Ang ilan sa mga kuwento at tema na kasama sa talaang ito ay kinabibilangan ng mga paglalarawan ng kamatayan, mga karanasang malapit nang mamatay, makabuluhang pisikal at sikolohikal na pinsala at mga pagtukoy sa mga karanasan ng pang-aabuso. Ang ilan sa mga paglalarawang ito ay nauugnay din sa mga karanasan ng mga bata. Ang mga kwentong ito ay maaaring nakababahalang basahin. Kung gayon, hinihikayat ang mga mambabasa na humingi ng tulong mula sa mga kasamahan, kaibigan, pamilya, grupo ng suporta o mga propesyonal sa pangangalagang pangkalusugan kung kinakailangan. Ang isang listahan ng mga suportang serbisyo ay ibinibigay din sa UK Covid-19 Inquiry website.
Paunang salita
Ito ang pangatlong tala ng Every Story Matters, na ginawa para sa imbestigasyon ng Module 7: Test, Trace at Isolate para sa Covid-19 Inquiry. Ang lahat ng mga tala ng Every Story Matters ay isinumite bilang ebidensya sa Chair of the Inquiry, Baroness Hallett, at magiging bahagi ng opisyal na pampublikong rekord ng Inquiry.
Ang Bawat Story Matters ay idinisenyo upang tipunin at maunawaan ang karanasan ng tao sa pandemya sa United Kingdom. Maraming libu-libong tao ang nagbahagi ng kanilang mga kuwento sa amin, at gusto naming pasalamatan ang mga taong naglaan ng oras upang gawin ito. Ang tungkulin ng Bawat Story Matters bilang isang 'pagsasanay sa pakikinig' ay nangangahulugan na ang halaga nito ay nasa pagdinig ng isang hanay ng mga karanasan, pagtukoy sa mga tema kung saan posible at, mahalaga, pagtiyak na ang mga karanasan ng mga tao ay bahagi ng pampublikong rekord ng Inquiry at maaaring isaalang-alang kapag bumubuo ng mga rekomendasyon. Dapat nating maunawaan ang epekto ng pandemya upang makagawa ng mga rekomendasyon na makakabawas sa mga pinsala mula sa isang pandemya sa hinaharap.
Titingnan ng Module 7 ang diskarte sa pagsubok, pagsubaybay at paghihiwalay sa panahon ng pandemya na pinagtibay ng Pamahalaan ng UK at mga devolved na administrasyon sa Northern Ireland, Scotland at Wales. Ang modyul ay tuklasin ang mga patakaran, estratehiya at desisyong ginawa ng mga pangunahing katawan at salik na maaaring nakaimpluwensya sa pampublikong pagsunod sa mga opisyal na alituntunin. Ang Bawat Story Matters ay nagdaragdag ng kakaibang pananaw ng tao, tinutuklas ang papel ng pag-uugali at karanasan ng mga tao sa loob ng konteksto ng sistemang ito ng pagsubok, pagsubaybay at paghihiwalay. Ang malinaw ay maraming tao ang nadala ng pagnanais na protektahan ang mga tao sa kanilang paligid, kabilang ang mga mas mahina.
Nagpapasalamat kami sa mga indibidwal, grupo at organisasyon na nagbigay sa amin ng feedback, ideya at tumulong sa amin na makarinig mula sa malawak na hanay ng mga tao. Kabilang sa mga ito ang: Long Covid Kids, Long Covid Scotland, Long Covid SOS, Long Covid Support, Clinically Vulnerable Families, SignHealth at ang Royal National Institute of Blind People. Ang bawat isa sa mga grupong ito ay nagbigay-daan sa amin na makipag-usap sa kanilang mga miyembro at matiyak na ang kanilang mga karanasan ay bahagi ng talaang ito.
Isang pribilehiyo na magtrabaho sa kakaibang aspetong ito ng Pagtatanong sa Covid-19.
Ang koponan ng Every Story Matters
Pangkalahatang-ideya
Ang maikling buod na ito ay nagbibigay ng mataas na antas na pangkalahatang-ideya ng mga tema mula sa maraming kuwentong narinig namin kaugnay ng pagsubok, pagsubaybay sa pakikipag-ugnayan at pag-iisa sa sarili sa panahon ng pandemya.
Paano sinuri ang mga kwento
Ang bawat kuwentong ibinahagi sa Inquiry ay sinusuri at mag-aambag sa isa o higit pang may temang mga dokumentong tulad nito. Ibinahagi ng mga tao ang kanilang mga karanasan sa Inquiry sa iba't ibang paraan. Ang mga kwentong naglalarawan ng mga karanasan ng pagsubok, pagsubaybay sa pakikipag-ugnay at pag-iisa sa sarili sa panahon ng pandemya ay pinagsama-sama at sinuri upang i-highlight ang mga pangunahing tema. Sa buod:
- Sinuri namin ang 44,775 na kwentong isinumite online sa Inquiry sa oras na isinulat ang rekord na ito, gamit ang natural language processing (NLP) at sinusuri at coding ng mga mananaliksik ang ibinahagi ng mga tao.
- Pinagsama-sama ng mga mananaliksik ang mga tema mula sa 340 na kwento ng mga tao na ibinahagi sa mga panayam sa pananaliksik at mga talakayan ng grupo.
- Ang mga mananaliksik ay gumuhit din ng mga tema mula sa Every Story Matters na mga kaganapan sa pakikinig kasama ang publiko at mga grupo ng komunidad sa mga bayan at lungsod sa buong England, Scotland, Wales at Northern Ireland. Gumawa kami ng punto ng pagsasalita sa mga miyembro ng mga pangunahing grupo kung saan gustong marinig ng Inquiry legal team.
Ang higit pang mga detalye tungkol sa kung kanino namin narinig at kung paano pinagsama-sama at sinuri ang mga kuwento ng mga tao sa talaang ito ay kasama sa apendiks. Ang dokumentong ito ay sumasalamin sa iba't ibang mga karanasan nang hindi sinusubukang ipagkasundo ang mga ito; kinikilala namin na ang karanasan ng bawat isa ay natatangi.
Sa buong talaan, tinukoy namin ang mga taong nagbahagi ng kanilang mga kuwento sa Every Story Matters bilang 'mga contributor'. Ito ay dahil may mahalagang papel sila sa pagdaragdag sa ebidensya ng Inquiry at sa opisyal na rekord ng pandemya. Kung naaangkop, inilarawan din namin ang higit pa tungkol sa kanila (halimbawa, mga taong may iba't ibang kapansanan o kondisyon ng kalusugan) o ang dahilan kung bakit ibinahagi nila ang kanilang kuwento (halimbawa, bilang mga tagapag-alaga o magulang). Ito ay upang makatulong na ipaliwanag ang konteksto ng kanilang kuwento.
Ang ilang mga kuwento ay ginalugad nang mas malalim sa pamamagitan ng mga quote at case study. Pinili ang mga ito upang i-highlight ang mga partikular na karanasan at ang epekto ng mga ito sa mga tao. Ang mga quote at case study ay nakakatulong sa pag-ground ng record sa kung ano ang ibinahagi ng mga tao sa Inquiry sa sarili nilang mga salita. Ang mga kontribusyon ay hindi nagpapakilala. Gumamit kami ng mga pseudonym para sa mga case study na nakuha mula sa mga panayam sa pananaliksik. Ang mga karanasang ibinahagi ng ibang mga pamamaraan ay walang mga pseudonym.
Pag-unawa at kamalayan ng Test, Trace at Isolate
Marami sa mga nagbahagi ng kanilang mga kuwento ang nagsabi sa amin na ang patnubay ay malinaw na may kaugnayan sa kung kailan magsusuri para sa Covid-19 at kung kailan maghihiwalay sa sarili. Habang umiral ang ilang pagkalito tungkol sa pag-alam sa pagkakaiba sa pagitan ng mga sintomas ng Covid-19 at iba pang katulad na sakit, tulad ng sipon at trangkaso, ang kamalayan at kumpiyansa sa kakayahang matukoy ang mga sintomas ay lumago sa panahon ng pandemya.
| “ | Sa pag-unlad nito sa paglipas ng panahon, naiintindihan namin kung kailan namin kailangan na subukan. Ito ay medyo malinaw.
– Kontribyutor ng Every Story Matters |
Ilang nag-ambag ang kumuha ng dalawang beses-lingguhang mabilis na pagsusuri nang maging available ito sa lahat noong Abril 2021 at ang ilan ay nahirapan sa katwiran para sa pagsusuri nang walang mga sintomas. Ang pagsubok na walang mga sintomas ay nauugnay sa kinakailangang gawin ito o dahil sa isang pangangailangan o pagnanais na makihalubilo sa iba.
Ang kamalayan at pag-unawa sa patnubay tungkol sa pagsubaybay sa contact ay hindi gaanong kalat. Narinig namin na mas mahirap maunawaan ang layunin ng pagsubaybay sa pakikipag-ugnay at kung paano sundin nang tama ang gabay.
Ang kamalayan sa pinansiyal at praktikal na suporta upang matulungan ang mga tao kapag ang pagbubukod sa sarili ay medyo mababa din.
| “ | Oo, hindi ko alam kung paano ito hahanapin, o kung ano pa man. Sa tingin ko, hindi naging maayos, malawak. Ang impormasyon para sa [pinansyal na tulong] ay hindi masyadong kumalat, dahil wala akong natatandaan tungkol sa £500.”
– Clinically vulnerable na tao |
Ang mga pagbabago sa opisyal na patnubay ng pamahalaan ay nagdulot ng pagkalito sa mga tao tungkol sa kung kailan magsusuri at maghihiwalay sa sarili. Nangangahulugan ang kawalan ng katiyakan tungkol sa mga alituntuning ipinatupad sa anumang oras, na, sa bandang huli ng pandemya, nagpasya ang ilang tao na gawin kung ano ang sa tingin nila ay angkop kahit na ito ay naaayon o hindi sa mga panuntunan.
| “ | Nakaramdam lang ako ng pagkalito sa buong bagay kung kailan kami dapat mag-test, sa anong yugto mo dapat subukan [...] patuloy nilang binabago ang mga patakaran tungkol dito."
– Kontribyutor ng Every Story Matters |
Ano ang nakatulong o naghikayat sa mga tao na lumahok sa pagsusuri, pagsubaybay sa pakikipag-ugnayan at pag-iisa sa sarili?
Maraming dahilan kung bakit handa ang mga tao na subukan at ihiwalay ang sarili, at maraming paraan ng pagtulong at paghikayat sa kanila na gawin ito.
- Pagprotekta sa mga taong pinapahalagahan nila: Para sa marami, ang pakiramdam ng moral na tungkulin na protektahan ang kanilang mga mahal sa buhay, ang kanilang mga komunidad at ang mga taong mahina ay nag-udyok sa kanila na makilahok sa pagsubok, pagsubaybay sa pakikipag-ugnay at pag-iisa sa sarili.
| “ | Ito ay [pag-iisa sa sarili] isa sa ilang bagay na may katuturan, dahil ang talagang ginagawa mo ay pinoprotektahan mo ang mga taong pinapahalagahan mo."
– Tagapag-alaga |
- Mga kinakailangan: Ang ilang mga tao ay kinakailangang magpasuri (anuman ang mga sintomas) bago pumasok sa trabaho at makipag-ugnayan sa ibang tao. Inilarawan ito ng ilan bilang bahagi ng kanilang 'tungkulin ng pangangalaga' na protektahan ang iba.
- Access sa suporta: Para sa ilan, ang suporta na kanilang natanggap - mula sa pamilya at mga kaibigan, mga lokal na organisasyon at mga grupo ng komunidad - ay nagbigay-daan sa kanila na makisali sa pagsubok, pagsubaybay sa pakikipag-ugnay at upang ihiwalay ang sarili.
| “ | Ang aming mga lokal na tindahan ay kamangha-mangha sa pag-aayos ng mga paghahatid ng pagkain para sa amin. Kami ay mapalad na nakatira sa isang rural na lugar at maaaring gumugol ng oras sa hardin. Ngunit sa palagay ko ito ay isang mas positibong karanasan kaysa sa inaasahan namin. Minsan sinasabi ng anak ko na nami-miss niya ang closeness na iyon.”
– Kontribyutor ng Every Story Matters |
- Kalayaan: Sa paglipas ng panahon, ang pagnanais na pumasok sa mga paaralan, kolehiyo at unibersidad, maglakbay at makihalubilo at makihalubilo sa iba ay naging dahilan ng pagsubok.
| “ | Sasabihin ko na naging mas mahalaga ang pagsubok, bilang isang pagsasanay. […] at lalo na […] kung ang mga tao ay bumibisita sa amin o […] Gusto kong […] makakita ng ibang tao, ang pagsubok para sa aking sarili at ang paghiling sa lahat na gawin iyon ay naging talagang mahalaga. Malamang na mas mahalaga kaysa makita sila, sa totoo lang."
– Miyembro ng pamilya o tagasuporta ng isang tao na kinakailangang ihiwalay ang sarili |
- Pag-alis ng takot: Ang mga tao ay natatakot na mahawaan ang virus at maging malubha o maipasa ito at sa gayon ay nasubok, nakikibahagi sa pagsubaybay sa pakikipag-ugnay at nag-iisa sa sarili.
- Access at kaginhawaan: Kung saan ang mga testing center ay madaling puntahan, at ang pagkakaroon ng mga appointment ay mabuti, nakita ng mga tao na madaling magpasuri. Nang ang Lateral Flow Tests (LFTs) ay ginawang available sa lahat ng tao noong Abril 2021, marami ang malugod na tinanggap ang kadalian at kaginhawahan ng mga libreng kit para masuri sa bahay.
| “ | Ang mga test center at vaccination center ay talagang madaling mag-book ng mga appointment at lahat ay nasa loob ng maikling distansya ng paglalakbay.
– Kontribyutor ng Every Story Matters |
Ano ang mga hadlang sa mga taong lumahok sa pagsubok, pagsubaybay sa pakikipag-ugnay at pag-iisa sa sarili?
Mayroong maraming mga tema na huminto o nagpahirap sa mga tao na mag-test, makipag-ugnayan sa pagsubaybay sa pakikipag-ugnay at upang ihiwalay ang sarili kapag kailangan nila.
- Tiwala: Ang pag-aalinlangan at kawalan ng tiwala ay lumago habang ang mga tao ay nakaranas ng mga problema sa pagsubok at pagsubaybay sa pakikipag-ugnay dahil inakala nila na sila ay hindi tumpak o hindi epektibo.
| “ | Hindi pa ako nakapagpositibo sa isang lateral flow test, ngunit alam ko na ang mga ito ay hindi na akma para sa layunin, at sa halip ay alam kong mayroon akong Covid dahil sa mga nakapaligid sa akin na may parehong mga sintomas na sumusubok na positibo sa oras na iyon.
– Kontribyutor ng Every Story Matters |
- Pagdama ng panganib: Kung gaano kalaki ang personal na panganib na kumportable ng mga tao ay nakaimpluwensya sa kanilang pakikibahagi sa pagsubok, pagsubaybay sa pakikipag-ugnay at pag-uugali sa pag-iisa sa sarili, at nagbago ito sa buong pandemya.
| “ | Dumating sa punto [na] lahat ay nagsawa na, kasama ko […] na parang ikaw lang, 'O, tuloy ang buhay.' Parang, hindi ka mabubuhay ng ganito sa natitirang bahagi ng iyong buhay, […] unti-unti mo nang nabawasan ang pansin. Hindi sa hindi pa rin ako mag-iingat hanggang sa isang lawak, ngunit hindi katulad ng magiging sukat ko sa unang dalawang taon.”
– Kontribyutor ng Every Story Matters |
- Access: Kung saan nakaranas ang mga tao ng mga hadlang sa pag-access (halimbawa, pag-book ng PCR test kapag mahirap i-navigate o i-access ang mga LFT sa system sa panahon ng kakulangan ng supply), mas mahirap ang pagsubok para sa Covid-19, at nagdulot ng pag-aalala at paghihirap.
| “ | Ang mga sentro ng pagsubok sa Covid ay maayos at mabuti kung madaling ma-access ng mga tao ang mga ito, na magagawa ko lamang sa pamamagitan ng paglalakbay sa pamamagitan ng hindi bababa sa dalawang uri ng pampublikong sasakyan habang nakahiwalay."
– Kontribyutor ng Every Story Matters |
- Accessibility at pagsasama: Ang mga hadlang ay lumitaw kung saan ang mga testing center ay hindi naa-access ng mga tao, kung saan ang mga tagubilin sa LFT kit ay mahirap maunawaan at gamitin, at kung saan ang mga tao ay hindi kasama sa mga digital na anyo ng pagsubaybay sa contact.
| “ | Napakaraming komunidad ang hindi marunong bumasa at sumulat, at sila ay umaasa sa mga miyembro ng pamilya upang gawin ito ng marami para sa kanila.”
– Taong mula sa pinagmulang etniko ng Roma |
- Kahirapan sa paggamit: Narinig din namin na ang mga tao ay nakaranas ng mga hadlang sa paggamit ng mga LFT nang tama, pagbibigay kahulugan sa mga resulta at paglipat sa pagitan ng iba't ibang variation ng mga test kit.
- Mga negatibong epekto: Sinabi sa amin ng mga tao ang tungkol sa mga negatibo, o potensyal na negatibo, na mga epekto kapag nakikibahagi sa pagsusuri, pagsubaybay sa pakikipag-ugnayan at pag-iisa sa sarili. Kabilang dito ang pagkawala ng personal na kalayaan, mga epekto sa kapakanan ng mga tao – kabilang ang kakulangan sa ginhawa at pagkabalisa mula sa pagsubok – at ang mga hamon ng pag-iisa sa sarili.
| “ | Ilang Covid test lang ang ginawa ko – kung may nakita akong mas hindi kasiya-siya kaysa sa pagbabakuna.”
– Kontribyutor ng Every Story Matters |
- Mga kaayusan sa pamumuhay: Para sa ilan, hindi palaging praktikal na sundin ang patnubay - lalo na tungkol sa pag-iisa sa sarili - halimbawa, kung nakatira sila sa mas maliliit o masikip na bahay.
- Kakulangan ng panlipunang suporta at insentibo: Kung saan walang access ang mga tao sa suportang panlipunan, nahirapan silang makisali sa pagsubok, pagsubaybay sa contact at pag-iisa sa sarili. Ang katotohanan na ang pag-uulat ng mga resulta ng pagsusulit ay hindi kinokontrol ay nangangahulugan na ang ilan ay nagtanong sa halaga ng pagsubok sa unang lugar.
| “ | Ang pag-upload ng mga resulta ng pagsusulit ay isang komedya rin dahil maaari kong i-upload ang mga resulta ng pagsusulit ng aking kapitbahay [natatawa]. Walang garantiya na iyon ang aking mga resulta. Ganap na kalokohan.”
– Kontribyutor ng Every Story Matters |
Ang mga karanasan ng mga magulang, mga sumuporta sa iba at mga nakaligtas sa pang-aabuso sa tahanan
Narinig namin mula sa maraming iba't ibang tao na nag-uusap tungkol sa kanilang mga karanasan sa pagsubok, pagsubaybay sa contact at pag-iisa sa sarili. Sa kabanatang ito, nakatuon tayo sa mga kuwento ng mga taong nahirapan sa mga aspetong ito ng pandemya. Kabilang dito ang mga magulang na kinailangang subukan ang maliliit na bata at mga nakaligtas sa pang-aabuso sa tahanan na kinailangang ihiwalay ang sarili sa mga kasosyo na nang-abuso sa kanila at/o hindi sumunod sa mga patakaran.
Mga mungkahi para sa mga pagpapabuti para sa hinaharap
Kapag iniisip kung paano mapapabuti ang pagsubok, pagsubaybay sa pakikipag-ugnayan at pag-iisa sa sarili sa isang pandemya sa hinaharap, sinabi ng mga kontribyutor na maaaring makatulong ang sumusunod:
- Higit na pagkakapare-pareho at kalinawan sa mga patakaran at pagmemensahe ng gobyerno sa mga bansang nakipag-devolve
- Higit pang pampublikong edukasyon sa pangangailangan para sa pagsubok, pagsubaybay sa pakikipag-ugnay at pag-iisa sa sarili
- Pinahusay na access sa suporta sa kalusugan ng isip at pinansyal at praktikal na suporta para sa mga tao sa mga panahon ng pag-iisa sa sarili
- Mas mahusay na paggamit ng mga pinuno ng komunidad sa pagpapalaganap ng impormasyon sa mga komunidad
- Mga alternatibong opsyon para sa digitally ibinukod na mga tao at sa mga nakatira sa liblib o rural na lugar
- Magagamit na impormasyon sa iba't ibang wika at format
Buong record
1. Panimula
Inilalahad ng dokumentong ito ang mga kwentong ibinahagi sa Every Story Matters na may kaugnayan sa Covid-19 testing, contact tracing at self-isolation.
Background at layunin
Ang Every Story Matters ay isang pagkakataon para sa mga tao sa buong UK na ibahagi ang kanilang karanasan sa pandemya sa UK Covid-19 Inquiry. Ang bawat kwentong ibinahagi ay susuriin at ang mga insight na nakuha ay gagawing mga may temang dokumento para sa mga nauugnay na module ng Inquiry. Ang mga talaang ito ay isinumite sa Pagtatanong bilang ebidensya. Sa paggawa nito, ang mga natuklasan at rekomendasyon ng Inquiry ay ipapaalam ng mga karanasan ng mga naapektuhan ng pandemya.
Pinagsasama-sama ng dokumentong ito ang sinabi sa amin ng mga nag-aambag tungkol sa kanilang mga karanasan sa pagsusuri sa Covid-19, pagsubaybay sa pakikipag-ugnayan at pag-iisa sa sarili sa panahon ng pandemya. Para sa rekord na ito, ang self-isolation ay tumutukoy sa isang taong naghihiwalay pagkatapos makatanggap ng positibong resulta ng pagsusuri sa Covid-19 o isang abiso tungkol sa isang malapit na contact na mayroong Covid-19 sa pamamagitan ng contact tracing system. Habang ang mga indibidwal na pinayuhan na mag-shield ay kinapanayam, ang mga panayam ay nag-explore ng kanilang pakikipag-ugnayan sa Test, Trace at Isolate system, hindi ang kanilang mga karanasan na may kaugnayan sa shielding.1 Ang tala na ito ay hindi kasama ang mga karanasan ng pagiging nakahiwalay o mga pakiramdam ng paghihiwalay bilang resulta ng isang pambansang lockdown.
Isinasaalang-alang ng UK Covid-19 Inquiry ang iba't ibang aspeto ng pandemya at kung paano ito nakaapekto sa mga tao. Nangangahulugan ito na ang ilang mga paksa ay tatalakayin sa iba pang mga tala ng module. Samakatuwid, hindi lahat ng karanasang ibinahagi sa Every Story Matters ay kasama sa dokumentong ito. Halimbawa, ang mga karanasan ng UK healthcare system at mga karanasan ng mga bakuna at therapeutics ay ginalugad sa iba pang mga module at kasama sa iba pang mga tala ng Every Story Matters. Matuto pa tungkol sa Bawat Kwento ay Mahalaga at basahin ang nakaraan mga tala.
Paano ibinahagi ng mga tao ang kanilang mga karanasan
Mayroong ilang iba't ibang paraan kung paano namin nakolekta ang mga kuwento ng mga tao para sa Modyul 7, ang mga ito ay nakalista sa ibaba.
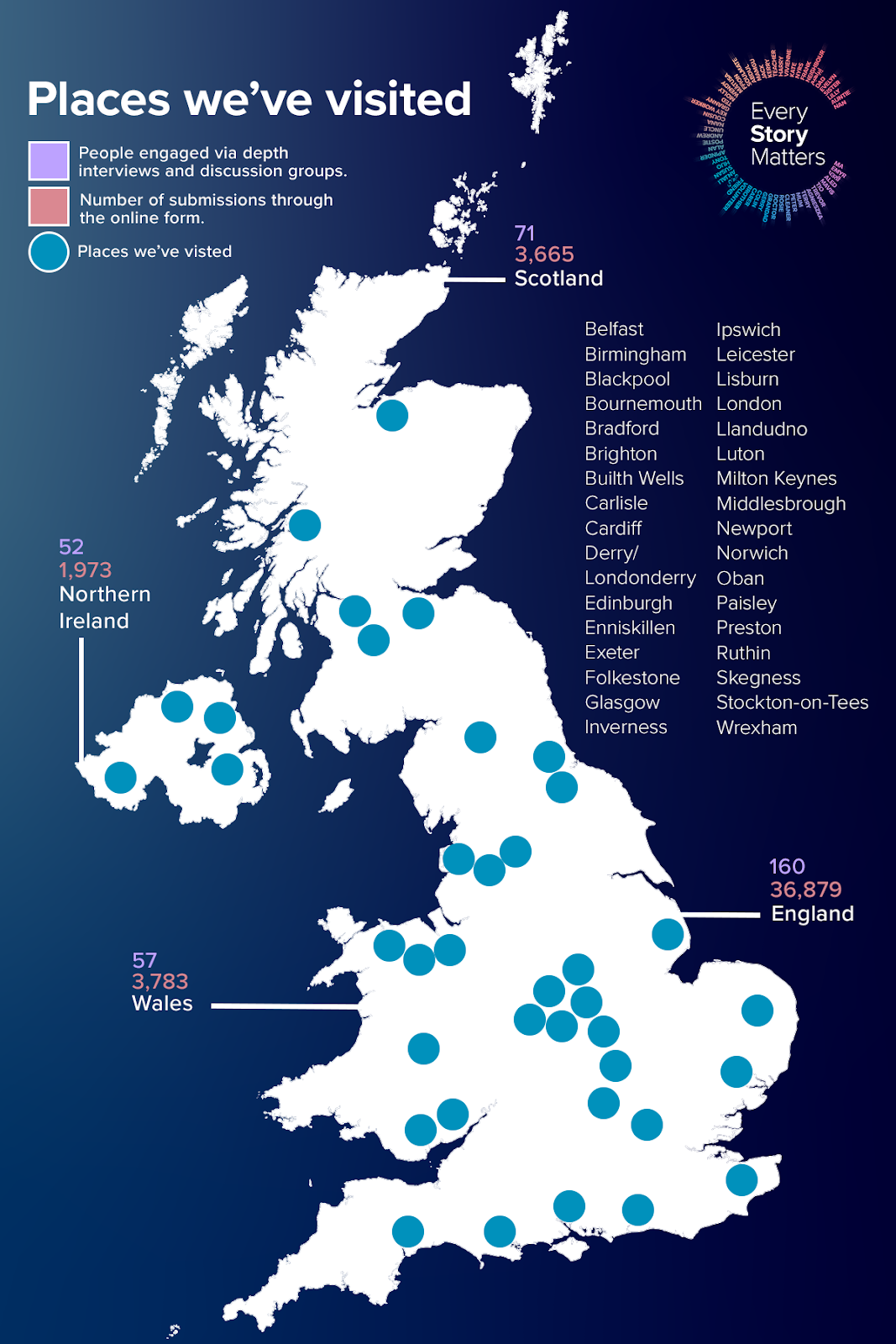
- Ang mga miyembro ng publiko ay inanyayahan upang kumpletuhin ang isang online na form sa pamamagitan ng website ng Inquiry (mga papel na form ay inaalok din sa mga kontribyutor at kasama sa pagsusuri). Hiniling nito sa kanila na sagutin ang tatlong malawak at bukas na mga tanong tungkol sa kanilang karanasan sa pandemya. Ang form ay nagtanong ng iba pang mga katanungan upang mangolekta ng background na impormasyon tungkol sa kanila (tulad ng kanilang edad, kasarian at etnisidad). Nagbigay-daan ito sa amin na marinig mula sa napakaraming tao ang tungkol sa kanilang mga karanasan sa pandemya. Ang mga tugon sa online na form ay isinumite nang hindi nagpapakilala. Para sa Modyul 7, sinuri namin ang 44,775 kuwento. Kasama rito ang 36,879 na kuwento mula sa England, 3,665 mula sa Scotland, 3,783 mula sa Wales at 1,973 mula sa Northern Ireland (nakapili ang mga nag-aambag ng higit sa isang bansa sa UK sa online na form, kaya mas mataas ang kabuuan kaysa sa bilang ng mga natanggap na tugon). Sinuri ang mga tugon sa pamamagitan ng 'natural language processing' (NLP), na tumutulong sa pagsasaayos ng data sa makabuluhang paraan. Sa pamamagitan ng algorithmic analysis, ang impormasyong nakalap ay isinaayos sa 'mga paksa' batay sa mga termino o parirala. Ang mga paksang ito ay sinuri ng mga mananaliksik upang matuklasan pa ang mga kuwento. Higit pang impormasyon sa NLP ay matatagpuan sa apendiks.
- Sa oras ng pagsulat ng talaang ito, ang koponan ng Every Story Matters ay napunta sa 33 bayan at lungsod sa buong England, Wales, Scotland at Northern Ireland upang bigyan ang mga tao ng pagkakataong ibahagi ang kanilang karanasan sa pandemya nang personal sa kanilang mga lokal na komunidad. Idinaos din ang mga virtual na sesyon sa pakikinig, kung ang pamamaraang iyon ay ginusto ng mga kalahok. Ang koponan ay nakipagtulungan sa maraming kawanggawa at mga grupo ng komunidad sa katutubo upang makipag-usap sa mga naapektuhan ng pandemya sa mga partikular na paraan. Para sa partikular na record na Every Story Matters, mga karanasan mula sa Bingi2 isinama ang mga tao at mga taong bahagyang nakikita. Ang mga maikling buod na ulat para sa bawat kaganapan ay isinulat, ibinahagi sa mga kalahok ng kaganapan at ginamit upang ipaalam ang dokumentong ito. Isang consortium ng panlipunang pananaliksik at mga eksperto sa komunidad ang inatasan ng Every Story Matters na magsagawa malalim na mga panayam at mga grupo ng talakayan upang maunawaan ang mga karanasan ng iba't ibang tao, batay sa gustong maunawaan ng legal team para sa Module 7. Kasama rito ang mga may partikular na kundisyon sa kalusugan na maaaring nakaapekto sa kanilang kakayahang sumubok o ihiwalay ang sarili, kabilang ang mga kondisyon at kapansanan sa pisikal at mental na kalusugan. Kasama rin dito ang mga miyembro ng pamilya o mga indibidwal na sumusuporta sa mga kinakailangang mag-self-isolate, lalo na sa mga sumusuporta sa mga matatandang tao, naulila na mga indibidwal, o mga naulilang kaibigan, pamilya at mga kasamahan, mga may dati nang kondisyong pangkalusugan, o yaong mga clinically vulnerable o shielding. Kasama rin ang mga may mga responsibilidad sa pag-aalaga at mga miyembro ng mga grupo ng komunidad upang tulungan ang mga tao na ihiwalay ang sarili. Ang mga panayam at grupo ng talakayan na ito ay nakatuon sa Mga Pangunahing Linya ng Pagtatanong (KLOEs) para sa Module 7, impormasyon kung saan makikita dito. Sa kabuuan, 340 katao sa buong England, Scotland, Wales at Northern Ireland ang nag-ambag sa ganitong paraan sa pagitan ng Hulyo at Oktubre 2024. Ang lahat ng malalalim na panayam at grupo ng talakayan ay naitala, na-transcribe, na-code at sinuri upang matukoy ang mga pangunahing tema na nauugnay sa Module 7 KLOEs.
- Ang bilang ng mga tao na nagbahagi ng kanilang mga kuwento sa bawat bansa sa UK sa pamamagitan ng online na form, mga kaganapan sa pakikinig at mga panayam sa pananaliksik at mga grupo ng talakayan ay ipinapakita sa ibaba:
Figure 1: Pakikipag-ugnayan sa Bawat Story Matters sa buong UK
Para sa karagdagang impormasyon kung paano kami nakinig sa mga tao at ang mga pamamaraang ginamit sa pagsusuri ng mga kuwento, pakitingnan ang apendiks.
Mga tala tungkol sa presentasyon at interpretasyon ng mga kuwento
Ang mga kuwentong nakolekta sa pamamagitan ng Every Story Matters ay hindi kumakatawan sa lahat ng karanasan. Naapektuhan ng pandemya ang lahat sa UK sa iba't ibang paraan, at habang lumalabas ang mga pangkalahatang tema at pananaw mula sa mga kuwento, kinikilala namin ang kahalagahan ng natatanging karanasan ng bawat isa sa nangyari. Nilalayon ng record na ito na ipakita ang iba't ibang karanasang ibinahagi sa amin, nang hindi sinusubukang i-reconcile ang magkakaibang mga account.
Ginagamit namin ang terminong 'marami' upang ilarawan kung saan laganap ang mga karanasan at 'ilan' kung saan hindi gaanong karaniwan ang mga ito.
Ang ilang mga kuwento ay binibigyang buhay sa pamamagitan ng mga quote. Pinili ang mga ito para i-highlight ang iba't ibang uri ng karanasang narinig namin at ang epekto nito sa mga tao. Ang mga quote ay tumutulong sa pag-ground ng record sa kung ano ang ibinahagi ng mga tao sa kanilang sariling mga salita. Ang mga kontribusyon ay hindi nagpapakilala.
Sa pamamagitan ng rekord, makikita mong tinutukoy namin ang mga taong nagbahagi ng kanilang mga kuwento sa Every Story Matters bilang 'mga nag-aambag' at kung minsan ay naglalarawan kami ng higit pa tungkol sa kanila (halimbawa, ang kanilang etnisidad o katayuan sa kalusugan) upang makatulong na magbigay ng higit na konteksto sa quote na ginamit namin. Para sa mga taong nag-ambag sa record na ito sa pamamagitan ng isang webform, ang lahat ng kanilang mga quote ay may label na "Every Story Matters contributor". Ang ilan na nagsabi sa amin ng kanilang mga kuwento sa pamamagitan ng mga focus group at mga panayam ay may label din sa ganitong paraan. Ito ay dahil ang karagdagang detalye tungkol sa kanilang background ay hindi gaanong nauugnay upang suportahan ang naunang teksto, ngunit ang kanilang mga karanasan ay mahalaga pa ring isama.
Ang mga kuwento ay kinolekta at sinuri sa buong 2023 at 2024, ibig sabihin, ang mga karanasan ay naaalala ilang sandali pagkatapos mangyari ang mga ito, na nakakaimpluwensya sa mga detalye at aspeto ng mga karanasang naaalala.
Istruktura ng talaan
Ang dokumentong ito ay nakabalangkas upang bigyang-daan ang mga mambabasa na maunawaan kung paano naranasan ng mga tao ang pagsusuri sa Covid-19, pagsubaybay sa pakikipag-ugnayan at pag-iisa sa sarili.
Nagsisimula ang rekord sa pamamagitan ng paggalugad sa pag-unawa ng mga tao sa pagsubok, pagsubaybay at paghihiwalay (Kabanata 2) bago magpatuloy upang talakayin ang mga salik na nag-udyok (Kabanata 3) at nawalan ng loob (Kabanata 4) ang mga tao na lumahok sa pagsubok, pagsubaybay sa pakikipag-ugnay at pag-iisa sa sarili. Ang talaan pagkatapos ay nakatuon sa mga karanasang ibinahagi sa amin ng mga nag-aambag sa mga partikular na pangyayari (Kabanata 5). Sa wakas, tinutuklasan nito ang mga potensyal na pagpapabuti sa paligid ng pagsubok, pagsubaybay at pag-iisa sa sarili para sa mga pandemya sa hinaharap (Kabanata 6).
