Rhagair
Dyma’r record gyntaf a gynhyrchwyd gan dîm Every Story Matters yn Ymchwiliad Covid-19 y DU. Mae’n dwyn ynghyd y profiadau a rannwyd gyda’r Ymchwiliad mewn perthynas â’i ymchwiliad i systemau gofal iechyd ac mae wedi’i gyflwyno gan y tîm i Gadeirydd yr Ymchwiliad, y Farwnes Hallett.
Fe wnaeth y Farwnes Hallett hi’n glir o’r cychwyn cyntaf ei bod hi eisiau
i glywed gan gynifer o bobl â phosibl, yn enwedig y rhai a oedd wedi dioddef caledi a cholled, fel y nodir yng Nghylch Gorchwyl yr Ymchwiliad. Felly fe wnaethon ni greu Mae Pob Stori’n Bwysig i’n helpu ni i glywed gan bobl mewn ffordd oedd yn addas iddyn nhw – yn ysgrifenedig, ar-lein neu ar bapur, mewn digwyddiad Mae Pob Stori’n Bwysig ledled y wlad, drwy gynhadledd fideo, gan ddefnyddio iaith arwyddion neu dros y ffôn. Mae straeon yn bwerus ac yn bersonol ac maen nhw'n dod ag effaith ddynol y pandemig yn fyw.
Drwy lansio Mae Pob Stori’n Bwysig, rhoddodd yr Ymchwiliad gyfle i bobl rannu eu profiad gyda ni, i gael rhywun i wrando arnynt, i gael eu profiad wedi’i recordio ac i gyfrannu at yr Ymchwiliad. Bydd ein cyfranwyr yn rhoi’r math o wybodaeth sydd ei hangen arni i’r Farwnes Hallett cyn dod i’w chasgliadau a gwneud argymhellion. Yn y ffordd honno, gallant helpu i sicrhau bod y DU wedi’i pharatoi’n well ar gyfer y pandemig nesaf a bod yr ymateb iddo yn fwy effeithiol.
Pan ddechreuon ni wrando ar bobl y DU am eu profiadau o'r pandemig, roeddem yn gwybod y byddai'r profiadau'n amrywiol. I lawer o bobl roedd effeithiau'r blynyddoedd hynny, a'r blynyddoedd ers hynny, yn bellgyrhaeddol. Mewn rhai achosion roedden nhw ac maen nhw'n hynod boenus, ac i rai bron yn rhy boenus i siarad amdanyn nhw. I lawer o bobl roedd y pandemig yn ddinistriol ac mae llawer yn dal i ddelio â'r canlyniadau boed yn brofedigaeth, cyflyrau meddygol hirdymor, neu fathau eraill o golled a chaledi. Clywsom hefyd fod rhai pobl eisiau symud ymlaen a pheidio â siarad am y pandemig mwyach. Weithiau clywsom bethau mwy cadarnhaol, lle roedd pobl wedi ffurfio cysylltiadau newydd, wedi dysgu rhywbeth neu wedi newid eu bywydau mewn rhyw ffordd er gwell.
Mae Every Story Matters wedi'i chynllunio i ddiogelu hunaniaeth pobl, osgoi aildrawmateiddio cymaint â phosibl a rhoi dewis iddynt sut i gyfrannu. Mae casglu a dadansoddi straeon fel hyn yn unigryw ar gyfer prosiect ymchwil; Nid yw Pob Stori o Bwys yn arolwg nac yn ymarferiad cymharol. Ni all fod yn gynrychioliadol o holl brofiad y DU ac ni chafodd ei gynllunio i fod, ond mae wedi ein galluogi i nodi themâu ymhlith profiadau pobl ac achosion nad ydynt yn ffitio i unrhyw grŵp penodol.
Yn y cofnod hwn rydym yn ymdrin â miloedd o brofiadau sy'n dangos effaith y pandemig ar gleifion, eu hanwyliaid, systemau a lleoliadau gofal iechyd, a gweithwyr allweddol ynddynt. Mae miloedd yn fwy o brofiadau nad ydynt yn ymddangos yn y cofnod hwn. Bydd yr holl brofiadau a rennir gyda ni yn llifo i gofnodion Mae Pob Stori o Bwys yn y dyfodol. Gan fod y cofnodion hyn wedi'u teilwra i'r gwahanol fodiwlau, rydym yn defnyddio straeon pobl lle gallant ychwanegu'r mewnwelediad mwyaf i'r meysydd dan ymchwiliad. Rydym yn parhau i annog pobl i rannu eu profiadau gyda ni, oherwydd eu straeon hwy sy'n gallu cefnogi a chryfhau argymhellion yr Ymchwiliad a helpu i leihau niwed pandemig yn y dyfodol. Gwiriwch wefan yr Ymholiad am y wybodaeth a'r amseroedd diweddaraf.
Rydym wedi cael cefnogaeth aruthrol gan unigolion, grwpiau a sefydliadau sydd wedi rhoi adborth a syniadau i ni ac wedi ein helpu i glywed gan ystod eang o bobl. Rydym yn ddiolchgar iawn iddynt ac rydym yn cydnabod llawer ohonynt ar y dudalen nesaf.
Mae Cyflawni Mae Pob Stori o Bwys wedi cyffwrdd â phawb a gymerodd ran. Dyma straeon a fydd yn aros gyda phawb sy'n eu clywed neu'n eu darllen am weddill eu hoes.
Tîm Mae Pob Stori o Bwys
Diolchiadau
Hoffai tîm Mae Pob Stori’n Bwysig fynegi ei werthfawrogiad diffuant i’r holl sefydliadau a restrir isod am ein helpu i ddal a deall llais a phrofiadau gofal iechyd aelodau o’u cymunedau. Roedd eich cymorth yn amhrisiadwy i ni gan helpu i sicrhau ein bod yn cyrraedd cymaint o gymunedau â phosibl. Diolch am drefnu cyfleoedd i dîm Mae Pob Stori’n Bwysig glywed profiadau’r rhai rydych yn gweithio gyda nhw naill ai’n bersonol yn eich cymunedau, yn eich cynadleddau, neu ar-lein.
- Cymdeithas yr Anesthetyddion
- Cymdeithas Geriatreg Prydain
- Carers UK
- Clinically Vulnerable Families
- Covid-19 mewn Profedigaeth Teuluoedd er Cyfiawnder Cymru
- Covid19 Families UK a Marie Curie
- Disability Action Northern Ireland, a’r Prosiect ONSIDE (a gefnogir gan Disability Action Northern Ireland)
- Gofalwyr Eden Carlisle
- Grŵp Cymorth Covid Enniskillen Long
- Cymdeithas y Byddar Foyle
- Healthwatch Cumbria
- Plant hir Covid
- Long Covid yr Alban
- Cefnogaeth Covid Hir
- SOS Covid hir
- Mencap
- Cyngor Menywod Moslemaidd
- Eiriolaeth Annibynnol Pobl yn Gyntaf
- PIMS-Hwb
- Cynghrair Hil Cymru
- Coleg Brenhinol y Bydwragedd
- Coleg Brenhinol y Nyrsys
- Sefydliad Cenedlaethol Brenhinol Pobl Ddall (RNIB)
- Scottish Covid Bereaved
- Sewing2gether Yr Holl Genhedloedd (mudiad cymunedol Ffoaduriaid)
- Self-Directed Support Scotland
- Cyngres yr Undebau Llafur
- UNSAIN
I’r fforymau Galarwyr, Plant a Phobl Ifanc, Cydraddoldeb, Cymru, yr Alban a Gogledd Iwerddon, a grwpiau Cynghori Long Covid, rydym yn wirioneddol werthfawrogi eich mewnwelediadau, eich cefnogaeth a’ch her ar ein gwaith. Roedd eich mewnbwn yn allweddol i'n helpu i lunio'r cofnod hwn.
Yn olaf ond nid yn lleiaf, hoffem gyfleu ein diolch o galon i’r holl deuluoedd, ffrindiau ac anwyliaid mewn profedigaeth am rannu eu profiadau gyda ni.
Trosolwg
Sut roedd straeon yn cael eu casglu a'u dadansoddi
Mae pob stori a rennir gyda'r Ymchwiliad yn cael ei dadansoddi a bydd yn cyfrannu at un neu fwy o ddogfennau thema fel hon. Cyflwynir y cofnodion hyn o Mae Pob Stori'n Bwysig i'r Ymchwiliad fel tystiolaeth. Mae hyn yn golygu y bydd canfyddiadau ac argymhellion yr Ymchwiliad yn cael eu llywio gan brofiadau'r rhai yr effeithiwyd arnynt gan y pandemig.
Rhannodd pobl eu profiadau gyda'r Ymchwiliad mewn gwahanol ffyrdd. Mae'r straeon a ddisgrifiodd brofiadau o ofal iechyd yn ystod y pandemig wedi'u dwyn ynghyd a'u dadansoddi i dynnu sylw at themâu allweddol. Mae’r dulliau a ddefnyddir i archwilio straeon sy’n berthnasol i’r modiwl hwn yn cynnwys:
- Dadansoddi 32,681 o straeon a gyflwynwyd ar-lein i'r Ymchwiliad, gan ddefnyddio cymysgedd o brosesu iaith naturiol ac ymchwilwyr yn adolygu a chatalogio'r hyn y mae pobl wedi'i rannu.
- Mae ymchwilwyr yn tynnu ynghyd themâu o 604 o gyfweliadau ymchwil gyda'r rhai a fu'n ymwneud â gofal iechyd yn ystod y pandemig mewn gwahanol ffyrdd gan gynnwys cleifion, anwyliaid a gweithwyr gofal iechyd.
- Ymchwilwyr yn tynnu ynghyd themâu o ddigwyddiadau gwrando Mae Pob Stori’n Bwysig gyda’r cyhoedd a grwpiau cymunedol mewn trefi a dinasoedd ar draws Lloegr, yr Alban, Cymru a Gogledd Iwerddon, gan gynnwys ymhlith y rhai a brofodd effeithiau pandemig penodol. Mae rhagor o wybodaeth am y sefydliadau y bu’r Ymchwiliad yn gweithio gyda nhw i drefnu’r digwyddiadau gwrando hyn wedi’i chynnwys yn yr adran gydnabyddiaeth.
Mae mwy o fanylion am sut y cafodd straeon pobl eu dwyn ynghyd a'u dadansoddi yn yr adroddiad hwn wedi'u cynnwys yn yr atodiad. Mae’r ddogfen hon yn adlewyrchu profiadau gwahanol heb geisio eu cysoni, gan ein bod yn cydnabod bod profiad pawb yn unigryw.
Drwy gydol yr adroddiad, rydym wedi cyfeirio at bobl a rannodd eu straeon ag Every Story Matters fel 'cyfranwyr'. Mae hyn oherwydd eu bod wedi chwarae rhan bwysig wrth ychwanegu at dystiolaeth yr Ymchwiliad ac at gofnod swyddogol y pandemig. Lle bo'n briodol, rydym hefyd wedi disgrifio mwy amdanynt (er enghraifft, gwahanol fathau o staff sy'n gweithio ym maes gofal iechyd) neu'r rheswm pam y bu iddynt rannu eu stori (er enghraifft fel cleifion neu anwyliaid) i helpu i egluro'r cyd-destun.
Archwilir rhai straeon yn fanylach trwy ddyfyniadau ac astudiaethau achos. Mae'r rhain wedi'u dewis i amlygu profiadau penodol a'r effaith a gawsant ar bobl. Mae'r dyfyniadau a'r astudiaethau achos yn helpu i seilio'r adroddiad ar yr hyn a rannodd pobl â'r Ymchwiliad yn eu geiriau eu hunain. Mae'r cyfraniadau wedi'u gwneud yn ddienw. Rydym wedi defnyddio ffugenwau ar gyfer astudiaethau achos sydd wedi'u tynnu o'r cyfweliadau ymchwil. Nid oes ffugenwau ar brofiadau a rennir gan ddulliau eraill.
Wrth roi llais i brofiadau’r cyhoedd, mae rhai o’r straeon a’r themâu a gynhwysir yn yr adroddiad hwn yn cynnwys disgrifiadau o farwolaeth, profiadau bron â marw, a niwed corfforol a seicolegol sylweddol. Mae gan y rhain y potensial i fod yn ofidus ac anogir darllenwyr i gymryd camau i gefnogi eu lles wrth iddynt wneud hynny. Gallai hyn olygu cymryd seibiannau, ystyried pa benodau sy’n teimlo’n fwy neu’n llai goddefadwy i’w darllen, a mynd at gydweithwyr, ffrindiau, teulu neu eraill cefnogol am help. Anogir darllenwyr sy'n profi trallod parhaus sy'n gysylltiedig â darllen yr adroddiad hwn i ymgynghori â'u darparwr gofal iechyd i drafod opsiynau ar gyfer cymorth. Rhestr o wasanaethau cefnogol yn cael eu darparu hefyd ar wefan UK Covid-19 Inquiry.
Y straeon a rannodd pobl am ofal iechyd yn ystod y pandemig
Dywedodd pobl wrthym am yr effeithiau newidiol niferus a gafodd y pandemig arnynt fel cleifion, anwyliaid a gweithwyr gofal iechyd, ac mae rhai yn dal i fyw gyda'r effeithiau hyn heddiw.
Roedd llawer o bobl yn wynebu problemau wrth gael mynediad at ofal iechyd yn ystod y pandemig, boed mewn sefyllfaoedd brys, ar gyfer cyflyrau iechyd acíwt, neu ar gyfer apwyntiadau mwy arferol.
Clywsom am y golled enbyd a brofwyd gan y rhai a oedd mewn profedigaeth yn ystod y pandemig. Clywsom am fywydau sydd wedi cael eu haflonyddu a’u difrodi gan ddal Covid-19, datblygu a byw gyda Long Covid ac oedi cyn derbyn triniaeth ar gyfer afiechydon difrifol eraill. Dywedodd pobl sy’n agored i niwed yn glinigol ac sy’n hynod agored i niwed yn glinigol wrthym am doll corfforol ac emosiynol gwarchod ac effaith barhaus Covid-19 ar eu bywydau.
Clywsom hefyd am bethau cadarnhaol a ddigwyddodd yn ystod y pandemig. Roedd gwasanaethau gofal iechyd yn parhau i gefnogi llawer o gleifion ac roedd enghreifftiau o ofal da i gleifion. Myfyriodd gweithwyr gofal iechyd ar bopeth a wnaethant i addasu sut yr oeddent yn trin ac yn gofalu am bobl a'r ffyrdd yr oeddent yn cefnogi anwyliaid cleifion mewn amgylchiadau heriol unigryw.
Newidiadau i ofal iechyd yn ystod y pandemig
Roedd yr ofn o ddal Covid-19 yn golygu bod llawer o bobl yn amharod i gael mynediad at wasanaethau gofal iechyd, yn enwedig yn gynnar yn y pandemig. Roedd yr ofnau cryfaf ynghylch mynd i'r ysbyty ond roeddent hefyd yn berthnasol i leoliadau gofal iechyd personol eraill. Roedd llawer o gleifion a'u hanwyliaid yn ofni y byddent yn cael eu gwahanu oherwydd polisïau ymweld.
| “ | A dweud y gwir, doedd neb eisiau mynd i'r ysbyty bryd hynny. Yn anffodus, doedd gen i ddim opsiwn. Roeddwn yn ambiwlansys i mewn. Roeddwn i wir yn ymladd i beidio â mynd i’r ysbyty bob tro, ond roedd yn beryglus, ac roedd angen i mi fod yno, ac roeddwn yn deall hynny.”
- Person yn yr ysbyty gyda Covid-19 |
| “ | Doeddwn i ddim eisiau i Dad fynd i'r ysbyty, doedd fy nhad ddim eisiau mynd i'r ysbyty chwaith. Roedd y ddau ohonom o'r un farn. Nid oedd eisiau mynd i'r ysbyty, roedd wrth ei fodd bod gartref, os yw'n mynd i farw, roedd am farw gartref. Roedden ni’n gwybod pe bai’n mynd i’r ysbyty, byddwn i’n ffarwelio wrth y drws a’r tebygrwydd yw na fyddwn i byth yn ei weld eto ac y byddai’n marw ar ei ben ei hun yn yr ysbyty.”
- Aelod o'r teulu mewn profedigaeth |
Roedd yr ofn o ddal Covid-19 ac ymwybyddiaeth y cyhoedd o'r pwysau ar systemau gofal iechyd yn golygu bod derbyniad eang i'r angen i ad-drefnu sut roedd gofal iechyd yn cael ei ddarparu yn ystod y pandemig. Rhannodd cyfranwyr lawer o enghreifftiau o ba mor heriol oedd y newidiadau hyn i gleifion, eu hanwyliaid a gweithwyr gofal iechyd.
Un newid pwysig oedd bod llawer mwy o wasanaethau’n cael eu darparu o bell, naill ai ar-lein neu dros y ffôn. Roedd cleifion, anwyliaid a chlinigwyr yn aml heb eu hargyhoeddi y gallai symptomau gael eu hasesu'n iawn heb ymgynghoriad wyneb yn wyneb.
| “ | Mae'n rhaid i mi anfon lluniau i grŵp WhatsApp fy meddyg. Mae gan fy meddygfa rif ffôn WhatsApp lle rydych chi'n anfon eich enw, dyddiad geni a'r ffotograffau ... nid yw'r un peth."
- Person sy'n byw gyda Long Covid |
Roedd rhywfaint o ddryswch ynghylch y canllawiau sydd ar waith yn ystod y pandemig - yn enwedig ar gyfer ymweld ag anwyliaid neu fynychu apwyntiadau gyda nhw. Clywsom hefyd nad oedd canllawiau’n cael eu cymhwyso’n gyson a’r problemau a’r rhwystredigaeth a achoswyd gan hyn.
Ar y pryd roedd canllawiau’r llywodraeth yn llawer mwy rhyddfrydol na’r rheolau y dewisodd yr ysbyty eu cymhwyso mewn gwirionedd, a oedd yn hynod rwystredig ac a gafodd effaith andwyol ar fy iechyd meddwl. Roedd ysbytai eraill yn llawer mwy parod, gyda defnydd o dosturi a synnwyr cyffredin.
I gleifion a oedd yn poeni am haint Covid-19, roedd Offer Amddiffynnol Personol (“PPE”) yn aml yn cael ei ystyried yn galonogol oherwydd y byddai’n lleihau’r risgiau yr oeddent yn eu hwynebu. I eraill, creodd PPE rwystr a oedd yn teimlo'n annaturiol neu'n frawychus, gan ychwanegu at eu pryder ynghylch bod yn sâl yn ystod y pandemig. Roedd rhai gweithwyr gofal iechyd yn cytuno bod PPE yn gosod rhwystr rhyngddynt a chleifion ac yn gwneud darparu gofal yn fwy heriol nag oedd cyn y pandemig.
Roedd ymweliadau ysbyty nad oeddent yn cael eu caniatáu neu'n cael eu cyfyngu yn rhwystredig ac yn aml yn frawychus i gleifion. Canfu anwyliaid nad oeddent yn gwybod beth oedd yn digwydd yn hynod o ofidus, yn enwedig pan oedd cleifion yn sâl iawn neu'n agosáu at ddiwedd eu hoes. Yn yr un modd, roedd llawer o weithwyr gofal iechyd yn rhannu pa mor ofidus nad oeddent yn gallu cyfathrebu yn y ffordd arferol ag anwyliaid a oedd mewn trallod.
| “ | 48 awr yn ddiweddarach, rydych chi'n eu ffonio i ddweud wrthyn nhw fod eu perthynas yn marw ac nad ydyn nhw'n eich credu chi a pham y dylen nhw? Ac mae ganddyn nhw gwestiynau na allwch chi eu hateb, ac mae gennych chi atebion nad ydyn nhw eu heisiau.”
-Meddyg ysbyty |
Problemau cyrchu gofal iechyd
Roedd pobl yn ei chael hi’n anodd cael mynediad at ofal iechyd yn ystod y pandemig, gydag effeithiau difrifol a pharhaol mewn rhai achosion. Roedd cleifion, anwyliaid a gweithwyr gofal iechyd wedi sylwi ar nifer o broblemau cyffredin:
- Rhannodd llawer o gleifion pa mor anodd oedd hi i drefnu apwyntiadau meddyg teulu, gan eu gadael heb unrhyw ffordd o gael cymorth meddygol arferol.
| “ | Nid oedd angen cau'r practisau meddygon teulu a lleihau hynny. Rwy'n meddwl y gallai llawer o bobl fod wedi cael eu gweld o hyd, pobl sydd â lympiau a thwmpathau neu sydd angen tynnu pethau. Rwy’n meddwl y gallent fod wedi delio â hynny. Rwy’n meddwl efallai y gallai hynny fod wedi achub ychydig o fywydau hefyd.”
– claf meddyg teulu |
- Cafodd gofal ysbyty nad yw'n gysylltiedig â Covid-19 ei gwtogi, gan arwain at oedi hir ar gyfer triniaeth, mewn rhai achosion ar gyfer salwch difrifol neu gyflyrau iechyd parhaus.
| “ | Mae gennyf sawl achos yn fy meddwl o bobl a oedd yn dioddef o gyflyrau anfalaen ond cyfyngol, a oedd yn hawdd iawn eu trwsio pe baent wedi cael mynediad at ofal iechyd acíwt yn gynt. Ond, wyddoch chi, roedd hi’n anodd iawn iddyn nhw gael mynediad at ofal iechyd, i weld y person roedd angen iddyn nhw ei wneud.”
-Meddyg ysbyty |
- Roedd y rhai a geisiodd gael mynediad at ofal brys weithiau’n methu â chael cymorth neu’n wynebu oedi sylweddol, hyd yn oed pan oedden nhw neu eu hanwyliaid yn sâl iawn.
| “ | Fel arfer efallai y bydd 30 galwad yn aros ar unrhyw un adeg. Ar adegau brig yn y pandemig roedd 900 o alwadau yn aros.”
– triniwr galwadau GIG 111 |
Myfyriodd cyfranwyr ar sut y cynyddodd dicter a rhwystredigaeth ynghylch cael mynediad at ofal wrth i'r pandemig fynd rhagddo. Roedd llawer ohonynt yn beio’r problemau hyn am bobl yn gorfod byw gyda phoen a symptomau eraill, gan leihau ansawdd eu bywyd ac arwain at waethygu iechyd. Roedd rhai achosion o oedi, canslo neu gamgymeriadau ar draws gofal iechyd yn ystod y pandemig yn cysylltu’n uniongyrchol â phroblemau iechyd difrifol neu farwolaeth anwylyd.
Roedd cleifion, anwyliaid a chlinigwyr yn aml yn rhwystredig bod trin Covid-19 a lleihau lledaeniad y clefyd yn cael ei flaenoriaethu dros anghenion gofal iechyd difrifol eraill. Dadleuodd llawer o gyfranwyr y gellid bod wedi gwneud mwy i osgoi’r effeithiau negyddol ar gleifion nad ydynt yn ymwneud â Covid.
Yn y cyfnod cloi, roedd pobl yn dal yn wael. Cafodd rhywun ddiagnosis o ganser ac ni allai gael apwyntiad. Peidiwch ag esgeuluso pobl ag anghenion triniaeth eraill. Cafodd y driniaeth chemo ei chanslo, datblygodd y canser, a buont farw.
Clywsom hefyd am y rhwystrau penodol niferus i gael mynediad at ofal – a derbyn gofal da – a wynebir gan bobl ag anabledd, y rhai nad ydynt yn siarad Saesneg a’r rhai heb dechnoleg ddigidol na rhyngrwyd dibynadwy.
| “ | Nid oedd deall gwybodaeth, bod yn fyddar, methu â chyfathrebu, llawer o bethau ar-lein, a gorfod defnyddio Saesneg ac ysgrifennu, wyddoch chi, e-byst a phethau felly a negeseuon testun yn hygyrch iawn i mi.”
- Person byddar |
Tynnodd rhai cyfranwyr sylw hefyd at sut y gwaethygodd y pandemig yr anghydraddoldebau presennol.
Gwelais yn uniongyrchol effaith Covid-19 ar gymuned a oedd eisoes dan anfantais oherwydd llawer o anfanteision cymdeithasol gan gynnwys tlodi. Unwaith eto, gwelais nad oes ots gan fywydau du. Rhwygwyd Covid-19 [lle roeddwn i’n byw] gan fod Covid-19 wedi cael effaith andwyol ar weithwyr rheng flaen, pobl o liw, pobl ar gontractau dim oriau na fyddent ar ffyrlo ac na allent fforddio rhoi’r gorau i weithio.
| “ | Byddwn i'n dweud fy mod i'n un o'r bobl fwyaf hyderus i ofyn cwestiynau, ond hyd yn oed fi rydw i weithiau'n teimlo ychydig o gywilydd, 'Ydw i'n gofyn gormod? Neu a all pobl ddeall yr hyn rwy'n ceisio'i egluro?' Ti'n gwybod? Roeddwn i'n adnabod rhai pobl, nid iaith yn unig oedd yn rhwystr, a dweud y gwir, y darn llythrennedd hefyd. Mae fel, dydyn nhw ddim yn gallu darllen, dydyn nhw ddim yn gallu ysgrifennu, dydyn nhw ddim yn deall yr iaith. Hyd yn oed pan wnaethoch chi ei esbonio mewn Tsieinëeg, roedd y term meddygol yn rhy gymhleth iddyn nhw. ”
- Person sy'n siarad Saesneg fel ail iaith |
Profiadau o Covid-19
Roedd rhai gweithwyr gofal iechyd yn teimlo eu bod wedi'u cymell i weithio'n uniongyrchol gyda chleifion Covid-19. Roeddent eisiau gwneud yr hyn a allent i helpu, er gwaethaf yr ofn o ddod i gysylltiad uniongyrchol â'r firws. Roedd llawer o weithwyr gofal iechyd yn poeni am ddal Covid-19 eu hunain a'i drosglwyddo i'w teuluoedd.
Bob dydd byddwn yn mynd i mewn i weld marwolaeth a bob dydd byddwn yn meddwl tybed ai dyma'r diwrnod yr wyf yn mynd ag ef adref at fy mhlant bach.
Rhannodd rhai sut y gwnaethant golli cydweithwyr i'r afiechyd.
| “ | Aeth y tri ohonom a aeth am hyfforddiant yn sâl… gyda symptomau Covid-19. Gwellodd ffrind arall a minnau (pob nyrs a pharafeddygon) ond o fewn pythefnos roedd ein ffrind arall wedi marw, a ganfuwyd gan barafeddygon gartref yn unig ar ôl galw am help oherwydd ar y pryd roedd pobl yn cael eu cynghori i beidio â theithio i'r ysbyty. Roedd hi’n 29 oed a bu farw ar ei phen ei hun.”
- Gweithiwr gofal iechyd proffesiynol |
Dywedodd gweithwyr gofal iechyd proffesiynol sy’n trin cleifion Covid-19 wrthym eu bod wedi gwneud eu gorau er gwaethaf yr heriau enfawr yr oeddent yn eu hwynebu, weithiau heb yr offer a’r adnoddau staff yr oedd eu hangen arnynt. Roedd hyn yn eu rhoi dan straen aruthrol a disgrifiodd llawer eu bod yn teimlo dan straen ac wedi blino'n lân. Dywedasant wrthym fod eu profiadau wedi cael effaith negyddol ar eu hiechyd meddwl. Er gwaethaf yr heriau, rhannodd y rhai a driniodd cleifion Covid-19 hefyd sut y gwnaeth y gofal a gynigiwyd ganddynt wella wrth i'r pandemig fynd rhagddo a dysgwyd mwy am y clefyd.
| “ | Rwy’n gwybod fy mod yn gweld llawer o drawma yn aml, ond roedd hyn… ar lefel wahanol. Roedd yn rhywbeth nad oedd yr un ohonom wedi ei brofi. Ac roedd pawb yn gwibio eu ffordd drwy’r sefyllfa hon, nad oedd neb yn gwybod sut i’w thrin, ond roedden ni’n gwneud ein gorau.”
- Parafeddyg |
Disgrifiodd llawer o gleifion Covid-19 pa mor ofnus oedd arnynt ynghylch cael eu derbyn i’r ysbyty yn annisgwyl gyda Covid-19 a pha mor ddryslyd ydoedd. Roedd rhai yn cael trafferth cofio llawer am eu hamser yn yr ysbyty oherwydd eu bod mor sâl.
Un diwrnod fe ddeffrais yn yr ICU methu symud, siarad, bwyta, yfed ac ati. Roeddwn i'n dibynnu'n llwyr ar staff i fynd i'm golchi, bwydo fi, ac ati. o dracheostomi yn fy ngwddf. Mae'n debyg, roeddwn i wedi bod mewn coma anwythol ers dau fis.
Dywedodd rhai cleifion a oedd yn yr ysbyty â Covid-19 difrifol wrthym eu bod yn dal i gael eu trawmateiddio gan eu profiadau. Clywsom pa mor annifyr oedd gweld marwolaethau cleifion Covid-19 eraill, a sut yr ychwanegodd hyn at ofnau am y clefyd.
| “ | Ychydig wythnosau wedyn, dirywiodd iechyd meddwl fy mab, roedd yn cael gweledigaethau o fod yn ôl yn ei ward ysbyty ac roedd y dyn o'r gwely drws nesaf iddo yn yr ysbyty yn sefyll yn ei ystafell ac yn grac nad oedd yn ei helpu ... fe yn crio yn Tesco oherwydd bod canu’r tiliau yn mynd ag ef yn ôl i’r monitors yn canu yn yr ysbyty.”
– Gofalwr ar gyfer claf yn yr ysbyty gyda Covid-19 |
Effaith y pandemig
Gofal diwedd oes a phrofedigaeth
Rhannodd llawer o deuluoedd, ffrindiau a chydweithwyr profedigaeth eu colled, dinistr a dicter. Yn aml, nid oeddent yn cael ymweld ac nid oedd ganddynt fawr o gysylltiad, os o gwbl, â'u hanwyliaid a oedd yn marw. Roedd yn rhaid i rai ffarwelio dros y ffôn neu ddefnyddio tabled. Roedd yn rhaid i eraill wneud hynny wrth gadw eu pellter a gwisgo PPE llawn.
Roedd gan deuluoedd a ffrindiau mewn profedigaeth lawer llai o ymwneud â phenderfyniadau am eu hanwyliaid nag y byddent fel arfer. Clywsom am anwyliaid yn cael trafferth cysylltu â gweithwyr gofal iechyd proffesiynol i ddarganfod beth oedd yn digwydd. Roedd hyn yn aml yn golygu bod y sefyllfa'n teimlo allan o'u rheolaeth, gan eu gadael yn ofnus ac yn ddiymadferth. Roedd eirioli dros eu hanwyliaid a’u gofal o bell yn llawer anoddach nag o dan amgylchiadau arferol, ac weithiau’n amhosibl.
| “ | Cafodd fy ngŵr ei gludo i’r ysbyty a’i ddileu yn y bôn oherwydd oedran a chyflyrau eraill… roedd yn negyddol i Covid a chafodd ei roi ar ward lle roedd yn rhemp. Doedden ni ddim yn cael ymweld, doedd gennym ni ddim syniad beth oedd yn digwydd. Bu farw a chefais alwad ffôn am 3:15am yn dweud wrthyf ei fod wedi mynd.”
- Aelod o'r teulu mewn profedigaeth |
| “ | Doeddech chi ddim yn gallu mynd drwodd i unrhyw un, doeddech chi ddim yn gallu siarad â neb, roedden ni i gyd yn ffonio am ddiweddariad ... roedd fy nhad yn ffonio'n ddyddiol i'w [nain] gael ei rhyddhau i ni ... Mae gennym bopeth wedi'i osod yma [yn y cartref ]. Roedd ganddi wely trydan hyd yn oed, roedd gennym ni gadeiriau olwyn a phopeth iddi. Gallem fod wedi ei helpu.”
– Gofalwr am aelod oedrannus o'r teulu |
Roedd yn rhaid i deuluoedd, ffrindiau a chydweithwyr mewn profedigaeth a oedd yn gallu ymweld wneud hynny'n aml mewn amgylchiadau eithriadol a chyfyng iawn, fel arfer pan oedd y claf ar ddiwedd ei oes. Roedd yn rhaid i rai ddewis pwy fyddai'n ymweld oherwydd bod y niferoedd yn gyfyngedig. Nid oedd llawer yn cael cyffwrdd â'u hanwyliaid ac roedd yn rhaid iddynt wisgo PPE. Roedd y cyfyngiadau yn golygu bod rhai yn ymweld ar eu pen eu hunain, heb gefnogaeth teulu a ffrindiau. Roedd y profiad yn aml yn ddryslyd ac yn frawychus.
Clywsom lawer am hysbysiadau peidiwch â cheisio dadebru cardio-pwlmonaidd (DNACPR) a gofal diwedd oes a sut nad oedd penderfyniadau bob amser yn cael eu hesbonio i anwyliaid. Dywedodd rhai teuluoedd a ffrindiau mewn profedigaeth wrthym nad oeddent yn gwybod pa benderfyniadau a wnaed tan ar ôl i'w hanwyliaid farw, neu nad oeddent yn gwybod o hyd.
| “ | Gofynnodd y meddyg teulu i DNACPR fod yn ei le, roedd fy nhad yn gwybod am hyn a'r canlyniadau posibl, roedd eisiau byw, nid oedd eisiau un. Yna darganfyddais fod y meddyg teulu wedi ymweld eto’n ddirybudd gyda chais DNACPR, ac ni wnaethant erioed sôn wrthyf amdano.”
- Aelod o'r teulu mewn profedigaeth |
Yn ogystal â'r heriau niferus a wynebwyd gan anwyliaid mewn profedigaeth, roedd y straeon yn cynnwys enghreifftiau o weithwyr gofal iechyd yn cynnig gofal diwedd oes rhagorol yn ystod y pandemig. Disgrifiodd rhai pa mor gefnogol oedd y staff a faint roedd hyn wedi gwella gofal diwedd oes. Un enghraifft gyffredin oedd gweithwyr iechyd proffesiynol yn torri canllawiau Covid-19 i roi cysur corfforol i'w hanwyliaid a oedd yn marw.
Rwy'n cofio, roedd un nyrs fel, 'O, roedd eich tad eisiau i mi roi cwtsh i chi, a dweud, “Dyma gwtsh.”' Yn amlwg, nid oedd angen iddi wneud hynny...dydych chi ddim hyd yn oed i fod i i fod yn dod yn agos, ond dim ond y math yna o deimlad trugarog, ac yr oeddwn yn union fel, o fy Nuw, sydd mor adfywiol i weld mewn person meddygol.
I lawer, roedd colli anwyliaid a methu â dweud hwyl fawr yn gwneud eu colled yn anoddach i'w derbyn a dod i delerau â hi. Mae rhai yn cael eu gadael gyda'r euogrwydd llethol y dylent fod wedi gwneud mwy i'w hamddiffyn rhag Covid-19 neu rhag gorfod marw mewn lleoliadau gofal iechyd yn unig.
Covid hir
Mae Long Covid yn set o gyflyrau iechyd a symptomau hirdymor y mae rhai pobl yn eu datblygu ar ôl cael eu heintio â firws Covid-19. Cafodd Long Covid – ac mae’n parhau i gael – effaith ddramatig ac yn aml yn ddinistriol ar bobl. Dywedodd llawer o bobl sy’n byw gyda Long Covid wrthym sut yr oeddent am gael gwell cydnabyddiaeth a mwy o ddealltwriaeth ymhlith y cyhoedd o’r symptomau y maent yn parhau i’w profi a’r effaith enfawr y mae’n ei chael ar eu gallu i fyw eu bywydau. Pwysleisiodd rhai hefyd bwysigrwydd mwy o ymchwil a datblygu sy'n canolbwyntio ar driniaethau ar gyfer Long Covid.
| “ | Rydyn ni'n cael ein gadael ar ein pennau ein hunain nawr; nid ydym yn gwybod beth y gallwn ei wneud. Mae angen iddyn nhw gydnabod bod Covid yn gyflwr hirdymor neu gydol oes i rai pobl.”
- Person â Covid Hir |
Rhannodd y rhai sy'n byw gyda Long Covid y problemau iechyd parhaus niferus y maent wedi'u profi, gyda gwahanol fathau a difrifoldeb y symptomau. Mae'r rhain yn amrywio o ddoluriau a phoenau parhaus a niwl yr ymennydd, i flinder meddyliol gwanychol. Dywedodd llawer wrthym sut y mae eu bywydau wedi cael eu difrodi, a sut nad ydynt bellach yn gallu gweithio, cymdeithasu a chyflawni tasgau o ddydd i ddydd.
| “ | “Doeddwn i ddim yn gallu dychwelyd i’r gwaith na fy mywyd arferol fel gadawodd fi yn wanychlyd iawn gan flinder cronig, a dysautonomia1, cur pen cronig, niwl yr ymennydd a chanolbwyntio gwael.” - Person sy'n byw gyda Long Covid |
Mae cael mynediad i ofal yn aml wedi bod yn hynod heriol i bobl sy’n byw gyda Long Covid. Rhannodd rhai sut yr oeddent yn teimlo nad oedd gan eu meddyg teulu ddiddordeb yn eu symptomau neu nad oeddent yn eu credu. Mewn sgyrsiau â meddygon teulu neu weithwyr gofal iechyd proffesiynol eraill, roeddent yn aml yn teimlo eu bod yn cael eu diswyddo. Weithiau, clywsom y byddai gweithwyr gofal iechyd proffesiynol yn awgrymu a/neu’n ceisio eithrio achos arall i’w symptomau megis problemau gyda’u hiechyd meddwl neu gyflyrau iechyd sy’n bodoli eisoes.
Roedd gennym ni feddygon teulu yn gwrthod credu mewn Covid Hir yma, gyda llawer o rai eraill ddim yn cael profion am symptomau.
Mae'r profiadau a rannwyd hefyd yn tynnu sylw at anghysondebau yn y modd y mae pobl â Long Covid wedi cael eu trin. Mae wedi bod yn boenus i'r rhai â symptomau parhaus sydd wedi cael eu trosglwyddo rhwng gwahanol rannau o'r system gofal iechyd heb dderbyn y gofal sydd ei angen, os o gwbl - yn aml tra'n sâl iawn. Disgrifiasant deimlo'n segur a diymadferth, ac yn ansicr ble i droi.
| “ | Does neb eisiau gwybod, dwi'n teimlo'n anweledig. Rwy'n cael fy nhrin fel difrod cyfochrog. Mae'r rhwystredigaeth a'r dicter rwy'n ei deimlo yn anhygoel; golau nwy meddygol, diffyg cefnogaeth a'r ffordd y mae pobl eraill yn fy nhrin, mae'r meddyg teulu yn dweud wrthyf fy mod yn rhy gymhleth, oherwydd mae gennyf gymaint o adweithiau meddyginiaeth."
- Person sy'n byw gyda Long Covid |
Cyfeiriwyd rhai yn ôl at eu meddyg teulu gan arbenigwyr ar gyfer profion pellach neu i drin symptomau eraill, tra bod eraill yn cael eu hatgyfeirio at glinigau Long Covid neu eu cyfeirio at gyrsiau ar-lein unwaith yr oedd y rhain wedi'u sefydlu mewn rhai ardaloedd o'r DU ddiwedd 2020. Rhai pobl yn byw gyda Long Covid yn gweld clinigau a chyrsiau ar-lein yn ddefnyddiol ond roedd llawer yn derbyn gofal gwael heb unrhyw gymorth na thriniaeth wedi'u teilwra.
| “ | Felly, rydym yn dal i deimlo ein bod yn cael ein hanfon at y meddyg teulu ac nid yw'r meddygon teulu yn gwybod beth i'w wneud â ni, mae meddygon teulu yn brysur gyda llawer o bethau eraill. Ac nid oes gan hyd yn oed y meddygon teulu sy'n cydymdeimlo â'r ewyllys gorau yn y byd unrhyw syniad beth i'w wneud â ni. Mae angen rhywbeth mwy arbenigol yn y bôn.”
- Person sy'n byw gyda Long Covid |
Clywsom hefyd am weithwyr gofal iechyd sydd wedi cael eu heffeithio, ac yn parhau i gael eu heffeithio gan Long Covid. Awgrymodd rhai cyfranwyr fod y ffaith bod gweithwyr gofal iechyd proffesiynol wedi datblygu Long Covid wedi lleihau gallu gwasanaethau gofal iechyd i ddarparu gofal heddiw.
Gwarchod
Dywedodd pobl a oedd yn agored i niwed yn glinigol ac yn glinigol hynod agored i niwed wrthym eu bod yn ofni Covid-19 yn fawr ac yn deall pam y gofynnwyd iddynt warchod. Fodd bynnag, roedd llawer yn rhannu pa mor anodd oedd dilyn y cyngor gwarchod a’r effeithiau negyddol a gafodd hyn arnyn nhw a’u teuluoedd.
Fe wnes i ymdopi trwy wneud pethau eraill ond pe bawn i wedi mynd ychydig yn hirach, ychydig mwy o wythnosau, rwy’n meddwl y byddwn wedi mynd dros y dibyn i fod yn onest â chi. Roeddwn i'n cyrraedd y cam lle nad oeddwn yn gallu ymdopi...a dim ond cael [fy mam] i siarad â hi mewn gwirionedd, roedd hynny'n beth mawr oherwydd roedd fy mywyd cyfan yn eithaf cymdeithasol. Roeddwn yn unig, a cheisiais beidio â gadael i hynny effeithio gormod arnaf. Gwnaeth fy ngyrru’n hollol wallgof.
Roedd pobl a oedd yn gwarchod yn rhannu sut roedd gwneud hynny’n aml yn arwain at arwahanrwydd, unigrwydd ac ofn. Roedd eu hiechyd corfforol a meddyliol yn aml yn gwaethygu. Mae rhai yn dal i deimlo ofn gadael y tŷ - iddyn nhw, nid yw'r pandemig drosodd.
| “ | Cwymp trefn arferol, dioddefodd iechyd meddwl, dioddefodd iechyd corfforol. Wnaeth hi [ei mam] ddim bwyta llawer a dweud y gwir, collodd lawer o bwysau oherwydd doedd hi ddim yn iach…ond do, felly roedd hi’n dioddef llawer o iechyd meddwl ac o ran iechyd corfforol oherwydd diffyg pobl eraill yn fwy na dim. unrhyw beth, diffyg unrhyw fath o ryngweithio.”
– Gofalwr am rywun a oedd yn hynod agored i niwed yn glinigol |
Gadawyd llawer yn sownd gartref yn teimlo'n gyfyng, yn bryderus neu wedi diflasu, ac mewn rhai achosion maent yn dal i fod. Fe wnaethant rannu pa mor rhwystredig oedd methu â gwneud ymarfer corff a gofalu am eu hiechyd yn iawn.
| “ | Roedd cael gwybod fy mod mewn cymaint o risg o Covid-19 yn gwneud i mi deimlo allan o reolaeth ar fy iechyd ac o dan straen aruthrol. Roeddwn i'n ofni y byddwn i'n marw pe bawn i'n dal Covid-19. Trwy warchod, y risg wirioneddol i mi oedd methu â rheoli fy nghyflwr iechyd, a dwi’n ei wneud yn bennaf trwy ymarfer corff.”
– Person a oedd yn hynod agored i niwed yn glinigol |
Roedd rhai cyfranwyr yn fwy cadarnhaol am warchod. Roedd hyn yn aml oherwydd eu bod yn gyfforddus gartref neu'n gallu cadw'n brysur ac yn gadarnhaol. Roedd gallu datblygu trefn gyda phethau ystyrlon i'w gwneud yn eu helpu i ymdopi.
| “ | Gyda chymorth gardd…cefais fy sbwylio am bethau i'w gwneud. Felly mae'n debyg bod hynny wedi fy arbed yn llwyr, o ran iechyd meddwl ... nid oedd yn effeithio cymaint arna i mae'n debyg, â rhywun mewn stad o dai neu, fflatiau uchel neu rywbeth, nad oedd â'r gofod hwnnw y tu allan i fynd iddo.”
– Person a oedd yn hynod agored i niwed yn glinigol |
Disgrifiodd rhai pobl sy’n hynod agored i niwed yn glinigol sut y maent yn dal i warchod oherwydd nad yw’r risgiau sy’n gysylltiedig â Covid-19 wedi diflannu er eu mwyn. Maent yn parhau i ofni cymysgu ag eraill ac yn aml wedi colli cysylltiad â'u cymunedau. Maen nhw eisiau mwy o gydnabyddiaeth bod effaith y pandemig yn parhau i'r rhai sy'n hynod agored i niwed yn glinigol.
Mae [un] o fy ffrindiau yn hŷn, mae hi yn ei 70au, nid yw wedi dod yn ôl i'r eglwys... does ganddi hi ddim bywyd cymdeithasol o gwbl bellach... ei her fwyaf yw'r ffaith ei bod yn teimlo ei bod yn cael y wybodaeth hon , sy'n dweud wrthi ei bod yn agored i niwed, bod angen iddi amddiffyn ei hun, bod angen iddi gadw draw oddi wrth bobl, ei bod mewn perygl, ac nad yw ei risg wedi newid, a bod Covid-19 yn dal i fod o gwmpas. Ac felly, mae hi'n ei chael hi'n anodd cysoni'r ffaith ei fod yn teimlo fel bod y cyngor wedi newid, ac eto, mae'r risg yn dal i fod yr un peth... Ac felly, rwy'n meddwl bod llawer o ofn, o hyd, wedi'i lapio o amgylch hynny i gyd am pobl.
Sut yr addasodd y system gofal iechyd
Yn ogystal â'r effaith ar gleifion a'u hanwyliaid, dywedodd gweithwyr gofal iechyd wrthym hefyd am eu profiadau yn ystod y pandemig. Disgrifiwyd y gwaith a wnaethant i barhau i gynnig gofal cystal ag y gallent, gyda llawer yn cyfeirio at y newidiadau enfawr a wnaed mewn lleoliadau gofal iechyd.
Dywedodd llawer o gyfranwyr sy'n gweithio ym maes gofal iechyd fod cyflymder y newid yn llawer cyflymach yn ystod y pandemig nag yr oeddent wedi'i brofi o'r blaen. Mae'r straeon a rannwyd gyda ni yn amlygu rhai tensiynau ac anghytundebau ymhlith gweithwyr gofal iechyd proffesiynol a achosir gan heriau gweithredu rheolau. Roedd y rhain yn aml rhwng y rhai sy'n gweithio'n uniongyrchol gyda chleifion a'r rhai mewn rolau rheoli neu uwch arweinyddiaeth. Er enghraifft, roedd rhai cyfranwyr o'r farn bod uwch arweinwyr yn aml yn aros am arweiniad gan y llywodraeth neu Ymddiriedolaethau'r GIG ar beth i'w wneud yn hytrach na chymryd camau rhagweithiol.
Clywsom hefyd fod rhai gweithwyr gofal iechyd proffesiynol yn cwestiynu’n gynyddol y sail ar gyfer canllawiau Covid-19 wrth i’r pandemig fynd rhagddo. Roedd y pryderon hyn yn aml yn canolbwyntio ar a oedd y canllawiau’n seiliedig ar dystiolaeth o’r hyn a weithiodd i atal haint.
Dywedodd gweithwyr gofal iechyd proffesiynol wrthym sut y daethant i wybod am ganllawiau drwy’r cyfryngau a’u cyflogwyr ac am y gwahaniaethau yn y ffordd y gweithredwyd canllawiau Covid-19 ar draws gwahanol rannau o’r gwasanaeth iechyd.
Offer amddiffynnol personol (PPE)
Dywedodd gweithwyr gofal iechyd ar draws gwahanol leoliadau wrthym nad oedd ganddynt y PPE yr oedd ei angen arnynt, yn enwedig ar ddechrau’r pandemig. Roedd dyluniad a ffit rhai PPE hefyd yn achosi problemau sylweddol, gan ei gwneud yn anoddach i rai wneud eu gwaith ac achosi anghysur.
| “ | Roedd gen i ffrindiau yn gweithio yn ICU yn gwisgo bagiau bin.”
– Nyrs gymunedol |
Roeddwn i'n arfer ei rolio hyd at fy ngwasg, cael ffedog a defnyddio'r ffedog fel gwregys, ac yna hongian beiro oddi ar hwnnw hefyd. Felly, nid oedd y maint yn wych ac yna rydych chi'n fwy nag yr ydych chi'n meddwl ydych chi ac rydych chi'n taro llawer o eitemau oherwydd bod gennych chi fwy o led arnoch chi.
Clywsom enghreifftiau o sut yr effeithiodd PPE a oedd yn ffitio’n iawn yn gorfforol ar rai staff pan oeddent yn ei wisgo am oriau lawer. Roedd hyn yn cynnwys enghreifftiau o frechau, sensitifrwydd croen a marciau argraff o wisgo masgiau am gyfnodau hir.
Roedd PPE hefyd yn gwneud cyfathrebu llafar rhwng gweithwyr gofal iechyd proffesiynol a chleifion yn fwy anodd. Roedd hon yn her arbennig i gleifion ag anghenion cyfathrebu ychwanegol, gan gynnwys pobl â nam ar eu clyw a phobl awtistig sy'n dibynnu ar fynegiant wyneb i gyfathrebu.
| “ | Rydych chi'n dweud, 'Rwy'n fyddar,' ac maen nhw'n siarad â chi trwy fwgwd, a byddaf yn dweud, 'Rwy'n fyddar.' Maen nhw, fel, 'O, na, na, ni allaf dynnu fy mwgwd. Efallai y byddwch chi'n rhoi Covid-19 i mi.' Rwy'n debyg, 'Wel, wyddoch chi, byddaf yn sefyll draw fan hyn, rydych chi'n sefyll draw acw. Tynnwch eich mwgwd i lawr, byddaf fwy na 2 fetr i ffwrdd,' ac fe wrthodon nhw o hyd. Roedd hynny’n anodd iawn ac yna’n llythrennol allwch chi ddim gweld eu ceg na’u hwyneb, felly does gennych chi ddim gobaith o’u deall.”
- Person byddar |
Roedd gan weithwyr gofal iechyd mewn gwahanol leoliadau argraffiadau cymysg o eglurder canllawiau a gofynion o ran profi. Roeddent yn cofio bod canllawiau hunan-ynysu yn arbennig o llym ar ddechrau'r pandemig, a oedd yn golygu nad oeddent yn gallu gweithio ar adegau pan oeddent yn iach.
Gofal sylfaenol
Roedd y rhai a oedd yn gweithio ym maes gofal sylfaenol yn aml yn rhannu sut roedd addasu i’r pandemig wedi bod yn heriol ac yn ei gwneud hi’n anoddach cynnig gofal da i gleifion. Serch hynny, bu iddynt fyfyrio ar faint y llwyddasant i newid a sut yr oedd hyn yn caniatáu iddynt ofalu am lawer o'u cleifion.
| “ | Fe wnaethon ni addasu, a dwi'n meddwl ein bod ni wedi newid. Rwy'n meddwl ein bod wedi gwneud yr hyn yr oedd yn rhaid i ni ei wneud. Roedd yn ddeinamig drwy'r amser a dweud y gwir, onid oedd? Roedd yn newid drwy’r amser, ac fe wnaethom ein gorau, rwy’n meddwl, i fynd i wneud yr hyn oedd yn rhaid i ni ei wneud.”
– nyrs meddyg teulu |
Teimlai rhai nad oedd meddygon teulu a fferyllwyr cymunedol yn cael eu hystyried yn briodol ac nad ymgynghorwyd â hwy, a bod yr ymateb pandemig mewn ysbytai yn cael ei flaenoriaethu. Roeddent yn rhwystredig ynghylch canllawiau a oedd yn newid yn gyflym, heb fawr o rybudd ac yn aml diffyg eglurder ynghylch sut yr oedd meddygfeydd teulu neu fferyllfeydd i fod i ymateb.
Clywsom am rai gwasanaethau meddygon teulu lleol yn cydweithio i rannu syniadau a chyfuno staff ac adnoddau, ac am 'ganolfannau Covid-19' i drin cleifion a lleihau derbyniadau i'r ysbyty. Roedd y dulliau hyn yn cael eu hystyried yn gadarnhaol ar y cyfan, gan roi mwy o hyder i’r rhai sy’n gweithio ym maes gofal sylfaenol wrth asesu a thrin Covid-19.
Myfyriodd meddygon teulu ar sut achosodd y pandemig rai problemau iechyd newydd. Er enghraifft, roedd rhai o’r farn bod pellhau cymdeithasol wedi arwain at fwy o arwahanrwydd, gan gyfrannu yn ei dro at fwy o faterion iechyd meddwl ymhlith eu cleifion.
Ysbytai
Clywsom gan weithwyr gofal iechyd am sut y gwnaeth ysbytai newidiadau i reoli’r mewnlifiad disgwyliedig o gleifion Covid-19. Dywedasant wrthym am y cynnwrf ar draws gwahanol rolau mewn ysbytai, nid ymhlith staff clinigol yn unig. Er bod rhai gweithwyr gofal iechyd yn gadarnhaol ynghylch y ffordd yr oedd yr ymateb yn cael ei reoli, dywedodd eraill nad oedd digon o ystyriaeth wedi'i rhoi iddo.
Gwnaed newidiadau enfawr. Ailddyrannu ardaloedd, ailddyrannu staff, pawb yn symud o le i le, newid yr hyn yr oeddent yn ei wneud.
| “ | Cafodd llawer o staff eu hadleoli i wahanol feysydd clinigol i ffwrdd o'r lle y maent fel arfer yn gweithio i gynorthwyo gyda'r ymateb i Covid - cafodd yr aelodau hyn o staff eu “taflu i mewn i'r pen dwfn” heb fawr o hyfforddiant ychwanegol a dim dewis ynghylch ble y cawsant eu hanfon. Cafodd hyn hefyd effaith ar lwybrau hyfforddi llawer o feddygon iau.”
-Meddyg ysbyty |
Roedd cynllunio a darparu gofal yn parhau i fod yn heriol yn ddiweddarach yn y pandemig. Rhannodd llawer o gyfranwyr sut y daeth gwneud newidiadau i ofal ysbyty yn fwy anodd oherwydd blinder staff a morâl isel. Disgrifiodd rhai ddiffyg cynllunio o ran sut i flaenoriaethu gofal nad yw'n ofal brys a thrin mwy o gleifion wrth i gyfyngiadau pandemig ddechrau lleddfu.
| “ | Nid oedd unrhyw gyngor ar sut i gamu'n ôl o unrhyw beth ac nid oedd unrhyw gymorth o gwbl i ddad-ddwysáu. Ac nid oedd yn teimlo, i ni, unrhyw synnwyr o ddysgu, 'Iawn, yr hyn a wnaethom yn y don gyntaf'.”
-Meddyg ysbyty |
Gofal brys a brys
Roedd pwysau aruthrol ar lawer o adrannau brys (EDs) yn ystod y pandemig, gyda heriau’n gysylltiedig ag addasrwydd adeiladau, prinder staff a chyfnodau o alw cynyddol am ofal brys. Roedd y pwysau oedd arnynt yn amrywio rhwng gwahanol adrannau achosion brys ac wedi newid ar wahanol gamau o'r pandemig.
Dywedodd llawer o'r rhai sy'n gweithio ym maes gofal brys nad oeddent ar adegau yn gallu cynnal rheolaethau heintiau oherwydd bod nifer fawr o gleifion a dim digon o le. Dywedodd rhai staff Adrannau Achosion Brys wrthym am orfod gwneud penderfyniadau ynghylch blaenoriaethu gofal a throsglwyddo cleifion i ofal dwys (ICU neu ITU), ac am ba mor anodd oedd y rhain oherwydd pa mor ddifrifol y gallent fod i gleifion.
| “ | Roedden ni’n cael ein gorfodi i chwarae Duw wrth benderfynu pwy oedd yn mynd i ITU – pwy gafodd newid i fyw a phwy oedd ddim.”
- Nyrs ysbyty |
Dywedodd cyfranwyr eraill a oedd yn gweithio mewn Adrannau Achosion Brys eu bod yn gweld llai o gleifion nag arfer ar adegau oherwydd bod pobl yn rhy ofnus i geisio triniaeth. Roedd llai o alw yn caniatáu i staff mewn rhai adrannau achosion brys dreulio mwy o amser yn gofalu am gleifion unigol nag yr oeddent yn gallu cyn y pandemig.
Dywedodd parafeddygon wrthym faint o bwysau oedd arnynt a faint y newidiodd eu rolau. Disgrifiasant aros y tu allan i ysbytai mewn ambiwlansys gyda chleifion sâl, yn aml am gyfnodau hir iawn. Roedd hyn yn golygu bod yn rhaid i barafeddygon ofalu am gleifion mewn ambiwlansys a rhybuddio staff ysbytai am newidiadau yn eu cyflwr.
Clywsom gan rai o’r rhai sy’n delio â galwadau 111 a 999 y GIG am y pwysau o orfod delio â nifer fawr o alwadau gan bobl bryderus a sâl iawn. Rhoesant enghreifftiau o'r problemau a achosir gan brinder ambiwlansys. Roedd hyn yn peri gofid arbennig i'r rhai sy'n delio â galwadau.
| “ | Byddent [galwyr] yn ein ffonio, a byddem fel, 'Ie, ond mae angen ambiwlans arnoch,' felly byddem yn mynd drwodd i ambiwlans, a byddent fel, 'Ond nid oes gennym ni ddim byd. i anfon.' Roedd hynny’n peri gofid.”
– triniwr galwadau GIG 111 |
Yr effaith ar y gweithlu gofal iechyd
Ysgogodd ymdeimlad o bwrpas a rennir lawer o weithwyr gofal iechyd proffesiynol yn ystod y pandemig. Ond dywedodd rhai fod yr ymdeimlad hwn o bwrpas wedi diflannu wrth i'r pandemig fynd yn ei flaen, gan gynyddu gorfoledd ymhlith staff wrth i donnau'r pandemig barhau.
| “ | Roeddech chi'n helpu pobl eraill. Roeddech mewn gwirionedd yn darparu gwasanaeth gwerthfawr. Fe wnaeth i chi deimlo'n falch o'r hyn wnaethoch chi."
- Fferyllydd ysbyty |
Rwy'n meddwl ar lefel bersonol, daeth yn anoddach ac yn anoddach. Fe wnaethoch chi flino mwy a mwy. Mae'n debyg ei fod wedi arwain at rywfaint o bryder. Anodd delio â phethau. Rwy’n meddwl mai dyna oedd yr heriau.
Yn aml roedd yn rhaid i staff sy'n gweithio ar draws gwahanol rolau ac mewn gwahanol rannau o systemau gofal iechyd ysgwyddo llwythi gwaith enfawr. Ychwanegodd hyn at eu swyddi oedd eisoes dan straen. Dywedodd gweithwyr gofal iechyd wrthym yn gyson fod cydweithwyr i ffwrdd yn sâl neu angen hunanynysu wedi ychwanegu at bwysau llwyth gwaith.
Clywsom fod staff yn cael eu hadleoli weithiau i leddfu’r pwysau ar dimau, ond dywedodd cyfranwyr ei bod yn heriol addysgu’r sgiliau arbenigol a’r arbenigedd sydd eu hangen i weithio mewn meysydd newydd yn gyflym. Er enghraifft, roedd nyrsys a drosglwyddwyd i weithio mewn ICUs Covid-19 yn rhannu rhai o'r profiadau rheng flaen mwyaf heriol.
| “ | Roeddwn i’n teimlo’n ddi-rym o gael fy ngorfodi i rolau anghyfarwydd heb hyfforddiant priodol.”
– Nyrs gymunedol i blant |
| “ | Roedd nyrs yr ICU yn goruchwylio … mewn gwirionedd yn gofalu am y claf, gan mai dim ond yn ei chynorthwyo yr oeddech chi, yn gwirio cyffuriau ac ati. y cwpl o ddyddiau cyntaf, ac yna y tu hwnt i hynny, chi oedd yn ei wneud mewn gwirionedd.”
- Nyrs ysbyty |
Rhannodd llawer o weithwyr gofal iechyd y cyfyng-gyngor moesegol yr oeddent yn ei wynebu ynghylch canllawiau Covid-19. Roedd y rhain yn aml yn benodol i’w rôl a’u profiad pandemig, ond roedd rhai themâu cyffredin. Er enghraifft, dywedodd rhai gweithwyr gofal iechyd proffesiynol nad oeddent yn dilyn canllawiau fel y gallent ddangos mwy o dosturi tuag at gleifion, teuluoedd a chydweithwyr.
Un o'r profiadau mwyaf gofidus a dirdynnol i lawer o weithwyr gofal iechyd oedd delio â marwolaeth ar raddfa nad oeddent erioed wedi dod ar ei thraws o'r blaen. Disgrifiodd rhai y niwed i'w hiechyd meddwl o ganlyniad. Roeddent yn dweud yn aml mai methu â gweld eu hanwyliaid oedd yn marw oedd un o'r pethau anoddaf yr oedd yn rhaid iddynt ymdopi ag ef.
Roedd fel parth rhyfel, dros nos daeth 18 o bobl yn bositif am Covid-19 heb unman i'w ynysu. Roeddent yn gollwng fel pryfed, roedd yn ofnadwy. Ni allwch ddiystyru'r hyn a wnaeth hyn i staff nyrsio, roedd methu â chynnig cysur i gleifion yn ddinistriol i'r enaid.
| “ | Daethom yn imiwn iddo. Fe wnaeth ein dad-ddyneiddio ni ychydig, rwy'n meddwl, ar y pryd. Teimlais hynny, a theimlais ei fod yn anodd delio ag ef.
– rheolwr practis meddyg teulu |
Pan oedd gweithwyr gofal iechyd proffesiynol yn profi sefyllfaoedd trallodus a phwysau llwyth gwaith, roedd rhai'n cael cynnig cymorth emosiynol, ac yn gwneud defnydd ohono. Roedd cymorth gan gymheiriaid o fewn timau hefyd yn bwysig i helpu staff i ymdopi â'r heriau yr oeddent yn eu hwynebu. Fodd bynnag, roedd hyn yn anghyson, ac nid oedd rhai gweithwyr gofal iechyd yn cael cynnig unrhyw gymorth gyda'u hiechyd meddwl.
| “ | “Rwy’n teimlo ein bod yn cael gwybod o hyd am yr hyn yr oedd yr ysbyty yn ei wneud ar gyfer staff a phethau, ond nid wyf yn meddwl eu bod erioed wedi gofyn i’r staff beth fyddai’n gwneud gwahaniaeth i fod yn y gwaith. Dwi’n meddwl mai dyna oedd y pethau bach hefyd, fel bydden nhw wedi dweud gallu parcio…gallu mynd am ginio mewn lle ymlacio.”
-Meddyg ysbyty |
Roedd rhai aelodau o staff yn dawelach, neu’n cael cyfnodau tawelach, yn ystod y pandemig oherwydd bod cleifion yn cadw draw neu oherwydd sut roedd gofal yn cael ei ad-drefnu. Er bod hyn fel arfer yn lleihau'r pwysau a'r straen uniongyrchol yr oeddent yn ei deimlo, roedd rhai'n teimlo'n euog bod gweithwyr gofal iechyd proffesiynol eraill dan fwy o straen. Roedd y rhai a oedd yn llai prysur hefyd yn poeni am y cleifion y byddent fel arfer yn eu gweld ac a oeddent yn cael y gofal a'r driniaeth yr oedd eu hangen arnynt.
Disgrifiodd rhai cyfranwyr effaith barhaol gweithio ym maes gofal iechyd yn ystod y pandemig. Fe wnaethant rannu sut roedd eu hiechyd meddwl bellach yn waeth nag y bu. Clywsom hefyd enghreifftiau o weithwyr proffesiynol a oedd wedi wynebu problemau personol fel tor-perthynas a oedd yn eu barn nhw o leiaf yn rhannol oherwydd eu profiadau yn y pandemig. Yn anffodus, dywedodd rhai gweithwyr gofal iechyd proffesiynol wrthym am orfod newid rolau neu roi’r gorau i weithio oherwydd cymaint y dirywiodd eu hiechyd meddwl yn ystod y pandemig.
| “ | Nid wyf yn meddwl fy mod wedi dod yn ôl i 100% o sut yr oeddwn fel arfer. Mae'n cymryd ei doll. Ond mae bron fel cael y darn hwn o bapur, sy'n neis, a fflat, ac yn syth, ac yna rydych chi wedi'i grychu ac yna rydych chi'n ceisio sythu'r darn hwnnw o bapur eto. Mae wedi cynyddu o hyd, ni waeth faint rydych chi'n ceisio ei sythu."
- Parafeddyg |
Ailadeiladu ymddiriedaeth mewn penderfyniadau am ofal iechyd
Rhannodd rhai cyfranwyr sut roedd eu hymddiriedaeth mewn systemau gofal iechyd wedi cael ei hysgwyd gan yr hyn a ddigwyddodd gan ddadlau bod hyn yn bryder i lawer ar draws cymdeithas. Roedd hyn yn aml yn ymwneud llai â'r gofal a gawsant gan weithwyr gofal iechyd proffesiynol unigol ac yn fwy am y penderfyniadau a wnaethpwyd ynghylch trefnu a darparu gofal.
Mae ymddiriedaeth mewn gwasanaethau gan y cyhoedd wedi mynd oherwydd y ffordd y cawsant eu trin yn y cloeon.
Mae llawer o'u rhesymau dros beidio ag ymddiried yn y penderfyniadau a wneir am ofal iechyd eisoes wedi'u hamlygu. Roeddent yn poeni am fynediad at ofal iechyd ac a fydd systemau gofal iechyd yn gallu gwella o'r pandemig. I lawer o gyfranwyr, roedd gwneud mwy i gadw ac ailadeiladu ymddiriedaeth y cyhoedd mewn gofal iechyd yn cael ei ystyried yn flaenoriaeth bwysig - nawr ac wrth ddelio â phandemigau ac argyfyngau yn y dyfodol.
Rhannodd miloedd o bobl eu profiadau am systemau gofal iechyd yn ystod y pandemig gyda ni. Yn yr adroddiad hwn rydym yn adeiladu ar y crynodeb hwn, gan amlygu’n fanylach y themâu allweddol o’r straeon a glywsom.
- Term ymbarél yw Dysautonomia sy'n disgrifio anhwylder ar y system nerfol awtonomig, sy'n rheoli swyddogaethau'r corff gan gynnwys rheoleiddio cyfradd curiad ein calon, pwysedd gwaed, tymheredd, treuliad ac anadlu. Pan fydd dadreoleiddio yn digwydd, gall y swyddogaethau hyn gael eu newid, gan arwain at ystod o symptomau corfforol a gwybyddol.
Adroddiad Llawn
1. Rhagymadrodd
Mae'r ddogfen hon yn cyflwyno'r straeon a rennir ag Every Story Matters yn ymwneud â systemau gofal iechyd y DU yn ystod y pandemig.
Cefndir a nodau
Mae Every Story Matters yn gyfle i bobl ledled y DU rannu eu profiad o’r pandemig ag Ymchwiliad Covid-19 y DU. Mae pob stori a rennir wedi'i dadansoddi a'i throi'n adroddiad â thema. Cyflwynir yr adroddiadau hyn i'r Ymchwiliad fel tystiolaeth. Wrth wneud hynny, bydd canfyddiadau ac argymhellion yr Ymchwiliad yn cael eu llywio gan brofiadau'r rhai yr effeithiwyd arnynt gan y pandemig.
Mae’r ddogfen hon yn dwyn ynghyd yr hyn a ddywedodd pobl wrthym am eu profiadau o systemau gofal iechyd y DU1 yn ystod y pandemig.
Mae Ymchwiliad Covid-19 y DU yn ystyried gwahanol agweddau ar y pandemig a sut yr effeithiodd ar bobl. Mae hyn yn golygu y bydd rhai pynciau yn cael sylw mewn adroddiadau modiwl eraill. Felly, nid yw'r holl brofiadau a rennir gyda Mae Pob Stori'n Bwysig wedi'u cynnwys yn y ddogfen hon. Er enghraifft, bydd profiadau o ofal cymdeithasol oedolion a’r effaith ar blant a phobl ifanc yn cael eu harchwilio mewn modiwlau diweddarach a’u cynnwys yn nogfennau Mae Pob Stori’n Bwysig yn y dyfodol.
Sut mae pobl yn rhannu eu profiadau
Rydym wedi casglu straeon pobl ar gyfer Modiwl 3 mewn sawl ffordd wahanol. Mae hyn yn cynnwys:
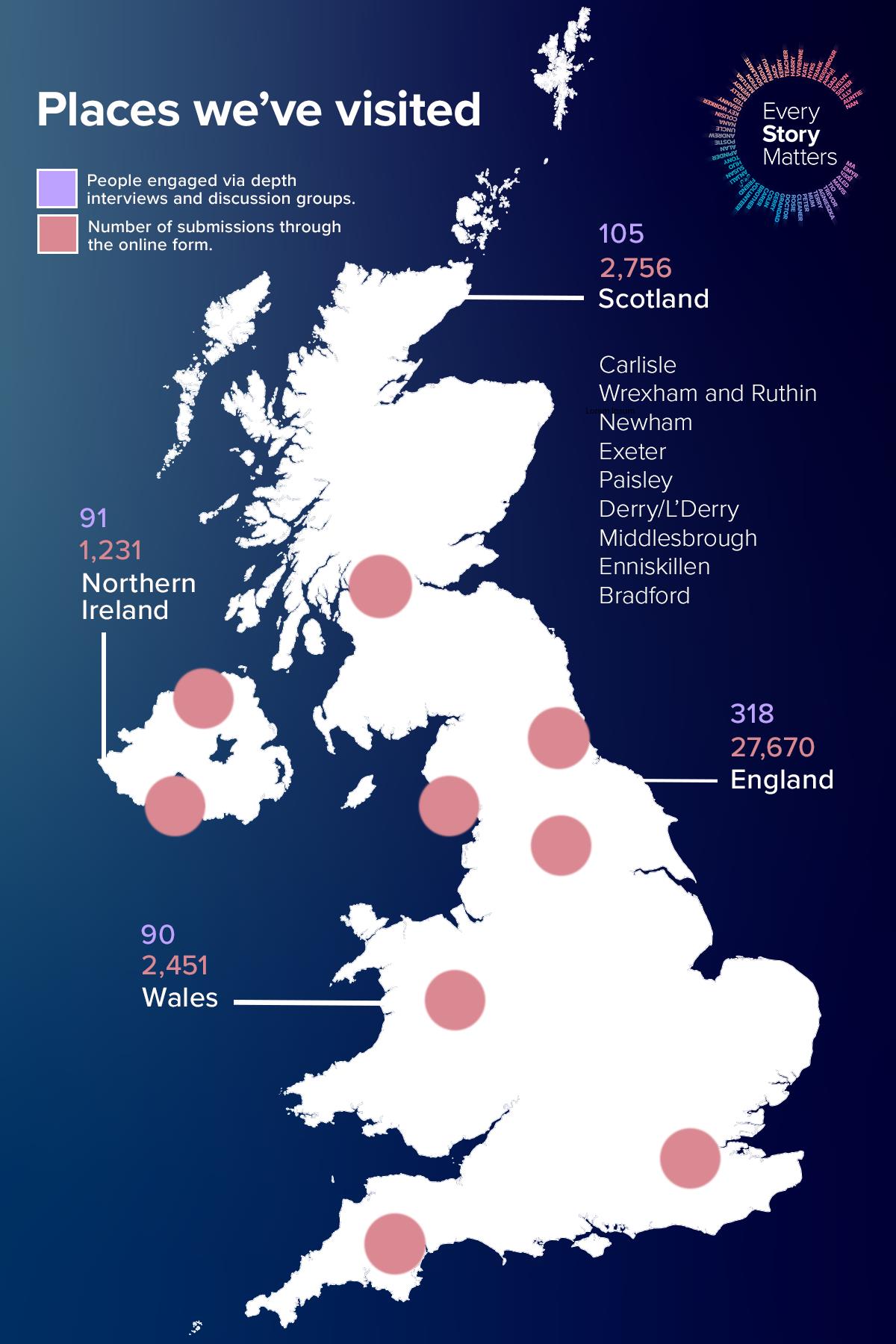
- Gwahoddwyd aelodau'r cyhoedd i lenwi ffurflen ar-lein trwy wefan yr Ymchwiliad (cynigiwyd ffurflenni papur hefyd i gyfranwyr a'u rhoi ar y ffurflen ar-lein i'w dadansoddi). Mae hyn yn caniatáu iddynt ateb tri chwestiwn eang, penagored am eu profiad pandemig. Mae'r ffurflen yn gofyn cwestiynau eraill i gasglu gwybodaeth gefndir amdanynt (fel eu hoedran, rhyw ac ethnigrwydd). Mae hyn yn caniatáu inni glywed gan nifer fawr iawn o bobl am eu profiadau pandemig. Mae'r ymatebion i'r ffurflen ar-lein yn cael eu cyflwyno'n ddienw. Ar gyfer Modiwl 3, dadansoddwyd 32,681 o straeon yn ymwneud â systemau gofal iechyd y DU. Mae hyn yn cynnwys 27,670 o straeon o Loegr, 2,756 o’r Alban, 2,451 o Gymru a 1,231 o Ogledd Iwerddon (roedd cyfranwyr yn gallu dewis mwy nag un wlad yn y DU ar-lein, felly bydd y cyfanswm yn uwch na nifer yr ymatebion a dderbyniwyd). Mae'r ymatebion wedi'u dadansoddi trwy brosesu iaith naturiol (NLP), sy'n defnyddio dysgu peirianyddol i helpu i drefnu'r data mewn ffordd ystyrlon. Yna defnyddir cyfuniad o ddadansoddiad algorithmig ac adolygiad dynol i archwilio'r straeon ymhellach.
- Tîm Mae Pob Stori yn Bwysig teithio i 17 o drefi a dinasoedd ledled Cymru, Lloegr, yr Alban a Gogledd Iwerddon, i roi cyfle i bobl rannu eu profiad pandemig yn bersonol yn eu cymunedau lleol. Cynhaliwyd sesiynau gwrando rhithwir hefyd lle'r oedd y dull hwnnw'n cael ei ffafrio. Buom yn gweithio gyda llawer o elusennau a grwpiau cymunedol llawr gwlad (a restrir yn y cydnabyddiaethau isod) i siarad â'r rhai yr effeithiwyd arnynt gan y pandemig mewn ffyrdd penodol. Mae hyn yn cynnwys teuluoedd mewn profedigaeth, pobl sy'n byw gyda Long Covid a PIMS-Ts, teuluoedd sy'n agored i niwed yn glinigol, pobl anabl, ffoaduriaid, pobl o gefndiroedd lleiafrifoedd ethnig a gweithwyr gofal iechyd proffesiynol. Ysgrifennwyd adroddiadau cryno ar gyfer pob digwyddiad, eu rhannu â chyfranogwyr y digwyddiad, a'u defnyddio i lywio'r ddogfen hon.
