereaved families and others who have suffered hardship or loss as a result of the pandemic. The Inquiry will do this in a number of different ways, including through its ‘listening exercise’, Every Story Matters.15 Those aged 18 or older are invited to share as much or as little information as they feel able, without the formality of giving evidence or attending a public hearing. Sharing experiences with the Inquiry will help the understanding of events and their impact, and the development of recommendations that could reduce suffering in the future. Experiences shared with the Inquiry will be analysed and reports will be produced highlighting the themes that emerge. The Inquiry is also undertaking a bespoke and targeted research project, hearing directly from some of the children and young people most affected by the pandemic, to help inform its findings and recommendations.16 |
Module 1
| A1.9. | This Report concerns Module 1, which opened on 21 July 2022, in which the Inquiry examined the topics of preparedness and resilience. The purpose of Module 1 was to assess whether there was proper planning for the pandemic and resilience to the pandemic. It examined the whole system of civil emergencies, including resourcing, risk management and pandemic readiness. |
| A1.10. | As set out in its Outline of Scope, Module 1 considered:
|
| A1.11. | Module 1 focused primarily, though not exclusively, on the period between 11 June 2009 and 21 January 2020, as set out in its List of Issues.18 In summary, the issues examined were:
|
| A1.12. | In accordance with rule 5 of the Inquiry Rules 2006 and the Inquiry’s Core Participant Protocol, the Chair designates a number of Core Participants – individuals, organisations or institutions with a specific interest – in each module.19 Core Participants have enhanced rights in the Inquiry process, including receiving disclosure of documents, being represented, making legal submissions and suggesting lines of enquiry. They are also able to apply to the Inquiry for funding to cover legal and other costs. In Module 1, the Inquiry received more than 100 applications for Core Participant status, and the Chair appointed 28 Core Participants. |
| Name of organisation/individual | Recognised legal representative (at publication) | Date of designation |
|---|---|---|
| Association of Directors of Public Health | Henry Bermingham (Weightmans) | 7 September 2022 |
| Chancellor of the Duchy of Lancaster | Sharanjeet Sidhu (Government Legal Department) | 7 September 2022 |
| Covid-19 Bereaved Families for Justice Cymru | Craig Court (Harding Evans) | 7 September 2022 |
| Covid-19 Bereaved Families for Justice | Elkan Abrahamson (Broudie Jackson Canter) | 7 September 2022 |
| Department for Business and Trade (formerly Department for Business, Energy and Industrial Strategy) | Rebecca Torsello (Government Legal Department) | 7 September 2022 |
| Secretary of State for Health and Social Care | Sarah Wise (Government Legal Department) | 7 September 2022 |
| The Executive Office of Northern Ireland | Joan MacElhatton (Departmental Solicitor’s Office) | 7 September 2022 |
| Government Office for Science | Amir Mughal (Government Legal Department) | 7 September 2022 |
| HM Treasury | Michael Cockings (Government Legal Department) | 7 September 2022 |
| Imperial College London | Paul Ridge (Bindmans) | 7 September 2022 |
| Local Government Association | Thelma Stober (Local Government Association) | 7 September 2022 |
| National Police Chiefs’ Council | Sarah Winfield (MPS Directorate of Legal Services) | 7 September 2022 |
| Department of Health (Northern Ireland) | Sara Erwin (Departmental Solicitor’s Office) | 7 September 2022 |
| NHS England | Alistair Robertson (DAC Beachcroft) | 7 September 2022 |
| NHS National Services Scotland | Morag Shepherd (NHS National Services Scotland) | 7 September 2022 |
| Northern Ireland Covid-19 Bereaved Families for Justice | Conal McGarrity (P.A. Duffy & Co) | 7 September 2022 |
| Office of the Chief Medical Officer | Warrick Olsen (Government Legal Department) | 7 September 2022 |
| Public Health Scotland | Stefano Rinaldi (Central Legal Office) | 7 September 2022 |
| Public Health Wales | Paul Veysey (NHS Wales Shared Services Partnership Legal and Risk Services) | 7 September 2022 |
| Scottish Covid Bereaved | Aamer Anwar (Aamer Anwar & Co) | 7 September 2022 |
| Scottish Ministers | Caroline Beattie (Scottish Government Legal Directorate) | 7 September 2022 |
| Secretary of State for Environment, Food and Rural Affairs | Luke Chattaway (Government Legal Department) | 7 September 2022 |
| Secretary of State for the Home Department | Warrick Olsen (Government Legal Department) | 7 September 2022 |
| UK Health Security Agency | Katrina McCrory (Mills & Reeve) | 7 September 2022 |
| Welsh Government | Stephanie McGarry (Browne Jacobson) | 7 September 2022 |
| Welsh Local Government Association | Thelma Stober (Local Government Association) | 7 September 2022 |
| British Medical Association | Brian Stanton (Innovo Law) | 28 September 2022 |
| Trades Union Congress | Harry Thompson (Thompsons Solicitors) | 28 September 2022 |
| A1.13. | In keeping with its public nature and the Chair’s commitment to conduct the Inquiry in as open and transparent a manner as possible, arrangements were made for the hearings to be accessible to all who wished to follow them. The hearings were broadcast via live stream on the Inquiry’s website or its YouTube channel (where they remain accessible) and members of the public were able to watch the hearings in person.20 |
| A1.14. | The Inquiry’s approach to documents is set out in its Protocol on Documents, which explains key principles for the delivery of documents to the Inquiry, including requests for documents or witness statements pursuant to rule 9 of the Inquiry Rules 2006.21 This should be read with the Inquiry’s Protocol on the Redaction of Documents, which details the approach to the redaction of documents for the purposes of both disclosure to Core Participants and publication.22 In this module, the Inquiry issued more than 200 requests for evidence. It received and considered in excess of 200 witness statements and 100,000 documents, containing over 1 million pages. Of these documents, more than 18,000 were disclosed to Core Participants. Relevant material is published on the Inquiry’s website.23 |
| A1.15. | In accordance with section 18 of the Inquiries Act 2005, the Chair is taking reasonable steps to ensure that members of the public are able to view documents provided to the Inquiry and attend Inquiry hearings.24 All witness statements and documents put into evidence during the course of the hearings have been published on the Inquiry’s website.25 There may be instances, however, where evidence (or parts of it) provided to the Inquiry ought to be excluded from disclosure to the public in order to protect against the risk of harm and damage to the public interest. As a general rule, the Inquiry will disclose all witness statements and documents it considers relevant, and to which restrictions do not apply, to Core Participants prior to the Inquiry’s public hearings. Documents used in the Inquiry’s public hearings or otherwise put in evidence will be published on the Inquiry’s website.26 In the event of there being a valid reason to object to disclosure or publication of such relevant material, an application may be made to the Chair for a restriction order in accordance with section 19 of the Inquiries Act 2005 and following the Inquiry’s Protocol on Applications for Restriction Orders.27 In Module 1, the Chair issued a restriction order dated 14 December 2023 concerning redacted material.28 |
| A1.16. | To assist the Inquiry, groups of scientific and other experts have been appointed, covering a range of different topics and views. This included, in Module 1, experts in relation to health inequalities, infectious disease epidemiology, risk management and resilience, infectious disease surveillance and public health structures. |
| Topic | Expert(s) appointed | Expert report |
|---|---|---|
| Health inequalities | Professor Clare Bambra (Professor of Public Health at Newcastle University) Professor Sir Michael Marmot (Professor of Epidemiology and Public Health at University College London) |
INQ000195843 |
| Infectious disease epidemiology | Professor David Heymann (Professor of Infectious Disease Epidemiology at the London School of Hygiene & Tropical Medicine) | INQ000195846 |
| Risk management and resilience | Professor David Alexander (Professor of Risk and Disaster Reduction at University College London) Bruce Mann (Director of the Civil Contingencies Secretariat from 2004 to 2009) |
INQ000203349 |
| Infectious disease surveillance | Professor Jimmy Whitworth (Emeritus Professor at the London School of Hygiene & Tropical Medicine) Dr Charlotte Hammer (Everitt Butterfield Research Fellow at Downing College, University of Cambridge) |
INQ000196611 |
| Public health structures | Dr Claas Kirchhelle (Assistant Professor of History at University College Dublin from 2020) | INQ000205178 |
| A1.17. | Witnesses are invited by the Inquiry to provide a statement if they have evidence relevant to a particular module. They give evidence on oath and are questioned by a Counsel to the Inquiry, and Counsel for Core Participants can also ask questions with the Chair’s permission. At the public hearings for Module 1, which commenced on 13 June 2023 and ended on 19 July 2023, the Inquiry heard evidence from 68 witnesses from the UK government, the devolved administrations, experts in epidemiology, resilience and health structures, civil society groups and bereaved people. |
| Witness (role/organisation) | Date of evidence |
|---|---|
| Professor Jimmy Whitworth (Emeritus Professor at the London School of Hygiene & Tropical Medicine) Dr Charlotte Hammer (Everitt Butterfield Research Fellow at Downing College, University of Cambridge) |
14 June 2023 |
| Professor David Heymann (Professor of Infectious Disease Epidemiology at the London School of Hygiene & Tropical Medicine) | 15 June 2023 |
| Professor David Alexander (Professor of Risk and Disaster Reduction at University College London) Bruce Mann (Director of the Civil Contingencies Secretariat from 2004 to 2009) |
15 June 2023 |
| Professor Clare Bambra (Professor of Public Health at Newcastle University) Professor Sir Michael Marmot (Professor of Epidemiology and Public Health at University College London) |
16 June 2023 |
| Katharine Hammond (Director of the Civil Contingencies Secretariat from August 2016 to August 2020) | 16 June 2023 |
| The Rt Hon David Cameron MP (Prime Minister from May 2010 to July 2016) | 19 June 2023 |
| Sir Christopher Wormald (Permanent Secretary to the Department of Health and Social Care from May 2016) | 19 June 2023 |
| Clara Swinson (Director General for Global and Public Health at the Department of Health and Social Care from November 2016 and Chair of the Pandemic Influenza Preparedness Programme Board from 2017 to 2022) | 19 June 2023 |
| The Rt Hon Sir Oliver Letwin MP (Minister for Government Policy from May 2010 to July 2016 and Chancellor of the Duchy of Lancaster from July 2014 to July 2016) | 20 June 2023 |
| The Rt Hon George Osborne MP (Chancellor of the Exchequer from May 2010 to July 2016) | 20 June 2023 |
| Professor Dame Sally Davies (Chief Medical Officer for England from June 2010 to October 2019) | 20 June 2023 |
| Professor Sir Mark Walport (Government Chief Scientific Adviser from April 2013 to September 2017) | 21 June 2023 |
| The Rt Hon Oliver Dowden MP (Parliamentary Secretary to the Cabinet Office from January 2018 to July 2019; Minister for the Cabinet Office from July 2019 to February 2020; Minister without Portfolio, Cabinet Office, from September 2021 to June 2022; Chancellor of the Duchy of Lancaster from October 2022; Secretary of State in the Cabinet Office from February 2023) | 21 June 2023 |