Terminolohiyang ginamit sa talaan
Pagsubok ay tumutukoy sa mga taong gumagamit ng kagamitan (inilalarawan sa ibaba) upang matukoy kung mayroon silang Covid-19 o wala.
Bakas ay tumutukoy sa prosesong ginamit upang tukuyin kung ang mga tao ay nakipag-ugnayan sa isang virus, sa kasong ito ng Covid-19, upang ang paghahatid ng virus ay maaaring pamahalaan at maitago hangga't maaari.
Ihiwalay ay tumutukoy sa panahon kasunod ng isang positibong pagsusuri sa Covid-19, na kadalasang tinutukoy bilang 'pag-iisa sa sarili'. Nagbago ang panahong ito sa paglipas ng pandemya at iba ito sa mga pakiramdam ng paghihiwalay na nangyari bilang resulta ng mga pambansang pag-lock.
Pinag-uusapan natin ang tungkol sa Lateral Flow Tests (LFTs) at Polymerase Chain Reaction (PCR) na mga pagsubok na dalawang pagsubok na ginamit upang matukoy ang pagkakaroon ng Covid-19.
Mga Pagsubok sa Lateral Flow (LFT)
Ang mga LFT ay isang home test na ginagamit upang makita ang isang aktibong impeksiyon. Gumagana ang pagsubok sa pamamagitan ng pagtuklas ng mga protina na naroroon sa isang pamunas na kinuha mula sa ilong at/o lalamunan. Nagtatampok ang pagsubok ng isang maliit na device na may absorbent pad sa isang dulo at isang reading window sa kabilang dulo. Sa loob ng device ay isang strip ng test paper na nagbabago ng kulay kung mayroong mga protina ng Covid-19.
Ang Lateral Flow Tests (LFTs) ay ginawang available sa lahat sa England, Scotland at Wales noong Abril 2021 na nagbigay-daan sa libreng access sa mabilis na pagsubok. Sumunod ang Northern Ireland noong Setyembre 2021.
Polymerase Chain Reaction (PCR)
Gumagana ang PCR test sa pamamagitan ng pagkuha ng sample gamit ang pamunas, kadalasan mula sa ilong at/o lalamunan. Pagkatapos ay ipapadala ang pamunas sa isang lab kung saan sinusuri ang sample para sa genetic material ng SARS-CoV-2 virus (Covid 19).
- Ang mga taong tinukoy bilang clinically very vulnerable at samakatuwid ay nasa napakataas na panganib ng malubhang sakit mula sa Covid-19 ay pinayuhan na 'magsanggalang' (ibig sabihin, protektahan ang kanilang sarili sa pamamagitan ng hindi pag-alis sa kanilang mga tahanan at bawasan ang lahat ng harapang pakikipag-ugnayan).
- Kinikilala ng Inquiry ang mas malawak na inklusibong termino ng "d/Deaf" bagama't ang mga taong kinakausap bilang bahagi ng record na kinilala bilang "Bingi".
2. Pag-unawa at kamalayan ng Test, Trace at Isolate |
 |
Sinasaliksik ng kabanatang ito ang kamalayan at pag-unawa ng mga nag-aambag sa pagsubok, pagsubaybay sa contact at pag-iisa sa sarili at ang mga panuntunang kailangan nilang sundin. Inilalarawan nito kung paano nalilito ang ilang tao sa mga komunikasyon, pati na rin ang mga karanasan ng mga nag-aambag sa kalidad ng impormasyong makukuha.
Pag-unawa at kamalayan sa patnubay
Inilarawan ng maraming kontribyutor kung paano nila naunawaan na kailangan nilang subukan kung mayroon silang mga sintomas ng Covid-19, tulad ng pag-ubo, pangkalahatang sintomas ng trangkaso - halimbawa, sipon at namamagang lalamunan - at pagkawala ng lasa at amoy. Ang kaalaman sa patnubay na ito ay dumating sa pamamagitan ng impormasyon mula sa mga awtoridad na ayon sa batas, ang NHS, mga employer at iba pang may kadalubhasaan sa medisina.
| “ | Palagi nilang ipinapaliwanag na [dapat kang magpasuri] anumang oras na naramdaman mong nagkakaroon ka ng mga sintomas, o kung nakipag-ugnayan ka sa isang taong nagpositibo sa Covid, o – kailangan mong magpasuri kung lilipad ka rin.”
– Kontribyutor ng Every Story Matters |
Inilarawan ng ilang kontribyutor kung paano lumaki ang kanilang kamalayan at kumpiyansa sa pag-alam kung kailan magsusuri sa paglipas ng panahon bilang resulta ng pagkakaroon ng mga sintomas at pagkaranas ng virus o pagdinig tungkol sa mga karanasan ng iba sa Covid-19.
| “ | Ang aking kumpiyansa [sa pagtukoy sa mga sintomas ng Covid-19] ay lumago sa paglipas ng panahon, pagkatapos kong marinig ang mga unang karanasan ng mga tao na alam kong […mayroon] nito. Dahil sa unang yugto, ito talaga ang makikita mo sa balita […], ang mga tao sa mga ventilator, at talagang, talagang seryoso […Akala ko] sinumang nakakuha ng Covid ay nasa bangkang iyon. Ngunit malinaw naman habang nagbabago ang mga strain, ngunit ang mga sintomas ay nanatiling magkatulad, lahat kami ay nagsimulang matuto.
– Kontribyutor ng Every Story Matters |
Ilang tao ang narinig namin mula sa alok ng dalawang beses na lingguhang mabilis na pagsubok (gamit ang mga LFT) noong inilunsad ito sa lahat mula Abril 2021 pataas. Sinabi sa amin ng mga tao na kapag nagpasuri sila nang walang mga sintomas, karamihan ay dahil sa mga kinakailangan sa lugar ng trabaho (saklaw sa ibaba) o gustong magpasuri bago makihalubilo sa iba (tingnan ang seksyong 'Mga Kalayaan' sa ibaba). Ang ilang mga nag-aambag ay nahirapan sa katwiran para sa pagsusuri nang walang mga sintomas, kadalasang nalilito kung paano kumalat ang virus sa pagitan ng mga tao nang hindi nagdudulot ng mga sintomas.
| “ | Nagpositibo ang anak ko, ngunit wala siyang anumang sintomas, kaya napakahirap malaman kung ano ang mga sintomas."
– Taong nagtatrabaho sa mga bata |
Naunawaan ng mga nagbahagi ng kanilang mga kwento na ang pagkakaroon ng mga sintomas ng Covid-19 ay nangangahulugang kailangan nilang ihiwalay ang sarili. Gayundin, sa karamihan (at lalo na sa simula ng pandemya), naunawaan ng mga tao na ang pagtanggap ng positibong pagsusuri para sa Covid-19 ay nangangahulugan ng pag-iisa sa sarili. Sinabi sa amin ng ilang kontribyutor kung paano sila naghiwalay sa sarili noong inakala nilang hindi tumpak ang mga resulta mula sa isang LFT dahil sa kanilang mga sintomas, o kapag naghihintay ng PCR test o dumating ang resulta.
| “ | Ihihiwalay namin [sa sarili] kung mayroon din kaming mga sintomas, hindi lamang sa pagsubok, dahil takot na takot kaming ibigay ito sa ibang tao dahil alam namin kung ano iyon."
– Nakaligtas sa pang-aabuso sa tahanan |
Inilarawan ng ilang nag-aambag kung paano nila sinubukan ang pandemya sa bandang huli (karaniwang gumagamit ng LFT) para kumpirmahin kung nakontrata ba sila ng Covid-19 bago magpasya kung mag-iisa o hindi.
| “ | Sa tingin ko, tulad ng tagapag-ayos ng buhok, kung saan nag-ping sila sa akin at sinabing, 'Nalantad ka, kailangan mong ihiwalay ang sarili mo sa loob ng pitong araw.' Nag-test ako sa bahay, at wala ako nito, at hindi ako nag-self-isolate. Sa palagay ko nagsusuri ako araw-araw, o bawat ibang araw."
– Taong may kapansanan |
Marami rin ang nakaunawa sa patnubay na ihiwalay ang sarili at subukan kung nakipag-ugnayan sila sa isang taong nagpositibo sa Covid-19. hindi alintana kung sila ay nakakaranas ng mga sintomas o hindi.
| “ | Nagkaroon ako ng tatlong PCR test […] na napakalapit [… Una] ang aking anak na babae […] ay nakaramdam ng hindi magandang pakiramdam, [… nang] ang isang tao sa kanyang paaralan ay nagkaroon ng Covid, kaya pumunta kaming lahat at nagpasuri. At pagkatapos ay nag-positive talaga siya sa bahay […] kaya nag-book kami ng PCR para sa aming lahat [kinabukasan]. At pagkatapos ay naging positibo ako [pagkalipas ng ilang araw].”
– Taong nabubuhay na may Long Covid |
| “ | Sigurado akong bumalik kami sa drama group [kapag may nasubok] na positibo para sa Covid [...] lahat ng iba ay gagawa lang ng pagsubok upang matiyak na [hindi nila ito nakuha]."
– Clinically vulnerable na tao |
Sinabi sa amin ng mga tao na mas naiintindihan nila ang mga proseso sa paligid ng pagsubok at pag-iisa sa sarili kumpara sa mga konektado sa pagsubaybay sa contact. Inilarawan ng ilang kontribyutor kung paano nila nakitang hindi malinaw ang impormasyon sa pagsubaybay sa contact, na mahirap maunawaan ang layunin nito at sundin nang tama ang gabay.
| “ | Ang pag-iisa sa sarili, naiintindihan ng lahat. Pagsubok, naiintindihan ng lahat. Ang pagsubaybay sa bit, kung marahil ay hindi ipinaliwanag kung bakit ito mahalaga o kung paano ito gumagana, o kung paano gumagana ang teknolohiya, o kung ano ang napakalinaw na isa, dalawa, tatlong hakbang na kailangan mong gawin. I think that bit for me, nagkaroon ng confusion.”
– Kontribyutor ng Every Story Matters |
Hindi alam ng maraming tao ang aming narinig mula sa pinansyal at praktikal na suporta upang tumulong sa panahon ng pag-iisa sa sarili. Bagama't sa pangkalahatan ay hindi alam na ang ganitong uri ng suporta ay magagamit, ang ilan ay sumasalamin na tatanggapin nila ito sa oras na iyon. Ipinaliwanag nila na mapapawi sana nito ang ilan sa pinansiyal na pasanin, lalo na para sa mga naapektuhan ang kita ng hindi makapagtrabaho. Para sa iba na nagtatrabaho at nagtatrabaho, binanggit ng ilan na hindi nila naisip na mag-aplay para sa suportang pinansyal.
| “ | Hindi ko man lang naisip na mag-apply, hindi ko akalain, kasi nagtatrabaho pa ako, kaya hindi ko naisip na nag-apply man lang ako.”
– Taong may pangmatagalang pisikal na kondisyon sa kalusugan |
| “ | Kinailangan kong gumawa ng maraming pananaliksik at makipag-usap din sa maraming tao upang makakuha ng sarili nilang mga karanasan sa kung ano ang nalaman nilang magagamit nila, mula rin sa pananaliksik. Sa palagay ko ay hindi ito madaling magagamit [impormasyon tungkol sa suporta para sa pag-iisa sa sarili] at sa palagay ko marami ring maling impormasyon."
– Kontribyutor ng Every Story Matters |
Nakarinig kami ng ilang halimbawa ng mga nag-aambag na nakarinig tungkol sa suportang pinansyal, partikular para sa pag-iisa sa sarili, sa pamamagitan ng salita ng bibig o sa kanilang trabaho. Nakita ng ilan na nakakatulong ito habang ang iba ay nagsabi sa amin na mas gusto nilang kumita ng sarili nilang pera sa halip na tuparin ang buong panahon ng pag-iisa sa sarili.
| “ | I did access them [grants to self-isolate], gusto ko lang ng pera. Na-access ko ang mga ito ngunit pagkatapos ay pinutol ko ang panahon upang kumita ng mas maraming pera. Dahil lahat ay gustong kumita ng mas maraming pera."
– Kontribyutor ng Every Story Matters |
| “ | Oo, maganda ang £500, sa totoo lang. Ang £500 na iyon para sa mga naapektuhan ng Covid ay talagang mahusay. Ngunit hindi lahat ay nakatanggap nito."
– Kontribyutor ng Every Story Matters |
Ang mga mapagkukunan ng impormasyon tungkol sa kung saan maa-access ang mga pagsusulit ay kasama ang internet, telebisyon, social media, mga polyeto at salita ng bibig. Ang mga nag-aambag na naalala na alamin ang tungkol sa mga pagsubok sa mga ganitong paraan ay nadama na ang impormasyon ay madaling makuha, malinaw at madaling sundin.
| “ | Naaalala ko na palagi nilang sasabihin sa iyo sa balita kung paano i-access ito [pagsubok]. Kung pumunta ka sa website ng NHS, magkakaroon ito ng malinaw na mga tagubilin. O kahit na tumawag ako sa aking GP, ipapaalam nila sa akin […] kung paano i-access ang mga ito [… Ang impormasyon] ay hindi masyadong kumplikado […] tulad ng ilang mga payo.”
– Tagapag-alaga |
Narinig din namin mula sa mga kontribyutor na naglalarawan ng mga kahirapan sa pag-access o pagsubaybay sa impormasyon tungkol sa pagsubok. Kasama rito ang mga taong hindi gumagamit ng internet at mga taong hindi Ingles ang unang wika. Ang limitadong pag-access sa impormasyon ay nangangahulugang hindi alam ng ilang nag-ambag na maaari nilang ma-access ang mga pagsubok nang libre, halimbawa, hanggang sa ilang paraan sa pandemya. Ang ilan ay hindi rin sigurado kung saan makakahanap ng mga pagsubok, o kung ano ang gagawin kapag may kakulangan.
Pagkalito
Sinabi sa amin ng ilang kontribyutor kung paano sila nalilito kung kailan at bakit sila susubok. Kadalasan ito ay dahil mahirap makilala ang Covid-19 at iba pang mga sakit dahil sa pagkakaiba-iba at kalubhaan ng mga sintomas na nauugnay sa Covid-19 at iba pang mga virus tulad ng sipon at trangkaso. Ang pinaghihinalaang kahirapan ay naging dahilan upang ang ilang mga kontribyutor ay mas malamang na sumubok kapag nakakaranas ng mga posibleng sintomas.
| “ | Well, I suppose, ako personally, I think naintindihan ko [kung kailan magpa-test]. Bagaman sa palagay ko ay may ilang pagkalito sa mga sipon, trangkaso, lahat ng mga bagay na maaaring magkaroon ng mga katulad na sintomas."
– Kontribyutor ng Every Story Matters |
Ang mga pagbabago sa opisyal na patnubay ng gobyerno ay nagdulot ng pagkalito sa mga tao tungkol sa kung kailan sila magsusuri at kung gaano katagal nila kailangang mag-self-isolate pagkatapos ng isang positibong pagsusuri. Ang pagkalito na ito ay pinalala ng iba't ibang mga diskarte sa iba't ibang mga bansa ng UK.
| “ | Sa una ay talagang malinaw at lahat ay nasa itaas nito sa aking […] ospital, at pagkatapos […] Sa tingin ko nagsimulang magbago ang mga patakaran at naging napakalabo […] Kailangan kong palaging […] mag-check online o magtanong sa trabaho, 'Ano ang sitwasyon ngayon? Magsusubok ba ako o hindi?' […] Sa palagay ko [ito] ay nagiging mas nakakalito habang tumatagal.”
– Taong nagtatrabaho sa pangangalagang pangkalusugan at panlipunan |
Nagkaroon din ng ilang pagkalito tungkol sa kung paano naiiba ang mga contact tracing app sa iba pang mga app na inilunsad noong panahong iyon upang suportahan ang mga paghihigpit sa Covid-19, halimbawa, isang app sa Scotland upang tumulong sa mga kahilingan sa parmasya, at kung paano gumagana ang iba't ibang system sa mga hangganan. Iminungkahi ng ilang kontribyutor na maaaring mayroong isang sistema para sa buong UK.
| “ | Masasabi ko lang na tila maraming apps, sabay-sabay. At maliban kung alam mo kung ano ang iyong ginagawa ay madaling mawala ng kaunti at gumamit ng mali gaya ng ilang beses kong ginawa.”
– Taong nakakuha ng suporta sa kalusugan ng isip |
| “ | Kinailangan kong maglakbay sa Scotland ng ilang araw para sa trabaho (ang aming punong tanggapan ay nasa Edinburgh) at nalaman kong ang mga QR code ng NHS app/government Covid app ay iba sa itaas. I find it wild na walang standardized system para sa UK."
– Kontribyutor ng Every Story Matters |
Ang ilang mga nag-ambag – lalo na ang mga matatandang nag-aambag at/o ang mga hindi kasama sa digital na paraan – ay nag-ulat na nalilito kung paano mag-access at gumamit ng mga app, na naging dahilan ng kanilang pagkabalisa. Halimbawa, nag-download ng app sa pagsubaybay sa contact ang isang contributor na may dati nang kundisyong pangkalusugan (na hindi rin kasama sa digital), ngunit hindi sigurado kung paano ito gumagana. Ang pagtanggap ng mga abiso ay nagparamdam sa kanila ng pagkabalisa at sa ilang mga kaso ay lubhang nababalisa.
| “ | Mayroon akong app sa telepono...ping, ping, at iniisip ko, 'Bakit ako pini-ping?' At pagkatapos ay lalabas ito...may nakahuli sa [Covid-19] sa iyong lugar...at iniisip ko, 'Oh, kumukurap na impiyerno.'...tinanggihan ko ito. Pero iniisip ko, 'Oh my God, oh my God, papalapit na, papalapit na.'”
– Taong digital na hindi kasama |
Mas partikular, narinig namin na madalas na hindi alam ng mga tao kung ano ang gagawin kapag nakatanggap sila ng notification ng isang contact. Lalo itong nakakalito kapag mahirap matukoy kung kailan ginawa ang contact, o kapag may nakakatanggap ng maraming notification.
| “ | Sa palagay ko sinabi nito, 'Maaaring nakipag-ugnayan ka.' Masyadong malabo…kung may kakilala ako sa opisina na [parang] siguradong may Covid, mas gusto kong [mag-isip], 'Well, siguro kailangan kong mag-test.'...[pero] parang hindi masyadong nasusukat ng siyentipiko."
– Taong nagtatrabaho sa pangangalagang pangkalusugan at panlipunan |
Habang nagpapatuloy ang pandemya, nalilito ang ilang tao kung gaano katagal nila kailangang ihiwalay ang sarili pagkatapos nilang magkaroon ng abiso sa pakikipag-ugnayan., ano ang patnubay kung mayroon na silang Covid-19 o nabakunahan na, at ano ang magiging parusa kung hindi nila sinunod ang patnubay.
| “ | Sa palagay ko kung mayroong milyun-milyong tao ang gumagamit nito [ang contact tracing app], marahil ay wala lang itong kapasidad na, uri-uriin, i-update ito at maging mas may kaugnayan o indibidwal sa tao kung ipinakita nila-, tulad ng ganap na nabakunahan ako...kaya sinasabi nito na kailangan ko pa ring mag-self-isolate, at noong pumunta ako sa website sinabi nito, 'Hindi, hindi mo kailangan mag-self-bakuna'
– Zero-hours contract worker |
Narinig din namin na ang pagbabago ng mga alituntunin tungkol sa mga panahon ng pag-iisa sa sarili ay nagdulot ng hindi katiyakan ng mga tao habang nagpapatuloy ang pandemya tungkol sa mga panuntunang ipinatupad sa anumang oras.4 Halimbawa, ibinahagi ng ilan kung paano hindi nila naunawaan kung bakit patuloy na nagbabago ang bilang ng mga araw para sa pag-iisa sa sarili, sa kabila ng pagiging parehong virus. Bilang resulta, maraming nag-ambag ang nagsabing nagpasya silang gawin ang sa tingin nila ay ang "tama" na bagay sa bandang huli ng pandemya, ito man ay naaayon sa mga panuntunan sa pag-iisa sa sarili o hindi. Ang iba ay nagpasya na tapusin ang mga panahon ng pag-iisa sa sarili pagkatapos ng negatibong pagsubok bagama't sila ay nasa loob pa rin ng inirekumendang timeframe para sa pag-iisa sa sarili.
| “ | Buweno, ang bagay na tumatak sa aking isipan ay, bumalik sa pagkalito muli, kung bakit 14 na araw sa simula, at pagkatapos ay malinaw na bumaba ito sa 5 araw, at naaalala kong naisip ko noong panahong iyon, 'Alinman sa napakalaking overdone natin ang pag-iisa sa sarili sa simula, at hindi na natin kailangan na gawin ito sa loob ng 14 na araw, o kung saan ang mga tao ay lumalabas na ngayon pagkatapos ng 5 araw, mayroon pa rin silang potensyal na pag-iwas sa sarili. sa mga tao.' Kaya lang, hindi ko naramdaman na mayroong [isang] malinaw na paliwanag kung bakit ang bilang ng mga araw ay nabawasan nang husto.”
– Taong nagtatrabaho sa mga bata |
| “ | Ang patnubay ay minsan ay hindi maliwanag at hindi malinaw o mahigpit - ang mga may sakit ay dapat na sinabihan noong Enero/Pebrero 2020 na ihiwalay ang sarili - at ginawa ng kaso na kung hindi nila gagawin, ang bansa ay magsasara."
– Kontribyutor ng Every Story Matters |
Ang pagtatapos ng mass testing ay nagpapataas din ng kalituhan para sa ilan.5 Nadama ng ilang kontribyutor na ang pagpapahinga ng mga kinakailangan sa pagsubok sa iba't ibang yugto ng pandemya ay tila hindi naaayon sa mga naunang kinakailangan sa pagsubok.
| “ | Noong napakataas pa ng mga impeksyon, mayroong […] malinaw na mga panuntunan, higit o hindi gaanong malinaw na ipinapahayag. Ito ay naging napakalinaw, nang ang pandemya ay medyo huminto […] ang rekomendasyon na ang pagsusuri ay hindi na kailangan pa [kahit] kung mayroon kang mga sintomas ay labis na nakakalito, pagkatapos naming [na] sinabihan sa loob ng dalawang taon na dapat kang magpasuri at manatili sa bahay.
– Kontribyutor ng Every Story Matters |
- Ang mga pangunahing uri ng contact tracing na ginagamit ng mga contributor ay ang contact tracing app. Tatlong Covid-19 contact tracing mobile app ang binuo para sa iba't ibang rehiyon ng UK: 'NHS COVID-19' para sa England at Wales, 'StopCOVID NI' para sa Northern Ireland at 'Protektahan ang Scotland' para sa Scotland.
- Ang mga panahon ng paghihiwalay ay madalas na nagbabago sa buong pandemya sa England, na nag-iiba mula 14 na araw (Marso 2020) hanggang 10 araw (Disyembre 2020), pagkatapos ay 7 araw (Disyembre 2021 – nakadepende sa dalawang negatibong LFT) at kalaunan ay nabawasan sa 5 araw (Enero 2022). Iba't ibang panuntunan ang inilapat kung nakipag-ugnayan ka sa isang taong nagpositibo sa Covid-19 (kadalasan ay kinakailangang ihiwalay ang sarili para sa isang partikular na panahon mula sa petsa ng kanilang positibong pagsubok). Ang mga pagbubukod ay ginawa sa ibang pagkakataon kung ikaw ay nabakunahan, o ang isang confirmatory PCR test ay negatibo. Ang mga pagbabago sa mga panuntunan ay nangyari sa magkakaibang panahon sa apat na bansa.
- Ang lahat sa England ay inalok ng access sa dalawang beses lingguhang mabilis na pagsusuri para sa Covid-19 mula 9 Abril 2021 sa pagpapalawak ng mass asymptomatic testing program ng gobyerno. Kilala ito bilang universal testing offer (UTO). Ang panahon ng UTO ay tumagal hanggang sa katapusan ng Marso 2022. Kasama ng ilang iba pang mga patakaran sa Covid-19, huminto ito habang ipinakilala ng gobyerno ng UK ang 'Pamumuhay sa COVID-19' diskarte.
3. Mga Enabler: Ano ang nakatulong o naghikayat sa mga tao na lumahok sa pagsubok, pagsubaybay sa pakikipag-ugnayan at pag-iisa sa sarili? |
 |
Ang kabanatang ito ay nagdedetalye ng mga salik na nakatulong o nagbigay-daan sa mga tao na lumahok sa pagsubok, pagsubaybay sa pakikipag-ugnayan at pag-iisa sa sarili. Inilalarawan nito ang mga enabler na ito at nagbibigay ng mga halimbawa kung saan at paano nila naiimpluwensyahan ang mga pag-uugali sa panahon ng pandemya. Ang kabanata ay nagtatapos sa mga pagmumuni-muni ng mga nag-aambag tungkol sa Nakapirming Mga Paunawa sa Parusa na nasa lugar.
Protektahan ang mga taong pinapahalagahan nila
Tinukoy ng mga kontribyutor na narinig namin mula sa isang pangkalahatang tungkulin na sundin ang patnubay ng pamahalaan upang protektahan ang kanilang mga sarili at ang mas malawak na populasyon, partikular na ang mga taong mahina.
Ang pakiramdam ng moral na obligasyon o 'konsensya' ay isang matibay na dahilan para sa mga tao na subukan, makisali sa pagsubaybay sa pakikipag-ugnayan at/o paghiwalay sa sarili kapag naramdaman nilang kailangan nila, upang 'gawin ang tamang bagay' at upang matiyak na ginagampanan nila ang kanilang bahagi sa paglimita sa paghahatid.
| “ | Hindi ako [...] isang rule-breaker, [...] Sinusunod ko ang lahat ng mga patakaran, kaya lahat ako ay para sa pagsubok, upang [...] mabawasan ang panganib ng pagkalat nito."
– Tagapag-alaga |
| “ | Kung mayroon akong Covid, ayaw kong ipasa ito sa ibang tao, kaya kung ang pagsasabi ko ng 'I've been somewhere' ay sapat na upang maiwasan ang ibang tao na mahuli ito, kung gayon iyon ay sapat na para sa akin."
– Taong may pangmatagalang pisikal na kondisyon sa kalusugan |
Para sa ilang mga tao na aming narinig mula sa, ang moral na obligasyon na protektahan ang iba ay sumalungat sa kanilang sariling pagnanais para sa kalayaan sa paggalaw (higit pang detalye tungkol dito sa seksyong 'Mga Kalayaan' sa ibaba), na lumilikha ng dilemma
| “ | The conscience kicking in. Ngunit sa lahat ng ito, ako, parang, ayoko mag-test, dahil kung mag-positive ako, hindi ko magagawa ang ilang bagay, alam mo, ito ay isang beses na wala tayo sa isang lockdown, at kailangan mong [self-] ihiwalay at iba pa. At ako ay nasa isang matinding salungatan sa moral kung uunahin ko ba ang aking sarili at hindi subukan, o talagang inuuna ko ba ang lahat at subukan para sa kanilang kapakinabangan.
– Zero-hours contract worker |
Ang mga nag-aambag na may mga responsibilidad sa pag-aalaga ay nakadama ng pagkabalisa sa panahon ng pag-iisa sa sarili. Namuhay sila na may malalim na pag-aalala at pakiramdam ng responsibilidad tungkol sa hindi pagpasa o kung hindi man ay hayaan ang kanilang mga mahal sa buhay na magkaroon ng Covid-19. Madalas nilang inilarawan kung gaano palagian at mahigpit ang pagsunod nila sa mga panuntunan sa pag-iisa sa sarili upang mabawasan ang panganib na ito, ngunit kung paanong ang pakiramdam ng pagkabalisa at pagkakasala tungkol sa kung ano ang ibig sabihin nito para sa kanilang mahal sa buhay ay napakahirap na makayanan. Partikular na naapektuhan sa ganitong paraan ang mga nag-aambag na naninirahan sa mga multi-generational na sambahayan at may mga kamag-anak na mahina sa klinikal.
| “ | Pangunahin, ito [pagsunod sa mga alituntunin sa pag-iisa sa sarili] ay dahil ayaw kong patayin sila [mga magulang ng nag-aambag]...kailangan mo lang maging makatotohanan, at kailangan mong protektahan ang mga tao. Ginagawa namin ang sinabi sa amin at iyon lang, alam mo ba?"
– Taong naninirahan sa isang multi-generational na sambahayan |
Sa ilang komunidad ng mga manlalakbay, sinabi ng mga kontribyutor na sumunod sila sa mahigpit na mga panuntunan sa pag-iisa sa sarili sa site anuman ang isang tao sa kanilang komunidad ay nagpositibo sa virus o nagkaroon ng mga sintomas. Nangangahulugan ito na kapag ang isang tao ay nagkasakit ng Covid-19, mayroon nang mga patakaran at gawi na pinadali ang isang mataas na antas ng pag-iisa at proteksyon sa sarili.
| “ | … [W]e ay walang darating sa site. Kaya naman, sa loob ng bawat sambahayan, ang bawat isa ay nanatili sa kanilang sariling sambahayan. Pwede tayong tumayo sa labas, may kalye na magkaharap lang, pwede kang mag-chat. Alam mo, huwag lumabas, makipag-chat sa isa't isa, ipaalam sa mga tao kung ano ang iyong nararamdaman doon. Pero wag ka sumama, wag kang lalabas, wag kang dumalaw. Kaya, noong mga oras na kailangan mong gawin iyon [mag-isa sa sarili], iyon ay pinanatili sa loob ng mga batas nang maayos sa loob ng komunidad.
– Taong mula sa pinagmulang etniko ng Roma |
Pangungulila
Para sa mga nawalan ng mga mahal sa buhay sa panahon ng pandemya at hindi nagawang magdalamhati o magdalamhati sa iba, ang emosyonal na pinsala ay napakalaki. Ang pagdanas ng pangungulila ay nagkaroon ng malaking epekto sa lawak kung saan naramdaman ng ilang tao na sumunod sa mga alituntunin sa pag-iisa sa sarili. Ibinahagi ng ilan kung paano ang ibig sabihin ng kanilang pagkawala ay nakita nilang mahalaga ang pagsunod sa mga alituntunin at madalas na mahigpit na nakikipag-ugnayan sa kanila.
| “ | Sineseryoso ito ng aking pamilya [mga alituntunin sa pag-iisa sa sarili], dahil nawalan kami ng isang taong malapit sa amin nang maaga sa pandemya, literal noong linggo ding iyon na inanunsyo ng lahat na manatili sa bahay. Kaya, oo, siniseryoso namin ito mula sa simula.
– Kontribyutor ng Every Story Matters |
Sinabi rin sa amin ng mga tao kung paano sila napag-isipan ng mga alituntunin sa pag-iisa sa sarili at isaalang-alang ang kanilang paggawa ng desisyon noong binisita nila ang isang mahal sa buhay sa ospital na namamatay. Nangangamba sila kung ang isang mahal sa buhay ay namatay pagkatapos ng pagbisita at sinabihan silang ihiwalay ang sarili, na hindi sila pisikal na naroroon upang aliwin ang kanilang pamilya sa panahon ng kanilang kalungkutan. Naniniwala sila na ito ay magkakaroon ng pangmatagalang at traumatikong epekto sa kanila at sa proseso ng pagdadalamhati ng kanilang pamilya. Ang ilan sa mga narinig namin mula sa na nawalan ng mga mahal sa buhay ay natagpuan din ang kanilang sarili na nahaharap sa napakahirap na suliranin ng pagpapasya kung ang panganib ng hindi pagsunod sa mga alituntunin sa paghihiwalay sa sarili ay higit pa sa mga potensyal na epekto ng pagsunod sa kanila.
| “ | Pinayuhan kami na isang miyembro lang ng pamilya ang maaaring bumisita sa ward [para makita ang kanyang 94-anyos na lola na may dementia, COPD at Leukemia na naghihingalo] na nakasuot ng full personal protective equipment (PPE), at kailangan nilang ihiwalay ang sarili pagkatapos. Ang nanay at tiyuhin ko ay clinically vulnerable, at ang aking kapatid na babae ay nag-iisa na sa sarili, kaya nag-iwan sa akin ng dilemma kung bibisita, alam na kung siya ay namatay, hindi ko magagawang yakapin ang aking 7-taong-gulang na anak na babae sa loob ng dalawang linggo, habang naranasan niya ang kanyang unang pangungulila.
– Kontribyutor ng Every Story Matters |
kwento ni RyanIbinahagi sa amin ni Ryan ang kanyang karanasan sa pag-iisa sa sarili noong ang kanyang ama ay tumatanggap ng end of life care sa ospital. Si Ryan ay may mga sintomas ng Covid-19 noong panahong iyon at hindi siya pinayagang bisitahin siya, sa halip ay kailangang makipag-ugnayan sa pamamagitan ng telepono. Habang siya ay nagbubukod sa sarili, ang ama ni Ryan ay malungkot na namatay at siya ay naiwang mag-isa na nagdadalamhati, na masama pa rin ang pakiramdam. Kinailangan din niyang gumawa ng funeral arrangement dahil mahirap ang kanyang ina at hindi na kaya. |
|
| “ | Namatay ang aking ama. Ako ay nag-iisa, may sakit at walang makitang sinuman.” |
| Nagpasya siyang ayusin ang isa pang pagsusuri sa Covid-19 sa pamamagitan ng telepono pagkatapos ng dalawang linggong pag-iisa sa sarili. Gayunpaman, ang kanyang resulta ay isang 'false' positive. Nakaramdam siya ng galit na hindi siya nalaman na ito ay isang posibilidad pagkatapos kumuha ng pagsusulit sa loob ng 90 araw pagkatapos mahawa ng virus. Nangangahulugan ito na kinakailangan siyang mag-self-isolate para sa karagdagang 10 araw, bagama't walang sintomas. Ilang beses siyang tumawag sa 119 upang tanungin ang kanyang resulta ngunit sinabihan siyang kailangan pa niyang mag-self-isolate.6 | |
| “ | Tumawag ako sa 119. Karaniwang sinasabi sa akin na walang kabuluhan ang pagtatalo at kailangan kong [mag-isa] na ihiwalay.” |
| Emosyonal at praktikal na naapektuhan si Ryan ng naramdaman niyang isang malaking kawalan ng pag-unawa sa kanyang sitwasyon mula sa mga taong nakausap niya sa 119, lalo na sa panahon ng pagdadalamhati. | |
| “ | tawag ko ulit. Sinabi sa akin na walang pagpipilian kundi ang [self-] ihiwalay. Mayroon na akong mga papeles na ginagawa para sa libing at pagpaparehistro ng pagkamatay ni tatay, na halos lahat ay hindi ko makumpleto dahil hindi ako makapunta sa bahay ng aking mga magulang upang hanapin ang impormasyon. Gusto kong puntahan si tatay sa funeral parlor. hindi ko kaya. Kailangan kong maglipat ng pera para bayaran ang libing. hindi ko kaya. Gusto kong suriin ang kalagayan ng aking ina dahil natagpuan ang isang lugar sa isang angkop na tahanan ng pangangalaga. Hindi ko kaya.” |
Mga kinakailangan
Inilarawan ng mga nag-aambag na nagtatrabaho sa isang hanay ng mga sektor kung paano naging bahagi ang regular na pagsusuri sa kanilang mga panuntunan at kinakailangan sa lugar ng trabaho sa panahon ng pandemya, may mga sintomas man o wala ang mga tao. Kasama dito ang pagkakaroon ng pagsubok sa isang lingguhan/dalawang beses-lingguhang batayan o bago ang bawat shift. Inilarawan ng ilang kontribyutor kung ano ang naramdaman nila na ang pagsubok sa trabaho ay nakatulong upang gawin itong mas ligtas na kapaligiran.
| “ | May patakaran talaga ang lugar ng trabaho ko, kaya kailangan naming mag-test every week.”