- Comisiynwyd consortiwm o bartneriaid ymchwil cymdeithasol ac ymgysylltu â’r gymuned gan Every Story Matters i’w gynnal cyfweliadau manwl a grwpiau trafod gyda'r rhai yr effeithir arnynt fwyaf gan y pandemig a'r rhai sy'n llai tebygol o ymateb mewn ffyrdd eraill. Roedd y cyfweliadau a’r grwpiau trafod hyn yn canolbwyntio ar y Prif Linellau Ymholi (KLOEs) ar gyfer Modiwl 3. Yn gyfan gwbl, cyfrannodd 604 o bobl ledled Cymru, Lloegr, yr Alban a Gogledd Iwerddon fel hyn rhwng Chwefror 2023 a Chwefror 2024. Mae hyn yn cynnwys 450 o gyfweliadau manwl â :
-
- Pobl yr effeithir yn uniongyrchol arnynt gan Covid-19.
- Pobl yr effeithir arnynt yn anuniongyrchol gan Covid-19.
- Gweithwyr gofal iechyd proffesiynol a staff cymorth.
- Grwpiau proffesiynol eraill sy'n gweithio yn y system gofal iechyd.
Ymgysylltwyd â 154 o bobl eraill o gymunedau y gwyddys eu bod yn profi anghydraddoldebau iechyd drwy allgymorth cymunedol. Helpodd y grwpiau trafod cymunedol a chyfweliadau hyn i sicrhau bod yr Ymchwiliad yn clywed gan bobl na fyddai'n bosibl eu cyrraedd mewn ffyrdd eraill. Roedd y bobl y siaradom â nhw yn cynnwys:
-
- Pobl o gefndir ethnig lleiafrifol.
- Pobl ag anabledd gan gynnwys nam ar y golwg, nam ar y clyw a'r rheini
ag anabledd dysgu. - Pobl o ardaloedd mwy difreintiedig yn y DU.
Cafodd yr holl gyfweliadau manwl a grwpiau trafod eu recordio, eu trawsgrifio, eu codio a'u dadansoddi trwy adolygiad dynol i nodi themâu allweddol sy'n berthnasol i Modiwl 3 KLOEs.
Mae nifer y bobl a rannodd eu straeon ym mhob gwlad yn y DU drwy’r ffurflen ar-lein, digwyddiadau gwrando a chyfweliadau ymchwil a grwpiau trafod i’w gweld isod:
Ffigur 1: Ymgysylltiad Mae Pob Stori o Bwys ledled y DU
I gael rhagor o wybodaeth am sut y gwnaethom wrando ar bobl a’r dulliau a ddefnyddiwyd i ddadansoddi straeon, gweler yr atodiadau.
Nodiadau am gyflwyniad a dehongliad straeon
Mae’n bwysig nodi nad yw’r straeon a gasglwyd drwy Every Story Matters yn cynrychioli’r holl brofiadau o ofal iechyd y DU yn ystod y pandemig nac o farn gyhoeddus y DU. Effeithiodd y pandemig ar bawb yn y DU mewn gwahanol ffyrdd, ac er bod digwyddiadau a ffeithiau allweddol, rydym yn cydnabod pwysigrwydd profiad unigryw pawb o'r hyn a ddigwyddodd. Nod yr adroddiad hwn yw adlewyrchu'r gwahanol brofiadau a rannwyd gyda ni heb gysoni'r amrywiad neu'r cyfrifon gwahanol.
Rydym wedi ceisio adlewyrchu’r amrywiaeth o straeon a glywsom, a all olygu bod rhai straeon a gyflwynir yma yn wahanol i’r hyn a brofodd pobl eraill yn y DU, ac weithiau’n cyferbynnu â chonsensws neu dystiolaeth wyddonol. O ystyried hyn, mae'r adroddiad hwn yn ceisio darparu cydbwysedd, naws, a chyd-destun o amgylch y straeon a rennir gyda ni.
Archwilir rhai straeon yn fanylach trwy ddyfyniadau ac astudiaethau achos. Mae'r rhain wedi'u dewis i dynnu sylw at y gwahanol fathau o brofiadau y clywsom amdanynt a'r effaith a gafodd y rhain ar bobl. Mae'r dyfyniadau a'r astudiaethau achos yn helpu i seilio'r adroddiad ar yr hyn a rannodd pobl yn eu geiriau eu hunain. Mae'r cyfraniadau wedi'u gwneud yn ddienw. Rydym wedi defnyddio ffugenwau ar gyfer astudiaethau achos sydd wedi'u tynnu o'r cyfweliad manwl a'r grwpiau trafod. Mae astudiaethau achos yn seiliedig ar brofiadau a rennir mewn ffyrdd eraill wedi'u gwneud yn ddienw.
Drwy gydol yr adroddiad, rydym yn cyfeirio at bobl a rannodd eu straeon gyda Every Story Matters fel 'cyfranwyr'. Lle bo'n briodol, rydym hefyd wedi disgrifio mwy amdanynt (er enghraifft, gwahanol fathau o staff sy'n gweithio ym maes gofal iechyd) neu'r rheswm pam y bu iddynt rannu eu stori (er enghraifft fel cleifion neu anwyliaid) i helpu i egluro cyd-destun a pherthnasedd eu profiad.
Yn ogystal â rhannu eu profiadau, gofynnwyd i gyfranwyr fyfyrio ar yr hyn y gall yr Ymchwiliad ei ddysgu o'u profiad. Canolbwyntiodd rhai ar sut y dylid bod wedi ymdrin yn well â phroblemau penodol a wynebwyd ganddynt. Rhannodd eraill yr hyn a oedd wedi mynd yn dda yn eu barn nhw. Clywsom rai themâu eang ar draws eu myfyrdodau, a chaiff y rhain eu hamlygu drwy gydol yr adroddiad.
Mae’n amlwg o’r straeon bod rhai a ymatebodd yn llawn cymhelliant i wneud hynny. Am y rheswm hwn, ni ddylid ystyried bod dadansoddiad o ymatebion i’r ffurflen ar-lein yn gynrychioliadol o brofiadau’r cyhoedd o’r pandemig yn ehangach. Yn lle hynny, maen nhw’n adlewyrchu profiadau’r rhai a ddewisodd rannu eu stori gyda Every Story Matters.
Strwythur yr adroddiad
Mae'r ddogfen hon wedi'i strwythuro i alluogi darllenwyr i ddeall sut yr effeithiodd y pandemig ar wahanol rannau o'r system gofal iechyd a grwpiau penodol o bobl.
Mae’n dechrau drwy archwilio profiadau mewn Gofal Sylfaenol (Pennod 2), Ysbytai (Pennod 3 a 4), a Gofal Argyfwng a Brys (Pennod 5). Yna mae’r adroddiad yn edrych ar effeithiau sy’n gysylltiedig â phrofion PPE a Covid-19 (Pennod 6), profiadau o ganllawiau’r llywodraeth a’r sector gofal iechyd (Pennod 7) ac effaith y pandemig ar weithwyr gofal iechyd proffesiynol (Pennod 8).
Yna mae’r ddogfen yn troi at brofiadau penodol o ofal iechyd yn ystod y pandemig, gan gynnwys gofal diwedd oes a phrofedigaeth (Pennod 9), Long Covid (Pennod 10), Gwarchod (Pennod 11) a’r defnydd o wasanaethau mamolaeth (Pennod 12).
- Rydym wedi cyfeirio at systemau gofal iechyd y DU yn hytrach na’r GIG lle bo modd drwy gydol yr adroddiad hwn er mwyn adlewyrchu’r gwahaniaethau yn y systemau gofal iechyd ar draws pedair gwlad y DU.
2. Gofal sylfaenol: profiadau gweithwyr gofal iechyd proffesiynol a chleifion |
 |
Gofal sylfaenol fel arfer yw'r pwynt cyswllt cyntaf pan fydd angen cyngor neu driniaeth iechyd ar bobl, ac mae'n gweithredu fel 'drws ffrynt' i systemau gofal iechyd. Mae gofal sylfaenol yn cynnwys practis cyffredinol, fferylliaeth gymunedol, deintyddol. Yn y bennod hon rydym yn rhannu’r straeon a glywsom gan feddygon teulu, nyrsys meddygon teulu, rheolwyr practis, a fferyllwyr cymunedol ochr yn ochr â phrofiadau cleifion o gael mynediad at wasanaethau gofal sylfaenol a’u defnyddio.
Ymateb i'r pandemig
Roedd camau cynnar y pandemig yn ddryslyd ac yn peri straen i feddygon teulu, fferyllwyr cymunedol ac eraill mewn gofal sylfaenol. Roedd cyfranwyr a oedd yn gweithio ym maes gofal sylfaenol yn ei chael yn heriol oherwydd eu bod am barhau i ofalu am eu cleifion, ond nid oedd llawer o eglurder ynghylch sut y dylent ymateb.
Gan fyfyrio ar eu profiad, dywedodd llawer o gyfranwyr nad oedd cynllunio strategol ar gyfer gofal sylfaenol wedi bod yn ddigon da. Roedd rhai o'r farn bod y llywodraeth a sefydliadau gofal iechyd lleol yn araf i ymateb, heb fawr o gyngor. Roedd y cyfranwyr hyn yn rhwystredig oherwydd nad oedd ganddynt y cymorth yr oedd ei angen arnynt pan ddechreuodd y pandemig.
| “ | Rwy'n meddwl lle'r oedd gan ysbytai gynlluniau torfol a chynlluniau brys, o fewn gofal sylfaenol roedd yn dameidiog ac yn ddatgymalog iawn ac, 'O, chi sydd i benderfynu.' Ac rwy'n cael hynny, ond roedd yn anodd ei wneud.”
– rheolwr practis meddyg teulu |
Teimlai cyfranwyr fod cynllunio brys yn canolbwyntio mwy ar ysbytai yn hytrach na gofal sylfaenol, oherwydd gallai newidiadau gael eu rheoli'n ganolog mewn ysbytai.
| “ | Rwy'n meddwl lle'r oedd gan ysbytai gynlluniau torfol a chynlluniau brys, o fewn gofal sylfaenol roedd yn dameidiog ac yn ddatgymalog iawn ac, 'O, chi sydd i benderfynu.' Ac rwy'n cael hynny, ond roedd yn anodd ei wneud.”
– rheolwr practis meddyg teulu |
Fodd bynnag, dywedodd llawer o feddygon teulu wrthym fod annibyniaeth practisau meddygon teulu yn caniatáu iddynt newid eu gwasanaethau’n gyflym a herio awgrymiadau byrddau iechyd nad oeddent yn credu eu bod o gymorth. Dywedodd y cyfranwyr hyn eu bod wedi gallu datblygu dulliau o ddarparu gwasanaethau a oedd yn gweddu i'r cyd-destun lleol.
| “ | Mae meddygon teulu yn griw eithaf dyfeisgar, arloesol o bobl. Rwy'n meddwl bod hynny'n cael ei helpu yn ôl pob tebyg gan eu bod yn cael eu busnesau eu hunain, maent yn cydnabod 'mae yna sefyllfa ac mae angen inni ddod o hyd i ateb'.”
- Meddyg Teulu |
Wrth i amser fynd yn ei flaen, rhannwyd mwy o arweiniad, ond dywedodd llawer fod hyn wedi dod yn llethol. Dywedodd staff gofal sylfaenol wrthym ei bod yn amhosibl cadw i fyny â phopeth a ddywedwyd wrthynt a gweithredu arno.
| “ | Roedd pethau swyddogol gan y bwrdd iechyd yn araf iawn… weithiau roedd gan yr e-bost hwnnw 20 atodiad iddo, a fyddai’n cael ei anfon allan am, fel, 7 o’r gloch ar nos Fawrth neu rywbeth chwerthinllyd, pan nad oedd yr un ohonom yn y gwaith. A byddech chi'n mynd i mewn ar fore Mercher ... a byddai disgwyl i chi fynd drwodd, cymathu, trefnu a gweithredu o fewn, yn eithaf aml, 24 awr neu lai. Roedd yn amhosibl.”
- Meddyg Teulu |
| “ | Mae'n debyg bod gen i tua 20 o ganllawiau gwahanol ar gyfartaledd i'w darllen yn ddyddiol yn y gwaith. Ar ddiwedd y dydd, roeddem yn canolbwyntio mwy ar ddarllen y canllawiau hyn nag yr oeddem ar weithredu dros ein cleifion mewn gwirionedd. Cymerodd lawer o amser clinigol gwerthfawr a phrofiad y claf.”
– nyrs meddyg teulu |
Dywedodd rhai cyfranwyr sy'n gweithio ym maes gofal sylfaenol eu bod yn gwneud defnydd o sefydliadau neu unigolion a ddaeth â gwybodaeth berthnasol ynghyd mewn un lle ar gyfer meddygon teulu. Roedd hyn yn eu helpu i ymdopi â’r newid cyson a’r ansicrwydd, ac yn golygu eu bod yn teimlo’n fwy hyderus ynghylch cadw’r cyhoedd yn ddiogel.
| “ | Dechreuodd [Yr Ymddiriedolaeth GIG leol] wneud cylchlythyr a oedd yn crynhoi’r holl e-byst gwahanol i lawr…felly roedd yn golygu y gallem fynd i’r cylchlythyr a chael gwybodaeth gryno… Pe bai hynny wedi dechrau [yn gynharach], efallai na fyddwn wedi fy llethu neu’n poeni cymaint fy mod wedi colli rhywbeth.”
– rheolwr practis meddyg teulu |
| “ | Yn amlwg, cawsom e-byst gan yr awdurdod iechyd ynghylch pa PPE yr oedd yn rhaid i ni ei wisgo a phethau felly ar gyfer rhai gweithdrefnau... hefyd mae gennym uwch ymarferydd nyrsio a oedd yn arfer cydlynu pethau'n eithaf da. Rwy'n credu iddo gael ei gyfleu'n eithaf da. Rwy'n credu nad oedd y cyfathrebu'n ddrwg.”
– nyrs meddyg teulu |
Newidiadau i wasanaethau gofal sylfaenol
Rhannodd cyfranwyr sut yng nghamau cynnar y pandemig Symudodd gwasanaethau meddygon teulu i gyflenwi o bell i leihau'r risgiau o ledaenu Covid-19. Roedd hyn yn golygu bod cleifion - o leiaf ar y dechrau - fel arfer yn cael eu cyfyngu i ymgynghoriadau ar-lein a thros y ffôn.
Wrth i'r pandemig fynd rhagddo, Parhaodd meddygon teulu i addasu a darparu mwy o wasanaethau wyneb yn wyneb lle bo modd. Dywedodd rhai wrthym fod y mesurau sydd eu hangen ar gyfer rheoli heintiau yn golygu ei bod yn amhosibl hyd yn oed yn ddiweddarach yn y pandemig i gynnig yr un mynediad i wasanaethau i gleifion â chyn-bandemig.
| “ | Roedd yn rhaid archebu lle, roedd yn rhaid iddynt hefyd gael eu tymheredd wedi'i wirio a'r math hwnnw o beth, nid oedd mynediad at wasanaethau cystal, yn sicr. Oedd, roedd hyfforddiant cynllunio at argyfwng a pharhad busnes, ond nid wyf yn gwybod bod unrhyw un yn gwybod beth yr oeddent yn delio ag ef.”
– rheolwr practis meddyg teulu |
Roedd practisau meddygon teulu a oedd wedi sefydlu ffyrdd o weithio o bell a brysbennu cleifion dros y ffôn cyn y pandemig mewn sefyllfa well i ymateb. Nid oedd gan bractisau meddygon teulu eraill y systemau hyn ar waith ac roedd yn rhaid iddynt ddod o hyd i ffyrdd dros dro o symud i weithio o bell ar ddechrau'r pandemig.
| “ | Roedd y rhan fwyaf o bractisau’n gweithio systemau apwyntiadau syml…roedd yn rhaid i feddygon teulu eraill sefydlu’r system yr oeddem wedi bod yn ei rhedeg ers tair blynedd dros nos.”
- Meddyg Teulu |
| “ | Roedd rhai achosion pan nad oedd pobl erioed wedi meddwl y byddai angen iddynt weithio gartref ... roedd yn rhaid iddynt ddod i'r maes parcio lle gallent gael derbyniad gan Wi-Fi y GIG ac roeddent yn gallu mewngofnodi ar y gliniaduron oherwydd eich bod chi methu mynd â'ch gliniadur gartref a mewngofnodi.”
- Meddyg Teulu |
Adlewyrchiad cyffredin ymhlith y rhai sy’n gweithio ym maes gofal sylfaenol oedd pwysigrwydd rhwydweithiau anffurfiol i gefnogi’r ymateb pandemig. Datblygwyd y rhwydweithiau hyn i fynd i'r afael â heriau niferus darparu gofal i gymunedau lleol. Roedd cyfranwyr sy’n gweithio ym maes gofal sylfaenol yn aml yn ymuno â grwpiau WhatsApp a Facebook lle gallent rannu gwybodaeth a chyngor ag eraill a oedd yn gwneud newidiadau tebyg i ddarparu gofal. Roedd y grwpiau hyn yn gweithredu fel ffynonellau cymorth pan oeddent yn gweld eu gwaith yn heriol neu'n ansicr ynghylch y ffordd orau o addasu gwasanaethau.
| “ | Rydyn ni i gyd yn ceisio dehongli'r un wybodaeth, a phan fydd manylebau'n agored i'w dehongli, mae hynny'n broblem ... roedden ni'n gallu gwneud trwy grwpiau WhatsApp a sefydlwyd gennym ni fel y gallem ofyn cwestiynau i'n gilydd a rhannu'r wybodaeth honno.”
– rheolwr practis meddyg teulu |
Stori AlaraMae Alara yn feddyg teulu sy'n gweithio mewn practis trefol prysur lle roedd cleifion yn aml yn galw heibio pan oedd angen apwyntiad arnynt neu i godi presgripsiynau. Newidiodd hyn i gyd ar ddechrau'r pandemig. “Yn sydyn, roedd y ganolfan med, a oedd yn gyfleus iawn ac yn hawdd iawn i alw heibio iddi, ar gau. Roedd y cyfan yn hysbysiadau mawr ar y drws a phopeth dros y ffôn. Ac roedd yn rhaid i ni addasu’n gyflym i ffordd newydd o weithio.” Gan weithio gyda phractisau lleol eraill, datblygodd practis Alara borth ymgynghori ar-lein, lle gallai cleifion gyflwyno a lanlwytho ffotograffau yn ogystal ag ateb y cwestiynau gosod. Yna gwelwyd cleifion trwy ymgynghoriadau ffôn. “Roedd y trothwy ar gyfer gweld rhywun wyneb yn wyneb yn llawer, llawer uwch, a chafodd unrhyw un a oedd yn dod ei sgrinio wrth iddynt gyrraedd a chymerwyd eu tymheredd. A phob cyswllt â chlaf, byddem yn rhoi PPE lefel 2 ymlaen, heblaw am yr amser pan oeddem yn gweithio yn y canolfannau Covid-19, lle’r oedd gennym gleifion â symptomau Covid-19 posibl, PPE lefel 3, ac roedd yn teimlo ei fod yn llawer. amgylchedd mwy diogel.” |
Ymunodd rhai cyfranwyr hefyd â gweminarau a chyfarfodydd rhithwir gyda chydweithwyr o wasanaethau gofal iechyd eraill. Roedd hyn yn caniatáu iddynt drafod newidiadau i wasanaethau a gweithio allan sut olwg fyddai ar wahanol ddulliau. Roedd y sesiynau hyn yn caniatáu i syniadau gael eu rhannu'n gyflym ac yn helpu practisau meddygon teulu i addasu.
Dywedodd rhai practisau meddygon teulu wrthym eu bod yn cynnig ymgynghoriadau wyneb yn wyneb cymaint â phosibl. Roedd hyn yn aml yn golygu symud i apwyntiadau a drefnwyd ymlaen llaw i reoli nifer y cleifion a lleihau risgiau heintiau. Disgrifiodd rhai sut y maent yn sefydlu 'ystafelloedd ymateb brys' gyda PPE gradd uwch yn hygyrch i staff, gan ganiatáu i gleifion â symptomau Covid-19 gael eu trin ar unwaith. Newidiodd meddygon teulu eraill y mathau o ofal yr oeddent yn ei gynnig i gleifion mewn ymateb i ofnau cleifion o fynd i'r ysbyty.
| “ | Roeddwn i a meddyg teulu arall yn cymryd y rhan fwyaf o'r risg drwy weld 10% o cleifion wyneb yn wyneb a'r gweddill dros y ffôn. Roedd hi hefyd ymweld â chleifion yn llawer amlach, yn enwedig yr henoed i ddarparu gwrthfiotig IVs nad oedd eisiau mynd i'r ysbyty.”
- Meddyg Teulu |
Roedd y fferyllwyr cymunedol y clywsom ganddynt yn adlewyrchu sut yr oedd pobl yn troi atynt am gymorth pan nad oeddent yn gallu cysylltu â’u meddyg teulu neu wasanaethau gofal iechyd eraill. Roedd hyn yn golygu bod rhai fferyllfeydd cymunedol wedi’u gorlethu â chleifion yr oedd angen cymorth arnynt, gyda chiwiau hir a llawer mwy o alwadau ffôn nag yr oeddent yn arfer â chyn y pandemig.
| “ | Gan fod meddygon yn cau i lawr, o, fy Nuw, daeth yn hysteria. Cawsom ddyddiau [lle] roedd 80 neu 90 o bobl yn ciwio [tu allan i’r fferyllfa].”
– Fferyllydd cymunedol |
| “ | Mae'r galwadau ffôn, lle'r oeddem yn arfer cael, dyweder, 50 o alwadau ffôn mewn diwrnod, cynyddodd y galwadau ffôn i 150. Ni ddaeth y ffôn i ben. Mae un [o’n] fferyllfeydd wedi’i lleoli mewn canolfan feddygol, ond roeddem yn dal i weithredu felly daeth llawer o bobl atom yn lle hynny.”
– Fferyllydd cymunedol |
Dywedodd rhai fferyllwyr wrthym eu bod hwythau hefyd wedi’i llethu gan y galw am ddosbarthu meddyginiaethau i gartrefi pobl yn ystod y pandemig, gan greu pwysau ychwanegol sylweddol. Roedd rhai’n cael eu cefnogi gan eu hawdurdod lleol neu wirfoddolwyr i gadw i fyny â’r galw. Rhannodd llawer sut mae ganddyn nhw fwy o ddanfoniadau o hyd nawr nag oedd cyn y pandemig.
| “ | Cyn i ni gael 10 danfoniad y dydd. Cynyddodd y danfoniadau o hynny i 50-60 danfoniad y dydd. Fe wnaeth y cyngor helpu, ac roedd yna dri neu bedwar o bobl ddosbarthu oedd yn arfer dod, a gwirfoddolwyr oedd eisiau helpu… [Mae danfoniadau] dal i fyny, ac rydyn ni nawr yn cadw gyrrwr.”
– Fferyllydd cymunedol |
Barn cleifion ar y newidiadau i wasanaethau gofal sylfaenol
Roedd cleifion yn gefnogol ar y cyfan ac yn deall y newidiadau i ofal sylfaenol yn ystod y pandemig ac roeddent yn ymwybodol o'r pwysau oedd ar feddygon teulu. Yr oedd cyfranwyr hefyd yn werthfawrogol iawn o wasanaethau fferylliaeth gymunedol, a’r ymdrechion a wneir i gyflenwi meddyginiaethau.
Fodd bynnag, roedd llawer o gleifion yn rhwystredig, yn enwedig ynghylch pa mor hir y bu'n rhaid iddynt aros am apwyntiadau meddyg teulu. Roedd y cyfranwyr hyn yn dadlau nad oedd cau meddygfeydd meddygon teulu yn gwneud synnwyr pan oedd angen enfawr am eu gwasanaethau. Clywsom lawer o enghreifftiau o fethu â chael mynediad at y gofal yr oedd ei angen arnynt, a oedd yn aml yn eu gwneud yn bryderus ac yn siomedig.
| “ | Roedd bron yn teimlo fel cadw pobl i ffwrdd o’r arferion, dull ‘cael ymlaen â’r peth’ yn hytrach na dull cynorthwyol, nad wyf yn eu beio amdano oherwydd mae’n rhaid ei fod wedi bod yn ofnadwy.”
– claf meddyg teulu |
| “ | Roedd yn anodd siarad â meddyg teulu, hyd yn oed ar y ffôn yn delio â materion anadlol, i ddechrau a thros y 2 flynedd gyntaf.”
– claf meddyg teulu |
| “ | Nid oedd angen cau'r practisau meddygon teulu a lleihau hynny. Rwy'n meddwl y gallai llawer o bobl fod wedi cael eu gweld o hyd, pobl sydd â lympiau a thwmpathau neu sydd angen tynnu pethau. Rwy’n meddwl y gallent fod wedi delio â hynny. Rwy’n meddwl efallai y gallai hynny fod wedi achub ychydig o fywydau hefyd.”
– claf meddyg teulu |
Dywedodd llawer o gleifion hefyd eu bod yn falch iawn pan gynigiwyd ymgynghoriadau wyneb yn wyneb eto, yn enwedig ar gyfer cleifion hŷn. Fodd bynnag, teimlai rhai fod y mesurau diogelwch Covid-19 a ddefnyddiwyd wedi achosi problemau eraill, gan ddisgrifio cleifion yn aros y tu allan neu’n cael asesiadau yn yr awyr agored.
| “ | Yn wreiddiol, gwrthodwyd i mi gael fy ngweld gan fy meddyg teulu a’r unig ffordd yr aseswyd fy nghyflwr oedd fy anfon i faes parcio’r feddygfa lle mae nyrs yn cynnal yr archwiliad o weld y cyhoedd yn cerdded heibio.”
– claf meddyg teulu |
Maes arall a oedd yn peri rhwystredigaeth i lawer o gyfranwyr oedd faint o’r newidiadau i ofal sylfaenol a wnaed yn ystod y pandemig ymddangos yn barhaol.
| “ | Mae apwyntiadau meddygon teulu wedi’u newid am byth – nawr rydyn ni’n cael galwad ffôn neu ymgynghoriad fideo yn hytrach na chael ein harchwilio’n bersonol.”
– claf meddyg teulu |
Heriau ymgynghoriadau o bell
Myfyriodd cleifion a chlinigwyr ar yr heriau a’r pryderon sylweddol roedd ganddynt gyda phractisau meddygon teulu yn cau ac yn symud i apwyntiadau o bell. Rhannodd rhai cleifion pa mor ddefnyddiol oedd apwyntiadau o bell yn ystod y pandemig, gan mai nhw yn aml oedd yr unig fath o gyngor a chymorth y gallent gael mynediad ato. Fodd bynnag, roedd llawer o rai eraill yn anhapus fel nad oeddent wedi'u hargyhoeddi y gallai eu symptomau gael eu hasesu'n iawn oni bai eu bod yn gweld rhywun yn bersonol.
Dywedodd rhai wrthym hefyd eu bod yn ei chael yn anodd disgrifio eu symptomau dros y ffôn neu ar-lein. Ar draws y straeon a rannwyd gyda ni, roedd llawer o enghreifftiau o problemau difrifol yn cael eu methu yn ystod ymgynghoriadau o bell, yn aml gyda chanlyniadau difrifol i iechyd pobl.
| “ | Roedd oedi wrth symud canser y croen gan fy modryb ac roedd yn ofnus iawn. Gwnaeth y meddyg teulu apwyntiad ffôn a gwnaeth ddyfarniad nad oedd yn ddim byd difrifol trwy edrych ar lun. Roedd yn anghywir.”
– claf meddyg teulu |
Roedd llawer o gyfranwyr yn bryderus iawn am berthnasau hŷn yn cael eu cyfeirio at wasanaethau ar-lein neu dros y ffôn. Disgrifiwyd yr heriau difrifol a wynebwyd gan eu perthnasau.
| “ | Yn ystod y cloi cyntaf yn 2020 roedd y fam (75 oed) yn cael anawsterau anadlu. Daeth yn rhwystredig gyda'i meddyg teulu oherwydd y diffyg apwyntiadau wyneb yn wyneb. Dros nifer o fisoedd cafodd apwyntiadau ffôn a rhagnodwyd amryw o wahanol anadlyddion a steroidau ar gyfer asthma nad oedd yn gweithio. Teimlai pe bai'r meddyg yn ei gweld yn bersonol ac yn gwrando ar ei brest y byddai'n helpu i ganfod y ... yn lle gwaith dyfalu aneffeithiol. Gwaethygodd ei hanadlu yn gynyddol tan un diwrnod, yn gynnar yn 2021, nid oedd gan fy nhad unrhyw opsiwn ond ffonio 999 a chafodd ei chludo i’r ysbyty.”
- Aelod o deulu'r claf |
Stori AnnaYn ystod y cyfnod cloi, dechreuodd mam-gu Anna ddangos arwyddion cynnar o ddementia. Roedd ei phractis meddyg teulu lleol wedi symud i wasanaethau o bell ac, ar ôl sawl ymgais i sicrhau apwyntiad, cynigiwyd asesiad ffôn. Er bod Anna'n teimlo nad oedd hyn yn ddelfrydol, roedd hi'n ddiolchgar y byddai'r apwyntiad yr wythnos ganlynol. Yn anffodus, ychydig cyn yr apwyntiad, profodd Anna’n bositif am Covid-19 a bu’n rhaid iddi ynysu gartref. Roedd hyn yn golygu na allai fynychu apwyntiad ei nain gyda hi. Wedi hynny, galwodd Anna ei nain i ofyn sut aeth pethau a beth ddywedodd y meddyg teulu. Nid oedd ei nain yn gallu cofio'r hyn a ofynnwyd iddi na'r hyn a ddywedwyd wrthi - ac nid oedd Anna'n gallu darganfod. “Daeth hwn yn gyfnod llawn straen a phryder. Gan nad oedd hi'n gallu cofio, fe wnes i ffonio'r feddygfa fy hun i weld a allent roi unrhyw syniad i mi a oedd yn ddementia a beth i'w wneud nesaf. Gwrthodwyd fi ar sail cyfrinachedd cleifion ac ni allwn gael unrhyw wybodaeth.” Roedd nain Anna hefyd yn cael cymorth gan glinig lles i gleifion hŷn, ond daeth y gwasanaeth hwn i ben yn ystod y pandemig. Roedd hyn yn golygu na chafodd ei chyflwr ei fonitro am y rhan fwyaf o'r pandemig. Pan ailddechreuodd y clinig, cafodd ei hasesu gan nyrs a oedd yn adnabod symptomau dementia a'i hatgyfeirio i'r ysbyty i gael sgan ar yr ymennydd, asesiad dementia ac ymgynghoriad. Ar y pwynt hwn cafodd ddiagnosis o'r diwedd fod ganddi Alzheimer's difrifol. “Ni fydd fy mam-gu yn adennill dim o’r cof a’r gallu meddyliol hwnnw a gollodd. Gallai hyn fod wedi'i ohirio pe bai camau'n cael eu cymryd yn yr apwyntiad cychwynnol gyda'r meddyg teulu. Er fy mod yn deall y risgiau a’r rhagofalon yr oedd eu hangen yn ystod y cyfyngiadau symud, rwy’n teimlo bod hwn yn ddiffyg mawr ac wedi costio llawer o niwed i iechyd a pherthynas i fy nain a’n teulu.” |
Roedd symud i ymgynghoriadau o bell yn anodd iawn i bobl f/Byddar a nam ar eu clyw, y rhai nad oeddent yn siarad Saesneg na Saesneg fel ail iaith, y rhai ag anabledd dysgu, a'r rhai ag awtistiaeth. Roeddent yn wynebu problemau yn deall gwybodaeth a chyfathrebu'n effeithiol, a oedd yn rhwystr i gael mynediad at ofal iechyd.
| “ | Nid oedd deall gwybodaeth, bod yn fyddar, methu â chyfathrebu, llawer o bethau ar-lein, a gorfod defnyddio Saesneg ac ysgrifennu, wyddoch chi, e-byst a phethau felly a negeseuon testun yn hygyrch iawn i mi.”
– d/person Byddar |
Roedd ymgynghoriadau ffôn yn anhygyrch ar y cyfan, gyda cyfieithwyr ddim ar gael yn aml. O ganlyniad, dywedodd rhai wrthym fod yn rhaid iddynt ddibynnu ar aelodau o'r teulu neu wirfoddolwyr a oedd yn gwybod iaith arwyddion i helpu gyda'r galwadau hyn.
| “ | Fe ddywedon nhw [y meddygon] y bydden nhw'n galw fy nhŷ, ond roeddwn i wedi dweud yn barod, 'Rwy'n fyddar, wyddoch chi, nid wyf yn mynd i allu cymryd galwad ffôn'. Rhaid bod ffordd arall, anfon e-bost ataf, anfon neges destun ataf,' ac fe wnaethant ei anwybyddu. Fe wnaethon nhw ffonio fy nhŷ a dweud, 'O, mae hwn yn argyfwng, mae angen ichi fynd i'r adran damweiniau ac achosion brys'. Yn ystod yr alwad ffôn gyntaf roeddwn wedi eu ffonio trwy wasanaeth cyfieithu, ond nid oeddent wedi fy ffonio yn ôl trwy'r gwasanaeth cyfieithu ar y pryd.”
– d/person Byddar |
Roedd ymgynghoriadau ffôn hefyd yn heriol i gyfranwyr nad oedd yn siarad Saesneg fel eu hiaith gyntaf. Roedd yn well gan lawer gael cyfarfodydd wyneb yn wyneb oherwydd gallent ddefnyddio cyfieithwyr yn haws.
| “ | Mae wyneb yn wyneb yn dda, dim ffôn, na, dydw i ddim yn hoffi'r ffôn. Gan fod wyneb yn wyneb yn dda ar gyfer hyder, mae gen i fwy o hyder, mwy o siarad. Beth yw'r broblem? Mae’n dda wyneb yn wyneb a dod â chyfieithydd ar y pryd.”
- Ffoadur |
Clywsom fod rhai pobl awtistig yn teimlo bod y newid sydyn i ymgynghoriadau ffôn yn anghyfforddus ac yn ofidus. Cawsant eu defnyddio ag ymgynghoriadau wyneb yn wyneb, ac roedd natur amhersonol apwyntiadau ffôn yn aflonyddgar iawn.
| “ | Roedd yn rhaid iddo fod mor gyfarwydd â'r aelod hwnnw o staff. Nid oedd yn hoffi newid. Ac roedd fy mab arall yr un peth, ac maen nhw'n dal i fod. Ond roedden nhw'n arfer rhoi rhifau allan i chi eu ffonio, fel y byddai gennych chi rywun i siarad â nhw. Ac roeddwn fel, 'Ni allwch wneud hynny pan fyddant yn awtistig.' Mae'n rhaid i chi gadw at y bobl maen nhw'n eu hadnabod oherwydd maen nhw'n teimlo'n gyfforddus."
– Rhiant person Awtistig |
Dysgu ar gyfer y dyfodol: mynediad teg a mynd i'r afael ag anghydraddoldebauUn thema gyffredin ym myfyrdodau cyfranwyr oedd sut i sicrhau bod cleifion yn gallu cael gafael ar y gofal sydd ei angen arnynt yn ystod argyfwng, ac yn enwedig pwysigrwydd deall a mynd i’r afael ag anghydraddoldebau o ran mynediad at ofal. Gwelwyd bod y newidiadau yn ystod y pandemig yn gwaethygu llawer o rwystrau presennol i gael mynediad at ofal, yn enwedig lle nad oedd gan gleifion neu ofalwyr fynediad at dechnoleg neu pan oeddent yn cael problemau teithio oherwydd cyfyngiadau Covid-19. Dywedodd llawer o gyfranwyr fod angen cynlluniau i fynd i’r afael ag anghydraddoldebau gofal iechyd yn ystod argyfyngau, er mwyn darparu cymorth cyson a theg i bob claf. Teimlai cyfranwyr fod cefnogaeth ychwanegol - megis dehonglwyr a deunyddiau wedi'u cyfieithu - yn ddiffygiol yn ystod y pandemig. Roedd hyn yn ei gwneud yn anodd neu'n amhosibl i rai pobl gael mynediad at wybodaeth bwysig am eu gofal iechyd, a chael y gofal yr oedd ei angen arnynt. Yn ei dro, roedd hyn yn golygu bod rhai pobl hyd yn oed yn fwy ymylol ac ynysig. Roedd y cyfranwyr hyn eisiau cynlluniau penodol i gefnogi pobl anabl, wedi’u teilwra i’w hanghenion mynediad a gofal iechyd, a chydnabod y rhwystrau ychwanegol y maent eisoes yn eu hwynebu a sut mae’r rhain yn gwaethygu yn ystod pandemig. “Mwy o arweiniad i bractisau meddygon teulu llai ac optegwyr nad oeddent yn gwybod beth y gallent neu na allent ei wneud, gan ohirio triniaethau a allai fod wedi achub fy ngolwg.” – Cyfrannwr Mae Every Story Matters |
Bu gweithwyr gofal iechyd proffesiynol sy'n gweithio ym maes gofal sylfaenol hefyd yn myfyrio ar effaith y symud i ymgynghoriadau o bell. Dywedasant wrthym pa mor anodd oedd hi i asesu cleifion heb eu gweld yn bersonol, yn aml disgrifio ymgynghoriadau o bell fel rhai peryglus a phryderus. Dywedodd y cyfranwyr hyn eu bod wedi colli mewnwelediadau gwerthfawr y byddent fel arfer yn eu hennill o apwyntiadau personol. Roedd eraill yn rhannu rhwystrau technolegol penodol, megis systemau TG nad oeddent yn ddigonol ar gyfer ymgynghoriadau o bell. O ganlyniad, dywedodd llawer o feddygon teulu eu bod poeni am ddiogelwch cleifion.
| “ | Gallwch chi ennill llawer iawn mwy pan welwch berson wyneb yn wyneb, felly roeddem yn teimlo ein bod yn gweithio gyda risg llawer uwch. Dim llawer risg uwch ar gyfer [cael eich heintio â] Covid-19 pe na baem yn gweld y cleifion, yn amlwg, ond ar gyfer ein diagnosis clinigol, yn enwedig gyda chleifion iechyd meddwl oherwydd nid oedd gennym allu fideo.”
- Meddyg Teulu |
| “ | Roeddent yn cael yr hyn a oedd yn teimlo fel sefyllfaoedd risg uchel dros y ffôn, roedd cleifion yn gwrthod dod i mewn neu fynd i'r ysbyty yn ystod rhai o'r galwadau hynny. Roedd pobl yn ymddwyn yn wahanol i’r hyn a fyddai ganddyn nhw fel arfer.”
- Meddyg Teulu |
Rhannodd gweithwyr gofal iechyd proffesiynol sut y newidiodd y dull arferol o ofalu am gleifion â chyflyrau hirdymor, megis diabetes, wrth symud i ofal o bell. Roedd ymgynghoriadau ffôn, er enghraifft, yn gofyn am sgiliau newydd.
Stori AnviMae Anvi yn gweithio fel nyrs meddyg teulu. Ar ddechrau'r pandemig, rhoddodd ei phractis y gorau i bob ymgynghoriad wyneb yn wyneb ar unwaith. Fe wnaethant symud y rhan fwyaf o apwyntiadau i ymgynghoriadau ffôn. Roedd Anvi yn gyfrifol am reoli cyflyrau cronig yn y feddygfa. Mae hyn yn cynnwys cleifion â diabetes a chlefydau anadlol. Trefnodd ymgynghoriadau ffôn yn gyflym i hyfforddi pobl â diabetes sut i roi inswlin a monitro eu lefelau glwcos gartref. I'r rhai â chlefydau anadlol, eglurodd sut i fonitro llifoedd brig. Roedd hyfforddi cleifion i hunanreoli a chynnal archwiliadau ac ymgynghoriadau dros y ffôn yn sgiliau newydd i Anvi. Roedd hi'n cael trafferth i ddechrau ond dros amser fe wellodd ac roedd yn fwy hyderus. “Doeddwn i ddim yn ei wneud yn dda iawn yn enwedig ar y dechrau, felly dod i arfer â hynny. Ceisio adnabod y cleifion. Fe wnes i ddarganfod eich bod wedi colli llawer yn yr ymgynghoriad bryd hynny o hynny ... ond dysgais i wneud pethau'n well." |
Sut yr addasodd y gweithlu gofal sylfaenol i'r pandemig
Roedd prinder staff yn her enfawr yn ystod y pandemig. Yr her gychwynnol oedd penderfynu pa apwyntiadau i'w canslo a phwy i'w blaenoriaethu ar gyfer triniaeth. Dywedodd cyfranwyr wrthym am y llwyth gwaith cynyddol a'r pwysau ar staff a oedd yn gweithio.
| “ | Roedd llawer o bobl i ffwrdd ... dwi'n meddwl mai dyna'r peth anoddaf yn ystod y ddwy flynedd gyfan; roedd i orchuddio pobl eraill drwy'r amser. Roedden ni bob amser yn un person i lawr, roedd yn ymddangos, ac mae hynny wedi parhau a dweud y gwir.”
– nyrs meddyg teulu |
Er mwyn mynd i'r afael â phrinder staff, bu'n rhaid i feddygfeydd newid sut roeddent yn gweithio. Roedd rhai yn gweithio mewn partneriaeth â meddygon teulu eraill yn lleol i rannu staff. Roedd hyn yn aml yn dechrau’n anffurfiol ond daeth yn fwy ffurfiol wrth i’r pandemig fynd rhagddo a daeth yn arbennig o bwysig wrth i absenoldebau staff gynyddu.
| “ | Roedd yn rhaid i ni gyfeillio â’n holl bractisau er mwyn i ni allu traws-lenwi a phethau felly… unrhyw bryd roedd gennym lawer o absenoldeb ymhlith ein staff, staff clerigol neu glinigol, gallem bob amser gyflenwi.”
- Meddyg Teulu |
Disgrifiodd cyfranwyr eraill sut y newidiodd eu patrymau gwaith i sicrhau y gallai gwasanaethau barhau.
| “ | Yn ystod y pandemig roedd partneriaid y feddygfa yn gefnogol iawn i'w staff. Fel gweinyddwyr, fe wnaethom newid ein horiau gwaith, i ddechrau o 6am, gorffen am 10pm a gweithio drwy'r penwythnos. Roedd rhannu ein horiau yn ein galluogi i barhau i gefnogi’r feddygfa, tra’n cadw ein swyddi a phellhau yn y gweithle.”
– aelod o staff meddygfa |
I fferyllwyr cymunedol, roedd rheoli cleifion a'r cyhoedd yn heriol. Clywsom gan rai fferyllwyr cymunedol am effaith cyfyngiadau cadw pellter cymdeithasol. Dim ond hyd at ddau o bobl y gallent eu caniatáu i mewn i'r fferyllfa ar y tro, a daeth eu rhyngweithio â chleifion yn fyr iawn ac yn fater o ffaith gan nad oeddent am i bobl ryngweithio'n hirach nag oedd angen. Roedd hyn yn newid mawr o'r ffordd yr oeddent fel arfer yn siarad â chleifion.
| “ | Roedd yn rhaid i mi newid fy holl ffordd o weithio. Byddwn yn fferyllydd cyffyrddus iawn. Roedd yn gymuned. Byddai pobl yn dod i mewn am baned o de, os oedd ganddynt newyddion drwg…roedd coffi yng nghefn y siop. Roedd yna fisgedi yno. Roedd yn deulu, a newidiodd hynny dros nos. Ni allem eu cael yn y siop oni bai eu bod angen rhywbeth.”
– Fferyllydd cymunedol |
Roedd enghreifftiau hefyd o gyfyngiadau ar nifer y bobl mewn fferyllfeydd sy'n achosi dicter a gwrthdaro mewn ciwiau y tu allan. Roedd hyn yn anodd i staff fferyllol ymdrin ag ef gan nad oedd ganddynt brofiad o reoli gwrthdaro a thorfeydd.
| “ | Y broblem oedd na allech chi adael gormod o bobl i mewn i'r siop oherwydd roedd yn rhaid i chi gadw pobl allan. Dim ond maint penodol yw’r fferyllfeydd, felly dim ond dau berson y gallech chi eu caniatáu i mewn ar y tro, gwneud y presgripsiwn, ac yna eu cael nhw allan mor gyflym ag y gallech chi. Gallai fod 80 neu 90 o bobl yn y ciw. Gallai pobl fod, ac roeddent yn wirioneddol ymosodol. Yn sarhaus tuag at staff a phobl a oedd, ar y pryd, dim ond yn gweithio.”
– Fferyllydd cymunedol |
Hybiau Covid-19 a gofal yn y gymuned
Clywsom gan rai cyfranwyr am sefydlu 'canolfannau Covid-19' i helpu i reoli achosion. Roedd hybiau Covid-19 yn dimau arbenigol a dynnwyd o blith y rhai sy’n gweithio ym maes gofal sylfaenol, a fyddai’n gweld cleifion yr amheuir bod ganddynt symptomau Covid-19 i’w hasesu a’u trin.
Dywedodd cyfranwyr mai bwriad hybiau Covid-19 oedd lleihau’r baich ar ysbytai trwy gefnogi a thrin cleifion Covid-19 mewn ardaloedd lleol, trwy gymysgedd o apwyntiadau wyneb yn wyneb ac o bell. Dywedodd rhai meddygon teulu â phrofiad o hybiau Covid-19 wrthym eu bod yn poeni am ba mor dda yr oeddent yn gallu barnu cyflyrau cleifion heb eu gweld yn bersonol.
| “ | Ein prif rôl mewn gwirionedd oedd peidio ag anfon yr holl bobl hynny i'r ysbyty ... rydych chi'n mynd adref ar ôl rhai dyddiau a bob amser yn meddwl o ddim, wnes i'r alwad iawn am y plentyn bach neu'r person hwnnw. Doeddwn i ddim yn gallu eu gweld. Roedd ar sail galwad ffôn yn unig.”
- Meddyg Teulu |
Rhannodd rhai cyfranwyr eu barn Roedd hybiau Covid-19 yn cynnig hyfforddiant a chymorth defnyddiol ar drin cleifion â Covid-19. Roeddent yn gweld hyn yn gadarnhaol, a rhoddodd fwy o hyder iddynt wrth asesu a thrin Covid-19.
| “ | Cawsom gyfarfodydd rheolaidd gyda’r ymgynghorwyr anadlol o’r ysbyty fel rhan o’r hwb Covid. Unwaith eto, roedd y canllawiau ganddynt ynghylch pa ffactorau risg i edrych arnynt a phryd i anfon rhywun i mewn… roedd llawer o ddysgu.”
– rheolwr practis meddyg teulu |
Dywedodd meddygon teulu eraill eu bod yn herio cyngor gan fyrddau iechyd lleol i ffurfio hybiau Covid-19 oherwydd nad oeddent yn meddwl y byddai'n eu helpu i drin cleifion. Roedd un meddyg teulu a rannodd ei stori gyda ni yn anhapus gyda’r syniad o ganolfan Covid-19 oherwydd ei fod yn meddwl y byddai gormod o absenoldebau staff iddo weithio.
Dywedodd cyfranwyr sy'n gweithio ym maes gofal sylfaenol wrthym am mentrau eraill i ofalu am bobl yn y gymuned. Er enghraifft, sicrhau bod peiriannau ocsimetrau curiad y galon a phwysedd gwaed ar gael er mwyn i gleifion allu asesu eu hunain. Dywedodd rhai meddygon teulu hefyd eu bod wedi rhagnodi mwy o wrthfiotigau nag y byddent yn ei wneud fel arfer yn ystod y pandemig i helpu i atal cyflyrau iechyd rhag dod yn fwy difrifol.
Gwneud atgyfeiriadau ysbyty
I gleifion â chyflyrau iechyd difrifol neu barhaus yr oedd angen triniaeth ysbyty arnynt, mae rôl meddygon teulu o ran sicrhau mynediad at wasanaethau ysbyty yn hollbwysig. Dywedodd llawer o gyfranwyr wrthym fod effaith y pandemig ar wasanaethau ysbytai yn golygu ei bod yn anodd sicrhau apwyntiadau i gleifion. Arweiniodd hyn at rwystredigaeth ymhlith cyfranwyr – clinigwyr a chleifion fel ei gilydd – a golygai hyn inni glywed am lawer o broblemau iechyd difrifol na chawsant eu trin, yn aml am gyfnodau hir.
| “ | Byddai cleifion yn cael eu cyfeirio at ofal eilaidd, [ond] ni fyddent yn gweld unrhyw un ... hyd yn oed ychydig iawn o ymgynghoriadau ffôn a gafwyd, a dweud y gwir. Byddai cleifion yn ein ffonio bryd hynny, yn amlwg yn flin oherwydd nad oedd eu problemau’n cael eu trin [ond] dyma’r rheswm pam y cawsant eu cyfeirio at ofal eilaidd, oherwydd roeddem wedi cyrraedd ein terfyn, mewn gwirionedd, o ran yr hyn y gallem ei wneud i helpu. nhw.”
– nyrs meddyg teulu |
| “ | O ran gofal eilaidd, felly gofal ysbyty, na, nid oedd dim o hynny’n rhywbeth a drafodwyd gyda meddygon teulu, neu roedd meddygon teulu yn ymwneud â datblygu protocolau neu unrhyw beth felly, yn sicr nid oeddwn, ac rwy’n amau nad oes unrhyw un o’m cyd-Aelodau wedi bod. chwaith.”
- Meddyg Teulu |
Disgrifiodd cyfranwyr sut yr arweiniodd oedi wrth driniaethau at gyflyrau'n gwaethygu, ac at restrau aros cynyddol.
| “ | Dywedwyd wrth bobl am aros adref, ond mae gofal iechyd mor hanfodol na allwch wneud y lleiafswm lleiaf posibl. Erbyn hyn mae ôl-groniadau enfawr. Roedd angen i’r ddarpariaeth fod wedi parhau.”
- Meddyg Teulu |
| “ | Dechreuais weithio mewn gwasanaeth canser ac roedd dwywaith nifer yr atgyfeiriadau oherwydd nad oedd pobl wedi bod at eu meddyg teulu felly yn hytrach na chael diagnosis cynnar, roedd yn gamau diweddarach ac roedd y pwysau’n aruthrol.”
- Gweithiwr gofal iechyd proffesiynol |
Roedd cleifion a rannodd eu stori gyda ni yn aml yn rhwystredig iawn gyda'r oedi cyn cael mynediad i ofal ysbyty. Roedd yn rhaid i lawer fyw gyda phroblemau iechyd pryderus nad oeddent wedi'u hasesu'n iawn neu lle nad oeddent yn cael y driniaeth gywir. Roeddent yn aml yn mynd yn ôl at eu meddygon teulu dro ar ôl tro i geisio cael y gofal yr oedd ei angen arnynt.
Stori cyfrannwr Mae Pob Stori o BwysRoedd mam cyfrannwr Every Story Matters i fod i weld ymgynghorydd anadlol yn ystod wythnos gyntaf y cloi cyntaf, ond cafodd yr apwyntiad wyneb yn wyneb ei ganslo, a chynigiwyd apwyntiad ffôn yn lle hynny. Nid oedd yr ymgynghorydd erioed wedi gweld ei fam o'r blaen ac wedi rhagnodi anadlwyr iddi yn dilyn yr apwyntiad. Fis yn ddiweddarach cafodd ei rhuthro i'r ysbyty mewn cyflwr difrifol, ond pan gafodd ei rhyddhau ar ôl dau ddiwrnod, nid oedd diagnosis ac nid oedd unrhyw brofion wedi'u cynnig. “Roeddwn yn parhau i ffonio ei meddyg teulu, ei thîm anadlol ac ati a [rhoi gwybod am ei chyflwr drwy mesuriadau ond fe ddywedon nhw wrtha i] “na all hynny ddim bod yn iawn, rhaid torri'r peiriant”, ac ni fyddai neb yn ei gweld hi o hyd… aeth hyn ymlaen am fisoedd a misoedd.” Wedi blino ar y sefyllfa gan ei fod yn gwybod bod ei fam yn sâl iawn, penderfynodd y cyfrannwr gwyno i feddyg teulu ei fam a siarad â'r Gwasanaeth Cyswllt Cleifion yn ei ysbyty. Yn y pen draw, ar ôl rhywfaint o ddyfalbarhad pellach gan y cyfrannwr, derbyniodd yr holl brofion yr oedd eu hangen arni ac yn anffodus cafodd ddiagnosis o emffysema Cam 4. Cafodd hyn effaith ddinistriol ar y cyfrannwr, eu mam a’u teulu gan eu bod wedi cael sioc a gofid gan y diagnosis. |
Rhannodd rhai cleifion sut yr oeddent talu am driniaeth breifat oherwydd yr oedi hwn. Roeddent yn aml yn flin iawn eu bod yn teimlo eu bod yn cael eu gorfodi i wneud hyn, ac mewn rhai achosion yn cael trafferth fforddio gwneud hynny.
| “ | Llwyddais i achub fy musnes pan godwyd cyfyngiadau dim ond er mwyn methu â chael yr anhawster i gael apwyntiad meddyg teulu pan ddechreuais gael problemau symudedd a drodd yn ddigon difrifol i golli fy musnes eto. Cefais fy siomi gan amseroedd aros y GIG a chefais fy ngorfodi i dalu am ofal preifat er mwyn osgoi parlys.”
– claf meddyg teulu |
Dysgu ar gyfer y dyfodol: gofal sylfaenol yn ystod y pandemigSymudodd y pandemig ffyrdd o weithio a daeth â newidiadau i ofal sylfaenol, gan ei gwneud hi'n bosibl darparu rhai apwyntiadau o bell. Myfyriodd llawer o’r rhai sy’n gweithio ym maes gofal sylfaenol ar lwyddiannau hyn a dweud y dylid dysgu gwersi ar gyfer gwella gofal yn y dyfodol. Fodd bynnag, roedd pryderon gwirioneddol hefyd ymhlith rhai cleifion, gofalwyr a gweithwyr cymorth ynghylch sut yr oedd y newid i ofal o bell yn creu rhwystrau ychwanegol i bobl agored i niwed a’r rhai o rai cymunedau. “Rydym wedi ceisio hyd yn oed ei wneud yn norm wrth symud ymlaen i newid y ffordd yr ydym yn cyflawni gwasanaethau. Ond mae hynny'n gofyn i ni newid - mae angen i chi fod, ni fyddwn yn dweud ailhyfforddi, ond cael gwahanol bobl yn gwneud sgiliau newydd. Felly, ffôn llawer mwy sy'n datblygu ymgynghoriadau, gweithio gyda ffonio cleifion, ond hefyd i gleifion newid; Fyddwn i ddim dyweder llai o ddibyniaeth, ond ceisiwch ddefnyddio – defnyddiwch y gwasanaethau yn nes adref.” — Fferyllydd “Rydym yn cychwyn ar oes newydd o feddygon teulu, gyda’r galw cynyddol yn gyrru’r angen am newid lle nad oes angen adolygiad wyneb yn wyneb ar bob problem a gall fod ymdrinnir ag ef o bell. Roedd angen newidiadau er mwyn diweddaru practis cyffredinol technoleg a defnyddio gwasanaethau o bell, fe ddigwyddodd yn gynt o lawer na’r disgwyl.” – Cyfrannwr Mae Every Story Matters Dadleuodd rhai cyfranwyr fod y ffocws ar ysbytai yn golygu bod gofal sylfaenol yn derbyn llai o gefnogaeth yn ystod y pandemig. Roeddent eisiau gwell cynllunio i gleifion barhau i gael mynediad at ofal sylfaenol ac eilaidd. “Rwy'n meddwl bod angen cynllun cenedlaethol arnom ar gyfer gofal sylfaenol mewn pandemig. Rwy'n meddwl nad oedd, nid oedd yno.” - Meddyg Teulu |
3. Ysbytai: profiadau gweithwyr gofal iechyd proffesiynol |
 |
Mae'r bennod hon yn rhannu'r hyn a ddywedodd gweithwyr gofal iechyd proffesiynol wrthym am ofal ysbyty yn ystod y pandemig. Mae’n amlinellu profiadau’r rhai a ddarparodd ofal i gleifion Covid-19 a chleifion eraill, yn ogystal â phrofiadau staff cymorth ysbytai.
Parodrwydd ac ymateb pandemig
Profiadau cyfranwyr o'r ymateb pandemig amrywio’n sylweddol yn seiliedig ar ba ran o’r ysbyty yr oeddent yn gweithio ynddo, eu rôl benodol, a pha mor agos yr oeddent at wneud penderfyniadau.
Roedd uwch staff yr ysbyty yn cymryd mwy o ran mewn cynllunio at argyfwng ac yn gwneud penderfyniadau ynghylch sut y byddai'r ysbyty yn ymateb. Cawsant ddiweddariadau cyson (weithiau bob dydd) gydag arweiniad gan y llywodraeth a systemau gofal iechyd ar fesurau rheoli heintiau yn ogystal â chynlluniau gweithredu.
Er mwyn ymateb i heriau'r pandemig, mae rhai ad-drefnodd ysbytai ac ail-lunio lleoedd i asesu cleifion a lleihau lledaeniad Covid-19. Roedd ad-drefnu hefyd yn golygu newidiadau sylweddol i'r ffordd y caiff ysbytai eu staffio a sut yr oedd gwasanaethau'n cael eu rheoli a'u darparu.
Er bod rhai gweithwyr gofal iechyd yn gadarnhaol am y ffordd y cafodd yr ymateb pandemig ei reoli, dywedodd eraill nad oedd digon o ystyriaeth wedi'i rhoi iddo.
| “ | Rwy'n meddwl bod yr holl staff clinigol, y ffordd yr oedd yn rhaid newid a threfnu popeth, yn ein hysbyty wedi'i wneud yn arbennig o dda. Gwnaed newidiadau enfawr. Ailddyrannu ardaloedd, ailddyrannu staff, pawb symud o le i le, newid yr hyn roedden nhw’n ei wneud.”
- Nyrs ysbyty |
| “ | Cafodd llawer o staff eu hadleoli i wahanol feysydd clinigol i ffwrdd o'r lle y maent fel arfer yn gweithio i gynorthwyo gyda'r ymateb i Covid - cafodd yr aelodau hyn o staff eu “taflu i mewn i'r pen dwfn” heb fawr o hyfforddiant ychwanegol a dim dewis ynghylch ble y cawsant eu hanfon. Cafodd hyn hefyd effaith ar lwybrau hyfforddi llawer o feddygon iau.”
-Meddyg ysbyty |
Disgrifiwyd mwy o staff ysbyty iau newidiadau cyson a chyflym i sut maent yn gweithio. Ar adegau, roedd y newidiadau hyn yn digwydd yn ddyddiol ac nid oeddent bob amser yn cael eu hesbonio fel rhan o gynllunio at argyfwng. Roedd rhai o’r cyfranwyr hyn o’r farn nad oedd yr hyn y gofynnwyd iddynt ei wneud bob amser yn gwneud synnwyr, yn enwedig gan nad oedd pethau’n cael eu gweithredu’n gyson ar draws yr ysbyty.
Yn nyddiau cynnar y pandemig, rhannodd cyfranwyr sut roedd rheoli heintiau a thriniaeth Covid-19 yn cael eu blaenoriaethu, ac arhosodd y cyhoedd i ffwrdd o'r ysbyty i raddau helaeth. Achosodd diffyg cysondeb o fewn a rhwng ysbytai rywfaint o rwystredigaeth ymhlith gweithwyr gofal iechyd proffesiynol a rannodd eu stori gyda ni. Soniodd cyfranwyr eraill am heriau oherwydd gofod cyfyngedig ac awyru gwael mewn ardaloedd penodol o fewn ysbytai. Roedd y ffactorau hyn yn ei gwneud yn anos cynnal pellter cymdeithasol, a chynyddodd hyn bryder ymhlith staff ysbytai.
Roedd cynllunio gofal a thriniaeth cleifion mewn ysbytai yn parhau i fod yn heriol yn ddiweddarach yn y pandemig. Pan godwyd cyfyngiadau Covid-19, roedd yn rhaid i ysbytai gydbwyso darparu gofal i fwy o gleifion nad oeddent yn ymwneud â Covid â lleihau lledaeniad Covid-19.
Roedd dychwelyd i 'fusnes fel arfer' weithiau'n gofyn cymaint o ymdrech i symud staff, adnoddau ac offer â'r ymateb cychwynnol i'r pandemig. Clywsom lawer o enghreifftiau o sut yr oedd yn rhaid ail-agor wardiau ac unedau, a phrynu neu symud offer. Dywedodd staff wrthym sut yr oeddent yn ceisio dychwelyd i rywfaint o normalrwydd wrth ddarparu gwasanaethau gofal iechyd a helpu cleifion wrth i'r pandemig barhau, ond roedd llawer o heriau ymarferol. Dywedodd cyfranwyr nad oedd cleifion yn aml yn derbyn y lefel arferol o ofal. Roedd gweithwyr gofal iechyd proffesiynol yn teimlo'n siomedig ac yn euog am fethu â darparu'r lefel o ofal yr oeddent ei heisiau.
Stori SarahMae Sarah yn arbenigo mewn gofal dietetig ar gyfer cleifion gastrig ac oesoffagaidd o fewn uned canser arbenigol ranbarthol. Roedd gan yr ysbyty y bu'n gweithio ynddo Uned Gofal Dwys (ICU) fach, a ddewiswyd fel uned ranbarthol ar gyfer gwelyau gofal dwys. Rhwng mis Mawrth 2020 a mis Mehefin 2022 bu’n rhaid i’r ganolfan ganser arbenigol symud o leiaf bedair gwaith er mwyn gallu parhau â gofal i gleifion canser. Myfyriodd Sarah ar heriau logistaidd hyn. Roedd y rhain yn cynnwys dod o hyd i le llawfeddygol priodol ac argaeledd ar gyfer eu cleifion, a oedd â gwrthimiwnedd, ac ailgynllunio parhaus, neu symud cleifion, offer a staff ar fyr rybudd. “Bob tro roedd yna newid mewn amgylchiadau lle roedden ni fel, 'Iawn, fe wnawn ni ailgychwyn cymorthfeydd', roedden ni fel, 'Iawn, sut ydyn ni'n gwneud hynny?' ac o fewn dau ddiwrnod byddem wedi symud uned lawn filltir ar draws y ddinas a chael y rheini wedi’u sefydlu.” Roedd Sarah a'i thîm yn ei chael hi'n heriol darparu gofal yn ystod y cyfnodau hyn o orfod stopio a symud. Roedd llawer o'r staff nyrsio medrus yr oeddent yn dibynnu arnynt wedi cael eu hadleoli i wardiau Covid-19 oherwydd eu harbenigedd. Teimlai fod triniaeth, cynllunio gwasanaethau a darparu gofal yn waeth oherwydd y problemau hyn. “Ni chafodd llawer ohonyn nhw’r llwybrau eithaf ac optimaidd y dylen nhw fod wedi bod arnyn nhw oherwydd Covid-19. Felly, mae hynny wedi arwain at effaith andwyol ar eu hansawdd bywyd yn unig, ond ar hyd eu hoes yn gyffredinol…sydd wedi cael effaith arnom ni, yn bersonol, oherwydd rydych yn teimlo nad ydych wedi gallu darparu'r gwasanaeth y byddech wedi'i obeithio. ” |
Yn nyddiau cynnar y pandemig, myfyriodd cyfranwyr ar sut yr oedd synnwyr cyffredin o bwrpas ar draws ysbytai. Disgrifiodd llawer sut yr aeth cydweithredu dan straen yn ystod y camau diweddarach wrth i wahanol wardiau ac arbenigeddau geisio cael eu gwasanaethau i redeg eto. Disgrifiodd rhai cyfranwyr ddiffyg cynllunio ar gyfer pan ddaeth y cyfyngiadau pandemig i ben. Dywedon nhw nad oedd 'strategaeth ymadael' o amodau llym yr ymateb cychwynnol i Covid-19. Yn eu barn nhw, dylai fod mwy o gynllunio a chanllawiau i gefnogi gwasanaethau nad ydynt yn rhai brys i ailagor yn gyflymach.
| “ | Nid oedd unrhyw gyngor ar sut i gamu'n ôl o unrhyw beth ac nid oedd unrhyw gymorth o gwbl i ddad-ddwysáu. Ac nid oedd yn teimlo, i ni, unrhyw synnwyr o ddysgu, 'Iawn, yr hyn a wnaethom yn y don gyntaf'.”
-Meddyg ysbyty |
Roedd ysbytai yn wynebu heriau pellach wrth ddychwelyd i ddarpariaeth arferol gwasanaethau iechyd. Un broblem oedd bod llawer o staff wedi gadael, wedi cael eu hadleoli i rywle arall, neu wedi llosgi gormod i weithio. Er enghraifft, disgrifiodd un meddyg sy'n rheoli theatrau llawfeddygol fod staff nyrsio wedi'u hanfon i ofal dwys (Uned Gofal Dwys neu Uned Therapi Dwys) yn ystod y pandemig. Canfuwyd, unwaith y gallai theatrau ddechrau gweithredu eto, nad oedd digon o nyrsys i'w staffio. Roedd y rhai a ddaeth yn ôl wedi gofidio ac wedi blino'n lân o weithio yn yr ICU.
Dysgu ar gyfer y dyfodol: cynllunio a pharatoi ar draws gofal iechydDywedodd llawer o gyfranwyr fod cynllunio ar gyfer gofal iechyd mewn achos o bandemig yn wael, a bod cyflymder yr ymateb i'r argyfwng yn rhy araf. Disgrifiwyd yr effaith enfawr ac yn aml niweidiol a gafodd hyn, gyda llawer o fywydau wedi'u colli neu eu difrodi a straen anhygoel ar y gweithlu gofal iechyd. Roeddent eisiau gwell cynllunio ar gyfer pandemigau yn y dyfodol a sicrhau na wneir yr un camgymeriadau eto. “Drwy gael mwy o brotocolau brys yn eu lle, yna mae'n helpu i atal y gwastraff amser ac adnoddau a chyllid. Gwn o hyd yn oed dim ond ein [tîm] bach, rydym wedi cael cryn ddysgu dim ond i gronni'r adnoddau ar draws y rhanbarth a gwneud y gorau o'r pethau syml. Mae gennym ni’r rheini yn eu lle nawr, os bydd angen rhywbeth felly eto.” – Gweithiwr gofal iechyd proffesiynol perthynol “Ar lefel genedlaethol, mae angen mynd i’r afael â materion blaengynllunio. Pobl sy'n agored i niwed i gael eu fflagio'n gynt a'u cefnogi'n well. Mae angen cryfhau cadwyni cyflenwi mewn argyfwng. Dylid cefnogi a chryfhau’r GIG, ni waeth beth yw’r gost.” – Cyfrannwr Mae Every Story Matters Myfyriodd rhai cyfranwyr ar sut i ymateb i’r pandemig sy’n datblygu’n gyflym pan oedd cyn lleied yn hysbys am Covid-19 ar y dechrau. Roedd eu ffocws yn llai ar yr ymateb cychwynnol, ac yn fwy ar sut y dylai dysgu am y firws, sut mae'n lledaenu a sut i'w drin fod wedi'i wreiddio'n gyflymach a'i gyfathrebu'n well wrth i'r pandemig fynd rhagddo. “Byddech chi'n gweld y pymthegfed iteriad o ddogfen a oedd prin ddim yn wahanol o ran y cyngor ar PPE ac amddiffyn staff a hynny i gyd flwyddyn yn ddiweddarach a byddech chi'n meddwl, 'Ie, ond mae hyn yn teimlo fel hyn. i'w ddechreu yn llwyr eto. Iawn, beth ddysgon ni o'r don gyntaf, nawr beth ddylem ni fod yn ei wneud? Dylai’r ddogfen hon edrych yn hollol wahanol, ac nid yw.” -Meddyg ysbyty Fodd bynnag, roedd llawer yn pryderu bod y pwysau parhaus ar systemau gofal iechyd yn golygu nad oedd unrhyw ffordd y gellid rhoi'r gwersi a ddysgwyd ar waith. Roedd hyn yn bryder arbennig i gyfranwyr sy'n gweithio ym maes gofal iechyd, ond hefyd i rai cleifion a'r cyhoedd. “Dim ond mater o amser yw hi cyn i ni gael ein herio… ond mae’n parhau i fod yn wir bod yr amgylchedd yn [gofal iechyd] yn anaddas i ymarfer. Mae'n risg i gleifion a staff; dyw hynny ddim wedi newid o gwbl, ac mae hynny'n siom chwerw... dwi'n meddwl nad ydyn ni wir wedi dysgu'r gwersi hynny, ac mae angen sylweddoli bod y wyddoniaeth yn cymryd sbel i ddal i fyny ac maen nhw wedi gwneud pethau aruthrol ond dyna'r rhai cyntaf dyddiau ac wythnosau lle mae bygythiad mawr i gymdeithas ac i staff, gweithwyr y GIG.” - Meddyg D&A |
Rheoli lledaeniad Covid-19
Clywsom sut y newidiodd ysbytai’r ffordd y maent yn gweithio i ofalu am gleifion Covid-19 a lleihau lledaeniad y clefyd. Adlewyrchodd rhai cyfranwyr fod y ffyrdd cynnar o weithio yn arbennig o llym oherwydd ofn Covid-19 ac ansicrwydd ynghylch sut y lledaenodd y clefyd a beth ddigwyddodd i bobl a'i daliodd.
| “ | Ar y dechrau, roeddem yn cynnig gwasanaeth cyfyngedig, roeddem yn gofyn i wardiau ffonio i lawr gyda'r hyn yr oeddent ei eisiau ac yn sganio siartiau a phethau drwodd i ni, ac yna roeddem yn cymryd pethau ac yn eu gadael y tu allan i wardiau. Nid oeddem yn mynd ymlaen i'r wardiau mewn gwirionedd felly nid oeddem yn rhoi gwasanaeth digonol iddynt mewn gwirionedd ond rwy'n meddwl bod llawer o hynny trwy godi bwganod hefyd. Rwy’n meddwl bod cymaint o ofn ar bawb gyda’r hyn oedd yn digwydd, ac oherwydd doedden ni ddim yn gwybod dim byd ar y dechrau.”
- Fferyllydd ysbyty |
Yn aml roedd gan ysbytai barthau llym ar gyfer trin gwahanol fathau o gleifion, yn enwedig cadw'r rhai sydd â Covid-19 ar wahân i eraill. Rhannodd cyfranwyr sut yr oedd rhai ysbytai’n labelu wardiau, cilfachau a mannau penodol fel rhai ‘poeth’ ac ‘oer’, neu ‘fudr’ a ‘glân’ i ddangos pa ardaloedd oedd â chleifion Covid-19 a pha rai nad oedd ganddynt. Roedd gan rai ICUs yn benodol ar gyfer cleifion Covid-19.
Roedd gan ardaloedd Covid-19 PPE a rheolau ymweld llymach fel arfer. Roedd enghreifftiau yn y straeon a glywsom am ysbytai yn rhoi systemau parthau ac un ffordd ar waith ar gyfer symud cleifion o fewn yr ysbyty ac ar draws gwahanol wardiau i gyfyngu ar gyswllt a lleihau trosglwyddiad Covid-19.
| “ | Yna cefais wybod gan fy rheolwr llinell y gallai ein ward ddod yn ward poeth Covid-19. Nid oedd neb yn deall yn iawn beth fyddai hynny'n ei olygu ond cawsom ein cyfarwyddo i fesur y pellter rhwng ein gwelyau ysbyty, i weld faint o gleifion y gellid eu nyrsio yn ein baeau a chynnal y pellter hwnnw o ddau fetr. Dywedwyd wrthym y byddai'n rhaid i ni wisgo offer amddiffynnol bob amser, ond nid oedd neb yn gwybod sut olwg fyddai ar hwnnw. ”
- Nyrs ysbyty |
Wrth i ysbytai dderbyn mwy o gleifion Covid-19, clywsom sut roedd wardiau dynodedig yn cael eu gwneud yn fwy, neu weithiau'n cael eu symud i ganiatáu mwy o le.
| “ | Penderfynodd yr ysbyty fod angen mwy o welyau Covid-19 arnynt. Felly, cawsom ni i gyd ein rhoi i fyny i’r chweched lefel, sef ward cardioleg. Roedd yn gymaint o drueni oherwydd bod yr holl staff yno wedi eu troi allan i lefydd eraill. Felly roedd hynny'n drist. Achosodd hynny ychydig bach o wrthdaro. Fe wnaethom ni ddwywaith.”
- Cynorthwyydd gofal iechyd ysbyty |
Unwaith y cyrhaeddodd ardaloedd a ddynodwyd ar gyfer cleifion Covid-19 gapasiti, weithiau roedd ysbytai, adeiladau neu wardiau eraill yn cael eu trosi i reoli nifer y cleifion Covid-19. Mae llawer o'r straeon yn disgrifio pa mor aflonyddgar oedd yr ad-drefnu hwn i'r rhai dan sylw. Roedd penderfyniadau am y mathau hyn o newidiadau yn aml yn anodd i staff eu deall, ac roedd staff a chleifion yn rhwystredig weithiau gan yr hyn oedd yn digwydd. Roedd y newidiadau yn ddryslyd a hefyd yn cyflwyno heriau staffio.
| “ | Ac yna, unwaith i hynny lenwi, roedd yn rhaid i ni symud i ward arall. Felly, yn y diwedd fe wnaethom orchuddio 2 lawr ein hysbyty. Ac rwy'n meddwl efallai mai dyna oedd yr uchafswm o 40. Rwy'n meddwl bod tua 40 o gleifion ar ein gwaethaf. Ond mae hynny'n llawer o nyrsys i ofalu am lawer o gleifion 24/7.”
- Nyrs ysbyty |
Roedd enghreifftiau hefyd o rai gwasanaethau, er enghraifft clinigau cleifion allanol, yn cael eu symud i ffwrdd o ysbytai yn gyfan gwbl i leihau nifer y bobl sydd angen dod i ysbytai a chymorth gyda chadw pellter cymdeithasol.
| “ | Rhoesom y gorau i gael cleifion allanol yn dod i'r adran. Roedden ni’n rhoi presgripsiynau iddyn nhw fynd i fferyllfeydd cymunedol, a doeddwn i ddim yn cytuno’n llwyr â nhw.”