| The Rt Hon Jeremy Hunt MP (Secretary of State for Health and Social Care from September 2012 to July 2018) | 21 June 2023 |
| Roger Hargreaves (Director of the COBR Unit from July 2022) | 22 June 2023 |
| Professor Sir Christopher Whitty (Chief Scientific Adviser for the Department of Health and Social Care from January 2016 to August 2021, Interim Government Chief Scientific Adviser from 2017 to 2018, Chief Medical Officer for England from October 2019) | 22 June 2023 |
| Professor Sir Patrick Vallance (Government Chief Scientific Adviser from April 2018 to March 2023) | 22 June 2023 |
| Dr Jim McMenamin (Head of Infections Service and Strategic Incident Director at Public Health Scotland) | 22 June 2023 |
| Emma Reed (Director of Emergency Preparedness and Health Protection in the Department of Health and Social Care from February 2018) | 26 June 2023 |
| Rosemary Gallagher (Professional Lead for Infection Prevention and Control at the Royal College of Nursing from July 2009) | 26 June 2023 |
| Professor Dame Jenny Harries (Chief Executive of the UK Health Security Agency from April 2021) | 26 June 2023 |
| The Rt Hon Matt Hancock MP (Secretary of State for Health and Social Care from July 2018 to June 2021) | 27 June 2023 |
| Duncan Selbie (Chief Executive of Public Health England from July 2012 to August 2020) | 27 June 2023 |
| Gillian Russell (Director of Safer Communities in the Scottish Government from June 2015 to March 2020) | 28 June 2023 |
| Caroline Lamb (Director General for Health and Social Care in the Scottish Government, and Chief Executive of NHS Scotland from January 2021) | 28 June 2023 |
| Jeane Freeman (Cabinet Secretary for Health and Sport in the Scottish Government from June 2018 to May 2021) | 28 June 2023 |
| Sir Jeremy Farrar (Chief Scientist at the World Health Organization from May 2023 and Director of the Wellcome Trust from 2013 to 2023) | 29 June 2023 |
| The Rt Hon Nicola Sturgeon MSP (First Minister of Scotland from November 2014 to March 2023) | 29 June 2023 |
| John Swinney MSP (Deputy First Minister in the Scottish Government from November 2014 to March 2023) | 29 June 2023 |
| Catherine Frances (Director General for Local Government, Resilience and Communities in the Department for Levelling Up, Housing and Communities from April 2019) | 29 June 2023 |
| Sir Frank Atherton (Chief Medical Officer for Wales from August 2016) | 3 July 2023 |
| Dr Andrew Goodall (Permanent Secretary to the Welsh Government from September 2021) | 3 July 2023 4 July 2023 |
| Dr Quentin Sandifer (Executive Director for Public Health Services and Medical Director at Public Health Wales from October 2012 to December 2020) | 4 July 2023 |
| The Rt Hon Vaughan Gething MS (Minister for Health and Social Services in the Welsh Government from May 2016 to May 2021) | 4 July 2023 |
| The Rt Hon Mark Drakeford MS (First Minister of Wales from December 2018 to March 2024) | 4 July 2023 |
| Dr Catherine Calderwood (Chief Medical Officer for Scotland from April 2015 to April 2020) | 5 July 2023 |
| Professor Jim McManus (President of the Association of the Directors of Public Health from October 2021 to October 2023) | 5 July 2023 |
| Professor Kevin Fenton (President of the Faculty of Public Health from July 2022) | 5 July 2023 |
| Professor Mark Woolhouse (Professor of Infectious Disease Epidemiology at the University of Edinburgh) | 5 July 2023 |
| Dr Denis McMahon (Permanent Secretary to The Executive Office of Northern Ireland from July 2021) | 6 July 2023 |
| Reg Kilpatrick (Director General for Covid Coordination in the Welsh Government from September 2020) | 6 July 2023 |
| Robin Swann MLA (Minister of Health in Northern Ireland from January 2020 to October 2022) | 6 July 2023 |
| Dr Claas Kirchhelle (Assistant Professor of History at University College Dublin from 2020) | 10 July 2023 |
| Professor Sir Michael McBride (Chief Medical Officer for Northern Ireland from September 2006) | 10 July 2023 |
| The Rt Hon Arlene Foster, Baroness Foster of Aghadrumsee DBE (First Minister of Northern Ireland from January 2016 to January 2017) | 11 July 2023 |
| Richard Pengelly (Permanent Secretary to the Department of Health (Northern Ireland) from July 2014 to April 2022) | 11 July 2023 |
| Michelle O’Neill MLA (deputy First Minister of Northern Ireland from January 2020 to February 2022) | 12 July 2023 |
| Mark Lloyd (Chief Executive of the Local Government Association from November 2015) | 12 July 2023 |
| Alison Allen (Chief Executive of the Association of Local Authorities of Northern Ireland from February 2022) | 12 July 2023 |
| Aidan Dawson (Chief Executive of the Public Health Agency in Northern Ireland from July 2021) | 12 July 2023 |
| Marcus Bell (Director of the Equality Hub from September 2020) | 13 July 2023 |
| Melanie Field (Chief Strategy and Policy Officer of the Equality and Human Rights Commission from 2015) | 13 July 2023 |
| Nigel Edwards (Chief Executive of the Nuffield Trust from 2014) | 13 July 2023 |
| Dr Richard Horton (Editor-in-Chief of The Lancet from 1995) | 13 July 2023 |
| The Rt Hon Michael Gove MP (Chancellor of the Duchy of Lancaster from July 2019 to September 2021, Minister for the Cabinet Office from February 2020 to September 2021, and Secretary of State for Levelling Up, Housing and Communities from September 2021 to July 2022 and from October 2022) | 13 July 2023 |
| Kate Bell (Assistant General Secretary of the Trades Union Congress from December 2022) | 17 July 2023 |
| Gerry Murphy (Assistant General Secretary of the Irish Congress of Trade Unions from December 2022) | 17 July 2023 |
| Professor Philip Banfield (Chair of the British Medical Association UK council from July 2022) | 17 July 2023 |
| Dr Jennifer Dixon (Chief Executive of the Health Foundation from 2013) | 17 July 2023 |
| Michael Adamson (Chief Executive of the British Red Cross from November 2014) | 17 July 2023 |
| Matt Fowler (co-founder of Covid-19 Bereaved Families for Justice) | 18 July 2023 |
| Jane Morrison (lead member of Scottish Covid Bereaved) | 18 July 2023 |
| Anna-Louise Marsh-Rees (co-leader of Covid-19 Bereaved Families for Justice Cymru) | 18 July 2023 |
| Brenda Doherty (one of the group leads of Northern Ireland Covid-19 Bereaved Families for Justice) | 18 July 2023 |
| A1.18. | A public inquiry is established to examine the facts and to find out exactly what happened. It is an inquisitorial, not an adversarial, process. This Report’s conclusions and recommendations are based on an objective assessment of the totality of the evidence received by the Inquiry. |
| A1.19. | Rule 13(3) of the Inquiry Rules 2006 prevents the inclusion of any “explicit or significant criticism” of any person in this Report unless a warning letter has been sent and the relevant person has been given a reasonable opportunity to respond.29 The phrase “explicit or significant criticism” has been interpreted generously to ensure that anyone whose conduct might be considered to have been the subject of criticism within this Report has the opportunity to respond. Warning letters were sent as appropriate to those who were covered by rule 13 and the Chair considered the responses to those letters before finalising this Report. |
| A1.20. | The purpose of the Inquiry’s investigation in this Report concerning Module 1 was to examine whether the groundwork had been laid to enable the UK government and devolved administrations to make the necessary decisions when the Covid-19 pandemic arose. In Module 2 (Core UK decision-making and political governance), the Inquiry is considering whether the policies pursued by these governments in response to the Covid-19 pandemic were the right ones, ie whether they were proportionate to the risk. |
| A1.21. | The Chair was greatly assisted in Module 1 by the Inquiry team of counsel, solicitors, paralegals and other members of the Secretariat. |
| Role | Name |
|---|---|
| Lead Counsel | Hugo Keith KC, Kate Blackwell KC |
| Junior Counsel | Jamie Sharma, Bo-Eun Jung, Joshua Cainer, Zeenat Islam |
Terminology and references
| A1.22. | The nature of the subject matter means that the evidence considered by the Inquiry contains significant technical and specialist language, which the Inquiry has tried to minimise in this Report. A number of witnesses and documents also used a range of abbreviations and acronyms. These terms are explained fully in Appendix 3: Glossary, but, to avoid any confusion and to assist the reader, the Inquiry has set out names and other key phrases in full in this Report. |
| A1.23. | Some terminology that is particularly key to understanding this Report is listed below for ease of reference. |
Key terminology
| A1.24. | The virus that causes the coronavirus disease known as Covid-19 is SARS-CoV-2. However, where this specificity is not necessary, in accordance with the practice of the World Health Organization, the Inquiry uses ‘Covid-19’ to refer to both the virus and the disease. |
| A1.25. | The Covid-19 pandemic required action by both national and devolved governments. Wales, Scotland and Northern Ireland each have a legislature and executive elected by their own electorates (referred to in this Report as ‘devolved administrations’). Although each devolution settlement is different, each administration is responsible for a range of topics, including health, education and transport. England has no legislature of its own and, instead, the UK Parliament legislates on UK-wide ‘reserved’ (ie not devolved) issues such as defence and foreign affairs, and legislates for England on issues devolved to other nations. The UK Parliament also, at times, legislates for other groupings – for example, in England and Wales on issues of justice. |
| A1.26. | The UK government is responsible for all aspects of government policy in England. At the time of the Covid-19 pandemic, the Department of Health and Social Care was responsible for policy on health and adult social care matters in England (and on a UK-wide basis for a few elements of the same matters that are not otherwise devolved). Prior to January 2018, the Department of Health and Social Care was called the Department of Health. This Report uses the correct name for the department and its Secretary of State according to the relevant time period. For references that span both before and after January 2018, the Report uses the current name. |
| A1.27. | The most complex civil emergencies have many potential impacts and so engage the ‘whole system’ of government or even the ‘whole of society’. Where this Report makes findings and recommendations concerning complex civil emergencies, the Inquiry refers to ‘whole-system civil emergencies’ that require a cross-departmental approach to preparedness and response by the governments. Some relate only to pandemics. |
References
| A1.28. | References such as ‘Clare Bambra 16 June 2023 46/18-23’ or ‘INQ000087205_0005’ in the footnotes of this Report relate to material that is available on the Inquiry’s website.30 |
| A1.29. | The transcripts of the Inquiry’s hearings are referenced by person, hearing date, and internal page and line numbers. For example, ‘Clare Bambra 16 June 2023 46/18-23’ refers to the evidence of Professor Clare Bambra on 16 June 2023, page 46, lines 18 to 23. |
| A1.30. | Documentary evidence is referenced by the document’s number and, where relevant, page and paragraph numbers. For example, ‘INQ000087205_0005 para 20’ refers to document INQ000087205, page 5, paragraph 20. |
| A1.31. | Publicly available documents are listed in the footnotes with both their wider internet and Inquiry website links. For example: The UK Government Resilience Framework, HM Government, December 2022, para 14 (https://www.gov.uk/government/ publications/the-uk-government-resilience-framework; INQ000097685). |
- See https://covid19.public-inquiry.uk/documents/terms-of-reference/, which includes translations of the Inquiry’s Terms of Reference; for the Inquiries Act 2005, see https://www.legislation.gov.uk/ukpga/2005/12/contents.
