Mae rhai o'r straeon a'r themâu sydd wedi'u cynnwys yn y cofnod hwn yn cynnwys disgrifiadau o farwolaeth, profiadau bron â bod yn farw, esgeulustod, gweithredoedd o hepgor a niwed corfforol a seicolegol sylweddol. Gall y rhain fod yn ofidus. Os felly, anogir darllenwyr i geisio cymorth gan gydweithwyr, ffrindiau, teulu, grwpiau cymorth neu weithwyr gofal iechyd proffesiynol lle bo angen. Darperir rhestr o wasanaethau cymorth ar wefan Ymchwiliad Covid-19 y DU.
Rhagair
Dyma bedwerydd cofnod Every Story Matters ar gyfer Ymchwiliad Covid-19 y DU. Mae'n dwyn ynghyd y miloedd lawer o brofiadau a rannwyd gyda'r Ymchwiliad yn ymwneud â'i ymchwiliad i'r sector gofal.
Cyffyrddodd y pandemig â bywydau cynifer o bobl mewn gofal – y rhai sy'n derbyn gofal a chymorth, eu teuluoedd, gweithlu cartrefi gofal, gofalwyr cartref a gofalwyr di-dâl a oedd yn gofalu amdanynt. Ar draws y DU roedd profiadau'n amrywio. Mae'r cofnod hwn yn dwyn ynghyd y profiadau hynny, gan roi llais i'r rhai a fu fyw a gweithio drwyddo.
Clywsom am yr heriau dwfn a wynebodd pobl – teuluoedd wedi’u cadw ar wahân, staff gofal wedi’u hymestyn i’w terfynau ac anwyliaid yn marw mewn amgylchiadau torcalonnus. Siaradodd llawer o bobl am boen peidio â gallu dal llaw, rhannu cwtsh, neu ffarwelio’n iawn. I’r rhai a adawyd ar ôl, roedd y galar yn aml yn cael ei wneud yn anoddach gan y cyfyngiadau a oedd ar waith. Clywsom hefyd am garedigrwydd, ymroddiad ac eiliadau bach o gysur – y gweithlu gofal cymdeithasol, â thâl a heb dâl, yn gwneud popeth o fewn eu gallu i ddod â chysur pan oedd ei angen fwyaf.
Mae'r cofnod hwn yn sicrhau nad yw'r profiadau hyn yn cael eu hanghofio, gan anrhydeddu brwydrau a gwydnwch anhygoel y rhai mewn gofal, eu hanwyliaid a'r rhai a ofalodd amdanynt.
Rydym yn diolch yn fawr iawn i bawb sydd wedi cyfrannu eu profiadau, boed drwy'r ffurflen we, mewn digwyddiadau neu fel rhan o ymchwil wedi'i thargedu. Mae eich myfyrdodau wedi bod yn amhrisiadwy wrth lunio'r cofnod hwn ac rydym yn wirioneddol ddiolchgar am eich cefnogaeth.
Diolchiadau
Hoffai tîm Pob Stori’n Bwysig hefyd fynegi ei werthfawrogiad diffuant i’r holl sefydliadau a restrir isod am ein helpu i gasglu a deall llais a phrofiadau gofal aelodau eu cymunedau. Roedd eich cymorth yn amhrisiadwy i ni gyrraedd cymaint o gymunedau â phosibl. Diolch i chi am drefnu cyfleoedd i dîm Pob Stori’n Bwysig glywed profiadau’r rhai rydych chi’n gweithio gyda nhw naill ai’n bersonol yn eich cymunedau, yn eich cynadleddau, neu ar-lein.
Carers UK
Gofalwyr yr Alban
Gofalwyr Cymru
Gofalwyr Gogledd Iwerddon
Cynghrair Cymdeithas Gofal
Preswylwyr a staff yng nghartrefi nyrsio a gofal Priory
Cymorth i Ofalwyr Caerliwelydd ac Eden
Ymddiriedolaeth Dementia
Ail-ymgysylltu
Cynghrair Darparwyr Gofal
Cymdeithas Gofal Genedlaethol
Ymddiriedolaeth Gofalwyr
Angor
Gofal Cysegr
Hosbis y DU
Rhwydwaith Menywod Mwslimaidd y DU
Cartrefi Methodistaidd (MHA)
Trosolwg
Sut y dadansoddwyd straeon
Mae pob stori a rennir gyda'r Ymchwiliad yn cael ei dadansoddi a bydd yn cyfrannu at un neu fwy o ddogfennau thema fel hon. Cyflwynir y cofnodion hyn o Mae Pob Stori'n Bwysig i'r Ymchwiliad fel tystiolaeth. Mae hyn yn golygu y bydd canfyddiadau ac argymhellion yr Ymchwiliad yn cael eu llywio gan brofiadau'r rhai yr effeithiwyd arnynt gan y pandemig.
Mae'r straeon a ddisgrifiodd brofiadau gofal cymdeithasol i oedolion yn ystod y pandemig wedi'u dwyn ynghyd a'u dadansoddi i amlygu themâu allweddol. Mae'r dulliau a ddefnyddiwyd i archwilio straeon sy'n berthnasol i'r modiwl hwn yn cynnwys:
- Dadansoddi 46,485 o straeon a gyflwynwyd ar-lein i'r Ymchwiliad, gan ddefnyddio cymysgedd o brosesu iaith naturiol (NLP) ac ymchwilwyr yn adolygu a chatalogio'r hyn y mae pobl wedi'i rannu. (Gweler tudalennau 26 a 27 am esboniad pellach o NLP)
- Ymchwilwyr yn tynnu ynghyd themâu o 336 o gyfweliadau ymchwil gyda'r rhai a oedd yn ymwneud â gofal cymdeithasol i oedolion yn ystod y pandemig. Roedd y rhai a gyfwelwyd yn cynnwys: pobl ag anghenion gofal a chymorth, eu hanwyliaid, gofalwyr di-dâl a gweithwyr gofal cymdeithasol proffesiynol.
- Ymchwilwyr yn tynnu ynghyd themâu a godwyd gan y cyhoedd a grwpiau cymunedol a gymerodd ran mewn digwyddiadau gwrando Mae Pob Stori yn Bwysig ledled Lloegr, yr Alban, Cymru a Gogledd Iwerddon. Mae rhagor o wybodaeth am y sefydliadau y bu’r Ymchwiliad yn gweithio gyda nhw i drefnu’r digwyddiadau gwrando hyn wedi’i chynnwys yn adran gydnabyddiaeth y cofnod hwn.
Mae rhagor o fanylion am sut y daethpwyd â straeon pobl ynghyd a'u dadansoddi yn y cofnod hwn wedi'u cynnwys yn y Cyflwyniad ac yn yr Atodiad. Mae'r ddogfen yn adlewyrchu gwahanol brofiadau heb geisio eu cymodi, gan ein bod yn cydnabod bod profiad pawb yn unigryw.
Drwy gydol y cofnod, rydym wedi cyfeirio at bobl sy'n rhannu eu straeon gyda Every Story Matters yn y ffyrdd a ddisgrifiwyd uchod fel 'cyfranwyr'. Mae cyfranwyr wedi chwarae rhan bwysig wrth ychwanegu at dystiolaeth yr Ymchwiliad ac at gofnod swyddogol y pandemig. Lle bo'n briodol, rydym hefyd wedi disgrifio mwy amdanynt (er enghraifft, gwahanol fathau o staff sy'n gweithio ym maes gofal cymdeithasol) neu'r rheswm pam y gwnaethon nhw rannu eu stori (er enghraifft, fel person ag anghenion gofal a chymorth neu fel gofalwr di-dâl). Mae'r tabl isod yn amlinellu'r gwahanol ymadroddion ac iaith a ddefnyddiwn drwy gydol y cofnod i ddisgrifio grwpiau allweddol.
| Ymadrodd | Diffiniad |
|---|---|
| Gweithiwr gofal cymdeithasol proffesiynol | Mae hwn yn derm cyffredinol ar gyfer y rhai sy'n gweithio ym maes gofal cymdeithasol, gan gynnwys gweithwyr gofal, rheolwyr cofrestredig (cartrefi gofal a darparwyr gofal cartref) a gweithwyr gofal cymdeithasol proffesiynol eraill, fel gweithwyr cymdeithasol. |
| Gweithwyr gofal | Mae hyn yn cynnwys y rhai sy'n gweithio mewn cartref gofal preswyl a gweithwyr gofal cartref sy'n darparu gofal a chymorth â thâl yng nghartref person ei hun. |
| Gofalwr di-dâl | Defnyddir y term hwn i ddisgrifio aelodau o'r teulu a ffrindiau sy'n darparu gofal a chymorth mewn rhinwedd bersonol yn hytrach na phroffesiynol, heb dderbyn iawndal ariannol. |
| Person ag anghenion gofal a chymorth | Rhywun sydd angen cymorth gyda bywyd bob dydd, a allai gynnwys cymorth gan ofalwyr di-dâl neu weithwyr gofal cartref gartref neu gan staff mewn cartref gofal. |
Y straeon a rannwyd gan bobl am ofal cymdeithasol yn ystod y pandemig
Cafodd y pandemig effaith ddinistriol ar y rhai ag anghenion gofal, eu teuluoedd a gofalwyr di-dâl a gweithwyr gofal cymdeithasol proffesiynol.
Disgrifiodd y rhai a oedd ag anwylyd ag anghenion gofal a chymorth a fu farw yn ystod y pandemig y trawma gwaethygol o beidio â gallu bod gyda'u hanwyliaid cyn a phan fyddant yn marw a pheidio â gallu galaru'n iawn drostynt. Disgrifiodd gweithwyr gofal cymdeithasol yr ofid o gefnogi pobl ar ddiwedd eu hoes a sefyll i mewn yn effeithiol dros deuluoedd y rhai sy'n marw.
Roedd unigrwydd, pryder, gofid a hwyliau isel yn gyffredin. Arweiniodd cyfyngiadau symud a chyfyngiadau ymweld at fwy o unigedd a gofid i bobl ag anghenion gofal a chymorth. Rhoddodd hyn bwysau enfawr ar anwyliaid, gofalwyr di-dâl a gweithwyr gofal cymdeithasol proffesiynol a chymerodd ei doll ar eu hiechyd meddwl a'u lles.
Cynyddodd y pwysau hwnnw ymhellach pan gafodd pobl eu rhyddhau o ysbytai i gartrefi gofal â staff cynyddol brin heb brofion Covid-19 neu gyda chanlyniadau profion anghywir neu hen ffasiwn.
Fodd bynnag, clywsom hefyd straeon cadarnhaol am sut y daeth cymunedau, ffrindiau a theulu at ei gilydd i gefnogi'r rhai mewn angen, gyda pherthnasoedd yn aml yn cryfhau o ganlyniad. Teimlai rhai cyfranwyr eu bod wedi'u hamddiffyn rhag y pandemig a chydnabu'r gofal rhagorol a gawsant mewn sefyllfaoedd heriol.
Effaith y pandemig ar ofal cymdeithasol
Cloeon a chyfyngiadau ar leoliadau gofal
Roedd llawer o bobl ag anghenion gofal a chymorth, eu hanwyliaid a gweithwyr gofal cymdeithasol proffesiynol yn teimlo bod y cyfyngiadau symud a'r mesurau cadw pellter cymdeithasol yn straen ac yn llethol. I bobl ag anghenion gofal a chymorth oedd yn byw gartref, roedd y cyfyngiadau symud yn arwain at deimladau o unigrwydd ac arwahanrwydd. Yn aml, roedd cyfyngiadau symud a chyfyngiadau yn golygu nad oeddent yn gallu cael mynediad at y gofal a'r cymorth oedd eu hangen arnynt, boed hyn gan anwyliaid neu weithwyr gofal cymdeithasol proffesiynol.
| “ | Doeddwn i a fy ngofalwr di-dâl ddim yn gallu gweld pobl eraill … Dw i'n meddwl bod fy mhoen a phethau fel hyn wedi gwaethygu, fel poen yn fy nghymalau, oherwydd fy mod i'n symud o gwmpas llai… Doeddwn i ddim yn gallu mynd i'm apwyntiadau ffisiotherapi chwaith ac nid oedd mynediad at apwyntiadau ar-lein. Felly, roedd hynny wedi dod i ben yn llwyr…roedd hynny'n ddrwg iawn.”
- Person ag anghenion gofal a chymorth, Lloegr |
Roedd teulu a ffrindiau’n teimlo pwysau ychwanegol i ddarparu gofal di-dâl oherwydd cyfyngiadau’r cyfnod clo. Roedden nhw’n ei chael hi’n anodd gwybod sut i ddarparu’r gofal cywir neu sut i gael mynediad at wasanaethau gofal a chymorth. Roedd eu cyfrifoldebau gofalu’n aml yn cynyddu, ac roedd hyn yn arwain at straen a phryder gyda llawer yn ansicr sut i ymdopi.
| “ | Roedd gan fy mam-gu ddementia, felly cyn i ni i gyd fod yn gofalu amdani…ond wedyn doedd neb yn cael ymweld â'i gilydd…dechreuodd hi fynd yn rhyfedd a dim ond fi a hi oedd yna…Roeddwn i'n arfer ei helpu i fwyta, ei brecwast, ei chinio, ceisio rhoi bath iddi, cael hi i sefyll i fyny a hyd yn oed fel yn yr ardd, ceisio gwneud iddi gerdded ychydig…weithiau, roedd yn mynd yn ormod, roedd yn mynd yn ormod [i fy iechyd meddwl].”
– Gofalwr di-dâl, Lloegr |
| “ | Penderfynon ni na allem adael i [fy nhad] fynd i'r ysbyty. Felly, fe wnaethon ni, fy chwaer a minnau, wneud gofal personol…y glanhawr oedd gan fy rhieni, roedd hi hefyd wedi bod yn ofalwr, a dysgodd hi i ni sut i wneud hynny.”
– Gofalwr di-dâl, Lloegr |
| “ | Yn sydyn, yn ystod Covid, doedd dim amser i ddianc i amgylchedd lle gallech chi fod yn chi'ch hun neu gyda phobl eraill sydd â phrofiadau tebyg, neu efallai dim ond cymryd amser i ffwrdd. Felly, roeddech chi'n gofalu am bobl yn gyson 24 awr a llai amdanoch chi'ch hun. Felly, roedd yn bryder ac yn anobaith eithafol.
– Gofalwr di-dâl, Lloegr |
Roedd cyfyngiadau ymweld hefyd yn anodd i deuluoedd a ffrindiau. Roeddent am sicrhau bod pobl ag anghenion gofal a chymorth yn ddiogel ac yn cael gofal priodol. Dywedodd cyfranwyr wrthym sut roeddent yn gwerthfawrogi ymweliadau ffenestr, galwadau ffôn a fideo ac, yn ddiweddarach yn y pandemig, ymweliadau â phellter cymdeithasol. Fodd bynnag, nid oedd hyn yn gwneud iawn am y diffyg cyswllt personol agos, yn enwedig gallu cyffwrdd yn gorfforol, cysuro a chofleidio'r rhai yr oeddent yn gofalu amdanynt.
| “ | Felly, ar un pen [o'r bwrdd] roedd fy mam, yn ei chôt yn ei chadair olwyn, ac roeddwn i ar y pen arall, rhyw fath, 6 neu 8 troedfedd i ffwrdd ac roedd yn ymweliadau 'carchar'…Rwy'n bloeddio arni o ben arall bwrdd hir…o flaen gofalwyr sydd fel gwarchodwyr ac roeddech chi eisiau dweud, 'Rwyf eisiau rhywfaint o breifatrwydd.' Doedd hi ddim yn gallu deall pam ar y ddaear nad oeddwn i'n eistedd gyda hi. Roedd yn eithaf gofidus mewn gwirionedd, ein bod ni'n cael ein trin fel 'na, roedd yn arfer fy ngwneud yn ddig iawn.”
– Anwylyd preswylydd cartref gofal, Lloegr |
Dywedodd rhai gweithwyr gofal cymdeithasol proffesiynol fod y gallu i barhau i weithio yn ystod y cyfnod clo wedi rhoi ymdeimlad o normalrwydd iddynt. Roedd llawer o rai eraill yn teimlo'n ynysig ac wedi'u llethu. Roedd rhaid i staff weithio dan bwysau difrifol i reoli gofynion cystadleuol darparu gofal, gyda llwyth gwaith uwch a llai o gefnogaeth dros fisoedd lawer. Symudodd rhai staff cartrefi gofal i'w gweithleoedd i amddiffyn preswylwyr a'u teuluoedd eu hunain. Treuliasant gyfnodau hir i ffwrdd oddi wrth anwyliaid. Arweiniodd hyn at deimladau o unigrwydd, blinder a gofid. Roedd y cyfyngiadau ar ymweliadau â chartrefi gofal hefyd yn rhoi pwysau a chyfrifoldeb ychwanegol ar staff, a oedd weithiau'n gorfod cymryd lle'r teulu wrth ofalu am breswylwyr.
| “ | Daethom yn fwy na dim ond gofalwyr y preswylwyr; tyfodd ein perthynas â nhw yn ystod y cyfnod hwnnw, daethom yn deulu iddyn nhw pan nad oedd eu plant eu hunain yn cael ymweld mwyach. Roedden ni'n eu caru nhw, fel ein rhai ni. Ni oedd yr unig bobl roedden nhw'n eu gweld bob dydd a daeth yn norm iddyn nhw.”
– Gweithiwr cartref gofal, Gogledd Iwerddon |
Cafodd pobl sy'n derbyn gofal cartref ymweliadau byrrach a llai aml wrth i wasanaethau gofal gael eu tarfu gan gyfnodau clo a phellhau cymdeithasol. Dywedodd gweithwyr gofal fod hyn yn lleihau cysondeb ac ansawdd y gofal y gallent ei ddarparu. Roedd staff hefyd yn ei chael hi'n anodd cefnogi pobl ag anghenion gofal cynyddol. Yn aml, gweithwyr gofal oedd yr unig bobl yr oeddent mewn cysylltiad â nhw yn ystod y cyfnodau clo.
| “ | Dim oedi, dim sgwrsio, dim gormod ar ôl i'r gofal hanfodol gael ei ddarparu; dim ond symud ymlaen i'r un nesaf oedd hi. Ie, roedd yn eithaf cyfyngedig…lle byddwn i fel arfer yn treulio awr a chwarter gydag un fenyw, efallai fy mod i wedi bod yno am 45 munud yn unig, felly ie, roedd yn anodd… roedd yn eithaf creulon ar y bobl agored i niwed roeddwn i'n darparu gofal iddyn nhw.”
– Gweithiwr gofal cartref, Cymru |
Roedd llawer o bobl ag anghenion gofal a chymorth yn cael trafferth ymdopi ag effaith llai o gyswllt cymdeithasol ac unigedd cynyddol. Roedd rhai yn datgysylltu'n emosiynol oddi wrth deulu a ffrindiau, tra bod eraill yn rhoi'r gorau i fwyta digon gan eu bod yn teimlo'n bryderus ac yn isel eu hysbryd.
| “ | Doedd hi ddim yn gallu deall pam mai dim ond drwy’r ffenestr y gallai fy ngweld…roedd hi’n rhoi’r gorau i fwyta oherwydd ei bod hi’n teimlo’n isel ei hysbryd gan fywyd heb ymwelwyr, ac ymweliadau gofal byr iawn gan y staff.”
– Aelod o deulu galarus preswylydd cartref gofal, yr Alban |
Clywsom hefyd sut y dechreuodd pobl ag anghenion gofal a chymorth ymddwyn mewn ffyrdd yr oedd gweithwyr proffesiynol teulu a gofal cymdeithasol yn eu cael yn heriol. Effeithiodd hyn yn arbennig ar bobl â dementia neu anabledd dysgu a phobl awtistig.
| “ | Roeddwn i'n gweithio mewn [cartref gofal]. Gwelais oedolion ag anableddau dysgu heb ddeall yn llawn pam roedd eu bywydau beunyddiol wedi newid, a oedd yn golygu bod staff wedi gweld ac wedi profi mwy a mwy o achosion o ymddygiad heriol ... cynyddodd ymosodiadau staff.”
– Gweithiwr cartref gofal, yr Alban |
| “ | Rwy'n gweithio mewn cartref gofal sy'n cefnogi oedolion ag anableddau dysgu. Cymerodd yr effaith ar y preswylwyr o gael eu hamddifadu o ymweliadau priodol gan eu teulu sawl ffurf: ymddygiad heriol, mynd yn encilgar… daeth preswylwyr a oedd fel arfer yn gymwynasgar iawn yn ddiog ac yn hwyliau mawr, daeth eu cyswllt â theuluoedd [ar y ffôn neu drwy alwad fideo] yn sbardunau [ar gyfer ymddygiad heriol].”
– Gweithiwr cartref gofal, yr Alban |
Roedd pobl ag anghenion gofal a chymorth hefyd yn ei chael hi'n anodd dychwelyd i'w gweithgareddau blaenorol a'u lefel o annibyniaeth ar ôl i'r cyfyngiadau gael eu llacio. Rhannodd llawer sut y gwnaethon nhw golli hyder ac maen nhw wedi parhau i fod yn encilgar.
| “ | Mae [y pandemig] wedi fy ngadael heb hyder… Doeddwn i ddim yn gallu, rhyw fath, cymysgu ac allwn i ddim mynd allan yn chwerthin a mwynhau fy hun. Roedd yn ddrwg iawn. Wyddoch chi, roeddwn i'n teimlo [fel] carcharor. Roeddwn i'n ei gasáu. Dioddefodd fy iechyd corfforol yn fawr oherwydd nad oeddwn i'n gwneud dim… a dydw i ddim wedi gallu ei gael yn ôl. Rwy'n ofalus ac yn bryderus iawn nawr.”
– Person ag anghenion gofal a chymorth, Cymru |
Rhyddhau o ysbytai i gartrefi gofal
Clywsom sut roedd cartrefi gofal yn aml yn derbyn preswylwyr newydd neu breswylwyr presennol yn cael eu rhyddhau o ysbytai heb rybudd digonol, gyda gwybodaeth gyfyngedig am eu cyflwr neu heb unrhyw brofion Covid-19 cywir neu ddiweddar. Creodd hyn heriau sylweddol i gartrefi gofal. Rhoddodd straen ar staff oherwydd y llwyth gwaith ychwanegol a'r ansicrwydd a theimlwyd ei fod yn cynyddu'r risg o Covid-19 yn lledaenu.
| “ | Dechreuon ni gael preswylwyr pan fydden nhw'n mynd i'r ysbyty, roedden nhw'n cael eu hanfon yn ôl i'r cartref gofal yn gyflym heb gynllun rhyddhau cadarn mewn gwirionedd. Ac yna digwyddodd bod pobl oedd yn cael eu hanfon yn ôl o'r ysbyty yn dod yn ôl gyda Covid ac yna, yn amlwg, byddai'n dechrau lledaenu. Ar y pryd, doedd dim canllaw o gwbl gan y llywodraeth, ddim yn swyddogol i ni a ddim hyd yn oed ar y teledu lle clywsom y rhan fwyaf o'r canllawiau. Doedd dim byd yna.”
– Nyrs yn gweithio mewn cartref gofal, Lloegr |
Rhannodd rhai cyfranwyr sut roeddent yn teimlo dan bwysau gan dimau rhyddhau ysbytai i dderbyn preswylwyr newydd o ysbytai er nad oedd ganddynt y wybodaeth na'r arbenigedd i ofalu amdanynt. Cododd hyn bryderon ynghylch diogelwch cleifion ac addasrwydd y gofal y gallent ei ddarparu.
| “ | Gofynnwyd i gartrefi gofal gymryd cleifion Covid o'r ysbyty i leihau'r pwysau ar wasanaethau acíwt. Yn lle hynny, gwrthodom, yn ystod y don gyntaf, gymryd preswylwyr newydd, er ein bod wedi ein rhoi dan bwysau i wneud hynny, gan gael gwybod mai 'ein dyletswydd foesol' oedd hi.”
– Rheolwr cofrestredig cartref gofal, Lloegr |
| “ | Ar y dechrau [rhyddhawyd pobl i gartrefi gofal] heb unrhyw brofion ar waith ac ar adegau hefyd heb unrhyw asesiad go iawn i benderfynu ar farn a dymuniadau'r bobl hŷn dan sylw. Roeddwn i'n teimlo bod hyn yn gyfaddawd enfawr ar fy ngwerthoedd moesegol. Roedd yn amlwg bod ysbytai'n cael eu llethu.”
– Gweithiwr cymdeithasol, yr Alban |
Fe greodd dyfodiad preswylwyr a brofodd yn bositif am Covid-19 yn fuan ar ôl eu rhyddhau ymdeimlad o gyfrifoldeb dros atal achosion ac amddiffyn preswylwyr a staff eraill. Rhannodd anwyliaid a gofalwyr di-dâl hefyd sut yr oeddent yn teimlo ymdeimlad o ofn a phanig pan glywsant am bobl a gafodd eu rhyddhau o'r ysbyty i'r cartref gofal yn profi'n bositif am Covid-19.
| “ | Dau berson a gafodd eu rhyddhau [o'r ysbyty yn ôl i'r cartref gofal, ar ôl profi] yn negatif. Ddeuddydd yn ddiweddarach, daeth i'r amlwg eu bod nhw'n dioddef o Covid. [Wrth glywed ei fod yn y cartref] roedd fel pe bai fy ofnau gwaethaf wedi dod i'r amlwg. Daliais i aros am yr alwad i ddweud bod ganddi Covid. Doeddwn i ddim yn gallu cysgu, doeddwn i ddim yn gallu bwyta - roedd yn artaith.”
– Anwylyd preswylydd cartref gofal, yr Alban |
Gofal diwedd oes a phrofedigaeth
Gwnaeth cyfyngiadau ymweld a mesurau rheoli heintiau Covid-19 eraill hi'n anodd iawn i anwyliaid ffarwelio â theulu neu ffrindiau ar ddiwedd eu hoes. Clywsom sut y bu farw pobl ag anghenion gofal a chymorth heb weld eu hanwyliaid oherwydd cyfyngiadau ymweld a oedd ar waith yn ystod y cyfnod clo cyntaf. Achosodd hyn alar a gofid aruthrol i aelodau'r teulu.
| “ | Wyddoch chi [pan oedd fy mam yn marw] byddwn i'n cael galwadau i ddweud bod hyn wedi digwydd neu hynny. Mae'n peri gofid. Mae'n dod â'r teimlad hwnnw o straen, am wn i, ond hefyd galar. Ac, am wn i, teimlad o unigedd, mewn gwirionedd, ynglŷn â... methu bod yno'n gorfforol na gwneud rhywbeth amdano. Diymadferthedd, dyna fyddai'r gair mewn gwirionedd. Diymadferthedd.”
– Aelod o’r teulu sydd wedi colli rhywun, Lloegr |
| “ | Doedden ni ddim yn gallu ei weld – wnaethon nhw byth ei weld eto. A phan fu farw, wrth gwrs, doedden ni ddim yn gallu mynd i angladd, doedden ni ddim yn gallu gwneud dim byd o gwbl. A dydw i ddim yn meddwl fy mod i erioed wedi teimlo mor annigonol.”
– Aelod o’r teulu sydd wedi colli rhywun, digwyddiad gwrando ar-lein |
Roedd pobl ar ddiwedd eu hoes a oedd yn cael gofal gartref gan ofalwyr di-dâl neu staff gofal cartref yn ei chael hi'n anodd cael gofal diwedd oes. Clywsom sut roedd yn rhaid i aelodau'r teulu ofalu amdanynt heb unrhyw gefnogaeth neu gymorth o bell yn unig gan weithwyr gofal iechyd a chymdeithasol proffesiynol. Roedd hyn yn rhoi cyfrifoldeb mawr ar anwyliaid.
| “ | Roedd [fy ngŵr] eisiau mynd i [gartref nyrsio] ac ni allent ei gymryd. [Felly fe wnaethon ni ofalu amdano gartref], nyrs neu feddyg gofal diwedd oes, dydw i ddim yn siŵr, yn ei ffonio bob pump neu chwe wythnos…y cyfan a wnaethon nhw, gyda phob problem fach oedd ganddo, bydden nhw'n archebu llwyth o gyffuriau. Doedden ni ddim yn hapus am hynny. Roeddwn i'n teimlo y gallai rhywun fod wedi dod i ymweld ag ef o ofal diwedd oes [a'n helpu ni].”
– Aelod o’r teulu sydd wedi colli rhywun, Lloegr |
Yn aml, roedd gweithwyr gofal yn cefnogi ac yn cysuro pobl wrth iddynt farw, gan nad oedd eu teulu a'u ffrindiau'n gallu ymweld. Rhannasant sut roeddent yn teimlo'n llethol ac yn cael y profiad yn heriol iawn. Dywedodd llawer wrthym sut roedd amlder marwolaethau, presenoldeb Offer Diogelu Personol (PPE) a'r cyfyngiadau ar ymweliadau teuluol yn gwneud i ofal diwedd oes deimlo'n amhersonol. Darparodd gweithwyr gofal ofal tosturiol pan oeddent eisoes dan bwysau difrifol a rhoddodd hyn doll emosiynol enfawr arnynt.
| “ | Roedd staff yn eistedd ar alwadau fideo gyda theuluoedd, yn ffarwelio â'u hanwyliaid am y tro olaf. Roedd hynny'n erchyll. Wyddoch chi, roedd staff yn crio gyda'r preswylwyr, oherwydd roedd mor emosiynol iddyn nhw. Roedden nhw'n dal eu dwylo nes iddyn nhw farw.”
– Gweithiwr cartref gofal, Gogledd Iwerddon |
| “ | Fe wnaethon ni wir geisio darparu'r gofal mwyaf tosturiol posibl… fe wnaethon ni barhau i ddarparu'r gofal proffesiynol oedd ei angen ac roedd yn fath cariadus o ofal…er gwaethaf yr holl heriau.”
– Gweithiwr cartref gofal, Lloegr |
Clywsom sut roedd rhai cartrefi gofal yn caniatáu i deulu a ffrindiau ymweld â'u hanwyliaid oedd yn marw hyd yn oed pan oedd cyfyngiadau ar waith. Roedd hyn yn cael ei werthfawrogi'n fawr gan anwyliaid ac roedd llawer yn cydnabod bod gweithwyr gofal yn gwneud eu gorau mewn sefyllfa anodd.
| “ | Byddaf yn ddiolchgar am byth i'r cartref gofal am ganiatáu inni gael yr amser byr hwnnw gyda [fy mam] ar ddiwedd ei hoes.”
– Aelod o’r teulu sydd wedi colli rhywun, Cymru |
Fodd bynnag, gadawyd llawer o anwyliaid ag atgofion poenus o frwydr a dioddefaint. Roeddent wedi’u difrodi’n llwyr na allent wneud mwy i helpu a chefnogi’r person yr oeddent yn gofalu amdano ar ddiwedd eu hoes.
| “ | Roedd fy mam mewn trallod mawr, mewn cyflwr ofnadwy, ac ni allent gael y mwgwd CPAP arni, felly es i mewn gyda PPE llawn ymlaen, gallwn ei chlywed yn sgrechian yn gofyn i'w mam ddod i'w chymryd i ffwrdd. Roedd hi'n gwthio ac yn ymladd, nid oedd hi'n wan. Ni allai glywed fy llais na gweld fy wyneb, roeddwn i eisiau eistedd a'i dal, ond ni chaniatawyd i mi. Ni allwn ei helpu, felly dywedwyd wrthyf fod yn rhaid i mi adael.”
– Aelod o’r teulu sydd wedi colli rhywun, digwyddiad gwrando, Gogledd Iwerddon |
Ar ôl y farwolaeth, effeithiodd cyfyngiadau ar baratoadau ar gyfer yr angladd a phwy allai fynychu. I bobl o grwpiau crefyddol a'r rhai o gefndiroedd lleiafrifoedd ethnig, effeithiodd hyn ar arferion ynghylch marwolaeth, megis paratoi'r corff a galaru am eu colled fel cymuned.
Cododd rhai anwyliaid a gweithwyr gofal cymdeithasol bryderon ynghylch y driniaeth a'r gofal a ddarperir i bobl ar ddiwedd oes. Rhannasant brofiadau o benderfyniadau triniaeth yn cael eu gwneud heb drafodaethau nac ymgynghori.
| “ | Am y pedair i bum wythnos [yn yr hosbis]…dywedwyd wrtha’i y byddai’n marw bob dydd. Tynnwyd y tiwb a’r IV allan a dydw i ddim yn gwybod pam eto. Yn y gwres ofnadwy, byddent yn cynnig dŵr oer iddo ac ni fyddent yn dod yn ôl. Ni allai fwyta na yfed, dim ond ei adael yn ei ystafell. Roedd yn ofnadwy.”
– Aelod o’r teulu sydd wedi colli rhywun, digwyddiad gwrando, Cymru |
| “ | Dywedais i roi hylifau iddo [pan wnaethon nhw ffonio i ddweud nad oedd e’n yfed llawer, sy’n gyffredin gyda dementia], ond roedden nhw wedi cael gwybod i beidio â rhoi hylifau iddo. Fe wnaethon nhw ei dynnu oddi ar ei feddyginiaeth teneuo gwaed – un o’r pethau allweddol a fe wnaethon nhw ei dynnu oddi ar y gwrthgeulydd, oddi ar ei glwt morffin a rhoi rhywbeth iddo ar gyfer cynhyrfu, dwi’n gwybod bod fy nhad yn gynhyrfus oherwydd ei fod yn ofnus, wedi’i adael gen i, roedd e wedi arfer â fi yno drwy’r amser.”
– Aelod o’r teulu sydd wedi colli rhywun, digwyddiad gwrando, Gogledd Iwerddon |
Roedd pryderon penodol ynghylch hysbysiadau Peidiwch â Cheisio Adfywio Cardiopwlmonaidd (DNACPR). Dywedodd rhai cyfranwyr wrthym am yr hyn yr oeddent yn credu oedd hysbysiadau DNACPR cyffredinol a osodwyd ar bobl oherwydd bod y person yn byw mewn cartref gofal neu ag anabledd dysgu. Achosodd y diffyg tryloywder a chyfranogiad yn y penderfyniadau hyn ofid ac ansicrwydd i deuluoedd.
| “ | Rhoddodd ein meddyg lleol waharddiad DNACPR cyffredinol ar ei holl gleifion i’w hatal rhag cymryd gwelyau yn yr ysbyty, rhywbeth a heriodd teuluoedd.”
– Gweithiwr cartref gofal, Cymru |
| “ | Gofynnodd y meddyg teulu am gael prawf DNACPR, roedd fy nhad yn gwybod am hyn a'r canlyniadau posibl, roedd eisiau byw, doedd e ddim eisiau un. Yna, darganfyddais fod y meddyg teulu wedi ymweld eto heb rybudd gyda chais DNACPR ac ni wnaethon nhw erioed sôn amdano wrtha i.”
– Aelod o’r teulu sydd wedi colli rhywun, digwyddiad gwrando, yr Alban |
| “ | Mae gen i anabledd…Rwy'n dal i gael fy ysgwyd i graidd fy modolaeth, eu bod nhw wedi gorfodi hysbysiadau 'Peidiwch ag Adfywio' ar y rhai ohonom sydd ag anabledd sylweddol neu dros oedran penodol.”
– Person ag anghenion gofal a chymorth, Cymru |
Dywedodd pobl ag anghenion gofal a chymorth a'r rhai oedd yn agored i niwed yn glinigol wrthym hefyd pa mor frawychus oedd sgyrsiau ynghylch diwedd oes a DNACPR.
| “ | Yn fuan ar ôl derbyn fy llythyr amddiffyn, cefais alwad ffôn gan fy meddygfa, a rhoddodd y galwad ffôn hon yr ofn mwyaf ynof hyd yma. Yn ystod y sgwrs gofynnwyd i mi a oeddwn wedi trafod fy nymuniadau diwedd oes gyda fy anwyliaid. Fel a oeddwn eisiau mynd i'r ysbyty neu aros gartref, a oeddwn wedi cael DNACPR. Gwnaeth hyn fy nychryn.”
– Person ag anghenion gofal a chymorth, yr Alban |
PPE a mesurau rheoli heintiau Covid-19
Roedd gweithwyr gofal cymdeithasol proffesiynol yn ddryslyd, dan straen ac yn ansicr ynghylch canllawiau sy'n newid yn aml ar Offer Diogelu Personol (PPE). Roedd yn rhaid i ddarparwyr gofal ailddefnyddio eitemau sengl, dogni cyflenwadau neu gaffael PPE o ysbytai, elusennau a sefydliadau neu fusnesau cymunedol eraill gan fod prinder PPE yn ystod camau cynnar y pandemig. Roedd darparwyr gofal yn bryderus ynghylch ansawdd ac addasrwydd PPE hyd yn oed wrth i'r pandemig fynd rhagddo a'r cyflenwad o PPE wella.
| “ | Y masgiau, ar un adeg pryd bynnag y byddech chi'n ceisio eu rhoi ymlaen, bydden nhw'n torri. Roedd y rheolwyr yn newid rhai gwahanol nes i ni gael yr un cywir.”
– Gweithiwr cartref gofal, Lloegr |
Roedd gweithwyr gofal cymdeithasol proffesiynol yn wynebu llwythi gwaith ac anghysur cynyddol wrth iddynt wisgo a thynnu PPE i ffwrdd yn gyson. Roedd protocolau glanhau a diheintio mwy trylwyr yn dwysáu'r pwysau ar y gweithlu ymhellach.
| “ | Byddem yn darganfod bod yn rhaid i ni wneud llawer mwy o waith oherwydd bod pobl yn ynysu…ni oedd yr unig bobl oedd yn mynd i mewn i weld pobl. Roeddem yn gweithio 16 awr y dydd… roedd [y PPE] yn cymryd llawer o amser ac yn sicr yn cymryd amser i ffwrdd o ochr gofal personol pethau.”
– Gweithiwr gofal cartref, Lloegr |
Roedd llawer o staff gofal cartref hefyd yn gweithio ar eu pennau eu hunain, gan ychwanegu at eu hynysu. Nid oeddent yn gallu cael cymorth gan gydweithwyr a rheolwyr eraill ynghylch PPE a heriau wrth ddarparu gofal.
Yn aml, byddai pobl ag anghenion gofal a chymorth, anwyliaid a gofalwyr di-dâl yn cael eu tawelu gan PPE. Fodd bynnag, roedd hefyd yn creu rhwystrau cyfathrebu. Roedd rhai pobl ag anghenion gofal a chymorth a gweithwyr gofal cymdeithasol proffesiynol yn ei chael hi'n anodd meithrin perthnasoedd. Roedd masgiau'n cuddio mynegiadau wyneb ac emosiynau, gan ei gwneud hi'n arbennig o anodd deall ciwiau di-eiriau.
| “ | Dim ond llygaid rhywun oeddech chi'n gallu eu gweld ac roeddwn i'n teimlo bod pobl yn llai agored pan nad oedden nhw'n gallu gweld eich wyneb. Roedd yn rhaid i chi geisio ymgysylltu â nhw'n fwy. Roedd hi'n anoddach ymgysylltu â phobl pan mae eich wyneb wedi'i orchuddio. Mae pobl yn fwy agored i chi pan allan nhw weld eich wyneb a dydych chi ddim yn hollol yn yr iwnifform honno.”
– Gweithiwr gofal iechyd, Lloegr |
I bobl oedd yn gofalu am unigolion oedd yn fyddar neu'n drwm eu clyw, roedd yr anallu i ddarllen gwefusau yn her sylweddol ac weithiau roedd yn rhaid i staff dynnu eu masgiau, gan gynyddu'r risg o drosglwyddo o bosibl. Clywsom hefyd sut roedd rhai pobl â dementia, unigolion ag anabledd dysgu a phobl awtistig hefyd yn cael PPE yn frawychus ac yn fygythiol. Mewn rhai achosion, arweiniodd hyn at ymddygiad heriol ac yn ei gwneud hi'n anoddach i ofalwyr di-dâl a gweithwyr gofal cymdeithasol proffesiynol ddarparu gofal.
Roedd cyfranwyr yn pryderu am y risgiau o ddal Covid-19 eu hunain neu ei drosglwyddo i aelodau o'r teulu, er gwaethaf y defnydd o PPE. Roedd aelodau o'r teulu a gweithwyr gofal cymdeithasol proffesiynol a oedd yn agored i niwed yn glinigol a phobl o gefndiroedd ethnig lleiafrifol yn arbennig o bryderus ynghylch dal Covid-19.
Prinder staff a sut y darparwyd gofal
Dywedodd cyfranwyr wrthym hefyd sut yr effeithiwyd ar y sector gofal cymdeithasol gan brinder staff difrifol drwy gydol y pandemig. I ddechrau, y rhesymau pam y gadawodd staff y gweithlu oedd yn bennaf oherwydd ofnau o haint, cyflyrau iechyd a oedd yn bodoli eisoes neu broblemau gofal plant yn gysylltiedig â chau ysgolion. Gostyngwyd argaeledd y gweithlu drwy gydol y pandemig ymhellach gan ofynion ynysu ar gyfer achosion positif o Covid-19.
| “ | Staff, gadawodd llawer o bobl oherwydd nad oedden nhw eisiau cael eu rhoi mewn perygl, a oedd wedyn yn golygu bod gennych chi fwy o rotas i'w gorchuddio, mwy o gwsmeriaid i'w gweld a llai o staff i'w defnyddio. Doedd y bobl ddim yn gallu gwisgo PPE, felly bydden nhw'n gadael, felly, unwaith eto, byddai gennych chi fwy o bethau i'w gorchuddio.”
– Gweithiwr gofal cartref, Lloegr |
O fis Tachwedd 2021 tan fis Mawrth 2022 roedd yn ofynnol i staff gofal yn Lloegr gael brechlyn Covid-19 er mwyn parhau i weithio, tra bod cyfranwyr yn yr Alban, Cymru a Gogledd Iwerddon wedi rhannu sut roedd disgwyliad cynyddol y byddent yn cael y brechlyn. Gadawodd rhai staff y gweithlu oherwydd bod cael y brechlyn yn erbyn eu credoau personol, tra bod gan eraill bryderon am sgîl-effeithiau posibl. Roedd y pryderon hyn yn effeithio'n arbennig ar bobl o gefndiroedd lleiafrifoedd ethnig. Clywsom hefyd sut roedd rhai pobl a oedd yn gweithio ar fisa iechyd a gofal, yr oedd eu preswylfa yn y DU yn dibynnu ar eu cyflogaeth, yn teimlo dan bwysau ychwanegol i gael y brechlyn gan eu bod yn poeni am effeithiau colli eu swydd.
| “ | Roedd gennym ni broblem; doedd cwpl o staff ddim eisiau cael brechlyn. Felly, dywedwyd wrthyn nhw fwy neu lai, 'Wel os nad ydych chi wedi cael eich brechlyn yna allwch chi ddim gweithio,' felly achosodd hynny gynhyrfusrwydd a dadleuon eraill.”
– Rheolwr cofrestredig cartref gofal, Lloegr |
Weithiau, roedd prinder staff yn arwain at berthnasoedd straen rhwng cydweithwyr wrth iddynt weithio o dan bwysau cynyddol ar sifftiau hirach gyda llwyth gwaith hyd yn oed yn fwy. Roedd prinder staff hefyd yn gadael darparwyr gofal yn ei chael hi'n anodd dod o hyd i adnoddau ar gyfer gwasanaethau ac i ofalu am bobl. Yn aml, roedd darparwyr gofal yn dibynnu ar staff asiantaeth i lenwi'r bylchau hyn. Yn aml, gweithwyr gofal dros dro oedd staff asiantaeth a oedd yn newid yn aml ac nad oeddent bob amser yn adnabod y bobl yr oeddent yn gofalu amdanynt, a oedd yn effeithio ar ansawdd y gofal a ddarparwyd.
| “ | Byddech chi'n cael staff asiantaeth. Maen nhw'n dda, ond dydyn nhw ddim yn rheolaidd. Dydyn nhw ddim yn adnabod y preswylwyr hyn cymaint. Ac maen nhw'n dod i mewn gyda'r ofn hwnnw, 'O, mae Covid yn y cartref hwn,' a dim ond y gofal sylfaenol [lefel y gofal] y byddan nhw'n ei wneud. Roedd y sefyllfa gyfan yn drychineb. Yn y rhan fwyaf o achosion, ni chafodd preswylwyr y gofal y dylen nhw ei gael.”
– Nyrs yn gweithio mewn cartref gofal, Lloegr |
Mynediad at wasanaethau gofal iechyd a phrofiad ohonynt
Clywsom sut y cafodd mynediad at wasanaethau gofal iechyd fel meddygon teulu, gwasanaethau cymunedol ac ysbytai ei leihau neu ei ohirio'n sylweddol yn ystod y pandemig. Dywedodd pobl ag anghenion gofal a chymorth wrthym sut y symudodd apwyntiadau i ymgynghoriadau ar-lein neu dros y ffôn, nad oeddent bob amser yn addas, yn enwedig i'r rhai ag anghenion cyfathrebu ychwanegol, pobl ag anabledd dysgu a'r rhai â dementia. Roedd mynediad at ofal iechyd brys hefyd yn heriol oherwydd pwysau cynyddol ar ysbytai ac ofnau o ddal Covid-19.
Disgrifiodd rhai gweithwyr gofal cymdeithasol proffesiynol enghreifftiau o rai gweithwyr gofal iechyd proffesiynol yn petrusgar neu'n methu ymweld â phobl yn bersonol oherwydd prinder staff. Arweiniodd hyn at lwyth gwaith cynyddol i staff gofal, a oedd yn gorfod hwyluso apwyntiadau rhithwir, dilyn triniaeth a chyngor a hyd yn oed ardystio marwolaethau.
| “ | Gofynnwyd i un o’n haelodau staff ardystio marwolaeth menyw drwy alwad ffôn. Ac roedd hi fel, ‘Dydw i ddim wedi cael hyfforddiant i wneud hynny.’ Mae hi ar y ffôn yn ffonio’r meddyg teulu wrth geisio cysuro’r teulu ac mae hi’n dweud, ‘Wel, gwaith y meddyg ydy o, nid fy un i’.”
– Rheolwr cofrestredig, Lloegr |
| “ | Roedd y baich yn drwm ar bob un ohonom oherwydd roedd hyd yn oed ceisio cael meddyg allan yn anodd iawn oherwydd eu bod nhw'n brin, felly'r effaith gynyddol o'r ysbyty, y meddygon, y meddygon teulu - pawb - daeth i lawr, wyddoch chi? Fel dominos.”
– Gweithiwr cartref gofal, Lloegr |
- Mae hysbysiadau DNACPR yn benderfyniadau a wneir naill ai gan y clinigwr (lle byddai adfywio cardiopwlmonaidd (CPR) yn aflwyddiannus a/neu heb fod er budd y claf) a/neu lle mae'r claf (gyda'r gallu) yn nodi y byddai'n well ganddo beidio â chael CPR. Felly, ni fydd CPR yn cael ei geisio pan fydd DNACPR ar waith os bydd claf yn cael ataliad ar y galon.
Cofnod llawn
1. Rhagymadrodd
Mae'r ddogfen hon yn cyflwyno'r straeon sy'n ymwneud â gofal cymdeithasol i oedolion yn ystod y pandemig sydd wedi'u rhannu gyda Every Story Matters.
Cefndir a nodau
Mae Every Story Matters yn gyfle i bobl ledled y DU rannu eu profiad o'r pandemig gydag Ymchwiliad Covid-19 y DU. Mae pob stori a rennir yn cael ei dadansoddi a'i throi'n gofnodion thema ar gyfer modiwlau perthnasol. Cyflwynir y cofnodion hyn i'r Ymchwiliad fel tystiolaeth. Wrth wneud hynny, bydd canfyddiadau ac argymhellion yr Ymchwiliad yn cael eu llywio gan brofiadau'r rhai yr effeithiwyd arnynt gan y pandemig.
Mae'r cofnod hwn yn adlewyrchu profiadau pobl ag anghenion gofal a chymorth (gan gynnwys y rhai sydd wedi marw), teulu a ffrindiau a ofalodd amdanynt a phobl sy'n gweithio ym maes gofal cymdeithasol.
Mae Ymchwiliad Covid-19 y DU yn ystyried gwahanol agweddau ar y pandemig a sut y gwnaeth effeithio ar bobl. Mae hyn yn golygu y bydd rhai pynciau'n cael eu trafod mewn cofnodion eraill o Every Story Matters. Er enghraifft, mae profiadau o ofal iechyd, y system brofi ac olrhain a'r effeithiau ar blant a phobl ifanc yn cael eu harchwilio mewn modiwlau eraill a byddant yn cael eu cynnwys mewn cofnodion eraill o Every Story Matters.
Sut mae pobl yn rhannu eu profiadau
Mae sawl ffordd wahanol rydyn ni wedi casglu straeon pobl ar gyfer Modiwl 6. Mae hyn yn cynnwys:
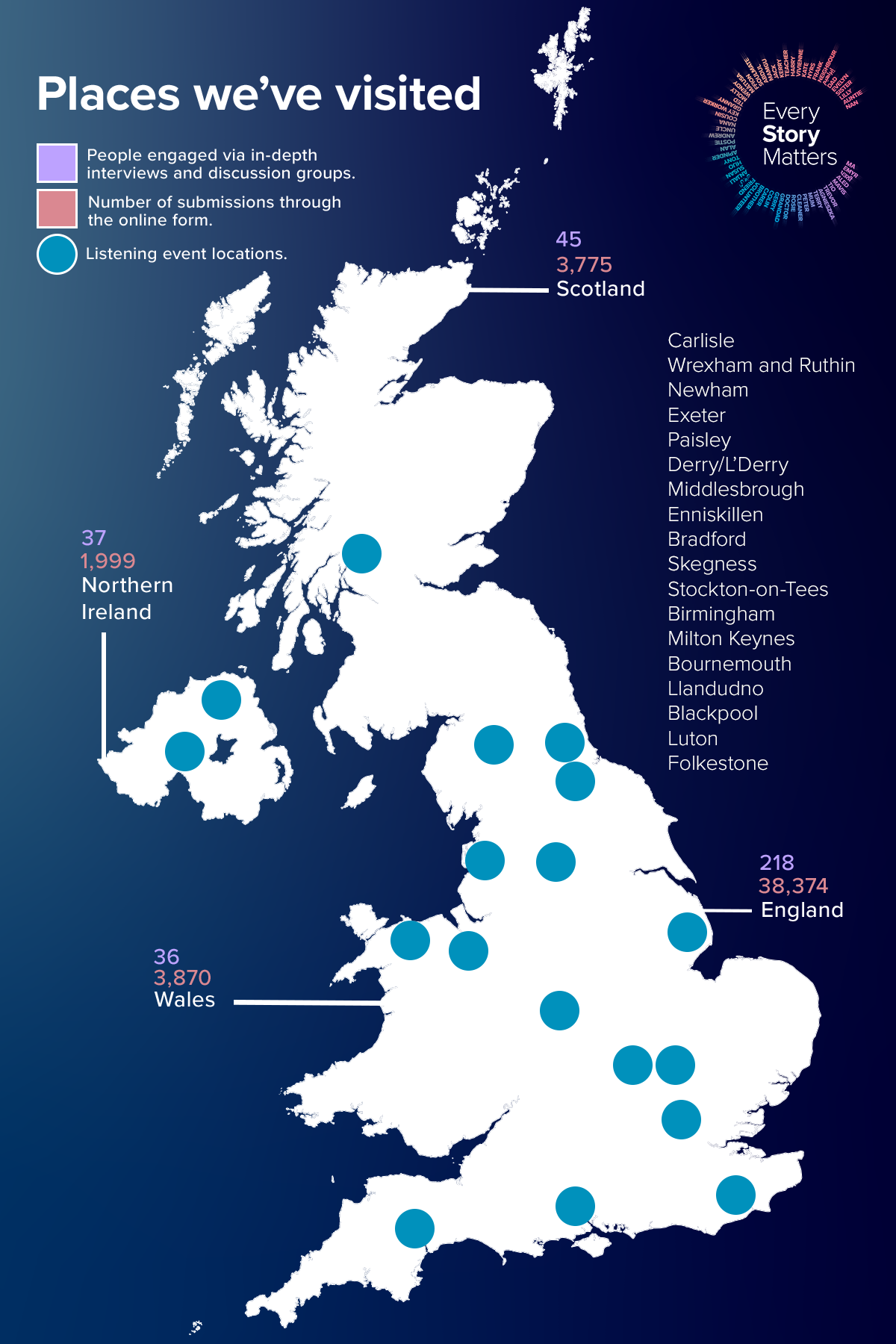
- Gwahoddwyd aelodau'r cyhoedd i gwblhau a ffurflen ar-lein drwy wefan yr Ymchwiliad (cynigiwyd ffurflenni papur i gyfranwyr hefyd a'u cynnwys yn y dadansoddiad). Gofynnodd hyn iddynt ateb tri chwestiwn eang, agored am eu profiad o’r pandemig. Gofynnodd y ffurflen gwestiynau eraill i gasglu gwybodaeth gefndirol amdanynt (megis eu hoedran, rhyw ac ethnigrwydd). Roedd hyn yn caniatáu inni glywed gan nifer fawr iawn o bobl am eu profiadau o’r pandemig. Cyflwynwyd yr ymatebion i’r ffurflen ar-lein yn ddienw. Ar gyfer Modiwl 6, dadansoddwyd 46,485 o straeon a oedd wedi dod i law erbyn i’r cofnod hwn gael ei baratoi. Roedd hyn yn cynnwys 38,374 o straeon o Loegr, 3,775 o’r Alban, 3,870 o Gymru ac 1,999 o Ogledd Iwerddon². Dadansoddwyd yr ymatebion drwy 'brosesu iaith naturiol' (NLP), sy'n helpu i drefnu'r data mewn ffordd ystyrlon. Drwy ddadansoddi algorithmig, trefnir y wybodaeth a gasglwyd yn 'bynciau' yn seiliedig ar dermau neu ymadroddion. Yna adolygwyd y pynciau hyn gan ymchwilwyr i archwilio'r straeon ymhellach (gweler yr Atodiad am fwy o fanylion). Defnyddiwyd y pynciau a'r straeon hyn wrth baratoi'r cofnod hwn.
- Aeth tîm Every Story Matters i 31 o drefi a dinasoedd ledled Lloegr, yr Alban, Cymru a Gogledd Iwerddon i roi cyfle i bobl rannu eu profiad o’r pandemig yn bersonol yn eu cymunedau lleol. Cynhaliwyd sesiynau gwrando rhithwir ar-lein hefyd, os oedd y dull hwnnw’n cael ei ffafrio. Buom yn gweithio gyda llawer o elusennau a grwpiau cymunedol ar lawr gwlad i siarad â’r rhai yr effeithiwyd arnynt gan y pandemig mewn ffyrdd penodol. Ysgrifennwyd adroddiadau crynodeb byr ar gyfer pob digwyddiad, rhannwyd hwy gyda chyfranogwyr y digwyddiad a’u defnyddio i lywio’r ddogfen hon. Ar gyfer y cofnod hwn am ofal cymdeithasol, cynhwyswyd cyfraniadau o 18 o’r digwyddiadau wyneb yn wyneb hyn, yn ogystal â digwyddiadau ar-lein ychwanegol.
- Comisiynwyd consortiwm o arbenigwyr ymchwil gymdeithasol a chymunedol gan Every Story Matters i gynnal cyfweliadau manwl i ddeall profiadau grwpiau penodol, yn seiliedig ar yr hyn yr oedd tîm cyfreithiol y modiwl eisiau ei ddeall. Cynhaliwyd cyfweliadau â phobl ag anghenion gofal a chymorth, y rhai sy'n darparu gofal a chymorth di-dâl (gan gynnwys anwyliaid, ffrindiau a theuluoedd sydd wedi colli rhywun) a'r rhai sy'n gweithio ym maes gofal cymdeithasol, boed yn darparu gofal cartref (gofal a ddarperir yng nghartref rhywun ei hun) neu'n gweithio mewn cartref gofal (gan gynnwys gweithwyr gofal iechyd proffesiynol a weithiodd yn agos gyda darparwyr gofal cymdeithasol). Canolbwyntiodd y cyfweliadau hyn ar y Prif Linellau Ymholi (KLOEs) ar gyfer Modiwl 6, y gellir eu canfod ymaAt ei gilydd, cyfrannodd 336 o bobl ledled Cymru, Lloegr, yr Alban a Gogledd Iwerddon yn y ffordd hon rhwng Mehefin a Hydref 2024. Cafodd yr holl gyfweliadau manwl eu recordio, eu trawsgrifio, eu codio a'u dadansoddi i nodi themâu allweddol sy'n berthnasol i Gyfweliadau Byw'n Deg Modiwl 6. Rhannodd y rhai a gymerodd ran eu profiadau eu hunain a myfyrio hefyd ar brofiadau eraill. Mae hyn yn golygu, trwy deulu ac anwyliaid a'r gweithlu gofal cymdeithasol, ein bod wedi clywed straeon y rhai ag anghenion gofal a chymorth nad oeddent yn gallu cymryd rhan eu hunain neu a fu farw yn ystod neu ar ôl y pandemig.
² Roedd cyfranwyr yn gallu dewis mwy nag un genedl yn y DU yn y ffurflen ar-lein, felly mae'r cyfanswm a grynhowyd ar draws y gwledydd yn uwch na chyfanswm gwirioneddol yr ymatebion a dderbyniwyd.
Dangosir isod nifer y bobl a rannodd eu straeon ym mhob gwlad yn y DU drwy'r ffurflen ar-lein, digwyddiadau gwrando a chyfweliadau ymchwil:
Ffigur 1: Ymgysylltiad Mae Pob Stori o Bwys ledled y DU
I gael rhagor o wybodaeth am sut y gwnaethom wrando ar bobl a’r dulliau a ddefnyddiwyd i ddadansoddi straeon, gweler yr atodiad.
Cyflwyno a dehongli straeon
Mae'n bwysig nodi nad yw'r straeon a gasglwyd drwy Every Story Matters yn gynrychioliadol o bob profiad o ofal cymdeithasol yn ystod y pandemig ac rydym yn debygol o glywed gan bobl sydd â phrofiad penodol i'w rannu gyda'r Ymchwiliad, yn enwedig ar y ffurflen we ac mewn digwyddiadau gwrando. Effeithiodd y pandemig ar bawb yn y DU mewn gwahanol ffyrdd ac, er bod themâu a safbwyntiau cyffredinol yn dod i'r amlwg o'r straeon, rydym yn cydnabod pwysigrwydd profiad unigryw pawb o'r hyn a ddigwyddodd. Nod y cofnod hwn yw adlewyrchu'r gwahanol brofiadau a rannwyd gyda ni, heb geisio cymodi'r gwahanol straeon.
Rydym wedi ceisio adlewyrchu'r amrywiaeth o straeon a glywsom, a allai olygu bod rhai straeon a gyflwynir yma yn wahanol i'r hyn a brofodd pobl eraill, neu hyd yn oed llawer o bobl eraill, yn y DU. Lle bo'n bosibl rydym wedi defnyddio dyfyniadau i helpu i seilio'r cofnod ar yr hyn a rannodd pobl yn eu geiriau eu hunain.
Archwilir rhai straeon yn fanylach trwy ddarluniau achos o fewn y prif benodau. Mae'r rhain wedi'u dewis i amlygu'r gwahanol fathau o brofiadau y clywsom amdanynt a'r effaith a gafodd y rhain ar bobl. Mae cyfraniadau wedi'u hanonymeiddio trwy ddefnyddio ffugenwau (yn hytrach nag enw go iawn y person).
Rydym hefyd wedi datblygu astudiaethau achos (Pennod 8), gan ddod â straeon gwahanol grwpiau o fewn lleoliad penodol ynghyd yn seiliedig ar ymweliadau personol â darparwyr gofal. Mae'r astudiaethau achos hyn yn rhoi cipolwg dyfnach ar y gwahanol fathau o brofiadau o fewn darparwyr gofal o wahanol safbwyntiau.
Drwy gydol y cofnod, rydym yn cyfeirio at bobl a rannodd eu straeon gyda Every Story Matters fel 'cyfranwyr'. Lle bo'n briodol, rydym hefyd wedi disgrifio mwy amdanynt (er enghraifft, eu rôl neu leoliad gofal) i helpu i egluro cyd-destun a pherthnasedd eu profiad. Rydym hefyd wedi cynnwys y genedl yn y DU y mae'r cyfrannwr yn dod ohoni (lle mae'n hysbys). Nid yw hyn wedi'i fwriadu i roi darlun cynrychioliadol o'r hyn a ddigwyddodd ym mhob gwlad, ond i ddangos y profiadau amrywiol ledled y DU o bandemig Covid-19. Casglwyd a dadansoddwyd straeon drwy gydol 2024, sy'n golygu bod profiadau'n cael eu cofio rywbryd ar ôl iddynt ddigwydd.
Mewn rhai mannau yn y cofnod, rydym yn adlewyrchu'r hyn a ddywedodd pobl wrthym am y berthynas waith rhwng gwasanaethau iechyd a gofal cymdeithasol yn ystod y pandemig. Mae profiadau'r system gofal iechyd yn ystod y pandemig wedi'u manylu yng nghofnod Modiwl 3. Mae'r cofnod hwn yn canolbwyntio ar brofiadau'r sector gofal cymdeithasol ac nid yw'n ceisio cymodi gwahanol safbwyntiau.
Strwythur y cofnod
Mae'r ddogfen hon wedi'i strwythuro i ganiatáu i ddarllenwyr ddeall sut brofiad oedd gan bobl o ofal cymdeithasol. Mae'r cofnod wedi'i drefnu'n thematig gyda phrofiad pobl ag anghenion gofal a chymorth, anwyliaid, gofalwyr di-dâl a'r gweithlu gofal cymdeithasol a geir ar draws pob pennod:
- Pennod 2: Cyfnodau clo a chyfyngiadau ar leoliadau gofal
- Pennod 3: Rhyddhau o ysbytai i gartrefi gofal
- Pennod 4: Gofal diwedd oes a phrofedigaeth
- Pennod 5: PPE a mesurau rheoli heintiau
- Pennod 6: Prinder staff a sut y darparwyd gofal
- Pennod 7: Mynediad at wasanaethau gofal iechyd a phrofiad ohonynt
- Pennod 8: Astudiaethau achos.
Terminoleg a ddefnyddir yn y cofnod
Defnyddir y termau a'r ymadroddion canlynol drwy gydol y cofnod i gyfeirio at grwpiau allweddol neu bolisïau ac arferion penodol a oedd yn berthnasol i'r sector gofal cymdeithasol yn ystod pandemig Covid-19. Rydym yn disgrifio gweithgareddau a lleoliadau gofal, mathau o anghenion gofal, y rhai sy'n darparu gofal a chymorth, ac yna rhai termau penodol a ddefnyddir yn y sector gofal cymdeithasol.
Gofal cymdeithasol i oedolion yn disgrifio cymorth gyda thasgau dyddiol fel y gall pobl fyw mor annibynnol â phosibl. Mae ar gyfer oedolion a allai fod angen cymorth ychwanegol oherwydd oedran, anabledd, salwch neu gyflyrau iechyd meddwl a chorfforol eraill. Gall gofal cymdeithasol oedolion helpu gyda thasgau dyddiol fel paratoi prydau bwyd, golchi a gwisgo, mynd i'r toiled a gofal personol arall i bobl hŷn ac oedolion o oedran gweithio. Gall hefyd gynnwys cymorth gyda chludiant fel y gall pobl deithio o gwmpas eu cymuned leol a chefnogaeth ar gyfer ynysu cymdeithasol ac unigrwydd. Gellir darparu gofal cymdeithasol oedolion mewn sawl lleoliad gwahanol. Ar gyfer Pob Stori yn Bwysig, canolbwyntiodd Modiwl 6 yn bennaf ar gartrefi gofal a gofal cartref.
Gofal cartref a elwir hefyd yn ofal cartref. Mae'n cynnwys gweithiwr gofal yn ymweld â chartref person i gefnogi gyda thasgau dyddiol fel rhoi meddyginiaethau, golchi a gwisgo, paratoi bwyd a glanhau'r cartref. Nod gofal cartref yw helpu pobl i fyw'n annibynnol yn eu cartref eu hunain ac i gynnal ansawdd eu bywyd.
Cartrefi gofal yn lleoedd lle mae pobl yn byw i dderbyn cymorth ychwanegol gyda gofal personol fel bwyta, golchi, gwisgo a chymryd meddyginiaeth. Mae gwahanol fathau o gartrefi gofal. Mae rhai yn cynnig gofal nyrsio neu ofal dementia arbenigol tra nad yw eraill yn gwneud hynny ac efallai y byddant yn cael eu hadnabod fel cartrefi gofal preswyl.
Pobl ag anghenion gofal a chymorth yn bobl 18 oed a throsodd sydd angen cymorth gyda gweithgareddau dyddiol gan gynnwys gofal personol a thasgau domestig oherwydd cyflyrau iechyd corfforol neu feddyliol, oedran neu anabledd. Gall hyn gynnwys pobl sydd:
- Oes gennych chi anabledd dysgu
- Yn awtistig
- Yn cael eu heffeithio gan gyflwr iechyd meddwl
- Yn cael eu heffeithio gan Ddementia
- Yn fregus oherwydd afiechyd neu anabledd corfforol.
Gofalwyr di-dâl yn aelodau o'r teulu neu'n ffrindiau sy'n gofalu am rywun sydd ag anghenion gofal a chymorth. Gall gofalu am rywun olygu ychydig oriau bob wythnos neu efallai eu bod yn gofalu amdano 24 awr y dydd, saith diwrnod yr wythnos. Mae rhai gofalwyr di-dâl yn byw gyda'r person maen nhw'n gofalu amdano neu'n agos ato tra gall eraill ddarparu mwy o gymorth o bell. Gall rhai gofalwyr di-dâl ofalu am fwy nag un person. Yn y cofnod rydym hefyd yn defnyddio'r term 'rhywun annwyl' ar gyfer pobl y mae aelod o'u teulu mewn cartref gofal ac efallai nad yw'n darparu gofal o ddydd i ddydd. Lle cafodd y person brofedigaeth yn ystod y pandemig, defnyddir y term hwn hefyd i ddisgrifio'r gofalwyr di-dâl neu'r anwyliaid.
Gweithwyr gofal cymdeithasol proffesiynol cefnogi pobl sydd ag anghenion gofal a chymorth. Mae hyn yn cynnwys sawl rôl broffesiynol gan gynnwys gweithwyr gofal, rheolwyr cofrestredig a gweithwyr cymdeithasol a ddisgrifir isod.
Gweithwyr gofal yn weithwyr proffesiynol sy'n cefnogi pobl ag anghenion gofal a chymorth i fyw'n annibynnol a chyflawni gweithgareddau dyddiol. Gall hyn gynnwys helpu gyda bwyta ac yfed, cynorthwyo gyda gofal personol, archebu neu fynd gyda phobl i apwyntiadau a helpu gyda meddyginiaethau.
Rheolwr cofrestredig yn rôl reoli sy'n ofynnol gan y Comisiwn Ansawdd Gofal ar gyfer pob lleoliad gofal cofrestredig gan gynnwys cartrefi gofal a darparwyr gofal cartref.
Gweithwyr cymdeithasol yn weithwyr proffesiynol sy'n cefnogi pobl agored i niwed i'w hamddiffyn rhag niwed neu gam-drin ac maen nhw'n helpu pobl i fyw'n annibynnol. Maen nhw'n gweithio gyda phobl ag anghenion gofal a chymorth, eu hanwyliaid a gweithwyr proffesiynol eraill i helpu i lywio heriau. Gall hyn gynnwys asesu anghenion pobl, trefnu cymorth a gwneud atgyfeiriadau at wasanaethau eraill.
Offer Diogelu Personol yw PPE sy'n cynnwys masgiau, menig, ffedogau a fisorau.
Gwisgo a thynnu i ffwrdd yw'r term a ddefnyddir am wisgo a thynnu PPE i ffwrdd, yn y drefn honno.
2. Roedd cyfranwyr yn gallu dewis mwy nag un genedl yn y DU yn y ffurflen ar-lein, felly mae'r cyfanswm a grynhowyd ar draws y gwledydd yn uwch na chyfanswm gwirioneddol yr ymatebion a dderbyniwyd.
2. Cloeon a chyfyngiadau ar leoliadau gofal |
 |
Mae'r bennod hon yn archwilio effeithiau cyfyngiadau'r cyfnod clo ar ofal cymdeithasol i oedolion. Mae'n disgrifio effeithiau peidio â gallu ymweld â phobl sy'n byw gartref neu eu cefnogi a'r pwysau ar ofalwyr di-dâl. Mae hefyd yn edrych ar gyfyngiadau ar ymweliadau â chartrefi gofal a symud o fewn cartrefi gofal a sut yr effeithiodd y newid i gyfathrebu rhithwir ar y sector gofal cymdeithasol i oedolion.
Sut effeithiodd cyfyngiadau symud ar ofal a chymorth gartref
Sut effeithiodd trefniadau byw ar brofiadau cyfnod clo
Roedd pobl ag anghenion gofal a chymorth nad oedd ganddynt unrhyw gymorth ffurfiol yn ystod y pandemig yn wynebu heriau difrifol a oedd yn eu gadael dan straen, yn flinedig ac yn ynysig.
| “ | Rwy'n anabl ac mae gen i glefyd hunanimiwn terfynol, felly roeddwn i'n amddiffyn fy hun…Yn ystod y pandemig, roeddwn i'n teimlo ar goll, ynysig, unig, wedi'm hanghofio ac yn ofnus…Er bod fy chwaer a'i theulu'n byw drws nesaf, wnaethon ni ddim cwrdd ond cawsom alwad ffôn ddyddiol am 10 munud wrth iddi ofalu am ei merch anabl, felly roeddwn i'n brysur iawn.”
- Person ag anghenion gofal a chymorth, Lloegr |
Roedd pobl ag anghenion gofal a chymorth a oedd yn byw ar eu pen eu hunain yn ei chael hi'n anodd ymdopi â thasgau sylfaenol fel coginio a golchi, a oedd yn eu gwneud nhw'n teimlo'n ddiymadferth ac wedi'u gadael ar adegau.Roedd rhaid i'r cyfranwyr hyn naill ai ddod o hyd i ffyrdd o ymdopi ar eu pen eu hunain neu roeddent yn ddibynnol ar gefnogaeth gyfyngedig iawn. Gadawyd pobl a oedd wedi byw'n annibynnol o'r blaen gyda chefnogaeth ac ymweliadau mynych gan deulu a ffrindiau heb neb i gadw llygad ar sut roeddent yn ymdopi.
| “ | Roeddwn i'n gaeth i'r gwely felly allwn i ddim hyd yn oed goginio, felly am ychydig ddyddiau doeddwn i ddim wedi coginio na bwyta dim byd, felly fe wnaeth un o fy ffrindiau goginio pryd o fwyd a'i adael wrth y drws ffrynt, canu'r gloch ac yna gadael.”
- Person ag anghenion gofal a chymorth, Lloegr |
| “ | Roedd yn lletchwith weithiau os yw hynny'n gwneud synnwyr, roeddwn i'n dal yn gallu rhoi fy mwyd fy hun ymlaen ac ati. Mae'n rhaid i mi gael fy ngwylio am adael y nwy ymlaen. Rydw i wedi gwneud hynny sawl gwaith.”
- Person ag anghenion gofal a chymorth, Lloegr |
Myfyriodd pobl sy'n defnyddio gwasanaethau gofal cartref ac sy'n byw ar eu pen eu hunain hefyd ar sut unig ac ynysig roedden nhw'n teimlo. Yn aml, yr unig berson yr oeddent yn rhyngweithio ag ef oedd eu gweithiwr gofal cartref.
| “ | Roedd ochr unigedd pethau'n real iawn oherwydd fy mod i'n byw ar fy mhen fy hun, felly, cyn iddyn nhw gyflwyno'r syniad o swigod, roeddwn i'n teimlo'n ynysig iawn. Felly, yr unig bobl roeddwn i'n cael cymysgu â nhw oedd fy ngofalwyr [cartref]. Y peth pwysicaf oedd unigedd difrifol.”
- Person ag anghenion gofal a chymorth, Lloegr |
Cafodd teuluoedd, ffrindiau a gofalwyr di-dâl eu hatal rhag ymweld â phobl ag anghenion gofal a chymorth nad oeddent yn byw gyda nhw oherwydd cyfyngiadau'r cyfnod clo. Nhw yn poeni'n fawr am y bobl yr oeddent yn gofalu amdanynt ac yn ofni am eu lles a'u diogelwch.
| “ | [Wnes i ddim gweld fy nhad am] 112 diwrnod ar gyfer y cyfnod clo cyntaf. Yn y pen draw, newidiodd y syniad y gallech chi fynd i dŷ rhywun os oeddech chi'n gofalu amdanyn nhw ond i ddechrau nid oedd hynny'n bosibl o gwbl.”