- Fferyllydd ysbyty |
Trin cleifion Covid-19
Roedd llawer o enghreifftiau o ysbytai yn creu timau newydd i drin cleifion Covid-19. Roedd hyn yn golygu bod llawer o staff yn cael eu hailddyrannu i gyflenwi, yn aml yn gofalu am gleifion y tu allan i'w harbenigedd arferol. Symudwyd rhai o staff ysbytai i weithio gyda chleifion Covid-19 gan reolwyr tra gwirfoddolodd eraill i wneud hynny. Disgrifiodd rhai gweithwyr gofal iechyd proffesiynol eu bod eisiau cefnogi’r ymateb pandemig drwy wneud beth bynnag a allant i helpu pobl â’r clefyd. Rhannodd eraill sut yr oeddent am leihau’r pwysau ar staff oedd â’r arbenigedd i drin Covid-19.
Daeth heriau a phwysau sylweddol i ofalu’n uniongyrchol am gleifion Covid-19. Roedd staff ysbytai yn poeni am y risgiau ychwanegol iddyn nhw a'u teuluoedd o ran dal a lledaenu'r afiechyd. Roedd llawer yn ofni'r hyn y byddent yn ei brofi wrth drin cleifion Covid-19, ac yn enwedig y marwolaethau y byddent yn dyst iddynt.
| “ | Doeddwn i ddim eisiau mynd i'r ysbyty maes. Roeddwn yn ofnus o fynd i'r ysbyty maes oherwydd yr ysbyty maes yr oeddem yn mynd i'w gael yma, nid oedd yn mynd i fod lle roedd pobl yn mynd i wella. Roedd yn mynd i fod am ddiwedd oes, felly roedd y cyfan yn mynd i fod yn lliniarol, ac yn y bôn roedd yn rhywle lle roedden nhw'n mynd i roi pobl. Ond diolch byth, dyna oedd y senario gwaethaf posib, ac ni ddaeth i hynny erioed. ”
- Fferyllydd ysbyty |
Roedd rhai meddygon a nyrsys a wirfoddolodd neu a drosglwyddwyd o rolau eraill yn gweithredu fel pâr ychwanegol o ddwylo, yn hytrach na thrin cleifion yn uniongyrchol. Roedd rhai cyfranwyr yn gweld y rolau hyn yn heriol, tra bod eraill yn falch o helpu mewn unrhyw ffordd y gallent.
| “ | Wrth weithio, rydych chi'n gwybod yn union fel dwylo ychwanegol, codi cleifion, gofalu am gleifion, gwneud rhai meddyginiaethau a phethau."
-Meddyg ysbyty |
| “ | Roedd y rhan fwyaf o'r meddygon ymgynghorol yn ymwneud â'r gwaith o fewnblannu a sefydlogi'r cleifion. Yna, byddai mwy o’r hyfforddeion yn ymwneud â gofalu amdanynt dros yr wythnos neu ddwy nesaf.”
-Meddyg ysbyty |
Dysgu ar gyfer y dyfodol: ysbytai NightingaleRoedd ysbytai Nightingale yn ysbytai dros dro a sefydlwyd yn ystod y pandemig fel rhan o'r ymateb i'r pandemig. Myfyriodd rhai cyfranwyr ar yr hyn y gellir ei ddysgu o’r ymdrechion enfawr a wnaed i roi ysbytai Nightingale ar waith i gynyddu capasiti gofal dwys. Roedd llawer o gyfranwyr yn deall pam y gwnaed hyn, ond dywedasant nad oeddent yn cael eu defnyddio ddigon neu nad oedd eu hangen. Soniodd y cyfranwyr am sut y gallai cynllunio gwell sicrhau bod yr adnoddau hyn yn cael eu defnyddio’n fwy effeithiol os bydd her debyg yn cael ei hwynebu yn y dyfodol. Er enghraifft, roedd awgrymiadau’n cynnwys canolbwyntio adnoddau ar ble roedd eu hangen fwyaf mewn systemau gofal iechyd neu adeiladu capasiti ysbyty ychwanegol ond nid ar gyfer cleifion gofal dwys. “Yn lle sefydlu ysbytai Nightingale nad ydynt yn cael eu defnyddio i raddau helaeth, dylai adnoddau fod wedi cael eu dargyfeirio i’r mannau lle roedd eu hangen fwyaf, hynny yw’r GIG ar lawr gwlad.” – Cyfrannwr Mae Every Story Matters “Fe wnaethon ni sefydlu ysbytai enfawr Nightingale gyda galluoedd ICU nad oeddent yn cael eu defnyddio'n ddigonol, yn debygol oherwydd diffyg staff hyfforddedig iawn neu angen ICU. Gallai ychydig o feddwl ochrol fod wedi golygu bod y rhain yn cael eu defnyddio ar gyfer gofal llai dwys fel gofal yr henoed, gwelyau adsefydlu neu welyau gofal canolraddol Covid+, gan ryddhau gwelyau ysbyty i gleifion oedd eu hangen.” – Cyfrannwr Mae Every Story Matters |
Clywsom gan rai staff oedd wedi’u hadleoli am ba mor anodd a llawn straen oedd hyn iddynt, a sut yr oedd yn rhaid iddynt ddysgu’n gyflym, yn aml heb ddigon o hyfforddiant na chymorth.
| “ | Gwirfoddolais i a sawl un arall o ffisiotherapyddion ICU profiadol i dreulio'r dyddiau ar ICU i helpu'r staff nyrsio i rolio a gwneud ffisiotherapi ar y frest yn ôl yr angen. O ran cael ein hadleoli, mewn gwirionedd cawsom ein hadleoli fel nyrsys ICU - nid oedd hyn wedi'i gyfleu i ni cyn dechrau ein sifftiau - a'r holl swyddi y mae hynny'n eu cynnwys. Ni chawsom unrhyw hyfforddiant – gan fod gormod o gleifion – a gofynnwyd i ni wneud sifftiau 12.5 awr. Fe wnaethom gyflawni hyn i gyd yn fodlon iawn gan ein bod yn gwybod bod hwn yn gyfnod heriol.”
- Ffisiotherapydd ysbyty |
| “ | Newidiodd fy rôl yn sydyn pan ges i fy adleoli i weithio ar ward lawfeddygol brysur gan gynnwys cleifion Covid-19 positif. Doeddwn i ddim wedi gweithio ar ward ysbyty ers dros 20 mlynedd, felly roeddwn i'n teimlo fel hwyaden allan o'r dŵr, roedd yn gromlin ddysgu serth i weithio mewn ardal mor straen heb fawr o gefnogaeth. Roedd angen nyrsys wedi’u hadleoli i lenwi’r bylchau pan oedd angen aelodau eraill o staff mewn mannau eraill.”
- Nyrs ysbyty |
Er enghraifft, roedd cael eu hadleoli i rannau eraill o'r system gofal iechyd yn brofiad cyffredin ymhlith gweithwyr gofal iechyd cymunedol proffesiynol a rannodd eu straeon gyda ni. Roedd hyn yn aml yn golygu symud i weithio mewn wardiau Covid-19 a rolau cymorth eraill mewn ysbytai. Roedd gweithio gyda chydweithwyr newydd, cyflawni tasgau nad oedd ganddynt fawr o brofiad ohonynt ac addasu i ganllawiau Covid-19 ar gyfer darparu gofal yn hynod o anodd i’r cyfranwyr hyn. Achosodd hyn straen a phryder enfawr, gyda rhai yn rhannu sut nad oeddent yn teimlo eu bod wedi'u paratoi ar gyfer y rolau y gofynnwyd iddynt eu gwneud ond na chawsant ddewis.
Stori KiratCyn y pandemig bu Kirat yn gweithio fel dietegydd pediatrig, yn cefnogi plant ag anghenion cymhleth sy'n cael eu bwydo â thiwb. Gweithiodd yn bennaf gydag ysgolion a hefyd mewn clinig arbenigol gyda phlant ag awtistiaeth i sicrhau eu bod yn cael y maeth cywir. Ychydig wythnosau i mewn i'r pandemig, symudwyd Kirat i wasanaeth newydd a oedd yn gofalu am gleifion oedrannus a oedd wedi dal Covid-19. Roedd hyn yn cynnwys cael hyfforddiant ar sut i symud a bwydo cleifion hŷn. Teimlai Kirat fod yr hyfforddiant wedi'i drefnu'n dda ond ni wnaeth ei pharatoi ar gyfer pa mor wahanol fyddai'r rôl i'w rôl arferol fel dietegydd pediatrig. “Cefais fy hyfforddi i ofalu am gleifion gofal henoed o ran codi a chario a’u bwydo. Gan fy mod i'n ddietegydd, roedden nhw'n meddwl, o, ie, wyddoch chi, mae honno'n rôl dda. Os oes angen bwydo rhywun, gallai dietegydd wneud hynny.” Fe'i disgrifiwyd fel gweithio mewn 'rhyfel' a theimlai nad oedd ganddi fawr o ddewis a oedd yn cymryd y rôl. Roedd y swydd newydd hon hefyd yn golygu bod yn rhaid iddi deithio ymhellach i gyrraedd yr ysbyty a oedd yn ei gwneud hi'n anodd codi ei phlant o'r ysgol. “Ni chawsom unrhyw ddewisiadau o ran, 'Iawn, rydych yn adleoli i safle gwahanol ac rydym angen i chi symud i'r ysbyty nawr, oherwydd mae angen cymorth ar y dietegwyr.' A oedd mewn gwirionedd dipyn ymhellach i ffwrdd oddi wrthyf, roedd yn fwy o straen, ac nid dyna'r hyn yr oeddwn wedi cofrestru ar ei gyfer, nid dyna'r swydd y gwnes i gais amdani." |
Hanes RobertMae Robert yn ymgynghorydd clefyd yr afu a thrawsblaniad a gafodd ei adleoli i gefnogi a thrin cleifion Covid-19 mewn ICU Covid-19. Trafododd Robert sut yr oedd yn bersonol ac yn logistaidd heriol i weithio mewn rôl newydd yn ystod y pandemig, tra hefyd yn ceisio cynnal ei wasanaeth clefyd yr afu / trawsblannu ar gyfer cleifion nad ydynt yn Covid-19. Roedd gweithio mewn ICU Covid-19 yn golygu ei bod yn ofynnol iddo weithio oriau hirach. Roedd hyn yn cynnwys gweithio sifftiau dydd 12 neu 13 awr am bedwar i bum diwrnod, yn ogystal â rhai sifftiau nos. “Ar lefel bersonol yn ymateb i hynny…meysydd gwaith nad oeddech chi'n gyfforddus ynddynt, [rydych] yn gweithio oriau gwahanol, [mae] effaith ar y teulu. Yna hefyd roedd y gwasanaeth roeddwn i'n gofalu amdano a sut roedd rhaid i ni geisio cadw hynny i fynd i raddau er ein bod ni'n gwneud yr holl bethau eraill hyn. Roedd hynny’n heriol iawn.” Gwaith arferol Robert oedd trin pobl â chlefyd yr afu difrifol sy'n marw'n aml. Roedd hyn yn golygu ei fod yn teimlo'n fwy parod ar gyfer marwolaethau cleifion na rhai o'i gydweithwyr a oedd wedi cael eu hadleoli i ICU Covid-19. “Doedd y gwaith ei hun ddim yn arbennig o heriol. Nid oedd cyflawni'r rôl yn arbennig o heriol. Rwy'n meddwl mai'r pethau a oedd yn heriol oedd gweld staff nyrsio yn arbennig yn cael trafferth. Cawsant amser caled mewn gwirionedd. Eu gweld wedi cynhyrfu. Roedd llawer o nyrsys mewn dagrau yn rheolaidd. Hefyd yn gweld cydweithwyr a nifer o feddygon yn ei chael hi'n anodd iawn. Roedd yr eiliadau hynny’n galed, ond rydw i wedi arfer ag arbenigedd lle mae gennym ni nifer gweddol o gleifion sy’n marw.” |
Clywsom hefyd brofiadau tebyg gan nyrsys cymunedol plant mewn digwyddiadau gwrando.
Straeon gan nyrsys cymunedol plantRoedd sawl nyrs gymunedol plant mewn digwyddiad gwrando Mae Pob Stori’n Bwysig yn cofio cael eu hadleoli i wasanaethau oedolion yn ystod y pandemig. Mynegasant ymdeimlad dwfn o bryder ynghylch hyfforddiant annigonol ar gyfer eu rolau newydd. “Roedd yna ymdeimlad o adlach gan gydweithwyr neu reolwyr; roedd yn anodd, yn enwedig i’r rhai nad oeddent yn gyfforddus gyda’r rolau newydd.” Roedd y diffyg paratoi hwn yn eu gadael yn teimlo dan straen ac yn bryderus, gan godi pryderon am ddiogelwch cleifion oherwydd eu bod yn anghyfarwydd â'r gwaith. Roeddent yn pwysleisio’r angen am hyfforddiant a chymorth cynhwysfawr pan fydd gweithwyr gofal iechyd yn cael eu neilltuo i feysydd anghyfarwydd, yn enwedig o ystyried yr effaith bosibl ar les cleifion a’r pryder y mae’n ei achosi iddynt. “Roedd rhai nyrsys yn teimlo na allent gyflawni eu rolau yn iawn, gan beryglu cleifion o bosibl.” |
Rhannodd nyrsys a drosglwyddwyd i weithio mewn wardiau ICU Covid-19 brofiadau rheng flaen trallodus a dirdynnol gyda ni. Er enghraifft, dywedodd rhai wrthym nad oedd digon o staff profiadol i'w goruchwylio. Roedd yn rhaid iddynt ennill profiad ymarferol yn gyflym, yn aml wrth ddelio â chleifion sâl iawn a chleifion yn marw. Efallai y bydd nyrsys wedi'u hadleoli yn dechrau trwy arsylwi nyrs â phrofiad o ICU a helpu i wirio meddyginiaeth ond yn gyflym daeth y prif berson sy'n gofalu am gleifion Covid-19. Roedd y nyrsys hyn yn aml yn teimlo ymdeimlad dwfn o bryder a phryder ac nid oeddent yn teimlo'n barod i drin cleifion. Gadawodd hyn rai gyda theimladau o euogrwydd a gofid.
| “ | Roedd galw mawr am bobl a oedd wedi cael rhywfaint o hyfforddiant ICU, galw mawr am nyrsys ICU na allai gadw i fyny â'r galw a oedd gennym ar y pryd. Roedd yn golygu bod nifer y staff oedd gennym, gyda’r set sgiliau priodol i wneud y pethau oedd wir angen eu gwneud, yn gorfod cael ei wneud gan lawer llai o bobl nag y byddech yn ei ddisgwyl fel arfer.”
– Gweithiwr gofal iechyd proffesiynol yn gweithio mewn ysbyty Nightingale |
| “ | Roedd nyrs yr ICU yn goruchwylio … mewn gwirionedd yn gofalu am y claf, gan mai dim ond yn ei chynorthwyo yr oeddech chi, yn gwirio cyffuriau ac ati. y cwpl o ddyddiau cyntaf, ac yna y tu hwnt i hynny, chi oedd yn ei wneud mewn gwirionedd.”
- Nyrs ysbyty |
Roedd darparu gofal i gleifion Covid-19 yn debyg i waith yr oedd rhai wedi'i wneud cyn y pandemig. Er enghraifft, dywedodd un cynorthwyydd gofal iechyd wrthym fod ei gyfrifoldebau yn cynnwys cymryd mesuriadau pwysedd gwaed, tymheredd a siwgr yn y gwaed yn ogystal â darparu gofal hylendid personol. Roedd rhai mewn rolau clinigol yn rhannu sut roedd y drefn o gwblhau rowndiau dyddiol, asesu, derbyn a gofalu am gleifion yn debyg iawn.
| “ | Roedd llawer o adnoddau’n dod allan yn rheolaidd a oedd yn cael eu diweddaru [yn aml hefyd] o ran… pa bethau sy’n cael eu canfod i fod yn effeithiol, a pha bethau nad ydynt yn arbennig o effeithiol o ran trin cleifion COVID-19. Rwy’n meddwl mai’r peth a fu’n help mawr oedd y byddem yn wynebu her benodol am ddiwrnod neu 2 neu 3, ac yna byddai rhywun yn y gymuned feddygol yn rhywle wedi darganfod rhywfaint o ateb… ychydig wythnosau’n ddiweddarach.”
– Gweithiwr gofal iechyd Nightingale |
Clywsom sut y Newidiodd y ffyrdd yr oedd cleifion Covid-19 yn derbyn gofal a thriniaeth wrth i ganllawiau a thystiolaeth newydd ddod i’r amlwg ac wrth i’r firws gael ei ddeall yn well.
Rhannodd ychydig o staff ysbytai sut yr oedd ansicrwydd cynnar ynghylch pa driniaeth oedd orau i gleifion Covid-19: mewndiwbio cleifion a’u rhoi ar beiriant anadlu, neu ddarparu Pwysedd Llwybr Anadlu Positif Parhaus (CPAP) i gleifion, sef peiriant cymorth anadlu anadlu. sy'n defnyddio pwysau aer ysgafn i gadw llwybrau anadlu anadlu ar agor tra bod y claf yn cysgu. Wrth i dystiolaeth newydd ddod i'r amlwg, fe wnaethant droi fwyfwy tuag at ddefnyddio masgiau wyneb CPAP fel y driniaeth a ffefrir.
| “ | Ac mae'n parhau i fod yn bwnc dadleuol. Beth yw'r ffordd orau o drin y cleifion hyn? A ddylech chi ddyfalbarhau gyda'r CPAP gyhyd ag y gallwch neu eu mewndiwbio? Er gwaethaf treialon sydd wedi’u cynnal yn ystod yr ychydig flynyddoedd diwethaf, nid yw wedi’i ddatrys.”
-Meddyg ysbyty |
Dywedodd gweithwyr gofal iechyd proffesiynol wrthym eu bod yn gwneud eu gorau i ofalu Cleifion Covid-19 mewn amgylchiadau anodd iawn, ac weithiau heb yr adnoddau yr oedd eu hangen arnynt.
Stori EmmaRoedd Emma yn nyrs mewn ICU Nightingale ar gyfer cleifion Covid-19. Yn ystod anterth y don gyntaf, cofiodd Emma orfod gweithio trwy amgylchiadau anodd, megis cael nifer cyfyngedig o beiriannau anadlu a dim digon o staff. “Yn rhedeg o un lle i'r llall, yn chwilio am offer, 'Oes dim angen offer ar y claf hwn mwyach? A allwn ni ei gymryd oddi ar y claf hwnnw a'i roi i'r claf hwn?' Fe allech chi fod yn rhedeg o amgylch yr ysbyty cyfan yn chwilio am adnoddau ychwanegol, fel adnoddau anadlol, felly gwn ei fod yn straen mawr.” Bu’n rhaid iddi hi a’i chydweithwyr yn ICU Nightingale wneud penderfyniadau triniaeth Covid-19 a phenderfyniadau gofal diwedd oes yn gyflym oherwydd y cyfyngiadau staffio ac adnoddau hyn. Roedd hyn weithiau'n digwydd heb fewnbwn gan deuluoedd, gan nad oedd modd cyrraedd anwyliaid bob amser dros y ffôn. Gan ei bod mewn swydd uwch, roedd Emma yn ei chael yn hynod o straen bod yn gyfrifol am y penderfyniadau hyn. Disgrifiodd lawer o'i chydweithwyr yn gadael ICU oherwydd y straen a brofwyd ganddynt. Er gwaethaf yr heriau hyn, dywedodd Emma ei bod yn teimlo ymdeimlad o gyfeillgarwch â'i chyd-weithwyr gofal iechyd proffesiynol. “Er ei fod yn straen, roedd y naws yn fawr iawn, 'Rydyn ni i gyd yn hyn gyda'n gilydd, rydyn ni i gyd yn gwneud ein gorau gyda'r hyn sydd gennym ni.' Ac o'r hyn y byddai'r llywodraeth yn ei ddweud wrthych am adnoddau, amdanynt yn ceisio cael offer amddiffynnol personol i chi, yn ceisio cael mwy o beiriannau anadlu inni, oherwydd bod y byd i gyd yn dioddef yn yr un modd, nid oeddem yn teimlo ein bod gadael i lawr gan ein cyflogwyr neu ein llywodraeth ein hunain.” Fodd bynnag, profodd Emma rwystredigaeth hefyd gan ei bod hi a’i chydweithwyr eisiau darparu’r lefel orau bosibl o ofal i bob claf, ond nid oeddent yn gallu gwneud hyn. Nid oedd ganddynt ddigon o adnoddau anadlol bob amser. Dywedodd Emma fod llawer o benderfyniadau triniaeth yn cael eu gwneud ar sail pwy fyddai â'r siawns orau o oroesi. “Roedd yn rhaid gwneud y penderfyniadau cyflym iawn hyn yn aml er mwyn i ni allu penderfynu i ble y gallai’r adnoddau fynd, oherwydd fe allech chi gael rhywun a oedd eisoes ar ddiwedd eu hoes gyda’u canser terfynol mewn un ambiwlans ac yna yn yr ambiwlans nesaf. gallai fod, wn i ddim, dyn 60 oed sy’n garddio bob penwythnos ac yn dal i chwarae gyda’i wyrion ac wyresau.” |
Mewn rhai achosion, dywedodd gweithwyr gofal iechyd proffesiynol a oedd â chyflyrau iechyd neu wendidau iechyd wrthym sut y rhoddwyd rolau gweithio o bell iddynt, rhai nad oeddent yn cynnwys gofal cleifion personol.
| “ | Doeddwn i ddim yn cael mynd allan am nifer o fisoedd oherwydd fy mod yn dioddef o gyflwr lle gallai fod wedi bod yn fygythiad bywyd. Felly, dywedwyd wrthyf am fynd adref, felly roeddwn i'n gweithio gartref.”
- Nyrs ysbyty |
| “ | Wrth gwrs roedd yna gyflyrau iechyd ymhlith staff meddygol eraill hefyd, felly roedd yn rhaid eu hadleoli. Ystyriwyd nad oedd rhai ohonynt, yn ôl iechyd galwedigaethol, yn ddigon ffit i weithio mewn cyfrifoldeb gofal claf uniongyrchol, felly rhoddwyd rolau ychydig yn wahanol iddynt.”
-Meddyg ysbyty |
I rai gweithwyr gofal iechyd proffesiynol, roedd y posibilrwydd o ddatblygu symptomau difrifol neu farw o haint Covid-19 yn ormod o risg. Roedd rhai gweithwyr gofal iechyd o gefndiroedd lleiafrifoedd ethnig yn bryderus iawn am y dystiolaeth a oedd yn dod i'r amlwg am wendidau i'r firws ac nid oeddent yn teimlo'n gyfforddus yn gweithio.
Straeon gan nyrsys cymunedol plantYn ystod digwyddiad gwrando Mae Pob Stori’n Bwysig, fe wnaeth gweithwyr gofal iechyd proffesiynol o gefndiroedd lleiafrifoedd ethnig gofio eu pryderon dwysach eu hunain am ddiogelwch personol a’r risg o Covid-19 ar ôl dysgu bod pobl o gefndiroedd ethnig Du ac Asiaidd mewn mwy o berygl o haint Covid-19. “Gan fy ngorfodi i hynny i gyd, dywedais wrthi [rheolwr] edrych. Asiaidd ydw i. Mae astudiaethau diweddar wedi dangos bod Asiaid a phobl Dduon yn cael eu heffeithio’n aruthrol o ran marwolaethau, ac os ydych chi’n bwydo ar y fron, yn methu â chael y brechlyn, ac nid oedd hi’n cymryd dim ohono i ystyriaeth.” Roeddent yn teimlo nad oedd eu cyflogwyr yn gwneud llawer i helpu i'w hamddiffyn, ac arweiniodd hyd yn oed at un yn gadael y proffesiwn gofal iechyd allan o ofn am eu diogelwch. |
Gofal diwedd oes i gleifion Covid-19
Dywedodd staff ysbytai wrthym fod gweld cymaint o farwolaethau ymhlith cleifion Covid-19 yn peri gofid mawr.
| “ | Rydych chi'n mynd i ddelio â marwolaeth a marw ac mae'n rhan bwysig iawn o'r swydd, ac mae'n swydd y mae angen i chi ei gwneud yn dda, o ran gofal, gofalu am deuluoedd yn ogystal â gofalu am gleifion."
-Meddyg ysbyty |
Disgrifiodd cyfranwyr pa mor ofidus oeddent ynghylch cleifion yn marw ar eu pen eu hunain heb eu hanwyliaid. Ar draws y straeon a rannwyd gyda ni, roedd hyn yn cael ei weld fel un o'r agweddau anoddaf ar weithio fel gweithiwr gofal iechyd proffesiynol yn ystod y pandemig.
| “ | Roedd y ffaith bod pobl yn ITU, ac roedden nhw ar eu pennau eu hunain yn ofnadwy oherwydd roeddech chi'n gallu ei weld yn eu llygaid nhw. Gallech ei weld yng ngolwg y staff, y nyrsys, y meddygon. Yn yr anterth, roedd yn lle erchyll iawn i fod… mae’n debyg mai dyna’r peth fydd yn glynu fwyaf gyda fi, yw bod cymaint o bobl wedi marw ar eu pen eu hunain, neu gymaint o bobl wedi marw ar eu pen eu hunain gyda dim ond un aelod o’r teulu o gwmpas nhw, a oedd yn arswydus.”
- Porthor ysbyty |
Buont hefyd yn myfyrio ar sut roedd staff yr ysbyty yno ar y diwedd yn cynnig cysur i anwyliaid rhai cleifion oedd yn marw.
| “ | Roedd [eu hanwyliaid] yn ddiolchgar iawn, oherwydd roeddech chi yno pan nad oedden nhw, ac roedd hynny wedi helpu llawer gyda nhw. Roedd ganddyn nhw dawelwch meddwl eu bod nhw'n gwybod eu bod nhw mewn dwylo da.”
- Cynorthwyydd gofal iechyd ysbyty |
Rhannodd cyfranwyr enghreifftiau o sicrhau y gallai o leiaf un aelod o’r teulu ffarwelio â chlaf sy’n marw, hyd yn oed pan nad oedd hyn yn cael ei ganiatáu’n llym yn ôl y rheolau ar y pryd. Teimlodd llawer o weithwyr gofal iechyd proffesiynol ryddhad anhygoel pan laciwyd cyfyngiadau a chaniatawyd i anwyliaid ymweld â'u perthnasau oedd yn marw.
| “ | Ond os oedd yna rywun yr oeddem ni'n meddwl nad oedd yn mynd i'w wneud… yna rhoddwyd gweithdrefnau arbennig ar waith… os oedd yna rywun yr oeddem yn disgwyl y byddai'n marw yn ystod yr ychydig oriau nesaf neu'r un diwrnod, roedd llawer o ymdrech ychwanegol yn digwydd. gwneud i geisio cael anwyliaid unigol i mewn i ffarwelio, dal eu llaw, pethau felly.”
– Gweithiwr gofal iechyd Nightingale |
Trafododd rhai staff ICU geisio peidio â rhoi triniaethau diangen ac anghyfforddus ar gleifion a oedd yn annhebygol o'u helpu. Disgrifiodd un sut y gwnaethant geisio sicrhau nad oedd masgiau wyneb CPAP yn cael eu hargymell yn ddiangen i gleifion Covid-19 gan nad oeddent am i'w dyddiau olaf gael eu treulio heb allu yfed, bwyta na siarad.
| “ | Ni allem roi baich poenus, trallodus ar y claf, a beth fyddai, yn y pen draw, yn driniaeth ofer.”
-Meddyg ysbyty |
Tynnodd cyfranwyr eraill ar draws rolau gofal iechyd ysbytai sylw at bwysigrwydd trin cleifion Covid-19 sy’n marw gyda’r urddas a’r parch yr oeddent yn ei haeddu a phwysleisiwyd ei bod yn fraint trin gofal diwedd oes.
| “ | Mae'n waith pwysig iawn, ac rydych chi'n teimlo'n freintiedig iawn i fod yn darparu'r gwaith hwn hefyd…nid wyf yn teimlo'n dda amdano. Ar y llaw arall, rwy’n teimlo’n freintiedig iawn yn ei gylch, ac mae’n ddyletswydd arnaf i wneud hynny.”
-Meddyg ysbyty |
Roedd y straeon a glywsom yn disgrifio sut yr oedd yn rhaid i uwch staff a staff iau wneud penderfyniadau am ofal diwedd oes. Mewn rhai ysbytai, dywedodd cyfranwyr wrthym mai dim ond uwch feddygon profiadol oedd yn gwneud penderfyniadau am ofal diwedd oes i gleifion Covid-19. Roeddent yn disgrifio nad oeddent am roi baich ar staff iau, yn enwedig y rhai nad oedd ganddynt y profiad a'r hyder i wneud y penderfyniadau hynny.
| “ | Ni ddylem faich ar staff gradd ganol, staff iau ... ni ddylem, ac ni ddylem, ac ni wnaethom faich arnynt gyda'r penderfyniadau hyn. Roedd y rhain yn benderfyniadau y mae gennym ni’r profiad i’w gwneud.”
-Meddyg ysbyty |
Mewn ysbytai eraill, dywedwyd wrthym fod amrywiaeth o weithwyr gofal iechyd proffesiynol o lefelau hynafedd ac arbenigedd gwahanol yn rhan o wneud penderfyniadau gofal diwedd oes. Soniodd llawer o’r cyfranwyr sut yr oedd gwneud y penderfyniadau hyn yn straen – yn enwedig i’r rhai nad oeddent wedi arfer gwneud hynny.
| “ | Ond, yn enwedig ar gyfer meddygon ifanc iawn sydd ar y ward neu bobl sydd wedi cael eu, math o, cyflymu drwy ysgol feddygol i gyflym mynd i'r gwaith doedd ganddyn nhw ddim yr hyder i wybod beth oedden nhw'n ei wneud oedd y peth iawn ai peidio. A chawsant eu hamgylchynu gan bobl yn marw, mwy nag un claf mewn diwrnod ac yn aml yn anghyfforddus ac yn edrych yn ofidus pan buont farw. Os nad oes gennych chi'r hyder hwnnw, mae'r sicrwydd hwnnw ac mae'r cyfan braidd yn newydd i chi ac rydych chi wedi'ch amgylchynu gan anhrefn a dioddefaint a marwolaeth, yna rwy'n meddwl ei fod llawer mwy o straen.”
-Meddyg ysbyty |
Clywsom sut y gwnaed penderfyniadau gofal ar gyfer cleifion Covid-19 yn seiliedig ar hanes meddygol, cyflyrau iechyd sylfaenol, ac ansawdd bywyd blaenorol. Trafododd cyfranwyr a oedd yn trin cleifion Covid-19 sâl iawn pa mor anarferol a heriol oedd gorfod gwneud penderfyniadau am ofal diwedd oes i gynifer o gleifion ar unwaith.
Dywedasant eu bod yn defnyddio'r holl wybodaeth oedd ganddynt am glaf i wneud y penderfyniadau hyn orau y gallent. Roedd hyn yn cynnwys yr hyn a oedd yn hysbys amdanynt, megis eu hoedran ac a oedd ganddynt gyflyrau sylfaenol a allai fod wedi'i gwneud yn fwy tebygol y byddent yn goroesi neu'n gweld y budd mwyaf o driniaethau penodol, fel awyru. Dywedodd rhai o staff ysbytai, yn enwedig meddygon, eu bod yn gallu defnyddio'r wybodaeth bresennol am sut i reoli a gwneud y mathau hyn o benderfyniadau. Roedd hyn yn seiliedig ar brofiadau tebyg mewn gofal dwys neu mewn meysydd fel meddygaeth resbiradol.
| “ | Roeddem yn gwybod yn gyflym iawn i bwy y dylem fod yn mynd yn syth i ofal diwedd oes. Claf 90 oed sydd wedi bod yn sâl ers rhai dyddiau, yr oedd cyfradd curiad ei galon yn uchel iawn, yr oedd ei bwysedd gwaed yn sydyn o isel, y cafodd pelydr-X o'r frest ei heintio'n ddifrifol gan y cyflwr llidiol, y cyflwr heintus a llidiol, sef Covid. -19. Roedden nhw'n ddiwedd oes. Dydyn ni ddim yn mynd ymlaen i oed ar ein pennau ein hunain gyda dim byd, gyda llaw, ond mae’n oed ac yn cyd-forbidrwydd gyda bod yn 95 oed daw salwch arall, daw eiddilwch.”
-Meddyg ysbyty |
| “ | Felly, pe bai gen i ddyn neu fenyw 70 oed neu 75 oed â Covid-19 a oedd yn methu CPAP a bod yn rhaid i mi naill ai eu rhoi ar beiriant anadlu neu beidio â'u rhoi ar beiriant anadlu, gallaf fod wedi trafodaeth gyda nhw… A byddai rhai pobl yn dweud, 'Rydw i eisiau rhoi cynnig arni', a byddai rhai pobl yn dweud, 'Dydw i ddim eisiau rhoi cynnig arni', ac yna o'r ddau grŵp hynny roedd rhai yn byw, bu farw rhai.”
-Meddyg ysbyty |
Clywsom enghreifftiau o gleifion Covid-19 a dderbyniwyd i’r ysbyty yn cael hysbysiad DNACPR. Roedd hyn yn golygu na fyddent yn cael eu dadebru. Rhannodd un cyfrannwr sut y byddai uwch feddygon yn ceisio esbonio’r amgylchiadau ar gyfer gwneud penderfyniad DNACPR i deuluoedd dros y ffôn.
| “ | Nid yw cleifion lle [maent] wedi cael ffurflen goch, sef DNACPR, yn dadebru, ond roedd ganddyn nhw Covid-19, ond roedd ganddyn nhw amodau eraill hefyd. Roedd o fudd iddyn nhw na fyddai galwad [am ddadebru] yn cael ei rhoi iddyn nhw, felly roedd yn rhaid i chi, fel y bu’n rhaid eu gwneud dros alwadau ffôn a galwadau fideo i deuluoedd.”
- Cynorthwyydd gofal iechyd ysbyty |
Dywedodd cyfranwyr wrthym fod gofal diwedd oes weithiau’n golygu bod staff ysbytai gyda chleifion sy’n marw pan na allai eu hanwyliaid wneud hynny.
| “ | Nid oes neb eisiau i neb farw ar ei ben ei hun, ac fel nyrsys rydych chi'n ymdrechu'n galed iawn i wneud yn siŵr nad yw hynny'n digwydd os na all aelodau'r teulu fod yno, rydych chi yno. Rydych chi'n unig. Rydych chi'n ei wneud e."
- Nyrs ysbyty |
Er enghraifft, trafododd un cynorthwyydd gofal iechyd ddal dwylo claf oedd yn marw wrth i'w deulu edrych ymlaen drwy ffenestr. Yn ogystal â bod gyda chleifion ar adeg eu marwolaeth, roedd staff ysbytai yn gweld darparu gofal personol a threulio amser gyda chleifion fel rhan bwysig o'u cyfrifoldebau gofal diwedd oes.
| “ | Cribo eu gwallt oedd o... hufennu eu cyrff, dangos hynny iddyn nhw cariad … newid eu cynfasau gwely, gwneud iddynt wrando ar eu ffefryn cerddoriaeth, yn rhoi bath i rai cleifion, wyddoch chi, yn eu maldodi.”
- Cynorthwyydd gofal iechyd ysbyty |
Dywedodd rhai o staff yr ysbyty wrthym eu bod yn gysylltiedig â chleifion Covid-19 yr oeddent yn gofalu amdanynt. Byddent yn galaru am golli eu cleifion, yn enwedig y rhai yr oeddent wedi dod yn agos atynt trwy ddarparu gofal dyddiol.
Cefnogi teuluoedd mewn profedigaeth
Dywedodd rhai o staff yr ysbyty wrthym pa mor anodd oedd hi i gefnogi teuluoedd mewn profedigaeth nad oeddent yn gallu ymweld pan fu farw eu hanwyliaid. Roedd y teuluoedd hyn yn gweld peidio â bod yno'n bersonol yn boenus iawn ac yn anodd ymdopi ag ef.
| “ | Ac yna, ar adegau, roedd gennyf berthnasau cleifion a fyddai'n fy ffonio a dweud, 'A yw fy mherthynas wedi marw mewn gwirionedd? Sut ydw i'n gwybod eu bod nhw wedi marw? Ffoniodd y ward fi a dweud wrthyf, ond doeddwn i ddim yn cael dod i mewn i weld y corff.'”
- Caplan yr ysbyty |
Rhannodd llawer o gyfranwyr sut roedd yn rhaid iddynt wneud galwadau ffôn i anwyliaid cleifion i naill ai drafod gofal diwedd oes neu roi gwybod iddynt fod eu hanwyliaid wedi marw. Cyn y pandemig, byddai'r sgyrsiau hyn fel arfer wedi digwydd yn bersonol. Roedd y gweithwyr gofal iechyd proffesiynol a wnaeth y galwadau hyn yn aml yn teimlo na allent gynnig y cymorth cywir na chyfleu digon o dosturi na chysur i deuluoedd mewn profedigaeth dros y ffôn neu drwy alwadau fideo. Disgrifiodd cyfranwyr deimlo’n rhwystredig, yn ofidus ac ar goll gan na allent roi’r atebion a’r esboniadau i’w hanwyliaid.
| “ | Nid gwaith corfforol, gwaith, gwaith yn unig ydyw; mae'n fwy ochr feddyliol ac emosiynol yr hyn yr ydym ni, yr hyn yr ydych yn delio ag ef. Cleifion [anwyliaid] yn crio i lawr y ffôn i chi a byddai gennyf [dim] atebion [ar eu cyfer], ac rydych yn mynd yn unig, 'Edrychwch, rydym yn ceisio ein gorau. Rydyn ni'n ceisio gwneud beth allwn ni', ond rydych chi'n gwybod mai dyna yw mam, tad, modryb, ewythr, merch, mab rhywun arall.”
– Gweithiwr gofal iechyd proffesiynol perthynol |
| “ | Roedd siarad â rhywun ar y ffôn ac esbonio iddynt beth sy’n mynd i ddigwydd, sut mae’n mynd i ddigwydd, yn hynod o anodd ac roedd y nifer enfawr yn llethol i lawer o’r staff a oedd yn ymwneud llawer mwy â darparu’r gofal.”
-Meddyg ysbyty |
Nid oedd sgyrsiau gyda theuluoedd mewn profedigaeth yn rhan o rolau arferol rhai gweithwyr gofal iechyd proffesiynol. I staff eraill a rannodd eu stori gyda ni, roedd delio â marwolaeth a phrofedigaeth yn fwy cyfarwydd, a pharhaodd hyn yn ystod y pandemig. Roedd hyn yn arbennig o wir yn achos cyfranwyr a oedd yn gweithio mewn wardiau fel yr ICU sy'n gweld marwolaethau cleifion yn amlach.
Stori RaviRoedd Ravi yn anesthetydd ac yn ymgynghorydd mewn ward ITU Covid-19. Fel ymgynghorydd, un o brif gyfrifoldebau Ravi oedd cyfathrebu â theuluoedd cleifion Covid-19 dros y ffôn. Roedd Ravi yn ei chael hi’n hynod o heriol cael sgyrsiau am ofal diwedd oes, marwolaeth claf, a phrofedigaeth bob dydd, yn enwedig pan oedd yn rhaid iddo ddweud wrth deuluoedd am farwolaeth gan wybod bod y cyfyngiadau pandemig yn golygu efallai na fyddai ganddyn nhw unrhyw un gyda nhw i ddarparu cysur. a chefnogaeth. I Ravi, roedd galw teuluoedd mewn profedigaeth y naill ar ôl y llall yn flinedig ac yn flinedig yn emosiynol. Disgrifiodd hyn fel un o'r pethau mwyaf 'erchyll' y mae wedi gorfod ei wneud. “I gael y sgyrsiau hynny dros y ffôn gyda phobl nad ydych erioed wedi siarad â nhw o'r blaen pan nad ydych chi'n gwybod pwy sydd yn yr ystafell ar y pen derbyn, pan fydd y person ar y pen derbyn weithiau ar ei ben ei hun ac rydych chi'n ymwybodol hynny nid oes ganddynt unrhyw un i roi cwtsh iddynt pan fyddwch yn rhoi'r ffôn i lawr, pan oedd y tro diwethaf iddynt weld eu perthynas yn iach, dim ond yn cael eu cludo i'r ysbyty i gael eu gwirio yr oeddent. Nawr 48 awr yn ddiweddarach, rydych chi'n eu ffonio i ddweud wrthyn nhw fod eu perthynas yn marw ac nad ydyn nhw'n eich credu chi a pham y dylen nhw? Ac mae ganddyn nhw gwestiynau na allwch chi eu hateb, ac mae gennych chi atebion nad ydyn nhw eu heisiau. Mae'n anodd iawn ac ni allant ymweld." Daeth Ravi hefyd i adnabod cleifion yn yr ITU a'u teuluoedd o ofalu amdanynt a'u trin, yn aml dros sawl wythnos. Roedd hyn yn golygu ei fod yn aml yn cael ei fuddsoddi'n bersonol yn y cleifion ITU. Er bod delio â'u marwolaethau yn heriol i Ravi, ceisiodd wneud marwolaeth ei gleifion mor urddasol â phosibl. Edrychodd am gyfleoedd i gleifion sy'n cyrraedd diwedd eu hoes gael un sgwrs olaf gyda'u hanwyliaid. “Rydym yn ceisio cael ansawdd i deuluoedd, ac felly, hyd yn oed os, wyddoch chi, gallaf ddeffro claf am 2 awr fel y gallant gael cyfle i gael sgwrs gydlynol gyda'u hanwyliaid, mae hynny'n fuddugoliaeth, oherwydd mae hynny'n werthfawr. Ac, wyddoch chi, os ydyn nhw'n mynd i farw, os gallwn ni wneud y pasio hwnnw mor urddasol a heb fod mor erchyll ag y gall fod, gan wybod ei fod yn mynd i fod yn erchyll, ac os gallwn ni dynnu dim ond rhai o'r ymylon oddi arno, mae'n dal i fod yn ddrwg." |
Clywsom hefyd pa mor anodd a dirdynnol oedd siarad â’r rhai a oedd yn credu y gallent fod wedi trosglwyddo Covid-19, ac felly’n teimlo’n gyfrifol am farwolaeth eu hanwyliaid, a’u cysuro. Roedd yr anwyliaid yn aml yn ofidus iawn ac yn teimlo'n euog nad oedd unrhyw beth y gallent ei wneud.
| “ | Cawsom glaf…[lle’r] ferch a oedd yn gweithio yn y ganolfan iechyd [dal] Covid-19 ac yna ei ledaenu iddo a bu farw o Covid-19. Felly, yn y senario hwnnw a oedd yn eithaf trallodus i’r teulu hwnnw oherwydd y pryder oedd mai canser a fyddai’n lladd y claf hwnnw, tra ildiodd i Covid-19 mewn gwirionedd.”
- Nyrs ysbyty |
Cefnogi cleifion â chyflyrau iechyd nad ydynt yn ymwneud â Covid
Er bod llawer o'r straeon a rannwyd gyda ni gan staff ysbytai yn canolbwyntio ar gefnogi cleifion Covid-19, parhaodd ysbytai i ofalu am gleifion eraill hefyd. Rhannodd y rhai a ddarparodd ofal y tu allan i wardiau Covid-19 lawer o straeon am yr heriau a wynebwyd ganddynt yn ystod y pandemig.
Roedd y galw am ofal ysbyty i gleifion nad ydynt yn ymwneud â Covid-19 yn amrywio. Disgrifiodd cyfranwyr sut roedd pobl yn ofni mynd i ysbytai. Roedd hyn yn golygu bod rhai staff ysbytai wedi gweld llai o gleifion nad oeddent yn ymwneud â Covid 19, yn enwedig yn gynnar yn y pandemig.
Yn ddiweddarach yn y pandemig, rhannodd cyfranwyr sut y gwelsant ôl-groniad o gleifion sydd angen gofal ar draws llawer o arbenigeddau. Roedd hyn yn cynnwys plant, cleifion canser, a chleifion â chlefydau difrifol eraill a chyflyrau iechyd parhaus. Dywedodd staff yr ysbyty fod yr ôl-groniad o ganlyniad i leihau neu gau'r ddau wasanaeth (fel y trafodir isod), a chleifion yn gyndyn o gael mynediad at ofal.
Fodd bynnag, rhannodd rhai o staff ysbytai sut yr oeddent yn parhau i weld cleifion drwy gydol y pandemig. Er enghraifft, soniodd y rhai sy'n gweithio ym maes obstetreg a gynaecoleg fod eu llwyth gwaith yn normal i raddau helaeth. Dywedodd un cyfrannwr, nyrs iechyd rhywiol, wrthym ei bod wedi gweld cynnydd yn nifer y cleifion sy’n ceisio triniaeth a gofal yn ystod y pandemig.
| “ | Roedd y llwyth gwaith oedd gen i ym maes iechyd rhywiol yn llawer mwy oherwydd doedd pobl ddim yn stopio cael rhyw. Wnaethon nhw ddim stopio cael heintiau a drosglwyddir yn rhywiol. Wnaethon nhw ddim stopio bod angen cyngor cynllunio teulu ac atal cenhedlu…mae’n debyg bod mwy o bobl gartref. Bu cynnydd mewn trais domestig a phethau felly hefyd, yr ydym yn ymdrin â hwy hefyd. Ymosodiad rhywiol. Felly, cynyddodd ein llwyth gwaith, ond roedd gennym lai o staff i ddelio ag ef.”
– Nyrs iechyd rhywiol |
Dywedodd cyfranwyr wrthym sut y cafodd gofal nad yw’n ymwneud â Covid-19 ei gwtogi, gyda chanlyniadau difrifol i lawer o gleifion, gan gynnwys marwolaethau y credent y gellid eu hosgoi. Mae llawer o'r straeon a rennir gan feddygon ysbyty yn disgrifio sut gwaethygodd cyflyrau meddygol cleifion oherwydd nad oedd gofal ysbyty ar gael. Teimlai rhai cyfranwyr fod y dad-flaenoriaethu hwn o ofal iechyd nad yw’n gysylltiedig â Covid-19 yn ganlyniad i ormod o bwyslais ar gyfyngiadau pandemig a Covid-19.
Dysgu ar gyfer y dyfodol: cydbwyso risgiau a pharhau i gynnig gofalThema gyffredin ym myfyrdodau cyfranwyr ar ofal iechyd yn ystod y pandemig oedd y dylid bod wedi rhoi mwy o bwyslais ar risgiau iechyd corfforol a meddyliol eraill. Roedd llawer o gyfranwyr yn meddwl y dylid bod wedi gwneud mwy i ystyried y risgiau iechyd hyn nad ydynt yn ymwneud â Covid-19 pan wnaed penderfyniadau am ganllawiau a chyfyngiadau Covid-19. “Fe wnaethon nhw ganolbwyntio ar un agwedd a cholli golwg ar y bobl hynny nad oedd yn mynd i gael diagnosis canser, ddim yn mynd i gael triniaeth, ddim yn mynd i gael llawdriniaeth gardiaidd. Mae yna lawer o bobl yn mynd i farw ac wedi marw oherwydd effaith Covid-19.” – Gweithiwr gofal iechyd proffesiynol perthynol “Rhaid i ni byth ailadrodd y neges, 'Os nad oes gennych chi Covid-19, nid oes gennym ni ddiddordeb ynoch chi'. Mae'n rhaid i'r neges fod gofal iechyd yn parhau yn ôl yr arfer ac os yw'n ormod o risg i adael y cartref, wel rydym yn cracio ymlaen ac rydym yn parhau i wneud y clinigau ac rydym yn defnyddio'r ffôn ac rydym yn defnyddio fideo a beth bynnag sydd gennym. Nid yn unig rydym yn cefnu ar bobl.” -Meddyg ysbyty Clywsom dro ar ôl tro sut y dylid bod wedi gwneud mwy i barhau â gofal meddygol arferol ac atal salwch difrifol a marwolaethau y gellir eu hosgoi. Roedd hyn yn aml yn cael ei weld fel rhywbeth a ddylai fod wedi bod yn bosibl gyda'r cynlluniau a'r rhagofalon cywir yn eu lle. “Os ydych chi'n meddwl am yr adrannau, wyddoch chi, cleifion allanol, a oedd ar gau ... rwy'n dal i feddwl bod lle i gadw rhai gwasanaethau i redeg gyda rhagofalon, ie, ar lif cleifion llawer is ond rwy'n cwestiynu, wyddoch chi, roedd yna llawer o bobl allan o’r ysbyty a allai fod wedi cael eu defnyddio mewn ffyrdd eraill i gadw atgyfeiriadau i fynd.” - Meddyg Teulu “Dywedwyd wrth bobl am aros adref, ond mae gofal iechyd mor hanfodol na allwch wneud y lleiafswm lleiaf posibl. Erbyn hyn mae ôl-groniadau enfawr. Roedd angen i'r ddarpariaeth fod wedi parhau. Roedd problem o ran adnoddau ac mae ôl-groniad bellach oherwydd dywedwyd wrth bobl am beidio â dod ymlaen a nawr mae ôl-groniad o apwyntiadau wedi’u canslo.” - Meddyg Teulu |
Clywsom sut roedd gofod wardiau a gwelyau ICU yn aml yn cael eu blaenoriaethu ar gyfer trin cleifion Covid-19, gan adael llai o adnoddau ar gyfer trin cleifion nad ydynt yn ymwneud â Covid-19. Tynnodd rhai gweithwyr gofal iechyd proffesiynol sylw at brinder gwelyau gofal dwys ar gyfer cleifion nad ydynt yn ymwneud â Covid-19. O ganlyniad, rhoddodd rhai cyfranwyr enghreifftiau o gleifion sâl iawn nad oeddent yn cael y gofal y byddent fel arfer yn ei gael.
| “ | Peth mawr yr ydym yn ei ddarparu yw gofalu am bobl â chlefyd yr afu o gwmpas y wlad a hefyd trawsblannu. Mae angen gwelyau gofal dwys ar drawsblannu… ac roedd gwir ddiffyg adnoddau gennym.”
-Meddyg ysbyty |
| “ | Rwy'n meddwl yn broffesiynol ei bod yn anodd iawn, iawn i beidio â gallu gwneud y swydd i'r safon yr ydym am ei gwneud. Rydym yn gosod safonau uchel iawn i ni’n hunain fel gweithwyr proffesiynol, ac ar y cyfan rydym yn gwneud popeth o fewn ein gallu i gyrraedd y safonau hynny, ond roedd yn amhosibl yn gorfforol i wneud hynny oherwydd cyfyngiadau adnoddau ar y pryd.”
-Meddyg ysbyty |
Myfyriodd llawer o weithwyr gofal iechyd proffesiynol ar ba mor bryderus oeddent ynghylch gadael cleifion yr oedd angen gofal nad oedd yn ofal brys arnynt. Nid oedd cau rhai gwasanaethau yn gwneud synnwyr i rai meddygon ysbyty, yn enwedig wrth i'r pandemig fynd rhagddo. Roeddent yn dadlau bod anghenion eu cleifion yn cael eu hanwybyddu neu eu dad-flaenoriaethu pan na ddylent fod wedi gwneud hynny.
Dywedodd cyfranwyr wrthym fod llai o lawdriniaethau dewisol mewn ysbytai hefyd. Mewn rhai achosion, dywedon nhw fod gweithrediadau brys dewisol a hyd yn oed arferol nad ydynt yn Covid-19 yn cau'n gyfan gwbl. Dywedasant wrthym sut yr oeddent yn credu bod hyn wedi arwain at farw rhai cleifion nad oeddent yn ymwneud â Covid-19 oherwydd nad oeddent wedi cael y llawdriniaethau achub bywyd na’r triniaethau brys eraill yr oedd eu hangen arnynt. Roedd gweithwyr gofal iechyd proffesiynol a rannodd y straeon hyn yn grac ac yn rhwystredig ac yn meddwl y gellid bod wedi osgoi'r marwolaethau hyn.
| “ | Pobl yn troi i fyny gyda chlefydau, canserau er enghraifft, a oedd yn fwy datblygedig nag y byddent wedi bod fel arall, yn aml gyda chanlyniadau a newidiodd eu bywydau oherwydd nad oeddent wedi gallu cael apwyntiad wyneb yn wyneb. Ac nid canser yn unig, ond hefyd afiechydon gwanychol iawn. Mae gennyf sawl achos yn fy meddwl o bobl a oedd yn dioddef o gyflyrau anfalaen ond cyfyngol, a oedd yn hawdd iawn eu trwsio pe baent wedi cael mynediad at ofal iechyd acíwt yn gynt. Ond, wyddoch chi, roedd hi’n anodd iawn iddyn nhw gael mynediad at ofal iechyd, i weld y person roedd angen iddyn nhw ei wneud.”
-Meddyg ysbyty |
Clywsom lawer o straeon am effaith barhaol hyn ar gleifion. Er enghraifft, disgrifiodd un cyfrannwr anghenion gofal lliniarol ychwanegol ar gyfer cleifion canser yr amharwyd ar eu cynlluniau triniaeth. Mae'r oedi i driniaeth hefyd wedi gwaethygu canlyniadau i gleifion â chyflyrau eraill.
| “ | Rwyf nawr yn ôl yn gweld cleifion ag MS a chlefydau ymennydd prinnach eraill, a'r hyn sy'n amlwg iawn yw faint o niwed sylweddol y maent wedi'i niweidio gan y pandemig, gan esgeulustod, felly dim ond newydd ddod i'r amlwg y mae hynny. Rydyn ni'n dal i weld pobl mewn clinigau nawr nad ydyn nhw wedi cael eu gweld ers 3 neu 4 blynedd wyneb yn wyneb, ac maen nhw wedi cael eu hesgeuluso ac maen nhw'n fwy anabl o ganlyniad, maen nhw'n fwy isel eu hysbryd, maen nhw' yn fwy ynysig ac nid yw eu problemau wedi cael sylw.”
-Meddyg ysbyty |
Nid oedd trafodaethau am ofal diwedd oes a phrofedigaeth yn llai emosiynol i gleifion nad oeddent yn ymwneud â Covid-19 a’u hanwyliaid. Yn yr un modd â chleifion Covid-19, canfu cyfranwyr fod cyfathrebu gwybodaeth sensitif ac emosiynol yn arbennig o anghyfforddus dros y ffôn.
| “ | Mae rhai meddygon yn dda iawn am gael y drafodaeth honno ac mae rhai meddygon yn gwbl ofnadwy ac rwy'n meddwl i rai cleifion mai'r adborth gan y cleifion i'r tîm oedd eu bod wedi canfod hynny'n eithaf syfrdanol. Felly, roedd negeseuon i gleifion neu berthnasau cleifion yn cael eu cyflwyno gan staff nad oedd yn ôl pob tebyg wedi’u hyfforddi’n dda iawn i gynnal y trafodaethau hynny.”
- Nyrs ysbyty |
Rhannodd rhai cyfranwyr sut yr oedd yn rhaid iddynt ddweud wrth anwyliaid fod eu perthynas wedi marw, neu eu bod ar ddiwedd eu hoes oherwydd bod gweithwyr gofal iechyd proffesiynol wedi awgrymu bod gwasanaethau nad oeddent yn ymwneud â Covid-19 yn cael eu cau. Roedd y sgyrsiau heriol iawn hyn weithiau'n cynnwys cleifion a oedd ar ddiwedd eu hoes.
| “ | Rwy’n cofio gorfod ceisio dweud wrtho ef a’i frawd yr un mor oedrannus dros y ffôn, nad oeddem yn mynd i fod yn gwneud llawdriniaeth, ac felly byddai’n bendant yn marw. Ac mae'n debyg bod hyn ym mis Mawrth 2020 pan na chawsom unrhyw ymwelwyr o gwbl mewn gwirionedd, ac felly roedd hynny'n anhygoel o galed. Ac yna roedd mewn ystafell ochr, felly yn gadael yr ystafell honno ac yn gwybod ei bod yn debyg na fyddai neb gydag ef yn y funud y bu farw, ac felly na fyddai'n cael y cysur dynol hwnnw. ”
-Meddyg ysbyty |
Rhannodd cyfrannwr arall ei brofiad o orfod dweud wrth glaf â thrydylliad coluddyn dros y ffôn eu bod yn mynd i farw oherwydd na ellid cynnig llawdriniaeth iddynt. Roedd hyn oherwydd bod y llawdriniaeth yn risg gymedrol uchel ac aseswyd ei bod yn fwy peryglus oherwydd Covid-19.
| “ | Ar y pryd roedd y dystiolaeth yn awgrymu nad oedd cynnal llawdriniaethau ar bobl yn arbennig o ddiogel, yn enwedig os oedd ganddynt Covid. Roedd yn golygu y byddai pobl a fyddai’n cael cynnig llawdriniaeth ar unrhyw adeg arall, llawdriniaeth frys i drwsio rhywbeth trychinebus o’i le arnynt fel trydylliad y coluddyn, y byddem fel arfer yn bwrw ymlaen ag ef heb feddwl ddwywaith, yn cynnig llawer llai o’r llawdriniaethau hynny. Ac wrth wneud hynny, yn gwybod bod pobl yn mynd i farw o ganlyniad, ac roedd hynny'n amlwg yn anodd iawn. ”
-Meddyg ysbyty |
Profiadau staff ysbyty anghlinigol
Dywedodd cyfranwyr wrthym fod y pandemig wedi cael effaith enfawr ar staff cymorth ysbytai, yn ymarferol ac yn emosiynol. Mae staff cymorth ysbytai anghlinigol, fel porthorion a staff arlwyo, yn darparu gwasanaethau hanfodol i alluogi gofal cleifion. Roedd rhai cyfranwyr a oedd yn gweithio yn y rolau hyn i raddau helaeth yn gallu parhau fel y byddent, ond profodd eraill newidiadau sylweddol. Er enghraifft, dywedodd rhai bod yn rhaid iddynt ganolbwyntio ar rai agweddau o’u rôl a blaenoriaethu tasgau’n wahanol tra bod eraill yn gorfod gweithio mewn ffyrdd newydd i gynnal pellter cymdeithasol.
| “ | Roedd ward arbennig, alla i ddim cofio pa un oedd hi, a pan wnaethon ni ddosbarthu bwyd yno, roedd rhwystr, reit, ac roedd rhaid gwthio'r troli drwy'r rhwystr a pheidio mynd i mewn yno...roedd rhaid i'r staff gwisgo rhywbeth fel siwtiau gofod i'w hatal rhag cael Covid. A hefyd, roedd yn rhaid i ni olchi ein dwylo’n fwy rheolaidd, roedd yn rhaid i ni wisgo masgiau drwy’r amser, dim esgus … roedd yn rhaid i ni fod yn ofalus iawn ynglŷn â hylendid a chyswllt corfforol ag eraill.”
– Staff arlwyo ysbytai |
Dywedodd cyfranwyr wrthym sut y profwyd y cynnwrf a achoswyd gan y pandemig ar draws gwahanol rolau mewn ysbytai, nid ymhlith staff clinigol yn unig. Er enghraifft, disgrifiodd caplaniaid ysbytai a rannodd eu stori gyda ni sut yr oeddent yn cefnogi cleifion Covid-19 trwy fod gyda nhw, dal eu dwylo, siarad a darllen gyda nhw, a gweddïo wrth erchwyn eu gwelyau. Mewn rhai ysbytai, nid oedd y caplaniaid yn cael cerdded y wardiau a bu'n rhaid i'r claf neu ei deulu, neu aelod o staff, ofyn iddynt ymweld â hwy. Soniodd un caplan ysbyty hefyd am drefnu galwadau ffôn rhwng cleifion Covid-19 a’u hanwyliaid.
Bu porthorion ysbytai hefyd yn trafod sut roedd yn rhaid iddynt ddysgu gwahanol ddulliau gwaredu ar gyfer deunyddiau sy'n dod gan gleifion Covid-19 na chan gleifion nad oeddent yn Covid-19.
| “ | Newidiodd y lliain i gyd, newidiodd y sbwriel i gyd, felly os oedd unrhyw beth o ward heintiedig, yn hytrach na mynd i mewn i fag gwastraff domestig arferol, byddai'n mynd i mewn i fag oren neu fag streipen teigr, felly byddai'n cael ei losgi yn hytrach na. tirlenwi.”
- Porthor ysbyty |
Dywedodd rhai cyfranwyr wrthym, lle bo modd, bod rolau desg yn cael eu symud i fod yn rhai anghysbell. Roedd hyn fel bod llai o bobl mewn ysbytai i gefnogi cadw pellter cymdeithasol. Mewn rhai achosion, roedd swyddfeydd yn cael eu hailosod i leoliadau gofal.
| “ | Ac un o'r dyddiau, fe aethon ni i mewn i'r gwaith, a dywedwyd wrthym yn y bôn, 'Paciwch eich bagiau a ewch adref,' ac roedd pawb yn gweithio gartref. Felly nid oedd unrhyw hysbysiad, dim byd. Yn y bôn, 'Paciwch eich bagiau, ewch adref,' ac yna yn amlwg fe wnaeth pawb bacio eu bagiau, aethant adref. Roedd pobl yn gofyn a allent fynd i'r swyddfa i godi eitemau eraill. Chewch chi ddim dychwelyd i'r swyddfa."
- Staff gweinyddol ysbytai |
Dywedodd staff gweinyddol a chymorth TG wrthym eu bod wedi profi newid mewn ffocws yn eu rôl. Roedd yn rhaid iddynt sicrhau bod systemau ar waith i gefnogi cadw pellter cymdeithasol a lleihau nifer y cleifion sy'n dod i'r ysbyty oni bai bod hynny'n gwbl angenrheidiol.
| “ | Fe wnaethom gysylltu â chwmni tacsi lleol i ddosbarthu meddyginiaeth i gleifion yn y bôn. Yn llythrennol o fewn dau ddiwrnod, roeddem ni o fewn ein tîm wedi gwneud dosbarthiad cartref ad hoc. Wedi cysylltu â chleifion, dywedodd wrthynt, 'Ni allwch ddod i fyny i'r ysbyty,' a byddwn yn dweud nad oedd 90 y cant am ddod i fyny beth bynnag. 'Bydd eich meddyginiaeth yn cael ei ddosbarthu mewn tacsi. Ni fydd y tacsi yn gwybod eich enw, ni fyddant yn gwybod y feddyginiaeth, byddant yn llythrennol yn ei ddosbarthu.' …aethant, 'Ie, fe gymerwn ni,' oherwydd doedden nhw ddim yn cael unrhyw waith.”
- Staff gweinyddol ysbytai |
Yng nghamau cynnar y pandemig, roedd yr ansicrwydd yn golygu dywedodd staff cymorth wrthym fod yn rhaid iddynt wneud eu gorau i helpu staff clinigol heb wybod beth oedd fwyaf defnyddiol na'r ffordd orau o reoli eu gwasanaeth yng nghyd-destun pandemig. Dywedodd un cyfrannwr a oedd yn gweithio mewn labordy ysbyty fod yn rhaid iddo addasu ei wasanaethau i ystyried halogiad Covid-19 mewn samplau er nad oedd yn cynnig profion Covid-19.
| “ | Nid oeddem yn profi am Covid-19, ond efallai bod samplau wedi'u heintio â Covid. Byddai swabiau gwddf ar gyfer unrhyw beth yn cael eu hystyried yn brawf heintus. Hyd yn oed pe baem ond yn gwirio am MRSA neu'n gwirio bod ganddynt strep gwddf, byddai'n rhaid gwneud hynny o dan amodau lefel cyfyngu oherwydd gallai fod ar ôl Covid-19. Ar y dechrau, doedden ni ddim yn gwybod dim byd. Nid oeddem yn gwybod a oedd yn sied mewn wrin. Doeddwn i ddim yn gwybod a oedd yn llenwi gwaed, felly gwnaed ein holl brofion trwy Gategori 3. Wrth gwrs, ni allem oherwydd mai dim ond 2 ystafell yw hynny.”
- Technegydd labordy ysbyty |
Rhannodd rhai staff cymorth sut y gwnaethant gynyddu eu horiau a’u cyfrifoldebau yn ystod y pandemig i reoli'r llwyth gwaith trymach. I rai, roedd hyn yn cael ei weld fel rhywbeth cadarnhaol oherwydd nid yn unig eu bod yn helpu, ond roedd eu set sgiliau hefyd yn cael ei ehangu.
| “ | Roeddwn i'n meddwl efallai eu helpu, oherwydd rwy'n gwybod eu bod yn brysur ... a dim ond helpu'r GIG yw hyn. Felly, roeddwn i'n meddwl ei fod yn weithred dda ac roeddwn i'n meddwl, wel, iawn, efallai y byddwn i'n ei wneud hefyd."
– Staff arlwyo ysbytai |
Disgrifiodd eraill eu rolau newydd fel rhai mwy heriol, yn enwedig lle'r oedd adleoli'n golygu eu bod yn gweithio'n agosach at wasanaethau rheng flaen nag yr oeddent wedi arfer ag ef.
| “ | Ni chawsant eu hyfforddi i fod ar y rheng flaen, i fod mewn gofal critigol, i weld cleifion a oedd mor sâl â hynny. Felly, roeddent yn dod yn ôl gyda phroblemau iechyd meddwl a methiannau, ac yn mynd i ffwrdd yn sâl, ac roedd lefelau salwch yn eithaf uchel. Roedd yr effaith yn enfawr.”
– Cefnogaeth rheoli ysbytai |
Er nad oeddent yn darparu gofal meddygol, dywedodd rhai staff cymorth ysbytai wrthym sut yr oeddent yn ceisio cysylltu â chleifion a'u teuluoedd. Roedd glanhawyr ysbytai a staff arlwyo yn rhyngweithio â chleifion a'u teuluoedd wrth iddynt gyflawni eu tasgau o ddydd i ddydd. Gallent weld pa mor anodd ydoedd i deuluoedd oedd wedi eu gwahanu oddi wrth eu hanwyliaid ac felly yn ceisio gwneud yr hyn a allent i gysylltu â chleifion a theuluoedd, er bod hyn yn aml yn peri gofid.
| “ | Roedd hi mor braf gwneud hynny ... mae'n debyg bod gennych chi lawer mwy o amser na rhai nyrsys, oherwydd ni yw'r rhai sydd yn eu hystafelloedd ac yn mopio i ffwrdd ac yn sgwrsio â nhw a gwneud paned o de iddynt. Rydych chi'n dod i'w hadnabod ychydig bach ... mae'n ei gwneud hi ychydig yn dristach, oherwydd rydych chi'n meddwl, maen nhw eisoes wedi cael eu lladrata.”
- Glanhawr ysbyty |
I rai cyfranwyr, roedd cynnig cymorth i gleifion yn cynnwys gofal diwedd oes ac ar gyfer profedigaeth. Roedd y profiadau hyn yn heriol ac yn emosiynol ac wedi aros gyda nhw.
| “ | Roeddwn i'n glanhau ei hystafell ac rwy'n cofio; cymerodd ei mwgwd oddi arnaf. Dim ond fel 24, 25 oed oedd hi ... anghofiaf hi byth, ac mae hi'n dweud, 'Roeddwn i'n meddwl nad oedd Covid-19 yn beth go iawn', aeth hi, 'Ond yn onest, mae'n fy lladd i…' [Yn wylo] mae'n gwneud fi yn eithaf emosiynol, a dweud y gwir, roedd yn drist.”
- Glanhawr ysbyty |
4. Ysbytai: profiadau cleifion |
 |
Mae’r bennod hon yn dwyn ynghyd yr hyn a ddywedodd cleifion ysbyty wrthym am eu profiadau o gael mynediad at ofal ysbyty a’i ddefnyddio yn ystod y pandemig. Mae'n cynnwys straeon y rhai a dderbyniwyd gyda symptomau Covid-19 difrifol.
Problemau cael mynediad at ofal ysbyty
Problemau gyda chael mynediad i ofal ysbyty yn bryder mawr i gleifion a gweithwyr gofal iechyd proffesiynol. Caewyd wardiau, rhoddwyd blaenoriaeth i ofal, a chafodd apwyntiadau eu canslo, eu gohirio a'u symud ar-lein yn aml.
Cafodd y newidiadau i wasanaethau ysbytai effaith niweidiol a pharhaol ar lawer o gleifion. Fe wnaethant rannu enghreifftiau o fethu â chael mynediad at y gofal yr oedd ei angen arnynt, ar draws pob math o ofal nad yw’n gysylltiedig â Covid a gofal wedi’i gynllunio.
| “ | Caewyd popeth, roedden nhw’n orlawn â chleifion…fe wnaethon nhw roi’r gorau i bopeth, bu farw pobl oherwydd na chawsant eu hapwyntiadau, na chawsant eu triniaeth, a pheidio â mynd a chael eu gwirio am fwy o lympiau, fel fi.”
- Claf ysbyty |
Yn ogystal â phroblemau cyffredinol gyda mynediad, roedd rhai pobl yn wynebu rhwystrau penodol. Er enghraifft, roedd rhai cyfranwyr â cholled golwg yn ei chael hi'n anodd dod o hyd i ysbytai a oedd yn anghyfarwydd ac yn newid. Ni allai rhai ddod o hyd i glinigau wedi'u hadleoli, ac roeddent yn wynebu rhwystrau wrth ymdrin â thasgau arferol fel ciwio a mewngofnodi. cyflwynodd newidiadau mewn ysbytai heriau ychwanegol fel dilyn marcwyr ymbellhau cymdeithasol, adnabod a defnyddio gorsafoedd glanweithdra, a nodi gweithwyr gofal iechyd proffesiynol sydd wedi gwisgo mewn PPE.
| “ | Aethon ni i Moorfields [ysbyty llygaid] ar gyfer ein glawcoma, yn ystod y cyfnod hwnnw symudon nhw’r clinigau, felly’r her oedd dod o hyd i ble roedden nhw. Roedd y ciwio a mewngofnodi yn heriol.”
- Person â cholled golwg |
Gwnaethpwyd hyn yn anos gan nad oedd digon o staff ar gael i gynnig cymorth, a oedd yn gadael y cyfranwyr wedi'u brifo'n aruthrol ac yn rhwystredig gyda'r system.
Disgrifiodd cyfranwyr lawer o broblemau ac oedi gyda gofal a thriniaeth ar gyfer cyflyrau hirdymor ac anghenion iechyd nad ydynt yn rhai brys. Ymhlith yr enghreifftiau roedd hormonau nad ydynt yn cael eu monitro ar gyfer cyflwr hirdymor, tonsilitis heb ei drin, a chleifion mewn poen yn aros am lawdriniaethau ar y pen-glin - ymhlith llawer o rai eraill.
| “ | Mae cau wardiau ysbytai yn rhagofalus yn 2020 a 2021 wedi diraddio fy ansawdd bywyd a’m hiechyd meddwl yn sylweddol … nawr nid oes gennyf fawr ddim gobaith o wella’n llwyr mwyach, gan fod fy iechyd cyffredinol wedi dirywio oherwydd fy anallu i wneud ymarfer corff a’r pethau annioddefol. sgil-effeithiau’r feddyginiaeth ar bresgripsiwn i reoli fy mhoen tra byddaf yn dal i aros am y llawdriniaeth ohiriedig yr oeddwn yn mynd i’w chael yn ystod gwanwyn 2020.”
- Claf ysbyty |
Roedd llawer yn beio oedi a phroblemau gyda’u gofal ar gamau a gymerwyd i leihau lledaeniad Covid-19 mewn ysbytai. Roedd y rhain yn cynnwys canllawiau cadw pellter cymdeithasol a arweiniodd at lai o gapasiti mewn ysbytai, ynghyd ag effaith prinder staff. Dywedodd llawer wrthym pa mor ofidus oedd aros am gyfnodau hir, yn aml tra'n teimlo'n sâl, neu'n poeni am eu cyflwr yn gwaethygu. Rhannodd rhai sut yr oeddent yn meddwl bod yr oedi hwn yn dal i effeithio ar ysbytai ar ôl y pandemig.
| “ | Mae effaith Covid-19 ar yr ysbytai yn ofnadwy, ac yn amlwg, yn amlwg iawn, maen nhw'n ei chael hi'n anodd iawn, maen nhw wedi gor-redeg, maen nhw'n brin o staff. ”
– Gofalwr |
Roedd rhai cyfranwyr yn ansicr mai'r pandemig yn unig oedd yn gyfrifol am y problemau a welsant gyda'u gofal yn yr ysbyty. Roeddent yn meddwl bod problemau ehangach mewn systemau gofal iechyd a waethygodd y pandemig yn hytrach na'u hachosi. Disgrifiodd rhai eu gofal fel gwael cyn, yn ystod, ac ar ôl y pandemig.
| “ | Roedd y GIG ar ei liniau hyd yn oed cyn y pandemig, byddwn yn aros 12 wythnos am apwyntiad hyd yn oed bryd hynny. Yn ystod y pandemig roedd y cyfan yn apwyntiadau ffôn. Nawr mae'n dal yn ddieflig. Dim ond esgus yw cloi i lawr a’r pandemig. ”
- Claf ysbyty |
| “ | Roeddem yn teimlo'n siomedig gyda'r adran honno yn gyffredinol hyd yn oed cyn y pandemig ac roedd llawer o gwynion ... nid oedd unrhyw un yn hapus yno; roedd wedi'i lechi'n llwyr”
- Claf ysbyty |
Clywsom fod y problemau hyn yn gadael cleifion a’u hanwyliaid yn hynod bryderus am gyflyrau difrifol nad oedd yn cael eu trin. Roedd eraill yn pryderu am y risgiau anhysbys heb y diagnosis yr oedd ei angen arnynt.
| “ | Oherwydd prinder staff, roeddent yn dweud, wyddoch chi, 'Ni allwn weithredu tan ei fod yn fywyd neu'n farwolaeth,' a dweud y gwir.”
- Claf ysbyty |
| “ | Gan fod fy llawdriniaeth wedi'i gohirio am 8 wythnos, treuliais yr amser hwnnw yn yr ysbyty, yn methu â chael ymweliadau teuluol gan ein bod dan glo; a phinio i fy ward ysbyty gan nad oeddem yn cael cylchredeg o amgylch yr ysbyty oherwydd gweithdrefnau Covid-19. Teimlais lawer gwaith fod y Llywodraeth hon eisiau i mi farw yn hytrach na chadw llygad amdanaf.”