- https://covid19.public-inquiry.uk/documents/terms-of-reference
- https://covid19.public-inquiry.uk/documents/terms-of-reference
- See https://covid19.public-inquiry.uk/structure-of-the-inquiry for further information.
- https://covid19.public-inquiry.uk/modules/resilience-and-preparedness/
- https://covid19.public-inquiry.uk/modules/core-uk-decision-making-and-political-governance-module-2/
- https://covid19.public-inquiry.uk/modules/core-uk-decision-making-and-political-governance-scotland-module-2a/
- https://covid19.public-inquiry.uk/modules/core-uk-decision-making-and-political-governance-wales-module-2b/
- https://covid19.public-inquiry.uk/modules/core-uk-decision-making-and-political-governance-northern-ireland-module-2c/
- https://covid19.public-inquiry.uk/modules/impact-of-covid-19-pandemic-on-healthcare-systems-in-the-4-nations-of-the-uk/
- https://covid19.public-inquiry.uk/modules/vaccines-and-therapeutics-module-4/
- https://covid19.public-inquiry.uk/modules/procurement-module-5/
- https://covid19.public-inquiry.uk/modules/care-sector-module-6/
- https://covid19.public-inquiry.uk/modules/test-trace-and-isolate-module-7/
- https://covid19.public-inquiry.uk/every-story-matters/
- See https://covid19.public-inquiry.uk/news/hundreds-of-children-and-young-people-set-to-tell-the-inquiry-how-the-pandemic-affected-them/ for further information.
- https://covid19.public-inquiry.uk/wp-content/uploads/2023/05/Module-1-Outline-of-Scope.pdf
- https://covid19.public-inquiry.uk/wp-content/uploads/2023/05/Module-1-List-of-Issues-dated-06-April-2023.pdf
- For the Inquiry Rules 2006, see https://www.legislation.gov.uk/uksi/2006/1838/contents/made; for Core Participant Protocol, see https://covid19.public-inquiry.uk/wp-content/uploads/2023/05/Core-Participant-Protocol.docx-1.pdf.
- https://covid19.public-inquiry.uk/hearings/resilience-and-preparedness/; https://www.youtube.com/@UKCovid-19Inquiry/videos
- https://covid19.public-inquiry.uk/wp-content/uploads/2022/11/2022-11-15-Protocol-on-Documents.pdf; https://www.legislation.gov.uk/uksi/2006/1838/article/9/made
- https://covid19.public-inquiry.uk/wp-content/uploads/2023/05/2022-10-04-Inquiry-Protocol-on-the-Redaction-of-Documents.pdf
- https://covid19.public-inquiry.uk/documents/
- https://www.legislation.gov.uk/ukpga/2005/12/contents
- https://covid19.public-inquiry.uk/documents/
- https://covid19.public-inquiry.uk/documents/
- For the Inquiries Act 2005, see https://www.legislation.gov.uk/ukpga/2005/12/section/19; for the Protocol on Applications for Restriction Orders, see https://covid19.public-inquiry.uk/wp-content/uploads/2022/11/2022-10-11-Inquiry-Protocol-on-Applications-for-Restriction-Orders-.pdf.
- https://covid19.public-inquiry.uk/wp-content/uploads/2023/12/15164756/2023-12-14-Module-1-General-Restriction-Order.pdf
- https://www.legislation.gov.uk/uksi/2006/1838/made
- https://covid19.public-inquiry.uk/hearings/resilience-and-preparedness/
Appendix 2: Exercises
| A2.1. | This appendix details the key simulation exercises relevant to pandemic preparedness and resilience that were conducted in the UK and the devolved nations between 2002 and 2018. There are four types of simulation exercises:
|
| Overview | Key objectives and participants | Key findings/concerns | Key recommendations |
|---|---|---|---|
| Exercise Shipshape 6 June 2003 England and Wales Table top exercise commissioned by the Health Protection Agency concerning severe acute respiratory syndrome (SARS) INQ000235217 |
To explore the capability of local healthcare systems in south-west England and Wales to cope with an increasing number of SARS cases. To explore other issues relevant to pandemic response, including contact tracing arrangements, isolation procedures and resourcing requirements (INQ000235216_0002). Participants included the Department of Health, the Health Protection Agency, NHS trusts, the Cabinet Office, the Scottish Executive and other government departments (INQ000235216_0014-0015). |
Capacity
|
Capacity
|
| Exercise Goliath 9 December 2003 Northern Ireland Live exercise commissioned by the Department of Health, Social Services and Public Safety concerning SARS INQ000206664_0001 |
To test the response of the health community in the event of a SARS outbreak in Northern Ireland. The Department of Health, Social Services and Public Safety and the Health Protection Agency participated. Observers (including other boards, trusts, government departments and jurisdictions) were also in attendance (INQ000206664_0002). | Capacity
|
Capacity
|
| Exercise Bennachie 2 December 2004 Scotland Table top exercise by Health Protection Scotland concerning SARS INQ000187903_0001 |
To test Scotland’s overall preparedness for dealing with SARS (and similar infections with the potential for major spread and impact on society). The exercise format was based on syndicates involving key representatives involved in the response. They singly and collectively explored a series of issues and questions related to a SARS outbreak. The exercise was developed in four phases spanning a notional 10-week scenario (INQ000187903_0001). Representatives from NHS trusts, the Scottish Ambulance Service, local authorities, the Grampian Regional Emergencies Committee – Strategic Group, Health Protection Scotland and the Scottish Executive attended (INQ000187903_0001). |
Capacity
|
Planning
|
| Exercise Winter Willow January–February 2007 UK-wide Table top and live exercise commissioned by the Health Protection Agency and the Cabinet Office concerning pandemic influenza INQ000128977 |
To check preparation for the major disruptive challenges that an influenza pandemic may bring. Exercise Winter Willow was delivered in two stages. Stage 1 was held on 30 January 2007 and comprised a national-level table top exercise. Stage 2, between 16 and 21 February 2007, followed up the decisions taken during Stage 1 with a full national exercise held over several days. This was designed to test the UK response at local, regional and national levels during UK alert level 4 (widespread cases in the UK) (INQ000128977_0004). Over 5,000 people participated from a large number of UK organisations representing government, industry and the voluntary sector (INQ000128977_0003). |
Communication
|
Communication
|
| Exercise Taliesin 18 November 2009 Wales Live exercise commissioned by the Welsh Government (Wales Resilience Partnership Team) concerning pandemic influenza INQ000128976 |
To test the Pan-Wales Response Plan and influenza pandemic plans by live exercise across Wales. The exercise formed part of the Cabinet Office’s work on developing resilience against an influenza pandemic. To this end, the Cabinet Office funded a series of ‘Gold Standard’ exercises across the English regions and Wales. In England, the exercise was run in one local resilience forum area per region, while in Wales it was run simultaneously at all four local resilience forum areas as part of Exercise Taliesin (INQ000128976_0003). A total of 62 participants from across Wales agreed to attend a workshop. Invitations were sent to local resilience forums and individual agencies to achieve a geographical and organisational balance (INQ000128976_0005). |
Planning
|
Planning
|
| Exercise Cygnus (Wales) October 2014 Wales Live exercise by the Welsh Government concerning pandemic influenza INQ000128979 INQ000107136 |
To implement the Pan-Wales Response Plan against a pandemic influenza scenario in order to exercise the strategic decision-making processes at both the local and national levels in Wales. The exercise was scheduled to be held in three phases: a workshop on health planning and response in May 2014; the main exercise from 13 to 16 October 2014; and a recovery exercise to follow. The Welsh Government, Public Health Wales and local resilience forums were involved, as well as the Wales Civil Contingencies Committee (INQ000107136_0001). |
Capacity
|
Capacity
|
| Ebola Preparedness Surge Capacity Exercise 10 March 2015 England Seminar-based exercise commissioned by NHS England concerning Ebola virus disease INQ000090428 |
To stress-test the surge capacity and resilience of UK hospitals and health agencies in response to a novel high consequence infectious disease (Ebola). The surge capacity exercise was a one-day event in London. The exercise consisted of facilitated discussions and a structured walkthrough of the required response to the scenario(s). It involved senior health and communications officers from NHS England, Public Health England, the four NHS surge centres, directors of public health and the four relevant ambulance service trusts. A panel of subject matter experts was also available to contribute and respond to any issues raised (INQ000090428_0007). |
Capacity
|
Capacity
|
| Exercise Valverde 25 May 2015 England Command post exercise by Public Health England Commissioned by the Global Health Security Initiative’s Sample Sharing Task Group concerning novel coronavirus – sample sharing INQ000022722 |
To test the arrangements in place for the rapid sharing of laboratory samples of non-influenza pathogens and related specimens during a public health emergency. This was an international exercise simulating an outbreak of novel coronavirus in the fictional country of Valverde in South America, which becomes a Public Health Emergency of International Concern. Participants in the exercise included representatives from the member countries and organisations in the Global Health Security Initiative’s Sample Sharing Task Group, ministries of health, national-level designated laboratories and other relevant stakeholders and government departments involved in the process of sample sharing across international borders. The European Commission also participated in the exercise in a supporting role (INQ000022722_0004). |
Training
|
Training
|
| Exercise Alice 15 February 2016 England Table top exercise commissioned by the Department of Health concerning Middle East respiratory syndrome coronavirus (MERS-CoV) INQ000090431 |
To explore the policies, response and issues associated with an outbreak in England. This exercise was commissioned by the Department of Health in response to concerns raised by the Chief Medical Officer about the planning and resilience to respond to a largescale outbreak of MERS-CoV in England. NHS England, Public Health England and the Department of Health participated. The exercise was observed by the Cabinet Office, the devolved administrations and the Government Office for Science (INQ000090431). |
Capacity
|
Capacity
|
| Exercise Silver Swan April 2016 Scotland Series of table top exercises led by the Scottish Government (Resilience Division) concerning pandemic influenza INQ000103012 |
To assess the preparedness and response of Scotland’s local and national arrangements to a pandemic influenza outbreak over a prolonged period. This was a new approach to national exercising. One of the most successful aspects of this approach was that the events provided an opportunity for over 600 people to take part, including participants from the NHS and local authorities (INQ000103012_0008). |
Capacity
|
Capacity
|
| Exercise Cygnus 18-20 October 2016 UK-wide Live exercise commissioned by the Department of Health concerning pandemic influenza INQ000022792 |
To assess the UK’s preparedness and response to a pandemic influenza outbreak (INQ000022792_0003). Based around four simulated COBR meetings. Set in the seventh week of a pandemic affecting up to 50% of the UK’s population and causing between 200,000 and 400,000 excess deaths. Over 950 representatives from the devolved administrations, the Department of Health and 12 other government departments, NHS Wales, NHS England, Public Health England, eight local resilience forums and six prisons took part in the exercise (INQ000022792_0005). |
Capacity
|
Capacity
|
| Exercise Broad Street 29 January 2018 England Discussion-based exercise commissioned by the High Consequence Infectious Diseases Programme board concerning future, definitive high consequence infectious disease (HCID) INQ000090442 |