– Kontribyutor ng Every Story Matters |
| “ | Ang trabaho ay isang […] pangunahing salik para sa akin […] nagtatrabaho sa A&E, kailangan naming subukan […] linggu-linggo […] gamit ang mga lateral flow […] madali lang. Malinaw na iyon ay para sa kaligtasan ng mga pasyente at sa aking [sariling], at […] mahalaga na patuloy kaming sumubok para maprotektahan din ang aming mga pamilya.”
– Kontribyutor ng Every Story Matters |
Ang isang karagdagang dahilan para sa pagsubok para sa ilang mga manggagawa sa mga tungkulin sa pamamahala ay isang pagnanais na magtakda ng isang halimbawa para sa iba pang mga kasamahan.
| “ | It [the discomfort] did put me off but at the same time, alam kong kailangan kong gawin ito. Kinailangan kong maging isang halimbawa rin, bilang tagapamahala, […] sa aking mga tauhan, kaya walang paraan na ako [magiging] mangaral, 'Gawin mo ito, gawin mo ito,' at hindi gawin ito [rin]."
– Taong may kahirapan sa pagbasa |
Nakatulong din ang pagsubok na maibsan ang mga takot tungkol sa paglalagay ng panganib sa iba sa pamamagitan ng pagpasa ng virus sa mga kasamahan o miyembro ng pamilya.
| “ | Mas malamang na mag-test ako dahil […] talagang natatakot akong makuha ito. […] Nasa placement ako nang malaman kong may Covid ako […]. Nagkaroon ako ng mataas na temperatura sa buong araw, pagpapawis, pananakit ng ulo […] isang oras bago natapos ang aking shift […] Nagawa ko na ang pagsusulit at ito ay positibo, kaya malinaw na nagdudulot din iyon ng pagkataranta sa mga tao na nagtatrabaho ka […] na parang, 'Buong araw na kasama kita.' […] nakakaramdam ka rin ng pagkakasala […], 'Inilagay ko sa panganib ang ibang tao'.”
– Taong nagtatrabaho sa pangangalagang pangkalusugan at panlipunan |
Para sa maraming nag-aambag na nakikipag-ugnayan nang harapan, sa propesyonal man o personal na kapasidad, sa mga taong mas mahina sa mga epekto ng virus, ang regular na pagsusuri ay inilarawan bilang isang mahalagang bahagi ng kanilang personal na tungkulin ng pangangalaga. Ito ay partikular na ang kaso para sa mga taong may mga responsibilidad sa pag-aalaga, o kung sino ang bumibisita sa mas matanda o mahinang kamag-anak. Inilarawan ng mga propesyonal sa pangangalagang pangkalusugan at panlipunan ang regular na pagsusuri bilang bahagi ng kanilang legal na tungkulin sa pangangalaga.
| “ | Pakiramdam ko ay tungkulin ko ng pangangalaga, sa mga pasyente at parmasya. […] nandoon kami na nag-aalok ng serbisyo na palagi naming inaalok, at pakiramdam ko ay tungkulin ko lang ito […] sa moral, […] kung mayroon akong Covid at hindi pa nagsusuri, at ipinasa iyon sa, sabihin nating, isang 90-taong-gulang na pasyente na pumasok para sa kanyang gamot, talagang malungkot ako […] hindi man lang sumagi sa isip ko […] na hindi magpasuri.' Dahil [naramdaman ko] na dapat akong sumubok."
– Taong nagtatrabaho sa pangangalagang pangkalusugan at panlipunan |
| “ | Dahil naging tagapag-alaga ako sa buong buhay ko, nakasanayan ko na […] na parang nauuna siya [ang aking ina], […] parang kung may mangyari sa aking ina dahil lagi siyang nasa bahay at nagbubukod. Hindi ko alam, kung hindi ako naging sapat na mapagbantay upang makilala na ang sintomas na ito ay maaaring nauugnay sa Covid at hindi kumuha ng pagsusulit, at pagkatapos, bilang isang resulta nito, hindi [pag-iisa] sa sarili at pagkatapos ay nasa paligid niya, at kailangan niyang makuha ito, oo, makaramdam ako ng pagkakasala na ako ang naging sanhi nito.
– Tagapag-alaga |
Kwento ni MichaelSi Michael ay isang estudyante at nagtrabaho sa isang supermarket noong panahon ng pandemya. Siya ay isang kabataan at sa kanyang unang taon sa unibersidad nang magsimula ang pandemya. Inilarawan niya kung gaano kalaki ang pandemya para sa kanya, dahil sa mga epekto sa kanyang pag-aaral, trabaho, at pamilya. Ang supermarket kung saan siya nagtrabaho ay may sariling internal testing system, na sinundan ni Michael. Nagtatrabaho sa isang tindahan kung saan siya nakipag-ugnayan sa mga miyembro ng publiko, naniniwala si Michael na mahalaga ang pagsubok upang maprotektahan ang iba. |
|
| “ | Malaking bahagi niyan ang trabaho, in terms of going to work, I didn't want to put anyone else at risk, especially the job that I was doing is, well, called a key worker, I never like to say it because in compared to the NHS, I was just working in a shop. |
| Nag-aalala rin si Michael para sa kanyang mga kapamilya. Siya ay may mga kamag-anak na naospital dahil sa Covid-19 at inilagay sa mga bentilador, na nakakaranas ng matinding paghinga. Ang kanyang ina ay mayroon ding pangmatagalang kondisyon sa kalusugan at nagkasakit nang malubha nang siya ay magkasakit ng Covid-19. Nag-aalala si Michael na kung pupunta siya sa ospital, ang kanyang kalusugan ay malalagay sa panganib dahil sa mas mataas na pagkakataon na magkaroon ng impeksyon. Nadama ni Michael na mahalagang magpasuri hindi lamang sa mga tuntunin ng kanyang sariling peligro para sa Covid-19, ngunit bilang isang paraan ng pagpapagaan ng panganib para sa ibang mga tao. Mahalaga sa kanya na maging maingat at magsuri nang madalas, sa halip na ipagsapalaran na mahawahan ang kanyang mas mahinang mga miyembro ng pamilya. | |
| “ | Wala akong pinagbabatayan na mga kondisyon sa kalusugan sa puntong iyon, ngunit ang aking ina ay nagkaroon at ang aking [mga kamag-anak] ay nagdurusa. Tulad ng, walang katuturan para sa akin na ipagsapalaran ito […] mas madaling sundin kung ano ang ipinayo kaysa subukan at maging napakatalino at pagkatapos ay potensyal na patakbuhin ang panganib kung makatuwiran iyon.” |
Katulad nito, ipinaliwanag ng ilang kontribyutor kung paano sinusuportahan ng kanilang mga lugar ng trabaho ang mahigpit na pagsunod sa mga itinakdang panahon ng pag-iisa sa sarili. Inilarawan ng mga taong nakausap namin na nakakaranas sila ng mas mababang antas ng stress kapag nasunod nila ang mga protocol nang walang panggigipit mula sa kanilang mga tagapag-empleyo, dahil alam nilang binigyan sila ng kapangyarihang maghiwalay sa sarili nang walang anumang negatibong kahihinatnan na nauugnay sa trabaho.
| “ | Yes I did, because work was quite strict, obviously if you have Covid, don't come in. Kasi, we need everyone we can. Oo, nanatili ako sa bahay, hindi ko na matandaan kung ilang araw ang iminungkahi nila, ngunit ginawa ko ang buong panahon. Kahit na bumuti na ang pakiramdam ko, naghintay ako hanggang sa mag-negative ako."
– Kontribyutor ng Every Story Matters |
Access sa suporta
Ang pag-access sa suporta ay susi para sa ilang mga tao na ma-access ang pagsusuri sa PCR. Kasama sa suporta ang tulong sa pag-unawa sa proseso, pag-book ng mga appointment o paghahatid sa bahay, pagdalo sa mga appointment o pagbabalik ng mga pagsusulit at pagtanggap ng mga resulta. Iba-iba ang antas ng suportang kailangan ng mga tao: ang ilan ay nangangailangan ng tulong sa isang elemento ng proseso ng pagsubok, halimbawa, paghahanap at paggamit ng mga online booking form, samantalang ang iba ay ganap na umaasa sa tulong sa pag-book ng mga appointment, paglalakbay sa mga test center at pag-access ng mga resulta ng pagsubok.
| “ | [Ang aking mga kamag-anak] ay matatanda na at walang sinuman sa kanila ang marunong bumasa o sumulat, wala silang mga telepono […] Kaya, ginawa ko iyon: tumawag ako, nakipag-appointment […] dinala sila [para sa pagsusulit...] at tiniyak na nasa kanila [ng staff] ang aking email at numero [para sa mga resulta].”
– Taong mula sa pinagmulang etniko ng Roma |
Mga organisasyong pangkomunidad na nakikipagtulungan sa mga komunidad ng Gypsy at Traveler, mga taong may mababang antas ng literacy at mga taong ang unang wika ay hindi Ingles na nag-aalok ng 1:1 na suporta upang ma-access ang mga pagsubok. Gumawa at nagbahagi ng mga video ang ilang miyembro ng komunidad upang ipaliwanag ang pangkalahatang pagsubok, pagsubaybay at paghiwalayin ang mga kinakailangan.
| “ | Ang lahat ay sakop sa paligid ng Covid at ibinahagi. Lahat ng nanggaling sa gobyerno ay ibinahagi, kaya tuwing may mga guide rules na inilalagay, gagawa ako ng live na video at i-share ito. Kaya, alam mo, at kilala ko ang mga taong hindi marunong bumasa o sumulat, at alam kong hindi magiging interesado ang mga nakababatang bata sa kung ano ang isusulat ko doon. Kaya, kung gumawa ako ng live na video at ibinahagi ito sa aking WhatsApp at ibinahagi ito sa aking Facebook, maaaring isang minuto lang ito.”
– Tao mula sa komunidad ng Manlalakbay |
Katulad nito, ang pag-access sa suporta mula sa mga kaibigan at miyembro ng pamilya sa mga panahon ng pag-iisa sa sarili ay mahalaga sa pagpayag sa mga tao na mag-isa. Nakatulong ang mga impormal na network ng suporta sa pamamagitan ng paghahatid ng mga mahahalaga at pagbibigay ng emosyonal na suporta sa mga nagbubukod sa sarili. Ang ganitong uri ng suporta ay kadalasang katumbas ng mga nag-aambag kung saan magiging napakahirap na ihiwalay ang sarili kung hindi man.
| “ | I-text ko ang aking kapatid na babae at kukunin niya ang kailangan ko at iniwan ito sa harap ng pintuan, at pagkatapos ay ililipat ko ang pera sa kanyang bangko para sa dinala niya sa akin, kaya mabuti iyon. At ganoon din ang ginawa ko para sa kanya. Para sa nanay ko, kapag nagtatrabaho ako, kukuha ako ng mga mensahe at ihahatid ito sa kanyang pintuan para sa kanya. So, we helped each other out as a family, especially if you're isolating.”
– Clinically vulnerable na tao |
Kadalasan ang lakas ng impormal na suporta sa pamamagitan ng mga kaibigan at pamilya ay nangangahulugan na ang pormal na suporta ay hindi kailangan upang ihiwalay ang sarili. Nangangahulugan ito na ang ilang mga kontribyutor ay hindi naghanap ng mga pormal na serbisyo ng suporta kaya hindi nila alam ang mga ito.
| “ | Hindi ko kailangang gamitin ito, ngunit alam ko na […] nagpatakbo ng iba't ibang mga scheme sa panahon ng lockdown. Pagsusuplay-, pagdadala ng mga panustos sa mga pamilyang nagbubukod at kailangan, ngunit tulad ng sinasabi ko, hindi ko kailangang gamitin ang mga ito sa aking sarili.”
– Manggagawa sa paggawa |
Ang patuloy na suporta ng espesyalista sa bahay sa panahon ng pandemya ay nakatulong sa ilang taong may mga kondisyon sa kalusugan na ihiwalay ang sarili. Ang mga nag-aambag na ito ay nagsalita tungkol sa kung paano ang pagpapatuloy ng suportang ito, madalas sa malayo, ay nagpapahintulot sa kanila na sumunod sa mga alituntunin sa pag-iisa sa sarili nang hindi bumababa ang kanilang kalusugan.
| “ | Sa tingin ko karamihan sa mga nauugnay na impormasyon ay dumarating sa pamamagitan ng [isang] consultant sa [ospital]. Iyon at siya [ang kanyang asawang may kanser] ay may isang nakatalagang nars doon. Tumatawag siya ng dalawa o tatlong beses sa isang linggo, para lang masigurado na maayos ang [kanyang asawa], at maayos ang mga bagay-bagay...mayroon kaming backup na maaari naming kausapin, at anumang mga tanong namin, nasasagot nila […] gaya ng sinabi ko kanina, na tiniyak namin na alam namin ang mga patakaran na dapat naming mahigpit na sundin sa panahong iyon.”
– Miyembro ng pamilya o tagasuporta ng isang tao na kinakailangang ihiwalay ang sarili |
Narinig namin mula sa iba ang tungkol sa pagiging kasangkot sa komunidad na nagbibigay ng suporta sa mga panahon ng pag-iisa sa sarili. Nag-iiba-iba ito sa iba't ibang lugar depende sa mga kasalukuyang network o suportang naka-set up sa panahon ng pandemya, na kung minsan ay nasasangkot ang lokal na pamahalaan. Naalala ng ilan ang paggamit ng mga app at social media upang malaman kung sino ang nangangailangan ng mga mahahalagang bagay sa panahon ng pag-iisa sa sarili upang makatulong ang mga tao sa komunidad na maibigay ang mga ito. Ito ay madalas na impormal at lumitaw nang maaga sa pandemya para sa mga kinakailangang ihiwalay ang sarili.
| “ | Kaya, mayroon kaming isang pangkat ng Covid sa WhatsApp na ginawa ng aming lokal na konseho, na kinuha ang bawat kalye at itinakda ang lahat ng ito upang ang lahat na online ay malinaw na may kontak na iyon. At, sinubukan nilang ipaalam sa mga tao kung aling mga tahanan ang walang access para matulungan sila ng mga lokal na tao kung wala silang access [sa mga mahahalaga].”
– Clinically vulnerable na tao |
Ang mga lokal na organisasyon ng komunidad ay may mahalagang papel sa pagbibigay ng direktang suporta sa ilan na nagbukod sa sarili, na partikular na mahalaga para sa mga sambahayang madaling maapektuhan ng klinikal at sa mga nakatira sa liblib o kanayunan. Gayunpaman, nakadepende ito sa perang magagamit, nililimitahan ang bilang ng mga tao na nasuportahan sa ganitong paraan.
| “ | Ang simbahan ko, [pangalan ng simbahan], talagang sinusuportahan nila ang marami sa aming mga kongregasyon na baka may sakit ang kanilang mga anak, at hindi sila pinapayagang magtrabaho o nasa isang tiyak na lugar. Nagde-deliver talaga sila ng mga pagkain na kailangan nila linggu-linggo. Kaya, ito ay isang napakagandang tulong para sa ilan sa aking mga miyembro ng simbahan. Bagaman, kung wala silang sapat na badyet upang suportahan ang maraming indibidwal na nangangailangan ng tulong na iyon, magagawa lang nila ang maliit na magagawa nila.
– Kontribyutor ng Every Story Matters |
| “ | Noong Marso 2020, nagpulong ang mga pinuno ng relihiyon, mga konsehal ng parokya, mga lokal na GP at mga may-ari ng negosyo upang talakayin kung paano masusuportahan ng ating nakahiwalay na komunidad sa kanayunan ang mga residente sa nayon at mga nasa labas na bukid at tahanan. Mahigit 100 boluntaryo ang dumating at bawat isa ay binigyan ng 20 tahanan sa loob ng isang partikular na postcode upang suportahan. Naghatid sila ng mga postkard na may mga pangalan at mga detalye sa pakikipag-ugnayan sa bawat isa sa 20 tahanan na iyon at naghatid ng mga gamot at pamimili, naglalakad-lakad sa mga aso, nakipag-chat mula sa isang ligtas na distansya at sa ilang mga kaso ay nakipagkaibigan sa mga nakatirang mag-isa na kung hindi man ay hindi nakipag-ugnayan sa sinuman sa loob ng maraming buwan.
– Kontribyutor ng Every Story Matters |
Kalayaan
Habang nagpapatuloy ang pandemya, ang pagnanais na makisali sa edukasyon at paglalakbay ay naging dahilan upang subukan ang ilan. Nagsalita ang mga tao tungkol sa kinakailangang magpasuri para makapag-aral sa kolehiyo at masuri ang kanilang mga anak para makapag-aral sila, gayundin ang mga legal na kinakailangan para makapagbigay ng negatibong PCR test para makapaglakbay sa ibang bansa.
| “ | Magbakasyon […] kailangan mong magsagawa ng mga pagsusuri sa PCR noong pumunta ka at pagkatapos ay pagbalik mo, kaagad […] noong nagsimula akong magbakasyon […] muli, [naaalala ko] na nagsimulang gumawa ng higit pang mga pagsusulit dahil lamang ito ay kinakailangan ng batas.”
– Kontribyutor ng Every Story Matters |
Gayundin, narinig namin mula sa mga taong nagsabi sa amin na ang pagsubok ay may papel sa pakiramdam ng mga tao na mas may kakayahan at handang makihalubilo, at narinig namin mula sa mga taong sumubok sa buong pandemya para sa kadahilanang ito. Ito ay dahil ang pagsusuri ay nakita bilang isang paraan ng pagbabawas ng panganib ng pagkalat ng virus. Ang isang negatibong LFT ay nagbigay ng 'patunay' na ang isang tao ay ligtas na makihalubilo sa iba.
| “ | Mahusay iyon dahil mapapatunayan kong malusog ako […] para makapunta ako [sa…] mga lugar [tulad ng] mga nightclub, […] aking kolehiyo o kahit saan.”
– Taong ang unang wika ay hindi Ingles |
Ang pagsali sa contact tracing ay nadama din na isang mahalaga at kinakailangang hakbang para makihalubilo sa iba sa labas ng tahanan, lalo na sa paglabas ng lipunan sa lockdown at muling nagbukas ang mga cafe, bar at restaurant.
| “ | Ito ay isang paraan para makalabas ang mga tao. Pinayagan nito ang mga tao na lumabas, alam mo, 'mag-sign in at maaari kang magkaroon ng pagkain sa restaurant na ito'. Nangangahulugan ito na kung makipag-ugnay ka, maaari kang [mag-isa] na ihiwalay, at halos nagbigay ito sa iyo ng pag-uudyok na pumunta, 'Sa totoo lang, dapat akong gumawa ng isang pagsubok'."
– Taong nakakaranas ng kahirapan sa pananalapi |
Pagpapagaan ng takot
Sinabi sa amin ng mga nag-aambag na lumahok sila sa pagsubok sa panahon ng pandemya upang maibsan ang kanilang takot at pag-aalala tungkol sa pagkakaroon ng virus. Ito ay lalo na ang kaso sa simula ng pandemya dahil nakatulong ito sa pagkumpirma kung ang kanilang mga sintomas ay dahil sa Covid-19 at nabawasan ang mga takot tungkol sa kanilang sariling kaligtasan at ang panganib ng impeksyon.
| “ | Anumang oras na bumahing o uubo ka, […] parang, 'Kailangan ko ba ng pagsusulit? [...] Nagkaroon na ba ako ng Covid?' at pagsubok.”
– Taong nabubuhay na may Long Covid |
| “ | Sa tingin ko panic, alam mo, kung nakakatanggap ka ng text message na nagsasabi sa iyo na nakasama mo ang isang taong nasubok na positibo, awtomatiko mong iisipin, 'Oh Diyos ko, makukuha ko ito.' Kaya oo, lalabas ka at magpasuri para dito. Para sa akin personal, ito ay gulat.
– Taong nagtatrabaho sa pangangalagang pangkalusugan at panlipunan |
Ang mga pag-aalala ay mas matinding naramdaman ng mga nag-aambag na may mga kasalukuyang kondisyon sa kalusugan.
| “ | Ako ay nasa [isang] high-risk na grupo, kaya alam ko na kailangan kong sundin ang mga alituntunin at magpasuri. Ito ay isang no-brainer para sa akin.
– Miyembro ng komunidad na sumuporta sa mga tao na ihiwalay ang sarili |
Ang takot at pag-aalala tungkol sa pagkontrata ng Covid-19 ay iniugnay ng ilang kontribyutor sa coverage ng media at pag-uulat sa bilang ng mga namamatay. Para sa ilan, ang pag-uulat tungkol sa mga pagkamatay ay nakaimpluwensya sa mga tao na subukan. Higit pa rito, ang personal na pagkilala sa mga taong may malubhang sakit o namatay mula sa virus ay nangangahulugan na ang ilang mga nag-ambag ay nakaramdam ng higit na takot sa Covid-19 na isa pang dahilan upang subukan ito.
| “ | Sinubukan ko ang lahat, dahil […] ang aking tiyuhin ay pumasok sa ospital na may menor de edad na kondisyon sa puso [at…] nahuli si Covid at […] siya ay talagang namatay. […] Nawalan ako ng miyembro ng pamilya dahil dito, [kaya alam ko] hindi lang media hype […] ito ay totoo. Kaya, nagpatuloy ako sa pagsubok hanggang sa sinabihan kami na huwag […] Mayroon akong app sa aking telepono, at regular na nasubok, at ibinigay ang aking mga resulta.”
– Zero-hours contract worker |
Access at kaginhawaan
Mga pagsusuri sa PCR
Sa unang bahagi ng pandemya, ang mga pagsusuri sa PCR ay magagamit upang mag-book online o sa pamamagitan ng telepono at ang mga appointment ay nasa mga testing center. Ang mga pagsusuri sa PCR ay maaari ding matanggap sa pamamagitan ng koreo at gawin sa bahay.
Maraming kontribyutor na narinig namin mula sa naglalarawan ng isang diretso at mabilis na proseso sa pag-book ng mga appointment sa PCR test online o sa pamamagitan ng telepono, na nagbibigay-daan sa kanila na sumubok kapag naisip nilang kailangan nila. Lumilitaw na ang pinaghihinalaang kaginhawahan ay isang pangunahing enabler para sa mga taong nagpapasyang sumubok. Pagkatapos ibigay ang kanilang postcode, inalok sila ng pagpipilian ng mga test center na nakalista ayon sa kalapitan at nakapili sila ng maginhawang timeslot.
| “ | Napakadaling sundan […] literal mong ilagay ang iyong postcode, at […] ito ay magsasabing, [...] 'ito ay 1.1 milya ang layo, ito ay 3.5 milya ang layo...' […] pipili ka lang […] pagkatapos ay [piliin] ang oras na maaari mong ilabas […] ilagay sa iyong mga detalye, at iyon na."
– Nag-iisang magulang |
| “ | Nag-book ako ng Covid test na talagang mabilis at madali. Ang test center ay halos 20 minutong biyahe mula sa akin. […] Ang buong proseso ay talagang malinaw at mahusay na binalak.”
– Kontribyutor ng Every Story Matters |
Ang ilan sa mga nag-isip sa kanilang sarili na hindi gaanong marunong sa teknolohiya ay nagsabi na ang proseso ng online booking ay naging mas madali sa paglipas ng panahon, habang sila ay naging pamilyar at habang ang system ay nag-save at naalala ang mga personal na detalye.
| “ | Lahat ng ito ay online, na […] isang bagay na hindi namin pamilyar [...] nahirapan namin ito sa simula, ngunit pagkatapos ay nakuha namin ito."
– Taong naninirahan sa isang multi-generational na sambahayan |
| “ | Ang mas maraming pagsubok na ino-order mo[ed] mas madali ito dahil ito [ang sistema ng booking] ay mayroong lahat ng iyong impormasyon [naimbak].”
– Taong may kahirapan sa pagbasa |
Ang opsyong mag-book sa pamamagitan ng telepono ay nakatulong sa ilang tao na mapagaan ang mga hadlang sa literacy.
| “ | Kinailangan naming tumawag at humingi ng pagsusulit […Na-book ko ito sa pamamagitan ng telepono] dahil hindi ako masyadong magaling sa pagbabasa.”
– Taong may kahirapan sa pagbasa |
Maraming kontribyutor na bumisita sa mga PCR test center ang nagsabing maganda ang pagkakaroon ng appointment. Ang mga pareho o susunod na araw na appointment ay karaniwang ibinibigay para sa mga nagbu-book nang maaga, at ang maikling oras ng paghihintay ay nagpadali sa pag-access para sa mga pumapasok sa mga drop-in center. Ang mga oras ng pagbubukas ng mga test center ay nagbigay-daan din sa mga tao na dumalo sa mga appointment sa maginhawang oras.
| “ | Ang mga istasyon ng [pagsubok] ay bukas sa loob ng mahabang panahon sa araw. Kaya, sabihin […] ang mga sintomas [nagsimula] sa gabi, hindi mo na kailangang maghintay ng matagal upang pumunta at magpasuri, maaari kang makapasok sa […] 7:00 ng umaga kung gusto mo.”
– Nag-iisang magulang |
Bagama't naramdaman ng ilang nag-aambag na ang mas malalaking test center ay mas madaling ma-access dahil sa kanilang kapasidad, ang iba ay sadyang humingi ng appointment sa mas maliliit na test center at/o sa mas tahimik na mga oras upang mabawasan ang inaasahang paghihintay. Ang pagkakaroon ng isang pagpipilian at hanay ng mga sentro ay nagpadali sa mga tao sa paggawa ng mga desisyon na nababagay sa kanila. Ang ibang mga tao na aming narinig mula sa ay hindi nakaranas ng madaling pag-access sa mga test center at ang mga kuwentong ito ay makikita sa 'Barriers' chapter.
| “ | Sinigurado namin na pumunta kami sa isang unsociable na oras, at hindi naman ito abala, walang pila. Diretso kaming pumasok, napakadali.”
– Miyembro ng pamilya o tagasuporta ng isang tao na kinakailangang ihiwalay ang sarili |
Maraming mga test center ang lokal, ang ilan ay nasa maigsing distansya, na naging madali at maginhawang puntahan. Ito ay partikular na ang kaso para sa mga taong may access sa isang kotse, o sa magandang pampublikong koneksyon sa transportasyon, sa parehong urban at rural/malayuang lugar.
| “ | Nagulat ako sa kung gaano kadali ito, kailangan kong aminin. Yung una kong ginawa, akala ko mas magiging hassle, samantalang [sa katunayan] may mga pagpipilian sa paligid ko. Hindi ko na kinailangan pang pumunta ng napakalayo […] dahil medyo rural ako.”
– Tagapag-alaga |
Ang ilang mga nag-ambag ay nagsabi na ang kalapitan ng mga sentro ng pagsubok ay tumaas sa paglipas ng panahon, na ang mga sentro ay nagbubukas nang mas malapit sa tahanan habang nagpapatuloy ang pandemya.
| “ | Sa mga unang yugto, napakaraming malalaking sentro ng pagsubok […] nang makarating ito sa akin, […] noong Agosto nang sumunod na taon, hindi naman ganoon kalayo ang aming pupuntahan.”
– Miyembro ng pamilya o tagasuporta ng isang tao na kinakailangang ihiwalay ang sarili |
Narinig namin mula sa ilang nag-ambag na natagpuan ang mga testing center na madaling ma-access para sa mga Bingi at mga taong may mga kapansanan, kabilang ang para sa mga may pisikal na kapansanan.7 Pinadali nito ang pag-access sa mga PCR test mula sa mga test center na ito.
| “ | Bumisita ako sa Covid test center. Mayroon silang A4 na piraso ng papel na nakalamina na may simpleng impormasyon dito. At saka pipirmahan nila ako, Bingi ka ba? At sasabihin kong oo. Pagkatapos ay ibibigay nila sa akin ang kapirasong nakalamina na papel na ito ay naa-access at ginamit ang simpleng komunikasyon. Marami tayong mga Bingi na nakatira sa lugar na ito. Ito ay isang magandang kasanayan at dapat i-set up sa lahat ng mga sentro.
– Bingi |
| “ | Ako ay gumagamit ng wheelchair [at may] isang WAV [wheelchair accessible vehicle…] kapag nagpunta kami sa mga test center, lahat ito ay may kapansanan sa pag-access, hindi pinaganang paradahan. Wala namang naging isyu doon.”
– Kontribyutor ng Every Story Matters |
Narinig din namin mula sa mga kontribyutor na naninirahan sa kanayunan/malayuang lokasyon na nadama na makatuwirang maglakbay nang higit pa upang maabot ang isang sentro ng pagsubok, dahil ang pagmamaneho ay karaniwan para sa kanila.8
Inilarawan ng maraming kontribyutor ang malinaw at maayos na proseso ng test center. Ang mga may positibong karanasan sa mga PCR test center ay nagsabing malinaw ang signposting papunta at sa loob ng mga center. Sinabi nila na ang mga na-pre-book na appointment para sa mga partikular na timeslot ay nakatulong upang mabawasan ang mga oras ng paghihintay, at ang paggabay mula sa mga kawani sa test center ay nakatulong din na gawing simple at diretso ang proseso.
| “ | Napakahusay ng pagkakaayos nila. Ito ay isang napakabilis, mahusay na proseso. […] Ikaw [ay] magda-drive papasok at sasabihin ng mga tao, 'Halika rito', 'Park dito', 'Window down'. […] Natapos ito sa ilang segundo at lalabas ka sa kabilang dulo […] hindi na namin kinailangan pang maghintay.”
– Tagapag-alaga |
| “ | Napaka-organized nila. Nang lumabas kami para sa mga pagsusulit, ang lahat ay naka-signpost nang maayos, mahusay na nakadirekta. Nagawa naming panatilihin ang aming mga distansya; madali ang parking. Nagkaroon kami ng aming mga timeslot at iningatan sila. Mabuti naman.”
– Clinically vulnerable na tao |
Ang social distancing at mga hakbang sa pagkontrol sa impeksyon (kabilang ang personal protective equipment (PPE) at mga regimen sa paglilinis) ay inilagay sa mga test center, na nakita ng ilang nag-ambag na nakapagpapatibay.
| “ | Masaya ako na mayroon silang [paglilinis] na mga punasan doon na handang punasan pagkatapos ng bawat tao.”
– Tagapag-alaga |
Nagkomento din ang mga taong narinig namin sa suporta, palakaibigan, at mahinahon na diskarte ng mga kawani ng test center, na binabanggit na ito ay pinadali ng mahusay na antas ng staffing. Ang mga malinaw na tagubilin mula sa madaling lapitan na kawani ay partikular na nakakatulong para sa mga taong hindi gaanong kumpiyansa, kabilang ang ilang halimbawa na ang unang wika ay hindi Ingles.
| “ | Sa oras na iyon, ang aking wikang Ingles ay napakasama. Hindi ko masundan ang mga patakaran sa application [contact tracing app], wala akong alam tungkol dito [… sa testing center] tinulungan nila ako, napakahusay, napakarami. Ito ay talagang nakakatulong para sa akin.”
– Taong ang unang wika ay hindi Ingles |
Ang ilang kontribyutor na hindi nakadalo sa mga test center dahil sa kondisyong pangkalusugan ay gumamit na lang ng mga home kit. Ang mga ito ay ipinadala sa pamamagitan ng post o sa pamamagitan ng courier. Pinahahalagahan ng mga nag-aambag ang kanilang pagiging naa-access at bilis ng paghahatid, ipinapaliwanag na ang kaginhawaan ay nagpadali sa pagsusuri sa PCR para sa kanila.
Ang kakayahang magbalik ng mga pagsubok sa pamamagitan ng mga post box na malapit ay naging maayos din para sa mga contributor na narinig namin mula sa kung sino ang gumamit nito. Ang mga nagbahagi ng kanilang mga kuwento ay nagsabi na ang kanilang karanasan ay ang mga kahon ng priyoridad ay mahusay na namarkahan at madaling mahanap. Ang pinalawig na oras ng koleksyon ay nag-aalok ng karagdagang flexibility at kaginhawahan. Ang mga nakatira sa malayo mula sa pinakamalapit na post box, gayunpaman, ay nagsabi na nahihirapan silang gamitin ang mga ito nang walang access sa kanilang sariling sasakyan.
| “ | Ito ay nasa tuktok ng aking kalsada, kaya hindi ko na kailangang maglakbay nang malayo, at naisip ko lamang na ito ay napaka-maginhawa. Sa tingin ko may mga talagang […] nahuling koleksyon din sa isang punto, kaya hindi mo ito makaligtaan.”
– Clinically vulnerable na tao |
| “ | [Ang] pinakamalapit na isa ay apat na milya mula sa akin […] kung wala akong access sa isang kotse, kung gayon ay magiging isang hamon iyon.”
– Miyembro ng pamilya o tagasuporta ng isang tao na kinakailangang ihiwalay ang sarili |
Inilarawan ng ibang mga kontribyutor ang pag-book ng mga koleksyon ng courier upang ibalik ang mga nakumpletong pagsubok. Nakakatulong ito para sa mga may isyu sa kadaliang kumilos.
Mga LFT
Ang Lateral Flow Tests (LFTs) ay ginawang available sa lahat sa England, Scotland at Wales noong Abril 2021 na nagbigay-daan sa libreng access sa mabilis na pagsubok. Sumunod ang Northern Ireland noong Setyembre 2021.
Ang bilis ng pag-access sa mga resulta ng LFT ay mahalaga sa mga nag-aambag. Ang mga instant na resulta ng LFT ay mas maginhawa kaysa sa mga araw ng paghihintay para sa resulta ng PCR test, lalo na dahil pinahintulutan nito ang mga tao na gumawa ng agarang desisyon tungkol sa kung kailangan ba nilang ihiwalay ang sarili o hindi.
| “ | Ang lateral flow testing ay napakadali kaysa sa PCR sa diwa na hindi na kailangang hintayin ang mga resulta na maipadala at bumalik. Alam mo doon at pagkatapos kung kailangan mong simulan ang iyong [self-] isolation o hindi [...] kung magpapadala ka ng PCR, sa pag-aakalang ikaw ay may Covid, ikaw ay [nag-iisa] sa loob ng tatlong araw [habang naghihintay ng resulta], at pagkatapos ay [minsan] lumalabas na ikaw ay [sarili] na nag-isolate para sa wala dahil hindi ito Covid. So maganda ang aspetong iyon, naisip ko.”
– Tagapag-alaga |
Malugod na tinanggap ng ilang nag-aambag ang kadalian at kaginhawaan ng kakayahang masuri para sa Covid-19 sa bahay nang hindi kinakailangang mag-book ng appointment sa isang testing center at pinahahalagahan na ang mga pagsusulit ay walang bayad.
| “ | Mas madalas kaming sumubok noon dahil hindi mo na kailangang mag-book o anumang bagay na katulad nito. Kapag nasa kamay na ang mga pagsusulit, maaari mong subukan kung kailan at kailan mo naramdaman na kinakailangan ito."