- Claf ysbyty |
Shanes ylvia a'i gwrWynebodd Sylvia a'i theulu nifer o heriau yn ystod y pandemig, gan gynnwys canslo apwyntiadau ysbyty ac oedi cyn cael triniaeth. Ar ôl cael pen-glin newydd 18 mis cyn y pandemig, canfu Sylvia fod ei holl apwyntiadau dilynol wedi'u canslo. Gadawodd hyn hi heb unrhyw ofal ôl-lawfeddygol. O ganlyniad, mae hi bellach yn profi poen yn ei phen-glin, sydd yn ei barn hi yn ganlyniad uniongyrchol i'r apwyntiadau hyn a gollwyd. Yn ogystal, roedd ei gŵr yn wynebu ei anghenion gofal iechyd ei hun. “Cafodd triniaeth fy ngŵr ar gyfer canser gwaelodol y croen ei ohirio o fwy na 18 mis oherwydd yr ôl-groniad ysbyty a achoswyd gan Covid-19.” Ychwanegodd yr ansicrwydd a'r pryder ynghylch ei ofal gohiriedig at straen llethol y pandemig. Roedd Sylvia yn bryderus iawn y byddai ei ganser yn gwaethygu yn ystod y cyfnod aros, a beth fyddai hyn yn ei olygu i'w siawns o wella. Fel nyrs ei hun, roedd Sylvia yn deall y pwysau aruthrol oedd ar systemau gofal iechyd. Fodd bynnag, yn sgil cael apwyntiadau wedi’u canslo ac oedi wrth drin triniaethau ar lefel bersonol, daeth realiti’r sefyllfa i’r amlwg. Roedd hi'n teimlo'n ddig ac wedi cael ei siomi gan y llywodraeth a'r system gofal iechyd, gan ddadlau na ddylai apwyntiadau byth fod wedi cael eu canslo yn y lle cyntaf. “Mae datganiadau gwleidyddol wedi achosi ac yn parhau i achosi llawer o drallod i fy nheulu.” |
Roedd y rhai a brofodd oedi eisiau gwybod a ellid bod wedi gwneud mwy i'w galluogi i gael mynediad at ofal ysbyty yn gyflymach. Roeddent yn teimlo bod eu problemau iechyd yn cael eu hanwybyddu i flaenoriaethu gofalu am y rhai â Covid-19.
| “ | Es i i'r ysbyty gyda sepsis, ac roeddwn i'n dal yn wan iawn. Roedd yr holl brofiad gyda hynny, rwy’n credu, oherwydd bod llawer o bobl sâl yn yr ysbyty eisoes â Covid-19. Felly, i mi, hebddo, nid oedd gwelyau ysbyty ar gael. I gael eich gadael allan mewn ambiwlans a chael eich rhoi ar wrthfiotigau mewn drip a phethau felly, nid oedd yn brofiad braf o gwbl.”
- Claf ysbyty |
Rhannodd llawer o gyfranwyr brofiadau o gweld pobl hŷn yn mynd yn fwyfwy sâl ac nad ydynt yn derbyn gofal amserol neu ddigonol. Roeddent yn credu bod modd osgoi'r oedi hwn mewn gofal a'i fod yn cyfrannu at farwolaethau y gellid eu hatal.
| “ | Er ei bod yn drist iawn bod cymaint o bobl wedi marw o Covid-19, mae’r un mor drist bod llawer o’r henoed wedi marw’n gynt nag y byddent wedi’i wneud oherwydd bod triniaeth yn cael ei thynnu’n ôl neu’n cael ei gohirio oherwydd Covid-19.”
- Claf ysbyty |
Roedd rhai cyfranwyr yn rhoi’r bai yn uniongyrchol ar arweinyddiaeth systemau gofal iechyd a’r llywodraeth am y dirywiad canfyddedig yn iechyd pobl yr oeddent yn eu hadnabod. Roeddent yn credu, trwy esgeuluso blaenoriaethu rhai materion iechyd, gadawyd unigolion i fynd yn sâl neu, mewn rhai achosion, i farw.
| “ | Pan ddigwyddodd Covid-19 ym mis Mawrth 2020, roedd fy ngŵr yn derbyn triniaeth ar gyfer canser y pancreas. Roedd newydd orffen 12 triniaeth folfirinox ac roedd i fod i ddechrau radiotherapi. Oherwydd mantra'r llywodraeth i achub y GIG, daeth gwasanaethau canser arferol i ben a chynhaliodd fy ngŵr radiotherapi ar ei ben ei hun…pam nad oedd ei ofal diwedd oes wedi'i ddiogelu a'i ymgorffori? Ni ddylai neb farw mewn poen o ganser. Roedd hyn oherwydd y cyfyngiadau a gyflwynwyd gan Covid-19 a brwdfrydedd y llywodraeth i achub y GIG.”
- Aelod o'r teulu mewn profedigaeth |
Pwysau ar staff ysbytai
Roedd llawer o gyfranwyr yn meddwl bod staff yn gwneud eu gorau ond yn amlwg dan bwysau. Roeddent yn aml yn myfyrio ar doll emosiynol y pandemig ar staff ysbytai. Gallent weld bod llawer yn cael trafferth gyda'r baich a'r straen a ddaeth yn sgil y pandemig.
| “ | Bob tro rwy’n ymweld â’r uned arennol nawr, neu’n siarad ag unrhyw un, maen nhw bob amser yn brin o staff…a llawer ohono yw sgil-effaith gorfod delio â Covid mewn gwirionedd, oherwydd mae llawer o’r nyrsys eu hunain wedi dioddef. â phroblemau iechyd meddwl oherwydd yr hyn yr oedd yn rhaid iddynt ei brofi.”
- Claf yn yr ysbyty gyda Covid-19 |
Er gwaethaf y pwysau, roedd llawer o gyfranwyr yn gadarnhaol ynghylch gweithwyr gofal iechyd proffesiynol unigol a dywedasant eu bod yn derbyn y gofal yr oedd ei angen arnynt. Roedd rhai’n rhannu sut roedd safon gyffredinol y gofal a gawsant yn parhau’n uchel hyd yn oed mewn amgylchiadau anodd. Disgrifiwyd staff yn aml fel bod yn sylwgar, yn ofalgar ac yn gynnes er gwaethaf yr holl bwysau oedd arnynt.
| “ | O staff yr Adran Damweiniau ac Achosion Brys i’r ward, i’r llawfeddyg, i staff y theatr, roedden nhw i gyd yn wych am yr hyn maen nhw’n ei wneud… er mai Covid oedd hi, roedden nhw’n mynd y tu hwnt i’r hyn roedden nhw i fod i’w wneud.”
- Claf ysbyty |
| “ | Ni allai’r staff ysbyty a ofalodd amdanaf fod wedi bod yn fwy caredig a thosturiol, er gwaethaf yr amgylchiadau anodd yr oeddent ynddynt.”
- Claf ysbyty |
Disgrifiodd eraill sut yr aeth staff ysbytai allan o'u ffordd i'w helpu yn ystod eu triniaeth, gan gynnwys gweithio goramser i sicrhau bod anghenion y cleifion yn cael eu diwallu pan oedd prinder staff.
| “ | Diolch byth daeth nyrs hyfryd o’i bractis i ymweld ag ef gyda’r nos ar y pumed diwrnod ac roedd wedi cynhyrfu cymaint gan ei driniaeth fel y bu’n gweithio goramser i wella pethau.”
– Gofalwr |
Cafodd rhai cyfranwyr lai o brofiadau cadarnhaol gyda staff ysbytai, a phriodolwyd hynny i'r pwysau yr oeddent yn gweithio oddi tano. Roeddent yn rhannu sut y gallai staff boeni a thynnu eu sylw ac nid oeddent bob amser yn cyfathrebu'n glir nac yn gwrtais.
| “ | Dydw i ddim yn gwybod bod lefel y gofal a gafodd yn cyrraedd y safon…roedden nhw'n eitha' anfoesgar tuag ati ac yn ddiystyriol o sut roedd hi'n teimlo a does gen i ddim ffordd i herio hynny, does gen i ddim ffordd i, caredig. o, cefnogwch hi ar hynny.”
- Aelod o deulu claf ysbyty |
| “ | Ar ryw adeg, daeth yr ymgynghorydd gwrywaidd. Wna i byth anghofio'r dyn yma. Dywedodd wrthyf, 'Rwy'n deall eich bod yn cael trafferth gyda'r CPAP.' Dywedais, 'Ie.' Dywedodd, 'Wel, os na allwch ymdopi â hynny, bydd yn rhaid i chi gael eich awyru ac yna mae'n 50/50 os byddwch chi'n byw neu'n marw [tôn galed],' yn llythrennol fel yna ac yna aeth.”
- Claf ysbyty |
Disgrifiodd straeon eraill a rannwyd gan y rhai a oedd yn derbyn gofal parhaus ar gyfer cyflyrau hirdymor newid yn y ffordd yr oedd staff yr oeddent yn eu hadnabod yn dod ar eu traws.
| “ | Roedd gen i gyflwr sy'n bodoli eisoes. Bob tro roeddwn i'n ymweld â'r ysbyty, roeddwn i'n gweld staff blinedig, digalon a llosg yn gweithio mewn system oedd wedi torri. Dim byd tebyg i sut roedden nhw'n arfer bod. Roedd tymer yn sicr wedi cael ei syfrdanu yn ystod y cyfnod hwnnw, ac rwy’n dal i boeni am yr effaith hirdymor a gafodd hyn oll ar eu hiechyd meddwl ac ansawdd y gofal y gallant ei ddarparu.”
- Claf ysbyty |
| “ | Mae effaith Covid-19 ar yr ysbytai yn ofnadwy, ac yn amlwg, yn amlwg iawn, maen nhw'n ei chael hi'n anodd iawn, maen nhw wedi gor-redeg, maen nhw'n brin o staff. ”
- Claf ysbyty |
Roedd nifer fach o straeon gan bobl â nam ar eu golwg a rannodd heriau eraill yr oeddent yn eu hwynebu, gan gynnwys enghreifftiau o elyniaeth gan weithwyr gofal iechyd pan fethasant yn anfwriadol â dilyn canllawiau.
Stori EmilyBu'n rhaid i Emily, dynes ddall 35 oed, ymweld â'r ysbyty i gael archwiliad arferol yn ystod y pandemig. Ar ôl cyrraedd yr ysbyty, daeth aelod o staff yn ei hwyneb ar unwaith a waeddodd arni am beidio â dilyn y system un ffordd a pheidio â defnyddio'r orsaf glanweithdra dwylo. Roedd hyn er bod ganddi ffon weladwy i helpu gyda llywio. Ceisiodd Emily egluro ei bod yn ddall ac na allai weld yr arwyddion. Fodd bynnag, roedd yr aelod o staff i'w weld yn anwybyddu ei hesboniad ac yn parhau i'w thorchi'n uchel o flaen cleifion ac ymwelwyr eraill. Teimlodd Emily don o embaras a rhwystredigaeth drosti wrth iddi geisio llywio cynllun anghyfarwydd yr ysbyty heb unrhyw gymorth. “Ro’n i’n teimlo’n fychanol. Roedd y staff yn fy nhrin fel pe bawn yn dwp neu’n bod yn anodd yn fwriadol, pan nad oeddwn yn gallu gweld yr arwyddion.” Roedd y profiad yn gadael Emily wedi'i brifo'n ddifrifol. “Roeddwn i’n teimlo fy mod yn cael fy nghosbi am rywbeth nad oedd gen i unrhyw reolaeth drosto.” |
Cleifion a gafodd driniaeth am Covid-19 mewn ysbytai
Disgrifiwyd llawer o'r straeon a rannwyd gyda ni gan gleifion Covid-19 yr ofn a deimlent ynghylch cael eu derbyn i’r ysbyty, gan gynnwys na fyddent yn gweld eu hanwyliaid eto.
| “ | Es i mewn i'r ysbyty mewn ambiwlans ar 19 Ionawr - 10 diwrnod ar ôl colli fy mam - ar ôl profi'n bositif a gofyn i'r parafeddygon a oeddwn i'n mynd i farw. Wnaeth cymaint o bobl ddim gadael yr ysbyty ar ôl ei gael.”
- Claf yn yr ysbyty gyda Covid-19 |
Rhannodd rhai cyfranwyr sut nad oeddent yn sylweddoli pa mor sâl oeddent, na bod eu symptomau'n gysylltiedig â Covid-19. Roedd yna hefyd enghreifftiau o gleifion yn mynd i’r ysbyty i gael triniaeth am gyflyrau eraill ond yn profi’n bositif am Covid-19 ac yn gorfod aros.
| “ | Y syndod mwyaf i mi oedd nad oeddwn yn meddwl fy mod yn mynd i gael fy nerbyn, felly es i'r adran damweiniau ac achosion brys yn yr hyn roeddwn i'n ei wisgo. Y peth a ddywedais wrth bawb pan ddes i'n ôl allan yw gwneud yn siŵr os ydych chi, eich bod chi'n meddwl efallai ei fod gennych chi neu beth bynnag, bod gennych chi fag gyda dŵr, charger ffôn, unrhyw beth. Doedd gen i ddim byd.”
- Claf yn yr ysbyty gyda Covid-19 |
I rai cleifion Covid-19, roedd hyn yn golygu trawsnewidiad sydyn a dryslyd o'u bywydau rheolaidd i fod yn gleifion ysbyty. Deffrodd rhai pobl mewn ysbyty heb unrhyw gof o sut y cyrhaeddon nhw yno. Dim ond yn ddiweddarach y sylweddolwyd bod eu hiechyd wedi gwaethygu'n gyflym a bu'n rhaid eu rhuthro i'r ysbyty.
Dywedodd rhai cleifion Covid-19 wrthym eu bod yn cael trafferth cofio eu hamser yn yr ysbyty oherwydd eu bod mor sâl. Roeddent yn disgrifio bod i mewn ac allan o ymwybyddiaeth neu, mewn rhai achosion, bod mewn coma am ddyddiau neu wythnosau. Roedd hyn yn eu gadael yn methu â siarad llawer am fanylion eu profiad, yn enwedig y triniaethau a gawsant, gan ei fod yn aml yn teimlo fel niwl.
| “ | Un diwrnod fe ddeffrais yn yr ICU yn methu symud, siarad, bwyta, yfed ac ati. Roeddwn yn gwbl ddibynnol ar staff i'm golchi, fy bwydo, ac ati. o dracheostomi yn fy ngwddf. Yn ôl pob tebyg, roeddwn i wedi bod mewn coma ysgogedig ers 2 fis.”
- Claf yn yr ysbyty gyda Covid-19 |
| “ | Cefais fy nerbyn i'r ysbyty. Wn i ddim pa mor hir cyn iddyn nhw fy rhoi i mewn – roeddwn i mewn gofal dwys. Roeddwn i ar beiriant anadlu. Felly, roeddwn i mewn coma anwythol am… gryn dipyn o'r amser roeddwn i yno. Ni allaf gofio os dywedasant ei fod tua phum wythnos.”
- Claf yn yr ysbyty gyda Covid-19 |
I eraill, eu cof parhaol oedd bod ar beiriant anadlu. Disgrifiodd y cyfranwyr hyn yr anghysur a'r ofn a brofwyd ganddynt oherwydd na allent anadlu ar eu pen eu hunain. Dywedon nhw eu bod yn teimlo'n ddryslyd, yn agored i niwed ac yn ofnus iawn.
| “ | Roedd y mwgwd ymlaen ers peth amser. Roedd rhai masgiau yn haws i'w goddef nag eraill. Roedd rhai yn arfer teimlo'n ofnadwy iawn. Roeddwn i'n ei gasáu, rhai ohonyn nhw. Oedd, felly roedd hynny'n anodd iawn, iawn oherwydd – ie, rhai ohonyn nhw – dydw i ddim yn gwybod. Roedd fel petai'n rhaid i chi anadlu ag ef, ac yna pan fyddech chi'n rhoi'r gorau i anadlu ag ef, byddwn i'n mynd i banig, a byddai popeth yn dechrau - byddai clychau'n dechrau canu, a [chwerthin] byddwn i'n hoffi, gallaf 'Ddim yn anadlu, alla i ddim anadlu."
- Claf yn yr ysbyty gyda Covid-19 |
Roedd llawer o gleifion yn yr ysbyty gyda Covid-19 mewn wardiau gorlawn, wedi'u gwahanu oddi wrth gleifion eraill gan lenni yn unig. Disgrifiwyd sŵn a goleuadau cyson yr ysbyty ganddynt, gyda staff yn edrych arnynt drwy gydol y nos. Roedd rhai yn ei chael hi'n anodd iawn cysgu.
| “ | Mae'n cynnwys rhai o'r elfennau o artaith, fel y goleuadau ymlaen yn gyson, lefel y sŵn…esgidiau gwichlyd, byddai'r staff yn siarad yn normal. Ar un adeg, roedden nhw'n malu blychau yn ystod canol y nos. Unwaith eto, rwy'n gwybod bod y rhan fwyaf o'r cleifion yn anymwybodol, ond fe effeithiodd yn bendant ar ansawdd fy nghwsg a phethau."
- Claf yn yr ysbyty gyda Covid-19 |
Cynigiwyd cyffuriau arbrofol i rai o’r rhai a oedd yn sâl iawn gyda Covid-19 neu i gymryd rhan mewn treialon clinigol, yn enwedig yng nghamau diweddarach y pandemig. Disgrifiodd y cyfranwyr hyn sut y siaradodd meddygon â nhw am eu hopsiynau, yn ogystal â chael eu caniatâd cyn i driniaethau ddechrau. Teimlai rhai yn freintiedig eu bod wedi cyfrannu at ddealltwriaeth o'r firws a chawsant gyfle i roi cynnig ar rywbeth a allai fod wedi helpu i achub eu bywyd.
| “ | Rwy’n meddwl eu bod wedi rhoi cyffur prawf i mi hefyd ac rwyf wedi’i ddarganfod ers hynny, a dyna un peth a helpodd fi.”
- Claf yn yr ysbyty gyda Covid-19 |
| “ | Oedd, roedd yn frawychus iawn i fod yn onest gyda chi oherwydd nad ydych yn gwybod beth sy'n digwydd nesaf. Rwy’n meddwl eu bod wedi rhoi cyffur prawf i mi hefyd ac rwyf wedi’i ddarganfod ers hynny, a dyna un peth a helpodd fi.”
- Claf yn yr ysbyty gyda Covid-19 |
Roedd cael eu trin wrth ymyl eraill a oedd yn sâl iawn weithiau'n golygu bod cleifion yn gwylio wrth i eraill farw o Covid-19. Dywedodd cyfranwyr wrthym pa mor deimladwy a brawychus oedd hyn, a sut roedd yn ein hatgoffa o ba mor farwol yw'r firws.
| “ | Rwyf wedi gweld rhywbeth nad oedd yn neis iawn. Roedd yn ddyn ifanc, ac roedd yn rhaid iddyn nhw roi cywasgiadau iddo, tra roedden nhw’n gwneud y cywasgiadau, dwi’n meddwl ei fod wedi fy sbarduno i mewn gwirionedd… dechreuais gael pwl o banig.”
- Claf yn yr ysbyty gyda Covid-19 |
Wrth iddynt wella, dywedodd cleifion Covid-19 wrthym eu bod am fynd allan o'r ysbyty cyn gynted â phosibl. Roedd rhai yn poeni eu bod yn cymryd gwely y gallai fod ei angen ar rywun mwy sâl. Disgrifiodd eraill gymaint yr oeddent yn gweld eisiau eu cartref a'u teulu, a pha mor anobeithiol oeddent i adael a pharhau â'u hadferiad.
| “ | Roeddwn i mor flinedig. Roedd yn fwy o flinder oherwydd y panig a'r hyn nad oedd wedi digwydd yn wreiddiol oherwydd ni allwn anadlu. Unwaith y bydd hynny wedi sefydlogi ac yn y blaen, roedd yn fwy o achos unwaith i mi ddechrau teimlo'n well, roeddwn i eisiau mynd adref oherwydd roeddwn i, fel, yn fath o, 'Pam ydw i'n cymryd gwely pan mae yna bobl sydd ei angen mewn gwirionedd?' Ond yn amlwg roedden nhw eisiau parhau i fy monitro.”
- Claf yn yr ysbyty gyda Covid-19 |
Dywedodd rhai o'r rhai a oedd yn yr ysbyty gyda Covid-19 wrthym eu bod yn dal i gael eu trawmateiddio gan eu profiad, hyd yn oed flynyddoedd yn ddiweddarach. Disgrifion nhw'r euogrwydd roedden nhw'n ei deimlo ar ôl goroesi tra nad oedd eraill a gafodd driniaeth yn gwneud hynny. Rhannodd eraill sut mae ganddynt ôl-fflachiau a phyliau o banig yn ail-fyw eu profiad.
| “ | Mae'n dal i effeithio arnaf yn ddyddiol. Rwy'n credu bod gennyf PTSD, ond nid yw hyn wedi'i ddiagnosio'n ffurfiol. Os bydd rhywun yn sôn am Covid-19 rwy’n feddyliol yn mynd yn syth yn ôl i’r ward a’r cleifion tlawd ar unwaith, y sŵn, yr arogl, y lleisiau, y teimladau.”
- Claf yn yr ysbyty gyda Covid-19 |
| “ | Ychydig wythnosau ar ôl i iechyd meddwl fy mab ddirywio, roedd yn cael gweledigaethau o fod yn ôl yn ei ward ysbyty ac roedd y dyn o'r gwely drws nesaf iddo yn yr ysbyty yn sefyll yn ei ystafell ac yn grac na wnaeth ei helpu ... mae crio yn Tesco oherwydd bod canu’r tiliau yn mynd ag ef yn ôl i’r monitors yn canu yn yr ysbyty.”
– Gofalwr ar gyfer claf yn yr ysbyty gyda Covid-19 |
Cyfathrebu mewn ysbytai yn ystod y pandemig
Roedd galwadau fideo a ffôn yn bwysig i alluogi cleifion i gyfathrebu ag anwyliaid. Roedd y galwadau hyn yn rhoi sicrwydd i deulu a ffrindiau, ac yn helpu cleifion i aros yn gysylltiedig â'r byd y tu allan.
| “ | Yr hyn a wnaed yn dda yn ystod y pandemig: Y defnydd o iPads i ddarparu cysylltiadau diriaethol i aelodau'r teulu yn Ward yr ICU yn ystod wythnosau cynnar y Cloeon 1af, cafodd hyn effaith enfawr ar les ein teulu mewn cyfnod heriol ac ni allaf ddiolch digon o staff. Fe wnaeth ein cadw mewn cysylltiad pan nad oeddwn yn meddwl ei fod yn bosibl.”
– Gofalwr ar gyfer claf yn yr ysbyty gyda Covid-19 |
Fodd bynnag, dywedodd cyfranwyr hynny wrthym roedd defnyddio technoleg yn heriol i rai cleifion. Er bod aelodau staff weithiau'n gallu cynorthwyo, nid oedd bob amser yn bosibl i gleifion drefnu galwadau na dod o hyd i staff gofal iechyd a oedd yn gallu helpu.
| “ | Roedd yn rhaid i fy nghefnder wthio i gael fy mam a fy chwaer i FaceTime. Wyddoch chi, nid oedd yn hawdd. Ond dyma ofal diwedd oes rydych chi'n ei roi. Gallaf ddeall, wyddoch chi, os oes gennych 100 o gleifion yno, nid oes gennych yr amser i FaceTime pawb, ond hyd yn oed os ydych yn ei gyfyngu i FaceTime 5 munud, ond nid oedd yn syml o gwbl. ”
– Gofalwr ar gyfer claf yn yr ysbyty gyda Covid-19 |
Rhai a rannodd eu stori gyda ni hefyd poeni am wneud penderfyniadau am eu hiechyd heb gyngor a chefnogaeth gan anwyliaid. Roedd staff ysbytai yn aml yn siarad â'u hanwyliaid os nad oedd cleifion yn gallu trafod eu gofal, ond nid oedd hyn bob amser yn digwydd.
| “ | Doedd [fy ngŵr] ddim yn cael dod, felly rydych chi'n colli'r gefnogaeth honno, yn enwedig pan nad ydych chi'n meddwl yn iawn oherwydd niwl yr ymennydd a phethau gwahanol eraill, [mae gennych chi] rhywun arall yn gwrando ar yr hyn y mae'r meddyg yn ei ddweud wrthych chi'ch dau. a deall os nad ydych yn iach.”
- Claf ysbyty |
Cael eich rhyddhau o'r ysbyty
Beth bynnag yw eu rheswm dros gael eu derbyn, dywedodd llawer o gleifion wrthym pa mor falch oeddent i oroesi eu harhosiad yn yr ysbyty. Roedd rhai cyfranwyr yn cyferbynnu hyn â’r ofn a deimlent pan gyrhaeddant yr ysbyty.
| “ | Yr unig gysylltiad â’r byd y tu allan am ran helaeth o’r diwrnod oedd clywed sgyrsiau roedd staff yn eu cael am sut oedd Covid-19 a’i effaith – profiad brawychus. Nod pawb ar y ward oedd mynd allan o'r ysbyty a chyrraedd adref. Roedd gan lawer bwysedd gwaed uchel oherwydd eu bod yn awyddus i gyrraedd adref.”
- Claf yn yr ysbyty gyda Covid-19 |
Dywedodd rhai cyfranwyr eu bod yn derbyn llai o ofal dilynol nag yr oeddent yn ei ddisgwyl ar ôl rhyddhau. Roeddent yn aml yn cysylltu hyn â materion capasiti a staffio yn yr ysbytai. Gadawodd hyn rai yn teimlo eu bod yn cael eu hesgeuluso, a'u bod wedi cael eu gadael i reoli eu hamodau ar eu pen eu hunain. Roedd hyn yn achos trallod a phryder sylweddol.
| “ | Cefais fy rhyddhau adref a'm gadael i ddelio â'm diagnosis heb unrhyw gymorth ychwanegol wedi'i drefnu. Ni chynghorwyd unrhyw apwyntiadau dilynol gydag anadlol neu gardioleg. Ar ôl cael fy rhyddhau, roeddwn yn parhau i fod yn sâl, ac ar ôl llawer o erlid a gwaethygu llwyddais o’r diwedd i gael mynediad at fy meddyg teulu – ac ar yr adeg honno dilynodd apwyntiadau pellach a chynhaliwyd profion.”
- Claf yn yr ysbyty gyda Covid-19 |
Roedd rhai cyfranwyr yn ddig ynghylch rhyddhau cleifion yn rhy fuan, yn enwedig pan oeddent yn meddwl bod pobl hŷn mewn perygl. Disgrifiodd cyfranwyr sut yr oeddent yn teimlo eu bod nhw neu anwyliaid yn cael eu hanfon adref o'r ysbyty i wneud lle i rywun arall.
Mae llawer o'r straeon yn disgrifio pobl hŷn a phobl agored i niwed yn cael eu rhyddhau i gartrefi gofal, ac roedd hwn yn cael ei ystyried yn fater arbennig o gynhennus. Dywedodd rhai cyfranwyr wrthym eu bod yn ddig iawn nad oedd y risgiau o ryddhau pobl i gartrefi gofal wedi’u hystyried yn briodol. Ystyriwyd bod hyn yn rhoi pobl agored i niwed mewn perygl ac yn cael eu beio gan gyfranwyr am farwolaethau yr oeddent yn eu hystyried yn rhai y gellid eu hosgoi.
| “ | Yn 2019 roedd fy mab, a oedd yn 32 oed ar y pryd, yn dioddef gwaedlif enfawr ar yr ymennydd oherwydd tiwmor a chafodd ei adael yn hynod anabl a bu’n rhaid iddo symud i gartref nyrsio. Yn ystod y pandemig roeddem yn ymwybodol bod ysbytai yn rhyddhau cleifion a oedd wedi’u heintio â Covid-19 yn ôl i gartrefi nyrsio ac roedd hwn yn gyfnod pryderus iawn i ni. Dylid ymchwilio’n drylwyr i ddiystyrwch ysbytai wrth ryddhau pobl heintiedig i gartrefi gofal ac roedd yn arfer hynod o wael a pheryglus.”
– Gofalwr |
Dysgu ar gyfer y dyfodol: cyfathrebu â chleifion, teuluoedd a gofalwyrPwysleisiodd llawer o gyfranwyr sut roedd angen dysgu gwersi am anwyliaid yn ymweld ag ysbytai neu’n mynychu apwyntiadau gyda chleifion, yn enwedig y rhai oedd angen cymorth ychwanegol. Roedd pryder dro ar ôl tro am anghysondeb ac annhegwch ar draws y profiadau a rannwyd gyda ni. Arweiniodd yr annhegwch hwn at ddrwgdeimlad a rhwystredigaeth. Clywsom lawer o enghreifftiau o’r effaith niweidiol ar gleifion a adawyd heb gymorth, weithiau wrth iddynt farw. Roedd cyfranwyr eisiau agwedd fwy cyson a thosturiol tuag at ymweliadau a bod gydag anwyliaid. “Dylai pawb fod wedi bod yn gwneud yr un peth, ac mae’n debyg eu bod nhw i fod, ond doedden nhw ddim. Doedden nhw ddim. Dylai pawb fod wedi bod yn gwneud yr un protocolau, a dylai’r un polisïau fod wedi’u gweithredu’n gyffredinol fel nad oedd camddealltwriaeth, a thrwy hynny roedd pawb yn gwybod y dylen nhw fod wedi bod yn gwneud yr un peth.” Gweithiwr gofal iechyd proffesiynol perthynol Dywedodd cyfranwyr eraill wrthym eu bod yn deall yr angen i gyfyngu ar ymwelwyr er mwyn lleihau lledaeniad Covid-19. Lle mae'n rhaid i'r mathau hyn o gyfyngiadau fod yn eu lle, roeddent yn dal i fod eisiau gwersi i'w dysgu am sut i flaenoriaethu cysylltiad dynol oherwydd pa mor bwysig yw hynny. Roedd sicrhau bod teuluoedd yn dal i allu siarad â’u hanwyliaid ac eiriol drostynt yn flaenoriaeth gyson. “Roedd y staff yn yr ysbyty yn anhygoel. Ond nid yw hynny'n gwneud iawn am ddiffyg eich anwyliaid ar adegau hollbwysig sy'n newid bywyd. Bydd effaith y cyfyngiadau yn para am genedlaethau. Y tro nesaf, mae angen i ni fod wedi paratoi'n well, ac mae angen i ni sicrhau, hyd yn oed pan fo cyfyngiadau ar waith, ein bod ni'n ddynol a'n bod ni'n caniatáu i eraill fod yn ddynol hefyd a chael cysylltiadau â'r rhai sydd eu hangen arnyn nhw fwyaf yn eu cyfnod anoddaf. ” Cyfrannwr Mae Pob Stori o Bwys Yn gysylltiedig â hyn, mae llawer o’r gwersi a ddysgwyd yn amlygu’r angen am well cyfathrebu o lawer rhwng gweithwyr proffesiynol a theuluoedd a oedd wedi’u gwahanu oddi wrth eu hanwyliaid. Clywsom lawer o enghreifftiau o gyfathrebu gwael a ychwanegodd at y trallod a deimlai teuluoedd. Roedd y ffordd yr oedd hyn yn cael ei reoli hefyd yn rhoi llawer o staff dan bwysau aruthrol. Dywedodd cyfranwyr yn aml fod hyn yn arbennig o bwysig i’r cleifion mwyaf agored i niwed neu’r cleifion sâl nad oeddent yn gallu defnyddio technoleg i gyfathrebu â’u hanwyliaid. “Pan fydd gwaharddiad ar ymweld yn ei le, rhaid sefydlu system lawer gwell o gyfathrebu gyda’r ysbyty. Roedd defnyddio rhif ffôn arferol y ward i geisio siarad â staff am eich perthynas yn rhwystredigaeth barhaus. Roedd yn ymgysylltu’n gyson oherwydd bod pob perthynas yn ei ddefnyddio ochr yn ochr â’r holl alwadau ffôn arferol a wneir i’r ward.” Cyfrannwr Mae Pob Stori o Bwys “Rwy’n meddwl mai un o’r pethau gwaethaf oedd ar y dechrau pan nad oedd teuluoedd yn gallu dod i mewn a dweud hwyl fawr. Sut y gellid bod wedi rheoli hynny’n well, nid wyf yn gwybod mewn gwirionedd oherwydd ei fod yn ddiogelwch iddyn nhw, roedd yn ddiogelwch i bawb mewn gwirionedd, ond roedd llawer iawn o boen yn gyffredinol yn hynny, nid yn unig staff, ond yn amlwg i’r teuluoedd eu hunain. Ond roedd yna boen i staff hefyd, oherwydd roedden nhw’n gwybod ei bod hi’n bwysig i bobl allu ffarwelio â’u hanwyliaid.” Caplan yr ysbyty |
5. Gofal brys a brys |
 |
Adrannau achosion brys (y cyfeirir atynt fel Adrannau Achosion Brys neu Ddamweiniau ac Achosion Brys yn y bennod hon) yw’r ffordd y mae pobl ag achosion mwy difrifol o Covid-19 yn cael eu hasesu a’u trin. Roedd cleifion â phroblemau gofal iechyd brys eraill hefyd yn parhau i fod angen cymorth trwy gydol y pandemig. Mae’r bennod hon yn rhannu straeon am ofal brys a gofal brys, gan gynnwys profiadau’r rhai sy’n gweithio mewn adrannau achosion brys ysbytai, parafeddygon a staff ambiwlans eraill. Mae hefyd yn amlygu profiadau'r rhai sy'n delio â galwadau brys drwy'r GIG 111 a 999. Mae'n gorffen drwy ddisgrifio profiadau cleifion o ofal brys.
Profiadau staff mewn adrannau achosion brys
Rhannodd cyfranwyr a oedd yn gweithio mewn adrannau achosion brys sut deimlad oedd trin cleifion ag anghenion gofal iechyd brys. Disgrifiodd rhai ofn cynyddol ynghylch yr hyn y byddai'n rhaid iddynt ddelio ag ef yn ystod y don gyntaf o heintiau. Roeddent yn gweld eu hunain fel y 'drws ffrynt' ar gyfer cael mynediad at ofal iechyd brys yn ystod argyfwng cenedlaethol.
| “ | Rhan o'r peth gyda meddygaeth frys yw nad ydych chi byth yn gwybod beth sy'n mynd i ddod i mewn trwy'r drysau ... felly, rydyn ni wedi arfer â'r anhysbys ac yn gorfod delio â beth bynnag sy'n digwydd, a blaenoriaethu pobl sydd mewn angen yn hytrach na phobl sy'n gallu aros.”
- Meddyg D&A |
Dywedodd y rhai a oedd yn gweithio mewn adrannau brys yn aml eu bod wedi arfer bod yn hyblyg ac addasu mewn sefyllfaoedd o argyfwng. Roedd gan staff a oedd wedi gwasanaethu am gyfnod hwy brofiadau o ddigwyddiadau yn y gorffennol ac epidemigau i'w defnyddio. Dywedodd rhai cyfranwyr fod yr hyn yr oeddent wedi'i weld a'i ddysgu o'r blaen wedi eu helpu i ddelio â'r pandemig.
| “ | Rydym wedi ein hyfforddi mewn rheoli clefydau heintus; rydym wedi ein hyfforddi ar sut i amddiffyn ein hunain rhag contractio pethau. Yn benodol [fy] hyfforddiant pwrpasol olaf oedd ar gyfer Ebola.”
- Meddyg D&A |
Er bod gweithio mewn argyfwng yn gyfarwydd, mae'r profiadau a rennir gan feddygon ED, nyrsys a pharafeddygon yn amlygu pa mor wahanol a llethol oedd y pandemig iddyn nhw. Mae'r heriau anghyfarwydd a'r llwyth gwaith trwm parhaus yn rhoi llawer o dan straen sylweddol. Roedd llawer o gyfranwyr yn rhannu pa mor ddwys a beichus oedd darparu gofal iechyd i’r rhai oedd angen cymorth brys.
| “ | Gweithiais fel nyrs GIG mewn adran damweiniau ac achosion brys ar gyfer Covid-19 i gyd. Roedd yn heriol iawn ac yn anodd iawn trwy gydol y profiad i gyd i weld cymaint o bobl mor sâl.”
– Nyrs Damweiniau ac Achosion Brys |
| “ | Roedd fy mhatrwm shifft yn fy swydd, sef yr Adran Damweiniau ac Achosion Brys, wedi newid…felly bob dydd byddwn yn mynd i mewn i weld marwolaeth a bob dydd byddwn yn meddwl tybed ai dyma’r diwrnod y byddaf yn mynd ag ef adref at fy mhlant bach.”
- Gweithiwr gofal iechyd proffesiynol |
Roedd gweithwyr gofal brys yn adlewyrchu bod cleifion yn marw yn rhywbeth yr oeddent wedi arfer ei brofi cyn y pandemig. Fodd bynnag, canfuwyd bod y cyferbyniad â gofal diwedd oes arferol yn boenus, yn enwedig pan na allai teuluoedd weld eu hanwyliaid.
| “ | Roeddwn i’n nyrs gofrestredig ar y rheng flaen yn gweithio yn yr Adran Damweiniau ac Achosion Brys yn ystod y pandemig…Y peth anoddaf oedd methu â chaniatáu i berthnasau fod gyda’u hanwyliaid tra roedden nhw’n marw.”
– Nyrs Damweiniau ac Achosion Brys |
Newidiadau i ofal brys a gofal brys yn ystod y pandemig
Cafodd pob ED brofiad gwahanol yn ystod y pandemig, gyda rhai cyfranwyr yn disgrifio cael eu gorlethu ar adegau ac eraill yn llawer tawelach nag arfer. Roedd profiadau staff Adrannau Achosion Brys yn dibynnu ar eu rôl a sut roedd eu hysbyty yn rheoli cleifion yr oedd angen cymorth brys arnynt, gan gynnwys y rheini â Covid-19 tebygol neu wedi’u cadarnhau. Dywedodd cyfranwyr fod y niferoedd a’r mathau o gleifion sydd angen gofal brys wedi newid wrth i’r pandemig fynd yn ei flaen, a bu’n rhaid iddyn nhw barhau i addasu. Roedd hyn yn golygu nad oedd un profiad unigol, a rennir ymhlith y rhai a oedd yn gweithio mewn gofal brys a gofal brys.
Disgrifiodd cyfranwyr bwysau enfawr ar lawer o adrannau brys yn ystod y pandemig. Dywedodd llawer eu bod yn hynod o brysur yn ystod cyfnodau brig mewn heintiau Covid-19. Dywedodd rhai staff nyrsio Adrannau Achosion Brys nad oeddent bob amser yn gallu darparu'r gofal yr oeddent ei eisiau i gleifion. Dywedasant wrthym pa mor ofidus ac emosiynol oedd hyn, gan ychwanegu at ofynion corfforol eu rôl. Roedd hyn yn arbennig o anodd yn gynnar yn y pandemig ac yn ystod cyfnodau brig o heintiau Covid-19.
| “ | Roedd yn drist iawn y gallai'r cleifion hyn fod wedi cael ... mwy yn cael ei roi iddyn nhw mewn lleoliad arferol i geisio eu helpu i wella. Gyda nifer y cleifion yn dod ein ffordd, ni allem ddarparu, ac ni allem ddarparu'r gofal llawn i bawb. Felly, roedd yn anodd iawn.”
– Nyrs Damweiniau ac Achosion Brys |
Stori cyfrannwr Mae Pob Stori o BwysBu cyfrannwr Mae Pob Stori’n Bwysig yn gweithio fel nyrs mewn ward derbyniadau brys Covid-19 yn ystod y pandemig. Er bod ganddi 35 mlynedd o brofiad, dioddefodd o straen wedi trawma oherwydd ei phrofiadau yn gofalu am gleifion yn ystod y pandemig. Yn anffodus bu farw llawer o bobl yn y ward lle'r oedd hi'n gweithio. Rhannodd sut roedd yn rhaid iddi ddelio â pherthnasau a oedd yn ysu am weld eu hanwyliaid a oedd yn marw ond na chaniatawyd iddynt wneud hynny. Ceisiodd Jane helpu pobl orau y gallai, ond roedd yn anodd dros ben. Defnyddiodd ei ffôn personol i ganiatáu i bobl ffarwelio cyn i'r ysbyty ddarparu iPads. “[Roeddwn i] yn bagio corff dwbl cleifion marw ac yn torri cloeon gwallt oddi arnyn nhw ar gyfer eu perthnasau.” Roedd heriau hefyd o ran trosglwyddo cleifion sâl iawn yr oedd angen iddynt fod mewn gofal dwys. Roedd hyn yn golygu bod yn rhaid iddi hi a'i thîm wneud penderfyniadau ynghylch pwy ddylai gael gwely ITU er mwyn iddynt allu cael mwy o driniaeth, a phwy oedd yn aros ar eu ward. “Roedden ni’n cael ein gorfodi i chwarae rhan Duw wrth benderfynu pwy oedd yn mynd i ITU – pwy oedd yn cael cyfle i fyw a phwy oedd ddim.” Rhannodd hefyd pa mor anodd oedd y pwysau ar ei chydweithwyr. Roedd hyn yn gwneud ei phrofiad ei hun yn anoddach fyth. “Staff nyrsio yn crio wrth gyrraedd shifft oherwydd eu bod mor ofnus o fod yno… gweld meddygon iau yn crio ac yn edrych yn ofnus a dim ond heb wybod beth i'w wneud.” Roedd y cyfrannwr yn sâl gyda Covid-19 ac yn y diwedd roedd yn glaf yn y ward lle roedd hi’n gweithio. Yna datblygodd symptomau Long Covid difrifol gan gynnwys methiant yr afu a'r pancreas ac nid yw wedi gallu gwella'n llwyr o hyd. |
I rai a oedd yn gweithio mewn Adrannau Achosion Brys, roedd y tonnau cychwynnol a hwyrach o achosion Covid-19 yn hylaw. Roeddent yn aml yn cyfeirio at brofiadau gwaeth mewn ysbytai eraill, neu ymhlith cydweithwyr sy'n gweithio mewn gofal dwys.
| “ | Roedd [EDs] o bryd i’w gilydd yn delio â chleifion Covid-19 sâl iawn, ond mewn gwirionedd roedd y prosesau a roddwyd ar waith ar gyfer y cleifion hynny yn aml yn golygu eu bod yn cael eu symud i ofal dwys yn eithaf cyflym.”
- Meddyg D&A |
| “ | Ein cydweithwyr gofal dwys…ddioddefodd y mwyaf o'r hyn a ddigwyddodd nesaf gyda'r cleifion pe baent mor sâl â hynny. Ond i ni wrth y drws ffrynt, gan dderbyn cleifion o’r gymuned drwodd i ofal eilaidd, rwy’n meddwl y gallem ddefnyddio’r arbenigedd sydd gennym ers yr holl flynyddoedd hyn a’i gymhwyso.”
- Meddyg D&A |
Disgrifiodd cyfranwyr sut roedd EDs yn paratoi i ddechrau ar gyfer trin ton fawr o gleifion Covid-19. Yn ystod wythnosau cynnar y pandemig, roedd y ffocws ar gyfer Adrannau Achosion Brys ar baratoi ar gyfer y don ddisgwyliedig o achosion Covid-19. Clywsom faint o ysbytai a symudodd yn gyflym i ynysu cleifion posibl Covid-19, naill ai mewn ardaloedd ar wahân yn eu hadran neu mewn adeiladau ar wahân.
| “ | Rydyn ni'n ysbyty mawr felly mae gennym ni ddau safle ar draws y ddinas. Roedd y tîm anadlol yn gofalu am Covid yn bennaf, felly ni welsom lawer o gleifion a ddaeth i mewn gyda Covid-19 yn unig - roeddent yn tueddu i fynd at y tîm anadlol yn uniongyrchol.”
- Meddyg D&A |
Rhannodd cyfranwyr brofiadau o batrymau sifft newydd, newidiadau ffisegol i gynllun adeiladau, a llwybrau newydd ar gyfer trin cleifion.
| “ | Gwnaethpwyd newidiadau i’r hyn roedden nhw’n ei wneud, sut roedden nhw’n gweithio, pawb yn dysgu sut i wisgo ac atal PPE, ynysu rhai cleifion, rhannu’r staff rhwng parthau.”
- Meddyg D&A |
Dywedodd rhai meddygon ED wrthym mai’r dybiaeth gynllunio oedd y byddai ICUs yn cyrraedd eu capasiti ac yn methu â mynd â chleifion a fyddai fel arfer yn cael eu trosglwyddo allan o Adrannau Achosion Brys i ITUs. Roedd hwn yn gyfnod pryderus ac anodd i staff yr Adran Achosion Brys a rannodd eu profiadau gyda ni.
| “ | Roeddem yn meddwl y byddai'n rhaid i ni fod yn mewndiwbio cleifion. Eu rhoi i gysgu yn ein hadran ein hunain ac yna eu trosglwyddo i ICU neu o bosibl cael nifer o gleifion awyru yn ein hadran ar adegau.”
- Meddyg D&A |
Fodd bynnag, nid oedd llawer o gyfranwyr yn cofio cynllun clir ar ddechrau'r pandemig ar gyfer sut y dylid newid eu gwasanaethau i ddelio â Covid-19. Ychydig iawn a wyddys am y clefyd, sut i'w drin, a faint o bobl y byddai'n rhaid i ysbytai unigol ofalu amdanynt. Yn lle hynny, roedden nhw’n aml yn rhannu sut roedd yn rhaid iddyn nhw ddysgu addasu wrth i’r sefyllfa newid. Dywedodd rhai cyfranwyr wrthym fod y math hwn o ymateb parhaus i argyfwng yn fwy cyfarwydd oherwydd bod staff adrannau brys wedi’u hyfforddi ac wedi arfer delio ag argyfyngau.
| “ | Ni fyddai’r cynllun yn debyg i gynllun swyddogol, byddai’n fwy, ‘gwnewch eich amser brysbennu yn gyflymach i gael pobl i mewn ac yn ddiogel,’ neu cyn gynted ag y byddwn yn cyrraedd, byddai’n gwneud yr holl drosglwyddiadau i’r ward, peidiwch â 'peidiwch â gwneud unrhyw beth arall, yna byddwn yn ailasesu. Ac roedd yn fwy o - yn dibynnu ar bwy oedd wrth y llyw - ymgyrch filwrol bron."
– Nyrs Damweiniau ac Achosion Brys |
| “ | Nid yw cynllunio rheolaeth barhaus yn rhan o strwythur yr adran achosion brys mewn gwirionedd. Rydyn ni'n mynd o argyfwng i argyfwng. ”
- Meddyg D&A |
Myfyriodd un cyfrannwr fod Covid-19 yn glefyd anhysbys, a pha mor anodd a wnaeth hynny i gamau cynnar y pandemig. Fe wnaethant rannu sut mae staff mewn meddygaeth frys yn gyffredinolwyr, ac yn aml yn dibynnu ar eraill ar shifft neu mewn timau ehangach i wybod sut i wneud diagnosis a thrin achosion anarferol. O ran delio â Covid-19, nid oedd unrhyw un yn gwybod beth oedd orau, gydag un cyfrannwr yn disgrifio timau ED fel rhai “anobeithiol am wybodaeth” i ddechrau.
Dywedodd llawer o gyfranwyr fod Adrannau Achosion Brys yn ei chael yn anoddach gweithredu mesurau rheoli heintiau a bod hyn yn cael ei waethygu gan adeiladau anaddas a diffyg lle. Roedd rhai a oedd yn gweithio mewn adrannau brys yn cyferbynnu eu problemau gyda rheoli heintiau â'r mesurau llymach, mwy amddiffynnol sydd ar waith mewn rhannau eraill o'r ysbyty. Dywedasant fod y dull hwn o reoli heintiau wedi achosi drwgdeimlad a rhwystredigaeth ymhlith staff.
| “ | Yn yr adran achosion brys, cawsom ein gadael yn fawr iawn a dywedwyd wrthym, 'Nid yw pellter cymdeithasol yn berthnasol yn yr adran achosion brys'. Mae'n dderbyniol i ni fod ar ben ein gilydd. Pan oedd hi’n ymddangos bod y wardiau’n derbyn gofal mawr, roedden ni fel petaen ni’n cael ein gadael ar fin y ffordd.”
– Nyrs Damweiniau ac Achosion Brys |
Roedd meddygon a nyrsys ED yn aml yn disgrifio sut roedd staff sy'n gweithio mewn wardiau mewn mannau eraill yn yr ysbyty wedi cael profiad gwahanol a mwy diogel o'r pandemig. Roedd rhai staff Adrannau Achosion Brys yn meddwl eu bod wedi cael eu hanghofio neu eu hanwybyddu er eu bod ar flaen y gad o ran ymateb gofal iechyd.
| “ | O siarad â chydweithwyr mewn [adrannau Damweiniau ac Achosion Brys] eraill ledled y wlad, roedd y cyfan yn debyg iawn, iawn. Doedd yr hyn oedd yn dda iddyn nhw ddim yn dda i ni.”
- Meddyg D&A |
Rhannodd cyfranwyr a oedd yn gweithio mewn rhai adrannau brys sut y gwelsant lai o gleifion yn ystod y cyfnod cloi cyntaf, o gymharu ag yn ddiweddarach yn y pandemig. Roeddent yn credu bod hyn oherwydd bod pobl ar y dechrau yn rhy ofnus i geisio triniaeth.
| “ | [Fel arfer] gallem gael hyd at 400 o gleifion drwodd y dydd, a chredaf ein bod yn ffodus pe baem yn taro 100 i 150.”
– Nyrs Damweiniau ac Achosion Brys |
Roedd llawer o gyfranwyr yn meddwl bod yr hinsawdd hon o ofn yn golygu bod pobl sy'n cyrraedd Adrannau Achosion Brys yn gynnar yn y pandemig yn fwy sâl nag y byddent fel arfer. Disgrifiodd staff yr Adran Achosion Brys sut yr oedd rhai pobl yn osgoi neu wedi methu â chael mynediad at ofal gan eu meddyg teulu. Yna, yn y diwedd, fe wnaethant alw ambiwlans neu gyrraedd yr adran damweiniau ac achosion brys yn anfoddog, oherwydd bod eu cyflwr wedi gwaethygu, neu eu bod yn teimlo nad oedd ganddynt unrhyw ddewis arall.
Roedd llai o alw yn caniatáu i gyfranwyr a oedd yn gweithio mewn rhai adrannau brys ganolbwyntio ar ofal cleifion, a oedd yn teimlo'n anarferol. Yn ogystal â gallu cynnig gwell gofal, roedd llai o bwysau llwyth gwaith yn caniatáu i rai cyfranwyr feithrin perthnasoedd fel tîm a gwella morâl. Roeddent yn gweld hyn yn bwysig o ystyried y pwysau ehangach yr oeddent yn eu hwynebu a'r ofn yr oeddent yn ei deimlo.
| “ | Caniataodd i ni fel tîm yn yr [adran] ddod i adnabod ein gilydd yn wirioneddol dda ac i adeiladu'r gwaith tîm a'r cyfeillgarwch proffesiynol hwnnw, a oedd yn wych. Yn sicr, cafodd unrhyw un a ddaeth i’r [adran] wasanaeth da iawn, iawn.”
- Meddyg D&A |
Stori MarthaGweithiodd Martha fel uwch feddyg yn ED yr ysbyty trwy gydol y pandemig. Er bod yn rhaid iddynt addasu eu gwasanaethau, mae hi'n edrych yn ôl ar y pandemig fel cyfnod pan oedd ei gwaith yn canolbwyntio mwy. Mynychodd llai o gleifion ei hadran, yn rhannol oherwydd bod y rhai â Covid-19 yn cael eu trin gan dimau eraill yn yr ysbyty. “Doedd gennym ni ddim llawer o gleifion Covid yn dod drwodd mewn gwirionedd oherwydd fe wnaethon nhw newid y llif trwy'r ysbyty. Felly, byddent yn mynd yn syth naill ai i ofal dwys neu i faes arall. Felly, roedd y niferoedd yn yr adran achosion brys yn isel iawn.” Rhannodd Martha sut, cyn y pandemig, roedd adrannau achosion brys yn aml yn delio â llawer o bobl nad oeddent yn ddigon sâl i fod yno ac y dylent gael eu gweld gan eu meddyg teulu yn lle hynny. Arhosodd y bobl hyn draw pan oedd y cyfyngiadau Covid-19 llymaf ar waith. Roedd hyn yn golygu ei bod hi a'i chydweithwyr ond yn delio â chleifion oedd wir angen eu cymorth. “Gwelsom lawer llai o gleifion, dylai pobl a oedd yno fod wedi bod yno ac roedd yn llawer llai o straen…roeddem yn delio â phobl â rhywbeth o'i le arnynt, nid dim ond ceisio osgoi cael apwyntiad gyda'u meddyg teulu. Felly, aeth ein llwyth gwaith i lawr yn anhygoel yn ystod y pandemig. ” Dywedodd hefyd fod gwell cydweithrediad rhwng Adrannau Achosion Brys a rhannau eraill o'r gwasanaeth iechyd, gan gynnwys arbenigeddau fel iechyd meddwl a gwasanaethau mamolaeth. Cawsant hefyd help ychwanegol gan feddygon iau a gafodd eu hailbennu o rannau o'r ysbyty nad oedd yn gweld cleifion. “Rwy'n golygu, mae'r cyfan wedi'i drawsnewid nawr ... ond yn ystod y pandemig fe allen ni wneud y gwaith yr oeddem i fod i'w wneud.” |
Er gwaethaf y manteision i gleifion unigol, disgrifiodd rhai cyfranwyr a oedd yn gweithio mewn adrannau achosion brys pa mor bryderus oeddent am y cleifion 'coll' a ddylai fod wedi bod yn ceisio cymorth. Roeddent yn poeni am yr hyn oedd yn digwydd i bobl a ddylai fod wedi bod yn derbyn triniaeth frys ond nad oedd. Clywsom sut y daeth Adrannau Achosion Brys eraill yn brysurach wrth i gyfyngiadau leddfu ac roedd angen triniaeth ar fwy o gleifion ar gyfer Covid-19 a phroblemau iechyd brys eraill.
| “ | Roedd ofn ar bobl, roedden nhw'n ufuddhau i'r hyn roedd y llywodraeth yn ei ddweud, ond roedd hynny er anfantais iddynt. Mae fel dweud bod EDs yn brysur, cadwch draw. Mae hynny'n iawn ac yn dda i'r bobl sy'n gwastraffu amser, nid yw ar gyfer y bobl sy'n sâl. ”
- Meddyg D&A |
Disgrifiodd rhai cyfranwyr pa mor gynnar yn y pandemig y bu mwy o gydweithredu rhwng Adrannau Achosion Brys a rhannau eraill o’r system gofal iechyd nag oedd cyn y pandemig, gan gynnwys o ran atgyfeiriadau cleifion. Yn ddiweddarach yn y pandemig, dywedodd cyfranwyr yn aml fod y pwysau ar Adrannau Achosion Brys wedi cynyddu oherwydd bod adrannau ysbytai eraill hefyd dan straen ac felly'n llai abl i gynnig cymorth.
| “ | Mae'r hyn y byddwn i'n ei ystyried yn rhyfela tywyrch rhyngom ni a gwahanol arbenigeddau newydd ailddechrau ... roedd gennym obaith y byddai'n ailosodiad mawr, ac mae wedi mynd yn ôl i'r hen ffyrdd i raddau helaeth - sy'n siom chwerw.”
- Meddyg D&A |
Yn yr un modd â rhannau eraill o'r system gofal iechyd, dywedodd cyfranwyr sy'n gweithio mewn adrannau achosion brys fod problemau gyda lefelau staffio wrth i brofi ac ynysu ddod yn fwy cyffredin. Roeddent yn rhannu sut yr oedd hyn yn arbennig o galed mewn adrannau brys o ystyried y galw cynyddol am ofal brys a gofal brys ar yr un pryd.
| “ | Roedd yna lawer o salwch ymhlith staff felly gyda’r staffio’n fyr yn amlwg, rydych chi’n rhyw fath o jyglo llwyth gwaith hynod o uchel ac yn bendant mae yna degwch uchel o gleifion na allwch chi eu rheoli.”
– Nyrs Damweiniau ac Achosion Brys |
Rhannodd llawer o gyfranwyr Adrannau Achosion Brys yr heriau o orfod gwneud penderfyniadau ynghylch blaenoriaethu gofal a throsglwyddo cleifion i UThD. Mewn rhai ysbytai roedd ITUs yn llawn neu bron yn llawn, a rhannodd cyfranwyr sut roedd hyn yn cael effaith ganlyniadol ar Adrannau Achosion Brys. Lle roedd cyfranwyr yn trin nifer fawr o gleifion Covid-19, roedd rhai yn rhannu pa mor anodd oedd hi i ddelio â diffyg capasiti ITU. Roedd yn rhaid iddynt wneud penderfyniadau ynghylch pwy i'w blaenoriaethu yn yr Adran Achosion Brys, a phwy fyddai'n cael eu trosglwyddo i UThD.
Stori DamiRoedd Dami yn nyrs staff mewn adran achosion brys yn ystod y pandemig. Disgrifiodd gamau cynnar y pandemig fel anhrefnus, gyda rheolau a phrosesau'n newid yn gyson. Teimlai Dami rywfaint o falchder ei fod ef a’i dîm wedi gwneud yr hyn a allent, er gwaethaf yr heriau enfawr a’r effaith sylweddol ar eu hiechyd meddwl eu hunain. “Roedd bob amser waith i’w wneud. Felly, dim ond clecian oedd y meddylfryd, fel bwrw ymlaen ag ef. Byddech chi'n hoffi cyfarfod yn y bore i ddweud beth sydd wedi newid a byddech chi'n mynd yn ôl ymlaen, ewch ymlaen ag ef. Ac unrhyw un sy'n cynhyrfu, rydych chi'n dod ymlaen yn llythrennol." Yn ystod cyfnodau brig o achosion, roedd Dami a'i gydweithwyr yn wynebu penderfyniadau anodd iawn am y gofal a gynigir i gleifion Covid-19. Dywedodd ei fod yn meddwl ei fod wedi rhwystro rhai o'r enghreifftiau gwaethaf oherwydd ei fod yn rhy drawmatig i feddwl amdano. “Fyddwn i ddim o reidrwydd yn falch o…y penderfyniadau oedd yn rhaid eu gwneud ar y pryd oherwydd diffyg offer neu staff.” Un o'r sefyllfaoedd mwyaf heriol oedd pan oedd pobl sâl eisoes wedi cael eu hawyru a bod angen eu trosglwyddo o'r ED i'r ITU. Roedd hyn yn cynnwys trafodaethau anodd rhwng staff ynghylch pwy i'w trosglwyddo yng nghyd-destun adnoddau cyfyngedig iawn. Teimlai Dami fod y ffocws yn aml ar yr offer oedd ar gael yn hytrach na’r hyn oedd yn iawn i’r unigolyn hwnnw, a bod presenoldeb DNR yn effeithio ar y penderfyniadau hyn. “…mae'r person hwnnw ar y pryd wedi'i awyru, nid oes ganddo lais. Ac awyru ar y pryd oedd yr unig driniaeth. ” |
Roedd ambiwlansys yn aml yn cael eu gadael yn ciwio y tu allan i ysbytai am gyfnodau hir iawn oherwydd bod adrannau brys yn derbyn llai o gleifion i osgoi gorlenwi ac i gynnal pellter cymdeithasol. Roedd hyn yn golygu bod yn rhaid i barafeddygon ofalu am gleifion mewn ambiwlansys a rhybuddio staff ysbytai am newidiadau yng nghyflwr pobl. Dywedodd llawer o gyfranwyr fod hyn wedi arwain at oedi mewn triniaeth, a phenderfyniadau anodd pan aeth cleifion a oedd yn aros yn fwy sâl.
| “ | Os oedd llawer o ambiwlansys a rhywun yn mynd yn ddifrifol [sāl] ac angen dod i mewn i'r adran...roedd angen i mi symud y claf oedd yn marw i goridor. Mae hwnnw'n benderfyniad ofnadwy iawn ac ni fyddai hynny'n cael ei ganiatáu heddiw, ond yn gorfforol, pan nad oes gennych le, beth allwch chi ei wneud?"
– Nyrs Damweiniau ac Achosion Brys |
Dywedodd cyfranwyr wrthym fod dulliau o drin Covid-19 mewn adrannau brys wedi newid wrth i’r pandemig fynd rhagddo, wrth iddynt rannu eu profiadau a’r effaith ar gleifion. Er enghraifft, yn hytrach na mewndiwbio cleifion yn yr ED neu eu trosglwyddo i ITU, roedd cleifion yn aml yn cael cymorth anadlol anfewnwthiol gan ddefnyddio CPAP, peiriant cymorth anadlu anadlu sy'n defnyddio pwysau aer ysgafn i gadw llwybrau anadlu anadlu ar agor tra bod y claf yn cysgu. Roedd y newid hwn yn cael ei ystyried yn gadarnhaol gan y rhai a soniodd amdano, ac yn rhywbeth a oedd yn caniatáu iddynt gynnig triniaeth fwy effeithiol ar gyfer Covid-19 mewn Adrannau Achosion Brys.
| “ | O'r cychwyn cyntaf, penderfynwyd bod y claf hwn yn cael mewndiwbio, gan fynd i ofal dwys. Dros y misoedd, fe sylweddolon nhw, na, mae'r cleifion hyn yn mynd i oroesi a chael gwell cyfle i gael eu rhoi ar y peth hwn o'r enw CPAP. Felly, fe wnaeth wella canlyniadau. Mae’n drueni meddwl bod y bobl ar y dechrau wedi cael y [gofal] anghywir – doeddech chi ddim yn gwybod.”
– Nyrs Damweiniau ac Achosion Brys |
| “ | Rwy'n meddwl bod rhai materion yn ymwneud â phryder ynghylch CPAP a thriniaethau i ddechrau, ond roeddent yn ymwneud yn bennaf â thriniaeth anadlol i gleifion. Ni welsom erioed gleifion difrifol wael ar wahân i'r rhai a oedd ar ddiwedd eu hoes.”
- Meddyg D&A |
Profiadau parafeddygon
Rhannodd parafeddygon y pwysau oedd arnynt, a sut y newidiodd eu rolau. Gan weithio fel rhan o wasanaeth rheng flaen hollbwysig, tynnodd llawer sylw at ba mor heriol oedd mynychu achosion brys a thrin cleifion ag anghenion iechyd brys.
I rai parafeddygon, roedd rhannau o'u rôl a oedd yn teimlo'n gyfarwydd. Roedd hyn yn cynnwys trin pobl â symptomau Covid-19 posibl mewn ffordd debyg i'r ffordd yr oeddent yn trin cleifion â salwch anadlol cyn y pandemig.
| “ | Rydyn ni'n mynd i gyflyrau sy'n debyg i Covid drwy'r amser, ac nid oedd y ffordd y cafodd ei drin yn ddim gwahanol i unrhyw salwch anadlol arall mewn gwirionedd. Ni allaf feddwl am unrhyw brotocolau penodol neu unrhyw beth felly.”
- Parafeddyg |
Ac eto, disgrifiodd parafeddygon y straen enfawr a wynebwyd ganddynt ar wahanol gamau o'r pandemig. I lawer, newidiodd eu patrymau gwaith. Roeddent yn aml yn disgrifio symud i sifftiau gwahanol a hirach, a dywedasant fod gweithio oriau estynedig am fisoedd i ben yn straen. Dywedodd rhai eu bod wedi'u paru â chydweithwyr nad oeddent wedi gweithio gyda nhw o'r blaen oherwydd sut roedd patrymau gwaith yn newid. Daeth hyn ag ansicrwydd pellach a newid mewn amgylchiadau a oedd eisoes yn heriol.
| “ | [Arweiniais] dîm o 57 i gyd yn darparu'r safon uchaf o ymateb a gofal i'r rhai yr effeithiwyd arnynt. I ddechrau, roedden ni...yn cael ein hamddiffyn yn wael, heb gyngor, ac yn gweithio oriau annynol. Ond fe wnaethon ni hynny heb amheuaeth…roedden ni i gyd wedi blino’n lân, yn wanychol ac yn ofnus yn fewnol.”
- Parafeddyg |
Dywedodd rhai parafeddygon wrthym fod y gofyniad i ddefnyddio PPE yn heriol o ystyried yr angen i weithredu’n gyflym mewn argyfyngau. I gyfranwyr eraill, fodd bynnag, roedd cydnabyddiaeth o bwysigrwydd PPE ar gyfer problemau anadlol, gan gynnwys lle na chadarnhawyd Covid-19.
| “ | Byddem yn cael pobl yn dod allan yn sgrechian arnom i frysio, ond yna byddai'n rhaid i ni wisgo ein PPE yn gyntaf cyn i ni allu mynd i mewn ... efallai mai rhywun yn y tŷ yr oeddent yn gwneud CPR arno, ond ni fyddech ddim yn gwybod a oedd ganddyn nhw Covid-19 ai peidio ar unwaith.”
- Parafeddyg |
| “ | Cafodd pawb eu trin fel rhai positif Covid-19 waeth beth oedd eu canlyniadau. Wyddoch chi, efallai eich bod wedi bod i mewn i'w cartref ac mae rhywun wedi dweud, 'O, rydw i wedi gwneud llif ochrol yno ac roedd yn negyddol,' ond gydag unrhyw un ag unrhyw gyflwr anadlol, nid oeddem yn cymryd y siawns. ”
- Parafeddyg |
Dywedodd rhai parafeddygon wrthym fe brofon nhw uchafbwyntiau ac isafbwyntiau o ran pa mor brysur oedden nhw yn ystod y pandemig, gyda chyfnodau dwys a adawodd lawer yn teimlo wedi blino'n lân, ond hefyd adegau pan oedd llai o alwadau i fynychu, yn enwedig yn ystod cloi cenedlaethol.
| “ | Cawsom y cyfnodau hynod ddwys hyn o weithio ac yna’r taweliadau mawr hyn lle’r oeddem yn eistedd o gwmpas…mae pawb yn clapio â photiau a sosbenni ac rydym yn meddwl, ‘Mae’n debyg mai dyma’r cyfnod hawsaf i mi ei gael erioed yn yr ambiwlans. gwasanaeth.'”
- Parafeddyg |
Clywsom gan lawer o barafeddygon am sut roedd pwysau mewn ysbytai, yn enwedig o ran derbyniadau, yn golygu eu bod yn cael eu gorfodi i ofalu am gleifion mewn ambiwlansys. Rhannodd y cyfranwyr hyn straeon am sut y gwnaethant hyn yn aml am oriau lawer a heb egwyl. Yn ogystal â bod yn anodd i gleifion, roedd yn heriol i barafeddygon ofalu am bobl sâl iawn mewn ambiwlansys. Dywedon nhw fod yr amseroedd aros am dderbyniadau i'r ysbyty wedi ychwanegu pwysau pellach ar wasanaethau ambiwlans sydd eisoes dan bwysau.
| “ | Roedd straen cynyddol yn y berthynas rhwng staff ysbytai a staff ambiwlans. Oherwydd nad yw ysbytai eisiau dadlwytho cleifion i mewn i’w hadran, byddem yn eistedd y tu allan yn ystod tywydd oer a phoeth gyda PPE llawn a dim seibiannau.”
- Parafeddyg |
| “ | Oherwydd bod ysbytai yn gorfod rhoi eu mesurau amddiffynnol yn eu lle oherwydd bod yn rhaid iddynt feddwl am eu staff eu hunain a'r cleifion, arweiniodd hynny at amseroedd hirach i gleifion y tu allan i archebu lle a bod eu triniaeth yn dechrau… galwad yn sydyn, yn lle para awr neu 2 awr, roedd yn troi’n 3 awr, 4 awr… gallai criw fod wedi mynd allan ac efallai treulio 8 awr ar un alwad yn unig rhwng trin y claf, dod â nhw i’r ysbyty a gorfod aros.”
– Rheolwr gwasanaethau ambiwlans |
Dywedodd parafeddygon mai dyma'r unig opsiwn i gleifion gael mynediad at ofal. Fel y straeon a glywsom gan gleifion (a drafodir yn ddiweddarach yn y bennod hon), rhoddodd rhai parafeddygon enghreifftiau o feddygon teulu nad oeddent am drin cleifion yr amheuir bod ganddynt Covid-19. Yn lle hynny, dywedodd meddygon teulu wrth gleifion am alw am ambiwlans. Roedd hyn yn cynnwys enghreifftiau o gleifion nad oedd angen gofal brys neu ofal brys arnynt.
| “ | Byddem yn cael ein hanfon allan yn rheolaidd i weld cleifion gartref nad oeddent yn gaeth i'r tŷ, y dywedwyd wrthynt am gadw draw o'u meddygfa ac aros am ymweliad gan barafeddyg. Ar un achlysur cytunodd meddyg teulu i ymweld dim ond ar ôl i mi asesu’r claf a phenderfynu nad oedd y salwch acíwt yn ganlyniad i Covid-19. Cawsom ein defnyddio fel caneris.”
- Parafeddyg |
| “ | Byddai’r meddygon teulu yn anfon ambiwlansys o gwmpas i gartrefi oherwydd nad oedden nhw am gael eu heffeithio ganddo.”
- Gweithiwr gofal iechyd proffesiynol |
Rhannodd llawer o gyfranwyr sut roedd hyn yn golygu bod parafeddygon wedi blino’n lân fwyfwy wrth i’r pandemig fynd rhagddo. Roedd absenoldeb salwch oherwydd Covid-19 hefyd yn gyffredin.
| “ | Roedd yna gyfnod pan oedd pentyrrau o bobl i ffwrdd a byddech chi'n siglo lan i'r gwaith ac yn edrych ar y bwrdd i weld pa ambiwlans rydych chi arno a gyda phwy rydych chi wedi'ch criwio, a'r bore hwnnw byddai hanner y bwrdd yn ysgafn. smotiau, oherwydd bod y bobl hynny wedi galw i mewn yn sâl gyda Covid, neu mae gan eu cyd-letywyr Covid, mae gan bartner Covid, felly ni allant ddod i mewn.”
- Parafeddyg |
Dywedodd rhai parafeddygon fod pwysau staffio wedi arwain at ambiwlansys yn cael eu hanfon at y galwadau mwyaf difrifol yn unig. Roedd hyn yn arbennig o broblemus pan gynyddodd y galw am ofal brys a gofal brys yn ddiweddarach yn y pandemig.
Stori TylerRoedd Tyler wedi ailhyfforddi fel parafeddyg yn ddiweddarach mewn bywyd, felly dim ond am gyfnod byr yr oedd wedi bod yn gwbl gymwys pan ddechreuodd y pandemig. Bu'n gweithio ar y rheng flaen drwy'r amser, gan ymateb i alwadau brys. “Roedden ni’n gweithio llawer o oriau, roedd llawer o salwch ac roedden ni wedi blino’n lân oherwydd doedden ni ddim yn gwybod beth oedd yn digwydd, doedden ni ddim yn gwybod beth i’w ddisgwyl, ond hefyd bob tŷ aethon ni iddo, wnaethon ni 'Ddim yn gwybod pwy oedd â Covid-19, pwy sydd ddim, sut wnaethon ni ei ddal." Ar y cyfan, roedd ei brofiad fel parafeddyg yn heriol iawn. Roedd yn cael trafferth gyda'i iechyd meddwl, a chyda theimlo'n ynysig oddi wrth ei gydweithwyr. Roedd gan barafeddygon eraill yr oedd yn gweithio gyda nhw broblemau tebyg, ac yn anffodus collodd un o'i gydweithwyr. “Roeddwn i wedi blino'n lân, yn ddraenio'n gyson, yn emosiynol iawn hefyd ... yr hyn na helpodd oedd mis i mewn i'r pandemig, cymerodd un o fy nghydweithwyr ei fywyd ei hun, a gafodd effaith enfawr bryd hynny arnom ni yn yr orsaf gyfan. ” Wrth i'r pandemig barhau, roedd heriau sylweddol gyda staffio oherwydd bod pobl i ffwrdd yn sâl gyda Covid-19, ac oherwydd bod criwiau'n treulio mwy o amser yn aros i gleifion gael eu derbyn i adrannau brys. Ar adegau, dim ond y galwadau mwyaf difrifol a brys yr oeddent yn eu mynychu. “Rydych chi mewn gwirionedd yn cymryd drosodd rôl yr ysbyty fel y gwely y tu allan…roedd yn cyrraedd y pwynt lle'r oeddem yn mynd i alwadau coch yn unig oherwydd dyna faint yr oeddem yn ei gael.” Roedd y pwysau staffio yn golygu bod y lluoedd arfog a diffoddwyr tân yn cael eu drafftio i mewn i helpu criwiau ambiwlansys. Er bod Tyler yn deall pam y digwyddodd hyn, roedd hefyd yn golygu ei fod i bob pwrpas yn rhoi sylw i'r gwaith a fyddai'n cael ei wneud fel arfer gan ddau barafeddyg. Ychwanegodd hyn at y pwysau a wynebai, a datblygodd bryder o ganlyniad. “Felly, daeth y fyddin i mewn i’n helpu ni a’r gwasanaeth tân…gan ein gwneud ni hyd yn oed yn fwy blinedig oherwydd rydych chi wedyn yn gwneud popeth gyda rhywun sydd ddim yn gwybod beth maen nhw’n ei wneud.” |
Profiadau trinwyr galwadau 111 a 999 y GIG
Disgrifiodd cyfranwyr a weithiodd fel trinwyr galwadau i GIG 111 a 999 yn ystod y pandemig y pwysau o siarad â phobl sâl ac yn aml mewn trallod.
Dywedodd y rhai oedd yn delio â galwadau wrthym fod yn rhaid iddynt ddelio â nifer fawr o alwadau gan bobl bryderus a sâl iawn, ac nid oeddent bob amser yn gallu cynnig cymorth yn enwedig yn ystod cyfnodau brig mewn heintiau Covid-19.
| “ | Fel arfer efallai y bydd 30 galwad yn aros ar unrhyw un adeg. Ar adegau brig yn y pandemig roedd 900 o alwadau yn aros.”
– triniwr galwadau GIG 111 |
| “ | Cawsom filoedd o alwadau’n cael eu pentyrru, roeddem yn poeni ein hunain gan fod yn rhaid i ni brofi’n rheolaidd, dim ond cyfradd is o gyflog y byddem yn ei chael felly roedd y straen ariannol hefyd yn amlwg.”