To consider the future definitive HCID service in England and the challenges that an HCID incident could present professional partners with the proposed HCID service in England (INQ000090442_0005). On 29 January 2018, this discussion- based exercise was conducted in London. Participants came from Public Health England and NHS England. Additionally, an observer from the Department of Health and Social Care attended (INQ000090442_0008). |
Capability
|
Capability
|
| Exercise Iris 12 March 2018 Scotland Table top exercise delivered by the Scottish Government Health Protection Division concerning MERS-CoV INQ000147839 |
To assess NHS Scotland’s response to a suspected outbreak of MERS-CoV. On 12 March 2018, a table top exercise was conducted in Scotland to explore the challenges that NHS Scotland boards would face in the event of suspected – and later confirmed – cases of MERS-CoV in one or more board areas. Participants in the exercise represented NHS Scotland boards, national boards including NHS 24 and Health Protection Scotland, and the Scottish Ambulance Service (INQ000147839_0004). |
Capacity
|
Capacity
|
| Exercise Pica 5 September 2018 England Table top exercise commissioned by NHS England concerning pandemic influenza INQ000023034 |
To review and assess pandemic influenza preparedness and response within primary care by providing an opportunity to explore the existing processes and arrangements. Its purpose was to identify lessons for the NHS primary care response to pandemic influenza over three key stages: detect and assess (first days/ weeks); treat and escalate (peak of the pandemic at weeks 6/7); and recovery (months later). It was supported by NHS England and Public Health England. Participants included NHS trusts, British Dental Association, British Medical Association GP Committee, College of Optometrists, Care Quality Commission and Royal Pharmaceutical Society (INQ000023034_0005). |
Capacity
|
Capacity
|
- The Exercise Planners Guide, Home Office, 1998 (https://assets.publishing.service.gov.uk/media/5a74b983ed915d4d83b5e717/the-exercise-planners-guide.pdf)
- Katharine Hammond 16 June 2023 178/2-7
- The Exercise Planners Guide, Home Office, 1998 (https://assets.publishing.service.gov.uk/media/5a74b983ed915d4d83b5e717/the-exercise-planners-guide.pdf)
- Katharine Hammond 16 June 2023 178/2-7
- The Exercise Planners Guide, Home Office, 1998 (https://assets.publishing.service.gov.uk/media/5a74b983ed915d4d83b5e717/the-exercise-planners-guide.pdf)
- The Exercise Planners Guide, Home Office, 1998 (https://assets.publishing.service.gov.uk/media/5a74b983ed915d4d83b5e717/the-exercise-planners-guide.pdf)
Appendix 3: Glossary
| Term (acronym) | Description |
|---|---|
| 10 Downing Street | The Prime Minister’s Office, which supports the Prime Minister in establishing and delivering the UK government’s overall strategy and policy priorities, and in communicating the UK government’s policies to Parliament, the public and international audiences. |
| Advisory Committee on Dangerous Pathogens | A scientific advisory committee of the Department of Health and Social Care. Its work includes providing the UK government with independent scientific advice on the risks of exposure to pathogens. |
| Airborne transmission | Transmission occurring across short or long distances through the air from very small virus-containing respiratory droplets produced by an infected individual. |
| Antibiotics | Medicines used to treat or prevent bacterial infections. |
| Antivirals | Medicines used to treat or prevent viral infections. |
| Association of Directors of Public Health | A representative organisation of directors of public health. |
| Asymptomatic | Having an infection but not showing any symptoms. |
| Avian influenza | A type of influenza virus adapted to bird populations. Avian influenza can also spill over to other animals, including humans, and may evolve the ability to transmit efficiently from person to person. |
| Behavioural science | The scientific study of human and animal behaviour, including disciplines such as psychology, anthropology and sociology. |
| Biosecurity | The preparation, policies and actions taken to protect human, animal and environmental health against biological threats. |
| ‘Black swan’ event | A catastrophic scenario that, in advance, is unprecedented, outside of our field of experience, beyond our abilities to reasonably contemplate and, therefore, so seemingly unlikely that it is unforeseeable. |
| British Medical Association | A trade union and professional body for doctors and medical students in the UK. |
| Cabinet | A team of the most senior government ministers who are chosen to lead on specific policy areas. |
| Cabinet Office | A ministerial UK government department, supported by 28 agencies and public bodies. It supports the Prime Minister, ensures the effective running of the government, and takes the lead in certain critical policy areas. |
| Case fatality ratio | The percentage of people diagnosed with a disease who die from it. |
| Category 1 and 2 responders | Under the Civil Contingencies Act 2004: Category 1 responders are those organisations (the emergency services, local authorities and NHS bodies) at the core of the response to most emergencies, which are subject to the full set of civil protection duties. Category 2 responders are organisations (the Health and Safety Executive, transport and utility companies) that are heavily involved in incidents that affect their particular sectors but are less likely to be involved at the heart of planning work. They have a lesser set of duties: cooperating and sharing relevant information with other Category 1 and 2 responders. |
| Chancellor of the Duchy of Lancaster | A senior Cabinet Office minister and member of the Cabinet who administers the estates and rents of the Duchy of Lancaster. Responsible for overseeing all Cabinet Office policy, civil contingencies, resilience and national security. |
| Chancellor of the Exchequer | The UK government’s chief financial minister, with overall responsibility for the Treasury. |
| Chief Medical Officer | A qualified medical practitioner, the most senior government adviser on health matters, and the professional head of all directors of public health in local government and the medical profession in government. There is a separate Chief Medical Officer for England, Wales, Scotland and Northern Ireland. The Chief Medical Officer for England is the UK government’s Chief Medical Adviser. |
| Chief scientific advisers | Senior science advisers, working in most government departments, who provide oversight and assurance of science capability and activities. |
| Civil Contingencies Act 2004 | Legislation providing a framework for civil protection in the UK. It also allows for the making of temporary special legislation (emergency regulations) to help deal with the most serious of emergencies. |
| Civil Contingencies Group (Northern Ireland) | The principal strategic civil contingencies preparedness body for the public sector in Northern Ireland, responsible for providing strategic leadership for civil contingencies preparedness by agreeing policy and strategy on cross-cutting issues. It is normally chaired by a senior civil servant, but may alternatively be chaired by the First Minister and the deputy First Minister acting jointly, or by another minister nominated jointly by the First Minister and deputy First Minister. It is attended by representatives from all Northern Ireland government departments, the Northern Ireland Office, as well as local government and the emergency services, among others. |
| Civil Contingencies Group (Wales) | A group of senior policy officials established around 2006 that meets to discuss strategy for emergency preparedness in Wales, considering emerging risks and determining appropriate planning, response and recovery across government departments. It also manages the Welsh Government’s internal response to emergencies. Where it is determined that wider external stakeholder attendance is needed, the group is formally reconstituted as the Wales Civil Contingencies Committee, under the terms of the Pan-Wales Response Plan. |
| Civil Contingencies Secretariat | A dedicated capability in the Cabinet Office that managed the UK government’s preparedness and response to major, nationwide events. Worked with government departments to determine and manage risks and coordinate civil emergency arrangements, provided advice to the Prime Minister about civil emergencies, ran COBR, worked with devolved administrations and local responders to ensure that plans and capabilities were in place, and oversaw high-level exercises or tests of the preparedness and response system. Replaced by the COBR Unit and a Resilience Directorate in July 2022. |
| COBR | The UK government’s national crisis management centre for responding to whole-system civil emergencies. It provides the coordination mechanism through which the UK government responds quickly to emergencies that require urgent decision- making. Its name was originally derived from its location in the Cabinet Office Meeting Rooms. |
| Community transmission | When a disease is spreading in the community and the specific source is unknown (for instance, it cannot be linked to a traveller from abroad). |
| Concept of Operations (UK government) | A document setting out UK arrangements for responding to and recovering from emergencies. |
| Contact | A person who has been close to someone who has tested positive for an infection. |
| Contact tracing | Identifying the source and contacts linked to a confirmed case of an infectious disease. A public health measure to contain the spread of an infection. |
| Containment | A disease control strategy aimed at preventing community transmission, such as through tracing the contacts of infected people. |
| Contingency planning | Planning to be ready to respond effectively in the event of an emergency. |
| Coronaviruses | A family of viruses that cause respiratory illnesses in people. |
| Countermeasures | Measures taken to mitigate or suppress the effects of a pandemic, such as contact tracing, therapeutics and vaccines. |
| Covid-19 | The disease caused by the coronavirus SARS-CoV-2. |
| Covid-19 Bereaved Families for Justice | A UK-wide campaign group representing the interests of bereaved family members of individuals who died from Covid-19. |
| Covid-19 Bereaved Families for Justice Cymru | A Welsh-focused group dedicated to campaigning for and giving a voice to people bereaved by Covid-19 in Wales. |
| Crimean-Congo haemorrhagic fever | A viral haemorrhagic fever, primarily contracted through tick bites. |
| Department for Business and Trade | A ministerial UK government department, supported by 19 agencies and public bodies, that is responsible for economic growth and international trade. |
| Department for Levelling Up, Housing and Communities | A ministerial UK government department, supported by 15 agencies and public bodies, that is responsible for housing, communities, local government, and levelling up policy. Known from May 2006 to January 2018 as the Department for Communities and Local Government, and from January 2018 to September 2021 as the Ministry of Housing, Communities and Local Government. Referred to in this Report by the correct name for the relevant time period or, for references that span before and after September 2021, by its current name. |
| Department of Health and Social Care/Department of Health | A ministerial UK government department with overall responsibility for health and care services. It sets strategy, and funds and oversees the health and care system in England, with equivalent counterparts in the devolved nations. Known prior to January 2018 as the Department of Health. Referred to in this Report by the name it had during the relevant time period, or, for references spanning both time periods, by its current name. |