– Taong may pangmatagalang pisikal na kondisyon sa kalusugan |
| “ | Nang ibigay sa amin ang [LFT] na mga kahon […] ito ay halos, parang, 'Okay, nakuha ko ito [isang LFT pack] kaya maaari ko ring [gamitin ito].' Hindi nakakaabala [gaya noong kailangan mong] pumunta at mag-test […] sa isang center […] Malamang na mas gusto kong gawin ito kapag nagkaroon na kami ng pasilidad na gawin ito mula sa bahay kasama ang mga lateral flow tests.”
– Taong nagtatrabaho sa pangangalagang pangkalusugan at panlipunan |
Ang libreng probisyon ay nagbigay-daan sa ilang organisasyon ng komunidad na mamahagi ng mga pagsubok sa mga tao at aktibong hinikayat ang mas malawak na pagsubok. Ang isang halimbawa ay sa isang foodbank, kung saan ang mga kawani ay mamamahagi ng mga pagsubok at maskara kasama ang mga pakete ng pagkain.
| “ | Nagawa naming […] bigyan sila ng isang pagsubok sa daloy [pati…] Hindi nila ito hiniling; parang kami [lang], 'Narito ang isang pagsubok sa daloy.' [...] namimigay din kami ng mga maskara. Ang mensahe ay, 'Keep safe.' At sa palagay ko natagalan ang mga tao, ngunit sinimulan nila [gamitin ang mga ito…].”
– Miyembro ng komunidad na sumuporta sa mga tao na ihiwalay ang sarili |
Ang pagkakaroon ng pagsubok sa bahay ay nakapagpapatibay din para sa mga taong nag-aalala tungkol sa panganib ng impeksyon sa o papunta sa mga sentro ng pagsubok. Kasama rito ang mga taong immunosuppressed, clinically vulnerable, o nakatira kasama ang Long Covid, pati na rin ang mga taong may mga mahal sa buhay na may ganitong mga kondisyon sa kalusugan.
| “ | Ang self-testing […] ay nangangahulugan na mayroon kang seguridad ng iyong sariling tahanan upang […] gawin ang mga bagay na ito; hindi mo na kailangang lumabas."
– Taong nabubuhay na may Long Covid |
Maraming nag-ambag ang nagsabi sa amin na ang mga LFT ay madaling magagamit sa kanila sa buong pandemya, sa kabila ng kaalaman sa mga kakulangan o paghihigpit. Sinabi ng mga nag-aambag na hindi sila personal na naapektuhan ng mga kakulangan at iniugnay ito sa priyoridad na pag-access para sa ilang partikular na grupo (gaya ng mga frontline healthcare staff), ang hanay ng mga lugar kung saan maaaring kolektahin ang mga test pack, ang kakayahang mag-order ng maraming pagsusuri kapag ang mga kakulangan ay hindi isang isyu at pagbabahagi sa pagitan ng mga pamilya o iba pang mga contact.
| “ | Madaling makuha ang mga lateral flow test. Wala kaming anumang isyu […] Laging sapat.”
– Tagapag-alaga |
| “ | Isinasantabi ko ang mga ito […] ginagamit lamang ang mga ito kapag kailangan ko, dahil alam kong may kakulangan sa isang pagkakataon. […] kung wala akong [anumang…] at gusto kong gumamit ng isa, tinawagan ko ang aking kapatid na babae at […] kumuha ng isa [mula sa] kanya [...] palaging may isang tao na maaari mong tawagan at sabihin, 'Mayroon ka bang ekstrang testing kit?'”
– Clinically vulnerable na tao |
Ang pag-order ng mga pagsubok para sa paghahatid sa bahay at pagkolekta ng mga ito sa lokal ay parehong inilarawan bilang medyo mabilis, madali at maginhawa. Ipinakita ng ilang nag-ambag na ang pagiging naa-access ay pareho para sa mga nasa liblib na lugar bilang mas maraming tao.
| “ | Ang mga tao sa aking maliit na isla ay nakakuha ng kanila sa parehong oras na ang mga tao sa […ang] mainland ay nakakuha ng kanila. Ako ay lubos na humanga sa kung gaano kabilis […] at kung gaano kadali […] ang ilan ay naipadala sa post, at pagkatapos ay nagbago ito sa pagkuha sa kanila mula sa iba't ibang mga sentro. Napakadali noon.”
– Taong nabubuhay na may Long Covid |
Napansin din ng mga kontribyutor na ang mga test pack ay madaling ibigay at magagamit, nang hindi kinakailangang hanapin ng mga tao ang mga ito. Kasama ito sa mga pampublikong espasyo tulad ng mga supermarket, aklatan, lugar ng pagsamba, mga foodbank, sa mga operasyon ng GP at sa mga site ng Gypsy at Traveler.
| “ | Inabutan ako ng isang kahon ng sampu sa labas [isang supermarket], kaya hindi ko na kinailangan pang hanapin. Itinulak sila sa iyo: 'Libre ang mga ito, iuwi mo sila. Gamitin ang mga ito sa tuwing kailangan mo ang mga ito'. Kaya [...] Hindi ko sasabihin na ang pagkuha ng access sa kanila ay mahirap sa lahat."
– Tagapag-alaga |
| “ | May isang [NHS] van na lumabas at […] nakaparada sa shopping precinct, at na-advertise [online] na pupunta ito doon […] sa ilang mga oras, at may mga tao doon […] na namimigay ng [LFT] na mga kahon […] at nagbibigay sa iyo ng payo kung hindi mo alam kung paano gamitin ang mga ito.”
– Clinically vulnerable na tao |
Naalala din ng ilang nag-aambag ang mga test pack na kasama sa mga paghahatid ng iniresetang gamot o ibinaba sa mga mahihinang sambahayan ng mga manggagawa sa pangangalagang pangkalusugan. Ang ilang mga kontribyutor na nagtrabaho sa mga organisasyong nakaharap sa komunidad ay nagsabi na ang mga pagsusulit ay ipinadala sa kanila para ipamahagi sa mga miyembro ng komunidad.
| “ | Dahil sa aking hika […] Maaari ko silang ihulog sa akin, o i-post din sa akin. […] dahil alam ko lang na opsyon iyon, sa tingin ko ay maganda iyon.”
– Clinically vulnerable na tao |
Pagsubaybay sa contact
Ang mga nag-aambag na may isa sa mga contact tracing app sa pangkalahatan ay nag-isip na ito ay madaling i-navigate at gamitin. Mabilis itong mag-download at mag-input ng impormasyon, tila tumatakbo sa tabi ng iba pang mga app sa kanilang mga smart phone nang walang panghihimasok at hindi nangangailangan ng maraming pakikipag-ugnayan mula sa user kapag na-set up na ito.
| “ | Diretso lang. Sa naaalala ko, diretsong ilagay ang iyong mga detalye, mga personal na detalye, mga dahilan kung bakit, napakabilis at madaling format na gawin iyon.”
– Zero-hours contract worker |
Pagtitiwala
Ang ilang mga kontribyutor ay nagtiwala ng higit sa mga pagsusuri sa PCR na isinasagawa ng mga kawani sa mga sentro ng pagsubok. Nadama nila na, dahil sa kanilang kadalubhasaan, ang mga tauhan ng PCR testing center ay magiging mas masinsinan at tumpak kaysa sa mga taong mismong gumagamit ng nasal o throat swab.
| “ | Naaalala ko noong una silang lumabas, ang mga PCR […] na ginamit nila para sa pagsusulit para sa iyo […] ay literal na hahatakin mo na parang [sa] isang drive-through, at [...]
– Taong nakakaranas ng kahirapan sa pananalapi |
Dali ng paggamit
Sa kabila ng pag-alala ng ilang kontribyutor na kailangan nilang basahin ang mga tagubilin sa tuwing gagamit sila ng mga LFT, ibinahagi ng mga kontribyutor na madaling gamitin ang mga pagsubok na ang mga hakbang ay diretso at maliwanag. Sinabi rin sa amin ng mga taong kumukumpleto ng PCR self-test sa bahay na nakakita sila ng mga tagubilin para sa pagkumpleto at pagbabalik ng malinaw sa mga pagsusuri.
| “ | Ang muling pagbabasa at pagsunod sa mga tagubilin ay mahalaga. Hindi […] instinctual na gamitin ang mga ito [ang mga pagsusulit,] ngunit maayos ang mga tagubilin at walang masyadong […] prosesong kasangkot na hindi ko maintindihan.”
– Miyembro ng pamilya o tagasuporta ng isang tao na kinakailangang ihiwalay ang sarili |
| “ | Ang pag-order ng Lateral Flow Test kit ay simple online at malinaw ang mga tagubilin sa [kanilang] paggamit."
– Kontribyutor ng Every Story Matters |
Sinabi ng ilang kontribyutor na gumamit sila ng mga diagram sa mga LFT kit at online na video para tulungan silang maunawaan ang mga hakbang na kinakailangan para sa pagsubok. Ang mga tutorial na ito ay kadalasang ginagamit bilang karagdagan sa, sa halip na, sa pagbabasa ng mga nakasulat na tagubilin.
| “ | Isa iyon sa mga bagay kung saan kahit hindi ka nagbabasa o nagsasalita ng Ingles, ang pagtingin sa mga larawan ay malalaman mo kaagad kung ano ang gagawin. […] mayroon pa ngang […] mga online na video kung saan makikita mo […] kung paano ito ginagawa ng mga tao […] para kopyahin mo lang […] hindi ito mahirap kahit ano pa man: napaka-simple.”
– Taong naninirahan sa isang multi-generational na sambahayan |
Ang pagpapakilala ng mga LFT na nangangailangan lamang ng mga pang-ilong na pamunas ay gumawa ng malaking pagkakaiba sa antas ng ginhawa ng ilang nag-aambag kapag sumusubok.9 Ang ilang mga nag-ambag ay nagpahayag ng isang malakas na kagustuhan para sa mga pamunas ng ilong at inilarawan na naibsan ng pagbabagong ito.
| “ | Ang mga pinakabago na may mas maikling usbong ay ang pinakamagandang bagay na nagawa nila […] na natural na pag-aatubili na maglagay ng mahabang […] itinaas ang iyong ilong na lumabas sa bintana. Talagang nakakita ako ng mas maraming tao na gustong gumamit ng [lateral] flow test."
– Miyembro ng komunidad na sumuporta sa mga tao na ihiwalay ang sarili |
Nakapirming Paunawa sa Parusa
Bagama't wala kaming narinig mula sa sinumang nagsabi sa amin na nakatanggap sila ng Fixed Penalty Notice (FPN), tinalakay ng ilang tao ang mga pananaw sa mga FPN at ang epekto nito sa pag-uugali.10
Kinausap kami ng mga kontribyutor tungkol sa kung paano mabisa o hindi epektibo, naisip nila na ang mga FPN ay isang hadlang sa paglabag sa mga panuntunan sa pag-iisa sa sarili, ang variable na kahihinatnan sa pananalapi ng mga multa, gayundin ang ilan mas malawak na implikasyon ng paggamit ng mga FPN sa pag-uugali ng patrol.
Para sa ilang indibidwal, ang banta ng mga multa ng parusa para sa paglabag sa mga panuntunan sa pag-iisa sa sarili ay nakaimpluwensya sa pag-uugali at hinihikayat ang pagsunod. Ang mga naiimpluwensyahan ng mga multa ay nagbigay-diin sa pasanin sa pananalapi, na naglalarawan sa halaga bilang makabuluhan kahit para sa mga may mas malaking pinansiyal na paraan.
| “ | … [Nang] narinig kong pinamulta ka, naisip ko, oo, talagang nagbubukod [ako] sa sarili. Oo. Sa palagay ko ay talagang positibo ang paglalagay ng multa dahil sa palagay ko ay ginawa nitong higit na ihiwalay ang mga tao."
– Tagapag-alaga |
| “ | Kung ako ay magkakaroon ng multa, ito ay makakaapekto sa akin sa pananalapi. Hindi ko pa rin kayang bayaran ito. Sa palagay ko, mabuti sa kanila na ipakilala iyon, upang ihinto ang mga tao na hindi [pagbukod sa sarili]."
– Taong nakatira sa masikip o masikip na tirahan |
Naniwala ang ilan mas malupit na parusa sa pananalapi sana nadagdagan ang bisa ng mga multa, dahil sa mga potensyal na nakamamatay na kahihinatnan ng paglabag sa mga panuntunan sa pag-iisa sa sarili.
| “ | Posibleng mas mabigat na parusa ang ipataw dahil buhay ang pinag-uusapan – dahil sa iyong kapabayaan humigit-kumulang 200 katao ang namatay, walang saysay. Kaya bukod doon, ang pag-uusapan ng multa na say £500 o anuman, maaaring may mas matarik na parusa dito. Buhay ang sinasabi mo. Ayokong mamatay dahil sa kapabayaan ng ibang tao."
– Tagapag-alaga |
Mayroong isang malakas na contingent ng mga nag-aambag na nag-isip na ang mga multa ng parusa ay hindi epektibo sa pagmamaneho ng sumusunod na pag-uugali. Ito ay dahil sa pangungutya tungkol sa kung paano maipapatupad ang pagpapatupad ng self-isolation sa katotohanan. Iminungkahi ng mga komento mula sa mga kontribyutor na ang ang kawalan ng transparency tungkol sa kung paano mapupulis ang pagpapatupad ay nagpapahina sa banta ng mga FPN.
| “ | Narinig ko ang tungkol sa kanila, ngunit sa palagay ko ay hindi talaga ito ipinatupad. Tulad ng, ang ilang mga tao ay mayabang, at hindi sila [nagbubukod] sa sarili, at sila ay dapat, ngunit wala akong nakitang anumang hakbang na ginawa laban sa kanila."
– Taong nabubuhay na may Long Covid |
Sa ilang mga kaso, ang kawalan ng katiyakan ng mga kontribyutor tungkol sa pagpapatupad ay nadagdagan ng a kawalan ng kamalayan ng sinumang pinagmumulta. Ipinadama nito sa mga kontribyutor na ito na, anuman ang kanilang pag-uugali, hindi sila pagmumultahin.
| “ | Well, wala akong natatandaan na kahit sinong kakilala ko o kakilala ko, na pinagmulta. Alam mo ba ang ibig kong sabihin? At, sa tingin ko, dahil hindi mo alam kung kailan ito nangyari, hindi ito mangyayari sa akin. Ganun yung mentality.”
– Miyembro ng komunidad na sumuporta sa mga tao na ihiwalay ang sarili |
Nagkaroon ng mungkahi mula sa isang maliit na minorya ng mga nag-aambag na ang pagkakaroon ng matinding mga hakbang sa pagpapatupad ay maaaring nagkaroon ng kabaligtaran na epekto, na nagdudulot sa kanila hindi sundin ang mga panuntunan sa pag-iisa sa sarili sa panahong iyon.
| “ | Habang higit [ang] mga hakbang ay inilagay upang subukang parusahan ang mga tao, mas hilig kong hindi sumabay sa kanilang pagtuturo.”
– Kontribyutor ng Every Story Matters |
Kapag tinatalakay ang mga FPN sa mga kontribyutor, marami ang nagsalita tungkol sa variable na epekto sa pananalapi ang mga multa ay sa mga tao depende sa mga personal na pangyayari.
Ang pagkakaiba ng epekto sa pananalapi sa mga taong hindi nagtatrabaho sa panahon ng pandemya, o na-furlough ang pinag-uusapan. Ito ay naisip na hindi patas na magpataw ng mga multa sa mga taong posibleng walang trabaho dahil sa pandemic.
| “ | It was ridiculous kasi parang hindi kumikita, mga katulad ko na hindi na-furlough, tapos parang pagmumultahin ako. Wala akong pera na mawawala sa oras na iyon.”
– Taong nakatira sa masikip o masikip na tirahan |
Katulad nito, binanggit din bilang isang grupo ang mga taong walang pagpipilian kundi ang paghiwalayin ang sarili (halimbawa upang kumita ng pera, para sa kalusugan ng isip, o tumulong sa ibang tao) at nanganganib na makakuha ng multa ay binanggit din bilang isang grupo na hindi gaanong naapektuhan ng mga multa ng parusa.
Higit pa sa mga implikasyon sa pananalapi ng mga multa sa parusa, ang mga nag-ambag na dumayo sa UK ay nag-usap din tungkol sa takot sa mas malawak na mga epekto kung mahuhuling lumabag sa pag-iisa sa sarili. Ito ang nagbunsod sa mga nag-aambag sa sitwasyong ito na mag-overcompensate sa pamamagitan ng pagiging sobrang maingat sa paglabag sa anumang mga panuntunan.
| “ | Kapag bago ka sa ibang bansa at hindi ka pa ganap na [aware] tungkol sa wikang iyon at wala kang kakilala, kailangan mo na lang sumunod [sa] mga patakaran dahil walang sinuman ang nandiyan upang suportahan [ka] kung gumawa ka ng maliit, maliit na pagkakamali. So, sinusundan namin silang lahat."
– Taong ang unang wika ay hindi Ingles |
| “ | Ngunit may takot na kapag lumabas ka, maaari kang pagmultahin. At pagkatapos ay naisip ko, 'Sus, kung ako talaga - dahil hindi ako isang mamamayan ng Britanya, kung pagmumultahin ako, kung sasabihin nila, 'Gumagawa ka ng isang bagay na hindi mo dapat gawin', maaaring may panganib na mawala ang aking karapatang manatili sa bansang ito.
– Taong digital na hindi kasama |
- Ang 119 na serbisyo ng telepono ay pangunahing nagsilbi bilang isang helpline at sistema ng pag-book para sa mga serbisyong nauugnay sa Covid-19 sa UK, gaya ng mga pagbabakuna at pagsubok. Nag-alok din ito ng suporta at patnubay tungkol sa self-isolation at tulong pinansyal para sa mga indibidwal na hindi makapagtrabaho dahil sa Covid-19. Ang serbisyo ay libre at magagamit mula sa mga landline at mobile phone. Nagsara ang serbisyong ito pagkatapos ng Enero 31, 2025.
- Kinikilala ng Inquiry ang mas malawak na inklusibong termino ng "d/Deaf" bagama't ang mga taong sinasalita bilang bahagi ng record na kinilala bilang "Bingi".
- Ang Scottish Government Urban Rural Classification ay gumagamit ng 'Remote' para sa mga lugar na higit sa 30 minutong biyahe, o mga lugar na may biyahe sa pagitan ng 30 at 60 minuto mula sa isang Settlement na may populasyon na 10,000 o higit pa.
- Nasal (ilong lang) Swab Lateral Flow Test, (sa halip na Nasopharyngeal (ilong at lalamunan) Lateral Flow Test, ay naging mas laganap noong 2021.
- Ang mga Fixed Penalty Notice (FPNs) na nauugnay sa self-isolation ay inisyu para sa mga paglabag sa legal na kinakailangan, sa England at Wales, na mag-self-isolate kapag kinakailangan:
- Kung nakatanggap ka ng positibong resulta ng pagsusuri sa Covid-19, legal na kinakailangan mong ihiwalay ang sarili para sa isang partikular na panahon.
- Kung ikaw ay nakipag-ugnayan sa pamamagitan ng NHS Test and Trace at natukoy bilang isang malapit na contact ng isang taong nagpositibo sa pagsusuri, legal din na kinakailangan mong ihiwalay ang sarili, kahit na ikaw mismo ang nagpasuri ng negatibo.
4. Mga hadlang: Ano ang mga hadlang sa mga taong nakikilahok sa pagsubok, pagsubaybay sa contact at pag-iisa sa sarili? |
 |
Ang kabanatang ito ay nagdedetalye ng mga karanasan ng mga nag-aambag sa mga hadlang sa pagsubok, pakikipag-ugnayan sa contact tracing system at sa self-isolate. Inilalarawan ng kabanata ang mga hadlang na ito at nagbibigay ng mga halimbawa kung saan at paano nakaimpluwensya ang mga ito sa mga pag-uugali sa panahon ng pandemya.
Magtiwala
Narinig namin mula sa mga nag-ambag na nagpahayag ng matinding pag-aalinlangan at pangkalahatang kawalan ng tiwala sa programa ng pagsubok. Ang isang halimbawa ay ang pananaw na ang mga pagsusuri sa PCR ay idinisenyo upang magbigay ng mga resultang 'false positive'.
| “ | Ang mga maling positibo ay ginamit upang lumikha ng libu-libong tinatawag na 'mga kaso' at makagawa ng nauugnay na isterya. [...] Wala akong anumang pagsubok (bilang isang bagay ng prinsipyo)."
– Kontribyutor ng Every Story Matters |
Nagkaroon din ng pag-aalinlangan sa mga kuwentong narinig namin na may kaugnayan sa katumpakan ng mga LFT at pagiging epektibo sa pagtuklas ng virus. Ang ilang mga nag-aambag, halimbawa, ay hindi kumbinsido na ang isang LFT na ginawa sa bahay, na nagbigay ng isang resulta nang napakabilis, ay maaaring maging tumpak kapag sila ay sanay sa tumpak na medikal na pagsusuri na ginagawa sa isang klinikal na setting.
| “ | […] bago ang pandemya, kung kailangan mong magkaroon ng pagsusulit kailangan mong pumunta sa lab o sa isang siruhano, at ngayon ay bigla mong magagawa ito sa bahay at […] makuha ang mga resulta pagkatapos ng dalawang minuto? […] Maaaring ito ay [totoo…] ngunit sa palagay ko ay hindi natin malalaman kung talagang nagtrabaho sila o hindi.”
– Zero-hours contract worker |
Itinuturing ng ilang nag-aambag na ang mga LFT ay hindi gaanong tumpak kaysa sa mga pagsusuri sa PCR, na naglalarawan sa mga pagsusuri sa PCR bilang mas sensitibo at mas nakakakuha ng mga kaso ng Covid-19 na walang sintomas.11 Nagmuni-muni ang mga tao sa kanilang mga direktang karanasan kung saan naniniwala silang nabigo ang mga LFT na makapaghatid ng positibong pagsusuri sa kabila ng pagkakaroon nila ng mga sintomas na pare-pareho sa virus, o kapag ang kanilang mga sintomas ay katulad ng mga nakapaligid sa kanila na nagpositibo sa virus.
| “ | Ang mga […] walk-in […] ay talagang mas tumpak. May isang pagkakataon na ako ay ganap na asymptomatic at nagpunta sa isang PCR […] walk-in center, at natapos na ako ay nagkaroon ng Covid. [… Sa isa pang] beses […] Nakumbinsi ako [nakuha ko]: Wala akong maamoy na anuman […] Nagkaroon ako ng trangkaso […] at […] tatlong araw na sunud-sunod na ginawa ko ang mga lateral flow […] Lahat sila ay negatibo at pagkatapos lamang sa ika-apat na araw, kapag ako ay napakasakit, lalabas na nagsasabing mayroon ako nito. […] Nawala ang aking amoy at […ay] napakasakit na, [ito] ay nagpapaisip sa iyo na hindi sila ganoon katumpak.”
– Kontribyutor ng Every Story Matters |
| “ | Nagpapakita ng negatibo ang aking lateral flow test, ngunit iba ang iminumungkahi ng aking mga sintomas, kaya nagsinungaling ako para makakuha ng PCR test. Ang mga resulta ay positibo.
– Kontribyutor ng Every Story Matters |
Nag-aalinlangan din ang mga kontribyutor tungkol sa kung gaano katumpak at epektibo ang contact tracing system. Inilarawan nila ang mga puwang sa system na sa tingin nila ay nagpapahina sa kung gaano ito kapaki-pakinabang, halimbawa:
- Gumagana lang ang contact tracing kung ang mga tao ay nagpasuri, at hindi isasama ang mga taong nagkaroon ng Covid-19 ngunit hindi pa nasusuri o umiiwas sa pagsusuri.
- Ang oras na ginugol upang ipaalam sa mga tao ay maaaring sapat na oras upang maikalat ang virus
- Imposibleng matukoy nang tama ang lahat ng mga taong nakipag-ugnayan sa isang taong may Covid-19
- Ang kahulugan ng isang contact ay hindi tiyak - at maaaring hindi ma-trigger sa pamamagitan ng pagiging malapit sa isang tao upang makuha ang virus
| “ | Hindi ko lang makita kung paano nila matutunton ang lahat o malaman ang mga pangalan ng mga tao kung sino ang iyong nakilala. Dahil kung ang tao ay nagdadala ng virus ngunit hindi nakakaramdam ng mga sintomas, pumunta sila sa isang tindahan, ngunit ang tindahan ay nag-aayos kung sino ang nagtatrabaho o kung sino ang maaaring kausapin nila, kaya ang buong bakas na bagay, nakita kong ito ay isang magandang ideya, ngunit sa palagay ko ay hindi ito gagana.
– Taong nabubuhay na may Long Covid |
| “ | Medyo mahirap sabihin kung epektibo ba ang system na iyon o hindi dahil depende sa kung gaano kabilis ang sulat sa iyo o depende sa kung gaano kabilis ang email na nakarating sa iyo, alam mo, dahil maaari ka pa ring makahawa ng mga tao."
– Taong may kahirapan sa pagbasa |
| “ | Makakakuha ka ng mga ping nang random na beses, sa palagay ko. Palagi mong iniisip kung nasaan ang pagkakalantad dahil ito ay dalawa o tatlong araw pagkatapos mong pumunta sa isang lugar, sa palagay ko, at may nasubok at nagparehistro ng kanilang pagsubok."
– Taong may pangmatagalang pisikal na kondisyon sa kalusugan |
Para sa ilan, ang katotohanan na ang pagsubaybay sa pakikipag-ugnay ay nasa lugar kasabay ng pagdistansya mula sa ibang tao at iba pang pag-iingat - tulad ng pagsusuot ng maskara, mga proteksiyon na screen at pakikisalamuha sa labas – nadama na walang kaugnayan at kontraproduktibo, na nagdaragdag sa kawalan ng tiwala sa system.
| “ | I found it a little pointless also, like if you did go in a restaurant and whatever, you have to socially distance, so all the tables and everything is set out really far, compared to normal...Ngunit, pagkatapos ay makakakuha ka pa rin, tulad ng, isang alerto mula sa track at trace.
– Taong nagtatrabaho sa pangangalagang pangkalusugan at panlipunan |
Itinuro din na ang mga contact tracing system na nakabatay sa app ay umaasa sa malaking bilang ng mga tao na gumagamit ng kanilang contact tracing app, pag-upload ng mga resulta ng pagsubok at paglalagay ng impormasyon sa pakikipag-ugnayan nang tumpak at tapat. Gayunpaman, ipinapalagay ng maraming nag-aambag na ang mga system ay hindi sinusunod ng lahat, na humantong sa karagdagang kawalan ng katiyakan tungkol sa pagiging kapaki-pakinabang at epekto. Itinuro ng ilang kontribyutor na madaling mag-upload ng hindi tumpak na impormasyon sa isang contact tracing system, gaya ng paggamit ng mga resulta ng pagsubok ng isang kaibigan. Alam din ng mga kontribyutor ang mga taong hindi nakikilahok sa pagsubaybay sa pakikipag-ugnayan, o ibinahagi na hindi sila nakilahok sa kanilang mga sarili, alinman sa una, o pagkatapos ng ilang oras na paggamit nito. Narinig din namin ang mga kuwento ng pag-aalinlangan tungkol sa pagiging epektibo ng mga contact tracing system na kumonekta at gumamit ng input mula sa mga QR check-in system sa mga lugar.
| “ | Maaasahan lang kasing inputter, di ba? Maaari kang magkaroon ng 100 tao na mag-scan nito, ngunit kung mayroon kang 200 tao, at ang iba pang 100 ay hindi nag-scan nito, kung gayon ito ay walang halaga.”
– Taong may pangmatagalang pisikal na kondisyon sa kalusugan |
Narinig namin mula sa mga kontribyutor na hindi gusto ang pagsubaybay sa contact dahil sa personal na impormasyong kailangan nito. Para sa kanila, ito ay hindi komportable at invasive. Bukod pa rito, hindi kumportable ang ilan sa pagbibigay ng mga detalye sa pakikipag-ugnayan ng kanilang mga kaibigan at miyembro ng pamilya. Mga alalahanin na nauugnay sa pangkalahatang kawalan ng tiwala sa paggamit ng gobyerno ng personal na data, takot tungkol sa cybercrime, hindi alam kung bakit at paano ginagamit ang kanilang impormasyon at pag-aalinlangan kung bakit kailangan talaga ang impormasyong ito, at ang potensyal na makaabala sa iba.
| “ | Ito ay isang pag-aalala kapag iniisip mo ang tungkol sa paglalagay ng iyong impormasyon doon, at sa ilan sa mga pangunahing hack na nangyayari kamakailan sa lahat ng aming impormasyon. Sa tingin ko ito ay maaaring medyo mahina sa na. Kaya lang siguro tinanggal ko, if I remember rightly. Sa palagay ko dumating ako sa punto na naisip ko, 'Sa palagay ko ay hindi maganda ang pagkakaroon nito sa aking telepono', kaya inalis ko ito."
– Clinically vulnerable na tao |
| “ | Tulad ng, naaalala ko ang pagpunta sa isang tunay na butas ng kuneho sa panahon ng Covid, kaya malamang na ako ay nagkaroon ng problema sa mga ito sa oras na iyon. Napunta ako sa buong ruta ng pagsasabwatan at lahat. Hindi ko matandaan nang eksakto, ngunit malaki ang posibilidad na nagkaroon ako ng problema dito.”
– Zero-hours contract worker |
Ang ilan na nagbahagi ng kanilang mga kuwento ay hindi lumahok sa pagsubaybay sa contact dahil sa mga alalahaning ito, o kalaunan ay ini-off ang app dahil sa mga alalahanin tungkol sa seguridad at privacy ng data.
| “ | Tinanong ko sila sa pagkuha ng napakaraming impormasyon mula sa amin. Naaalala ko noong panahong iyon, ang aking kapareha, tiyak na sinabi niya, 'Wala akong ibinibigay sa kanila. Kung mayroon akong Covid, magsusuri ako, mag-iisa ako, gagawin ko ang lahat, ngunit hindi ko sila binibigyan ng anumang impormasyon na hinihiling nila.
– Kontribyutor ng Every Story Matters |
Marami kaming narinig na halimbawa ng pagsubaybay sa contact, at partikular na ang mga app, hindi gumagana nang maayos. Kung mas maraming tao ang nakaranas ng mga isyung ito, mas nawalan sila ng tiwala at tiwala sa system. Ang mga problemang naranasan ay mula sa pagtanggap ng abiso kahit na ang tao ay hindi umalis ng bahay o nakipag-ugnayan sa sinuman, hanggang sa pagsubok na positibo para sa Covid-19 ngunit hindi nakatanggap ng abiso na sila ay nakipag-ugnayan sa sinumang may virus.
| “ | Nakatanggap ako dati ng mga regular na alerto na nagsasabing nakipag-ugnayan ako sa isang tao, o posibleng makipag-ugnayan, kaya medyo hindi ako nagtitiwala sa akin dahil minsan ay hindi pa ako nakakalabas at nagpi-ping ako at lahat ng kakilala ko na nakatrabaho ko ay hindi pa nakakatanggap ng ping pero araw-araw akong nakikisama sa kanila."
– Kontribyutor ng Every Story Matters |
Muli, narinig namin na humantong ito sa ilang tao na i-off ang app, Bluetooth o mga device sa lokasyon, iwan ang kanilang mga telepono sa bahay, o ihinto ang pagbibigay ng tumpak na impormasyon sa pakikipag-ugnayan.
| “ | Nag-sign up ako dito sa simula at pagkatapos, tulad ng, marahil sa isang taon na lumipas, ito ay nawala dahil, muli, ikaw ay umaasa nang husto sa pagsunod sa ibang mga tao, at ito ay naging isang maliit na bagay na walang kapararakan.
– Kontribyutor ng Every Story Matters |
| “ | Naaalala ko na, parang, umalis ako para magtrabaho nang mag-isa dahil lahat ng iba sa aking koponan ay wala, at ito ay katawa-tawa. Parang, 'I'm turn off this, this is so stupid.' Tulad ng, hindi nila alam kung mayroon silang Covid o wala, ngunit hindi alintana na kailangan nilang manatili sa trabaho sa loob ng dalawang linggo. Nakakatawa lang.”
– Zero-hours contract worker |
| “ | Oo, may mga pagkakataon na sasabihin sa iyo ng iyong app na [para mag-self-isolate] sa iyo ngunit hindi ko ito pinansin, sa totoo lang, para sabihin sa iyo ang totoo dahil binibigyan ako nito ng lahat ng negatibo, walang anumang positibo kaya sinubukan ko na huwag pansinin ngunit hindi iyon gumana, alam mo ba kung ano ang ibig kong sabihin? Dapat sinabi sa kapatagan na nakipag-ugnayan ka sa isang tao o isang bagay na katulad niyan."
– Miyembro ng komunidad na sumuporta sa mga tao na ihiwalay ang sarili |
Narinig din namin na ang kawalan ng tiwala at pag-aalinlangan ng mga tao sa mga app sa pagsubaybay sa kontrata ay nangangahulugan na mas malamang na hindi sila sumunod sa patnubay sa self-isolation, lalo na kung gaano kahirap at potensyal na nakaka-stress ang pag-iisa sa sarili para sa ilan.
| “ | Noong na-dinged ako sa app, hindi ko na lang pinansin, dahil, muli, ang dami ng mga taong nagsabi, muli, 'yun ay hindi tumpak at hindi gumana,' at naninira nang hindi pa sila nakakapunta kahit saan, ito ay isang kaso ng, 'Ito ay isang load lamang ng [kabastusan], kaya, alam mo, itutuloy ko ang aking buhay,' dahil walang sinuman."
– Kontribyutor ng Every Story Matters |
Narinig namin mula sa ilang mga nag-aambag na nakarinig tungkol sa o na-target ang kanilang mga sarili sa pamamagitan ng mga mensahe ng scam na nagpapanggap bilang bahagi ng opisyal na sistema ng pagsubaybay sa contact. Binawasan nito ang kumpiyansa at tiwala sa system para sa mga kontribyutor na ito.
| “ | Napakaraming scam na nagte-text, at medyo mahirap gawin. Sa sandaling na-click mo ito, at pagkatapos ay nagsimula silang magtanong ng mga personal na katanungan, o mga detalye ng bangko, malalaman mo na ito ay isang scam.”
– Clinically vulnerable na tao |
| “ | Anumang ibang mga text na natanggap ko ay tiyak na mula sa mga scam account. At ang lahat ng iyon ay talagang mabilis na nangyari pagkatapos ng track at trace na bagay. At naisip ko, 'Oh mabilis lang iyon.' Ang mga scammer ay napunta sa ganyan, talagang mabilis.