– triniwr galwadau GIG 111 |
Roedd rhai atebwyr galwadau yn rhannu pa mor anodd oedd hi i siarad â chleifion a oedd wedi aros am amser hir. Roedd delio â phobl yr oedd angen cymorth brys arnynt yn llethol i rai cyfranwyr, yn enwedig pan na allent gynnig y gofal a'r cyngor yr oedd pobl eu heisiau. Fe wnaethon nhw roi enghreifftiau o bobl a ddywedodd eu bod yn dirfawr angen ambiwlans, ond nid oedd eu symptomau yn ddigon brys i un gael ei anfon. Roedd hyn yn arbennig o heriol i'r rhai oedd yn delio â galwadau a oedd yn teimlo na allent ddianc o'r pandemig y tu allan i'r gwaith.
| “ | Byddwn yn gweithio 8, 10 sifft 12 awr weithiau ac yna'n dod adref i'r newyddion lle byddai'n rhaid i mi wylio faint o bobl a fu farw, mynd i'r ysbyty neu'r effaith yr oedd yn ei chael ar y byd i gyd. Ond ni allai unrhyw hyfforddiant erioed fod wedi dysgu person sut i ddelio â’r galwadau roedd yn rhaid i mi eu cymryd yn ddyddiol.”
– triniwr galwadau GIG 111 |
Disgrifiodd cyfranwyr a oedd yn gweithio fel trinwyr galwadau sut roedd newidiadau i’w sgript arferol, gan ei gwneud yn ofynnol iddynt sgrinio pob claf am symptomau Covid-19 posibl. Roedd llawer o’r galwadau’n gysylltiedig â Covid beth bynnag, gyda phobl yn poeni am symptomau a beth ddylen nhw ei wneud neu gan bobl oedd eisiau diweddariad yn dilyn galwadau cynharach.
| “ | Roedd pobl [yn] mynd i banig, yn ofnus, yn gynhyrfus, yn aml yn galw’n ôl oherwydd nad oeddent wedi cael unrhyw ddilyniant na chymorth.”
– triniwr galwadau GIG 111 |
Stori MehreenRoedd Mehreen wedi bod yn gweithio fel triniwr galwadau GIG 111 ers sawl blwyddyn. Ar ddechrau'r pandemig, dechreuodd dderbyn diweddariadau e-bost rheolaidd gyda gwybodaeth newydd a newidiadau i'w sgriptiau galwadau. Weithiau, byddai’r newidiadau hyn yn cael eu rhoi ar waith yng nghanol ei shifft, a oedd yn golygu bod Mehreen, a’i chydweithwyr yn addasu’n gyson i’r cyngor a’r arweiniad newidiol. Yn aml, byddai'r rheolwyr ardal lleol yn cerdded o amgylch y ganolfan alwadau i wirio bod y rhai oedd yn delio â galwadau wedi gweld y cyngor a'r arweiniad diweddaraf. “Rwy’n meddwl bod ein rheolwyr lleol, fel fy rheolwr llinell uniongyrchol y byddwn i wedi’i weld yn bersonol, roedden nhw’n wych. Roeddent bob amser yn cerdded o amgylch y ganolfan alwadau, 'Ydych chi wedi gweld y diweddariad hwn? Ydych chi'n gwybod bod hyn wedi newid?" Roedd Mehreen yn gweld gweithio yn y pandemig yn ddwys iawn, byddai'n aml yn dod i'w gwaith yn gynnar yn y bore ac yn ateb galwadau'n gyson. Roedd ymbellhau cymdeithasol yn golygu nad oedd yn bosibl eistedd yn agos at ei chydweithwyr, a oedd yn ei gadael yn teimlo'n unig. Wrth i'r pandemig fynd rhagddo cynyddodd y pwysau ar Mehreen, gyda'r rhai sy'n trin galwadau yn cymryd galwadau anodd ac emosiynol trwy gydol y dydd. Byddai'n aml yn cysuro cydweithwyr ar ôl galwad annifyr. “Byddech chi'n gwybod pan oedd rhywun wedi cymryd galwad anodd oherwydd rwy'n cofio i un o fy ffrindiau gymryd galwad lle dywedodd ei bod yn swnio fel petai'r person yn cymryd ei hanadl olaf cyn iddynt basio drwodd i'r gwasanaeth ambiwlans.” Teimlai fod cefnogaeth emosiynol dda ar gael yn ei chanolfan alwadau, gyda mynediad at rif therapi testun. Byddai ei rheolwyr llinell hefyd yn cofrestru ac yn gofyn i bobl gymryd seibiannau pan oedd angen. I Mehreen, y galwadau mwyaf trallodus oedd y rhai lle roedd pobl eisoes wedi ffonio 999 a chael gwybod nad oedd ambiwlansys ar gael. “Bydden nhw'n ein ffonio ni, a bydden ni fel, 'Ie, ond mae angen ambiwlans arnoch chi,' felly fe fydden ni'n mynd drwodd i ambiwlans, a bydden nhw fel, 'Ond does gennym ni ddim byd i'w anfon. .' Roedd hynny’n peri gofid.” Dros amser, effeithiodd dwyster ac effaith emosiynol gweithio yn y ganolfan alwadau ar Mehreen. Byddai'n crio weithiau ar ei dreif adref gan ei bod yn teimlo mor drist ac wedi ei llethu. “Tynais drosodd ar y ffordd adref i mewn i gilfan a chael gwaedd oherwydd ei fod mor galed. Fe wnes i ddarganfod bod yn rhaid i mi - ti'n gwybod lle ti ... cerddoriaeth oedd yr allfa, a byddwn i'n chwarae cerddoriaeth yn y car mor uchel â phosib yr holl ffordd adref i geisio gadael yr hyn roeddwn i wedi delio ag ef ar y ffonau ar ôl.” |
Yn ogystal â galwadau brig yn ymwneud â Covid-19, roedd cyfranwyr a oedd yn gweithio fel trinwyr galwadau ar gyfer GIG 111 neu 999 yn cofio llawer o alwadau a oedd yn canolbwyntio ar broblemau iechyd eraill, gan gynnwys effaith y pandemig ar iechyd meddwl. Rhannodd un cyfrannwr sut y cymerodd nifer o alwadau yn canolbwyntio ar iechyd meddwl, yn enwedig gyda'r nos.
| “ | Roedd mwy o alwadau hunanladdol a galwadau yn ymwneud ag iechyd meddwl nad oedd yr hyfforddiant wedi fy mharatoi ar eu cyfer mewn gwirionedd.”
– triniwr galwadau 999 |
Dywedodd y derbynwyr galwadau y clywsom ganddynt pan oeddent yn delio â galwad anodd, roedd rhyw lefel o gymorth cymheiriaid ar gael fel arfer. Fodd bynnag, roedd hyn yn aml yn anoddach ei gyrchu oherwydd ymbellhau cymdeithasol. Roedd hyn yn golygu y gallai'r rhai sy'n delio â galwadau gael cynnig cymorth drwy ystafell ymneilltuo neu gael eu hanfon adref.
O ystyried y pwysau y mae'r rhai sy'n delio â galwadau yn eu hwynebu, roedd rhai cyfranwyr yn rhannu sut rhoddwyd cymorth emosiynol mwy strwythuredig ar waith lle'r oeddent yn gweithio. Mewn un ganolfan alwadau, roedd y cymorth hwn yn cynnwys cael mynediad am ddim i ap myfyrio, mynediad at gwnsela, a rheolwyr a oedd ar lawr gwlad ac yn eu gweld bob shifft. Soniodd cyfranwyr eraill pa mor gefnogol oedd eu rheolwyr llinell.
| “ | Fy rheolwr llinell uniongyrchol, roedden nhw'n wych. Does dim amheuaeth o gwbl felly petaech chi wedi cael galwad anodd, bydden nhw'n dweud, 'Ewch i gael paned o de. Ewch i eistedd i lawr, bum munud.' Roedden nhw wir yn gofalu am y staff, maen nhw'n gwybod sut brofiad yw cael y bîp hwnnw yn eich clust a pheidio â gwybod beth fydd pwrpas yr alwad.”
– triniwr galwadau GIG 111 |
Clywsom hefyd gan y rhai oedd yn delio â galwadau a oedd yn teimlo nad oeddent yn cael eu cefnogi yn ystod y pandemig. Mewn rhai canolfannau galwadau, dywedodd cyfranwyr nad oedden nhw'n cael cymryd gwyliau hyd yn oed pan oedd ganddyn nhw bryder neu broblemau iechyd meddwl eraill. Beirniadodd rhai uwch reolwyr am nad oeddent yn poeni digon am yr effaith ar y rhai sy'n delio â galwadau.
| “ | Roeddwn i'n teimlo fy mod i'n rhedeg yn wag ... roedd hi'n teimlo [fel] eich bod chi'n trin galwadau, roeddech chi'n rhif, ac roedd disgwyl i chi fod yn y gwaith, wyddoch chi. Doedd dim ots beth oedd yn digwydd doeddwn i ddim yn teimlo fy mod yn cael fy nghefnogi o gwbl gan fy ngwaith…nid gan y rhai uwch i fyny. Roeddwn i'n teimlo nad oedd y gefnogaeth yno."
– triniwr galwadau GIG 111 |
Addaswyd canolfannau galwadau i leihau'r risg o haint Covid-19. Rhoddodd cyfranwyr enghreifftiau o’r camau a gymerwyd i leihau lledaeniad Covid-19 mewn canolfannau galwadau, gan gynnwys deiliadaeth desg is, mesurau cadw pellter cymdeithasol, darparu deunyddiau glanhau a chofnodi ble roedd staff yn gweithio i alluogi olrhain a lleihau lledaeniad y firws.
| “ | Fe wnaethon nhw gicio llawer o bethau diogelwch i mewn yn gyflym iawn, iawn, roedd bwlch mawr rhyngom ni i gyd, a masgiau, a daeth popeth i mewn ar unwaith.”
– triniwr galwadau 999 |
Mewn rhai canolfannau galwadau nid oedd digon o staff i ddelio â galwadau. Yn yr un modd â gwasanaethau eraill a welodd alw mawr yn ystod y pandemig, roedd lefelau staffio yn her. Roedd staff canolfannau galwadau yn aml i ffwrdd yn sâl neu'n hunanynysu ac roedd hyn yn lleihau maint y timau a oedd yn gweithio, gan waethygu'r capasiti a oedd eisoes wedi'i leihau oherwydd canllawiau cadw pellter cymdeithasol. Roedd hyn yn golygu nad oedd y rhai oedd yn delio â galwadau a oedd yn gweithio weithiau'n cael egwyl rhwng galwadau, gan gynyddu straen a blinder.
Rhoddodd y cyfranwyr enghreifftiau o rai ymgyrchoedd recriwtio llwyddiannus, yn enwedig dod â phobl i mewn o ddiwydiannau fel twristiaeth lle'r oeddent wedi colli eu swyddi yn ystod y pandemig.
| “ | Fe wnaethom recriwtio llawer o bobl yn ystod y cyfnod hwnnw. Yn rhyfedd ddigon, llawer o bobl o dwristiaeth. Hyd yn oed ar yr adegau gorau, mae'n swydd llawn straen. Gyda phandemig byd-eang yn mynd rhagddo, a phwysau galwadau yn ddi-ildio, gall fod hyd yn oed yn fwy o straen. Felly do, roedd yna lawer o bobl wedi ymuno, ond mae llawer o bobl hefyd wedi gadael.”
– triniwr galwadau 999 |
Profiadau cleifion o ofal brys a gofal brys
Roedd cael mynediad at ofal brys yn aml yn anoddach yn ystod y pandemig, hyd yn oed pan oedd pobl yn sâl iawn. Roedd diffyg cymorth mewn sefyllfaoedd brys neu argyfwng yn brofiad cyffredin, ac felly hefyd oedi hir hyd yn oed pan gynigiwyd triniaeth.
Cafodd y problemau hyn effaith sylweddol a thrasig ar gleifion. Mae’r straeon a rannwyd gyda ni gan glinigwyr a chleifion yn cynnwys enghreifftiau o oedi wrth gael mynediad at ofal brys ar bob cam: pobl yn aros yn hirach nag y byddent fel arfer i ofyn am help; mae'n cymryd amser i ddod o hyd i wasanaeth sy'n fodlon eu hasesu a chynnig gofal; ambiwlansys yn araf i gyrraedd; a derbyniadau i'r ysbyty yn cymryd sawl awr, gan adael cleifion yn aros mewn ambiwlansys.
| “ | Erbyn Rhagfyr 2020 nid oedd unrhyw ambiwlansys, dim meddygon teulu, dim lle yn yr adran damweiniau ac achosion brys ac roedden ni'n llythrennol yn troi lan i gartrefi pobl i ddosbarthu ocsimetrau gan erfyn am help. Roedd cleifion yn marw cyn i ni allu cyrraedd yno neu'n gyfan gwbl yn y tywyllwch ynghylch pa mor sâl oeddent. Aelodau teulu anobeithiol yn erfyn arnom am help pan gyrhaeddon ni gan ddisgwyl i ni allu helpu.”
- Parafeddyg |
Rhannodd cleifion lawer o brofiadau eu bod nhw neu anwyliaid yn sâl iawn ac yn ffonio eu meddyg teulu, GIG 111 neu 999 i ofyn am gymorth, ond yn wynebu oedi neu ddim yn derbyn gofal. Roedd rhai cyfranwyr naill ai'n rhoi'r gorau iddi neu'n gorfod aros nes bod eu symptomau'n mynd yn ddifrifol iawn cyn ceisio eto. Roedd profiadau tebyg ymhlith y rhai a oedd wedi amau neu wedi cadarnhau Covid-19 a’r rhai oedd â phroblemau meddygol brys eraill.
| “ | Un noson roeddwn yn sâl dro ar ôl tro. Am 1am galwais 999 a dywedasant y byddent yn anfon ambiwlans. Erbyn 6am nid oedd wedi cyrraedd o hyd ac fe es i yn ôl i'r gwely, yn feichiog ac wedi blino'n lân. Am 11am fe ffoniodd rhywun i ofyn a oeddwn i angen yr ambiwlans o hyd a bod achosion eraill yn fwy “brys”. Fe wnaethon nhw fy nghynghori i gysylltu â fy meddyg teulu. Fe wnes i a gwrthododd y meddyg teulu fy ngweld gan ddweud y dylwn gysylltu â 999 eto. Ar y pwynt hwn rhoddais y gorau iddi. Doedd dim help.”
- Person a ffoniodd 999 |
Yn nyddiau cynnar y pandemig, dywedodd rhai cyfranwyr ei bod yn aneglur sut yr oedd achosion amheus o Covid-19 yn cael eu trin. Roeddent yn meddwl bod gwasanaethau iechyd yn ofalus ynghylch darparu gofal o ystyried y risgiau, a bod hyn yn golygu oedi a phroblemau i gleifion. Roedd cael eu cyfeirio rhwng gwasanaethau yn parhau i fod yn broblem i lawer o gyfranwyr a geisiodd gael mynediad at ofal brys trwy gydol y pandemig.
| “ | Roedd ffrind agos iawn wedi bod yn dangos symptomau Covid-19 am fwy na phythefnos yn gynnar ym mis Mawrth 2020. Ffoniodd y meddyg teulu a GIG 111 sawl gwaith ond dywedwyd wrtho am aros gartref ac ynysu. Roedd yn byw ar ei ben ei hun ond fe wnes i gadw mewn cysylltiad... un diwrnod doeddwn i ddim yn gallu cael ateb ar y ffôn. Penderfynodd ffrind agos arall fynd i mewn i'w dŷ, a chanfu ef bron yn ddigyswllt ac yn ddadhydredig, ambiwlans a elwir felly. Gwrthododd y parafeddygon fynd i fyny’r grisiau i’w helpu, a gadawyd i’w ffrind ei gael i lawr y grisiau ac i mewn i’r ambiwlans.”
– Ffrind i berson oedd angen gofal |
Myfyriodd rhai cleifion hefyd ar ba mor ofnus oedd pobl i ofyn am help, hyd yn oed mewn sefyllfaoedd brys. Dywedodd llawer o gyfranwyr wrthym fod eu hofn o ysbytai a pheidio â bod eisiau llethu systemau gofal iechyd yn golygu eu bod nhw neu eraill yr oeddent yn eu hadnabod yn oedi neu’n osgoi ceisio gofal brys, gyda chanlyniadau ofnadwy weithiau.
| “ | Roedd fy nhad-yng-nghyfraith yn sâl ym mis Mai 2020 a chafodd rai cyfnodau chwydu a haint ar y frest wedi hynny oherwydd dyhead. Ffoniodd fy mam-yng-nghyfraith fi mewn dagrau - nid oedd wedi ffonio eu meddyg teulu na GIG 111 oherwydd bod y newyddion wedi bod yn llawn adroddiadau bod y GIG wedi’i lethu, ond roedd fy nhad-yng-nghyfraith erbyn hynny yn eithaf sâl.”
– Aelod o deulu rhywun oedd angen gofal |
Hanes HarriDaliodd Henry Covid-19 ym mis Awst 2020. Ar ôl teimlo ychydig yn sâl am bythefnos aeth yn ôl i'w waith. Ar ôl ychydig ddyddiau dechreuodd gael anawsterau anadlu ofnadwy ac roedd yn teimlo'n sâl iawn. Cysylltodd â'i feddyg teulu, a ofynnodd iddo gysylltu â 119 i drafod ei symptomau penodol. Dywedodd 119 y dylai siarad â’i feddyg teulu eto gan na allent wneud atgyfeiriad i glinig Covid. Aeth Henry yn ôl ac ymlaen rhwng ei feddyg teulu a’r gwasanaeth 119 cyn iddo gael ei atgyfeirio i ganolbwynt Covid-19 lleol. Fodd bynnag, ni chlywodd gan y ganolfan, a phan gysylltodd â hwy dywedasant nad oedd ganddynt unrhyw gofnod o’i atgyfeiriad. Ar y pwynt hwn gwaethygodd symptomau Henry. Yn y diwedd fe ffoniodd GIG 111 i geisio cael cymorth, ond dywedodd y person y siaradodd ag ef am alw ambiwlans os oedd ei symptomau'n ddigon drwg. “Roeddwn i’n ysu am help, poenau yn y frest, yn brwydro i anadlu ac yn gaeth i’r gwely yn bennaf.” Teimlai Henry na allai gysylltu â 999 oherwydd bod cymaint yn y newyddion am bobl yn peidio â ffonio ambiwlans oni bai ei fod yn argyfwng difrifol. Roedd yn poeni y byddai'n gwastraffu amser staff y GIG, yn enwedig pan nad oedd yr un o'r gweithwyr gofal iechyd proffesiynol y siaradodd â nhw wedi ystyried ei symptomau fel argyfwng. Yn y pen draw, aeth Henry yn ôl at ei feddyg teulu a'i atgyfeiriodd at glinig anadlol. Ar ôl iddo gael ei asesu gan y clinig, fe'i cynghorwyd i fynd yn syth i'r adran damweiniau ac achosion brys. “Ces i fy nhywys yn syth bin a'm cysylltu â monitor calon. Llawer o brofion yn ddiweddarach, dywedwyd wrthyf fod fy mhwysedd gwaed mor uchel fel fy mod ddyddiau i ffwrdd o fethiant y galon. Fe gymerodd ddau fis i rywun weld, ni ddylai hynny fod wedi cymryd cymaint o amser.” |
Pan anfonwyd ambiwlansys, roedd amseroedd aros hir mewn ysbytai yn achosi problemau sylweddol ac yn rhoi cleifion mewn perygl. Fel y rhannodd parafeddygon, roedd cleifion brys yn aml yn gorfod aros mewn ambiwlans am sawl awr cyn cael eu derbyn i'r ysbyty. Rhoddodd cleifion a gofalwyr lawer o enghreifftiau o'r profiadau anodd hyn. Roedd rhai cyfranwyr yn beio'r oedi cyn cael eu derbyn i'r ysbyty am gleifion yn mynd yn ddifrifol wael neu'n marw.
| “ | Cefais fy rhuthro i mewn i'r ysbyty ac oherwydd bod yr ysbyty mor brysur ar y pryd, gallaf gofio cael gwybod fy mod wedi bod allan mewn ambiwlans am fwy na chwe awr ac roeddwn ar drip ac yn sâl iawn oherwydd roedd yr ysbyty mor llawn o pobl sâl yn ystod yr amser. Fe aethon nhw [yr ambiwlans] â fi yno, roeddwn i [yno tan] dri y bore, a dweud y gwir yn ceisio cael gwely i mi.”
– Claf damweiniau ac achosion brys |
| “ | Dioddefodd fy nhad farwolaeth araf a phoenus. Nid oedd ganddo Covid-19 ond fe’i gadawyd heb oruchwyliaeth mewn ambiwlans yn yr adran damweiniau ac achosion brys yn hytrach na bod ei arwyddion hanfodol wedi’u cofnodi. Erbyn iddo gael ei ddarganfod, roedd hi'n rhy hwyr, fe ddioddefodd ataliad y galon ar ei ffordd i gael sgan CT. Awst 2020 oedd hwn.”
- Aelod o'r teulu mewn profedigaeth |
Clywsom hefyd enghreifftiau o sut roedd pobl yn teimlo y gwahaniaethwyd yn eu herbyn wrth geisio cael mynediad at ofal brys. Er enghraifft, roedd rhai cyfranwyr o gefndir ethnig lleiafrifol yn teimlo eu bod yn cael eu dad-flaenoriaethu gan y gwasanaethau ambiwlans oherwydd eu hil ac ethnigrwydd, a bod gwahaniaethu wedi chwarae rhan wrth benderfynu pwy oedd yn cael blaenoriaeth ar gyfer triniaeth.
| “ | Byddwn yn dweud, roedd pobl wyn yn cael eu trin yn gyflymach ac yn gyflymach, wyddoch chi. Roedden nhw’n Ddu, yn cael eu gadael am oriau mewn, fel gofal brys, neu hyd yn oed yn cael gwybod am fynd adref.”
– Person o gefndir ethnig Du |
Clywsom hefyd enghreifftiau o aelodau teulu yn wynebu gwahaniaethu wrth geisio dod o hyd i wybodaeth am eu hanwyliaid mewn sefyllfaoedd brys.
Stori PriyaCafodd ewythr Priya ei ruthro i'r ysbyty ar ôl dioddef gwaedlif ar yr ymennydd, cyrhaeddodd tua 20 aelod o'r teulu, yn bryderus am ddiweddariadau ar ei gyflwr. Gan ddeall cyfyngiadau Covid-19, siaradodd y teulu â'r derbynnydd a chytuno mai dim ond pedwar ohonyn nhw fyddai'n aros yn yr ystafell aros tra bod y lleill yn mynd adref. Am y chwe awr nesaf, wrth i ewythr Priya gael llawdriniaeth, cymerodd y pedwar aelod o'r teulu eu tro gan fynd at ddesg y dderbynfa bob dwy awr i gael diweddariadau. Roedd y derbynnydd ar ddyletswydd yn garedig ac yn deall eu sefyllfa. Fodd bynnag, pan newidiodd y sifftiau, daeth Priya a'i chwaer ar draws gwahaniaeth mawr yn y driniaeth. Wrth iddynt gerdded tuag at y ddesg dderbynfa, edrychodd derbynnydd gwyn ar Priya a'i modryb, troi at ei chydweithiwr, a dweud rhywbeth anghlywadwy. Pan gyrhaeddodd Priya a'i chwaer y cownter, gwrthododd y derbynnydd arall siarad â nhw, gan ohirio i'w chydweithiwr. Yna siaradodd y derbynnydd â Priya a'i theulu mewn ffordd oddefgar a gwahaniaethol. Roedd Priya wedi'i syfrdanu ac wedi'i chythruddo gan y ffordd y cawsant eu trin, gan ei bod hi a'i theulu wedi bod yn gydweithredol ac yn parchu polisïau'r ysbyty. “Dw i’n meddwl mai dyna lle roedden ni’n teimlo ychydig o hiliaeth, gyda’r ail dderbynnydd a ddaeth ar shifft.” Ni allai Priya helpu ond sylwi ar y gwrthgyferbyniad clir yn agwedd y derbynnydd tuag at deulu gwyn yn yr ystafell aros, a oedd fel pe baent yn gallu mynd at y ddesg yn amlach heb unrhyw broblemau. Ychwanegodd y gwahaniaethu a diffyg empathi gan y derbynnydd gwyn drallod ychwanegol at sefyllfa a oedd eisoes yn drawmatig. “Yr unig beth fyddwn i’n ei ddweud yw trin pawb yn gyfartal. Does dim ots o ble maen nhw'n dod, dim ots sut maen nhw'n edrych, dim ots pa iaith maen nhw'n siarad. Jest, dwi’n meddwl, dylai pawb gael eu trin yn gyfartal.” |
Er gwaethaf y problemau ynghylch oedi a phrofiadau anodd eraill, rhannodd rhai cyfranwyr brofiadau mwy cadarnhaol o ofal brys. Er enghraifft, ambiwlansys yn cyrraedd pan fo angen, ac yn derbyn lefel uchel o ofal gan barafeddygon.
| “ | Ffoniodd fy ngŵr am ambiwlans, a chyrhaeddodd o fewn 6 munud. Roedd y parafeddygon yn hyfryd. Gan fod curiad fy nghalon yn afreolaidd a fy mod hefyd wedi anafu fy wyneb pan gwympais, penderfynwyd y dylwn fynd i'r ysbyty. Roedd y staff yn yr adran damweiniau ac achosion brys yn garedig, yn gyfeillgar ac yn broffesiynol, er gwaethaf y cyfyngiadau pandemig parhaus.”
– Claf damweiniau ac achosion brys |
| “ | Deuthum yn sâl ym mis Hydref 2020 ni allwn gael apwyntiad [meddyg teulu] wedi cael galwad ffôn a chefais wrthfiotigau. Gwaethygodd yn y pen draw ar ôl dim cymorth gan feddygfa leol [ffoniodd fy] gŵr am help. Cyrhaeddodd parafeddygon yn gyflym iawn, yna cyrhaeddodd ambiwlans a chael eu cludo i'r ysbyty lleol. Oddi yno o fewn awr trosglwyddo i'r prif ysbyty gyda sepsis. Wedi gweithredu ar unwaith ac achubwyd fy mywyd.”
- Claf ysbyty |
2. Roedd 119 yn llinell rhadffôn a ddefnyddiwyd yn y pandemig i drin achosion penodol o Covid-19 ac i dynnu pwysau oddi ar GIG 111.
6. PPE a phrofion mewn lleoliadau gofal iechyd |
 |
Mae’r bennod hon yn dod â phrofiadau o offer amddiffynnol personol (PPE) ynghyd yn ystod y pandemig a phrofion Covid-19 ar draws staff gofal iechyd yn ystod y pandemig. Mae PPE a phrofion yn chwarae rhan bwysig mewn atal a rheoli heintiau. Mae'r bennod hon yn dechrau drwy ddisgrifio profiadau gweithwyr gofal iechyd proffesiynol o argaeledd, ansawdd a ffitrwydd PPE. Yna mae’n trafod effaith PPE ar ofal cleifion, cyn rhannu profiadau o brofion Covid-19 ymhlith gweithwyr gofal iechyd proffesiynol.
Argaeledd PPE
Mae PPE yn cynnwys eitemau neu ddillad amddiffynnol a ddefnyddir i atal lledaeniad a haint Covid-19. Mae hyn yn cynnwys masgiau wyneb, gynau, offer amddiffyn llygaid a menig.
Un o'r heriau anoddaf a rannwyd gyda ni gan weithwyr gofal iechyd proffesiynol sy'n gweithio mewn ysbytai dim digon o PPE o ansawdd da, yn enwedig ar ddechrau’r pandemig. Dywedodd cyfranwyr fod anghysondeb yn aml rhwng maint ac ansawdd y PPE oedd ganddynt, a’r PPE a argymhellwyd ar y pryd er eu diogelwch. Dywedodd rhai nad oedd ganddyn nhw'r amddiffyniad cywir a'u bod yn teimlo eu bod wedi'u gadael gan y llywodraeth.
Dywedodd llawer wrthym am eu rhwystredigaeth a'u hofn, a sut roeddent yn teimlo nad oedd eu diogelwch yn cael ei gymryd o ddifrif. Roedd hwn yn brofiad cyffredin ymhlith staff ar draws llawer o wahanol rolau, ond yn enwedig yn rheng flaen yr ymateb pandemig.
| “ | [Roedden ni] yn dadlau drwy'r amser ynghyd â'n holl gydweithwyr ar hyd a lled y wlad bod angen gwell lefelau o PPE arnom...pe bai'n firws tebyg i Ebola neu rywbeth tebyg, rwy'n meddwl y byddai pob un ohonom ni' wedi cael eu dileu. Does dim ffordd bod y lefel hon o PPE yn addas…Y ffordd sy’n eich gadael chi’n teimlo yw bod braidd yn waradwy am wn i.”
-Meddyg ysbyty |
Er y dywedodd cyfranwyr wrthym fod argaeledd PPE wedi gwella’n gyffredinol wrth i’r pandemig fynd rhagddo, disgrifiodd rhai broblemau'n parhau am gyfnod hwy. Fe wnaethant rannu straeon am heriau parhaus gyda chyflenwadau PPE neu newid cyflenwadau a oedd yn golygu bod yn rhaid eu gosod dro ar ôl tro ar gyfer gwahanol fathau o PPE.
Roedd hyn yn hynod bryderus i staff sy’n gofalu’n uniongyrchol am gleifion â Covid-19. Roedd llawer o gyfranwyr yn grac am y risgiau y gorfodwyd iddynt eu cymryd. Gwnaeth rhai gysylltiad uniongyrchol rhwng PPE o ansawdd gwael a hwythau neu eu cydweithwyr yn cael eu heintio â Covid-19.
| “ | Roedd llawer o ddicter ymhlith staff yr ysbyty, o bob gradd. Achoswyd llawer o hyn gan gyflenwadau achlysurol o PPE a’r diffyg gwybodaeth ynghylch a fyddai gennym ddigon i’n cadw’n ddiogel trwy gydol y pandemig.”
- Gweithiwr gofal iechyd proffesiynol |
Amlygodd cyfranwyr o gefndiroedd lleiafrifoedd ethnig eu pryderon ynghylch diogelwch, a’u hofnau y byddai diffyg PPE yn cael effaith anghymesur arnynt hwy ac ar bobl o’u cymuned. I rai, ychwanegodd hyn at y pryder a'r straen yr oeddent yn ei deimlo am weithio ym maes gofal iechyd.
| “ | Pan ddechreuon ni glywed am bobl o liw yn marw, roedden ni allan yma heb ddim i'n hamddiffyn. Doeddwn i ddim eisiau gweithio, heb sôn am fod yn nyrs.”
– Nyrs ysbyty o gefndir ethnig lleiafrifol |
| “ | Yn y dechrau, gwrthodwyd PPE i mi gan fy nghyflogwr GIG – nid oeddwn yn cael gwisgo mwgwd wyneb ac ni allwn ddefnyddio unrhyw un fy hun, er gwaethaf cael cysylltiad uniongyrchol â chleifion a oedd yn dod i’r ward. Rwy'n credu bod llawer o bobl o liw wedi'u rhoi mewn sefyllfaoedd a oedd yn bygwth bywyd yno. Yn y diwedd ces i doriad i lawr oherwydd y straen a achosodd i mi.”
– Gweithiwr gofal iechyd proffesiynol o gefndir ethnig lleiafrifol |
Roedd llawer o gyfranwyr sy’n gweithio ym maes gofal sylfaenol hefyd yn rhannu problemau gyda chyflenwad PPE ar ddechrau’r pandemig. Dywedasant ei bod yn anodd ac yn araf i gael gafael ar y math cywir o PPE i'r lefel o ansawdd yr oedd ei angen arnynt. Roedd barn gref hefyd ymhlith llawer o gyfranwyr bod ysbytai yn cael eu blaenoriaethu dros leoliadau gofal iechyd eraill.
| “ | Ar y cychwyn cyntaf dyna pryd roedd angen y PPE gorau arnom, a doedd gennym ni ddim byd…daeth y PPE yn nes ymlaen. Nid oedd yr ymateb cychwynnol yn ddigonol. Roedd hyn yn golygu bod mwy o staff yn sâl ac yn dod i gysylltiad yn gynnar. Cymerodd ei doll yn feddyliol. Nid oedd gan y derbynyddion PPE ac roedden nhw’n wynebu cleifion, a nhw oedd yn sâl.”
- Meddyg Teulu |
Disgrifiodd llawer o gyfranwyr sy’n gweithio ym maes gofal sylfaenol sut y bu i’r cyflenwad PPE wella dros amser, ac yn ddiweddarach roeddent yn gallu cael gafael ar PPE yn haws.
| “ | Rwy'n meddwl i ddechrau, ychydig yn araf ond nid oedd yn hir; yn sicr cawsom ddigon [PPE] yn weddol gyflym ar ôl oedi cychwynnol.”
– nyrs meddyg teulu |
Dywedodd staff iechyd cymunedol fod rhai cyflenwadau sylfaenol ar gael yn ystod wythnosau cynnar y pandemig. Fodd bynnag, roedd llawer o gyfranwyr yn rhannu barn staff gofal sylfaenol bod PPE yn cael ei flaenoriaethu ar gyfer ysbytai, gan adael staff cymunedol heb yr offer angenrheidiol.
| “ | Roedd gennym ni fenig a ffedogau bob amser beth bynnag…cymerodd amser hir i ni gael y fisorau, a dweud y gwir, oherwydd bod y fisorau’n cael eu rhoi i staff yr ysbyty, ac rwy’n meddwl nad oedd hi tan tua’r Pasg cyn i ni gael y fisorau yn y gymuned .”
– Gweithiwr gofal iechyd proffesiynol perthynol |
Dywedodd cyfranwyr wrthym am ysbytai yn rhannu PPE gyda thimau cymunedol i helpu i gefnogi darparu gofal yn ddiogel. Fodd bynnag, roedd yn ymddangos bod yr ymagwedd at hyn yn amrywio mewn gwahanol leoedd ac yn dibynnu ar benderfyniadau a wneir yn lleol.
| “ | Yn y gwasanaeth cleifion mewnol, roedd gennym fynediad ar unwaith. Pan ddechreuodd gwasanaethau cymunedol ailgychwyn, roedd ychydig yn fwy heriol. Pe baem yn gwybod bod gwir angen gweld claf yn y gymuned, roedd yna adegau pan fyddem yn cynnig mynediad i’r timau gwasanaethau cymunedol i rai o’n PPE… Rwy’n sicr yn gwybod bod gan wasanaethau cymunedol lawer mwy o heriau o ran gallu cael PPE. Dydw i ddim yn meddwl ei bod yn gymaint o her i wasanaethau cleifion mewnol.”
– Gweithiwr gofal iechyd proffesiynol perthynol |
Clywsom am sut yr oedd dod o hyd i PPE i ddechrau yn ymddangos yn anhrefnus i rai staff, a sut roedd yn rhaid iddynt ddod o hyd i gyflenwadau mewn ffyrdd eraill. Lle nad oedd gan leoliadau gofal iechyd ddigon o PPE, rhannodd cyfranwyr sut yr oeddent yn cynyddu archebion trwy gyflenwyr rheolaidd. Rhannodd rhai hefyd sut yr oeddent yn edrych am PPE nas defnyddiwyd gan sefydliadau eraill yn lleol. Mae'r straeon yn cynnwys enghreifftiau o dderbyn masgiau o garejys ceir neu gynau gan filfeddygon. Dywedodd staff eu bod yn defnyddio eu rhwydweithiau i ddod o hyd i wahanol lwybrau i gael mynediad at PPE, gan wneud eu gorau i ddod o hyd i'r hyn a allent.
| “ | O ran offer PPE, rwy'n meddwl mai ar y dechrau [bod yna] y bu'r prinder, ond yr ysgolion a'r cymunedau oedd yn gwneud fisorau a phethau. Roedd yn anhygoel pa mor gyflym a faint yr oeddent am ei helpu. Rwy'n meddwl bod rhywfaint o'r pethau a wnaeth pobl o hyd yn yr ysbyty. Roedd yn fewnlifiad o bobl a oedd yn barod i wneud unrhyw beth, dim ond i wneud yn siŵr ein bod yn gallu amddiffyn ein hunain a helpu i amddiffyn cleifion. Roedd yn wirioneddol, roedd yn ysbrydoledig gweld beth oedd y gymuned yn ei wneud i ni, a gwnaeth i ni wybod eu bod yn ceisio helpu mewn unrhyw ffordd y gallent."
- Nyrs ysbyty |
Roedd gweithwyr gofal iechyd proffesiynol yn ddiolchgar am unrhyw roddion ac ewyllys da gan y gymuned. Disgrifiwyd y cymorth cymunedol hwn yn aml fel rhywbeth hanfodol, gyda phractisau meddygon teulu weithiau’n defnyddio PPE a roddwyd wrth iddynt aros am gyflenwadau canolog.
Clywsom hefyd am bractisau meddygon teulu yn prynu eu PPE eu hunain drwy gyflenwyr preifat i sicrhau eu bod yn cael eu stocio’n ddigonol. Roedd enghreifftiau o systemau rhybuddio yn cael eu sefydlu i fonitro'r defnydd o PPE ac i nodi pan oedd angen mwy. Roedd rhai o’r rhai sy’n gweithio ym maes gofal sylfaenol yn rhannu bod cyflenwad PPE wedi bod yn weddol anhrefnus yn seiliedig ar eu profiad ym misoedd cynnar y pandemig.
| “ | Roedd yr ymchwydd mewn gofynion PPE a hynny i gyd braidd yn wallgof ac roedd llawer o le storio pethau a phethau yn cael eu prynu gan filfeddygon a Duw a ŵyr ble i geisio gosod masgiau a masgiau FFP3 yn gyntaf. Rwy’n meddwl efallai pe bai wedi cael ei feddwl ychydig yn fwy yn hytrach nag adweithiol drwy’r amser, efallai y byddai wedi cael ei drin yn well.”
– rheolwr practis meddyg teulu |
Hyd yn oed pan oedd meddygon teulu yn gallu dod o hyd i PPE, gallai hyn achosi problemau gwahanol. Er enghraifft, rhannodd un cyfrannwr sy'n gweithio ym maes gofal sylfaenol sut y dechreuodd redeg allan o ofod storio. Yn y diwedd, cawsant gyflenwad o PPE nad oedd ei angen mwyach. Fe wnaethon nhw ei roi i sefydliadau eraill fel cartrefi gofal.
| “ | Cawsom ein hunain yn gyson yn gorfod cysylltu â’r bwrdd iechyd yn gofyn a allem eu dychwelyd, ac ni allem hynny, felly byddai’n rhaid inni gysylltu â meddygfeydd eraill i weld a allent ddefnyddio’r PPE. Yn y diwedd fe wnaethon ni roi llawer o PPE i gartrefi gofal lleol.”
– rheolwr practis meddyg teulu |
Rhannodd gweithwyr gofal iechyd proffesiynol broblemau a gawsant gydag ansawdd PPE mewn ysbytai a gofal sylfaenol. Dywedodd cyfranwyr wrthym fod ansawdd PPE yn wael, hyd yn oed pe bai wedi cael ei gyflenwi iddynt yn gymharol gyflym. Roedd cyfranwyr yn meddwl ei bod yn haws dod o hyd i PPE o ansawdd is. Teimlai llawer eu bod wedi cael eu rhoi mewn perygl oherwydd Covid-19 mewn ffordd na ddylent fod wedi bod.
| “ | Roedd y ddarpariaeth PPE i feddygon teulu yn wael. Neu'n wael o ran ansawdd, rwy'n meddwl ein bod wedi cael ein ffedogau plastig simsan a'n masgiau papur yn weddol gyflym ... y diffyg derbyniad bod tystiolaeth sylweddol bod mwgwd o ansawdd gweddus yn gwneud llawer o wahaniaeth os ydych mewn cysylltiad â chleifion gyda Covid-19. A’i bod wedi cymryd cymaint o amser, ei bod wedi cymryd cymaint o amser i hynny gael ei gyflwyno.”
- Meddyg Teulu |
Rhannodd cyfranwyr a oedd yn gweithio mewn ysbytai straeon am PPE a fyddai'n torri neu â thyllau. Rhoesant hefyd enghreifftiau o PPE gyda sticeri a oedd yn dangos ei fod wedi dyddio. Disgrifiodd rhai orfod ailddefnyddio PPE a oedd wedi'i olchi. Nid oeddent yn ymddiried y byddai'r PPE hwn yn eu hamddiffyn.
| “ | Ar ôl cael gwybod bod y siwt neidio plastig melyn rydych chi'n ei gwisgo yn mynd i gael ei golchi a'i hailddefnyddio, a bod y gogls rydych chi'n eu gwisgo yn mynd i gael eu golchi a'u hailddefnyddio, roedd yn teimlo'n ail-law. Oherwydd y gallech weld eich hun yn chwysu a dim ond y rheolaeth haint ohono, pwy sy'n ei olchi? Ble mae'n mynd? Ac yna rydych chi'n gwisgo rhai rhywun arall. Roedd llawer o’r offer yn teimlo’n rhad iawn hefyd, yn enwedig y gogls a fyddai’n torri.”
- Nyrs ysbyty |
Er bod rhai cyfranwyr wedi siarad yn gadarnhaol am ansawdd y PPE oedd ar gael iddynt. Er enghraifft, disgrifiodd arbenigwr mewn uned ganser ranbarthol ychydig o broblemau cychwynnol ond teimlai wedyn eu bod yn cael cyflenwad digonol o PPE o ansawdd da.
Ffit a chysur PPE
Teimlai cyfranwyr a oedd yn gweithio ym maes gofal iechyd yn ystod y pandemig fod dyluniad a ffit rhai PPE yn achosi problemau sylweddol. Roedd y problemau hyn yn aml yn gysylltiedig â mathau newydd neu anghyfarwydd o PPE.
| “ | Roeddwn i'n arfer gwneud rhai sifftiau yn y ward esgor…pe bai'n rhaid i ni fynd i mewn i theatr [llawdriniaeth] gyda rhywun ... roedd rhaid i ni wisgo'r gynau mawr glas, menig dwbl, yr het, y mwgwd [wedi'i ffitio]. Roedd yn rhaid i chi gael eich ffitio ar gyfer eich mwgwd a'ch pethau eich hun, felly unwaith roeddech yn y theatr honno, roeddech i mewn. Ni allech fynd allan, ni allech gael diod oherwydd yn amlwg, ni allech dynnu'ch mwgwd, ac yr oedd hyny yn gwbl arswydus. Dyna oedd y teimlad gwaethaf, gorfod gwisgo hynny i gyd [am] hyd llawn yr adran c brys. Roedd hynny’n gwbl erchyll, a dyna oedd pob shifft.”
- Cynorthwyydd gofal iechyd ysbyty |
Rhannodd gweithwyr gofal iechyd proffesiynol lawer o enghreifftiau o PPE nad oedd yn eu ffitio'n iawn ac roedd yn rhaid eu haddasu. Er enghraifft, tynnodd ychydig o weithwyr gofal iechyd proffesiynol benywaidd sylw at y ffaith nad oedd PPE yn aml yn ffitio ac yr oedd yn ymddangos ei fod wedi'i gynllunio i ffitio dynion.
| “ | [Cafodd PPE] ei archebu mewn meintiau a oedd yn gweddu’n bennaf i’r gwryw cyffredin, nid y gweithiwr GIG cyffredin, roeddwn yn aml wedi fy llethu cymaint yn fy PPE fel ei fod yn anghyfforddus ac yn gyfyngol.”
- Gweithiwr gofal iechyd proffesiynol |
Roedd gorfod gwneud addasiadau neu addasiadau yn lleihau hyder ynghylch pa mor dda yr oedd y PPE yn gweithio i’w hamddiffyn, yn ogystal â’i gwneud yn anoddach iddynt gyflawni tasgau yr oedd angen iddynt eu gwneud.
| “ | Roeddwn i'n arfer ei rolio hyd at fy ngwasg, cael ffedog a defnyddio'r ffedog fel gwregys, ac yna hongian beiro oddi ar hwnnw hefyd. Felly, nid oedd y maint yn wych ac yna rydych chi'n fwy nag yr ydych chi'n meddwl ydych chi ac rydych chi'n taro llawer o eitemau oherwydd mae gennych chi fwy o led."
- Nyrs ysbyty |
Hyd yn oed ar gyfer offer cyfarwydd neu safonol, roedd staff yn gorfod gwisgo PPE am gyfnodau hir yn arwain at broblemau gyda ffit a chysur a effeithiau corfforol negyddol ar staff.
| “ | Dim ond y pethau o ddydd i ddydd rydyn ni'n eu gwneud - ac rydych chi'n dueddol o esgeuluso'ch hun, fel diod neu fynd i'r toiled oherwydd roedd yn rhaid i chi dynnu'ch holl PPE ac roedd hynny'n flinedig. Yna byddai'n rhaid i chi ddod yn ôl a rhoi'r cyfan ymlaen. Felly roedd hynny’n anodd…[ac] roedd hynny dros ddwy flynedd.”
- Cynorthwyydd gofal iechyd ysbyty |
Mae effeithiau corfforol eraill yn cynnwys enghreifftiau o frech, sensitifrwydd croen, a marciau o wisgo masgiau am gyfnodau hir. Rhannodd un cyfrannwr sut y gwnaethant ddisodli masgiau FFP3 (math o fasg wyneb sy'n cael ei wisgo dros y trwyn a'r geg i amddiffyn y gwisgwr rhag anadlu sylweddau peryglus) â chyflau awyru oherwydd bod masgiau rheolaidd yn rhoi briwiau pwyso iddynt.
Roedd problemau gydag anghysur nid yn unig oherwydd ffit gwael. Rhannodd cyfranwyr enghreifftiau o broblemau gyda PPE yn cael ei wneud o ddeunyddiau anghyfforddus a gorfod defnyddio PPE mewn amgylcheddau poeth.
| “ | Roeddwn i'n casáu'r masgiau; Roeddwn i'n casáu'r gynau. Roeddech chi'n chwysu, roedd hi mor ddrwg. Y wardiau oedd, mae ein wardiau yn cael eu rheoleiddio gan generaduron stêm, y gwresogyddion, ac maent yn eu rhoi ymlaen yn yr haf a hynny i gyd. Roedden ni’n diferu o chwys gyda’r holl PPE yma ymlaen ac yn ceisio cael y cleifion i olchi a chael cawod, a doedd hynny ddim yn brofiad da, a dweud y gwir.”
- Cynorthwyydd gofal iechyd ysbyty |
Roedd barn gymysg ar yr hyfforddiant sydd ar gael ar gyfer defnyddio PPE. Disgrifiodd rhai cyfranwyr nad oedd PPE bob amser yn cael ei ddefnyddio’n gywir (ac felly’n llai effeithiol) oherwydd nad oedd staff wedi’u hyfforddi’n briodol. Roedd diffyg mynediad at hyfforddiant hefyd yn cyfrannu at bwysau staffio mewn lleoliadau gofal iechyd lle nad oedd staff yn gallu gweithio nes bod yr hyfforddiant wedi'i gwblhau. Rhoddodd y cyfranwyr enghreifftiau o'r rhai yr oedd angen yr hyfforddiant fwyaf arnynt oedd leiaf abl i gymryd amser i ffwrdd o ofal cleifion i'w gwblhau.
| “ | Roedd gennych sefyllfa lle roedd staff swyddfa, sy'n rhydd i fynd am yr hyfforddiant ar gyfer masgiau FFP3, i gyd wedi'u gosod. Gallent wisgo'r masgiau hyn yn ddiogel. Nid oedd y bobl ar lawr y siop yn yr Adran Damweiniau ac Achosion Brys yn gallu gadael. Yn gyfreithiol, nid oeddent yn cael gwisgo'r offer amddiffynnol yn swyddogol oherwydd nad oeddent wedi cael eu hyfforddi rhag ofn i ni gael ein heintio ac erlyn y sefydliad am beidio â'n hyfforddi'n iawn. ”
-Meddyg ysbyty |
| “ | Gwisgo PPE, a bod yn gwbl onest. Felly, un o'r heriau cychwynnol, rwy'n meddwl am y pandemig, oedd nad oeddem wedi cael unrhyw hyfforddiant i'w roi ymlaen. Roeddwn yn sicr wedi cael rhywfaint o hyfforddiant ar ryw adeg, ond roedd amser maith yn ôl. Ac, yn fy marn i, mae'n debyg nad oedd mwyafrif fy nghydweithwyr wedi cael unrhyw hyfforddiant ar wisgo siwtiau a masgiau lefel 3 yn gywir. Ac, fel y gwyddoch yn iawn yn ôl pob tebyg, y mater mwyaf, y pryder mwyaf wrth roi PPE ymlaen yw ei dynnu i ffwrdd yn y drefn gywir. ”
- Parafeddyg |
Stori JulieGweithiodd Julie fel meddyg yn ystod y pandemig mewn ysbytai a hosbisau. Roedd gwisgo PPE yn anodd iawn iddi, gan achosi adweithiau alergaidd ac anghysur corfforol. “Y peth mawr i mi gyda chyflwyno gwisgo masgiau wyneb a'r holl hylendid dwylo - rwy'n dioddef o lawer o alergeddau ac ecsema, a daeth i'r amlwg bod gen i alergedd i'r nicel, y metel yn y masgiau llawfeddygol, felly dwi' ch cael llawer o adweithiau wynebol a oedd yn boenus iawn. Y masgiau FFP3, doeddwn i ddim yn gallu gwisgo oherwydd roedd ganddyn nhw fetel i mewn hefyd. Mae gen i alergedd i latecs a'r ewyn, felly hyd yn oed wrth wisgo'r fisorau, yr ewyn ar ben y fisorau, byddwn yn dechrau mynd yn cosi iawn ac anghyfforddus.” Roedd PPE yn ei gwneud hi'n anodd iddi wneud ei gwaith yn iawn. Roedd hefyd yn lleihau ansawdd ei bywyd. Arweiniodd fflamychiadau ecsema difrifol at friwiau amrwd ac wylofain a chwsg gwael. Roedd hyn yn gwneud ymdopi â phwysau gwaith yn fwy heriol fyth. Yn y diwedd, canfu Julie na allai barhau i weithio yn yr ysbyty. “Treuliais oesoedd yn ceisio dod o hyd i ffyrdd y gallwn i wisgo PPE heb iddo fod yn niweidiol i mi fy hun, a daeth pwynt pan aeth yn rhy anodd mewn gwirionedd. Camais yn ôl o wasanaethu'r uned cleifion mewnol ac yn bennaf yn cwmpasu'r gymuned lle nad oedd angen i chi - nid oeddech yn ymweld â chleifion mor aml, felly nid oedd yr un dwyster wrth gadw at y PPE, ond wedyn roeddwn yn teimlo'n euog iawn am siomi cydweithwyr.” |
Cafodd rhai cyfranwyr brofiadau gwell o PPE, yn enwedig y rhai sy'n gweithio mewn lleoliadau gofal iechyd risg uwch. Er enghraifft, roedd un cyfrannwr a oedd yn gweithio yn ICU yn fwy cadarnhaol am ffit a chysur. Soniwyd am faint y profion ffit (proses o sicrhau bod PPE yn cael ei osod yn y ffordd gywir i atal heintiau rhag lledaenu a sicrhau diogelwch gweithwyr gofal iechyd proffesiynol) yr aethant drwyddynt i sicrhau bod eu masgiau'n eu hamddiffyn cymaint â phosibl. Dilynwyd hyn a'i ailadrodd yn achos newidiadau stoc.
| “ | Doedd gen i ddim problem, o gwbl. Ar y cychwyn cyntaf, cawsom rai problemau gyda’n masgiau cychwynnol yn unig, ond cafodd hynny ei ddatrys yn llythrennol o fewn wythnos neu ddwy, ac yna roedd gennym gyflenwad parhaus, felly ni chawsom erioed broblemau penodol. ”
– Gweithiwr gofal iechyd proffesiynol perthynol |
Effaith PPE ar ofal a thriniaeth cleifion
Roedd defnyddio PPE yn un o'r gwahaniaethau mwyaf amlwg mewn lleoliadau gofal iechyd o'i gymharu â chyn y pandemig. I rai cleifion, roedd croeso i weld gweithwyr gofal iechyd proffesiynol mewn PPE. Roeddent yn teimlo'n dawel eu meddwl ac wedi'u hamddiffyn yn well rhag risgiau Covid-19.
| “ | Roedden nhw [staff yr ysbyty] i gyd yn ofalus iawn [yn gwisgo PPE] ac yn sychu pethau, ac roeddwn i'n teimlo'n ddiogel. Roeddwn i’n teimlo’n gyfforddus iawn gyda’r gofal roedden nhw’n ei gymryd i ofalu amdanaf, fy amddiffyn i.”
- Claf ysbyty |
Ar y llaw arall, rhannodd rhai cleifion sut roedd gweld gweithwyr gofal iechyd proffesiynol mewn PPE yn peri gofid a hyd yn oed yn frawychus. Roedd hyn yn fwy o broblem ar ddechrau'r pandemig pan nad oedd cleifion yn gwybod beth i'w ddisgwyl, yn enwedig mewn ysbytai. I rai cyfranwyr, roedd gweld gweithwyr gofal iechyd proffesiynol mewn PPE am y tro cyntaf yn dod â realiti’r pandemig yn ôl.
| “ | Felly, yn bendant nid dyna oeddwn i wedi arfer ag ef mewn ysbyty, yn enwedig o ystyried fy mod wedi cael fy mabi yn yr ysbyty 3 mis cyn hynny, ac roedd yn brofiad hyfryd. Roedd yn frawychus iawn oherwydd nid ydych erioed wedi gweld ysbytai fel hynny. Rwy’n meddwl mai dyma’r pwynt lle’r oedd y PPE brawychus yn dod i mewn hefyd.”
- Claf ysbyty |
Roedd rhai cyfranwyr yn meddwl bod PPE yn creu rhwystrau ychwanegol rhwng gweithwyr gofal iechyd proffesiynol a chleifion, a bod hyn yn gwneud darparu gofal yn fwy heriol. Roedd masgiau'n cuddio mynegiant yr wyneb neu emosiynau, gan leihau cysylltiad personol. Roedd rhai cyfranwyr o’r farn bod hyn yn ychwanegu at bryder a oedd eisoes wedi cynyddu yn ystod camau cynnar y pandemig.
| “ | Fe wnaethon nhw ein tywys ni i gyd i mewn i un ystafell ac roedd pawb yn cerdded o gwmpas gyda masgiau wyneb…nid oedd yn teimlo fel amgylchedd gofal; roedd yn teimlo un cam ar wahân oherwydd bod y mwgwd, am fod mor fach, yn cuddio darn mor werthfawr o’ch wyneb, p’un a oeddech yn gwenu, p’un a oeddech yn ceisio cysuro rhywun neu beth bynnag.”
- Claf ysbyty |
Yn ogystal â lleihau cysylltiad personol, Roedd PPE yn gwneud cyfathrebu llafar rhwng gweithwyr gofal iechyd proffesiynol a chleifion yn fwy heriol. Roedd hon yn her arbennig i gleifion ag anghenion cyfathrebu ychwanegol, gan gynnwys d/Byddar a nam ar y clyw a rhai pobl awtistig sy'n dibynnu ar fynegiant wyneb i gynorthwyo cyfathrebu.
| “ | Yr elfen arall o wisgo'r PPE, oedd ei bod yn anodd iawn bryd hynny i ddarparu rhai o'n gwasanaethau, oherwydd rydym yn wasanaeth strôc. Felly, byddai gan rai o’n cleifion namau cyfathrebu ar ôl strôc, neu byddai pobl hŷn yn eithaf byddar, ac roeddent yn gweld hynny’n anodd iawn… yn enwedig os oeddent yn affasig (anhawster gydag iaith neu leferydd a achosir fel arfer gan niwed i’r ymennydd) ar ôl eu strôc, yna doedden nhw ddim wir yn deall beth roeddech chi'n ei ddweud, a doedden nhw ddim yn gallu gweld eich ymadroddion, a phethau felly."
– Gweithiwr gofal iechyd proffesiynol perthynol |
| “ | Cefais chwalfa nerfus hunanladdol […] Mae fy anabledd yn ei gwneud yn amhosibl i mi gyfathrebu oni bai fy mod yn gweld wynebau llawn. Rwy’n dal i deimlo’n drawmatig os gwelaf rywun mewn un [mwgwd].”
- Person awtistig |
Rhoddodd pobl a oedd yn f/fyddar neu â nam ar eu clyw lawer o enghreifftiau o ofyn i staff gofal iechyd dynnu masgiau er mwyn darllen gwefusau, ond gwrthodwyd hyn oherwydd pryderon ynghylch lledaenu Covid-19. Roedd hyn yn gadael y cleifion hyn mewn sefyllfaoedd anodd, yn cael trafferth deall yr hyn a ddywedwyd wrthynt.
| “ | Rydych chi'n dweud, 'Rwy'n fyddar,' ac maen nhw'n siarad â chi trwy fwgwd, a byddaf yn dweud, 'Rwy'n fyddar.' Maen nhw, fel, 'O, na, na, ni allaf dynnu fy mwgwd. Efallai y byddwch chi'n rhoi Covid-19 i mi.' Rwy'n debyg, 'Wel, wyddoch chi, byddaf yn sefyll draw fan hyn, rydych chi'n sefyll draw acw. Tynnwch eich mwgwd i lawr, byddaf fwy na 2 fetr i ffwrdd,' ac fe wrthodon nhw o hyd. Roedd hynny’n anodd iawn ac yna, yn llythrennol, ni allwch weld eu ceg na’u hwyneb, felly does gennych chi ddim gobaith o’u deall.”
– d/person Byddar |
Mewn sefyllfaoedd lle mae bywyd yn y fantol, roedd rhai cyfranwyr yn teimlo bod rhoi PPE llawn ymlaen yn golygu bod amser gwerthfawr yn cael ei golli. Roedd hyn yn golygu nad oedd cyfranwyr bob amser yn teimlo mai dilyn y canllawiau PPE oedd y peth gorau i'w wneud - neu ei fod bob amser yn gwneud synnwyr.
| “ | Roeddem hefyd ychydig yn amheus bod y canllawiau wedi newid o fasgiau FFP3 a phethau y byddech chi'n eu defnyddio ar gyfer clefyd aerosol canlyniad uchel [i fasgiau wyneb rheolaidd]. Fe gawson ni un penwythnos o ddefnyddio’r canllawiau hynny… [ac fel] pe bai trwy hud, o fewn tridiau, oedd, ‘O, jyst angen mwgwd wyneb,’ ac aethon ni i gyd, ‘O, wel, mae hynny’n ddiddorol,’ ond ni aeth ag ef.”
-Meddyg ysbyty |
Cyflwynodd PPE hefyd gyfyng-gyngor moesegol i weithwyr gofal iechyd proffesiynol. Er enghraifft, bu un cyfrannwr yn trafod gorfod dewis a ddylid dadebru claf Covid-19 heb PPE yn gyflym a chynyddu’r risg o ddod i gysylltiad â’r firws neu aros i ddadebru’r claf unwaith y byddai pawb yn gwisgo PPE.
Stori JacMae Jack yn gweithio fel llawfeddyg ymgynghorol, yn gofalu am gleifion GIG a phreifat. Yn ystod y pandemig, aeth un o'i gleifion i ataliad y galon. Arweiniodd greddf Jack ato i ddechrau dadebru'r claf, ond tynnodd ei gydweithwyr ef i ffwrdd oherwydd nad oedd ganddo'r math cywir o PPE ymlaen. “Dechreuais ei ddadebru a chefais fy nhynnu oddi arno oherwydd dywedodd pawb, 'Na, mae'n rhaid i chi roi eich PPE ymlaen.' A doeddwn i ddim ac roeddwn i newydd ei wneud mor reddfol ac yn awtomatig ac yna’r math o ofn llwyr wedyn.” Unwaith y daethpwyd â hyn i sylw Jack, roedd yn teimlo'n bryderus ac yn mynd i banig gan ei fod yn poeni ei fod wedi amlygu ei hun yn uniongyrchol i Covid-19. Roedd yn poeni am ei iechyd ei hun ond hefyd iechyd ei deulu, gan nad oedd am ddod â'r firws adref. Roedd Jack hefyd yn teimlo’n euog am yr angen i wisgo a thynnu PPE yn ddiogel mewn argyfwng, gan ei fod yn sylweddoli bod mwy o amser roedden nhw’n ei dreulio yn rhoi PPE ymlaen yn llai o amser i’r tîm geisio dadebru’r claf, a oedd yn golygu llai o siawns o oroesi. . “Roedd y wybodaeth bod yr amser y mae'n ei gymryd i chi wisgo a diffodd PPE yn ddiogel yn golygu nad oedd y dyn tlawd hwnnw'n cael ei ddadebru am gyfnod eithaf hir o amser tra roeddem ni i gyd yn rhoi ein PPE ymlaen. Rydych chi'n gwybod, a dim ond eich bod chi wir yn sownd rhwng craig a lle caled a'ch bod chi'n gwybod ie. Rwy’n meddwl na allwch chi byth ddal y realiti na fydd unrhyw berson normal byth yn deall, yn y ffordd neisaf bosibl, beth oedd yn ei olygu.” |
O ran gwisgo PPE eu hunain, roedd cleifion ac ymwelwyr fel arfer yn disgrifio gwisgo masgiau yn cael eu gorfodi'n llym yn ystod y pandemig, gydag ychydig eithriadau. Dywedodd rhai cyfranwyr fod yn rhaid iddynt wisgo PPE ychwanegol fel gynau, esgidiau uwch a menig.
Myfyriodd rhai cleifion ar yr heriau y daethant ar eu traws wrth wisgo mwgwd, yn enwedig yn wyneb gorfodi llym gan weithwyr gofal iechyd proffesiynol. Soniasant eu bod yn cael trafferth anadlu wrth eu gwisgo, a oedd yn achosi problemau i rai cyflyrau iechyd. Dywedodd y cyfranwyr hyn eu bod yn teimlo dan bwysau i wisgo mwgwd yn gyson, yn enwedig gan aelodau staff.
| “ | Oedd, roedd yn rhaid i mi wisgo fy mwgwd … ond roeddwn yng nghanol bod yn sâl, yn yr ysbyty, fy hun, pan nad oedd mwgwd yn flaenoriaeth. Ond fe fydden nhw, bob tro maen nhw'n dod i mewn, 'Rhowch eich mwgwd yn ôl ymlaen.' Roeddwn i'n teimlo'n farnedig iawn oherwydd roeddwn i'n ceisio mor galed i wisgo mwgwd, ac yna allwn i ddim."
- Claf ysbyty |
Roedd rhai enghreifftiau o bobl angen eu masgiau eu hunain er mwyn ymweld ag anwyliaid mewn ysbytai. Ar adegau, nid oedd gan rai ysbytai PPE ar gael i ymwelwyr.
| “ | Roedd gen i PPE ar gyfer fy ngwaith bob dydd yn fy mag gwaith ... pan gyrhaeddais y ward, roedden nhw mor falch bod gen i PPE gan eu bod nhw newydd ddod i ben yn llwyr. Roeddent i gyd yn ailddefnyddio PPE a dywedasant y byddai wedi gorfod fy nhroi i ffwrdd pe na bai gennyf rai. Pe na bawn wedi troi i fyny yn gwisgo PPE ni fyddai wedi bod yn bosibl i unrhyw un ofalu am Nan gan nad oedd yr ysbyty ar ôl o gwbl.”
- Gweithiwr gofal iechyd proffesiynol |
Dysgu ar gyfer y dyfodol: PPERoedd yr angen i gael digon o PPE o ansawdd da ar gael ar gyfer pandemigau yn y dyfodol yn adlewyrchiad cyffredin a rennir gan lawer o gyfranwyr. Clywsom fod problemau gyda PPE yn golygu nad oedd gan lawer o weithwyr gofal iechyd proffesiynol yr hyn yr oedd angen iddynt gael ei amddiffyn, gan eu gadael yn teimlo'n ofnus ac yn cael eu tanbrisio. Roedd hyn yn rhywbeth y dywedodd llawer o gleifion a gofalwyr fod angen dysgu ohono hefyd. Roedd cyfranwyr eisiau gwell systemau ar waith i gryfhau cadwyni cyflenwi PPE a sicrhau bod pentyrrau stoc yn eu lle ar gyfer pandemigau yn y dyfodol. Roeddent hefyd eisiau mynediad tecach at PPE ar draws gofal iechyd, ac nid yn unig ar gyfer staff mewn ysbytai ar reng flaen yr ymateb. “Dim ond cael cyflenwadau brys, fel PPE, pethau felly. Os oes gennym ni bandemig arall, dylai fod gan arweinwyr ledled y byd ryw fath o system cynllunio at argyfwng ar waith ar gyfer y pethau hyn.” – Cefnogaeth rheoli systemau gofal iechyd “Rwy’n meddwl, wrth weithio ym maes gofal iechyd, ein bod wedi tybio’n anghywir bod darpariaeth eisoes wedi’i gwneud gyda phentyrrau o PPE pe bai pandemig yn taro. Methodd y cyflymder yr oeddem yn gofyn am y dosbarthiad hwn dro ar ôl tro ac roedd y cynhyrchion eu hunain yn aml o ansawdd annigonol. Hoffwn feddwl bod profion a chaffaeliad mwy trwyadl ar gyfer cyflenwyr priodol bellach ar waith a bod logisteg cyflenwad/galw wedi’i gynnwys pe bai eu hangen arnom eto.” – Cyfrannwr Mae Every Story Matters Roedd llawer o’r rhai sy’n gweithio ym maes gofal iechyd eisiau gweld canllawiau cliriach ar ddefnyddio PPE ar gyfer pandemigau yn y dyfodol, gan wneud yn siŵr bod hwn wedi’i deilwra i leoliadau penodol. “Roeddech chi'n cael cymaint o bolisïau a chanllawiau allan a oedd yn gwrth-ddweud ei gilydd. Felly dywedwyd wrthym ar un adeg nad oedd yn rhaid i ni wisgo masgiau y tu allan i'r gwaith, ond yna dywedwyd wrthym fod yn rhaid i ni eu gwisgo o hyd y tu mewn i'r gwaith. Mae fel ein bod ni'n deall ein bod ni mewn ysbyty a bod pobl ar wardiau yn dal i orfod gwisgo masgiau ac mae hynny'n iawn, ond os ydyn ni mewn swyddfa ... wnaethon nhw ddim nodi pa feysydd yn union.” – Cefnogaeth rheoli systemau gofal iechyd |
Profiadau o brofion Covid-19 ymhlith gweithwyr gofal iechyd proffesiynol
Mae profion Covid-19 yn cyfeirio at argaeledd a defnydd profion adwaith cadwyn polymeras (PCR) a phrofion llif ochrol.
I lawer o’r staff gofal iechyd y clywsom ganddynt, nid oedd profi yn rhan bwysig o'u profiad. Yn hytrach, roeddent yn tueddu i ganolbwyntio ar newidiadau eraill i'r ffordd yr oeddent yn gweithio ac yn darparu gofal i gleifion.
Roedd gan lawer o gyfranwyr a oedd yn gweithio mewn lleoliadau gofal iechyd fynediad da at brofion Covid-19, ond dywedodd rhai nad oedd ganddynt ddigon, yn enwedig yn gynnar yn y pandemig. Roedd rhai staff rhwystredig oherwydd y diffyg profi cynnar hwn, neu gefnogaeth gyfyngedig gan reolwyr ynghylch profi. Er enghraifft, roedd un cyfrannwr yn ei chael yn anodd cael mynediad at brofion yn lleol. Roeddent hefyd yn teimlo nad oedd rheolwyr yn annog staff i brofi oherwydd prinder staff acíwt.
| “ | Yn bendant nid oedd yn cael ei annog cystal oherwydd roedd neges o, 'Nid ydym am i chi fod yn sâl.' Yn bendant roedd llawer o bwysau i weithio…profais yn bositif, ac rwy'n cofio dweud wrth yr arweinydd tîm ar y pryd ac roedd hi'n ffwndro. Agorodd hi’r drws, dywedais wrthi, ac fe slamiodd y drws … roedd hi’n grac bod rhywun arall yn sâl.”
– Nyrs Damweiniau ac Achosion Brys |
Dywedodd rhai cyfranwyr sy’n gweithio ym maes gofal sylfaenol ei bod yn heriol cael mynediad at brofion PCR ar ddechrau’r pandemig. Roeddent yn teimlo y dylai'r rhai sy'n gweithio mewn practis cyffredinol fod wedi cael mynediad i brofion ar gyfer achosion asymptomatig yn gynt. Fodd bynnag, wrth i'r pandemig fynd rhagddo, gwellodd mynediad at brofion - roedd hyn yn cynnwys profion PCR a phrofion llif ochrol.
| “ | Cawsom fynediad atynt, felly roedd hynny'n eithaf calonogol. Nid oedd byth unrhyw amheuaeth a fyddem yn gallu profi ein staff i weld a oeddent yn ffit i weithio.”
– rheolwr practis meddyg teulu |
Wrth i brofion Covid-19 ddod yn fwy ar gael, gallu profi gwneud i rai aelodau o staff deimlo'n fwy cyfforddus a hyderus ynghylch risgiau haint. Roeddent yn meddwl bod hyn yn lleihau'r siawns eu bod yn gweithio'n agos gyda rhywun a allai drosglwyddo Covid-19. Roedd hyn yn arbennig o bwysig i rai cyfranwyr mewn lleoliadau prysur, gan gynnwys meddygaeth frys.
| “ | Rhoddodd yr hyder i ni wybod bod y rhai sy'n sefyll gyda ni yn annhebygol o fod â Covid-19. Roeddem yn dal i gadw at fygydau wyneb ac oherwydd yr union ddiwrnod hwn, wrth gwrs, ac felly rwy’n hyderus bod y staff yn cymryd y camau angenrheidiol. Ond roedd argaeledd prawf llif ochrol yn gam da i'r cyfeiriad hwnnw. ”
- Meddyg D&A |
Roedd gan y cyfranwyr farn gymysg ar eglurder y canllawiau a’r gofynion ar gyfer profi. Dywedodd rhai gweithwyr gofal iechyd proffesiynol eu bod yn derbyn cyfathrebiadau rheolaidd a'u bod yn ei chael yn hawdd dilyn y canllawiau yn eu lleoliadau. Roedd eraill yn gweld canllawiau yn fwy amwys ac yn agored i'w dehongli.
| “ | Rwy'n cofio pan ddaeth y profion i mewn ac a dweud y gwir, roedd hynny'n eithaf lan yn yr awyr oherwydd, wyddoch chi, rydym wedi cael y llifau ochrol ac roedd rhai pobl yn dweud, 'Mae'n rhaid i chi eu gwneud yn wythnosol ac adrodd am y prawf,' ac roedd rhai pobl yn dweud ei fod os ydych chi'n symptomatig… Ac yna fe wnes i lifau ochrol oddi ar fy nghefn fy hun i mi fy hun a fy nheulu, yn amlwg oherwydd bod gennyf ddyletswydd gofal, ond ni ofynnodd neb erioed i mi, yn fy ngwaith, os oeddwn yn gwneud nhw neu eu canlyniad.”
– rheolwr practis meddyg teulu |
Clywsom am wahaniaethau o ran pa mor aml yr oedd angen cynnal profion mewn gwahanol leoliadau ar draws gofal iechyd. Er ei bod yn ofynnol i rai cyfranwyr brofi yn rheolaidd (ee wythnosol, neu cyn pob sifft), i eraill roedd yn fwy ad hoc.
Rhannodd cyfranwyr a oedd yn gweithio ym maes gofal iechyd hefyd sut y newidiodd gofynion profi dros amser. Roedd hyn yn cynnwys symud o fod angen profion dim ond os oedd gan staff symptomau i brofi'n rheolaidd waeth beth fo'r symptomau. Dywedasant fod y newid hwn wedi digwydd pan ddaeth profion llif ochrol gartref ar gael yn haws.
| “ | Hwn oedd y cam hwnnw o fynd o ddim profion ar gael i rai profion sydd ar gael - wel, i brofion cyfyngedig sydd ar gael, pwy sy'n mynd i gael hyn, hyd at beth ydych chi'n mynd i fod yn ei wneud? ”
– Staff gofal lliniarol |
Roedd cyfranwyr sy’n gweithio mewn lleoliadau gofal iechyd yn cofio bod canllawiau hunan-ynysu yn arbennig o llym ar ddechrau’r pandemig. Fe wnaethant rannu enghreifftiau o fod angen hunan-ynysu wrth aros am ganlyniadau profion a hefyd gorfod hunan-ynysu os oedd ganddynt gysylltiad â rhywun sydd wedi'i heintio â Covid-19.
Arweiniodd ofn gorfod hunan-ynysu i rai cyfranwyr a oedd yn gweithio ym maes gofal iechyd i beidio â chydymffurfio â chanllawiau profi, yn enwedig os nad oeddent yn profi unrhyw symptomau Covid-19.
| “ | Efallai na wnes i mor aml ag y dylwn fod wedi'i wneud. Un o fy mhryderon, ac mae hyn yn swnio'n hunanol iawn, a gobeithio nad yw hyn yn dod ar ei draws yn anghywir, [oedd hynny] doeddwn i ddim eisiau gwybod fy mod wedi ei gael, oherwydd mae'n debyg nad oeddwn i eisiau colli gwaith. . Pe bawn i wedi teimlo’n arw neu’n crap ar unrhyw adeg, ie, byddwn wedi ei gymryd a heb fynd i mewn pe bawn i’n bositif.”
- Porthor ysbyty |
7. Profiadau o ganllawiau'r llywodraeth a'r sector gofal iechyd |
 |
Mae'r bennod hon yn amlinellu safbwyntiau ar ganllawiau drwy gydol y pandemig mewn lleoliadau gofal iechyd. Mae hyn yn cynnwys sut y cawsant eu cyfleu i weithwyr gofal iechyd proffesiynol, a sut y cawsant eu gweithredu ganddynt, a'r heriau ymarferol a moesegol o weithio o fewn y canllawiau. Mae hefyd yn ymdrin â safbwyntiau cleifion.
Cyfathrebu a gweithredu canllawiau Covid-19
Dywedodd gweithwyr gofal iechyd proffesiynol wrthym eu bod wedi derbyn gwybodaeth gyffredinol am reolau a rheoliadau Covid-19 o'r newyddion a'r cyfryngau, yn aml ar yr un pryd ag aelodau'r cyhoedd.
Roedd y cyfranwyr hyn yn aml yn teimlo'n bryderus ynghylch y cyfyngiadau a'r canllawiau, ac yn teimlo eu bod yn 'mynd i'r anhysbys'. Clywsant am reolau a pholisïau mwy penodol yn ymwneud â’u rolau proffesiynol trwy e-byst a sesiynau briffio gydag uwch arweinwyr yn y gwaith.