| Department of Health (Northern Ireland) | A devolved government department in the Northern Ireland Executive with a statutory responsibility to promote the physical and mental health and social wellbeing of people in Northern Ireland and for the prevention, diagnosis and treatment of illness. Until 9 May 2016, the department was known as the Department of Health, Social Services and Public Safety, but it is referred to in this Report as the Department of Health (Northern Ireland) unless specifically referring to before May 2016. |
| Deputy Chief Medical Officer | Three Deputy Chief Medical Officers support the Chief Medical Officer. |
| Deputy First Minister, Northern Ireland Executive | Joint chair (with the First Minister) of the Northern Ireland Executive. All statutory functions assigned to the deputy First Minister (and First Minister) by the Northern Ireland Act 1998 must be exercised jointly. |
| Deputy First Minister, Scottish Government | A Cabinet Secretary in the Scottish Government, supporting the work of the First Minister. Until 2023, the Deputy First Minister was responsible for the resilience function of the Scottish Government. |
| Diagnostic test | A test that can confirm if someone has a disease. |
| Directors of public health | In England, specialists employed by every local authority with public health responsibilities, who have primary responsibility for the health of their communities and are accountable for the delivery of their authority’s public health duties. In Scotland and Wales, they are employed by NHS health boards, and in Northern Ireland, the sole Director of Public Health is accountable to the Chief Medical Officer. |
| ‘Disease X’ | An infectious disease that is currently not known to infect humans but could cause a serious epidemic or pandemic. |
| DNA | Deoxyribonucleic acid, a molecule that carries genetic instructions for the growth and functioning of all known organisms and many viruses. |
| Ebola | Can refer to the Ebola virus or the disease it causes. The virus is transmitted from animals (such as bats or non-human primates) to people, and can spread from person to person through bodily fluids. It causes a severe and often fatal haemorrhagic fever. |
| Ebola Preparedness Surge Capacity Exercise | A March 2015 exercise commissioned by NHS England to assess NHS and Public Health England capabilities and resources to manage multiple Ebola cases within England. |
| Effectiveness | When discussing a drug such as a treatment or vaccine, this refers to how well the drug achieves the intended effect when it is used in real-world settings. |
| Efficacy | The extent to which a drug works as intended when it is tested in ideal circumstances, such as in a controlled research study. |
| Emergency preparedness groups | Multi-agency groups in Northern Ireland set up to ensure appropriate preparedness to enable an effective response to emergencies. |
| Emergency preparedness, resilience and response | Within a government department, the emergency preparedness, resilience and response function leads on the planning for and response to all incidents where there is a potential risk to public health. |
| Emergency Response Department | A department of what was Public Health England that worked to improve public health resilience by providing emergency preparedness, resilience and response services backed by evidence-based scientific and medical research. |
| Endemic disease | A disease that remains at a stable, predictable incidence rate in a geographical region. |
| Epidemic | A sudden increase in incidence of a disease that is higher than expected in a geographical region. |
| Epidemiology | The study of the distribution, patterns and determinants of health and disease conditions in a defined population. |
| Eradication | Complete reduction of all cases of a disease around the world to zero, without the ongoing need for interventions. |
| European Centre for Disease Prevention and Control | An agency of the European Union focusing on infectious disease surveillance, response and preparedness. |
| Excess deaths | The number of additional deaths in a time period that is higher than would usually be expected based on recent years. |
| The Executive Office, Northern Ireland | A devolved Northern Ireland government department in the Northern Ireland Executive with principal policy responsibility for civil contingencies matters. The ministers with overall responsibility for the department are the First Minister and deputy First Minister. |
| Exercise Alice | A February 2016 exercise to assess the challenges of a large-scale outbreak of Middle East respiratory syndrome coronavirus (MERS- CoV) in England. |
| Exercise Bennachie | A one-day table top exercise in December 2004 that aimed to test overall preparedness for dealing with severe acute respiratory syndrome (SARS). |
| Exercise Broad Street | A January 2018 exercise to develop an agreed approach to managing the end-to-end patient pathway for known and unknown high consequence infectious diseases and to ensure a sustainable response was in place. |
| Exercise Cerberus | A February 2018 internal assessment of Public Health England’s organisational preparedness and response to public health emergencies. |
| Exercise Cygnus | An October 2016 exercise assessing the UK’s preparedness and response to a pandemic influenza outbreak. |
| Exercise Goliath | A December 2003 test of the response to a severe acute respiratory syndrome (SARS) outbreak in Northern Ireland. |
| Exercise Iris | A March 2018 exercise to assess Scotland’s response to an outbreak of Middle East respiratory syndrome coronavirus (MERS-CoV). |
| Exercise Pica | A September 2018 test of the preparedness and response capabilities of NHS primary care to pandemic influenza. |
| Exercise Shipshape | A June 2003 exercise that was carried out following confirmation of the first case of severe acute respiratory syndrome (SARS) in the UK. |
| Exercise Silver Swan | A series of exercises delivered across Scotland in April 2016 to assess the preparedness and response of Scotland’s local and national arrangements to a pandemic influenza outbreak over a prolonged period. |
| Exercise Taliesin | A November 2009 exercise to assess the Pan-Wales Response Plan and local pandemic influenza plans across Wales. |
| Exercise Typhon | A February 2017 test to assess Public Health England’s capacity to respond to and manage two concurrent enhanced level incidents (a major chemical incident and a confirmed positive case of a viral haemorrhagic fever). |
| Exercise Winter Willow | A January and February 2007 exercise to assess preparations for an influenza pandemic. |
| Exercise Valverde | A May 2015 exercise of the Global Health Security Initiative to test the draft arrangements of member countries for the sharing of laboratory samples of non-influenza pathogens during a public health emergency. |
| Exponential spread | An infection can spread exponentially (ie accelerating over time) when the pathogen enters a population with little or no immunity. |
| First Minister, Northern Ireland Executive | Joint chair (with the deputy First Minister) of the Northern Ireland Executive. All statutory functions assigned to the First Minister (and deputy First Minister) by the Northern Ireland Act 1998 must be exercised jointly. |
| First Minister of Scotland | Head of the Scottish Government, responsible for the overall development, implementation and presentation of the administration’s policies and for promoting and representing Scotland at home and overseas. |
| First Minister of Wales | Head of the Welsh Government, responsible for the overall development and coordination of Welsh Government policy. |
| Foreign, Commonwealth and Development Office | Ministerial government department, supported by 12 agencies and public bodies. |
| Four nations | The four nations of the UK: England, Wales, Scotland and Northern Ireland. |
| Fukushima radiological incident | A 2011 nuclear accident involving radiation leaks at the Fukushima Daiichi Nuclear Power Plant in Japan. |
| G7 | The Group of Seven (G7) is an informal intergovernmental forum made up of the UK, USA, Canada, France, Germany, Italy and Japan. Representatives from the European Union also attend. |
| Global Outbreak Alert and Response Network, World Health Organization | A World Health Organization network of technical institutions and networks globally that respond to acute public health events with the deployment of staff and resources to affected countries. |
| Government Chief Scientific Adviser | The Chief Scientific Adviser provides scientific advice to the Prime Minister and members of Cabinet, and coordinates the network of chief scientific advisers. |
| Government Office for Science (GO- Science) | A science office that advises the Prime Minister and members of the Cabinet to ensure that government policies and decisions are informed by the best scientific evidence and strategic long-term thinking. |
| Groupthink | A science office that advises the Prime Minister and members of the Cabinet to ensure that government policies and decisions are informed by the best scientific evidence and strategic long-term thinking. |
| Groupthink | A phenomenon by which people in a group tend to think about the same things in the same way. |
| Health Emergency Preparedness and Response Authority, European Commission | Supports projects that strengthen preparedness and response capacities in the field of health. |
| Health Protection Agency | A former non-departmental public body, sponsored by the Department of Health and Social Care, which became part of Public Health England in 2013. Its role was to provide an integrated approach to protecting UK public health through the provision of support and advice to the NHS, local authorities, emergency services and the Department of Health and Social Care and other agencies. |
| Health protection teams | A part of the UK Health Security Agency. They consist of professionally qualified consultants in health protection who provide specialist public health advice and operational support to the NHS, local authorities and other agencies. |
| Henipaviral diseases | Moderate to severe neurological and respiratory diseases caused by a genus of viruses with their main natural reservoir in fruit bats. Hendra virus cases have been linked to close contact with infected horses in Australia, and larger Nipah virus outbreaks have occurred in several South-East Asian countries, with transmission from pigs and bats, and some person-to-person transmission reported. |
| High consequence infectious disease | An acute infectious disease that:
|
| High Consequence Infectious Diseases Programme | A programme created by Public Health England and NHS England in 2015 to develop an agreed method for managing suspected and confirmed cases of high consequence infectious diseases and put in place additional specialist facilities where patients with these diseases could be treated. |
| Home Office | A UK government department, supported by 29 agencies and public bodies. The lead government department for immigration and passports, drugs policy, crime, fire, counter-terrorism and police. |
| Human Animal Infections and Risk Surveillance | A multi-agency cross-government, horizon-scanning and risk assessment group that considers emerging and potentially zoonotic infections. |
| Human immunodeficiency virus (HIV) | A blood-borne or sexually transmitted virus that, if untreated, causes acquired immunodeficiency syndrome (AIDS) – a potentially fatal multi-system disease. |
| Immunisation | When individuals become protected from a disease, either following natural infection or vaccination. |
| Immunity | The ability to defend the body from a pathogen’s infection. Acquired immunity describes how the body builds immunological memory – so that if the person is exposed to the same infection again, the body’s response is enhanced. This is the basis for immunisation with vaccines. |