- Gofalwr di-dâl yn byw ar wahân i'r person y maent yn gofalu amdano, yr Alban |
Ar gyfer gofalwyr di-dâl a oedd yn byw ar wahân i'w hanwyliaid, roedd y cyswllt wedi'i gyfyngu i sgyrsiau ffôn neu ar-lein neu adael hanfodion fel siopa bwyd ar garreg y drwsRoedd gofalwyr di-dâl yn ei chael hi'n heriol ac yn llawn straen i drefnu gofal i bobl nad oeddent yn byw gyda nhw.
| “ | Mae fy mam a fy nhad yn eu 70au, ac nid Saesneg yw eu hiaith gyntaf… byddwn i’n mynd i’w tŷ, a byddwn i’n sefyll y tu allan… bydden nhw ar garreg y drws a byddem ni’n siarad am, beth ydych chi wedi’i wneud, ydych chi wedi ffonio’r gofalwyr? Beth maen nhw’n ei gynnig? Ydyn nhw’n dod o hyd? Ydych chi eisiau i mi eu ffonio nhw?”
- Gofalwr di-dâl yn byw ar wahân i'r person y maent yn gofalu amdano, Lloegr |
Disgrifiodd llawer o bobl deimlo'n rhwygo rhwng yr awydd i dreulio amser gyda'u hanwyliaid a'r awydd i'w hamddiffyn rhag haint Covid-19 posibl.Achosodd rheoli'r tensiwn rhwng risgiau haint Covid-19 a risgiau gadael aelodau'r teulu heb gefnogaeth ofid mawr ar y pryd. Wrth fyfyrio ar hyn ar ôl y pandemig, roedd rhai'n difaru dilyn cyfyngiadau a pheidio â threulio mwy o amser gyda'r person yr oeddent yn gofalu amdano, yn enwedig y rhai sydd wedi cael profedigaeth. Mae aelodau'r teulu a gofalwyr di-dâl yn parhau i deimlo'n edifeirwch ac yn ofidus am yr amser a gollwyd ganddynt.
| “ | Fyddwn i ddim yn treulio cymaint ag y byddwn i wedi hoffi, byddai hi'n dweud, “O, rhowch y tegell ymlaen, cael paned o de gyda fi” ac [doeddwn i ddim yn gallu…] Yr holl bethau hyn rydych chi'n difaru wedyn roedd yn anodd; roedd hi'n unig.”
- Gofalwr di-dâl yn byw ar wahân i'r person y maent yn gofalu amdano, Cymru |
| “ | Roeddwn i wedi dilyn y rheolau o ddechrau'r cyfnod clo ac ni wnes i ymweld â fy rhieni, rhywbeth rwy'n ei ddifaru nawr, gan nad oedd yr un ohonom wedi dal Covid a byddai wedi bod yn ddiogel eu cael yn ein swigen ni. Rwy'n teimlo fy mod i wedi colli allan ar rai wythnosau pwysig iawn ar ddiwedd bywyd iach mam.”
- Gofalwr di-dâl yn byw ar wahân i'r person y maent yn gofalu amdano, Lloegr |
Mewn rhai achosion, gwnaeth anwyliaid a gofalwyr di-dâl y penderfyniad i dorri cyfyngiadau er mwyn iddynt allu cynnal cysylltiad neu ddarparu gofal hanfodol i'r person yr oeddent yn gofalu amdano. Weithiau byddai rheolau’n cael eu torri os oeddent yn byw mewn ardal wahanol ac roedd cyfyngiadau ar deithio rhwng ardaloedd mewn gwahanol haenau o’r cyfnod clo. Fodd bynnag, roedd torri cyfyngiadau’r cyfnod clo i wneud hyn hefyd yn ffynhonnell o poeni.
| “ | Dylwn i fod wedi cael mynd i mewn i dŷ fy mam-gu a'i eistedd gyda hi a rhyngweithio llawer mwy na gadael y siopa wrth ei drws ffrynt ac yna ei gario allan i'r ardd. Ar ôl ychydig, torrais y rheolau oherwydd gwelais pa mor gyflym yr oedd hi'n dirywio a meddyliais, 'Does dim ffordd ar y blaned hon na fyddaf yn mynd i mewn i weld fy mam-gu. Dydw i ddim yn mynd i'w wneud.'”
- Gofalwr di-dâl yn byw ar wahân i'r person y maent yn gofalu amdano, Lloegr |
| “ | Roedd gan fy nhad glefyd niwronau modur ac yn ystod Covid roedden ni'n teimlo fel pe bai wedi'i adael i ofalu amdano'i hun. Roedd yng nghyfnodau diweddarach y clefyd ac yn cael trafferth mawr gyda symudedd. Gadawyd gofal dyddiol fy nhad i fy mam sydd hefyd â chyflwr iechyd cronig. Pan fu bron â chael chwalfa oherwydd straen gofalu am fy nhad, torrais reolau'r cyfnod clo i helpu i ofalu amdano.”
- Gofalwr di-dâl, Lloegr |
Stori AndyMae Andy yn byw yn yr Alban ac yn darparu gofal i'w neiniau a theidiau yn ystod y pandemig. Nid oedd yn byw yn agos atynt. Myfyriodd ar ba mor anodd oedd penderfynu a ddylid dilyn cyfyngiadau'r cyfnod clo neu flaenoriaethu gofal ei neiniau a theidiau. Roedd ei benderfyniad i ymweld â nhw yn golygu ei fod yn aml yn teimlo'n bryderus ac yn llawn straen. |
|
| “ | Roeddwn i'n torri'r rheolau bob dydd, ond roeddwn i fel, 'Gallan nhw fy nirwyo, gallant fy rhoi yng nghefn car heddlu yn llythrennol.' Felly, cafodd effaith andwyol ar fy iechyd, ond beth yw rhan fach o'r effaith andwyol honno o'i gymharu â'r magwraeth a roddodd [fy nhaid a theidiau] i mi, y cariad, y gofal, y gefnogaeth.” |
| Roedd Andy hefyd yn poeni'n fawr am drosglwyddo Covid-19 i'w neiniau a theidiau pan ymwelodd â nhw, i'r graddau y byddai'n effeithio ar ei gwsg. | |
| “ | Roeddwn i'n deffro am 2 o'r gloch, 3 o'r gloch, 4 o'r gloch y bore gyda chrychguriadau'r galon, chwysu, dan straen, 'Ydw i'n mynd i roi Covid iddyn nhw?' Roeddwn i'n gwneud 2 neu 3 prawf y dydd a phethau fel 'na cyn i mi fynd drwodd i'w gweld nhw.” |
| Pan oedd nain Andy yn marw, anwybyddodd ei deulu'r rheolau i sicrhau y gallent fod gyda hi. | |
| “ | Fe wnaethon ni dorri pob rheol dan yr haul a theithiodd fy modryb i fyny. Ei chwaer hi yw hi, fel y gwyddoch chi. Mae ei chwaer yn marw ac roedden ni i gyd yn teimlo fel pe baen ni wedi eu siomi gymaint yn ystod [y pandemig] a bod y system wedi eu siomi. Doedden ni ddim am eu siomi.” |
Penderfynodd gofalwyr di-dâl eraill symud, i fyw gyda'r person yr oeddent yn gofalu amdano, er mwyn sicrhau y gallent ddarparu'r gefnogaeth oedd ei hangen.Profodd rhai ymdeimlad mwy o undod ac agosrwydd gyda'u teulu oherwydd eu bod wedi treulio cymaint o amser gyda'i gilydd. Yn gysylltiedig â hyn, roeddent yn ddiolchgar iawn am y cyfle a gawsant i dreulio amser gyda'u hanwyliaid a gofalu amdanynt.
| “ | Cafodd fy nhad ei ryddhau cyn y cyfnod clo oherwydd bod yr ysbyty yn gwybod y byddai'n fwy diogel gartref. Doedd e ddim yn teimlo'n ddiogel cael gofalwyr felly symudais i mewn gyda fy rhieni… Am chwe mis, gwnes i'r rhan fwyaf o bethau i fy nhad. Tynnais ei bad anymataliaeth bob bore, ei olchi a'i eillio bob dydd. …Roedd yn fraint gofalu amdano.”
- Gofalwr di-dâl a symudodd i mewn gyda'r person yr oeddent yn gofalu amdano, Lloegr |
| “ | Roedd gofalu am fy nain yn anodd iawn, ond ar yr un pryd, rwy'n ddiolchgar fy mod i wedi cael ei wneud… Rwy'n gwybod ei fod wedi fy ngwthio i lawr a phopeth, ond… Rwy'n teimlo'n ddiolchgar iawn bod yr un person a'm helpodd pan oeddwn i'n fabi, wedi fy magu, wedi gwneud cymaint i mi ac yna fi yn tyfu i fyny a gallu gofalu amdanyn nhw… Rwy'n ei chael yn fendith.”
- Gofalwr di-dâl a symudodd i mewn gyda'r person yr oeddent yn gofalu amdano, Lloegr |
Dywedodd pobl ag anghenion gofal a chymorth wrthym fod byw gyda theulu neu ofalwyr wedi gwneud addasu i'r cyfyngiadau symud yn haws. Roedd cael rhywun i siarad ag ef a'u cefnogi gyda'u hanghenion gofal yn gwneud pethau'n haws i'w rheoli. Rhannodd cyfranwyr enghreifftiau o'u teuluoedd ac eraill yn gwneud iawn am fynediad llai at wasanaethau iechyd a gofal cymdeithasol yn ystod y pandemig. Siaradodd rhai yn gynnes am ba mor dda y gofalwyd amdanynt a'u cefnogi a gwerthfawrogasant yr amser y gallent ei dreulio gyda'i gilydd. O ganlyniad, roedd rhai pobl ag anghenion gofal a chymorth yn edrych yn ôl ar yr amser hwn gyda rhywfaint o hoffter.
| “ | O ran y gofal rwy'n ei dderbyn, oherwydd ein bod wedi llwyddo i gael fy merch adref cyn y cyfnod clo ac yn amlwg ni allai fy ngwraig wneud unrhyw waith o gwbl nes i'r cyfnod clo lacio, roedd gen i ddau oedolyn yn y tŷ mewn gwirionedd ar gyfer y gofal dyddiol ychwanegol ... ond ie, o ran fy ngofal dyddiol gwirioneddol, roedd yn well ... ac yn amser hapus.”
- Person ag anghenion gofal a chymorth, Lloegr |
Stori HalemaMae Halema yn 74 oed ac yn byw yng Nghanolbarth Lloegr. Mae ganddi glefyd rhwystrol cronig yr ysgyfaint (COPD) sy'n cyfyngu ar ei hanadlu. Mae ganddi reolydd calon hefyd a chyflyrau iechyd eraill sy'n gysylltiedig â'i hoedran. Mae hi'n byw ar ei phen ei hun mewn fflat yn agos at ganol y dref. Roedd cyflwyno’r cyfyngiadau symud yn heriol iawn iddi. Roedd hi wedi bod yn aelod o wahanol grwpiau cymunedol o’r blaen, a roddodd hynny drefn iddi a chaniatáu iddi ryngweithio â phobl. Roedd y cyfyngiadau symud yn sioc fawr yr oedd yn anodd addasu iddi. |
|
| “ | Roedd yn newid enfawr peidio â gweld ffrindiau na theulu, roedd yn heriol iawn.” |
| Fodd bynnag, cafodd gefnogaeth gan ei nith a dorrodd gyfyngiadau’r cyfnod clo i ymweld â hi bob dydd i baratoi ei meddyginiaeth a gwneud rhywfaint o fwyd. | |
| “ | Dyw fy iechyd ddim wedi bod yn dda ers amser maith, ond mae wedi gwaethygu o'r holl amser a dreuliais ar fy mhen fy hun y tu mewn. Gwelais lawer mwy ohoni, oherwydd ei bod hi'n dod i lawr yn fwy i wneud yn siŵr fy mod i'n iawn, yn gwneud yr holl bethau y mae hi bob amser wedi'u gwneud, rhywbeth fel, fy nghael i fyny lawer o'r amser, allan o'r gwely, glanhau cyffredinol o amgylch y tŷ. Paratoi bwyd i mi, roedd hi'n arfer gwneud y siopa ar-lein, wel yn bennaf ar-lein, gofalu am y tabledi.” |
| Cryfhaodd y gofal a ddarparodd nith Halema a'r amser a dreuliasant gyda'i gilydd eu perthynas. Mae Halema yn ddiolchgar iawn am yr holl gefnogaeth a gafodd yn ystod y pandemig. | |
| “ | Mae hi wastad wedi gofalu amdanaf, cyn y pandemig, ond mae'r amser hwnnw, wrth edrych yn ôl arno, yn gwneud i mi feddwl pa mor lwcus oeddwn i i'w chael hi a fy ffrindiau eraill a helpodd fi ac a wiriodd sut roeddwn i'n teimlo." |
Teimladau unigrwydd ac arwahanrwydd gofalwyr di-dâl
Roedd rhai gofalwyr di-dâl yn teimlo'n ynysig ac yn gaeth yn eu cartref er gwaethaf y ffaith eu bod yn falch eu bod yn gallu byw gyda'r person yr oeddent yn gofalu amdano. Roedden nhw'n teimlo bod y cyfyngiadau symud yn glaustroffobig, yn llawn straen ac yn teimlo'n llethol gan y gofynion sylweddol a roddwyd arnyn nhw.
| “ | Mae'n rhaid i mi boeni'n gyson am [fy mhartner]. Weithiau roeddwn i'n teimlo braidd yn fygythiad ac yn gaeth, ac nid oedd unrhyw ffordd o ddianc o hynny. Dyna sut roeddwn i'n teimlo ar adegau yn ystod y pandemig oherwydd roeddwn i'n teimlo fel petawn i'n garcharor wedi'i ddal yn fy nghartref fy hun heb ddihangfa.”
- Gofalwr di-dâl yn byw gyda'r person y maent yn gofalu amdano, yr Alban |
| “ | Roedd yn llawn straen i mi, cael plentyn [a fy ngŵr, a oedd â chanser] yn y tŷ. Rydych chi i gyd wedi'ch cyfyngu mewn un lle. Roedd yn rhaid i mi wneud popeth o gwmpas y tŷ. Roeddwn i'n gofalu am y plentyn, rwy'n gofalu am [fy ngŵr], rwy'n gofalu am y tŷ, rwy'n gwneud y pethau ariannol, rwy'n siopa, wyddoch chi? Ac yna doedd gen i ddim amser i mi fy hun.”
- Gofalwr di-dâl yn byw gyda'r person y maent yn gofalu amdano, Lloegr |
Teimlai aelodau'r teulu a gofalwyr di-dâl absenoldeb eu rhwydweithiau cymorth arferolNid oeddent yn gallu gweld ffrindiau nac aelodau eraill o'r teulu ac nid oedd ganddynt gyfleoedd i gael seibiant pan oedd gofalu fwyaf anodd. Roedd hyn yn arbennig o wir am y rhai a symudodd i mewn i ddarparu gofal yn ystod y cyfnod clo ac a oedd i ffwrdd o'u trefn arferol a'u hamgylchedd.
| “ | Pan aeth yn sâl iawn, roedd yn wirioneddol flinedig ac yn frawychus ac yn unig iawn, iawn. Wrth gwrs, byddai pobl yn ffonio ac yn dweud, 'Os oes unrhyw beth y gallem ei wneud' ond nid oedd dim oherwydd, yn y cyfnod [cyflymder clo] cyntaf, nid oeddent yn cael mynd i mewn i'r tŷ. Roeddech chi'n gwbl ynysig.”
- Gofalwr di-dâl yn byw gyda'r person y maent yn gofalu amdano, Cymru |
| “ | Doedd gan yr un ohonom blant…felly symudais i mewn i ofalu amdano…Doeddwn i erioed wedi gwneud unrhyw beth tebyg ac roedd yn wirioneddol ddwys gofalu am rywun oedd yn sâl…heb neb arall…wnaem ni ddim gweld unrhyw deulu na ffrindiau am dros flwyddyn.”
- Gofalwr di-dâl a symudodd i mewn gyda'r person yr oeddent yn gofalu amdano, Lloegr |
| “ | Roedd cael fy nghyfyngu i un amgylchedd…roedd yn eithaf anodd…roedd yn golygu hyd yn oed fi fy hun, wel, roedd cyfyngiadau i fynd allan a sawl gwaith y gallech chi fynd allan, roedd yn cael effaith arnaf i, oherwydd roedd yn golygu, wyddoch chi, eich bod chi'n canolbwyntio ar un person ac mae'n teimlo fel eich bod chi'n esgeuluso popeth arall. Rwy'n credu bod ganddo ryw fath o effaith seicolegol [arnaf i].”
- Gofalwr di-dâl a symudodd i mewn gyda'r person yr oeddent yn gofalu amdano, Lloegr |
Hyd yn oed pan oedd gofalwyr di-dâl ac aelodau o'r teulu yn gallu cymryd seibiannau byr o'r cartref (er enghraifft trwy gerdded y ci neu siopa am fwyd) fel ffordd o ymdopi â phwysau darparu gofal, roedden nhw'n aml yn bryderus iawn am y risg o ddal Covid-19Roeddent yn gyson ar eu gwyliadwriaeth i leihau'r risg iddynt eu hunain a'r bobl yr oeddent yn eu cefnogi.
| “ | Fe wnes i fynd â'r cŵn allan, dyna oedd fy synnwyr cyffredin, rhywfaint o amser i mi fy hun, mwynhau'r golygfeydd heb neb o gwmpas, ond ar yr un pryd [roeddwn i bob amser] yn dal i boeni beth petawn i'n taro i mewn i rywun. Os byddwn i'n ei ddal, yna mae'n bendant yn mynd yn ôl ato ac mae'n fy mai i.”
- Gofalwr di-dâl yn byw gyda'r person y maent yn gofalu amdano, yr Alban |
Roedd pobl oedd yn darparu gofal di-dâl wedi’u llethu gan effeithiau’r cyfyngiadau symud a darparu gofal ar hyd yr oriau. Clywsom am effeithiau negyddol eang a sylweddol ar eu hiechyd corfforol a meddyliolRoedd hyn yn cynnwys straen, blinder a phryder llethol.
| “ | Ar un adeg, dim ond tua phedair awr o gwsg y dydd oeddwn i'n ei gael am fisoedd, ac fe ddaeth yn norm. Roeddwn i'n meddwl fy mod i'n iawn, ond roeddwn i wedi blino'n llwyr.”
- Gofalwr di-dâl yn byw gyda'r person y maent yn gofalu amdano, Gogledd Iwerddon |
| “ | Roedd y gofal parhaus a gwaethygu iechyd [anwylyd] wedi cael effaith arnaf. Roeddwn i'n teimlo dan straen mawr i'r pwynt nes i mi sylweddoli weithiau na allwn i wneud pethau normal, gallaf gofio [i mi geisio] gwagio'r peiriant golchi llestri ac roeddwn i'n ei chael hi'n rhy anodd… Doeddwn i ddim yn gallu ei wneud.”
- Gofalwr di-dâl yn byw gyda'r person y maent yn gofalu amdano, Cymru |
Straeon gan ofalwyr di-dâlClywsom hefyd mewn digwyddiad ar-lein gyda Carers UK sut yr effeithiodd pwysau darparu gofal yn ystod y pandemig ar iechyd meddwl a lles pobl. |
|
| “ | Y baich o weithio efallai 14 neu 15 awr y dydd, saith diwrnod yr wythnos a gofalu am fy rhieni oedd ill dau yn gwarchod fy hun, cefais fy llosgi allan. Un diwrnod, dechreuais grio.”
– Gofalwr di-dâl, digwyddiad gwrando, Gogledd Iwerddon |
Clywsom am effaith cymryd cyfrifoldebau gofalu ychwanegol a arweiniodd at anwyliaid a gofalwyr di-dâl yn mabwysiadu arferion afiach i ymdopi. Roedd hyn yn cynnwys mwy o yfed alcohol a newidiadau mewn diet.
Stori SallyYn ystod y pandemig, bu Sally yn byw yn yr Alban, gan ddarparu gofal a chefnogaeth i'w mab sy'n oedolyn a'i dau riant. Gadawodd gofynion gofalu am aelodau ei theulu hi'n teimlo'n flinedig ac effeithiodd ar ei hiechyd corfforol a meddyliol. |
|
| “ | Saethodd fy mhwysedd gwaed drwy’r to a hyd yn oed nawr mae’n rhaid i mi gymryd lefel uchel iawn o feddyginiaeth pwysedd gwaed uchel.” |
| Mae mab Sally yn gwadriplegig. Cyn y pandemig, roedd ganddo ofal 24 awr ac roedd angen tri gofalwr arno i'w symud i mewn ac allan o'r gwely. Yn ystod y pandemig, cymerodd Sally ei holl ofal a'i godi, er gwaethaf cael dau lawdriniaeth ar ei asgwrn cefn ei hun. Mae hi bellach yn dibynnu ar forffin i reoli poen sy'n parhau i effeithio ar ei lles cyffredinol. | |
| “ | Aeth fy nghefn yn llwyr felly mae'n rhaid i mi gymryd morffin ddwywaith y dydd i allu codi o'r gwely. Dydy fy nghefn ddim wedi gwella o'r holl godi a'r rhedeg i fyny ac i lawr a chario'r siopa a helpu mam a dad. Mae'n debyg fy mod i ar forffin am oes ac mae hynny'n cael effaith enfawr arna i, ar fy lles.” |
| Dywedodd Sally wrthym sut yr effeithiodd y straen a deimlai yn ystod y pandemig ar ei harferion bwyta, gan arwain at amrywiadau yn ei phwysau. | |
| “ | Aeth fy mwyta’n wallgof, rhoddais bwysau ymlaen, yna collais bwysau, yna rhoddais bwysau yn ôl ymlaen, yna collais ef a dyna un o’r ffyrdd rwy’n ymdopi â straen ac anhapusrwydd. Rwy’n bwyta’n gysurus ac yna rwy’n rhoi’r gorau i fwyta. Dydw i ddim wedi gwella.” |
Dywedodd rhai gofalwyr di-dâl eu bod wedi colli eu ymdeimlad o hunan wrth iddynt flaenoriaethu anghenion pobl eraill o flaen eu hanghenion eu hunain ac nad oedd ganddynt fawr ddim mynediad at seibiant na chefnogaeth.
| “ | Dydy llawer o bobl ddim yn deall, pan mae'n rhaid i chi ddarparu gofal, fod hynny fel swydd amser llawn ynddo'i hun. Mae'n heriol ac mae'n draenio'n gorfforol ac yn feddyliol. Llawer o'r amser, rwy'n teimlo nad ydw i'n berson fy hun oherwydd nad ydw i'n cael y cyfle hwnnw i feddwl amdanaf fy hun a beth yw fy anghenion. Mae'n rhaid i mi ganolbwyntio ar bawb arall.”
- Gofalwr di-dâl yn byw gyda'r person y maent yn gofalu amdano, yr Alban |
Effeithiwyd hefyd ar berthnasoedd gofalwyr di-dâl ag aelodau eraill o'u teulu yn ystod y cyfnod clo. Roedd rhai perthnasoedd dan straen o dan bwysau gofalu.
| “ | Roedd e [fy mhartner] yn arfer mynd yn flin gyda fi a byddwn i'n mynd yn flin gydag e. Roedd e'n dda iawn, iawn gyda fy mam ond byddai'n bigog gyda fi, oherwydd roedden ni'n dau wedi blino'n lân, roedd e'n cael effaith arnom ni fel cwpl, yn bendant. Roedd yn llawer o straen ar y pryd.”
- Gofalwr di-dâl, Lloegr |
| “ | Cyrhaeddodd y pwynt gyda fy mhartner lle symudodd i mewn gyda'i rieni yn ystod y cyfnod clo. Y pwysau o ofalu am fy mam a phopeth arall. Roedden ni wedi cael digon.”
- Gofalwr di-dâl, Lloegr |
Disgrifiodd rhai gofalwyr di-dâl hefyd yr effaith bersonol o ofalu am sawl person, er enghraifft plant sy'n oedolion anabl neu briod a'u rhieni eu hunain, wrth wneud gwaith â thâl a chyfrifoldebau teuluol eraill.
| “ | Mae gan fy mab wyth gofalwr sy'n cylchdroi ac yn gwneud sifftiau. Daeth hynny i gyd i ben yn ystod y pandemig. Roeddwn i'n gofalu amdano, symudodd fy mam i mewn ac roeddwn i'n gofalu amdani hi, roedd hi'n hen iawn, ac mae gen i fy merch. Roeddwn i'n teimlo fel pe bai fy hun a fy mywyd cyfan yn cael ei rannu mewn tair ffordd.”
- Gofalwr di-dâl, Lloegr |
Straeon gan ofalwyr di-dâlMewn Digwyddiad Gwrando ar-lein gyda gofalwyr di-dâl gyda Carers UK, dywedodd y rhan fwyaf o'r cyfranwyr wrthym sut roeddent yn teimlo nad oeddent yn cael eu gwerthfawrogi gan weddill cymdeithas am y gefnogaeth yr oeddent yn ei darparu, y pwysau yr oeddent oddi tano a'r doll yr oedd gofalu ar wahân yn ystod y cyfnod clo yn ei gymryd arnynt. Atgyfnerthwyd hyn ymhellach gan arddangosiadau cyhoeddus o werthfawrogiad a chefnogaeth i'r gweithlu iechyd a gofal cymdeithasol nad oedd yn cynnwys gofalwyr di-dâl. |
|
| “ | Dw i'n meddwl bod yr unigedd yn wirioneddol, wirioneddol llym, doedd neb yn gofalu amdanom ni, doedd ein [archfarchnad leol] ddim yn agor yn gynnar i ofalwyr. Roedden ni wir ar ein pennau ein hunain.”
– Gofalwr di-dâl, digwyddiad gwrando |
| “ | Doedd neb yn poeni amdano ni. Neb. Rydyn ni'n cymeradwyo dros ofalwyr, ond wnaethon ni ddim cymeradwyo droson ni oedd yn ymladd y tu ôl i ddrysau caeedig.”
– Gofalwr di-dâl, digwyddiad gwrando |
| “ | Rydych chi'n teimlo'n ynysig iawn. Does neb yn ffonio i ddweud, dim hyd yn oed galwad ffôn i ddweud, sut wyt ti, gartref yn llawn amser yn gofalu am ddau berson sy'n wirioneddol sâl? Rydw i wedi blino'n llwyr, mae gen i PTSD [anhwylder straen wedi trawma], blinder tosturi, hynny i gyd o fy rôl ofalu. Does neb yn poeni, oherwydd maen nhw'n meddwl eich bod chi'n nyrs. Ac wyddoch chi, os oes rhywbeth o'i le, rydych chi'n rhy flinedig i ofyn am help. Fel mae llawer o'r bobl eraill hyn yn ei ddweud, os oes angen help arnoch chi, wyddoch chi, mae'n rhaid i chi ymladd amdano, ymladd ac ymladd ac ymladd.”
– Gofalwr di-dâl, digwyddiad gwrando |
| “ | Arferai gofalwyr allu cael gofal seibiant. Yn sydyn, yn ystod Covid, doedd dim amser i ddianc i amgylchedd lle gallech chi fod yn chi'ch hun neu gyda phobl eraill sydd â phrofiadau tebyg, neu efallai dim ond cymryd amser i ffwrdd. Felly, roeddech chi'n gofalu am bobl yn gyson 24 awr a llai amdanoch chi'ch hun. Roedd yn bryder ac yn anobaith eithafol."
– Gofalwr di-dâl, digwyddiad gwrando |
Pobl ag anghenion gofal a chymorth a theimladau o unigrwydd ac arwahanrwydd
Dywedodd gweithwyr gofal cartref wrthym fod y rhai yr oeddent yn gofalu amdanynt wedi dod yn bryderus ac yn bryderus yn ystod y pandemig. Daeth rhai yn emosiynol yn ôl ac fe wnaethant roi'r gorau i ymgysylltu ag eraill. Clywsom hefyd gan weithwyr gofal cartref am sut yr achosodd unigrwydd ac arwahanrwydd pobl ag anghenion gofal a chymorth golli archwaeth neu ddiddordeb mewn bwyd neu ddiffyg cymhelliant i goginio a bwyta ar eu pen eu hunain.
| “ | Aeth llawer ohonyn nhw'n isel eu hysbryd, wyddoch chi, yn ddagreuol iawn ac yn bryderus. Roedd un o fy merched yn ddall, mae hi wedi marw nawr yn drist. Felly, gallwch chi ddychmygu, roedd hi'n ddall ac felly roedd hi'n ddigon anodd fel yr oedd hi gyda hi. Ac yna, hynny ar ben hynny pan nad oedd ganddi gwmni fel y cyfryw ar wahân i mi fy hun, a oedd yn dibynnu ar ba ddiwrnod ac fel arfer, weithiau dim ond dwy awr, weithiau tair awr, weithiau pedair awr yn dibynnu. Ie, felly roedd hi'n ei chael hi'n anodd iawn.”
- Gweithiwr gofal cartref, Cymru |
| “ | Doedden nhw ddim eisiau bwyta, fel, fe aethon nhw oddi ar eu bwyd ac oherwydd iechyd meddwl yn amlwg fe benderfynon nhw nad oedden nhw'n mynd i fwyta.”
- Gweithiwr gofal cartref, Lloegr |
Mewn rhai achosion, ymatebodd pobl ag anghenion gofal a chymorth i deimladau o unigrwydd ac arwahanrwydd drwy ymosod ar eraill, gan anafu eu hunain yn anfwriadol mewn rhai achosion. Newidiodd y pandemig safbwyntiau gweithwyr gofal hefyd ar yr hyn yr oedd yn rhaid ei flaenoriaethu ac fe daeth anoddach monitro ymddygiadau a oedd angen sylw manwl a phryderon diogelu gan na allent ymweld â phobl yn bersonol. Roedd hon yn broblem benodol i rai pobl awtistig o oedran gweithio, oedolion ag anabledd dysgu a phobl hŷn â dementia.
| “ | Roedd gennym ni drigolion yn byw gyda dementia. Roedd ymddygiad mwy heriol yn dod yn amlwg. Oherwydd eu bod nhw'n rhwystredig ac ar eu pen eu hunain.”
- Gweithiwr cartref gofal, Cymru |
Myfyriodd cyfranwyr ar pa mor anodd oedd hi i rai pobl adennill annibyniaeth ar ôl i'r cyfyngiadau symud gael eu llacio a dechreuodd cymdeithas agor eto.
| “ | Roeddwn i'n arfer bod yn gerddwr da, byddwn i'n cerdded i bobman. Ac nawr mae gen i drafferth hyd yn oed mynd allan o'r drws. Felly weithiau dw i'n teimlo'n well os ydw i'n ynysu fy hun ac yn y pen draw, dydw i ddim yn mynd i unman.”
- Person ag anghenion gofal a chymorth, Lloegr |
| “ | Sylwais fod rhai ohonyn nhw'n llai tebygol o wneud pethau drostyn nhw eu hunain oherwydd eu bod nhw mor gyfarwydd â phobl yn eu gwneud drostyn nhw. Yn ystod Covid fe wnaethon nhw stopio, felly dw i'n meddwl nad oedd rhai pobl wedi mynd yn ôl eto yn amlwg oherwydd, wyddoch chi, po hynaf ydych chi, y anoddaf ydyw. Felly, doedd rhai ohonyn nhw byth yn gallu mynd yn ôl allan ar ôl meddylfryd Covid a dyna lle byddai eu bywyd wedi newid, mewn gwirionedd yn ystod Covid.”
- Gweithiwr gofal cartref, Lloegr |
Mynediad at gefnogaeth gymunedol a chysylltiadau cymdeithasol
Roedd llawer o bobl ag anghenion gofal a chymorth sy'n byw ar eu pen eu hunain neu sy'n cael gofal gan deulu yn teimlo'n ddiymadferth ac yn methu â rheoli eu bywydau beunyddiol gan fod llawer o'r gwasanaethau cymorth yr oeddent yn dibynnu arnynt wedi cau yn ystod y cyfnod clo ac wedi cymryd amser hir i ailagor.
| “ | Daeth canolfannau oedolion i ben, daeth popeth i ben, doedd dim tripiau iddyn nhw mwyach, wnaethon nhw ddim dechrau mynd i'r ganolfan oedolion eto tan ymhell ar ôl i bopeth arall agor eisoes.”
– Gweithiwr gofal cartref, Gogledd Iwerddon |
Roedd rhai pobl ag anghenion gofal a chymorth yn mewn gofid mawr oherwydd y newid sydyn yn eu trefn arferol a'r aflonyddwch a'r golled lwyr o'u gweithgareddau arferol a chefnogaeth y gymunedDywedodd rhai gofalwyr di-dâl sy'n gofalu am oedolion ag anabledd dysgu neu bobl awtistig fod eu perthnasoedd dan straen oherwydd y newidiadau hyn, yn enwedig lle nad oedd y bobl yr oeddent yn gofalu amdanynt yn gallu deall beth oedd yn digwydd a pham. Mewn rhai achosion, roedd pobl ag anghenion gofal a chymorth yn tybio mai penderfyniad eu gofalwyr oedd hwn, gan gredu eu bod yn cael eu cadw oddi wrth bobl eraill, a arweiniodd at wrthdaro a rhwystredigaeth i bawb dan sylw.
| “ | [Pan aeth hi o chwe awr y dydd gyda gofalwyr i ddim] roedd hi'n meddwl mai dim ond rhywbeth roeddwn i'n ei wneud oedd e: roeddwn i'n ei chadw hi i mewn, doeddwn i ddim yn caniatáu iddi fynd i gwrdd â'i ffrindiau. Felly, fe wnaethon ni ddadlau cryn dipyn.”
– Gofalwr di-dâl sy'n byw gyda'r person y maent yn gofalu amdano, Cymru |
Cafodd y golled hon o drefn effaith niweidiol iawn. Disgrifiodd gofalwyr di-dâl bobl ag anghenion gofal a chymorth, yn enwedig pobl awtistig ac unigolion ag anabledd dysgu, gan arddangos ymddygiadau yr oeddent yn eu cael yn heriol ac yn ofidus i ddelio â nhw..
| “ | Collodd fy mhlentyn awtistig ei threfn arferol a fyddai’n arwain at gyfnodau anodd a theimlo’n llethol nad oedd hi’n cael seibiant o’r amgylchedd cartref gwenwynig. Effeithiodd ar ei chwsg a’i hymddygiadau; byddai hi’n cysgu am bedair awr y nos yn unig ac roedd hi’n ymosodol iawn tuag ataf gan mai dyna oedd ei hunig ffordd o gyfleu’r effaith.”
– Gofalwr di-dâl yn byw gyda'r person y maent yn gofalu amdano, Lloegr |
Stori Anne a TimAnne, sy'n byw yng Ngogledd Iwerddon, oedd gofalwr di-dâl ei mab Tim, 23 oed, sydd ag awtistiaeth ddi-eiriau. Cyn y pandemig roedd Tim yn byw gartref ac yn mynychu canolfan ddydd i oedolion, lle'r oedd wrth ei fodd ac yn gwneud yn dda iawn. Newidiodd hyn i gyd yn ystod y cyfnod clo. Pan na allai Tim fynd i'r ganolfan ddydd i oedolion a oedd ar gau yn ystod y cyfnod clo, tarfwyd ar ei drefn arferol ac effeithiodd hyn ar ei ymddygiad a'i lesiant. |
|
| “ | Roedd e’n tynnu arnoch chi’n gyson i wisgo ei ddillad, i wisgo ei gôt, i gael ei fag i fynd i’r ganolfan oedolion. Roedd e jyst yn canolbwyntio’n fawr ar fynd yn ôl i’r ganolfan oedolion. Dyna oedd e eisiau ei wneud.” |
| “ | Roedd e’n aros yn gyson i’r bws ddod. Roedd ganddo fag gyda ffolder ynddo fel ffolder dyddiol lle roedden nhw’n ysgrifennu pa fath o ddiwrnod oedd ganddo. Roedd hwnnw yn ei ddwylo drwy’r amser. Roeddwn i wedi sylwi bryd hynny nad oedd e’n cysgu o gwbl bryd hynny. Doedd e ddim yn cysgu. Roedd e efallai’n cael 40 munud y nos. Gweddill yr amser roedd e’n gynhyrfus iawn, yn rhedeg i fyny ac i lawr y grisiau, yn rhoi cynnig ar bob drws yn gyson.” |
| Er bod Anne wedi mynd â Tim am dro i fynd allan o'r tŷ, roedd yn dal yn gynhyrfus ac yn ymosod yn gorfforol mewn ffordd nad oedd wedi'i gwneud ers pan oedd yn blentyn ifanc. | |
| “ | Rydyn ni'n cael ein brathu. Mae'n brifo ei hun. Mae hefyd yn brathu ei hun ac yna byddai'n difrodi'r tŷ. Byddai'n cicio drysau.” |
| Effeithiodd hyn ar y teulu cyfan gan gynnwys ei frodyr a'i chwiorydd iau a oedd hefyd yn byw yn y cartref. | |
| “ | Roedd fy merch yn ceisio astudio ar gyfer ei TGAU gyda fy mab [awtistig] nad oedd yn cysgu o gwbl ac yn swnllyd iawn. Felly, roedd yn rhaid i [fy mhlant iau] gael cloeon ar gyfer drysau eu hystafelloedd gwely, felly roedd yn rhaid iddyn nhw gloi eu hunain yn eu hystafelloedd gwely yn y nos oherwydd ei fod yn gyson yn agor yr holl ddrysau, yn troi'r holl oleuadau ymlaen. Byddai'n rhedeg o amgylch y tŷ o ystafell i ystafell.” |
| Ymyrrodd y gwasanaethau cymdeithasol oherwydd pryderon ynghylch yr effaith ar y brodyr a'r chwiorydd a'r risg tân o blant yn cael eu cloi yn eu hystafelloedd gwely yn y nos. Effeithiodd straen gofalu am Tim heb gefnogaeth y teulu ehangach ar iechyd Anne a'i gallu i ymdopi hefyd. | |
| “ | Dim ond blinedig fel asgwrn. Roedd gen i bryder. Roedd gen i iselder. Roedd gen i bethau nad oeddwn i erioed wedi'u cael o'r blaen.” |
| O ganlyniad i effeithiau'r cyfyngiadau symud a chau'r ganolfan oedolion ar ymddygiad ac iechyd meddwl Tim ei hun, y straen ar Anne a'r effeithiau ar ei phlant eraill, symudwyd Tim i leoliad byw â chymorth yn ystod 2021 ac nid yw wedi bod yn gartref i dŷ ei fam ers hynny. | |
| “ | Mae'n anodd iawn i mi ymweld â Tim oherwydd ei fod mor ofidus. Dydy o dal ddim yn teimlo'n naturiol i mi fod dieithriaid yn gofalu am fy mab, ac roeddwn i'n meddwl yn gryf y byddwn i'n dod ag e'n ôl adref unwaith y byddai'r ganolfan oedolion yn ôl. Mae Tim wedi ei gwneud hi'n glir iawn nad yw am ddod adref gyda mi ac na fydd hyd yn oed yn dod adref am ymweliad.” |
| Mae Anne yn teimlo pe bai'r ganolfan ddydd i oedolion wedi aros ar agor yn ystod y pandemig na fyddai dim o hyn wedi digwydd a byddai Tim yn dal i fyw gartref gyda hi. | |
Storïaid o GaerliwelyddMewn Digwyddiad Gwrando gyda Carlisle Eden Carers, sefydliad cymorth penodol ar gyfer gofalwyr di-dâl, clywsom sut y sefydlodd awdurdodau lleol ac elusennau brosiectau i helpu pobl sy'n byw ar eu pen eu hunain nad oeddent yn gallu cael cymorth gan ffrindiau a theulu. Fel arfer, roedd y prosiectau hyn yn cynnwys gwirfoddolwyr yn ffonio pobl i gael sgyrsiau, darparu gwybodaeth a chefnogi eu hiechyd corfforol a meddyliol. |
|
| “ | Sefydlwyd dau brosiect a gafodd effaith gadarnhaol: 'Cadw Pobl yn Gysylltiedig a 'Llwybr Sero', y ddau yn cynnwys galw pobl i fynd i'r afael ag unigrwydd ac arwahanrwydd a hefyd i ddarparu gwybodaeth glir.”
– Cyfrannwr Every Story Matters, digwyddiad gwrando, Lloegr |
| “ | Roedden ni’n gwirio ac yn cael sgyrsiau gyda phobl oedd wedi’u hynysu ac yn byw am eich galwad chi gyda llawer o alwadau. Roedden ni’n gallu meithrin perthynas wych gyda nhw. Roedd yn brofiad gostyngedig a sobr. Roedd hi’n teimlo’n anodd iawn dod â’r prosiect i ben pan oedd y prosiect drosodd. Roedd yn ofnadwy iawn; rydyn ni’n bobl ofalgar ac eisiau achub pawb. Roedd hi’n teimlo fel pe baen ni’n gwnselydd neu’n therapydd iddyn nhw erbyn y diwedd.”
– Cyfrannwr Every Story Matters, digwyddiad gwrando, Lloegr |
Trafododd y rhai a oedd yn derbyn gofal gan anwyliaid nad oeddent yn byw gyda nhw neu a oedd yn dibynnu ar rwydweithiau ehangach hefyd sut roedd yn rhaid iddynt dysgu sut i ddefnyddio technolegau newydd fel Zoom neu FaceTime yn ystod y cyfnod clo cyntaf er mwyn iddyn nhw allu cadw mewn cysylltiad â theulu a ffrindiau.
| “ | Dydw i ddim yn dda iawn gyda thechnoleg, dydw i ddim yn deall y sgwrs Zoom yma a phethau fel 'na…felly roedd rhaid i mi ddysgu cadw mewn cysylltiad â theulu a ffrindiau.”
– Person ag anghenion gofal a chymorth, Lloegr |
| “ | Roedd rhaid i mi ddysgu Skype a Zoom…technoleg yw’r peth a’n daeth â ni at ein gilydd. Cymuned yw popeth.”
– Person ag anghenion gofal a chymorth, Lloegr |
Cyfyngiadau ar symud preswylwyr o fewn cartrefi gofal
Sut y rheolwyd symudiadau trigolion
Cafodd pobl sy'n byw ac yn gweithio mewn cartrefi gofal eu heffeithio'n fawr gan gyfyngiadau symud a phellhau cymdeithasol. Cymerodd cartrefi gofal wahanol ddulliau o weithredu cyfyngiadau gyda rhai yn cadw pobl yn eu hystafelloedd drwy'r amser, tra bod eraill yn ceisio cael cyfyngiadau ar waith dim ond pan oedd achosion positif o Covid-19, neu pan oedd preswylwyr yn cael eu hynysu ar ôl cael eu rhyddhau o'r ysbyty.
Ni allai trigolion oedd yn ynysu ddefnyddio mannau cymunedol fel ystafelloedd cyffredin, ystafelloedd bwyta a llyfrgelloedd. Yn ystod cyfnodau o ynysu, rhoddwyd y gorau i weithgareddau a chymerwyd prydau bwyd i'w hystafelloedd, ac roedd hyn yn atal trigolion rhag cymdeithasu â'i gilydd.
| “ | Meddyliwch mai dim ond peidio â gweld pobl oedd e. Cael eich cau i ffwrdd. Yn amlwg, wyddoch chi, doedd neb yn cael mynd i mewn i unrhyw un o'r mannau cymunedol. Roedd pawb wedi'u cyfyngu i'w hystafelloedd.”
– Person ag anghenion gofal a chymorth, Lloegr |
| “ | Doeddwn i ddim yn mynd allan o fy ystafell. Doeddwn i ddim yn mynd i lawr am ginio. Bydden nhw'n ei adael neu efallai'n gwisgo mwgwd ac yn ei ddod i mewn neu'n ei adael ar fy silff. Doedden ni ddim yn mynd i lawr am weithgareddau cymdeithasol. Roeddwn i ychydig flynyddoedd yn iau ac yn fwy symudol, ond ie, rydych chi'n colli'r cwmni.”
– Person ag anghenion gofal a chymorth, Lloegr |
Roedd bod yn gyfyngedig i'w hystafell yn arbennig o anodd i breswylwyr nad oeddent yn gallu deall pam roedd hyn yn digwydd. Treuliodd staff cartrefi gofal amser yn gwirio preswylwyr â dementia pan oeddent wedi'u hynysu ac wedi'u cyfyngu i'w hystafell. Roedd hyn yn golygu bod ganddyn nhw lai o amser i'w dreulio yn darparu gofal i eraill.
| “ | Roedd rhai yn iawn gyda aros yn eu hystafelloedd. Y rhai heb gymaint o gapasiti, doedden nhw ddim yn gallu deall. Dw i'n meddwl eu bod nhw'n teimlo eu bod nhw'n cael eu cosbi am rywbeth nad oedden nhw'n gwybod eu bod nhw wedi'i wneud.”
– Gweithiwr cartref gofal, Lloegr |
| “ | Roedd yn gyfnod arwyddocaol [o amser] ac roedd yn anodd bryd hynny pan oedd gennych chi unigolion â dementia nad oeddent yn deall na allent adael eu hystafell, yn ceisio gadael eu hystafell, wyddoch chi ac yn amlygu pawb i risg haint…roedd hynny'n her eithaf anodd.”
– Gweithiwr cartref gofal, Cymru |
Roedd sut roedd staff yn gweithredu cyfyngiadau yn dibynnu ar faint, cynllun ac oedran y cartref gofal a'r hyn yr oeddent yn ei ystyried yn ymarferol ac yn bosibl o ystyried adeilad a chyfleusterau'r cartref. Er enghraifft, roedd rhai cartrefi gofal yn gallu parhau â rhai gweithgareddau cymunedol, trwy gael preswylwyr i sefyll wrth ddrws eu hystafell, lle gallent siarad a chymryd rhan mewn gweithgareddau grŵp. Clywsom sut roedd ansawdd bywyd preswylwyr yn well lle'r oedd cartrefi gofal yn dod o hyd i ffyrdd o ganiatáu symudiad a rhyngweithio parhaus.
| “ | Gwnaeth [y staff] bopeth o fewn eu gallu i ni ac roedd gennym ni weithgareddau prynhawn o hyd…crefftau, ymarfer corff, cawson ni gwis…roedden ni’n gwerthfawrogi hynny’n fawr.”
– Person ag anghenion gofal a chymorth, Lloegr |
Er mwyn cadw symudiadau o fewn cartrefi gofal i'r lleiafswm ond sicrhau nad oedd y rhai heb Covid-19 yn cael eu cyfyngu, dywedodd cyfranwyr wrthym fod weithiau byddai llawr neu ardal benodol yn cael ei dynodi ar gyfer ynysu preswylwyrRoedd cartrefi gofal eraill yn trefnu rhannau o'r cartref gofal yn adrannau neu 'swigod', a oedd yn golygu y gallai pobl â dementia ryngweithio â'i gilydd ond i ffwrdd o breswylwyr eraill y cartref gofal.
| “ | Roedd rhai yn ofidus iawn. Maen nhw'n hoffi eu harferion arferol. Maen nhw'n hoffi pethau cyfarwydd ac ni ellid cyfyngu rhai preswylwyr i'w hystafelloedd oherwydd eu bod nhw'n crwydro ac nid ydyn nhw'n ddiogel, felly roedd yn rhaid i ni wneud darpariaethau i lawr yma, fel y gallen nhw fod mor ddiogel ag y gallen nhw fod. Fe wnaethon ni hysbysu atal heintiau, 'Ni allwn atal y crwydriaid rhag cymysgu,' ac fe ddywedon nhw'n y bôn, 'Wel, arsylwch a beth fydd yn digwydd'.”
– Gweithiwr cartref gofal, Lloegr |
Esboniodd y staff sut roedd sicrhau bod trigolion yn aros yn yr ardaloedd hyn yn anodd ei orfodi, yn enwedig i bobl awtistig ac unigolion ag anabledd dysgu neu ddementia. Roedd yr amhariad ar drefn arferol y preswylwyr yn golygu eu bod yn aml yn ddryslyd ac nad oeddent yn deall pam roedd yn rhaid iddynt aros yn eu hystafell eu hunain neu yn eu man dynodedig.
| “ | Roedd gennym ni bobl ag anableddau dysgu gydag awtistiaeth, ni allent aros mewn un lle ac nid oeddent yn deall am reoli heintiau, felly roedd hi'n anodd i aelodau staff geisio gwahanu'r preswylwyr oddi wrth ei gilydd pan nad oeddent yn deall yn iawn ac nad oedd ganddynt y gallu i wybod beth oedd yn digwydd.”
– Gweithiwr cartref gofal, Lloegr |
I breswylwyr cartrefi gofal eraill a oedd â'r gallu i ddeall y cyfyngiadau, roedd cael gwybod am newidiadau yn y cartref trwy hysbysiadau ysgrifenedig neu esboniadau llafar yn cael ei werthfawrogi.
| “ | Cawson ni ein prydau bwyd yn ein hystafelloedd…mae gennym ni gogydd da iawn, trefnydd da, gyda’i staff. Aeth popeth yn esmwyth. Fe syrthiodd i’w le, popeth oedd yn digwydd yma. Cawson ni ein hysbysu, roedd hynny’n beth pwysig.”
– Person ag anghenion gofal a chymorth, Lloegr |
| “ | Daethant atom ni a siarad â ni neu byddai hysbysiadau wedi'u hargraffu. Roedden ni'n gwybod beth oedd yn digwydd. Roeddwn i'n ddigon ffodus; gallwn i ddeall y cyfan. Yn amlwg, roedd gan y menywod oedd â dementia fwy o broblem.”
– Person ag anghenion gofal a chymorth, Lloegr |
Fodd bynnag, ar adegau Roedd staff cartrefi gofal yn teimlo bod egluro'r rheolau ac ateb cwestiynau ynghylch pam na allai preswylwyr symud o gwmpas y cartref yn rhydd yn heriolRoedd sawl rheswm dros hyn. Weithiau roedd ganddyn nhw deimladau cymysg am y cyfyngiadau ac ar rai achlysuron roedd eu hymatebion yn arwain at wrthdaro. Mynegodd staff cartrefi gofal deimladau o euogrwydd am orfodi'r rheolau atal heintiau a chynyddu unigedd preswylwyr.
| “ | Roedd rhaid i breswylwyr ymdopi â byw mewn ystafell fach, ynysig, heb unrhyw gyswllt â'u teuluoedd na'i gilydd. Rhoddodd hyn straen enfawr ar y gweithwyr gofal, a gafodd eu peledu â chwestiynau, eu hymosod a heb ateb i'w roi, gyda'r esboniadau'n anghredadwy i'r preswylwyr.
– Gweithiwr cartref gofal, Lloegr |
Effaith cyfyngiadau ar symudCafodd cyfyngiadau ar symud mewn cartrefi gofal effaith ddofn ar rai preswylwyr cartrefi gofal, yn cyfyngu ar eu gallu i gymryd rhan yn eu gweithgareddau cymdeithasol arferol a rhyngweithio â phreswylwyr eraill cartrefi gofalRoedd anwyliaid yn poeni am yr unigedd a brofwyd gan breswylwyr mewn cartrefi gofal, heb eu cyswllt teuluol arferol na'u gweithgareddau cymdeithasol. Dywedodd llawer fod aelod o'u teulu neu ffrind a oedd yn byw mewn cartref gofal yn unig, ynysig ac yn isel eu hysbryd. Achosodd hyn lawer o dristwch a phryder i aelodau'r teulu.
| “ | Roedden ni’n bryderus iawn ynglŷn â pha lefel o gyfathrebu roedd mam yn ei gael. Oedd unrhyw un hyd yn oed yn eistedd i lawr gyda hi am ychydig funudau’r dydd dim ond i siarad â hi? Byddwn i’n synnu’n fawr.”
– Anwylyd preswylydd cartref gofal, Gogledd Iwerddon |
| “ | Ar y ffôn, dywedodd, 'Dw i wedi diflasu, alla i ddim mynd allan, alla i ddim mynd allan.' iddi hi roedd yn gyfnod eithaf unig. Dw i'n meddwl ei fod yn eithaf dryslyd iddi hi. Ac ie, byddwn i'n dweud, o farnu yn ôl rhai o'i hymddygiadau, ei fod mewn gwirionedd yn eithaf gofidus iddi hi, a oedd yn ei dro yn ofidus i mi.”
– Anwylyd preswylydd cartref gofal, Lloegr |
Nid oedd pob profiad cartref gofal yr un fath. I rai pobl oedd yn byw mewn cartrefi gofal, roedd y pandemig yn llai heriol. oherwydd nad oedd y cyfyngiadau'n newid eu harferion a'u gweithgareddau arferol. Dywedodd rhai nad oedd gorfod aros yn eu hystafelloedd drwy'r dydd oherwydd y cyfyngiadau symud wedi newid eu bywydau'n sylweddol. Hyd yn oed cyn y pandemig, roeddent yn aml yn aros y tu mewn i'r cartrefi gofal, neu yn eu hystafelloedd ac yn cadw eu hunain yn brysur yn gwylio'r teledu, yn gwrando ar gerddoriaeth neu'n darllen.
| “ | Roedden nhw’n dod â fy mhrydau bwyd ataf bob dydd.…Doedd e byth wedi cael effaith wirioneddol ar fy mywyd. Ac roedd gen i fy ngliniadur gyda mi…Defnyddiais y Rhyngrwyd [hono] oedd fy nghyswllt â’r byd y tu allan, oherwydd roeddwn i wedi fy nghysylltu â ffrindiau a theulu.”
– Person ag anghenion gofal a chymorth, Lloegr |
Straeon o WrecsamMewn digwyddiadau gwrando gyda chartrefi gofal a nyrsio yn Wrecsam, rhannodd trigolion pa mor ffodus yr oeddent yn teimlo i fod yn byw mewn cartref gofal yn ystod y pandemig, gan eu bod yn agos at bobl eraill ac nid mor ynysig ag y byddent wedi bod yn byw ar eu pen eu hunain. |
|
| “ | Roeddwn i'n hoffi bod gen i bobl o'm cwmpas pan oeddwn i yn y cartref gofal, roeddwn i bob amser yn gallu siarad â phobl.”
– Person ag anghenion gofal a chymorth sy'n byw mewn cartref gofal, digwyddiad gwrando, Cymru |
| “ | Roeddwn i wedi fy nghloi yn fy ystafell gyda'r cyfyngiadau symud, byddai pobl yn curo ar fy nrws i roi sudd oren i mi weithiau. Roedd yn braf. Doedden ni ddim wedi cael hi'n rhy ddrwg mewn gwirionedd.”
– Person ag anghenion gofal a chymorth sy'n byw mewn cartref gofal, digwyddiad gwrando, Cymru |
Steve ac Irene storiMae Steve ac Irene yn byw yng Ngogledd Lloegr ac wedi bod yn briod ers 45 mlynedd. Ar ddechrau'r pandemig, roedden nhw ill dau yn 92 oed. Gofalodd Steve am Irene gartref am flynyddoedd lawer, fodd bynnag, ar ôl cwymp a achosodd waedu ar yr ymennydd, cafodd ei dderbyn i'r ysbyty. Ychydig cyn y cyfnod clo cyntaf, dychwelodd Steve adref o'r ysbyty, ond nid oedd yn gallu gofalu am Irene mwyach na byw'n annibynnol. |
|
| “ | Gartref, roedd hynny'n anodd oherwydd roeddwn i'n gallu siopa o'r blaen a bod, fel, yn brif ofalwr, ond roeddwn i'n ofalus iawn ac yn poeni oherwydd na allwn i wneud y pethau hynny mwyach.” |
| Fe wnaeth merch Steve ac Irene eu helpu i ddod o hyd i le mewn cartref gofal trwy ffrind i'r teulu ar ddechrau'r pandemig. Bedwar diwrnod ar ôl gadael yr ysbyty, symudodd Steve ac Irene i'r cartref gofal, gan eu bod yn poeni am beidio â gallu mynd i mewn, gan fod staff y cartref gofal wedi cynghori y byddai'n rhaid iddynt gloi'r cartref yn fuan. Am y tri i bedwar mis cyntaf, roedd yn rhaid iddynt aros yn eu hystafell a rennir ac ni wnaethant ryngweithio ag unrhyw breswylydd arall.
Roedd Steve ac Irene yn gymharol fodlon â'u sefyllfa byw gan eu bod yn derbyn gofal a chefnogaeth dda ac roeddent yn teimlo bod y pandemig yn rhywbeth a oedd yn digwydd y tu allan i bobl eraill. |
|
| “ | Doedden ni ddim yn sylweddoli pa mor ddrwg oedd e. Roedden ni’n lwcus, doedd gennym ni ddim syniad bach ohono yma, oherwydd roedden ni’n cael ein cadw yn ein hystafelloedd ac yn cael gofal ac roedd y staff bob amser yn gwisgo masgiau pan oedden nhw’n dod i mewn.” |
| Dros gyfnod y pandemig, gwellodd iechyd Steve tra bod anghenion gofal Irene wedi cynyddu. Wrth edrych yn ôl ar y pandemig, roeddent yn gwerthfawrogi ac yn mwynhau'r amser a dreuliasant gyda'i gilydd ac yn teimlo eu bod yn cael cefnogaeth dda gan y cartref gofal. | |
| “ | Ar yr adeg benodol honno, doedden ni ddim yn gallu gofalu amdanom ni ein hunain mewn sawl ffordd. Rydw i wedi gwella llawer; dim ond fy nghydbwysedd sydd gen i broblemau ag ef nawr. Felly, a dweud y gwir, doedd effeithiau Covid ddim yn effeithio arnom ni gymaint ag ar bobl eraill. Roedden ni yn ein hystafell ni; roedden nhw'n gofalu amdanom ni pryd bynnag roedden ni eisiau ac roedden ni'n gofalu am ein gilydd.” |
Disgrifiodd staff gofal sut y dirywiodd iechyd corfforol a meddyliol preswylwyr yn ystod y cyfnod clo. Effeithiwyd yn arbennig ar symudedd a gallu gwybyddol gan fod preswylwyr yn treulio cymaint o amser yn eistedd yn eu hystafelloedd ar eu pen eu hunain. Awgrymodd staff cartrefi gofal fod mwy o'u preswylwyr bellach mewn iechyd gwaeth o'i gymharu â'r rhai yr oeddent yn gofalu amdanynt cyn y pandemig.
| “ | Dirywiodd ei dementia yn gyflym pan ddigwyddodd y cyfyngiadau symud ac nid oedd ganddi unrhyw gefnogaeth gan ei theulu. Felly, nid oedd hi wedi cael ei theulu i ddod i'w gweld. Collodd ei holl ewyllys i raddau. Doedd hi ddim yn poeni. Gwrthododd o ddifrif. Gallwch chi siarad â nhw dros y ffôn. Ond nid oedd hi'n deall mai ei merch neu ei mab neu ei hwyrion oedd hi'n siarad â nhw, oherwydd nad oedd hi'n gallu gweld eu hwyneb yn gorfforol.
– Gweithiwr cartref gofal, Gogledd Iwerddon |
| “ | Daeth ffrind oedrannus mewn cartref gofal yn fwyfwy isel ei ysbryd oherwydd y cyfnod clo. Cafodd ymweliad brys â'r deintydd, cafodd ei chloi yn ei hystafell am bythefnos, mewn cwarantîn. Ar ôl y cwarantîn hyn, collodd y gallu i ganolbwyntio a rhoddodd y gorau i ddarllen yn gyfan gwbl. Daeth yn isel ei hysbryd yn ddwfn.”
– Anwylyd preswylydd cartref gofal, Lloegr |
Dywedodd staff cartrefi gofal wrthym hefyd fod gwrthododd rhai trigolion fwyta neu fwytaodd lai wrth fwyta ar eu pennau eu hunain yn eu hystafelloedd heb ryngweithio cymdeithasol, anogaeth gan eu teuluoedd i fwyta, ac esiampl eraill yn bwyta o'u cwmpas. Mewn rhai achosion, daeth eu pwysau'n beryglus o isel. Arweiniodd hyn at staff gofal yn chwilio am gymorth a chyngor gan weithwyr gofal iechyd proffesiynol ynghylch diffyg maeth a sut i annog pobl i fwyta mwy.
| “ | Dw i'n meddwl mai dim ond yr agwedd gymdeithasol o allu mynd i mewn i ystafell fwyta ac eistedd i lawr a bwyta pryd o fwyd gyda phobl eraill, rydyn ni'n gweld gyda'r preswylwyr eu bod nhw'n tueddu i fwyta'n well mewn grwpiau. Ac nid yw'r rhai sy'n bwyta yn eu hystafelloedd yn gyffredinol yn bwyta cymaint ag y bydden nhw pe bydden nhw yn yr ystafell fwyta, gyda'r agwedd gymdeithasol.”
– Nyrs yn gweithio mewn cartref gofal, Lloegr |
| “ | Byddwn i'n dweud y preswylwyr hynny â dementia datblygedig, ie, oherwydd bod yr anwyliaid yn arfer dod i mewn, a byddai'n eu hannog i fwyta. Byddai rhai pobl yn annog eu hanwyliaid i fwyta, oherwydd eu bod nhw'n adnabod y person hwnnw. Felly, byddwn i'n dweud yn bendant ie, colli pwysau, trwy ddiffyg ysgogiad gan bobl maen nhw'n eu hadnabod.”
– Rheolwr cofrestredig cartref gofal, Lloegr |
| “ | Un o'n merched ni, byddai hi'n mynd trwy gylchoedd heb fwyta, colli pwysau, pethau fel 'na ac ... aeth hi i lawr i rywbeth fel, dyweder ei bod hi'n dair ar ddeg stôn, aeth hi i lawr i tua chwe stôn. Collodd lawer o bwysau ac roedd hi'n gwrthod bwyta, gwrthod popeth, ddim eisiau gofal personol.
– Gweithiwr cartref gofal, yr Alban |
Yn ogystal, ni fyddai rhai preswylwyr yn ymgysylltu â'r gweithgareddau a drefnir gan weithwyr gofal i gadw preswylwyr yn feddyliol egnïol ac yn ymgysylltu.
| “ | Roedden nhw wedi colli diddordeb oherwydd eu bod nhw allan o'u trefn arferol, allan o'r amgylchoedd cyfarwydd ac o bosibl yn gor-feddwl, rhywbeth y byddech chi'n ei wneud. 'Pam rydw i yma? Pam na allaf godi a cherdded? Pam?'”
– Gweithiwr cartref gofal, Lloegr |
Aina's storiMae Aina yn byw yng Nghanolbarth Lloegr. Mae hi wedi gweithio ym maes gofal cymdeithasol ers dros ddeng mlynedd ac yn ystod y pandemig, bu’n gweithio mewn cartref gofal a oedd yn darparu gofal nyrsio. Drwy gydol y pandemig, sylwodd fod preswylwyr cartrefi gofal yn mynd yn encilgar ac, ar adegau, roedd rhai’n ymddangos yn teimlo’n anobeithiol ac yn drist. Roedd rhai o’r bobl yr oedd hi’n gofalu amdanyn nhw’n ymddangos yn cau eu hunain i ffwrdd o’r byd. |
|
| “ | Doedd rhai o fy nghleientiaid ddim eisiau gwylio'r teledu na gwrando ar y radio hyd yn oed, felly'r adegau gyda'r gofalwyr, roedd yn bopeth ac yna, mwy o siarad am eu plentyndod ac roedden nhw'n drist iawn. Mae rhai ohonyn nhw wedi bod yn dweud, 'Rydw i eisiau marw.' Roedd yn dorcalonnus oherwydd rydych chi eisiau eu helpu, rydych chi'n ceisio, wyddoch chi, rhywsut i wneud eu bywyd yn well, yn fwy cyfforddus.” |
| Rhannodd Aina hefyd sut roedd y bobl yr oedd hi'n gofalu amdanyn nhw wedi rhoi'r gorau i fwyta gan eu bod nhw'n teimlo mor iselderus, yn encilgar ac ynysig. Cafodd hyn effaith ar eu hiechyd corfforol a'u symudedd a wnaeth eu gofal yn fwy cymhleth. | |
| “ | Maen nhw wedi rhoi’r gorau i fwyta, maen nhw’n wannach, felly rydyn ni’n ceisio dod o hyd i ffordd a cheisio gwneud iddyn nhw ddal gafael er mwyn sicrhau eu bod nhw ychydig yn gryfach. Aeth eu symudedd i lawr, roedd rhai bron â rhoi’r gorau iddi, [roedden nhw’n gofyn] ‘Beth sy’n mynd i fod nawr? Nawr mae pawb yn mynd i farw.’” |
| Yn aml, cysylltodd Aina â meddygon teulu a dietegwyr i gael cymorth gyda bwydo a sicrhau bod gan bobl ag anghenion gofal a chymorth y maeth cywir. Fodd bynnag, wrth fyfyrio ar ei phrofiad, teimlai, er gwaethaf eu hymdrechion i ddarparu gofal a chymorth, fod rhai pobl wedi 'rhoi'r gorau iddi' wrth iddynt gael eu gwahanu oddi wrth eu teulu a'u hanwyliaid, a dyma'r rheswm pam roedd rhai pobl wedi rhoi'r gorau i fwyta a bod eu hiechyd wedi gwaethygu. | |
| “ | Un person dw i'n meddwl amdano…dw i'n meddwl iddo roi'r gorau iddi. Roedd yn ormod, ond fel y dywedais i does gen i ddim prawf, alla i ddim dweud hynny'n sicr. Dw i'n credu nad oedd o'n gallu clywed llais ei wraig a'i ferch. Dydw i ddim yn dweud mai dyna'r prif reswm [dros ei farwolaeth], ond dw i'n dweud dyna pam y stopiodd fwyta'n llwyr.” |
Cyfyngiadau ar ymweld â chartrefi gofal
Barn anwyliaid ar gyfyngiadau ymweld
Roedd anwyliaid yn teimlo bod y cyfyngiadau ar ymweld â chartrefi gofal yn annheg i bobl ag anghenion gofal a chymorth sy'n byw mewn cartrefi gofalEr bod y cyfyngiadau wedi'u bwriadu i amddiffyn pobl rhag dal Covid-19, mewn rhai achosion disgrifiodd cyfranwyr sut y gwnaeth y cyfyngiadau arwain at niwed a gofid difrifol, yn enwedig i bobl awtistig, pobl ag anabledd dysgu a phobl â dementia. Er gwaethaf hyn, roeddent hefyd yn cydnabod bod angen y cyfyngiadau i amddiffyn trigolion.
| “ | Mae gan fy mab awtistiaeth ddifrifol ac anawsterau dysgu, nid oes ganddo leferydd a dealltwriaeth gyfyngedig, roedd mewn cartref gofal preswyl, doeddwn i ddim yn gallu ymweld ag ef am 24 wythnos, doedden ni ddim yn gallu ymweld trwy ffenestr na FaceTime gan na fyddai'n deall ac felly'n mynd yn ofidus, roedd yn ddewis rhwng ei gadw'n dawel neu ein cynhyrfu ni i gyd trwy ei weld trwy ffenestr.”
– Anwylyd preswylydd cartref gofal, Lloegr |
| “ | Ar y pryd, roeddech chi'n meddwl, 'Mae'n ormod', ond roedden nhw'n ceisio amddiffyn bywyd, onid oedden nhw. Doedd neb ohonom ni'n gwybod beth i'w wneud, felly roedden nhw'n llym iawn ac oni bai amdanyn nhw, byddem ni wedi colli mwy o fywydau.”
– Anwylyd preswylydd cartref gofal, yr Alban |
Dywedodd anwyliaid wrthym am yr effaith emosiynol sylweddol a gafodd cyfyngiadau ymweld arnyn nhw a'u hanwyliaid. Byddai colli mynediad i'r cartref gofal ei hun, ynghyd ag ymwybyddiaeth o'r pwysau ychwanegol y byddai staff yn delio â nhw, yn aml yn gwneud iddyn nhw deimlo'n bryderus ynghylch ansawdd y gofal a ddarperir mewn cartrefi gofal. Byddai'r teimladau hyn yn cael eu gwaethygu gan ymdeimlad o euogrwydd pan fyddai aelod o'r teulu'n symud i gartref gofal.
| “ | Doeddech chi ddim yn gallu mynd i'w weld. Gwnaeth hynny i mi deimlo'n euog am fy mhenderfyniad [i'w symud i'r cartref gofal ... roedd ein plant] bellach yn cael eu hatal rhag gweld eu tad.”
– Anwylyd preswylydd cartref gofal, Gogledd Iwerddon |
| “ | Roedd yn anodd iawn, iawn. Roedd fel profedigaeth, oherwydd roedd e’n rhywle ac allwn i ddim ei weld. Mae gen i deimladau euog o hyd fy mod i wedi colli’r holl ymweliadau hynny y byddwn i wedi’u gwneud [pe bawn i wedi gallu].”
– Anwylyd preswylydd cartref gofal, Lloegr |
Sut y cynhaliodd cartrefi gofal gyfyngiadau ymweld
Dywedodd staff cartrefi gofal wrthym pa mor anodd oedd hi i gadw i fyny â'r canllawiau a'r gweithdrefnau ar gyfer rheoli ymweliadau wrth i'r cyfyngiadau ar ymweld lacio.Er gwaethaf yr ansicrwydd, soniodd rheolwyr cofrestredig am eu penderfyniad i sicrhau bod staff, preswylwyr a theuluoedd mor gyfredol â phosibl gyda'r canllawiau. Siaradodd rhai am rannu gwybodaeth trwy e-byst neu gynhyrchu taflenni a roddasant i deuluoedd. Ychwanegodd hyn i gyd at eu llwyth gwaith.
| “ | Daeth y rhan gyfathrebu yn beth mawr iawn i mi, dim ond sicrhau bod pawb yn gwybod beth oedd yn digwydd a'n bod ni'n rhoi'r wybodaeth ddiweddaraf i'r holl berthnasau pan ddaeth canllawiau [ar gyfer rheoli ymweliadau] allan. Roedd adegau pan oedd efallai'n newid bob yn ail wythnos, felly byddem ni wedi'u rhoi nhw'n gyfredol.”
– Rheolwr cofrestredig cartref gofal, Lloegr |
| “ | Roedd pob preswylydd yn gallu cael un neu ddau bartner gofal a allai ddod i mewn ac ymweld ar unrhyw adeg. Felly, fe wnaethon ni drefnu hynny i gyd a rhoi'r holl waith papur yn ei le ar ei gyfer. Roedd yn gyson.”
– Gweithiwr cartref gofal, Lloegr |
Disgrifiodd gweithwyr cymdeithasol fod dan straen ac yn bryderus oherwydd y pwysau teuluoedd yn eu rhoi arnyn nhw i ymweld â'u hanwyliaid. Byddai'r teuluoedd hyn yn aml yn troi at eu gweithiwr cymdeithasol am gefnogaeth emosiynol ychwanegol ac am sicrwydd y byddai eu hanwylyd yn iawn. Byddai gweithwyr cymdeithasol yn cefnogi ei gilydd i reoli eu hemosiynau eu hunain.
| “ | Byddai'n rhaid i weithwyr cymdeithasol sy'n gweithio gyda'r teuluoedd hyn ddod i mewn a rhoi'r baich [i gydweithwyr] oherwydd bod y cyfan wedi'i daflunio arnyn nhw, y tristwch a'r pryder oedd gan deuluoedd am eu hanwylyd.”
– Gweithiwr cymdeithasol, Lloegr |
Roedd anwyliaid yn gallu ymweld â phobl mewn cartrefi gofal wrth i'r pandemig fynd rhagddo ac wrth i gyfyngiadau gael eu llacio. Gweithiodd cartrefi gofal yn galed i roi prosesau a gweithdrefnau ar waith a oedd yn caniatáu i deuluoedd a ffrindiau ymweld wrth atal lledaeniad yr haintEr enghraifft, roedd rhai cartrefi gofal yn caniatáu ymweld yn yr ardd neu drwy ffenestr neu'n gosod rhaniadau a phodiau plastig fel y gallai pobl aros ar wahân wrth barhau i gyfathrebu. Defnyddiodd eraill ystafelloedd cyfarfod ar gyfer ymweliadau â phobl ag anghenion gofal a chymorth.
| “ | Yna fe wnaethon nhw godi tŷ haf yn yr ardd, a oedd yn anhygoel. Roedd ganddyn nhw siaradwr dwy ffordd ac roedd ganddyn nhw Perspex drwodd. Felly, yna daeth hynny, dw i'n meddwl, pan wnaethon nhw gyflwyno hynny, roedd hynny fel bendith i mi.”
– Anwylyd preswylydd cartref gofal, Lloegr |
| “ | Roedd pod gwydr i lawr y grisiau ar y llawr cyntaf a dim ond dau [ymwelydd] oedd yn cael eu caniatáu ar y tro. Roedd ymwelwyr yn cael dod i mewn trwy fynedfa'r ardd, fel nad oeddent yn dod i mewn i'r cartref mewn gwirionedd. Ond roedd yn rhaid iddynt brofi bod ganddynt brawf Covid negyddol. Roedd yn rhaid iddynt hefyd gael eu tymheredd wedi'i gymryd. Roedden ni, y preswylwyr, yn eistedd yn yr ystafell i lawr y grisiau ac roedden ni'n gallu eu gweld nhw trwy'r pod ac roedd gennym ni setiau radio bach, fel y gallem gyfathrebu.”