Roedd grwpiau WhatsApp yn ffordd gyffredin o rannu gwybodaeth am bolisïau penodol fel gweithdrefnau cwarantîn, polisïau salwch staff, newidiadau i ofal cleifion, a rheolau a phrosesau PPE.
| “ | Polisïau cenedlaethol, mae'r mathau hynny o bethau yn amlwg o'r cyfryngau a sianeli newyddion a beth sydd gennych chi. O fewn yr ymddiriedolaeth, defnyddiwyd gwahanol grwpiau WhatsApp fel ffordd gyflym o gylchredeg polisi, newidiadau deddfwriaethol a wnaed o fewn y sefydliad ymhlith amrywiol bwyllgorau ac uwch reolwyr a swyddogion gweithredol.”
-Meddyg ysbyty |
| “ | Do, cawsom ddiweddariadau rheolaidd. Felly, cafodd y Prif Weithredwr ddiweddariadau rheolaidd. Roedd gennym ni gyfathrebiadau e-bost hefyd, felly cyfathrebiadau ysgrifenedig yn ogystal â chyfathrebu geiriol, ac yna hidlo gwybodaeth o'r math hwn hefyd. Dydw i ddim yn meddwl bod pwynt lle nad oeddwn yn gwybod beth oedd yn digwydd. Dw i’n meddwl ein bod ni wastad yn ymwybodol.”
- Gwyddonydd clinigol |
Myfyriodd llawer o weithwyr gofal iechyd proffesiynol ar sut roedd y wybodaeth yn llethol yn ystod y pandemig a faint o faich oedd cadw i fyny â'r rheolau, rheoliadau a chanllawiau newidiol.
| “ | Byddwn yn dweud bod cyfathrebu wedi cynyddu'n aruthrol. Roedd presenoldeb uwch o uwch swyddogion gweithredol a rheolwyr. Roedd strwythurau lle byddai cyfarfodydd boreol, ac maent yn dal i barhau yn awr, o'm dealltwriaeth i. Bu manteision o’r ochr gyfathrebu honno, ond roedd mwy yn cael gwybod beth i’w wneud yn hytrach na thrafod beth i’w wneud.”
– Cefnogaeth rheoli systemau gofal iechyd |
Fodd bynnag, roedd rhai cyfranwyr sy'n gweithio mewn lleoliadau gofal iechyd yn teimlo 'allan o'r ddolen', gan nad oedd eu sefydliad yn cyfathrebu â nhw'n rheolaidd. Roedd hyn yn gwneud i'r gweithwyr gofal iechyd proffesiynol hyn deimlo eu bod wedi'u hallgáu ac yn aneglur ynghylch y ffyrdd diweddaraf o weithio.
Roedd cyfranwyr a oedd yn gweithio ym maes gofal sylfaenol yn tueddu i gael trafodaethau am ganllawiau gyda chydweithwyr. Dywedasant fod newidiadau yn gyfrifoldeb i bractisau meddygon teulu unigol, a bod ganddynt rywfaint o hyblygrwydd i deilwra'r hyn a wnânt. Rhoddodd rhai o’r cyfranwyr hyn enghreifftiau o wneud penderfyniadau drwy drafod pethau o fewn practis a thrwy siarad â meddygfeydd eraill.
| “ | Fe'i cyfathrebir mewn gwirionedd ar lafar gwlad am lawer o bethau. Byddai ein hardal leol wedi cael grŵp meddygon teulu, a byddent wedi bod ar weminarau ac yn trafod y ffordd orau o symud ymlaen. Roedd yn weddill i raddau helaeth iddynt eu hunain sut yr oeddent am symud ymlaen â'u harferion. Yna efallai y byddai fy meddygon teulu wedi dod yn ôl o'r cyfarfodydd a dweud, 'Edrychwch, mae pawb arall yn cael ystafell wedi'i neilltuo, felly fe wnawn ni hynny hefyd.' Felly, nid oedd fel petai yna lawer o gyngor a oedd i’w weld yn dod gan y bwrdd iechyd ar gyfer yr agweddau ymarferol o ddydd i ddydd.”
– rheolwr practis meddyg teulu |
Dywedodd cyfranwyr sy'n gweithio mewn ysbytai fod newidiadau i ganllawiau yn aml yn cael eu cyfathrebu trwy e-bost, gyda system fwy o'r brig i'r bôn. Dywedasant fod rhywfaint o wybodaeth yn cael ei rhannu trwy gydweithwyr.
| “ | Roedd y gwasanaethau ysbyty roeddech chi bob amser yn clywed am yr hyn oedd yn digwydd trwy e-bost, ond meddygon teulu a stwff ei fod yn ail law a hyd yn oed weithiau rhywfaint o bethau ysbyty yn newyddion ail law hefyd. Felly oedd, roedd yn anodd ceisio cadw i fyny â’r newidiadau, beth oedd yn digwydd, pa bolisïau oedd wedi’u rhoi ar waith i helpu mwy o bobl, offer PPE, yr holl newidiadau a aeth ymlaen yno hefyd.”
- Gwyddonydd clinigol |
Myfyriodd llawer o weithwyr gofal iechyd proffesiynol ar ba mor gyflym oedd y broses o wneud penderfyniadau. Roedd ymdeimlad o angen ymateb i argyfwng, a oedd yn wahanol iawn i sut mae newidiadau fel arfer yn digwydd mewn gofal iechyd.
I rai cyfranwyr, roedd yr ymdeimlad newydd hwn o frys a chyflymder yn gadarnhaol. Roeddent yn tueddu i fod yn rhai a ddywedodd eu bod yn flaenorol yn gweld gweithio yn y system gofal iechyd yn araf ac yn rhwystredig. Fodd bynnag, yn ystod y pandemig diflannodd llawer o'r rhwystrau arferol i newid a chanfu cyfranwyr ei bod yn bosibl gwneud pethau'n wahanol.
| “ | Byddwn yn dweud am y tro cyntaf erioed, symudodd pethau'n gyflym iawn yn y GIG. Roedd y gallu hwn i wneud penderfyniadau ac i wneud newidiadau yn gyflym iawn, ond nid yw hynny'n arfer arferol yn y GIG. Mae pethau'n aml, wyddoch chi, mae yna lawer o fiwrocratiaeth, am resymau, ac mae llawer o haenau y mae'n rhaid i chi fynd drwyddynt. Mae pethau’n cymryd llawer o amser, ond yn y pandemig roedd y gallu i wneud newid yn gyflym yn anghredadwy.”
– cymorth rheolaethol y GIG |
Dywedodd llawer o gyfranwyr wrthym ei bod yn heriol rhoi canllawiau ar waith yn gyflym. Roedd gweithwyr gofal iechyd proffesiynol a rheolwyr yn rhannu’r cyflymder yr oedd yn rhaid iddynt ystyried gwahanol safbwyntiau a’r effaith bosibl ar wahanol wasanaethau a’u cleifion.
Rhoddodd rhai cyfranwyr sy’n gweithio mewn lleoliadau gofal iechyd enghreifftiau o orfod ystyried sut roedd eu cydweithwyr yn teimlo am eu penderfyniadau. Disgrifiodd llawer o gyfranwyr ofn a phryder am Covid-19, a gwnaeth hyn bobl sy'n gweithio ym maes gofal iechyd yn ofalus iawn ynghylch y risgiau. Yn aml roedd safbwyntiau gwahanol ar y ffordd orau o roi canllawiau a pholisïau ar waith.
| “ | Heriol, oherwydd nid oedd gan bawb yr un farn. Yn ystod y pandemig, byddwn yn dweud bod delio â gwahanol lefelau o bryder a phryder gan wahanol grwpiau yn her enfawr. Mae gennych chi rai pobl sy'n hollol iawn ac yn ymdopi'n dda iawn, gadewch i ni gario ymlaen, i bobl na allent ymdopi mewn gwirionedd, ond i gyd yn gorfod bod ar yr un daith. Rwy’n meddwl bod ychydig o her wrth gadw popeth i fynd, ac roedd hynny’n anodd.”
– Cefnogaeth rheoli systemau gofal iechyd |
Newidiadau i ganllawiau Covid-19
Clywsom sut mae newidiadau i ganllawiau Covid-19 wedi creu dryswch ymhlith gweithwyr gofal iechyd proffesiynol. Roedd llawer o gyfranwyr yn ei chael hi’n anodd ymdopi â pha mor aml roedd canllawiau’n newid, a pha mor anghyson yr oedd yn ymddangos. Roedd hyn yn bryder cyffredin ar draws gwahanol leoliadau gofal iechyd.
Rhoddodd y cyfranwyr enghreifftiau o ganllawiau a fyddai gwrth-ddweud canllawiau blaenorol, ac roedd hyn yn aml yn heriol ar gyfer y rhai a oedd yn ceisio gwneud ac ymgorffori newidiadau mewn gwasanaethau. Roedd rhai cyfranwyr yn teimlo bod hyn yn ychwanegu at ymdeimlad o anhrefn ac ansicrwydd ar draws y system gofal iechyd. Roeddent yn meddwl bod hyn yn lleihau hyder yn y sail ar gyfer y rheolau ac wedi arwain at rywfaint o rwystredigaeth wrth i'r pandemig fynd rhagddo.
| “ | Roedd yn anhrefnus iawn o ran rheolau'n newid drwy'r amser a'ch sylfaen wybodaeth yn dod o'r newyddion yn hytrach na'r canllawiau safonol y byddech yn eu disgwyl gan werslyfrau. Ac yn amlwg, nid yw wedi'i ysgrifennu eto. ”
- Nyrs ysbyty |
| “ | Roedd hi fel nad oeddech chi'n gwybod pa ddiweddariad yr oeddech chi'n ei ddarllen hanner yr amser, neu daeth y llythyrau y byddai'n rhaid i chi gysylltu â chleifion agored i niwed neu ba bynnag grŵp. Byddech chi'n meddwl, wel, wn i ddim. Dydw i ddim hyd yn oed yn gwybod ble i ddechrau gyda hyn, ac yna mae cymaint o systemau clinigol gwahanol. Nid oedd y canllawiau hyd yn oed yn glir bryd hynny, felly roedd yn ddryslyd, nid oedd yn glir.”
– rheolwr practis meddyg teulu |
Roedd rhai cyfranwyr a oedd yn gweithio sifftiau gwahanol, neu ar benwythnosau, yn rhannu enghreifftiau o ddod yn ôl i’r gwaith i ganfod bod y canllawiau a’r protocolau wedi newid. Roedd hyn yn cynnwys canllawiau ar wisgo PPE, trosglwyddo cleifion, a gweithdrefnau clinigol.
| “ | Roeddwn i’n gallu troi i fyny un penwythnos ac roedd yr holl weithdrefnau a oedd ar waith yr wythnos flaenorol i gyd wedi newid yn llwyr, a’r wythnos ar ôl i mi ddod yn ôl, roedden nhw i gyd wedi newid yn llwyr eto.”
- Nyrs ysbyty |
| “ | Roedd newid pethau bob dydd yn ymwneud yn fwy â sut roedd Covid-19 yn cael ei reoli. Sut dylech chi weld eich cleifion. A ddylech chi gynnig wyneb yn wyneb? A ddylech chi fod yn gwisgo mwgwd ar gyfer rhai cleifion? A allech chi fod yn gwneud gweithdrefnau cynhyrchu aerosol yn ymarferol pan na allwch chi awyru ystafell? Pethau felly.”
– nyrs meddyg teulu |
Mae'r straeon a rannwyd gyda ni yn amlygu rhai tensiynau ac anghytundebau ymhlith gweithwyr gofal iechyd proffesiynol oherwydd heriau gweithredu rheolau. Roedd y rhain yn aml rhwng y rhai sy'n gweithio'n uniongyrchol gyda chleifion a'r rhai mewn rolau rheoli neu uwch arweinyddiaeth. Er enghraifft, roedd rhai cyfranwyr yn meddwl bod uwch arweinwyr yn aml yn aros am arweiniad gan y llywodraeth ar beth i'w wneud yn hytrach na chymryd camau rhagweithiol.
| “ | Roedd yn teimlo fel bod uwch arweinwyr yr ysbyty yn aros am gyfarwyddiadau a bod yr ysbytai a wnaeth ddefnyddio eu menter yn well ac a oedd yn annibynnol ac yn meddwl, 'Beth yw'r peth gorau i'w wneud?'”
-Meddyg ysbyty |
Ar y llaw arall, roedd enghreifftiau hefyd o weithwyr gofal iechyd proffesiynol yn cymryd yr awenau heb ymgynghori ag eraill ac yn wynebu gwthio'n ôl ar eu penderfyniadau.
| “ | Fe wnaethom benderfynu'n lleol, dyma sut y byddwn yn staffio ar gyfer y don gyntaf, dyma sut y byddwn yn cynyddu, dyma sut y byddwn yn lleihau. Ac yna, tua 6 mis yn ddiweddarach, daeth, 'Dyma beth wnaethom ni ar gyfer hyn, sut y byddwn yn ei wneud eto?' Ac ymateb y bwrdd oedd, 'Wel, wnaethon ni ddim gofyn i chi wneud hynny.'”
- Nyrs ysbyty |
Teimlai gweithwyr gofal iechyd proffesiynol eraill fod cydweithwyr yn defnyddio'r canllawiau a'r rheoliadau er eu lles eu hunain. Soniodd y cyfranwyr hyn am enghreifftiau o gydweithwyr yn cymryd amser i ffwrdd pan fyddant mewn cysylltiad agos â Covid-19 yn rhy aml neu’n ceisio bod ar ffyrlo. Creodd hyn densiynau mewn timau a sefydliadau, gan gynnwys rhwng y rhai sy'n darparu gofal uniongyrchol a rheolwyr neu arweinwyr tîm, a rhwng y rhai sy'n gweithio wyneb yn wyneb â chleifion a'r rhai sy'n gweithio o bell.
| “ | Dehonglodd rhai arbenigeddau eu canllawiau cenedlaethol i weddu iddynt … yn enwedig gyda rhai gweithdrefnau tebyg iawn, un grŵp yn hapus i wneud hynny, brwydro ymlaen yr holl ffordd drwodd, grŵp arall yn anhapus iawn, gwrthododd ei wneud.”
-Meddyg ysbyty |
| “ | I mi fel prif gaplan, mae'n debyg nad oeddwn i ffwrdd unrhyw bryd, ac efallai bod hynny'n rhwystredigaeth oherwydd pan oedd llawer o bobl yn gallu gweithio gartref ... tra bod rhai ohonom yn dod i'r gwaith fel arfer bob dydd , ac yn dal i fod ar gael bob dydd.”
- Caplan yr ysbyty |
Dywedodd rhai cyfranwyr eu bod cwestiynodd yn gynyddol ganllawiau Covid-19 a sut roedd yn berthnasol mewn lleoliadau gofal iechyd yn ddiweddarach yn y pandemig. Er enghraifft, roedd rhai o'r pryderon hyn yn canolbwyntio ar a oedd y canllawiau'n seiliedig ar dystiolaeth.
| “ | Adwaith iawn ac roedd yn dibynnu ar farn rhywun yn hytrach na thystiolaeth, dwi'n meddwl. Roedd yn dibynnu ar yr hyn yr oedd y cynlluniwr strategol yn ei feddwl y dylai ddigwydd, yn hytrach na thystiolaeth o’r hyn sy’n mynd i weithio i hyn.”
- Meddyg Teulu |
Er enghraifft, awgrymodd un cyfrannwr mai dim ond er mwyn cynyddu argaeledd y gweithlu gofal iechyd sydd ar gael, a hynny drwy leihau nifer y dyddiau yr oedd yn rhaid i weithwyr gofal iechyd proffesiynol eu hynysu, y gwnaed newid ym mholisi ynysu Covid-19.
| “ | O'm safbwynt i, 'A yw'n newid oherwydd bod y wyddoniaeth yn newid ac mae wedi'i brofi'n wyddonol mai dyma'r dewis gorau, neu a yw'r penderfyniad hwn yn cael ei wneud oherwydd bod 50,000 o swyddi gwag yn yr ysbyty ar hyn o bryd?' Roedden ni’n teimlo, yn bendant i’r casgenni hynny ar y rheng flaen ei fod yn cael ei newid dim ond i gael casgenni yn ôl i’r gwaith.”
– Nyrs a oedd yn gweithio mewn ysbyty Nightingale |
Dilyn arweiniad a chyfyng-gyngor moesegol
Dywedodd llawer o weithwyr gofal iechyd proffesiynol wrthym am gyfyng-gyngor moesegol anodd yr oeddent yn ei wynebu ynghylch canllawiau Covid-19. Roedd y cyfyng-gyngor hyn yn aml yn benodol i’w profiad unigol, ond roedd rhai themâu cyffredin ar draws y straeon a rannwyd gyda ni.
Er enghraifft, dywedodd rhai gweithwyr gofal iechyd proffesiynol nad oeddent yn dilyn canllawiau fel y gallent ddangos mwy o dosturi tuag at gleifion, teuluoedd a chydweithwyr. Roeddent yn aml yn teimlo dyletswydd i ddarparu gofal a oedd yn ddynol ac yn dosturiol, ac roeddent yn teimlo gwrthdaro ynghylch cydbwyso hyn â dilyn y canllawiau yn gaeth.
Rhannodd un cyfrannwr sut na wnaethant hwy a’u cydweithwyr ddilyn canllawiau swyddogol, gan adael i gleifion sy’n marw aros yn yr adran achosion brys yn hirach fel y gallai eu hanwyliaid ffarwelio.
| “ | Nid oeddent yn anfon y cleifion i'r ward. Gallant aros yma gyda'u teulu a marw yn yr adran achosion brys a gall eu teulu aros gyda nhw heb sôn am y pedair awr. Mae hynny'n digwydd.' Ac rwy'n credu bod y nyrs â gofal wedi dweud y gwir.”
– Nyrs Damweiniau ac Achosion Brys |
Soniodd un arall sut y daeth galwad o gartref gofal i mewn yn gofyn am anfon ambiwlansys i fynd â chleifion oedrannus sy’n marw i’r ysbyty. Fodd bynnag, nid oedd cludiant i'r ysbyty mewn ambiwlans yn unol â phrotocolau yn ystod y cyfnod hwnnw. Y cyfrannwr, gyda chytundeb staff yr ambiwlans, a ddarparodd yr ambiwlans.
Disgrifiodd rhai gweithwyr gofal iechyd proffesiynol eraill hefyd beidio â dilyn canllawiau PPE wrth ofalu am gleifion. I'r cyfranwyr hyn, roedd rhai o'r canllawiau yn cyfyngu ar y math a lefel y gofal y gallent ei ddarparu, a oedd yn anghywir yn eu barn nhw. Disgrifiodd un cyfrannwr ddewis peidio â gwisgo'r holl PPE gofynnol, gyda chaniatâd y claf, wrth drin merched sy'n cael genedigaethau cymhleth. Maent yn gadael i'r cleifion ddewis a oeddent am i staff dynnu eu PPE neu ei gadw ymlaen. Roeddent yn cynnig y dewis i beidio â gwisgo PPE llawn i gael gwared ar y rhwystr a grëwyd rhwng cleifion ac ymarferwyr gofal iechyd a chynyddu cysylltiad dynol.
| “ | Y peth cyntaf a wnes i, byddwn yn dweud wrth y fenyw, 'Rwy'n anghyfforddus iawn yn cael y sgwrs hon am yr hyn yr ydych yn mynd drwyddo o ran gwisgo mwgwd a methu â chyffwrdd â chi.' Felly, y peth cyntaf a wnaethom, yn aml iawn, oedd tynnu ein masgiau ac anwybyddu'r cyfyngiadau oherwydd roedd yn ymddangos bod cyswllt dynol pan fydd rhywun yn mynd trwy golled a newid eithafol yn trechu'r rheolau. Dyna'r math o faes rwy'n arbenigo ynddo, genedigaeth gynamserol iawn a babanod ag annormaleddau. Yn amlwg fe wnaethon ni roi’r dewis i fenywod a’u teuluoedd… ni allaf feddwl am achos lle nad oedd yn well ganddyn nhw gael rhyngweithio arferol a chymryd pa bynnag risg oedd yna.”
- Nyrs ysbyty |
Canfyddiadau cleifion o reolau a rheoliadau mewn lleoliadau gofal iechyd
Roedd cyfranwyr yn aml yn canolbwyntio ar ysbytai wrth drafod rheoliadau Covid-19. Ar gyfer ysbytai, roedd dryswch ymhlith llawer o gleifion ynghylch polisïau ymwelwyr, gofynion PPE, a phrotocolau profi. Achosodd y dryswch hwn ansicrwydd a phryder i lawer o gleifion ysbyty.
Roedd cleifion yn aml yn sôn am “sïon” a glywsant am reolau a rheoliadau. Er enghraifft, roedd un cyfrannwr yn meddwl bod gwisgo mwgwd yn orfodol, dim ond i ddarganfod nad oedd nifer sylweddol o gleifion eraill yn eu gwisgo. Daeth un arall i fyny yn disgwyl cael ei brofi am Covid-19 ar ôl cyrraedd, dim ond i ddarganfod nad oedd profion yn cael eu cynnal fel mater o drefn. Ychwanegodd hyn at straen yn ystod cyfnod a oedd eisoes yn heriol.
| “ | Roeddem hefyd yn siomedig iawn i ddarganfod, trwy'r cyfryngau, bod rhai ymddiriedolaethau ysbytai yn caniatáu ymweliadau â chleifion a oedd ar wardiau Covid-19, cyn belled â bod PPE priodol yn cael ei wisgo. Gofynnais yn daer am yr un peth, i weld fy mam ond gwrthodwyd y fraint yn bendant. Ni fyddai eu hymddiriedaeth yn caniatáu hynny. Doedd neb yn cael ei gweld hi.”
- Aelod o'r teulu mewn profedigaeth |
| “ | Os oeddech chi'n aros yno, doedden nhw ddim yn disgwyl i'r cleifion eistedd yn y gwelyau, 24 awr, cysgu gyda masgiau ymlaen, blah, blah, blah felly unwaith roeddech chi i fyny i'r ward, roeddech chi'n cael tynnu'r mwgwd i ffwrdd. . Ond roedd yn rhaid i chi wisgo un - roedd mor anghyson.; roedd fel bod un person wedi dweud hyn wrthych, roedd un person wedi dweud hynny wrthych. Yna roedd yn rhaid i chi fath o, wn i ddim, gobeithio am y gorau eich bod chi'n gwneud y peth iawn."
– Menyw a ddefnyddiodd wasanaethau mamolaeth |
Straeon gan bobl ag anabledd dysguYn y digwyddiadau gwrando gyda phobl ag anabledd dysgu, dywedasant wrthym ei bod yn anodd addasu i'r byd newidiol yn ystod y pandemig. “Roedd yn rhaid i chi aros yn eich ystafell a chadw at eich hun. Doedd dim opsiwn i ddeall beth ydoedd.” – Person ag anabledd dysgu Roedd diffyg canllawiau clir a hawdd eu deall ynghylch cloeon, PPE a newidiadau neu gau gwasanaethau yn gadael llawer yn teimlo'n ddryslyd ac yn ansicr. Roedd y diffyg gwybodaeth hygyrch hwn yn ei gwneud hi'n arbennig o anodd iddynt ddeall y rheolau a'r rheoliadau newidiol, gan arwain at deimladau o bryder, unigedd a gwaharddiad. Roeddent yn argymell y dylai llywodraethau a gwasanaethau iechyd gynnwys pobl ag anableddau dysgu yn y dyfodol wrth greu canllawiau hygyrch a chyfrannu at wneud penderfyniadau. “Byddwn i wedi cael pawb ag anableddau dysgu yn rhan o wneud penderfyniadau ac yn gallu meddwl beth i’w wneud a’i wneud yn well.” – Person ag anabledd dysgu |
Disgrifiodd rhai cleifion reolau nad oeddent yn cael eu cymhwyso'n gyson gan weithwyr gofal iechyd proffesiynol, er bod cyfranwyr weithiau'n croesawu'r hyblygrwydd hwn. Er enghraifft, caniatawyd un claf â phryder yn y wardiau i weld lle y byddai'n cael ei llawdriniaeth ymlaen llaw er nad oedd hynny'n cael ei ganiatáu yn unol â'r rheolau.
Rhoddodd rhai cyfranwyr hefyd enghreifftiau o gleifion yn cael gweld perthnasau yn yr ysbyty hyd yn oed pan nad oedd hyn yn cael ei ganiatáu gan y rheolau. Roeddent yn aml yn ddiolchgar pan ddigwyddodd hyn.
| “ | Yn annisgwyl, cafodd tad fy merch yng nghyfraith strôc ddifrifol, ac ni lwyddodd i oroesi, ond roedd yn yr adran gofal dwys niwrolegol yn Newcastle. Ac yn swyddogol, dim ond 2 oedd ganddyn nhw wrth erchwyn ei wely wrth iddo farw, ond mewn gwirionedd fe blygodd y staff y rheolau a chaniatáu mwy yr oeddent yn ddiolchgar iawn amdano.”
- Aelod o'r teulu mewn profedigaeth |
Ar y llaw arall, dywedodd llawer o gyfranwyr hefyd fod rheolau sy'n cael eu gweithredu yn anghyson yn achosi problemau ac ansicrwydd. Er enghraifft, disgrifiodd un claf sut yr oedd gweithwyr gofal iechyd proffesiynol yn caniatáu i aelod o’r teulu fod gyda hi yn yr ysbyty, ond yn ddiweddarach yn y dydd gwnaeth aelod arall o staff wneud iddynt adael. Y diwrnod wedyn caniataodd trydydd gweithiwr gofal iechyd proffesiynol hwy yn ôl eto.
Pan ddigwyddodd hyn, roedd cleifion yn teimlo bod y negeseuon cymysg yn anodd eu deall ac yn rhwystredig. Roedd hyn yn arbennig o anodd pan oedd yr anghysondeb wedi effeithio ar eu profiad o ofal cleifion neu'n golygu nad oeddent yn gallu gweld anwyliaid.
| “ | Ar y pryd roedd canllawiau’r llywodraeth yn llawer mwy rhyddfrydol na’r rheolau y dewisodd yr ysbyty eu cymhwyso mewn gwirionedd, a oedd yn hynod rwystredig ac a gafodd effaith andwyol ar fy iechyd meddwl. Roedd ysbytai eraill yn llawer mwy croesawgar, gyda defnydd o dosturi a synnwyr cyffredin.”
- Claf ysbyty |
Bu cyfranwyr hefyd yn trafod sut roedd canllawiau a rheoliadau yn amrywio ar draws lleoliadau gofal iechyd. Roedd teimlad y gallai rheolau fod yn berthnasol mewn un ysbyty neu bractis meddyg teulu a bod yn wahanol mewn un arall.
Rhoddodd rhai cleifion enghreifftiau o weithwyr gofal iechyd proffesiynol nad oedd i'w gweld yn talu llawer o sylw i rai canllawiau a phrosesau a oedd yn peri dryswch iddynt. Er enghraifft, dywedodd un claf ei fod wedi llenwi ffurflenni ynghylch a oedd wedi ynysu cyn ei lawdriniaeth, dim ond i gael neb i ofyn am y ffurflenni i sicrhau ei fod wedi dilyn y weithdrefn.
| “ | Bob tro roeddwn i'n mynd i mewn, roedd yn rhaid i mi wneud fy nhymheredd ac ysgrifennu a ydw i wedi ynysu yn ystod y 10 diwrnod diwethaf, a doedd neb erioed wedi gwirio'r ddalen ar ôl i mi fynd i mewn beth bynnag. Fe wnes i gadw'r dalennau i gyd fy hun. Ni chymerodd neb ef i mewn i edrych arno. Felly, roeddwn i'n teimlo bod cymaint o swyddi ticio blychau yn digwydd lle roeddwn i newydd feddwl, 'Wel, beth yw pwynt hyn?'”
- Aelod o'r teulu mewn profedigaeth |
Mewn enghraifft arall, esboniodd claf nad oedd rhai o'r meddygon a'r nyrsys a oedd yn gofalu amdanynt yn gwisgo masgiau, er bod ei angen ar y pryd.
Hanes GbemiBu'n rhaid i Gbemi dreulio sawl diwrnod yn yr ysbyty oherwydd cymhlethdodau gyda'i beichiogrwydd. Yn ystod ei harhosiad, roedd yn ymddangos bod y polisïau a'r rheolau yn newid yn ddyddiol heb gyfathrebu clir na rhesymeg gan staff. Dim ond yn ystod oriau penodol y caniatawyd i ŵr Gbemi ymweld, ond roedd yr oriau hyn yn amrywio o ddydd i ddydd. Ar un achlysur, cyrhaeddodd ganol dydd ac roedd yn ofynnol iddo aros yn yr ystafell tan 8 pm heb adael, hyd yn oed i gael bwyd. Pe bai'n gadael yr ystafell am unrhyw reswm, ni fyddai'n cael mynd yn ôl i mewn. Fodd bynnag, ar ddiwrnodau eraill, caniatawyd iddo adael yr ystafell, ac roedd yr amseroedd ymweld naill ai'n fyrrach neu'n hirach. Teimlai Gbemi fod y rheolau hyn yn methu ag ystyried anghenion ymarferol cleifion a'u teuluoedd, megis cael prydau bwyd neu gymryd egwyl. “Roedd yn teimlo fel eu bod nhw newydd dynnu’r rheolau hyn allan o’r awyr a meddwl, 'O mae hyn yn iawn, dyma beth fydd yn ei leihau.” Ychwanegodd diffyg cyfathrebu clir gan staff yr ysbyty at y dryswch. Ni chymerodd neb yr amser i esbonio'r rhesymeg y tu ôl i'r rheolau ymweld na'r rhesymau dros y newidiadau. Gadawodd hyn Gbemi a'i gwr yn teimlo'n rhwystredig ac yn bryderus, heb wybod beth i'w ddisgwyl o un diwrnod i'r llall. Sylwodd Gbemi fod gorfodi'r rheolau hyn yn anghyson ymhlith staff yr ysbyty. Roedd rhai nyrsys yn fwy trugarog, gan ganiatáu ymweliadau byr gan aelodau'r teulu, tra bod eraill yn cadw'n gaeth at y rheolau. Gwaethygodd yr anghysondeb hwn ymhellach y straen a'r rhwystredigaeth o fod yn yr ysbyty yn ystod pandemig. Ar adegau, teimlai Gbemi y gallai cyfathrebu'r staff fod yn anghwrtais, heb fawr o ystyriaeth i'r effaith ar gleifion a theuluoedd. Er bod Gbemi yn deall y pwysau oedd ar weithwyr gofal iechyd, roedd hi'n credu y gallai'r ysbyty fod wedi trin y sefyllfa'n well. “Ro’n i’n teimlo trueni drostyn nhw oherwydd wrth weithio yn y sector cyhoeddus fy hun rwy’n gwybod pa mor ddrwg yw e ac roeddwn i’n gwybod pa mor gorslyd oedden nhw, ond doedd y rheolau ddim yn gwneud synnwyr.” |
Roedd rheolau ynghylch ymweliadau ag ysbytai yn rhwystredig iawn ac yn peri gofid i gleifion a’u hanwyliaid. Yn ystod y pandemig cyfyngwyd ymweliadau ag ysbytai i leihau nifer y bobl sy'n mynd i'r ysbyty a lledaeniad Covid-19. Roedd llawer o gyfranwyr yn rhwystredig bod disgwyl i gleifion fynd i ysbytai ar eu pennau eu hunain yng nghamau cynnar y pandemig. Parhaodd nifer yr ymwelwyr ac amseroedd ymweld i gael eu cyfyngu wrth i'r pandemig fynd rhagddo.
| “ | Roedd yn ofnadwy. Doeddwn i ddim yn cael fy chwaer i mewn, nid oedd, nid oedd fy nghariad yn cael bod yno. Felly, roeddwn i'n eistedd yno yn aros, ac rydych chi yn eich ystafell eich hun ac yn aros yno i rywun ddechrau torri'ch gwddf ar agor. Roedd yn ddigon anodd wynebu’r llawdriniaeth, ond yna rydych chi’n ei wynebu ar eich pen eich hun.”
– Person oedd yn glinigol agored i niwed |
Roedd gorfod mynd i'r ysbyty ar ei ben ei hun heb gefnogaeth perthnasau a ffrindiau yn anodd iawn i gleifion a oedd eisoes yn ofni. Roedd y posibilrwydd y gallent farw ar eu pen eu hunain yn peri gofid arbennig i gleifion â chyflyrau sy'n peryglu bywyd. Rhannodd aelodau o'r teulu a ffrindiau hefyd yr ofn a'r pryder roedden nhw'n ei deimlo, a sut roedd eu hanwyliaid yn ei chael hi'n anodd mynd i'r ysbyty ar eu pen eu hunain.
| “ | Ni allem gysylltu ag ef oherwydd ni fyddai'r wardiau'n codi'r ffôn. Nid oedd Dad yn ddigon da i ddefnyddio ei ffôn, mae’n mynd yn groes i’n siarter hawliau dynol i drin unrhyw un felly, wyddoch chi.”
- Aelod o'r teulu mewn profedigaeth |
| “ | Cymerwyd fy ngŵr i'r ysbyty a chafodd ei ddileu yn y bôn. oherwydd oedran a chyflyrau eraill...roedd yn negyddol ar gyfer Covid-19 a chafodd ei roi ar ward lle'r oedd yn rhemp. Doedden ni ddim yn cael ymweld, doedd gennym ni ddim syniad beth oedd yn digwydd. Bu farw a chefais alwad ffôn am 3:15 yb yn dweud wrthyf ei fod wedi mynd.”
- Aelod o'r teulu mewn profedigaeth |
8. Effaith y pandemig ar y gweithlu gofal iechyd |
 |
Mae'r bennod hon yn rhannu straeon am yr effaith a gafodd y pandemig ar y gweithlu gofal iechyd. Mae'n canolbwyntio ar sut yr effeithiodd y pandemig ar iechyd meddwl a llwyth gwaith gweithwyr gofal iechyd, argaeledd cymorth, a mynediad at ddatblygiad proffesiynol a hyfforddiant. Mae’n gorffen drwy rannu rhai enghreifftiau o’r effaith barhaol ar staff.
Marwolaethau cleifion a chefnogi teuluoedd mewn profedigaeth
Arweiniodd y pandemig at nifer fawr o farwolaethau cleifion, ymhlith cleifion Covid-19 a'r rhai â chyflyrau iechyd eraill. Cafodd profi cymaint o farwolaethau effaith emosiynol enfawr ar lawer yn y gweithlu gofal iechyd a rannodd eu straeon gyda ni.
| “ | Rwy'n gwybod fy mod yn gweld llawer o drawma yn aml, ond roedd hyn ... ar lefel wahanol. Roedd yn rhywbeth nad oedd yr un ohonom wedi ei brofi. Ac roedd pawb yn gwibio eu ffordd drwy’r sefyllfa hon, nad oedd neb yn gwybod sut i’w thrin, ond roedden ni’n gwneud ein gorau.”
- Parafeddyg |
Collodd llawer o weithwyr gofal iechyd proffesiynol deulu a ffrindiau agos yn ystod y pandemig.
| “ | Cymerodd dro bach yn y tŷ, ac roedd yn rhaid iddo fynd i'r adran damweiniau ac achosion brys, ac roedden nhw'n mynd i adael iddo fynd adref, ac roeddwn i wedi dweud, 'Edrychwch, Dadi, y ward rydw i'n gweithio ynddi, mae ganddyn nhw ystafell ochr ar ei chyfer. ti. Nid oes rhaid i chi aros i gael eich apwyntiadau ar gyfer y profion hyn. Mae'r meddyg yn mynd i fynd â chi, ac fe fydd yn gwneud y profion, y sganiau sydd eu hangen arnoch chi, a byddwch chi'n mynd a byddwch chi'n aros yn yr ystafell ochr am ychydig ddyddiau.' Felly, cytunodd wedyn. Roedd mewn ystafell ochr. Bedwar diwrnod yn ddiweddarach profodd yn bositif am Covid-19, ni wellodd byth yn llwyr; ni wellodd erioed, ond yna daeth y meddyg ataf a dweud, 'Mae angen i ni gael y sgwrs hon am ofal diwedd oes.'”
- Cynorthwyydd gofal iechyd |
Rhoddodd llawer o gyfranwyr sy’n gweithio ym maes gofal iechyd enghreifftiau o sut yr oeddent yn trin ac yn cefnogi cleifion ar ddiwedd eu hoes a’u hanwyliaid mewn amgylchiadau anodd a llawn straen. Roedd staff yn y rolau hyn yn aml dan bwysau aruthrol gyda llwythi gwaith llethol. Roeddent yn aml yn cael trafferth disgrifio'r hyn yr oeddent wedi'i weld a'r effaith a gafodd hyn arnynt.
Stori MarionBu Marion yn gweithio fel cynorthwyydd gofal iechyd yn ystod y pandemig, ac roedd hi'n newydd i'r rôl. Roedd ei swydd yn cynnwys monitro cleifion a chyfathrebu â nhw a'u hanwyliaid. Roedd hyn yn golygu yn ystod y pandemig y byddai'n rhaid iddi ddweud wrth bobl fod eu hanwylyd wedi marw. Roedd gweithio ym maes gofal iechyd a wynebu marwolaeth claf a galar ymhlith teulu a ffrindiau mewn profedigaeth yn newydd i Marion. Roedd nifer y cleifion ar ddiwedd eu hoes yn gwneud cyfathrebu ag anwyliaid yn arbennig o anodd, fel y gwnaeth cyfyngiadau ar ymwelwyr. Roedd yna adegau pan fyddai hi'n cyrraedd ystafell claf i ddysgu eu bod wedi marw'r diwrnod hwnnw, ac nid oedd yn glir pwy ddylai gael gwybod na sut i'w cyrraedd. “Rwy’n meddwl ei fod yn teimlo’n anodd oherwydd i mi gan mai dyma’r tro cyntaf i mi weithio ym maes gofal iechyd, dyma’r tro cyntaf i mi brofi bod yn weithiwr gofal iechyd yn wynebu marwolaeth claf. Ond dwi’n meddwl ei fod wedi’i waethygu gan y ffaith bod yna ymdeimlad o ddiymadferthedd i unrhyw un oedd yno.” Rhai o'r sefyllfaoedd mwyaf gofidus ac anodd oedd pan fu'n rhaid i Marion ddweud wrth bobl fod y person yr oeddent yn dod i ymweld ag ef wedi marw. Oherwydd cyfyngiadau ar ymwelwyr, roedd y bobl hyn yn aml ar eu pen eu hunain. Roedd hi'n ei chael hi'n anodd gwybod beth i'w wneud i helpu pobl. “Dim ond un ymwelydd ar y tro oedd ganddyn nhw. Ac felly, cefais y peth anoddaf mewn gwirionedd oedd siarad â nhw a chlywed eu holl ofid pan fydd eu hanwylyd a fu farw, efallai na fyddent yn gallu dweud hwyl fawr. Roeddent yn ceisio prosesu hyn, ond nid oedd ganddynt unrhyw un arall gyda nhw. Felly, roedd hynny i gyd yn anodd iawn yn emosiynol i’w gymryd, ei amsugno a’i brosesu.” |
Roedd yn arbennig o ofidus a thrallodus i wylio dirywiad dramatig cleifion Covid-19 a oedd fel arall wedi bod ymhell cyn y pandemig. I rai cyfranwyr, cynyddodd eu hofn o Covid-19 ar ôl iddynt weld pobl iau, iachach yn marw.
| “ | I ddechrau nid oedd gennyf ofn mawr ohono, ac yna dechreuasom weld marwolaethau iau lle na allech gymhwyso rhesymeg clefyd cronig neu unrhyw beth arall yn union fel effaith ar eu canlyniad gwael. Daeth hynny’n llawer anoddach.”
- Meddyg D&A |
Gweithwyr gofal iechyd proffesiynol a ddeliodd â marwolaeth rhannu sut y bu iddynt ymateb mewn gwahanol ffyrdd. Roedd cyfranwyr a gafodd fwy o brofiad yn aml yn cymharu'r hyn a ddigwyddodd yn ystod y pandemig â marwolaethau cleifion yr oeddent wedi'u gweld o'r blaen. Teimlai rhai fod y profiad hwn wedi eu helpu i ymdopi.
| “ | Rwy'n falch iawn fy mod wedi cael y profiad bywyd rydw i wedi'i gael ... oherwydd rwy'n meddwl fel person iau, ni allwn fod wedi ymdopi â'r pethau roedden ni'n eu gweld a maint y farwolaeth a ...ceisio esbonio i'r perthnasau o bobl na allent ddod i mewn nad oeddent yn mynd i ddod allan.”
- Meddyg D&A |
Ond dywedodd llawer o gyfranwyr eu bod wedi profi effeithiau niweidiol ar eu hiechyd meddwl a’u lles. Rhannodd rhai pa mor ddiymadferth y teimlent yn wyneb cymaint o fywydau’n cael eu colli. Yn ychwanegol at hyn, roeddent yn aml yn ofni oherwydd eu bod yn gwybod bod eu swyddi yn eu rhoi mewn mwy o berygl o haint.
| “ | Llawer o bryder...Dechreuais ysmygu eto oherwydd y straen... Roeddwn i'n ei chael hi'n anodd iawn ... roeddwn i'n ddagreuol llawer. Roedd bron yn teimlo’n eithaf manig wrth geisio dal i fyny… cefais gwnsela yn y gwaith i’m helpu i ymdopi â’r straen emosiynol”
- Gweithiwr gofal iechyd proffesiynol |
Disgrifiodd cyfranwyr eraill ymwahanu oddi wrth y pethau ofnadwy a welsant. Dywedodd llawer wrthym eu bod yn ei chael yn amhosibl cydnabod ac ymdrin â'u teimladau ar y pryd oherwydd pwysau gwaith parhaus. Rhannodd rhai sut y maent yn dal i gael trafferth dod i delerau â'r hyn a welsant.
| “ | Daethom yn imiwn iddo. Fe wnaeth ein dad-ddyneiddio ni ychydig, rwy'n meddwl, ar y pryd. Roeddwn i’n teimlo hynny, ac roeddwn i’n teimlo bod hynny’n anodd delio ag ef.”
– rheolwr practis meddyg teulu |
| “ | Roedd gennym ni gleifion a welsom yn rheolaidd a oedd wedi marw ohono, ie. Roedd hynny'n ysgytwol oherwydd ei fod mor drist, oherwydd rydych chi'n adeiladu perthynas mor dda gyda'ch cleifion - ac yna doedd clywed bod un ohonyn nhw wedi mynd oherwydd Covid ddim yn braf... Dim ond y teimlad na fyddwch chi byth yn ei anghofio, jyst y sioc o weld bod llawer o bobl yn marw…y sioc a’r anghrediniaeth a pha mor ddrwg oedd y firws hwnnw.”
– nyrs meddyg teulu |
Disgrifiodd rhai cyfranwyr sut roedd eu rôl yn gofyn am lefel o uniondeb gyda pherthnasau a oedd yn anodd iddynt yn emosiynol. Roedd yn rhaid i rai ddatblygu ffyrdd newydd o gefnogi cleifion a oedd yn marw a'u teuluoedd, a oedd y tu allan i'w rolau arferol.
| “ | Roedd y swydd newydd fynd mor oer. Ac nid oedd yn fwriadol, roedd yn rhaid iddo fod felly. Wyddoch chi, ni allech chi blygu'r rheolau, oherwydd roedd bywydau pobl mewn perygl. Felly weithiau…roedd yn rhaid i chi fod yn eithaf di-flewyn ar dafod gyda nhw a dyna wnaeth fy ypsetio i.”
- Parafeddyg |
| “ | Daethom yn fwy profiadol mewn profedigaeth nag o'r blaen … Rwy'n meddwl bod ein rôl wedi cynyddu yn y bôn, yn gwneud y cwnsela profedigaeth. Ond nid yw’n rôl hawdd…byddai’n well gennyf i’r cynghorydd profedigaeth wneud hynny.”
- Meddyg Teulu |
Dywedodd llawer o gyfranwyr mai methu â gweld eu hanwyliaid oedd yn marw oedd un o’r pethau anoddaf y bu’n rhaid iddynt ymdopi ag ef. Gwnaeth rhai eu gorau i ofalu am gleifion pan nad oedd eu teulu yn gallu ymweld â nhw.
Roedd yn anodd iawn i staff ymdrin â chleifion nad oeddent gyda'u teuluoedd yn feddyliol ac yn gorfforol. Rhannodd llawer sut y gwnaethant gymryd hyn i ffwrdd o’r gwaith, gan ei chael yn anodd gwahanu’r profiadau hyn oddi wrth eu bywydau personol.
| “ | Roedd fel parth rhyfel, dros nos daeth 18 o bobl yn bositif am Covid-19 heb unman i'w ynysu. Roeddent yn gollwng fel pryfed, roedd yn ofnadwy. Allwch chi ddim diystyru’r hyn a wnaeth hyn i staff nyrsio, roedd methu â chynnig cysur i gleifion yn difetha enaid.”
- Nyrs yn byw gyda Long Covid |
Trafododd rhai cyfranwyr sut yr effeithiwyd arnynt hwy, a’u cydweithwyr, ar iechyd meddwl a chorfforol. Rhannodd cyfranwyr pa mor anodd oedd hi pan fu farw cydweithiwr, nhw yn eu galaru yn fawr hyd yn oed os nad oeddent yn eu hadnabod yn bersonol. Roedd yna ymdeimlad o annhegwch bod rhai gweithwyr gofal iechyd wedi marw, a phryder am yr effaith ddinistriol ar eu hanwyliaid.
| “ | Dim ond gorfod colli cydweithwyr hefyd. Roedd gennym gydweithwyr a oedd yn sâl iawn, rhai a fu farw. Mae'n newid morâl, a dweud y gwir. Mae'n gwneud i bawb deimlo'n ofidus iawn. Mae pobl yn teimlo fel, pam mae hyn wedi digwydd? Mae'n rhywbeth na fyddwn byth yn ei ddeall mewn gwirionedd, a dweud y gwir.”
– nyrs meddyg teulu |
| “ | Fe gollon ni gydweithiwr i hunanladdiad tua diwedd y pandemig. Ni fyddwn byth yn gwybod pam y gwnaethant ladd eu hunain, ond gwyddom fod y pandemig wedi cael effaith sylweddol ar eu hiechyd meddwl.”
- Gweithiwr gofal iechyd proffesiynol |
Rhannodd un porthor ysbyty sut y gwnaethant golli ffrind agos a chydweithiwr yr oeddent yn teimlo'n debygol o farw o ddal Covid-19 wrth weithio yn yr ysbyty. Er gwaethaf hyn, ni roddodd yr ysbyty unrhyw gymorth i'r teulu mewn profedigaeth. Arweiniodd hyn at borthor yr ysbyty yn cwestiynu a oedd risgiau'r swydd yn werth chweil.
| “ | Bryd hynny, a dweud y gwir, roeddwn i'n meddwl, fel, ydw i eisiau bod yma? Fe’i daliodd o’r ysbyty, o’r gwaith yr oedd yn ei wneud…cafodd ei heintio oddi yno, ond nid oedd neb o’r ysbyty wedi rhoi unrhyw ychydig o gefnogaeth i’w deulu, a dyna’r rhan dristaf…maen nhw’n disgwyl ichi wneud cymaint , ond ar ôl i rywun newydd golli eu bywyd, nid ydych yn rhoi unrhyw beth i'w deulu. Ychydig o gefnogaeth neu ddangos ychydig o gydymdeimlad. Dim byd.”
- Porthor ysbyty |
Effaith addasu i'r pandemig
Roedd newidiadau a phwysau'r pandemig yn golygu bod rhai gweithwyr gofal iechyd proffesiynol yn cael trafferth ymdopi. Disgrifiodd llawer o gyfranwyr fywyd gwaith heb drefn arferol a rhagweladwyedd. Dywedodd rhai wrthym fod diffyg eglurder a thryloywder am y pandemig a’u gwaith wedi gwaethygu pethau, gan gynyddu straen a phryder i lawer.
| “ | Rwy'n hoffi trefn arferol, rwy'n hoffi rheoli, rwy'n meddwl ein bod ni i gyd fel llawfeddygon yn hoffi bod mewn rheolaeth, dim ond natur y bwystfil ydyw. Ac felly roedd cael dau o blant bach, gŵr sydd hefyd yn llawfeddyg, hefyd ar rota brys, ac yn llythrennol aros ar nos Sul am amserlen yr wythnos i ddod allan yn hynod o straen. Ac fe ychwanegodd straen diangen ychwanegol at yr hyn a oedd eisoes yn amlwg yn hynod o straen yn broffesiynol.”
- Llawfeddyg |
Ni wynebodd pawb a rannodd eu profiadau gyda ni y pwysau cyson hwn trwy gydol y pandemig. Fodd bynnag, cyfeiriodd rhai cyfranwyr at eu llwyth gwaith fel bod yn llethol yn gyson, gan ddweud ei bod yn amhosibl delio ag ef. Clywsom enghreifftiau o staff a oedd yn gorfod gwneud gwaith ychwanegol heb unrhyw gydnabyddiaeth, yn gweithio mewn timau a oedd yn brin o staff ac o dan bwysau cyson, ac nad oeddent yn gallu cymryd gwyliau neu seibiannau blynyddol.
| “ | Rydych chi'n cyrraedd pwynt lle rydych chi'n gwneud shifftiau ychwanegol ac rydych chi wedi blino, ac rydych chi'n meddwl, o, mae gen i benwythnos i ffwrdd. Ond beth oedd yn digwydd yn gyson, oherwydd byddai pobl yn dal i fynd i ffwrdd, roedd rhywun bob amser yn cysylltu â chi, 'Unrhyw siawns y gallech chi ddod i mewn a gwneud shifft ychwanegol?' mor effeithiol doeddech chi byth i ffwrdd.”
-Meddyg ysbyty |
| “ | Roedd yn anodd iawn. Rwy'n meddwl eich bod wedi cael eich rhuthro oddi ar eich traed. Gostyngwyd eich seibiannau. Roeddech chi'n newynog, roeddech chi wedi blino. Yna ar ôl cyrraedd adref gyda'r nos a gwybod bod yn rhaid i chi fynd i'w wneud eto, a chi jyst, mae'n fath o, roedd yn ofn roeddech chi'n ei deimlo, yn meddwl, beth ydw i'n cerdded i mewn yfory? Rydyn ni fel teulu bach, felly rydw i'n meddwl ein bod ni wedi gwneud, wel, fel y gallwn ni orau pan oeddech chi'n teimlo'n isel, dim ond i geisio cadw eraill i fynd”
- Nyrs ysbyty |
Roedd llwythi gwaith cynyddol a delio â newidiadau yn eu rolau yn golygu bod rhai staff gofal iechyd wedi esgeuluso eu hiechyd meddwl a chorfforol eu hunain er mwyn blaenoriaethu cleifion. Roedd llawer o gyfranwyr yn rhannu pa mor anodd oedd hi i ofalu am eu hunain pan oeddent yn cael eu gorymestyn ac yn cymryd sifftiau ychwanegol i lenwi bylchau mewn gofal. Roedd yn aml yn hynod heriol gofalu am eu lles eu hunain a darparu'r gofal yr oedd ei angen ar gleifion.
| “ | Nid oedd gennych amser i gael problemau iechyd meddwl, roedd angen i chi fwrw ymlaen ag ef oherwydd eich bod yn gwneud swydd ac roeddech, roeddech yn teimlo eich bod yn ymladd am eich bywyd eich hun bob dydd.”
- Meddyg D&A |
Er mwyn delio â’r pwysau llwyth gwaith, dywedodd cyfranwyr wrthym sut roedd rolau ychwanegol yn cael eu creu, staff o dimau eraill yn gwirfoddoli i helpu, a defnyddiwyd staff banc ac asiantaeth, yn aml i gyflenwi yn ystod salwch staff. Roedd cael eu talu’n ychwanegol am oramser, sifftiau nos, neu sifftiau brys yn annog rhai staff i gymryd gwaith ychwanegol, oherwydd eu bod yn teimlo eu bod yn cael eu cydnabod yn iawn.
| “ | Gwn fod gennym ychydig o fferyllwyr wrth gefn rhag ofn. Dywedwch fod rhywun wedi galw i mewn a dweud bod ganddyn nhw symptomau neu beth nad oedd ganddyn nhw, yna roedd yna grŵp a oedd yn ddigon parod mewn ffordd. Roedden ni'n gwybod ar ba ddyddiau roedden nhw'n rhydd a ddim yn rhydd. Byddem yn ceisio cadw hynny mewn cof, ond diolch byth nid oedd angen i ni ddefnyddio hynny’n ormodol.”
- Fferyllydd ysbyty |
Fodd bynnag, mewn rhai achosion, nid oedd gan y staff a ddaeth â hwy i mewn fawr ddim profiad perthnasol, os o gwbl, ac ni allent wneud fawr ddim i helpu. Lle digwyddodd hyn, roedd yn aml yn ychwanegu at bwysau ar staff â'r sgiliau cywir, gan fod yn rhaid iddynt uwchsgilio'r staff hyn yn y swydd yn anffurfiol. Un enghraifft oedd recriwtio diffoddwyr tân i wneud i fyny criwiau ambiwlans oherwydd prinder gweithwyr ambiwlans a pharafeddygon. Gallai'r defnydd o staff asiantaeth hefyd fod yn anrhagweladwy oherwydd ansicrwydd ynghylch eu set sgiliau.
| “ | Ar un adeg, cynigiwyd aelod o staff asiantaeth i ni, ond ni fyddech byth yn gwybod pa sgiliau fyddai gan staff asiantaeth.”
- Nyrs ysbyty |
Roedd rhai cyfranwyr yn rhannu ei bod hefyd yn fwy anodd dod o hyd i aelodau priodol o staff gyda’r profiad addas i gyflenwi yn ystod absenoldeb wrth weithio mewn meysydd arbenigol.
| “ | Ar rai dyddiau roeddech chi'n fyr, byddech chi'n ceisio cael staff o wardiau eraill, ond pan fyddwch chi'n gweithio mewn maes arbenigol, nid yw nyrsys ward yn gallu helpu oherwydd nad ydyn nhw'n deall y cyfarpar neu'r monitro rydyn ni wedi arfer ag ef. Ni allwch eu rhoi mewn sefyllfa. Yna maen nhw hefyd yn mynd i'r wardiau, roedden nhw mor fyr fel nad oedden nhw'n gallu dod i'n helpu ni beth bynnag. Yn syml, roedd yn rhaid i chi wneud yr hyn y gallech chi."
- Nyrs ysbyty |
Roedd gweithwyr gofal iechyd proffesiynol yn aml yn rhannu sut roedd pobl sy'n dal Covid-19 wedi cael effaith fawr ar eu timau, gan na fyddai aelodau'r tîm yn gallu gweithio am ddyddiau neu wythnosau. Roedd hyn yn golygu bod maint timau, rotâu ac oriau gwaith yn newid yn gyflym. Arweiniodd hyn at oriau gwaith hirach i rai.
| “ | Roedd diffyg staff oherwydd bod pawb yn cael y firws eu hunain. Felly gwnaeth eraill sifftiau dwbl yn barhaus oherwydd os nad ydyn nhw yno, does neb yno. Oedd, felly gostyngwyd staffio mewn gwirionedd. Roedd pawb yn mynd i ffwrdd yn sâl, felly staffio oedd y peth anoddaf hefyd.”
– Gweithiwr gofal iechyd proffesiynol perthynol |
Arweiniodd y cynnydd yn y llwyth gwaith oherwydd absenoldeb staff at disgwyliadau uwch fyth yn cael eu gosod ar weddill y staff a llai o opsiynau i leddfu'r pwysau.
| “ | Yn bendant roedd yna lawer o bobl i ffwrdd yn sâl, pobl o fewn y gwasanaeth a oedd yn gwarchod, felly fe wnaethon nhw dynnu'n ôl yn syth, wyddoch chi, ac yna dechreuodd y salwch ac roedd y gwasanaeth yn rhedeg gyda chyn lleied â phosibl, fe allech chi weld gwahaniaeth enfawr yn bendant. . Roedd yn anodd iawn. Roedd pethau'n cynyddu. Daeth yn eithaf brawychus oherwydd, wyddoch chi, gallai fod pwyntiau lle na allai neb fod wedi bod ar ôl ond fe wnaethom ni fwrw ymlaen â'r peth, nid oedd unrhyw ateb iddo, nid oedd unrhyw beth y gallem ei wneud.”
- Parafeddyg |
| “ | Roedd yn heriol iawn. Roedd yn heriol oherwydd roedd yn rhaid inni weithiau wneud swydd lle’r oedd yn swydd 3, 4, neu 5 person, ac roedd yn rhaid i un person gymryd y rôl honno. Fel y dywedais wrthych, roeddem yn rhedeg, ac roedd mor ddwys oherwydd eu bod yn brin o staff, roedd cymaint o bobl yn mynd i ffwrdd yn sâl, cymaint o bobl yn mynd i ffwrdd â Covid-19. Felly, roedd y dwyster arnom ni, ac roedd yn rhaid i ni, fel, gymryd y rôl honno hefyd.”
- Cynorthwyydd gofal iechyd ysbyty |
Er mwyn ymateb i'r lefelau anarferol o uchel o absenoldeb staff, bu'n rhaid newid dulliau staffio. Er enghraifft, soniodd rhai cyfranwyr am fwy o hyblygrwydd yn cael ei gynnwys mewn rotâu. Dywedasant fod rotâu yn cael eu newid yn gyson oherwydd bod staff yn amau symptomau Covid-19 neu oherwydd nad oeddent yn gallu gweithio am resymau eraill. Digwyddai hyn yn aml ar fyr rybudd.
Stori JoeRoedd Joe yn gweithio fel rheolwr practis i Feddyg Teulu. Roedd ei bractis yn rhannu adeiladau a chyfleusterau â phedwar practis arall. Cyn y pandemig, roeddent wedi gweithio gyda'i gilydd lle bo angen. Roedd ei swydd yn cynnwys cydlynu gwasanaethau, trefnu meddygon teulu a staff gofal iechyd eraill, a bod yn bwynt galw ar gyfer e-byst yn dod i mewn i'r practis. Roedd hyn yn golygu ei fod yn ymwneud yn uniongyrchol ag ad-drefnu sut yr oeddent yn darparu gofal yn ystod y pandemig, a hefyd yn rheoli staffio. Roedd practis Joe yn wynebu problemau gyda salwch staff trwy gydol y pandemig. I Joe roedd hon yn her fawr ac roedd yn rhaid iddo dreulio cryn dipyn o amser yn sicrhau y gallent ddod o hyd i ddigon o yswiriant. Bob mis byddai o leiaf dau aelod o'r tîm yn absennol oherwydd salwch. Cafodd hyn effaith fawr ar eu tîm bach. “Roedd yn ddrwg iawn. Bob mis roeddwn yn adrodd efallai 50, 60 diwrnod salwch ymhlith staff. Ar gyfartaledd efallai y byddwn ni’n cael dau ddiwrnod sâl y mis – roedd yn ofnadwy.” Bu'n rhaid i Joe ganslo apwyntiadau cleifion, ad-drefnu gwasanaethau a blaenoriaethu'r cleifion a allai dderbyn gofal. Roedd hefyd yn cefnogi cydweithwyr oedd yn wynebu anawsterau iechyd meddwl. Roedd hyn yn cynnwys un cydweithiwr a oedd i ffwrdd o'r gwaith am dri mis gyda phryder. Roedd y pandemig yn gyfnod dirdynnol iawn i Joe. Roedd rheoli disgwyliadau cleifion a chydweithwyr yn llethol iddo. “Roedd yn rhaid i mi reoli teimladau ac ofnau llawer o bobl yn y gwaith. Rhwng hynny a salwch staff, doedd gennych chi ddim amser a’r effaith ar fy rôl, roeddwn i’n gwneud gwaith pawb arall heblaw am swydd y Meddyg Teulu mewn gwirionedd, oherwydd roedd yn rhaid i chi wneud hynny.” |
Rhannodd llawer o gyfranwyr sut yr aeth staff yn gynyddol flinedig a’i chael yn anodd delio â newidiadau parhaus wrth i’r pandemig fynd rhagddo. Dywedodd gweithwyr gofal iechyd proffesiynol wrthym fod eu harferion a’u patrymau gwaith yn parhau i newid wrth i’r pandemig fynd rhagddo. Dechreuodd llawer weld mwy o gleifion wyneb yn wyneb, tra hefyd yn parhau ag apwyntiadau ar-lein. Disgrifiodd rhai o’r rhai a oedd yn gymharol dawel yn ystod camau cynnar y pandemig weithio mwy o oriau, gan gynnwys sifftiau ychwanegol a mwy o benwythnosau.
| “ | Roedd yn rhaid i ni weithio shifftiau 12-15 awr yn rheolaidd yn lle’r shifftiau 6 awr.”
– Gweithiwr gofal iechyd proffesiynol perthynol |
Myfyriodd rhai cyfranwyr ar sut roedd staff yn ymateb yn wahanol i'r pwysau parhaus hyn. Disgrifiwyd rhai fel camu i fyny i lenwi bylchau, ac eraill a oedd yn cael eu gweld gan rai fel rhai nad oeddent yn gwneud digon. Er enghraifft, gwrthododd rhai aelodau o staff weithio y tu allan i'r maes arbenigedd yr oeddent wedi'i drwyddedu ar ei gyfer (yn unol â chyngor y Cyngor Meddygol Cyffredinol). Roedd y canfyddiad nad oedd rhai aelodau o staff yn ymgymryd â'r gwaith y dylen nhw wedi arwain at siom a dicter rhwng ac o fewn timau.
| “ | Ac roedd yna rai pobl a gamodd i fyny mewn gwirionedd. Mae yna ddyn a oedd yn rheolwr cymharol iau ac roedd yn wirioneddol drawiadol yn cymryd rheolaeth o'r sefyllfa anodd, pobl eraill ddim cymaint. Ac roedd yna lawer o bobl a oedd yn siomedig yn ei ddefnyddio i osgoi cyfrifoldebau.”
-Meddyg ysbyty |
| “ | Roedd gennym ni ddau neu dri aelod o staff a benderfynodd nad oedden nhw eisiau gweithio yn yr ysbyty bellach, ac aethon nhw ar salwch hirdymor oherwydd nad oedden nhw eisiau mynd â dim byd adref i'w teuluoedd. Achosodd hynny dipyn o ddrwgdeimlad o fewn yr adran oherwydd yn amlwg roedd rhai pobl yn cael cyflog llawn am aros gartref, tra bod pawb arall yn mynd i weithio a gweithio fel tîm.”
- Fferyllydd ysbyty |
Cymhelliant staff
Disgrifiodd cyfranwyr yn aml sut yr oeddent yn teimlo ymdeimlad o bwrpas yn gweithio mewn lleoliadau gofal iechyd yn ystod y pandemig. Dywedodd llawer eu bod yn ffodus eu bod yn dal i allu mynd i'r gwaith a gwneud rhywbeth ystyrlon. Roedd eu rolau yn bwysig yn ystod argyfwng iechyd gwladol.
| “ | Roeddech chi'n helpu pobl eraill. Roeddech mewn gwirionedd yn darparu gwasanaeth gwerthfawr. Fe wnaeth i chi deimlo'n falch o'r hyn wnaethoch chi."
- Fferyllydd ysbyty |
Canfu llawer o weithwyr gofal iechyd proffesiynol fod eglurder pwrpas yn y gwaith wedi helpu i dynnu eu sylw oddi wrth bryderon a phryderon eraill, gan gynnwys effaith y pandemig arnyn nhw a’u teuluoedd. Roedd rhai hyd yn oed yn fwy cadarnhaol am y strwythur a'r pwrpas a roddodd eu gwaith iddynt yn ystod y pandemig.
| “ | Ar y Pasg roeddwn i fod i gael 4 diwrnod i ffwrdd, ac fe wnaethon nhw fy ffonio'n ôl ar ôl 2 ddiwrnod, ac roeddwn i'n hapus iawn i fynd oherwydd mae'n eithaf diflas bod gartref heb ddim i'w wneud ychwaith."
-Meddyg ysbyty |
Roedd treulio amser gyda chydweithwyr hefyd yn werthfawr i lawer o weithwyr gofal iechyd proffesiynol. Yn ogystal â chynnig cymorth gan gymheiriaid yn eu rolau, roedd llawer o’r farn bod y rhyngweithio cymdeithasol sydd ar gael iddynt mewn lleoliadau gofal iechyd yn eu helpu i ymdopi. Roeddent yn gwybod nad oedd pawb yn gallu gweld pobl yn ystod y pandemig ac nid oeddent yn cymryd hyn yn ganiataol.
Siaradodd rhai aelodau o staff a gafodd eu cymeradwyo o'r gwaith neu o weithio gartref yn ystod y pandemig sut roedden nhw'n teimlo eu bod wedi gadael eu tîm i lawr. Cawsant hyn yn arbennig o anodd oherwydd eu bod yn gwybod bod angen eu sgiliau a'u harbenigedd.
| “ | Yr ychydig wythnosau cyntaf hynny ar ôl i'r penderfyniad gael ei wneud i weithio gartref, roeddwn i wedi fy siomi ... roeddwn i'n teimlo fy mod wedi eu siomi. Roeddwn i hefyd mewn ffordd yn teimlo fymryn yn cael fy ngadael, wyddoch chi, dyma’r peth mwyaf i ddigwydd i iechyd yn fy ngyrfa, ac roeddwn i’n mynd i gael fy rhoi o’r neilltu”
- Meddyg D&A |
Fodd bynnag, roedd rhai cyfranwyr yn meddwl hynny ni pharhaodd cydweithio ar draws gwahanol rannau o ofal iechyd. Disgrifiwyd straen y pandemig gan lawer o gyfranwyr fel rhywbeth a arweiniodd at berthnasoedd gwaith cynyddol dynn. Digwyddodd rhywfaint o hyn o fewn lleoliadau neu dimau gofal iechyd unigol.
| “ | Felly dwi'n meddwl, ar y dechrau, roedd 'na ryw fath o dynnu at ei gilydd o bawb. Ac roedd hynny, yn fath o, yn neis ac roedd llawer o ewyllys da. Rwy'n meddwl bod hynny wedi llosgi allan yn y cyfnod 3- neu 4 mis. Ond i ddechrau, roedd yna lawer o gydymdeimlad neis.”
-Meddyg ysbyty |
| “ | Rwy'n meddwl bod pobl yn canolbwyntio'n fawr ar un gelyn, pawb yn tynnu at ei gilydd a doedd pethau eraill ddim o bwys bellach, roedd yn ymwneud mwy â'r teulu. Mae'n dangos bod bodau dynol yn llawer gwell pan fydd ganddyn nhw bwrpas cyffredin ac un peth y gallant ganolbwyntio arno. Ac yna wrth iddo fynd yn ei flaen, a dod yn fwy tameidiog, rwy’n meddwl inni fynd yn ôl at ein hymddygiad mwy normal, ac yna roedd yn teimlo ychydig o siom”
-Meddyg ysbyty |
Rhannodd rhai gweithwyr gofal iechyd sut y daeth yn fwyfwy anodd delio â gwahanol donnau Covid-19. Roedd staff yn gynyddol flinedig ac yn cael trafferth, ond yn dal i weithio oherwydd bod yn rhaid iddynt gyflenwi ar gyfer cydweithwyr a oedd yn sâl neu'n hunanynysu. Roedd gan rai cyfranwyr rwystredigaethau cynyddol nad oedd staff yn cael eu cydnabod a'u digolledu'n iawn, yn enwedig o ystyried y risgiau personol a gymerodd yn ystod y pandemig.
| “ | Erbyn yr ail flwyddyn, roedd y seilwaith, y staffio, y blinder yn gymaint fel ei fod yn dioddef yn fawr. Roedden ni i gyd wedi blino’n lân a dydw i erioed wedi cyfarfod â’r fath grŵp o fodau dynol ystyrlon â’r rhain…ac eto, i weld cyn lleied o arian wrth gefn oedd ar ôl ac…mae wastad rhywun yn sâl a, wyddoch chi, mae’n anodd iawn bod hynny person eich hun hefyd, felly nid oes unrhyw un yn mynd i ffwrdd yn sâl nes eu bod yn [] llanast llwyr sy'n eithaf ofnadwy hefyd."
-Meddyg ysbyty |
Teimlai cyfranwyr i raddau helaeth eu bod yn cael eu cefnogi gan y cyhoedd, yn enwedig yng nghamau cynnar y pandemig. Roeddent yn rhannu enghreifftiau o gael eu trin â charedigrwydd ac yn aml yn teimlo eu bod yn cael eu dal i fyny fel 'arwyr'. Dywedodd llawer fod cleifion a'u teuluoedd yn deall pan oedd pethau'n cymryd mwy o amser nag arfer neu pan oedd gofal yn symud i apwyntiadau o bell. Roedd rhywfaint o ofn hefyd, gyda phobl yn poeni am ddal Covid-19 gan y rhai a oedd yn gweithio mewn lleoliadau gofal iechyd.
| “ | Rwy'n meddwl bod y cyhoedd yn gyffredinol yn gefnogol iawn i weithwyr gofal iechyd, ond hefyd, rwy'n meddwl eu bod yn wyliadwrus iawn ohonoch chi hefyd. Yn amlwg, doedden ni ddim yn mynd allan mewn iwnifform na dim byd ond os oeddech chi – fe allech chi ddangos eich cerdyn i fynd i’r archfarchnad os oedd angen neidio’r ciw neu rywbeth. Dim ond pe bawn i ar frys i gyrraedd y gwaith, byddwn i'n gwneud hynny beth bynnag, ond doedd neb i weld yn meddwl; roedden nhw’n gwybod bod angen i chi gyrraedd y gwaith ac rwy’n meddwl bod aelodau’r cyhoedd yn gefnogol iawn, iawn.”
- Fferyllydd ysbyty |
Adlewyrchodd rhai cyfranwyr ar y gwahaniaethau rhwng canfyddiad y cyhoedd o’r gweithlu gofal iechyd a’u profiadau eu hunain o’r pandemig.
| “ | Dyna oedd y disgwyliad o weithio yno, fel y dylech chi deimlo'n falch, rydych chi ar y rheng flaen, rydych chi'n filwr, rydych chi'n arwr ... pan mewn gwirionedd ni fyddech chi'n dweud beth sy'n digwydd y tu ôl i ddrysau caeedig. A fyddwn i ddim o reidrwydd yn falch o bopeth roeddwn i wedi’i wneud, na’r penderfyniadau roedd yn rhaid eu gwneud ar y pryd oherwydd diffyg offer neu staff neu beth bynnag.”
- Nyrs ysbyty |
Stori HelenBu Helen yn gweithio fel parafeddyg yn ystod y pandemig. Mae'n byw gyda'i thri o blant, yn agos at ei theulu estynedig. Rhannodd Helen sut y teimlai fod ei gwaith yn aml yn cael ei gamddeall gan y cyhoedd a bod y camddealltwriaeth hyn yn waeth yn ystod y pandemig. Dywedodd fod cleifion yn disgwyl gormod gan barafeddygon a'r cymorth meddygol a chymorth arall y gallent ei gynnig. Er enghraifft, roedd cleifion yn aml yn disgwyl i barafeddygon allu eu trin gartref fel nad oedd yn rhaid iddynt fynd i'r ysbyty. Roedd llawer o'r cleifion a'r teuluoedd y daeth ar eu traws yn ystod y pandemig yn ddiamynedd, yn ddig ac yn ymosodol gyda hi. Roedd hi'n meddwl bod hyn oherwydd pa mor ofnus oedden nhw. “Roedd y disgwyliad arnom ni, fel gweithwyr gofal iechyd, yn afreal. Ac mae bron fel ein bod ni i fod i fod yn oruwchddynol, a pheidio â mynd yn sâl, gwybod yr atebion i bopeth, annog pawb, tra roedden ni'n teimlo'n ofnus ein hunain.” Er bod Helen yn gwerthfawrogi cael ei chlapio amdano ar nos Iau, dros amser tyfodd i ddigio. Nid oedd yn teimlo'r un cynhesrwydd a gwerthfawrogiad yn ei hymwneud â chleifion. Nid oedd ychwaith yn teimlo ei bod yn cael ei gwobrwyo gan ei chyflogwr na'r llywodraeth am yr holl risgiau personol yr oedd yn eu cymryd. “Roedd yn rhaid i mi geisio cael y cydbwysedd hwn yn fy meddwl, nad yw'r cyhoedd yn cael yr hyn yr ydym yn ei wneud yn union. Felly, maen nhw'n gwybod ein bod ni'n feddygol, maen nhw'n gwybod y gallwn ni helpu i ryw raddau, ond dydyn nhw ddim yn gwybod yn iawn fanylion ein swydd ... maen nhw'n disgwyl i chi allu rhoi rhyw fath o sicrwydd iddynt, rhyw fath o driniaeth …oherwydd efallai na fydd llawer o bobl yr ydym yn mynd atynt yn gyffredinol eisiau mynd i'r ysbyty. Dywedon nhw, rydw i eisiau cael fy nhrosi, ni allaf fynd drwodd at fy meddyg teulu, neu ni allaf beth bynnag. Mae fel, nid dyna beth rydyn ni yma ar ei gyfer. Mae hyn ar gyfer os ydych mewn damwain, neu os oes argyfwng yn digwydd. Nid yw hyn yn argyfwng.” |
Roedd gweithwyr gofal iechyd proffesiynol yn wynebu’r un heriau personol ag y gwnaeth pawb mewn cymdeithas, ac ychwanegodd hyn bwysau a straen pellach. Yn y llu o’r straeon y gwnaethant eu rhannu â ni, roedd yr effaith ar eu bywydau y tu allan i’r gwaith yn hynod bwysig i’w profiad o’r pandemig. Er enghraifft, rhoddodd cau ysgolion bwysau aruthrol ar y rhai â phlant wrth iddynt ysgwyddo mwy o gyfrifoldeb am addysg, gan jyglo hyn ag ymrwymiadau gwaith. Disgrifiodd eraill gymryd gofal am anwyliaid a oedd yn agored i niwed neu'n gwarchod.
| “ | Y ing meddwl, rydych chi'n dweud wrthych chi'ch hun bod yn rhaid i chi ei barcio, mae'n rhaid i chi ddod ymlaen i'ch teulu, i'ch plant, mae pawb yn edrych atoch chi oherwydd eich bod mewn gofal iechyd, mae'n rhaid i chi ddal y cyfan gyda'ch gilydd. Roeddwn i'n teimlo dros y plant ... mae'r euogrwydd yna o hyd, ond roedden nhw [staff] yn fyr, felly roedd yn rhaid i mi fynd i mewn.”