| Incidence | The number of new cases of a disease in a population during a particular time period. Calculating incidence rates can indicate how quickly an infectious disease is occurring in a population. |
| Infection fatality ratio | The percentage of people with a disease (diagnosed or undiagnosed) who die from it. |
| Influenza (flu) | A viral respiratory infection that infects humans globally and several other host species. Causes both seasonal endemic waves of infection and, when new strains emerge against which the population has less immunity, causes more severe epidemics or pandemics. |
| Intensive care unit | A type of hospital ward that provides specialised care for critically ill patients, such as mechanical ventilation for respiratory failure. |
| International Health Regulations | A legally binding instrument providing the overarching legal framework for states’ obligations and duties when faced with a public health event or emergency that could have international implications. There are 196 signatory states, including the 194 Member States of the World Health Organization. |
| Interventions | Any activity undertaken with the objective of improving human health by preventing disease, by curing or reducing the severity or duration of an existing disease, or by restoring function lost through disease or injury. |
| Joint Committee on Vaccination and Immunisation | A scientific committee that advises UK health departments on immunisation. |
| Just-in-time | A stock control method that emphasises keeping inventory to a minimum and using short-term, flexible contracts that can be adjusted quickly to changes in demand. |
| Lassa fever | A viral haemorrhagic fever caused by the Lassa virus. The disease is generally less severe than Ebola and is primarily transmitted by inhalation of dust contaminated by rat faeces or contact with infected bodily fluids. |
| Lead government department | The government department responsible for leading work to identify particular risks and ensuring that the right planning, response and recovery arrangements are in place. |
| Local Government Association | A national membership body for local authorities in England and Wales. |
| Local health resilience partnerships | Local health resilience partnerships bring together local health organisations, regional representatives of Public Health England – and subsequently the UK Health Security Agency – and other local stakeholders. They are responsible for identifying risks and developing plans relating to health and emergency preparedness, resilience and response, and linking into local resilience forums. |
| Local resilience forums | Multi-agency partnerships in England and Wales made up of local responders. The principal mechanism in England and in Wales for emergency preparedness and cooperation between agencies. Their main purpose is to ensure that local responders are able effectively to act on the duties imposed upon them under the Civil Contingencies Act 2004. |
| Local responders | Representatives from local public services, including the emergency services, local authorities, the NHS, the Health and Safety Executive and other organisations involved in emergency preparedness. |
| Lockdown | A mandatory stay-at-home order, a legal prohibition placing blanket restrictions on the whole population (apart from specified activities) for the purpose of limiting the spread of a disease. |
| Malaria | A parasitic disease that is spread to humans in endemic tropical areas by mosquitoes. |
| Marburg virus disease | A disease similar to Ebola that causes severe haemorrhagic fever and can spread from person to person via bodily fluids. |
| Mass testing | Using tests in a large number of asymptomatic people to detect those who are infected. |
| Middle East respiratory syndrome (MERS) | The disease caused by MERS-CoV. |
| Middle East respiratory syndrome coronavirus (MERS-CoV) | A respiratory virus with a reservoir in dromedary camels that can also spread from person to person. |
| Mitigation | A strategy aiming to use limited but effective interventions to delay and minimise the peak of waves of infections and to reduce their size. The goal is primarily to spread pressure on the healthcare system over a longer time period, while accepting that a similar number of people will become infected eventually. |
| Moral and Ethical Advisory Group | An advisory group that provided independent advice to the UK government on moral, ethical and faith considerations on health and social care related issues. Closed in October 2022. |
| Mortality rate | An expression of the number of deaths for a given cause divided by the whole population. |
| National Institute for Biological Standards and Control | A UK government agency that protects and improves public health by assuring the quality of biological medicines. |
| National Institute for Health and Care Research (NIHR) | One of the UK’s major funders of health and care research, which invests in pandemic preparedness research, clinical research infrastructure and ‘hibernated’ research projects. Until 2022, was known as the National Institute for Health Research. |
| National Resilience Standards | Non-statutory guidance for local responders issued by the Civil Contingencies Secretariat. |
| National Risk Assessment | The UK government’s main tool for identifying and assessing the most serious domestic emergencies facing the UK over a five-year timescale. It was combined with the National Security Risk Assessment in 2019. |
| National Risk Register | A public-facing version of the National Security Risk Assessment, aimed at providing detailed information for those with formal contingency planning responsibilities at a national and local level. |
| National Security Adviser | The central coordinator and adviser to the Prime Minister and members of the Cabinet on security, intelligence, defence and certain foreign policy matters. Leads the National Security Secretariat. |
| National Security Council | The main forum for collective discussion of the UK government’s objectives for national security. |
| National Security Council (Resilience) | A sub-Committee of the National Security Council that supports a strategic and closely coordinated cross-government approach to risks and opportunities facing the UK, specifically focused on resilience. |
| National Security Council (Threats, Hazards, Resilience and Contingencies) | A sub-Committee of the National Security Council that considered issues relating to security threats, hazards, resilience and civil contingencies. Effectively abolished in July 2019. |
| National Security Risk Assessment | The main tool for assessing the most serious civil contingency risks facing the UK. It assesses, compares and prioritises the top national-level risks, focusing on both the likelihood of the risk occurring and the impact it would have. |
| National Security Secretariat | A team providing coordination on security and intelligence issues of strategic importance across government. Advises the National Security Council and is headed by the National Security Adviser. |
| New and Emerging Respiratory Virus Threats Advisory Group (NERVTAG) | An expert scientific committee of the Department of Health and Social Care that advises the Chief Medical Officer and, through them, the UK government. It provides scientific risk assessment and mitigation advice on the threat posed by new and emerging respiratory viruses and on options for their management. |
| NHS England | An executive non-departmental public body, sponsored by the Department of Health and Social Care, that leads and oversees the NHS in England. |
| (NHS) Test and Trace | A service set up in May 2020 as part of the Department of Health and Social Care to provide Covid-19 testing and contact tracing. Working with local authorities, it contacted people who had tested positive and their recent contacts to advise them to self-isolate, as well as providing telephone monitoring and support. |
| Nipah | Can refer to the Nipah virus or the disease it causes. Its symptoms can include moderate to severe neurological and respiratory disease. Its main natural reservoir is fruit bats. Outbreaks have occurred in several South-East Asian countries, with transmission from pigs and bats, and with some person-to-person transmission reported. |
| Non-pharmaceutical interventions | Non-drug measures to limit the transmission of an infectious disease. These can be measures at the individual level, such as physical distancing, the use of face masks and coverings, and improved hygiene measures. They can also be measures to constrain activities, such as the closure of various premises, including sporting venues, pubs or shops. |
| Northern Ireland Covid-19 Bereaved Families for Justice | A branch of the UK-wide Covid-19 Bereaved Families for Justice. Represents bereaved family members of individuals who died from Covid-19 in Northern Ireland. |
| Northern Ireland Executive | The Northern Ireland Executive is the administrative branch of the Northern Ireland Assembly, the devolved legislature for Northern Ireland. It is responsible for matters including enterprise, trade and investment, agriculture and rural development, education, health, policing and justice, environment and regional development. |
| Northern Ireland Pandemic Flu Oversight Group | Established in 2018, it leads on health and social care preparedness and response, and oversees development of surge and triage guidance for the health and social care system in Northern Ireland. Chaired by the Director of Public Health. |
| Office for Budget Responsibility | An executive non-departmental public body, sponsored by the Treasury, that provides independent analysis of the UK’s public finances. |
| Office for National Statistics | The UK’s largest independent producer of official statistics and the recognised national statistical institute of the UK. |
| Operation Yellowhammer | The UK government’s contingency planning for a ‘no deal’ exit from the European Union. |
| Outbreak | The occurrence of cases of disease in excess of what would normally be expected in a defined community, geographical area or season. |
| Pandemic | An epidemic occurring worldwide, or over a very wide area, crossing international boundaries and usually affecting a large number of people. |
| Pandemic Diseases Capabilities Board | A cross-government board that worked to enhance preparedness for a wide range of pandemic disease scenarios. Replaced the Pandemic Flu Readiness Board in July 2021. |
| Pandemic Flu Readiness Board | A cross-government board set up to oversee pandemic influenza preparedness in light of the lessons learned from Exercise Cygnus. |
| Pandemic Influenza Preparedness Programme | Established by the Department of Health in 2007 as the umbrella programme for all activity to prepare for and respond to an influenza pandemic within the health and social care system |
| Pathogens | Infectious organisms, such as viruses, bacteria or parasites, that can produce a disease. |
| Paymaster General | A government minister who is officially responsible for making government payments. |
| Permanent secretary | A senior civil servant responsible for the day-to-day running of a government department. In the UK government and in Northern Ireland, there is a permanent secretary to each government department. There is a single permanent secretary to each of the Scottish and Welsh Governments. |
| Personal protective equipment (PPE) | Equipment that minimises exposure to hazards. In health and social care, it ranges from basic items, such as aprons, gowns and disposable gloves, to specialised items, such as face shields and respirator masks. |
| Preparedness and resilience | The extent to which the UK government and devolved administrations were ready for, and could withstand and adapt to an emergency such as the coronavirus (Covid-19) pandemic. |
| Prevalence | A measurement that expresses the proportion of people who have a disease at or during a given time period. Prevalence rates for disease are calculated by dividing the number of cases by the total number of people in the sample. |