– Person ag anghenion gofal a chymorth, Lloegr |
Anwyliaid wedi'u disgrifio mesurau rheoli heintiau eraill sydd ar waith mewn cartrefi gofal, a oedd yn cynnwys nifer gyfyngedig o bobl yn ymweld, archebu apwyntiadau, gwisgo PPE llawn, profi cyn mynd i mewn a drws ar wahân i fynd i mewn i'r cartref gofal. Roedd y rhan fwyaf o gartrefi gofal hefyd yn sicrhau bod cynhaliwyd pellhau cymdeithasol yn ystod ymweliadauRhai roedd anwyliaid yn canfod bod y protocolau ymweld hyn yn heriol, yn cymryd llawer o amser ac yn anodd addasu iddynt.
| “ | Byddai'n rhaid i ni ffonio awr cyn hynny, os oedd Covid, ni fyddem yn cael mynd i mewn i'r adeilad. Ac yna, newidiodd y ffaith ein bod yn cael eu gweld yn yr ardd, ond dim ond os oedd y ddau ohonom yn profi'n negatif. Ni fyddem yn cael ei chyffwrdd â hi.”
– Anwylyd preswylydd cartref gofal, Lloegr |
| “ | Profiad ofnadwy iawn oherwydd na allech chi fynd i mewn…roedd yna adegau penodol; roeddech chi wedi'ch cyfyngu i nifer y bobl…a chymerodd y broses gyfan tua thair awr dim ond i'w gweld hi am 15 munud oherwydd bod yn rhaid i chi brofi cyn mynd i mewn.”
– Anwylyd preswylydd cartref gofal, Lloegr |
Roedd rhai cartrefi gofal yn cyfyngu ymweliadau i un 'gyswllt dynodedig'. Mewn achosion eraill, dim ond un neu ddau ymwelydd a ganiatawyd ar y tro. Roedd yn anodd i rai anwyliaid ddeall yr angen am rai o'r cyfyngiadau, yn enwedig lle'r oedd rhagofalon eraill yn cael eu cymryd. Mewn rhai achosion, roedd y berthynas â'r cartref gofal wedi'i heffeithio gan y cyfyngiadau hyn.
| “ | Does dim gwahaniaeth i'ch siawns o gael eich heintio [pwy sy'n ymweld] roedd yna rai rheolau mympwyol iawn a oedd yn teimlo'n afresymol.”
– Anwylyd preswylydd cartref gofal, Cymru |
| “ | Dywedais i, 'Dydyn ni ddim hyd yn oed yn dod yn yr un car. Rydyn ni'n gwisgo masgiau. Rydyn ni'n eistedd pedair troedfedd ar wahân. Rydyn ni y tu allan. Pam nad ydyn ni'n cael gwneud hynny [gyda un ymwelydd arall]?'
– Anwylyd preswylydd cartref gofal, yr Alban |
Pan mai dim ond un neu ddau o bobl oedd yn gallu ymweld bob tro, roedd dewis pa aelodau o'r teulu fyddai'n ymweld yn achosi dadleuon a thensiwn.
| “ | Roeddech chi wedi'ch cyfyngu [o ran] faint o bobl oedd yn gallu mynd, felly byddai naill ai fy chwaer a'i merch, neu fi a fy merch ac fe wnaeth bron achosi rhwyg teuluol oherwydd bod pobl yn dadlau ynghylch pwy fyddai'n ymweld. Daeth bron fel trefn bigo, felly roedd hynny'n ei wneud ychydig yn lletchwith.
– Anwylyd preswylydd cartref gofal, Scotlandr |
Gallai'r rheolau 'cyswllt dynodedig' fod yn heriol hefyd oherwydd y cyfrifoldeb a roddir ar y person enwebedig.
| “ | Roedd yn gyfrifoldeb uffernol…does gennych chi neb i rannu’r [profiad anodd] yna ag ef.”
– Anwylyd preswylydd cartref gofal, Lloegr |
| “ | Pan gawson ni ganiatâd i ddod i mewn, roedden nhw wedi cychwyn [polisi] un ymwelydd dynodedig a oedd yn rhoi cryn straen arnaf. Yn amlwg, roedd yn rhaid i mi gadw'n iach oherwydd nad oedd cyfnewid. Ac yna roedd yn rhaid i mi adrodd yn ôl i weddill y teulu.”
– Anwylyd preswylydd cartref gofal, Lloegr |
Nid oedd gan rai cartrefi gofal ymwelwyr dynodedig penodol ond yn hytrach roeddent yn cyfyngu ar nifer yr ymwelwyr ar unrhyw un adeg, tra mewn achosion eraill roeddent yn caniatáu i'r cyswllt enwebedig newid. Yn yr achosion hyn, defnyddiodd teuluoedd yr hyblygrwydd hwn i ganiatáu i wahanol anwyliaid ymweld. Fodd bynnag, roedd gallu gwneud hyn yn cynyddu rhwystredigaeth gyda rheolau a oedd yn ymddangos yn fympwyol ac yn ddibwrpas, er bod gallu cynnwys mwy o'u hanwyliaid mewn ymweliadau yn groesawgar.
| “ | Ar un adeg dim ond dau ymwelydd enwebedig oeddech chi'n cael eu caniatáu, ond gallech chi newid y rheini drwy ffonio. Doedd dim terfyn ar ba mor aml. Roedd hi'n boen gorfod gwneud galwad ddibwrpas, gan eu gwneud nhw'n ymwelwyr enwebedig.”
– Anwylyd preswylydd cartref gofal, Cymru |
Nid oedd rhai pobl hŷn â dementia mewn cartrefi gofal yn gallu cofio aelodau o'u teulu pan wnaethon nhw ymweld yn bersonol eto yn y pen drawRoedd hyn oherwydd bod cymaint o amser wedi mynd heibio ers iddyn nhw eu gweld ac roedd eu cof a'u hiechyd wedi dirywio.
| “ | Roedd gan rai o'r rhai oedd â theuluoedd, ond ni allai eu teuluoedd ddod i'w gweld, roedden nhw'n eu colli. Roedden nhw wir yn eu colli ac yna pan ddechreuodd y cyfyngiadau ddiflannu a'u teuluoedd ddechrau dod, doedden nhw ddim yn cofio eu teulu, neu doedden nhw ddim yr un fath â nhw oherwydd nad oedden nhw wedi'u gweld ers cyhyd. Pobl â dementia, roedden nhw'n anghofio pwy oedden nhw. Roedden nhw'n dal i siarad amdanyn nhw, ond pan oedden nhw yno o'u blaenau, doedden nhw ddim yn gwybod pwy oedd e, a oedd yn eithaf trist. Roedd yn anodd i'r teuluoedd hefyd.”
– Gweithiwr cartref gofal, Lloegr |
| “ | Doedd dim ymweliadau na dim byd am amser hir iawn, a oedd yn eithaf trist. Doedd rhai ohonyn nhw ddim hyd yn oed yn adnabod pwy oedd eu teulu oherwydd erbyn hynny roedden nhw wedi anghofio'n llwyr, a oedd yn wirioneddol ofidus i'r teulu.”
– Gweithiwr cartref gofal, yr Alban |
Soniodd cyfranwyr eraill am yr effaith hirdymor a gafodd cyfyngiadau ymweld ar berthnasoedd rhwng preswylwyr cartrefi gofal a'u teuluoedd ac yn enwedig eu hwyrion.
| “ | Roeddwn i'n agos iawn at fy wyrion ac roedden nhw'n treulio llawer o amser yma gyda fi ac, wyddoch chi, byddem ni'n gwneud ein holl bethau celf a chrefft bach, er eu bod nhw'n eu harddegau. Felly, welais i ddim un ohonyn nhw ac yna wrth gwrs, ar ôl hynny, doedden ni ddim mor agos â hynny ar ôl y misoedd hynny o fod ar wahân. Nawr rwy'n meddwl amdano, dydyn ni erioed wedi bod mor agos eto. Dydy fy wyrion ddim yn dod i'm gweld cymaint nawr. Covid wnaeth i hynny ddigwydd. Y cwpl o fisoedd yna o seibiant oddi wrthyn nhw ac yna doedden ni ddim yn ymddangos i gael yr agosrwydd go iawn hwnnw yn ôl eto.”
– Person ag anghenion gofal a chymorth, Lloegr |
Roedd profiadau cyfranwyr o ymweliadau wedi'u cadw ar bellter cymdeithasol yn gymysg.Roedd rhai o’r farn bod siarad drwy raniadau neu yn yr awyr agored yn gweithio’n eithaf da ac roeddent yn falch o allu rhyngweithio â’u hanwylyd mewn ffordd a oedd yn ymddangos yn ddiogel.
| “ | Roedd y cartref gofal, a bod yn deg, yn dda iawn. Roedd ganddyn nhw lolfa wedi'i rhannu â phaneli gwydr [fel] y gallem ni fynd i mewn a gweld ein perthnasau a siarad â meicroffon trwy'r gwydr. Doedden ni ddim yn gallu cyffwrdd â nhw, ond gallem ni weld ein gilydd a siarad â gwydr rhyngom ni - popeth yn ddiogel.”
– Anwylyd preswylydd cartref gofal, yr Alban |
Fodd bynnag, roedd eraill yn cael ymweliadau cadw pellter cymdeithasol yn heriolRoedd preswylwyr weithiau'n ddryslyd ynghylch pam nad oeddent yn gallu eistedd gyda'i gilydd na mynd i mewn. Roedd y diffyg cyswllt corfforol hefyd yn anodd ymdopi ag ef, yn enwedig gan ei fod mor wahanol i sut y byddent yn rhyngweithio mewn amgylchiadau arferol. Roedd gwrthod cyffwrdd â'r rhai yr oeddent yn gofalu amdanynt yn teimlo'n annaturiol ac yn boenus i anwyliaid. Weithiau roedd hyn yn arwain anwyliaid i osgoi ymweld oherwydd y brifo a achosodd i'w haelod teulu a oedd yn byw yn y cartref gofal.
| “ | Roedden ni’n cael caniatâd i’w gweld nhw yn yr ardd, ond dim ond os oedd y ddau ohonom yn profi’n negatif. Ac yna, doedden ni ddim yn cael caniatâd i’w chyffwrdd hi, ond mewn gwirionedd, daeth hynny’n anodd iawn wedyn oherwydd ei bod hi eisiau dal ein dwylo, ac fe aeth hi’n flin, ac fe aeth yn emosiynol iddi, felly wnaethon ni ddim mynd i’w gweld hi mewn gwirionedd oherwydd yna fe aeth hi’n anoddach iddi ac fe aeth hi’n fwy flin.”
– Anwylyd preswylydd cartref gofal, yr Alban |
Roedd pobl a oedd yn ymweld yn yr awyr agored yn ystod misoedd oerach yn teimlo'n anghyfforddus yn gorfforol ac yn poeni am effaith yr oerfel ar y person yr oeddent yn gofalu amdano.
| “ | Pan ddaeth allan i [yr ardd], roedd yn bedrongl yng nghanol y cartref gofal, cyn gynted ag y byddech chi'n eistedd i lawr, roedd yn oer, oherwydd ei bod hi y tu allan. Roedd ganddo flanced o'i gwmpas bob amser, gyda'i gap ymlaen, a daeth i'r pwynt lle meddyliais, 'Dydw i ddim yn ei roi trwy hynny', oherwydd doeddwn i ddim yn teimlo ei fod yn gwneud unrhyw les iddo. Roedd yn ei ofid yn fwy na'i helpu, rhywbeth felly.”
– Anwylyd preswylydd cartref gofal, Lloegr |
Roedd cyfranwyr hefyd yn teimlo bod y diffyg preifatrwydd yn heriol ac yn ei chael hi'n anodd cyfathrebu'n effeithiol o bell.
| “ | Doedd gennych chi ddim preifatrwydd oherwydd roedd yn rhaid i chi adael y drws ar agor. Doeddech chi ddim yn gallu cau'r drws ac allwn i ddim cael sgwrs gyda fy nhad i ofyn iddo beth oedd yn digwydd a sut mae'n teimlo, oherwydd bob tro ro'n i'n troi o gwmpas, byddai gofalwr yn sefyll wrth y drws yn gwrando.”
– Anwylyd preswylydd cartref gofal, Cymru |
Roedd preswylwyr cartrefi gofal â dementia hefyd yn flin oherwydd ymweliadau â phellter cymdeithasol, gan eu bod yn cael anhawster deall pam roedd yn rhaid iddynt gadw pellter oddi wrth eu hanwyliaid.
| “ | Fe wnaethon nhw osod podiau oedd wedi'u rhannu i lawr y canol. Gallem ni ymweld â mam nawr, ond doedd hi ddim yn gallu deall pam na allem ni eistedd gyda hi na dal ei llaw – unwaith eto, yn ofidus iawn.”
– Anwylyd preswylydd cartref gofal, Lloegr |
| “ | Roedd gweld fy mherthynas yn yr ystafell hon wedi'i rhannu gan sgrin Perspex yn ofnadwy, methu â'i gyffwrdd yn gorfforol, na siarad ag ef yn iawn. Roedd yn ofidus iawn. Roedd bron yn waeth na pheidio â'i weld o gwbl. Roedd ganddo ddementia cymysg Alzheimer. Doedd dim modd esbonio pam ei fod yno [ar un ochr i sgrin] a ninnau yno [ar yr ochr arall].”
– Anwylyd preswylydd cartref gofal, Lloegr |
Trafododd staff cartrefi gofal hefyd yr anhawster yn gweld anwyliaid yn gorfod sefyll y tu ôl i sgrin i ymweld ag aelod o'u teuluDywedon nhw wrthym y gallai fod yn heriol gorfodi'r cyfyngiadau, a oedd rhai'n ystyried yn annheg, yn enwedig gan eu bod yn achosi i anwyliaid a phreswylwyr fod yn ofidus ar ôl yr ymweliadau. Clywsom fod staff brwydrodd i fod y rhai sy'n gyfrifol am orfodi cyfyngiadau.
| “ | Roedden nhw’n gallu sefyll y tu allan, edrych drwy’r ffenestri, chwifio. Roedd hynny’n anodd, oherwydd byddai rhai o’r preswylwyr mewn dagrau a byddai’n rhaid i ni eu cysuro wedyn. Ac i’r rhai oedd â dementia, neu broblemau cof ysgafn, yna daeth hynny’n broblem, oherwydd na allent ddeall pam.”
– Gweithiwr cartref gofal, Lloegr |
| “ | Nid oedd [rhai teuluoedd] yn cytuno â ni yn gweithredu [y cyfyngiadau], felly roedd gennym lawer o deuluoedd yn flin iawn ar y pryd, ond unwaith eto, rydym yn gweithio'n galed ac wedi eu hargyhoeddi am agweddau diogelwch hynny. Roedd gennym gwpl o ferched yn flin iawn gyda ni ac yn mynnu dod i mewn beth bynnag, a phethau fel 'na.”
– Gweithiwr cartref gofal, yr Alban |
Roedd hi'n anodd i bobl ag anghenion gofal a chymorth ddeall pam fod hyd pob ymweliad wedi'i gyfyngu mewn rhai cartrefi gofal, gan fod y cyfyngiadau eraill a oedd ar waith yn golygu na fyddent yn dod i gysylltiad â phreswylwyr eraill. Roedd anwyliaid yn ei chael hi'n boenus gadael y rhai yr oeddent yn ymweld â nhw cyn eu bod nhw'n barod.
| “ | Roedd yn ofnadwy. Doedd e ddim eisiau i mi fynd. Hanner awr, i rywun â dementia, oedd dim amser. Roedd ceisio egluro beth oedd wedi bod yn digwydd, ble roeddwn i wedi bod a chyfarfod eto ar ôl misoedd…mor anodd. Roedd e’n ddarnau pan adawais i ei ystafell ac roeddwn i’n ddarnau.”
– Anwylyd preswylydd cartref gofal, Lloegr |
Roedd rhai anwyliaid yn bryderus ynghylch trosglwyddo Covid-19 wrth ymweld â chartrefi gofal ac roedd hyn yn effeithio ar eu lles meddyliol ac yn golygu eu bod wedi cymryd camau ychwanegol i amddiffyn eu hunain a'r person yr oeddent yn ymweld ag ef.
| “ | Roeddwn i'n teimlo'n baranoaidd ynglŷn â sicrhau bod gen i lanweithydd dwylo a masgiau bob amser, a byddwn i'n newid fy nillad, dim ond i wneud yn siŵr. Ar y pryd doedd neb yn gwybod sut roedd yn cael ei basio o gwmpas, felly byddwn i'n sicrhau bod popeth oedd gen i yn lân [pan es i'w weld]. Byddwn i hyd yn oed yn newid fy esgidiau.”
– Anwylyd preswylydd cartref gofal, Lloegr |
| “ | Meddyliais i, 'felly beth ddylwn i ei wneud nawr os oes gen i imiwnedd gwan, os ydw i mewn perygl o ddal yr haint hefyd?' Cymerais bob rhagofal y gallwn i amddiffyn fy hun, [ond] rydw i wedi cael anhwylder pryder sy'n gysylltiedig â hynny i gyd, roedd yn eithaf anodd.”
– Anwylyd preswylydd cartref gofal, yr Alban |
Jean's storiYn ystod y pandemig, roedd mam Jean yn byw mewn cartref gofal yn Lloegr. Teimlai Jean eu bod wedi gweithredu cyfyngiadau llym ac anhyblyg ar ymwelwyr. |
|
| “ | Roedd ei chartref gofal yn cyfyngu ar bob ymwelydd wyneb yn wyneb ac ar amseroedd ymweld (o ran amlder a hyd). O fis Mawrth 2020 ymlaen, gwaharddodd y cartref gofal bob ymwelydd yn llwyr am sawl mis.” |
| Yn y pen draw, caniataodd y cartref gofal ymweliadau wyneb yn wyneb 20 munud bob pythefnos. Arhosodd y preswylwyr y tu mewn i'r cartref gofal, yng nghwmni gweithiwr gofal, tra bod ymwelwyr yn sefyll y tu allan ac yn gorfod siarad yn uchel trwy ffenestr. Yn ddiweddarach, symudwyd yr ymweliadau hyn i ystafell a oedd wedi'i rhannu gan sgrin blastig o'r llawr i'r nenfwd, gyda'r preswylydd a'r gweithiwr gofal ar un ochr a'r ymwelydd ar yr ochr arall. | |
| “ | Yna gwaharddwyd pob ymweliad wyneb yn wyneb o unrhyw fath gan y cartref gofal eto yn ystod cyfnod clo Omicron, pan fu farw fy mam ym mis Ionawr 2021. Cydymffurfiodd y cartref gofal yn llym â rheolau'r cyfnod clo adeg ei marwolaeth trwy ganiatáu i mi ymweld â hi wyneb yn wyneb a chael cyswllt corfforol â hi am y tro cyntaf ers mis Mawrth 2020, ond wedi gwisgo o'r pen i'r traed mewn PPE, am ddim ond 30 munud wrth iddi orwedd yn marw - ond roedd hi mewn coma ac erbyn hynny roedd hi'n rhy hwyr i ni siarad.” |
| Ers y pandemig, mae Jean wedi cael trafferth dod i delerau â marwolaeth ei mam. Mae hi'n teimlo'n flin ac wedi'i siomi gan yr ymateb i'r pandemig. | |
| “ | Marwolaeth fy mam yn y cartref gofal – ar fy mhen fy hun ac yn ddryslyd ynglŷn â pham roedd yn ymddangos bod ei hunig blentyn wedi ei gadael. Mae'n fy lladd yn llwyr i feddwl amdano. Roeddwn i'n teimlo, ac yn dal i deimlo, yn ddig, yn ddi-rym ac yn ofidus… Achosodd [y cyfyngiadau] ddryswch llwyr i glaf dementia, a gofid calon yn unig, [fe] effeithiodd ar iechyd meddwl fy mam, gan achosi i'w dementia waethygu, gan arwain at ddirywiad sydyn [a] gorffen yn ei marwolaeth ar ei phen ei hun heb fi wrth ei hochr.” |
Nid oedd preswylwyr cartrefi gofal yn gallu cael ymweliadau gan ddarparwyr gweithgareddau a gwasanaethau oherwydd cyfyngiadau. Roedd preswylwyr yn ei chael hi'n heriol pan ddaeth y gweithgareddau a'r gwasanaethau a gynigiwyd yn y cartref i ben yn llwyr., gan ychwanegu at yr ymdeimlad o unigedd. Effeithiodd hyn ar ddarparwyr gweithgareddau fel y rhai oedd yn trefnu ymarfer corff a gweithgareddau creadigol. Nid oedd gwasanaethau, fel trin traed ar gyfer torri ewinedd a thrinwyr gwallt, a oedd yn helpu i gynnal iechyd, urddas a balchder pobl, ar gael mwyach chwaith. Weithiau roedd staff cartrefi gofal yn gallu darparu dewisiadau eraill, ond roedd y rhain yn gyfyngedig.
| “ | Roedd gennym ni’r ciropodydd, doedd gennym ni ddim y triniwr gwallt, doedd neb yn dod i mewn o gwbl. Ac rwy’n cofio bob amser [y gweithiwr gofal] yn dweud, ‘Mi wnaf i olchi dy wallt tra byddaf i yma,’ ac fe wnaeth hi fy socian yn llwyr. Roeddwn i wedi gwlychu’n lân. Ond doedd dim modd torri dy wallt, doedd dim modd cael dim wedi’i wneud.”
– Person ag anghenion gofal a chymorth, Lloegr |
Cyswllt rhithwir ar-lein a thros y ffôn
Trafododd anwyliaid ffyrdd newydd o gyfathrebu a sut y gwnaethon nhw addasu i'r rhain pan oedd cyfyngiadau'n eu hatal rhag ymweld â phobl mewn cartrefi gofalCeisiodd staff gynnal cysylltiad rhwng y rhai yr oeddent yn gofalu amdanynt a'u hanwyliaid drwy alwadau ffôn neu fideo. I staff cartrefi gofal, roedd galwadau ffôn mynych a cheisiadau am alwadau fideo yn ychwanegu at eu llwyth gwaith ac yn effeithio ar y gofal y gallent ei ddarparu i breswylwyr eraill.
| “ | Byddai'r ffôn yn canu'n amlach yn rheolaidd, dim ond gan deuluoedd, ffrindiau, dim ond eisiau siarad â pherthnasau, preswylwyr os gallent. Roedden ni'n sicr yn ateb y ffôn llawer mwy ac yn delio â llawer mwy o gwestiynau ac yn hynny o beth, ychwanegwyd gwaith ychwanegol.”
– Gweithiwr cartref gofal, Lloegr |
Roedd galwadau fideo yn cynnig y cyfle i weld a sgwrsio ag anwyliaid ac i fonitro eu lles, a gadarnhaodd y diweddariadau a ddarparwyd gan staff cartrefi gofal.
| “ | O leiaf roeddwn i'n gallu ei gweld hi ac roeddwn i'n gallu gweld ei bod hi wedi'i golchi a'i glanhau ac yn edrych yn dda. Roeddwn i'n gallu ei gweld hi felly, i mi, roedd yn iawn - ond roedd hi'n ei chael hi'n anodd i mi beidio â bod yno.”
– Anwylyd preswylydd cartref gofal, Lloegr |
| “ | Pan fydden ni’n eu ffonio nhw, bydden nhw’n dweud, ‘Ydy, mae eich mam yn iawn. Rydyn ni wedi gwneud hyn gyda hi heddiw ac mae hi wedi cael bath’ yna bydden ni’n defnyddio FaceTime arni [ac] gallen ni weld ei bod hi’n lân ac yn daclus…mae’n rhaid i chi ymddiried ynddyn nhw, onid ydych chi [ei bod hi’n cael gofal er na allem ni fynd i mewn yno.”
– Anwylyd preswylydd cartref gofal, Lloegr |
Roedd rhai o'r farn bod galwadau fideo yn ffordd well o gael cysylltiad nag opsiynau eraill, fel ymweld â ffenestri cartrefi gofal.
| “ | Wrth ffenestr, dwi'n meddwl y byddai wedi bod yn waeth i mi. Roeddwn i eisiau rhoi cwtsh mawr iddo [ac] allwn i ddim bod wedi gwneud hynny, felly byddai bod mor agos wedi bod yn rhwbio halen i'r clwyf. Dwi'n gwybod y byddwn i wedi bod yn llanast emosiynol tra ar FaceTime neu ar y ffôn, gallaf gerdded i ffwrdd, ffonio'n ôl.”
– Anwylyd preswylydd cartref gofal, Lloegr |
Dywedodd rhai anwyliaid nad oedd ganddyn nhw unrhyw fodd o ddarganfod sut roedd y person oedd yn derbyn gofal yn y cartref. Cyfrannodd hyn atynt yn teimlo'n bryderus ynghylch lles ac unigrwydd y person yr oeddent yn gofalu amdano. Dywedodd eraill eu bod wedi cael eu gwneud i deimlo fel niwsans pan wnaethant ffonio i ofyn am y person yr oeddent yn gofalu amdano.
| “ | Doedd gennym ni bron ddim cyswllt o'r cartref gofal. Doedden nhw ddim yn ateb y ffôn, aeth fy mab i gnocio ar y drws a doedd e ddim yn cael ateb o gwbl. Roedd fel carchar. Fe wnaethon nhw gau'r drws a doedden nhw ddim yn siarad ag unrhyw un ar y tu allan.”
– Anwylyd preswylydd cartref gofal, Gogledd Iwerddon |
| “ | Roeddech chi hefyd yn teimlo eich bod chi'n drafferth pan wnaethoch chi ffonio, roedd bron fel ymateb 'ochneidio' pan feiddioch chi ffonio.
– Anwylyd preswylydd cartref gofal, Lloegr |
Er bod rhai preswylwyr yn gallu cadw mewn cysylltiad â'u hanwyliaid gan ddefnyddio ffonau a thabledi, gyda chefnogaeth staff cartrefi gofal, nid oedd hyn yn gwneud iawn am ddiffyg rhyngweithio wyneb yn wyneb. Nid oedd galwadau fideo yn opsiwn ar gael i bawbNododd rhai nad oedd pobl mewn cartrefi gofal yn gallu ymgysylltu â'r math hwn o dechnoleg, gan wneud cysylltiad â nhw'n fwy heriol.
| “ | Trefnodd cartref gofal fy mam alwad iPad wythnosol a oedd yn erchyll, sut mae menyw 90 oed yn gwybod sut i ddefnyddio iPad a siarad â chi ar alwad Zoom? Mae gen i luniau o'r galwadau Zoom lle rydyn ni'n ceisio siarad â hi ac roedd hi'n dal i ddiflannu. Gofynnais a allai hi gael ei dwyn i lawr i ffenestr y swyddfa fel y gallem ni siarad â hi'n gorfforol drwy'r ffenestr.
– Anwylyd preswylydd cartref gofal, Lloegr |
Roedd rhai pobl ag anabledd dysgu a'r rhai â dementia yn teimlo bod galwadau ffôn neu fideo yn hynod o ofidusDywedodd anwyliaid a gofalwyr di-dâl wrthym nad oedd y bobl yr oeddent yn eu cefnogi yn gallu ymgysylltu neu eu bod yn eu cael yn ofidus oherwydd eu bod am weld eu perthnasau wyneb yn wyneb.
| “ | Doedd hi ddim yn ei ddeall ac roedd hi'n eithaf cynhyrfus gyda'r galwadau fideo [oherwydd] nad oedd hi'n gallu deall na allwn i fod gyda hi [yn bersonol]. Dyna oedd y peth anoddaf.”
– Anwylyd preswylydd cartref gofal, Lloegr |
Y graddau y cefnogwyd cartrefi gofal cyfathrebu dros y ffôn neu ar-lein gydag anwyliaid a rhoi'r wybodaeth ddiweddaraf amdanyn nhw, wedi gwneud gwahaniaeth i ddealltwriaeth eu teulu o'u gofal. Fe wellodd hefyd lesiant anwyliaid eu hunain pan oeddent yn teimlo'n fwy mewn cysylltiad â'r hyn oedd yn digwydd yn y cartref gofal. Roedd aelodau'r teulu'n ddiolchgar am sut helpodd aelodau staff nhw i gadw mewn cysylltiad â'u hanwyliaid.
| “ | Aethant y tu hwnt i'r disgwyl o ran cyfathrebu, o ran fy nghadw mewn cysylltiad â hi dros y ffôn, doedd dim amser pan wnes i ffonio ac roedden nhw'n dweud, 'O, rydyn ni'n rhy brysur, rydyn ni'n rhy brysur'.”
– Anwylyd preswylydd cartref gofal, Lloegr |
Trafodir pwysigrwydd cyswllt ag aelodau’r teulu sy’n byw mewn cartref gofal ar ddiwedd oes ym Mhennod 4 ac archwilir y ffyrdd y cyfrannodd cynnal cyswllt at lwythi gwaith gweithwyr gofal ym Mhennod 6.
3. Rhyddhau o ysbytai i gartrefi gofal |
 |
Mae'r bennod hon yn amlinellu profiadau pobl yn cael eu rhyddhau o'r ysbyty i gartrefi gofal yn ystod y pandemig. Mae'n disgrifio sut y rhannwyd gwybodaeth, gallu cartrefi gofal i dderbyn cleifion a ryddhawyd a'u haddasrwydd i ddiwallu anghenion gofal penodol.
Rhannu gwybodaeth
Yn ystod y pandemig, symudodd pobl o ysbytai i gartrefi gofal. Weithiau roedd hyn yn cynnwys preswylydd cartref gofal a oedd wedi bod i'r ysbyty am driniaeth yn dychwelyd i'r un cartref gofal. Mewn achosion eraill, byddai cleifion yn cael eu rhyddhau o'r ysbyty i gartref gofal am y tro cyntaf. Yn y ddau sefyllfa, roedd angen gwybodaeth gan yr ysbyty ar gartrefi gofal am y profion a'r driniaeth yr oedd y person oedd angen gofal wedi'u derbyn a'u meddyginiaeth gyfredol. Wrth dderbyn preswylydd newydd i'r cartref, roedd gwybodaeth am anghenion gofal a chymorth y person hefyd yn bwysig er mwyn iddynt allu cael eu diwallu'n briodol.
Rhannu gwybodaeth am ryddhau o'r ysbyty
Yn aml, derbyniodd cartrefi gofal breswylwyr newydd neu breswylwyr presennol a ryddhawyd o ysbytai gyda gwybodaeth gyfyngedig iawn am eu cyflyrau iechyd a'r gofal yr oedd ei angen arnynt.
| “ | Hyd yn oed ein preswylwyr ein hunain yn mynd i'r ysbyty am driniaeth, nid oeddent yn cael y papur rhyddhau, nid oeddem yn cael y cyfathrebu drwodd gan yr ysbytai. Yr unig beth yr oeddem yn ei gael oedd canlyniad Covid trwy e-bost. Hyd yn oed i lawr i newidiadau mewn meddyginiaeth, nid oeddem yn cael unrhyw wybodaeth o gwbl. Yna roedd yn rhaid i ni ffonio drwodd, i ddweud, 'Pam mae preswylydd A, beth oedd y cyflwr, beth ddigwyddodd, pa feddyginiaeth yw'r hon maen nhw'n ei chymryd?' Aeth y papur i lawr y badell yn y bôn.”
– Rheolwr cofrestredig cartref gofal, Lloegr |
| “ | Yn sydyn daeth y nodiadau rhyddhau i ben [yn ystod y pandemig]. Rydyn ni wedi arfer â gwybodaeth a nodyn rhyddhau. Mae'n rhoi eglurder i ni ynglŷn â meddyginiaeth. Os oedd meddyginiaeth newydd [gyda'r preswylydd], yna roedden ni'n gwybod, ond fel arall, os oedden nhw'n dod yn ôl gyda'u meddyginiaeth eu hunain, roedden ni'n gwybod nad oedd pethau wedi newid. Gyda phreswylydd newydd, gallem ffonio'r meddyg teulu a dweud, 'Gwrandewch, rydyn ni wedi cael un o'ch cleifion. Dyma beth sydd gennym ni, oes unrhyw beth arall?' neu os oedd un ychwanegol, 'Mae hwn yn feddyginiaeth ychwanegol sydd gennym ni nawr. A allech chi edrych ar eich porth a dweud wrthyf a yw wedi'i ychwanegu?' Dyna oedd yr unig ffordd y gallem ni ei wneud.”
– Gweithiwr cartref gofal, Lloegr |
Yn aml, roedd cartrefi gofal yn teimlo dan bwysau i dderbyn cleifion a ryddhawyd oherwydd prinder gwelyau mewn ysbytaiDywedodd cyfranwyr wrthym sut roedd cartrefi gofal yn derbyn preswylwyr heb ddigon o wybodaeth am eu hanghenion.
| “ | Roedden ni mor dan bwysau yn ein gwaith, hyd yn oed yn ceisio paratoi ystafell. Doeddech chi byth yn gwybod pwy y byddech chi'n ei gael, a fydden nhw'n dreisgar, a oes ganddyn nhw ddementia. Byddech chi'n cael crynodeb o'r person, ond yn amlwg ni fyddech chi'n gwybod nes iddyn nhw gyrraedd y byddech chi'n cael y darlun llawn.”
– Rheolwr cofrestredig cartref gofal, Lloegr |
Dywedodd staff cartrefi gofal wrthym hefyd sut roedd gwybodaeth am ryddhau yn aml yn anghywir, felly roeddent yn aml yn derbyn cleifion ag anghenion gofal uwch a mwy cymhleth nag a ddisgwyliwyd.
| “ | Yr hyn oedd yn ein cythruddo ni oedd y ffaith ein bod ni'n cael negeseuon, roedden ni'n cael rhywun i mewn, felly roedden ni'n gofyn cwestiynau, 'Ydyn nhw wedi cael hyn a'r llall?' Ac roedden nhw'n dweud, 'Ydyn, maen nhw wedi cael eu profi, maen nhw wedi gwneud hyn, maen nhw wedi gwneud hynny. Gallan nhw gerdded, gallan nhw siarad, gallan nhw fwyta'. Ac yna pan oedd y claf hwnnw'n dod i mewn, oherwydd gwnaethon ni brofion Covid yn awtomatig hefyd pan ddaethon nhw i mewn, roedd yn teimlo fel pe baent yn cael ein twyllo oherwydd bod rhai pobl yn dod i mewn na allent fwyta ar eu pen eu hunain, na allent gerdded, na allent wneud dim byd drostyn nhw eu hunain.”
– Rheolwr cofrestredig cartref gofal, yr Alban |
Mewn rhai achosion, cynyddodd diffyg gwybodaeth bwysig y risg nad oedd gan y staff yr arbenigedd priodol a'r potensial na fyddai preswylwyr cartrefi gofal yn derbyn y math cywir o ofal.
| “ | Roedden ni’n cael ein twyllo. Mae’n rhoi pwysau arnom ni oherwydd wedyn does gennym ni ddim y staff chwaith i ddelio â rhywun fel ‘na, dydyn ni ddim wedi ein hyfforddi i ddelio â rhywun sydd â phroblemau iechyd a iechyd meddwl difrifol sydd angen eu rhoi mewn uned arbenigol.”
– Rheolwr cofrestredig cartref gofal, Lloegr |
Weithiau roedd yn rhaid i staff cartrefi gofal ymweld â'r ysbyty neu gysylltu ag ef i egluro pa ofal a meddyginiaeth yr oedd preswylydd wedi'i dderbyn a beth oedd ei angen arnynt nesaf.Ychwanegodd hyn at y pwysau gwaith sylweddol yr oedd staff cartrefi gofal yn eu hwynebu. Roedd staff yn poeni ynghylch a oeddent yn darparu'r gofal cywir gan nad oedd ganddynt yr holl wybodaeth gywir.
| “ | Roedd rhaid i mi fynd i'w hasesu nhw oherwydd doeddwn i ddim am ei gymryd dros y ffôn na'r cynllun gofal roedden nhw'n ei ddefnyddio i'w anfon atom ni; hoffwn i fynd i'w gweld nhw, ac roedd rhaid i mi fynd gydag aelod o staff, gyda masgiau a'n pinnies a gel a phopeth a byddwn i'n eu hasesu nhw.”
– Rheolwr cofrestredig cartref gofal, Cymru |
| “ | Byddem yn chwilio'r bagiau [am nodyn rhyddhau] ac ni fyddai dim byd yno a byddwn i'n dweud, 'Does dim nodyn rhyddhau'. Byddech chi'n ceisio cyrraedd y ward, yn amlwg maen nhw mor brysur fel nad oes neb yn ateb ac roeddech chi ar ôl gyda, 'Wel, beth ddylwn i ei wneud? Ydyn ni'n ei chwarae wrth y glust? Ydyn ni'n aros i weld? Beth ydyn ni'n ei wneud?'”
– Gweithiwr cartref gofal, Lloegr |
Rheoli trosglwyddiad Covid-19
Drwy gydol y pandemig, pryder allweddol pan gafodd pobl eu derbyn i gartrefi gofal o'r ysbyty, oedd a allent fod â Covid-19 ac a allent ledaenu'r firws, gan roi pobl yn y cartref mewn peryglFodd bynnag, Disgrifiodd cyfranwyr sut roedd profion a chyfathrebu am ganlyniadau profion yn anghyson a bod hyn yn golygu bod cartrefi gofal weithiau'n derbyn cleifion o ysbytai heb wybod a oedd ganddynt Covid-19.
| “ | Roedd yr ychydig wythnosau cyntaf yn eithaf llawn straen, gan nad oeddent wedi cael gafael ar brofi cleifion cyn iddynt eu symud allan o'r ysbyty a'u rhoi mewn gofal cam-i-lawr lle'r oedden ni. Felly, roedd llawer o ansicrwydd gyda chleifion yn dod i mewn, a fyddent yn lledaenu Covid ymhellach? Camreoli hynny oedd y broblem, felly roedd hynny'n deimlad eithaf aflonydd."
– Gweithiwr gofal iechyd, Lloegr |
Dywedodd staff cartrefi gofal wrthym hefyd, yng nghyfnodau cynnar y pandemig, nid oedd ysbytai yn profi pobl am Covid-19 cyn eu rhyddhau i gartrefi gofal.
| “ | Roedd hynny'n broblem fawr ar y dechrau, y ffaith eu bod nhw wedi gwagio ysbytai a heb brofi neb. Dw i'n meddwl hyd yn oed pe baen nhw wedi gwneud hynny, nad oedd ganddyn nhw unrhyw gyfleuster i'w hynysu nhw yn unman ar y pwynt hwnnw.”
– Ffisiotherapydd yn gweithio mewn cartref gofal, Lloegr |
Dywedodd rhai cyfranwyr sy'n gweithio mewn cartrefi gofal wrthym am ganlyniadau profion nad oeddent yn ddigon diweddar i fod yn gywir. gan eu gadael yn teimlo bod ysbytai yn ceisio rhyddhau capasiti trwy drosglwyddo'r bobl i gartrefi gofalRoedd canfyddiad, o ganlyniad, nad oedd pobl bob amser yn cael eu profi adeg eu rhyddhau.
| “ | Byddem yn cael gwybod ar lafar eu bod wedi cael eu profi, ond byddent yn dod yn ôl a byddai'r dyddiad yn anghywir arno. Ni fyddai'n ddyddiad rhyddhau cywir. Felly, os oeddent wedi cael y prawf 32 diwrnod ynghynt, ar y dyddiad rhyddhau byddent yn dweud, 'Ydy, maen nhw wedi cael prawf negyddol'. Ond ni fyddai bob amser ar ddiwrnod y rhyddhau.”
– Gweithiwr gofal iechyd, Lloegr |
| “ | Byddai'r ysbyty yn dweud nad oedd ganddyn nhw'r fe. Yna pan fydden nhw'n dod drwy'r drws atom ni a byddem ni'n eu profi a bydden nhw'n bositif am Covid. Dw i'n credu na allai'r ysbytai reoli nifer y cleifion oedd ganddyn nhw, felly roedd hi'n haws iddyn nhw adael i'r preswylwyr fynd yn ôl i'w cartrefi gofal a gadael i'r gofalwyr a'r nyrsys ddelio â nhw.”
– Rheolwr cofrestredig cartref gofal, Cymru |
Weithiau roedd yna dryswch ynghylch canlyniadau a darparodd ysbytai ganlyniad positif wedi'i ddiweddaru ar ôl i'r claf gael ei dderbyn i'r cartref gofal eisoes.
| “ | Dw i'n cofio i ni gael galwad ffôn o ysbyty am 2:00 y bore i ddweud, 'Y person hwnnw y gwnaethon ni ei anfon yn ôl ato ac roedd ei brawf yn negatif. Maen nhw'n bositif mewn gwirionedd'.”
– Gweithiwr cartref gofal, Lloegr |
| “ | Cawson ni’r person hwn a gafodd ei dderbyn i’n cartref, dywedwyd wrthym ‘Mae wedi cael ei brofi, gall ddod i mewn i’r cartref’. Yna cawson ni alwad ffôn o’r ysbyty yn dweud, ‘O, gyda llaw, fe wnaethon ni brofi ond mae wedi profi’n bositif mewn gwirionedd’.”
– Rheolwr cofrestredig cartref gofal, Lloegr |
Mewn achosion eraill, dywedodd staff cartrefi gofal eu bod wedi derbyn cleifion a ryddhawyd pan oeddent yn hysbys bod ganddynt Covid-19 ond nad oedd dewis arall ond eu cymryd.
| “ | Dw i'n cofio un o'r cartrefi gofal rydyn ni'n gofalu amdano fel y cyfryw, doedd ganddyn nhw ddim cleifion Covid positif ynddo. Roedd yn rhaid iddyn nhw dderbyn claf Covid positif. Roedden nhw'n gorfod cymryd yr un person yma…ac yna collon nhw 36 o breswylwyr.”
– Gweithiwr gofal iechyd, Lloegr |
| “ | Gwnaed penderfyniadau’n gwbl i ffwrdd oddi wrthyf fy hun, oddi wrth y rheolwyr. Dywedwyd wrthym gan berchnogion y cwmni, os oedd gennym ystafell sbâr, fod angen y lle ar yr ysbyty. Roeddent yn cludo pobl o’r ysbyty i gartrefi gofal nes y gallent ddod o hyd i rywle iddynt fynd… felly doedd gennym ni ddim rheolaeth dros hynny o gwbl. Pan oeddwn i’n arfer cael galwad ffôn yng nghanol y nos i ddweud, ‘Mae ambiwlans yn mynd i ddod i mewn ac yn dod â rhywun i mewn sydd â Covid-bositif’, doedd gen i ddim dweud yn y mater. Roedd yn rhaid i ni eu derbyn nhw i mewn.”
– Rheolwr cofrestredig cartref gofal, Lloegr |
Clywsom hefyd enghreifftiau o aelodau o'r teulu yn gorfod trefnu i gael eu profi eu hunain gan nad oedd profion yn cael eu darparu.
| “ | Aeth i'r ysbyty unwaith, nid am arhosiad hir. Mynnais iddi gael y profion cyn iddi gael ei rhyddhau. Roedd yn rhaid i mi ddarparu'r citiau prawf iddi gael eu gwirio. Dywedon nhw nad oedd yn bolisi iddyn nhw brofi. Nad oedd hi'n dangos unrhyw arwyddion o Covid.”
– Anwylyd preswylydd cartref gofal, yr Alban |
Pan oedd anwyliaid yn gwybod bod preswylwyr eraill wedi cael eu rhyddhau o'r ysbyty i gartref gofal, fe wnaethon nhw yn poeni'n fawr am iddyn nhw gael y firws a'i ledaenu o fewn y cartrefDywedodd rhai cyfranwyr wrthym am yr effaith a gafodd y pryder hwn ar eu lles corfforol eu hunain, er enghraifft, amharu ar eu harchwaeth a'u cwsg.
Nicole's storiMae Nicole yn byw yn Aberdeen gyda'i theulu. Roedd ei mam a'i thad, Colin a Christine, yn byw mewn cartref gofal preifat ychydig o fewn pellter gyrru ohoni. Roedd Colin a Christine wedi byw yn y cartref gofal am ychydig flynyddoedd cyn y pandemig. Roedden nhw ill dau yn gymdeithasgar ac yn egnïol iawn, roedden nhw'n arddwyr brwd ac yn cymryd rhan mewn llawer o'r gweithgareddau a gynigiwyd gan y cartref gofal. Pan ddechreuodd y pandemig, cyflwynodd y cartref gofal gyfyngiadau ymweld a mesurau rheoli heintiau a roddodd sicrwydd i Nicole a'i rhieni. Roedd gan y cartref lolfa gymunedol ar bob adain o'r adeilad, a gadwyd ar agor i ganiatáu rhywfaint o gymysgu rhwng preswylwyr. Ddechrau mis Ebrill 2020, derbyniodd Nicole lythyr gan y cartref yn dweud y byddent yn derbyn cleifion a oedd wedi cael eu rhyddhau o'r ysbyty. Gwnaeth hyn iddi hi a theuluoedd eraill deimlo'n flin ac yn ofnus iawn y byddai hyn yn arwain at ledaeniad y firws yn y cartref gofal ac fe wnaethant symud yn gyflym i brotestio yn erbyn y penderfyniad hwn. |
|
| “ | Cawsom lythyr gan y cartref gofal ar 8fed Ebrill yn cynghori eu bod yn derbyn cleifion a oedd wedi cael eu rhyddhau o ysbytai. Protestiodd y teuluoedd. Cafodd y penderfyniad ei wrthdroi o fewn 48 awr. Mae'r llythyr yn dweud bod y cartref gofal wedi cael ei ofyn i wneud hyn gan y GIG lleol. Cawsom lythyr arall ar 10fed Ebrill yn dweud, mewn ymateb i bryderon perthnasau, na fyddent yn derbyn cleifion a oedd wedi cael eu rhyddhau o'r ysbyty.” |
| Roedd Nicole yn falch na fyddai'r cartref yn derbyn unrhyw un o'r ysbyty. Fodd bynnag, yn ddiweddarach ym mis Ebrill derbyniodd alwad i ddweud nad oedd ei thad yn teimlo'n dda a phrofodd yn bositif am Covid-19. Cafodd ei dderbyn i'r ysbyty a thair awr yn ddiweddarach derbyniodd Nicole alwad o'r ysbyty i ddweud nad oeddent yn credu y byddai'n goroesi. Yn anffodus bu farw Colin ar ddechrau mis Mai.
Roedd marwolaeth Colin yn anodd iawn i'r teulu. Yn ddiweddarach yn ystod y pandemig, dywedwyd wrthi fod y cartref gofal wedi derbyn pobl a gafodd eu rhyddhau o'r ysbyty ddechrau mis Ebrill heb eu profi am Covid-19. |
|
| “ | Darganfyddais drwy ddata iechyd cyhoeddus fod naw claf wedi cael eu rhyddhau i'r cartref gofal rhwng mis Mawrth a mis Mai, pump ohonynt heb gael eu profi ac o leiaf un wedi profi'n bositif. Dim ond 10% o welyau'r cartrefi gofal oedd yn llawn, rwy'n credu eu bod wedi ildio ar draul fy rhieni a phreswylwyr eraill.” |
| Roedd Nicole a'i theulu mewn gofid mawr ac yn flin iawn am yr hyn a ddigwyddodd ac maen nhw'n dal i gael trafferth dod i delerau ag e. | |
Lle roedd cartrefi gofal yn derbyn preswylwyr newydd a brofodd yn bositif am Covid-19 wrth eu derbyn, neu'n fuan ar ôl hynny, roedd hyn weithiau'n cael ei ystyried fel y rheswm dros achosion yn y cartref.
| “ | Ac ar y pwynt hwn, roedd y dyn hwn [a gafodd ei dderbyn gyda Covid-19] eisoes yn ein cartref ar uned dementia. Ac wrth gwrs, unwaith iddo gyrraedd yr uned dementia honno lle mae pawb yn symudol, fe ledaenodd drwy'r cartref fel tân gwyllt.”
– Rheolwr cofrestredig cartref gofal, Lloegr |
O ystyried y risgiau sy'n gysylltiedig â throsglwyddo Covid-19, cymerodd cartrefi gofal gamau, lle bo modd, i ynysu'r rhai a oedd wedi cael eu rhyddhau o'r ysbyty ac i weithredu mesurau a fyddai'n amddiffyn preswylwyr eraill, rhag ofn bod y person sy'n cael ei ryddhau wedi profi'n bositif am Covid-19. Mae pwnc profion Covid-19 mewn cartrefi gofal ar gyfer staff, preswylwyr ac ymwelwyr wedi'i drafod ym Mhennod 5 ar PPE a mesurau rheoli heintiau.
Amseriad rhyddhau o'r ysbyty i gartrefi gofal
Cyn y pandemig, byddai cartrefi gofal yn derbyn rhybudd ymlaen llaw bod rhywun yn cael ei ryddhau i'r cartref gofal. Dywedodd rhai gweithwyr gofal iechyd a chymdeithasol proffesiynol fod y broses ryddhau yn ystod y pandemig yn llyfn ac yn debyg i sut roedd pethau'n gweithio o'r blaen. Er enghraifft, byddai rhai nyrsys cymunedol yn cael gwybod am ryddhau disgwyliedig y diwrnod cynt.
| “ | Dw i'n meddwl ein bod ni wedi cael ein rhyddhau arferol, fel, roedden nhw'n rhoi gwybod i ni'r diwrnod cynt eu bod nhw'n cael eu rhyddhau.”
– Nyrs gymunedol, Lloegr |
Fodd bynnag, profiad mwy cyffredin yn ystod y pandemig oedd cyfathrebu gwael rhwng ysbytai a chartrefi gofal. Yn aml, cwblhawyd rhyddhau cleifion o'r ysbyty o fewn ychydig oriau ac, mewn rhai achosion, cyrhaeddodd preswylwyr gartref gofal mewn ambiwlans heb unrhyw rybudd ymlaen llaw.
| “ | Weithiau, doedden ni ddim hyd yn oed yn cael gwybod eu bod nhw'n cael eu rhyddhau, bydden nhw'n troi i fyny gydag ambiwlans…roedd diffyg cyfathrebu mawr gyda'r ysbytai.”
– Gweithiwr cartref gofal, Lloegr |
Y rhain mae amserlenni byrrach yn rhoi pwysau ychwanegol sylweddol ar staff cartrefi gofal sydd eisoes dan bwysauRoeddent yn gorfod gweithredu'n gyflym, yn aml heb ddigon o amser ar gyfer mesurau rheoli heintiau neu i sicrhau y gallent ddiwallu anghenion preswylwyr a oedd yn dod i mewn. Roedd hyn yn straen enfawr i staff ac yn rhoi'r rhai ag anghenion gofal mewn perygl posibl.
| “ | Roedd yn amrywio mewn gwirionedd, weithiau dim rhybudd, weithiau hanner awr, weithiau byddem yn cael cwpl o oriau o rybudd, ond eto nid oedd digon o amser i baratoi'r tîm staff a ble roedden ni'n mynd i'w rhoi. Nid oedd gennym amser i wneud yr holl lanhau pwynt cyffwrdd a'r stemio yr oedd yn rhaid i ni ei wneud ym mhob ystafell a dadhalogi.”
– Gweithiwr cartref gofal, Lloegr |
| “ | Roedd pobl mewn sefyllfa llawer mwy agored i niwed oherwydd bod pwysau ar weithwyr cymdeithasol fel fi i gwblhau rhyddhau cleifion o'r ysbyty mewn dwy awr yn lle ein 48 awr arferol. Nid oedd neb yn ymddangos i ofalu am y posibilrwydd o heintio preswylwyr cartrefi gofal, nac a oedd ganddynt hyd yn oed ofal priodol i fynd adref iddo. Roedd yn hynod o straenus.”
– Gweithiwr cymdeithasol, Lloegr |
Rheoli haint Covid-19
Lle roedd anwyliaid yn helpu pobl i symud rhwng yr ysbyty a'r cartref gofal ar gyfer apwyntiadau neu driniaeth, gwelsant fesurau rheoli heintiau drostynt eu hunain ac fe'u cawsant yn galonogol.
| “ | Es i i’w chasglu hi o’r ysbyty. Roedd rhaid i mi aros yn y car ac yna fe wnaethon nhw ei dwyn hi allan. Dywedodd yr ysbyty nad oedd yn bolisi ganddyn nhw i brofi wrth gael ei rhyddhau os nad oedd hi’n dangos unrhyw arwyddion o Covid. Pan gyrhaeddon ni’n ôl i’r cartref gofal, roedd rhaid iddi wneud y profion ac yna cafodd ei hail-dderbyn. Unwaith eto, yn syth yn ôl i’w hystafell a’i hynysu. Roeddwn i’n hoffi eu bod nhw wedi gwneud hynny.”
– Anwylyd preswylydd cartref gofal, yr Alban |
Fodd bynnag, mae rhai roedd yn rhaid i bobl ag anghenion gofal a chymorth wynebu cyfnodau hir o ynysu ar ôl iddynt gael eu rhyddhau i gartrefi gofalRoedd staff yn poeni am yr effaith a gafodd hyn ar iechyd meddwl y preswylwyr.
| “ | Byddent wedi cael eu profi yn yr ysbyty, wedi cael eu clirio yno ac yna pan ddaethant yn ôl yma, roedd yn rhaid iddynt ynysu yn eu hystafell. Sydd, unwaith eto, ychydig yn gyfyngol. Felly, maen nhw wedi cael eu clirio o Covid, dydyn nhw ddim yn Covid-bositif, ac mae'n rhaid iddynt aros yn eu hystafell am wythnos. Sy'n ofnadwy, os ydych chi'n meddwl amdano. Ofnadwy. Ac ni fyddai hynny'n digwydd yn y gymuned. Fyddech chi ddim yn dweud ewch adref a pheidiwch â mynd allan eto.”
– Gweithiwr cartref gofal, Lloegr |
| “ | Roedd yn anodd iawn oherwydd roedden ni’n disgwyl iddyn nhw gael eu cadw yn yr ysbyty nes nad oedden nhw’n heintus. Felly, roedden nhw’n dod yn ôl yn dal i brofi’n bositif ac i rywun ddod i gartref lle nad oedd gennym ni’r cyfleuster i gael yr ynysu hwnnw, roedd hynny’n broblem hefyd, felly fe geision ni ynysu pobl yn eu hystafelloedd eu hunain, ond roedd hynny’n effeithio ymhellach ar eu lles meddyliol.”
– Gweithiwr cartref gofal, Lloegr |
Roedd staff cartrefi gofal yn wynebu pwysau ychwanegol oherwydd mesurau rheoli heintiau ac ymdrechion i sicrhau bod y firws wedi'i gynnwys.
Stori AbigailAbigail yw rheolwr cofrestredig cartref gofal yn Ne-ddwyrain Lloegr. Mae hi wedi gweithio yn y cartref gofal ers dros 20 mlynedd. Yn ystod y pandemig, oherwydd pwysau gan yr ysbyty lleol, derbyniodd ei chartref gofal breswylwyr heb wybod a oeddent wedi profi'n bositif am Covid-19. |
|
| “ | Roedd hi i fod i fod na allem ni eu derbyn pe bai'r bobl yn dod â halogiad, ond dywedodd yr ysbyty fod yn rhaid i mi.” |
| Creodd hyn heriau ychwanegol, gan fod yn rhaid i Abigail weithredu mesurau rheoli heintiau llym, gan gynnwys sterileiddio pob eitem a ddefnyddiwyd a thrin deunyddiau a allai fod wedi'u halogi yn ofalus. | |
| “ | Roedd rhaid i mi gymryd y rhagofalon, fe wnaethon ni baratoi hambwrdd gyda phopeth oedd ei angen a defnyddiwyd hwn ar gyfer y person hwnnw a rhoddon nhw ddŵr poeth i mewn, sterileiddio popeth ar eu cyfer a rhoi popeth ar wahân. Roedd rhaid i mi wneud y golchiadau ar wahân.” |
| Neilltuwyd cyfrifoldeb i staff am loriau penodol yn y cartref gofal i atal y feirws rhag lledaenu. | |
| “ | Roedd gennym ni loriau wedi'u dyrannu, roedd gennym ni aelod ar bob llawr, byddech chi'n glynu wrth eich llawr y shifft gyfan honno.” |
Ym Mhennod 5 (PPE a rheoli heintiau) a Phennod 6 (Prinder staff a sut y darparwyd gofal) rydym yn archwilio mesurau rheoli heintiau a'u heffaith ar breswylwyr a staff cartrefi gofal yn fanylach, gan nad oedd y materion hyn yn effeithio ar bobl ar yr adeg y derbyniwyd preswylwyr i gartrefi gofal yn unig.
Capasiti ac addasrwydd cartrefi gofal
Capasiti staffio
Teimlai staff cartrefi gofal dan bwysau i dderbyn pobl sy'n cael eu rhyddhau o ysbytai er gwaethaf capasiti staffio cyfyngedigRoedd y pwysau hwn yn arbennig o gryf i breswylwyr presennol a oedd yn dychwelyd i'r cartref.
| “ | Fel rheolwr cartref gofal, roeddwn i dan bwysau cyson i dderbyn pobl o'r ysbyty gyda galwadau ffôn ac e-byst sawl gwaith y dydd. Roedd galwadau ffôn yn aml yn elyniaethus ac yn fygythiol.”
– Gweithiwr cartref gofal, Lloegr |
| “ | Ar y pwynt hwnnw, oherwydd bod pobman dan gymaint o bwysau ac roedden ni’n cael gwybod, ‘Wel, maen nhw’n byw yn eich cartref chi, dyna lle mae angen iddyn nhw fod, maen nhw’n addas i gael eu rhyddhau, mae angen y gwely arnon ni, mae angen i chi eu cymryd nhw’n ôl’. Felly, doeddech chi ddim wir yn teimlo y gallech chi [ddweud na].”
– Rheolwr cofrestredig cartref gofal, Gogledd Iwerddon |
Yn yr un modd, Disgrifiodd gweithwyr cymdeithasol a nyrsys cymunedol deimlo na allent ddweud na wrth geisiadau am gymorth rhyddhau hyd yn oed os oeddent yn llawn eu gallu.Rhoddodd hyn straen ar adnoddau staff oedd eisoes dan bwysau, gan achosi straen sylweddol. Ynghyd â'r ffaith bod anwyliaid yn tynnu eu dicter am y sefyllfaoedd hyn allan arnynt, rhoddodd hyn staff gofal iechyd dan straen emosiynol mawr.
| “ | Doedden ni ddim yn gallu dweud na. Roedden nhw'n dod adref ac roedden nhw ein hangen ni. Felly, roedd y llwyth achosion cyn Covid tua 510. Yn ystod uchafbwynt Covid, roedden ni ar 650 a mwy, rydyn ni'n cael ffacsys neu e-byst yn cael eu hanfon atom ni. Rydyn ni'n cael, 'Mae Mr Smith wedi cael ei ryddhau i Gartref Gofal Smithy heddiw. Mae wedi profi'n bositif am Covid. Mae angen i chi ofalu am hyn, cadwch lygad ar ei arsylwadau cyffredinol. Diolch, hwyl fawr'.”
– Nyrs gymunedol, Lloegr |
| “ | Roedd pobl mor flin oherwydd y sefyllfa. Gwaeddodd un fenyw arnaf dros y ffôn sawl gwaith oherwydd bod ei thad yn cael ei ryddhau o'r ysbyty ac na allwn gael y gwasanaethau iddo. Doeddwn i ddim yn gallu cysgu am nosweithiau wedyn.”
– Ffisiotherapydd, Lloegr |
Teimlai cyfranwyr fod preswylwyr yn cael eu rhyddhau i gartrefi gofal nid oedd ganddo ddigon o gapasiti wedi gostwng ansawdd gofal cymdeithasol a dderbyniasant.
| “ | Cafodd ei ryddhau i gartref 'gofal'. Roedden nhw'n brin o staff ac yn methu diwallu ei anghenion. Un diwrnod aethon ni i ymweld am 2pm. Roedd e heb ei olchi a heb ei eillio yn y gwely gydag ewinedd budr a doluriau ar ei sodlau.”
– Anwylyd preswylydd cartref gofal, Lloegr |
Addasrwydd cartrefi gofal ac arbenigedd arbenigol
Er mwyn rhyddhau gwelyau mewn ysbytai, weithiau byddai pobl ag anghenion gofal a chymorth yn cael eu rhyddhau i gartrefi gofal. Roedd capasiti cyfyngedig mewn ysbytai a chartrefi gofal yn golygu bod pobl ag anghenion gofal a chymorth weithiau'n cael eu rhyddhau i cartrefi gofal nad oedd ganddynt y staff neu'r arbenigedd priodol i ddiwallu eu hanghenionWeithiau roedd cyfranwyr sy'n gweithio mewn cartrefi gofal yn teimlo dan bwysau i dderbyn preswylwyr newydd hyd yn oed pan nad oedd ganddynt y wybodaeth neu'r arbenigedd cywir i ofalu amdanynt. Arweiniodd hyn at bryderon gwirioneddol ynghylch diogelwch preswylwyr ac addasrwydd y gofal y gallent ei ddarparu. Dywedodd cyfranwyr wrthym sut na fyddai'r cartrefi gofal hyn wedi derbyn y preswylwyr hyn y tu allan i'r pandemig, yn ôl pob tebyg.
| “ | Oherwydd diffyg gwelyau ac yna mewnlifiad Covid yn dod i mewn ac yn cymryd drosodd y ward honno, roedd y claf â methiant y galon yn cael ei anfon adref oherwydd nad oedd ganddo Covid. Rydym yn mynd â chlaf sydd â methiant y galon i gartref nyrsio nad oes ganddo'r tîm hwnnw o bobl.”
– Gweithiwr cartref gofal, Gogledd Iwerddon |
Disgrifiwyd y cyfranwyr enghreifftiau o gartrefi gofal na allent ddarparu gofal arbenigol ar ôl rhyddhauMewn rhai achosion, roedd rhaid gofalu am bobl gartref yn hytrach na dychwelyd i'r cartref gofal.
| “ | Cafodd ei symud allan o'r ysbyty ac i gartref gofal oherwydd polisi'r llywodraeth ar symud cleifion oedrannus allan o'r ysbyty. Yn amlwg, nid oedd y driniaeth a gafodd fy mam-gu mewn cartref gofal o'i gymharu â'r gofal clinigol yr oedd hi wedi bod yn ei dderbyn yn yr ysbyty yr un fath ac fe ddirywiodd yn gyflym.”
– Anwylyd preswylydd cartref gofal, Lloegr |
| “ | Roedd fy mam hefyd mewn cartref gofal preifat anhrefnus, ofnus a heb baratoi. Fe wnes i ddod â hi adref yn ystod y pandemig, pan ystyriwyd bod ei bywyd yng nghyfnod gofal lliniarol. Roedd ei chartref gofal wedi gwrthod caniatáu iddi ddychwelyd ar ôl cael ei rhyddhau o'r ysbyty.”
– Gofalwr di-dâl, Lloegr |
Clywsom hefyd sut mae rhai preswylwyr angen gofal arbenigol colli eu lle yn y cartref gofal tra roedden nhw yn yr ysbyty ac roedd yn rhaid ei drosglwyddo i gartref gofal arall ar ôl cael ei ryddhau. Os oedd y cartref newydd yn llai addas, roedd hyn yn ei gwneud hi'n anoddach darparu gofal o ansawdd uchel. Pan oedd mewn lle gwahanol, roedd hyn weithiau'n ei gwneud hi'n anoddach i anwyliaid ymweld. Roedd cyfranwyr yn rhwystredig ac yn siomedig ynghylch y penderfyniadau hyn a'u diffyg cyfranogiad yn y broses.
| “ | Collodd ei le [yn y cartref gofal arbenigol, oherwydd nad oedd yr ysbyty] yn gwybod am ba hyd y byddai'n rhaid iddyn nhw ei gadw ynddo. Felly, cafodd ei symud a'r unig un addas y gallen nhw ddod o hyd iddo oedd 25 milltir i ffwrdd. Fe wnaethon ni barhau i ofyn i'r gwasanaethau cymdeithasol, 'A allwn ni ei symud yn agosach at ei gartref?' [Ond] ni ddigwyddodd hynny erioed.”
– Anwylyd preswylydd cartref gofal, Cymru |
Penderfynu pwy gafodd ei ryddhau i gartref gofal
Rhai pobl sydd ag anghenion gofal a chymorth dywedodd wrthym sut nad oedd neb wedi dweud wrthyn nhw y bydden nhw'n cael eu rhyddhau i gartref gofalClywsom enghreifftiau o bobl ag anghenion gofal a chymorth yn disgwyl dychwelyd adref ac yn lle hynny'n cael eu rhyddhau i gartref gofal. Roedd hwn yn brofiad gofidus ac aflonyddgar iawn.
| “ | Wel, mae'n debyg, doedd gen i ddim dweud dim byd am y mater mewn gwirionedd. Fe wnaeth yr ysbyty ei ddatrys. Dwn i ddim…Ddes i nôl ac roedd y gweithiwr cymdeithasol yn ymwneud â mi. Ac roeddwn i wedi cael fy archebu i ddod allan ac roedden ni wedi bod yn aros ac aros am ambiwlans ac yn y diwedd, dywedodd hi, o, mi af â chi. Felly, daeth â fi yma.”
– Person ag anghenion gofal a chymorth, Lloegr |
| “ | Doeddwn i ddim wir eisiau dod yma, na, roeddwn i wir eisiau mynd yn ôl adref. Wnaethon nhw ddim siarad â mi amdano o gwbl. Dywedon nhw, 'Rydych chi'n mynd adref heddiw', ac roeddwn i'n meddwl ein bod ni'n mynd i'r tŷ a dywedon nhw, 'Na, rydych chi'n mynd i [gartref gofal]'. Wnaethon nhw ddim trafod dim byd o gwbl, fe wnaethon nhw ein hanfon ni yma.”
– Person ag anghenion gofal a chymorth, Lloegr |
Dywedodd anwyliaid preswylwyr cartrefi gofal a oedd yn yr ysbyty wrthym eu bod nhw ddim bob amser yn rhan o benderfyniadau am ofal ar ôl gadael yr ysbytyYchydig iawn o rybudd a roddwyd i rai anwyliaid am bobl yn cael eu symud o ysbytai i gartrefi gofal. Ni chafodd eraill wybod nes bod newidiadau wedi digwydd felly erbyn iddynt ddeall y goblygiadau roedd hi'n rhy hwyr i wneud trefniadau eraill. Dywedodd cyfranwyr eu bod wedi cael hyn yn hynod o ofidus, gan eu gadael yn teimlo'n ddi-rym ac yn aml yn ddig.
| “ | Unwaith iddyn nhw [ei symud i'r cartref gofal], doedd dim mynd yn ôl. Aeth i ofal bryd hynny ac ni ddaeth allan erioed. Dw i'n meddwl y byddai wedi bod yn llawer gwahanol i ni pe baem wedi gwybod y broses a'r cyfyngiadau, a pha mor anodd oedd hi mewn gwirionedd [ymweld â hi], dw i'n meddwl y byddai wedi bod yn llawer gwahanol i ni.”
– Anwylyd preswylydd cartref gofal, Lloegr |
| “ | Ffoniwyd fi gan yr ysbyty i ddweud na ellid rhyddhau mam i'w chartref, oherwydd nad oeddent yn gallu darparu pecyn gofal cartref oherwydd Covid ac y byddai'n cael ei rhoi mewn cartref nyrsio gofal.”
– Anwylyd preswylydd cartref gofal, Lloegr |
Canfu cyfranwyr fod symud i gartref gofal nid yn unig yn anodd ar yr adeg y cawsant eu rhyddhau ond hefyd yn achosi problemau yn ddiweddarach pan oeddent am adael y cartref gofal am leoliad gofal gwahanol yr oeddent yn ei ystyried yn fwy addas ar gyfer eu hanghenion.
Stori Mary ac AlfieMae Mary ac Alfie wedi bod yn briod ers 49 mlynedd, maen nhw ill dau yn eu 80au. Ar ddechrau'r pandemig, roedden nhw'n byw yn eu cartref eu hunain yng Nghanolbarth Lloegr ac am flynyddoedd lawer gofalodd Mary am Alfie, a oedd â symudedd cyfyngedig. Yn ystod y cyfnod clo cyntaf, gwaethygodd eu hiechyd yn fawr ac roedd angen cymorth cymydog ar Mary pan syrthiodd Alfie. |
|
| “ | Syrthiodd ar y llawr bedair gwaith ac roedd rhaid i mi ffonio cymydog i fyny'r ffordd yn gyson i ddod i'm helpu. Doeddwn i ddim yn gallu ei godi, wyddoch chi, felly roedd rhaid i'r dyn ddod i lawr bedair gwaith, roedd rhaid i mi ffonio'n gyson, i'w godi. Felly ie, dim ots o gwbl, dim byd o gwbl.” |
| Fodd bynnag, wrth i'r pandemig fynd ymlaen, roedd pobl yn fwy gofalus ynglŷn â helpu ac nid oedd ganddyn nhw deulu i'w cefnogi. Wrth gefnogi Alfie i ddringo'r grisiau un noson, llithrodd Mary a thorri ei ffêr ac anafodd Alfie ei glun. | |
| “ | Pan aeth i fyny'r grisiau, doedd e ddim yn gallu mynd i fyny'r grisiau'n iawn a syrthiais i lawr y grisiau, torrais fy ffêr, wyddoch chi, doedd ganddo ddim gofal o gwbl, gyda fi yn unig.” |
| Llwyddodd Mary i ffonio ambiwlans ac ar ôl sawl awr aethpwyd â'r ddwy i'r ysbyty i gael triniaeth. Fe'u rhoddwyd mewn cysylltiad â'r awdurdod lleol hefyd fel y gallent gael eu cefnogi gan weithiwr cymdeithasol.
Ar ôl ychydig wythnosau yn yr ysbyty, dywedwyd wrth Mary ei bod hi ac Alfie yn cael eu symud i gartref gofal. Dyma'r tro cyntaf iddi glywed am hyn ac roedd hi eisiau mynd yn ôl i'w cartref, ond dywedwyd wrthi nad oedd opsiwn arall. Nid oedd eu gweithiwr cymdeithasol yn ymwybodol o'r symudiad hwn chwaith. |
|
| “ | Des i o'r ysbyty yn syth yma. Fe wnaethon nhw fy anfon yn syth yma … Wnaethon nhw ddim trafod dim byd. Dywedon nhw, 'O, rwyt ti'n mynd adref heddiw i [Cartref Gofal]'… wnaethon nhw ddim trafod y pris na dim byd yma o gwbl… Doeddwn i ddim wir eisiau dod yma, na, roeddwn i eisiau mynd yn ôl adref mewn gwirionedd, dim byd tebyg i dy dŷ dy hun.” |
| Ers iddyn nhw symud i'r cartref gofal nid yw Mary ac Alfie wedi bod yn ôl i'w cartref eu hunain. Er eu bod wedi derbyn gofal da yn y cartref gofal dros yr ychydig flynyddoedd diwethaf, mae Mary ac Alfie bellach yn ceisio dod o hyd i le mewn llety gwarchod. | |
| “ | Ddylwn i ddim bod wedi bod yma [yn y cartref gofal] cyhyd â hyn oherwydd rydw i wedi bod yma bron i dair blynedd bellach ac mae Alfie wedi bod yma bron i dair blynedd hefyd. Wel, gwelsom y gweithiwr cymdeithasol heddiw, i ddod o hyd i lety gwarchod i ni ac mae hi'n edrych arno nawr. Mae hi'n edrych arno. Dywedodd hi [y gweithiwr cymdeithasol], 'Ddylech chi ddim bod wedi dod yma yn y lle cyntaf'. Dywedais i, 'Wel, yr ysbyty anfonodd ni, wyddoch chi'. Dywedon nhw, 'Mae'n rhaid i chi fynd yma'.” |
| Mae Mary yn bryderus iawn bod y cartref gofal yn costio £900 yr wythnos yr un iddi hi ac Alfie ac yn gobeithio y bydd symud i lety gwarchod yn rhatach, yn ogystal â'i galluogi i fyw'n agosach at ei brawd. | |
3. I ddarllen mwy am benderfyniadau DNACPR gweler gwefan y GIG: https://www.nhs.uk/conditions/do-not-attempt-cardiopulmonary-resuscitation-dnacpr-decisions/.
4. I ddarllen mwy am ffurflenni ReSPECT gweler gwefan Cyngor Adfywio'r DU: https://www.resus.org.uk/respect/respect-healthcare-professionals.
4. Gofal diwedd oes a phrofedigaeth |
 |
Mae'r bennod hon yn disgrifio sut yr effeithiwyd ar bobl ar ddiwedd eu hoes gan y pandemig a sut y darparwyd gofal. Mae hefyd yn archwilio profiadau o golled a galar.
Yn agosáu at ddiwedd oes
Gofal diwedd oes yw cefnogaeth i bobl sydd ym misoedd neu flynyddoedd olaf eu bywyd. Ei nod yw helpu pobl i fyw mor gyfforddus â phosibl yn yr amser sydd ganddynt ar ôl ac i farw ag urddas. Gall pobl dderbyn gofal diwedd oes yn eu cartref, mewn cartref gofal neu mewn ysbyty neu hosbis.