– Nyrs gymunedol i blant |
Roedd y pwysau hyn yn aml yn ychwanegu at broblemau gyda’u hiechyd meddwl a’u lles. Un her a amlygwyd gan rai cyfranwyr oedd pa mor anodd oedd hi i wahaniaethu'n glir rhwng eu bywydau personol a'u bywydau gwaith. Er enghraifft, roedd llawer yn delio ag anghenion cleifion anodd a chymhleth o gartref am y tro cyntaf.
| “ | Gan weithio o gartref a delio â chleientiaid â cham-drin domestig, cam-drin sylweddau, dementia, roedd mor amrywiol, roedd yn anodd. Roedd yn anodd cael y sgyrsiau hyn gartref lle gallai fy merch glywed, ac ni fyddai’n deall pam roedd rhywun yn crio / gweiddi arnaf.”
- Gweithiwr gofal iechyd proffesiynol |
Hyfforddiant a sgiliau
Ar draws gwasanaethau gofal iechyd yn y DU mae yna gyrsiau hyfforddi statudol a gorfodol y mae gweithwyr gofal iechyd proffesiynol yn eu cwblhau i sicrhau bod eu gwybodaeth a'u sgiliau'n parhau'n gyfredol. Er enghraifft, mae gweithwyr gofal iechyd proffesiynol yn cael hyfforddiant ar bynciau fel iechyd, diogelwch a lles, atal a rheoli heintiau, symud a thrin cleifion, dadebru a diogelu.
Clywsom sut y daeth hyfforddiant gorfodol i ben neu wedi ymlacio mewn llawer o leoliadau gofal iechyd i flaenoriaethu ymateb Covid-19. Roedd dealltwriaeth ymhlith uwch staff nad oedd modd cydymffurfio, yn enwedig gan fod staff yn gorweithio. Nid oedd hyfforddiant yn gymaint o flaenoriaeth â’r ymateb pandemig – a chroesawyd hyn gan staff a oedd dan straen.
| “ | Nid oedd y gallu meddyliol a'r amser i wneud y pethau hynny ar yr agenda o gwbl...mae'n debyg bod timau gweithredol [yn gwybod] mai dyna oedd yr achos. Nid oedd ar agenda neb yn y math hwnnw o amser diffodd tanau.”
- Gweithiwr proffesiynol AD ysbyty |
Rhannodd un cyfrannwr sut nad oedd hyfforddiant gorfodol ar ddadebru wedi'i gynnal ers dwy flynedd a dim ond yn 2022 y cafodd ei gynnig eto. Awgrymodd eraill nad oedd hyfforddiant gloywi ar bethau fel rheoli heintiau wedi'i ddarparu ers sawl blwyddyn.
| “ | Fel arfer byddwn i’n mynd i hyfforddi gyda’r nos, ac fe stopiwyd hynny i gyd a doedd dim o hynny ymlaen, a does dim llawer o hynny ymlaen wedi bod ers tair blynedd mewn gwirionedd.”
– nyrs meddyg teulu |
| “ | Yn y pandemig rwy’n meddwl… aeth llawer o’r hyfforddiant gorfodol hwnnw a sicrhau bod iechyd a diogelwch gweithwyr yn cael ei gynnal, yn y bôn allan o’r ffenest.”
- Staff labordy ysbytai |
Fodd bynnag, rhannodd cyfranwyr eraill sut roedd rhywfaint o hyfforddiant gorfodol yn parhau. I rai cyfranogwyr, gan gynnwys nyrsys, trosglwyddwyd hyfforddiant ar-lein. I rai gweithwyr proffesiynol, roedd eu hyfforddiant gorfodol eisoes ar gael ar-lein, a oedd yn golygu nad oedd unrhyw newid i’r ddarpariaeth.
| “ | Yr unig hyfforddiant gorfodol bryd hynny oedd…yr holl PPE a rheoli heintiau, ac fe aeth hynny ymlaen am dros flwyddyn, efallai blwyddyn a hanner. Dyna’r unig hyfforddiant a roddwyd, ac o hynny, roedd llawer o hyfforddiant sydd bellach wedi mynd i e-ddysgu. Felly, rydych chi'n cwblhau'r cyflwyniad ar-lein yn hytrach nag wyneb yn wyneb. Dim ond sleidiau rydych chi'n edrych drwyddynt ar-lein ac rydych chi'n cael tystysgrif ar y diwedd.”
- Cynorthwyydd gofal iechyd |
| “ | Do, fe wnaethon ni'r cyfan, ac mae gennym ni systemau ar-lein da iawn, felly roedden ni'n gallu - felly hyfforddiant ar-lein ... yn amlwg fe wnaethon ni gadw i fyny â'r holl hyfforddiant gorfodol, ni lwyddodd i lithro ... roedd ar-lein yn barod. Yr unig un sydd fel arfer wyneb yn wyneb yw’r dadebru, rydyn ni nôl wyneb yn wyneb â hynny nawr, ond roedden ni’n gallu gwneud hynny ar-lein yn ystod y pandemig.”
– rheolwr practis meddyg teulu |
Daeth llawer o'r datblygiad proffesiynol a phersonol arferol i ben hefyd yn ystod y pandemig, gyda rhai yn mynegi effaith bosibl ar ddiogelwch cleifion. Roedd enghreifftiau yn cynnwys hyfforddiant ar sgiliau gweinyddol, gwasanaeth cwsmeriaid a chyrsiau addysgol untro (hy y rhai a ddarperir gan gwmnïau cyffuriau a chynrychiolwyr ar ymweliadau ysbyty).
| “ | Byddem wedi cael pethau fel dysgu seiliedig ar ymarfer – roedd y rheini wedi mynd ers 2 flynedd. Ni chafodd myfyrwyr meddygol newydd sesiynau tiwtorial…byddem yn siarad am benderfyniadau clinigol yn anffurfiol, ond ni allai meddygon fod yn yr un ystafell rhag ofn i un ohonynt gontractio Covid heb yn wybod. Cymerodd addysg sedd gefn.”
- Meddyg Teulu |
Amlygodd cyfranwyr rai bylchau mewn hyfforddiant wrth i bopeth symud ar-lein. Er enghraifft, collodd rhai staff iau allan ar hyfforddiant craidd oherwydd gweithio ar ward Covid-19 am flwyddyn heb gael eu cylchdroi i wardiau eraill. Dywedodd un cyfrannwr nad oedd unrhyw hyfforddiant i barafeddygon dan hyfforddiant am resymau tebyg.
Roedd enghreifftiau o hyfforddiant wedi'i ganslo yn effeithio ar ddilyniant. Roedd rhai cyfranwyr hefyd yn poeni y gallai diffyg hyfforddiant ar gyfer staff iau leihau diogelwch cleifion yn y dyfodol.
| “ | Rwy'n cofio'n glir fod rhai cyrsiau yr oeddwn yn disgwyl eu mynychu, yr oeddwn wedi bod yn aros amdanynt ers 2 neu 3 blynedd. Cafodd ei ganslo ac yna yn y pen draw cafodd ei aildrefnu am tua blwyddyn, flwyddyn a hanner yn ddiweddarach. Mae’n bosibl bod hynny wedi effeithio ar fy natblygiad gyrfa.”
-Meddyg ysbyty |
| “ | Felly, ni chawsom ddysgu unrhyw fyfyrwyr meddygol y tro hwnnw. Rwy’n meddwl bod 1 neu 2 swp wedi dod heb gael eu harchwilio a gallaf ddweud wrthych, fel claf, ni hoffwn gael fy nhrin gan unrhyw un ohonynt… dim ond oherwydd ei fod yn gyfnod Covid, a nodwyd fel argyfwng meddygol, rydych yn gostwng y bar cymaint nes bod pob person yn neidio drosto. Y meddygon sydd wedi dod o gwmpas yr amser hwnnw, maen nhw'n anniogel i weithio gyda nhw. ”
-Meddyg ysbyty |
Roedd safbwyntiau gwahanol ymhlith gweithwyr gofal iechyd proffesiynol ynghylch pa mor dda oedd hyfforddiant ar-lein. Roedd rhai cyfranwyr yn teimlo bod hyfforddiant ar-lein yn fwy hygyrch ac yn haws ei gyd-fynd ag amserlen waith brysur. Roedd staff hefyd yn gallu cael mynediad at hyfforddiant cofnodedig yn ddiweddarach os nad oeddent yn gallu bod yn bresennol.
| “ | Daeth rhywfaint o addysg yn fwy hygyrch: roedd cyfarfodydd strategol mawr yn cael eu rhedeg gan y pwyllgor meddygol lleol a oedd yn wych – mynychodd cannoedd o feddygon teulu a chafwyd diweddariadau ar e.e. y brechiad…oherwydd y pwysau amser daeth y cyfarfodydd ar-lein – cadwyd rhai yn bersonol yno wedi bod y newid diwylliannol hwn a mwy o hygyrchedd i hyfforddiant a datblygiad, roedd llawer mwy o ddewis.”
- Meddyg Teulu |
Fodd bynnag, roedd cyfranwyr eraill yn fwy negyddol am hyfforddiant ar-lein yn ystod y pandemig. Dywedodd rhai fod yn rhaid i hyfforddwyr fod yn ddeinamig yn y ffordd yr oedd hyfforddiant yn cael ei ddarparu i annog ymgysylltiad, ac nad oedd hyn bob amser yn digwydd mewn lleoliad rhithwir.
Disgrifiwyd pa mor gyfyngedig oedd hyfforddiant ar-lein ar gyfer rhai pynciau, yn enwedig y rheini a oedd yn canolbwyntio ar elfennau mwy ymarferol o ofal iechyd. Ymhlith yr enghreifftiau roedd darparu gofal ymarferol i gleifion yn ogystal â sgiliau rhyngbersonol. Er enghraifft, mae hyfforddiant trais ac ymddygiad ymosodol fel arfer yn cynnwys cyswllt rhwng cyfranogwyr.
Mae hyfforddiant personol hefyd yn cynnig buddion fel gallu rhwydweithio a chael sgyrsiau anffurfiol gyda chydweithwyr. Dywedodd rhai cyfranwyr fod hyn yn llawer anoddach i'w ailadrodd ar-lein.
Stori CarysMae Carys yn Nyrs Bresgripsiynydd mewn practis meddyg teulu. Pan ddechreuodd y pandemig, rhoddodd ei phractis system brysbennu ffôn ar waith yn gyflym ar gyfer pobl sy'n gofyn am apwyntiadau i leihau cyswllt wyneb yn wyneb ac amlygiad i Covid-19. Roedd hi hefyd yn gyfrifol am ragnodi meddyginiaeth dros y ffôn. “Roedd yn heriol oherwydd ni chawsom unrhyw fath o hyfforddiant na pharatoi ar sut i ddelio ag ef. Tra, fel arfer byddai cleifion yn dod i mewn i’r feddygfa, a byddem yn eu gweld wyneb yn wyneb, roedd yn rhaid inni addasu i allu brysbennu, a oedd yn rhywbeth nad oedd y rhan fwyaf ohonom erioed wedi’i wneud o’r blaen. Mae'n debyg bod meddygon teulu wedi ei wneud, ond yn amlwg nid oeddem ni fel nyrsys, felly roedd yn gyfnod anodd i allu rheoli cyflyrau pobl. Gallai llawer o bethau fynd ar goll, oherwydd gallwch chi ddweud llawer trwy weld claf, a dim ond siarad dros y ffôn, ni allwch wneud yr asesiad hwnnw mewn gwirionedd." Mae'n cofio paratoi ar gyfer y newid hwn yn ei rôl fel rhywbeth sylfaenol iawn ac yn y pen draw, bu'n rhaid iddi addasu a dysgu yn y swydd. Darparodd meddygon teulu arweiniad lefel uchel ar fod yn fanwl gywir gyda'r cwestiynau a ofynnodd, gan nodi baneri coch, a chyfeirio cleifion at 999 pe bai'r cyflwr yn gwaethygu. Ni roddwyd templed o gwestiynau iddi ei defnyddio. Pwysleisiodd Carys y risg o asesu cleifion o bell a chydnabu hefyd ei bod yn sylwi ei bod yn gwella dros amser. “Felly dim ond asesu ac addasu, fel y dywedais, i frysbennu dros y ffôn, rhywbeth nad oedd gennyf unrhyw brofiad blaenorol ohono, dim hyfforddiant. Roedd yn rhaid i chi fwrw ymlaen ag ef, yn y bôn, felly roeddwn i'n teimlo bod llawer o gefnogaeth yn ddiffygiol ar y pryd. Yn amlwg, po fwyaf y gwnaethom ni, y mwyaf y dysgon ni ohono, a gorau oll y gwnaethom ni ei wneud.” |
Cefnogaeth i weithwyr gofal iechyd proffesiynol
Pan brofodd gweithwyr gofal iechyd proffesiynol sefyllfaoedd trallodus a phwysau llwyth gwaith, dywedodd cyfranwyr fod rhywfaint o gymorth ar gael yn aml. Er enghraifft, trafododd un cyfrannwr sut roedd ei gyflogwr wedi creu 'canolfannau cymorth' a oedd yn annog pobl i gymryd seibiannau drwy gydol y dydd.
| “ | Yn sydyn, cawsom ddau neu dri arall o'r slotiau gweinyddol hyn, ac fe'u gelwir yn slotiau lles mewn gwirionedd. Ac rwy’n meddwl ei fod wedi’i gynllunio i roi ychydig o amser segur i ni, ychydig o anadlu, ac oherwydd bod popeth yn cymryd cymaint o amser gyda chleifion i roi ychydig o amser i ni ddal i fyny ar nodiadau a phethau felly.”
– Gweithiwr gofal iechyd proffesiynol perthynol |
Rhoddodd gweithwyr gofal iechyd enghreifftiau o sut y gwnaeth yr ansicrwydd a'r pwysau waethygu cyflyrau iechyd meddwl a oedd yn bodoli eisoes, a chynyddu pryder ac iselder. Roedd rhai cyfranwyr yn gallu cael cymorth emosiynol ac iechyd meddwl trwy eu cyflogwyr. Darparwyd y cymorth hwn mewn amrywiaeth o ffyrdd, o apiau ar-lein i linellau cymorth ffôn neu nifer benodol o sesiynau wyneb yn wyneb gyda therapydd. Ar y cyfan, roedd y cyfranwyr a ddefnyddiodd y cymorth hwn yn ei chael yn ddefnyddiol.
| “ | Mae gennym adran yn y Gymdeithas Fferyllol lle, os oes angen cymorth arnoch, gallwch ffonio'r rhif hwn ac mae rhywun yno i siarad â chi, hyd yn oed nawr. Felly, mae gennym y llinell gymorth honno, oherwydd mae llawer o fferyllwyr yn dal i fod dan straen, yn gweithio dan straen hyd yn oed nawr, felly mae'r fferyllwyr hynny nad ydynt yn gallu ymdopi ond sy'n gorfod gweithio, nid ydynt am adael, yna byddant yn siarad â nhw. y tîm cymorth.”
- Fferyllydd ysbyty |
| “ | Rhithwir yn bennaf ond dyna oedd achos y rhan fwyaf o'r cymorth oedd ar gael. Rwy’n meddwl bod hynny wedi’i wneud yn gymharol dda, roedd yn teimlo bod cymorth ar gael ac rwy’n meddwl bod cryn dipyn wedi manteisio arno.”
- Nyrs ysbyty |
| “ | Llawer o bryder...Dechreuais ysmygu eto oherwydd y straen...roeddwn yn ei chael hi'n anodd iawn...roeddwn i'n ddagreuol llawer. Roedd hi bron yn teimlo'n eithaf manig wrth geisio cadw i fyny â'r rheolau diweddaraf o ran beth oedd yn digwydd, beth oedd hawl i ni ei wneud a beth na allem ni ei wneud. Es i trwy gyfnod pan gefais gwnsela yn y gwaith i fy helpu i ymdopi â’r straen emosiynol.”
– rheolwr practis meddyg teulu |
Ystyriwyd bod cefnogaeth gan gydweithwyr yn arbennig o werthfawr yn ystod y pandemig.
| “ | Cawsom grŵp cymorth bach gyda’r holl nyrsys eraill a oedd yn ceisio siarad â’i gilydd a rhannu ein profiadau. Rhoddodd cwpl o nyrsys y gorau i nyrsio oherwydd eu bod wedi gweld golygfeydd mor erchyll, felly rwy’n meddwl ei bod yn bwysig siarad amdano, am yr hyn yr oeddem wedi’i weld, dim ond rhannu profiadau.”
– nyrs meddyg teulu |
Fodd bynnag, nid oedd y cymorth yn gyson, ac nid oedd rhai gweithwyr gofal iechyd proffesiynol yn cael y cymorth emosiynol ac iechyd meddwl yr oedd ei angen arnynt. Dywedodd eraill nad oeddent yn ymwybodol pa gymorth oedd ar gael, gan ddisgrifio sut y gallai cyfathrebu fynd ar goll mewn amgylcheddau pwysedd uchel.
| “ | Rwy’n gwybod bod cymorth ar gael i staff os oedd ei angen arnynt, doeddwn i ddim yn gwybod ble y byddech chi’n cael mynediad iddo pe bai ei angen arnaf.”
- Nyrs ysbyty |
Teimlai rhai cyfranwyr fod cymorth yn cael ei roi ar waith heb ystyried beth fyddai'n helpu staff fwyaf. Achosodd hyn rwystredigaeth ymhlith y staff hyn.
| “ | Rwy'n teimlo ein bod yn cael gwybod o hyd am yr hyn yr oedd yr ysbyty yn ei wneud ar gyfer staff a phethau, ond nid wyf yn meddwl eu bod erioed wedi gofyn i'r staff beth fyddai'n gwneud gwahaniaeth i fod yn y gwaith. Dwi’n meddwl mai dyna oedd y pethau bach hefyd, fel bydden nhw wedi dweud gallu parcio…gallu mynd am ginio mewn lle ymlacio.”
-Meddyg ysbyty |
Dywedodd rhai cyfranwyr eraill fod y cymorth a gawsant yn ystod y pandemig yn dibynnu ar eu rheolwr llinell a diwylliant y sefydliadau yr oeddent yn gweithio ynddynt.
| “ | Fy rheolwr llinell, hi yw'r un orau i mi ei chael erioed. Yn galonogol, yn ddeallus, yn gefnogol, ie. Felly, ymhellach ymlaen, ie, roedd yn ymddangos bod pawb yn gwneud yr hyn a allent i gefnogi pawb.”
- Gwyddonydd clinigol |
Clywsom rai enghreifftiau penodol o reolwyr llinell yn gweithio gartref ar gyfer llawer o’r pandemig. Arweiniodd hyn at y ffaith bod cyfranwyr yn teimlo nad oeddent yn cael eu cefnogi gyda thasgau a phroblemau o ddydd i ddydd.
| “ | Roedd fy rheolwr yn gweithio o gartref, felly ni allai hi fy nghefnogi i a'm cydweithwyr a oedd yn gweithio. Roedd hi eisiau gweithio o gartref ei hun. Roeddwn i’n arfer ei chael hi’n annifyr ac yn anghefnogol gan fy rheolwr…a dweud y gwir, fe ddylen ni i gyd fod wedi parhau i wneud ein rôl fel yr oedden ni.”
– Gweithiwr gofal iechyd proffesiynol perthynol |
Effaith barhaol y pandemig
Rhannodd llawer o gyfranwyr pa mor niweidiol oedd y pandemig i’w hiechyd meddwl. Teimlai rhai eu bod wedi symud ymlaen, ond yn aml dywedodd gweithwyr gofal iechyd proffesiynol wrthym eu bod yn dal i brosesu'r hyn a ddigwyddodd iddynt. Myfyriodd y cyfranwyr hyn ar eu hatgofion trawmatig o ddarparu gofal yn ystod y pandemig.
| “ | Nid wyf yn meddwl fy mod wedi dod yn ôl i 100% o sut yr oeddwn fel arfer. Mae'n cymryd ei doll. Ond mae bron fel cael y darn hwn o bapur, sy'n neis, a fflat, ac yn syth, ac yna rydych chi wedi'i grychu ac yna rydych chi'n ceisio sythu'r darn hwnnw o bapur eto. Mae wedi cynyddu o hyd, ni waeth faint rydych chi'n ceisio ei sythu."
- Parafeddyg |
| “ | Cafodd effaith fawr a dweud y gwir… ni allem ddatrys llawer o faterion. Roedd gan ein hysbyty penodol ni broblem fawr gyda nifer y marwolaethau yr oeddem yn eu cael, a oedd weithiau tua 80 y dydd, ac oherwydd ein bod fel ysbyty blaenllaw eithaf bach mewn gwirionedd, ni allem storio'r cyrff. Roedd yn rhaid i ni ddod ag uned rhewgell enfawr, fawr, a oedd yn ddigrif, dim ond i roi'r cyrff hyn i mewn. Nid wyf erioed wedi gweld unrhyw beth felly. Roedd hi'n eithaf hoffi mynd i fyny i weld y cyrff wedi'u gosod yn y coridor - oedd, roedd yn emosiynol. Roedd yn eithaf dinistriol gweld, mae’n parhau i gael effaith arnaf.”
- Nyrs ysbyty |
Clywsom rai enghreifftiau o weithwyr proffesiynol a oedd wedi wynebu anawsterau yn eu bywydau megis yfed gormod neu fynd drwy ysgariad. Roedd rhai o'r cyfranwyr hyn yn meddwl bod eu profiadau o leiaf yn rhannol oherwydd y pandemig.
| “ | Yn iach, yn sicr oherwydd dyfodiad fy yfed [a ddechreuodd yn y pandemig] nad yw fy iechyd wedi bod yn rhy dda. Mae gen i iau brasterog ac mae alcohol yn cael effaith gynyddol gyda llawer o bethau.”
- Meddyg Teulu |
| “ | Dechreuon ni daith o wahanu a dod i ysgariad nawr. A fyddai hynny wedi digwydd heb y pandemig? Dydw i ddim yn gwybod, a dweud y gwir. Efallai na fu gen i’r dewrder i’w wneud.”
– rheolwr practis meddyg teulu |
Yn anffodus, dywedodd rhai gweithwyr gofal iechyd proffesiynol wrthym am brofi argyfwng seicolegol yn ystod y pandemig, yr oeddent yn parhau i wella ohono.
| “ | Gan weithio mewn ICU Covid-19, cefais chwalfa gyflawn yn y gwaith. Doeddwn i ddim yn ei weld yn dod. Dywedodd fy nghyd-Aelodau eu bod yn ei weld yn dod mewn gwirionedd. Roeddwn i'n mynd yn bryderus iawn a bron yn grac, fel, wel roeddwn i'n cael fy ystyried yn un o'r nyrsys mwyaf profiadol yn yr Uned, felly roedd unrhyw un o'r achosion mawr a oedd yn dod drwodd yr oeddwn i'n gweithio arnynt, roeddwn i wrth fy modd yn edrych ar ôl, pan oedd llawer yn digwydd. ymlaen roeddwn i'n hoffi bod yno a dod yn drefnus. Ond yn sydyn iawn, fe es i i mewn i'r troell gwbl ar i lawr hwn, ac fe ddigwyddodd dros tua 2 wythnos, dwi'n meddwl, a chyrraedd y pwynt lle nes i dorri i mewn i ddagrau ar yr Uned. Fi jyst yn crio ac yn crio ac yn crio."
– Nyrs Damweiniau ac Achosion Brys |
Dysgu ar gyfer y dyfodol: cymorth i weithwyr proffesiynolEr bod profiadau gwahanol ar draws y gweithlu, dywedodd llawer o weithwyr gofal iechyd proffesiynol wrthym am y pwysau aruthrol a oedd arnynt yn ystod y pandemig. Cafodd hyn effaith niweidiol ar lawer, ac yn enwedig ar eu hiechyd meddwl. Roeddent yn dadlau bod angen dysgu gwersi am gefnogi a gwerthfawrogi gweithwyr gofal iechyd proffesiynol. Roedd rhai eisiau i'r llywodraeth a systemau gofal iechyd wneud mwy i gefnogi a gwobrwyo staff, gan gydnabod effaith barhaol argyfwng fel y pandemig. Roedd eraill eisiau i'r cyhoedd werthfawrogi'r pwysau y mae gweithwyr gofal iechyd proffesiynol yn eu hwynebu o hyd. “Gwerthfawrogi’r staff, y gwahanol weithwyr gofal iechyd proffesiynol, nid dim ond pan fyddwch eu hangen. Gwerthfawrogwch yr hyn y gallant ei wneud, oherwydd o ble rwy'n sefyll, mae'r GIG mewn gwirionedd yn cwympo'n ddarnau, ac mae angen cymorth arno. Mae staff wedi'u draenio. Does ganddyn nhw ddim byd i’w roi, ac mae angen ateb.” Fferyllydd “Yr agwedd a newidiodd pan ddaeth pobl yn fwy beichus a dwi’n meddwl eu bod nhw wedi gohirio pethau yn y pandemig ac roedden nhw eisiau cael eu gweld, ac roedden nhw eisiau cael eu gweld nawr… [ydynt] yn sicr yn llai cydymdeimladol eich bod chi yno yn gwneud eich swydd mewn cyfnod o risg, a dweud y gwir.” Nyrs meddyg teulu Dadleuodd rhai cyfranwyr y dylid cael gwell cefnogaeth ar gyfer iechyd meddwl a lles i staff gofal iechyd mewn pandemigau yn y dyfodol. Roedd rhai cyfranwyr yn dadlau dros gefnogaeth iechyd meddwl mwy cadarn o fewn gofal iechyd, yn enwedig yn ystod galw uwch. Roeddent yn argymell blaenoriaethu adnoddau iechyd meddwl, cynnig gwasanaethau cwnsela, a chreu amgylchedd cefnogol i fynd i'r afael â'r doll emosiynol aruthrol a wynebir gan weithwyr gofal iechyd mewn gwahanol rolau. “Rwy’n credu y gallai mwy o gymorth wedi’i hysbysebu [fod] wedi’i gynnig ar gyfer canlyniad iechyd meddwl effaith Covid ar nyrsys ICU. Rwyf wedi cael cwnsela trwy'r RCN, ond dim ond oherwydd i mi ddod arno ar gyfryngau cymdeithasol. Rydyn ni'n dal i ddioddef. ” Cyfrannwr Mae Pob Stori o Bwys “Rwy’n dal yn drist nad yw’r GIG yn cynnig cwnsela am ddim i staff sydd ag elfen o PTSD o’r pandemig. Mae’n rhaid i ni dalu’n breifat i gael unrhyw gymorth, fodd bynnag, mae fy nghydweithwyr a minnau yn aml yn cael eu prisio gan fod cymorth iechyd meddwl preifat yn ddrud iawn.” Cyfrannwr Mae Pob Stori o Bwys “Roedd angen mwy o gefnogaeth iechyd meddwl ar y GIG ar y pryd. Cafodd 'gweithwyr rheng flaen' driniaeth arbennig mewn adrannau fel adrannau damweiniau ac achosion brys a gofal critigol, ond roedd wardiau'r ysbyty hefyd yn brwydro yn erbyn yr un frwydr. Rhoddwyd basgedi ffrwythau a bariau grawnfwyd i ni pan ddylen ni fod wedi bod yn cael ôl-drafodaeth a therapi rheolaidd.” Cyfrannwr Mae Pob Stori o Bwys |
9. Profiadau o ofal diwedd oes a phrofedigaeth |
 |
Mae’r bennod hon yn amlinellu profiadau o brofedigaeth a gofal iechyd yn ystod y pandemig. Mae'n cynnwys profiadau teuluoedd mewn profedigaeth, gan gwmpasu pa mor heriol oedd cyfathrebu â gweithwyr gofal iechyd proffesiynol a methu ymweld ag anwyliaid sy'n marw neu ymweliadau'n cael eu cyfyngu. Mae hefyd yn rhannu profiadau o sut y rheolwyd gofal diwedd oes, gan gynnwys hysbysiadau DNACPR.
Profiadau teuluoedd o ofal diwedd oes
Roedd teuluoedd mewn profedigaeth, ffrindiau a chydweithwyr yn rhannu sut y gwnaethant Mae profiadau trawmatig eu hanwyliaid yn marw yn yr ysbyty yn ystod y pandemig yn golygu eu bod yn teimlo tristwch dwfn - ac yn aml euogrwydd neu ddicter - sy'n anodd symud y tu hwnt iddo.
| “ | Collais fy nhad ym mis Tachwedd 2021 o Covid-19. Yr oedd yn 65 mlwydd oed. Roedd ganddo chwech o blant, pump o wyrion, gyda dau arall yn ymuno â'n teulu ers iddo ein gadael. Bu farw o fewn chwe diwrnod i gael ei dderbyn i'r ysbyty. Rwy’n dal i gael fy syfrdanu gan feddwl ysbytai a’r ofn a’r boen y mae’n rhaid ei fod wedi’i deimlo.”
- Aelod o'r teulu mewn profedigaeth |
| “ | Rydyn ni wedi colli ffydd ac ymddiriedaeth yn y system gofal iechyd. Mae angen i ni gael ein lleisiau wedi'u clywed…Rwy'n byw gydag euogrwydd am bethau y gallem fod wedi'u gwneud i'w hatal [rhieni] marwolaethau."
- Aelod o'r teulu mewn profedigaeth |
Mae methu â threulio amser gyda'u hanwyliaid a dweud hwyl fawr yn iawn yn golygu ei bod yn llawer anoddach dod i delerau â'u colled. Fe wnaethant rannu'r boen a'r pryder yr oeddent yn ei deimlo o fethu â chynnig cysur, cefnogaeth ac eiriolaeth oherwydd cyfyngiadau pandemig. Dywedodd llawer o deuluoedd a ffrindiau mewn profedigaeth wrthym pa mor ofidus yw hi o hyd i feddwl nad yw eu hanwyliaid yn deall pam nad oedd eu teulu a’u ffrindiau gyda nhw.
| “ | Ni allaf symud y tu hwnt i'm trawma, ni allaf symud trwy'r galar hwn ... bu farw fy nhad o effeithiau unigrwydd, o'r torcalon o fethu â gweld ei wraig a'i deulu, o'r diffyg gofal a chariad y dylai fod wedi'i dderbyn mor haeddiannol. .”
- Aelod o'r teulu mewn profedigaeth |
| “ | Roeddwn i'n teimlo'n ofnadwy, yn hollol dorcalonnus oherwydd roeddwn i'n gwybod, cymaint ag y mae'n debyg ei bod hi'n wael, bod mwy o hynny'n dioddef o beidio â'n gweld. Roeddwn i'n gallu dweud ei bod hi'n fwy o hynny, felly roedd hi'n dorcalonnus gwybod ei bod hi yno...roedden ni yma, fi a fy merch a fy modrybedd... Roedd yn teimlo fel, 'Dydyn ni ddim yn mynd i'w gweld hi eto.''
- Aelod o'r teulu mewn profedigaeth |
Clywsom faint o deuluoedd a ffrindiau mewn profedigaeth a oedd yn meddwl bod eu hanwylyd yn teimlo ei fod wedi'i adael yn yr ysbyty. Fe wnaethant rannu enghreifftiau o weithwyr gofal iechyd proffesiynol ddim yn ymateb i gleifion er eu bod yn galw am gymorth. Mae pobl mewn profedigaeth yn ddealladwy yn ddig, yn sioc ac yn siomedig na chafodd eu hanwyliaid y gofal yr oedd ei angen arnynt yn eu dyddiau olaf.
| “ | Mae tua 6 neu 7 achos wedi bod pan anfonodd neges destun atom i ffarwelio. Byddem yn ceisio ffonio neu anfon neges destun yn ôl ond, wyddoch chi, roedd ei negeseuon testun, oherwydd na allai ddal ei ffôn yn dda iawn, yn aml ychydig yn ddryslyd i ni. Y peth arall oedd ei fod mor wan ar brydiau, nid oedd yn gallu codi ei ffôn ... mae'n gorwedd yn y gwely, nid yw'n gallu symud ... ni all gael mynediad at unrhyw ffurf o gyfathrebu ac maent [gweithwyr gofal iechyd proffesiynol] mor brysur pan fyddai’n pwyso’r gloch yn aml, a neb yn dod.”
- Aelod o'r teulu mewn profedigaeth |
Roedd yna hefyd deuluoedd a ffrindiau mewn profedigaeth a ddisgrifiodd eu hanwylyd yn derbyn gofal gwael ac a ddywedodd eu bod yn credu bod hyn wedi cyfrannu at eu marwolaeth. Er eu bod yn aml yn cydnabod y pwysau ar weithwyr gofal iechyd proffesiynol, roeddent am gael gwell gofal i'w hanwyliaid. Dywedodd rhai cyfranwyr eu bod yn teimlo'n euog nad oedden nhw'n gallu eirioli mwy ar eu rhan. Roedd hyn yn ei gwneud hi'n anoddach i deuluoedd a ffrindiau mewn profedigaeth ddod i delerau â'u colled.
| “ | Fe gollon ni fy nhad am 36 awr [yn yr ysbyty]; aethpwyd ag ef yma ac acw a’i adael am oriau ar ei ben ei hun wedi parcio mewn ambiwlans heb fwyd na dŵr.”
- Aelod o'r teulu mewn profedigaeth |
| “ | Daliais hi [nain] law a hi a ddywedodd, ' Yr oeddwn yn meddwl dy fod wedi fy ngadael, ac yr oedd cymaint o ofn arnaf.' Dywedais, 'rydym wedi bod yn ceisio'ch cael chi adref.' Daeth adref ar y dydd Mercher, a bu farw ar y Sul. Roedd hi wedi cael ei gadael yn llythrennol. Roedd hi wedi'i gorchuddio â doluriau gwely, ar ei thraed, ar ei phen ôl. Yn amlwg doedd hi ddim wedi bod yn bwyta. Yn amlwg doedd hi ddim wedi bod yn yfed. Roedd yn ofnadwy.”
- Aelod o'r teulu mewn profedigaeth |
| “ | Fe wnaethon nhw ei symud i ward Covid-19, ar ddiwrnod 4 ni welodd unrhyw un trwy'r dydd. Roedd ei gathetr wedi'i rwystro, doedd ganddo ddim help, gan fy ffonio mewn dagrau i ddweud wrthyf i'r nyrs ddweud nad oedd ganddyn nhw halwyn i'w olchi allan. Ffoniais am hanner nos a dywedodd y nyrs, 'beth ydych chi am i mi ei wneud am y peth?'.”
- Aelod o'r teulu mewn profedigaeth |
Y straeon a rannwyd gyda ni gan anwyliaid mewn profedigaeth hefyd cynnwys enghreifftiau o weithwyr gofal iechyd proffesiynol yn cynnig gofal diwedd oes rhagorol ac arloesol yn ystod y pandemig. Disgrifiodd y teuluoedd hyn pa mor gefnogol oedd staff a faint y gwnaeth hyn wella gofal diwedd oes eu hanwyliaid. Un enghraifft gyffredin oedd gweithwyr iechyd proffesiynol yn torri canllawiau Covid-19 i ddarparu cysur corfforol tra roedd y claf yn marw.
| “ | Rwy'n cofio, roedd un nyrs fel, 'O, roedd dy dad eisiau i mi roi cwtsh i chi, a dweud, “Dyma gwtsh.”' Yn amlwg, doedd dim angen iddi wneud hynny…Dydych chi ddim hyd yn oed i fod i fod. dod yn agos, ond y math yna o deimlad trugarog, ac roeddwn i'n union fel, o fy Nuw, sydd mor braf i'w weld mewn person meddygol."
- Aelod o'r teulu mewn profedigaeth |
| “ | Cefais alwad ffôn i ddweud nad oedd ganddi hir ac a oeddwn i eisiau galwad fideo eto. Wrth gwrs, fe wnes i, a'r tro hwn siaradodd Dad â hi dros y ffôn yn erbyn y gliniadur. Roeddwn ar yr alwad am amser hir ac yn gallu gweld y gofal yr oedd yn ei gael gan y staff nyrsio anhygoel.”
- Aelod o'r teulu mewn profedigaeth |
Rhannodd cyfranwyr eraill sut oedd gweithwyr gofal iechyd proffesiynol vRoeddem yn gofalu am anwyliaid mewn profedigaeth ac yn myfyrio ar ba mor drawmatig ydoedd i staff gofalu am gleifion sy’n dod i ddiwedd eu hoes.
| “ | Edrychodd y nyrs arnaf, dim ond ei llygaid uwchben y mwgwd y gallai ei gweld, a gofynnodd a oeddwn yn iawn a dywedais, 'ydych chi'n iawn? Rydych chi'n gofalu amdanyn nhw ac yn treulio 30 munud olaf eu bywyd gyda nhw.' Fy mhryder i oedd nyrsys sy’n gorfod profi’r trawma hwnnw a pharhau ag ef.”
- Aelod o'r teulu mewn profedigaeth |
Cyfathrebu yn ystod gofal diwedd oes
Dywedodd llawer o'r rhai mewn profedigaeth y clywsom ganddynt ni chawsant esboniadau clir gan weithwyr gofal iechyd proffesiynol am yr hyn a oedd yn digwydd ar ddiwedd bywydau eu hanwyliaid. Mae hyn wedi gwneud eu profiad anodd o golled hyd yn oed yn fwy o straen a gofid.
| “ | Roedden ni wedi dychryn heb wybod beth oedd yn digwydd. Rwy’n teimlo y gallem fod wedi cael mwy o wybodaeth drwy gydol yr holl broses o’r hyn oedd yn digwydd.”
- Aelod o'r teulu mewn profedigaeth |
Roedd y profiadau hyn yn fwy cyffredin yn gynnar yn y pandemig, pan ddywedodd llawer nad oeddent yn gallu darganfod beth oedd yn digwydd gydag aelodau eu teulu. Roedd y diffyg cyfathrebu hwn hefyd yn golygu nad oeddent yn rhan o benderfyniadau am eu gofal.
| Storïau gan bobl mewn profedigaeth
Siaradodd pobl mewn profedigaeth mewn digwyddiad gwrando Mae Pob Stori’n Bwysig am broblemau cyfathrebu â gweithwyr gofal iechyd proffesiynol sy’n gofalu am eu hanwyliaid. Disgrifiasant lawer o anawsterau wrth geisio cysylltu â'u hanwyliaid neu ddarganfod beth oedd yn digwydd iddynt. Roedd hyn yn cynnwys oedi cyn cael diweddariadau am gyflwr eu hanwyliaid, cynlluniau triniaeth a phenderfyniadau. Roedd hyn yn gadael teuluoedd mewn profedigaeth yn teimlo'n bryderus ac yn anwybodus. “Roedd y cyfathrebu a phopeth yn ofnadwy. Ychydig cyn i fy nhad farw roedden ni’n cael adroddiadau da ac yn sydyn fe ddywedon nhw ei bod hi’n bryd dod â’r teulu at ei gilydd.” Aelod o deulu mewn profedigaeth Roedd y teuluoedd hyn mewn profedigaeth eisiau cyfathrebu mwy tryloyw a chael eu cynnwys yn fwy yn y broses ofal. “Doedden ni ddim yn cael rhoi unrhyw fewnwelediad i helpu gyda'u gofal. Pe byddem wedi cael ymweld â fy nhad byddem wedi gwybod nad oedd yn ffit i gael ei anfon adref. Pe baem wedi gallu ymweld â mami byddem wedi gallu sylwi ar bethau cyn ei bod yn rhy hwyr.” Aelod o deulu mewn profedigaeth |
Disgrifiodd rhai cyfranwyr pa mor anodd oedd hi i gysylltu â gweithwyr gofal iechyd proffesiynol pan oeddent am anfon cyflenwadau personol neu rannu negeseuon terfynol â'u hanwyliaid.
Stori Phillipa ac AliceDywedodd Phillipa wrthym am yr amgylchiadau torcalonnus ynghylch marwolaeth ei nain annwyl, 95 oed, Alice. Roedd Alice wedi byw gyda Phillipa ers pum mlynedd cyn y pandemig Roedd y ddwy ddynes yn rhannu cwlwm anhygoel o agos - dywedodd Philippa wrthym nad ei mam-gu yn unig oedd Alice, ond un o'i ffrindiau gorau a'i hysbrydoliaeth. Pan darodd y pandemig, cysgododd Phillipa ac Alice gyda'i gilydd. Un diwrnod syrthiodd Alice, gan dorri ei choes yn ddifrifol. Er gwaethaf ymdrechion Phillipa i atal y gwaedu, galwyd ambiwlans, ac aethpwyd ag Alice i'r ysbyty yn groes i ddymuniad Phillipa. Roedd hi wedi bod eisiau gofalu am ei nain gartref o ystyried y risgiau o fynd i'r ysbyty ar y pryd. Am y pedair wythnos nesaf teimlai Phillipa fod Alice yn mynd ar goll yn yr ysbyty gorlawn, heb ddigon o staff. Galwodd Phillipa ac aelodau eraill o'r teulu yn ddyddiol i ddarganfod beth oedd yn digwydd i Alice ac i geisio ei chael hi adref. Yn y cyfamser, contractiodd Alice Covid-19 yn yr ysbyty. Pan ganiatawyd i Alice ddod adref o'r diwedd, cafodd Phillipa sioc gyda'i chyflwr - roedd hi wedi colli pwysau ac wedi'i gorchuddio â dolur gwely. Bu farw Alice ychydig ddyddiau yn ddiweddarach. Mae Phillipa wedi'i syfrdanu gan yr unigrwydd, yr ofn a'r boen y mae'n rhaid bod Alice wedi'u profi. Mae hi'n teimlo bod yr ysbyty wedi'i hesgeuluso ac wedi lladd ei nain yn y pen draw. “Rydw i mor grac nes bod rhywun yn meddwl bod ganddyn nhw'r hawl i gadw fy nain, fy nghnawd a gwaed fy hun, draw oddi wrthym ni. Ni allem fynd i'w gweld, ac ni allem ddod o hyd iddi. Roedd hi’n teimlo fel petaen ni wedi ei gadael, fel petaen ni newydd ei gadael hi.” Mae'r niwed i iechyd meddwl a chorfforol Phillipa wedi bod yn ddifrifol. Mae hi'n cael trafferth teimlo'n isel ei hwyliau, yn bryderus am adael y tŷ ac yn anobeithiol. “Mae wedi fy ngadael â galar ofnadwy, naws ar fy ysgwydd… y gall rhywun gymryd y pethau mwyaf gwerthfawr yn eich bywyd, eich anwyliaid, a'u cadw, fel pe bai ganddynt yr hawl i wneud y penderfyniad hwnnw. Roeddwn i'n ffodus, cefais fy nain adref, ond fe wnaethon nhw ei lladd hi ... dwi'n gwybod bod Covid-19 yn ddrwg, ond fe wnaethon nhw roi Covid-19 i lawr gan nad oedd ei marwolaeth hi ac nid Covid-19 oedd ei marwolaeth. Ei marwolaeth oedd yr ysbyty a’i lladdodd.” |
Dywedodd llawer o deuluoedd a ffrindiau mewn profedigaeth nad oedd ganddynt unrhyw gyswllt, neu gyswllt trwy alwad fideo yn unig, ag anwyliaid ac roeddent yn meddwl y gellid bod wedi gwneud mwy i'w helpu i ffarwelio. Disgrifiodd llawer o straeon mai dim ond un person), neu deulu agos yn unig, a allai siarad â chlaf a oedd yn marw ar y ffôn neu drwy alwad fideo. Roedd hyn yn golygu nad oedd perthnasau eraill yn cael sgyrsiau gyda'u hanwyliaid. Dywedodd teuluoedd mewn profedigaeth wrthym eu bod yn meddwl y gellid bod wedi rheoli hyn yn well. Roeddent yn aml yn rhannu sut y byddai mwy o aelodau o'r teulu yn gallu siarad â'u hanwyliaid wedi eu helpu i alaru.
| “ | 'O dim ond teulu agos ydyw. Dim ond teulu agos.' Ond dyma ofal diwedd oes rydych chi'n ei roi. Gallaf ddeall os oes gennych 100 o gleifion yno, nid oes gennych yr amser i FaceTime pawb, ond gofal diwedd oes ydyw. Hyd yn oed os ydych yn ei gyfyngu i FaceTime 5 munud, dylech allu dod o hyd i’r amser ar gyfer hynny, ond nid oedd yn syml o gwbl.”
- Aelod o'r teulu mewn profedigaeth |
Roedd teuluoedd a ffrindiau mewn profedigaeth yn meddwl y dylai galwadau fideo fod wedi digwydd yn gyson. Roedd rhai eisiau mwy o dosturi gan weithwyr gofal iechyd proffesiynol a mwy o hyblygrwydd mewn canllawiau i alluogi hyn i ddigwydd.
| “ | [Fy nhad] bu yn yr ysbyty am 7 diwrnod ac yna cefais alwad ffôn gan y ward yn dweud nad oedd yn gallu goddef y peiriant CPAP bellach. Roeddwn yn gallu siarad ag ef ar y ffôn, ond nid oedd ganddynt dabledi i wneud galwadau fideo, felly nid oeddwn yn gallu ei weld hyd yn oed ar fideo. Bu farw’n ddiweddarach y noson honno ar 11 Ebrill heb deulu o’i gwmpas.”
- Aelod o'r teulu mewn profedigaeth |
| “ | gwn [ewythr fy] Caniatawyd i'm merch i FaceTime ond roedd hynny'n ofnadwy, a chyrhaeddodd bwynt lle na es i hyd yn oed i'r angladd oherwydd fy mod wedi cynhyrfu cymaint, ac ni allwn gael y cau oedd ei angen arnaf. Rwy'n gwybod bod fy mam wedi cynhyrfu'n fawr â mi, ond dywedais, 'Ni allaf fynd i'r angladd. Ni allaf ei wneud…'”
- Aelod o'r teulu mewn profedigaeth |
| “ | Roedd fy mam yn gorwedd ar wely gyda rhywbeth allan o le yn sefyll wrth ei hymyl [staff mewn PPE], dywedwyd wrthi i chwifio at ei theulu ar iPad, chwifiodd fel plentyn a daeth yr alwad chwyddo i ben. Dywedodd y meddyg wrthi nad oedd hi'n mynd i ddeffro eto, felly fe chwifio mor galed i ffarwelio â'i theulu. Ni allwn gredu bod y meddygon wedi dweud hynny wrthi, na fyddai'n deffro ar ôl y peiriant anadlu. Fe wnaethon ni wylio ein mam ar iPad ar beiriant anadlu yn marw. ”
- Aelod o'r teulu mewn profedigaeth |
Roedd llawer o deuluoedd a ffrindiau mewn profedigaeth yn rhannu pa mor bryderus oeddent am eu hanwyliaid yn cael eu hynysu a'u drysu. Rhannodd rhai straeon am gleifion yn methu â defnyddio technoleg i gadw mewn cysylltiad.
Ymweld i ffarwelio
Roedd pobl mewn profedigaeth yn ei chael yn drallodus ac yn dorcalonnus iawn pan na allent ymweld â'u hanwyliaid. Mae'r straeon a rennir yn tynnu sylw at y ffaith bod y canllawiau ar gyfer ymweliadau ysbyty yn anghyson ac wedi newid yn ystod y pandemig. Roeddent yn amrywio o ysbyty i ysbyty, rhwng adrannau ysbyty, a chawsant eu cymhwyso'n wahanol gan staff. Roedd cyfranwyr yn aml yn teimlo bod diffyg tosturi yn y canllawiau a oedd ar waith ac y dylent fod wedi’u rhoi ar waith gyda mwy o sensitifrwydd a hyblygrwydd.
| “ | Pan wyddys bod rhywun yn marw, mae'n teimlo'n annynol ac yn ddideimlad, i'r sawl sy'n marw a'i deulu, gael ei wahardd rhag ymweld. Mae marwolaeth aelod o'r teulu yn foment eithriadol mewn bywyd. Fy ngobaith diffuant yw y bydd gweithdrefnau yn eu lle i ganiatáu ymweld mewn unrhyw sefyllfaoedd yn y dyfodol.”
- Aelod o'r teulu mewn profedigaeth |
| “ | Rwy'n meddwl nad oedd pobl hŷn yn gweld eu gwragedd, ac ati - hynny i gyd, rwy'n meddwl bod hynny'n erchyll, ac rwy'n meddwl bod yna ffordd o gwmpas hynny. Cael nhw [ymwelwyr] eu profi a gadael iddynt fynd i mewn. Rwy'n meddwl mai dyna oedd un o'r camgymeriadau mawr, yn bersonol o fy safbwynt i.”
- Ffrind claf Covid-19 |
Mewn rhai achosion, dywedodd teuluoedd eu bod yn cael ymweld fel eithriad neu wrth i'r cyfyngiadau ar ymweld leihau.
| “ | Gwelais fy mam y diwrnod cyn iddi farw, a gadawodd yr ysbyty fi i mewn i'w gweld oherwydd ei bod mewn ystafell ar ei phen ei hun ... cefais yr argraff eu bod yn gwneud eithriad oherwydd yr amgylchiadau yr oedd fy mam ynddi.”
- Aelod o'r teulu mewn profedigaeth |
Yn aml, dim ond un person oedd yn cael ymweld, neu roedd y niferoedd wedi'u cyfyngu'n ddifrifol. Dywedodd y rhai a rannodd y profiadau hyn wrthym mor annychmygol oedd gorfod penderfynu pwy ddylai ymweld. Mewn rhai achosion, arweiniodd hyn at wrthdaro a rhaniadau o fewn teuluoedd.
| “ | Yn anffodus, cymerodd fy ngŵr dro er gwaeth. Cawsom ein galw i’r ysbyty gan nad oedd dim byd arall y gallent ei wneud. Mae gen i 4 o blant oedd eisiau gweld eu tad ond ni chaniatawyd hynny. Dim ond fy mab hynaf allai fod gyda mi, a oedd yn peri gofid iddynt orfod dweud eu hwyl fawr trwy iPad yn y maes parcio yn yr ysbyty.”
- Aelod o'r teulu mewn profedigaeth |
| “ | Yn y bôn, roeddent yn dweud wrthym, 'Nid yw'n mynd i oroesi.' Ac yna, dywedwyd wrthym mai dim ond un ohonom oedd yn cael mynd i'w weld oherwydd dim ond un ymwelydd dynodedig oedd ganddo. Felly roedd hynny'n anodd iawn, oherwydd pwy sy'n ei wneud?"
- Aelod o'r teulu mewn profedigaeth |
Disgrifiodd rhai o'r straeon sut roedd yn rhaid i bobl wisgo PPE i ymweld â'u hanwyliaid oedd yn marw. Clywsom am y torcalon o fethu â chyffwrdd yn gorfforol â’r rhai yr oeddent yn ymweld â nhw. Dywedodd cyfranwyr hefyd fod rhieni hŷn â dementia yn ofni oherwydd bod eu perthnasau yn gwisgo PPE.
| “ | Caniatawyd i fy merch a minnau fynd i'w weld [gŵr], ar ôl mynd trwy sawl cam i roi offer PPE ymlaen. Dywedwyd wrthym, er ei fod yn anymwybodol, mae'n debyg y gallai ein clywed, a buom yn siarad ag ef, ond torrodd fy nghalon na allwn ei ddal yn fy mreichiau. Roeddwn i’n gallu dal ei law a strôc ei wyneb, ond nid oedd yr un peth yn gorfod gwisgo menig.”
- Aelod o'r teulu mewn profedigaeth |
| “ | Roedd fy nhad, claf gofal dementia... wedi dychryn, ac roedd wedi dychryn, roedd yn meddwl ei fod mewn cartref meddwl. Hynny yw, o'i ganfyddiad, y cyfan y gallai ei weld oedd pobl yn cerdded o gwmpas fel siwtiau gofod, wyddoch chi? Ac ni allai neb esbonio iddo oherwydd bod ei feddwl eisoes ar y cam lle nad oedd meddwl rhesymegol yno mwyach.”
- Aelod o'r teulu mewn profedigaeth |
Profiadau o hysbysiadau DNACPR
Peidiwch â cheisio dadebru cardiopwlmonaidd (DNACPR) argymhellion meddygol a ysgrifennwyd gan feddyg. Maent yn argymell na ddylai gweithwyr gofal iechyd proffesiynol geisio adfywio cardio-pwlmonaidd os yw claf yn rhoi'r gorau i anadlu neu os yw ei galon yn peidio â churo. Gelwir y rhain weithiau yn DNR (peidiwch ag adfywio) neu DNAR (peidiwch â cheisio dadebru). Mae hyn yn wahanol i gynllun uwchgyfeirio triniaeth, sy'n cael ei roi ar waith i helpu i gofnodi a chyfleu nodau triniaeth pan fydd rhywun yn dod tuag at ddiwedd eu hoes.
Clywsom sut yr oedd rhai cleifion yn trafod hysbysiadau DNACPR eu hunain, ond roedd eraill yn dibynnu ar y rhai sydd agosaf atynt. Amlygodd hyn bwysigrwydd cynnwys anwyliaid yn gynnar mewn trafodaethau am hysbysiadau DNACPR. Roedd anawsterau wrth gysylltu â'r gweithwyr gofal iechyd proffesiynol perthnasol yn gwneud hyn yn fwy heriol. Roedd rhai teuluoedd a ffrindiau mewn profedigaeth yn ofnus ac yn poeni am beth fyddai'n digwydd pe na allent eiriol dros eu hanwyliaid.
| “ | Hwn oedd yr amser mwyaf brawychus i mi a fy nheulu gan ein bod ni i gyd yn meddwl fy mod yn mynd i farw o ystyried fy mhroblemau anadlol difrifol. Teimlaf y gallai’r ysbyty fod wedi cysylltu mwy gyda fy mab a’m merch yn enwedig ynghylch y DNR gan nad oeddwn yn ddigon iach i wneud penderfyniad mor bwysig ar y pryd.”
- Claf yn yr ysbyty gyda Covid-19 |
Clywsom mai dim ond ar ôl i’w hanwyliaid farw, neu ar ôl iddynt gael eu rhyddhau o’r ysbyty, y darganfu rhai pobl fod hysbysiad DNACPR wedi’i roi ar waith.
| “ | Doedden ni ddim yn gwybod bod ganddo DNR…ac roedd gan fy mam bŵer atwrnai…Yr unig reswm rydyn ni'n ei wybod yw oherwydd pan gafodd ei ryddhau, roedd yn ei becyn. Ond y ffaith nad oeddem yn rhan o'r penderfyniad a gwybod bod gan dad Alzheimer's. Roedd yn teimlo fel eu bod yn taflu hen bobl i ffwrdd. Roedd fel nad ydyn nhw'n flaenoriaeth oherwydd eu bod nhw'n hen."
– Gofalwr claf Covid-19 |
| “ | Ymgynghorydd cyntaf fy mam [yn yr ysbyty] rhoi nodiadau fy nhad yn anghywir [o'i gyfaddefiad Covid-19] iddi hi a’i rhoi ar DNACPR – ni chawsom wybod am hyn, ni ofynnwyd i ni egluro ei hanes meddygol, roeddem yn gwbl anghofus, yn gwbl anymwybodol o’r canlyniadau ar ei thriniaeth.”
- Aelod o'r teulu mewn profedigaeth |
Rhannodd teuluoedd mewn profedigaeth sut y credant fod henaint neu gyflyrau iechyd presennol wedi arwain at weithwyr gofal iechyd proffesiynol yn rhoi hysbysiad DNACPR ar waith.
| “ | Galwodd ymgynghorydd i ddweud ei fod [gŵr â dementia a Covid] yn sâl iawn [ar ôl cwympo yn yr ysbyty], ni allwn ddeall pam, roedd yn gryf yn gorfforol, dywedodd yr ymgynghorydd, 'gallwch ddadlau os hoffech fy mod wedi gwneud penderfyniad', mae wedi ymddiheuro i mi ers hynny. Gofynnais a oedd y diagnosis dementia yn effeithio ar y penderfyniad [DNACPR] ac ni roddodd ateb."
- Aelod o'r teulu mewn profedigaeth |
Roedd argymell DNACPRs heb eu trafod ag anwyliaid yn cael ei ystyried yn arbennig o amhriodol lle roedd gallu cleifion yn gyfyngedig. Roedd hyn yn cynnwys lle roedd gan berthnasau atwrneiaeth arhosol. Roedd y profiadau hyn yn fwy cyffredin ymhlith perthnasau pobl hŷn a phobl anabl.
| “ | Cefais neges llais gan y cofrestrydd yn dweud wrthyf fod gan mam sepsis ac fe wnaethant roi DNR arni. Dywedais fod gennyf atwrneiaeth, ond dywedasant fod angen inni weld copi o hwn cyn trafod unrhyw beth. Yna bu'n rhaid i mi gysylltu â chyfreithiwr, a oedd ar gau, i gael copi wedi'i argraffu. Euthum i'r ysbyty a gwneud iddynt dynnu'r DNR a dweud na allwch wneud hyn heb fy nghaniatâd, ond dywedasant y gallwn, oherwydd ei bod dros 60 oed. Buont yn siarad am ansawdd ei bywyd, mae ganddi beth da iawn. ansawdd bywyd, mae ganddi wyrion! Sut ydych chi'n penderfynu pwy sy'n byw a phwy sy'n marw?"
- Aelod o'r teulu mewn profedigaeth |
| “ | Ar arhosiad arall yn yr ysbyty, er ei bod yn fyddar, heb unrhyw gymorth clyw ynddi neu gyda hi ac yn methu â siarad oherwydd ei bod wedi goroesi strôc, rhoddwyd DNR ar waith heb unrhyw gyfathrebu â hi nac unrhyw aelod o’r teulu a oedd yn bresennol. Dywedais yn glir NA dros y ffôn ac fe’i hanwybyddwyd yn llwyr.”
– Gofalwr |
Teimlai rhai anwyliaid dan bwysau i gytuno â phenderfyniad DNACPR. Fe wnaethon nhw dynnu sylw at y sylw yn y cyfryngau i Covid-19, a'r ofn roedd hyn yn ei greu. Ar y pryd pwysleisiodd y cyfryngau pa mor beryglus oedd Covid-19 i rai mathau o bobl, a faint o bwysau oedd ar systemau gofal iechyd. Rhannodd rhai cyfranwyr sut roedd hyn yn golygu nad oedd gan gleifion lawer o obaith yn aml o wella o'r afiechyd, yn enwedig os oeddent yn hŷn neu â chyflyrau iechyd a oedd yn bodoli eisoes. Dywedodd rhai teuluoedd fod eu hanwyliaid yn cytuno i DNACPRs pan fyddant yn credu na ddylent fod wedi gwneud hynny.
| “ | Mae rhan ohonoch yn dymuno hynny, os nad oedd yn Covid-19, ac fe ddigwyddodd hynny [daeth taid yn sâl], a fyddai wedi gwneud hynny [cytuno i DNR]? A fyddai wedi dweud, 'Nid wyf am gael fy nwyn yn ôl'? Ond os oedd yn gyfiawn, roedd yn sâl, yn 69 oed, yna byddai'r ysbyty wedi gwneud popeth o fewn ei allu. Ni fyddent yn dweud, 'O, rydym yn atal unrhyw driniaeth.' Bydden nhw'n dal i ymladd.”
- Aelod o'r teulu mewn profedigaeth |
| “ | Cawsoch eich gwthio i mewn iddo [llofnodi hysbysiad DNACPR]. Rwy'n credu mai oherwydd ei fod o oedran penodol a bod ganddo rai cyflyrau iechyd, fe benderfynon nhw hynny. Peidiwch â’m gwneud yn anghywir, mae’n debyg y byddai wedi bod eisiau DNR beth bynnag, ond cafodd ei wthio i mewn iddo gan feddygon a nyrsys, 100%.”
- Aelod o'r teulu mewn profedigaeth |
Roedd penderfyniadau DNACPR yn cael eu gwneud yn wahanol yn dibynnu ar yr amgylchiadau. Roedd gwneud penderfyniadau arafach yn cynnig mwy o amser i gleifion a pherthnasau brosesu'r penderfyniad a'r hyn yr oedd yn ei olygu. Roedd enghreifftiau o hyn fel arfer yn digwydd gartref neu gyda chymorth meddygon teulu. Pan ddigwyddodd hyn, dywedodd rhai teuluoedd mewn profedigaeth wrthym eu bod wedi canfod eu bod yn gallu ymdopi'n well â'u colled gan fod amser wedi'i gymryd i ystyried y penderfyniad yn llawn.
| “ | Gwyddom hynny o'r cychwyn cyntaf [penderfynwyd eisoes ar DNR]. Felly, pan oedd yn yr ysbyty, dywedodd y meddyg, 'Edrychwch, a oes angen ichi roi DNR yn ei le, neu beth bynnag.' Felly, fe wnaethon ni oherwydd dyna beth roedd e eisiau.”
- Aelod o'r teulu mewn profedigaeth |
| “ | Rydyn ni'n credu mai dyna beth fyddai mam-gu wedi'i ddymuno oherwydd bod ganddi ddementia bryd hynny, ond mae hi bob amser wedi dweud, 'Rwyf wedi cael fy mywyd, rwyf wedi cael batiad da, a phan fyddaf yn mynd ...' mae hi eisiau mynd. Nid yw hi eisiau hongian o gwmpas. Felly, fe wnaethon ni siarad am hynny.”
- Aelod o'r teulu mewn profedigaeth |
Roedd rhai cyfranwyr yn beio iaith dechnegol am ddryswch ynghylch yr hyn yr oedd hysbysiadau DNACPR yn ei olygu iddyn nhw a’u hanwyliaid. Cynyddodd hyn gamddealltwriaeth a gallai arwain at gwestiynau heb eu hateb ynghylch sut y cymhwyswyd y rhain.
Stori NoorYn ystod y pandemig, derbyniwyd tad Noor i'r ysbyty oherwydd ei gyflyrau iechyd presennol. Tra roedd yno, derbyniodd Noor a'i theulu alwad brysiog ac annisgwyl gan feddyg am DNACPR. Achosodd y sgwrs ddryswch a straen mawr. Y sioc fwyaf oedd pa mor gyflym yr aeth pethau ymlaen – o gael ei dderbyn i DNACPR yn cael ei drafod. Ychwanegodd yr iaith feddygol a ddefnyddiwyd i ddisgrifio sefyllfa ei thad at y dryswch. Teimlai Noor ei fod wedi cyfrannu at sgwrs â'i mam nad oedd yn ddigon gwybodus am gymhwyso DNACPR i dad Noor. Roedd hyn yn rhywbeth roedd hi eisiau ei newid yn gyflym. Teimlai hefyd fod y ffordd yr esboniodd gweithwyr gofal iechyd proffesiynol bethau yn ei gwneud hi'n anodd deall sut y daethant i argymell DNACPR. “Mae'n rhaid bod rhywun wedi pigo, fel, ydych chi eisiau DNR ar eich gŵr, ac roedd mam yn debyg, ie. Ond yna mae'n rhaid ei bod hi wedi ffonio fi neu fy mrawd, a dwi'n ei chofio hi'n dweud wrthon ni. 'O, fe wnaethon nhw fy ffonio a dweud, 'Ydych chi eisiau DNR?' felly dywedais ie.' Roeddem ni fel, 'Ydych chi hyd yn oed yn gwybod beth yw DNR?' ac roedd hi fel, 'Na, nid wyf yn gwybod, ond dywedais ie yn unig oherwydd fy mod yn cymryd yn ganiataol ei fod yn rhyw fath o driniaeth. Roedd yn rhaid i ni fynd yn ôl yn syth ar y ffôn.” Roedd Noor yn gweld y profiad o wneud penderfyniadau DNACPR yn hynod o anodd. Roedd yn arbennig o ofidus i gael ei holi droeon ynghylch a ddylai ei thad gael ei ddadebru pe bai'r achlysur yn codi. Digwyddodd hyn bob un o'r pum gwaith y cafodd ei drosglwyddo i ward wahanol. Holwyd ei thad hefyd bob tro. Er ei bod yn cydnabod y pwysau ar staff ysbytai ar y pryd, teimlai fod trafodaethau'n cael eu trin yn ansensitif iawn. Mae hi'n dal i ofni pan fydd ei thad yn cael ei dderbyn i'r ysbyty nawr. “Rydyn ni wedi dweud yn benodol nad ydyn ni eisiau DNR bum gwaith. Mae'n cymryd un person i wneud y llithriad hwnnw a allai fod wedi costio bywyd rhywun. Roeddwn i'n meddwl i mi fy hun, dychmygwch os nad oedden ni, fel, ar ben y peth. Allwch chi ddychmygu? Felly nawr, mae gen i ofn bob tro mae dad yn mynd i mewn.” |
Er gwaethaf yr heriau, dywedodd llawer o berthnasau wrthym eu bod yn parhau i chwarae rhan bwysig mewn penderfyniadau gofal diwedd oes yn ystod y pandemig. Roedd y pwysau ar wasanaethau yn gwneud i deuluoedd deimlo bod eu rôl fel eiriolwr yn arbennig o bwysig.
Roedd yr angen hwn am eiriolaeth yn arbennig o bwysig o ran trafodaethau am hysbysiadau DNACPR. Dywedodd llawer o gyfranwyr ag anwyliaid sy'n marw eu bod am barhau i fod yn rhan o benderfyniadau gofal iechyd am eu gofal, yn enwedig ar gyfer y rhai a oedd yn agored i niwed ac yn llai abl i eiriol drostynt eu hunain. Roedd rhai teuluoedd mewn profedigaeth yn pryderu y dylai eu hopsiynau triniaeth eraill fod wedi cael eu hystyried cyn i hysbysiadau DNACPR gael eu cymhwyso.
Dysgu ar gyfer y dyfodol: profedigaeth a gofal diwedd oesClywsom gan lawer o bobl mewn profedigaeth a oedd am i wersi gael eu dysgu o'r niwed a wnaed pan fu farw eu hanwyliaid yn ystod y pandemig. Galwodd llawer am fwy o empathi a thosturi tuag at y rhai a oedd yn agored i niwed mewn ysbytai a lleoliadau gofal iechyd eraill. Roeddent eisiau mwy o gydnabyddiaeth ac ymgynghori â theuluoedd a gofalwyr eraill, a gwell cymorth a chyfathrebu i adlewyrchu hyn. “Dylai fod cyfathrebu gwell wedi bod gyda theuluoedd am eu hanwyliaid a dylem fod wedi cael y cyfle i ffarwelio.” Cyfrannwr Mae Pob Stori o Bwys “Ymagwedd fwy strategol at gydnabod a meddwl yn benodol iawn am y meysydd gofal hyn, diwedd oes lliniarol, profedigaeth ond [hefyd] ymweld ar gyfer teuluoedd.” Staff gofal lliniarol Dywedodd rhai cyfranwyr na ddylai atal anwyliaid rhag ymweld â chleifion sy’n marw fod wedi digwydd. Roedd llawer yn dadlau dros ddull gwahanol yn y dyfodol a fyddai’n caniatáu ymweliadau yn ystod gofal diwedd oes, neu i bobl farw gartref gyda’u hanwyliaid. Byddai hyn yn cynnig mwy o dosturi i gleifion a'u teuluoedd. “Meddyliwch am bobl fregus mewn ysbytai a chartrefi gofal. Os bydd hyn yn digwydd eto, meddyliwch am y teulu. Roedden ni eu hangen ac roedden nhw ein hangen ni. Cawsom ein gwadu hynny.” Aelod o deulu mewn profedigaeth “Dylai o leiaf un aelod o’r teulu fod wedi cael eistedd gyda pherthynas sy’n marw (mewn PPE), ni ddylai unrhyw un farw ar ei ben ei hun yn yr 21ain ganrif.” Cyfrannwr Mae Pob Stori o Bwys “Wrth edrych ar y ffordd yr ymdriniwyd â’r broses o ddod â bywyd claf i ben mewn sefyllfa o’r fath, gan ystyried yr effaith barhaol ar berthnasau agos, (a allai arwain yn ddiweddarach at angen am driniaeth), efallai cael person hyfforddedig sy’n gwneud hynny’n anodd. galwad ffôn a chwrdd â’r teulu yn yr ysbyty, ar gael i fod gyda nhw ar yr eiliad hollbwysig ac yn cynnig cymorth wedyn.” Cyfrannwr Mae Pob Stori o Bwys Roedd cyfranwyr hefyd eisiau protocol mwy tosturiol ar gyfer trafod hysbysiadau DNACPR gyda chleifion a'u hanwyliaid. Roeddent am weld cyfathrebu mwy agored gyda theulu a gofalwyr eraill, yn enwedig ar gyfer cleifion â gallu cyfyngedig i wneud eu penderfyniadau eu hunain. Roedden nhw hefyd eisiau mwy o gefnogaeth ar ôl i benderfyniadau anodd gael eu gwneud. |
10. Covid hir |
 |
Mae'r bennod hon yn rhannu straeon pobl sy'n byw gyda Long Covid. Mae Long Covid yn set o gyflyrau iechyd a symptomau hirdymor y mae rhai pobl yn eu datblygu ar ôl cael eu heintio â firws Covid-19. Mae'r bennod yn dechrau trwy archwilio iechyd pobl cyn ac ar ôl contractio Covid-19. Yna mae’n symud ymlaen i rannu profiadau pobl o ddiagnosis a cheisio cael mynediad at wasanaethau iechyd, cymorth a chyngor angenrheidiol, yn ogystal ag effaith barhaus Covid Long.
Bywydau a lles pobl cyn ac ar ôl contractio Covid-19
Roedd cyfranwyr â Long Covid yn aml yn cychwyn eu straeon trwy gymharu eu hiechyd cyn ac ar ôl dal Covid-19. llawer disgrifio eu bywydau cyn y pandemig fel rhai iach ac egnïol. Roeddent yn aml yn gweithio'n llawn amser ac roedd ganddynt fywydau cymdeithasol prysur. Roedd datblygu Long Covid yn golygu bod yn rhaid i lawer ail-werthuso eu bywydau, eu hunaniaeth a'u cynlluniau ar gyfer y dyfodol yn llwyr. I rai, roedd hyn yn golygu newid llwyr mewn hunaniaeth a sut yr oeddent yn dychmygu y gallai eu bywyd fod yn y dyfodol.
| “ | Mae'n argyfwng hunaniaeth mawr; roedd fy mam a minnau yn bobl heini, actif, roeddwn i fod i ddechrau pro-balet fel gyrfa, mae mynd o hynny i fod yn y gwely drwy'r amser yn enfawr, yn ifanc yn anodd gan eich bod yn darganfod pwy ydych chi . Rwy'n 18 ac yn dal ddim yn gwybod pwy ydw i, bedair blynedd yn ddiweddarach. Mae'n hunaniaeth nad ydw i eisiau."
– Person ifanc yn byw gyda Long Covid |
| “ | Roeddwn i'n rheoli bar, tua 60 o staff…roeddwn i'n arfer rhedeg yn rheolaidd, marathonau, hanner marathon. Roeddwn i'n rhedwr brwd iawn. Ond nawr ers Covid-19 prin y gallaf fynd o gwmpas y parc.”
- Person sy'n byw gyda Long Covid |
Dywedodd cyfranwyr eraill fod ganddyn nhw iechyd gwael cyn dal Covid-19. Roedd hyn yn cynnwys cyflyrau iechyd a oedd yn bodoli eisoes fel asthma, gordewdra a meigryn. Mewn rhai achosion, pan ddatblygodd cyfranwyr Long Covid, roedd eu cyflyrau a oedd yn bodoli eisoes yn ei gwneud hi'n anoddach nodi achos eu symptomau.
Yn gyffredinol, dywedodd cyfranwyr fod eu profiad o Long Covid wedi dechrau ar ôl iddynt wybod eu bod wedi dal Covid-19. Dechreuodd hyn fel arfer gyda symptomau Covid-19 yn para llawer hirach na'r disgwyl. Byddai'r symptomau wedyn yn newid ac yn datblygu wrth i amser fynd yn ei flaen. I'r rhai a ddatblygodd Long Covid yn gynnar yn y pandemig, roedd hwn yn gyfnod anodd a brawychus gan nad oedd llawer yn hysbys am y clefyd. Nid oedd pobl eraill yn ymwybodol o ddal Covid-19 erioed. Roeddent yn teimlo'n ddryslyd, yn ansicr ac yn rhwystredig am eu hiechyd.
| “ | Cyn belled [fel] Rwy'n gwybod, ni chefais Covid-19 erioed, nid wyf erioed wedi cael diagnosis ohono. Fodd bynnag, credaf yn gryf fy mod wedi ei gael. Ers mis Chwefror [2021] Nid wyf wedi bod yn iawn o ran iechyd, ac mae gennyf broblemau iechyd sylfaenol beth bynnag, ond mae gennyf broblemau anadlu yn awr [a materion iechyd parhaus eraill].
- Person sy'n byw gyda Long Covid |
Newidiodd symptomau Covid hir a difrifoldeb y symptomau hynny dros amser. Disgrifiodd cyfranwyr amrywiaeth o symptomau yn ymwneud â Long Covid, gan gynnwys:
- Anawsterau anadlu a lefelau ocsigen isel.
- Dolur gwddf a pheswch parhaus.
- Heintiau rheolaidd.
- Llai o symudedd.
- Cur pen a golwg gwael.
- Poenau a doluriau parhaus.
- Blinder, dryswch a 'niwl yr ymennydd'.
| “ | Dim ond eistedd yma, byddwn yn dechrau gwichian ac yn methu anadlu. Roedd yn rhaid i mi brynu ocsimedr i'w gadw ar fy mys ac roedd fy lefelau ocsigen yn 85 ac edrychais arno ar wefan y GIG a dywedodd, 'Ffoniwch ambiwlans os yw'n mynd o dan 95.'…byddwn yn cael heintiau ar hap ar fy mysedd ; Rydw i wedi dod yn alergedd i bethau nad oedd gen i alergedd iddynt o'r blaen. Mae fy nwy glust wedi'u cywasgu'n llwyr."
- Person sy'n byw gyda Long Covid |
| “ | Mae fy llygaid wedi bod yn beth mawr. Rwyf wedi teimlo llawer o boen yn fy llygaid na chefais erioed o'r blaen. Rwy'n ei chael hi'n anodd iawn ei weld. Byddwn i’n cael styes yn fy llygaid na fyddwn i erioed wedi’i chael o’r blaen.”