| Prime Minister of the UK | The leader of the UK government, ultimately responsible for the policy and decisions of the UK government. |
| Public health | The science and art of preventing disease, prolonging life and promoting health through organised efforts of society. |
| Public Health Emergency of International Concern | A formal designation declared by the World Health Organization, giving a special status for an emergency caused by an infectious disease outbreak. The International Health Regulations specify that it is a serious, sudden, unusual or unexpected outbreak, which carries implications for public health beyond the affected state’s national border, and which may require immediate international action. |
| Public Health England | An executive agency of the Department of Health and Social Care until it was replaced by the UK Health Security Agency and Office for Health Improvement and Disparities in October 2021. It was responsible for all aspects of public health. |
| Public Health Laboratory Service | Established with the NHS in 1948 and oversaw a network of local, regional and national laboratories. Abolished in 2003 when its functions were taken over by the Health Protection Agency. |
| Public Health Scotland | Scotland’s national public health body, working to prevent disease, prolong healthy life, and promote health and wellbeing. |
| Public Health Wales | An NHS trust, which aims to protect and improve health and wellbeing, and reduce health inequalities in Wales. |
| Quarantine | A period of isolation to reduce the risk of incoming travellers transmitting infectious diseases. Quarantine is distinct from medical isolation, where people with a confirmed case of disease or their contacts are isolated. The two terms are often used interchangeably. |
| Reasonable worst-case scenario | A tool used for planning purposes to illustrate the worst manifestation of a risk that can reasonably be expected potentially to occur based on current information and data. |
| Regional Resilience Partnerships/Local Resilience Partnerships | Key planning and preparedness bodies on the ground in Scotland. Regional Resilience Partnerships support multi-agency coordination at a regional level and are made up of several Local Resilience Partnerships, which support local working arrangements and maintain local liaison. |
| Resilience and Emergencies Division (now called the Resilience and Recovery Directorate), Department for Levelling Up, Housing and Communities | Helped responders identify for themselves the risks they faced, how to mitigate those risks and how to manage the impact of risks that materialised. |
| Respiratory transmission | Transmission occurring via the mouth or nose from virus-containing droplets of any size. Respiratory transmission is sometimes divided into larger droplets, which fall to the ground more quickly, and smaller droplets, known as aerosols, which can remain suspended in the air for longer periods. |
| Rift Valley fever | A viral infection that can cause mild or more severe symptoms, including haemorrhagic fever. It is usually transmitted by contact with infected animal carcasses or from mosquito bites. Direct person-to-person transmission has not been reported. It has caused outbreaks across Africa and the Arabian Peninsula. |
| Risk | The possibility of a harmful event. In the context of civil emergency preparedness and resilience, an event, person or object that could cause loss of life or injury, damage to infrastructure, social and economic disruption, or environmental degradation. |
| Risk assessment | A systematic process for evaluating the likelihood of a potential risk occurring and the potential impact it would have if it were to happen. |
| Royal Academy of Engineering | A charity serving as a national Academy of Engineering and a Fellowship that provides leadership for engineering and technology, and technical leadership for wider society. |
| Royal College of Nursing | A nursing union and professional body. |
| Scenarios | A tool for risk assessment that involves developing models of what might happen in the future, identifying risk, and exploring uncertainty, consequences and interdependencies. |
| Scientific Advisory Group for Emergencies (SAGE) | An advisory group convened to provide independent scientific advice to support decision-making in COBR in the event of a national emergency. |
| Scientific Pandemic Infections Group on Modelling (SPI-M) | An advisory group of the Department of Health and Social Care that provides expert advice to the UK government based on infectious disease modelling and epidemiology. Until 2022, it was the Scientific Pandemic Influenza Group on Modelling. |
| Scientific Pandemic Infections Group on Modelling, operational sub- group (SPI-M-O) | An operational sub-group of the Scientific Pandemic Infections Group on Modelling that meets more regularly whenever there is a pandemic. It was set up during the 2009 to 2010 H1N1 influenza pandemic (‘swine flu’) and was stood up again during the Covid-19 pandemic. |
| Scientific Pandemic Insights Group on Behaviours (SPI-B) | An expert group that provides independent, expert, social and behavioural science advice to the Scientific Advisory Group for Emergencies (SAGE). |
| Scottish Covid Bereaved | A group representing bereaved relatives of individuals who died from Covid-19 in Scotland. |
| Scottish Government | The devolved administration for Scotland. |
| Scottish Resilience Partnership | A group of the most senior statutory responders and key resilience partners in Scotland. Provides collective assurance to Scottish ministers and statutory responders and gives advice to the resilience community on how best to ensure that Scotland is prepared to respond effectively to major emergencies. |
| Secretary of State | A Cabinet minister in charge of a government department. |
| Self-isolation | Staying at home or avoiding other people because of a suspected or confirmed infection. |
| Sensitivity | The probability that a person with a disease will receive a positive result on a diagnostic test. |
| Severe acute respiratory syndrome (SARS) | The disease caused by SARS-CoV-1. |
| Severe acute respiratory syndrome coronavirus 1 (SARS- CoV-1) | A coronavirus that causes severe acute respiratory syndrome. Considered to have emerged in 2002 from a wet market in the Guangdong Province of China. Closely related to SARS-CoV-2. |
| Severe acute respiratory syndrome coronavirus 2 (SARS- CoV-2) | The coronavirus that causes the Covid-19 disease (distinct from severe acute respiratory syndrome (SARS)). |
| Shielding | An intervention introduced to support those who are clinically extremely vulnerable and therefore considered to be most at risk of serious illness from, for example, Covid-19. |
| Side effects | Unwanted effects that occur during use of a drug or vaccine, such as pain at the injection site of a vaccine. |
| Social distancing | Measures to reduce the contact people have with each other, which may include temporarily reducing socialising in public places, such as entertainment or sports events, reducing the use of non- essential public transport, or recommending more home working. |
| Social enterprise | A business with primarily social objectives whose surpluses are principally reinvested for that purpose in the business or in the community, rather than being driven by the need to maximise profit for shareholders and owners. |
| Society of Local Authority Chief Executives (Solace) Cymru | The Welsh branch of the Society of Local Authority Chief Executives and Senior Managers, a membership network for public sector and local government professionals. |
| Spanish flu | The largest recorded influenza pandemic, which began in 1918. |
| Suppression | A more extreme form of mitigation, along the lines of a lockdown, that aims to quash transmission completely. |
| Surge capacity | The ability of a healthcare system to manage and respond to unpredictable and sudden increases in demand for healthcare services. |
| Swine flu | A relatively mild influenza pandemic, which began in 2009. |
| Symptomatic | Showing symptoms following an infection. |
| Therapeutics | A drug used to treat rather than prevent a disease. |
| Trades Union Congress | A federation of trade unions in England and Wales. |
| Transmissibility | The ability of a pathogen, such as a virus, to spread from one person to another. |
| Transmission | The process by which a pathogen, such as a virus, spreads from one infected person to another. |
| The Treasury (HM Treasury) | A ministerial government department that acts as the economic and finance ministry, maintaining control over public spending and setting the direction of UK economic policy. |
| UK government | The central government for the UK, headed by the Prime Minister. The UK government is responsible for non-devolved policy matters across the UK. (The Scottish Government, Welsh Government and Northern Ireland Executive are separate from the UK government and are responsible for devolved policy matters in their respective nations.) |
| UK Health Security Agency | An executive agency, established in April 2021 and sponsored by the Department of Health and Social Care, responsible for public health protection and infectious disease capability. |
| UK Influenza Pandemic Preparedness Strategy 2011 | The UK’s emergency response strategy for dealing with an influenza pandemic. |
| UK National Statistician | The principal adviser on official statistics to the UK government. |
| UK Vaccine Network | A network of industry, academia and relevant funding bodies to advise the Department of Health and Social Care on research and development investment relating to infectious diseases with the potential to cause an epidemic in low and middle-income countries. |
| UK Zoonoses, Animal Diseases and Infections Group | An independent committee made up of experts from across the agricultural and public health departments that provides a strategic overview to ensure overall coordination of public health. |
| Vaccination | Protecting individuals from a disease by treating them with a vaccine. |
| Vaccine | Vaccines train the immune system to recognise a pathogen and to defend the body from it at the next encounter. |
| Ventilation | The process of introducing fresh air into indoor spaces while removing stale air. |
| Ventilator | A life support machine used to mechanically support breathing by pumping air into a patient’s lungs. |
| Virology | The scientific and medical discipline concerned with understanding the biology of viruses and viral diseases, their treatment and prevention. |
| Virus | A parasitic infectious agent that replicates only inside the cells of an organism. |
| Wet market | A market at which live animals are sold. |
| Whole-system civil emergencies | The most complex civil emergencies, which require a cross- departmental approach by government to preparedness and response. |
| World Health Organization | A specialised agency of the United Nations responsible for international public health. |
| Zika | Can refer to the Zika virus or the disease it causes. A mosquito- borne virus that causes a very mild illness for most infected people, but in pregnant women can lead to serious brain defects in an unborn baby. |
| Zoonotic disease (zoonosis) | Diseases caused by pathogens that originated from animals other than humans. |
| Zoonotic spillover | The process by which a pathogen is transmitted from animals to humans. |
Appendix 4: List of recommendations made in this Report
| A4.1. | In this Report concerning Module 1, the Inquiry makes 10 recommendations relating to the resilience and preparedness of the UK. |
Recommendation 1: A simplified structure for whole-system civil emergency preparedness and resilience
The governments of the UK, Scotland, Wales and Northern Ireland should each simplify and reduce the number of structures with responsibility for preparing for and building resilience to whole-system civil emergencies.