Clywsom sut roedd pobl ag anghenion gofal a chymorth yn ynysig ac ar eu pen eu hunain yn ystod y pandemig. Pan oeddent hefyd yn ei chael hi'n anodd cael cefnogaeth gan y teulu, roedd hyn yn aml yn cael effaith ar eu cryfder corfforol a'u lles. Roedd hyn yn golygu bod aelodau'r teulu a gweithwyr gofal cymdeithasol proffesiynol yn gweld y roedd iechyd pobl ag anghenion gofal a chymorth yn dirywio ac roeddent yn aml yn teimlo eu bod yn agosáu at ddiwedd eu hoes yn gynt na'r disgwyl.
| “ | Gwelsom lawer ohonyn nhw'n dirywio. Yn bendant fe welwch chi bobl a aeth allan bob dydd, hyd yn oed os oedd dim ond i'r ardd, neu'n gweld eu teulu bob dydd, yn llythrennol yn colli eu hewyllys i fyw. Ac roedd gennym ni lawer o bobl a fu farw oherwydd hynny. Ac nid oedd oherwydd nad oedden ni'n ceisio…roedd yn anodd. Roedd yn anodd iawn.”
– Gweithiwr cartref gofal, yr Alban |
| “ | Aeth fy nhad i gartref gofal ychydig cyn y pandemig gyda dementia cynyddol, ni ellid gofalu amdano gartref. Ni chaniatawyd i ni ymweld ag ef am tua 6 mis [unwaith yr oedd yn byw yn y cartref gofal] dirywiodd yn gyflym dros y 6 mis […] a bu farw cyn i ni gael ei weld.”
- Aelod o'r teulu sydd wedi colli rhywun, Lloegr |
Roedd pobl a oedd yn agosáu at ddiwedd eu hoes hefyd yn wynebu rhwystrau wrth geisio cael mynediad at wasanaethau iechyd a gofal cymdeithasol.Dywedodd cyfranwyr wrthym sut y gwaethygodd iechyd pobl pan nad oeddent yn cael y cymorth oedd ei angen arnynt yn ddigon cynnar.
| “ | Yn aml, rwy'n credu ei fod oherwydd nad oeddent wedi gallu cysylltu â gwasanaethau eraill fel eu meddyg teulu. Nid oeddent wedi gallu cysylltu neu roedd wedi'i ohirio neu ddim ar gael… llawer o'r adborth gan y teuluoedd oedd [eu bod] wedi rhoi cynnig ar bawb arall, a bod yn rhaid iddynt ffonio'r gwasanaeth ambiwlans oherwydd nad oedd neb arall ar gael i'w helpu.”
- Parafeddyg, Lloegr |
Roedd rhai pobl ag anghenion gofal a chymorth yn teimlo'n bryderus ac yn isel eu hysbryd oherwydd y cyfyngiadau symud a'r unigedd. Weithiau roedd hyn yn golygu eu bod yn gwrthod bwyta neu yfed, gan waethygu eu hiechyd ymhellach (archwilir y profiadau hyn yn fanwl ym Mhennod 2).
| “ | Roedd gennym un preswylydd a fyddai’n cerdded o gwmpas ei ystafell neu yn yr ardal lolfa’n gyson. Pan fyddai wedi blino, byddai’n gorwedd ar y llawr ac yn plygu i safle ffetws gyda’i lygaid ar gau nes iddo godi a dechrau eto. Fe wnaethon ni geisio ei annog i fwyta, yfed a chymryd meddyginiaeth ond byddai’n ei gwrthod trwy droi i ffwrdd, ei phoeri allan neu [dod yn] ymosodol. Ar ôl ychydig ddyddiau o hyn, dirywiodd yn gyflym [ac] roedd yn y gwely ar ofal diwedd oes.”
– Gweithiwr cartref gofal, Lloegr |
Y rhan fwyaf o aelodau'r teulu a gofalwyr di-dâl dywedasant eu bod yn cael eu diweddaru ynglŷn â sut roedd eu hanwyliaid yn gwneud a phan ddechreuodd y person yr oeddent yn gofalu amdano dderbyn gofal diwedd oes. Fodd bynnag, nid oedd hyn yn wir am bob aelod o'r teulu a gofalwyr di-dâl.Roedd hyn yn golygu bod rhai cyfranwyr wedi synnu ac wedi cynhyrfu pan ddaethant i'r casgliad bod y person yr oeddent yn gofalu amdano yn agosáu at ddiwedd eu hoes.
| “ | Roedd hi mewn meddwl da pan aeth i mewn i'r cartref hwnnw, y cyfan y gallai ei wneud oedd methu defnyddio ei choesau… Ac o fewn yr amser yr oedd hi yno hyd at yr amser y tarodd Covid, ac roedd hi wedi'i chyfyngu, pan es i mewn pan oedden nhw'n meddwl ei bod hi'n marw, roedd hi'n anadnabyddadwy… Roedd hi wedi colli cymaint o bwysau, roedd hi'n gorwedd ar y gwely, roedd ei llygaid ar gau, bydden nhw'n agor ond dim ond mwmian pethau y gallai hi. Hynny yw, dydw i ddim eisiau beio'r cartref…ond dydych chi ddim yn gwybod beth sy'n digwydd, unwaith nad ydych chi'n cael mynd i mewn a dydych chi ddim yn gweld a dydych chi ddim yno, dydych chi ddim yn gwybod. A dydw i ddim yn meddwl bod ganddyn nhw'r staff i eistedd i lawr a sicrhau ei bod hi'n bwyta neu'n yfed neu'n siarad â hi.”
- Aelod o deulu galarus preswylydd cartref gofal, Lloegr |
Straeon o GaerdyddClywsom brofiadau tebyg mewn digwyddiadau gwrando yng Nghaerdydd hefyd. |
|
| “ | Y sgwrs olaf a gefais gyda'r cartref gofal oedd dweud wrthyf fod fy mam wedi marw…Roeddwn i'n gwybod ei bod hi'n sâl, ond roedd hi'n amhenodol iawn, dim ond dweud ei bod hi'n cysgu llawer. Roedden ni mewn cyfyngiadau symud, doeddwn i ddim wedi gallu ymweld â fy mam ers dros bedair wythnos felly doedd gen i ddim syniad beth oedd wedi digwydd, ar y pryd roeddwn i wedi cael fy sicrhau ac yn teimlo y byddai hi'n ddiogel gan nad oedd unrhyw ymwelwyr ond nid dyna oedd yr achos…Dw i newydd ddechrau mynd ar ôl y nodiadau cartref gofal ac dydw i ddim wedi'u cael nhw eto…Roedd hi mewn cartref a ariennir yn rhannol a'r unig ohebiaeth a gefais oedd nhw'n mynd ar ôl taliad fy mam.”
– Aelod o deulu galarus preswylydd cartref gofal, digwyddiad gwrando, Cymru |
Dywedodd cyfranwyr eraill wrthym sut roedd y person yr oeddent yn gofalu amdano wedi bod yn byw gyda chyflyrau iechyd terfynol fel canser neu fethiant yr afu. Yn yr amgylchiadau hyn, roedd y teulu a'r person ag anghenion gofal a chymorth wedi paratoi ar gyfer gofal diwedd oes. Fodd bynnag, yn aml, roedd pobl yn newid eu cynlluniau oherwydd bod cyfyngiadau pandemig ar ymweld ag ysbytai a chartrefi gofal yn golygu nad oedd y cynlluniau hyn yn gweithio mwyach i'r person yr oeddent yn gofalu amdano. Er enghraifft, roedd rhai cyfranwyr wedi bwriadu derbyn gofal yn yr ysbyty ond roedden nhw mor ofidus nes i'w teuluoedd benderfynu gofalu amdanyn nhw gartref. Gwrthododd pobl eraill fynd i'r ysbyty o gwbl. Roedd yr ansicrwydd a'r newidiadau munud olaf i gynlluniau gofal diwedd oes yn straen mawr i lawer o aelodau'r teulu a gofalwyr di-dâl.
| “ | Roedd fy nhad a fy mam yn teimlo ei bod hi'n drawmatig cael eu gwahanu ac ni allai ymdopi â chael ei drin gan bobl a ddisgrifiodd fel 'heb wynebau' (e.e., yn gwisgo masgiau a fisorau). Felly, daeth adref am ofal diwedd oes a chafodd ofal 24 awr y dydd gan fy mam. Yn anffodus, roedd hyn yn ormod iddi ei reoli, gan fod angen rhywun gydag ef bob amser ac nid oedd yn bosibl iddi gysgu.”
- Aelod o deulu galarus rhywun sy'n derbyn gofal cartref, Lloegr |
| “ | Roedd eisiau aros adref. Dywedodd wrtha i nad oedd eisiau mynd i'r ysbyty. Roedd ofn mynd. Doedd gan fy rhieni ddim cefnogaeth i ofalu amdano gartref, fe wnaethon nhw dorri'r rheolau i roi'r gofal diwedd oes oedd ei angen arno.”
- Aelod o'r teulu sydd wedi colli rhywun, Lloegr |
Stori AmitMae Amit yn byw yng Ngogledd Iwerddon ac yn ystod y pandemig darparodd ofal diwedd oes i'w dad, Rohit a gofalu am ei fam, Priya. Yn 2018, cafodd mam Amit strôc a'i dad oedd ei phrif ofalwr. Fodd bynnag, ym mis Mawrth 2020, cafodd Rohit ddiagnosis o ganser. Roedd ei ddiagnosis yn sioc fawr i'r teulu. Roedd salwch Rohit yn golygu bod yn rhaid i Amit a'i frodyr a'i chwiorydd ysgwyddo cyfrifoldebau gofalu yn ystod y cyfnod clo cyntaf. Nid oedd gan fam Amit lawer o symudedd ac roedd angen gofal arni ar hyd y cloc, felly symudodd Amit i'w cartref i ofalu am Priya a Rohit. |
|
| “ | Roeddwn i'n gyfrifol am goginio pob pryd bwyd – brecwast, cinio, swper, byrbrydau, y siopa bwyd ar gyfer hynny ac yna glanhau'r fflat. Doedd fy mam ddim hyd yn oed yn gallu gwneud paned o de, felly, roedd rhaid coginio a glanhau popeth. Roedd hi'n anymataliol hefyd felly roedd rhaid i ni newid cynfasau a rhoi padiau arni ac yna dod â hi i'r toiled yn ystod y dydd ac yn y nos byddem yn aml yn gorfod codi yng nghanol y nos.” |
| Dirywiodd iechyd Rohit yn gyflym hefyd. Cyn y pandemig roedd yn nofio dair gwaith yr wythnos ac yn cerdded milltiroedd bob dydd, ond o fewn chwe wythnos nid oedd yn gallu cerdded. Yn sydyn, roedd Amit a'i frodyr a'i chwiorydd yn wynebu darparu gofal diwedd oes gyda chefnogaeth fach iawn gan wasanaethau iechyd a gofal. | |
| “ | Yn y bôn, dywedodd yr ysbytai yma, fe wnaethon nhw anfon Dadi adref a dweud, 'Does dim byd arall y gallwn ni ei wneud drosto ac os na fyddwch chi'n ei gymryd adref nawr bydd yn marw yn yr ysbyty oherwydd ein bod ni'n cloi'r ysbyty'. A digwyddodd hynny ychydig ddyddiau'n ddiweddarach lle nad oedd neb yn gallu mynd yn ôl i'r ysbyty eto. Felly, roedd yn rhaid i ni fynd ag ef adref a gofalu amdano. Ond fe ddywedon ni, fel, nad oedden ni'n gwybod beth oedden ni'n ei wneud a doedd neb yno i'n helpu ni. Daeth y nyrs Marie Curie ddwywaith, ond eto meddyliais, 'Onid yw hi i fod i ddod bob dydd' neu oherwydd yn amlwg mae'n rhywbeth newydd, doedden ni ddim yn gwybod beth oedd i fod i ddigwydd. Felly, rydyn ni'n teimlo ein bod ni wedi ein gadael, oherwydd roedden ni'n teimlo fel, 'O Dduw, roedd y pandemig newydd ddigwydd ac aeth adnoddau pawb i rywle arall'. Dw i'n cofio pan oedd Dadi yn marw a meddwl, 'Pam rydyn ni yma yn gwneud hyn ar ein pennau ein hunain? Pam nad oes rhywun yn dod i mewn ac yn ein helpu ni? Dydyn ni ddim yn gwybod beth rydyn ni'n ei wneud. Dydyn ni ddim yn gwybod sut i ofalu am ddyn yn marw'.” |
| Gwnaeth Amit a'i frodyr a'i chwiorydd eu gorau i ofalu am Rohit a bu farw ddiwedd mis Ebrill 2020. Er bod Amit yn gwerthfawrogi treulio cymaint o amser gyda'i fam a'i dad yn yr wythnosau olaf hynny, roedd yn teimlo'n flin ac yn flinedig. | |
| “ | Roedd yn…drawmatig, byddwn i'n dweud mai galar a thrawma a blinder gofalwyr fyddai'r geiriau y byddwn i'n eu defnyddio pe bawn i'n meddwl yn ôl ar yr amser hwnnw a'r unigedd a theimlo'n unig llawer o'r amser gyda'r gofal am ein tad oedd yn marw a'r gofal am ein mam.” |
Dywedodd rhai cyfranwyr wrthym hefyd am sgyrsiau gofidus gyda staff iechyd a gofal cymdeithasol pan oedd y person yr oeddent yn gofalu amdano yn agosáu at ddiwedd oes.
Straeon o ddigwyddiadau gwrandoClywsom gan gyfranwyr mewn digwyddiadau gwrando ledled y DU am y sgyrsiau anodd ynghylch y ffordd orau o ofalu am bobl ar ddiwedd eu hoes. |
|
| “ | Yn anffodus, roedd rhai meddygon nad oeddwn yn cytuno â nhw. Roedden nhw'n dweud wrtha i [am fy ngwraig], 'oni wyt ti'n dymuno bod popeth drosodd iddi hi?' Eisteddais yno yn edrych yn ddryslyd oherwydd ei bod hi wedi bod yn briod ddwywaith o'r blaen a phan gyfarfu â mi, cymerais i'w salwch fel neb arall ac roedd hi'n poeni y byddwn i'n gwneud yr un peth â'r ddau [ŵr] cyntaf, ond dywedais i 'na, dw i wedi gwneud fy mhenderfyniad, byddaf yn glynu wrthyt ti nawr'. Sut gall meddygon ddweud nad yw [bywyd] yn werth ei fyw - mae'n werth ei fyw - pan mae hi'n gweld ei bechgyn, mae ganddi wên fawr ar ei hwyneb.”
– Aelod o deulu galarus preswylydd cartref gofal, digwyddiad gwrando, Lloegr |
Mynediad at wasanaethau a chymorth
Fe wnaeth rhai teuluoedd a gofalwyr di-dâl ei ganfod anodd cael cymorth gyda gofal diwedd oes gan yr ysbyty neu wasanaethau cymunedol yn ystod y pandemigClywsom enghreifftiau gofidus o beidio â gallu trefnu gofal lliniarol ar ddechrau'r pandemig, wrth i ddarparwyr geisio darganfod sut i ymateb.
| “ | O'm profiad i, roeddwn i'n teimlo nad oedd gofal diwedd oes yn y gymuned. Methodd y system yn ystod y pandemig.”
- Nyrs gymunedol, Lloegr |
| “ | Ni ddaeth neb o ofal diwedd oes i'w weld [ei gŵr]…ni allai'r cartref nyrsio ei gymryd…felly gadawyd i ni [gofalu amdano…dim ond bob ychydig wythnosau, yn gwirio ei gyffuriau, oedd y fenyw hon yn ffonio.”
- Gofalwr di-dâl, Lloegr |
Gadawyd anwyliaid a gofalwyr di-dâl i ddarparu gofal diwedd oes eu hunain os nad oeddent yn gallu cael cymorth proffesiynol. Pan ddigwyddodd hyn, cafodd doll emosiynol a chorfforol ddinistriol. Teimlai llawer yn flin ac yn euog nad oeddent yn gallu darparu'r lefel o ofal oedd ei hangen. Roedd aelodau'r teulu a gofalwyr di-dâl yn ddigalon oherwydd y boen a'r anghysur a brofodd y person yr oeddent yn gofalu amdano yn eu dyddiau olaf. Esboniodd gofalwyr di-dâl a ddarparodd ofal diwedd oes pa mor anodd oedd dod o hyd i'r math cywir o offer a chynhyrchion meddygol i'w helpu i ddarparu gofal.
| “ | Ches i ddim byd pan oedd fy ngŵr yn sâl, dim byd. Aeth yn sâl yn ystod wythnos gyntaf y pandemig yn unig ac allwn i ddim cael unrhyw help ar y cam hwnnw, yn anodd iawn hyd yn oed cael meddyg, dw i'n meddwl i mi gael un ymweliad gan y meddyg ac roedd yn rhaid i mi ofalu amdano fy hun ac aeth yn anymataliol ac roedd gen i drafferth ofnadwy cael padiau iddo. Roedd yn rhaid i mi ymladd dros y ffôn i'w cael, yn anodd ond llwyddais i wneud popeth a bu farw'n dawel yn fy mreichiau ar 8fed Mai. COPD [clefyd rhwystrol cronig yr ysgyfaint] oedd o mewn gwirionedd a'i galon, nid Covid-19 oedd o.”
- Gofalwr di-dâl ac aelod o'r teulu sydd wedi colli rhywun, Lloegr |
Clywsom hefyd gan nyrsys cymunedol fod darparu gofal lliniarol yn heriol oherwydd prinder meddyginiaethWrth i'r pandemig fynd rhagddo a gwasanaethau addasu, roedden nhw'n meddwl bod meddyginiaethau diwedd oes yn cael eu dargyfeirio a'u blaenoriaethu ar gyfer cleifion ysbyty. Roedd hyn yn golygu nad oedd pobl ar ddiwedd eu hoes gartref yn derbyn y driniaeth oedd ei hangen arnynt ac roeddent mewn poen diangen.
| “ | Weithiau, byddech chi'n mynd at glaf oedd yn cael trafferth gyda'i anadlu. Doedd gennym ni ddim y meddyginiaethau, oherwydd bod prinder cyflenwad, oherwydd eu bod nhw'n mynd i'r ysbytai. Felly, fel nyrs gymunedol, roeddwn i'n teimlo'n cael fy ngadael allan yn fawr. Roedd popeth yn ymddangos fel pe bai'r ysbytai yn ei gael. Felly, roedden ni'n rhedeg allan o feddyginiaethau, felly roedd cleifion yn marw mewn poen, yn cael trafferth.”
- Nyrs gymunedol, Lloegr |
Dywedodd pobl sy'n gweithio mewn cartrefi gofal roedden nhw'n teimlo eu bod nhw wedi cael eu gadael gan eu cydweithwyr gofal iechyd o ran gofal diwedd oesRoedd hyn yn golygu bod yn rhaid i weithwyr gofal ddarparu gofal nad oedd ganddynt unrhyw brofiad na hyfforddiant ynddo, gan nad oedd gweithwyr gofal iechyd proffesiynol yn ymweld â chartrefi gofal yn bersonol. Er enghraifft, roedd yn rhaid i rai staff cartrefi gofal ardystio marwolaethau a pharatoi pobl ar gyfer trefnwyr angladdau, a oedd yn peri gofid mawr iddynt.
| “ | Roedd hynny'n anodd oherwydd ni fyddai neb yn dod i mewn i'r cartref gofal. Felly, byddai gennych feddygon yn gwrthod dod i mewn yn llwyr, neu os oeddent yn gwneud hynny, byddai'n rhaid i chi aros oriau absoliwt iddynt ddod i ardystio'r marwolaethau. Byddai'r meddyg yn ei ardystio, heb gyffwrdd â nhw. Yna byddem yn galw'r trefnwyr angladdau. Roedden ni'n cael golchi'r corff wedyn. Ni chaniatawyd i ni ei ddilladu.”
- Gweithiwr cartref gofal, Cymru |
Daeth gweithwyr cartrefi gofal o hyd iddo yn ofidus gweld preswylwyr a fu farw heb gael eu casglu ac yn aros yn y cartref am gyfnodau hirRoedd y staff yn teimlo bod y diffyg urddas a gynigiwyd i breswylwyr yn peri gofid, fel pobl yn cael eu cludo i ffwrdd a'u claddu yn eu pyjamas i osgoi'r risg o drosglwyddo Covid-19. Mae'r profiadau hyn yn parhau i effeithio'n ddwfn ar rai gweithwyr cartrefi gofal, gyda rhai yn cael trafferth gyda'u hatgofion o'r hyn a ddigwyddodd.
| “ | Yn aml, nid oedd meddygon ar gael i ddatgan bod y trigolion wedi marw, felly byddent yn aros yn eu hystafelloedd gwely am hyd at 15 awr. Pan gasglwyd y cyrff, cyrhaeddodd y trefnwyr angladdau mewn siwtiau peryglus llawn, gogls, menig a masgiau wyneb. Dywedwyd wrthym am roi ein crysau-t dros ein hwynebau mewn ymgais i efelychu masgiau wyneb.”
- Gweithiwr cartref gofal, Lloegr |
| “ | Doeddwn i erioed wedi cael fy hyfforddi i ardystio rhywun yn farw, dros Covid dyna oedd un o'r pethau a wnaethom, oedd cael yr holl reolwyr wedi'u hardystio eu bod nhw'n gallu ei wneud. Roedd yn rhaid iddyn nhw fod yn trinwyr gwallt, yn artistiaid colur, roedden nhw'n sicrhau bod y preswylwyr yn cael eu hanfon i ffwrdd yn edrych yn gyflwyniadwy, fel y byddech chi pe bydden nhw'n arch agored. Delio â phobl sydd wedi marw - gadawodd un o fy rheolwyr ar ôl Covid mewn gwirionedd, roedd ei PTSD mor ddrwg. Roedd yr effaith iechyd meddwl a gafodd arnyn nhw yn erchyll.”
- Gweithiwr cartref gofal, Gogledd Iwerddon |
Ymweld a dweud hwyl fawr
Wynebodd aelodau’r teulu a gofalwyr di-dâl yr her o gyfathrebu ac ymweliadau cyfyngedig (fel y manylir ym Mhennod 2) yn ystod y pandemig. I bobl ar ddiwedd eu hoes a'u teulu, arweiniodd y cyfleoedd cyfyngedig i gyfathrebu at brofiadau gofidus iawn, a dywedodd rhai pobl y byddent yn aros gyda nhw am byth.Dywedodd staff cartrefi gofal wrthym sut roedd cyfyngiadau ar ymweld â phobl sy'n derbyn gofal diwedd oes yn arbennig o llym yn ystod y cyfnod clo cyntaf. Roedd darparwyr gofal cymdeithasol yn dal i ddysgu am y feirws ac nid oedd ganddynt ganllawiau ar sut i reoli ymweliadau.
Dywedodd llawer o gyfranwyr nad oeddent yn gallu gweld y person yr oeddent yn gofalu amdano ar ddiwedd eu hoes yn ystod y cyfnod clo cyntaf.Mae anwyliaid nad oeddent yn gallu ymweld yn parhau i fod yn ofidus iawn am aelod o'u teulu neu ffrind yn bod ar eu pennau eu hunain ac yn ynysig yn eu dyddiau olaf, hyd yn oed pan oedd staff gofal cymdeithasol gyda nhw. Teimlai rhai teuluoedd mewn galar y gallent fod wedi cael y cyfle i ffarwelio pe bai cartrefi gofal wedi cyfathrebu'n fwy effeithiol.
| “ | Roedd y gofalwr [a ffoniodd], roedd hi'n eithaf newydd i'r rôl ac nid oedd hi'n gwybod sut i'w ddweud mewn gwirionedd. Pe byddent wedi cyfathrebu'n well, byddem wedi mynd yn gynharach i'r cartref gofal [fy ngwraig o bosibl] a allai fod wedi bod yno pan aeth ef [ei thad] mewn gwirionedd, yn hytrach nag ar ôl y digwyddiad.”
- Aelod o deulu galarus preswylydd cartref gofal, Cymru |
Yn ystod y cyfnod clo cyntaf, clywsom sut Trefnodd gweithwyr gofal cymdeithasol alwadau fideo neu ffôn a rhoi'r wybodaeth ddiweddaraf drwy e-bostDywedodd anwyliaid wrthym fod y galwadau ar ddiwedd oes yn hynod o ofidus a gofidus.
| “ | Am sawl mis cyn marwolaeth ei [dad] dim ond unwaith yr wythnos am awr drwy alwadau Skype yr oeddem wedi gallu ei weld. Roedd y galwadau fideo hyn yn hynod o ofidus gan fod ganddo ddementia ac ni allai ddeall pam na allem ddod i'w ymweld mwyach!”
- Aelod o deulu galarus preswylydd cartref gofal, Lloegr |
| “ | Cawson ni ein galwad fideo olaf…ac yna fe wnaethon nhw ei rhoi hi ar ofal diwedd oes…roedd hynny ar y dydd Llun a bu farw hi [ei mam-yng-nghyfraith] ar y dydd Sadwrn…roedd yn eithaf ofnadwy mewn gwirionedd.”
- Aelod o deulu galarus preswylydd cartref gofal, Lloegr |
Rhannodd gweithwyr gofal cymdeithasol proffesiynol hefyd pa mor emosiynol a thrawmatig oedd y galwadau hynArhosodd llawer o staff gyda'r person yr oeddent yn gofalu amdano tan eu munudau olaf.
| “ | Byddem yn ffonio'r teulu ac yn dweud, 'Rydym newydd gael nyrs allan i ymweld â'ch mam. Yn anffodus, mae'r nyrs wedi cadarnhau ein hamheuon, mae eich mam yn oriau olaf ei bywyd. Pryd hoffech chi i ni ffonio?'...Roedd yn ofidus ac yn draenio'n emosiynol oherwydd roeddem yn ceisio gwneud popeth o fewn ein gallu i'r person a'i deulu...ond roedd adegau pan oedd yn rhaid i ni feddwl am iechyd meddwl staff hefyd. Y peth olaf maen nhw eisiau ei weld yw rhywun yn gwbl ddigalon pan na allwch chi roi eich llaw arnyn nhw a'u tawelu.”
- Nyrs gymunedol yn gweithio i ddarparwr gofal cartref, Lloegr |
Wrth i'r pandemig fynd rhagddo, llacio cyfyngiadau fel y gallai teulu a ffrindiau ymweld â phobl mewn cartrefi gofal ar ddiwedd eu hoes. Profwyd anwyliaid am Covid-19 cyn ymweld ac roedd yn rhaid iddynt wisgo PPE pan oeddent yn y cartref gofal, yr ysbyty neu'r hosbis. Clywsom lawer o enghreifftiau o aelodau o'r teulu yn ymweld â phobl yn eu dyddiau olaf yn ddiweddarach yn y pandemigRoeddent yn gwerthfawrogi cefnogaeth staff cartrefi gofal ac yn ddiolchgar eu bod wedi gallu cael y sgyrsiau olaf hynny.
| “ | Roedden ni mor ffodus oherwydd na chafodd cymaint o bobl gyfle i [ymweld ar ddiwedd oes a] chael y cyfle hwnnw, ac mae ein teulu’n ddiolchgar iawn am hynny. Ond wrth gwrs, ni fyddai hynny wedi bod fel arfer, byddai hi wedi bod wedi’i hamgylchynu gan lu o bobl oedd yn ei charu…yn amlwg roedden ni’n ddigalon iawn wrth golli mam, ond bydden ni wedi bod beth bynnag, dw i’n meddwl mai’r haen honno o euogrwydd na fydd byth yn lleihau.”
- Aelod o deulu galarus preswylydd cartref gofal, Gogledd Iwerddon |
| “ | Rwy'n ddiolchgar iawn eu bod nhw wedi gadael i mi fod yno gyda hi o leiaf. Treuliais lawer o amser yno. Byddwn i'n mynd ganol bore ac yn aros cyhyd ag y gallwn. Rwy'n cofio troi i fyny'r bore olaf, daeth y nyrs ar ddyletswydd y diwrnod hwnnw allan pan oeddwn i'n gwneud fy mhrawf Covid, a dweud, 'Does gan eich mam ddim llawer o amser i fyw', ac roeddwn i'n gwerthfawrogi hynny'n fawr, mae'n rhaid ei bod hi wedi gwybod, ac mae'n debyg iddi fy mharatoi ar ei gyfer.”
- Aelod o deulu galarus preswylydd cartref gofal, Lloegr |
Fodd bynnag, roedd cyfranwyr eraill yn fwy beirniadol ynglŷn â sut y trefnwyd ymweliadau ar ddiwedd oes rhywun. Trefnodd pob darparwr gofal ymweliadau mewn gwahanol ffyrdd. Er enghraifft, roedd rhai darparwyr gofal yn cyfyngu ar hyd yr amser y gallai aelodau'r teulu a ffrindiau ymweld neu dim ond nifer gyfyngedig o bobl a ganiatawyd. Mynegodd aelodau teulu mewn galar pa mor rhwystredig oedden nhw gyda rhai o'r trefniadau ymweld ar ddiwedd oes gan eu bod nhw'n teimlo'n fympwyol, yn groes i'w gilydd ac ar adegau'n greulon.
| “ | Roedd Mam yn ofnus o farw ar ei phen ei hun heb i mi nac un o'i pherthnasau yno gyda hi. Fodd bynnag, dim ond awr y dydd oeddwn i'n cael ei threulio gyda hi felly roedd siawns uchel na fyddwn i gyda hi ar y diwedd. Roedd hyn yn teimlo'n fympwyol oherwydd unwaith roeddwn i yn yr hosbis, does dim ots pa mor hir roeddwn i'n aros.”
- Aelod o deulu galarus preswylydd cartref gofal, Lloegr |
| “ | Cafodd fy meibion eu heffeithio'n fawr ganddo. Roedd yn ofnadwy iddyn nhw edrych drwy'r ffenestr a gweld eu mam-gu yn marw a pheidio â gallu bod yno a siarad â hi. Ac i ni [y tu mewn, wedi'n pellhau ac yn gwisgo PPE], roedd yn ofnadwy ac yn glinigol. Ac roeddwn i'n teimlo dicter.”
- Aelod o deulu galarus preswylydd cartref gofal, Lloegr |
| “ | Dydy Mam byth yn hoffi bod ar ei phen ei hun, ac roedd hi wastad yn hoffi cwmni. Felly, cael eich rhoi yn eich ystafell ar eich pen eich hun ar y diwedd…roedd yn eithaf creulon mewn gwirionedd pan fyddwch chi'n meddwl amdano.”
- Aelod o deulu galarus preswylydd cartref gofal, Cymru |
Straeon gan deuluoedd mewn galar yng Nghaeredin, Rhuthun a BelfastClywsom hefyd mewn digwyddiadau gwrando yn yr Alban, Cymru a Gogledd Iwerddon am y rhwystredigaeth a'r dryswch a achosir gan drefniadau ymweld â chartrefi gofal i'r rhai sy'n agosáu at ddiwedd eu hoes a'u hanwyliaid. |
|
| “ | Doedden ni ddim yn gallu ffonio na defnyddio FaceTime oherwydd ei fod yn fyddar, felly gofynnon ni i'r teulu ysgrifennu llythyrau a lluniau i'w gadw'n gyfredol. Wrth ymweld roedd yn rhaid i ni esbonio iddo nad oedden ni'n gallu dod i mewn, y troeon cyntaf rhoddodd wên a chwif i ni, y tro diwethaf i ni ei weld wrth y ffenestr doedd e ddim yn effro, ni chawson ni unrhyw ymateb na rhyngweithio, roedden ni'n poeni.”
– Aelod o deulu galarus preswylydd cartref gofal, digwyddiad gwrando, yr Alban |
| “ | Roedden ni’n cael caniatâd i ymweld â ffenestri yn yr haf, ond doedd e ddim yn deall pam nad oedden ni yno, doedd e ddim yn gallu cerdded. Byddai’n mynd yn ofidus iawn, roedd e eisiau marw oherwydd ei fod e’n gwybod bod rhywbeth o’i le mewn gwirionedd ac yn erfyn arna i i adael iddo farw, gadael iddo fynd.”
– Aelod o deulu galarus preswylydd cartref gofal, digwyddiad gwrando, Cymru |
| “ | Doeddwn i ddim yn hapus gyda'r driniaeth a pham roedden nhw'n dweud na alla i ddod, roedd yn rhwystredig iawn ac yn anodd iawn. Es i ddod i'w gweld hi [ar ôl iddi gael ei hanfon yn ôl o'r ysbyty], gwelais ei chyflwr. Bu farw yn oriau mân y bore wedyn, doeddwn i ddim yn gallu deall pam eu bod nhw wedi gwneud popeth fel y gwnaethon nhw.”
– Aelod o deulu galarus preswylydd cartref gofal, digwyddiad gwrando, Gogledd Iwerddon |
I bobl sy'n derbyn gofal diwedd oes gartref, clywsom sut mae rhai torrodd aelodau’r teulu a ffrindiau gyfyngiadau’r cyfnod clo er mwyn bod gyda’r person yr oeddent yn gofalu amdano yn eu dyddiau olafYn aml, roedden nhw'n teimlo'n euog am dorri cyfyngiadau ond yn meddwl ei bod hi'n angenrheidiol helpu'r person roedden nhw'n gofalu amdano.
| “ | Roedden ni'n teimlo bod yn rhaid i ni fynd i mewn i'w weld ef [ei thad] yn fwy ... felly mewn gwirionedd, fe wnaethon ni dorri'r rheolau. Dw i'n un sy'n glynu wrth bethau, roeddwn i'n poeni'n fawr amdano. Doedd fy mrawd ddim, ond roeddwn i wedi ymddeol beth bynnag, doedd fy ngŵr ddim yn gweithio, dywedodd, 'Does neb ohonom ni'n mynd allan felly dydyn ni ddim yn cymysgu â phobl eraill. Byddwn ni'n ofalus'. ... Roedd angen i ni fod yno iddo ar y diwedd.”
- Aelod o'r teulu sydd wedi colli rhywun, Lloegr |
Roedd torri cyfyngiadau hefyd yn anodd i weithwyr gofal iechyd a chymdeithasol proffesiynol a oedd yn darparu gofal yn y cartref i aelodau o'r teulu, gan eu bod yn gwybod ei fod yn erbyn y rheolau ond yn teimlo llawer iawn o gydymdeimlad a thrugaredd tuag at y teuluoedd.
| “ | Byddai gennych chi deuluoedd a oedd fel, 'Wel, stwffio fe'. Mae hynny'n swnio'n ofnadwy iawn. Roedden nhw'n mynd, 'Wel, stwffio fe. Mae fy mam yn marw, dw i'n mynd i fod wrth ei hochr hi'. Gan mai eu cartref eu hunain ydyw, doedd gennym ni ddim dewis. Ond eto, rydych chi wedyn yn eich rhoi eich hun mewn perygl oherwydd bod gennych chi bobl yn y tŷ hwnnw na ddylent fod yn y tŷ hwnnw. Ond wedyn, fel bod dynol sy'n poeni, sut ydych chi'n mynd i wneud hynny wedyn, rydych chi i fod i'w riportio a dweud, 'Ie, wel, dydyn nhw ddim yn rhan o'r swigen', neu beth bynnag. Ond mae eu mam yn marw. Felly, dydych chi ddim yn mynd i wneud hynny. Roedd yn rhyfedd.”
- Gweithiwr gofal cartref, Lloegr |
Cyflwyno gofal
Cafodd gofal diwedd oes ei darfu'n ddifrifol gan y pandemig. Er gwaethaf yr heriau hyn, disgrifiodd staff gofal cartref, gweithwyr cartrefi gofal, nyrsys cymunedol a gofalwyr di-dâl y ffyrdd y maent yn ceisio gwneud pobl sydd ag anghenion gofal a chymorth mor gyfforddus â phosibl.
| “ | Byddem yn rhoi cerddoriaeth gorawl hyfryd ymlaen, ac roedd hi'n mwmian, ac yn cysgu, ac yna byddai hi'n aml yn estyn allan… roedd hi'n gwybod ein bod ni yno… roeddwn i'n eistedd gyda hi gyda'r gerddoriaeth hyfryd, ac yna roedd pwynt lle roedd hi'n gwasgu ei llygaid yn dynn iawn, fel, ei chorff cyfan yn barod, ac yna anadlodd hi allan, ac roeddwn i'n gwybod ei bod hi wedi marw, roeddwn i'n gwybod mai dyna oedd ei hanadl olaf. Aac roedd un deigryn yn rholio allan o'i llygad.”
- Gofalwr di-dâl, Lloegr |
| “ | Roedden ni bob amser yn sicrhau bod gennym ni un person yn eistedd gyda nhw, un o'r nyrsys o'r ysbyty, neu weithiwr cymorth. Roedden ni'n arfer dod i ymweld, roedd yn debycach i ymweliad emosiynol, cymdeithasol na gofal corfforol gwirioneddol, oherwydd yn amlwg roedden nhw ar eu gwelyau angau ac ni welson nhw eu teuluoedd. Felly, rydyn ni wedi bod yno i'w helpu nhw i ymdopi ag e mewn gwirionedd.”
- Gweithiwr gofal cartref, Lloegr |
Dywedodd cyfranwyr wrthym am brofiadau gwahanol iawn o ofal diwedd oesDerbyniodd rhai pobl ofal rhagorol gan gynnwys cyngor parhaus a defnyddiol gan nyrsys ardal a nyrsys gofal lliniarol.
| “ | Cawson ni gefnogaeth y nyrsys ardal a oedd yn wych. Roedden nhw'n dod o gwmpas bob dydd am yr ychydig wythnosau cyntaf, yn ein cynghori ac yn rhoi meddyginiaethau [gan gynnwys 'rhag ofn'] meddyginiaeth diwedd oes a fyddai'n lleddfu ei dioddefaint [os oedd angen]. Roeddwn i'n teimlo ein bod ni wedi cael cefnogaeth eithaf da.”
- Aelod o'r teulu sydd wedi colli rhywun, Cymru |
Helpodd y gefnogaeth ychwanegol hon i roi rhywfaint o seibiant i ofalwyr di-dâl ac anwyliaid, er bod rhai yn ei chael hi'n anodd ymdopi â phresenoldeb sydyn pobl ychwanegol ac offer swnllyd yn y cartref. Roedd anwyliaid eraill yn synnu o ganfod bod y gefnogaeth yn fwy cyfyngedigRoedd hyn yn cynnwys gweithwyr gofal yn unig ar gael yn ystod y dydd neu ofyniad i bobl gael eu symud i wely ysbyty gartref i dderbyn gofal, nad oedd bob amser yn bosibl. Roedd hyn yn golygu bod rhai aelodau o'r teulu a gofalwyr di-dâl yn parhau i ysgwyddo rhywfaint neu'r cyfan o'r baich am ddarparu gofal diwedd oes.
| “ | Dywedodd y gofalwyr, gan nad oedd mewn gwely ysbyty, na allent ddod mwyach a gwneud unrhyw beth [am resymau iechyd a diogelwch]. Roedd ganddo ganser y prostad, a oedd yn effeithio ar ei asgwrn cefn, ac roeddwn i wedi cael gwybod, os byddwn i'n ei symud, y byddai'n ei ladd. Felly roedd hynny'n dipyn o gic yn y dannedd… Ac roedd peidio â chael cefnogaeth ar y diwedd yn ofnadwy, ond fe wnes i barhau ag e fel rydw i bob amser wedi gwneud.”
- Aelod o'r teulu sydd wedi colli rhywun, Gogledd Iwerddon |
| “ | Ni ddaeth y meddyg. Dywedodd nad oedd unrhyw ofalwyr ar gael ar gyfer gofal diwedd oes. Dywedodd yr ambiwlans na ddylwn i a fy mrawd fod yn gwneud hyn, ond dywedon nhw pe bydden nhw'n mynd â fy mam i'r ysbyty, na fyddem yn ei gweld hi eto. Roedd y meddyg locwm a'r nyrs ardal o sir arall yn ardderchog, fe wnaethon ni ffonio llinell gymorth, roedd yn rhaid i rywun ein helpu ni.”
- Aelod o'r teulu sydd wedi colli rhywun, Lloegr |
Cafodd aelodau o'r teulu mewn galar eu heffeithio gan y ffordd y gofalwyd am eu haelod o'r teulu neu ffrind ar ddiwedd eu hoes. Dywedodd rhai cyfranwyr fod y gofal a ddarparwyd wedi mynd 'y tu hwnt i'r disgwyl'. yr hyn yr oeddent yn ei ddisgwyl. Lle'r oedd gofal yn fwy tosturiol a phersonol, gan ystyried anghenion penodol, roedd hyn yn galonogol ac yn gysurus.
| “ | Bob [newid shifft] bydden nhw bob amser yn dod i mewn i ddweud nos da neu fore da wrtho. Gofynnodd rhai ohonyn nhw a allent weddïo gyda ni drosto. Roedd y staff nyrsio mor ofalgar, roedden nhw'n fwy na gwych.”
- Aelod o deulu galarus preswylydd cartref gofal, yr Alban |
| “ | Ffoniodd y cartref gofal fy chwaer i ddweud, 'Dewch i lawr gyda'ch teulu, rydyn ni'n meddwl bod eich mam ar ddiwedd ei hoes'. Roedd hynny'n dda iawn, oherwydd roedd yn dangos tosturi [a'u bod nhw'n ymwybodol o'r hyn oedd yn digwydd gyda fy mam. Roedden nhw'n ofalgar ac felly rwy'n gwybod bod mam yn gyfforddus iawn pan aeth hi.”
- Aelod o deulu galarus preswylydd cartref gofal, yr Alban |
Teimlai teuluoedd eraill mewn galar eu bod wedi cael eu siomi gan ofal diwedd oes. Dywedodd rhai cyfranwyr wrthym sut roedd diffyg cydymdeimlad a dealltwriaeth gan weithwyr gofal yn aruthrol yn ofidus ac yn achosi dicter a straen ychwanegol i deuluoedd mewn galar a gofalwyr di-dâl.
| “ | Roedd fy mam yn y dyddiau pan oedd hi'n marw yn mynd yn llai eglur, yn fwy rhithdybiol ac mae hynny'n digwydd, wyddoch chi. Roedd gennym ni bobl a fyddai'n gofalu amdani yn y nos ac weithiau un yn y dydd. Y fenyw a ddaeth i mewn am y nosweithiau, doedd hi ddim yn poeni dim, roedd hi i fod i ddod i'm casglu pe bai angen unrhyw feddyginiaeth ar fy mam neu ffonio'r nyrs ardal. Wnaeth hi ddim o hynny. Yn y diwedd, roedd y gofalwr yn dadlau gyda mi o flaen fy mam, roedd yn rhaid i mi ddweud 'allwch chi ostwng eich llais o flaen fy mam, os gwelwch yn dda?'
- Aelod o'r teulu sydd wedi colli rhywun, Lloegr |
| “ | Y gofalwr oedd yn gwneud nosweithiau ar y noson y bu farw, wnaeth hi ddim ein gadael ni ar ein pennau ein hunain…[gan ddweud] pethau fel 'Does dim rhaid i chi siarad ag e drwy'r amser', 'O, gallwch chi gau'r ffenestr honno'. Doedd hi ddim yr un fath â'r person arferol. Rhaid ei bod hi wedi dod o'r tu allan, ond roedden ni'n siomedig iawn yn [agwedd y gofalwr] hynny.”
- Aelod o'r teulu sydd wedi colli rhywun, Cymru |
Teimlai gweithwyr gofal cymdeithasol proffesiynol hefyd y boen a'r gofid o fod gyda rhywun pan fu farw, yn enwedig pan oeddent yno oherwydd na allai eu teulu a'u hanwyliaid fod.
| “ | Roedd yn ofnadwy, ni oedd yn eistedd yno, yn dal eu llaw wrth iddyn nhw farw. Ni oedd yn ffonio'r teulu i ddweud, 'Mae eich mam wedi marw y bore yma'.”
- Gweithiwr gofal cartref, Lloegr |
Stori FatemaMae Fatema yn byw yn Birmingham ac wedi bod yn gweithio ym maes gofal cartref ers sawl blwyddyn. Yn ystod y pandemig, gofalodd am sawl person a oedd yn dod at ddiwedd eu hoes. Ymwelwyd â'r bobl yr oedd Fatema yn gofalu amdanynt gan nyrs o'r hosbis leol a roddodd feddyginiaethau iddynt a sicrhau eu bod yn gyfforddus. Teimlai Fatema fod y bobl yr oedd hi'n gofalu amdanynt yn fwy diogel yn derbyn gofal yn eu cartref o'i gymharu â mynd i hosbis neu ysbyty. |
|
| “ | Bydden nhw'n dod unwaith neu ddwywaith yr wythnos ac yn dod â'r holl offer gyda nhw… bydden nhw'n hyfforddi aelodau'r teulu ac ychydig ohonom ni ofalwyr sut i'w defnyddio i helpu gyda'r anadlu.” |
| Hyfforddodd y nyrsys o'r hosbisau hi a'r gofalwyr di-dâl ar sut i ddefnyddio offer i helpu pobl i deimlo'n fwy cyfforddus wrth iddynt farw. Roedd hyn yn cynnwys peiriant ocsigen a pheiriant sugno i helpu gyda'r anadlu.
Byddai Fatema yn cynorthwyo gyda galwadau fideo neu ffôn fel y gallai pobl siarad â'u hanwyliaid, ac roedd hi'n teimlo bod hyn yn emosiynol iawn. Roedd Fatema a'i chydweithwyr hefyd yn gofalu am bobl ar ddiwedd eu hoes nad oedd ganddynt deulu. |
|
| “ | Un neu ddau o'r cleientiaid, doedd ganddyn nhw neb, roedden nhw'n unig. Dim teuluoedd, neb. Dim ond y gofalwyr a'r asiantaeth gofal. Felly, roedden ni'n arfer cymryd gofal ychwanegol pan oedden ni'n mynd yno, roedden ni'n arfer gwirio'r ffeil, pwy oedd wedi cael ymweliad, pwy sydd heb. Os oedd unrhyw bryderon, bydden ni'n ffonio'r nyrsys hosbis.” |
Gweithwyr proffesiynol iechyd a gofal cymdeithasol hefyd myfyriodd ar ba mor bwysig oedd y gofal diwedd oes a gynigiasant. Roeddent yn gwerthfawrogi negeseuon a gawsant gan deuluoedd a ffrindiau yn fawr. o bobl yr oeddent yn gofalu amdanynt.
| “ | Byddai'r gweinyddwyr yn dilyn galwadau ffôn ac weithiau byddent yn anfon cerdyn wedi'i lofnodi gan staff neu, yn ddiweddarach, wedi'i ysgrifennu gan y sefydliad at y teulu ac yn y blaen ... roedden ni'n cael ymatebion gan y teuluoedd yn diolch i'r holl staff am y gofal yr oeddent yn ei roi. Cefais fy synnu [bryd hynny] ein bod ni wedi derbyn mwy o ganmoliaeth nag erioed ... gallech chi weld bod y gymuned gyfan yn gwerthfawrogi'r hyn rydych chi'n ei wneud.”
- Gweithiwr cartref gofal, Lloegr |
Clywsom hefyd sut y byddai nyrsys yn gweithio oriau ychwanegol i sicrhau nad oedd preswylwyr ar eu pen eu hunain ar ddiwedd eu hoes.
| “ | Roedd yn gwneud i chi eisiau ceisio bod yno, does neb eisiau treulio'r cyfnod olaf hwnnw o'u bywyd ar eu pen eu hunain. Felly, byddai pobl [staff gofal iechyd] yn gorchuddio, neu'n aros yn hirach.”
- Nyrs gymunedol, Lloegr |
| “ | Dw i'n cofio mynd i gartref gofal, y staff a'r preswylwyr yn ofnus a menyw 92 oed yn marw ar ei phen ei hun. Doedden ni ddim yn gwybod a oedd ganddi Covid, ond roedd y staff yn rhy ofnus neu ddim yn cael aros gyda hi. Gorweddais ar ei llawr am oriau gyda hi, oherwydd fel nyrs dyna beth rydych chi'n ei wneud: rydych chi'n rhoi eich cleifion yn gyntaf ac yn meddwl amdanoch chi'ch hun yn ail.”
- Nyrs gymunedol, Lloegr |
Fodd bynnag, roedd gweld cymaint o farwolaeth a pheidio â bod bob amser yn gallu cynnig y gofal yr oeddent ei eisiau, hefyd wedi gadael rhai gweithwyr gofal cymdeithasol proffesiynol cwestiynu eu galluoedd proffesiynolRoedden nhw'n ei chael hi'n anodd cael ymdeimlad o gyflawniad o'u gwaith pan nad oedden nhw'n gallu cynnig yr urddas a'r gofal y bydden nhw fel arfer yn eu cynnig.
| “ | Dydych chi ddim yn cael unrhyw foddhad swydd o'r [gofal diwedd oes] hwnnw o gwbl oherwydd eich bod chi'n teimlo, er nad ydych chi'n methu'r person yn unigol, bod eich gwasanaeth yn gwneud hynny. Ac roeddwn i'n teimlo bod y pethau hynny [diffyg adnoddau staff ar gyfer gofal diwedd oes] yn anodd iawn.”
- Nyrs yn gweithio mewn cartref gofal, yr Alban |
Defnyddio hysbysiadau DNACPR
Trafododd teulu, ffrindiau a gweithwyr gofal cymdeithasol proffesiynol rôl DNACPR³ hefyd. hysbysiadau. Mae hysbysiadau DNACPR yn cofnodi penderfyniadau a gymerwyd gan y claf a/neu'r meddyg i ddangos na ddylai gweithwyr gofal iechyd proffesiynol geisio adfywio cardiopwlmonaidd (CPR) os yw'r claf yn rhoi'r gorau i anadlu neu os yw ei galon yn rhoi'r gorau i guro. Dylid gwneud y penderfyniadau hyn ar sail unigol, sy'n golygu na ddylid cymhwyso hysbysiadau DNACPR i grwpiau o bobl yn seiliedig ar nodweddion fel oedran, anabledd, neu breswylfa mewn cartref gofal.
Roedd rhai cyfranwyr yn ymwybodol bod gan y person yr oeddent yn gofalu amdano DNACPR ar waith.Roedden nhw’n gallu deall pam roedd angen hyn, gan fod y person ag anghenion gofal a chymorth yn aml mewn iechyd gwael a byddai ymestyn eu hoes yn arwain at fwy o ddioddefaint. Serch hynny, gallai fod yn anodd iawn i aelodau’r teulu ei dderbyn.
| “ | I mi, roedd gan fy nhad hysbysiad DNACPR. Felly, i mi, roedd yn debyg iawn i, wel, oherwydd ei alluoedd, ni ddylid ei adfywio oherwydd byddai'n dod yn llai o berson fyth, yn ddyn llai… Roedd yn un o'r pethau anoddaf i ollwng gafael ar reolaeth dros anghenion fy nhad ar y diwedd.”
- Aelod o'r teulu sydd wedi colli rhywun, Lloegr |
Dywedodd cyfranwyr eraill fod sgyrsiau am hysbysiadau DNACPR wedi cael eu trin yn amhriodol ac yn ansensitif yn ystod y pandemig. Achosodd hyn ofid a dicter mawr i bobl ag anghenion gofal a chymorth a'u hanwyliaid.
| “ | Ffônodd fy mam-gu fi mewn gofid ar ôl i'r meddyg ddweud wrthyf am y DNACPR ac na fyddent yn ei hadfywio. Roeddwn i'n flin nad oedd unrhyw dosturi nac urddas wedi'i roi i fy mam-gu a bod yn rhaid iddi ddioddef hyn ar ei phen ei hun.”
- Anwylyd preswylydd cartref gofal, Cymru |
Clywsom adroddiadau am hysbysiadau DNACPR yn cael eu rhoi ar draws cartref gofal neu i bobl â math penodol o gyflwr iechyd fel dementia. Mewn rhai achosion, heriodd aelodau o'r teulu, ffrindiau neu staff gofal hysbysiadau DNACPR.
³ I ddarllen mwy am benderfyniadau DNACPR gweler gwefan y GIG: https://www.nhs.uk/conditions/do-not-attempt-cardiopulmonary-resuscitation-dnacpr-decisions/.
| “ | Gwrthodais pan ddywedon nhw, ‘Rydyn ni’n mynd i roi DNACPR i bawb’, a dywedais i, ‘Dydych chi ddim o gwbl’. Bydd fy mhreswylwyr yn gwneud y penderfyniad hwnnw drostynt eu hunain. Dydych chi ddim yn mynd i orfodi hynny, felly peidiwch ag anfon unrhyw un yma oherwydd dydych chi ddim yn gwneud hynny. Gofynnais y cwestiwn. Gofynnais y cwestiwn i bawb oherwydd pwy a wyddai beth fyddai'n digwydd, ond ni fyddwn yn gadael i neb ddod i mewn a gwneud hynny”
- Rheolwr cofrestredig cartref gofal, Lloegr |
| “ | Wrth i'r cyfnod clo ddechrau cael ei drafod, blaenoriaeth y meddygon teulu ar gyfer y cartrefi gofal oedd symud yr holl breswylwyr i DNACPRs. Ni fu unrhyw drafodaeth ar unrhyw adeg ar y ffyrdd gorau o gefnogi neu drin preswylwyr â Covid. DNACPRs cyffredinol yn hytrach na gofyn 'sut fyddwn ni'n trin pobl?' NID OEDD UNRHYW gynlluniau triniaeth ar waith..”
- Aelod o'r teulu sydd wedi colli rhywun, Lloegr |
| “ | Aeth hawliau dynol pobl allan o'r ffenestr, felly hefyd y Deddf Gofal a'r Ddeddf Iechyd Meddwl. Roedd awdurdodau lleol yn cymhwyso'r gyfraith mewn gwahanol ffyrdd, roedd rhai yn anwybyddu'r gyfraith yn llwyr. Ffoniodd un meddyg lleol deuluoedd dim ond i ddweud eu bod wedi rhoi DNACPR ar eu hanwylyd oherwydd anabledd dysgu neu henaint, heb erioed gwrdd â'r bobl hyd yn oed.”
- Gweithiwr gofal, Cymru |
Awgrymodd eraill fod rhoddwyd blaenoriaeth i wasanaethau gofal iechyd dros wasanaethau gofal cymdeithasol a'r prif ffocws oedd amddiffyn y gofal iechyd system.
| “ | FiAr lefel leol, hyd y gwelaf i, roedd pobl yn camddehongli’n fwriadol…hysbysiadau DNACPR. ‘Dydyn nhw ddim eisiau CPR’, ie, ond dydy hynny ddim yn golygu nad ydyn nhw eisiau gwrthfiotigau. Gwrthododd fy llysfam fy hun gael un am amser hir, oherwydd ei bod hi’n gweld hynny fel ffordd o beidio â’i chymryd i’r ysbyty os oedd rhywbeth o’i le arni ac allwn i ddim dadlau â hi mewn gwirionedd, oherwydd roeddwn i’n gweld bod hynny’n digwydd. Doedd dim gorchymyn, dim ond, ‘Amddiffyn y GIG ar bob cyfrif’ oedd hyn. Ie, iawn, ond doedd e ddim wedi’i gau mewn gwirionedd. Yr agwedd yn lleol a’r cyfathrebu, bron oedd, ‘Chi sy’n gyfrifol yn unig am amddiffyn y GIG’, a dyna oedd y broblem gyfathrebu.”
- Nyrs gymunedol, Lloegr |
Clywsom hefyd gan feddygon teulu a nyrsys cymunedol a rannodd y pwysau yr oeddent yn gweithio oddi tanynt a'r ystyriaethau y bu'n rhaid iddynt eu gwneud wrth asesu'r angen am hysbysiadau DNACPR.
| “ | Rwy'n gweithio fel meddyg teulu yn yr Alban. Dechreuon ni ymgynghoriadau ffôn gyda chyfarfodydd dyddiol gyda'r bwrdd iechyd ynglŷn â pharatoi ar gyfer cwymp y GIG. Cawsom gyngor i siarad â chleifion oedrannus a'u rhybuddio am Covid a 'chynnig' DNACPR. Roedd cleifion yn dal i gael eu rhyddhau o'r ysbyty i gartrefi nyrsio gan fod y pryder [ynghylch] cwymp y system ysbytai. Daeth yn hunllef swrrealaidd dros nos. Cawsom ein rhybuddio y byddai ysbytai mawr yn cyflwyno system goleuadau traffig ac os oeddech chi'n goch neu'n ambr ar y system sgorio Covid, mae'n annhebygol y byddech chi'n goroesi. Roedd oedran dros 65 oed yn un o'r paramedrau.”
- Meddyg Teulu, yr Alban |
| “ | Ar ddechrau'r achosion o Covid roeddwn i'n cael fy nghyflogi fel Matron Cymunedol, yn gweithio gyda chleifion yn eu cartrefi eu hunain â chyflyrau hirdymor a gofal diwedd oes. Roedd hyn yn cynnwys gweithio ochr yn ochr â gofalwyr a gyflogwyd gan asiantaethau gofal cymdeithasol a oedd yn gofalu am fy nghleifion…Rhan o fy rôl oedd cael trafodaethau cynllunio diwedd oes gyda chleifion a'u teuluoedd…Cyn bo hir gofynnwyd i mi weld nifer o gleifion…Fy nhasg oedd egluro iddyn nhw, pe baent yn dirywio, na fyddai derbyniad i'r ysbyty yn cael ei ystyried a'u bod yn cael eu hannog i gael DNACPR. Byddai hyn yn golygu, pe baent yn dirywio, mai dim ond mesurau cysur fyddai'n cael eu defnyddio.”
- Nyrs gymunedol, Lloegr |
Dywedodd aelodau o'r teulu a gofalwyr di-dâl wrthym fod cyfathrebu ynghylch hysbysiadau DNACPR, sut y cawsant eu defnyddio a'r goblygiadau ar gyfer triniaeth wedi achosi dryswch, gofid a dicter. Roedd rhai o'r farn bod y person yr oeddent yn gofalu amdano wedi cael ei wrthod o driniaeth neu ymyriadau, gan gyfrannu at bryderon ynghylch ansawdd gofal a pharch at ddymuniadau unigolion yn eu munudau olaf.
| “ | Roeddwn i'n hwyr iawn yn darganfod bod ffurflen DNACPR wedi'i llofnodi. Rhoddwyd fy mhartner ar Forffin a Midazolam, cafodd yr holl ddŵr [a] bwyd ei dynnu oddi arno, a chafodd ei gadw mewn coma lled-goma nes iddo farw. Mae'r nodiadau meddygol yn cynnwys rhai datganiadau chwerthinllyd ac amhosibl.”
- Aelod o'r teulu sydd wedi colli rhywun, Lloegr |
| “ | Y peth gyda DNACPR yw bod y rhan fwyaf o bobl yn meddwl bod hyn yn golygu dim adfywiad, ond yn y cyd-destun hwn [Covid-19 yn y cartref gofal] roedd yn golygu dim triniaeth, dim hylifau, dim bwyd.”
- Cyfrannwr Every Story Matters, digwyddiad gwrando, Gogledd Iwerddon |
Clywed straeon am hysbysiadau DNACPR yn cael eu defnyddio i atal triniaeth yn ystod y pandemig achosodd ofid ac ansicrwydd enfawr i rai teuluoedd. Arweiniodd hyn at rai gofalwyr di-dâl yn newid trefniadau gofal ar gyfer aelod o'u teulu.
| “ | Roedd fy mab, sydd â Syndrom Down ac a oedd yn 24 oed ar y pryd, yn byw mewn lleoliad byw â chymorth cyn Covid. Roeddwn i'n gallu rhagweld risg i'w fywyd ac fe'i symudais yn ôl i'n cartref teuluol. Gadawodd polisi DNACPR awtomatig fi mor ofnus rhag ofn i fy mab ei ddal, cafodd ei gludo i'r ysbyty ar ei ben ei hun ond yn methu cyfathrebu gan nad yw'n siarad yn llafar a chafodd ei adael i farw.”
- Gofalwr di-dâl, Lloegr |
Ffurflenni ReSPECT
Trafododd y cyfranwyr hefyd y defnydd o ffurflenni ReSPECT (Cynllun Cryno Argymhelliedig ar gyfer Gofal a Thriniaeth Brys).4 ar ddiwedd oes. Defnyddir ffurflenni ReSPECT i sefydlu argymhellion personol ar gyfer gofal person mewn argyfwng yn y dyfodol lle nad ydynt yn gallu gwneud penderfyniadau na mynegi dymuniadau. Bwriad y broses yw parchu dewisiadau cleifion a barn glinigol.
Teuluoedd a staff gofal cymdeithasol codi pryderon ynghylch sut y dehonglwyd ffurflenni ReSPECT yn ystod y pandemigEr enghraifft, roedd rhai gweithwyr gofal cymdeithasol proffesiynol o'r farn bod y cynlluniau'n effeithio ar ba driniaeth feddygol a gynigiwyd i berson. Mewn achosion eraill, roedd anwyliaid yn teimlo nad oedd ffurflenni ReSPECT yn darparu digon o fanylion am ba driniaeth oedd ei hangen.
| “ | Mae wedi bod yn broblem ers tro byd, bod ffurflenni ReSPECT yn cael eu rhoi ar waith ond heb eu llenwi bob amser…gall rhai fod yn sylfaenol iawn, gan roi gwybodaeth gyfyngedig i chi. Yma mae gennym ymarferydd nyrs uwch o'r feddygfa yn cynnal adolygiad gyda phreswylwyr newydd ac mae hi'n cwblhau un newydd pan fyddant yn dod. Ond rydym yn tueddu i ganfod, ar adegau, nad oedd y preswylwyr o'r ysbyty yn gwybod eu bod yn eu lle, roeddent wedi dweud nad oeddent wedi cael eu hymgynghori â nhw. Ac roedd llawer ohonyn nhw'n rhoi'r wybodaeth sylfaenol, gyfyngedig i chi nad oedd yn ddefnyddiol iawn mewn gwirionedd.”
- Gweithiwr cartref gofal, Lloegr |
4 I ddarllen mwy am ffurflenni ReSPECT gweler gwefan Cyngor Adfywio'r DU: https://www.resus.org.uk/respect/respect-healthcare-professionals.
Clywsom hefyd achosion lle rhoddwyd ffurflenni ReSPECT i breswylwyr cartrefi gofal yn gynnar yn y pandemig heb unrhyw drafodaethMewn un enghraifft, nid oedd staff a thrigolion yn ymwybodol o hyn tan archwiliad gan y cyngor lleol yn ddiweddarach yn ystod y pandemig.
| “ | Rywbryd yn gynnar, ym mis Hydref 2020, dim ond ffurflenni ReSPECT cyffredinol oedd yn cael eu gwneud i bawb. Bydden nhw'n llythrennol yn llenwi'r ffurflenni hyn ar gyfer y person ac yn penderfynu'n awtomatig, felly byddai pawb dros oedran penodol yn cael eu penderfynu'n awtomatig, eu hystyried, i beidio â bod yn werth eu hadfywio… Cawson ni archwiliad cyngor, dw i'n anghofio pryd mae hyn, yn mynd yn ôl yn ôl i 2021 mae'n debyg, ac roedd archwilydd y cyngor, dyn hyfryd, yn gwirio'r holl bethau gwahanol hyn ac yn sylwi nad oedd gan bob ffurflen ReSPECT unrhyw sylwadau, nac unrhyw lofnodion gan drigolion. Roedden nhw i bob pwrpas yn-, dim ond ffurflenni cyffredinol oedden nhw wedi'u llenwi, ie.”
- Rheolwr cofrestredig cartref gofal, Lloegr |
Roedd y cyfranwyr yn flin ac yn ofidus iawn bod penderfyniadau ynghylch ffurflenni ReSPECT wedi'u gwneud heb gynnwys preswylwyr, aelodau o'u teuluoedd na staff.Teimlai staff cartrefi gofal fod agweddau gwahaniaethol tuag at bobl hŷn ac anabl wedi arwain at y penderfyniadau hyn. Rhannasant pa mor ddiymadferth yr oeddent yn teimlo pan glywsant allan ac roeddent yn arbennig o bryderus nad oeddent wedi cael y cyfle i eiriol dros breswylwyr.
| “ | Cafodd hynny effaith feddyliol arna i. Un fawr iawn. A byddaf yn onest gyda chi, roeddwn i mewn dagrau dros lawer ohonyn nhw. Dagrau llwyr. Gwnaed y galwadau hyn am y ffurflenni ReSPECT i gyd dros y ffôn ac i weld preswylwyr rydyn ni'n gofalu amdanyn nhw'n cael gwybod nad oedden nhw'n mynd i gael unrhyw driniaeth oherwydd eu hoedran, neu anableddau neu unrhyw beth, roedd yn dorcalonnus. Dyna oedd y mwyaf trawmatig.”
- Gweithiwr cartref gofal, Lloegr |
Profiadau o golled a galar
Dywedodd cyfranwyr mewn galar wrthym am eu galar a'u colled, yn ogystal â theimladau o ryddhad, sioc, dicter ac anobaith..
Mewn rhai achosion, nid oedd anwyliaid yn gwybod bod aelod o'u teulu neu ffrind yn agosáu at ddiwedd eu hoes a dim ond ar ôl i'w haelod o'r teulu neu ffrind farw y cysylltwyd â nhw. Roedd hyn yn golygu nad oeddent yn ymwybodol o sut yr oedd eu hiechyd wedi dirywio yn eu dyddiau olaf ac nad oedd ganddynt gyfle i baratoi na ffarwelio. Gadawodd hyn aelodau'r teulu a gofalwyr di-dâl yn teimlo'n ddryslyd ac yn flin.
| “ | Curodd plismon ar y drws, cerddodd i mewn, dywedodd, 'O, gyda llaw, mae eich gwraig wedi marw' dyna sut y dywedodd e. Dywedodd, 'O, ie, bu farw hi y bore yma. Dw i newydd gael gwybod i ddod i ddweud wrthych chi ei bod hi wedi marw'. Doedd ganddyn nhw [y cartref gofal] ddim y gwedduster i ffonio fi a rhoi gwybod i mi cyn i'r plismon gyrraedd.”
- Aelod o deulu galarus preswylydd cartref gofal, Cymru |
| “ | Cefais alwad am 4am i ddweud bod dad wedi marw ar ei ben ei hun, cafodd ei roi mewn dau fag corff ac mewn arch wedi'i selio. Dydw i dal ddim wedi gallu galaru'n iawn, roedd yn swreal, fel breuddwyd ddrwg a dydw i ddim wedi delio ag e.”
- Aelod o deulu galarus preswylydd cartref gofal, digwyddiad gwrando, Gogledd Iwerddon |
Rhannodd cyfranwyr am y tristwch ac euogrwydd roedden nhw'n teimlo pan oedden nhw'n gwybod bod aelod o'u teulu yn marw. Roedd y teimladau hyn yn arbennig o gryf os nad oeddent yn cael cyfle i ffarwelio, neu roedden nhw'n meddwl bod aelod o'u teulu neu ffrind wedi dioddef.
| “ | Roedd Dad mewn cartref gofal, nid carchar, sef yr hyn a ddaeth yn wir. Methoddais Dad ar ddiwedd ei oes drwy beidio ag ymladd drosto, byddaf yn byw gyda’r euogrwydd o hynny am byth.”
- Aelod o deulu galarus preswylydd cartref gofal, Lloegr |
| “ | Mae'r teulu wedi'i ddigalonni na allem fod gydag ef ar ddiwedd ei oes. Rydym yn galaru na chafodd yr anrhydedd yr oedd yn ei haeddu gan ei deulu cariadus ac agos iawn ac mae'n torri ein calonnau wrth i ni deimlo ei fod wedi'i adael ar yr union adeg yr oedd ei angen arno ni.”
- Aelod o deulu galarus preswylydd cartref gofal, Cymru |
Mewn rhai achosion, cafodd anwyliaid mewn galar eu cysuro oherwydd eu bod yn gwybod roedd staff gofal yno ar ddiwedd oes aelod o'u teulu.
| “ | Roedden nhw wedi symud lluniau mam a'i blodau yn union wrth ymyl ei gwely. Roedd ganddyn nhw gerddoriaeth glasurol yn ysgafn yn y cefndir. [Pan gyrhaeddais i yno, cyflwynodd aelod o staff] fi i [y person arall yno 'Dyma [enw]. Roedd hi gyda'ch mam pan fu farw.' Torrais i mewn i ddagrau ac ni allent fod wedi bod yn neisach.”
- Aelod o deulu galarus preswylydd cartref gofal, yr Alban |
| “ | Yn ffodus, cafodd taid ofal da yn y cartref gofal a phan fu farw, er ein bod ni i gyd yn ôl mewn cyfnod clo eto ac yn methu bod yno ein hunain, roedd e gyda rhai gofalwyr hyfryd.”
- Aelod o deulu galarus preswylydd cartref gofal, Lloegr |
| “ | Fi gofynnodd a oedd unrhyw un gydag ef a dywedodd y cynorthwyydd gofal iechyd 'Ie, roeddwn i gydag ef'. Roeddwn i eisiau gwybod a oeddech chi o asiantaeth? 'Na', meddai, 'aelod parhaol o staff' a dechrau crio ar y ffôn ac roeddwn i'n teimlo bod hynny'n gysur mawr oherwydd ei bod hi'n adnabod fy nhad a dywedodd ei bod hi'n meddwl y byd ohono. Dyna'r unig gysur.”
- Aelod o'r teulu sydd wedi galaru, Digwyddiad Gwrando, Cymru |
Ar ôl marwolaeth aelod o'r teulu mewn cartref gofal, clywsom am gyfyngiadau pellach fel mynychu lleoliadau gofal ar eu pen eu hunain neu aros ymhell o'r corffRhannodd cyfranwyr sut roedd hyn yn teimlo'n wahanol iawn i sut y byddent wedi ffarwelio â rhywun mewn amgylchiadau arferol.
| “ | Fi es i â fy ngwraig i'r cartref gofal [i weld ei thad] ond dim ond hi oedd yn cael mynd i mewn, a oedd yn anodd iawn i fy ngwraig fod yno ar ei phen ei hun heb gefnogaeth. Doedd neb gyda hi. Ac roedd y ffaith nad oedd hi'n cael ei gyffwrdd o gwbl yn ymddangos braidd yn rhyfedd pan nad oedd cysylltiad Covid â'i farwolaeth.”
- Aelod o deulu galarus preswylydd cartref gofal, Cymru |
Roedd y ffordd y gofalwyd am gorff y sawl a fu farw hefyd yn bwysig.Pan gafodd cyrff eu trin yn sensitif ac yn urddasol, gadawodd hyn argraff barhaol ar rai teuluoedd galarus a rhoddodd rywfaint o gysur yn eu galar.
| “ | Gofynnodd y nyrs i mi a oeddwn i eisiau ei helpu i'w golchi a'i rhoi i orwedd. Doeddwn i ddim yn gwybod beth oedd hynny'n ei olygu mewn gwirionedd ond roedd yn beth da iawn i'w wneud, ei golchi a brwsio ei gwallt; roedd yn teimlo fel peth da i'w wneud.”
- Aelod o deulu galarus preswylydd cartref gofal, yr Alban |
Clywsom hefyd enghreifftiau o bobl nad oeddent yn cael eu trin â'r gofal a'r urddas yr oeddent yn ei ddisgwyl gan anwyliaid. Achosodd hyn ofid mawr i aelodau'r teulu.
| “ | Hyd yn oed ar ôl marwolaeth, wnaethon nhw ddim trin [fy mam] ag urddas, drwy beidio â dilyn cais syml i roi tegan clyd gyda hi, gan golli ei “blanced hapus” ac achosi oedi cyn rhyddhau’r dystysgrif marwolaeth.”
- Aelod o deulu galarus preswylydd cartref gofal, Lloegr |
Casglodd rhai teuluoedd mewn galar eiddo eu hanwyliaid o leoliadau gofal. Fodd bynnag, roedd yn rhaid i rai wneud hyn mewn ffordd sy'n cadw pellter cymdeithasol.Ni allent fynd i mewn i'r ystafell a phacio eitemau eu hunain na siarad â gweithwyr cartrefi gofal. Creodd hyn deimlad o oerfel a datgysylltiad, gan na allent fyfyrio ar eu hanwylyd na siarad â staff am eu munudau olaf. Dywedodd aelodau o'r teulu a oedd wedi galaru fod hyn yn teimlo'n ddi-hid, yn ofidus ac nad oeddent yn cydnabod eu galar.
| “ | Roedd rhaid i ni fynd yn ôl ychydig ddyddiau [ar ôl ei farwolaeth] i gasglu ei holl eiddo oedd wedi cael eu rhoi y tu allan yn barod ac yn aros i ni eu rhoi yn y car a'u symud. Roedd yn teimlo fel pe baent eisiau gwagio'r ystafell er mwyn iddyn nhw allu cael rhywun arall i mewn. Cael y pethau allan cyn gynted â phosibl. Roedd y peth cyfan yn teimlo'n oer iawn.”
- Aelod o deulu galarus preswylydd cartref gofal, Cymru |
| “ | Yna cefais wybod bod yn rhaid selio ei ystafell am o leiaf dri diwrnod cyn y gellid symud unrhyw eiddo. Cefais fy synnu o ddarganfod eu bod wedi'u dympio mewn blwch ger y brif fynedfa, ac ni chaniatawyd i mi weld na siarad ag unrhyw un o'r staff. Tarodd y ffordd arwynebol y deliwyd â hyn fi'n galetach nag yr oeddwn wedi'i ddisgwyl, roedd yn ymddangos mor ddi-hid.”