– Taong nakakuha ng suporta sa kalusugan ng isip |
Sa pangkalahatan, ang ilang mga nag-aambag ay nagsalita tungkol sa isang malawak na kawalan ng tiwala sa pangkalahatang sistema at impormasyong ibinabahagi tungkol sa pagsubok at ang virus. Naranasan nila ito ng personal o pangalawang kamay.
| “ | Ang mga una ay talagang hindi kumportable […] ang mga pamunas ay napakahaba, kaya't napigilan ang mga tao, ngunit sa palagay ko ito ay higit na lubos na kawalan ng tiwala sa sistema [… at] sa pangkalahatan, ang elementong ito ng mga tao na nag-iisip lang, 'Hindi, hindi ako nagtitiwala dito. Hindi ako [magsusubok].' […] sarili kong kapareha […] Kinailangan kong ipaglaban siya para kumuha ng pagsusulit dahil […Ako ay] mataas ang panganib at kailangan kong sabihin sa kanya, 'Ayoko na nasa tabi mo ako maliban na lang kung mapatunayan mong wala kang Covid' [...] napakatagal bago siya makarating doon."
– Miyembro ng komunidad na sumuporta sa mga tao na ihiwalay ang sarili |
Ang mga balita tungkol sa mga pulitiko at opisyal ng gobyerno na hindi sumusunod sa mga alituntunin ay inilarawan bilang isang punto ng pagbabago ng maraming nag-aambag sa kanilang mga saloobin sa pagsunod sa mga patakaran. Madalas nitong binago kung paano nila inilapat ang mga alituntunin sa pag-iisa sa sarili sa kanilang sariling sitwasyon. Ibinahagi nila na hindi nila naiintindihan kung bakit dapat nilang ihiwalay ang sarili kung ang mga nasa posisyon sa pamumuno ay hindi sumusunod sa mga patakaran. Sinabi sa amin ng maraming kontribyutor na dahil sa mga kaganapang ito, nagpasya silang gamitin ang kanilang paghuhusga sa kung gaano sila kalapit na dapat sumunod sa mga panuntunan sa pag-iisa sa sarili, lalo na sa stress at pagkabalisa na tinutukoy ng marami kung sila ay nag-iisa.
| “ | Nang malaman ang impormasyon tungkol sa mga iskandalo sa gobyerno… at napapagod na ang mga tao sa mahigpit na mga patakaran sa paghihiwalay, sa tingin ko ay dumating sa yugto kung saan nagsimulang magrebelde ang mga tao, at nagsimulang magsabi ng hindi, sapat na. I think it got to a stage, I'll be totally honest with you, people were going, 'Alam mo ba, kung mamamatay ako, mamamatay ako kasama ang buong pamilya ko sa paligid ko.'”
– Clinically vulnerable na tao |
Sinabi rin sa amin ng mga nag-aambag kung paano binago ng mga pagkilos ng mga pulitiko at opisyal ng gobyerno kung paano nila tiningnan ang pagpapatupad ng gabay sa pag-iisa sa sarili. Sinabi sa amin ng mga taong ito kung paano nila hindi gaanong sineseryoso ang mga parusa bilang isang pagpigil sa paglabag sa mga patakaran bilang resulta.
| “ | Sa palagay ko ang mga parusa ay naging isang maliit na komedya sa huli dahil ito ay tulad ng, sa tuwing nakikita mo ang mga tao na lumalabag sa mga patakaran mula sa… pamahalaan, ito ay naging medyo nakakatawa.”
– Kontribyutor ng Every Story Matters |
Pagdama ng panganib
Ang mga personal na pagtatasa ng panganib ay ibinibigay sa lawak kung saan lumahok ang mga tao o hindi sa pagsubok, pagsubaybay sa pakikipag-ugnay at pag-iisa sa sarili.
Narinig namin mula sa mga taong nag-alinlangan sa pangangailangan para sa pagsusuri o pakikilahok sa pagsubaybay sa pakikipag-ugnay, lalo na kapag wala silang mga sintomas, o naramdaman nila na ang kanilang pamumuhay ay nangangahulugan na sila ay nasa mas mababang panganib na magkaroon ng Covid-19. Naniniwala ang ilan sa mga kontribyutor na ito na ang paraan ng kanilang paggugol ng kanilang oras, tulad ng pagiging nasa bahay na may kaunting mga contact, ay naglagay sa kanila sa kaunting panganib. Narinig namin ang mga kuwento ng mga taong gumagawa ng sarili nilang pag-iingat sa halip na sundin ang opisyal na patnubay.
| “ | Minsan maiisip mo, 'Wala talaga akong napuntahan kamakailan, kaya paano ko makukuha ito?' [...] kung literal na nasa bahay ako sa loob ng limang araw [...] at wala akong mga sintomas, bakit kailangan kong subukan ito? Walang punto. Kaya, sinubukan ko lang mag-apply ng kaunting common sense at logic dito."
– Nag-iisang magulang |
| “ | [nagpapaliwanag kung bakit hindi sila lumahok sa pagsubaybay sa pakikipag-ugnay] Karamihan sa mga oras, kami ay bumubula, kaya napakaliit ng mga tao na aming nakikita. We were not seeing friends, we were only seeing family and even then, we were very careful when we were seeing them, making sure that we were negative and everything else.”
– Clinically vulnerable na tao |
Ang antas kung saan ang mga sambahayan ay naghiwalay sa sarili nang hiwalay ay kadalasang nakadepende sa mga pananaw sa panganib mula sa Covid-19. Narinig namin mula sa ilang kontribyutor na nagsabi sa amin tungkol sa kung paano hindi sinunod ng kanilang mga sambahayan ang mahigpit na patnubay sa pag-iisa sa sarili (ibig sabihin, upang ikulong ang mga indibidwal sa isang silid) at sa halip ay malayang gumagalaw sa paligid ng bahay at nag-iisa bilang isang sambahayan. Nadama nila na ang paggamit ng buong bahay kumpara sa isang silid-tulugan upang gawin ito ay mas praktikal at komportable. Ang pagkakaroon ng puwang para makagalaw sa panahon ng self-isolation ay mahalaga din sa kanilang pananaw. Ang iba't ibang uri ng sambahayan ay nagpasya na gawin ito, kabilang ang mga may mga anak at ang mga may maraming kasambahay.
| “ | Sa buong katapatan, tulad ng kung ang isa sa amin ay may Covid sa bahay, hindi kami mag-iisa sa sarili sa isang silid-tulugan gaya ng sinabi sa amin na gawin. Iyon ay medyo katawa-tawa para sa amin, dahil lahat kami ay nasa isang bahay, nagbabahagi ng mga bagay, nagbabahagi ng kapaligiran. Ang pagbubukod sa sarili, para sa akin, ay tinitiyak na ako ay nasa aking tahanan, at hindi lumalabas sa mga pampublikong espasyo.”
– Kontribyutor ng Every Story Matters |
Ang ilang mga nag-aambag ay umiwas sa mga sentro ng pagsubok dahil sa mga potensyal na panganib ng alinman sa pagpasa o pagkontrata ng virus, kung saan malamang na makatagpo sila ng ibang tao, kabilang ang mga maaaring may Covid-19, na nagsisilbing hadlang sa pagsubok.
| “ | Sa totoo lang, masyado akong paranoid para pumunta sa isa sa mga test center dahil mas natatakot ako sa, 'Paano kung hindi ko pa talaga nakuha, at pagkatapos ay pumunta ako doon, at [… ibang tao] sila ay umuubo tulad ng mga pumapalakpak, at pagkatapos ay nakuha ko ito dahil nagpunta ako sa testing center?' Kaya iyon ay palaging isang pag-aalala.
– Kontribyutor ng Every Story Matters |
Mayroon ding mga nag-aambag na nagsabing nabawasan ang kanilang pakikipag-ugnayan sa pagsubok sa panahon ng pandemya, dahil itinuring nila na ang mga panganib na nauugnay sa pagkontrata ng virus ay bumaba sa paglipas ng panahon. Ang mga dahilan na tinalakay ng mga tao ay kasama ang pagkakaroon ng virus dati at samakatuwid ay iniisip na sila ay immune; saklaw ng media kabilang ang bumababang bilang ng mga namamatay; at pag-aalis ng mga paghihigpit.
| “ | Sa sandaling nakuha namin ang Covid, pagkatapos nito, sa mga bagay-bagay na umiikot at sa napakaraming media na ang iyong katawan ay nagiging immune dito, kaya nagsimula akong magbayad ng mas kaunting pansin sa pagpapasuri, hindi ito madalas."
– Zero-hours contract worker |
| “ | Habang tumatagal […] at […] Nakuha ko ito sa pangalawang pagkakataon […] Naisip ko, 'Naku, hindi naman talaga masama.' At sinasabi ng ibang tao, [...] 'Kailangan lang nating ipagpatuloy ito, hindi ba? […] wala kaming pakialam kung mayroon kang Covid o wala, wala itong pinagkaiba.' So, [naisip ko], 'Well, I won't bother to test then.'”
– Kontribyutor ng Every Story Matters |
Ang pagtanggap ng isa o higit pang mga dosis ng bakuna sa Covid-19 ay nagparamdam sa ilan na narinig namin na hindi gaanong kailangan na subukan para sa Covid-19. Sinabi nila na ito ay dahil ang bakuna ay nag-aalok ng proteksyon na nagpababa sa kanilang posibilidad na mahawaan ang virus.
| “ | Pagkatapos din ng bakuna, parang hindi ako gaanong nasubok dahil mas kaya kong labanan ito, kaya mas maliit ang pagkakataon kong makuha ito.”
– Zero-hours contract worker |
Bukod pa rito, ang pagtatapos ng malawakang libreng pagsubok mula Abril 2022 ay, para sa ilang nag-aambag, isang senyales na ang pandemya ay hindi na kasing seryoso ng dati at ang panganib ng pagkontrata ng Covid-19 ay nabawasan. Ang pagsubok ay itinuturing na hindi gaanong kinakailangan, na ang responsibilidad ay higit sa mga indibidwal na kagustuhan tungkol sa kung susuriin o hindi.
| “ | Nang huminto sila sa paggawa ng libreng pagsubok ay nagsimula akong mag-isip, 'Tama, hindi na ito seryoso. Kung hindi nila ibinibigay ang […] serbisyong ito para sa mga tao', halos sabihin na […], 'Bahala ka […] ngayon isa na lang itong tawag sa paghatol. Kailangan mo lang […] magpasya sa iyong sariling isip kung sa tingin mo ay mahina ka o hindi'.”
– Manggagawa sa paggawa |
Access
Mga pagsusuri sa PCR
Narinig namin mula sa mga kontribyutor na nagsabi sa amin na nakita nilang mahirap ang proseso ng pag-book ng PCR, lumilikha ng mga hadlang sa pagsubok para sa kanilang sarili o sa iba. Ang pag-navigate sa sistema ng booking, kasama ang mga opsyon na ipinakita nito, ay maaaring nakakalito at nakaka-stress; Ang pag-access sa suporta at patnubay ay napapanahon din. Ang ilang mga kontribyutor ay nakaranas ng mga error sa pag-book kung saan ang mga appointment ay hindi naitala sa system, na maaaring magresulta sa pagtalikod sa kanila.
| “ | Nagkaroon ako ng mga problema sa booking [...] akala mo na-book mo na ang slot [...] at pagdating mo doon, sinabi nila, 'Well, wala ang pangalan mo sa [aming listahan]'. […] Naghintay ako sa mahabang pila at ngayon ay pinaalis mo na ako.”
– Miyembro ng pamilya o tagasuporta ng isang tao na kinakailangang ihiwalay ang sarili |
| “ | Nagkamali akong na-book ang drive-through sa halip na ang [walk-]in center. […] Nang dumating ang address, isa itong drive-through. Hindi ito ang inaasahan ko.”
– Tagapag-alaga |
Sinabi ng ilang nag-ambag na ang pag-access sa mga appointment sa PCR ay mas mahirap sa simula ng pandemya at kapag pinahintulutan ang paglalakbay sa ibang bansa na may negatibong pagsusuri sa PCR.
| “ | Sa una medyo mahirap makakuha ng slot; kailangan mong patuloy na suriin dahil ito ay abala […] lahat ay ginagawa ang lahat ng ito sa parehong oras. […] walang gaanong set up at […] mas maraming tao [naghahanap ng mga pagsusulit] kaysa sa mga boluntaryo.”
– Taong naninirahan sa isang multi-generational na sambahayan |
Ang isa pang hadlang para sa ilan ay ang pag-access sa mga test center na malapit sa kanilang tinitirhan, alinman dahil hindi ito ibinigay sa lokal, o dahil hindi available ang mga appointment sa mga sentrong malapit. Ang pagbibiyahe ng mas malalayong distansya ay nagpapataas ng gastos at nag-aalala tungkol sa pagkuha sa mga appointment sa pagsubok.
| “ | Palagi kang kailangang maglakbay. […] Kami ay medyo semi-rural at walang mga pasilidad para sa sinuman […] kahit saan malapit. Mayroon kaming maliit na ospital sa aming bayan ngunit, sa puntong iyon […] walang ginawang pagsusuri doon […] ginawa lang sa malalaking sentro […] ang mensahe ay, 'Pumunta ka at magpasuri. Madali lang, diretso, 'pero hindi."
– Taong nabubuhay na may Long Covid |
Ito ang nangyari sa ilang taong naninirahan sa mga urban na lugar, gayundin sa mga nasa mas malayong lugar/rural na lokasyon.
| “ | Nakatira kami sa isang sentro ng lungsod, na talagang nagpahirap sa pag-access sa mga sentro ng pagsubok dahil madalas silang nasa labas ng lungsod. [Ang] pinansiyal na pasanin ng pagkakaroon ng pribadong transportasyon sa mga test center na iyon […] nagdagdag ito ng stress, idinagdag ang pagpaplano at logistik.
– Miyembro ng pamilya o tagasuporta ng isang tao na kinakailangang ihiwalay ang sarili |
Ang mga taong hindi nakakuha ng pribadong transportasyon ay hindi palaging nakaka-access sa mga appointment sa pagsubok. Ang ilang mga test center ay drive-through lamang, habang ang iba ay malayo sa mga ruta ng pampublikong sasakyan. Minsan din pinaghihigpitan ang pampublikong sasakyan.
| “ | Kailangan kong maglakad nang matagal dahil […] Alam ko lang na mayroon akong [Covid], kaya ayokong may sumama sa akin at hindi ako marunong magmaneho, kaya literal na kailangan kong maglakad, parang, 50 minuto papunta sa testing center na ito […] sa gilid ng motorway […] dahil wala nang mas malapit sa akin.”
– Kontribyutor ng Every Story Matters |
Ang paglalakbay sa mga test center ay mas mahirap din para sa mga may sakit na sintomas ng Covid-19.
| “ | Nagkaroon kami ng aking partner ng Covid sa mga unang buwan ng pandemya. Napakasakit ng aking kapareha at malapit nang ma-ospital, na lubhang nakakatakot […] kapag mahirap humingi ng tulong. Ang aming pinakamalapit na testing center ay 40 milya ang layo."
– Kontribyutor ng Every Story Matters |
| “ | Nahirapan akong makarating sa testing center dahil masama ang pakiramdam ko - [ako ay] nanghihina, [na may] matinding ubo, mataas na temperatura at sakit ng ulo."
– Kontribyutor ng Every Story Matters |
Mga LFT
Narinig namin mula sa mga nag-aambag na naapektuhan ng hindi madaling pag-access sa mga LFT, lalo na sa simula ng pandemya, kapag muling binuksan ang mga paaralan at kapag pinahintulutan ang paglalakbay sa ibang bansa. Ang mga kakulangan o pagrarasyon ng mga LFT ay nagdulot sa kanila ng pag-aalala, takot at ilang panic.
| “ | Sa simula pa lang, napakataas ng pangangailangan para sa pagsusuri, ang ilan sa mga pharmacist […] ay hindi makakuha ng mga test kit.”
– Taong mula sa pinagmulang etniko ng Roma |
| “ | Nang magbukas muli ang mga paaralan, nagpatuloy ako sa pagtatrabaho bilang [isang] supply at ito ay nakakatakot. Halos araw-araw akong nakakakuha ng mga alerto sa Covid sa aking telepono para makipag-ugnayan, ngunit dahil sa kakulangan ng pagpaplano ay wala lang available na mga pagsubok, ibig sabihin, kailangan kong pumili sa pagitan ng kumita ng pera na lubhang kailangan ko, o potensyal na pagkalat ng nakamamatay na sakit na ito. Hindi iyon isang bagay na dapat nasa balikat ng isang taong kumikita ng kaunti kaysa sa minimum na sahod.”
– Tagapag-alaga |
Sa bandang huli ng pandemya, ang bilang ng mga libreng pagsusuri sa bawat tao ay limitado minsan. Naapektuhan nito ang mga may malalaking sambahayan, na mas mabilis na nakalusot sa mga pagsubok. Naapektuhan din nito ang mga taong naghahangad na mag-order ng mga pagsusuri sa ngalan ng iba - para sa mga miyembro ng pamilya na nahirapan sa proseso ng pag-order mismo, o para sa mga propesyonal na bumibisita sa kanilang tahanan upang magbigay ng mga serbisyo tulad ng pangangalaga sa tahanan.
| “ | Kung ang [mga tagapag-alaga] ay hindi nakakuha ng mga pagsusuri sa Covid [at ang aming mga libre ay naubos…] Kailangan kong lumabas at bumili ng marami sa kanila. Naramdaman ko na pinaparusahan ako...ang ibang tao ay walang ganoong dagdag na gastos.”
– Kontribyutor ng Every Story Matters |
Accessibility at pagsasama
Mga pagsusuri sa PCR
Nadama ng ilang nag-aambag na ang mga pangangailangan ng mga taong hindi kasama sa digital, o may mas mababang antas ng literacy o Ingles, ay hindi sapat na suportado ng mga PCR booking system. Nagresulta ito sa mataas na antas ng pag-asa sa impormal na suporta mula sa pamilya o mga kaibigan.
| “ | Ang mga matatandang tao […] ay talagang nahirapan sa teknikal na bahagi ng […] nagbu-book ng kanilang PCR test [...] madalas kaming may mga matatandang pasyente na tumatawag sa amin upang magtanong sa amin tungkol sa pag-book [...] walang sinuman ang nag-isip na maraming matatandang tao, wala silang mga mobile phone."
– Kontribyutor ng Every Story Matters |
Inilarawan ng ilan na nagbahagi ng kanilang mga kuwento kung paano nila nadama na ang mga test center ay naa-access para sa mga taong may mga kapansanan, alinman sa mga tuntunin ng pisikal na layout o ang mga protocol sa lugar. Halimbawa, mahirap ang mahabang pila at social distancing para sa mga taong may ilang kundisyon at ang ilang test center ay hindi naa-access sa wheelchair.
| “ | Mahirap para sa [aking kapatid na may kapansanan sa pag-aaral] na pumila at sumunod sa [gabay sa pagdistansya sa lipunan…] walang sitwasyon kung saan [kung] mahina ka o mayroon kang kapansanan sa pag-aaral o autism, [magagawa ang mga akomodasyon, na kinikilala,] 'Mahirap ito, malalampasan ka namin mula sa mahabang pila na ito at maaari kang pumasok' [diretso]."
– Miyembro ng pamilya o tagasuporta ng isang tao na kinakailangang ihiwalay ang sarili |
| “ | [Ang test center] ay maraming hagdan at talagang makitid na cubicle. [Ang isang gumagamit ng wheelchair] ay hindi rin makakaupo doon. At pagkatapos ay ang susunod na magagamit ko ay malapit sa paliparan, at iyon ay isang drive-through, ngunit iyon ay isang oras-at-kalahating paglalakbay [ang layo].”
– Kontribyutor ng Every Story Matters |
| “ | Ang mga pagsusuri sa PCR ay lubos na kasangkot at para sa ilang mga tao, medyo mahirap makuha, o nakakapukaw ng pagkabalisa."
– Kontribyutor ng Every Story Matters |
Narinig namin mula sa mga taong may pagkawala ng paningin na hindi nakasama sa kanila sa isang PCR testing center, at sinabi nitong naging mahirap ang proseso.
| “ | Nawala ang aking paningin sa panahon ng Covid, kailangan kong gawin ito nang mag-isa dahil walang pinayagang sumama sa akin.
– Taong may pagkawala ng paningin |
Narinig din namin ang mga taong nagkaroon ng negatibong pakikipag-ugnayan at karanasan sa mga kawani sa mga PCR test center, halimbawa ang mga kawani na nagpaparamdam sa mga tao na nasa ilalim ng presyon sa panahon ng mga pagsubok at kakulangan sa ginhawa sa paligid ng pisikal na kalapitan ng mga kawani kapag nagbibigay ng mga pagsusulit.
| “ | Kinailangan talaga nilang gawin ito para sa iyo, at nalaman kong talagang mahirap iyon, talagang nakaka-trigger, talagang hindi komportable at hindi kailangan. Pakiramdam ko, bakit hindi ko magawa ang sarili ko? Napaka-invasive, lalo na sa isang taong nakaranas ng trauma. Parang isang paglabag sa aking personal na espasyo."
– Taong may pangmatagalang pisikal na kondisyon sa kalusugan |
| “ | Sa pangalawang pagkakataon na pumunta kami sa isang test center, sinubukan ng staff na gawin akong, isang buntis na babae, na umakyat sa likod upang subukan ang aking anak na babae. Hindi ko ito pisikal na magagawa sa pitong buwang buntis. Mayroong isang malaking walang laman na paradahan ng kotse; walang nanganganib na maipasa ko ang [Covid] sa kanila dahil walang tao doon. Umalis kami nang hindi siya sinusubok."
– Kontribyutor ng Every Story Matters |
Ang mga nag-aambag mula sa mga komunidad ng Gypsy, Roma at Traveler ay partikular na nag-ulat ng mga negatibong karanasan sa propesyonalismo ng mga kawani ng test center.
| “ | Ganap na hindi propesyonal […] Sumulat kami at nagreklamo, [kabilang ang…] isang paliwanag kung ano ang nangyari [… at na] hindi nila nasagot nang maayos ang [aming mga tanong] […] nang tanungin namin sila, 'Sigurado ka bang gumagana ito?' minsan tumatawa pa sila, [na nagsasabing] 'Wag kang mag-alala, alam namin ang ginagawa namin.' [… Ang impormasyon na gusto namin] ay mahirap makuha. Nagpasya kaming hindi na kami pupunta doon."
– Tao mula sa komunidad ng Manlalakbay |
Nahirapan din ang ilang kontribyutor na nagsasalita ng Ingles bilang pangalawang wika na maunawaan ang mga pandiwang tagubilin na ibinigay ng mga kawani ng test center nagpapahirap sa pag-access ng mga tagubilin at impormasyon. Dahil dito, naging partikular na nakaka-stress ang kanilang karanasan sa mga pagsusuri sa PCR. Ang ilang nag-aambag na Bingi ay nagsalita tungkol sa kung paano sila nakaranas ng mga hadlang sa komunikasyon sa mga test center, at sinabing ang mga kawani na nagtatrabaho doon ay mukhang hindi nasangkapan upang suportahan ang mga taong may iba't ibang pangangailangan.
| “ | Wala talaga akong sapat na English para makipag-usap sa […] may sasabihin ang taong sumusubok sa akin, at hindi ko maintindihan ang sinabi nila, na mas nakaka-stress para sa akin […] nagdudulot lang ito sa akin ng pagkabalisa dahil hindi ko lang maintindihan kung ano ang nangyayari sa paligid ko.”
– Taong nakatira sa masikip o masikip na tirahan |
| “ | Walang impormasyon sa Bingi o kapansanan na ibinigay sa sinumang kawani maliban sa isa, sa aking lokal na lugar. Maraming mga Bingi ang naninirahan dito. Ngunit hindi iyon direktiba ng gobyerno.”
– Bingi |
Mga LFT
Ang mga taong may pisikal na kapansanan ay nag-ulat ng higit na kahirapan sa paggamit ng mga LFT. Halimbawa, ang pagbubukas ng packaging ay mahirap para sa mga taong may kapansanan na nakaapekto sa kanilang kahusayan, at ang maliit na teksto ay mahirap para sa mga may kapansanan sa paningin na basahin.
| “ | Natagpuan ko silang pisikal na mahirap buksan minsan. Mayroon akong kaunting panginginig, kaya ang pag-tipping ng maliliit na piraso ng likido [ay mahirap], at ito ay isang napakasalimuot na proseso na medyo mahirap sa pisikal."
– Kontribyutor ng Every Story Matters |
| “ | Ang impormasyon [mga leaflet] sa isang […] maliit na pag-print, [nangangahulugan] na ang mga pagsusuri sa Covid ay hindi naa-access ng mga bahagyang bulag na tao."
– Taong may pagkawala ng paningin |
Ang mga matatandang tao, mga Bingi, ang mga may Ingles bilang pangalawang wika, ang mga mula sa mga komunidad ng Gypsy, Roma at Traveller at mga taong mula sa mga komunidad na naapektuhan ng mga hadlang sa pagbasa at pagsulat ay minsan ay nahihirapang unawain ang mga nakasulat na tagubilin sa LFT (at PCR) na mga test kit. Ang ilang mga tao ay nangangailangan ng suporta mula sa mga kaibigan o pamilya upang gumamit ng mga pagsubok. Para sa iba, ang mga hamong ito ay nangangahulugang hindi sila gumamit ng mga pagsubok.
| “ | Naaalala kong pinag-usapan sila [ng mga magulang ko] habang nasa labas ako at nasa kusina nila […] na nakabukas ang bintana [… ginagabayan] sila [habang ginagamit nila ang pamunas], 'Oo, gawin mo ito at ilagay mo sa likod'. […] Hindi nila ito magagawa kung hindi nila ako kakausapin tungkol dito.”
– Miyembro ng pamilya o tagasuporta ng isang tao na kinakailangang ihiwalay ang sarili |
| “ | Sa kulturang naglalakbay […] marami sa mga miyembro ng aking pamilya ang hindi marunong magbasa [dahil maaga silang umalis ng paaralan], kaya maliban na lang kung may magpapakita sa kanila o tumulong sa kanila, […] hindi nila masusunod ang [mga nakasulat na tagubilin…]. Kailangan nila ng isang bagay na nakikita nila, o isang audio [recording] na maaaring ipaliwanag sa kanila kung ano ang gagawin.”
– Tao mula sa isang nomadic na komunidad |
Ang ilang mga nag-aambag, lalo na ang mga taong ang unang wika ay hindi Ingles (kabilang ang mga Bingi), ay nagsabi na ang mga tagubilin sa LFT sa ibang mga format ay nakakatulong sana para sa kanila. Kasama sa mga mungkahi ang pagdaragdag ng higit pang mga diagram sa mga leaflet ng test pack, at mga link sa mga online na video na nagpapakita ng mga hakbang na kasangkot, gamit ang British Sign Language (BSL). Ang ilang mga nag-ambag ay tila walang kamalayan sa mga online na video na magagamit sa panahon ng pandemya, na nagmumungkahi na ang mga ito ay maaaring mas malawak na naipahayag. Ang isa pang mungkahi ay para sa mga boluntaryo sa mga organisasyon o komunidad na magbigay ng mga demonstrasyon.
| “ | Ang mga bingi ay tumatanggap ng mga test kit, at […] hindi sigurado kung paano gamitin ang mga ito. Patuloy lang silang nakikipag-ugnayan sa akin habang nagtatrabaho ako para sa pangangalagang panlipunan: 'Pakiusap, maaari mo bang ipaliwanag kung paano gamitin ang mga kit na ito?' Walang […] sa sign language na maipapakita sa mga tao kung paano gamitin ang mga ito […] Kinailangan kong gumawa ng uri ng facetime […] mga tutorial [upang matulungan silang maunawaan…] talaga. At sa tingin ko ang NHS ay dapat gumawa ng mga video sa sign language upang ipakita kung paano gamitin ang test kit."
– Bingi |
Pagsubaybay sa contact
Napansin din ng ilang kontribyutor na ang mga hadlang sa paggamit ng digital na teknolohiya ay isang dahilan para hindi makilahok sa mga app at online na paraan ng pagsubaybay sa contact. Ito ay dahil sa kakulangan ng kaalaman tungkol sa kung paano i-download ang app o i-access ang web page o walang mobile phone na susuporta sa app. Napakakaunting mga matatandang nag-aambag na may edad na 75+ ang gumamit ng contact tracing app o online na paraan ng pagsubaybay sa contact. Sinabi rin ng ilang nakababatang contributor na hindi nagamit ng kanilang mga magulang ang app o mga online na bersyon ng contact tracing.
| “ | [Ang] test and trace system ay hindi naaangkop sa akin dahil hindi ako gumagamit ng mobile phone."
– Kontribyutor ng Every Story Matters |
| “ | Hindi ako kailanman na-ping dahil wala akong app at ang pangunahing dahilan kung bakit wala ako ng app ay dahil mayroon akong napakalumang telepono na hindi sana susuportahan doon, at hindi ako bibili ng bagong telepono para lang makuha ang app.”
– Kontribyutor ng Every Story Matters |
Ang ilang mga nag-aambag mula sa mga komunidad na ang unang wika ay hindi Ingles ay inilarawan din ang paglikha ng kanilang sariling mga diskarte sa pagsubaybay sa pakikipag-ugnay, sa halip na lumahok sa opisyal na sistema. Halimbawa, inilarawan ng isang kontribyutor mula sa komunidad ng Bangladeshi ang pagsubaybay sa pakikipag-ugnayan na hindi gaanong naaabot sa kanilang komunidad dahil sa mababang antas ng digital literacy at English. Sa halip, ang komunidad ay may mahalagang papel sa pagsubaybay sa mga impeksyon ng Covid-19 sa kanilang mga sarili, halimbawa ng pag-alerto sa mga tao sa mga impeksyon sa kanilang kapitbahayan, at pagtiyak na ang mga apektadong tao ay nasuri at nabawasan ang kanilang pakikipag-ugnayan sa iba.
| “ | Dahil…ang ilang mga tao ay hindi pa rin magagamit ang mga app, at ito ay medyo nakakakuha ng impormasyon [at] pagkatapos ay binasa ito ng mga tao at natunaw nila ang impormasyon, at sinubukan nila ang kanilang makakaya. Pero maliban sa mga app, parang one-to-one na impormasyon...sabihin kung alam ko, kaya ipasa ito [sa] ibang tao, katulad niyan maliban sa paggamit ng mga app na iyon...salita ng bibig."
– Taong ang unang wika ay hindi Ingles |
Kahirapan sa paggamit
Sinabi sa amin ng mga kontribyutor na hindi palaging diretso ang pag-aaral kung paano gumamit ng test kit.
Maaaring mahirap bigyang-kahulugan kung paano gamitin nang tama ang mga LFT, at ilang kontribyutor na narinig namin mula sa inilarawan na nakakaramdam na hindi sigurado na nakagawa sila ng mga pagsubok nang tumpak, na kadalasang humahantong sa pag-uulit nila sa proseso. Kasama sa mga dahilan ang kawalan ng katiyakan tungkol sa mga tamang proseso ng pagsubok tulad ng kung gaano kalayo ang dapat ipasok ng mga pamunas o ang haba ng oras na dapat nilang punasan ang kanilang ilong o lalamunan; pagkakaiba-iba sa katumpakan sa pagitan ng mga pamunas ng ilong at lalamunan; at mga maling pagsusuri, halimbawa, kung saan walang laman ang extraction tube o naglalaman ng kaunting likido.
| “ | Palagi kong iniisip, 'Nakarating ba ako sa aking ilong? [...] Ginawa ko ba ito ng maayos?' Moreso kung masama ang pakiramdam ko at ito ay negatibo, iisipin ko, 'Oh, nagawa ko ba ito ng maayos?' at pagkatapos ay […] gawin mo ito nang paulit-ulit [dahil] sinasabi ng iyong isip na baka mayroon ka nito.”
– Taong may kahirapan sa pagbasa |
Ang ilang mga tao ay napagtanto sa ibang pagkakataon na sila ay mali sa pagbasa ng mga resulta sa loob ng mahabang panahon, na maaaring magkaroon ng pangmatagalang epekto, halimbawa, sa pamamagitan ng pag-akay sa mga pamilya na ihiwalay ang sarili nang hindi kinakailangan.
| “ | Nagkulong kami sa bahay nang halos apat na linggo sa Pasko dahil mali ang pagbabasa namin ng mga pagsusulit! [...] sarili naming kasalanan iyon."
– Tagapag-alaga |
Narinig din namin mula sa mga taong natagpuan ang mga pagkakaiba-iba sa pagitan ng mga test kit na naging mas mahirap para sa ilan na gamitin. Ang mga kit mula sa iba't ibang brand ay may iba't ibang bahagi at tagubilin, at naalala ng mga kontribyutor na kailangang suriin ang mga tagubilin sa tuwing gumamit sila ng bagong uri ng pagsubok. Ang ilang mga nag-ambag ay nagsabi na ang mga pagsubok ay naging mas madaling gamitin sa paglipas ng panahon gayunpaman, dahil ang kanilang pagiging pamilyar ay tumaas at dahil ang mga test kit ay bumuti. Ang isang halimbawa ay ang pagsasama sa ilang mga test kit ng isang cardboard stand upang hawakan ang extraction tube, na inilarawan ng ilang tao bilang nakakatulong.
| “ | Nasanay na kaming gawin ito sa isang paraan at pagkatapos ay dumating ang isa pa [iba] [...] ikaw ay parang, 'Oh Diyos, kailangan kong ibigay ito dito at hindi [...] doon [ngayon]' [...] kailangan lang ng kaunting pagsisikap na basahin ang ilang [higit pang] mga tagubilin, ngunit hindi iyon ang katapusan ng mundo, talaga, hindi ba? Parang five minutes out of your day.”
– Tagapag-alaga |
Mga negatibong epekto
Narinig namin ang tungkol sa isang hanay ng mga hadlang sa pagsubok, pagsubaybay sa pakikipag-ugnayan at pag-iisa sa sarili na nauugnay sa negatibo, o potensyal na negatibo, na mga epekto sa mga tao sa iba't ibang kalagayan. Kabilang dito ang pagkawala ng mga kalayaan, mga implikasyon sa pananalapi, mga epekto sa kapakanan ng mga tao tulad ng kakulangan sa ginhawa at pagkabalisa mula sa pagsubok, at mga implikasyon sa kalusugan ng isip ng pag-iisa sa sarili.
Pagkawala ng mga kalayaan
Narinig namin mula sa mga nag-aambag na maaaring umiwas o naantala ang pagsusuri, at/o umiwas sa pag-iisa sa sarili kapag nagkaroon sila ng mga sintomas, nang sa gayon ay hindi sila pinaghihigpitan sa mga tuntunin ng paghahalo at pakikisalamuha sa iba.
| “ | Sinubukan ko lang talaga kung may nagsabi, 'Kailangan mong mag-test.' [...] kung ako ay may runny nose o kung ano man at ang isang tao ay tulad ng, 'Sa tingin mo ba ay mayroon kang Covid?' Hindi ko na talaga iisipin […] Gusto ko, 'Marahil ay nilalamig lang' [...] Kailangan talaga nilang itulak ako [...] Ang bahagi ko ay, tulad ng, 'Kung bumalik itong positibo, hindi ako makakalabas sa Sabado, kaya magpipigil ako. Sa palagay ko wala ako nito, titingnan ko kung bumuti ang pakiramdam ko' […] kung talagang itinulak ako ng mga tao ay kukuha ako ng pagsusulit.”