The core structures should be:
- a single Cabinet-level or equivalent ministerial committee (including the senior minister responsible for health and social care) responsible for whole-system civil emergency preparedness and resilience for each government, which meets regularly and is chaired by the leader or deputy leader of the relevant government; and
- a single cross-departmental group of senior officials in each government (which reports regularly to the Cabinet-level or equivalent ministerial committee) to oversee and implement policy on civil emergency preparedness and resilience.
This should be put in place within 12 months of the publication of this Report.
Within 6 months of the creation of the group of senior officials, it should complete a review to simplify and reduce the number of structures responsible for whole- system civil emergency preparedness and resilience.
Subsequently, within 24 months of the publication of this Report, the ministerial committee should rationalise and streamline subordinate or supporting groups and committees responsible for whole-system civil emergency preparedness and resilience. Any groups and committees retained or created to support this core structure should have a clear purpose and should report regularly about progress with, and completion of, tasks assigned to them.
Recommendation 2: Cabinet Office leadership for whole-system civil emergencies in the UK
The UK government should:
- abolish the lead government department model for whole-system civil emergency preparedness and resilience; and
- require the Cabinet Office to lead on preparing for and building resilience to whole-system civil emergencies across UK government departments, including monitoring the preparedness and resilience of other departments, supporting departments to correct problems, and escalating issues to the UK Cabinet-level ministerial committee and group of senior officials in Recommendation 1.
Recommendation 3: A better approach to risk assessment
The UK government and devolved administrations should work together on developing a new approach to risk assessment that moves away from a reliance on single reasonable worst-case scenarios towards an approach that:
- assesses a wider range of scenarios representative of the different risks and the range of each kind of risk;
- considers the prevention and mitigation of an emergency in addition to dealing with its consequences;
- provides a full analysis of the ways in which the combined impacts of different risks may complicate or worsen an emergency;
- assesses long-term risks in addition to short-term risks and considers how they may interact with each other;
- undertakes an assessment of the impact of each risk on vulnerable people; and
- takes into account the capacity and capabilities of the UK.
In doing so, the UK government and devolved administrations should perform risk assessments that reflect the circumstances and characteristics particular to England, Wales, Scotland, Northern Ireland and the UK as a whole.
Recommendation 4: A UK-wide whole-system civil emergency strategy
The UK government and devolved administrations should together introduce a UK-wide whole-system civil emergency strategy (which includes pandemics) to prevent each emergency and also to reduce, control and mitigate its effects.
As a minimum, the strategy should:
- be adaptable;
- include sections dedicated to each potential whole-system civil emergency – for example, one on pandemics with a clear explanation of the roles and responsibilities of the UK government, devolved administrations and their departments/directorates as well as local responders;
- consider a wide range of potential scenarios for each type of emergency;
- identify the key issues and set out a range of potential responses;
- identify how the strategy is to be applied to ensure that any potential responses are proportionate to the particular circumstances of the emergency;
- include an assessment in the short, medium and long term, based on published modelling, of the potential health, social and economic impacts of the emergency and of potential responses to the emergency on the population and, in particular, on vulnerable people; and
- include an assessment of the infrastructure, technology and skills the UK needs to respond effectively to the emergency and how those needs might change for different scenarios.
The strategy should be subject to a substantive reassessment at least every three years to ensure that it is up to date and effective, incorporating lessons learned between reassessments.
Recommendation 5: Data and research for future pandemics
The UK government, working with the devolved administrations, should establish mechanisms for the timely collection, analysis, secure sharing and use of reliable data for informing emergency responses, in advance of future pandemics. Data systems should be tested in pandemic exercises.
The UK government should also commission a wider range of research projects ready to commence in the event of a future pandemic. These could be ‘hibernated’ studies or existing studies that are designed to be rapidly adapted to a new outbreak. Better working with international partners should be encouraged. This should include projects to:
- understand the prevalence of a new virus;
- measure the effectiveness of a range of different public health measures; and
- identify which groups of vulnerable people are hardest hit by the pandemic and why.
Recommendation 6: A regular UK-wide pandemic response exercise
The UK government and devolved administrations should together hold a UK-wide pandemic response exercise at least every three years.
The exercise should:
- test the UK-wide, cross-government, national and local response to a pandemic at all stages, from the initial outbreak to multiple waves over a number of years;
- include a broad range of those involved in pandemic preparedness and response; and
- consider how a broad range of vulnerable people will be helped in the event of a pandemic.
Recommendation 7: Publication of findings and lessons from civil emergency exercises
For all civil emergency exercises, the governments of the UK, Scotland, Wales and Northern Ireland should each (unless there are reasons of national security for not doing so):
- publish an exercise report summarising the findings, lessons and recommendations, within three months of the conclusion of the exercise;
- publish an action plan setting out the specific steps that will be taken in response to the report’s findings, and by which entity, within six months of the conclusion of the exercise; and
- keep exercise reports, action plans, and emergency plans and guidance from across the UK in a single, UK-wide online archive, accessible to all involved in emergency preparedness, resilience and response.
Recommendation 8: Published reports on whole-system civil emergency preparedness and resilience
The governments of the UK, Scotland, Wales and Northern Ireland should each produce and publish reports to their respective legislatures at least every three years on whole-system civil emergency preparedness and resilience.
The reports should include as a minimum:
- the risks that each government has identified are likely to result in whole-system civil emergencies;
- the recommendations that have been made to each government to mitigate those risks, and whether these recommendations have been accepted or rejected;
- a cost–benefit analysis setting out the economic and social costs of accepting the risks as against taking action to mitigate the risks;
- who may be vulnerable to the risks and what steps are being taken to mitigate those risks;
- a plan setting out the timescales for implementing the recommendations that have been accepted; and
- an update on the progress that has been made on implementing previously accepted recommendations.
Recommendation 9: Regular use of red teams
The governments of the UK, Scotland, Wales and Northern Ireland should each introduce the use of red teams in the Civil Service to scrutinise and challenge the principles, evidence, policies and advice relating to preparedness for and resilience to whole-system civil emergencies. The red teams should be brought in from outside of government and the Civil Service.
Recommendation 10: A UK-wide independent statutory body for whole-system civil emergency preparedness and resilience
The UK government should, in consultation with the devolved administrations, create a statutory independent body for whole-system civil emergency preparedness and resilience.
The new body should be given responsibility for:
- providing independent, strategic advice to the UK government and devolved administrations on their planning for, preparedness for and building resilience to whole-system civil emergencies;
- consulting with the voluntary, community and social enterprise sector at a national and local level and directors of public health on the protection of vulnerable people in whole-system civil emergencies;
- assessing the state of planning for, preparedness for and resilience to whole-system civil emergencies across the UK; and
- making recommendations on the capacity and capabilities that will be required to prepare for and build resilience to whole-system civil emergencies.
As an interim measure, the new body should be established on a non-statutory basis within 12 months of this Report, so that it may begin its work in advance of legislation being passed.
E03069239
Alternative formats
This report is also available in a range of other formats.