- Aelod o deulu galarus preswylydd cartref gofal, Gogledd Iwerddon |
I rai teuluoedd sydd wedi colli galar, roedd cael caniatâd i ymweld â'r cartref gofal i gasglu eiddo yn ddryslyd ac yn ofidus pan wrthodwyd mynediad iddynt i ymweld aelod o'u teulu pan oeddent yn fyw.
| “ | Ffoniodd [y cartref gofal] fi a dweud, “Allwch chi ddod i glirio’r ystafell?” Dywedais i, “Na. Rydych chi wedi fy nghadw allan o’r fan’na drwy’r amser hwn; nawr rydych chi’n gofyn i mi fynd i’r lle mae Covid a chlirio’r ystafell? Na, dydw i ddim yn mynd yno. Roeddwn i’n flin iawn am hynny.”
- Aelod o deulu galarus preswylydd cartref gofal, Lloegr |
Straeon o Gaerdydd a BelfastRhannodd cyfranwyr mewn galar mewn digwyddiadau gwrando yng Nghaerdydd a Belfast hefyd sut nad oeddent yn gallu casglu eiddo ar ôl i aelod o'u teulu farw a sut nad oedd y gofal a'r gefnogaeth a dderbyniwyd yn ddigon da. |
|
| “ | Pan gadarnhawyd ei bod wedi marw, bu’n rhaid i mi adael yr ystafell ac roedd yr ystafell wedi’i selio ac ni allwn gael ei dillad, dywedon nhw [staff y cartref gofal] wrtha’i y byddai’n cael ei bagio ddwywaith, ei bod hi mewn gwisg nos rhywun arall a dim esgidiau, roedd yn ymddangos yn anghywir iawn. Ni ddylai neb byth fynd trwy hyn eto.”
– Aelod o deulu galarus preswylydd cartref gofal, digwyddiad gwrando, Gogledd Iwerddon |
| “ | Bu farw ar ei ben ei hun ar ôl dal niwmonia eto ar ôl cael ei drosglwyddo i'r cartref gofal [o'r ysbyty]. Doedden nhw ddim hyd yn oed yn gwybod ble roedd ei gorff. Wnaethon nhw ddim rhoi unrhyw beth o'i bethau yn ôl fel cardiau banc na ffôn ac roedd ganddyn nhw'r hyfdra i roi ei fisgedi 6 mis oed yn ôl i mi a dweud wrtha i am eu bwydo i'r adar.”
– Aelod o deulu galarus preswylydd cartref gofal, digwyddiad gwrando, Cymru |
Dywedodd teuluoedd mewn galar wrthym sut roedd eu colled wedi effeithiau parhaol ar eu hiechyd meddwl a'u lles, gan gynnwys teimlo'n bryderus, yn iselderus ac yn tarfu ar eu bywydau beunyddiol, a hynny i gyd wrth alaru.
| “ | Fi arhosais yn gryf nes bod fy mam yn y ddaear ac yna cefais chwalfa nerfol. Mewn gwirionedd, syrthiais i iselder. Roeddwn i wedi blino'n gorfforol beth bynnag ac yn obsesiynu amdano, torrais i lawr, mewn gwirionedd.”
- Aelod o deulu galarus preswylydd cartref gofal, yr Alban |
| “ | Dydych chi ddim hyd yn oed yn gwybod beth i'w wneud nesaf, mae eich holl feddyliau am eich mam yn unig. Es i sâl a wnes i ddim dychwelyd yn ôl i'r gweithle hwnnw. Dw i'n meddwl mai oherwydd fy mam oedd hynny, allwn i ddim rhoi'r gorau i feddwl amdani a'i cholli.”
- Aelod o deulu galarus preswylydd cartref gofal, yr Alban |
Stori EmmaMae Emma yn byw yn Ne Lloegr. Cyn y pandemig, roedd hi wedi bod yn gofalu am ei mam, Sandra, a oedd yn 89 oed ac yn dioddef o ddementia. Ar ddechrau 2019, gwnaeth Emma a'i theulu'r penderfyniad i symud Sandra i gartref gofal wrth i'w hanghenion gofal gynyddu. Roedd y cartref gofal bum munud o waith cerdded o dŷ Emma ac yn cefnu ar ei gardd. Byddai Emma a'i chwiorydd yn ymweld â Sandra bob dydd. Pan ddechreuodd y pandemig a chyflwynwyd cyfyngiadau symud, roedd Emma'n ei chael hi'n anodd byw mor agos at ei mam ond heb allu ymweld â hi. |
|
| “ | Roeddwn i yno bum gwaith yr wythnos, mae'n debyg. Felly, roedd hynny'n anodd iawn i mi. Dw i'n meddwl mai dyna oedd y peth gwaethaf i mi yn y pandemig, oedd [bod] yn sydyn ddim yn gallu gwneud yr hyn oedd eich trefn ddyddiol i'w wneud. Roeddwn i'n teimlo'n ddiymadferth na allwn i hyd yn oed fynd i mewn drwy'r drws ffrynt ac, wyddoch chi, roeddwn i'n arfer cerdded fy nghi heibio'r drws, ond yn amlwg nid oedd hi ar yr ochr lle mae'r ffenestri'n wynebu'r ffordd hon, felly, allwn ni ddim gweld-, roedd yn ofnadwy mewn gwirionedd a dweud y gwir. Dyna oedd y peth gwaethaf i mi yn y pandemig. Roeddwn i'n teimlo'n ddiymadferth, dw i'n meddwl yn ddiymadferth iawn mewn gwirionedd.” |
| Tua thri mis i mewn i'r pandemig, cafodd Emma sgwrs gyda rheolwr y cartref gofal ynglŷn â beth fyddai'n digwydd pe bai Sandra yn marw tra nad oedd y cartref gofal yn caniatáu ymwelwyr. Cafodd Emma sicrwydd y byddai ei chwiorydd a'i phlant yn cael dod i mewn i ffarwelio â Sandra pe bai hi ar ddiwedd ei hoes. | |
| “ | Yn amlwg, roeddech chi'n clywed straeon arswyd ar y newyddion nad oedd pobl yn cael mynd i mewn a dweud hwyl fawr. Felly, fe wnes i ei ffonio mewn gwirionedd a dweud wrtho, 'Os bydd unrhyw beth yn digwydd i fam, a fyddwn ni'n cael dod i mewn?' A dywedodd, 'Yn hollol'. Dywedais i, 'Ydy hynny'n golygu pawb?' Oherwydd yn amlwg mae gen i ddau o blant, mae gan fy chwaer dri. Ac yna dywedodd, 'Yn hollol, byddwch chi'n cael dod i mewn a dweud hwyl fawr'.” |
| Fodd bynnag, pan dderbyniodd Emma alwad ffôn o'r cartref gofal i ddweud bod Sandra yn dod at ddiwedd ei hoes, dim ond dau berson y byddent yn eu gadael i eistedd gyda Sandra. | |
| “ | Ni fyddai'r gofalwr oedd yn gyfrifol am fy mam yn gadael i rai ohonom ni ddod i mewn. Felly, fel y gallwch chi ddychmygu, roedd yn drawmatig ac roedd fy mam yn marw. Cael yr holl straen ychwanegol hwnnw o beidio â gadael i bobl ddod i mewn.” |
| Ychydig cyn i Sandra farw, dywedodd staff gofal wrth Emma a'i chwaer fod yn rhaid iddyn nhw fynd adref. Arweiniodd hyn at ddadl ddwys wrth i Emma wrthod gadael ei mam ar ei phen ei hun. | |
| “ | Dywedodd wrtha i, 'Mae'n rhaid i ti fynd adref'. A dywedais i, 'Dydw i ddim yn mynd adref ac yn gadael Mam i farw ar ei phen ei hun'. Felly, fel arfer dydw i byth yn mynd yn wrthdaro, ond dw i'n cofio fy nhad yn dweud pan oedd e'n marw, 'Peidiwch byth â gadael Mam ar ei phen ei hun, wnewch chi?' Dywedais i, 'Na, wnaf i ddim. Fyddwn ni ddim. Byddwn ni bob amser yn gofalu amdani hi'. Dywedais i wrthi, 'Mae'n ddrwg iawn gen i, ond dydw i ddim yn mynd. Dydw i ddim yn ei gadael hi yma i farw ar ei phen ei hun'.…Ar ôl dadlau am ychydig, collais i fy meddwl, fe wnes i regi arni. Collais i fy meddwl.” |
| Mae'r profiad trawmatig o eistedd gyda Sandra tra bu hi farw a'r sioc o gael gwrthdaro â staff gofal wedi bod yn anodd i Emma ei gymodi ac mae ganddi lawer o emosiynau cymysg o hyd am farwolaeth ei mam ac a gafodd ei siomi ar ddiwedd ei hoes. | |
| “ | Mae gen i deimladau cymysg amdano… Dw i’n meddwl wrth edrych yn ôl arno ein bod ni wedi cael ein trin yn ffiaidd, rhai o’r pethau a ddywedodd y staff wrtha i, mewn gwirionedd ar y pryd mae’n debyg y dylwn i fod wedi gwneud cwyn swyddogol, ond rydych chi mor ddigalon, dydych chi ddim yn gwybod beth i’w wneud. Ac yna’n sydyn, rydych chi’n dal yn y pandemig.” |
Ar ôl marwolaeth aelodau o'u teulu, roedd rhaid i anwyliaid drefnu angladdau a chladdedigaethauNewidiodd cyfyngiadau’r cyfnod clo a phellhau cymdeithasol sut y cynhaliwyd angladdau. Ychwanegodd hyn at dristwch, euogrwydd a theimlad o golled y cyfranwyr.
| “ | Cawson ni dri angladd o berthnasau agos dan glo, pob un ohonyn nhw wedi'u cyfyngu o ran niferoedd. Roedd yn rhaid i ni sefyll ymhell oddi wrth ein gilydd y tu allan i'r amlosgfa ac yna aethoch chi adref. Dw i'n meddwl bod hynny wedi cael effaith fwy arna i, oherwydd roedd hynny'n teimlo'n anghywir ac roeddwn i'n teimlo fel fy mod i wedi ei siomi.”
- Aelod o'r teulu sydd wedi colli rhywun, Lloegr |
| “ | Doedden ni ddim yn cael cael gwylnos nac angladd ac nid oedd offeren angladd, roedd yn cael ei wneud ar-lein ac yna pan ddaeth pawb, doedd neb yn cael dod i'r tŷ i'r arch adael y tŷ. Doedden ni ddim yn cael ymgynnull fel teulu i alaru.”
- Aelod o'r teulu sydd wedi colli rhywun, Gogledd Iwerddon |
| “ | Roedd hi [mam] yn cael ei hamlosgi, ac ni allent roi diwrnod i ni oherwydd bod ôl-groniad. Pan gawson ni ddiwrnod ni fyddent yn dweud amser i ni, yna cafodd fy mrawd alwad i ddweud, 'gyda llaw mae hi wedi cael ei hamlosgi', roedd yn anodd iawn.”
- Aelod o'r teulu sydd wedi colli rhywun, digwyddiad gwrando, Gogledd Iwerddon |
Stori SophieMae Sophie o Lundain, bu’n gweithio ym maes gofal cymdeithasol yn ystod y pandemig, yn ogystal â chefnogi ei mam-yng-nghyfraith a oedd yn byw mewn cartref gofal. Roedd gan fam-yng-nghyfraith Sophie ddementia a bu farw yn ei chartref gofal yn ystod y pandemig. Roedd y cyfyngiadau’n atal teulu Sophie rhag ei gweld ar ôl iddi farw, a chafodd yr angladd ei ohirio hefyd. |
|
| “ | Bu farw ddydd Sadwrn. Ac oherwydd ein crefydd, rydych chi'n cael eich claddu'n gyflym iawn. Dw i'n Iddew. Ac fel arfer, byddai hi wedi cael ei chladdu'r un diwrnod, ond oherwydd Covid, ni allai fod tan ddydd Llun.” |
| Arhosodd mam-yng-nghyfraith Sophie yn ei hystafell tan ei hangladd, gyda gweithiwr cartref gofal yr unig berson a oedd yn gallu ei gweld. | |
| “ | Doedd dim modd mynd â hi i'r tŷ marwolaeth oherwydd Covid. Felly, roedd rhaid iddi aros yn ei hystafell a dywedodd ei gofalwr y byddai'n ei gwylio, ac y byddai'n dal i edrych arni, a oedd yn golygu llawer i ni.” |
| Mynegodd Sophie bryder am nad oedd ei mam-yng-nghyfraith yn cynnal y defodau claddu arferol. | |
| “ | Dydw i ddim yn gwybod a wnaethon nhw eu rhoi mewn arch blastig, dydw i ddim yn gwybod beth wnaethon nhw. Doeddwn i ddim yn gallu gweld hynny. Ond cafodd ei chymryd, ei rhoi'n syth mewn arch ac i'r fynwent. Dydw i ddim yn meddwl y byddan nhw wedi ymolchi'r corff na gwneud unrhyw beth.” |
Mae llawer o deuluoedd mewn galar yn parhau i deimlo'n flin ynghylch yr amgylchiadau sy'n ymwneud â marwolaeth y rhai yr oeddent yn gofalu amdanyntRoedden nhw'n teimlo eu bod nhw wedi cael eu siomi gan y rheolau a'r cyfyngiadau oedd ar waith, yn ogystal â'r ymateb ehangach i'r pandemig.
| “ | Pan fu hi farw, mae'n rhaid fy mod i wedi bod yn flin am flwyddyn dda wedyn, os nad yn hirach. Yn flin iawn nad oedd pobl yn gwrando ar y rheolau – wel, nid oedd y llywodraeth.”
- Aelod o deulu galarus preswylydd cartref gofal, Lloegr |
| “ | Roeddwn i'n flin iawn wedyn…ond allwch chi ddim troi amser yn ôl…cawson ni gymaint wedi'i gymryd oddi wrthym ni yn y blynyddoedd hynny.”
- Aelod o deulu galarus preswylydd cartref gofal, Lloegr |
Dywedodd rhai cyfranwyr mewn galar wrthym sut mae eu mae eu lles a'u hiechyd meddwl eu hunain yn parhau i ddioddef oherwydd natur drawmatig marwolaeth aelod o'u teulu.
| “ | Cymerodd ddwy flynedd i mi ddod i delerau â sut y bu farw, roeddwn i'n arfer deffro yn y nos mewn panig llwyr [am y peth].”
- Aelod o'r teulu sydd wedi colli rhywun, Cymru |
| “ | Roeddwn i’n dal i gael breuddwydion am fy nhad yn marw a’i wyneb ar ôl iddo farw. Byddwn i’n mynd yn flin am beidio â gallu ei weld.”
- Aelod o'r teulu sydd wedi colli rhywun, Lloegr |
5. PPE a mesurau rheoli heintiau |
 |
Mae'r bennod hon yn archwilio'r heriau ac effeithiau o weithredu mesurau rheoli heintiau yn ystod y pandemig. Mae'n disgrifio pryderon ynghylch trosglwyddo'r feirws, Offer Diogelu Personol (PPE) a'u heffaith ar weithwyr gofal, gofalwyr di-dâl a phobl ag anghenion gofal a chymorth.
Pryderon ynghylch trosglwyddo'r firws
Pryder mawr i weithwyr gofal, gofalwyr di-dâl ac anwyliaid yn ystod y pandemig oedd y ofn dal Covid-19 a'i drosglwyddo i eraill, yn enwedig pobl sydd ag anghenion gofal a chymorth.
| “ | Gan eich bod yn rheolwr cartref gofal, dydych chi ddim eisiau bod yn eich rhoi eich hun mewn sefyllfa lle rydych chi'n mynd i ddod â haint i'r cartref, felly roedd fy nghyswllt fy hun â fy nheulu fy hun yn eithaf cyfyngedig. Roedd fy chwaer yn cael triniaeth canser, felly allwn i ddim treulio llawer o amser gyda hi chwaith oherwydd nad oeddwn i eisiau mynd ag unrhyw beth ati, felly roedd y profiad cyfan yn ofnadwy.”
- Rheolwr cofrestredig cartref gofal, Gogledd Iwerddon |
| “ | Roedd yn ddinistriol. Fe wnaeth gau pob agwedd ar fy mywyd i lawr. Mae gen i hunllefau o hyd am fy mab yn marw ohono, fy mam yn ei ddal, roeddwn i wedi fy nychryn.”
- Gofalwr di-dâl, Lloegr |
Roedd gweithwyr gofal cymdeithasol proffesiynol yn ymwybodol iawn o'r risg uwch o drosglwyddo mewn gofal cymdeithasol, a gynyddodd eu pryder. Dywedodd y cyfranwyr wrthym pa mor bryderus oeddent drwy gydol y pandemig, hyd yn oed pan nad oedd ganddyn nhw Covid-19 a bod y pryder hwn wedi effeithio ar eu hiechyd a'u lles corfforol.
| “ | Doeddwn i ddim yn cysgu'n iawn, doeddwn i ddim yn bwyta'n iawn – ond roedd hynny i gyd yn ymwneud â'r pryder o ddal Covid.”
- Gweithiwr gofal iechyd, yr Alban |
Roedd gweithwyr gofal iechyd a chymdeithasol o gefndiroedd lleiafrifoedd ethnig yn arbennig o bryderus ynghylch dal Covid-19 oherwydd yr effaith anghymesur a gafodd Covid-19 ar bobl o'r cefndiroedd hynny. Canfu cyfranwyr nad oedd asesiadau risg yn y gweithle yn ystyried eu risg uwch o ddal a marw o'r feirws.
| “ | Hoffwn ddweud fy mod i'n teimlo fel person eithaf cryf ac annibynnol sydd â meddwl rhesymegol… Y pandemig… oherwydd fy nghefndir ethnig, fe wnaeth greu ofn llwyr. Doeddwn i ddim yn adnabod fy hun… Roedd gen i bryder. Roedd gen i feddyliau afresymol. Byddwn i'n panicio… Felly roedden nhw'n cyhoeddi gwybodaeth eu bod nhw, wn i ddim yr ystadegau, ddwy neu dair gwaith yn fwy tebygol o farw na'u cymheiriaid gwyn pe bydden nhw'n cael Covid. Roeddwn i'n unigolyn BAME [Du, Asiaidd a Lleiafrifoedd Ethnig] nad oedd ganddo ddewis ond gweithio trwy'r pandemig, oherwydd fy rôl i oedd mewn gofal cymdeithasol… Nid oedd ganddo, yn yr asesiad risg, y risg o fod o'r gymuned BAME ac roeddwn i'n dadlau yn fy ngweithle gan ddweud, 'Dylech chi gael asesiad risg arbennig i mi'.”
- Gweithiwr gofal iechyd, yr Alban |
| “ | Bu farw llawer o bobl yn ein cymuned Ddu o ganlyniad i Covid-19 neu Covid-19 yn gwaethygu neu'n achosi cymhlethdodau anhwylderau sylfaenol. Fel y clywsom am fwy a mwy o gydweithwyr, teulu, ffrindiau, henuriaid eglwysig yn marw mewn niferoedd mawr. Llawer o gydweithwyr nyrsio yn cael eu gorfodi i weithio mewn ardaloedd Covid-19 risg uchel hyd yn oed os ydyn nhw eu hunain yn agored i niwed ac mewn perygl uchel o gael eu heintio gyda thebygolrwydd o gael canlyniad gwaeth. Y peth gwaethaf am oes pandemig Covid-19 yw'r ofn, ofn cael yr haint, ofn anabledd posibl fel cymhlethdod Covid-19, ofn marwolaeth, yr unigedd yn enwedig wrth dreulio llawer o ddyddiau'n gweithio o gartref, heb weld teulu, ffrindiau, cydweithwyr.
- Gweithiwr gofal iechyd, Lloegr |
Ar gyfer gweithwyr iechyd a gofal a deithiodd rhwng sawl lleoliad, fel gweithwyr gofal cartref a nyrsys gofal lliniarol, Nid oedd pryderon ynghylch rheoli heintiau yn ymwneud â diogelu'r bobl yr oeddent yn gofalu amdanynt yn unig ond hefyd aelodau eu teulu eu hunainNid oedd ganddyn nhw hyder yn rhai o'r mesurau atal heintiau gan eu bod nhw'n treulio amser gyda chynifer o bobl ac yn poeni am eu hamlygiad eu hunain i haint.
Gwnaeth yr ofnau hyn weithwyr gofal cymdeithasol yn arbennig o ofalus ac, mewn rhai achosion, fe gymerasant ragofalon ychwanegol, fel diheintio eu hunain cyn mynd i mewn i'r cartrefi yr ymwelasant â nhw ar gyfer gwaith yn ogystal â'u cartrefi eu hunain, er mwyn osgoi lledaenu'r firws.
| “ | Roedden ni'n mynd i gartrefi gofal i bobl â salwch meddwl yr henoed [EMI]. Roedden ni'n mynd i gartrefi gofal anabledd dysgu, roedden ni'n mynd i hosteli lle'r oedd pobl oedd wedi cael eu rhyddhau'n gynnar o garchardai, yn mynd i ymweld â nhw. Yna, roedden ni'n amlwg yn mynd o gartrefi gofal yn llawn Covid, yna'n mynd i gartrefi cleifion sy'n cael cemotherapi. Felly, roedd yn gymysg iawn. Roedd yn frawychus iawn. Doeddwn i ddim yn gwybod, pan ddes i allan o'r cartref gofal hwnnw, ni waeth pa mor dda oedd ein PPE, a allwn i o bosibl ei roi i'r claf nesaf a welwn i, a allai fod wedi bod ar gemotherapi ac wedi'i imiwneiddio'n wael.”
- Nyrs gymunedol, Lloegr |
Roedd gan rai cartrefi gofal ystafelloedd newid dynodedig, fel y gallai eu staff newid i mewn ac allan o'u gwisg, gan atal lledaeniad haint rhwng eu cartref eu hunain a'r cartref gofal.
| “ | Doeddech chi ddim yn dod i'r gwaith yn eich gwisg ysgol chwaith, roeddech chi'n newid yma. Roedd gennym ni ystafell newid wedi'i gwneud i fyny'r grisiau, felly roeddech chi'n newid yma ac yna ar ddiwedd y dydd roedd eich gwisg ysgol yn cael ei thynnu i ffwrdd yma, ei golchi yma ac yn amlwg roeddech chi'n ei gwisgo yn ôl y bore wedyn.”
- Gweithiwr cartref gofal, Lloegr |
Clywsom hefyd enghreifftiau o staff yn symud dros dro i'r cartref gofal er mwyn osgoi trosglwyddo haint i'r cartref gofal neu yn ôl i'w cartref eu hunain. Roedd hyn yn golygu treulio cyfnodau hir i ffwrdd o'u teulu a'u ffrindiau eu hunain. Dywedodd cyfranwyr a wnaeth hynny wrthym sut y gwnaethon nhw brofi teimladau cynyddol o ynysu ac unigrwydd o ganlyniad.
Stori SofiaRoedd Sofia yn gweithio mewn cartref gofal yng Ngogledd Lloegr. Ym mis Mai 2020, roedd gan un o breswylwyr y cartref gofal haint Covid-19 tybiedig. O ganlyniad, symudodd Sofia a'i chydweithwyr i'r cartref gofal i ddarparu gofal wrth gefn rhag ofn salwch staff ac i amddiffyn eu preswylwyr agored i niwed. Symudodd rhai o gydweithwyr Sofia i'r cartref gofal hefyd i amddiffyn eu teuluoedd eu hunain. |
|
| “ | Symudon ni i mewn am ychydig wythnosau oherwydd roedden ni’n poeni pe bai llawer o staff yn mynd i ffwrdd y bydden ni’n camu i mewn ac hefyd, roedd gennym ni bobl agored i niwed gartref. Felly, pan wydden ni ei fod wedi cyrraedd yma mewn gwirionedd, symudon ni i mewn yn syth.” |
| Pan gafodd mab Sofia Covid-19 ac nad oedd digon o le yn eu fflat iddo ynysu, symudodd Sofia i'r cartref gofal eto i'w hamddiffyn ei hun a phreswylwyr y cartref gofal.
Drwy gydol y pandemig, byddai Sofia a'i chydweithwyr hefyd yn aros yn y cartref gofal am un neu ddau ddiwrnod pan fyddai achosion o'r afiechyd yn bygwth, oherwydd ansicrwydd ynghylch lefelau staffio ac anghenion cymorth. |
|
Straeon o Stockton-on-TeesRhannodd staff gofal cymdeithasol yn Stockton-on-Tees, mewn digwyddiad gwrando, pa mor ofnus oeddent ynghylch lledaenu Covid-19 i'w teuluoedd. Disgrifion nhw'r frwydr o gydbwyso blaenoriaethau wrth i'r pandemig achosi tensiwn rhwng cyfrifoldebau proffesiynol a chadw eu teuluoedd eu hunain yn ddiogel. |
|
| “ | Roeddwn i'n ofni am fy nheulu fy hun; roedd fy mhartner yn agored i niwed. Pan gyrhaeddwn adref ar ôl shifft, byddwn i'n rhedeg i fyny'r grisiau; roeddwn i'n ofni y byddwn i'n dod â Covid adref. Doeddwn i ddim hyd yn oed eisiau mwytho fy nghŵn.”
– Gweithiwr gofal, digwyddiad gwrando, Lloegr |
| “ | Mae fy ngwraig hefyd yn gweithio yn y maes cymorth ac roedd yn anodd iddi. Ar adegau, byddai hi'n aros mewn gwesty ac weithiau, byddem yn aros gyda'n gilydd gartref, ond roedd llawer o lanhau i'w wneud. Byddwn i'n glanhau'r llawr isaf ac yn sychu popeth. A byddai fy ngwraig yn mynd i fyny'r grisiau.”
– Gweithiwr gofal, digwyddiad gwrando, Lloegr |
Gofynion, canllawiau a chydymffurfiaeth PPE
Cyhoeddodd yr Adran Iechyd a Gofal Cymdeithasol (DHSC) ac Iechyd Cyhoeddus Lloegr (PHE) ganllawiau ar atal a rheoli heintiau (IPC) drwy gydol y pandemig. Roedd hyn yn cynnwys canllawiau ar y defnydd cywir o Offer Diogelu Personol (PPE), fel masgiau, menig, ffedogau, fisorau a diheintydd dwylo. Yna lledaenwyd hyn drwy'r sector gofal drwy awdurdodau lleol a darparwyr gofal.
Roedd canllawiau PPE ar gyfer pobl sy'n derbyn gofal yn amrywio rhwng lleoliadau gofal.Yn aml, nid oedd yn ofynnol i bobl a oedd yn derbyn gofal a chymorth mewn cartrefi gofal wisgo masgiau. Yn gyffredinol, roedd cyfranwyr yn deall y rhesymeg dros hyn, ond myfyriodd rhai ar y risg gynyddol yr oedd yn ei beri.
| “ | Nid oedd rhaid i'n cleientiaid wisgo mwgwd drwy'r amser, weithiau roedd yn teimlo fel ein bod ni'n ceisio eu hamddiffyn - ond pa mor ddiogel oedden ni? Nid oedd cleientiaid yn cael eu gorfodi i wisgo mwgwd.”
- Gweithiwr gofal cartref, Gogledd Iwerddon |
Esboniodd y gweithlu gofal cymdeithasol sut roedd canllawiau PPE yn newid yn aml gan greu dryswch, straen ac ansicrwydd.
| “ | Dw i'n meddwl mai'r newid mwyaf i ni oedd y PPE, oherwydd dw i'n cofio pan ddaeth rhywun i mewn am y tro cyntaf yn gwisgo mwgwd oherwydd nad oedd wedi'i ddarparu, fe wnaethon nhw ei brynu, gofynnodd y rheolwr i'r person hwnnw ei dynnu i ffwrdd oherwydd eu bod nhw'n dweud, 'Sut ydych chi'n disgwyl cyfathrebu â'r preswylwyr? Rydych chi'n mynd i ddychryn y preswylwyr'. Yna, ychydig ddyddiau'n ddiweddarach, roedd yn orfodol i bawb wisgo mwgwd. Felly, roedd yn newid mawr iawn ac yn rhyfedd iawn.”
- Nyrs gymunedol, Lloegr |
Disgrifiodd llawer o weithwyr cartrefi gofal a rheolwyr cofrestredig sut cyfathrebu, rheolau a gweithdrefnau sy'n nodi Roedd yr hyn oedd ei angen yn newid yn gyson a gallai wrth-ddweud cyngor blaenorol. Arweiniodd hyn at heriau o amgylch cynllunio a gwneud penderfyniadau gwybodus yng nghanol canllawiau aneglur.
Ar gyfer gweithwyr gofal cartref, negeseuon anghyson gan eu cyflogwyr a'r llywodraeth eu gadael yn ansicr ynghylch pryd a ble roedd angen iddynt ddefnyddio PPE. Roedd y cyfranwyr hyn yn aml yn gweithio ar eu pen eu hunain mewn gwahanol gartrefi ac yn ei chael hi'n anodd gwybod beth ddylent ei wneud heb gefnogaeth a chyngor gan gydweithwyr.
| “ | Roedd Iechyd Cyhoeddus Lloegr yn cyhoeddi canllawiau bob dydd – yn arbennig cyhoeddwyd y newid i ganllawiau ar PPE am 11pm nos Wener heb unrhyw gyfarwyddyd ar sut y gallem gaffael offer o'r fath. Cyfriais dros 200 o ddarnau o ganllawiau a gyhoeddwyd mewn mis y bu'n rhaid i mi eu darllen a'u rhoi ar waith yn bersonol.”
- Rheolwr cofrestredig, Lloegr |
| “ | Cafodd y newidiadau eu gorfodi'n rhy gyflym, roedden ni'n gwybod bod angen iddyn nhw fod yn gyflym oherwydd bod y llywodraeth yn ymateb yn hwyr, ond roedd y newidiadau'n rhy gyflym ac yn rhy afreolaidd. Newidion nhw ormod - un diwrnod roedd hyn, y diwrnod arall roedd hynny. Doedden nhw ddim yn canolbwyntio digon ar y prif beth - PPE - doedd gennym ni ddim yr hyn oedd ei angen arnom ni o ran PPE.”
- Gweithiwr cartref gofal, Lloegr |
| “ | Anfonwyd negeseuon e-bost allan [gan y rheolwyr] yn dweud bod yn rhaid i ni wisgo mwgwd, lle mewn negeseuon e-bost eraill dywedasant nad oes rhaid i ni. Roedd bob amser braidd yn ddryslyd.”
- Gweithiwr gofal cartref, Lloegr |
Wrth i'r pandemig fynd rhagddo, gweithredwyd canllawiau PPE llymach, gan gynnwys gweithdrefnau penodol ar gyfer gwisgo a thynnu PPE (gwisgo a thynnu PPE i ffwrdd). Dywedodd y gweithlu gofal cymdeithasol wrthym sut roedd yn rhaid tynnu masgiau, menig a ffedogau i ffwrdd a'u gwaredu'n gywir rhwng pob pennod o ofal i atal lledaeniad yr haint.
Rhannodd rhai gweithwyr cartrefi gofal sut maen nhw wedi derbyn hyfforddiant mynych a thrylwyr ynghylch sut i ddefnyddio PPE. Roedd hyn yn cynnwys hyfforddiant ac arddangosiadau ar-lein ac wyneb yn wyneb a hyfforddiant gloywi ynghylch sut i wisgo PPE, sicrhau hylendid dwylo a rheoli heintiau yn gyffredinol.
| “ | Cawson ni lawer o hyfforddiant dwys oherwydd roedd yn rhaid i mi gael briffiau gyda'm holl ofalwyr i wneud yn siŵr eu bod nhw'n dilyn yr holl ganllawiau a gyflwynwyd gan y llywodraeth.”
- Rheolwr cofrestredig, Lloegr |
| “ | Roedd yn rhaid i ni wneud modiwl hyfforddi mewn gwirionedd, fideo i wylio sut i ddefnyddio a gwaredu PPE drwy gydol y pandemig. Felly, roedd yr un peth ag ar gyfer golchi hefyd.”
- Nyrs gofal lliniarol, yr Alban |
Fodd bynnag, mynegodd nifer o reolwyr cartrefi gofal bryderon ynghylch y pwysau ychwanegol o oruchwylio hyfforddiant PPE a diffyg cefnogaeth ac arweiniad allanol.
| “ | Yn aml, daeth cymorth yn rhy hwyr i fod yn effeithiol. Roedden ni’n brysur yn ceisio hyfforddi staff cartrefi gofal i ddefnyddio PPE yn gywir. Yn y diwedd, cynigiwyd cefnogaeth i ni gan y CCG [Grŵp Comisiynu Clinigol] ar gyfer yr hyfforddiant hwn – naw mis i mewn i’r pandemig. Dywedwyd wrthym fod gennym ni arweinydd dynodedig a oedd i fod yn gysylltiad â’r GIG. Ni ddywedwyd wrthym ni erioed pwy oedd y person hwn na sut i gysylltu â nhw. Yn sicr, ni wnaethon nhw erioed gysylltu â ni.”
- Rheolwr cofrestredig mewn cartref gofal, Lloegr |
Yn gyffredinol, y roedd defnyddio PPE mewn lleoliadau gofal yn rhoi ymdeimlad o sicrwydd i weithwyr gofal cymdeithasol proffesiynol, gofalwyr di-dâl, anwyliaid a phobl ag anghenion gofal a chymorth. Yn benodol, roedd dealltwriaeth gyffredin ar draws y grwpiau hyn bod PPE yn bwysig i atal y feirws rhag lledaenu.
| “ | Roeddwn i'n teimlo'n well eu bod nhw'n gwisgo PPE ac yn rhoi amddiffyniad i ni fel na fyddem ni'n dal unrhyw beth hefyd ... roedd yn galonogol.”
- Person ag anghenion gofal a chymorth, Lloegr |
| “ | Y ffaith bod gennym y PPE oedd ei angen arnom, roeddwn i'n gwybod sut i'w defnyddio, ond roedd y gefnogaeth honno ar gael bob amser os oedd ei hangen arnom. Roeddwn i'n teimlo bod y polisïau oedd ar waith yn cyrraedd y safon, yn ddigon i'm cadw'n ddiogel.”
- Gweithiwr gofal cartref, Lloegr |
Dywedodd pobl ag anghenion gofal a chymorth wrthym fod gweithwyr gofal yn defnyddio PPE fel ffedogau a menig yn rheolaidd cyn y pandemig. Y prif newid unwaith i'r pandemig ddechrau oedd y defnydd o fasgiau wyneb.
| “ | Yr unig PPE ychwanegol a ddefnyddiwyd mewn gwirionedd oedd masgiau. Hynny yw, maen nhw'n defnyddio menig a ffedogau beth bynnag. Maen nhw'n amlwg yn defnyddio menig drwy'r amser. Ond weithiau, byddan nhw'n defnyddio ffedogau, yn dibynnu ar yr hyn maen nhw'n ei wneud. Felly, yr unig ychwanegiad newydd go iawn oedd y masgiau.”
- Person ag anghenion gofal a chymorth, yr Alban |
Fodd bynnag, dywedodd rhai cyfranwyr eraill wrthym sut roedd gweithwyr gofal yn gwisgo PPE yn anghywir, neu ddim o gwbl, ar adegau a arweiniodd at bryder ynghylch lledaeniad yr haint.
| “ | Dylai gofalwyr wisgo masgiau ond, yn anffodus, roedd llawer ohonyn nhw'n gwisgo eu masgiau o dan eu trwynau ac yn gorchuddio eu cegau bron. Ac fe benderfynodd rhai ohonyn nhw nad oedd hynny hyd yn oed yn angenrheidiol a'u gwisgo o dan eu genau.”
- Person ag anghenion gofal a chymorth, Gogledd Iwerddon |
| “ | Doedd gan y staff ddim PPE llawn ymlaen. Byddai rhai staff yn dod i mewn, bydden nhw'n gwisgo mwgwd. Doedd gan rai ohonyn nhw ddim ffedog ymlaen a doedd gan rai ohonyn nhw ddim hyd yn oed fenig ymlaen, felly meddyliais i, wel, does ryfedd fod hanner y bobl yma'n marw, oherwydd rydych chi'n ei basio ymlaen i bawb oherwydd nad ydych chi'n gwisgo'r PPE cywir.”
- Anwylyd preswylydd cartref gofal, Gogledd Iwerddon |
Yn gynnar yn y pandemig, dywedodd rhai pobl ag anghenion gofal a chymorth wrthym eu bod wedi gofyn yn rhagweithiol i staff gofal cartref wisgo masgiau oherwydd eu bod mor bryderus am ddal Covid-19. Fodd bynnag, hyd yn oed pan ofynnwyd am fasgiau'n benodol, nid oedd gweithwyr gofal bob amser yn eu gwisgo'n iawn.
| “ | Roeddwn i'n dechrau poeni'n fawr amdano. Ar ôl i mi ddweud fy mod i eisiau i'r gofalwyr wisgo masgiau, roedd yn rhaid i mi siarad â'r gofalwyr yn unigol a dweud wrthyn nhw, 'Os gwelwch yn dda, os gwelwch yn dda, er fy mwyn i, a fyddech chi'n gwisgo masgiau?' Gwnaeth rhai ohonyn nhw hynny. Yna dechreuais wisgo'r masg ond mae hynny ychydig yn anodd os ydych chi'n cael eich gwallt wedi'i olchi oherwydd mae'r peth yn mynd i ddadfeilio.”
- Person ag anghenion gofal a chymorth, Gogledd Iwerddon |
Er gwaethaf rhai pryderon, adroddodd pobl ag anghenion gofal a chymorth a'u hanwyliaid am ddefnydd da a chyson o PPE mewn cartrefi gofal a chan weithwyr gofal cartref. Trafododd preswylwyr cartrefi gofal dderbyn eu gel gwrthfacteria a’u PPE eu hunain i’w defnyddio pan fo angen a gofynnwyd iddynt olchi eu dwylo mor rheolaidd â phosibl. defnyddio PPE yn galonogol ac roeddent yn teimlo'n fwy diogel pe bai pobl eraill yn defnyddio PPE wrth ryngweithio'n agos â nhw.
| “ | Rhoddwyd diheintyddion bach i ni, poteli bach o ddiheintyddion. Cafodd popeth ei ofalu amdano. Hynny yw, fe wnaethon nhw waith da iawn.”
- Person ag anghenion gofal a chymorth, Lloegr |
| “ | Roedd y staff yn glynu'n gaeth at yr hyn yr oeddent yn cael eu gofyn i'w wneud, gan fabwysiadu'r mesurau newydd mewn perthynas â rheoli heintiau. Fel teulu, roeddem yn dawel ein meddwl bod y staff yn gymwys ac yn brofiadol.”
- Anwylyd preswylydd cartref gofal, Lloegr |
Prinder PPE
Roedd y rhan fwyaf o gyfranwyr yn pryderu am yr amrywiol argaeledd PPERoedd y galw mawr, ynghyd ag aflonyddwch yn y gadwyn gyflenwi, yn golygu bod y rhan fwyaf o weithwyr gofal cymdeithasol proffesiynol yn wynebu heriau. cael mynediad at PPE, yn enwedig ar ddechrau'r pandemig. Er bod rhai gweithwyr gofal iechyd proffesiynol, fel nyrsys gofal lliniarol, wedi nodi bod ganddynt gyflenwadau PPE digonol, roedd eraill, gan gynnwys nyrsys cymunedol, gweithwyr cymdeithasol, dietegwyr a'r rhai sy'n gweithio mewn cartrefi gofal a lleoliadau gofal cartref, yn wynebu prinder sylweddol.
Trafododd rhai cyfranwyr fod PPE yn cael ei ddargyfeirio o gartrefi gofal i ysbytai, yn ogystal â chartrefi gofal yn cael blaenoriaeth dros ofal cartref. Roedd y rhai a oedd yn gweithio mewn lleoliadau cymunedol yn teimlo eu bod yn cael eu tanbrisio a'u diogelu'n annigonol, gan gredu bod ysbytai yn cael eu trin yn ffafriol.
| “ | Ar ddechrau 2020 roeddwn i'n gynorthwyydd gofal iechyd mewn cartref nyrsio. Es i i mewn i'r storfa – 15 troedfedd x 18 troedfedd – felly nid cwpwrdd bach mohono. Roedd yr ystafell storio bob amser yn llawn i'r ymyl, dyna lle roedd yr holl PPE yn cael ei storio, menig, ffedogau, bagiau golchi dillad, cadachau, padiau ac ati. Cefais fy synnu, roeddwn i'n meddwl ein bod ni wedi cael ein hysbeilio. Roedd yr ystafell yn wag ar wahân i 2 focs o fenig ac ychydig o badiau. Dywedwyd wrthym fod yr angen gan y GIG yn fwy. Roedd gan y staff PPE sydd wedi dyddio, os o gwbl.”
- Gweithiwr gofal iechyd, Lloegr |
| “ | Roedd gennym gyflenwyr a oedd wedi caffael PPE i ni a fyddai'n ein ffonio ni ar y bore pan oedd llwyth ar fin cyrraedd y DU ac yn dweud wrthym fod y danfoniad wedi'i herwgipio i bob pwrpas gan y llywodraeth a'i fod wedi'i flaenoriaethu ar gyfer y GIG ac felly na fyddent yn gallu ei gyflenwi i ni mwyach.”
- Gweithiwr gofal cartref, Lloegr |
Gorfodwyd llawer o weithwyr gofal cymdeithasol proffesiynol i ddod o hyd i'w cyflenwyr eu hunain o PPE a'u sicrhau oherwydd prinder eang.Cafodd llawer ohonynt PPE o ffynonellau anarferol fel gwefannau, cysylltiadau personol neu drwy roddion gan y gymuned leol. Disgrifiodd staff hefyd orfod talu am eu PPE eu hunain i wneud yn siŵr eu bod wedi'u diogelu. Trafododd cyfranwyr hefyd wneud eu masgiau eu hunain, prynu diheintydd dwylo gan fusnesau lleol neu ddibynnu ar roddion. Cymerodd hyn i gyd amser ac ymdrech.
| “ | Ar y dechrau, nid oedd y PPE yn dod o fewn gofal iechyd na'r llywodraeth, roedd yn dod gan bobl leol a busnesau oedd â masgiau ar gyfer eu llinell waith ac roedden nhw'n eu dwyn i ddrws y cartref oherwydd eu bod nhw'n gwybod bod gennym ni gyn lleied. Gwnaeth pobl leol fisorau a sgwrbs. Cymeron ni'r hyn a roddodd y bobl garedig hyn i ni ac roedden ni'n ddiolchgar iawn..”
- Gweithiwr cartref gofal, Lloegr |
| “ | Byddwn i'n mynd at fy nghymydog drws nesaf oedd yn dda am wnïo masgiau, oherwydd ei bod hi'n anodd cael masgiau sylfaenol. Yr offer PPE, jôc oedd hwnnw oherwydd roedd diffyg ohono..”
- Gweithiwr gofal cartref, Lloegr |
Dywedodd pobl ag anghenion gofal a chymorth wrthym hefyd sut y cawsant eu cefnogi gan deulu, ffrindiau neu sefydliadau cymunedol i ddod o hyd i PPE fel masgiau wyneb, menig a gel gwrthfacteria. Dywedodd rhai gofalwyr di-dâl wrthym sut roeddent yn poeni am brinder offer glanhau fel diheintydd dwylo.
| “ | Fe'u danfonwyd atom ni…cawsom fasgiau a menig, felly roedd hynny'n iawn, wnaeth hynny ddim costio dim i ni ac fe wnaethon nhw roi hynny i ni a datrys y broblem [o beidio â gallu dod o hyd i PPE].”
- Gofalwr di-dâl, Gogledd Iwerddon |
| “ | Daeth glanweithydd yn broblem ar un adeg, oherwydd i mi fynd mor obsesiynol-cyfyngedig ag ef. Es i drwyddo. Yna, aeth i bwynt lle na allech chi ei gael yn unman..”
- Gofalwr di-dâl, yr Alban |
Tynnodd llawer o gyfranwyr sylw at gost uwch PPE yn ystod y pandemig, gan arwain at ddrwgdeimlad eang tuag at gyflenwyr PPE ac elwa o'r pandemig.
| “ | Cafodd pethau a oedd fel arfer yn costio ceiniog neu ddwy geiniog i chi eu chwyddo, fel, i £1. Ac os meddylia i'n ôl i'r adeg pan oedd yn rhaid i ni godi arian, dyna oedd y neges yr oeddem yn ei rhoi i roddwyr..”
- Gweithiwr cartref gofal, Lloegr |
| “ | Oherwydd yn amlwg roedd pobl yn neidio ar y bandwagon oherwydd yn sydyn roedd llawer o elw i'w wneud ar PPE. Ac fe brynon ni lwyth o gynwysyddion, costiodd gymaint i ni…dw i'n meddwl ei fod yn £72,000.
- Rheolwr cofrestredig, Lloegr |
| “ | Roedd pobl yn codi'r prisiau. Roedd y prisiau'n ormodol ar y pwynt hwnnw, ac yna roedd llawer o gwmnïau a ddechreuodd eu cynhyrchu, ac roedd yn fusnes mawr iawn.”
- Rheolwr cofrestredig, Gogledd Iwerddon |
Pan nad oedd y gweithlu gofal cymdeithasol yn gallu dod o hyd i PPE, fe wnaethant eitemau untro wedi'u hailddefnyddio (megis masgiau a ffedogau) neu cyfyngedig pa mor aml yr oeddent yn defnyddio PPE ac roeddent yn ymwybodol o beidio â'i wastraffu.
| “ | Roedd gennym ni brinder o PPE. Ar y dechrau, roedd un mwgwd y nos yn cael ei ddarparu. Ac yna os oeddech chi'n trin claf Covid, roedd yn rhaid i chi ail-wisgo hwnnw, ei roi mewn amlen fach, ei wisgo, mynd i mewn i'r ystafell, fel pan fyddwch chi'n mynd i mewn i'r claf hwnnw eto, roedd yn rhaid i chi ail-wisgo'ch mwgwd.”
- Gweithiwr cartref gofal, yr Alban |
Roedd diffyg mynediad at PPE yn golygu nad oedd rhai gweithwyr eisiau cyflawni eu rôl gofalu, rhag ofn dal y feirws. Mewn cartrefi gofal, cafodd hyn ei waethygu trwy weld gweithwyr gofal iechyd allanol a gweithwyr proffesiynol eraill yn cyrraedd y cartref gofal mewn PPE llawn, gan wneud i staff deimlo nad oeddent yn cael blaenoriaeth.
| “ | Roedd angladdwyr yn dod yma gyda siwtiau deunydd peryglus a'r anadlyddion mawr hyn ac rydyn ni'n eistedd gyda masgiau bregus a ffedog.”
- Gweithiwr cartref gofal, Gogledd Iwerddon |
| “ | Dw i'n cofio'r rheolwyr yn cael eu cynghori mor wael ar PPE, ond roeddwn i'n gallu gweld staff y GIG mewn masgiau a dillad amddiffynnol llawn, roedd gennym ni fasgiau papur a dywedwyd wrthym i'w gwisgo dim ond pan fyddwch chi'n darparu gofal personol i'r rhai mwyaf agored i niwed gan nad oedd gan y cartref gofal ddigon o stoc.”
- Cyn gweithio gartref, Lloegr |
Dywedodd cyfranwyr o bob grŵp wrthym, yn gyffredinol, daeth mynediad at PPE yn llai o bryder yn ddiweddarach yn y pandemig wrth i'r llywodraeth ddechrau cyhoeddi cyflenwadau am ddim ac roedd digon o PPE i ddiwallu eu hanghenion.
Ansawdd PPE
Roedd barn gymysg ar ansawdd y PPE ar draws y gweithlu gofal cymdeithasol. Roedd rhai pobl yn fodlon ar ansawdd y PPE a gawsant tra bod eraill yn mynegi pryder. Roedd staff yn poeni am y risg o haint gan fod PPE o ansawdd gwael yn ychwanegu at yr amser gwisgo a thynnu i ffwrdd. Gallai ansawdd PPE hefyd amrywio rhwng sypiau neu yn ôl cyflenwr., gan ychwanegu at y gwaith o archebu PPE a chreu ansicrwydd.
| “ | Roedd ansawdd y PPE yn eithaf da. Doeddwn i ddim yn gallu cwyno amdano. Gwnaeth y gwaith, a dweud y gwir.”
- Gweithiwr gofal iechyd mewn cartref gofal, Lloegr |
| “ | Byddech chi'n tynnu un ffedog allan, byddai'n rhwygo, byddech chi'n tynnu un arall allan ac yn treulio mwy o amser yn ceisio gwisgo'r dillad amddiffynnol priodol. Roedd yr un peth gyda'r masgiau wyneb, byddai'r elastig yn dod i ffwrdd, byddai'n cwympo i lawr, roeddech chi'n agored i niwed.”
- Gweithiwr cartref gofal, Lloegr |
| “ | Roedd yr ansawdd yn ofnadwy. Roedden ni wedi mynd o rai eithaf trwchus, o ansawdd da i rai o'r menig, roeddech chi'n arfer codi'r pâr ac roeddech chi'n gallu gweld yn syth drwyddynt. Roedd masgiau'n fregus iawn. Menig, dwi'n cofio un o'r merched, fe ddaethon ni o hyd i hen flwch o fenig. Llenwodd hi ef â dŵr o'r tap, roedd yn dal dŵr. Y menig newydd, ie, darnau bach o ollyngiad, nad yw'n dda pan fyddwch chi'n delio â hylifau corfforol a phethau. Diferynnau dŵr. Aeth y masgiau o fod yn dri haen i ddau haen. Yn amlwg, gan gymryd yr haen ychwanegol honno, bydd mwy o ddiferion yn dod drwodd.”
- Nyrs gymunedol, Lloegr |
Dywedodd gweithwyr gofal wrthym hefyd eu bod wedi derbyn PPE a oedd allan o ddyddiad. Mynegodd rhai bryder ynghylch defnyddio PPE sydd wedi dyddio, ond fe wnaethant barhau i'w ddefnyddio gan mai dyma'r cyfan yr oeddent yn gallu ei gael. teimlo'n danbrisiedig pan ddigwyddodd hyn. Roedden nhw'n meddwl bod hyn yn arwydd bod roedd eu hamddiffyn yn llai pwysig.
| “ | Mae sut y gall [PPE] fod allan o ddyddiad ychydig y tu hwnt i'm dealltwriaeth i, ond roedd gan yr hyn a roddwyd i ni ddyddiad arno a oedd allan o ddyddiad. Felly, rwy'n teimlo mai dyna faint roedden ni'n bwysig.”
- Gweithiwr gofal cartref, Lloegr |
Defnyddio PPE a mesurau rheoli heintiau eraill
Ar y cyfan, cafodd cyfranwyr eu sicrhau gan y defnydd o PPE yn ystod y pandemig ac roeddent yn teimlo ei bod yn bwysig atal y feirws rhag lledaenu. Trafodasant hefyd sut mae gwisgo masgiau wyneb a PPE arall bellach wedi dod yn norm. Roeddent yn teimlo bod hyn yn effaith gadarnhaol y pandemig gan iddo leihau lledaeniad yr haint yn gyffredinol.
| “ | Os oes gan rywun annwyd neu rywbeth ac nad ydych chi eisiau ei ddal neu nad ydych chi eisiau cael eich tisian drostoch chi neu beth bynnag, gallwch chi ofyn iddyn nhw wisgo mwgwd os oes ganddyn nhw rai. Felly, mae hynny'n eithaf da.”
- Person ag anghenion gofal a chymorth, Lloegr |
Er bod y rhan fwyaf o gyfranwyr yn cydnabod pwysigrwydd PPE ac yn cefnogi ei ddefnydd, roeddent hefyd yn cydnabod yr heriau a'r anghysur y gallai eu hachosi. Cafodd gweithwyr gofal eu heffeithio'n andwyol gan effeithiau corfforol gwisgo PPE, yn enwedig pan gafodd ei ystyried yn ansawdd gwael. Rhannodd rhai sut Roedd PPE yn eu gwneud yn boeth ac yn anghyfforddus i'w wisgoDywedodd gweithwyr gofal wrthym sut roedd masgiau’n achosi cleisiau ar eu hwyneb, brechau, anawsterau anadlu a blinder o’u gwisgo’n barhaus.
| “ | Roedd hi'n boeth, roedd hi'n chwyslyd, roedd gennych chi frechau ar hyd a lled eich wyneb…y golchi dwylo gormodol, y geliau: dydy o ddim wedi gwneud dim i'm croen.”
- Gweithiwr gofal cartref, Lloegr |
Gwaethygwyd yr anghysur a brofwyd gan weithwyr gofal gan orfod gwisgo PPE am gyfnodau hir o amser oherwydd cyflenwadau cyfyngedig, sy'n golygu nad oeddent yn gallu bwyta, yfed na mynd i'r toiled.
| “ | Byddem yn gwisgo'n arbennig am y diwrnod yn y cartref ac yn methu tynnu'r PPE i ffwrdd tan egwyl benodedig, felly allwn ni ddim defnyddio'r toiled, allwn ni ddim cael diod, dim byd. Y cyfan y gallem ei wneud oedd chwysu o dan haenau a haenau o blastig, gyda masgiau a sgriniau wyneb, gan geisio tawelu meddyliau pobl hŷn dryslyd nad oeddent yn deall pam roedden ni'n edrych fel 'na, pam na allent wneud y pethau a chael yr ansawdd bywyd yr oeddent wedi arfer ag ef.”
- Gweithiwr gofal iechyd, Lloegr |
Roedd y gweithlu gofal cymdeithasol hefyd yn cofio sut y gwnaed ffedogau symud a thrin yn fwy lletchwith gan y byddent yn mynd yn y ffordd wrth ddarparu gofal. Yn ogystal, roeddent yn teimlo bod PPE yn anghyfforddus a bod hynny'n effeithio ar eu lles yn y gwaith.
| “ | Yn aml, byddai [PPE] yn arwain at i chi deimlo'n llawer poethach ac yn eithaf anghyfforddus, a fydd wedyn yn bwydo i ffactorau eraill fel sut rydych chi'n cyflawni eich rôl.”
- Gweithiwr cartref gofal, Gogledd Iwerddon |
Mae'r defnydd o PPE, er ei fod yn galonogol i bawb, hefyd rhwystrau cyfathrebu wedi'u creuRhannodd gweithwyr gofal a phobl ag anghenion gofal a chymorth sut roedd methu â gweld mynegiadau wyneb a dehongli arwyddion di-eiriau wrth wisgo masgiau yn gwneud cyfathrebu'n fwy heriol ac yn peri straen ar berthnasoedd.
| “ | Roeddwn i'n teimlo'n flin dros y bobl rwy'n eu cefnogi, pobl nad ydyn nhw'n siarad; mae angen ciwiau arnyn nhw, ond doedden nhw ddim yn gallu gweld ein hwynebau pan oedden ni'n siarad gyda'r holl PPE ymlaen. Doedden nhw ddim yn gallu deall pan oedden ni'n siarad pan oedden ni'n gwisgo PPE. Roedden nhw'n ceisio ei rwygo oddi arnoch chi ar adegau, ac yna roedden nhw'n cael eu gweld fel rhai heriol, ond doedden nhw ddim, doedden nhw ddim yn gallu ein gweld na'n clywed ni.”
- Gweithiwr cartref gofal, Lloegr |
Myfyriodd pobl ag anghenion gofal a chymorth ar ba mor anodd oedd cyfathrebu a deall y rhai oedd yn gofalu amdanynt pan oeddent yn gwisgo masgiau wyneb.
| “ | Mae [gwisgo mwgwd] yn datgysylltu oddi wrth, fel, ni allwch chi ddarllen mynegiant wyneb yn yr un ffordd… Doeddwn i ddim yn sylweddoli faint rydych chi'n naturiol yn dibynnu ychydig ar ddarllen gwefusau heb sylweddoli.”
- Person ag anghenion gofal a chymorth, Lloegr |
I'r rhai oedd yn gofalu am unigolion oedd yn fyddar neu'n drwm eu clyw, roedd yr anallu i ddarllen gwefusau yn her sylweddolI oresgyn hyn, roedd gweithwyr gofal yn siarad yn uwch, a allai gael ei ystyried yn anghwrtais. Nododd eraill sut na allai pobl fyddar ddibynnu ar ddarllen gwefusau mwyach ac weithiau byddent yn ceisio tynnu masgiau'r gweithwyr gofal yn gorfforol. Weithiau roedd yn rhaid i weithwyr gofal dynnu eu masg i gyfathrebu â phobl, a allai gynyddu'r risg o drosglwyddo iddynt hwy eu hunain a'r rhai sy'n derbyn gofal.
Roedd y defnydd o PPE yn amrywio ymhlith gofalwyr di-dâl, yn dibynnu ar anghenion penodol eu cartref. Dewisodd rhai beidio â defnyddio PPE yn y cartref neu mewn cysylltiad agos â ffrindiau neu deulu wrth iddynt agosáu at ddiwedd eu hoes, gan eu bod yn well ganddynt gadw pethau mor normal â phosibl a'i gwneud hi'n haws cyfathrebu.
| “ | Roedd Mam eisiau gweld ein hwynebau ac roedd ein tad yn marw, felly, roedd hi fel, 'Os yw e'n cael Covid nawr does dim ots'. Roedd hi'n ddibwrpas ein gorchuddio ein hunain ac roedd e eisiau ein gweld ni ac roedden ni eisiau ei weld e.”
- Gofalwr di-dâl, Gogledd Iwerddon |
Awgrymodd gofalwyr a gweithwyr gofal di-dâl fod achosodd masgiau wyneb ofid a gofid i rai pobl â dementia a'r rhai ag anabledd dysgu, gan eu bod yn ei chael hi'n frawychus ac yn ddryslyd peidio â gallu gweld wynebau pobl. Lle'r oedd gofyn iddynt wisgo mwgwd, nid oeddent bob amser yn gallu deall pam. Mewn rhai achosion, arweiniodd hyn at ymddygiadau heriol. Roedd darparu gofal yn yr amgylchiadau hyn yn anodd i ofalwyr a gweithwyr gofal di-dâl.
| “ | Roedd [Fy mam] yn cael trafferth gyda'r mwgwd ac roedd hi'n panicio ychydig ac roedd yn anodd iawn ac roedd yn rhaid i mi ddweud, 'Ceisia gadw dy fwgwd ymlaen, Mam. Rhowch ef dros dy drwyn, rhowch ef dros dy geg'. Doedd e ddim yn hawdd.”
- Anwylyd rhywun sy'n derbyn gofal cartref, Cymru |
Roedd anwyliaid a gofalwyr di-dâl eisiau i fesurau rheoli heintiau gael eu rhoi ar waith mewn ffordd a oedd yn dangos gofal ac ystyriaeth i bobl sy'n byw mewn cartrefi gofal.Roedd cyfranwyr yn ei chael hi'n ofidus ac yn bryderus lle nad oedd hyn yn ymddangos yn wir. Roeddent yn aml yn poeni am lesiant y rhai a oedd yn derbyn gofal. Er enghraifft, dywedodd cyfranwyr wrthym am PPE yn cael ei adael ar ôl wrth i staff adael ystafell preswylydd a oedd yn gwneud iddynt deimlo'n llai cyfforddus a'u bod yn cael gofal llai.
| “ | Bob tro bydden nhw'n defnyddio'r PPE, wrth iddyn nhw gerdded allan, bydden nhw'n tynnu eu holl PPE i ffwrdd ac yn ei adael [yno]. Felly, roedd yr ystafell yn teimlo fel bin sbwriel gwaedlyd.”
- Anwylyd preswylydd cartref gofal, Lloegr |
Roedd y gofyniad i wisgo a thynnu PPE rhwng ymweliadau gofal, yn unol â chanllawiau Covid-19, hefyd yn rhoi pwysau amser sylweddol ar weithwyr gofal, yn enwedig staff gofal cartref a oedd yn ymweld â'r cartref sawl gwaith bob dydd. Roedd yr angen cyson hwn i newid a chael gwared ar PPE ar ôl pob cyswllt gofal yn effeithio ar rai gweithwyr yn gorfforol, gan achosi anghysur, tra i eraill roedd yn lleihau'r amser a oedd ar gael i ddarparu gofal.
| “ | Os oedden ni'n mynd i mewn i dŷ, roedd yn rhaid i ni wisgo'n ffansi; cyn i chi ddod allan, roedd yn rhaid tynnu popeth i ffwrdd. Roedd yn rhaid cofio'r weithdrefn. Roeddech chi'n mynd i mewn iddo yn y pen draw, ond roedd yr holl newid cyson hwn yn rhywbeth.”
- Gweithiwr gofal cartref, Lloegr |
Profi Covid-19
Roedd profion Covid-19 yn fesur rheoli heintiau hanfodol yn ystod y pandemigRhoddodd cyflwyno profion sicrwydd mawr ei angen. Roedd mynediad at brofion Covid-19 yn hanfodol i weithwyr gofal cymdeithasol proffesiynol o ystyried symud gweithwyr gofal rhwng cartrefi gofal, lleoliadau gofal eraill a'u cartrefi eu hunain. Mae pwnc profion Covid-19 ar gyfer preswylwyr wrth eu rhyddhau o'r ysbyty i gartrefi gofal wedi'i drafod ym Mhennod 3.
Nodweddwyd camau cynnar y pandemig gan mynediad amrywiol at brofion Covid-19 a rhwystrau logistaiddI ddechrau, dim ond profion PCR oedd ar gael, ac roedd angen eu prosesu mewn safleoedd pwrpasol. Blaenoriaethwyd profion PCR ar gyfer grwpiau penodol, megis unigolion â chyflyrau iechyd sylfaenol, staff rheng flaen y GIG a gweithwyr gofal. Nododd cyflwyniad Profion Llif Ochrol (LFTs) wedi hynny symudiad sylweddol tuag at brofion mwy hygyrch a chyflym..
I ddechrau, roedd rhai gweithwyr cartrefi gofal yn ei chael hi'n anodd cael profion iddyn nhw eu hunain a phreswylwyrYn ogystal, cafwyd adroddiadau am brofion PCR coll ac oedi wrth dderbyn canlyniadau profion.
| “ | Cafodd profion eu gohirio, aeth citiau prawf ar goll ar ôl eu casglu, bu’n rhaid mynd ar ôl canlyniadau profion a methodd â’u canfod – cyflwynwyd profion dro ar ôl tro am y rheswm hwn, a wastraffodd y PPE cyfyngedig yr oeddem yn gallu ei gael.”
- Gweithiwr cartref gofal, Gogledd Iwerddon |
Fodd bynnag, yn ddiweddarach yn y pandemig, nododd cyfranwyr fod ganddynt fynediad digonol at brofion, yn enwedig LFTs.
Roedd protocolau profi yn amrywio ar draws lleoliadau gofal, rolau swyddi a thrwy gydol y pandemigRoedd rhai sefydliadau gofal yn gweithredu neu'n gofyn am brofion dyddiol gan staff, tra bod eraill yn profi'n wythnosol neu dim ond pan gododd symptomau. Helpodd profion lawer o staff i deimlo'n fwy hyderus nad oeddent yn lledaenu'r feirws i'r rhai yr oeddent yn darparu gofal iddyntFodd bynnag, roedd yna achosion hefyd lle roeddent yn teimlo dan bwysau i brofi'n aml, hyd yn oed pan oeddent yn asymptomatig. Roedd profion rheolaidd hefyd yn ychwanegu at eu llwyth gwaith.
| “ | Roedd gennym drefn brofi llym iawn ond drwy gydol 2020 roedd yn brawf PCR wythnosol tan fis Rhagfyr 2020 pan gyflwynwyd profion llif ochrol ddwywaith yr wythnos ynghyd â phrofion PCR wythnosol.”
- Gweithiwr cartref gofal, Lloegr |
| “ | Bob bore, roedden ni i fod i gael prawf Covid. Roedd yn rhaid i chi dynnu llun ac anfon e-bost i'n swyddfa yn dweud, 'Dyma brawf heddiw dim ond i brofi nad ydw i'n lledaenu haint. Mae fy mhrawf yn negyddol a gallaf barhau i weithio', ar y diwrnod hwnnw.”
- Gweithiwr gofal cartref, Lloegr |
Profi daeth preswylwyr cartrefi gofal yn weithdrefn safonol. Yn gynnar yn y pandemig, roedd hyn yn arbennig o bwysig pan gafodd cleifion ysbyty eu rhyddhau i gartrefi gofal. I ddechrau, defnyddiwyd profion PCR, a oedd angen eu prosesu mewn safleoedd pwrpasol. Yn ddiweddarach, caniataodd cyflwyno Profion Llif Ochrol (LFTs) brofion cyflymach. Gellir dod o hyd i fwy o fanylion am brofiadau rhyddhau o'r ysbyty i gartrefi gofal ym Mhennod 3.
Cafodd gweithwyr gofal cymdeithasol anawsterau wrth weinyddu profion, yn enwedig y rhai sy'n gofalu am unigolion â dementia neu anableddau dysgu, a nododd yr effaith negyddol a gafodd hyn ar bobl ag anghenion gofal a chymorth.
| “ | Roedd yn rhaid i ni brofi ein preswylwyr dementia, a oedd yn anodd iawn gan nad oedd ganddyn nhw unrhyw ddealltwriaeth na phrofiad blaenorol o'r math hwn o brofi.”
- Gweithiwr cartref gofal, Gogledd Iwerddon |
| “ | Siaradais â theuluoedd oedd yn teimlo na ddylai aelodau eu teulu gael eu profi a dywedwyd wrthym fod yn rhaid i ni wneud hynny. Felly, fy ffordd i o osgoi hynny oedd, os es i fyny i brofi rhywun ac roedden nhw'n gwrthod yn llwyr, wnes i ddim gwneud hynny. Rydym yn trawmateiddio'r cleifion hyn sydd ag anabledd dysgu sy'n ein gweld ni, yn y masgiau hyn, yn rhoi hyn i fyny eu trwynau.”
- Nyrs gymunedol, Gogledd Iwerddon |
Wrth i gyfyngiadau lacio ac ymweliadau â chartrefi gofal ailddechrau, profion ar daeth ymwelwyr hefyd yn weithdrefn safonolPan ganiatawyd i anwyliaid ymweld â phobl yn bersonol mewn cartrefi gofal, roedd y niferoedd yn gyfyngedig ac roedd yn rhaid iddynt archebu apwyntiadau, cymryd prawf Covid-19, gwisgo PPE a chynnal pellter cymdeithasol. Roedd rhai yn teimlo bod y protocolau ymweld hyn yn heriol, yn cymryd llawer o amser ac yn anodd addasu iddynt.
| “ | Roedd yn rhaid i ni eistedd y tu allan i roi ffedogau a masgiau ymlaen; roedd yn rhaid i ni wneud swabiau ar y trwyn ac yna mynd i mewn wedi gwisgo masgiau a ffedogau i fynd i eistedd gyda fy nhad.”
- Anwylyd preswylydd cartref gofal, yr Alban |
Defnyddiodd pobl ag anghenion gofal a chymorth sy'n byw gartref, a'u gofalwyr di-dâl a oedd yn byw ar wahân, hefyd LFTs i wirio a allent ymweld â'i gilydd.Unwaith eto, rhoddodd hyn rywfaint o sicrwydd, gyda chyfranwyr yn rhannu'r effaith gadarnhaol a gafodd hyn ar eu hofnau ynghylch dal y feirws.
| “ | Cael y profion Covid, fel y gallem weld ein gilydd, gwirio a oedd gennym dwymyn neu rywbeth. Wyddoch chi, doedden ni ddim yn mynd allan yn aml.”
- Person ag anghenion gofal a chymorth, Lloegr |
Cadw pellter cymdeithasol
Roedd gweithwyr gofal cymdeithasol proffesiynol yn wynebu anawsterau sylweddol yn gysylltiedig â chadw pellter cymdeithasol. Clywsom fod llawer o weithwyr gofal yn methu â chynnal pellter corfforol wrth ddarparu gofal personol i bobl.
| “ | Doedden ni ddim yn gallu cadw pellter, oherwydd rydyn ni yno yn gorfod gwneud ein troeon [y preswylwyr] ac yn gorfod eu bwydo. Dydy rhai ohonyn nhw ddim yn gallu bwydo eu hunain. Roedden ni'n gorfod rhoi sipian o ddŵr iddyn nhw a sipian o ddiod a chwpanau o de a'u bathu a phethau fel 'na.”
- Gweithiwr cartref gofal, Lloegr |
| “ | Ni allwch gadw pellter cymdeithasol oddi wrth rywun rydych chi'n gweithio gydag ef, mae'n rhaid i ddau ohonoch ofalu am y preswylydd. Roedd yn amhosibl. Felly, fe wnaethon ni ddefnyddio'r PPE a gwneud yr hyn oedd angen i ni ei wneud, ond nid oedd yn bosibl i'r ddau [gweithiwr cartref gofal] fod pellter o ddau fetr [o'r preswylydd]. Os ydw i'n mynd i sefyll ar un ochr i'r gwely ac ar ochr arall y gwely mae fy nghydweithiwr, nid dyna'r pellter maen nhw'n chwilio amdano, ond dyna oedd ei angen i ofalu am y preswylydd.”
- Gweithiwr cartref gofal, Lloegr |
Roedd llawer yn ei chael hi'n anodd llywio sefyllfaoedd lle nad oedd cyswllt corfforol â'r rhai yr oeddent yn gofalu amdanynt, rhan allweddol o ofal arferol ar gyfer rhoi sicrwydd a meithrin perthnasoedd, yn bosibl mwyach, er gwaethaf y cais amdano.Roedd hyn yn arbennig o heriol i bobl ag anabledd dysgu neu ddementia nad oeddent yn deall pam roedd staff yn ymddwyn yn wahanol.
| “ | Byddai rhai o'n [pobl ag] anableddau dysgu [neu] ddementia yn hapus i'ch gweld chi ac yna bydden nhw eisiau cwtsh, neu [i] ddod i eistedd gyda fi, dal fy llaw. Doeddech chi ddim yn gallu gwneud hynny. Doeddech chi ddim yn cael gwneud hynny ac roedd hi'n anodd ceisio dweud wrthyn nhw, 'Na, alla i ddim eich cofleidio chi heddiw'.”
- Gweithiwr cartref gofal, yr Alban |
Rhai aelodau o'r teulu disgrifiodd deimlo rhyddhad pan oedd staff yn plygu neu'n torri'r rheolau er mwyn cefnogi pobl mewn ffordd empathig neu fwy dyngarol.
| “ | Doedd dim cyswllt corfforol i fod, [ond] torrodd menyw hyfryd [yn y cartref gofal] y rheolau, oherwydd pan oedd mam mewn gofid, dywedodd hi, 'Mae hi angen cwtsh arni'. Doedden ni ddim yn gallu gwneud hynny ac roedd hi'n dda gwybod bod rhywun yn torri'r rheolau i roi'r cyswllt hwnnw iddi.”
- Anwylyd preswylydd cartref gofal, yr Alban |
Gofalwyr di-dâl ac aelodau o'r teulu wedi'u canfod roedd cefnogi pobl awtistig a phobl ag anableddau dysgu i ddilyn cadw pellter cymdeithasol yn heriolEr enghraifft, trafododd gofalwyr di-dâl orfod eu goruchwylio drwy'r dydd a'r nos pan oedd aelod arall o'r teulu wedi'i ynysu yn eu hystafell.
| “ | Doedd [fy merch sydd ag anableddau dysgu] ddim yn gallu deall yr angen am fwgwd na'r defnydd o fwgwd…Roedd yn eithaf dwys, y ffaith bod yn rhaid iddi fod yng nghwmni'r holl amser fel nad oedd hi [yn dod i gysylltiad â'r aelod o'r teulu oedd yn ynysu â Covid].”
- Gofalwr di-dâl, Lloegr |
Roedd cadw pellter cymdeithasol hefyd yn berthnasol i ymweld â phobl mewn cartrefi gofal. Rheolwyd hyn mewn gwahanol ffyrdd wrth i'r pandemig ddatblygu o ddim ymweliadau o gwbl, i ymweliadau ffenestr allanol, i ymweliadau o bell y tu mewn i'r cartref gofal. Trafodir hyn yn fanylach ym Mhennod 2.
Glanhau, diheintio a chadw tŷ
Roedd mesurau rheoli heintiau eraill mewn cartrefi gofal yn cynnwys gweithdrefnau glanhau gwell a diheintio arwynebau sy'n cael eu cyffwrdd yn aml.
Chwaraeodd staff cadw tŷ rôl ganolog wrth gynnal y safonau hylendid uwch hyn, gan sicrhau bod lleoliadau gofal yn cael eu glanhau a'u diheintio'n drylwyr., weithiau sawl gwaith y dydd. Soniodd rhai preswylwyr cartrefi gofal sut y byddai staff gofal neu staff cadw tŷ yn diheintio eu hystafell unwaith yr wythnos. Roedd llawer yn teimlo bod y lefel hon o lanhau yn gysurus ac yn gwerthfawrogi'r ymdrechion a wnaeth staff y cartref gofal.
| “ | Arferai dyn mewn siwt oren ddod i lanhau fy ystafell gyfan. Roedd rhaid i mi eistedd y tu allan ar y gadair am 10 munud. Ac fe fyddai'n chwistrellu popeth ac yna, roedd rhaid i mi aros 10 munud iddo sychu ac yna gallwn fynd yn ôl. Ond bob dydd pan ddeuai'r glanhawyr, byddent yn lanhau dolenni'r drysau. Wyddoch chi, roeddent yn fanwl iawn yn yr hyn a wnaethant. Cafodd popeth ei ofalu amdano. Hynny yw, fe wnaethon nhw waith da iawn.”