– Kontribyutor ng Every Story Matters |
| “ | Minsan parang, kailangan mo na ngayong [self-] ihiwalay sa loob ng sampung araw, limang araw, o maaari mong hulaan na magsinungaling at maging tulad ng, kung anong araw mo nakita ang tao at inilagay ito nang mas maaga kaysa sa aktwal na para mas maaga kang makaalis sa pagkakahiwalay. Pakiramdam ko ay medyo sobra-sobra ang haba ng paghihiwalay, at muli ay nagkaroon ng ripple effect…. Nagkaroon kami ng Christmas thing sa bahay ng kaibigan ko at noong nakaraang araw ay medyo mabigat ang pakiramdam ko, pero nagpa-test ako sa umaga, ayos lang ako. Nagpunta ako doon, kaya nandoon ako buong gabi, lahat ng mga bintana, ilang mga bintana ay nakabukas... [Tapos] Naaalala ko noong panahong iyon, parang hindi maganda ang pakiramdam ko, ngunit hindi ito tipikal na Covid, masakit lang ang balikat ko at medyo nilalamig... Kinaumagahan, nagising ako, talagang walang panlasa o amoy, sobrang sakit. Ako kaagad, kailangan kong kumuha ng pagsusulit, at pagkatapos ay tulad ko sa lahat, 'I'm really sorry, nakuha ko na."
– Taong may pangmatagalang pisikal na kondisyon sa kalusugan |
Inilarawan din ng mga kabataan at magulang na nahihirapang sumunod sa mga alituntunin sa pag-iisa sa sarili, lalo na sa pandemya. Nakarinig kami ng mga halimbawa ng mga kinakailangan sa self-isolation na pakiramdam na malayo sa kanilang karaniwang gawain at ang pagbawas sa pisikal na kalayaan na mahirap pangasiwaan.
| “ | Ang dalawang linggong iyon, akala ko ay kakila-kilabot. Noong una ay masaya, ngunit nakakulong ako sa isang silid. Hindi ako nakakulong sa isang bahay, tulad ko ngayon, kung ako ay [mag-iisa] sa sarili. Mayroon akong isang double bed at mayroon akong isang tuta na nagngingipin, at ito ay nakaka-stress, lalo na kapag sinabi sa akin na hindi ako maaaring lumabas. That's what made me want to defy it, actually, was when I've got someone telling me I can't leave my room, I can't walk the dog. Iyon ang nagpaisip sa akin, 'Hindi, hindi ko ginagawa iyon.'”
– Kontribyutor ng Every Story Matters |
| “ | In terms of everything else, well, we don't tend to go out a lot anyway talaga, it didn't affect us [parents] greatly. Sa tingin ko, mas naapektuhan nito ang aking anak dahil hindi niya nakita ang kanyang kasintahan at, alam mo, sila ay lubos na nagmamahalan at nahirapan sila sa pag-iisip.”
– Taong naninirahan sa isang multi-generational na sambahayan |
Mga implikasyon sa pananalapi
Para sa iba na narinig namin, ang kawalan ng kakayahang magtrabaho at potensyal na pagkawala ng kita ay isang hadlang sa pagsubok. Ito ay dahil hindi sila makakapagtrabaho kung sila ay nagpositibo. Naalala ng mga kontribyutor ang pagdinig mula sa iba na hindi sumunod sa patnubay para sa pagsubok dahil hindi nila kayang lumiban sa trabaho kung sila ay positibo.
| “ | Naaalala ko ang mga taong nagsasabi, 'Hindi ako makakapag-test dahil, kung mag-test ako at positibo ako, hindi ako makakapagtrabaho at, kung hindi ako makapagtrabaho, hindi ko masusuportahan ang aking pamilya.' Maiintindihan mo sila sa paggawa ng mga pagpipiliang iyon, tama man o mali, mauunawaan mo na kailangan nilang tustusan ang kanilang pamilya.”
– Kontribyutor ng Every Story Matters |
| “ | I actually never take any test at all whatsoever […], puro lang dahil ayokong paghigpitan ako o diktahan ako kung paano-, alam mo, ang mga galaw ko dahil medyo abala ako.[…] dahil maraming kontradiksyon, alam mo, kapag nasubok ka, ilang araw ka makakaalis, kung saan ka pupunta […] Pinili ko na lang na huwag gumamit ng test' […] at hindi ako nakagamit ng kahit ano […]
– Taong nagtatrabaho sa pangangalagang pangkalusugan at panlipunan |
Ito ay partikular na nangyari para sa mga kawani ng ahensya o sa mga nagtatrabaho sa mga zero-hour na kontrata na nagbahagi sa amin ng stress at mga panggigipit sa pananalapi na kanilang kinaharap sa trabaho at pag-iisa sa sarili. Ang mga panggigipit na ito ay madalas na humantong sa pag-iwas ng mga tao sa paggamit ng contact tracing app, hindi pagsubok bago magtrabaho at pag-iwas, o paikliin, pag-iisa sa sarili upang hindi maapektuhan ang kanilang kita.
| “ | Ang dahilan kung bakit hindi ako sumali sa app ay dahil bumalik ako sa trabaho noong Hulyo 2020, at pagkatapos ay sinabi ng aking manager kung na-ping kami kailangan naming umalis sa trabaho, at sa aking trabaho, hindi ako binabayaran kung hindi ako magtatrabaho. Iniisip ko, 'Hindi lang ako sasali dito dahil halatang kailangan natin ng pera kaya dapat ako ay nagtatrabaho. At saka, positive ako na hindi ko makukuha ang Covid.'”
– Taong nagtatrabaho sa pangangalagang pangkalusugan at panlipunan |
| “ | Obviously na [paid sick leave by employers when took ill with Covid-19], was happening at the start but towards the end, like, work are saying, 'No, we're not paying, we're not doing this, we're not doing that.' Sa puntong iyon ang lahat ay nagsasabi lang, 'Well, hindi ako kumukuha ng 10 araw na walang bayad na bakasyon, kaya papasok ako. Wala akong ginagawa.'”
– Zero-hours contract worker |
May mga halimbawa rin, ng mga employer na nagpapayo o nagtuturo sa kanilang mga empleyado na ihinto ang paggamit ng contact tracing app at/o pagsasabi sa mga tao na huwag mag-self-isolate, o paikliin ang inirerekomendang panahon ng self-isolation, para makapagpatuloy sila sa trabaho. Inilarawan ng ilan sa mga kontribyutor na ito ang galit at pagkadismaya sa pagtrato ng mga employer. Sinabi nila sa amin kung paano nila sinubukang sundin ang mga alituntunin sa pag-iisa sa sarili ngunit nakaramdam sila ng pressure na huwag gawin iyon.
| “ | Ang payo/instruksyon mula sa gobyerno noong panahong iyon ay ang sinumang may temperatura at/o bagong ubo ay dapat mag-self-isolate, kaya kapag nagkaroon siya ng ubo, tumawag siya sa trabaho at sinabi sa kanila na mayroon siyang bagong ubo at kakailanganing huminto sa trabaho at ihiwalay ang sarili alinsunod sa mga alituntunin ng gobyerno. Gayunpaman, sinabi sa kanya ng kanyang manager sa [supermarket kung saan siya nagtatrabaho] na nagpahinga na siya noong nakaraang linggo at maraming dahilan kung bakit siya maaaring magkaroon ng bagong ubo at kung hindi siya papasok sa trabaho, gagawa ng aksyong pandisiplina. Kailangan niya ang kanyang trabaho at kita, kaya pumasok siya sa trabaho, ngunit siya at ako ay nananatiling takot at galit tungkol sa tugon ng [kanyang amo] sa sitwasyong ito. Ang pagsusuri sa Covid ay hindi malawakang magagamit noong panahong iyon at hindi namin malalaman kung ang aking anak na babae ay may Covid-19 o iba pang hindi gaanong nakakapinsalang virus, ngunit sa palagay ko ay hindi dapat igiit ng [pinag-empleyo ng anak na babae] na balewalain niya ang payo ng gobyerno sa panahong iyon at pumasok sa trabaho habang siya ay may mga sintomas na maaaring Covid-19.
– Kontribyutor ng Every Story Matters |
| “ | Nang magkaroon ako ng Covid noong unang bahagi ng 2021, dalawang linggo akong nakaratay sa kama. Ang aking amo ay hinarass ako sa buong oras, na nagpapasuri sa akin araw-araw at tumatawag sa akin ng 9am araw-araw upang malaman ang mga resulta. Nais nilang bumalik ako sa trabaho sa sandaling makakuha ako ng negatibong pagsusuri, kung bumuti na ba ang pakiramdam ko o hindi.
– Kontribyutor ng Every Story Matters |
Halaga ng mga pagsubok
Ang kailangang magbayad para sa mga pagsubok ay naging hadlang para sa ilan na nagbahagi ng kanilang mga kuwento sa amin. Nangangahulugan ito na ang ilan na sumubok kapag kailangan nilang (gamit ang isang LFT) ay hindi na nahanap na madaling gawin ito. Ito ay itinuturing na hindi patas para sa mga taong itinuturing na mahina, dahil sa kanilang pag-asa sa mga pagsubok upang manatiling ligtas.
| “ | Kung kailangan kong magbayad para sa kanila, hindi ko na sinubukan ang labis. Nagbayad nga kami para sa isang batch ng mga pagsubok [kapag] nagkaroon ng isa pang strain at […] Sa palagay ko ay wala kaming […] mga pagsubok [natitira] sa puntong iyon o sila ay luma na […] Medyo hindi ako handang magbayad para sa kanila kaysa sa paghawak ko sa kanila nang libre. Sa tingin ko ito ay £8 para sa apat o isang katulad nito, kaya hindi ito partikular na mura.
– Taong may pangmatagalang pisikal na kondisyon sa kalusugan |
Kwento ni PatriciaSi Patricia ay isang ina at isa sa kanyang mga anak ay nauri bilang clinically vulnerable sa panahon ng pandemya. Natagpuan niya ang pandemya na napakalaki at nakababahalang sa lahat ng aspeto ng kanyang buhay. Nakatira siya sa isang rural na lugar, kung saan ang pinakamalapit na testing center ay 30 minutong biyahe ang layo mula sa kanyang tahanan. Si Patricia ay madalas na nagpasuri sa buong pandemya dahil sa klinikal na kahinaan ng kanyang anak. Kailangan din niyang tiyakin na ang mga tagapag-alaga at manggagawa na pumapasok sa bahay ay nasubok. Minsan ito ay nakaka-stress, lalo na kung ang mga tao ay tumanggi na subukan o walang access sa kanilang sariling mga pagsubok. Minsan ay nagbibigay si Patricia ng mga pagsusuri sa ibang tao, ngunit maaaring mahirap ito dahil maraming LFT ang ginagamit ng kanyang sambahayan. Nahirapan si Patricia na subukan ang kanyang mga anak at kung minsan ay kailangang gumawa ng maraming pagsubok gamit ang ilang mga test kit, kung ang kanyang anak ay nahihirapan sa pagsubok. |
|
| “ | Naging mahirap para sa akin na gawin ito, kaya kung minsan ay nalampasan mo ang mga tatlong pamunas na sinusubukang tanggalin ang isa sa bata dahil... Lalo na sa mga LFT, ibig kong sabihin, nalampasan mo ang ilang pamunas dahil dumura siya o umubo o hinila ito […] o kung ano pa man.” |
| Dahil kailangan niyang ipagpatuloy ang regular na pagsubok kahit na tumigil ang mga LFT na malayang magagamit, nadama ni Patricia na pinansiyal na pinarusahan ng dagdag na gastos na ipinataw sa kanyang pamilya sa pamamagitan ng pagbabayad para sa mga pagsusulit. | |
| “ | Naramdaman ko na pinaparusahan ako dahil mayroon akong bata na mahina, samantalang ang ibang mga taong may mga anak - hindi sa wala silang pakialam, iyon ang ganap na maling salita - ngunit walang isyu na iyon. Wala silang ganoong dagdag na gastos. Ito ay tulad ng, muli, ito ay isa pang gastos sa mundong ito para sa pagkakaroon ng isang sakit. |
Ang ilang mga organisasyong pangkomunidad ay nakapagpatuloy sa pagbibigay ng mga libreng pagsusuri pagkatapos ng mass testing, na pinahaba ang panahon kung saan maaaring ma-access ng mga mahihinang tao ang mga pagsubok. Nadama ng mga nag-ambag na ito ay susi sa pagtiyak na ang mga taong mababa ang kita ay patuloy na gumagamit ng mga pagsubok na hindi nila magagawa o handang ma-access.
Pisikal na kakulangan sa ginhawa na nauugnay sa pagsubok
Tinalakay ng mga nag-aambag ang mga damdamin ng pisikal na kakulangan sa ginhawa na nauugnay sa paggamit ng mga LFT mula sa banayad hanggang makabuluhan. Dahil sa pagsubok, ang ilang narinig namin mula sa isang pakiramdam ay napakasakit at para sa ilan ang pisikal na kakulangan sa ginhawa ng pagsubok ay nagpababa sa kanila ng pagsubok sa paglipas ng panahon.
| “ | Noong […] inilagay ko ang pamunas sa aking lalamunan upang subukan, […] Hindi ako makahinga. Parang may kumapit sa leeg ko, sa lalamunan ko. Nahirapan ako, talagang nahirapan - at nakakatakot - na huminga."
– Tagapag-alaga |
| “ | Hindi ko talaga na-enjoy ang pagdikit nito sa aking ilong o sa likod ng aking lalamunan! Naaalala ko noong aktwal na pumasok ako sa aking C-section upang kunin ang aking maliit na batang babae, [paggawa ng isang pagsusuri sa Covid-19] ay hindi nabanggit, at ako ay parang, baka makatakas lang ako, [...bilang] hindi sila dumating at nagtanong. Pagkatapos [pagkatapos] ng limang minuto […], dumating sila at ginawa ito. Nagkaroon lang ako ng masamang gag reflex, sa totoo lang, at hindi ito magandang pakiramdam. Kaya, kung hindi ko kailangan mag-test, hindi ko na lang gagawin.”
– Tagapag-alaga |
Ang mga pamunas sa lalamunan ay nagdulot ng gagging reaksyon para sa ilan na nagbahagi ng kanilang mga kuwento. Ang mga pamunas ng ilong ay naging hamon din para sa ilan dahil may pagkaunawa na ang pamunas ay kailangang umabot sa ilong upang makakuha ng magandang kalidad na sample. Minsan ito ay maaaring mag-alala sa mga tao na maaari nilang saktan ang kanilang sarili. Nakarinig kami ng mga halimbawa ng pamunas ng ilong na naging sanhi ng pagdurugo ng ilong.
| “ | Ang unang pagsubok, kailangan mong gawin ito sa likod ng iyong lalamunan at iyong ilong, at pagkatapos ay [ang istilo ng pagsubok] ay nagbago kaya kailangan mo lang gawin ito sa iyong ilong [...] Naaalala ko na naisip ko, 'Oh, salamat sa diyos', dahil ito [ang unang uri ng pagsubok] ay nagparamdam sa iyo, [...] kapag ginawa mo ito sa likod ng iyong lalamunan, at hindi naman masama ang pagdikit ng iyong noseb."
– Clinically vulnerable na tao |
| “ | Ang mga testing kit ay nagdulot sa akin at sa iba pa na magkaroon ng pananakit ng lalamunan at pagdurugo ng ilong.”
– Kontribyutor ng Every Story Matters |
Ibinahagi ng mga taong neurodivergent na nakaranas sila ng mas mataas na kakulangan sa ginhawa at pagkabalisa dahil sa mga sensitibong pandama. Nangangahulugan ito na gumugol sila ng mas mahabang pagsubok na kumpletuhin ang mga pagsubok nang mag-isa, kung PCR home test man o LFT, at nahirapan din sila sa proseso ng pagsubok ng ibang tao.
Kwento ni ChloeSi Chloe ay isang autistic na nasa hustong gulang na may trabaho na nangangailangan sa kanya na magsuri nang madalas sa panahon ng pandemya. Ang unang ilang beses na nasuri si Chloe ay nasa isang setting ng ospital kung saan siya ay sinuri ng mga doktor. Natagpuan ni Chloe na ang karanasan ng pagsubok ng ibang tao ay lubhang hindi komportable at ipinahayag ang kanyang karanasan sa pagiging "pinned down" ng mga tauhan. Sa mga pagkakataong ito, sa huli ay hindi nakumpleto ng mga doktor ang pagsusuri. |
|
| “ | Ito ay nakababahalang. Sa tingin ko dahil […] maraming mga pagpapasigla na mayroon akong mga isyu. Kaya, sa mga tao, na may ingay, amoy, at mga bagay na katulad niyan. […] Nasa mga doktor ako at kailangan nilang gawin ang pagsusulit, at gumugol sila ng halos isang oras sa pagsisikap na pilitin ako. At pagkatapos, sinabi lang nila, 'Kailangan mong umuwi dahil hindi ka namin masusulit. Umuwi ka na, hindi ka namin mapupunta dito." |
| Kalaunan ay nagpalit ng trabaho si Chloe at pinayagang tapusin ang mga pagsusulit sa bahay. Bagama't hindi pa rin kumportable ang pagsubok sa kanyang sarili at tumagal ng mahabang panahon, nalaman niyang mas madali ito kaysa sa ibang tao ang magsagawa ng pagsusulit. | |
| “ | Kaya ko lang gawin ito sa bahay […] inabot pa rin ako, parang, isang oras para gawin dahil sa […] mga sensasyon, ngunit mas maganda ito dahil hindi ko pinilit [ang pagsusulit], pisikal na inilalagay sa aking bibig.” |
| Dahil sa kanyang negatibong karanasan, huminto si Chloe sa pagsusuri sa sandaling hindi na siya kinakailangan. Nadama niya na ang kanyang karanasan sa pagsubok ay magiging mas mahusay kung siya ay may higit na kontrol sa proseso, tulad ng kakayahang subukan ang kanyang sarili, o pagkakaroon ng mga pagsusulit sa isang tahimik na lugar, kung saan ang tao lamang ang gumagawa ng pagsusulit sa silid na kasama niya. | |
Nakita ng ilang nag-aambag ang mga pagsusuri sa PCR na pinangangasiwaan ng mga propesyonal na hindi gaanong komportable kaysa sa mga LFT na ginamit nila mismo. Mas mainam ang self-led testing dahil naramdaman nilang may kontrol sila at maaaring pumunta sa sarili nilang bilis. Inilarawan din ng ilang kontribyutor ang mga karanasan kung saan ang mga pagsusulit na pinangangasiwaan ng mga propesyonal ay tila hindi gaanong maingat na pinangangasiwaan, na nagdaragdag sa kanilang kakulangan sa ginhawa.
| “ | Ang pagsubok sa bahay ay mas mahusay, dahil kung minsan, kapag lumabas ka at ginawa ang pagsubok ng mga tao, sila ay napakahirap. Nagkaroon ako ng isa […] sa ospital at pinabuhusan niya ng dugo ang ilong ko.”
– Taong mula sa pinagmulang etniko ng Roma |
| “ | Ang isa sa mga nars ay partikular na malisya sa throat swab para sa pagsusuri sa Covid at patuloy na ginagawa ang mga ito, na tila hindi kinakailangan. Ako ay nasubok na positibo sa pagpasok ng isa pang nars, at [pagkatapos] muli niya ang pagsusulit na iyon ng tatlong beses sa siyam na oras na ako ay naroroon.
– Kontribyutor ng Every Story Matters |
Epekto sa kagalingan at kalusugan ng isip
Narinig din namin mula sa mga kontribyutor na nagsalita tungkol sa pag-iwas sa pagsusuri dahil nag-aalala sila tungkol sa isang positibong resulta at ang mga implikasyon ng diagnosis ng Covid-19 sa kanilang kalusugan sa isip.
| “ | Wala akong mga pagsusulit na iyon […] dahil hindi ako pumunta kahit saan […] Literal na hindi ako umalis sa aking lugar dahil sa sobrang takot na magkasakit ako, kaya hindi ko [kailangan] ang alinman sa mga pagsusulit na iyon [...] kung nalaman kong mayroon akong Covid, magkakaroon ako ng 10 beses na mas masahol na pagkabalisa, kaya hindi ko ginawa ito. Marahil ay nagkaroon ako ng Covid, dahil madalas akong nagkasakit na may mga sintomas tulad ng trangkaso, ngunit ayaw ko lang itong harapin.
– Tao mula sa isang nomadic na komunidad |
Ang mga taong nakausap namin ay gumawa ng koneksyon sa pagitan ng pagbabago sa pag-uugali ng pagsubok sa buong pandemya at ang epekto nito sa kalusugan ng isip ng mga tao. Ang isang halimbawa ay ang madalas na pagsusuri sa maagang bahagi ng pandemya ay nauugnay sa mga damdamin ng pagkabalisa, at ang pagbawas sa dami ng pagsubok na ginawa sa paglipas ng panahon ay nakatulong upang maibsan ito.
| “ | Sa simula […] Marahil ay masyado ko nang ginagawa ang mga ito, ngunit […] nang kahit ang gobyerno […at iba pang] mga tao sa pangkalahatan ay hindi na ito sineseryoso, sinimulan kong isuko ang aking sarili, at nagsimulang gumawa ng mas kaunting pagsubok. […] Nagsimula akong [na] medyo nahumaling […] sa paggawa ng mga pagsusulit dahil sa sobrang pagkabalisa ko, at iyon [sa ibang pagkakataon ay lumipat] din ako […] na pinipilit ang aking sarili na gumawa ng mas kaunting mga pagsubok […] upang pakalmahin din ang sarili kong mga pagkabalisa. Tulad ng nabanggit ko, mayroon akong matagal na mga isyu sa kalusugan ng isip, ang aking pagkabalisa [at] depresyon, kaya medyo mahirap pamahalaan sa bagay na iyon.
– Tagapag-alaga |
Ang pagtanggap ng abiso ng isang contact ay inilarawan bilang isang nakababahalang at hindi kasiya-siyang karanasan ng maraming nag-aambag. Kasama sa mga hindi kasiya-siyang aspeto ng karanasan ang alarma mismo (tumunog sa telepono sa pamamagitan ng app), ang stress ng hindi alam kung saan maaaring nakipag-ugnayan, o kung kanino kasama, at ang paghihintay kung mayroon silang Covid-19 – sa pamamagitan ng pagsusuri o paghihintay kung nagsimula ang mga sintomas.
| “ | Sa tingin ko, medyo nakakatakot para sa mga tao na makatanggap ng mensahe na nagsasabing nakipag-ugnayan ka sa isang tao. Depende sa kung ano ang tao, kung ito ay isang tao na nagkaroon na ng isang uri ng pagkabalisa, ito ay magpapalala sa kanila ng 100 beses."
– Kontribyutor ng Every Story Matters |
Inilarawan ng mga nag-aambag ang isang hanay ng mga epekto sa kanilang kalusugan ng isip dahil sa pagsunod sa mga alituntunin sa pag-iisa sa sarili. Kabilang dito ang pag-aalala, kalungkutan, stress at mababang mood. Nadama nila na ang mga kinakailangan ng pag-iisa sa sarili ay mahirap na kung minsan ay may pangmatagalang negatibong epekto sa kanilang kalusugan sa isip.
| “ | Hindi [ako] makalabas, hindi makalakad; ito [self-isolation] ay nakaapekto sa aking kalusugang pangkaisipan, sa aking kalusugan. Akala ko ay gagaling ang mga bagay, ngunit hindi; natagalan.”
– Bingi |
| “ | Nag-self-isolate ako para sa sarili ko sa loob ng 11 araw. Ang paghihiwalay ay talagang mahirap kumpara sa anumang bagay, alam mo. Ang pagkuha ng mga pagsusulit ay kahit na okay. Alam mo, ang pagpunta sa ospital ay okay, ngunit ang paghiwalayin ang iyong sarili mula sa lahat ay hindi okay. Kasi, alam mo, hindi ka mabubuhay nang walang kausap, nang hindi tumitingin sa sinuman o walang kinakausap.”
– Nakaligtas sa pang-aabuso sa tahanan |
Nakarinig din kami ng mga karanasan mula sa mga taong may dati nang kundisyon sa kalusugan ng isip na lumala ang mga kondisyon bilang resulta ng pag-iisa sa sarili. Inilarawan ng ilan sa mga kontribyutor na ito ang pakiramdam ng pagkabalisa dahil sa mahabang panahon ng pag-lock at na ang mga damdaming ito ay pinalala ng mga kinakailangan sa pag-iisa sa sarili. Ang pag-iisa sa sarili sa mga pagkakataong ito ay madalas na parang pagpapatindi ng mga paghihigpit sa lockdown para sa kanila.
| “ | With my mental health, it, for a while after I remember na ayokong lumabas at manatili lang sa bahay. Ang pagkakaroon ng social na pagkabalisa na ito, na palagi kong pinaglalabanan ang pagkabalisa, ngunit ito [pag-iisa sa sarili] ay pinalala pa ito ng sampung beses."
– Taong nakatira sa masikip o masikip na tirahan |
Ang ilang mga panahon ng pag-iisa sa sarili, at lalo na sa magkakalapit, ay nagkaroon din ng negatibong epekto sa kalusugan ng isip ng ilang nag-aambag. Ang ilan ay nagsabi sa amin kung paano ang pananatili sa loob ng bahay at malayo sa mga tao ay paulit-ulit na nakadama sa kanila ng higit na pagkabalisa at hindi gaanong hilig na lumabas pagkatapos ng kanilang mga panahon ng pag-iisa sa sarili.
| “ | Mahirap manatili sa loob ng mahabang panahon, lalo na sa site. Kailangan mong maghintay, dahil hindi ka makalabas. Alam mo ba ang ibig kong sabihin? Hindi ka maaaring lumabas at makihalubilo sa mga tao, dahil nasa sitwasyon ka kung saan nakipag-ugnayan ka sa Covid. Masasabi kong, 'Buweno, hindi,' at magpatuloy, ngunit nahirapan akong [sa isip] na ihiwalay ang sarili, dahil kinailangan naming [mag-isa] na ihiwalay ng ilang beses."
– Taong mula sa pinagmulang etniko ng Roma |
Nakahanap ang ilang nag-ambag ng suporta sa kalusugan ng isip na nakatulong sa kanila na makayanan ang pag-iisa sa sarili. Ang mga serbisyong ito ay karaniwang umiral bago ang pandemya sa mga kontribyutor na aming nakausap.
| “ | Ngunit oo, pinagdadaanan mo ang lahat ng mga pakiramdam ng pagiging masama at maaari itong medyo nakakatakot, sa palagay ko. Dahil ako ay ganap sa aking sarili. Ngunit sa palagay ko kung wala ako sa aktibong therapy sa oras na iyon ay talagang nahihirapan ako sa pag-iisip at pinapanatili ang aking sarili araw-araw. Kaya, napakaswerte ko.”
– Taong nakakuha ng suporta sa kalusugan ng isip |
| “ | At sa aming isla, mayroon kaming, kung ano ang tinatawag na, isang pagtitiwala sa pag-unlad. Hindi mo na kailangan pang humingi [ng tulong]. Kaya, mayroon talaga kaming health and wellbeing coordinator sa isla, na ang trabaho ay alamin kung sino ang maaaring, alam mo, hindi masyadong mahusay, o medyo nakahiwalay... At ang ethos ay, 'Kung sinuman ang nahihirapan, ipaalam sa amin. May mga tao doon na tutulong."
– Taong nabubuhay na may Long Covid |
Kwento ni IvankaIbinahagi ni Ivanka ang kanyang karanasan sa pag-isolate sa sarili sa loob ng mahabang panahon dahil sa kanya at sa iba pa sa kanyang sambahayan na nagpositibo sa Covid-19, pati na rin ang pakikipag-ugnayan sa Covid-19 sa kanyang lugar ng trabaho. Si Ivanka ay 27 taong gulang at tumira kasama ang kanyang kapareha at isang kaibigan sa panahon ng pandemya. Kapwa siya at ang kanyang kapareha ay mga manggagawa sa pangangalaga at naglakbay sa iba't ibang mga tahanan ng pangangalaga bilang bahagi ng kanilang trabaho sa isang ahensya. Sa loob ng dalawang buwan, sinabihan siyang mag-self-isolate sa ilang pagkakataon dahil sa positibong resulta ng Covid-19 sa kanya o ng iba. Ipinaalam sa kanya ang mga resultang ito sa pamamagitan ng alinman sa kanyang rehistro sa trabaho o sa contact tracing app. Ibinahagi niya kung gaano kahirap ang manatili sa loob para sa pinalawig na panahon ng pag-iisa sa sarili. Sa panahong ito, hindi siya binayaran at kinailangan niyang gamitin ang kanyang credit card para makabili ng mga mahahalagang bagay. Inilarawan din niya kung gaano kahirap na makakuha ng regular na paghahatid dahil ang ibang mga grupo ay inuuna para sa serbisyong ito. |
|
| “ | Nang walang kita, kailangan kong umasa sa aking credit card at nagtapos ako ng kaunting bayarin sa credit card pagkatapos ng panahong iyon na kailangan kong magtrabaho sa pagbabayad para sa ilang taon pagkatapos dahil malinaw na may mga pangangailangan at lahat ng bagay. |
| Natagpuan ni Ivanka ang pagkabalisa at stress dahil sa pag-iisa sa sarili na partikular na mahirap, sa kabila ng pag-access ng suporta sa kalusugan ng isip. Natagpuan niya ito mismo sa pamamagitan ng isang mental health organization para sa mga kabataan. Ipinaliwanag niya na nakakatulong ang pagkakaroon ng propesyonal na tulong sa labas ng kanyang kapareha at kaibigan, gayunpaman ipinaliwanag niya na nabubuhay pa rin siya sa pagkabalisa. | |
| “ | Hindi man lang lumalabas para sa sariwang hangin sa loob ng halos dalawang buwan na halos makuha mo-, nababalisa kami nang dumating ang oras ng pag-alis. Naaalala ko noong huling araw na lahat kami ay naalis sa mga bagay na kami, uri ng, nakaupo lang sa harap ng pinto nang kalahating oras at parang, 'So, lalabas na ba tayo ngayon?' Talagang nagkaroon ito ng negatibong epekto sa aming kalusugang pangkaisipan." |
| “ | Sa tingin ko ay isang malaking bagay iyon. Lahat tayo ay mas madaling ma-trigger, mas nababalisa at sa palagay ko ang buong sitwasyon sa kabuuan, sa palagay ko nagtatrabaho tayo sa isang propesyon kung saan nakilala tayo ng maraming pagkakalantad sa virus, ngunit marami ring pagkamatay na nagmula sa virus, nag-iwan ito ng isang malaking trauma. |
Mga kaayusan sa pamumuhay
Nakarinig kami ng mga halimbawa ng mga sitwasyon sa pamumuhay ng mga tao na nagsilbing hadlang sa pagsunod sa mga panuntunan sa pag-iisa sa sarili sa lahat o ganap.
Inilarawan ng mas malalaking pamilya o sambahayan ang pagbubukod sa sarili bilang mahirap kapag nakatira sa maliliit na espasyo. Nakarinig kami ng mga halimbawa ng mga partisyon upang matulungan ang mga nag-aambag o ang mga kasama nilang nakatira na ligtas na ihiwalay ang sarili. Kung saan may access ang mga nag-aambag sa ilang silid-tulugan o silid, ibinahagi nila na ang pag-isolate sa sarili ay hindi gaanong mahirap. Naisip nila na pinadali nito ang pagkumpleto ng buong panahon ng pag-iisa sa sarili.
| “ | I can't [self-]isolate sa bahay anyway because everyone's literally on top of each other. Halos parang, 'Kung hindi ako lalabas, bakit kailangan kong gawin ito?'… Hindi ito praktikal para sa lahat. It would depend if you have, we're in a small flat, some people might have a bigger house and, I guess, the guidelines that gave out didn't suit everyone and their situation.”
– Taong nakatira sa masikip o masikip na tirahan |
Para sa mga nag-aambag na naninirahan sa masikip, masikip at magkabahaging tirahan, hindi laging posible na ganap na ihiwalay ang sarili dahil sa kanilang mga kondisyon sa pamumuhay. Ang ilan ay nagsalita kung paano sila nag-aalala at nababalisa tungkol sa pamumuhay sa isang maliit na espasyo kasama ng ibang mga tao dahil sa panganib ng paghahatid ng virus.
| “ | Kaming lahat, hinding-hindi kami makapag-self-isolate pa rin dahil kami ay nagsasalo sa isang silid. Oo, nakuha namin lahat, sa palagay ko nakuha namin lahat."
– Taong nakatira sa masikip o masikip na tirahan |
| “ | Mayroong ilang mga pagkakataon na nagkaroon ako ng Covid-19 at [naipit] sa bahay at iniisip, 'Iyon na nga, mamamatay tayo, at lahat ng tao sa bahay ay magkakasakit sa akin.' Pagkatapos ay sisimulan mong sisihin ang bagay sa iyong sarili sa pagkakaroon ng sakit sa bahay, kung saan iniisip ko, 'Bibigyan ko siya ng Covid-19, bibigyan ko siya ng Covid-19.'”
– Taong nakatira sa masikip o masikip na tirahan |
kwento ni AngusSi Angus ay isang transgender na lalaki at nakaligtas sa pang-aabuso sa tahanan. Siya ay nasa maagang twenties noong panahon ng pandemya nang siya ay nawalan ng tirahan. Ibinahagi niya sa amin kung paano nakaapekto ang pagiging walang tirahan sa panahong ito kung paano niya nagawang makisali sa test, trace at isolate system. Ipinaliwanag ni Angus kung paano nakadama sa kanya ng labis na pagkabalisa ang pagsubok na positibo para sa Covid-19 dahil wala siyang lugar na komportableng ihiwalay ang sarili. |
|
| “ | Bago ako magkaroon ng matatag na pabahay, tulad ng, ang paghiwalay sa sarili ay nangangahulugan ng pagiging hindi handa sa pagkakaroon ng pagkain o pagkakaroon ng sapat na mapagkukunan para maging komportable ang lahat na maghiwalay sa sarili. At pagkatapos, sa mga susunod na panahon…nangangahulugan ito na umasa sa mga paghahatid ng pagkain o mga sitwasyon ng Uber Eats at iwan ang mga ito sa labas ng pinto at mga bagay. Ngunit imposible pa rin itong gawin, sa palagay ko, sa isang ganap na mahusay na paraan kung saan ikaw ay ganap na nakahiwalay dahil sa, sa palagay ko, ang aking demograpikong napakababang kita, ang mga kaibigang regular na hindi matatag na tinitirhan, napakaimposible na ito ay ganap na nakahiwalay.” |
| Sa isang yugto, habang naghihintay siya ng tirahan, nakikitira siya sa isang kapareha sa isang masikip na flat na may dalawang silid-tulugan nang ang isang flatmate ay nasubok na positibo para sa virus. Nangangahulugan ito na ang lahat sa flat ay kailangang mag-self-isolate hanggang sa masuri sila ng negatibo. Gayunpaman, hindi ito posible na gawin nang ligtas dahil sa bilang ng mga taong naninirahan doon.