- Person ag anghenion gofal a chymorth, Lloegr |
Cynyddodd protocolau, amserlenni ac archwiliadau glanhau llym lwyth gwaith gweithwyr cartrefi gofal a oedd eisoes yn brysurFodd bynnag, roedd cyfranwyr yn deall pwysigrwydd y mesurau hyn ar gyfer rheoli heintiau. Trafododd rhai gweithwyr cartrefi gofal gyflwyno rolau newydd, fel hyrwyddwyr rheoli heintiau, i orfodi mesurau rheoli heintiau ac i ddarparu diweddariadau.
| “ | Yn y diwedd, fe wnaeth [rheolwyr cartrefi gofal] weithredu trefn briodol lle'r oedd glanhau canllawiau, drysau, popeth, bob tair awr, ledled yr adeiladau a phethau. Roeddwn i'n un o'r prif rai oedd yn ei wneud. Roeddwn i'n sicrhau ein bod ni'n ei wneud ac roedd gennym ni wiriadau i wneud hynny i gyd. Felly, roedd yn llawer o waith yn gyson. Cyn gynted ag y byddech chi'n glanhau un ardal, roeddech chi'n glanhau eto.”
- Gwraig tŷ mewn cartref gofal, Lloegr |
Stori ClaireRoedd Claire yn brif wraig tŷ llawn amser mewn cartref nyrsio yn Lloegr yn ystod y pandemig. Roedd hi'n rheoli tîm o wraig tŷ ac wedi bod yn gweithio yn y cartref nyrsio ers dros bum mlynedd. Disgrifiodd sut y gweithredodd brotocolau glanhau a hylendid gwell i atal lledaeniad Covid-19 yn y cartref. |
|
| “ | Fe wnaethon ni lanhau’n drylwyr os oedd amheuaeth y gallai rhywun gael Covid. Roedd gennym ni faddon traed y tu allan lle roedden ni’n diheintio esgidiau cyn i ni ddod i mewn. Roedden ni’n glanhau’r rheiliau, y mannau cyffwrdd, y lifft yn gyson.” |
| Yn ogystal, rhoddwyd sylw i groeshalogi, gan sicrhau bod preswylwyr yn derbyn eu tywelion a'u dillad dynodedig eu hunain, a gafodd eu golchi'n unigol. | |
| “ | Roedd yn sicrhau, hyd yn oed [eu] tywelion, wyddoch chi, nad oedd unrhyw ddryswch ar dywelion, dim dryswch ar ddillad, felly roedd popeth oedd yn mynd at y preswylydd yn eiddo iddyn nhw ac mae wedi cael ei olchi'n unigol.” |
Trafododd gofalwyr di-dâl fesurau rheoli heintiau fel blaenoriaeth, yn enwedig ar ddechrau'r pandemig. Roedd protocolau glanhau a diheintio yn faich a oedd yn cymryd llawer o amser i rai.Roedd hyn yn arbennig o heriol yn gynnar yn y pandemig, pan fyfyriodd cyfranwyr nad oedd neb yn gwybod yn union sut y trosglwyddwyd y firws Covid-19, ac felly roedd amrywiaeth o wahanol fesurau rheoli heintiau yn gyffredin. Yn ymarferol, roedd ymdrechion i leihau'r risg o ddal Covid-19 yn aml yn cymryd cryn dipyn o amser ac egni o ddydd i ddydd i ofalwyr di-dâl. Soniodd pobl ag anghenion gofal a chymorth, gofalwyr di-dâl ac anwyliaid hefyd am gymryd mesurau rhagofalus ychwanegol, fel sychu eitemau yr oeddent wedi'u prynu o'r siopau gyda weips gwrthfacteria, tra bod eraill wedi dechrau defnyddio platiau papur a chyllyll a ffyrc.
Er bod rhai cyfranwyr yn gallu rheoli'r gweithgareddau hyn, roedd eraill yn ei chael hi'n anodd gwneud hynny, gan ei chael hi'n anodd ymdopi â'r pryder ychwanegol ynghylch sicrhau bod popeth sy'n dod i mewn i'r cartref wedi'i ddiheintio. Effeithiodd hyn ar ofalwyr di-dâl sy'n byw gyda'r person yr oeddent yn gofalu amdano a'r rhai sy'n byw ar wahân. Clywsom sut disgrifiodd rhai gofalwyr di-dâl brofiadau o feddyliau ymwthiol ac ymddygiadau cymhellol ynghylch pwysigrwydd glanhau.
| “ | Roeddwn i'n chwistrellu diheintydd ym mhobman. Ar un adeg, roeddwn i'n ei ychwanegu at boteli o [ddiheintydd]. Troais i'n wallgof diheintio llwyr. Cefais y pethau dosbarthu cadachau ym mhobman yn y tŷ. Troais i'n ffric obsesiynol.”
- Gofalwr di-dâl, yr Alban |
Roedd y pwysau o orfod bod yn ofalus yn gyson hefyd yn flinedig. Disgrifiodd rhai straen ychwanegol o fod angen tawelu meddyliau'r person yr oeddent yn gofalu amdano gartref, gan reoli eu pryder yn ogystal â'u pryder eu hunain.
| “ | Roeddwn i'n ei chael hi'n fwy heriol yn feddyliol. Roeddwn i mor flinedig o orfod ei dawelu [y person roedden nhw'n gofalu amdano]. Roedd e'n gyson yn bryderus, er enghraifft, os oedd yn rhaid i mi fynd i'r siop iddo, roeddwn i'n meddwl, 'Os yw rhywun sydd â Covid wedi cyffwrdd â hynny, rydych chi'n mynd i ddod â hynny'n ôl ataf i.'”
- Gofalwr di-dâl, Lloegr |
6 Prinder staff a sut y darparwyd gofal |
 |
Mae'r bennod hon yn disgrifio achosion prinder staff yn ystod y pandemig a sut yr effeithiodd y rhain ar ffyrdd o weithio a chyfathrebu ac arweiniodd at fwy o ddibyniaeth ar staff asiantaeth. Mae hefyd yn archwilio'r effaith a gafodd hyn ar y gweithlu gofal cymdeithasol i oedolion a phobl sy'n derbyn gofal a chymorth.
Achosion prinder staff
Esboniodd cyfranwyr yr achosion lluosog dros brinder staff yn ystod y pandemig. Newidiodd pwysigrwydd gwahanol resymau dros brinder staff wrth i amser fynd yn ei flaen. Roedd y rhesymau hyn yn cynnwys pryderon ynghylch trosglwyddo'r feirws, gwarchod yn gysylltiedig â chyflyrau iechyd staff, gofynion hunanynysu, straen oherwydd llwythi gwaith mwy, absenoldeb salwch yn gysylltiedig â Covid Hir ac anesmwythyd ynghylch pwysau i gael y brechlyn.
Yn ystod y cyfnod clo cyntaf, gadawodd staff y gweithlu gofal oherwydd eu bod nhw yn poeni am ddal Covid-19 a'r cymhlethdodau iechyd posibl o'r feirws iddyn nhw a'u teuluoeddRoedd staff a arhosodd yn poeni am yr hyn a fyddai'n digwydd i'w teuluoedd pe byddent yn mynd yn sâl iawn neu'n marw o Covid-19.
| “ | Gadawodd llawer o bobl [staff] oherwydd nad oedden nhw eisiau cael eu rhoi mewn perygl, a oedd wedyn yn golygu bod gennych chi fwy o rotas i'w gwasanaethu [a] mwy o gwsmeriaid i'w gweld a llai o staff i'w defnyddio.”
– Rheolwr cofrestredig, yr Alban |
| “ | Roeddwn i'n gweithio i gwmni gofal yn ystod Covid ac fe adawais oherwydd bod eu harferion yn anghyson ac yn anniogel. Roeddwn i'n byw gyda phobl agored i niwed ac yn codi pryderon yn barhaus wrth i ni fynd i gyfnod clo. Roeddwn i'n poeni am y diffyg PPE ac arferion hylendid wrth i ni fynd i mewn i gartrefi pobl i'w cefnogi.”
– Gweithiwr gofal, Lloegr |
| “ | Roeddwn i'n gydlynydd gofal ar gyfer gwasanaeth gofal cartref. Roedd yn frawychus gan ein bod ni i gyd yn meddwl ein bod ni'n mynd i farw. Dw i'n cofio gwirio fy yswiriant bywyd gan fod yn rhaid i mi sicrhau y gallai fy ngŵr a'm plant ymdopi ar ôl i mi farw gan fy mod i'n argyhoeddedig y byddwn i'n cael y clefyd trwy fy swydd. Wrth i'r llywodraeth gau'r wlad, roedd gennym ni 14 o staff yn mynd i ffwrdd o fewn y cartref gofal ac ar ochr y gofal cartref.”
– Gweithiwr gofal, Lloegr |
Roedd gan rai staff gyflyrau iechyd sy'n bodoli eisoes hefyd a oedd yn golygu eu bod mewn mwy o berygl o ddal y firws. Gadawodd llawer y gweithlu oherwydd bod yn rhaid iddynt amddiffyn eu hunain rhag y tywydd..
| “ | Roeddwn i yn y gwaith un diwrnod yn gweithio fy ffordd trwy'r pandemig a chefais alwad ffôn gan fy rheolwr [yn dweud] 'Mae'n rhaid i chi amddiffyn eich hun'. Rydw i'n eistedd yn y tŷ yn barod i fynd i'r gwaith ac nid wyf yn cael caniatâd.
– Gweithiwr gofal cartref, yr Alban |
| “ | Roedd yn anodd iawn gyda'r gwarchodaeth…roedd gennym ni 60% o'n staff yn gwarchodaeth ar y cychwyn cyntaf, felly roedd yn rhaid i ni ymdopi [gyda] lefelau staffio o 40%.”
– Rheolwr cofrestredig, Cymru |
Disgrifiodd gweithwyr gofal cymdeithasol proffesiynol hefyd gorfod ynysu pan wnaethon nhw ddal Covid-19 neu ddod i gysylltiad â rhywun â Covid-19, a oedd yn golygu na allent weithio.
| “ | Os byddai aelod o staff yn cael Covid, yna ni chaniatawyd iddynt ddod i'r gwaith. Roedd yn rhaid iddynt ynysu. Felly nid yn unig roedd yr holl ddefnyddwyr gwasanaeth yn mynd yn sâl, roedd yr holl staff yn mynd yn sâl hefyd…roedd y prinder staff yn anghredadwy.”
– Gweithiwr cartref gofal, Lloegr |
Straeon o SkegnessClywsom straeon tebyg hefyd mewn digwyddiad gwrando yn Skegness, lle trafododd cyfranwyr yr heriau o weithio goramser oherwydd prinder staff. |
|
| “ | Aeth yn anodd oherwydd bod pawb yn mynd i ffwrdd yn sâl – oherwydd y diffyg gorchudd roedden ni’n gweithio drwy’r oriau heb unrhyw seibiant.”
– Gweithiwr gofal, digwyddiad gwrando, Lloegr |
| “ | Roedden ni’n gweithio-cysgu-gweithio-cysgu. Doedd gennym ni ddim diwrnodau i ffwrdd i sicrhau bod pawb yn cael gofal oherwydd bod gennym ni bobl i ffwrdd yn sâl gyda Covid.”
– Gweithiwr gofal, digwyddiad gwrando, Lloegr |
| Effeithiodd y prinder staff ar y staff a oedd yn gorfod parhau i weithio. | |
| “ | Parhaodd y staff i ddod i'r gwaith er eu bod nhw'n ofnus.”
– Gweithiwr gofal, digwyddiad gwrando, Lloegr |
| “ | Roedd rhaid iddyn nhw ddod yn ôl i'r gwaith gan nad oes tâl salwch mewn gofal. Yn sicr nid oedd Covid Hir wedi'i gynnwys mewn gofal. Yng nghanol [y pandemig] dechreuodd y llywodraeth daflu arian atom i helpu, ond fel arall dim ond tâl statudol a gawson ni. Doedd neb eisiau dod i weithio.”
– Gweithiwr gofal, gwrando eawyrell, Lloegr |
Roedd rhai cyfranwyr hefyd yn meddwl tybed a oedd rhai o'u cydweithwyr ddim yn dod i'r gwaith am resymau heblaw bod yn sâl gyda Covid-19.
| “ | Roedd yna feysydd yno [yn y canllawiau Covid-19] y gallai staff fanteisio arnynt [i] osgoi gorfod dod i'r gwaith.”
– Rheolwr cofrestredig, Lloegr |
| “ | Fel nyrs, roedd gen i deimlad bob amser o, 'Dyna fy swydd i', a dim ond oherwydd bod hyn wedi digwydd, roedd gennym ni gynifer o nyrsys heb ddod i'r gwaith ac rydw i fel, 'Ond dyna dy swydd di, allwch chi ddim penderfynu dim ond oherwydd bod Covid yma na allwch chi ddod i'r gwaith'.”
– Nyrs yn gweithio mewn cartref gofal, Cymru |
Achosodd prinder staff straen difrifol i weithwyr gofal cymdeithasol proffesiynol a barhaodd i weithio, a arweiniodd yn ei dro at fwy o absenoldebau staff a phrinder pellach.
| “ | Dw i'n meddwl bod un shifft benodol yno oedd rhywbeth fel 20% o'r gweithlu yn gweithio, oherwydd naill ai roedd ganddyn nhw Covid, neu roedden nhw i ffwrdd oherwydd y straen.”
– Gweithiwr gofal cartref, Lloegr |
Yn ddiweddarach yn y pandemig pan gyflwynwyd y brechlyn, roedd rhai gweithwyr gofal cartref a chartrefi gofal yn poeni am sgîl-effeithiau posibl y brechlyn ac a oedd yn ddiogel o ystyried pa mor gyflym y cafodd ei ddatblyguRoedd y pryderon hyn yn waeth i'r rhai â chyflyrau iechyd sy'n bodoli eisoes.
| “ | Rwy'n gwybod bod rhai pobl yn ansicr ynglŷn â'r brechiad a pha mor gyflym y daeth allan. Hefyd, roedd y rhai a oedd â chyflyrau iechyd sylfaenol yn amharod.
– Gweithiwr gofal iechyd, Lloegr |
Achosodd y gofyniad i weithwyr gofal gael y brechlyn Covid-19 yn Lloegr, a'r pwysau i wneud hynny gan rai darparwyr gofal yn y gwledydd datganoledig, i rai gweithwyr gofal adael y gweithlu., gwaethygu prinder staff ymhellachDisgrifiodd rhai cyfranwyr sut y gwnaethon nhw adael oherwydd nad oedd gofynion brechu yn cyd-fynd â'u gwerthoedd na'u credoau neu deimlo ei fod yn peryglu eu rhyddid personol. Rhannodd rhai staff a arhosodd yn y gweithlu gofal cymdeithasol y pryder hwn. Roedd staff yn gadael oherwydd teimlo dan bwysau i gael y brechlyn yn tanseilio parhad gofal i bobl ag anghenion gofal a chymorth, yn enwedig wrth i staff adael yn sydyn.
| “ | Roedd rhai [gweithwyr gofal] yn gwrthod cael y brechlyn oherwydd yr holl sgîl-effeithiau yr oeddent yn cael eu trafod ac…yna rhoddwyd yr wltimatwm iddynt, 'Os nad oes gennych y brechlyn, ni allwch weithio'.”
– Gweithiwr gofal cartref, Lloegr |
| “ | Ymddiswyddais o fy swydd gan nad oeddwn yn cytuno â brechiadau gorfodol i'm staff, er i mi gael y brechlyn fy hun. Rwy'n ei chael hi'n anamddiffynadwy yn foesol orfodi pobl i gael unrhyw ymyrraeth feddygol.”
– Rheolwr cofrestredig cartref gofal, Lloegr |
| “ | Pan ddywedodd y llywodraeth fod yn rhaid i bob gweithiwr gofal gael ei frechu, gadawodd hanner ein gweithwyr ymroddedig a oedd wedi bod yma ers blynyddoedd.”
– Rheolwr cofrestredig cartref gofal, Lloegr |
| “ | Roeddwn i'n gweithio mewn cartref gofal, dywedwyd wrthym fod yn rhaid i ni gael y brechlynnau neu golli ein swydd.”
– Gweithiwr cartref gofal, yr Alban |
Stori AmaraMae Amara yn fenyw Brydeinig Ddu-Caribïaidd sy'n byw yn ne-orllewin Lloegr. Bu'n gweithio fel cynorthwyydd gofal iechyd mewn cartref gofal nyrsio am bum mlynedd cyn y pandemig. Roedd gan Amara record presenoldeb a pherfformiad rhagorol yn ystod ei chyfnod yno. Fodd bynnag, pan oedd y cartref nyrsio yn gofyn am frechiadau Covid-19 i'r holl staff, cafodd Amara ei diswyddo am wrthod cael y brechlyn oherwydd amheuon personol. |
|
| “ | Fy mhrofiad negyddol mwyaf yw cael fy niswyddo o fy swydd fel cynorthwyydd gofal iechyd mewn cartref nyrsio am wrthod cymryd y brechlyn Covid…Doeddwn i ddim eisiau’r brechlyn oherwydd fy mod i’n credu mewn ymreolaeth y corff ac yn teimlo fy mod i wedi cael fy mwlio i gael rhywbeth yn fy nghorff nad oeddwn i eisiau.” |
| Disgrifiodd Amara y pwysau ar staff cartrefi gofal i gael y brechlyn, er gwaethaf amharodrwydd rhai. Nododd fod y pwysau hwn i gael y brechlyn ac osgoi colli eu swydd yn effeithio'n arbennig ar weithwyr o wledydd eraill a anfonodd arian at eu teuluoedd neu a oedd ar fisâu gwaith ac yn poeni am eu statws preswylio, a oedd yn dibynnu ar eu swydd gofal.
Achosodd colli staff broblemau i'r cartref nyrsio ac, er gwaethaf y ffaith bod yr holl staff sy'n weddill wedi cael eu brechu, cawsant achos wedi hynny. |
|
| “ | Roedd fy rheolwr yn flin gan ei bod wedi colli tua 10 aelod o staff ac eisiau i mi aros gan fy mod yn ofalwr da.” |
| “ | Yr eironi yw, yn fuan ar ôl i mi a staff eraill gael ein diswyddo, cafodd y cartref gofal achos enfawr o Covid a bu’n rhaid iddo gau i ymwelwyr. Felly, mae’n rhaid bod rhai o’r staff a gafodd eu brechu wedi dod ag ef i’r cartref gofal gan fod yr HOLL staff wedi’u brechu erbyn hynny. Felly, beth oedd pwynt y gorchymyn os gallai staff ddal Covid o hyd a’i ddod ag ef i’r cartref? Doedd dim synnwyr o gwbl.” |
| Gwnaeth hyn i Amara gwestiynu pwrpas y gorchymyn brechu, yn enwedig gan fod y gofyniad wedi'i wrthdroi'n ddiweddarach. Mae hi'n dal yn flin ynghylch yr effaith ar y sector gofal cymdeithasol o golli sgiliau a phrofiad. | |
| “ | Am wastraff o gael gwared ar filoedd o staff gofal profiadol heb reswm, mewn sector a oedd eisoes yn brin o staff yn gronig. Ni fydd y rhan fwyaf o'r staff hynny byth yn mynd yn ôl i waith gofal, rhag ofn y bydd yn digwydd eto yn y dyfodol. Felly, ni fydd fy mhrofiad o 5 mlynedd o ddementia a NVQ lefel 2 byth yn cael eu defnyddio eto.” |
| Mae colli ei swydd gofal wedi cael canlyniadau hirdymor i Amara. Daeth o hyd i swydd newydd mewn ffatri, ond nid oedd hyn yn addas iddi a chollodd y swydd. Mae hi bellach yn ddi-waith, mewn dyled ac ar fudd-daliadau, ac mae ei phrofiadau wedi effeithio ar ei hiechyd meddwl. | |
| “ | [Rwy'n] ôl ar fudd-daliadau ac yn awr ar wrthiselyddion ar ôl cael chwalfa.” |
Roedd prinder staff yn cael effeithiau uniongyrchol ar ansawdd gofal wedi'i ddarparu a lleihau'r amser sydd ar gael i godi pobl, eu golchi a darparu agweddau eraill ar ofal personol. Sylwodd anwyliaid yn ogystal â'r gweithlu ar hyn.
| “ | Oedd, roedd ganddyn nhw brinder staff. Roedd hyn ar ôl Brexit, roedden nhw wedi colli rhai o'u staff o ddwyrain Ewrop, a oedd yn ardderchog. Yn amlwg, daeth a aeth pobl beth bynnag. Rwy'n credu bod rhai wedi'u heffeithio gan y pandemig oherwydd eu bod nhw'n gweithio yn yr amgylchedd dan bwysau mawr hwnnw ac roedden ni'n ymwybodol o bobl oedd wedi gadael, mae'n debyg oherwydd na allent ymdopi â mwy. Roedd problemau recriwtio. Hynny yw, tua'r diwedd pan es i mewn, alla i ddim dod o hyd i'r dyddiad nawr, ond roedd mam mewn cyflwr gwael iawn. Roedd hi'n flêr, doedd hi ddim wedi cael ei dannedd, doedd hi ddim wedi cael ei sbectol, roedd yr ystafell yn fudr, roedd hi'n fudr ac fe wnes i gŵyn ffurfiol bryd hynny. Darganfyddais nad oedd y glanhawr wedi bod i mewn oherwydd na allent recriwtio un felly roedd bylchau a phroblemau.”
– Anwylyd preswylydd cartref gofal, Lloegr |
| “ | Roedd rhaid i mi gadw pobl yn y gwely oherwydd angenrheidrwydd, nid dewis. Roedd rhaid i mi roi llyfiad cyflym iddyn nhw ac addewid. Doedd dim cawodydd yn cael eu darparu oherwydd nad oedd gennym lefelau staffio, roedd yn fwy diogel cadw rhai pobl yn y gwely ar y pryd.”
– Nyrs yn gweithio mewn cartref gofal, Gogledd Iwerddon |
Mwy o ddefnydd o staff asiantaeth
Prinder staff dibyniaeth gynyddol ar staff asiantaethauRoedd hyn yn aml yn hanfodol i gynnal gofal diogel a phriodol yn ystod y pandemig, ond disgrifiodd cyfranwyr ganlyniadau negyddol hefyd. Roedd y rhain yn cynnwys risg uwch o ledaenu Covid-19 ac ansawdd gofal is oherwydd nad oedd staff yr asiantaeth yn gyfarwydd â'r bobl yr oeddent yn gofalu amdanynt.
| “ | Mae staff yr asiantaeth yn mynd i gartref gofal ac nid oes ganddyn nhw unrhyw syniad pwy yw'r preswylydd. Nid oes ganddyn nhw amser i ddarllen pob cynllun gofal. Nid ydyn nhw'n adnabod y preswylwyr. Gofal sylfaenol ydyw [y gallant ei ddarparu o ganlyniad]. Nid oes gofal sy'n canolbwyntio ar y person yno.”
– Gweithiwr cartref gofal, Lloegr |
| “ | Mae bod mewn cartref gofal preswyl bach ar gyfer anableddau dysgu yn swydd sy'n dibynnu ar gyfarwyddrwydd. Roedd angen gofal parhaus ar ein preswylwyr gan bobl a oedd yn gwybod eu nodweddion, [gan gynnwys] sut roeddent yn bwydo, yn yfed ac [yn derbyn] gofal personol.”
– Rheolwr cofrestredig cartref gofal, Lloegr |
| “ | Byddwn i'n mynd i mewn ac yn gorfod mynd i ofalu am gleifion â dementia a'u cynorthwyo, gallwn i gael fy rhoi ar wardiau gwahanol, doeddwn i ddim yn cael fy rhoi ar yr un ward, a oedd yn chwerthinllyd hefyd, oherwydd bydden nhw wedi fy rhoi ar 1 ward ac yna fy rhoi ar un arall ac roedd 4 coridor gwahanol. Felly, gallwn i fod yn gweithio ar bob coridor gwahanol drwy'r wythnos, a oedd yn chwerthinllyd. Gallwn i fod yn gofalu am gleifion dementia, neu os oeddwn i ar goridor penodol, dim ond 1 gofalwr oedd gan rai coridorau, roedd gan rai coridorau 2 ofalwr. Y coridorau oedd yn goridorau llai a oedd â hyd at 12 o bobl arnyn nhw, dim ond 1 [dyraniad staff] oedd hynny, felly roedd yn rhaid i mi ofalu am 12 o bobl ar fy mhen fy hun.”
– Gweithiwr cartref gofal asiantaeth, Lloegr |
Disgrifiodd rhai cyfranwyr staff asiantaeth â lefelau is o hyfforddiant neu eu bod yn gwbl newydd i waith gofal. Roedd hyn yn golygu bod yn rhaid i weithwyr gofal presennol dreulio amser yn hyfforddi staff asiantaeth oherwydd nad oeddent yn gwybod sut i ddiwallu anghenion penodol y bobl yr oeddent yn eu cefnogi. Roedd hyn yn aml yn rhwystredig, gan adael gweithwyr cartrefi gofal gyda hyd yn oed llai o amser i ddarparu'r gofal angenrheidiol.
Stori JanetRoedd Janet yn gweithio mewn cartref gofal yn darparu gofal un i un i bobl ag anafiadau i'r ymennydd. Pan ddechreuodd y pandemig, gadawodd llawer o staff y cartref gofal gan eu bod yn ofnus ac anfonwyd staff nyrsio'r cartref gofal i gefnogi'r ysbyty lleol. Arweiniodd hyn at brinder staff sylweddol. Canfu Janet fod recriwtio staff yn anodd drwy gydol y pandemig ac mae'r heriau hyn yn dal i barhau. Roedd ei chartref gofal yn dibynnu'n fawr ar staff asiantaeth, ond ychwanegodd hyn at lwyth gwaith mawr Janet eisoes gan fod angen mwy o gefnogaeth a hyfforddiant arnynt. |
|
| “ | Roedd hi’n anodd iawn cael staff newydd, felly fe wnaethon ni orffen gyda llawer o asiantaethau…roedd hynny’n anodd oherwydd nad oeddech chi’n gwneud eich gwaith yn unig, rydych chi’n ceisio dweud wrth berson asiantaeth sut i wneud eu gwaith nhw hefyd. Roedd hynny’n dipyn o straen.” |
| Bu’n rhaid i Janet hyfforddi staff asiantaeth ar weithdrefnau cartrefi gofal, protocolau Covid-19 ac ar anghenion penodol preswylwyr unigol. Bu’n rhaid iddi hefyd eu monitro i sicrhau eu bod yn dilyn y canllawiau a’r protocolau hyn. Roedd hyn yn golygu jyglo ei dyletswyddau ei hun wrth oruchwylio a chefnogi staff asiantaeth, gan ychwanegu mwy o straen. Roedd llawer o achosion lle nad oedd staff asiantaeth yn ymddangos ar gyfer eu sifftiau, a olygai fod disgwyl i staff parhaol weithio sifftiau dwbl i sicrhau bod gofal yn cael ei ddarparu. | |
| “ | Nid oedd rhai asiantaethau bob amser yn cyrraedd pan oeddent i fod i gyrraedd. Neu fe ddaeth nyrs asiantaeth i fyny ac nid oedd ganddi syniad sut i wneud pethau.” |
| Er bod Janet a'i thîm wedi parhau i ddarparu gofal o ansawdd da i drigolion drwy gydol y pandemig, daeth y llwyth gwaith llethol yn annioddefol ar adegau. Mae llawer o gydweithwyr Janet a oedd yn gweithio ar ddechrau'r pandemig wedi gadael ers hynny oherwydd llosgi allan a'r heriau a wynebwyd yn ystod y pandemig. | |
Apwyntiadau rhithwir ac o bell
Rhannodd cyfranwyr eraill sut roedd cydweithwyr yn teimlo cymaint o straen a llosg allan fel na allent barhau i weithio a dewis gadael y gweithlu. Roedd hyn yn golygu bod staff parhaol yn aml yn gweithio gyda chydweithwyr newydd, ac roedd hyn yn niweidiol i forâl y tîm.
| “ | Roedd y trosiant staff yn erchyll, roedd gennym ni ofalwyr newydd yn dod i mewn bob dydd, [a oedd] yn anodd i reoli heintiau ac i staff, roedd cwrdd â phobl newydd bob dydd yn golygu nad oedd gennym ni wir undod â'n gilydd. Roedd yn teimlo fel pe baem ni'n dafladwy.”
– Rheolwr cofrestredig, Lloegr |
Newid patrymau gwaith
Newidiodd llawer o weithwyr gofal cymdeithasol proffesiynol eu horiau gwaith a'u patrymau sifftiau yn ystod y pandemig i sicrhau y gallent gefnogi pobl ag anghenion gofal a chymorth. Dywedodd cyfranwyr eu bod yn gweithio oriau hir gyda seibiannau bach iawn a dywedodd wrthym am y doll a gymerodd hyn arnom nhw a'u teuluoedd.
| “ | Roeddwn i'n gweithio oriau hir a blinedig iawn oherwydd diffyg staffio, lle roedd yn rhaid i staff adael oherwydd eu bod nhw'n agored i niwed [neu oherwydd bod ganddyn nhw] broblemau gofal plant [roeddwn i'n] gweithio hyd at chwe diwrnod a noson yr wythnos. Gan weithio mor galed nes bod anghenion fy nheulu yn dod yn ail.”
– Gweithiwr cartref gofal, Lloegr |
Bu’n rhaid i weithwyr gofal, yn enwedig y rhai mewn cartrefi gofal, newid eu patrymau gwaith fel y gallent gadw pellter cymdeithasol yn y gwaith. Lleihaodd hyn faint o amser y gallai staff ei dreulio gyda'i gilydd, gan erydu morâl y tîm ymhellach a gan adael gweithwyr gofal yn teimlo'n unig ac ynysig, hyd yn oed wrth weithio gydag eraill.
| “ | Roedd gennym ni swyddfa staff ond oherwydd y lle oedd ar gael i ni – gan mai cartref gofal yw hwn, nid yw mor eang â’r ysbytai cyffredinol – roedd cyfyngiad ar faint o staff fyddai’n bresennol ar unrhyw adeg er mwyn cyfyngu ar ledaeniad y feirws Covid.”
– Gweithiwr cartref gofal, Lloegr |
| “ | Roedd hi’n anodd i’r staff hefyd, peidio â chael eu seibiannau gyda’i gilydd. Ar gyfer cartref mor fach, rydym yn tueddu i eistedd i lawr am 10 o’r gloch a chael ein brecwast gyda’n gilydd. Ond roedd yn rhaid i ni ei wahanu fel bod rhai staff ar y bwrdd hwnnw [a] rhai staff ar fwrdd [arall]. Roeddent yn ei chael hi’n anodd oherwydd nad oeddent yn gallu siarad â’i gilydd.”
– Rheolwr cofrestredig cartref gofal, Lloegr |
Pan oedd staff yn profi'n bositif am Covid-19 neu'n methu â gweithio oherwydd salwch neu losgi allan, roedd yn rhaid diwygio rotas staff. Yn aml, roedd hyn yn golygu bod yn rhaid i'r rhai oedd yn gweithio wneud sifftiau hirach neu ymgymryd â llwythi gwaith mwy i lenwi dros gydweithwyr. Teimlai rhai cyfranwyr fod hyn yn arwain at ofal anniogel i breswylwyr.
| “ | Roedd staff yn aml yn sâl gan eu bod yn aml yn dal Covid…nid oedd y gofal a roesom yn teimlo'n ddiogel ac nid oeddem yn teimlo'n ddiogel.”
- Gweithiwr cartref gofal, Lloegr |
| “ | Nid oedd yn gwestiwn o, 'Wel, dydw i ddim yn gwneud hynny [shifft hirach]'. Roedd yn, 'Does gennym ni ddim staff, dyna beth rydych chi'n ei wneud'. Does gennych chi ddim dewis, mae angen gofalu am bobl, onid oes ganddyn nhw?”
- Gweithiwr cartref gofal, Lloegr |
| “ | Roedd ansawdd y gofal yn cael ei frysio, oherwydd bod gennych chi lai o staff. Felly, roedd yn rhaid i chi roi mwy o waith ar staff. Byddai'n rhaid i chi ofyn i staff gasglu pethau ychwanegol ar eu diwrnodau i ffwrdd. Doedd gennych chi ddim diwrnodau i ffwrdd oherwydd nad oeddech chi'n cael diwrnodau i ffwrdd, oherwydd roedd gennych chi ofal i'w gyflawni.”
- Gweithiwr cartref gofal, Lloegr |
Nid oedd rhai gweithwyr gofal yn gallu parhau i weithio pan oedd gofyn iddynt amddiffyn eu hunain neu ynysu. Roedd hyn yn anodd iddynt yn emosiynol os oeddent am barhau i ddarparu gofal ac yn gwybod bod eu cydweithwyr dan bwysau. Profodd eraill effeithiau ariannol, yn enwedig staff ar gontractau dim oriau, a gollodd incwm pan nad oeddent yn gweithio. Hyd yn oed pan allent weithio, roedd y rhai ar gontractau dim oriau yn poeni am y golled incwm bosibl pe byddent yn dal Covid-19.
| “ | Roeddwn i'n gweithio mewn cartref gofal ym mis Mawrth 2020. Yn 63 oed, roeddwn i'n cael fy ystyried yn agored i niwed ond allwn i ddim cael fy rhoi ar ffyrlo ac allwn i ddim fforddio aros oddi ar y gwaith a gwarchod fy hun… Cefais Covid ac nid oeddwn i'n gallu gweithio o gwbl am gyfnod ac yn y pen draw roeddwn i'n gallu gwneud 1 shifft yr wythnos ond allwn i ddim gwneud dim byd o gwbl ar ôl y shifft. Cymerodd fwy na blwyddyn i mi fynd yn ôl i rywbeth tebyg i ffitrwydd arferol. Roeddwn i ar gontract dim oriau, felly doedd gen i ddim tâl salwch a chollais lawer o incwm.”
- Gweithiwr cartref gofal, Lloegr |
| “ | Gweithiais fel gofalwr cartref drwy gydol Covid, gan weithio hyd at 70 awr a mwy yr wythnos, daliais Covid bedair gwaith, a phob tro roeddwn i i ffwrdd o'r gwaith am 10 diwrnod heb dâl gan ein bod ni ar gontractau dim oriau.”
- Gweithiwr gofal cartref, Lloegr |
| “ | Cefais lythyr gan fy meddyg teulu yn dweud fy mod mewn perygl uchel pe bawn i'n dal Covid ac yn cael fy rhoi ar ffyrlo am 3 mis. Yna siaradais â fy meddyg. Esboniais fy mod i'n ddiflas iawn gartref, bod gan fy ngweithle fesurau ar waith, ac fe wnaethon nhw asesiad risg fel bod modd i mi fynd yn ôl yn gynnar.”
– Gweithiwr gofal, Lloegr |
Disgrifiodd rhai cyfranwyr patrymau gwaith yn newid ar fyr rybudd neu heb unrhyw rybudd o gwbl pan nad oedd cydweithwyr yn mynychu'r gwaith yn annisgwyl. Yn aml, roedd hyn yn golygu bod yn rhaid i gyfranwyr barhau i weithio ar ddiwedd eu shifft nes bod rhywun arall yn gallu gwneud y gwaith. Roedd hyn yn dod â phwysau a straen ychwanegol a theimlad o gael eu siomi gan gydweithwyr, gan roi straen ar berthnasoedd gwaith a lleihau morâl.
Newidiadau yn y ffordd y darparwyd gofal cartref
Roedd prinder staff yn arbennig o heriol mewn gofal cartref (darparu cefnogaeth i unigolion yn eu cartrefi). Dywedodd cyfranwyr wrthym sut roedd prinder staff yn golygu na allai staff ymweld â chartrefi pobl ag anghenion gofal a chymorth cyhyd neu mor aml ag y byddent wedi dymuno. Cyn y pandemig, byddai'r math hwn o ofal fel arfer yn cynnwys elfen o gymorth cymdeithasol, ond symudodd y ffocws i gwmpasu gofal personol hanfodol yn unig.
| “ | O ran fy ngofal i, fe syrthiodd i fod yn elfen gyfyngedig iawn – fe wnaethon nhw dorri allan yr hyn a alwon nhw’n bopeth nad oedd yn hanfodol. Felly, dim ond dod i mewn a gwneud yr isafswm llwyr, o ran gofal personol a hylendid a phethau fel hynny. Fydden nhw ddim yn mynd â chi allan na mynd i siopa, na dim byd fel hynny. Ac fe wnaethon nhw geisio byrhau galwadau a phethau i leihau’r amlygiad.”
– Person ag anghenion gofal a chymorth, Lloegr |
| “ | Doedden nhw ddim yn gallu aros yn hir gyda chi, felly bydden nhw'n dod i mewn am gyfnod byr iawn. Doeddwn i ddim yn eu beio nhw oherwydd bod ganddyn nhw gymaint o bobl roedd yn rhaid iddyn nhw ofalu amdanyn nhw.”
– Person ag anghenion gofal a chymorth, Lloegr |
| “ | “Fe wnaethon ni leihau ein gwasanaeth hefyd. Er enghraifft, pedwar ymweliad y dydd i berson. Felly, gyda chaniatâd y bobl rydyn ni'n gofalu amdanyn nhw, fe wnaethon ni hi'n ddau ymweliad, yr ymweliadau angenrheidiol ar gyfer y gofal personol.”
– Gweithiwr gofal cartref, Gogledd Iwerddon |
Teimlai staff gofal cartref hefyd yn fwy cyfrifol am bobl ag anghenion gofal a chymorth a oedd yn byw ar eu pen eu hunain yn ystod y pandemigHeb gysylltiad â theulu a ffrindiau yn ystod y cyfnod clo, roedd pobl a oedd yn byw ar eu pennau eu hunain yn aml yn dod yn fwy ynysig. Fodd bynnag, roedd gan staff gofal cartref lai o amser i'w dreulio gyda phobl ac roedd hyn yn golygu na allent gynnig llawer o ryngweithio cymdeithasol. Teimlai llawer o weithwyr eu bod yn siomi pobl oherwydd bod yn rhaid iddynt adael mor gyflym. Roedd hyn yn golygu eu bod yn teimlo'n rhwystredig ac yn euog am beidio â darparu'r ansawdd gofal yr oeddent ei eisiau.
| “ | Dim oedi, dim sgwrsio gormod ar ôl i'r gofal hanfodol gael ei ddarparu; dim ond symud ymlaen i'r un nesaf oedd hi. Ie, roedd yn eithaf cyfyngedig, os ydw i'n onest, roedd yn eithaf creulon.”
– Gweithiwr gofal cartref, Cymru |
| “ | Dwi ddim yn meddwl ei fod yn deg ar y cleient oherwydd eu bod nhw eisoes yn oedrannus. Maen nhw eisoes yn unig…mae gennym ni 20 o gleientiaid ac mae'n rhaid i ni ddweud 'Dyma'ch cinio, syr, oes angen unrhyw beth arall arnoch chi? Dyma'ch paned o de. Ydych chi eisiau gwylio'r teledu? A ddylem ni roi'r teledu [ymlaen]? Iawn, rydyn ni'n mynd i olchi'ch cwpanau, hwyl fawr'. Rydych chi'n teimlo'n euog.”
– Gweithiwr gofal cartref, Lloegr |
Dywedodd pobl ag anghenion gofal a chymorth fod prinder staff yn golygu roedd darparwyr gofal yn llai hyblyg ynghylch amseriad a darpariaeth eu gofal. Roedd hyn yn aflonyddgar ar gyfer pobl ag anghenion gofal a chymorth a roedden nhw'n teimlo bod derbyn cefnogaeth leiafswm yn llawn straen ac yn bryderus.
| “ | Dim ond un gofalwr oedd gen i yn ystod y pandemig…oherwydd bod gan gwpl o fy ngofalwyr rheolaidd gyflyrau iechyd eu hunain…felly doedden nhw ddim yn cael gweithio. Felly, roedd [fy] nghefnogaeth gofal i lawr i'r lleiafswm llwyr.”
– Person ag anghenion gofal a chymorth, Lloegr |
Roedd adegau hefyd pan fyddai gweithwyr gofal cartref yn cyrraedd yn hwyr neu ddim yn dod o gwbl. Roedd hyn yn golygu bod yn rhaid i bobl ag anghenion gofal a chymorth wneud newidiadau sylweddol i'r ffordd yr oeddent yn byw, ac effeithiodd hyn ar agweddau pwysig ar eu bywydau, fel sut yr oeddent yn cysgu.
| “ | Roedd disgwyl i'r gofalwyr ddod am 7 o'r gloch y bore, ond weithiau doedden nhw ddim yn dod tan hanner deg, 11 y bore. Felly, os oedd gen i apwyntiad gwaith, fyddwn i ddim yn mynd i'r gwely'r noson cynt. Byddwn i'n cysgu yn fy nghadair am ddyddiau a dyddiau ar ôl dydd, oherwydd roeddwn i'n rhy ofnus i fynd i'r gwely rhag ofn na fyddai'r gofalwyr yn fy nghodi i fyny.”
– Person ag anghenion gofal a chymorth, Cymru |
Rhoddodd rhai staff gofal cartref enghreifftiau o anwyliaid nad ydynt eisiau cynnig gofal i aelod o'r teulu sydd ag anghenion cymorth oherwydd eu bod nhw eisiau amddiffyn eu hunain a'r person roedden nhw'n gofalu amdano rhag Covid-19. Roedd staff gofal yn bryderus am y baich cynyddol y mae hyn yn ei roi ar ofalwyr di-dâl a'r effeithiau ar lesiant pobl ag anghenion gofal a chymorth. Er enghraifft, roedd gan staff bryderon am unigolion oedd angen eu codi ond nad oedd eu teuluoedd wedi derbyn hyfforddiant ar sut i wneud hyn yn ddiogel. Mewn rhai achosion, arweiniodd gwrthodiadau munud olaf gan deuluoedd at weithwyr gofal cartref yn cael eu gwrthod wrth y drws.
| “ | Fyddai rhai teuluoedd ddim eisiau ni yno hyd yn oed: bydden nhw angen y gofal ond yna bydden nhw'n dweud, 'Na, wel, dydych chi ddim yn dod i mewn heddiw' oherwydd bod pobl yn ofni [trosglwyddo Covid-19].”
- Gweithiwr gofal cartref, Lloegr |
Cyfathrebu
Newidiodd y pandemig gyfathrebu o fewn y gweithlu gofal cymdeithasol i oedolion a chreu pwysau newydd i gefnogi cyfathrebu rhwng teuluoedd, ffrindiau a phobl ag anghenion gofal a chymorth.
Roedd staff yn gyfrifol am gyfathrebu â theulu, ffrindiau a gofalwyr di-dâl a'u diweddaru, yn enwedig yn ystod y cyfnod clo, fel y crybwyllwyd ym Mhennod 2. Roedd gweithwyr gofal cymdeithasol proffesiynol yn hanfodol ar gyfer trefnu galwadau ffôn a fideo.
| “ | Roedd staff yn cyfathrebu â theuluoedd drwy alwadau ffôn neu alwadau fideo.…maen nhw wedi ffonio llawer mewn gwirionedd, dw i'n teimlo, yn ystod y cyfnod hwnnw. Oherwydd eich bod chi'n dod o hyd i lawer, y teuluoedd oedd y rhai oedd bob amser yn eithaf panic i wneud yn siŵr bod perthnasau'n iawn, gan obeithio nad ydyn nhw wedi dal unrhyw beth, neu'n gobeithio nad ydyn nhw wedi profi'n bositif am Covid. Felly, roedd nifer fawr o alwadau ffôn yn gyson.”
– Gweithiwr cartref gofal, Cymru |
Defnyddiodd staff y ffôn neu'r e-bost i roi'r wybodaeth ddiweddaraf yn rheolaidd am iechyd a lles y bobl yr oeddent yn gofalu amdanynt. Clywsom hefyd enghreifftiau o gartrefi gofal yn sefydlu grwpiau WhatsApp ar gyfer ffrindiau a theulu a rhai yn anfon cylchlythyrau wythnosol.
| “ | [Fe wnaethon ni roi’r wybodaeth ddiweddaraf i deuluoedd y preswylwyr] yn bennaf dros y ffôn. Yna fe wnaethon ni sefydlu grŵp WhatsApp lle gallwn ni nodi unrhyw anghenion bach y gallwn ni anfon neges at deuluoedd yn dweud, wyddoch chi, 'Dyma lun o fam yn gwneud gweithgaredd', neu 'Mae angen gel cawod ar fam, os gallech chi eu galw i mewn.'”
– Rheolwr Cofrestredig cartref gofal, Lloegr |
Roedd gweithwyr gofal cymdeithasol proffesiynol yn wynebu penbleth barhaus llawn straen wrth geisio cydbwyso gwerth clir cefnogi cyfathrebu ag anwyliaid â darparu gofal arferol yng nghyd-destun prinder staffRoedd y galwadau ffôn rheolaidd, diweddaru grwpiau WhatsApp a threfnu cyfarfodydd ar-lein yn golygu gwaith ychwanegol a oedd yn ychwanegu at y pwysau ar y gweithlu.
| “ | Yr unig newid rôl, byddwn i'n ei ddweud, oedd ceisio hyrwyddo lles y preswylwyr a thawelu meddyliau teuluoedd yn gyson. Wyddoch chi, byddai'r ffôn yn canu'n amlach, dim ond gan deuluoedd, ffrindiau, eisiau siarad â pherthnasau, preswylwyr os gallent. Neu eisiau'r wybodaeth ddiweddaraf am y canllawiau a'r gweithdrefnau ymweld. Ac felly, rwy'n credu eich bod chi'n sicr yn ateb y ffôn llawer mwy ac yn delio â llawer mwy o gwestiynau ac yn ceisio tawelu meddyliau. Ie, felly, mae'n debyg yn hynny o beth, na fyddwn i'n dweud trafferth, ond gwaith ychwanegol a ychwanegwyd.”
– Gweithiwr cartref gofal, Lloegr |
Defnyddiodd staff gofal cymdeithasol offer digidol – weithiau am y tro cyntaf – i gyfathrebu â chydweithwyr. Roedd hyn yn cynnwys Microsoft (MS) Teams, Zoom a WhatsApp.
| “ | Doedden ni byth yn gwybod dim am Webex, doedden ni byth yn gwybod dim am [MS] Teams, doedden ni byth yn gwybod dim am Zoom [cyn y pandemig] ac yn gyflym iawn roedd yn rhaid i ni ddod o hyd i ffordd newydd o gyfathrebu.”
– Gweithiwr cartref gofal, Lloegr |
| “ | Roedd gennym ni gyfarfodydd dyddiol bob bore am 9:30 drwy MS Teams lle byddem ni'n adrodd yn ôl beth oedd yn digwydd ar ein pen ni ac roedden ni'n cael yr alwad ffôn ddyddiol hon, dim ond i gael syniad o ble roedden ni, a oedd gennym ni ddigon o gyflenwadau. Byddem ni'n mynd drwy staffio a dyna sut y byddem ni'n derbyn y canllawiau diweddaraf hefyd.”
– Rheolwr cofrestredig ar gyfer gofal cartref, Lloegr |
Trafododd rhai cyfranwyr y manteision cyfathrebu ar-leinEr enghraifft, roedd staff gofal cartref a nyrsys cymunedol yn gadarnhaol ynglŷn â sut roedd hyn yn lleihau amser teithio, tra bod eraill yn gallu cwrdd ag ystod ehangach o gydweithwyr. Mae'r ffyrdd hyn o weithio a'r manteision wedi parhau ers y pandemig.
| “ | [Yn] nghyfarfod y tîm amlddisgyblaethol, roedden ni’n arfer mynd yn bersonol i neuadd y dref i gyfarfod, ond nawr, mae popeth ar-lein. Mae’n beth cadarnhaol: gallwn ni arbed…amser teithio [a] arian [a] gallwn ni gynnwys mwy o bobl yn y cyfarfod Zoom.”
– Rheolwr cofrestredig, yr Alban |
| “ | Dysgon ni i gyd sut i ddefnyddio Zoom a [MS] Teams a phethau gwahanol fel 'na a newid y ffordd mae llawer ohonom ni'n gweithio. Dw i'n meddwl bod pethau wedi dod i'r amlwg sydd wedi gwella sgiliau pobl, eu cydbwysedd rhwng bywyd a gwaith, pethau maen nhw'n eu gwneud o ddydd i ddydd. Mae pobl efallai'n teithio llai ac, wyddoch chi, yn addasu mwy i bethau.”
– Nyrs gymunedol, Lloegr |
Cymryd cyfrifoldebau ychwanegol
Roedd prinder staff yn golygu bod yn rhaid i lawer o weithwyr gofal cymdeithasol proffesiynol ymgymryd â rolau a chyfrifoldebau ychwanegol. Clywsom sut y gwnaeth gweithwyr gofal cymdeithasol proffesiynol ymgymryd â thasgau a fyddai fel arfer yn gyfrifoldeb gweithwyr gofal iechyd proffesiynol (a ddisgrifir ym Mhennod 7), yn ogystal â chyfrifoldebau ar ddiwedd oes (gweler Pennod 4).
Mewn rhai cartrefi gofal, roedd gweithgareddau cymdeithasol a grŵp fel ioga a chelf a chrefft yn cael eu darparu gan ddarparwyr allanol cyn y pandemig. Roedd hyn yn golygu bod gweithwyr gofal cymdeithasol yn aml yn cymryd y cyfrifoldeb ychwanegol am y rhain yn ystod y pandemig. Roedd staff eisiau i'r rhain barhau i gefnogi lles ac ymgysylltiad cymdeithasol ymhlith preswylwyr. Dywedodd gweithwyr cartrefi gofal ei bod yn arbennig o heriol jyglo anghenion cymdeithasol ochr yn ochr â gofynion darparu gofal personol, a hynny i gyd wrth gynnal mesurau rheoli heintiau.
| “ | Byddem yn ceisio gwneud pethau [cymdeithasol] mor aml ag y gallem, ond…pan fyddwch chi'n gweithio ac yn gwneud gofal personol a beth bynnag [arall y mae'n rhaid i chi ei gwmpasu i ddiwallu anghenion gofal sylfaenol pobl] dim ond cymaint o weithgareddau cymdeithasol y gallwch chi eu gwneud.”
– Gweithiwr cartref gofal, Lloegr |
Dywedodd rheolwyr cartrefi gofal wrthym hefyd sut roedd yn rhaid i staff eraill, fel staff y gegin, gweithwyr tŷ, glanhawyr a phorthorion, weithiau ddarparu gofal neu rannu cyfrifoldebau i wneud iawn am brinder staff, pan oedd staff yn absennol ar fyr rybudd.
| “ | Roedd rhaid i mi gymryd cogyddion allan o'r gegin i ddarparu gofal personol oherwydd pan ddechreuon nhw brofi pobl, dyna pryd roeddech chi i ffwrdd am y 14 diwrnod, roedd gen i 35 o staff mewn un diwrnod yn mynd i lawr, mae gen i gleifion oedd â Covid, nid oedd teuluoedd yn cael ymweld, a fyddai wedi bod yn wych i'n helpu ni. Felly, rwy'n cofio gorfod [cymryd] staff allan o'r gegin, roedd rhaid i mi gymryd staff oddi ar ddyletswyddau glanhau [gan ddweud wrthyn nhw], 'Mae angen i chi wneud gofal personol'.”
– Rheolwr cofrestredig cartref gofal, Gogledd Iwerddon |
| “ | Roedd yn rhaid i ni weithio’n brin o staff. Y diwrnod pan brofodd wyth o staff yn bositif, des i i mewn, daeth yr arweinwyr tîm i mewn, daeth y gweithwyr tŷ yn staff cegin. Felly, roedd yn rhaid i ni i gyd ymdopi.”
– Rheolwr cofrestredig cartref gofal, Lloegr |
Dywedodd gweithwyr gofal cymdeithasol proffesiynol wrthym sut roedd rheolwyr a goruchwylwyr yn darparu gofal personol uniongyrchol i lenwi bylchau mewn rotas. Fodd bynnag, roedd hyn yn golygu nad oedd rheolwyr ar gael i ymateb i broblemau neu faterion.
| “ | Weithiau, byddai'n rhaid iddyn nhw [goruchwylwyr] gamu i mewn i wneud ein rôl ni fel gweithwyr cymorth, sydd wedyn yn golygu bod llai o oruchwylwyr i fynd i siarad â nhw os oes problem neu i ymateb os oes problem. Byddai'n bendant yn creu llawer mwy o straen.”
– Gweithiwr cymorth, Gogledd Iwerddon |
Pan oedd anwyliaid yn gallu dod yn ôl i'r cartref gofal ac ymweld â phreswylwyr, daeth glanhau a diheintio hyd yn oed yn bwysicach a chymerodd hyn amser.
| “ | Pan fyddai'r ymweliad wedi gorffen, byddech chi wedyn yn defnyddio chwistrell cefn ac yn chwistrellu popeth, yn rhoi'r aerdymheru yno am hanner awr ac yna byddech chi'n trefnu ymweliadau, un ar ôl y llall.”
– Gweithiwr cartref gofal, Lloegr |
Cefnogaeth i'r gweithlu
Effeithiwyd ar lesiant meddyliol staff gofal cymdeithasol gan faint o werthfawrogiad a chefnogaeth yr oeddent yn teimlo yn ystod y pandemigGwnaeth cael eu gwerthfawrogi gan eu cyflogwr, y bobl yr oeddent yn gofalu amdanynt, y gymuned ehangach a'r llywodraeth wahaniaeth gwirioneddol i gyfranwyr a oedd yn gweithio ym maes gofal cymdeithasol. Er enghraifft, derbyniodd rhai gweithwyr cartrefi gofal wiriadau lles, tra bod eraill yn derbyn anrhegion gan eu cymuned. Helpodd yr ystumiau hyn weithwyr gofal i deimlo eu bod yn cael eu gwerthfawrogi a'u cymell i barhau, er gwaethaf y pwysau arnynt.
| “ | Hefyd, dim ond anrhegion bach fel rhoddion a gawson ni, ond pethau oedd yn wirioneddol neis…wrth i ni gasglu PPE, fe gasglon ni flwch o siocledi. Trwy'r post, cawson ni docyn bach a ddywedodd, 'Anfon cwtsh mawr atoch chi'.”
– Gweithiwr cartref gofal, Lloegr |
Dywedodd gweithwyr proffesiynol nad oeddent yn teimlo eu bod yn cael eu gwerthfawrogi wrthym am y dicter a'r dicter a deimlent oherwydd nad oeddent yn cael eu cefnogi'n iawn.
| “ | Wrth edrych yn ôl nawr, rwy'n flin. Roeddwn i'n flin ac yn rhwystredig gyda fy ngwaith oherwydd na wnaethon nhw ddim byd i'm helpu, dw i ddim yn meddwl. Mae gen i'r problemau hynny fel dicter a rhwystredigaeth gan feddwl, 'A wnaed hyn i gyd yn iawn?'”
– Gweithiwr cymdeithasol, yr Alban |
Dywedodd rhai rheolwyr cartrefi gofal wrthym sut yn ystod y cyfnod clo daeth cefnogaeth gan eu pencadlysoedd neu grwpiau sector eraill yn gyfyngedig. Cyfrannodd hyn at deimladau o ynysu, gan eu bod yn aml yn gorfod gweithio trwy heriau cymhleth heb fawr o gefnogaeth.
| “ | Fel rheolwr roedd hi'n anodd iawn pan oedden ni dan glo, allwn i ddim cael unrhyw ymweliadau o'r pencadlys, felly dim ond fi oedd yno mewn gwirionedd a doedd neb yn dod i mewn i'm cefnogi ac roedd yn rhaid i mi gefnogi pawb.”
– Rheolwr cofrestredig cartref gofal, Lloegr |
Disgrifiodd gweithwyr gofal cymdeithasol deimlo'n gymdeithasol ynysig yn ystod y pandemigCaeodd y wlad i lawr yn gyflym iawn ac roedd hyn yn cyferbynnu'n llwyr â'r angen i weithwyr gofal cymdeithasol proffesiynol barhau â'u gwaith, yn aml gyda gofynion hyd yn oed yn fwy arnynt nag cyn y pandemig. Arweiniodd hyn at deimlad o bellter oddi wrth weddill cymdeithas, lle cafodd llawer o bobl eu rhoi ar ffyrlo neu ddechrau gweithio o gartref.
| “ | Roedden ni’n arfer clywed bod y bobl oedd yn gorfod aros gartref wedi blino arnyn nhw gartref ond y cyfan roedden ni wir eisiau ei wneud oedd aros gartref, ond allwn ni ddim aros gartref oherwydd roedd yn rhaid i ni ddod i’r gwaith, roedd ein trigolion ein hangen ni.”
– Rheolwr cofrestredig cartref gofal, Gogledd Iwerddon |
| “ | Roedd yn ymddangos yn ddryslyd iawn am amser hir, i weddill y wlad, oherwydd eu bod nhw wedi’u cloi i lawr, roedd yn eithaf syml iddyn nhw. Ond nid oedd ein gweithle ni – roedden ni’n fusnes fel arfer ond heb unrhyw ganllawiau na fframwaith i’n helpu ni.”
– Gweithiwr gofal iechyd, yr Alban |
Roedd rhai gweithwyr gofal cymdeithasol proffesiynol yn teimlo nad oeddent wedi cael eu cynnwys yn yr arddangosiadau cyhoeddus o gefnogaeth i weithwyr gofal iechyd a gweithwyr gofal proffesiynol, fel y 'clapio i ofalwyr'. Dywedasant nad oedd llawer o werthfawrogiad na dealltwriaeth o'r pwysau yr oeddent yn eu hwynebu yn y gwaith.
| “ | Roeddwn i'n teimlo'n gryf iawn fod pobl yn ysgwyd sosbenni a phethau, ond fydden nhw ddim wir eisiau dod yn agos atom ni. Felly, roedd y cyfan braidd yn symbolaidd ac roedden ni'n teimlo ein bod ni wedi ein gadael.”
– Gweithiwr gofal cartref, Lloegr |
| “ | Nid y GIG oedd yr unig arwyr. Roedd y gweithwyr gofal cartref tawel, heb gyflog digonol, wedi gweithio'n ormodol, heb werthfawrogi'r cyfan, ac wedi'u hanwybyddu yn [arwyr hefyd]!”
– Gweithiwr gofal cartref, Lloegr |
Er gwaethaf yr holl bwysau a'r heriau ac effeithiau parhaus y rhain, disgrifiodd pobl a oedd yn gweithio ym maes gofal cymdeithasol yn ystod y pandemig hefyd y balchder a'r boddhad a gawsant yn y cyfraniad a wnaethant yn ystod y pandemig.
Stori IsabellaMae Isabella yn gweithio fel gweithiwr gofal uwch mewn cartref gofal preswyl i bobl â dementia yng Nghymru. Mae hi wedi gweithio yn y cartref ers 14 mlynedd. Pan ddechreuodd y pandemig, roedd rheolwr cofrestredig y cartref gofal wedi'i adael dramor oherwydd cyfyngiadau teithio, tra bod y dirprwy reolwr a'r gweinyddwr i ffwrdd yn sâl gyda symptomau Covid-19. Yn fuan dechreuodd preswylwyr a staff hefyd gael symptomau. Wythnos cyn i'r llywodraeth orfodi cyfyngiadau symud, siaradodd Isabella â rheolwr y cartref gofal, a oedd yn dal i fod yn sownd dramor, a gwnaethon nhw'r penderfyniad anodd i gloi'r cartref gofal. Yr wythnos honno, bu farw eu preswylydd cyntaf o Covid-19 a amheuir. Bu’n rhaid i Isabella rannu’r newyddion gyda’r teulu dros y ffôn, a oedd yn peri gofid mawr iddi. Gwrthododd gweithwyr gofal iechyd proffesiynol ddod i’r cartref gofal i wirio’r farwolaeth, a oedd hefyd yn peri gofid mawr iddi. Yn y pen draw, cadarnhawyd y farwolaeth drwy alwad fideo. Yn ddiweddarach y diwrnod hwnnw, cyrhaeddodd ymgymerwyr mewn siwtiau peryglus, a oedd yn dychryn staff a phreswylwyr eraill. |
|
| “ | Ni fyddai neb yn dod allan i wirio ei farwolaeth, ar ôl 5 awr cadarnhawyd ei farwolaeth trwy alwad fideo, ffoniais y trefnwyr angladdau a gofynasant a oedd ganddo symptomau Covid ac atebais ie, pan ddaethant i'w gasglu roeddent yn edrych fel dynion gofod, roedd yn farwolaeth mor anurddasol, ni chawsom roi ein gofal diwedd oes arferol, ni wnaeth unrhyw staff rewi i roi ffarwel iddo fel y byddem fel arfer oherwydd nad oedd gennym staff, roedd y preswylwyr eraill yn ofnus. |
| Y farwolaeth hon oedd y gyntaf o lawer mwy dros y misoedd nesaf, a oedd yn gyfnod emosiynol heriol a dan bwysau dwys i Isabella. Roedd y cartref gofal hefyd yn cael trafferth gyda phrinder staff yn gysylltiedig â salwch, ofnau o ddal Covid-19, rhieni sengl yn cael trafferth gyda gofal plant oherwydd cau ysgolion ac eraill yn gwarchod eu hunain oherwydd cyflyrau iechyd sylfaenol. O ganlyniad, roedd yn rhaid i gartref gofal Isabella ddibynnu ar staff asiantaeth, a oedd yn cymhlethu rheoli heintiau gan fod y staff hyn yn gweithio mewn sawl cartref gofal gwahanol.
Roedd Isabella yn wynebu'r her gyson o reoli teuluoedd oedd yn awyddus i weld preswylwyr y cartrefi gofal. Roedd hi wedi gobeithio y byddai'r cyfyngiadau symud yn cynnig rhywfaint o seibiant, ond newidiodd y gofynion yn syml. Roedd y ffonau'n canu'n barhaus gyda galwadau gan deuluoedd oedd yn ei chael hi'n anodd cysylltu â phreswylwyr trwy alwadau fideo oedi neu ffonau heb eu hateb ac yn teimlo'n rhwystredig ac yn flin. Ar un adeg, gweithiodd Isabella 23 diwrnod yn olynol. Yn ystod y cyfnod hwn roedd hi'n delio â phrinder PPE, rhyddhau annisgwyl o'r ysbyty yng nghanol y nos a thrigolion yn teimlo'n ofnus ac wedi'u gadael. Nid oedd gweithwyr gofal iechyd proffesiynol yn gallu ymweld â'r trigolion. Gadawodd hyn Isabella yn teimlo'n cael ei gadael ac ystyriodd roi'r gorau iddi sawl gwaith. |
|
| “ | Roedd yn uffern, meddyliais am roi'r gorau iddi, roeddwn i'n teimlo fel ein bod ni ar ein pennau ein hunain, doedd gweithwyr iechyd proffesiynol ddim eisiau gwybod, doedd timau iechyd meddwl, dietegwyr, nyrsys ymataliaeth ddim yn ymweld mwyach.” |
| Mae effeithiau emosiynol hirdymor y pandemig yn parhau i fodoli i Isabella, yn enwedig pan mae hi'n cofio gofid y preswylwyr na chawsant ofal diwedd oes priodol a'r teuluoedd nad oeddent yn gallu ffarwelio. | |
| “ | Gallwn fynd ymlaen ac ymlaen a phobl yn dweud ei fod yn teimlo cyhyd yn ôl nawr ond i mi mae'n dal i deimlo fel ddoe, rwy'n teimlo'n drist dros y rhai a gollon ni ac na chawsant y gofal diwedd oes yr oeddent yn ei haeddu, rwy'n teimlo'n drist dros y staff da a gollon ni oherwydd eu bod nhw'n ofni cael Covid, mae fy nghalon yn torri dros y teuluoedd na chawsant ffarwelio ac rwy'n drist amdanaf i yn sownd gyda'r atgofion o'r pethau gwaethaf y bu'n rhaid i mi eu dioddef erioed heb fawr o gefnogaeth gan y rhai a ddylai fod wedi." |
| Ar yr un pryd, mae Isabella yn hynod falch o'r hyn a gyflawnodd yn ystod y pandemig. | |
| “ | Rwy'n dal i deimlo'n emosiynol iawn nawr yn siarad am Covid a gweithio drwyddo yn y sector gofal, rwy'n teimlo'n freintiedig ac yn drist ar yr un pryd, mae'n un o'm cyflawniadau mwyaf balch mewn bywyd, ond ar y pryd roedd yn teimlo fel na fyddai byth yn dod i ben. |
Effaith barhaus y pandemig
Dywedodd rhai staff gofal cymdeithasol wrthym, oherwydd gweithio yn ystod y pandemig, eu bod wedi dal Covid-19 ac wedi mynd ymlaen i ddatblygu Covid Hir. Yn aml, mae hyn yn parhau i gael effaith niweidiol ar eu bywydau.I rai, roedd teimladau cryf o fai a dicter tuag at eu swydd, yr amodau yr oeddent yn gweithio ynddynt a'r sector gofal cymdeithasol. Teimlai'r cyfranwyr hyn, pe na byddent wedi bod yn gweithio ym maes gofal cymdeithasol, na fyddent wedi bod mewn perygl mor uchel o ddal y feirws. Ni all rhai weithio mwyach, ac mae eraill wedi'u cyfyngu o ran y math o waith y gallant ei wneud neu'r oriau y gallant eu gweithio.
| “ | Mae gen i Covid Hir. Fyddwn i ddim wedi cael hynny pe bawn i wedi cael fy amddiffyn. Dyna'r gwir amdani. Mae'n debyg na fyddwn i wedi'i gael, oherwydd fy mod i'n feudwy. Felly, fyddwn i ddim wedi gadael y tŷ.”
– Gweithiwr gofal cartref, Lloegr |
| “ | Mae'n cymryd amser hir i mi wneud pethau o gwmpas y tŷ. Mae fy ngŵr yn glanhau ac yn coginio. Mae'n cymryd amser hir i mi gael cawod a pharatoi ar gyfer y diwrnod. Roeddwn i'n arfer mynd allan am dro, ond alla i ddim ei wneud mwyach oherwydd fy anadlu ac mae fy nghorff yn wan. Rwy'n teimlo fy mod i wedi cael fy siomi gan lawer o bobl a allai fod wedi gwneud yn llawer gwell.”
– Gweithiwr cartref gofal, Lloegr |
| “ | Ni allaf bellach wthio cadeiriau olwyn na gwneud gofal personol. Mae fy llwyth gwaith yn gyfyngedig. Felly, dim ond contract 18.5 awr sydd gennyf nawr gan na allaf weithio'n llawn amser mwyach.”
– Gweithiwr gofal, Lloegr |
Roedd y rhai oedd yn byw gyda Covid Hir hefyd yn rhwystredig ac yn flin nad oeddent yn cael cynnig digon o gefnogaeth tymor hwy.Fe wnaethant dynnu sylw at y gwahaniaeth rhwng y risgiau a gymerasant a'r ymdrechion a wnaethant wrth weithio yn ystod y pandemig a'r diffyg cefnogaeth sydd ar gael iddynt nawr.
| “ | Mae pobl sydd â Covid Hir wedi cael eu gadael, dyna faint o arwr oedden ni, nad ydyn ni'n bwysig nawr…Dw i'n meddwl ei fod wedi gadael blas straen wedi trawma iawn i lawer o bobl nawr.”
– Gweithiwr cartref gofal, Lloegr |
Stori SabinaMae Sabina yn byw yn Lloegr ac yn gweithio fel therapydd galwedigaethol. Cyn y pandemig, roedd hi'n helpu pobl â chyflyrau iechyd meddwl i gael mynediad at gymorth ac ymgysylltu â gweithgareddau dyddiol yn y gymuned. Unwaith i'r pandemig ddechrau, roedd hi'n cefnogi pobl ag anghenion gofal mwy cymhleth mewn uned adsefydlu. Daliodd Sabina Covid-19 ac aeth ymlaen i ddatblygu Long Covid, sydd wedi newid ei bywyd. Mae hi'n teimlo'n flin iawn tuag at ei chyflogwr a'r system iechyd a gofal cymdeithasol oherwydd ei bod hi'n teimlo nad yw wedi cael ei chefnogi o gwbl. |
|
| “ | Rydw i wedi mynd ymlaen i ddatblygu Long Covid, sydd wedi newid fy mywyd ac efallai na fyddai hynny wedi bod yn wir [pe na bawn i wedi bod yn gweithio yno yn ystod y pandemig…] Rydw i'n teimlo ein bod ni wedi cael ein siomi, oherwydd bod yr adeilad yn hen adeilad, [doedd] ddim yn addas at y diben mewn gwirionedd [gyda awyru]. Gallen nhw fod wedi darparu uned aer o ryw fath o leiaf i ddod ag aer ffres i mewn a [lleihau] y diferion a'r [risg] trosglwyddo.” |
| “ | Roedd yn fraint helpu pobl, ond rwyf wedi blino’n lân ac mae’n frawychus…Rwy’n teimlo nad oeddem wedi cael ein cefnogi gan haenau uwch y rheolwyr, mewn gwirionedd…Cawsom ein gorfodi i sefyllfaoedd na fyddem efallai wedi bod ynddynt fel arall.” |
Rhai o'r gweithlu datblygu afiechydon corfforol eraill a gysylltwyd ganddynt â phwysau gweithio yn ystod y pandemigEr enghraifft, mae rhai cyfranwyr yn credu eu bod wedi datblygu diabetes o ganlyniad i ddeiet gwael, tra bod eraill yn dweud eu bod wedi profi bregusrwydd tymor hwy i firysau. Clywsom hefyd straeon eraill am gyflyrau iechyd a newidiodd fywydau yr oedd cyfranwyr yn teimlo eu bod wedi'u hachosi gan straen gweithio yn ystod y pandemig.
| “ | Erbyn diwedd y cyfnod clo, roeddwn i'n wael iawn ac fe ges i ddiagnosis o ddiabetes mewn gwirionedd. Gan fy mod i'n gweithio cymaint o oriau [a] heb fawr o gwsg, roeddwn i'n byw ar fwyd sothach.”
– Gweithiwr cartref gofal, Lloegr |
| “ | Cefais strôc ym mis Tachwedd y llynedd…Rwyf wedi colli rhywfaint o fy ngolwg ac fe dreuliais ychydig wythnosau yn yr ysbyty…mae effaith y pedair blynedd a hanner diwethaf ar gynifer ohonom yn y mathau hyn o rolau wedi bod yn enfawr. Mae fy iechyd corfforol a meddyliol wedi dioddef yn sylweddol o ganlyniad.”
– Gweithiwr cartref gofal, yr Alban |
Dywedodd gweithwyr gofal cymdeithasol proffesiynol eraill, er eu bod wedi llwyddo i ymdopi yn ystod y pandemig, mai dim ond ar ôl i gyfnodau mwyaf anhrefnus y pandemig fynd heibio y gwnaethon nhw sylweddoli'r effaith feddyliol yr oedd wedi'i chymryd arnynt.
| “ | Roedd yr her feddyliol a wynebais, wrth i bethau ddirywio, o ganlyniad i'r hyn a aethom drwyddo i gyd… fe wnaethon ni ffynnu oddi ar yr argyfwng o orfod delio [ag ef] ac ymateb i bethau [bryd hynny], ond fe gymerodd ei doll rai blynyddoedd yn ddiweddarach.”
– Rheolwr cofrestredig, Lloegr |
| “ | Cefais chwalfa nerfol ym mis Hydref y llynedd ac roedd y cyfyngiadau symud a gweithio mewn cartref gofal trwy Covid yn gyfrannwr mawr at hynny.”
– Gweithiwr cartref gofal, Lloegr |
7 Mynediad at wasanaethau gofal iechyd a phrofiad ohonynt |
 |
Mae'r bennod hon yn archwilio sut y gwnaeth pobl ag anghenion gofal a chymorth gael mynediad at ofal iechyd yn ystod y pandemig. Mae'n disgrifio'r symudiad tuag at apwyntiadau rhithwir, rôl gynyddol y gweithlu gofal cymdeithasol wrth ddarparu gofal iechyd a'r pwysau cynyddol y mae hyn yn ei roi ar staff a gofalwyr di-dâl.
Gallu a pharodrwydd i gael mynediad at ofal iechyd
Arweiniodd cyfyngiadau symud a phandemig at ostyngiad neu oedi wrth gael mynediad at wasanaethau gofal iechyd arferol. Disgrifiodd gofalwyr di-dâl eu bod wedi profi pryder a rhwystredigaeth ychwanegol pan oedd yn anodd cael mynediad at wasanaethau. Dywedodd rhai eu bod yn cael trafferth cysylltu â meddygon teulu tra bod eraill yn ymatebol iawn. Roedd rhai cyfranwyr eraill yn rhwystredig oherwydd yr amser a'r ymdrech a gymerodd i drefnu apwyntiadau ar gyfer y person yr oeddent yn gofalu amdano.
| “ | Roedden nhw [y meddygon teulu] yn wych. Bydden nhw'n cysylltu'n ôl â ni ar unwaith ar ôl i ni ffonio. Dim problemau yno.”