Nahawa si Angus ng virus nang maraming beses sa panahon ng pandemya. Nakatira siya ngayon kasama si Long Covid. |
|
| “ | Ito ay isang bagay na sa tingin ko ang mga tao ay emosyonal na salungat sa pag-alam sa [mga resulta ng pagsusuri sa Covid], at kapag nalaman nila dahil kailangan nilang malaman, pagkatapos ay magkakaroon, tulad ng, mga negatibong kahihinatnan sa halip na nasa bahay lamang sa isang ligtas na kapaligiran. |
Kakulangan ng panlipunang suporta at insentibo
Kung saan sinabi sa amin ng mga nag-aambag na wala silang mga kaibigan at pamilya sa malapit, minsan ay nahihirapan sila sa pag-iisa sa sarili. Pakiramdam nila ay inabandona sila nang wala ang mga network na ito at hindi laging alam kung saan hihingi ng suporta sa mga panahong ito. Ibinahagi din ng mga nag-aambag na ang pagiging mag-isa habang may sakit ay maaaring maging malungkot, kahit na ang mga mahal sa buhay ay nag-iwan ng mga mahahalagang bagay.
| “ | May dementia ako diba? At para sa akin, ito ang pinakamasama kong bangungot. Ito ay. At pagkatapos, dahil sa oras na ako ay may Covid sa aking sarili at walang sinumang sumusuri sa akin, at ako ay talagang may sakit. Talagang, talagang may sakit sa loob ng halos dalawang linggo, at sa bahay mismo. Alam mo, sa sarili ko, at walang makakapasok sa akin."
– Kontribyutor ng Every Story Matters |
Ang mga nag-aambag na may mga pangangailangan sa accessibility ay partikular na naapektuhan ng pagsasara o pagbabawas ng mga serbisyo ng mga organisasyong pangkomunidad, kabilang ang mga hindi kasama sa digitally at mga taong may mga kapansanan o kahirapan sa pag-aaral. Natuklasan nilang mahirap ayusin ang mga online na paghahatid habang nagbubukod sa sarili dahil sa pagbaba sa mga antas ng kawani. Halimbawa, ang ilang mga nag-aambag ay walang tumulong sa kanila na ayusin ang mga online na paghahatid ng pagkain mula sa mga supermarket. Naging mas mahirap itong i-access ang mga mahahalaga habang nagbubukod sa sarili.
| “ | Natamaan at na-miss ang kanyang [pagkain] box. Kung minsan ay magkakaroon siya ng isa sa isang linggo, at sa susunod na linggo ay maaaring wala na siya, ngunit sa susunod na linggo ay maaari siyang maghatid ng dalawang kahon. So, I think hindi siya makakaligtas, food-wise.”
– Clinically vulnerable na tao |
Bagama't hinikayat ang mga tao na itala ang mga resulta ng pagsusuri sa bahay ng Covid-19 sa pamamagitan ng mga app o online, ito ay hindi kinokontrol, kaya maaaring piliin ng mga tao kung mag-uulat o hindi ng isang positibong pagsusuri, na nangangahulugang hindi sila mananagot ng isang pormal na sistema upang ihiwalay ang sarili. Ito ay humantong sa ilang mga nag-aambag na tanungin ang halaga ng pagsubok sa unang lugar.
| “ | Pinapatunayan mo lang ito sa iyong sarili sa mga LFT [samantalang sa] isang PCR, [kung] nagpositibo ka, [...] alam ng mga tao na mayroon kang Covid at halos may pressure na gawin ang tamang bagay [...] dahil ngayon ay nasa iyong mga talaan ng NHS ang [resulta ng pagsubok] na iyon. Samantalang ang isang LFT, maaari akong magkaroon ng Covid, tulad ng ginawa ko, at pumunta sa isang konsyerto.
– Kontribyutor ng Every Story Matters |
5. Ang mga karanasan ng mga magulang, mga sumuporta sa iba at mga nakaligtas sa pang-aabuso sa tahanan |
 |
Tinutuklas ng kabanatang ito ang mga partikular na karanasang ibinahagi ng mga magulang, ng mga sumuporta sa iba at ng mga nabubuhay sa mga mapang-abusong sitwasyon sa paligid ng pagsubok at pag-iisa sa sarili.
Ang mga karanasan ng mga magulang na may maliliit na anak
Inilarawan ng mga magulang ang pagsubok sa kanilang mga anak bilang isang hamon at ang mga magulang ng mga bata na may karagdagang mga pangangailangan ay nahirapan. Ang ilang mga magulang na narinig namin mula sa naalala ay kinakailangang pisikal na pigilan ang kanilang mga anak upang subukan ang mga ito at inilarawan ang karanasan bilang nakababahalang. Ang mga kahirapan sa pagsubok kung minsan ay humantong sa mga alalahanin tungkol sa epekto sa bata, pati na rin ang mga resulta ng pagsusulit na hindi tumpak.
| “ | Sinubukan kong gawin ang aking anak na babae ng dalawa o tatlong beses, at hindi niya ito magawa. [...] Siya ay bumubula. At pagkatapos ay ipapadala mo iyon at babalik […] malinaw. Ngunit alam mong tingnan mo siya, [...] may sakit siya. Nawalan siya ng lasa, wala siyang amoy. Nagkasakit siya ng trangkaso sa loob ng ilang linggo […] at sa tingin mo, 'Mayroon siya nito. Ngunit hindi ko makuha ang pagsubok na ito upang patunayan na mayroon siya nito'."
– Taong mula sa pinagmulang etniko ng Roma |
| “ | Para sa mga bata, ito ay isang bangungot! Hinahabol sila sa paligid, pinning down, bribing sa kanila. Pero ano pa ang magagawa mo?"
– Taong may pangmatagalang pisikal na kondisyon sa kalusugan |
Ang mga magulang ng mga batang may autism, ADHD at iba pang kumplikadong mga pangangailangan ay nahirapang subukan ang kanilang mga anak. Ito ay dahil sa tumaas na sensitibong pandama at, tulad ng kaso para sa mga bata sa pangkalahatan, nahihirapang ipaliwanag kung bakit kailangan ang pagsusulit at pangangatuwiran sa bata o kabataan.
| “ | Naiisip mo bang mahikayat ang isang autistic na bata na ipa-swab para sa isang pagsubok sa Covid? Iyon ang pinakamasamang panahon sa buhay ko.”
– Kontribyutor ng Every Story Matters |
Kwento ni GraceNakatira si Grace kasama ang kanyang asawa at anak, na wala pang limang taong gulang sa simula ng pandemya. Ang kanyang anak ay mula noon ay na-diagnose na may autism at naghihintay ng pagtatasa para sa ADHD. Nakipaglaban siya sa maraming elemento ng pandemya, kabilang ang malayong pag-aaral, kakulangan ng oras na ginugol sa labas at ang mga pagbabago sa kanyang normal na gawain. Masigasig si Grace na sundin ng kanyang pamilya ang patnubay ng gobyerno at regular na sumubok dahil nagkaroon sila ng bula kasama ang kanyang nakatatandang ina. Gayunpaman, ang pagsubok sa anak ni Grace ay napatunayang napakahirap, dahil sa mga sensitibong sensitibo na nauugnay sa kanyang autism. Mabilis na nabalisa ang kanyang anak nang dalhin siya nito upang masuri sa mga PCR test center. Ang kahirapan sa pagsubok sa kanyang anak ay nag-ambag sa isang pakiramdam ng matinding stress para kay Grace. |
|
| “ | Dahil sa kanyang pagkasensitibo na may kaugnayan sa autism, nakita niya ang mga pamunas ng ilong na lubhang nakababalisa at ang mga pamunas sa lalamunan ay ganap na hindi mabata - kinailangan namin siyang pigilan habang sumisigaw sa kotse sa mga istasyon ng pagsubok habang siya ay nagsusuka sa mga pamunas sa matinding pagkabalisa. |
| Si Grace at ang kanyang asawa ay gumawa ng mga pagsasaayos upang suportahan ang neurodivergence ng kanilang anak at ngayon ay nararamdaman nila na sila ay nasa "mas magandang lugar". | |
Ang mga magulang ay nagpahayag ng mga alalahanin tungkol sa pagiging angkop ng pagsubok sa napakaliit na mga bata dahil sa pagkabalisa at kakulangan sa ginhawa na dulot nito. Ang mga kahirapan sa pagsubok sa mga bata ay nangangahulugan na ang ilang mga magulang ay nagpasya na ihiwalay ang sarili sa halip na magpatuloy sa pagsubok. Nagkaroon din ng ilang pagkalito tungkol sa kung kinakailangan ang pagsubok sa mga bata pagkatapos ng isang panahon ng pag-iisa sa sarili.
| “ | Umabot sa punto na huminto ako sa pagsubok sa mga bata dahil mas madaling [mag-isa] ng sarili, manatili sa bahay at lumayo sa mga tao sa loob ng pitong araw, kaysa [...]
– Kontribyutor ng Every Story Matters |
| “ | May isang punto kung saan ang aking anak na lalaki ay bumalik sa paaralan at sila ay […] kinakailangan na [magsubok…] araw-araw. At naisip ko lang, 'Hindi ko alam kung gaano kasarap ang pakiramdam ko tungkol sa paglalagay niya ng bagay na iyon sa kanyang ilong araw-araw.' […] ang discomfort lang […] na sinamahan ng hindi ako sigurado kung gaano ito katumpak... […] Naisip ko, […] 'kayong lahat ay malulusog na bata talaga, pabalik sa paaralan. Sapat na ang pagsusuot mo ng maskara at lahat ng iba pa, kaya sa palagay ko marahil ay medyo maluwag ako sa pagpapagawa sa kanya ng ganoon araw-araw.
– Nag-iisang magulang |
Ang mga magulang na may maliliit na anak ay nahihirapan ding mag-isa sa sarili para sa mga praktikal na dahilan. Ang mga nag-aambag na ito ay nagtaas ng mga alalahanin tungkol sa kung ano ang maaaring mangyari sa kanilang mga anak kung ang parehong mga magulang ay nagkasakit ng virus. Ibinahagi ng ibang mga magulang na kailangan nilang ihiwalay ang sarili kasama ang mga bata sa kanilang mga silid-tulugan upang mapanatiling ligtas ang natitirang bahagi ng pamilya.
| “ | Oo, maliwanag na ang maliit na batang babae ay mga siyam lamang, kaya hindi siya maaaring [mag-isa] mag-isa sa kanyang silid, kaya nagboluntaryo ang kanyang ina. Ito ay hindi na masama, hindi ko iniisip. Ang aking asawa ay walang anumang mga sintomas, kaya hindi niya ito nakuha sa pangalawang pagkakataon, pinananatili niya ang aking anak na babae para sa isang linggo na naglalaro at nanonood ng TV at binabantayan lamang siya, kaya iyon ay isang silid lamang na nakahiwalay."
– Clinically vulnerable na tao |
Ang mga magulang na may maliliit na anak ay nagsalita tungkol sa pangangailangang lapitan ang self-isolation sa isang pragmatikong paraan. Sinabi nila sa amin ang tungkol sa pamamahala nito nang maingat habang sinusubukang balansehin ang mga pangangailangan ng kanilang anak pati na rin ang natitirang bahagi ng pamilya. Ibinahagi nila na kung minsan ay hindi posible ang pagsunod sa mga alituntunin sa pag-iisa sa sarili upang makapagbigay ng pangangalaga, at kung paano sila gumamit ng mga hakbang sa proteksyon sa halip. May mga nag-ambag na nagsabi sa amin na ang walang suporta mula sa pamilya o pormal na mga serbisyo ng suporta ay nagpapataas ng kanilang posibilidad na hindi sumunod sa mga panuntunan sa pag-iisa sa sarili upang pangalagaan ang kanilang mga anak.
| “ | Ngunit ang bagay ay, ang aking mga anak ay maaaring [mag-isa] at manatili sa kanilang silid at maaari kong dalhin ang kanilang pagkain sa kanila, ngunit kapag ito na ang aking pagkakataon, alam mo, ang mga bata ay igiit, ngunit pagkatapos ay may pananagutan sa akin bilang pinuno ng pamilya upang matiyak na ang lahat ay gumagana. Kaya, hindi ko [self-] ihiwalay nang madalas.”
– Kontribyutor ng Every Story Matters |
Mayroon ding mga emosyonal na dahilan kung bakit ang mga magulang na may maliliit na anak ay natagpuang mahirap ang pag-iisa sa sarili. Sinabi sa amin ng ilang kontribyutor kung gaano kabalisa at kawalang-kakaya ang naramdaman nila sa panahong ito, lalo na kapag wala silang suporta mula sa ibang magulang o pormal na serbisyo at nagkasakit sila ng virus. Ang sitwasyong ito ay naging mas mahirap kapag ang mga tao ay nagkaroon ng maraming anak na dapat alagaan.
| “ | I just felt really lonely. Sa tingin ko, madalas akong umiyak kapag kailangan kong ihiwalay ang sarili ko. Alam mo, dahil masama ang pakiramdam ko at kinailangan kong alagaan ang pitong bata dahil walang sinuman ang maaaring pumasok upang tumulong sa akin... Gaya ng sinabi ko, nakaramdam ako ng labis na pagkabalisa, nakaramdam ako ng depresyon.”
– Taong nakakuha ng suporta sa kalusugan ng isip |
Sinabi sa amin ng ibang mga magulang na may maliliit na anak kung paano sila nakatanggap ng suporta mula sa mga lokal na organisasyon tulad ng mga simbahan at kawanggawa noong sila ay nahawa ng virus. Ibinahagi nila kung paano nagbigay ang mga organisasyong ito ng mga paghahatid ng pagkain na nagbigay-daan sa kanila bilang mga magulang na ganap na ihiwalay ang sarili. Ipinaliwanag ng ilan na kung wala ang tulong na ito, ang pagluluto at paghahanda ng pagkain para sa mga bata ay hindi magiging posible, kung hindi man ay pinipilit ang mga magulang na lumihis sa mga alituntunin at maiwasan ang pag-iisa sa sarili.
| “ | Ang aking simbahan ay kamangha-mangha. Dumating sila na may dalang lutong pagkain, at maraming mga restawran ang nagbibigay ng […] lutong pagkain, […] kaya ang aking simbahan ay kamangha-mangha, dahil dadating lang sila at ihahatid sila sa pintuan, susunduin sila ng anak, kaya, para doon, lubos akong nagpapasalamat at nagpapasalamat sa kanila… Kahit na mag-order ka online, kailangan pa rin silang lutuin at hindi ka makakabili ng takeaway araw-araw. Kaya, kung wala ang tulong ng aking simbahan at mga kapitbahay, hindi, talagang hindi [hindi magiging posible ang self-isolation].”
– Taong nakakaranas ng kahirapan sa pananalapi |
| “ | Nagkaroon kami ng ilang parcel ng pagkain mula sa isang lokal na kawanggawa, dahil nahihirapan ako sa pagluluto para sa mga bata…. Kaya, nakakuha kami ng mga frozen na pagkain na personal na niluto ng isang tao sa isang lugar... Iyon ang pinakakapaki-pakinabang na bagay na naranasan ko, dahil ang pagkakaroon ng tatlong maliliit na anak at pagiging buntis, parang ako, ang pagluluto ay impiyerno, ito ay kakila-kilabot. Malaking pagbabago iyon sa aming sambahayan.
– Taong may pangmatagalang pisikal na kondisyon sa kalusugan |
Ang mga karanasan ng mga sumuporta sa iba upang subukan
Inilarawan ng ilang kontribyutor ang pangangailangang suportahan ang iba upang makapagsubok, alinman sa propesyonal na kapasidad o tulungan ang mga miyembro ng pamilya sa bahay.
Pagtulong sa mga taong may kapansanan o mga taong neurodivergent na magsuri
Inilarawan ng ilang miyembro ng pamilya na sumuporta sa mga taong may kapansanan at mga taong neurodivergent para masuri ang kanilang mga kamag-anak na hindi laging nauunawaan kung bakit kailangan nilang magpasuri. Sa ilang mga kaso, ang mga sinusuri ay lalaban sa mga pagtatangka sa pagsubok, na ginagawa itong mas mahirap. Ito ay nakababahala kapwa para sa taong sinusubok at sa mga sumusubok na magbigay ng pagsusulit.
| “ | Pagdating sa aking mga kapatid na may mga kapansanan, parang, […] 'Bakit mo itinataas ito sa aking ilong? Ayoko nito'. Hindi nila ako papayagan na gawin iyon. Iyon ay talagang kakila-kilabot, sinusubukan na [pangasiwaan ang isang pagsusulit…] Napakahirap [... ngunit] sila ay mga nasa hustong gulang na, [kaya] kung tumanggi sila […] hindi ko ito mapipilit.”
– Miyembro ng pamilya o tagasuporta ng isang tao na kinakailangang ihiwalay ang sarili |
| “ | Ang aking mga kapatid na lalaki ay hindi maaaring gawin ito sa kanilang sarili [...] sila na lang ihagis [...] ang pagsubok [pababa, at] pagkatapos ito ay marumi, hindi ba? Kaya, kung hindi ko ito nakuha nang tama […] maraming pag-aaksaya.”
– Miyembro ng pamilya o tagasuporta ng isang tao na kinakailangang ihiwalay ang sarili |
Nadama ng ilang kontribyutor na ang pagsusuri ay maaaring magpalala sa mga kasalukuyang kondisyon ng kalusugan. Ang isang halimbawa ay kung saan lumitaw ang mga pagsusuri upang mag-trigger ng mga epileptic seizure. Upang maiwasan ito, mas madalas na sinubukan ng mga kontribyutor na iyon ang ibang tao ngunit pinataas ang kanilang sariling pagsusuri upang matiyak na mas mababa ang panganib ng impeksyon.
Pagtulong sa mga matatandang tao sa pagsubok
Sinabi sa amin ng mga nag-aambag na ang mga matatandang tao na may pisikal na kondisyon tulad ng arthritis o panginginig ay kadalasang nangangailangan ng iba upang tulungan silang magsuri. Ang ilang mga nag-aambag ay nadama na ang mga pagsusulit ay maaaring maging mas inklusibo para sa mga taong may limitadong manual dexterity upang payagan silang gumamit ng mga pagsusulit nang nakapag-iisa.
| “ | May arthritis ang nanay ko. Ang pagtanggal sa maliliit na bagay na iyon ay talagang mahirap, kaya mabuti na siguro na magkaroon ng ilang magagamit para sa mga taong may pisikal na kapansanan upang aktwal na magamit.”
– Tagapag-alaga |
Ang mga miyembro ng pamilya at mga propesyonal sa pangangalagang pangkalusugan na sumusubok sa mga matatandang tao na may mga kondisyong neuropsychological, tulad ng demensya, ay natagpuan na ito ay mahirap. na gawin ito dahil sa kakulangan ng pag-unawa sa mga sinusuri tungkol sa kung ano ang pagsubok at kung bakit ito kinakailangan.
| “ | Palagi kong nakikita itong diretso sa aking sarili, ngunit ang mga pasyente ay maaaring maging isang kaunting isyu, lalo na ang mga matatandang pasyente na may demensya […] Talagang hindi nila naiintindihan kung ano ang iyong ginagawa at kung bakit.”
– Taong nagtatrabaho sa pangangalagang pangkalusugan at panlipunan |
Ang mga karanasan ng mga nakaligtas sa pang-aabuso sa tahanan
Narinig namin mula sa mga kontribyutor na may mga karanasan sa pang-aabuso sa tahanan at nakatira kasama ang isang mapang-abusong kasosyo sa panahon ng pandemya. Ang mga kontribyutor na ito ay nagpahayag kung paano sila nakaramdam ng panggigipit ng kanilang kapareha na sundin o hindi sundin ang mga alituntunin sa pag-iisa sa sarili sa parehong paraan ng kanilang kapareha. Naiulat din na ang mga mapang-abusong kasosyo sa pangkalahatan ay hindi isinasaalang-alang ang mga kahihinatnan ng hindi pagsunod sa mga alituntunin (kung saan nauugnay). Kung minsan ay inilalagay nito ang mga bata sa sambahayan sa panganib, kabilang ang mga taong mahina rin sa klinika, kasama ang iba pang nakipag-ugnayan sa kanila sa labas ng bahay.
| “ | Para sa akin ay mas mahirap dahil nakatira ako sa isang mapang-abusong kapareha na napaka-makasarili at hindi sumusunod sa mga patakaran, hindi naisip na sila ay nag-apply sa kanya. At kaya, sinisikap kong panatilihing ligtas ang aking anak, sinusubukang makipaglaban sa kanya, ito ay talagang mahirap na oras.
– Nakaligtas sa pang-aabuso sa tahanan |
Kwento ni MillieIbinahagi sa amin ni Millie ang kanyang mga karanasan sa salungatan sa kanyang mapang-abusong kapareha kapag sinusubukang sumunod sa mga alituntunin sa pag-iisa sa sarili. Nahirapan siyang sundin ang mga alituntunin nang maramdaman niyang palagi siyang nakikipagtalo sa kanyang kapareha kung dapat nilang sundin ang mga ito o hanggang saan ang dapat nilang gawin. Naniniwala siya na ang "tamang bagay na dapat gawin" ay ang sundan sila habang hindi niya iniisip na ito ang palaging nangyayari. |
|
| “ | Nakakadismaya dahil nagdulot ito ng maraming pagtatalo [nakipagdebate sa mga alituntunin sa paghihiwalay sa sarili kasama ang kanyang kapareha]. Sinabi niya na ako ay isang tupa at sumusunod lang sa lahat, [na] ito ay katawa-tawa, ito ay hindi totoo, ito ay ang gobyerno lamang ang gumagawa ng mga bagay upang kontrolin kami… Oo, ito [ang pagtatalo tungkol sa kung paano sumunod sa mga alituntunin] ay nagdulot ng maraming salungatan, tiyak. |
| Natatakot din si Millie na ang kanyang anak na lalaki, na may clinically vulnerable, ay makontrata ng Covid-19 ng sambahayan na hindi sumusunod sa mga alituntunin sa pag-iisa sa sarili. Sinabi niya sa amin na mas gusto ng kanyang partner na unahin ang kanyang kapakanan kaysa sa pamilya na sa tingin niya ay nakababahala. | |
| “ | Siya [ang kanyang anak] ay dapat na nasa kategoryang nasa panganib. Pero kinumbinsi ako ng papa niya na hindi. Siya ay, tulad ng, 'Well, hindi siya dahil hindi siya na-diagnose na may hika, wala siyang diagnosis ng hika.' Ako, tulad ng, 'Oo, ngunit ginagamot nila siya para sa hika, mayroon siyang lahat ng mga epekto ng hika. Kakasabi lang nila na hindi nila siya legal na ma-diagnose dahil mas matanda na siya.' [Sabi ng partner ni Millie] – 'Well, then, wala siyang asthma, kaya hindi siya at-risk category.' Ako, parang, 'Well, siya talaga.' Kaya, sinubukan kong gawin ang mga karagdagang pag-iingat at labis na ihiwalay siya. Naramdaman na lang siya ng tatay niya sa panganib. Ito ay [diskarte ng kasosyo sa pagsunod sa mga alituntunin], tulad ng, 'Well, hindi ako maaaring umupo lang sa bahay,' ako ay, 'Well, ang buong bansa ay nakaupo sa bahay,' 'Well, hindi ko [kasosyo] magagawa iyon, kailangan kong magkaroon ng aking oras at aking espasyo.' |
| Ang mga panahon ng pag-iisa sa sarili na nangyari ay nagdulot ng karagdagang pagtatalo sa pagitan ng mag-asawa dahil kailangan nilang manatili sa iisang bahay. Dahil dito, mas naka-stress ang sambahayan para kay Millie. | |
| “ | Ito [pag-iisa sa sarili] ay nag-iisa at nagdulot ito ng mas maraming argumento. Higit pa sa dati. Ito ay mahirap. Noong kinailangan naming [self-] i-isolate, minsan siya ay [self-]isolate. But then it just caused more arguments because we were just on top of each other.” |
| Naalala ni Millie ang isang pagkakataon kung saan siya ay nakipag-ugnayan sa pamamagitan ng contact tracing app tungkol sa pagkakaroon ng malapit na pakikipag-ugnayan sa isang taong nagpositibo sa virus. Gayunpaman, naramdaman niyang pinilit siya ng kanyang kapareha na huwag ihiwalay ang sarili, kahit na inirerekomenda ito ng mga alituntunin. | |
| “ | I'd be pressured to, [partner reported speech] 'Naku, huwag kang katawa-tawa, sinusubaybayan ka lang nila. Hindi mo kailangang [mag-self-] ihiwalay, hindi ka pa nakaka-contact. Malamang dude lang yung nilagpasan namin ng tatlong segundo nung isang araw.' So, may mga pagkakataon na kailangan kong [mag-self-] mag-isolate technically, pero hindi namin ginawa dahil sinabi niya na huwag." |
| Ibinahagi ni Millie na ang ganitong uri ng pagkontrol sa pag-uugali ay nagpatuloy sa buong pandemya na naging dahilan upang subukang sundin ang pag-iisa sa sarili na napakahirap at nakababahalang. Lalo siyang nag-aalala tungkol sa kapakanan ng kanyang anak at sa panganib sa kanya. | |
Naalala din ng mga taong nagtatrabaho upang suportahan ang mga nakaligtas sa pang-aabuso sa tahanan o ang mga nasa panganib ng pang-aabuso, na naninirahan sa bahay, kung gaano kahirap ang nakita nila sa mga sitwasyon kung saan alam nilang nagbubukod sa sarili ang mga apektadong tao.
| “ | Wala akong pinagsisisihan sa aking mga ginawa noong panahong iyon, ngunit wala akong ibang nararamdaman kundi ang paghamak at kung minsan ay matinding pagkapoot sa mga taong diumano'y namamahala sa bansa na gumawa ng kanilang sariling bagay habang ako ay nagmamaneho sa paligid ng aking lugar upang tingnan ang mga kababaihan na ngayon ay nakulong na may mga abusadong lalaki sa kanilang mga tahanan, nagsasagawa ng mga pagpupulong mula sa isang telepono o laptop sa isang paradahan ng kotse dahil ang aking mga opisina at ang aking bahay ay hindi naka-lock sa pagitan ng aking mga opisina at ang aking bahay. habang nagpapadala ako ng mga parsela ng pang-emerhensiyang pagkain sa mga pamilyang nag-iisa sa sarili nang walang suporta ng pamilya sa paligid upang tulungan sila, habang sinisikap kong tiyakin na ang mga bata ay hindi masasaktan at inaabuso sa kanilang mga tahanan."
– Kontribyutor ng Every Story Matters |
6. Iminungkahing mga pagpapabuti para sa hinaharap |
 |
Inilalarawan ng kabanatang ito ang mga mungkahi ng mga nag-aambag para sa pagpapabuti ng sistema ng pagsubok, pagsubaybay at paghihiwalay. Nagsisimula ito sa isang talakayan ng mga pagmumuni-muni ng mga nag-aambag sa mga pagpapabuti sa sistema sa kabuuan, bago hiwalay na tugunan ang mga mungkahi para sa kung paano mapapabuti ang pagsubok, pagsubaybay sa pakikipag-ugnayan at pag-iisa sa sarili sa hinaharap na pandemya.
Kinilala ng mga kontribyutor na ang pagsubok, pagsubaybay, at paghihiwalay na sistema sa kabuuan ay inilagay nang mabilis at sa ilalim ng mga pambihirang pagkakataon. Marami ang nakaunawa sa kahalagahan nito, at nagbigay ito ng ilang katiyakan tungkol sa pagkontrol sa pagkalat ng virus habang sila ay lumabas sa lockdown.
| “ | Ito ay isang paraan para makalabas ang mga tao. Pinayagan nito ang mga tao na lumabas, alam mo, 'mag-sign in at maaari kang magkaroon ng pagkain sa restaurant na ito'. Nangangahulugan ito na kung nakipag-ugnayan ka, maaari mong ihiwalay ang iyong sarili, at halos nagbigay ito sa iyo ng pag-uudyok na pumunta, 'Sa totoo lang, dapat akong gumawa ng pagsusulit.'”
– Kontribyutor ng Every Story Matters |
Gayunpaman, mayroong ilang iminungkahing pagpapahusay, na ginalugad sa loob ng kabanatang ito.
Impormasyon at Komunikasyon
Nais ng mga nag-aambag ng higit na pagkakapare-pareho at kalinawan sa mga patakaran at pagmemensahe ng pamahalaan. Sinabi ng mga nag-ambag na nahirapan silang sumunod sa mga alituntunin, na sa tingin ng marami ay patuloy na nagbabago (ibig sabihin, tungkol sa mga kinakailangan sa self-isolation at timeframe). Iminungkahi din nila na ang parehong patnubay at impormasyon sa mga bansang pinag-uukulan ay magiging kapaki-pakinabang - lalo na para sa mga tao sa mga hangganan na kailangang sumunod sa parehong hanay ng mga panuntunan, halimbawa, (hal.
| “ | Sa tingin ko kailangan mong magkaroon ng pamantayan sa UK. Hindi ka maaaring magkaroon ng kakaiba sa [bawat bansa sa UK]. Kapag nakatira ka nang malapit sa isang hangganan, maaari kang nagtatrabaho sa England at nakatira sa Wales, o kabaliktaran, at mayroon kang dalawang magkaibang mga alituntunin.”
– Kontribyutor ng Every Story Matters |
| “ | Malaki rin ang naitulong ng patnubay/impormasyon ng gobyerno. Ang mga kritisismo, na kadalasang nakabatay sa mga pananaw sa pulitika, ay hindi nakakatulong. Ang patuloy na paghahambing sa Scotland o Europe o kung saan man ay hindi kapaki-pakinabang - ang mga istatistika ay maaaring gamitin sa iba't ibang mapanlinlang na paraan."
– Kontribyutor ng Every Story Matters |
Sa Scotland, positibo ang ilang nag-ambag tungkol sa komunikasyon ng pamahalaan. Ito ang kaso para sa mga pangkalahatang pag-update tungkol sa Covid-19 ngunit gayundin ang buong pagsubok, pagsubaybay at paghihiwalay ng sistema. Ang malinaw at regular na pagmemensahe mula sa mga opisyal ay nakatulong sa pagbuo ng tiwala sa mga tao na ginagawa nila ang tama.
| “ | I think, say that communication was vital but I actually think in Scotland, maganda ang communication. Ang Unang Ministro ay darating sa telebisyon araw-araw. Ang mga medikal na opisyal ay nagsasalita araw-araw. Kaya, sa palagay ko, ang mga tao ay hindi maaaring umasa ng higit pa kaysa doon at ito ay isang natatanging sitwasyon.
– Miyembro ng komunidad na sumuporta sa mga tao na ihiwalay ang sarili |
| “ | Sa Scotland ang Gobyerno ay mahusay sa pagbibigay ng impormasyon at talagang hinangaan ko [sila sa pag-una] sa Scotland at sa mga tao nito.”
– Kontribyutor ng Every Story Matters |
Gusto rin ng mga taong narinig namin ang mas mahusay na pag-iwas sa maling impormasyon tungkol sa test, trace at isolate system dahil ito ay itinuturing na nakaimpluwensya sa pag-uugali.
| “ | Nagkaroon ng maraming disinformation at maling impormasyon tungkol sa NHS Covid app para sa mga smart phone. Masaya akong gamitin ang app dahil akala ko ito ay isang kapaki-pakinabang na tool ngunit maraming mga taong kilala ko ay hindi nag-download o nag-alis nito sa kanilang mga smart phone dahil inaakala nilang sinusubaybayan ng gobyerno ang kanilang mga paggalaw at may ilang isyu sa pag-develop ng app.
– Kontribyutor ng Every Story Matters |
Nakarinig kami ng ilang mungkahi tungkol sa kung paano naging mas madaling maunawaan ang impormasyon para mas maraming tao ang gagamit ng contact tracing system. Kasama rito ang impormasyong makukuha sa iba't ibang wika na may kaugnayan sa mga lokal na konteksto sa pamamagitan ng isang call center na may mga tagasalin, at mga liham sa pamamagitan ng pinto upang ipaliwanag ang patnubay. Iminungkahi ng mga taong may kapansanan na maaaring magkaroon ng mas maraming paggamit ng mga video, visual at madaling basahin na mga format (halimbawa sa loob ng mga test kit). Iminungkahi rin ng mga nag-aambag na kinikilala bilang Bingi ang pagbibigay ng impormasyon sa Sign Language, upang matulungan ang audience na ito na mas maunawaan kung ano ang kinakailangan sa kanila upang sumunod sa system.
| “ | Pagdating mo sa test center, kailangan mong gawin ang pagsubok sa iyong sasakyan ngunit mayroon lamang espasyo upang ibaba ang bintana ng kaunti. Sa tingin ko ang isang benepisyo ay maaaring magkaroon ng isang QR code. Kaya, maaari kong gamitin ang aking telepono at makuha ang lahat ng mga tagubiling iyon kung paano gawin ang pagsubok mula sa isang QR code sa Sign Language, iyon ay kamangha-mangha."
– Bingi |
Ipinakita ng mga pinuno ng komunidad na maaari silang gumanap ng mas malaking papel sa pagpapalaganap ng impormasyon tungkol sa pagsubok, pagsubaybay at paghiwalay ng sistema sa kanilang mga komunidad, at pagsuporta sa pagsunod. Ito ay dahil nakita ng ilang grupo na mahirap maunawaan ang impormasyon tungkol sa test, trace at isolate system. Sa halip, madalas silang umasa sa word-of-mouth na impormasyon na kumakalat sa kanilang komunidad. Iminungkahi ng mga pinuno ng komunidad na pahalagahan nila ang higit pang talakayan at materyal tungkol sa kung paano gumagana ang sistema upang maipamahagi nila ang impormasyong ito nang tumpak at maiangkop ito nang naaangkop para sa kanilang mga lokal na komunidad. Ang ilang mga nag-ambag na ang unang wika ay hindi Ingles, at ang mga mula sa mga komunidad ng Gypsy at Traveler, ay nagsabi na mas pinahahalagahan nila ang mas praktikal na personal na suporta.
| “ | Kami ay nakahiwalay, at walang sinuman sa amin ang marunong bumasa at sumulat, hindi kami marunong bumasa o sumulat, walang talagang lumabas at nagpaliwanag sa amin, tulad ng isang health nurse, o isang taong mula sa propesyon sa kalusugan, ay lumabas at nakipag-usap sa amin, o isang pulong, isang malayo lamang. Hindi namin naintindihan.”
– Taong mula sa pinagmulang etniko ng Roma |
| “ | Hands on… suportahan iyon, oo, ito ang iyong ginagawa, ito ang iyong-, sa isang leaflet, kung paano mo gagawin ang lateral flow test. Lahat ng mga bagay na iyon, kung may dumating at nagpakita na ito ang ginagawa mo.”
– Taong ang unang wika ay hindi Ingles |
Accessibility para sa mga taong hindi kasama sa digital
Ang isang pangunahing tagapag-ambag ng pagpapabuti na iminungkahi ay ang higit na pagiging naa-access at inclusivity para sa mga matatandang tao at hindi kasama sa digital. Napagtanto nila na maraming tao ang hindi kasama sa paggamit ng app at mga online na bersyon (ng tracing system/ng test booking system) dahil sa kakulangan ng mga kasanayan o access sa digital na teknolohiya. Gusto sana nilang makakita ng higit pang mga opsyon na magagamit tulad ng mga call center sa telepono upang mag-book ng mga appointment, mga non-tech-based na sistema upang maghatid ng contact tracing at higit pa sa isang hyper local na tugon partikular na sa liblib o rural na lugar.
| “ | Sa tingin ko ang tanging bagay na sasabihin ko ay isang uri lamang, gawin itong mas madaling ma-access para sa mga matatanda. Hindi ko alam kung paano nila gagawin iyon. Sa tingin ko marami sa mga ito ay malinaw na magiging nauugnay sa smart phone at nauugnay sa app."
– Kontribyutor ng Every Story Matters |
Pagpapatupad at Pagsunod
Ang mga nag-aambag ay nagmuni-muni kung paano nila gustong makita ang isang mas mataas na antas ng pampublikong pagsunod sa pagsubok, pagsubaybay at paghihiwalay ng sistema upang matiyak na ito ay gumagana nang maayos. Kinikilala ng ilan na ito ay isang mahirap na bagay na makamit at maaaring umasa sa lawak kung saan naramdaman ng mga tao na konektado sa kanilang komunidad pati na rin ang kanilang pakiramdam ng responsibilidad sa isa't isa - at ang mga pananaw sa kung paano mas mahusay na naipapatupad ang pagsubok, pagsubaybay at paghihiwalay na sistema ay pinaghalo.
Narinig namin mula sa ilang kontribyutor na nagmungkahi ng mas mahigpit na pagpapatupad at mga parusa para sa hindi pagsunod, tulad ng mas malaking pagpupulis, mas mataas na multa, at mga sentensiya sa bilangguan. Gayunpaman, nagkaroon din ng pagkilala na ang mas mataas na mga parusa ay mahirap ipatupad, halimbawa ang pagkilala na ang mga bilangguan ay sobra na ang populasyon at ang mga tao ay maaaring hindi makabayad ng mas mataas na multa, at malamang na hindi epektibo bilang resulta.
| “ | Kung ang mga multa ay talagang mataas, ang mga tao ay magiging mas hilig na sumunod nang higit pa at kaya, ang pagpapatupad... Ang mga app na may bakas at contact ay naroon lahat, ngunit paano ito talagang ipinatupad? Sino ang talagang nagpapatupad ng mga patakarang iyon - at ano ang mga parusa?"
– Taong nagtatrabaho sa mga bata |
Mayroon ding mga mungkahi para sa paggalugad ng mga insentibo upang mapabuti ang pagsunod sa halip na magpataw ng mga parusa para sa hindi paglahok. Karaniwan, ang mga mungkahi ay nakatuon sa mga insentibo sa pananalapi.
| “ | …kung bibigyan mo sila ng insentibo na sundin ang panuntunan, mas malamang na gawin nila ito...kung nag-aalok ka ng tamang insentibo, sa palagay ko makukuha mo ang tamang resulta.”
– Tagapag-alaga |
Iminungkahi din ng ilang kontribyutor na maaaring magkaroon ng mas malaking pagsisikap na turuan ang publiko sa pangangailangan para sa test, trace at isolate system upang magkaroon ng mas malaking buy-in sa system na sa tingin nila ay nangangahulugan na mas maraming tao ang gagamit nito.
| “ | It's really educating them, just remind people, 'Tingnan mo, ganito ang nangyayari.' Tulad ng, mga nursing home at mga bagay, makikita mo ito sa telebisyon. Dapat kang [self-] ihiwalay dahil nakikitungo ka sa buhay ng mga tao. Kaya, magiging napakahalaga na sumunod sa lahat ng mga patakaran, na ginagawa ang mga patakaran, mga resulta, at pag-uusig upang subukang ilagay ang takot sa mga tao na may ganoong paraan."
– Taong nakakuha ng suporta sa kalusugan ng isip |
Mga pagpapabuti sa pagsubok
Karaniwang nadama ng mga kontribyutor na gumagana nang maayos ang mga proseso ng pagsubok. Ang malawak na magagamit at libreng mga pagsusuri ay nagbigay bigat sa kabigatan ng Covid-19 at pinahahalagahan.
Ang mga pagpapabuti sa elemento ng pagsubok ng system ay nakatuon sa paggawa ng mga pagsubok na mas malawak na magagamit at madaling ma-access. Ang isa sa kanilang mga mungkahi - para sa mga pagsubok na maihahatid sa bahay - ay magagamit na sa panahon ng pandemya. Isinasaad nito na maaaring magkaroon ng higit pang kakayahang magamit, o pag-promote ng paghahatid ng mga pagsubok sa mga tao sa bahay. Iminungkahi din ng mga nag-aambag na ang pagtatatag ng mas maliliit na sentro ng pagsubok sa mas maraming lokasyon, at samakatuwid ay mas malapit sa tahanan upang ang mga tao ay makapaglakbay ng mas maiikling distansya upang makakuha ng pagsusulit ay magiging kapaki-pakinabang.
Maraming nag-ambag ang natagpuan ang mga tagubilin para sa pagsubok na madaling maunawaan. Gayunpaman, mayroon ding mga mungkahi para sa kung paano sila mapapabuti: halimbawa, sa pamamagitan ng paggamit at pag-promote ng mga tagubilin sa larawan at video upang ipaliwanag kung paano pangasiwaan ang parehong mga pagsusuri sa PCR at LFT. Nadama ng mga nasa komunidad ng Bingi at mga taong hindi marunong magsalita ng Ingles na mapapabuti nito ang accessibility.
Mga pagpapabuti sa pagsubaybay sa contact
Kapag pinag-iisipan ang pagsubaybay sa contact, maraming nag-ambag ang nagsabi sa amin na ang ideya ay maganda sa prinsipyo, at ang system ay diretso - lalo na para sa mga komportable sa paggamit ng mga app at webpage. Gayunpaman, ang mga nag-aambag sa pangkalahatan ay nadama na sa pagsasagawa ng sistema ay hindi gumagana nang maayos. Ito ay higit sa lahat dahil sa isang pang-unawa ng hindi magandang pagsunod mula sa iba, kanilang sariling hindi pagsunod, at ang mga bahid sa sistema na kanilang naranasan (tinalakay kanina).
| “ | Ano ang silbi ng 10% ng populasyon na may app at nagbibigay ng tamang numero ng telepono at lahat ng bagay at sinabihan na [self-] ihiwalay, kapag marahil 90% ng mga tao ay hindi ginagawa iyon, kaya ito ay nasa loob o lahat. It becomes a bit of a nonsense otherwise, para sa akin.”
– Kontribyutor ng Every Story Matters |
Karamihan sa mga mungkahi para sa mga pagpapabuti ay nakatuon sa mga paraan upang matiyak na ang system ay mas partikular sa mga indibidwal na kaso. Halimbawa, gusto ng mga nag-aambag ng higit na kalinawan sa kung ano ang direkta at hindi direktang pakikipag-ugnayan upang makapagsagawa sila ng aksyon nang naaayon. Maaaring kabilang dito ang mabilis at tumpak na impormasyon tungkol sa oras at lokasyon ng isang contact na maaaring direktang i-link ng mga tao sa kung saan sila napunta at kung sino ang kanilang nakasama. Nadama nila na ito ay maghihikayat ng higit na pagtitiwala sa sistema.
| “ | Siguro kung ito ay isang sistema na may mga landas. Kaya, karaniwang lumabas ka sa iyong mga detalye, kung anong petsa ka nagkaroon ng positibong pagsubok at anuman. At ito ay nagtrabaho para sa iyo. Ito ay mas partikular sa iyong kaso kumpara sa pagiging blankong impormasyon lamang na ibinibigay nila doon at bukas sa maling interpretasyon."
– Taong nagtatrabaho sa pangangalagang pangkalusugan at panlipunan |
Mayroon ding ilang suhestyon para sa higit pang personalized na gabay na ibinigay kasama ng notification ng contact. Halimbawa, ang pagbibigay ng isang partikular na petsa kung kailan dapat huminto ang pag-iisa sa sarili, o ang patnubay na isinasaalang-alang ang kanilang katayuan sa pagbabakuna. Ang isa pang halimbawa ng naka-personalize na contact na ito ay ang pagkakaroon ng paraan upang makilala ang mga manggagawa sa front line, kaya hindi sila palaging inaabisuhan.
| “ | Sabihin nating mayroon ka ng app. Masama ka, nagkaroon ka ng positibong pagsubok. Pagkatapos ay sasabihin sa iyo ng app, 'Okay, kailangan mong [self-] ihiwalay hanggang sa ganitong tagal ng oras at subukang muli sa petsang ito, at ang impormasyong ito ay partikular sa iyo at sa iyo lamang.' Imbes na medyo hit and miss kung kailan magkatugma ang mga petsa.”
– Taong nagtatrabaho sa pangangalagang pangkalusugan at panlipunan |
Kasama sa iba pang mga suhestyon ang kakayahang pumili ng mga kagustuhan sa pakikipag-ugnayan, upang ang mga tao ay makapag-opt out sa mga malamig na tawag, halimbawa.
Mga pagpapabuti sa self-isolation
Sa pangkalahatan, ang paghihiwalay na bahagi ng system ay tiningnan ng mga kontribyutor kung kinakailangan upang limitahan ang pagkalat ng virus. Ang mga pagpapabuti sa self-isolation ay pangunahing nakatuon sa iba't ibang paraan ng pagbibigay ng suporta sa mga taong nagbubukod sa sarili.
Ang pangunahing priyoridad para sa maraming nag-aambag ay ang pagsuporta sa mga taong nag-iisa sa sarili sa mga epekto nito sa kanilang kalusugang pangkaisipan at pagkabalisa. Marami ang hindi nakapagbigay ng mga partikular na halimbawa kung anong mga pagpapabuti ang maaaring gawin sa paligid ng suporta sa kalusugan ng isip, ngunit gusto lang na makakita ng higit pang suporta lalo na para sa mga mahihinang indibidwal at sa mga namumuhay nang mag-isa, upang gawing mas madaling pamahalaan ang panahong ito. Ang mga gumawa ng mga mungkahi ay nagsabi na ang pagpapabuti ng access sa online na therapy o pag-check in sa mga tao (hal. sa telepono) habang sila ay nag-iisa sa sarili upang tumulong sa kalungkutan. Ang paggamit ng suportang nakabatay sa komunidad upang maabot ang mga taong nagbubukod sa sarili ay isang paraan na iminungkahi ng mga nag-aambag na ito ay maaaring makamit.
| “ | Sa palagay ko kung ang isang sitwasyong tulad nito ay paulit-ulit, kumatok sa kahoy na hindi, ngunit kung ito ay dapat magkaroon ng higit na priyoridad sa kalusugan ng isip, naniniwala ako, dahil sa tingin ko hindi lamang para sa aking sarili ngunit mula sa kung ano ang naiintindihan ko na ang kalusugan ng isip ay nasa lahat ng oras na mababa sa iba't ibang edad. Walang sapat na mapagkukunan.”
– Taong ang unang wika ay hindi Ingles |
Ang ilang mga nag-aambag ay gusto rin ng mas mahusay na tulong pinansyal para sa mga indibidwal na nangangailangan nito sa panahon ng pag-iisa sa sarili. Kasama rito ang tulong pinansyal sa mga taong hindi makapagtrabaho habang nag-iisa sa sarili at hindi nakakakuha ng sick-pay mula sa kanilang mga amo.
| “ | Sa palagay ko, kung kailangan mong [mag-isa], mababayaran ka pa rin, sa halip na – napakaraming tao sa industriya na walang sick pay, kaya kung kailangan mong [mag-isa] sa anumang dahilan, hindi sila binayaran sa loob ng dalawang linggo.
– Tagapag-alaga |
Iminungkahi din ng mga nag-aambag na ang pag-promote ng impormasyon tungkol sa kung anong suportang pinansyal ang magagamit at kung paano ma-access ang suportang ito ay maaaring maging mas mahusay – ito ay lalo na ang kaso para sa mga nag-ambag na ang unang wika ay hindi Ingles.
| “ | Para sa akin, [what could be improved] is more information, like proactive information, as you mention, the help with food, wala pa akong masyadong alam at yung support for financial support, I knew some people have but I never understand, never knew how they get it.”
– Taong ang unang wika ay hindi Ingles |
7. Apendise |
Module 7 pansamantalang saklaw
Ang pansamantalang saklaw ng Modyul 7 ay ginamit upang gabayan kung paano tayo nakikinig sa mga tao at sinuri ang kanilang mga kuwento.
Ang module na ito ay titingnan, at gagawa ng mga rekomendasyon sa, ang diskarte sa pagsubok, pagsubaybay at paghihiwalay na pinagtibay sa panahon ng pandemya sa England, Wales, Scotland at Northern Ireland mula Enero 2020 hanggang 28 Hunyo 2022. Kabilang dito ang Test and Protect (Scotland), Test and Trace (England), Test, Trace, Protect (Wales) at Test, Trace and Protect (Northern Ireland).
Isasaalang-alang ng module ang mga patakaran at estratehiya na binuo at ipinakalat upang suportahan ang pagsubok, pagsubaybay at paghihiwalay ng sistema ng gobyerno ng UK at ng mga devolved na administrasyon. Isasaalang-alang nito ang mga desisyong ginawa ng mga pangunahing katawan, iba pang mga opsyon o teknolohiya na magagamit at mga salik na maaaring nakaimpluwensya sa pagsunod ng publiko.
Sa partikular, susuriin ng modyul na ito ang:
- Ang pagsubok, pagsubaybay at paghihiwalay ng mga patakaran at estratehiya na binuo at inilagay, na isinasaalang-alang ang pagmomodelo, kapasidad ng mga sistema sa buong pandemya at ang katwiran, pagiging angkop at data na magagamit para sa mga desisyon ng UK at mga devolved na administrasyon at mas malawak na pagsasaalang-alang sa patakaran sa hangganan.
- Ang pagkakaroon, paggamit at pagiging epektibo ng iba't ibang pagsubok, pagsubaybay at paghihiwalay ng mga teknolohiya, mga patakaran at diskarte kabilang ang lateral flow at PCR (polymerase chain reaction) na mga pagsubok, pagsubok para sa mga variant, digital contact tracing at iba pang mga diskarte sa pagsubok.
- Ang istruktura ng test, trace at isolate system at ang mga pangunahing katawan na kasangkot sa paggawa ng desisyon sa UK at mga devolved na administrasyon. Isasama nito ang bisa at epekto ng mga modelong pinagtibay, ang paggamit ng pribadong sektor at iba pang institusyon at ang gastos.
- Pagpapatupad ng mga pamamaraan ng pagsubok, pagsubaybay at paghihiwalay at mga salik na nakakaimpluwensya sa pagsunod, tulad ng kasapatan at pagtitiwala sa pagmemensahe, pinansyal at praktikal na suporta sa mga kinakailangan upang ihiwalay ang sarili at ang pagkakaroon at paggamit ng data sa paggawa ng desisyon.
- Ang pangangalaga ng imprastraktura, kapasidad at pananaliksik upang mapabuti at bumuo ng pagsubok, pagsubaybay at paghiwalayin ang mga pamamaraan para sa mga pandemya sa hinaharap.
Kung paano ibinahagi ng mga tao ang kanilang kuwento sa amin
May tatlong magkakaibang paraan ng pagkolekta ng mga kuwento ng mga tao para sa Module 7:
Online na form
Ang mga miyembro ng publiko ay inanyayahan upang kumpletuhin ang isang online na form sa pamamagitan ng website ng Inquiry (Ang mga papel na form ay inaalok din sa mga kontribyutor at idinagdag sa pamamagitan ng online na form para sa pagsusuri). Hiniling nito sa kanila na sagutin ang tatlong malawak at bukas na mga tanong tungkol sa kanilang karanasan sa pandemya. Ang mga tanong na ito ay:
- Sabihin sa amin ang tungkol sa iyong karanasan
- Sabihin sa amin ang tungkol sa epekto sa iyo at sa mga tao sa paligid mo
- Sabihin sa amin kung ano sa tingin mo ang maaaring matutunan
Ang form ay nagtanong ng iba pang mga demograpikong tanong upang mangolekta ng background na impormasyon tungkol sa kanila (tulad ng kanilang edad, kasarian at etnisidad). Ang mga tugon sa online na form ay isinumite nang hindi nagpapakilala.
Sa likas na katangian nito, ang mga nag-ambag sa online na form ay ang mga piniling gawin ito, at ibinahagi lamang nila kung ano ang kanilang komportable.
Para sa Module 7, sinuri namin ang 44,775 na kwentong nauugnay sa pagsubok, trace at isolate system ng Covid-19. Kasama rito ang 36,879 na kuwento mula sa England, 3,665 mula sa Scotland, 3,783 mula sa Wales at 1,973 mula sa Northern Ireland (nakapili ang mga nag-aambag ng higit sa isang bansa sa UK sa online na form, kaya mas mataas ang kabuuan kaysa sa bilang ng mga natanggap na tugon).
Sinuri ang mga tugon sa pamamagitan ng natural language processing (NLP), na gumagamit ng machine learning para tumulong na ayusin ang data sa makabuluhang paraan. Ang isang kumbinasyon ng algorithmic analysis at pagsusuri ng tao ay pagkatapos ay ginagamit upang higit pang galugarin ang mga kuwento.
Tinutukoy ng pagsusuri ng NLP ang mga paulit-ulit na pattern ng wika sa loob ng data ng libreng text. Pagkatapos ay ipapangkat nito ang data na ito sa 'mga paksa' batay sa mga termino o pariralang karaniwang nauugnay sa paksang iyon (halimbawa, ang wikang ginagamit sa isang pangungusap tungkol sa pagkabalisa ay maaaring halos kapareho ng ginagamit kapag pinag-uusapan ang tungkol sa depresyon, na pinagsama-sama sa isang paksa sa kalusugan ng isip). Ito ay kilala bilang isang 'bottom-up' na diskarte sa text analytics dahil lumalapit ito sa data na walang preconceptions tungkol sa mga paksang nilalaman nito, sa halip ay nagbibigay-daan ito sa mga paksa na lumabas batay sa mga nilalaman ng teksto.
Pinili ang mga kwento para isama sa modelo ng paksa sa dalawang paraan. Una lahat ng mga tugon sa bawat tanong ay kinuha mula sa online na form at ang blangkong data ay inalis. Pangalawa, ang mga tugon ay na-filter batay sa kanilang kaugnayan sa Modyul 7.
Itinuring na may kaugnayan ang mga kuwento kung pinili ng mga nagbahagi ng mga ito ang alinman sa mga sagot sa ibaba sa tanong na 'Ano ang gusto mong sabihin sa amin?':
- Pamumuhay kasama ang Long Covid;
- Opisyal na impormasyon ng pamahalaan, halimbawa, payo sa pagbubukod ng sarili sa bahay
- Pagsusuri at pagbabakuna sa Covid-19;
- Mga serbisyong pangkalusugan, halimbawa ang NHS o HSCNI (Health and Social Care Northern Ireland), kabilang ang mga GP surgeries;
- Pangangalaga, halimbawa, mga tahanan ng pangangalaga o pangangalagang panlipunan;
- Araw-araw na buhay, halimbawa, pista opisyal, paglabas, pamimili o palakasan;
- Kalusugan ng isip, halimbawa, malungkot, galit, pagkabalisa o stress;
- Edukasyon, halimbawa paaralan o unibersidad;
- Ang pagkakaroon ng Covid-19; at
- Komunidad, halimbawa, mga kapitbahay o lugar ng pagawaan.
Kasunod ng pagkakakilanlan ng nauugnay na data, isang modelo ng paksa ang pinatakbo sa bawat tanong. Natukoy nito ang kabuuang 193 paksa sa lahat ng mga tugon sa Q1, 240 sa Q2, at 221 sa Q3. Dahil maaaring pumili ang mga nag-aambag ng maraming tugon sa tanong na 'Ano ang gusto mong sabihin sa amin?' posibleng ang mga sagot na pinili para sa pagsasama ay naglalaman ng data na hindi nauugnay sa Module 7. Dahil dito, kasunod ng paunang pagmomodelo ng paksa ay sinuri ng pangkat ng pananaliksik sa Ipsos ang lahat ng paksa para sa kaugnayan at inalis ang mga paksang hindi nauugnay sa Module 7 mula sa huling yugto ng pagsusuri. Nag-iwan ito ng kabuuang 57, 131 at 57 na paksa bawat tanong ayon sa pagkakabanggit. Nangangahulugan ito na 57 na paksa ang nasa loob ng 13 pangkalahatang tema. Upang ipakita ang mga temang ito, inilalarawan ang mga ito sa Appendix 1 sa ibaba.
Kasunod ng pag-alis ng mga paksang hindi nauugnay sa Module 7, isinagawa ang statistical factor analysis upang i-map ang mga ugnayan sa pagitan ng mga paksa at ipangkat ang mga ito batay sa mga terminong karaniwang nangyayari sa tabi o malapit sa isa't isa. Halimbawa, ang mga paksang nagsasalita tungkol sa kawalan ng tiwala sa gobyerno, kawalan ng tiwala sa media ay awtomatikong pinagsama sa isang kadahilanan tungkol sa kawalan ng tiwala sa mga pangunahing salaysay. Ang factor analysis ay gumawa ng 17 overarching factor sa 57 na paksang nauugnay sa Q1, 22 factor sa Q2, at 17 na salik sa Q3.
Kasunod ng pagmomodelo ng paksa at pagsusuri ng kadahilanan, nabuo ang isang codeframe batay sa mga paksang iyon na nauugnay sa Module 7. Kasangkot dito ang pagsusuri ng tao sa mga pinakakaraniwang salita at parirala, kapwa sa buong dataset at sa loob ng bawat paksa, upang matukoy ang mga keyword at pattern na maaaring magamit sa pagpangkat ng mga kuwento sa naaangkop na mga paksa at sub-paksa. Sa paggawa nito, binigyan nito ang pangkat ng pananaliksik ng mas tumpak na dami ng laki at mga elemento ng mga paksa, upang ipaalam ang diskarte sa pagsusuri.
Dahil mas maraming tao ang nagbahagi ng kanilang kuwento sa Pagtatanong sa pagitan ng pagmomodelo ng paksa at pagtutugma ng keyword, isang karagdagang hanay ng mga kuwento ang ibinigay sa Ipsos para sa huling yugto ng pagsusuri na ito. Sa kabuuan, 44,775 na kuwento ang isinama sa puntong ito, at hindi na na-filter ang mga ito ng tanong na 'Ano ang gusto mong sabihin sa amin?'. Ang desisyong ito ay ginawa upang matiyak na ang lahat ng nauugnay na kwento ay nakuha, batay sa mga salitang ginamit ng mga tao.
Pagkatapos ay sinuri ng mga mananaliksik ang iba't ibang paksang nauugnay sa Modyul 7 upang tuklasin ang mga kuwento. Pinagsama-sama ang mga ito sa mga kuwentong ibinahagi sa Inquiry sa ibang mga paraan (inilarawan sa ibaba) upang isama sa talaang ito.
Ipinapakita ng diagram sa ibaba ang mga tema na kasama sa online na form at ang dami ng beses na binanggit ng isang contributor ang bawat tema sa kanilang tugon. Ang laki ng bawat bloke ay kumakatawan sa dami ng mga tugon na nauugnay sa tema. Tandaan na ang mga nag-aambag ay maaaring nagbanggit ng maraming tema sa loob ng kanilang tugon at samakatuwid ay maaaring bilangin nang ilang beses.
Appendix 1: Mga tema ng NLP
Ang diagram ay naglalarawan kung aling mga nag-aambag ng pangkalahatang tema ang binanggit sa online na form at kung gaano kadalas lumabas ang mga tema. Ang mas malalaking bloke ay nangangahulugang binanggit ang isang tema ng mas maraming nag-aambag.
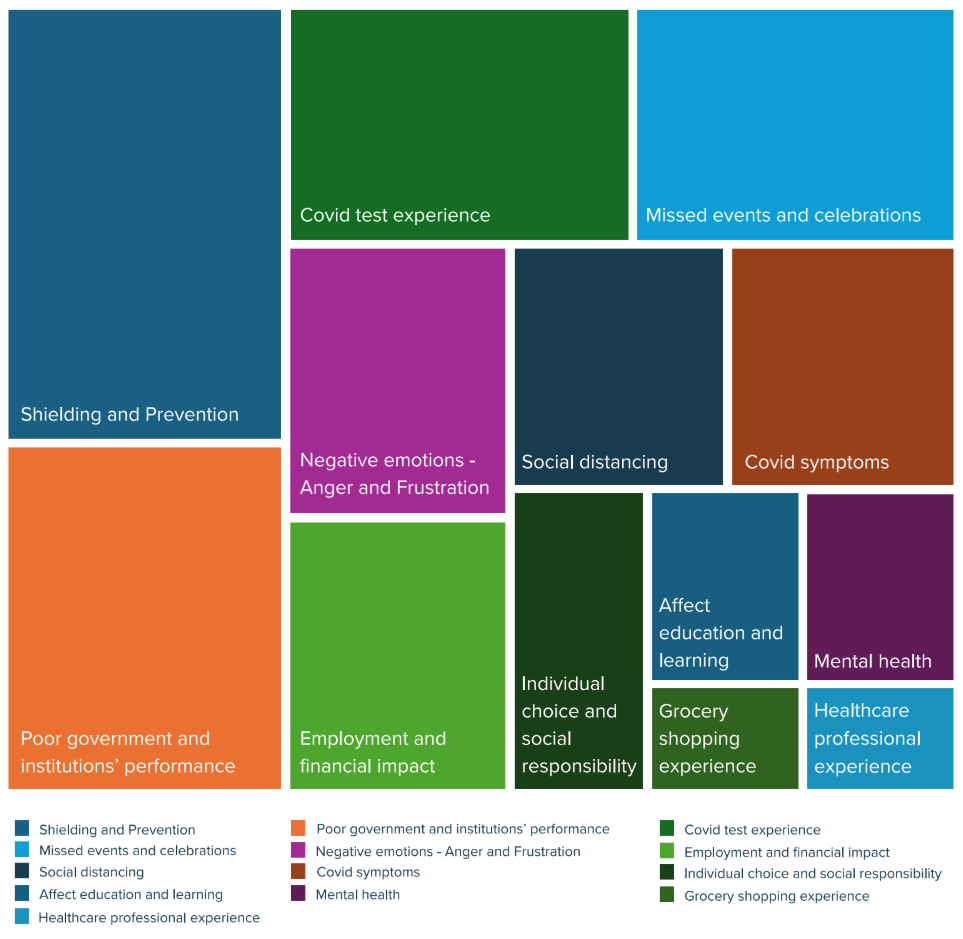
Mga kaganapan sa pakikinig
Sa oras ng pagsulat ng talaang ito, ang koponan ng Every Story Matters naglakbay sa 33 bayan at lungsod sa buong England, Wales, Scotland at Northern Ireland, upang bigyan ang mga tao ng pagkakataong ibahagi ang kanilang karanasan sa pandemya nang personal sa kanilang mga lokal na komunidad. Ang mga kaganapan sa pakikinig ay ginanap sa mga sumusunod na lokasyon:
- Belfast
- Birmingham
- Blackpool
- Bournemouth
- Bradford
- Brighton
- Nagtayo ng mga Wells
- Carlisle
- Cardiff
- Derry/ London Derry
- Edinburgh
- Enniskillen
- Exeter
- Folkestone
- Glasgow
- Inverness
- Ipswich
- Leicester
- Lisburn
- London
- Llandudno
- Luton
- Milton Keynes
- Middlesborough
- Newport
- Norwich
- Oban
- Paisley
- Preston
- Ruthin
- Skegness
- Stockton-on-Tees
- Wrexham
Idinaos din ang mga virtual na sesyon sa pakikinig kung saan mas gusto ang diskarteng iyon. Kabilang dito ang mga naulilang pamilya at indibidwal, mga taong nabubuhay kasama ang Long Covid, mga pamilyang may kapansanan sa klinika, mga taong may kapansanan, mga grupo ng kabataan, tagapag-alaga, mga refugee, mga taong mula sa mga etnikong minorya na pinagmulan at mga propesyonal sa pangangalagang pangkalusugan. Ang mga maikling buod na ulat para sa bawat kaganapan ay isinulat, ibinahagi sa mga kalahok ng kaganapan at ginamit upang ipaalam ang dokumentong ito.
Naka-target na pakikinig
Ang isang consortium ng mga social research at mga eksperto sa komunidad ay inatasan ng Every Story Matters na magsagawa ng malalim na mga panayam at mga grupo ng talakayan upang maunawaan ang mga karanasan ng mga partikular na grupo, katulad ng mga may partikular na kondisyon sa kalusugan na maaaring makaapekto sa kanilang kakayahang mag-self-isolate, kabilang ang mga pisikal at mental na kondisyon at kapansanan sa kalusugan, gayundin ang mga miyembro ng pamilya o mga tagasuporta ng mga kinakailangang mag-self-isolate, ang mga may malasakit na mga miyembro ng mga grupo ng komunidad na mag-set up ng sarili, at tumulong sa mga miyembro ng mga grupo ng komunidad na mag-isa. Ang mga panayam at mga grupo ng talakayan ay nakatuon sa Mga Pangunahing Linya ng Pagtatanong (KLOEs) para sa Module 7. Sa kabuuan, 340 katao sa buong England (160), Scotland (71), Wales (57) at Northern Ireland (52) ang nag-ambag sa ganitong paraan sa pagitan ng Hulyo at Oktubre 2024. Kabilang dito ang 217 malalim na panayam sa:
- Ang mga taong may partikular na kundisyon sa kalusugan na maaaring nakaapekto sa kanilang kakayahang sumubok o maghiwalay sa sarili, kabilang ang mga kondisyon at kapansanan sa kalusugan ng pisikal at mental.
- Ang mga miyembro ng pamilya o mga tagasuporta ng mga kinakailangang mag-self-isolate (lalo na ang mga sumusuporta sa mga matatandang tao, ang mga may dati nang kondisyong pangkalusugan, o ang mga clinically vulnerable o shielding).
- Mga taong may mga responsibilidad sa pangangalaga.
- Mga taong nakatira sa masikip o masikip na tirahan.
- Mga tao mula sa Gypsy, Roma at mga komunidad ng Manlalakbay at mga taong Nomadic.
Ang lahat ng mga malalim na panayam at mga grupo ng talakayan ay isinagawa ng mga sinanay na mananaliksik na sumunod sa isang gabay sa talakayan. Kung kinakailangan, susuriin ng mga mananaliksik ang mga nag-aambag para sa karagdagang impormasyon tungkol sa kanilang karanasan. Ang bawat panayam ay tumagal ng hanggang 60 minuto at ang lahat ng focus group ay tumagal ng hanggang 90 minuto. Ang mga panayam at gabay sa talakayan ay naitala, na-transcribe at na-code at sinuri sa pamamagitan ng pagsusuri ng tao upang matukoy ang mga pangunahing tema na nauugnay sa Module 7 Key Lines of Inquiry (KLOEs).
Binabalangkas ng mga talahanayan sa ibaba ang bilang ng mga panayam at mga grupo ng talakayan sa pangkalahatang publiko at sa mga taong hindi pantay na naapektuhan ng Covid-19 kaugnay ng Test, Trace at Isolate System.
| Uri ng kalahok | Nakumpleto ang mga panayam |
|---|---|
| Mga grupo ng talakayan | |
| Pangkalahatang publiko | 69 na kalahok sa 12 mga grupo ng talakayan |
| Mga taong nagtatrabaho sa mga setting ng pangangalagang pangkalusugan at panlipunan sa panahon ng pandemya | 20 kalahok sa 4 na grupo ng talakayan, kabilang ang 11 kalahok mula sa mga grupo ng etnikong minorya |
| Mga taong nagtatrabaho sa edukasyon o pangangalaga sa bata sa panahon ng pandemya | 22 kalahok sa 4 na grupo ng talakayan |
| Mga taong nagtatrabaho sa mga zero-hour na kontrata | 12 kalahok sa 2 grupo ng talakayan |
| Mga malalim na panayam | |
| Mga taong may kondisyon o kapansanan sa kalusugan | 70 |
| Mga taong may kahirapan sa wika at o literacy | 33 |
| Ang mga taong may mga responsibilidad sa pangangalaga at ang mga sumuporta at tumulong sa mga tao na ihiwalay ang sarili | 48 |
| Mga tao mula sa iba't ibang sambahayan | 66 |
| Kabuuan | 340 |
Appendix 2: Timeline stimulus na ginagamit sa discussion groups
Mga pangunahing kaganapan sa pagsubok sa Covid-19
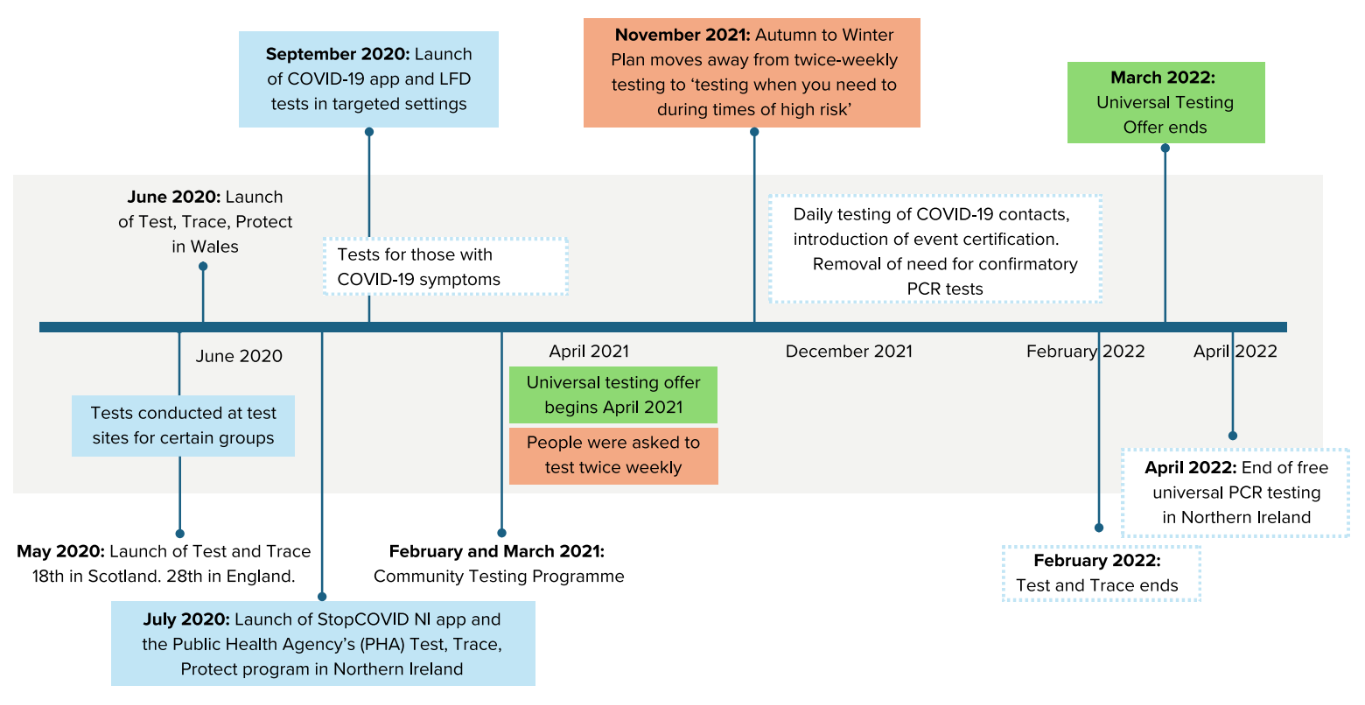
Mga alternatibong format
Available din ang tala na ito sa iba't ibang mga format.