– Nyrs gymunedol, Lloegr |
| “ | Chawson ni ddim llawer o lwc i gyrraedd y feddygfa [meddyg teulu], gallai hynny fod yn hanner awr o aros weithiau i gyrraedd y feddygfa, ac roedden ni’n ei chael hi’n rhwystredig.”
– Gofalwr di-dâl, Cymru |
| “ | Roeddwn i'n flin, gan feddwl, 'Beth sy'n digwydd?'. Dim ond amseroedd aros oedd o ac roedd yn rhwystredig bryd hynny. Nawr, pan edrychwch chi arno, roedd yn newydd i bawb ac mae'n rhaid i chi feddwl am y darlun mawr.”
– Gofalwr di-dâl, Lloegr |
Roedd gan lawer o bobl ag anghenion gofal a chymorth gyflyrau iechyd hirdymor ac roeddent yn dibynnu ar triniaeth barhaus reolaidd, megis ffisiotherapi, podiatreg, iechyd meddwl neu wasanaethau cymunedol eraill, i gynnal eu hiechyd a'u lles. Cafodd apwyntiadau ar gyfer gwasanaethau gofal iechyd yr oedd yn rhaid eu darparu yn bersonol eu haildrefnu, eu gohirio neu eu canslo, weithiau ar fyr rybudd. Arweiniodd hyn at ddirywiad iechyd cyfranwyr a chynyddu eu hanghenion gofal cymdeithasol. wrth i'r pandemig fynd ymlaen. Gwnaeth hyn i'r rhai ag anghenion gofal a'u gofalwyr di-dâl deimlo'n bryderus. Gwaethygodd prinder staff gofal cymdeithasol effaith hyn (fel y manylir ym Mhennod 6).
| “ | Doedd gen i ddim ffisiotherapi am gwpl o fisoedd, dw i'n meddwl, yn ystod uchafbwynt y pandemig, a oedd yn anodd iawn i mi ei reoli oherwydd, yn amlwg, heb symudedd a phethau fel 'na, mae fy nghyflwr yn dirywio, felly mae hynny'n rhoi mwy o bwysau ar fy nhîm gofal ar y pryd."
– Person ag anghenion gofal a chymorth, Lloegr |
| “ | Wythnos neu ddwy i mewn i'r pandemig, [ffoniwyd] ei seiciatrydd i ddweud na fyddent yn parhau. Ni allent ei gyfiawnhau oherwydd nad oedd yn hanfodol. Byddent yn cynyddu ei chyffuriau gwrthseicotig [ac] byddai'n cael ailwaelu o bryd i'w gilydd. Roedd yn wirioneddol frawychus - yn ofnadwy i bawb. Fe wnaethon ni gwyno ac erfyn ond dywedon nhw 'Na, na, na.'”
– Anwylyd preswylydd cartref gofal, Cymru |
| “ | Pethau fel podiatreg a'r holl bethau hynny, a aeth allan o'r ffenestr. Doedd dim o hynny i'w wneud.”
– Gofalwr di-dâl, Lloegr |
Straeon o Stockton-on-Tees a WrecsamClywsom brofiadau tebyg hefyd mewn digwyddiadau gwrando gyda staff gofal cymdeithasol mewn gwasanaeth anabledd dysgu yn Stockton-On-Tees a chartref nyrsio yn Wrecsam. |
|
| “ | Roedd gennym ni bobl oedd â chyflyrau difrifol fel epilepsi; roedd eu hapwyntiadau'n cael eu gohirio.”
– Gweithiwr gofal mewn lleoliad gofal preswyl, digwyddiad gwrando, Lloegr |
| “ | Wnaethon ni erioed weld meddyg. Maen nhw jyst yn meddwl am oedran [preswylydd y cartref gofal] ac nid ydyn nhw'n trafferthu.”
– Gweithiwr cartref gofal, digwyddiad gwrando, Cymru |
Weithiau hyfforddwyd cyfranwyr i roi triniaethau arferol, megis pigiadau, iddyn nhw eu hunain neu'r rhai yr oeddent yn gofalu amdanynt.
| “ | Yr un peth mawr, mae gen i sawl cyflwr iechyd eithaf difrifol ac un ohonyn nhw yw problem croen cronig hirdymor iawn. Ac fe gyrhaeddodd bwynt lle roedd yn rhaid i mi gael pigiadau bron yn rheolaidd. Felly, cwrs dros chwe mis, unwaith y mis. Nawr, roeddwn i newydd ddechrau cwrs pan ddigwyddodd y cyfyngiadau symud. Cefais alwad ffôn gan fy nyrs, yn dweud, 'Iawn, dydyn ni ddim yn siŵr a allwn ni eu gwneud ar hyn o bryd. Byddwn ni'n rhoi galwad i chi o fewn wythnos i ddweud sut allwn ni barhau i roi'r feddyginiaeth hon', ac yn y diwedd, cafodd fy ngwraig a fy merch diwtorial awr trwy Skype gyda'r nyrs ar sut i roi fy mhigiadau i mi ac fe'u danfonwyd i'r tŷ.
– Person ag anghenion gofal a chymorth, Lloegr |
Cafodd pobl ag anghenion gofal a chymorth eu heffeithio'n ddifrifol gan lai o fynediad at apwyntiadau diagnostig a thriniaeth ar gyfer cyflyrau sy'n peryglu bywyd, fel problemau gyda'r galon neu ganser, yn ystod y pandemig.
| “ | Cafodd apwyntiadau rheolaidd eu hatal, oherwydd cafodd pob angen arall ei hatal oherwydd bod popeth yn canolbwyntio ar Covid. Felly, yn amlwg fe effeithiodd ar apwyntiadau, dim ond ar gyfer [apwyntiadau] rheolaidd, ar gyfer sgan calon neu lawdriniaeth, efallai eu bod nhw i fod i gael eu canslo i gyd. Yn amlwg, cafodd hynny effaith enfawr ar rai cleifion, ie.”
– Gweithiwr gofal iechyd mewn cartref gofal, Gogledd Iwerddon |
| “ | Mae gennym ni lawer o gleifion sy'n cael triniaethau canser a phethau fel 'na. Cafodd triniaeth llawer o'r cleifion ei hatal yn ystod y pandemig ac yna ar ôl y pandemig fe'i dechreuodd eto. Ond erbyn y pwynt hwnnw, roedd y canser newydd ledu. Felly, er enghraifft mewn sefyllfaoedd fel 'na, a fyddai'r cleifion hynny ar y pwynt hwnnw pe na bai eu triniaeth wedi'i hatal ar y pwynt hwnnw, neu a fyddent yn byw bywyd gyda'u canser mewn maddeuant ac yn gallu bwrw ymlaen â'u bywydau?”
– Gweithiwr gofal iechyd, Lloegr |
Roedd cyfranwyr dan straen ac yn bryderus oherwydd anawsterau i gael mynediad at ofal iechyd brys. Anogwyd pobl i aros gartref oni bai ei fod yn gwbl angenrheidiol, hyd yn oed os oedd hyn yn golygu na allent gael mynediad at y gofal iechyd yr oedd ei angen arnynt.
| “ | Byddai ysbytai yn derbyn [argyfyngau] yn unig, oherwydd eu bod yn gwybod bod… dod â chleifion oedrannus i'r ysbytai yn eu hamlygu. Felly, roedd yn rhaid iddynt gymryd mesurau ychwanegol penodol, o ran y drefn dderbyn. Os oedd yn unrhyw beth y gellid ei reoli o fewn y gymuned, byddent yn hytrach yn dod â pharafeddygon i'r cartref gofal a'u cael i wirio'r claf.”
– Gweithiwr cartref gofal, Lloegr |
| “ | Hynny yw, roeddwn i eisoes yn gwybod bod yr Adran Damweiniau ac Achosion Brys yn brysur oherwydd, ar ôl dod o'r fan honno, o [enw'r ardal leol], mae'n rhaid bod tua 40 o bobl wedi bod yno ac roedd hynny am hanner awr y bore, dau o'r gloch y bore. Felly, roeddwn i'n gwybod y byddai'n aros ac fe geisiais hyd yn oed ei roi mewn ambiwlans, gan feddwl bod ganddyn nhw lwybr cyflymach i mewn. A dywedon nhw na, roedd 11 ambiwlans y tu allan, pob un â chleifion ar fwrdd, pob un yn aros yn yr un ciw i fynd i mewn i [yr Adran Damweiniau ac Achosion Brys] - ...suddodd fy nghalon ar y pwynt hwnnw. Ac rwy'n teimlo mai dim ond fy nghynnwrf yn yr Adran Damweiniau ac Achosion Brys a gafodd ateb digonol i ni.”
– Gofalwr di-dâl, Cymru |
Roedd oedi dro ar ôl tro i apwyntiadau yn gadael pobl ag anghenion gofal a chymorth yn teimlo eu bod wedi'u hanghofioUnwaith y cytunwyd ar ddyddiad apwyntiad, roedd cleifion yn ofni dal Covid-19 a sut y gallai hyn ohirio eu triniaeth eto.
| “ | Dw i'n teimlo fel petawn i wedi cael fy anghofio amdano, a dweud y gwir, oherwydd, fel, daeth llawer o fy apwyntiadau i ben. Roedden nhw fel, 'O, bydd popeth yn iawn, bydd yn symud ar-lein' ac yna wnaeth rhai o'r pethau hynny ddim digwydd. Roedd y llawdriniaeth yn cael ei gohirio hefyd ac yna roedd bron yn teimlo fel eu bod nhw'n dweud, 'O, wel os cewch chi Covid, wel dyna ni, fyddwn ni ddim yn gallu eich helpu chi'. Felly, roedd hynny'n frawychus iawn oherwydd, wyddoch chi, rydych chi eisoes yn poeni am gael Covid os oes gennych chi glefyd hunanimiwn. Ond yna roedd yn teimlo fel pe bai'n cael ei ddal uwch fy mhen, fel, fyddwch chi ddim yn gallu cael y llawdriniaeth yr oeddwn i wir ei hangen, felly dim ond haenau lluosog o straen oedd hi, ac roedd yn teimlo fel petawn i wedi cael fy anghofio ar y system.”
– Person ag anghenion gofal a chymorth, Lloegr |
Roedd ofn hefyd ynghylch ymweld ag ysbytai, gan fod pobl yn deall eu bod yn lleoedd risg uchel. Roedd mynychu apwyntiadau ysbyty yn bersonol yn bwysig ar gyfer rheoli cyflyrau iechyd ond roedd pryderon ynghylch dal Covid-19 a'r angen i wisgo masgiau yn golygu bod hyn yn anodd i rai cleifion.
| “ | Mae gen i ddirywiad macwlaidd yn y ddau lygad, sy'n effeithio llawer ar fy ngolwg, rwy'n cael pigiadau bob 6 wythnos ac mae hynny'n gwneud rhyfeddodau. Roeddwn i mor ofnus, roeddwn i'n casáu mynd [i'r ysbyty]. Ond dyna oedd yr unig beth - os byddwn i'n ei adael, yna byddai fy ngolwg yn dirywio llawer, felly roedd yn rhaid i mi orfodi fy hun yn fawr ac, oherwydd ei fod fel ambiwlans, mae'n dod ac yn ein codi, felly nid fi oedd yr unig un yno, roedd pobl eraill yno, ond roedd gennym ni i gyd fasgiau ymlaen, hyd yn oed y criw ar yr ambiwlans, roedd ganddyn nhw fasgiau a phethau bob amser.”
– Person ag anghenion gofal a chymorth, Lloegr |
| “ | Roedd hi'n arfer ofni cael apwyntiad ysbyty yn llwyr. Roedd hi'n ei chael hi'n eithaf gofidus. Roedd hi'n cael trafferth gyda'r mwgwd, ac roedd hi'n panicio ychydig, roedd yn anodd iawn [ei reoli].”
– Gofalwr di-dâl, Cymru |
Er gwaethaf y problemau gyda gwasanaethau gofal iechyd yn ystod y pandemig, clywsom hefyd lawer o enghreifftiau o ofal o ansawdd uchel, gan gynnwys rhai gwasanaethau wyneb yn wyneb a barhaodd. Dywedodd cyfranwyr wrthym am Meddygon teulu yn ymweld â chartrefi gofal yn bersonol os oes angenFodd bynnag, roedd hyn yn aml yn dibynnu ar gryfder y berthynas waith a'r cydweithio blaenorol rhwng y meddyg teulu a'r cartref gofal.
| “ | Roedden ni’n ffodus iawn oherwydd daeth y meddygon teulu i mewn ac roedden nhw wedi gwisgo PPE ac wedi profi eu hunain. Roedd gennym ni berthynas wych.”
– Rheolwr cofrestredig cartref gofal, Lloegr |
| Stori Lucy
Yn yr wythnos cyn y cyfyngiadau symud cyntaf, cafodd tad Lucy, Frank, syrthiad yn y stryd. Dirywiodd iechyd Frank yn gyflym, gan olygu bod angen gofal cartref a chymorth meddygol arno. Disgrifiodd Lucy yr anawsterau a gawsant wrth gael mynediad at gymorth meddyg teulu yn ystod camau cynnar y pandemig. |
|
| “ | Roedd hi’n anodd iawn, dw i’n meddwl, yn gyntaf oll doedd y meddygon teulu ddim yn gwybod beth oedden nhw i fod i’w wneud ac roedd galwadau cartref a phethau fel hyn yn ymddangos yn eithaf anodd cael mynediad atyn nhw. Roedd y meddyg teulu yn amharod iawn i ddod allan.” |
| O ganlyniad, trodd Lucy a'i theulu at y tîm nyrsio cymunedol lleol. Fe wnaethon nhw adeiladu perthynas i gael y gefnogaeth oedd ei hangen ar Frank. | |
| “ | Doedden ni ddim wir yn deall sut roedd iechyd yn gweithio i bobl hŷn mewn lleoliad cymunedol nes i ni weithio allan, wel, efallai nad y meddyg teulu oedd y gorau mewn gwirionedd ac yn y pen draw dechreuon ni ddeall mai'r tîm nyrsio cymunedol oedd y bobl a allai helpu mewn gwirionedd ac yna, o fis Mehefin ymlaen, dechreuon ni gael mwy o berthynas â nhw.” |
| Roedd Lucy yn ddiolchgar iawn am y gefnogaeth reolaidd a pharhaus yr oedd y nyrsys cymunedol yn gallu ei darparu. | |
| “ | Roedd angen ymyrraeth fwy rheolaidd ar fy nhad, rhywbeth na fyddai meddyg teulu yn ei ddarparu beth bynnag. Felly, gyda'r cwympiadau, felly parhaodd y cwympiadau, byddai'n cwympo o leiaf ddwywaith y mis ac yn gwaedu, oherwydd ei fod yn denau iawn; collodd lawer o bwysau. Byddai'n gwaedu, doedd dim padiau arno, hynny yw, byddai'n gwaedu'n eithaf hawdd ac roedd ganddo glwyfau drwy'r amser oedd angen eu hail-rhwymo a beth bynnag. Ac yna, oherwydd diffyg, oherwydd nad oedd yn symud, dechreuodd gael, fel, briwiau gwely, yn y bôn, felly roedd angen mewnbwn nyrsio cymunedol arno'n rheolaidd a fyddai'n dod i reoli clwyfau.” |
Apwyntiadau rhithwir ac o bell
Pan oedd angen cyngor gan feddyg teulu neu apwyntiad ar bobl ag anghenion gofal a chymorth, roedd hyn fel arfer ddigwyddodd ar-lein neu dros y ffôn.
| “ | Roedd rowndiau meddygon teulu yn y bôn o bell y rhan fwyaf o'r amser. Roedd meddygon teulu bob amser eisiau cadw llygad ar y preswylwyr, felly gallaf gofio cerdded o amgylch y cartref gyda'r iPad bach a, rhyw fath, ei roi o flaen y preswylwyr a dweud, 'Dywedwch helo wrth Doctor Kennedy'. Wyddoch chi, a byddent yn edrych ar y peiriant ac yn gwenu ac yn chwifio eu dwylo rhyw fath o beth.”
– Gweithiwr cartref gofal, Lloegr |
| “ | Roedd y meddyg teulu yno i roi cyngor ac arweiniad o'r dechrau. Wnaethon ni ddim eu gweld nhw wyneb yn wyneb mewn gwirionedd, ond roedden nhw yno ar y ffôn ac fe wnaethon nhw ein cefnogi ni drwyddo draw, a dweud y gwir.”
– Gweithiwr cartref gofal, Lloegr |
Fodd bynnag, clywsom sut roedd pobl â chyflyrau hirdymor cymhleth neu waethygol, oedolion awtistig a phobl yr effeithir arnynt gan ddementia yn cael apwyntiadau dros y ffôn ac ar-lein yn heriol.
| “ | Digwyddodd fy ailwaelu MS [sglerosis ymledol] adeg y pandemig hefyd ac roeddwn i eisiau help gan y meddygon a'r nyrsys, roeddwn i eisiau cwrdd â nhw'n bersonol, wyneb yn wyneb, ond ar y pryd, roedden nhw'n mynnu, 'Os gwelwch yn dda, peidiwch â dod i'r ysbyty ac arhoswch gartref', sut alla i aros gartref a gofalu amdanaf fy hun?”
– Person ag anghenion gofal a chymorth, Lloegr |
| “ | Fel oedolyn awtistig, roedd y diffyg gwasanaethau wyneb yn wyneb yn effeithio arnaf ac mae'n parhau i wneud hynny. Rwy'n cael trafferth siarad ar y ffôn a sylweddolais fod apwyntiadau meddyg teulu wyneb yn wyneb wedi cael eu gwrthod i mi am gyfnod o dros ddwy flynedd.”
– Person ag anghenion gofal a chymorth, Cymru |
Dywedodd staff sy'n gweithio mewn cartrefi gofal wrthym fod ymweliadau personol â meddygon teulu yn anaml iawn ac yn lle hynny'n defnyddio galwadau ffôn ac ar-lein.
| “ | Ein meddyg teulu, gwnes i lawer o alwadau fideo gyda nhw, roedd hi'n anodd eu cael i ddod allan.
– Gweithiwr cartref gofal, Lloegr |
| “ | Cyn gynted ag y tarodd Covid a’n bod ni wedi mynd i gyfnod clo, roedden ni’n cael trafferth mawr cael unrhyw feddygon, neu’r meddygon yn bennaf oedd yn gwrthod dod i’r cartref gofal…dechreuon nhw roi cyfarwyddiadau dros y ffôn yn gyflym a rhoi mwy a mwy o gyfrifoldebau i ni o ran sut roedd angen i ni reoli’r preswylwyr.”
– Nyrs yn gweithio mewn cartref gofal, Lloegr |
Dywedodd aelodau’r teulu wrthym hefyd eu bod yn bryderus ac yn flin am feddygon yn gwneud asesiadau o bell gan nad oeddent yn teimlo'n hyderus ynghylch cywirdeb y diagnosis. Disgrifiodd pobl ag anghenion gofal a chymorth pa mor rhwystredig oedd apwyntiadau o bell iddynt oherwydd nad oeddent yn teimlo y gellid deall eu cyflwr yn llawn heb gyswllt wyneb yn wyneb.
| “ | Roeddwn i'n flin nad oedd y meddyg teulu wedi bod i'r cartref gofal. Eu bod nhw newydd wneud galwad Zoom. Oherwydd pan nad ydych chi'n cyffwrdd â rhywun neu'n gwrando ar eu calon neu beth bynnag, yn gwrando ar yr ysgyfaint, dydych chi ddim yn gwybod beth sy'n digwydd.”
– Anwylyd preswylydd cartref gofal, Lloegr |
| “ | Doeddech chi ddim yn gallu gweld meddyg na meddyg teulu na ffisio na neb yn gorfforol, wyddoch chi? Roedd yn ynysig ac yn rhwystredig iawn oherwydd bod siarad ar y ffôn, heb i rywun eich gweld chi'n weladwy, wedi effeithio ar fy iechyd meddwl oherwydd roeddwn i mor rhwystredig nad oeddwn i'n cael fy nghlywed na'm deall na'm gweld.
– Person ag anghenion gofal a chymorth, Gogledd Iwerddon |
Cefnogi pobl sydd ag anghenion gofal a chymorth i gael mynediad at ofal iechyd
Rhoddodd y newidiadau i ofal iechyd lawer o bwysau ar gyfranwyr ac achosodd gryn bryder a straen. Er bod apwyntiadau wyneb yn wyneb yn hanfodol ar gyfer iechyd a lles pobl, soniodd rhai cyfranwyr pa mor rhwystredig oedd peidio â chael eu hanwylyd gyda nhw i'r apwyntiadau hynRoedd hyn yn arbennig o wir lle'r oedd cyfranwyr wedi arfer â'u hanwylyd yn eiriol drostynt ac yn rheoli sgyrsiau gyda gweithwyr gofal iechyd proffesiynol.
| “ | Roedd rhaid i mi weld ymgynghorydd yn ystod y pandemig, nad aeth yn dda o gwbl oherwydd nad oedd fy ngwraig yn gallu dod i mewn i'r ysbyty gyda mi, felly roedd rhaid i mi ddelio ag e fy hun, sydd, iawn, gallaf ddelio â phethau. Felly, yn y diwedd, codais a cherdded allan ar ôl ychydig o ddadl, wyddoch chi, 'Mae hyn yn wastraff o fy amser'. Felly, byddwn i'n dweud, ie, roedd hynny'n effaith ac, ie, yn un eithaf mawr mewn gwirionedd. Gallai fy ngwraig fod wedi dod i mewn a delio â'r sefyllfa, mae hi'n llawer tawelach na fi.”
– Person ag anghenion gofal a chymorth, Cymru |
Roedd y symudiad i apwyntiadau ar-lein hefyd yn golygu bod angen cymorth ar rai pobl na fyddai ei angen arnynt yn bersonol.
| “ | Os oes gennych chi rywun â dementia sydd ddim yn deall y ffôn, sut maen nhw'n mynd i ddweud wrth y meddyg dros y ffôn nad ydyn nhw'n teimlo'n dda iawn? Dydyn nhw ddim...roedd yn rhaid i chi ymwneud ag apwyntiadau gyda'r meddyg teulu.”
– Gweithiwr gofal cartref, Lloegr |
Roedd angen staff gofal cymdeithasol hefyd i gefnogi gofal brys neu argyfwng. Disgrifion nhw deimlo straen oherwydd y cynnydd mewn amseroedd aros ar gyfer ambiwlansys neu wasanaethau brys eraillDywedodd gweithwyr gofal cartref wrthym sut y gwnaethon nhw aros gyda phobl ag anghenion gofal a chymorth tra roedden nhw'n aros am y gwasanaethau brys er mwyn sicrhau eu bod nhw'n parhau'n ddiogel. Roedd hyn yn golygu bod eu hymweliadau â phobl eraill wedi cael eu gohirio neu eu canslo.
| “ | Roedd rhaid i ni ffonio ambiwlans ac yn amlwg dydych chi byth yn gwybod gyda'r ambiwlansys hyn pa mor hir fyddan nhw, felly roedd hynny'n anodd oherwydd roedd rhaid i ni aros cryn dipyn o amser iddyn nhw ddod ac yna mae hynny'n cael effaith ar weddill y cleientiaid yr oeddem i fod i'w gweld.”
– Gweithiwr gofal cartref, Cymru |
Clywsom hefyd gan ofalwyr di-dâl am amseroedd aros hir ar gyfer gofal brysRoedd methu aros gyda'r person yr oeddent yn gofalu amdano yn arbennig o llawn straen.
| “ | Dywedodd y gwasanaeth ambiwlans y bydden nhw'n dod amdano yn y bore [ond dim ond am 5 o'r gloch y nos y gwnaethon nhw gyrraedd] a chawsom ein cludo i'r Adran Damweiniau ac Achosion Brys. Ni fydden nhw'n gadael i mi fynd drwodd ac roedd yn rhaid i mi aros yn y dderbynfa tan 9 o'r gloch. Doeddwn i ddim yn gallu rhoi'r gorau i feddwl amdano yn gorwedd yno ar ei ben ei hun heb neb yn deall beth oedd o eisiau.”
– Gofalwr di-dâl, yr Alban |
Straeon gan ofalwyr di-dâlMewn digwyddiad gwrando ar-lein gyda gofalwyr di-dâl gyda Carers UK, clywsom nad oedd gofalwyr di-dâl yn aml yn gallu mynd gyda'r rhai yr oeddent yn gofalu amdanynt i'r ysbyty. Roedd hyn yn peri gofid mawr i'r gofalwr di-dâl a'r person yr oeddent yn gofalu amdano. |
|
| “ | Roedd ganddo ddeliriwm ac fe'i cludwyd mewn ambiwlans ac ni chefais ganiatâd i fynd gydag ef. Ac roeddwn i'n gwybod y byddai wedi cynhyrfu'n llwyr. Fi oedd ei atgof. Doedd e ddim yn gwybod ei hanes meddygol.”
– Gofalwr di-dâl |
| “ | Roedd y gofal yn anhygoel o ddifrifol ac ni chefais ganiatâd i'w gweld, ni chefais ganiatâd i fynd i mewn i'r adeilad. Ni chaniatawyd iddi fynd allan, doedd dim ffordd y byddwn i'n mynd heibio'r drws ffrynt.”
– Gofalwr di-dâl |
Siaradodd nyrsys cymunedol ac ardal am ddilyn i fyny gyda chleifion i ddarganfod canlyniad eu hapwyntiadau rhithwir a gwneud ymweliadau yn lle meddygon teulu.
| “ | Doedd meddygon teulu ddim yn ymweld o gwbl. Newidiodd fy rôl, gan fod disgwyl i mi fod gyda chleifion a gwneud galwadau Zoom gyda'r meddyg teulu, oherwydd byddent yn gwrthod dod i mewn. Fel nyrs ardal, rydym yn aml yn disgwyl llawer o rolau ychwanegol [ond] cawsom ein boddi â rolau newydd ac roedd yn rhaid i ni fwrw ymlaen ag e, allwn ni ddim dweud na.”
– Nyrs ardal yn ymweld â chleifion mewn cartrefi gofal, Lloegr |
| “ | Y meddygon teulu rydyn ni'n gweithio gyda nhw, fydden nhw ddim yn ymweld ag unrhyw gleifion. Fydden nhw ddim yn gweld cleifion mewn llawdriniaeth, felly popeth roedden nhw angen ei weld, roedden nhw'n ein hanfon ni allan i fynd i weld. Felly, roedd hynny'n rhoi llwyth gwaith ychwanegol ar ein gwasanaeth ni hefyd.”
– Nyrs gymunedol, Lloegr |
Cefnogaeth i'r gweithlu gofal cymdeithasol
Arweiniodd y canllawiau ynghylch apwyntiadau wyneb yn wyneb ac amharodrwydd rhai gweithwyr gofal iechyd proffesiynol i ymweld â phobl wyneb yn wyneb at llwyth gwaith cynyddol i staff gofal gan fod yn rhaid iddynt ymgymryd â thasgau gofal iechydRoedd gweithwyr gofal yn rhwystredig ac wedi blino’n lân heb gefnogaeth gan weithwyr gofal iechyd proffesiynol, ochr yn ochr â’u llwyth gwaith cynyddol (fel y disgrifiwyd ym Mhennod 6). Dywedodd cyfranwyr wrthym am codi tasgau, fel newid rhwymynnau neu rwymynnau, nad oeddent wedi derbyn hyfforddiant na chanllawiau ar eu cyferYn aml, roedd hyn yn gwneud iddyn nhw deimlo eu bod nhw'n peryglu eu hunain a'r person roedden nhw'n gofalu amdano.
| “ | Dydyn ni ddim wedi ein hyfforddi i wneud hynny. Ond roedd yn rhaid i chi. Doedd gennych chi ddim dewis. Roedd y dresin hwnnw wedi'i orchuddio â baw neu wedi cwympo i ffwrdd. Doedd gennych chi ddim dewis ond gwneud rhywbeth amdano.”
– Gweithiwr gofal cartref, Lloegr |
| “ | Gyda phethau fel nyrsys ardal, roedd yn rhaid i ni ddod yn nyrsys yn sydyn. Dydyn ni ddim wedi cymhwyso ac os oedden nhw'n dod i mewn i drin clwyfau neu unrhyw beth felly neu os oedd gan rywun anaf, rhwyg croen neu rywbeth a byddem ni'n eu galw'n naturiol, dim ond rhwymynnau oedden ni'n cael eu taflu at y drws.”
– Gweithiwr cartref gofal, Lloegr |
| “ | Ni fyddai meddygon teulu yn dod, yn sydyn roedden ni’n feddygon hefyd. Gofynnwyd i ni dynnu lluniau o unrhyw beth yr oeddem yn poeni amdano. Ar un adeg, roeddwn i’n dweud wrth y meddyg beth oedd ei angen arnaf o ran meddyginiaeth oherwydd yr hyn yr oedd defnyddiwr gwasanaeth yn ei arddangos ac roedden nhw’n ei roi i mi.”
– Gweithiwr cartref gofal, Lloegr |
Arweiniodd y mynediad llai at feddygon teulu hefyd at ddicter a rhwystredigaeth ymhlith gweithwyr gofal. wrth iddynt barhau i ofalu am bobl yn bersonol tra roedd yn ymddangos bod gan rai proffesiynau fwy o hyblygrwydd yn y ffordd yr oeddent yn cynnig apwyntiadau.
| “ | Rwy'n gwybod ei fod yn swnio'n ddrwg, ond roeddwn i'n dadlau gyda nhw [meddygon teulu] oherwydd ein bod ni allan yna'n darparu gofal i bobl ac roedden nhw'n meddwl ei bod hi'n iawn eistedd mewn meddygfa a dweud, 'Wel, allwn ni ddim dod allan oherwydd Covid'.”
– Gweithiwr gofal cartref, Lloegr |
8 Astudiaethau achos |
 |
Mae'r bennod hon yn rhoi trosolwg o sut yr effeithiodd y pandemig ar ddarparwyr gofal trwy ddefnyddio astudiaethau achos. Mae'n dwyn ynghyd brofiadau gweithwyr gofal cymdeithasol proffesiynol, y rhai sy'n byw mewn lleoliadau gofal a'u teulu a'u hanwyliaid i ddangos y gwahanol brofiadau.
Astudiaeth achos 1: Heriau darparu gofal gyda chefnogaeth gyfyngedig gan weithwyr gofal iechyd proffesiynol mewn cartref gofal bach yng Nghymru
Cefndir
Clywsom gan staff a phreswylwyr o gartref gofal preswyl bach yng Nghymru. Mae'r cartref yn fusnes preifat a redir gan deulu, sy'n darparu gofal a chymorth i bobl hŷn, gan gynnwys y rhai â dementia. Mae gan bob preswylydd ei ystafell sengl ei hun, rhai gydag ystafelloedd ymolchi en-suite ac eraill gydag ystafelloedd ymolchi cymunedol. Mae yna hefyd sawl man cymunedol mawr a gweithgareddau wedi'u trefnu i ganiatáu i breswylwyr gymdeithasu.
Newidiadau mewn gofal a heriau sy'n gysylltiedig â'r pandemig
Arweiniodd dechrau'r pandemig yn gyflym at newidiadau sylweddol i'r rhai oedd yn darparu gofal a'r rhai oedd yn ei dderbyn. Ar ddechrau'r pandemig, roedd preswylwyr wedi'u hynysu yn eu hystafelloedd, ac ni chaniatawyd gweithgareddau cymdeithasol ac ymweliadau gan anwyliaid mwyach. Fodd bynnag, gyda llawer o breswylwyr y cartref yn byw gyda dementia, roedd cyfyngiadau ar bellhau corfforol yn anodd eu gweithredu a'u cynnal.
| “ | Yn amlwg, pan fydd gan rywun â dementia Covid-19 rydych chi'n ceisio eu hynysu yn eu hystafell, fel nad ydyn nhw'n lledaenu o amgylch yr adeilad. Ond weithiau allwn ni ddim gwneud hynny bob amser. Felly, y person hwnnw, wyddoch chi, weithiau maen nhw'n teimlo'n sâl felly byddan nhw'n cysgu. Ond pan maen nhw i fyny wedyn, mae fel eu bod nhw allan o'u hystafelloedd. Ni allwn eu gorfodi yn ôl i'w hystafelloedd.”
– Gweithiwr cartref gofal |
Rhannodd staff gofal sut y newidiodd eu rolau yn ystod y pandemig. Fe wnaethant ymgymryd â chyfrifoldebau ychwanegol, gan gynnwys mesurau atal heintiau fel glanhau gwell, defnyddio PPE a glynu wrth weithdrefnau gwisgo a diosg (gwisgo PPE ac i ffwrdd) llym. Fe wnaethant hefyd gynnig mwy o gefnogaeth emosiynol i breswylwyr a'u teuluoedd. Roedd hyn yn cynnwys treulio mwy o amser gyda phreswylwyr mewn hunanynysu a chyfathrebu'n amlach ag anwyliaid i gynnig tawelwch meddwl ac ymdrin ag unrhyw bryderon a oedd ganddynt.
| “ | Dw i'n cofio un dydd Sadwrn y des i i mewn, roeddwn i yno'n llythrennol fel gofalwr. Roedd pawb arall wedi cael Covid. Roedd gen i lanhawr domestig, roedd hi'n fy helpu gyda'r preswylwyr, mae hi'n gwneud [gwaith domestig]. Felly, roedd y preswylwyr yn ynysu yn eu hystafelloedd, roedden ni'n cymryd eu prydau bwyd, shifft 13 awr y gwnes i hynny ar ei chyfer, roeddwn i'n rhedeg yn flinedig... Roeddwn i'n mynd â hambyrddau i fyny i un ystafell, mynd i un arall, tynnu ffedogau i ffwrdd. Y biniau y tu allan, roedd y cyfan yn cymryd llawer o amser, mynd i mewn i breswylydd arall, ffedog yn ôl ymlaen. Felly, roedd yn waith caled iawn.”
– Gweithiwr cartref gofal |
| “ | Byddai'r ffôn weithiau'n mynd yn gyson gydag aelodau'r teulu'n gwirio. Ac roedd yn rhaid iddyn nhw gymryd ein gair ni amdano eu bod nhw'n iawn.”
– Gweithiwr gofal |
Roedd staff yn y cartref yn aml yn gweithio sifftiau ychwanegol i weithio dros gydweithwyr oedd yn sâl neu'n hunanynysu. Roeddent yn myfyrio ar yr ysbryd tîm a'r undod yn ystod y cyfnod hwn, gyda staff ar bob lefel yn gweithio i sicrhau bod preswylwyr yn derbyn gofal digonol.
| “ | Fe wnaethon ni i gyd wneud gwaith ychwanegol, aros os oedden nhw’n brin o staff, felly hyd yn oed y rheolwr oedd yn ei wneud mewn gwirionedd, gweithiais shifft gyda’r rheolwr…roedd hi’n gweithio ar y llawr hefyd mewn gwirionedd.”
– Gweithiwr cartref gofal |
Mynediad at ofal iechyd
Er bod y cartref gofal yn teimlo eu bod wedi addasu'n eithaf da i gyfyngiadau'r pandemig, un o'r prif heriau a wynebwyd ganddynt oedd cael mynediad at wasanaethau gofal iechyd i breswylwyr. Teimlai'r staff eu bod wedi cael cefnogaeth gyfyngedig iawn a dywedasant wrthym am weithwyr gofal iechyd proffesiynol yn gwrthod mynd i mewn i'r cartref gofal drwy gydol y pandemig, p'un a oedd Covid-19 yn bresennol ai peidio.
| “ | Dwi ddim yn meddwl bod hyd yn oed y meddygon eisiau dod i mewn yma. Os oedden nhw'n meddwl ei fod yn ddifrifol, dywedon nhw wrthon ni i ffonio 999. Ond dyna beth oedd o.”
– Gweithiwr cartref gofal |
| “ | Dw i'n meddwl ei bod hi'n anodd yma, fel, nyrsys ardal ac nid oedden nhw eisiau dod i mewn, wel, cartref preswyl ydyn ni. A, meddygon a phethau, wyddoch chi, roedden ni angen y gofal yna oherwydd ein bod ni'n gartref preswyl ac nid ydyn ni'n gwneud hynny. Ac nid oedden nhw'n ymddangos eisiau dod i mewn, mae'n rhaid i ni wneud ein gwaith, felly dylen nhw fod wedi gallu gwneud eu gwaith nhw hefyd. Mae'n rhan annatod ohono, felly roedd hynny braidd yn annifyr.”
– Gweithiwr cartref gofal |
Effaith ar y rhai sy'n darparu ac yn derbyn gofal
Roedd amharodrwydd neu anallu gweithwyr gofal iechyd i ddod i mewn i'r cartref yn ychwanegu at lwythi gwaith y staff ac yn eu rhoi dan straen sylweddol. Roeddent yn rhwystredig ac wedi blino'n lân gyda'r tasgau ychwanegol y bu'n rhaid iddynt eu gwneud a'r pwysau cyson yr oeddent oddi tano.
| “ | Roedd yn anodd. Roedd yn anodd mynd. Fyddwn i ddim yn dweud bod y gefnogaeth yno. Fel yn, meddygol, fel meddygon a nyrsys a phethau fel 'na. Roedd yn teimlo fel ein bod ni wedi ein gadael i'r peth. Wyddoch chi, 'Ewch ymlaen ag e'.”
– Gweithiwr cartref gofal |
| “ | “Roedd gennym ni ŵr bonheddig oedd ar ddiwedd ei oes ond na chafodd ei ladd yn yr ysbyty oherwydd ein bod ni wedi’i nyrsio ein hunain, sydd, unwaith eto, nid cartref nyrsio ydym ni. Felly, mewn gwirionedd, ni ddylem fod yn gwneud hynny. Roedd yn rhaid i ni ffonio’r teulu i mewn ar y funud olaf, er mwyn iddyn nhw allu ffarwelio ac yna roedd yn rhaid iddyn nhw adael, roedd yn ofnadwy, roedd yn hollol ofnadwy. Dwi ddim yn meddwl y byddwn i wedi’i oddef pe bai’n fy nheulu i.”
– Gweithiwr cartref gofal |
Gadawodd y diffyg cefnogaeth hwn staff yn teimlo eu bod wedi cael eu gadael. Er enghraifft, rhannasant enghreifftiau o nyrsys ardal yn dod at y drws i roi offer iddynt ac yn dweud wrthynt am wneud triniaethau meddygol eu hunain, er nad oedd ganddynt unrhyw hyfforddiant meddygol.
| “ | Roedd gennym ni'r ddynes hon. Fedra i ddim cofio'r holl afiechydon oedd ganddi ar ei chorff nawr, ond daeth y ddynes hon allan mewn pothelli mawr, enfawr, iawn?… Felly, digwyddodd hyn pan oedd hi'n gyfnod clo ac rwy'n cofio na fyddai'r nyrsys yn dod i mewn i'r adeilad hwn o gwbl. Roedd hi'n rhoi rhwymynnau i ni wrth y drws cefn i ni ddelio ag ef, fi a'r dirprwy reolwr, oherwydd, yn amlwg, roedd hi'n un o fy mhreswylwyr, felly roedd hi'n fy adnabod yn dda a beth bynnag. A fi a'r dirprwy reolwr yn gwisgo'r ddynes hon. Fedra i ddim cofio nawr, efallai ei bod hi bob dydd neu bob yn ail ddiwrnod, ei chorff o'r top i'r gwaelod. Byddai'n rhaid ei hufennu, ei rhwymo. Roedd yn rhaid i ni ei nyrsio o'r gwely. Ac roedd fel nad oedd y nyrsys eisiau gwybod. Rwy'n gwybod bod popeth wedi'i gloi i lawr a beth bynnag. Hyd yn oed y meddygon, roedd yn fath o, 'Ewch ymlaen ag e.'”
– Gweithiwr cartref gofal |
Yn ogystal â'r pwysau a ddaeth gyda gorfod cynnig rhywfaint o ofal iechyd, roedd staff hefyd yn bryderus iawn nad oedd preswylwyr yn cael y gofal oedd ei angen arnynt. Rhannodd un aelod o staff ddigwyddiad lle aeth preswylydd â dementia yn sâl iawn gyda Covid-19, gan eu harwain i ffonio 999. Fodd bynnag, gwnaeth amharodrwydd staff brys i fynd â'r preswylydd i'r ysbyty iddi gwestiynu ei barn.
| “ | Fe wnaethon nhw [parafeddygon] ei chymryd hi yn y diwedd, ond cefais yr argraff nad oedden nhw wir eisiau ei chymryd hi. Ac yna ni ddaeth hi byth yn ôl. Ni fu farw ohono nac unrhyw beth. Ond fe wnaeth i rai ohonom ni gwestiynu ein hunain, 'Ydyn ni'n gwneud y peth iawn?'”
– Gweithiwr cartref gofal |
Roedd eu llwyth gwaith cynyddol a phrinder staff yn gadael staff yn bryderus nad oeddent yn treulio digon o amser gyda phreswylwyr. Er eu bod yn gwneud eu gorau glas, roeddent yn poeni am ba mor unig oedd preswylwyr yn ystod cyfnodau hir o ynysu ac am effaith rhyngweithio cymdeithasol a symbyliad cyfyngedig.
| “ | Fe wnaethon ni geisio gwneud yr hyn a allem, ond… nid oedd bob amser yn [bosibl], os ydw i'n onest. Os oedd gennym ni staff sgerbwd hefyd ac nad oedd staff i'w cael fel y cyfryw, roedd yn rhaid i ni wneud yr hyn a allem ei wneud. Fe wnaethon ni geisio gwneud ychydig o bethau gyda nhw. Boed yn bingo neu rywbeth, ond mae'n dibynnu a oedden ni'n cael diwrnodau da, diwrnodau drwg, sut oedd sefyllfa'r staff.”
– Gweithiwr cartref gofal |
| “ | Mae'n sicr o gael effaith ar swyddogaeth wybyddol eu [preswylwyr] oherwydd nad ydyn nhw'n gwneud cymaint ag y dylen nhw fod yn ei wneud. Byddem ni'n ceisio gwneud pethau mor aml ag y gallem ni, ond dim ond cymaint sydd pan fyddwch chi'n gweithio ac yn gwneud gofal personol a beth bynnag.”
– Gweithiwr cartref gofal |
Gan fod y rhan fwyaf o'r preswylwyr yn byw gyda dementia, teimlai'r staff fod gan lawer ohonynt ddealltwriaeth gyfyngedig o'r cyfyngiadau a chyd-destun y pandemig.
| “ | Mae gan y trigolion yma ddementia, y rhan fwyaf ohonyn nhw. Felly, dydw i ddim yn meddwl ei fod wedi effeithio arnyn nhw oherwydd dydyn nhw ddim yn cofio. Byddai'r rhai sy'n cofio wedi bod eisiau gweld eu hanwyliaid ac yna byddai hynny'n effeithio arnyn nhw, ond pan fydd ganddyn nhw ddementia, mae'n stori hollol wahanol.”
– Gweithiwr cartref gofal |
Rhannodd un preswylydd y clywsom ganddi sut nad oedd gan y cyfyngiadau effaith sylweddol ar ei phrofiad o fyw yn y cartref. Teimlai ei bod hi ac eraill yn parhau i dderbyn lefel dda o ofal gyda'r cyngor a'r cymorth yr oeddent eu hangen.
| “ | Doedden ni ddim wedi ein cyfyngu mewn gwirionedd; roedden ni’n ffodus iawn. Ac os oedd gennym ni broblem, bydden ni’n mynd at rywun ac yn ei thrafod, a byddai’n cael ei datrys neu ei rhoi o’r neilltu. Un neu’r llall, wyddoch chi.”
– Person sydd ag anghenion gofal a chymorth |
Astudiaeth achos 2: Profiadau o weithredu cyfyngiadau ar symud mewn cartref gofal yng Ngogledd Iwerddon
Cefndir
Ymwelsom â chartref gofal preswyl a dementia yng Ngogledd Iwerddon. Mae'r cartref yn cynnwys coridorau ar wahân, pob un yn cynnwys tua deg fflat hunangynhwysol. Addaswyd un o'r coridorau i gefnogi'r rhai yng nghyfnodau diweddarach dementia. Mae gan bob fflat ei gegin fach a'i ystafell ymolchi en-suite ei hun sy'n cefnogi preswylwyr i fyw'n annibynnol. Mae gan y cartref hefyd fannau a rennir gan gynnwys lolfa, ystafell fwyta a chegin, i ganiatáu i breswylwyr a'u hanwyliaid gymdeithasu. Mae gan y cartref ardd gyda seddi ac mae'n cynnig gwahanol weithgareddau a theithiau allan.
Newidiadau mewn gofal a heriau sy'n gysylltiedig â'r pandemig
Gyda chyflwyniad y cyfyngiadau symud, cafodd preswylwyr eu hynysu yn eu fflatiau a chafodd prydau bwyd eu danfon iddynt. Gan fod y fflatiau'n hunangynhwysol, roedd gan breswylwyr eu cyfleusterau eu hunain ac nid oedd yn rhaid iddynt ryngweithio â'i gilydd. Byddai staff yn dod â phreswylwyr at eu drysau ffrynt i chwarae gemau a chanu caneuon, gan gynnal pellter cymdeithasol, i'w helpu i gadw'n brysur ac yn ymgysylltu.
| “ | Fe wnaethon ni gloi i lawr, ie. Ond roedden ni'n ffodus iawn gan fod gan bob un o'n hystafelloedd en-suite. Felly, doedd dim 20 o bobl wedi ciwio i fynd i'r toiled neu beth bynnag. Roedd gennym ni ein toiled ein hunain, ein cawod ein hunain, dyna wnaeth ein hachub ni yma. Felly, ie, roedden ni yn ein hystafelloedd. Ond cawsom ein prydau bwyd yn ein hystafelloedd, doedd dim problem gyda hynny, wyddoch chi, ac roedden ni'n cael gofal da.”
– Person sydd ag anghenion gofal a chymorth |
Roedd rhai staff o'r farn bod y cyfyngiadau cychwynnol ar symud yn ormodol i bobl a oedd eisoes yn byw gyda'i gilydd mewn lleoliad gofal.
| “ | Roeddwn i'n meddwl ei fod yn ormod i ddechrau; rydych chi'n rhoi'r bobl hynny mewn cyfyngiadau symud pan maen nhw'n byw gyda'i gilydd beth bynnag. Os yw'n salwch, haint a gludir yn yr awyr, ni fydd eu cloi yn eu hystafelloedd gwely yn ei atal, o ystyried ein bod ni'n agor drysau'r ystafelloedd gwely tua 10 gwaith y dydd. Pwy sydd i ddweud nad oedden ni'n ei gario i mewn iddyn nhw? Pwy sy'n mynd i ofalu amdanyn nhw? Na, dydw i ddim yn cytuno â hynny o gwbl.”
– Arweinydd tîm |
Wrth i'r cyfyngiadau lacio, cafodd pob un o brif goridorau'r cartref eu 'swigo', pob un â'i dîm ei hun o staff. Byddai staff hefyd yn gwisgo PPE llawn i leihau trosglwyddiad rhwng coridorau. Roedd hyn yn caniatáu i breswylwyr ddod at ei gilydd yn y mannau cymunedol i gymryd rhan mewn gweithgareddau a bwyta'n gymdeithasol. Pe bai achos o Covid-19, byddai preswylwyr yn cael eu hynysu yn eu hystafelloedd eto.
| “ | Rydyn ni wedi cael pob math o ynysu yma ond, ie, felly am gryn amser, roedden nhw [preswylwyr] wedi'u hynysu i'w hystafelloedd, yna roedden ni'n gallu eu rhoi mewn cohort fesul aelwyd mewn coridor, ond roedd yn newid yn dibynnu ar ble roedd yr achosion ar y pryd, o ran yr hyn y gallem ni ei wneud. Fe wnaethon ni geisio bod mor gyfyngedig ag y gallem ni ond ie, roedd cyfnod o amser, dwi'n meddwl, efallai, y gallai fod wedi bod yn 8 wythnos, ar un adeg, roedden nhw yn eu hystafelloedd, yn syth.”
– Rheolwr cofrestredig |
Roedd y coridor, a oedd eisoes wedi'i addasu ar gyfer y rhai yng nghyfnodau diweddarach dementia, wedi'i agor ar ddechrau'r pandemig ac arhosodd fel hyn drwyddo draw. Gan fod gan y preswylwyr hyn ddealltwriaeth gyfyngedig o'r angen i gadw pellter corfforol, roedd hi'n anoddach i staff gynnal cyfyngiadau. Dynododd y cartref gofal ddau neu dri aelod o staff i weithio yn y coridor arbenigol hwn, er mwyn lleihau trosglwyddiad ac felly nid oedd yn rhaid i breswylwyr ddefnyddio PPE, yr oedd ei ddefnyddio'n aml yn achosi gofid a dryswch.
| “ | Mae [y coridor dementia] wedi'i adeiladu fel gweddill y tŷ, lle mae ganddyn nhw eu fflatiau unigol eu hunain, ond dydy e ddim yn gweithio. Dydy e ddim yn gweithio, felly roedd yn rhaid i ni ail-edrych ar sut roedden ni'n gweithio a chyfyngu, dwi'n meddwl mai 2, neu efallai 3, aelod o staff oedd i lawr yno. Bydden nhw'n ei gylchdroi allan, fel bod y [coridor] hwnnw'n gallu bod fel yr oedd ac os oedd y preswylwyr eisiau dod allan, eistedd yn y lolfa, roedd yn iawn. Doedd dim ffordd y gallen ni osgoi hynny o gwbl.”
– Dirprwy reolwr |
Effaith ar y rhai sy'n darparu ac yn derbyn gofal
Cafodd cyfyngiadau ar symud, yn enwedig yng nghyfnodau cynnar y pandemig, effaith sylweddol ar y rhai oedd yn derbyn a'r rhai oedd yn darparu gofal. Gadawodd cyfnodau hir o ynysu breswylwyr yn teimlo'n ddiflas ac yn unig. Dywedodd un preswylydd wrthym sut y collai'r rhyddid oedd ganddynt o'r blaen yn ystod y pandemig.
| “ | Yr unig newid i mi oedd dim rhyddid o gwbl. Roeddwn i yn fy ystafell 24 awr y dydd am amser hir iawn. Mewn cyfyngiadau symud llwyr am amser hir iawn. A'r unig beth oedd, nid y rhyddid sydd yna nawr i fynd i gael pryd o fwyd neu ddod allan a mynd allan neu beth bynnag.”
– Person sydd ag anghenion gofal a chymorth |
Gwelodd y staff effaith yr unigedd hwn ar iechyd meddwl y preswylwyr. Rhannasant sut roedd y preswylwyr yn ofidus oherwydd eu bod yn unig ac yn colli eu hanwyliaid.
| “ | Er bod ein preswylwyr yn wych… roedd peidio â gweld anwyliaid y byddent wedi’u gweld efallai 2 neu 3 gwaith yr wythnos yn sicr yn effeithio arnynt…roedd yna adegau pan oedd rhai preswylwyr efallai’n crio oherwydd eu bod wedi colli’r ymweliadau.”
– Dirprwy reolwr |
Cafodd yr unigedd a brofodd y preswylwyr effaith ganlyniadol ar lwyth gwaith y staff, a gymerodd rolau ychwanegol a olygai eu bod yn aml yn ymddwyn yn fwy fel aelodau o'r teulu, yn ogystal â gweithwyr gofal proffesiynol. Roedd yn rhaid iddynt hefyd roi mwy o sicrwydd i berthnasau nad oeddent yn gallu ymweld.
| “ | Roedd y preswylwyr gymaint yn fwy dibynnol arnom ni nag y byddent wedi bod o'r blaen, daethoch chi'n deulu iddyn nhw yn ogystal â gofalwr, sy'n beth da, dw i'n meddwl, rydyn ni eisiau bod yn deulu iddyn nhw, ond roedd yn rhaid i chi roi mwy o gefnogaeth emosiynol iddyn nhw nag y bydden ni wedi'i gorfod ei wneud o'r blaen. Rydyn ni bob amser wedi gorfod diwallu'r anghenion a helpu i sicrhau eu bod nhw wedi cael eu holl dasgau a phethau wedi'u cyflawni ond ar y pwynt hwnnw, roedd yn sicrwydd cyson iawn, roedd yn frawychus iddyn nhw, roedd yn ynysig.”
– Rheolwr cofrestredig |
| “ | Roedd llawer iawn o bobl yn dibynnu arnoch chi fwy. Yn amlwg, nid oedd y perthnasau'n dod i mewn cymaint, i lawr i nifer penodol o bobl a allai ddod i mewn. Roeddech chi'n canfod eich hun yn ateb llawer iawn o gwestiynau, neu bobl yn gofyn cwestiynau i chi nad oeddech chi'n gwybod yr atebion llawn iddynt. Yn amlwg, oherwydd mai eu hanwyliaid nhw ydyn nhw, roedd pethau'n ymddangos yn mynd yn anoddach arnom ni. Roedd fel, 'Dydych chi ddim yn gwneud hyn, dydych chi ddim yn gwneud hyn'.”
– Arweinydd tîm gofal |
I breswylwyr eraill, roedd cyfyngiadau ar ymweld yn cael llai o effaith. Clywsom sut, i lawer, roedd llawer o'u perthnasau yn hŷn ac yn ynysu hefyd, felly fe'i gwelwyd fel profiad a rennir. Roedd un preswylydd y siaradom ag ef nad oedd mewn cysylltiad â'i deulu yn teimlo ei fod wedi cael cefnogaeth dda ac wedi addasu'n dda i ynysu ar ei ben ei hun.
| “ | Roedd yn gyfnod clo 24 awr am gryn amser. Ond doeddwn i ddim yn ei chael hi'n rhyfedd mewn gwirionedd. Fe wnes i am gwpl o ddiwrnodau, mae'n debyg, ond fe wnes i arfer ag e'n eithaf cyflym. Ac rwy'n gaeth i chwaraeon beth bynnag, felly mae chwaraeon ar y teledu yn rhywle bob amser. A'r tîm sydd gennym ni yma, rydyn ni'n ffodus iawn, iawn yma.”
– Person sydd ag anghenion gofal a chymorth |
Roedd cyfyngiadau ar symud hefyd yn ei gwneud hi'n anoddach i staff, a oedd hefyd yn profi unigedd oherwydd na allent gymysgu â'u cydweithwyr. Er bod y system goridorau wedi gweithio'n dda i leihau trosglwyddiad a chaniatáu i breswylwyr ryngweithio, roedd y diffyg gwaith tîm yn gadael staff yn teimlo'n unig.
| “ | Roedd pawb yn gweithio'n unigol. Doeddech chi ddim cymaint yn rhan o dîm mwyach. Roedd pawb yn cael eu coridor eu hunain a dyna lle roedden nhw'n aros, lle byddai ein tîm staff yma'n gymdeithasol iawn, bydden nhw'n cael ciniawau gyda'i gilydd, brecwast gyda'i gilydd, felly daeth hynny i ben i gyd… Roeddwn i'n teimlo'n ynysig iawn drwy gydol fy niwrnod gwaith. Ie, byddai'r tîm rheoli a'r tîm uwch wedi ymyrryd dim ond i wneud yn siŵr bod popeth yn iawn a'm bod i'n teimlo fy mod i'n cael fy nghefnogi yn y ffordd honno, ond roeddwn i'n colli'r gwaith tîm.”
– Dirprwy reolwr |
Dywedodd staff wrthym am effaith barhaol unigedd ar y rhai sydd ag anghenion gofal. Roeddent o'r farn bod hyn wedi cyfrannu at ddirywiad meddyliol a chorfforol sylweddol ymhlith preswylwyr.
| “ | Roedd cymaint o ddirywiad. Felly, byddwn i'n dweud, o ddiwedd y pandemig hyd yn hyn, mae'n debyg bod 70% o'n preswylwyr wedi newid, lle maen nhw'n gorfod mynd i ofal nyrsio neu wedi marw, felly ie, gwelsoch chi'r dirywiad ynddyn nhw, yn feddyliol, yn gorfforol. Cafodd rhai ddementia yn y diwedd, dirywiodd rhai i'r pwynt lle roedd yn rhaid iddyn nhw fynd i ofal nyrsio yn gorfforol yn y pen draw.”
– Rheolwr cofrestredig |
Astudiaeth achos 3: Heriau darparu gofal gyda phrinder staff mewn cartref gofal yn yr Alban
Cefndir
Ymwelsom â chartref gofal preswyl bach di-elw yn yr Alban, sy'n cynnig cefnogaeth i fenywod hŷn. Mae gan bob preswylydd ei ystafell wely en-suite ei hun ac mae yna wahanol fannau cymunedol sy'n helpu i greu ymdeimlad o gymuned yn y cartref. Mae'r mannau cyffredin hyn yn caniatáu i breswylwyr ddod at ei gilydd i fwyta, cymdeithasu a chymryd rhan mewn amrywiaeth o weithgareddau, fel dosbarthiadau cadw'n heini, cwisiau a chanu gyda'n gilydd. Mae yna hefyd sawl cyfrifiadur i breswylwyr eu defnyddio yn ogystal â gardd fawr.
Newidiadau mewn gofal a heriau sy'n gysylltiedig â'r pandemig
Newidiodd dechrau'r pandemig a'r cyfyngiadau symud dilynol fywyd yn y cartref gofal yn sylweddol. Gyda phreswylwyr wedi'u hynysu yn eu hystafelloedd, roedd yn rhaid i staff gofal addasu i ffyrdd newydd o weithio, fel dosbarthu prydau bwyd yn unigol a darparu gofal un-i-un. Dywedodd un cyfrannwr a oedd yn gweithio yn y gegin ac yn gwneud gwaith tŷ wrthym am y protocolau hylendid llym a gyflwynwyd i leihau trosglwyddiad.
| “ | O, fe aethon ni, i ryw raddau, y tu hwnt i'r canllawiau. Mae gennym ni beiriant golchi llestri; mae'n glanhau ar dymheredd penodol ond ar gyfer unrhyw beth a ddaeth yn ôl gan y menywod roedd gennym ni doddiant, neu dywedwyd wrthym ni pa doddiant o gymhareb cannydd i ddŵr y caniateid i ni ei ddefnyddio. Felly, byddem ni wedyn yn eu socian ac rydym ni bob amser yn ei wneud beth bynnag ar ôl pob gwasanaeth neu byddai'n weithdrefn wahanol pe bai gan rywun Covid mewn gwirionedd. Wyddoch chi, byddem ni'n cadw'r holl bethau hynny ar wahân. Ac yna, byddai'r peiriant yn cael ei wagio, felly roedd yn llawer mwy o waith.”
– Gweithiwr cegin a gwas tŷ |
Dywedodd staff wrthym sut roeddent yn gweithio goramser neu sifftiau dwbl yn rheolaidd ac yn ymgymryd â chyfrifoldebau ychwanegol, fel dyletswyddau glanhau ychwanegol, i sicrhau bod preswylwyr yn cael gofal da. Dywedodd uwch staff wrthym sut y gwnaethant symud i'r cartref gofal yn ystod achosion, er mwyn sicrhau y gallai gofal digonol barhau. Roedd hyn hefyd yn golygu nad oedd yn rhaid iddynt ddefnyddio staff asiantaeth, nad oedd preswylwyr yn gyfarwydd â nhw.
| “ | Weithiau bydden ni'n symud i mewn am noson neu ddwy efallai pan fydden ni'n meddwl y byddai achosion eraill o'r clefyd yn digwydd, oherwydd doedden ni ddim yn gwybod a fydden ni'n cael staff ai peidio, neu doedden ni ddim yn gwybod effaith faint o help y byddai ei angen arnyn nhw. Roedd yna hefyd, fel, darparu'r gofal i'r cleientiaid, felly weithiau os oedd gennych chi - os yw rhywun yn sâl iawn, mae'n rhaid i chi ganolbwyntio ar y person hwnnw a chymryd rhywun oddi ar eu llawr cyffredinol. Felly, bydden ni'n camu i mewn ac yn helpu.”
– Rheolwr cofrestredig |
Roedd sicrhau digon o PPE hefyd yn heriol, yn enwedig yn ystod camau cynnar y pandemig. Roedd staff o'r farn bod cyflenwadau'n cael blaenoriaeth ar gyfer y GIG a soniasant am heriau wrth gael mynediad at fasgiau priodol, a arweiniodd at sicrhau eu cyflenwadau eu hunain gan fusnesau lleol. Archebodd rheolwr y cartref gofal gyflenwadau hefyd a chymerodd ragofalon cyn i'r pandemig ddechrau'n swyddogol.
| “ | Dechreuais archebu pethau cyn, wyddoch chi, cawson ni gyfarwyddiadau i wneud hynny neu gyfarwyddiadau gan y llywodraeth. Felly, fe wnaethon ni archebu masgiau ymhell cyn i ni fod i wneud hynny ac archebu gel glanhau hefyd ac, yn ffodus, fe wnaethon ni hynny oherwydd ar un adeg, allwn ni ddim cael dim byd oherwydd eu bod nhw i gyd yn cyflenwi'r GIG… Mae gennym ni gytundeb gyda chwpl o siopau mewn gwirionedd ac fe wnaethon ni siarad â nhw. Fe wnaethon nhw gael masgiau i mewn ac, yn lle eu gwerthu i'r cyhoedd, fe wnaethon nhw eu cadw yn ôl i mi.”
– Rheolwr cofrestredig |
Roedd hyn yn golygu bod gan y cartref gofal ddigon o PPE yn gyffredinol, yn bennaf oherwydd y penderfyniadau rhagweithiol gan uwch staff.
Effaith ar y rhai sy'n darparu ac yn derbyn gofal
Cafodd heriau unigryw’r pandemig a’r cynnydd canlyniadol yn y llwyth gwaith effaith sylweddol ar staff yn y cartref gofal. Roedd gorfod ymweld â phob preswylydd yn unigol i ddarparu gofal un-i-un, gan sicrhau bod canllawiau PPE yn cael eu dilyn, yn rhoi straen sylweddol ar staff. Roeddent yn poeni’n gyson am drosglwyddo’r firws ac yn flinedig o wisgo a thynnu PPE ymlaen a’i dynnu i ffwrdd ar ôl pob gweithdrefn. Arweiniodd hyn at bwynt torri i rai.
| “ | Roedd y staff yn dechrau crio ac wedi cael eu llethu. Roedd yn anodd iawn i'r staff gofal, a bod yn deg, oherwydd maen nhw'n mynd i mewn i ystafelloedd ac, bob tro, roedden nhw'n gwneud gweithdrefn; roedd yn rhaid iddyn nhw newid popeth a glanhau popeth.”
– Gweithiwr cegin a gwas tŷ |
Roedd staff hefyd yn poeni am yr effaith y byddai llai o gyswllt â phreswylwyr yn ei chael ar ansawdd y gofal yr oeddent yn gallu ei ddarparu. Yn hytrach na monitro a rhyngweithio â phreswylwyr mewn mannau cymunedol drwy gydol y dydd, dim ond cyfnod cyfyngedig o amser y gallai staff ei dreulio gydag unigolion yn eu hystafelloedd. Gadawodd hyn iddynt deimlo'n euog.
| “ | Dwi ddim yn meddwl bod prinder staff wedi [effeithio ar ansawdd y gofal]. Dwi jyst yn meddwl mai'r ffaith nad oedden nhw'n gallu bod yng nghwmni ei gilydd ac i gyd yn eu hystafelloedd eu hunain oedd yr hyn a wnaeth eu gofal yn llai. Allwch chi ddim treulio cymaint o amser gyda nhw.”
– Gweithiwr cartref gofal |
Rhannodd staff sut y byddai preswylwyr yn aml yn pwyso'r byswyr i gael sicrwydd a chwmni. Myfyriodd un cyfrannwr ar ba mor anodd oedd hyn i staff gofal.
| “ | Roedden nhw jyst wedi diflasu ac ychydig yn isel eu hysbryd ac yn ddryslyd. Ar y pryd roedd yn anodd i'r staff. Ie. Oherwydd bydden nhw'n pwyso'r byswyr drwy'r amser.”
– Gweithiwr cegin a gwas tŷ |
Teimlai staff fod cyfyngiadau’r pandemig wedi cael effeithiau gwahanol ar breswylwyr ag anghenion gofal gwahanol.
| “ | Yn enwedig, wel, fel, y rhai heb ddementia, a oedd yn effeithio arnyn nhw oherwydd bydden nhw'n meddwl am Covid yn gyson ac yn gwrando ar y newyddion… Y rhai â dementia, roedd yn peri gofid iddyn nhw, oherwydd roedd gennym ni rai menywod na fyddai byth yn gallu eistedd yn llonydd. Fel, roedden nhw bob amser yn cerdded yn gyson.”
– Gweithiwr cartref gofal |
Dywedon nhw wrthym sut mae cyfyngiadau wedi cael effaith barhaol ar breswylwyr. Er bod preswylwyr yn arfer mwynhau dod i lawr a chymryd rhan mewn gweithgareddau, roedd staff yn teimlo eu bod bellach yn cael trafferth gyda'u hyder ac yn aml yn aros yn eu hystafelloedd.
| “ | Cyn Covid, byddai pawb yn dod i lawr ac yn ymuno. Rydyn ni'n gweld bod pobl yn dal yn eu hystafelloedd, heb fod eisiau dod allan.”
– Gweithiwr cartref gofal |
Er bod staff yn cael trafferth gyda'r llwyth gwaith cynyddol, roeddent yn teimlo eu bod yn cael cefnogaeth dda gan y rheolwyr ac yn cydnabod y mesurau rhagataliol a gymerwyd i gadw staff a phreswylwyr yn ddiogel.
| “ | Rhaid i mi ddweud yma ein bod ni wedi bod yn lwcus iawn, [gyda]'r tîm rheoli. Daethant i lawr bob bore ac, i ryw raddau, cawsant sgwrs gyda ni a phethau felly, a thrwy ei fewnwelediad [llwyddon ni] i gael pethau i mewn ymlaen llaw. Roedd ganddo, fel, masgiau a phopeth a ffedogau a phopeth. Pan oedd pobl yn brin, roedden ni'n lwcus iawn ei fod wedi rhagweld hynny'n dod.”
– Gweithiwr cegin a gwas tŷ |
Yn yr un modd, roedd y preswylwyr yn cydnabod parodrwydd y cartref gofal a'r hyder yr aeth y staff iddo er mwyn eu diogelwch. Rhannodd un preswylydd sut roedd y mesurau diogelwch yn ei gwneud hi'n teimlo'n ddiogel.
| “ | Roedden ni wedi paratoi’n ddigonol iawn. Pan ddywedaf wedi paratoi, dw i’n golygu, wyddoch chi, roedd yn rhaid i ni i gyd aros yn ein hystafelloedd, ond roedd ganddyn nhw ddiogelwch ar gyfer y staff gyda gwisgoedd a dillad amddiffynnol…Gwnaeth i mi deimlo’n ddiogel iawn.”
– Person sydd ag anghenion gofal a chymorth |
Canmolodd preswylwyr hefyd ymroddiad y staff a'r oriau ychwanegol a roddasant i mewn i osgoi'r angen am staff asiantaeth nad oeddent yn gyfarwydd â'u hanghenion gofal. Dywedodd un preswylydd wrthym sut roedd hi'n teimlo bod hyn yn arbennig o bwysig i breswylwyr â dementia sy'n cael mwy o sicrwydd gan drefn a chysondeb.
| “ | Dyna un peth arbennig roeddwn i'n mynd i'w grybwyll beth bynnag oherwydd gwnaeth hynny wahaniaeth mawr ac, nid yn erbyn nyrsys asiantaeth, maen nhw'n angenrheidiol, ond o ran cyfathrebu, sydd mor bwysig yn fy marn i, doedden nhw ddim yn adnabod y menywod mewn gwirionedd ac efallai'r holl fanylion y mae pobl â dementia eu hangen yn arbennig.”
– Person sydd ag anghenion gofal a chymorth |
Astudiaeth achos 4: Profiadau o ofalu am bobl ag anabledd dysgu a phobl awtistig yn ystod y pandemig
Cefndir
Clywsom gan ddarparwr gofal cymdeithasol preifat yn ne-ddwyrain Lloegr, sy'n cefnogi oedolion ag anabledd dysgu a phobl awtistig. Mae'r darparwr yn rheoli sawl lleoliad gofal, gan gynnwys cartrefi gofal cofrestredig a thai byw â chymorth. Mae'r holl bobl y maent yn gofalu amdanynt yn derbyn cymorth 24/7, gan gynnwys staffio dros nos. Mae'r darparwr gofal yn cefnogi pobl o oedran gweithio (18-64) a phobl hŷn (65+).
Newidiadau mewn gofal a heriau sy'n gysylltiedig â'r pandemig
Yng nghyfnodau cynnar y pandemig, gweithredodd y darparwr gofal system 'swigog' a oedd yn caniatáu i breswylwyr ryngweithio'n normal o fewn tai, gan leihau'r aflonyddwch i'w bywydau beunyddiol. Dim ond yn ystod achosion y byddai preswylwyr yn cael eu hynysu, lle byddai staff yn dod â'u prydau bwyd iddynt. Cyfyngwyd ar symud rhwng tai a chymerodd staff gyfrifoldebau ychwanegol o fewn y cartref pan oedd prinder staff.
| “ | Felly, ie, pan nad oedd ganddyn nhw Covid, roedden nhw'n gallu cymysgu, yn amlwg, yn y tŷ fel arfer ond os oedd ganddyn nhw Covid, yna roedden nhw i, ryw fath, aros yn eu hystafelloedd gwely a byddem ni'n codi pethau gyda nhw ac yn gwneud hynny."
– Gweithiwr cymorth |
Ar ddechrau'r pandemig, roedd cyfyngiadau'n golygu nad oedd pobl ag anghenion gofal a chymorth yn gallu mynd allan i wneud eu gweithgareddau arferol a gweld eu teulu a'u ffrindiau. Clywsom sut roedd yr aflonyddwch ar eu harferion yn drysu pobl ag anghenion gofal a chymorth. Dywedodd gweithwyr cymorth wrthym sut roeddent yn trefnu gweithgareddau ac yn darparu mwy o gefnogaeth emosiynol i gysuro'r bobl yr oeddent yn gofalu amdanynt. Wrth i gyfyngiadau'r pandemig lacio, aeth gweithwyr cymorth â phobl ag anghenion gofal a chymorth ar deithiau cerdded rheolaidd, a helpodd i gefnogi eu lles.
| “ | Fe wnaethon ni ddarparu cefnogaeth emosiynol, rhyw fath, er mwyn iddyn nhw deimlo'n gyfforddus gyda phopeth oedd yn digwydd oherwydd roedd hi'n rhyfedd iawn iddyn nhw ein gweld ni gyda masgiau ymlaen a gwybod bod firws allan yna, felly yn amlwg, roedden nhw'n eithaf pryderus. Ac yna, o ddydd i ddydd, yn amlwg pan na allent fynd allan, gorfod dod o hyd i weithgareddau mewnol iddyn nhw eu gwneud a cheisio eu diddanu cymaint â phosibl.”
– Gweithiwr cymorth |
Cymerodd uwch staff a rheolwyr gyfrifoldebau ychwanegol, a oedd yn cynnwys cyfleu canllawiau a chyfyngiadau i wahanol dimau, rhoi'r wybodaeth ddiweddaraf i bobl ag anghenion gofal a chymorth a'u teuluoedd a gweithredu mesurau rheoli heintiau. Dywedodd un rheolwr wrthym pa mor anodd oedd hi i gael y wybodaeth ddiweddaraf am y canllawiau diweddaraf. Yn benodol, roedd y canllawiau'n wahanol i'r rhai mewn cartrefi gofal a'r rhai oedd yn byw mewn cartrefi gofal oherwydd sut roeddent yn cael eu rheoleiddio.
| “ | Roedd canllawiau eithaf clir ar ymweld â lleoliadau gofal a chartrefi gofal ac yn amlwg, ar y dechrau cafodd y cyfan ei grwpio o dan un canllaw ac yna, yn y pen draw, fe wnaethon nhw ei rannu. Felly, byddai gennym gartrefi gofal a lleoliadau byw â chymorth sy'n darparu gofal 24 awr. Felly, yna roedd yn rhaid i ni ddehongli rhwng gwahanol fathau o reoliadau a chanllawiau.”
– Cyfarwyddwr |
Teimlai gweithwyr cymorth fod natur eu rolau wedi aros yr un fath i raddau helaeth, ond bod yn rhaid iddynt ymgymryd â mwy o dasgau mewn rhai meysydd o'u gwaith. Er enghraifft, er y byddent fel arfer wedi gwneud y glanhau gyda phreswylwyr, yn ystod y pandemig roedd ganddynt brotocolau hylendid llymach a mwy rheolaidd i geisio atal haint. Roedd hyn yn golygu bod yn rhaid i staff wneud mwy o lanhau eu hunain. Yn yr un modd, yn hytrach na mynd ag unigolion allan i siopa bwyd wythnosol, roedd yn rhaid i staff wneud hyn ar eu pen eu hunain.
| “ | Yn y bôn, mwy o lanhau. Roedd yn gyson, fel, bob awr mae'n debyg, yn gwneud yr holl ddolenni drysau, switshis golau.”
– Gweithiwr cymorth |
| “ | Doedd e ddim yn rhy ddrwg, na, doedd e ddim yn gwneud llawer o wahaniaeth mewn gwirionedd, ar yr ochr ychwanegol -, yn amlwg, roedd yn fwy o lanhau ond yna doedden ni ddim yn mynd allan cymaint, felly doedd e, rhyw fath, ddim yn ormod o broblem, ie.”
– Gweithiwr cymorth |
Effaith ar y rhai sy'n darparu ac yn derbyn gofal
Roedd prinder staff yng nghyfnodau cynnar y pandemig oherwydd gofynion gwarchod ac ynysu. Cynyddodd hyn lwythi gwaith y staff sy'n weddill, gan eu rhoi dan straen. Mewn cyfnodau o brinder sylweddol, roedd staff weithiau'n cael eu rhannu rhwng dau leoliad gwahanol (cartrefi gofal cofrestredig a thai byw â chymorth). Fodd bynnag, er mwyn lleihau'r risg o drosglwyddo, ceisiodd y darparwr gyfyngu ar symud rhwng lleoliadau ac yn lle hynny roedd yn dibynnu ar oramser neu lefelau staffio is (pan oedd yn ddiogel ac yn ganiataol) i lenwi'r bylchau hyn. Gadawodd hyn staff yn teimlo'n flinedig ac wedi'u disbyddu.
| “ | Byddai [prinder] yn golygu bod staff eraill yn codi llwythi o sifftiau, cryn dipyn o oramser ac yna byddech chi'n blino'n fawr ac wedi'ch draenio'n emosiynol ac yn feddyliol.”
– Gweithiwr cymorth |
Roedd y rhai ag anghenion gofal yn ei chael hi'n anodd addasu i'r cyfyngiadau. Clywsom sut roedd yr aflonyddwch ar drefn arferol a'r diffyg strwythur yn gadael preswylwyr yn teimlo'n unig, yn ddiflas ac yn bryderus. Roedd pobl ag anghenion gofal a chymorth yn colli eu gweithgareddau arferol a'u rhyngweithiadau â'u gweithwyr cymorth, ffrindiau ac anwyliaid. Dywedodd un cyfrannwr wrthym sut y byddai staff weithiau'n dod i eistedd yn eu hystafell i gadw cwmni iddynt.
| “ | Weithiau bydden ni’n arfer gwylio ffilm yn fy ystafell wely, aelod o staff [a minnau]. Roedd ganddyn nhw’r mwgwd ymlaen, dw i’n cofio. Oherwydd roeddwn i eisiau ychydig o gwmni ar y pryd oherwydd fy mod i braidd yn unig yn fy ystafell wely, ar fy mhen fy hun. Oherwydd roeddwn i eisiau siarad â rhywun.”
– Person sydd ag anghenion gofal a chymorth |
Roedd staff yn ei chael hi'n anodd esbonio i bobl ag anghenion gofal a chymorth pam na allent barhau i fyw eu bywydau beunyddiol.
| “ | Dw i'n meddwl ei fod yn dipyn o sioc i rai ohonyn nhw i ddechrau. Roedd yn rhaid iddyn nhw addasu eu harferion, addasu'r hyn roedden nhw'n ei wneud o ddydd i ddydd, eu gweithgareddau ac i rai, roedden nhw'n cael hynny'n eithaf anodd. Mae llawer o'n pobl ni ar y sbectrwm awtistig, felly maen nhw wedi arfer â'r cyfarwyddyd hwnnw a, 'Ar ddydd Mercher dw i'n mynd yma ac dw i'n gwneud hyn.' ac ati, felly, roedd eu helpu nhw i ddeall beth sy'n digwydd yn y byd ar hyn o bryd yn anodd.”
– Cyfarwyddwr |
Roedd preswylwyr nad oeddent yn rhyngweithio cymaint ag eraill cyn y pandemig yn teimlo eu bod wedi cael llai o effaith gan gyfyngiadau'r pandemig. Dywedodd un person ag anghenion gofal a chymorth wrthym nad oeddent yn teimlo'n ofnus, eu bod wedi parhau â bywyd ac wedi cadw eu hunain yn brysur gyda glanhau.
| “ | Fy iechyd meddwl, o, mae'n wych. Mae fy iechyd meddwl yn wych ac rwyf bob amser mor brysur y tu mewn i'r adeilad, fel mynd â'r ailgylchu allan, sbwriel allan. Rwyf wedi bod yn gwneud hynny ers 6 mlynedd bellach.”
– Person sydd ag anghenion gofal a chymorth |
Clywsom hefyd enghreifftiau o sut roedd bod mewn tŷ gyda'r un bobl am gyhyd yn gwaethygu gwrthdaro personoliaeth presennol ac yn achosi tensiynau. Roedd pobl ag anabledd dysgu yn ei chael hi'n anodd deall newidiadau, gan eu gadael yn teimlo'n bryderus ac dan straen, a fyddai'n aml wedyn yn sbarduno dadleuon ac anghytundebau eraill gyda'r rhai sy'n byw yn y tŷ.
| “ | Roedden nhw'n teimlo'n emosiynol iawn. Dryslyd iawn. Doedden nhw ddim yn deall pam roedd yn rhaid iddyn nhw wisgo mwgwd, na pham roedd yn rhaid iddyn nhw gadw pellter cymdeithasol…os oedd un, fel, dan straen, neu oddi ar ei linell sylfaen, byddai'n gwrthwynebu'r llall a bydden nhw'n dod yn dan straen. Yna roedd hi'n ymwneud â cheisio eu tawelu a phethau felly.”
– Gweithiwr cymorth |
Daeth rhai pobl ag anghenion gofal a chymorth yn fwyfwy ynysig er mwyn osgoi'r sefyllfaoedd hyn. Dywedodd un cyfrannwr wrthym sut y byddent yn aros yn eu hystafell er mwyn osgoi eraill yn y tŷ.
| “ | Arhosais yn yr ystafell wely, cadwais i ffwrdd o'r ddau ddyn. Arhosais yn yr ystafell wely, fel, yn glanhau.”
– Person sydd ag anghenion gofal a chymorth |
Er gwaethaf yr heriau hyn, sylwodd staff ar ostyngiad yn nifer cyffredinol y digwyddiadau ymddygiadol wrth i'r pandemig fynd rhagddo. Er bod y bobl ag anghenion gofal a chymorth yn teimlo'n bryderus ac yn unig oherwydd y cyfyngiadau, roeddent hefyd yn wynebu llai o heriau o'r byd y tu allan. Yn ddiweddarach yn y pandemig, pan ddechreuodd cymdeithas agor eto, roedd llawer o bobl ag anabledd dysgu yn teimlo'n ansefydlog. Mae eu profiad pandemig yn parhau i gael effaith barhaol ar eu rhyngweithiadau â'r byd y tu allan.
| “ | Yna gwelsom gynnydd sydyn mewn digwyddiadau a phobl yn anesmwyth oherwydd, unwaith eto, newid mawr arall ac roedd gorfod ailgyflwyno pethau i bobl nad oeddent wedi'u gwneud ers cyhyd yn anodd. Felly, cymerodd hynny amser ac i lawer o unigolion, nid yw eu lefelau gweithgaredd yn dal i fod ar lefelau cyn y pandemig oherwydd unwaith eto, collwyd llawer o weithgareddau yn ystod y cyfnod hwnnw, collwyd llawer o adnoddau cymunedol. Felly, mae llawer o bethau a wnaethant cyn y pandemig wedi newid neu wasgaru neu ni ddechreuodd mewn gwirionedd. Felly, ie, mae'n dal i ail-grynhoi, ie.”
– Cyfarwyddwr |
Astudiaeth achos 5: Gofalu am bobl â chyflyrau iechyd meddwl hirdymor yn ystod y pandemig
Cefndir
Ymwelsom â chartref gofal preswyl yn ne-orllewin Lloegr, sy'n cynnig cefnogaeth i bobl 18 i 65 oed â chyflyrau iechyd meddwl hirdymor. Mae'n gartref bach, gyda llai na deg o breswylwyr a thîm bach o weithwyr cymorth sy'n cynnig gofal a chefnogaeth 24 awr y dydd. Mae gan bob preswylydd ei ystafell ei hun, gydag ystafelloedd ymolchi cymunedol a mannau byw a rennir i bobl gymdeithasu.
Newidiadau mewn gofal a heriau sy'n gysylltiedig â'r pandemig
Fel cartref bach gyda rhai preswylwyr nad oeddent yn deall yr angen am gyfyngiadau, roedd addasu i'r pandemig yn heriol. Disgrifiodd y staff pa mor anodd oedd gweithredu rheolau a chyfyngiadau yn eu lleoliad.
| “ | Roeddwn i'n gallu gweld pam eu bod nhw ar waith. Roedd eu rhoi ar waith yma gyda chleientiaid oedd yn ei chael hi'n anodd derbyn y wybodaeth yn llawn, neu o leiaf dderbyn y wybodaeth yn gyson, yn wastraff amser mewn gwirionedd. Doedd ceisio cloi'r llawr neu atal pobl rhag mynd i mewn ac allan pan oedden nhw'n teimlo'n sâl, ddim yn gallu ei wneud. Ie, doedd e ddim yn digwydd yma, ddim mewn gwirionedd.”
– Gweithiwr cymorth |
Roedd maint a chynllun y tŷ yn ei gwneud hi'n anodd gorfodi cadw pellter corfforol. Er enghraifft, roedd ystafelloedd ymolchi cymunedol yn golygu ei bod hi'n anodd cadw preswylwyr ar wahân. Yn hytrach na cheisio gorfodi ynysu, parhaodd staff a phreswylwyr i ryngweithio o fewn y tŷ, gan lynu wrth reol pellter o un metr yn bennaf pan oedd hynny'n bosibl.
| “ | Oedd, roedd hi'n anodd oherwydd mai tŷ bach yw hwn ac mae llwyth o bobl yma…roedd bron yn amhosibl gweithredu'r rheol dau fetr y rhan fwyaf o'r amser. Dim ond pan oedd rhywun yn dangos symptomau [Covid] y byddem ni, wyddoch chi, yn ei gweithredu go iawn. Gwnaethom ein gorau, ond roedd hi'n anodd…Mae'r cleientiaid bob amser eisiau dod i mewn i'r swyddfa yma oherwydd dyma ganolbwynt y tŷ, wyddoch chi, dydyn nhw ddim eisiau teimlo'n ynysig. Maen nhw eisiau rhyngweithio ac mae'n swyddfa fach, felly roedd hi'n anodd ei gadw ar ddau fetr. Byddai tua metr, ie.”
– Gweithiwr cymorth |
Roedd gan y cartref dîm staff bach felly roedd prinder staff yng nghyfnodau cynnar y pandemig yn aml yn broblemus. Clywsom faint o'r gweithwyr cymorth a adawodd oherwydd eu bod yn agored i niwed ac yn gwarchod eu hunain neu oherwydd eu bod yn poeni am ddal Covid-19.
| “ | Roedd hi'n anodd iawn cadw staff. Mae fel, roedd gennym ni rywun, aeth hi'n sâl ar unwaith oherwydd nad oedd hi eisiau cymryd y risg, felly roedd hi'n sâl, ar salwch hirdymor.”
– Rheolwr cofrestredig |
Mewn ymateb, fe wnaethon nhw geisio defnyddio staff asiantaeth a banc am y tro cyntaf. Fodd bynnag, roedd anawsterau parhaus i ddod o hyd i staff gan fod cymaint o alw gan ddarparwyr gofal eraill.
| “ | Doedden ni erioed wedi gorfod defnyddio staff asiantaeth o'r blaen ac fe wnaethon ni, roedd angen i ni ddefnyddio staff asiantaeth oherwydd nad oedd gennym ni staff, ond doedd dim staff asiantaeth. Ni chawsom un shifft wedi'i chyflenwi gan asiantaeth oherwydd nad oedd ganddyn nhw staff.”
– Rheolwr cofrestredig |
Yng nghyfnodau diweddarach y pandemig, roedd rhai staff yn anghyfforddus gyda gofynion brechu gorfodol yn y gweithle a arweiniodd at fwy o staff yn gadael.
| “ | Y brechu gorfodol ymhlyg; 'Byddwch yn colli eich swydd os na chewch eich brechu a chael 2 bigiad'. Doedd hynny ddim yn cael ei werthfawrogi o gwbl. Collon ni gwpl o aelodau staff oherwydd hynny.”
– Gweithiwr cymorth |
Effaith ar y rhai sy'n darparu ac yn derbyn gofal
Ni chafodd y cartref unrhyw achosion o Covid-19 tan lawer yn ddiweddarach yn y pandemig. Roedd hyn yn golygu eu bod yn rhyngweithio fel arfer yn y cartref yn ystod y rhan fwyaf o'r cyfnodau clo. Er hynny, roedd y cyfyngiadau'n dal i gael effeithiau sylweddol ar y gweithlu a'r preswylwyr.
Cafodd prinder staff effaith enfawr ar y tîm, gan greu pwysau a chynyddu llwythi gwaith. Dywedodd gweithwyr cymorth wrthym sut roedden nhw weithiau'n gweithio hyd at dri diwrnod yn syth oherwydd nad oedd ganddyn nhw'r staff i orchuddio sifftiau. Gadawodd hyn nhw'n teimlo dan straen ac wedi blino'n lân.
| “ | Llosgi allan a straen yn bennaf. Ie, oherwydd roedden ni i gyd yn gweithio cymaint o sifftiau. Yna byddai rhywun yn mynd yn sâl gyda Covid, yn methu dod i mewn am gyfnod hir, neu'n mynd yn sâl a pheidio â dod i mewn am gyfnod hir. Felly, ie, roedd yna lawer o bwysau.”
– Gweithiwr cymorth |
Dywedodd staff wrthym eu bod yn teimlo nad oeddent yn cael cefnogaeth fawr gan uwch reolwyr ac nad oeddent yn barod ar gyfer yr heriau yr oeddent yn eu hwynebu. Er bod gweithwyr cymorth yn gweithio goramser, ychydig iawn o gymorth a gynigiwyd gan y rheolwyr, gan eu gadael yn teimlo'n ynysig ac wedi'u gadael. Dywedasant fod maint bach y sefydliad wedi cyfrannu at hyn.
| “ | Wyddoch chi, byddai gennym ni hysbyseb allan, ni fyddai neb yn gwneud cais. Roedden ni'n gweithio ar eu holl sifftiau. Doedden ni ddim yn gallu cael staff banc ac rwy'n credu, yn y diwedd, ie, doedden nhw [y rheolwyr] ddim yn gwybod beth i'w wneud mewn gwirionedd ac roedden nhw'n dal i'n twyllo ni ac yn dal i ddweud, 'O, dwi'n gwybod, mae ym mhobman, mae'n digwydd ym mhobman. O diar, wel, rydyn ni'n ddiolchgar iawn', wyddoch chi, a dyna oedd eu hymateb am oesoedd ... wnaeth ein rheolwr ar y pryd ddim un sifft ychwanegol.”
– Rheolwr cofrestredig |
Roedd staff yn poeni am effaith y prinderau hyn ar ansawdd y gofal y gallent ei ddarparu i breswylwyr.
| “ | Oedd, roedd yn eithaf llawn straen, eithaf llawn straen gyda llosgi allan, roedd yn rhaid i chi fod yn ymwybodol o hynny oherwydd yna mae hynny'n adlewyrchu sut rydych chi'n delio â'r cleientiaid hefyd a pha mor hir allwch chi barhau i'w wneud dros gyfnod o amser yn ddiogel.
– Gweithiwr cymorth |
Roeddent yn teimlo bod preswylwyr yn gyffredinol wedi ymdopi'n dda drwy gydol y pandemig, er bod rhai wedi ynysu eu hunain yn eu hystafell oherwydd ofn. Addasodd llawer, a oedd yn aml eisoes wedi bod ar wahân yn gymdeithasol cyn y pandemig, i'r cyfyngiadau yn eithaf cyflym.
| “ | Nawr ein bod ni’n siarad amdano, rwy’n synnu nad oedd y peth cyfan, y PPE, y profion, Covid yn gyffredinol, wedi effeithio’n fawr ar y bobl hyn. Os oes unrhyw beth, mae wedi eu gwneud yn fwy gwydn.”
– Gweithiwr cymorth |
| “ | Siaradais i ag un o'r dynion a ddywedodd, iddo fe, nad oedd yn effeithio arno o gwbl. Mae'n gymdeithasol ynysig iawn beth bynnag, mae symptomau ei salwch yn golygu ei fod yn encilgar iawn ac felly nid yw'n cymryd rhan mewn cymdeithas yn y ffordd honno beth bynnag. Felly, iddo fe, nid oedd unrhyw newid, felly dywedodd nad oedd yn effeithio arno o gwbl ac rwy'n credu bod hynny'n wir, i ryw raddau, gan y rhan fwyaf o'r cleientiaid, oherwydd natur gronig eu salwch a'u symptomau, maen nhw'n teimlo'n eithaf, braidd, wedi'u tynnu oddi wrtho beth bynnag ond rwy'n credu ei fod hefyd yn frawychus i rai ohonyn nhw. Felly, mae fel, syndod yw'r mwyaf cadarnhaol ac yna ychydig yn ofnus.
– Rheolwr cofrestredig |
Felly parhaodd llawer o drigolion â'u trefn arferol. Esboniodd y staff, oherwydd natur cyflyrau iechyd meddwl y trigolion, mai dim ond cymaint y gallent ei wneud i orfodi cyfyngiadau.
| “ | Fe wnaethon ni geisio dro ar ôl tro i wneud pethau i bobl, siopa i bobl a cheisio eu cadw nhw yma. Yn y diwedd, fe wnaethon nhw, i ryw raddau, yr hyn roedden nhw eisiau ei wneud. Ac roedd hynny'n rhaniad 70/30, roedd gennym ni bobl oedd yn mynd allan bob dydd yn llythrennol. Bydden nhw'n dilyn eu harferion beth bynnag. Felly, doedd dim llawer o bwynt cael eich cythruddo na'ch poeni ganddo, dim ond cymaint o wybodaeth y gallem ei rhoi i chi dro ar ôl tro. Ie, doedd gan [y pandemig] ddim effaith enfawr, mae'n debyg.”
– Gweithiwr cymorth |
Roedd un preswylydd y siaradon ni ag ef yn mwynhau pa mor dawel oedd y strydoedd yn ystod y cyfnod clo. Creodd hyn amgylchedd mwy heddychlon gyda llai o sbardunau allanol, gan leihau straen a phryder.
| “ | Roedd mor dawel. Roedd yn llawenydd pan dreulioch chi'r awr neu ddwy honno [y tu allan].”
– Person sydd ag anghenion gofal a chymorth |
Astudiaeth achos 6: Darparu gofal canolradd mewn cartref nyrsio yng Ngogledd Lloegr
Cefndir
Siaradom â staff a phreswylwyr o gartref nyrsio yng Ngogledd Lloegr. Mae'n gartref bach, preifat sy'n cynnig gofal preswyl a nyrsio i bobl hŷn â chyflyrau corfforol a gwybyddol. Mae'n cynnig cefnogaeth i'r rhai sy'n byw gyda dementia, cyflyrau iechyd meddwl ac anableddau corfforol, gyda'r rhan fwyaf o breswylwyr yn derbyn gofal nyrsio.
Newidiadau mewn gofal a heriau sy'n gysylltiedig â'r pandemig
Ar ddechrau'r cyfnod clo, rhannwyd y cartref yn dair parth yn seiliedig ar system raddio RAG (coch, ambr, gwyrdd) a oedd yn adlewyrchu presenoldeb neu risg achosion Covid-19. Roedd gan bob parth ei dîm ei hun o weithwyr gofal a gweithwyr tŷ. Os oedd angen i aelod o staff fynd i mewn i'r parth coch yn ystod eu shifft, byddent yn aros yno tan ddiwedd eu shifft i leihau'r risg o drosglwyddo. Oherwydd nifer gyfyngedig y nyrsys (gyda dwy ar shifft dydd ac un yn y nos), nhw oedd yr unig aelodau o staff a ganiatawyd iddynt symud rhwng parthau.
| “ | Felly, roedd gennym ni dair parth: y parth gwyrdd ar gyfer pobl oedd yn asymptomatig ac wedi profi'n negatif, yr ambr ar gyfer y bobl a allai fod wedi cael y cyflwr, neu roedden ni'n aros am ganlyniad Covid ar eu cyfer ac yna [y coch ar gyfer] y rhai oedd yn bositif ac yn symptomatig…Felly, roedd chwe gofalwr a dau ym mhob parth ond, gyda'r tîm nyrsio, gyda'r rowndiau meddyginiaeth a, wyddoch chi, eich holl ddyletswyddau nyrsio roedd yn rhaid i ni symud rhwng y parthau a oedd yn peri pryder ond roedd yn angenrheidiol.”
– Nyrs sy'n gweithio mewn cartref gofal |
Yng nghyfnodau cynnar y pandemig, cafodd yr holl breswylwyr eu hynysu i'w hystafelloedd. Daethpwyd â gweithgareddau cymunedol ac ymweliadau i ben a chafodd prydau bwyd eu danfon yn unigol. Wrth i'r cyfyngiadau lacio, roedd preswylwyr yn gallu rhyngweithio ag eraill yn eu parth gan gynnal pellter o ddau fetr. Ar yr adeg hon, caniatawyd i anwyliaid ymweld â phreswylwyr trwy ffenestr hefyd. Yna cyflwynwyd ymweliadau gardd â phellter cymdeithasol ac yng nghyfnodau diweddarach y cyfnod clo, adeiladodd y cartref fwth mewn coridor, gan ganiatáu i breswylwyr gofleidio eu hanwyliaid.
| “ | Dw i'n meddwl y gallen ni gael ymweliadau yn yr ardd, ond dw i'n cofio'r tywydd yn oer. Felly, roedd llawer ohonyn nhw wedi'u dosbarthu fel rhai rhy fregus mewn gwirionedd i eistedd allan ar ddiwrnod rhewllyd, dim ond i weld eu perthnasau. Felly, roedd llawer ohonyn nhw'n ei wneud trwy'r ffenestr, gyda'r intercom, ond, unwaith eto, problemau gyda chlyw, golwg ac nid oedd yr un peth â, wyddoch chi, paned braf o de a chwtsh.”
– Nyrs sy'n gweithio mewn cartref gofal |
Profiadau o ofal canolraddol
Yn ystod camau cynnar y pandemig, roedd y cartref hefyd yn darparu gofal canolraddol. Mae hyn yn cynnwys darparu cefnogaeth tymor byr i unigolion sy'n gadael yr ysbyty nad ydynt eto'n ddigon da i ddychwelyd adref.
Roedd hyn yn golygu bod y cartref wedi derbyn nifer fawr o gleifion a gafodd eu rhyddhau o'r ysbyty. Dywedodd y staff wrthym sut roedden nhw'n teimlo pwysau ychwanegol i dderbyn pobl ac yn aml yn cael gwybodaeth anghywir am eu rhyddhau, gan dderbyn cleifion a gafodd eu rhyddhau â mwy o anghenion nag a ddisgwyliwyd.
| “ | Mae gen i'r ddau wely bob amser, felly roedd gen i welyau gofal canolradd a gwelyau cyffredin…mae gofal canolradd yn cael ei redeg gan y GIG a'r ysbyty ac maen nhw'n talu am y gwelyau, mae'n archeb bloc, bron. Dw i'n meddwl eu bod nhw'n teimlo bod ganddyn nhw fwy o rym i ddweud, 'Byddwch chi'n cymryd y person hwn', ac i beidio â gwneud dim byd pan aeth pethau o'i le.”
– Cyfarwyddwr |
Roedd staff yn y cartref hefyd yn bryderus ynghylch pa mor dda yr oedd protocolau profi yn cael eu dilyn mewn ysbytai ac yn teimlo bod rhai cleifion yn cael eu rhyddhau er mwyn rhyddhau gwelyau ar wardiau ysbytai.
| “ | Wel, cawson ni bedwar achos mewn deuddeg mis, ym mhob achos, roedd fy nghlaf mynegai wedi cael ei dderbyn o'r ysbyty, gyda phrawf negyddol yn ôl pob sôn ac wedi datblygu Covid mewn 48 awr. Mae'n ddrwg iawn gen i, mae'n ddrwg iawn gen i, fy nghwestiwn yw, a oedden nhw'n gwybod sut i brofi? Oedden nhw'n ei wneud yn iawn?”
– Cyfarwyddwr |
Rhannodd y wraig tŷ sut roedd y cartref yn gweithredu'n effeithiol fel ward Covid-19 gorlif i'r GIG.
| “ | Roedden ni'n wahanol bryd hynny oherwydd fe wnaethon ni agor fel rhwyd i gymryd cleifion y GIG, fe wnaethon ni agor fel ward Covid y GIG. Felly, fe wnaethon ni gymryd pobl â Covid o'r GIG draw i fan hyn. Felly, fel eu ward gorlifo.”
– Cadwr tŷ |
Effaith ar y rhai sy'n darparu ac yn derbyn gofal
Cafodd gwybodaeth anghywir am ryddhau'r rhai a drosglwyddwyd i gyfleusterau gofal canolraddol y cartref effeithiau sylweddol ar y gweithlu a diogelwch preswylwyr eraill. Clywsom sut y cafodd yr achos cyntaf yn y cartref ei achosi gan unigolyn a adroddwyd ei fod yn ansymudol ac yn profi'n negatif am Covid-19. Fodd bynnag, yn ddiweddarach y noson honno fe'i canfuwyd yn crwydro'r coridorau ac wedi hynny cafodd yr holl breswylwyr ar y coridor hwnnw eu heintio.
| “ | Cyrhaeddodd y dyn hwn yn hwyr, ar ôl yr amser torri i ffwrdd, a helpodd fy nyrs nos ef i'r gwely, roedd yn ymddangos ei fod wedi codi ar ei draed, roedd yn rhaid i ni ei godi i'r gwely a dwy awr yn ddiweddarach, cafodd ei ddarganfod yn eistedd ar wely rhywun arall yn ceisio yfed ei sudd hi a chael sgwrs hir gyda hi ac roedd wedi bod ym mhob ystafell wely ar hyd y coridor hwnnw. Mae'r dyn hwn i fod ...
– Cyfarwyddwr |
Rhoddodd yr achosion hyn bwysau enfawr ar staff yn y cartref. Roedd monitro cleifion newydd a allai beryglu diogelwch preswylwyr presennol yn cynyddu llwythi gwaith ac yn gadael bylchau yn y gefnogaeth. Siaradodd staff hefyd am y cyfnodau rhybudd byr cyn derbyn cleifion a ryddhawyd, gan ddarganfod ar y diwrnod yn aml. Fodd bynnag, dim ond unigolion os oedd ganddynt ystafell yn barod y byddent yn eu derbyn.
| “ | Ydw, dw i'n meddwl ei fod yn fyr rybudd, efallai y bydden ni'n cael gwybod y bore hwnnw, ond dim ond os oes gennym ni ystafell y bydden ni'n ei dderbyn."
– Cadwr tŷ |
Cafodd cyfyngiadau ar symud o fewn y cartref yng nghyfnodau cynnar y pandemig wahanol effeithiau ar breswylwyr yn dibynnu ar eu hanghenion gofal. I rai, roedd gorfod aros yn eu hystafell yn effeithio ar eu lles a'u hiechyd meddwl gan eu bod yn teimlo mor unig. Rhannodd staff yr heriau o dawelu meddyliau preswylwyr a oedd yn teimlo'n ddryslyd ac ynysig.
| “ | Yn feddyliol, rwy'n cofio llawer ohonyn nhw'n dweud, 'Pa ddiwrnod yw hi?' Oherwydd eu bod nhw wedi bod yn yr un ystafell am x nifer o ddyddiau ac roedden nhw wedi colli amserlen gyfan, dim ond pa ddiwrnod oedd hi, pa amser oedd hi. A dywedodd llawer ohonyn nhw eu bod nhw'n teimlo wedi'u carcharu, sydd, mewn ffordd, mae'n debyg eu bod nhw, ond, er eu diogelwch eu hunain. Felly, ie, iechyd meddwl i mi, roedd ceisio eu tawelu yn her anodd.”
– Nyrs sy'n gweithio mewn cartref gofal |
Fodd bynnag, cafodd preswylwyr ag anghenion gofal uwch eu heffeithio llai gan y cyfyngiadau hyn. Myfyriodd sawl cyfrannwr ar sut nad oedd gan bobl ag anghenion gofal a chymorth ddewis yn aml ynghylch a allent adael eu hystafelloedd hyd yn oed cyn y pandemig gan fod angen cymorth arnynt i godi o'r gwely a symud o gwmpas.
| “ | Dydy hi ddim yn gallu codi o'r gwely, wyddoch chi, mae'n rhaid iddyn nhw ei chael hi allan, ond yn amlwg wnaethon nhw ddim ei chymryd hi allan a'i symud hi drosodd na beth bynnag.”
– Anwylyd preswylydd cartref gofal |
| “ | Caeth i'r tŷ, caeth i'r ystafell, caeth i'r gwely, beth bynnag, alla i ddim codi o gwbl oherwydd alla i ddim plygu fy ngliniau na dim byd felly, felly [dw i] yn y gwely drwy'r amser.”
– Person sydd ag anghenion gofal a chymorth |
Yr effaith anoddaf i breswylwyr oedd methu gweld eu hanwyliaid. Rhannodd gŵr un preswylydd, a oedd yn gaeth i'w wely ac ag anawsterau lleferydd yn dilyn strôc, yr effaith sylweddol o deulu ddim yn gallu ymweld â'i wraig, yn enwedig ar ba mor unig yr oedd hi'n teimlo. Cyn y pandemig, byddai'n ymweld am 4-5 awr y dydd ac yn bwydo cinio iddi ac roedd yn teimlo ei bod hi'n colli'r gefnogaeth hon yn ystod y cyfnod clo.
| “ | Dw i'n meddwl mai dyna'r prif beth, roedd hi'n colli ni'n dod i fyny…pan oedden ni'n arfer dod, pan ddechreuon ni ddod i fyny gyntaf, y blynyddoedd cyntaf hynny, roedden ni yma efallai 4, 5 awr y dydd. Bydden ni'n rhoi cinio iddi, yna bydden ni'n rhoi te iddi.”
– Anwylyd preswylydd cartref gofal |
Clywsom sut roedd preswylydd arall â chlefyd Parkinson a dementia datblygedig yn ei chael hi'n anodd addasu ar ôl symud i mewn yn ystod y pandemig ac yn colli ei anwyliaid yn fawr. Dywedodd ei wraig wrthym sut y ceisiodd redeg i ffwrdd o'r cartref sawl gwaith a bu'n rhaid ei ddwyn yn ôl.
| “ | Daliodd ati i ddweud ei fod eisiau dod adref ac fe aeth allan unwaith neu ddwywaith mewn gwirionedd. Wel, roedd y rheolwr ar y pryd yn meddwl ei fod wedi cofio'r rhif ar y drws i fynd allan. Dwi ddim yn meddwl ei fod wedi gwneud mewn gwirionedd ond, beth bynnag, fe aeth allan a chyrraedd y siop i fyny'r stryd a cheisio mynd adref. Ac fe wnaeth hynny ddwywaith, ceisiodd fynd adref. Felly, roedd hynny braidd yn dorcalonnus.”
– Anwylyd preswylydd cartref gofal |
Dywedodd staff wrthym am y pryder ychwanegol yr oeddent yn ei deimlo am lesiant preswylwyr a'r pwysau i ddarparu cefnogaeth yn lle eu hanwyliaid. Gadawodd yr anawsterau o gydbwyso'r gefnogaeth emosiynol hon â'u rolau beunyddiol iddynt deimlo'n flinedig yn emosiynol ac yn gorfforol.
| “ | Roedd cyfnod lle aethon ni i gyfnod clo ac roedd yr holl breswylwyr yn eu hystafelloedd am gryn dipyn o amser. Ac rwy'n cofio mynd o gwmpas ac roedd rhai o'r preswylwyr mor falch o'ch gweld chi ac eisiau cael sgwrs. Ond roeddech chi'n gwybod yn isymwybodol fod amser yn…brin a bod gennych chi'r holl swyddi hyn i'w gwneud. Felly, roeddech chi'n teimlo'n rhwygo rhwng eu tawelu a'u heistedd gyda nhw oherwydd mai chi yw'r unig berson maen nhw wedi'i weld ers tro. Ond, yna'n amlwg, eich swydd chi hefyd o allu rhoi meddyginiaethau ar amser, rhwymynnau a'r holl swyddi arferol eraill yr oedd yn rhaid i chi eu gwneud. Felly, ie, roedd yn flinedig yn gorfforol ac yn feddyliol, dim ond oherwydd eich bod chi wedi'ch gwasgaru'n denau.”
– Nyrs sy'n gweithio mewn cartref gofal |
Fodd bynnag, roeddent yn teimlo bod y cyfyngiadau ar ymweld yn cael llai o effaith ar breswylwyr oedd yn hen iawn neu a oedd ag anghenion gofal uwch, oherwydd bod ganddynt lai o ddealltwriaeth o'r hyn oedd yn digwydd.
| “ | Mae'n rhyfedd oherwydd eu bod nhw'n adnabod ein hwynebau, maen nhw'n gwybod pryd rydyn ni wedi cael diwrnod i ffwrdd. Maen nhw wir yn gwybod. Nid pob un ohonyn nhw, ond maen nhw wir yn gwybod. Felly, maen nhw, mae'n debyg, yn dibynnu arnom ni am yr wyneb cyfeillgar yna i gerdded i mewn i'r ystafell oherwydd nad oedd ganddyn nhw i gyd eu hymwelwyr, wyddoch chi? ... Ond mae gennym ni'r henoed iawn, iawn. Dydyn nhw ddim i gyd yn cofio. Felly, dydyn nhw ddim yn dibynnu ar ein hwynebau, rhai ohonyn nhw, wyddoch chi?”
– Cadwr tŷ |
9 Atodiad
|
Cwmpas Modiwl 6
Mae Modiwl 6 yn ystyried amrywiaeth o faterion sy'n ymwneud â gwasanaethau gofal cymdeithasol i oedolion yn ystod pandemig Covid-19 yng Nghymru, Lloegr, yr Alban a Gogledd Iwerddon.
Defnyddiwyd cwmpas dros dro Modiwl 6 i arwain sut y gwnaethom wrando ar bobl a dadansoddi eu straeon. Amlinellir cwmpas y modiwl isod a gellir ei ganfod hefyd ar wefan Ymchwiliad Covid-19 y DU. yma.
Bydd y modiwl hwn yn archwilio effaith pandemig Covid-19 ar y sector gofal cymdeithasol i oedolion a ariennir yn gyhoeddus ac yn breifat (y “Sector Gofal”) yng Nghymru, Lloegr, yr Alban a Gogledd Iwerddon.
Bydd yn ystyried canlyniadau penderfyniadau’r llywodraeth ar y rhai sy’n byw ac yn gweithio yn y Sector Gofal. Mae hyn yn cynnwys gofal i oedolion a chartrefi preswyl gan gynnwys gofal a ddarperir yn y cartref (ond nid gofal a ddarperir mewn canolfannau gofal dydd neu mewn tai â chymorth). Mae hefyd yn cynnwys y penderfyniadau i ryddhau capasiti mewn ysbytai trwy ryddhau cleifion i gartrefi gofal i oedolion a chartrefi preswyl. Bydd yn mynd i’r afael â’r camau a gymerwyd mewn cartrefi gofal i oedolion a chartrefi preswyl i atal lledaeniad Covid-19 ac yn archwilio gallu’r sector gofal i oedolion i ymateb i’r pandemig. Bydd y modiwl hefyd yn ystyried effaith y pandemig ar dderbynwyr gofal a’u hanwyliaid a’r effaith ar staff sy’n gweithio yn y Sector Gofal.
Yn benodol, bydd y modiwl hwn yn archwilio:
- Effaith y pandemig ar brofiad pobl o'r Sector Gofal. Bydd hyn yn canolbwyntio ar y rhai sy'n derbyn gofal a'u hanwyliaid a'r rhai sy'n gweithio yn y Sector Gofal. Bydd yn cynnwys ystyried yr effeithiau anghyfartal arnynt.
- Strwythur y Sector Gofal a'r cyrff allweddol sy'n ymwneud â Gweinyddiaethau'r DU a'r Gweinyddiaethau Datganoledig ar ddechrau ac yn ystod y pandemig. Bydd hyn yn cynnwys lefelau staffio a chapasiti gwelyau yn union cyn y pandemig.
- Y penderfyniadau allweddol a wnaed gan Lywodraeth y DU a'r Gweinyddiaethau Datganoledig mewn perthynas â'r Sector Gofal, gan gynnwys y penderfyniadau sy'n ymwneud â rhyddhau pobl o ysbytai i gartrefi gofal oedolion a chartrefi preswyl yng nghyfnodau cynnar y pandemig.
- Rheoli'r pandemig mewn cartrefi gofal a phreswyl i oedolion. Bydd hyn yn cynnwys y mesurau sy'n atal lledaeniad Covid-19, megis mesurau atal a rheoli heintiau, profi am Covid-19, argaeledd a digonolrwydd offer amddiffynnol personol (PPE), cyfyngiadau ar fynediad gan/at weithwyr gofal iechyd proffesiynol ac ymweliadau gan anwyliaid.
- Defnyddio Peidiwch â Cheisio Adfywio Cardiopwlmonaidd (DNACPRs) a chyfathrebu â derbynwyr gofal a'u hanwyliaid am gyflwr a thriniaeth derbynnydd gofal gan gynnwys trafodaethau a phenderfyniadau am DNACPRs.
- Y newidiadau i'r cyfundrefnau arolygu rheoleiddiol o fewn y Sector Gofal.
- Marwolaethau sy'n gysylltiedig â haint Covid-19 gan gynnwys marwolaethau derbynwyr gofal a staff.
- Mesurau atal a rheoli heintiau ar gyfer y rhai sy'n darparu gofal yn y cartref, gan gynnwys gan ofalwyr di-dâl.
Sut roedd pobl yn rhannu eu stori gyda ni
Mae tair ffordd wahanol y gwnaethom gasglu straeon pobl ar gyfer Modiwl 6: ffurflen ar-lein, digwyddiadau gwrando a gwrando wedi'i dargedu sy'n cynnwys cyfweliadau manwl. Disgrifir pob un o'r rhain isod.
Ffurflen ar-lein
Gwahoddwyd aelodau'r cyhoedd i gwblhau a ffurflen ar-lein drwy wefan yr Ymchwiliad (cynigiwyd ffurflenni papur a rhif ffôn i’w ffonio i gyfranwyr hefyd ac ychwanegwyd nhw drwy’r ffurflen ar-lein i’w dadansoddi). Gofynnwyd iddynt ateb tri chwestiwn eang, agored am eu profiad o’r pandemig. Y cwestiynau hyn oedd:
- C1: Dywedwch wrthym am eich profiad
- C2: Dywedwch wrthym am yr effaith arnoch chi a phobl o'ch cwmpas
- C3: Dywedwch wrthym beth ydych chi'n meddwl y gellid ei ddysgu.
Gofynnodd y ffurflen gwestiynau demograffig eraill i gasglu gwybodaeth gefndirol amdanynt (megis eu hoedran, rhyw ac ethnigrwydd). Cyflwynwyd yr ymatebion i'r ffurflen ar-lein yn ddienw. Mae delwedd o'r ffurflen ar-lein wedi'i chynnwys isod.
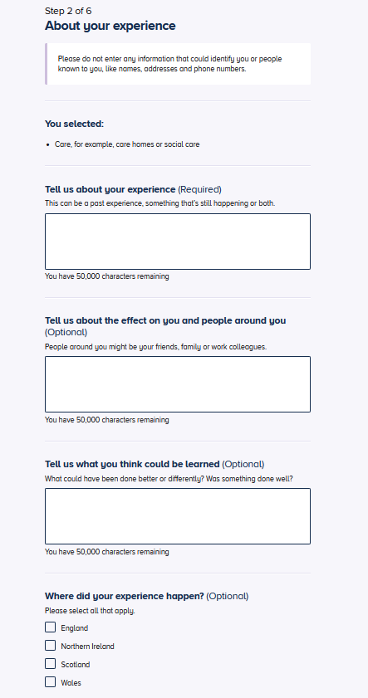
Ffigur 1: Ffurflen ar-lein
Yn ei natur, y rhai a gyfrannodd at y ffurflen ar-lein oedd y rhai a ddewisodd wneud hynny a dim ond yr hyn yr oeddent yn gyfforddus ag ef a rannasant.
Ar gyfer Modiwl 6, fe wnaethom gynnwys 46,485 o straeon yn ymwneud â Gofal Cymdeithasol. Mae hyn yn cynnwys 38,374 o straeon o Loegr, 3,775 o'r Alban, 3,870 o Gymru a 1,999 o Ogledd Iwerddon (roedd cyfranwyr yn gallu dewis mwy nag un genedl yn y DU yn y ffurflen ar-lein, felly bydd y cyfanswm yn uwch na nifer yr ymatebion a dderbyniwyd).
Digwyddiadau gwrando
Tîm Mae Pob Stori yn Bwysig teithiodd i 31 o drefi a dinasoedd ledled Lloegr, yr Alban, Cymru a Gogledd Iwerddon, i roi cyfle i bobl rannu eu profiad o’r pandemig yn bersonol yn eu cymunedau lleol. Cynhaliwyd digwyddiadau gwrando yn y lleoliadau canlynol:
- Carlisle
- Wrecsam a Rhuthun
- Newham
- Caerwysg
- Paisley
- Derry / Londonderry
- Middlesborough
- Enniskillen
- Bradford
- Sgegness
- Stockton-on-Tees
- Birmingham
- Milton Keynes
- Bournemouth
- Llandudno
- Blackpool
- Luton
- Folkestone.
Y tu hwnt i'r digwyddiadau wyneb yn wyneb hyn, cynhaliwyd sesiynau gwrando rhithwir hefyd lle'r oedd y dull hwnnw'n cael ei ffafrio. Gweithiodd Ymchwiliad Covid-19 y DU gyda llawer o elusennau a grwpiau cymunedol ar lawr gwlad i siarad â'r rhai yr effeithiwyd arnynt gan y pandemig mewn ffyrdd penodol. Mae hyn yn cynnwys gofalwyr â thâl a heb dâl, staff cartrefi gofal, defnyddwyr gwasanaeth a theuluoedd a gollodd eu bywydau yn ystod y pandemig.
Gwrando wedi'i dargedu sy'n cynnwys cyfweliadau manwl
Comisiynwyd consortiwm o arbenigwyr ymchwil gymdeithasol a chymunedol gan Every Story Matters i gynnal cyfweliadau manwl. Canolbwyntiodd y cyfweliadau hyn ar y Prif Linellau Ymholi (KLOEs) ar gyfer Modiwl 6.
At ei gilydd, cyfrannodd 336 o bobl ledled Lloegr (218), yr Alban (45), Cymru (36) a Gogledd Iwerddon (37) yn y ffordd hon rhwng Mehefin 2024 a Medi 2024. Mae hyn yn cynnwys 336 o gyfweliadau manwl gyda:
- Gweithlu gofal cymdeithasol (mewn cartrefi gofal ac yn darparu gwasanaethau gofal cartref)
- Gweithwyr gofal iechyd (megis nyrsys a chymdeithion nyrsio, ffisiotherapyddion, dietegwyr a pharafeddygon) a weithiodd yn agos gyda gwasanaethau gofal cymdeithasol i oedolion yn ystod y pandemig
- Gofalwyr di-dâl ac anwyliaid pobl ag anghenion gofal a chymorth
- Pobl ag anghenion gofal a chymorth (oedolion oedran gweithio a hŷn), gan gynnwys preswylwyr cartrefi gofal gyda a heb nyrsio a phobl sy'n derbyn gofal gartref gan ofal cartref neu ofal di-dâl (ffrindiau ac aelodau o'r teulu) yn ystod y pandemig.
Cynhaliwyd yr holl gyfweliadau manwl a grwpiau trafod gan ymchwilwyr hyfforddedig gan ddefnyddio canllawiau trafod strwythuredig. Datblygwyd canllawiau trafod penodol ar gyfer pob cynulleidfa, gan gynnwys pobl ag anghenion gofal, gofalwyr di-dâl ac anwyliaid, a'r gweithlu iechyd a gofal cymdeithasol. Cynlluniwyd y canllawiau trafod hyn i gwmpasu meysydd penodol o KLOEs Modiwl 6. Roedd hyn yn cynnwys:
- Profiad o'r pandemig; gan gynnwys trefniadau byw, trefniadau gofal ac effeithiau'r pandemig
- Profiadau o dderbyn gofal
- Profiadau o ddarparu gofal
- Rhyddhau o ysbytai i gartrefi gofal
- Mesurau atal a rheoli heintiau mewn cartrefi gofal a gofal cartref
- Profiadau o ofal diwedd oes a phrofedigaeth.
Lle bo angen, byddai ymchwilwyr yn holi cyfranwyr am ragor o wybodaeth am eu profiad. Roedd pob cyfweliad yn para hyd at 60 munud.
Mae cyfanswm y cyfranogwyr a adroddwyd uchod yn cynnwys y rhai a rannodd eu stori fel rhan o astudiaeth achos. Er mwyn clywed profiad pobl sy'n byw mewn cartrefi gofal, fe wnaethom ymweld â darparwyr gofal i siarad â phobl ag anghenion gofal a chymorth, staff ac anwyliaid. Rhoddodd y dull astudiaeth achos hwn gyfle hefyd i gael darlun cyfannol o'r profiadau mewn lleoliad o safbwyntiau lluosog. Cwblhawyd cyfanswm o 15 astudiaeth achos ledled Lloegr, yr Alban, Cymru a Gogledd Iwerddon.
Darperir rhagor o fanylion am ddadansoddiad niferoedd y samplau ar gyfer gwrando wedi'i dargedu yn nhablau 1 a 2 yn yr adran 'Niferoedd y samplau ar gyfer gwrando wedi'i dargedu ac astudiaethau achos'.
Ein dull o ddadansoddi straeon pobl
Cyfunwyd a dadansoddwyd y straeon a rannwyd gan bobl gan ddefnyddio'r ffurflen ar-lein, digwyddiadau gwrando a gwrando wedi'i dargedu i baratoi'r cofnod hwn. Mae profiadau a straeon o'r tair ffynhonnell ddata wedi'u cyflwyno gyda'i gilydd drwy gydol y cofnod i ddarparu un cyfrif thematig nad yw'n rhoi mwy o bwyslais i unrhyw un o'r ffynonellau. Er bod canfyddiadau o ddigwyddiadau gwrando wedi'u nodi, nid yw'r cofnod yn gwahaniaethu rhwng dyfyniadau a phrofiadau o'r ffurflen ar-lein a'r gwrando wedi'i dargedu. Roedd y themâu a ddaeth i'r amlwg ar draws y tair ffynhonnell yn gyson. Yma rydym yn disgrifio'n fanylach y dulliau penodol a ddefnyddiwyd i ddadansoddi straeon o bob ffynhonnell.
Ffurflen ar-lein
Dadansoddwyd yr ymatebion o'r ffurflen ar-lein drwy broses o'r enw prosesu iaith naturiol (NLP), sydd yn defnyddio dysgu peirianyddol i helpu i drefnu data testun rhydd (yn yr achos hwn yr ymatebion a ddarperir ar y ffurflen ar-lein) mewn ffordd ystyrlonCyfuniad o dadansoddiad algorithmig ac adolygiad dynol yna caiff ei ddefnyddio i ymhellach archwilio'r straeon.
Mae'r dadansoddiad NLP yn nodi patrymau iaith ailadroddus o fewn data testun rhyddMae'n rhannu'r data yn frawddegau cyfansoddol ac yna yn grwpio'r rhain yn 'bynciau' yn seiliedig ar dermau neu ymadroddion a ddefnyddir yn gyffredin gyda'i gilydd ac sy'n gysylltiedig â'r pwnc hwnnw (er enghraifft, gallai'r iaith a ddefnyddir mewn brawddeg am bryder fod yn debyg iawn i'r iaith a ddefnyddir wrth siarad am iselder, sydd wedi'i grwpio i mewn i bwnc ar iechyd meddwl). Fe'i gelwir yn dull 'o'r gwaelod i fyny' o ddadansoddi testun gan ei fod yn mynd ati i ymdrin â'r data heb unrhyw ragdybiaethau am y pynciau y bydd yn dod o hyd iddynt, yn hytrach mae'n caniatáu i bynciau ddod i'r amlwg yn seiliedig ar gynnwys y testun.
Dewiswyd straeon i'w cynnwys yn yr NLP mewn dwy ffordd. Yn gyntaf, cymerwyd yr holl ymatebion i bob cwestiwn o'r ffurflen ar-lein a tynnwyd data gwagYn ail, hidlwyd yr ymatebion yn seiliedig ar eu perthnasedd i Fodiwl 6.
Ystyriwyd bod straeon yn berthnasol os oedd y rhai a'u rhannodd wedi dewis unrhyw un o'r ymatebion isod i'r cwestiwn 'Beth hoffech chi ei ddweud wrthym ni amdano?':
- Gofal, er enghraifft, cartrefi gofal neu ofal cymdeithasol (5,332 o straeon)
- Teuluoedd, gan gynnwys rhieni, plant a pherthnasau hŷn (10,531 o straeon).
Yn dilyn nodi straeon perthnasol, Cynhaliwyd dadansoddiad NLP ar gyfer pob un o'r tri chwestiwn agored wedi'i gynnwys yn y ffurflen ar-lein. Yr allbwn o'r dadansoddiad hwn oedd rhywbeth o'r enw a model pwnc, sy'n crynhoi'r gwahanol bynciau a nodwyd mewn siart haul-ffrwydrad sy'n cynrychioli'n weledol y gwahanol bynciau a nodwyd. O hyn fe wnaethon ni nodi cyfanswm o 223 o bynciau ar draws yr holl ymatebion i C1, 222 yn C2 a 231 yn C3. Gan y gallai cyfranwyr ddewis ymatebion lluosog i'r cwestiwn 'Beth hoffech chi ddweud wrthym amdano?', roedd yn bosibl bod y straeon a ddewiswyd i'w cynnwys yn cynnwys gwybodaeth nad oedd yn berthnasol i Fodiwl 6 (er enghraifft, pynciau sy'n ymwneud â rhianta plant). Am y rheswm hwn, yn dilyn y dadansoddiad NLP cychwynnol, adolygodd y tîm ymchwil yn Ipsos yr holl bynciau i weld a ydynt yn berthnasol a chyfuno a dileu pynciau nad oeddent yn berthnasol i Fodiwl 6. o gam olaf y dadansoddiad. O hyn cyfanswm o 32 tynnwyd pynciau yn Ch1, 19 yn Ch2 a 30 yn Ch3. Gadawodd hyn gyfanswm o 191 o bynciau yn Ch1, 203 yn Ch2 a 201 yn Ch3.
Yn dilyn tynnu pynciau ddim yn berthnasol i Fodiwl 6 cynhaliwyd dadansoddiad ffactorau ystadegol i fapio perthnasoedd rhwng pynciau a'u grwpio'n ffeithiau (y cyfeirir atynt yma fel themâu) yn seiliedig ar y rhai sy'n digwydd yn gyffredin gyda'i gilydd neu o fewn tair brawddeg i'w gilydd. Grwpiodd y dadansoddiad ffactorau'r pynciau yn 27 thema ar gyfer C1, 24 thema ar gyfer C2, a 23 thema ar gyfer C3.
Yn dilyn y dadansoddiad hwn cynhyrchwyd un ffrâm god gyfunol yn seiliedig ar y pynciau sy'n berthnasol i Fodiwl 6 ac yn tynnu ar y themâu a nodwyd ar gyfer pob cwestiwnRoedd hyn yn cynnwys adolygiad dynol o'r geiriau a'r ymadroddion mwyaf cyffredin, o fewn pob pwnc, i nodi allweddeiriau a phatrymau sy'n dangos perthnasedd stori i un o'n themâu a nodwyd a chreu codau sy'n seiliedig ar reolau (yn seiliedig ar y pynciau ac wedi'u grwpio yn ôl themâu). Mae'r Roedd y ffrâm cod gyfunol derfynol, yn seiliedig ar y themâu unigol o'r dadansoddiad ffactorau a mewnbwn yr ymchwilydd, yn cynnwys 28 thema a 362 cod.
Yna defnyddiwyd y ffrâm god hon sy'n seiliedig ar allweddeiriau ar gyfer dadansoddiad a tagiodd straeon fel rhai perthnasol i Fodiwl 6 hyd yn oed os nad oedd y cyfrannwr wedi nodi mai dyma oedd yr achos trwy eu hateb i'r cwestiwn 'Beth hoffech chi ddweud wrthym amdano?'. Cafodd straeon a dderbyniwyd ar ôl y cam modelu pwnc cychwynnol eu cynnwys yn y dadansoddiad hwn hefyd. At ei gilydd, roedd 46,485 o straeon wedi'u cynnwys ar y pwynt hwn. Mae'r diagram isod yn dangos crynodeb o'r broses ddadansoddi ar gyfer data'r ffurflen ar-lein. Mae pynciau yn grwpiau manwl o gynnwys a nodwyd gan y dadansoddiad NLP ac mae themâu yn grwpiau o bynciau a nodwyd trwy ddadansoddi ffactorau. Codau yw'r codau penodol o fewn y themâu a ddefnyddiwyd ar gyfer y dadansoddiad terfynol.
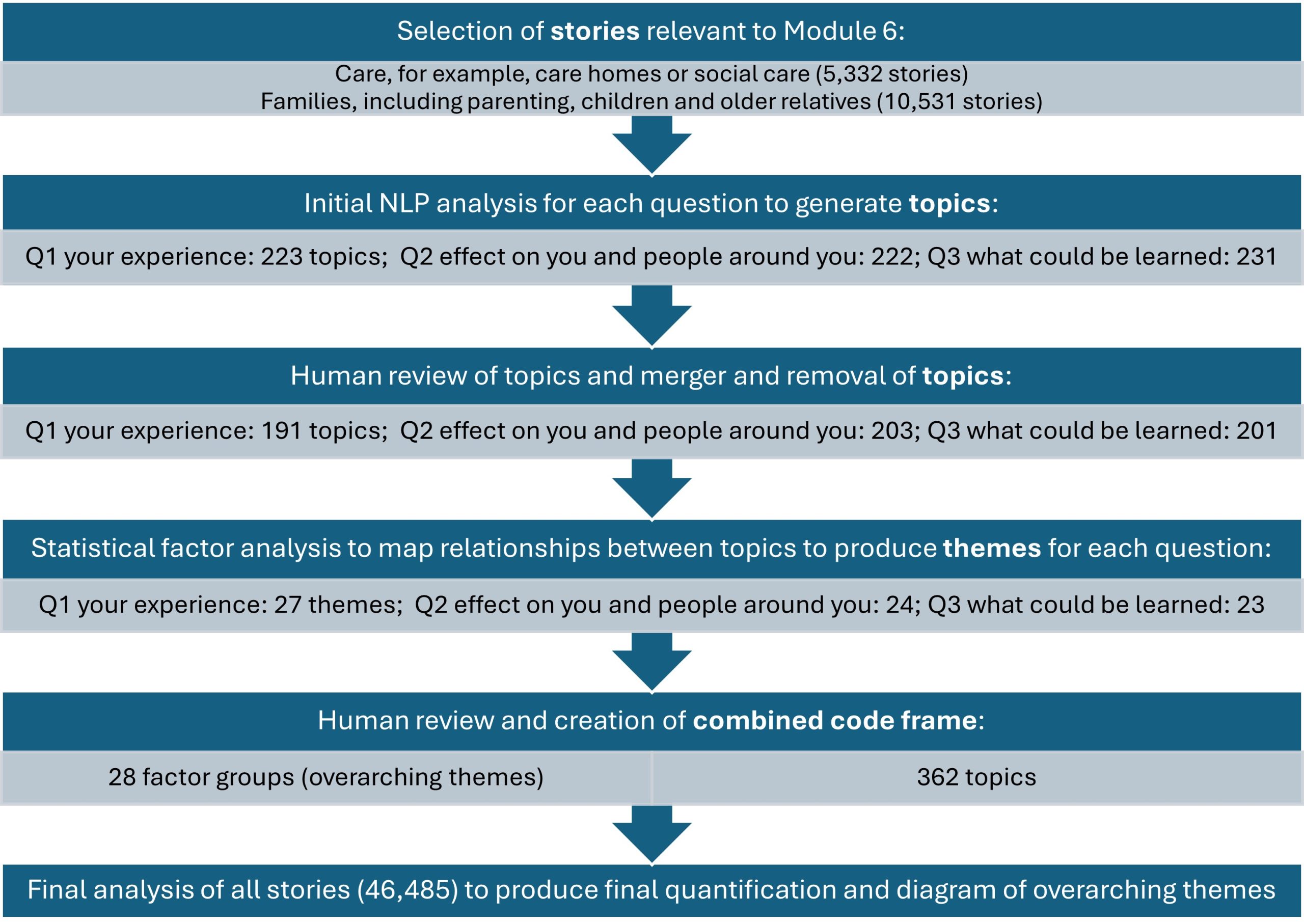
Ffigur 2: Proses NLP: Mae'r diagram yn dangos y camau sy'n gysylltiedig â'r dadansoddiad NLP.
Yna defnyddiodd ymchwilwyr y pynciau wedi'u tagio i archwilio'r straeon sy'n berthnasol i Fodiwl 6.Daethpwyd â’r rhain ynghyd â straeon a rannwyd gyda’r Ymchwiliad mewn ffyrdd eraill (a ddisgrifir isod) i’w cynnwys yn y cofnod hwn.
Mae'r Mae'r diagram isod yn dangos y themâu a nodwyd gan y dadansoddiad NLP a nifer y troeon y soniwyd am bob thema gan gyfrannwr yn eu hymateb. mae maint pob bloc yn cynrychioli nifer yr ymatebion sy'n gysylltiedig â'r themaNoder y gallai cyfranwyr unigol fod wedi crybwyll sawl thema yn eu hymateb ac felly gellir eu cyfrif fwy nag unwaith.
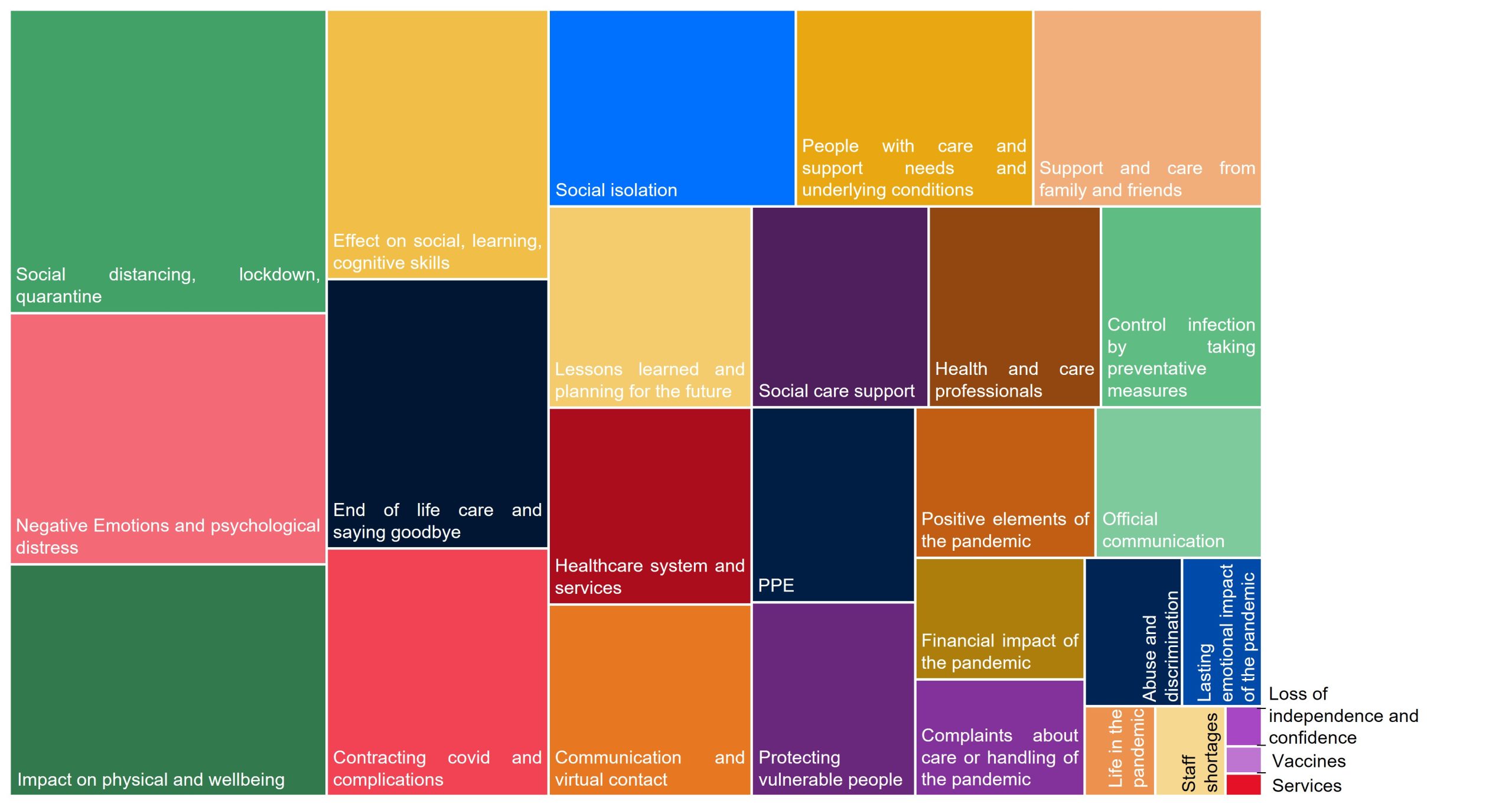
Ffigur 3: Themau NLP: Mae'r diagram yn dangos pa themâu a grybwyllwyd gan gyfranwyr yn y ffurflen ar-lein a pha mor aml y daeth y themâu hyn i'r amlwg. Mae blociau mawr yn golygu bod thema wedi'i chrybwyll gan fwy o gyfranwyr.
Digwyddiadau gwrando
Ysgrifennwyd adroddiadau crynodeb byr ar gyfer pob digwyddiad, rhannwyd hwy gyda chyfranogwyr y digwyddiad a'u defnyddio i lywio'r cofnod hwn. Lle bo'n briodol, darparwyd dyfyniadau gan dîm y digwyddiad gwrando i'w cynnwys yn y cofnod.
Gwrando wedi'i dargedu
Cafodd cyfweliadau eu recordio ar sain, eu trawsgrifio, eu codio a'u dadansoddi drwy adolygiad dynol i nodi themâu allweddol sy'n berthnasol i KLOEs Modiwl 6. Defnyddiwyd meddalwedd dadansoddi ansoddol (NVivo) i reoli a chodio'r data yn themâu. Roedd 21 cod ar gyfer themâu cysylltiedig â phynciau (e.e. effeithiau ar iechyd corfforol, ansawdd gofal, prinder staff ac ati). Yn ogystal, roedd pum cod i gynrychioli'r math o ofal a ddisgrifiwyd (nyrsio, preswyl, gofal cartref, gofal di-dâl, arall) a phum cod i gynrychioli amseriadau ar draws y pandemig (yn gynharach ac yn ddiweddarach yn y pandemig ac un ar gyfer pob cyfnod clo). Gellid codio pob rhan o drawsgrifiad sawl gwaith i adlewyrchu un neu fwy o themâu pwnc, y math o ofal a'r amseriad.
Rhifau sampl ar gyfer gwrando wedi'i dargedu ac astudiaethau achos
Mae'r tabl isod yn amlinellu nifer y cyfweliadau a gynhaliwyd ar draws gofal cymdeithasol i oedolion.
Tabl 1: Gofal cymdeithasol i oedolion – gwrando wedi'i dargedu
| Cyfranogwr | Cwblhawyd y cyfweliadau | |
| Gweithlu |
151 |
|
| Math o leoliad gofal | Cartref nyrsio |
33 |
| Cartref gofal gyda gwelyau ar gyfer dementia |
40 |
|
| Cartref gofal heb welyau dementia |
24 |
|
| Gofal cartref |
54 |
|
| Rôl | Rheoli |
25 |
| Gofal uniongyrchol |
97 |
|
| Gweithiwr Proffesiynol Rheoleiddiedig |
45 |
|
| Arall |
1 |
|
| Math o ddarparwr | Preifat |
80 |
| Nid er elw / Elusen |
27 |
|
| Cyhoeddus |
37 |
|
| Maint y cartref gofal | Hyd at 24 gwely |
36 |
| 25 a mwy o welyau |
53 |
|
| Pobl ag anghenion gofal a chymorth |
69 |
|
| Math o leoliad gofal | Cartref gofal gyda nyrsio |
19 |
| Cartref gofal heb nyrsio |
14 |
|
| Gofal cartref |
16 |
|
| Gofal di-dâl |
17 |
|
| Oedran y person sydd ag anghenion gofal a chymorth | Oedolyn hŷn (65+) |
39 |
| Oedolyn o oedran gweithio (18-64) |
27 |
|
| Gofalwyr di-dâl ac anwyliaid |
116 |
|
| Math o leoliad gofal | Anwyliaid preswylwyr cartrefi gofal – gyda nyrsio |
44 |
| Anwyliaid preswylwyr cartrefi gofal – heb nyrsio |
30 |
|
| Gofalwyr di-dâl (ffrindiau a theulu) – Gofal Cartref |
20 |
|
| Gofalwyr di-dâl (ffrindiau a theulu) – Gofal di-dâl yn unig |
21 |
|
| Oedran y person sydd ag anghenion gofal a chymorth | Oedolyn hŷn (65+) |
80 |
| Oedolyn o oedran gweithio (18-64) |
35 |
|
| Cyfanswm |
336 |
|
Mae cyfanswm y cyfranogwyr a adroddwyd uchod yn cynnwys y rhai a rannodd eu stori fel rhan o astudiaeth achos. Er mwyn clywed profiad pobl sy'n byw mewn cartrefi gofal, fe wnaethom ymweld â darparwyr gofal i siarad â phobl ag anghenion gofal a chymorth, staff ac anwyliaid. Rhoddodd y dull astudiaeth achos hwn gyfle hefyd i gael darlun cyfannol o'r profiadau mewn lleoliad o safbwyntiau lluosog. Cwblhawyd cyfanswm o 15 astudiaeth achos ledled Lloegr, yr Alban, Cymru a Gogledd Iwerddon, gweler tabl 2.
Tabl 2: Astudiaethau achos
| Lleoliad | Math o ofal | Cyfweliadau astudiaeth achos |
|---|---|---|
| Llundain | Cartref gofal | Pobl ag anghenion gofal a chymorth (3), Nyrs (1), Rheolwr (1) |
| Caint | Cartref gofal | Pobl ag anghenion gofal a chymorth (2), Gweithwyr gofal cymdeithasol i oedolion (3), Anwylyd (1) |
| Wolverhampton | Cartref gofal | Pobl ag anghenion gofal a chymorth (3), Gweithwyr gofal cymdeithasol i oedolion (3) |
| Caeredin | Cartref gofal | Pobl ag anghenion gofal a chymorth (1), Gweithwyr gofal cymdeithasol i oedolion (5) |
| Nottingham | Cartref gofal | Gweithwyr gofal cymdeithasol oedolion proffesiynol (3), pobl ag anghenion gofal a chymorth (1) |
| Belfast | Cartref gofal | Gweithwyr gofal cymdeithasol oedolion proffesiynol (3), pobl ag anghenion gofal a chymorth (2) |
| Leeds | Cartref gofal | Gweithwyr gofal cymdeithasol oedolion proffesiynol (3), pobl ag anghenion gofal a chymorth (3), Anwylyd (2) |
| Sussex | Cartref gofal | Gweithwyr gofal cymdeithasol oedolion proffesiynol (3), pobl ag anghenion gofal a chymorth (4) |
| Caerfaddon | Cartref preswyl | Gweithwyr gofal cymdeithasol oedolion proffesiynol (3), pobl ag anghenion gofal a chymorth (1) |
| Worksop | Cartref gofal | Pobl ag anghenion gofal a chymorth (3), Rheolwr (1) |
| Llundain | Pentref ymddeol | Pobl ag anghenion gofal a chymorth (3), Rheolwr (1) |
| Castell-nedd | Cartref gofal | Gweithwyr gofal cymdeithasol oedolion proffesiynol (3), pobl ag anghenion gofal a chymorth (1) |
| Watford | Cartref gofal | Pobl ag anghenion gofal a chymorth (4), Anwylyd (1), Nyrs (2), COE (1) |
| Gogledd Swydd Efrog | Cartref gofal | Pobl ag anghenion gofal a chymorth (2), Anwylyd (1), Gweithwyr gofal cymdeithasol oedolion (2), Rheolwr (1) |
| Thame | Cartref gofal (gyda Nyrsio) | Pobl ag anghenion gofal a chymorth (3) |
Cyfyngiadau
Dylid nodi bod cyfyngiadau i'r dull gwrando a gymerir gan Every Story Matters. Er enghraifft, trwy gyfweliadau manwl wedi'u targedu rydym wedi archwilio'r gwahanol safbwyntiau a phrofiadau o'r pandemig o fewn lleoliadau gofal gan gynnwys cartrefi gofal, gofal cartref a phobl na dderbyniodd unrhyw gefnogaeth ffurfiol. Mae hyn yn cwmpasu profiadau llawer mewn gofal cymdeithasol. Fodd bynnag, mae sawl lleoliad gofal nad oeddent wedi'u cynnwys yng nghwmpas y modiwl, megis pobl a gyflogodd gynorthwyydd personol, y rhai sy'n byw mewn cynlluniau bywydau a rennir neu bobl a dderbyniodd gefnogaeth tymor byr trwy wasanaethau ailalluogi.
Drwy’r ffurflen ar-lein a chynnal digwyddiadau gwrando, mae Every Story Matters hefyd wedi gallu clywed gan ystod eang o bobl a phrofiadau ar draws gofal cymdeithasol. Fodd bynnag, dim ond gan bobl sydd wedi dewis rhannu eu barn gyda’r Ymchwiliad yr ydym wedi clywed, ac a allai fod â phrofiadau penodol a allai fod yn fwy negyddol neu gadarnhaol na phrofiadau eraill. Mae hyn yn golygu na ddylid eu hystyried yn adlewyrchu profiadau’r cyhoedd yn gyffredinol, yn enwedig y rhai o grwpiau sy’n llai tebygol o ymgysylltu ag offer adborth ar-lein. Nid oedd y rhai a fu farw yn ystod y pandemig yn gallu rhannu eu profiadau, felly maent wedi cael eu cynrychioli gan y bobl a ofalodd amdanynt neu eu hanwyliaid.
Mae cyfyngiadau hefyd i ddefnyddio NLP fel ffordd o drefnu a dadansoddi'r profiadau a rennir trwy'r ffurflen ar-lein. Mae'r cyfyngiadau hyn yn ymwneud â chymhlethdod iaith a sut mae pobl yn siarad am eu profiadau mewn gwahanol gyd-destunau. Her arall yw y gall rhai profiadau sy'n unigryw i nifer fach o bobl nad ydynt yn cydymffurfio â phatrymau dominyddol barhau i gael eu tangynrychioli neu eu hanwybyddu'n llwyr, gan nad oes ganddynt y màs critigol i ffurfio pwnc penodol. I liniaru'r cyfyngiad hwn, rhedwyd modelau pwnc ar wahân ar gyfer pob un o'r tri chwestiwn yn lle un model cyffredinol, er mwyn caniatáu gwell cyfle i bynciau llai a allai fod wedi bod yn fwy cysylltiedig â chwestiwn penodol ddod i'r amlwg. Mae camau adolygu dynol lluosog yn rhan annatod o'r broses ddadansoddol ac yn helpu i liniaru'r cyfyngiadau hyn. Trwy adolygu â llaw o bynciau a themâu a gynhyrchir yn y cam modelu pynciau, mae'r themâu hyn yn cael eu mireinio i sicrhau bod naratifau unigryw yn cael eu dehongli'n gywir a bod themâu'n gywir yn eu cyd-destun.
Mae cyfyngiadau hefyd ar sut rydym wedi cyflwyno'r profiadau a rannwyd gydag Every Story Matters. Rydym wedi dewis cyflwyno dyfyniadau o gyfweliadau manwl a'r dadansoddiad NLP yn yr un modd, gan fod pob stori a phrofiad yn gyfartal. Dylid nodi bod y cyfweliadau manwl o samplau wedi'u targedu, tra bod y ffurflen ar-lein a'r digwyddiadau gwrando yn samplau hunan-ddethol, y gellir canolbwyntio ar brofiad penodol. Mae hyn yn golygu bod angen dehongli ar draws y tair ffynhonnell ddata wahanol i lunio naratif cyffredinol sy'n gytbwys ac yn adlewyrchu'r gwahanol leisiau rydym wedi'u clywed.
5. C1: Dywedwch wrthym am eich profiad; C2: Dywedwch wrthym am yr effaith arnoch chi a phobl o'ch cwmpas; C3: Dywedwch wrthym beth ydych chi'n meddwl y gellid ei ddysgu.