- Person sy'n byw gyda Long Covid |
Rhannodd llawer sut roedd math a difrifoldeb eu symptomau yn parhau i newid. Dywedodd rhai cyfranwyr y gallai Long Covid deimlo fel 'targed symudol' a oedd yn anodd ei ragweld. Roedd hyn yn aml yn niweidiol iawn i'w hiechyd meddwl, gyda llawer o deimladau wedi blino'n lân, yn rhwystredig ac yn ddigalon. Mae'n aml ei gwneud hi'n anodd codi o'r gwely neu hyd yn oed neu gyflawni gweithgareddau syml o ddydd i ddydd.
| “ | Roedd gen i boen cracio a gwahanol bethau felly, a byddai'n brigau a chafnau... roedd yn dal i fod felly, felly byddwn yn dweud am o leiaf 9 mis, ni allwn wneud unrhyw beth. Prin y gallwn i godi o'm gwely. Yna dechreuais gael cyfnodau hirach o fod yn well a byddwn i'n meddwl fy mod drosto eto a byddwn i allan o'm gwely. Rwy'n ôl yn y gwaith ... yn gwneud yn llawer gwell ond mae'n rhaid i mi gyflymu fy hun ... oherwydd gallwn fynd yn ôl yn syth.”
- Person sy'n byw gyda Long Covid |
Llwybrau at ddiagnosis a thriniaeth o Long Covid
Cyfranwyr yn ei chael yn anodd deall beth oedd yn digwydd i’w hiechyd gan mai ychydig iawn oedd yn hysbys am y cyflwr ar ddechrau’r pandemig. Roedd llawer yn chwilio am wybodaeth a chymorth, gan ddechrau’n aml gyda chwiliadau ar-lein neu drwy ffonio GIG 111 neu’r hyn sy’n cyfateb iddo. Siaradodd eraill â'u meddyg teulu neu wasanaethau gofal iechyd eraill i geisio canfod y rhesymau dros eu symptomau a dod o hyd i driniaeth. Yn gynnar yn y pandemig, dywedodd cyfranwyr sy'n byw gyda Long Covid ei bod yn heriol dod o hyd i unrhyw wybodaeth, cyngor neu ganllawiau triniaeth.
Roedd hyn i gyd yn hynod o straen i bobl â Long Covid. Dywedodd llawer wrthym eu bod wedi mynd i banig ac yn bryderus oherwydd nad oeddent yn gwybod beth oedd yn digwydd ac na allent gael yr help yr oedd ei angen arnynt.
| “ | Siaradais â fy meddyg teulu ac ar yr un pryd roeddwn mewn cysylltiad ag iechyd meddwl y gymuned ... dyna lle buom yn trafod Long Covid oherwydd y problemau blinder. Ond doedd dim llawer ar gael ar y pryd.”
- Person sy'n byw gyda Long Covid |
Rhannodd rhai cyfranwyr gyda Long Covid sut yr oeddent yn teimlo nad oedd gan eu meddygon teulu ddiddordeb yn eu symptomau neu nad oeddent yn eu credu. Pan ddigwyddodd hyn, roedd cyfranwyr yn aml yn teimlo eu bod wedi'u gadael yn segur ac yn ddiymadferth, ac yn ansicr ble i droi.
| “ | Roedd gennym ni feddygon teulu yn gwrthod credu yn Long Covid, gyda llawer o rai eraill ddim yn cael profion am symptomau.”
- Person sy'n byw gyda Long Covid |
Roedd rhwystredigaeth gyda gweithwyr gofal iechyd proffesiynol hefyd yn cael ei adlewyrchu mewn digwyddiadau gwrando.
Storïau gan bobl â Long CovidRhannodd cyfranwyr mewn digwyddiadau gwrando Every Story Matters sut y gwnaethant brofi bwlch sylweddol mewn dealltwriaeth feddygol, ymchwil, a thriniaeth, gan arwain at rwystredigaeth, siom a dicter. “Roedd fel fy mod wedi cael 50 o wahanol ddiagnosisau, ond gadawyd 50 o bethau heb eu diagnosio heb unrhyw driniaethau, iachâd na chymorth.” Person sy'n byw â Covid Hir Soniwyd am agweddau diystyriol gan weithwyr gofal iechyd proffesiynol. Ar ôl misoedd o orffwys yn y gwely ac ynysu, dim ond gwiriad brysiog a gafodd un cyfrannwr o'i arwyddion hanfodol cyn cael ei ddiswyddo gan ei feddyg teulu. “Ar ôl 6/7 mis o orffwys yn y gwely a dim cymdeithasu fe gawson ni apwyntiad gyda’r meddyg teulu o’r diwedd, a rhoddodd unwaith eto o’m hanfodion i mi a dweud nad yw’n gwybod dim am Long Covid, llofnododd fi a dyna ni.” Person sy'n byw â Covid Hir |
Mewn cyferbyniad, y rhai a dderbyniodd cymorth gan eu meddyg teulu gwerthfawrogi'r gofal a gawsant.
| “ | Roeddwn i mor ffodus, roedd fy meddyg teulu yn gwrando, roedden nhw'n malio, sy'n swnio'n wirion oherwydd dyna eu swydd. Ni allaf gredu bod meddygon teulu yn dal i ddweud wrth bobl nad oes y fath beth â Long Covid.”
- Person sy'n byw gyda Long Covid |
Ar draws y straeon a rennir, mae’n ymddangos bod mater diagnosis a chymorth wedi gwella’n araf wrth i’r pandemig fynd rhagddo. Fodd bynnag, mae llawer wedi parhau i ganfod triniaeth, cymorth a chyngor yn wael iawn, gydag ychydig neu ddim help ar gael iddynt.
| “ | Rydw i wedi cael fy nhrosglwyddo o gwmpas arbenigeddau, o biler i bost, yn aros dwy flynedd am gardioleg, nid wyf yn gwybod ble i droi.”
- Person sy'n byw gyda Long Covid |
Dywedodd llawer o gyfranwyr gyda Long Covid wrthym eu bod yn ei chael hi’n anodd cael diagnosis a’u bod yn rhwystredig ac wedi eu cythruddo gan y broses. Roedd cyfranwyr fel arfer yn cael diagnosis o Long Covid ar ôl proses o ddileu. Yn aml byddai'n rhaid iddynt fynd trwy gyfres o brofion ac asesiadau i ddiystyru cyflyrau iechyd eraill. Er bod hwn yn arfer clinigol safonol ar gyfer y rhan fwyaf o gyflyrau iechyd, ychwanegodd at y pryder, y straen a'r pryder yr oeddent yn ei deimlo. Gallai hefyd gyfrannu at deimladau pellach o flinder, a gwaethygu symptomau, wrth i gyfranwyr lywio drwy'r system gofal iechyd a chyflwyno eu hachos dros driniaeth i weithwyr gofal iechyd proffesiynol.
Roedd y rhai a rannodd eu straeon yn aml yn aros am amser hir gyda phroblemau iechyd difrifol na allai neb eu hegluro iddynt. Disgrifiodd rhai sut roedd gweithwyr gofal iechyd proffesiynol yn diystyru eu salwch dro ar ôl tro, gan waethygu eu trallod ymhellach.
| “ | Pan adewais y meddyg teulu, cefais fy dinistrio, cyrhaeddais adref ac ni allwn siarad. Rwyf wedi cael fy ngwrthod o haematoleg, cardioleg, clefydau heintus, mae'r rhestr yn mynd ymlaen. Dywedodd fy ngŵr, ‘Dydw i ddim yn gwybod pam rydych chi’n mynd drwy’r meddyg teulu neu’r GIG’.”
- Person sy'n byw gyda Long Covid |
| “ | Roeddwn i'n sâl am ychydig, felly fe wnes i alw [GIG] 111 am gyngor, ac fe ddywedon nhw i mi fynd i’r ysbyty, es i ac ar ôl rhai profion cefais fy nerbyn i’r ysbyty i gael profion pellach…ar ôl i’r profion fod wedi’u cwblhau a [nhw] doedd gen i ddim syniad o’r achos o hyd…cefais fy anfon adref wedyn fel claf allanol yn aros am fwy o atgyfeiriadau.”
- Person sy'n byw gyda Long Covid |
Cyfeiriwyd cyfranwyr eraill at arbenigwyr mewn cyflyrau iechyd penodol. Er enghraifft, weithiau roedd y rhai â phoenau a phoenau parhaus yn cael eu cyfeirio at glinigau rheoli poen, ac roedd rhai cleifion a oedd yn adrodd am niwl yr ymennydd yn cael eu cyfeirio at niwrolegwyr.
| “ | Cefais fy nghyfeirio at y tîm anadlol a chefais fy atgyfeirio at y cardiolegydd ar yr adeg benodol honno, cefais byliau tebyg lle’r oeddent yn meddwl ei fod fel syndrom brech.
- Person sy'n byw gyda Long Covid |
Mae'r straeon yn amlygu anghysondebau yn y ffordd y mae pobl sy'n byw gyda Long Covid wedi cael eu trin. Atgyfeiriwyd rhai yn ôl at eu meddyg teulu am brofion pellach neu i drin symptomau eraill, tra bod eraill yn cael eu hatgyfeirio i glinigau Long Covid neu eu cyfeirio at gyrsiau ar-lein (unwaith yr oedd y rhain wedi’u sefydlu). Achosodd hyn ragor o rwystredigaeth, gyda rhai cyfranwyr yn dweud wrthym am orfod mynychu ymgynghoriadau lluosog a siarad dro ar ôl tro â’u meddyg teulu a chlinigwyr eraill.
| “ | Felly, rydym yn dal i deimlo ein bod yn cael ein hanfon at y meddyg teulu ac nid yw'r meddygon teulu yn gwybod beth i'w wneud â ni, mae meddygon teulu yn brysur gyda llawer o bethau eraill. Ac nid oes gan hyd yn oed y meddygon teulu sy'n cydymdeimlo â'r ewyllys gorau yn y byd unrhyw syniad beth i'w wneud â ni. Mae angen rhywbeth mwy arbenigol yn y bôn.”
- Person sy'n byw gyda Long Covid |
| “ | Dechreuais gael mynediad at Feddyg Teulu newydd, a oedd o leiaf yn gwrando ac yn dilysu fy mhrofiad, ac yn gwneud atgyfeiriadau priodol, gan gynnwys niwroleg, cardioleg, clinigau Covid Hir, gwasanaethau blinder ac ati.”
- Person sy'n byw gyda Long Covid |
Roedd atgyfeiriadau i glinigau Covid Long arbenigol fel arfer yn digwydd trwy eu meddyg teulu ar ôl i achosion eraill gael eu diystyru. Yn ddiweddarach yn y pandemig, atgyfeiriwyd rhai pobl â Long Covid i'r clinigau arbenigol hyn gan weithwyr gofal iechyd proffesiynol eraill, megis y rhai sy'n gweithio ym maes iechyd meddwl a ffisiotherapi.
Stori GarethMae Gareth yn 40 oed ac yn byw ar ei ben ei hun, yn agos at ei deulu. Ar ddechrau'r pandemig roedd Gareth mewn iechyd cymharol dda a bu'n helpu pobl hŷn yn ei gymuned i ddelio â'r cyfyngiadau pandemig trwy ddosbarthu siopa neu helpu pobl i archebu siopa ar-lein, yn ogystal â swyddi rhyfedd cyffredinol eraill yr oedd angen cymorth ar bobl â nhw. Yn 2020 dechreuodd Gareth gael problemau stumog difrifol. Aeth at ei feddyg teulu i ddechrau a chafodd ei atgyfeirio at sawl arbenigwr ar gyfer ymgynghoriadau a phrofion. Nid oedd profion ar gael i Gareth ar yr adeg gynnar hon yn y pandemig a chan nad oedd ganddo symptomau nodweddiadol Covid-19 (e.e. peswch, twymyn, colli blas ac arogl neu anawsterau anadlu) parhaodd i gael profion ar gyfer eraill. cyflyrau iechyd. “Yn sydyn iawn [Roeddwn i'n sâl] a doedd gen i ddim y peswch nodweddiadol, y symptomau hynny. Roedd gen i lawer o symptomau yn fy stumog, ac roedd yn fwy cysylltiedig â'r perfedd ... doedden ni ddim yn gwybod beth ydoedd, oherwydd ni chafodd ei brofi [ac mae'n] ddim mor eang. Gan nad oeddwn yn dangos y symptomau nodweddiadol roeddwn yn ôl ac ymlaen at fy meddyg teulu ac yn y pen draw yn gorfod aros yn yr ysbyty, ni chefais brawf byth.” Yn y pen draw, datblygodd symptomau Gareth i gynnwys meigryn difrifol, poenau yn y cyhyrau, blinder ac asthma a chafodd ei dderbyn i'r ysbyty. Ar y pwynt hwn yr awgrymwyd diagnosis o Long Covid gan y meddygon yn yr ysbyty, gan eu bod wedi diystyru cyflyrau eraill. Dros yr ychydig flynyddoedd diwethaf mae iechyd Gareth wedi gwella dro ar ôl tro ac yna wedi gwaethygu eto. Mae hyn wedi cael effaith negyddol ar ei iechyd meddwl. “Fe fydda i’n dechrau teimlo’n well a’r peth nesaf byddwn i’n isel [gyda'r symptomau] eto. Byddwn i mewn dagrau pan fydd hynny'n digwydd." |
Daeth rhai pobl mor rhwystredig gyda’r gofal oedd ar gael fel eu bod wedi talu am wasanaethau gofal iechyd preifat i gael diagnosis Long Covid.
| “ | Aethom yn breifat ac wythnos yn ddiweddarach gwelsom yr ysbyty a gadarnhaodd ei bod yn meddwl mai Long Covid ydoedd ond nad oedd yn gwybod sut i drin [mae'n].”
- Person sy'n byw gyda Long Covid |
Trafodwyd y baich ariannol sylweddol ar bobl sy'n byw gyda Long Covid hefyd mewn digwyddiadau gwrando.
| “ | Cefais rwystrau i gael mynediad at ofal arbenigol er gwaethaf y ffaith fy mod yn gallu fforddio triniaeth breifat. Roedd y diffyg cydgysylltu rhwng y GIG a gwasanaethau preifat nid yn unig yn rhwystredig ond hefyd yn straen ariannol. Roedd angen amynedd ac adnoddau personol aruthrol i lywio’r system gymhleth hon.”
- Person sy'n byw gyda Long Covid |
| “ | Ceisiais ofal gan feddyg teulu preifat sy’n arbenigo mewn Long Covid, sydd wedi bod yn amhrisiadwy.”
- Person sy'n byw gyda Long Covid |
| “ | Mae’n rhaid i ni dalu drwy’r trwyn am breifat…mae’n system iechyd dwy haen.”
- Person sy'n byw gyda Long Covid |
Roedd newidiadau pandemig eraill i ofal iechyd yn aml yn ei gwneud hi'n anoddach cael mynediad at ofal ar gyfer Long Covid, gan ychwanegu rhwystredigaeth bellach. Er enghraifft, mae rhai profiadau yn amlygu’r anawsterau a wynebir wrth ddefnyddio ymgynghoriad dros y ffôn neu ar-lein i gyfleu eu symptomau a’r effaith a gafodd hyn arnynt. Roedd cyfranwyr yn rhwystredig nad oedd apwyntiadau ffôn neu ar-lein yn darparu gofal i’r un safon â gweld gweithiwr gofal iechyd proffesiynol wyneb yn wyneb.
| “ | Mae hi mor anodd gweld meddyg teulu nawr…mae'n rhaid i mi anfon lluniau at grŵp WhatsApp fy meddyg. Mae gan fy meddygfa rif ffôn WhatsApp lle rydych chi'n anfon eich enw, dyddiad geni a'r ffotograffau ... nid yw'r un peth."
- Person sy'n byw gyda Long Covid |
| “ | Llwyddais i weld gweithwyr gofal iechyd proffesiynol, trwy ymgynghoriadau rhithwir. Fe wnaethon nhw fy nghyfarwyddo i fonitro fy arwyddion hanfodol fy hun fel pwls a phwysedd gwaed a hyd yn oed fy arwain trwy archwilio fy ngwddf fy hun. Ond canfûm fod y dull hwn o ymgynghori yn annigonol; does dim byd yn lle archwiliad corfforol gan weithiwr proffesiynol. Cefais ddiagnosis o Long Covid. Er bod y diagnosis hwn yn rhyddhad, dysgodd wers hollbwysig i mi hefyd: mae cyfyngiadau i ymgynghoriadau rhithwir. ”
- Person sy'n byw gyda Long Covid |
Dywedodd pobl sy’n byw gyda Long Covid sy’n profi blinder, niwl yr ymennydd a chur pen wrthym eu bod yn ei chael hi’n arbennig o anodd cael mynediad at ofal. Dywedodd y cyfranwyr hyn wrthym eu bod yn cael trafferth llywio newidiadau, megis defnyddio bwydlenni ffôn neu offer ar-lein i sgrinio symptomau.
Roedd rhai gweithwyr gofal iechyd proffesiynol sy’n gweithio ym maes gofal sylfaenol hefyd yn pryderu am y diffyg ffocws ar Long Covid o’i gymharu â blaenoriaethau eraill. Roeddent yn teimlo bod angen gwell arweiniad ar sut i wneud diagnosis a thrin neu atgyfeirio cleifion at ffynonellau cymorth eraill fel clinigau Long Covid.
| “ | Roedd popeth yn ymwneud â’r brechlyn, ond ni fyddem yn cael cyngor wedi’i ddiweddaru ar sbirometreg (prawf anadlu cyffredin i wneud diagnosis a monitro rhai cyflyrau ysgyfaint), ni fyddem yn cael cyngor wedi’i ddiweddaru ar sut i atgyfeirio rhywun i glinig Long Covid. Cymerodd y brechlynnau flaenoriaeth dros bopeth. ”
– nyrs meddyg teulu |
Gwasanaethau gofal iechyd Covid hir
Dywedodd cyfranwyr wrthym y prif gefnogaeth a gynigiwyd ar gyfer symptomau Long Covid oedd cael ei gyfeirio at glinig Long Covid. Trwy'r clinigau Long Covid byddai symptomau pobl yn cael eu hasesu a chynigiwyd offer, cyngor ac arweiniad iddynt i'w helpu i ddeall a rheoli eu cyflwr.
Rhannodd y rhai a gyfeiriwyd at glinigau Long Covid sut yr oeddent yn gallu cael cymorth am gyfnod penodol - unrhyw le rhwng chwech a deuddeg wythnos. Dywedodd rhai wrthym eu bod wedi cael dyddiadur templed i'w helpu i olrhain symptomau a chyfnodau pan oeddent yn teimlo'n flinedig. Roeddent hefyd yn gallu cael mynediad at wasanaethau ffisiotherapi arbenigol a chyngor gofal iechyd arbenigol arall. Er enghraifft, dangoswyd technegau i reoli a rheoli anadlu i rai cyfranwyr a oedd yn byw gyda Long Covid ac a gafodd anawsterau anadlu, a sut i addasu gweithgareddau dyddiol i osgoi colli eu gwynt yn rhy gyflym.
| “ | Fe wnaethant ddarparu dyddiadur i nodi eich symptomau a gallant wneud pethau os oes gennych anawsterau anadlu sy'n dda.”
- Person sy'n byw gyda Long Covid |
| “ | Fe wnes i ddefnyddio gwasanaeth Long Covid ar gyfer ffisio. Fe wnes i ddefnyddio ffisiotherapi arferol, ac fe wnaethon nhw fy anfon i'r gwasanaeth Long Covid ers iddyn nhw ddweud, 'Fe fyddan nhw'n gwybod yn well beth sy'n digwydd gyda chi.'…rhoddon nhw ychydig iawn o ymarferion i mi yn hytrach nag ymarferion mawr. Felly dyna’r un peth oedd o gymorth…cael gwared ar yr holl broblemau ar y cyd a gefais.”
- Person sy'n byw gyda Long Covid |
Meddai rhai cyfranwyr Fe wnaeth clinigau Long Covid eu helpu i ddarganfod pa mor heini oeddent, a deall yn well ble mae angen iddynt wella. Er enghraifft, rhannodd un cyfrannwr sut y gofynnwyd iddo sefyll i fyny ac i lawr o gadair gymaint o weithiau ag y gallent mewn munud, ac roedd yn synnu pa mor anodd oedd hi iddo. Dywedodd y cyfranwyr hynny a oedd yn fwy cadarnhaol am glinigau Long Covid eu bod nhw eu helpu i ddeall sut roedd y cyflwr yn gweithio a pham ei fod yn effeithio ar eu corff mewn ffyrdd penodol.
| “ | Mynychais glinig Long Covid lle esboniodd y ferch yno, wyddoch chi, fod y Covid-19 yn aros yn eich corff, ond mae'n ymosod ar wahanol rannau o'ch corff. ”
- Person sy'n byw gyda Long Covid |
Fodd bynnag, dywedodd llawer o gyfranwyr wrthym am brofiadau negyddol o glinigau Long Covid, heb fawr o gymorth wedi’i deilwra a gofal gwael. Disgrifiodd y rhai a gafodd gymorth yn gynharach yn y pandemig glinigau Long Covid fel ‘gwasanaeth cyfeirio’ ac roeddent yn siomedig â’r hyn a gynigiwyd iddynt.
Stori PhoebeMae Phoebe yn 50 oed. Roedd hi'n gweithio ym maes cyllid ond bu'n rhaid iddi gymryd seibiant oherwydd heriau gyda'i hiechyd meddwl. Yn flaenorol, cafodd Phoebe ddiagnosis o anhwylder deubegwn, gorbryder ac iselder, ac mae ganddi ddiabetes math 2 hefyd. Ar ddechrau mis Mawrth 2020, datblygodd Phoebe gyflwr croen, a symptomau eraill fel blinder, niwl yr ymennydd a phroblemau gyda'i hanadl a'i stumog. Cafodd y rhain eu diagnosio fel Long Covid. Fe’i hatgyfeiriwyd gan ei meddyg teulu at gwrs ar-lein Long Covid a’i helpodd i reoli ei symptomau. Trwy'r cwrs hwn, cyfeiriwyd Phoebe at glinig Long Covid chwe wythnos. “Roeddwn i wedi bod ar y cwrs, cefais fynediad, mynediad cynnar iawn i glinig Long Covid. Yn awr, yr oedd hyn [y] ddechrau’r llynedd.” Canfu Phoebe fod rhai rhannau o'r clinig yn ddefnyddiol, yn enwedig o ran deall sut mae Long Covid yn 'ymosod' ar wahanol rannau o'r corff i achosi amrywiaeth o symptomau. Cynigiodd y gweithwyr gofal iechyd proffesiynol yn y clinig gyngor hefyd ar y ffordd orau o reoli ei hanadlu ac awgrymodd Phoebe gadw dyddiadur i olrhain ei blinder. Fodd bynnag, roedd Phoebe yn teimlo'n siomedig gan glinig Long Covid. Roedd yn ymddangos yn bennaf ar gyfer cyfeirio cleifion at wasanaethau gofal iechyd a sefydliadau cymorth eraill. Roedd hi wedi disgwyl cael cynnig triniaeth fwy pwrpasol a fyddai'n ei helpu gyda chyflwr ei chroen. “Os oes gennych chi anawsterau anadlu, gallant wneud pethau gyda chlinig Long Covid. Unrhyw beth arall, ei anghofio. Ac nid ydynt yn barod i gefnogi pobl mewn gwirionedd, oherwydd mae'n ymwneud â'ch cyfeirio at wasanaethau eraill. Ac oherwydd bod fy ngwasanaethau iechyd meddwl yn cael eu cynnwys beth bynnag, ni allent fy helpu gyda hynny.” |
Clywsom enghreifftiau o broblemau eraill gyda chlinigau Long Covid, gyda chyfranwyr yn tynnu sylw at faterion gan gynnwys oedi gyda phrofion, profion ddim yn cael eu cynnal, a cham-gyfathrebu am hanes cleifion.
| “ | Roedd fy nghlinig Long Covid lleol yn warthus, yn gyngor a rheolaeth gwbl amhroffesiynol, er enghraifft dweud bod profion yn frys ac yna ddim yn cael eu harchebu, gan ddechrau fy ail ymgynghoriad fel pe bawn i’n glaf newydd, felly nid oedd yr un o’r atgyfeiriadau cychwynnol wedi’u gwneud.”
- Person sy'n byw gyda Long Covid |
Roedd eraill yn rhwystredig bod y clinigau'n canolbwyntio ar sut i reoli symptomau, yn hytrach na phrofi gwahanol driniaethau a allai leddfu neu hyd yn oed ddod â'u symptomau i ben. Ar gyfer y cyfranwyr hyn, nid oedd y clinigau 'yn addas i'r diben'. Fe wnaethant awgrymu y dylai'r system gofal iechyd ganolbwyntio ar ymchwil a datblygu triniaethau ar gyfer Long Covid. Dywedodd rhai fod y clinigau ond wedi ychwanegu at y trallod o fyw gyda Long Covid.
| “ | Mae clinig Long Covid yn darparu cefnogaeth ar gyfer yr anabledd newydd, nid triniaeth.”
- Person sy'n byw gyda Long Covid |
| “ | Mae clinigau Covid hir nad ydynt yn addas i’r diben yn ychwanegu at y rhwystredigaeth, y trawma a’r ansicrwydd i mi – buddsoddwch yr arian a ddefnyddir yn y clinigau hynny mewn treialon ac ymchwil ystyrlon.”
- Person sy'n byw gyda Long Covid |
| “ | Gydag actifyddion eraill, rwyf wedi bod yn galw am sefydlu clinigau priodol i gynnal profion manwl, trylwyr, ar lefel ymchwil ac arbed samplau ar gyfer ymchwil yn y dyfodol, gyda diagnosteg ddigonol.”
- Person sy'n byw gyda Long Covid |
Rhannodd cyfranwyr wahaniaethau yn y gwasanaethau Covid Long sydd ar gael i bobl ledled y DU ac yn fyd-eang. Er enghraifft, roedd canfyddiad ymhlith rhai cyfranwyr bod Lloegr ar y blaen i’r Alban, Cymru a Gogledd Iwerddon o ran sefydlu clinigau Long Covid a datblygu cymorth i gleifion.
| “ | Yng Nghymru yn arbennig, mae gwasanaethau Long Covid wedi bod yn dipyn o ôl-feddwl. Nid oes clinig Long Covid da iawn fel sydd gennych chi yn Lloegr, wyddoch chi? Mae gennych chi'r un ymgynghorydd yng Nghaerdydd sy'n gwneud ei gorau. Bu’n rhaid iddi ddechrau’r gwasanaeth hwnnw ar gyfer Long Covid yn ei hamser ei hun, nid oedd yn wasanaeth swyddogol o gwbl, ac nid yw hi wedi cael ei chefnogi ag ef ychwaith mewn gwirionedd.”
- Person sy'n byw gyda Long Covid |
Yn yr un modd, roedd cyfranwyr yn teimlo bod y DU wedi bod yn araf i ddarparu cefnogaeth a thriniaeth i Long Covid o gymharu â gwledydd eraill fel America a Chanada.
| “ | Byddwn yn dweud y ffaith ei fod wedi cymryd yr Alban ... rydym ychydig flynyddoedd ar ôl oherwydd rydych chi'n edrych ar bethau i fyny, dros y byd a dweud y gwir, ac roeddech chi'n clywed o America ac roedd ganddyn nhw glinigau, ac roedd gan Loegr glinigau, a doedd gennym ni ddim byd. . A dyna fi nawr, 2 flynedd yn ddiweddarach, newydd gael gwybod am y clinig Long Covid hwn.”
- Person sy'n byw gyda Long Covid |
Cefnogaeth a chyngor ar gyfer rheoli Long Covid
I ddechrau, ychydig iawn o gymorth a chyngor oedd ar gael, ond dywedodd llawer o gyfranwyr fod hyn wedi gwella ers hynny.
| “ | Yn ystod misoedd cyntaf Long Covid, doedd gen i ddim cefnogaeth na gwybodaeth.”
- Person sy'n byw gyda Long Covid |
Yng nghamau cynnar y pandemig bu cyfranwyr yn chwilio ar-lein am wybodaeth ac yn defnyddio cyfryngau cymdeithasol i ddod o hyd i bobl a oedd yn profi symptomau tebyg. Defnyddiodd pobl lwyfannau fel Facebook, Instagram a Twitter/X i bostio cwestiynau, dod o hyd i grwpiau a darllen gwybodaeth.
| “ | Pan es i ar-lein a dechrau dod o hyd i’r grwpiau Long Covid, roedd yna bobl eraill yn cael profiadau tebyg i mi, felly doeddwn i ddim yn teimlo mai dim ond fi oedd yn mynd yn wallgof oedd hi, a dyna sut deimlad oedd hi.”
- Person sy'n byw gyda Long Covid |
Roedd y grwpiau cyfoedion hyn yn ffynhonnell cefnogaeth a sicrwydd i bobl yn ystod cyfnod ansicr, ynysu a phryderus. Roedd cyfranwyr yn gallu cysylltu ar-lein i rannu cyngor a chynnig cymorth i bobl a oedd mewn sefyllfa debyg.
| “ | Fe wnes i ffeindio’r grwpiau mae’n debyg dwi’n meddwl ym mis Mehefin… erbyn diwedd Mehefin dechreuais gymryd mwy o ran oherwydd bod popeth arall wedi mynd yn fy mywyd a bryd hynny doeddwn i ddim yn ddigon da. Roeddwn i'n gallu sgwrsio ychydig ar-lein ac yna, dros amser, roedd yna adegau pan ymunais â sgwrs Zoom a chwrdd â rhai o'r bobl. Roedd hynny'n anhygoel. Roedd fel therapi grŵp i bob un ohonom.”
- Person sy'n byw gyda Long Covid |
Wrth i amser fynd yn ei flaen, roedd y grwpiau a'r rhwydweithiau hyn yn ffynhonnell hanfodol o sicrwydd a chefnogaeth i bobl â Long Covid. Wrth i amser fynd yn ei flaen, mae mathau eraill o gymorth a chyngor gan elusennau a sefydliadau eraill wedi gwella hefyd. Dywedodd cyfranwyr wrthym yn aml fod cymorth wedi’i deilwra ar gyfer cyflyrau iechyd penodol fel asthma neu iechyd y galon a’r ysgyfaint yn ddefnyddiol.
Effaith Long Covid ar weithwyr gofal iechyd proffesiynol
Ychydig o gyfranwyr a oedd yn gweithio fel gweithwyr gofal iechyd proffesiynol rhannu eu profiad o ddal Covid-19 yn y gwaith a’r effaith ddinistriol a gafodd Long Covid arnynt wedyn. Disgrifiodd eraill yr effaith a gafodd hyn ar eu teulu.
| “ | Daeth fy ngŵr i’r ysbyty yn y pen draw ond yn ddigon ffodus roedd allan mewn tua 4 neu 5 diwrnod, ond mae’n dal i ddioddef o Long Covid ac roedd hynny oherwydd fy mod wedi mynd ag ef adref o’r ward.”
– Gweithiwr gofal iechyd proffesiynol a gofalwr |
Clywsom gan rai gweithwyr gofal iechyd proffesiynol am pa mor hir yr oedd Covid wedi effeithio ar gydweithwyr ac wedi arwain at bwysau staffio. Roedd cydweithwyr oherwydd salwch hirdymor yn ei gwneud hi'n anoddach i wasanaethau gofal iechyd weithredu hyd eithaf eu gallu a darparu gofal i gleifion.
| “ | O fewn y bobl roeddwn i'n gyfrifol [ar gyfer] roedd yna nifer o bobl sydd wedi cael symptomau Long Covid…mae'n debyg bod tua 5 o bobl wedi cael yr hyn fyddwn i'n ei ddweud am gyfnod sylweddol o newid yn eu gallu corfforol. Efallai mwy na hynny, efallai tua 10.”
-Meddyg ysbyty |
| “ | Llawer o Long Covid ymhlith fy nghydweithwyr, blinder cronig, symptomau Long Covid, diffyg anadl, sydd i gyd yn gorfforol hefyd. Mae’n debyg nad oedd yn help iddyn nhw gael eu llosgi allan ar yr adeg pan gawson nhw Covid-19 hefyd.”
- Meddyg Teulu |
Rhannodd rhai gweithwyr gofal iechyd proffesiynol sut roedd eu habsenoldeb salwch hirdymor oherwydd Long Covid wedi arwain at broblemau a gwrthdaro â’u cyflogwr. meddent roedd diffyg dealltwriaeth neu adnabyddiaeth o Long Covid fel cyflwr iechyd parhaus yn y system gofal iechyd.
| “ | Hyd heddiw, hyd yn oed gyda digwyddiad gan fy nghyflogwyr maen nhw'n dal i wadu fy mod wedi ei gael yn y gwaith ... ysgrifennu e-bost at [y] Dywedodd Prif Weithredwr fy Ymddiriedolaeth fy mod yn teimlo fy mod wedi gadael yn llwyr, nad oedd fy nghyflogwyr eisiau gwybod.”
- Person sy'n byw gyda Long Covid |
Dywedodd rhai gweithwyr gofal iechyd proffesiynol wrthym hefyd nid oedd sefydliadau yn mesur effaith Long Covid ar y system gofal iechyd yn gywir. Roeddent yn teimlo bod angen gwneud mwy i ddeall yr effaith y bydd Long Covid yn ei chael ar y gweithlu gofal iechyd.
| “ | O ran monitro staff y GIG sydd â Long Covid, rwy’n cael fy nghyfrif pan fyddaf i ffwrdd yn sâl, ond nid pan fyddaf yn dychwelyd yn raddol – felly nid oes cofnod o ba mor hir yr effeithiwyd ar staff heb ddychwelyd i’w rôl a’u horiau swydd gwreiddiol, felly sut allwch chi fonitro gwir effaith covid ar weithwyr y GIG?”
- Gweithiwr gofal iechyd proffesiynol yn byw gyda Long Covid |
Effaith barhaus Covid Long
Mae Covid Hir yn parhau i gael effaith ddramatig a niweidiol ar fywydau llawer o bobl. Dywedodd cyfranwyr sy’n byw gyda Long Covid wrthym eu bod yn parhau i wynebu anawsterau anadlu. Mae hyn yn ei gwneud hi'n anodd symud o gwmpas yn hawdd a chyflawni tasgau o ddydd i ddydd. Disgrifiodd cyfranwyr hefyd effeithiau difrifol eraill, megis colli symudedd sylweddol.
| “ | Rwyf bellach yn ddefnyddiwr cadair olwyn oherwydd niwroopathi yn rhan isaf fy nghoes chwith/troed chwith, blinder a diffyg anadl a achosir gan Long Covid.”
- Person sy'n byw gyda Long Covid |
| “ | Nid oeddwn yn gallu dychwelyd i’r gwaith na fy mywyd normal gan ei fod yn fy ngadael yn wanychedig iawn gyda blinder cronig a dysautonomia (cyflwr sy’n effeithio ar y system nerfol), cur pen cronig, niwl yr ymennydd a chanolbwyntio gwael.”
- Person sy'n byw gyda Long Covid |
Disgrifiwyd y cyfranwyr sut na allant weithio mwyach ac effaith colli eu hincwm. Roedd pobl sy'n byw gyda Long Covid eisiau ailafael yn eu bywydau arferol ar ôl iddynt ddechrau teimlo'n well, ond canfuwyd nad oeddent yn gallu gwneud hynny.
| “ | Dwi allan o wynt drwy'r amser. Rwy’n dal i deimlo’n flinedig, rwy’n dal i gael niwl yr ymennydd, ac mae hyn ddwy flynedd yn ddiweddarach, felly mae gwaith yn wirioneddol, anodd iawn.”
- Person sy'n byw gyda Long Covid |
| “ | Es i yn ôl i'r gwaith, dylwn i ddim fod wedi mynd yn ôl i'r gwaith mor fuan ... es yn ôl, dwi'n meddwl, tua 5 neu 6 wythnos ar ôl i mi ddod allan o'r ysbyty...efallai bod hynny wedi achosi i'r dilyniant fod [yn well] yn llawer arafach, Dydw i ddim yn gwybod.”
- Person sy'n byw gyda Long Covid |
Disgrifiodd rhai cyfranwyr gyda Long Covid hefyd eu profiadau o deimlo’n unig ac yn ynysig, a sut roedd y cyflwr yn ei gwneud hi’n anodd cynnal cyfeillgarwch. Disgrifiwyd sut yr oedd pobl eraill yn cael eu dychryn gan eu hiechyd ac y gallent ei chael yn drallodus.
| “ | Fy anadlu, os yw'n mynd yn anodd, mae'n swnio'n ofnadwy. Mae pobl o'm cwmpas yn mynd i banig, oherwydd mae'n swnio fel fy mod yn cael trafferth anadlu'n fawr. Ni allaf gael digon o aer i'r ysgyfaint. Felly, os ydw i'n cerdded i fyny allt, neu'n cario rhywbeth i fyny'r grisiau, yna rydw i'n mynd i fod yn fyr iawn o wynt…Nid yw'n brifo, nid yw'n peri gofid i mi, oherwydd rwy'n gwybod, mewn munud, y bydd byddwch yn iawn. Ond, i bobl o’m cwmpas, gall fod yn eithaf trallodus.”
- Person sy'n byw gyda Long Covid |
Storïau gan bobl â Long CovidSiaradodd cyfranwyr mewn digwyddiad gwrando Mae Pob Stori’n Bwysig am effeithiau parhaol Long Covid, yn enwedig ar eu lefelau egni a’u hiechyd meddwl. Dywedasant ei fod yn effeithio ar eu lles a'u gallu i gyflawni eu rolau'n effeithiol. “Gallaf fyw gyda’r cur pen, ond y blinder sydd mor galed. Rwy’n mynd adref ar ôl gwaith, ac rwy’n cwympo i gysgu ar unwaith.” Fe wnaethant rannu eu profiad o deimlo’n flinedig yn gyson, gyda’u hegni wedi’i “rhwygo’n llwyr” ar ôl contractio Covid-19. Siaradodd staff gofal iechyd am y cur pen parhaus a'r blinder llethol a brofwyd ganddynt, gan effeithio ar eu gallu i dreulio amser gwerthfawr gyda'u teulu. Roeddent yn mynegi teimlad fel person gwahanol, tristwch llethol a diffyg cymhelliant. “Ni ddylai bywyd fod fel hyn; Dydw i ddim yn gwybod beth sy'n bod gyda mi. Mae gen i dri o blant, i gyd wedi tyfu i fyny. Nid wyf yr un peth bellach. Dw i eisiau crio; Dw i ddim yn siŵr pam rydw i mor isel, ddim yn siŵr pam nad ydw i yr un dyn.” |
Mae Long Covid wedi cyfyngu'n sylweddol ar yr hyn y gall llawer o gyfranwyr ei wneud o ddydd i ddydd. Mae hwn wedi bod yn brofiad trawmatig a thrawsnewidiol i lawer a rannodd eu stori gyda ni a’u teuluoedd.
| “ | Rwy'n dda iawn yn y boreau…am 1 o'r gloch, gallaf deimlo'r blinder yn dod ymlaen. Mae fel storm sy'n dod tuag atoch, ac mae fel storm yn fy mhen, dyna beth mae'n ei wneud i fy mhen. Gallaf deimlo popeth yn mynd o'i le, mae'n dechrau [mynd] niwlog, ac rwy'n dechrau cael ychydig o gur pen. Yna byddaf yn teimlo'n flinedig ... rhan o'r broblem yw, nid yw'n rheolaidd fel clocwaith. Felly, ar rai dyddiau gallaf fynd ychydig yn hirach, dyddiau eraill, gallaf ddechrau ei deimlo am 11 o’r gloch y bore.”
- Person sy'n byw gyda Long Covid |
| “ | Mae bywyd wedi bod yn uffern a phoenyd, mae'r effeithiau ar fy nheulu wedi bod yn erchyll. Cyn i mi fod yn hapus, yn iach, yn iechyd gorau fy mywyd, yna ymhell cyn cloi cawsom ein heintio, ymhell cyn profi neu roedd unrhyw un yn credu ei fod yn y wlad hon. ”
- Person sy'n byw gyda Long Covid |
Dywedodd llawer o gyfranwyr gyda Long Covid eu bod yn teimlo eu bod wedi cael eu hanghofio gan y system gofal iechyd a'r gymdeithas ehangach, ac nad oes neb yn poeni dim mwy. Maent am gael cydnabyddiaeth am eu cyflwr iechyd ac i'r cyhoedd yn ehangach ddeall yr heriau y maent hwy a'u teuluoedd yn eu hwynebu.
| “ | Does neb eisiau gwybod, dwi'n teimlo'n anweledig. Rwy'n cael fy nhrin fel difrod cyfochrog. Mae'r rhwystredigaeth a'r dicter rwy'n ei deimlo yn anhygoel; golau nwy meddygol, diffyg cefnogaeth a'r ffordd y mae pobl eraill yn fy nhrin.”
- Person sy'n byw gyda Long Covid |
Fe wnaethon nhw hefyd bwysleisio eu rhwystredigaeth a'u dicter bod Long Covid yn cael ei siarad amdano fel rhywbeth a ddigwyddodd yn y gorffennol.
| “ | Mae dogfennau a gwyddonwyr yn cyfeirio at Covid-19 fel peth o'r gorffennol; mae hyn yn rhwystredig ac yn ddig.”
- Person sy'n byw gyda Long Covid |
Dysgu ar gyfer y dyfodol: Covid HirMyfyriodd pobl sy'n byw gyda Long Covid ar yr hyn yr oeddent yn ei feddwl sydd angen ei ddysgu o'u profiadau. Mae llawer eisiau mwy o gydnabyddiaeth, ymchwil a dealltwriaeth o Long Covid a chyflyrau cysylltiedig ôl-Covid-19. Dywedwyd wrthym fod angen i drin y cyflyrau ôl-Covid hyn gael ei wreiddio’n well yn y system gofal iechyd, gan gynnwys meddygon teulu yn fwy ymatebol a chydymdeimladol, a gwell gofal ar gael. “Mae angen cyllid ar frys ar y GIG, mwy o staff a mwy o hyfforddiant ac adnoddau ar gyfer cefnogi a thrin pobl â Covid Hir. Mae angen i fynediad at glinigau Long Covid fod yn hynod gyflym, ac mae angen llawer mwy o gefnogaeth o ran helpu cleifion Long Covid i gael mynediad at y wybodaeth a’r adnoddau sydd ar gael a allai eu helpu i wella.” Cyfrannwr Mae Pob Stori o Bwys Roedd sicrhau diagnosis a thriniaeth Covid Hir yn digwydd yn gyflymach yn flaenoriaeth i lawer. Disgrifiwyd hyn yn hanfodol oherwydd pa mor wanychol yw Long Covid i bobl, ac oherwydd y dirywiad corfforol a meddyliol parhaus a brofir gan lawer â'r cyflwr. “Gallai ymchwil pellach i Long Covid a chymhlethdodau cardiofasgwlaidd helpu gyda diagnosis a thriniaeth gyflym, gan rannu arfer da a chanfyddiadau cleifion hefyd rhwng meddygon ymgynghorol a meddygon ledled Cymru a Lloegr/y DU gyfan a gwledydd eraill hefyd er mwyn sefydlu’r llwybrau gofal cleifion gorau yn gynnar. , fel bod cleifion yn cael eu trin yn gyflym cyn dirywiad corfforol a meddyliol, ac effaith ariannol ar deuluoedd.” Cyfrannwr Mae Pob Stori o Bwys Roedd llawer sy'n byw gyda Long Covid eisiau i fwy gael ei wneud i godi ymwybyddiaeth a dealltwriaeth. Er enghraifft, galwasant am ymdrechion wedi’u targedu i addysgu’r cyhoedd a gweithwyr gofal iechyd proffesiynol am Long Covid trwy negeseuon iechyd cyhoeddus, ac am fwy o gyllid ar gyfer ymchwil ar gyfer cyflyrau ôl-Covid. Yn ogystal â bod y peth iawn i'w wneud i gefnogi a thrin y rhai sydd eisoes yn byw gyda Long Covid, roedd hyn yn cael ei ystyried yn hanfodol i atal mwy o anghenion gofal iechyd ôl-Covid rhag datblygu yn y dyfodol. “Byddwch yn onest â’r cyhoedd am Long Covid fel y gallwn ofalu, cefnogi ac addysgu ein hunain a’n gilydd. Buddsoddi mewn ymchwil a darparu triniaeth. Cydnabod risgiau canlyniadau hirdymor Long Covid (patholeg cardiaidd, dementia, canser, ac ati) o lid cronig, dadreoleiddio imiwnedd, camweithrediad gastroberfeddol, ac ati Darparu gofal nawr. Mae trin Long Covid yn rhatach na’r afiechyd cronig sy’n deillio o hynny.” Cyfrannwr Mae Pob Stori o Bwys |
11. cysgodi |
 |
Mae'r bennod hon yn amlinellu profiadau pobl a oedd yn gwarchod yn ystod y pandemig, a'r gweithwyr gofal iechyd proffesiynol sy'n gofalu am gleifion sy'n agored i niwed yn glinigol ac sy'n hynod agored i niwed yn glinigol . Mae'n ymdrin â chyfathrebu ynghylch gwarchod, effaith gwarchod ar iechyd meddwl a chorfforol, a phrofiadau o gael mynediad at ofal iechyd wrth warchod.
Cyfathrebu ynghylch gwarchod
Dywedodd llawer o gyfranwyr a oedd yn glinigol agored i niwed ac yn hynod agored i niwed yn glinigol wrthym pa mor ofnus oeddent ar ddechrau’r pandemig. Roeddent yn aml yn poeni am gontractio Covid-19 a sut y byddai'n effeithio arnyn nhw a'u teuluoedd. Yn gynnar yn y pandemig, roedd rhai yn osgoi pob cysylltiad â phobl y tu allan i'w teulu agos oherwydd eu bod yn bryderus am ddal y firws. Gwnaeth rhai hyn cyn cael unrhyw gyngor swyddogol, yn ymwybodol o'r risgiau sy'n gysylltiedig â'u cyflyrau iechyd.
| “ | Doeddech chi ddim yn gwybod pa ffordd yr oedd yn mynd i fynd na pha mor ddrwg oedd yn mynd i fod, yn enwedig y rhan gynnar. Roedd pobman yn cau, roedd yn frawychus iawn, iawn. ”
– Person sy’n agored i niwed yn glinigol/yn hynod agored i niwed yn glinigol |
3. Sylwch nad yw'n bosibl gwahaniaethu rhwng pobl sy'n agored i niwed yn glinigol neu'n hynod o agored i niwed yn glinigol yn y straeon a gasglwyd gan Every Story Matters. Felly, priodolir pob dyfyniad fel 'Person sy'n agored i niwed yn glinigol/yn hynod agored i niwed yn glinigol.
| “ | Rwyf wedi niweidio'r ysgyfaint a'r arennau, felly byddai unrhyw fath o salwch anadlol yn beryglus. Peidiwch â mynd allan. Roeddwn i yn yr un sefyllfa â phawb, doedd neb yn gwybod beth i’w ddisgwyl.”
– Person sy’n agored i niwed yn glinigol/yn hynod agored i niwed yn glinigol |
Roedd cyfranwyr y dywedwyd wrthynt am warchod eu hunain fel arfer yn derbyn llythyr gan eu meddyg teulu. Esboniodd hyn eu bod mewn mwy o berygl pe baent yn dal y firws. Roedd cyfranwyr yn aml yn disgwyl y newyddion hyn, gyda llawer yn derbyn bod gwarchodaeth yn angenrheidiol iddynt. Gallai llawer weld manteision gwarchod pe bai hyn yn eu cadw'n ddiogel.
| “ | Wel, roeddwn i'n gwybod ei fod er fy amddiffyniad fy hun, wyddoch chi, felly doeddwn i ddim yn gwrthwynebu. Roedd yn gyfyngol ond roeddwn i'n gwybod fy mod mewn sefyllfa lle byddai'n llawer gwaeth pe bawn i'n cael y clefyd. Felly, doedd dim ots gen i.”
– Person a oedd yn glinigol agored i niwed/yn hynod agored i niwed yn glinigol |
Dywedodd cyfranwyr eraill eu bod wedi'u synnu gan ba mor gyfyngol oedd y rheolau gwarchod a'u bod yn ei chael yn anodd eu derbyn. Roedd rhai yn bryderus iawn am ddal Covid-19, ond hefyd sut y byddent yn ymdopi â'r cyfyngiadau.
| “ | Roedd yn anodd derbyn y llythyr hwnnw a chael gwybod na allwch fynd allan. Ie, dim ond darllen drwy'r manylion yr oeddwn yma, ac mae'n dweud, 'Ewch allan i'r ardd neu eisteddwch ar garreg y drws os gallwch chi.' Felly, doedden ni ddim yn cael mynd allan am dro hyd yn oed. Felly, roedd hynny’n anodd.”
– Person a oedd yn glinigol agored i niwed/yn hynod agored i niwed yn glinigol |
| “ | Dywedwyd wrthyf am beidio â mynd allan i fy min fy hun hyd yn oed oherwydd ystyriwyd ei fod yn rhy beryglus. Roedd hyn yn ofnadwy o frawychus, pan ddywedwyd wrthyf fy mod yn debygol o fynd yn ddifrifol wael neu farw pe bawn yn dod i gysylltiad â Covid-19. Bob tro roedd y llywodraeth yn codi cyfyngiadau [agored i niwed yn glinigol] cynghorwyd pobl i barhau i warchod oherwydd nad oedd y risg i ni wedi lleihau.”
– Person a oedd yn glinigol agored i niwed/yn hynod agored i niwed yn glinigol |
Roedd y rhai a oedd yn agored i niwed yn glinigol weithiau wedi drysu ynghylch y canllawiau, a chysylltodd rhai â'u meddyg teulu i gael eglurhad ynghylch yr hyn yr oedd angen iddynt ei wneud. Dywedodd meddygon teulu fod y dryswch hwn yn fwy o broblem ar ddechrau'r pandemig, gan nad oedd y dosbarthiad 'agored i niwed yn glinigol' yn glir ac wedi newid dros amser. Roedd rhai meddygon teulu yn ei chael yn anodd cynghori cleifion oherwydd nad oedd dealltwriaeth dda o'r risgiau ar gyfer gwahanol gyflyrau.
| “ | Felly [agored i niwed yn glinigol] pobl [oedd yn galw] yn gofyn beth ddylen nhw ei wneud, a oedden nhw i fod yn gwarchod, a oedden nhw i fod i fod yn newid eu meddyginiaeth, sut oedden nhw'n mynd i gael eu meddyginiaethau a'r math yna o beth... roedden ni'n cael gwybodaeth gyfyngedig iawn ynglŷn â phwy oedd yn risg uchel…os bu ychydig mwy o gyfathrebu ynghylch pwy y credwyd ei fod yn risg uchel, byddai wedi’i wneud ychydig yn symlach.”
- Meddyg Teulu |
Rhoddodd rhai meddygon teulu enghreifftiau hefyd o gleifion clinigol agored i niwed a chlinigol hynod agored i niwed nad oeddent yn dilyn y canllawiau oherwydd eu bod yn eu gweld yn rhy gyfyngol.
| “ | Roedd gennym ni bobl a oedd i fod ar restrau gwarchod yn dod i mewn i'r feddygfa ac yn dweud wrthym eu bod yn mynd i ffwrdd at eu ffrindiau gorau i gael te prynhawn a phethau, ac rydych chi fel, 'Rydych chi i fod i fod yn cysgodi…Dydych chi ddim hyd yn oed i fod i fynd i'r archfarchnad, beth yw'r uffern ydych chi'n meddwl eich bod chi'n ei wneud yn mynd i dŷ rhywun arall? Does neb yn cael mynd i dŷ rhywun arall.”
- Meddyg Teulu |
Dywedodd rhai cyfranwyr ag anghenion ychwanegol eu bod yn ei chael yn anodd cael gafael ar wybodaeth gan eu meddygon teulu yn y fformat cywir ar eu cyfer. Roedd hyn yn golygu nad oeddent yn deall beth oedd ystyr gorfod gwarchod yn ymarferol, gan wneud iddynt deimlo'n llai diogel ac yn fwy ynysig.
| “ | Gofynnais am gefnogaeth gan y gwasanaethau cymdeithasol a fy meddyg teulu, ac nid oedd unrhyw un ar gael, roedd pawb wedi'u hynysu ac rydych chi'n gadael y rhai sy'n agored i niwed ac yn eu gwthio i'r naill ochr ac rydych chi'n teimlo'n wrthodedig, doeddwn i ddim yn teimlo'n ddiogel o gwbl."
- Person â cholled golwg |
Effaith cysgodi ar iechyd meddwl a chorfforol
Dywedodd cyfranwyr wrthym fod gwarchod yn aml yn arwain at, ac yn parhau i gyfrannu at, deimladau o ynysu, unigrwydd, pryder ac ofn. Mae gwarchod yn cael llawer o effeithiau niweidiol ar iechyd corfforol a meddyliol pobl. Disgrifiodd rhai sut roedd yr ofn o ddal Covid-19 yn parhau ac yn draenio. Roedd llawer yn teimlo'n ymylol yn barhaus ac yn ofnus, angen bod yn ymwybodol o bwy roedden nhw'n rhyngweithio â nhw a sut y gallent amddiffyn eu hunain.
| “ | Roeddwn wedi fy syfrdanu, oherwydd roeddwn yn gwybod ar y pryd pe bawn yn ei ddal y byddai'n rhaid i mi fynd i'r ysbyty. Roeddwn i’n ei ofni’n fawr, felly wyddoch chi, roedd menig glas ym mhobman, roeddech chi’n golchi dwylo’n gyson…rydych chi’n rhoi’r gel ar eich dwylo.”
– Person a oedd yn glinigol agored i niwed/yn hynod agored i niwed yn glinigol |
| “ | Roeddwn i mor ofnus o ddal Covid-19 a marw; bu farw cymaint o bobl. Mae gen i'r canser llygad prin iawn hwn ... roeddwn i mor ofnus o gael Covid-19. Wnes i ddim gadael [fy nhref] heblaw am un tro, a oedd yn apwyntiad ar gyfer fy niabetes.”
- Person â cholled golwg |
Clywsom lawer o straeon am sut i warchod amharu'n llwyr ar drefn arferol pobl a gwneud iddynt deimlo bod eu bywyd normal wedi dod i ben. Dywedasant wrthym na allent dreulio amser gyda ffrindiau a theulu mwyach, hyd yn oed pan oedd eraill yn gallu. Fe wnaethant rannu sut na allent wneud ymarfer corff mwyach, a sut roedd eu hobïau yn dod i ben yn aml. Dywedodd llawer nad oeddent yn gallu gweithio neu'n gweithio ar eu pen eu hunain.
Yn ogystal â bod yn ofnus, roedd yr aflonyddwch yn golygu cyfranwyr a oedd yn gwarchod yn aml profi diflastod ac unigedd llethol. Roedd llawer o'r straeon yn rhannu sut y dirywiodd iechyd corfforol a meddyliol pobl yn gyflym trwy gydol y pandemig.
| “ | Cwymp trefn arferol, dioddefodd iechyd meddwl, dioddefodd iechyd corfforol. hi [ei mam] ddim yn bwyta llawer a dweud y gwir, collodd lawer o bwysau oherwydd doedd hi ddim yn iach … ond ie, felly roedd hi'n dioddef llawer o ran iechyd meddwl ac iechyd corfforol oherwydd diffyg pobl eraill yn y bôn yn fwy na dim, diffyg unrhyw math o ryngweithio.”
– Gofalwr am rywun a oedd yn glinigol agored i niwed/yn hynod agored i niwed yn glinigol |
| “ | Fe wnes i ymdopi trwy wneud pethau eraill ond taswn i wedi mynd ychydig yn hirach, ychydig mwy o wythnosau, dwi'n meddwl y byddwn i wedi mynd dros y dibyn i fod yn onest gyda chi. Roeddwn i'n cyrraedd y cam lle na allwn ymdopi ... a dim ond cael [fy mam] a dweud y gwir, roedd hynny'n beth mawr oherwydd roedd fy mywyd cyfan yn eithaf cymdeithasol. Roeddwn yn unig, a cheisiais beidio â gadael i hynny effeithio gormod arnaf. Roedd yn fy ngyrru’n hollol wallgof.”
– Person a oedd yn glinigol agored i niwed/yn hynod agored i niwed yn glinigol |
Roedd llawer o gyfranwyr sy’n agored i niwed yn glinigol ac yn hynod agored i niwed yn glinigol yn ei chael hi’n arbennig o anodd pan na chawsant ymuno â ffrindiau a theulu wrth i gloeon gloi leddfu yn ddiweddarach yn y pandemig. Yr oedd hyn hynod o ofidus i bobl hŷn neu bobl sy'n byw ar eu pen eu hunain.
| “ | Roedd fy chwiorydd yn gallu mynd i lefydd gyda'i gilydd a gwneud pethau, ac roedd fy merch a'i phlant a stwff, roedden nhw i gyd yn gallu ... ac roedd yn rhaid i mi eu gwylio, felly daethom yn fwy ynysig wrth i'r amser fynd yn ei flaen ac roedd gennych lai o bobl i siarad â. Ac fe gyrhaeddodd y llwyfan wedyn lle...fe wnaethoch chi fynd i'r gwely yn y diwedd a doeddech chi ddim eisiau dod allan, hyd yn oed ar ddiwrnod harddaf y flwyddyn, oherwydd doedd gen i ddim byd i godi amdano."
– Person a oedd yn glinigol agored i niwed/yn hynod agored i niwed yn glinigol |
Roedd rhai cyfranwyr a oedd wedi gwarchod yn gallu cadw mewn cysylltiad â'u teuluoedd trwy alwadau fideo gan ddefnyddio llwyfannau fel WhatsApp a FaceTime. Roedd hyn yn eu helpu i deimlo'n fwy cysylltiedig â'u hanwyliaid a lleihau teimladau o unigrwydd ac unigedd.
Clywsom enghreifftiau o bobl a oedd yn gwarchod eu hunain yn ymuno â 'swigod' cartref yn ddiweddarach yn y pandemig. Roedd dychwelyd mwy o gyswllt cymdeithasol yn rhyddhad enfawr i'r cyfranwyr hyn ac wedi helpu'n fawr i wella iechyd meddwl rhai pobl.
| “ | Byddwn yn dweud hynny [un] cadarnhaol oedd cael byrlymu gyda theulu arall. Roedd hynny'n newid bywyd. Rwy’n cofio bod hynny wedi fy ngalluogi i fynd i aros gyda fy ffrindiau adeg y Nadolig, a oedd ar garreg y drws pan nad oeddwn yn gallu gweld fy nheulu. Dwi jyst yn cofio, mi wnes i wylo pan ges i fy nghwt am y tro cyntaf ers amser maith.”
– Person a oedd yn glinigol agored i niwed/yn hynod agored i niwed yn glinigol |
Dywedodd rhai cyfranwyr â chyflyrau iechyd a oedd yn bodoli eisoes fod y rhain wedi gwaethygu oherwydd cysgodi.
| “ | Roedd cael gwybod fy mod mewn cymaint o risg o Covid-19 yn gwneud i mi deimlo allan o reolaeth ar fy iechyd ac o dan straen aruthrol. Roeddwn i'n ofni y byddwn i'n marw pe bawn i'n dal Covid-19. Trwy warchod, y risg wirioneddol i mi oedd methu â rheoli fy nghyflwr iechyd, a dwi’n ei wneud yn bennaf trwy ymarfer corff.”
– Person a oedd yn glinigol agored i niwed/yn hynod agored i niwed yn glinigol |
| “ | [Fy] daeth clefyd yr afu brasterog i fyny [yn ystod] y pandemig ac eto, mae'n debyg bod hynny oherwydd eich bod chi yn y tŷ, dim ymarfer corff, roeddech chi'n bwyta mwy. ”
– Person a oedd yn glinigol agored i niwed/yn hynod agored i niwed yn glinigol |
Roedd rhai cyfranwyr yn fwy cadarnhaol am warchod, yn aml oherwydd eu bod yn gyfforddus gartref, neu'n gallu cadw'n brysur ac yn gadarnhaol. Roedd y cyfranwyr hyn yn poeni am ddal Covid-19 ac nid oeddent am fentro gyda'u hiechyd. Yn aml roedd ganddyn nhw lety da, mynediad i ardd neu roedd ganddyn nhw anifail anwes i gadw cwmni iddyn nhw. Roedd llawer yn gallu cadw mewn cysylltiad â theulu o bell neu barhau i weithio mewn swyddi yr oeddent yn eu mwynhau. Roedd gallu datblygu trefn gyda phethau ystyrlon i'w gwneud yn lleihau teimladau o ddiflastod neu unigedd a'u helpu i aros yn bositif.
| “ | Gyda chymorth gardd…cefais fy sbwylio am bethau i'w gwneud. Felly mae'n debyg bod hynny wedi fy arbed yn llwyr, o ran iechyd meddwl ... nid oedd yn effeithio cymaint arna i mae'n debyg, â rhywun mewn stad o dai neu, fflatiau uchel neu rywbeth, nad oedd â'r gofod hwnnw y tu allan i fynd iddo.”
– Person a oedd yn glinigol agored i niwed/yn hynod agored i niwed yn glinigol |
| “ | Doedd neb o fy nghwmpas wrth i mi gysgodi ar fy mhen fy hun, roeddwn i'n teimlo'n ddiogel ac yn cael fy nerbyn gan y broses. [dw i] yn teimlo ychydig yn unig ar brydiau, ond gan fy mod yn gweithio gartref, roeddwn yn cael llawer o alwadau fideo bob dydd a hyd yn oed anfon dyfais fideo at fy mam a fy nhad fel y gallem gael prydau gyda'n gilydd dros y cyswllt fideo.”
– Person a oedd yn glinigol agored i niwed/yn hynod agored i niwed yn glinigol |
Heriau ymarferol gwarchodaeth
Disgrifiodd llawer o gyfranwyr a warchododd bod yn ofnus ynghylch gadael cartref ond hefyd yn ysu i weithio allan sut y byddent yn cael y cyflenwadau hanfodol yr oedd eu hangen arnynt. Roedd hyn yn aml yn canolbwyntio ar fwyd, ond roedd meddyginiaethau hefyd yn bwysig. Fe wnaethon nhw ofyn i deulu, ffrindiau neu gymdogion helpu neu ymweld â'r siopau ar eu rhan.
| “ | Pan fydd y cyngor [canllawiau] daeth yn amlwg, cawsom ein cadw bron fel carcharorion yn ein cartrefi ein hunain. Cawsom drafferth i gael slotiau siopa a bu’n rhaid i ni ddibynnu ar deulu nad oedd yn byw gerllaw, a chollasom ein rhwydwaith cymorth ar gyfnod anodd iawn yn ein bywydau.”
– Person a oedd yn glinigol agored i niwed/yn hynod agored i niwed yn glinigol |
| “ | Hwn oedd yr amser mwyaf brawychus i mi, gan nad oedd gen i neb, dim syniad sut y byddwn i’n cael help, bod ar fy mhen fy hun, gyda chael bwyd, moddion ac ati, yn enwedig gan fy mod yn byw yng nghefn gwlad… Roedd un ffrind… yn rheolwr rhanbarthol i Tesco a'i hymdrechion hi a'm rhoddodd ar restr eu blaenoriaeth. Yn y pen draw, roeddwn mewn dagrau pan ffoniais nhw, ac roedd y rhyddhad yn anfesuradwy. Ar ôl mis, roeddwn i’n gallu cael bwyd.”
– Person a oedd yn glinigol agored i niwed/yn hynod agored i niwed yn glinigol |
Profiadau o gael mynediad at ofal iechyd
Roedd profiadau o gael mynediad at wasanaethau gofal iechyd yn gymysg ond dywedodd rhai cyfranwyr a warchododd fod ganddynt fynediad da at ofal iechyd a meddyginiaethau, a'u bod yn ddiolchgar am y cymorth a gawsant. Dywedodd cyfranwyr wrthym fod y rhan fwyaf o’u hapwyntiadau meddyg teulu yn mynd rhagddynt ar-lein neu dros y ffôn. Yng nghamau cynnar y pandemig, roeddent yn aml yn teimlo bod galwadau ffôn neu fideo yn fwy diogel ac yn lleihau'r risg o ddal Covid-19.
Dywedodd y cyfranwyr hynny a gafodd archwiliadau rheolaidd gyda’u meddygon teulu yn gyffredinol fod ansawdd y gofal a gawsant drwy apwyntiadau o bell yn dda. Disgrifiodd cyfranwyr â chyflyrau iechyd hirdymor pa mor ddefnyddiol oedd eu meddygon teulu yn ystod y cyfnod hwn. Clywsom enghreifftiau o weithwyr gofal iechyd proffesiynol yn mynd gam ymhellach i’w cefnogi.
| “ | Gwnaeth fy mhractis meddyg teulu eu gorau i’m cadw’n ddiogel tra’n sicrhau fy mod yn dal i allu eu gweld ar gyfer gweithdrefnau angenrheidiol fel monitro profion gwaed.”
– Person a oedd yn glinigol agored i niwed/yn hynod agored i niwed yn glinigol |
| “ | Cefais fy mod yn cysylltu â nhw unrhyw bryd [Meddyg Teulu] am unrhyw beth…achos rydych chi'n cael pethau [bod] ewch ymlaen â'ch arthritis a'ch diabetes...byddent wedi gofyn i mi anfon ffotograff o'm cymalau neu fy monitro ar y ffôn...roeddent yn dda iawn. Roedd y meddyg ar y ffôn yn gwirio gyda mi yn gyson. Dim ffwdan o gwbl, ro’n i’n meddwl eu bod nhw ar y bêl mewn gwirionedd.”
– Person a oedd yn glinigol agored i niwed/yn hynod agored i niwed yn glinigol |
Stori LeilaCafodd Leila ddiagnosis o ganser ac arthritis soriatig cyn y pandemig. Dywedwyd wrthi am gysgodi yn ystod y pandemig gan fod ei chyflyrau iechyd yn ei gwneud yn ofynnol iddi gymryd cyffuriau gwrthimiwnedd. Oherwydd brys y driniaeth canser, nid oedd Leila wedi gofyn am driniaeth bellach ar gyfer ei chrydcymalau. Fodd bynnag, ar ôl llawdriniaeth, cafodd ei hun yn ei chael hi'n anodd rheoli'r boen a'r chwydd a chysylltodd â'i meddyg teulu ddiwedd 2021. Roedd yn anodd cael yr apwyntiad meddyg teulu cychwynnol, ond cynigiwyd prawf gwaed iddi yn y diwedd a chafodd ei chyfeirio at ymgynghorydd. O hyn ymlaen, gwnaeth y gefnogaeth a gafodd argraff fawr ar Leila. Cynigiwyd apwyntiadau iddi gydag ymgynghorwyr i sicrhau nad oedd mewn poen a bod ei chyflwr yn cael ei fonitro. “Yn fy mhrofiad gyda’r GIG, rydw i wedi cael pob apwyntiad y dylwn i fod wedi’i gael… Er bod argyfwng yn digwydd, rhywsut roedden nhw’n gallu rhoi’r gwasanaethau hynny i mi.” Weithiau roedd yn rhaid rheoli triniaethau o bell, a allai fod yn frawychus – er enghraifft, roedd angen iddi newid o dabledi i bigiad – ond llwyddodd i oresgyn ei hofnau gyda chymorth tîm yr ysbyty. “Cafodd yr hyfforddiant ar gyfer y pigiadau ei wneud ar y ffôn, ac roeddwn i ychydig yn bryderus oherwydd roeddwn i'n meddwl, 'O gosh, dwi ddim yn gwybod sut rydw i'n mynd i allu gwneud hyn.' Ond mewn gwirionedd, roedd yn syml, ac aeth y nyrs â mi drwyddo, wyddoch chi, ar ochr arall y ffôn, ac roedd yn llwyddiannus. A dyna un a fyddai [ddim?] gwaith i bawb nawr, ond i mi roedd yn wych, oherwydd nid oes rhaid i mi drafferthu [teithio].” |
Dywedodd y cyfranwyr a warchododd wrthym eu bod fel arfer yn gallu cael gafael ar feddyginiaethau trwy fferyllfa leol. Trefnodd nhw neu eu teulu i bresgripsiynau gael eu dosbarthu, neu i deulu a ffrindiau gasglu eu presgripsiynau.
| “ | Nid oedd cael presgripsiynau a phethau yn broblem...roedd yn ailadrodd [presgripsiwn] ar gyfer fy meddyginiaeth ... bu'n rhaid i mi ffonio ac yna 24 awr yn ddiweddarach roedd yn barod i'w gasglu. Felly, byddai’r wraig yn mynd i’w godi.”
– Person a oedd yn glinigol agored i niwed/yn hynod agored i niwed yn glinigol |
Pan oedd yn rhaid i bobl a oedd yn gwarchod eu hunain gael apwyntiad personol, fe wnaethant adrodd eu bod wedi derbyn citiau profi cartref Covid-19 yn y post ymlaen llaw. Fodd bynnag, i rai, roedd cyrraedd apwyntiadau meddygol yn anodd. Er enghraifft, rhannodd un cyfrannwr fod ganddo fertigo yn ystod y pandemig a phenderfynodd beidio â mynd i apwyntiad personol gyda'i feddyg teulu. Teimlent ei bod yn rhy anodd trefnu eu cludiant i gyrraedd yno.
| “ | Cyrraedd yno a chyrraedd yn ôl eto oedd hi oherwydd dydw i ddim yn meddwl fy mod i'n gallu gyrru, mae gen i vertigo, felly byddwn i wedi gorfod cael tacsi neu Uber neu rywbeth ac yna gwnaeth hynny i mi feddwl, 'Do Rydw i wir eisiau mynd i mewn i dacsi, mynd yr holl ffordd yno, efallai ddim, ac yna dod yn ôl eto?'…felly yn y pen draw fe wnes i adael iddo fynd ac ymdopi ag ef y ffordd orau y gallwn i.”
– Person a oedd yn glinigol agored i niwed/yn hynod agored i niwed yn glinigol |
Dywedodd cyfranwyr eraill wrthym eu bod yn ei chael yn anos cael mynediad at ofal a bod ganddynt rwystredigaethau ynghylch apwyntiadau o bell. Ymhlith y rhai a warchododd, roedd profiadau gofal sylfaenol yn ystod y pandemig yn debyg i gleifion eraill. Dywedon nhw y gallai fod yn anodd archebu apwyntiad meddyg teulu oherwydd y galw mawr. Er enghraifft, galwodd un cyfrannwr eu practis meddyg teulu bob dydd am bythefnos cyn iddynt allu gweld meddyg.
| “ | Mae'n rhaid i chi ffonio ar y diwrnod am 8:30 yn y bore, ynghyd â phawb arall, ac ymuno â'r galwadau hir i aros yn y ciw i gael apwyntiad. Ac, yn aml, byddech chi'n dod drwodd ac roedd yr holl apwyntiadau wedi mynd ... felly, mae wedi bod yn heriol hyd yn oed cael mynediad at y meddygon teulu.”
– Person a oedd yn glinigol agored i niwed/yn hynod agored i niwed yn glinigol |
Cafodd llawer o apwyntiadau gofal sylfaenol eu gohirio neu eu canslo hefyd. Rhai cyfranwyr a warchododd wedi cael problemau gyda chael mynediad at ofal, neu wedi dweud ei bod yn anoddach i weithwyr gofal iechyd proffesiynol asesu eu cyflwr iechyd heb gael ei archwilio yn bersonol.
Pan oedd cyfranwyr yn gallu gweld gweithiwr gofal iechyd proffesiynol yn bersonol, dywedasant eu bod yn gwisgo PPE. Maent hefyd teimlo'n galonogol gan faint o PPE roedd gweithwyr gofal iechyd proffesiynol yn ei wisgo wrth ymweld â'u meddyg teulu neu ysbyty.
| “ | Mewn ffordd, dwi'n meddwl fy mod i'n teimlo'n fwy diogel yn y feddygfa ac yn yr ysbyty, ble [gwisgo PPE] cael ei orfodi ac roedd pawb yn ei wneud, nag mewn siopau.”
– Person a oedd yn glinigol agored i niwed/yn hynod agored i niwed yn glinigol |
Dywedodd cyfranwyr eraill nad oeddent yn hoffi gwisgo PPE i'w hapwyntiadau. Roeddent yn teimlo ei fod yn gyfyngol neu'n ei gwneud yn anodd cyfathrebu â gweithwyr gofal iechyd proffesiynol.
| “ | Teimlai...ychydig yn glawstroffobig. Nid oeddwn yn gallu anadlu'n iawn gyda'r ewyllys gorau yn y byd. Mae masgiau yn gwneud ichi deimlo'n gyfyngedig. ”
– Person a oedd yn glinigol agored i niwed/yn hynod agored i niwed yn glinigol |
Myfyriodd rhai cyfranwyr ar yr hyn yr oedd eu profiad o warchod yn ei olygu i’w hiechyd hirdymor. Fe wnaethant awgrymu, wrth i gymdeithas ddechrau agor wrth gefn, fod llawer o bobl wedi symud ymlaen. Roeddent yn teimlo nad oedd y cyhoedd yn gwerthfawrogi'r bygythiad parhaus y mae Covid-19 yn ei achosi o hyd i bobl sy'n agored i niwed yn glinigol. Mae rhai yn dal i gyfyngu ar eu rhyngweithio cymdeithasol a'r hyn yr oeddent yn teimlo'n gyfforddus yn ei wneud y tu allan i'w cartrefi eu hunain. Roeddent eisiau mwy o gefnogaeth i bobl yn eu sefyllfa yn y dyfodol.
| “ | [Un] o fy ffrindiau yn hŷn, mae hi yn ei 70au, nid yw hi wedi dod yn ôl i'r eglwys ... mewn gwirionedd nid oes ganddi fywyd cymdeithasol o gwbl mwyach ... ei her fwyaf yw ei bod yn teimlo ei bod yn cael y wybodaeth hon, sy'n dweud wrthi ei bod yn agored i niwed, bod angen iddi amddiffyn ei hun, bod angen iddi gadw draw oddi wrth bobl, ei bod mewn perygl, ac nad yw ei risg wedi newid, a bod Covid-19 yn dal i fod o gwmpas. Ac felly mae hi’n ei chael hi’n anodd cysoni’r ffaith ei fod yn teimlo fel bod y cyngor wedi newid, ac eto, mae’r risg yn dal i fod yr un peth…Ac felly, rwy’n meddwl bod yna lawer o ofn, o hyd, wedi ei lapio o amgylch hynny i gyd i bobl.”
– Person a oedd yn glinigol agored i niwed/yn hynod agored i niwed yn glinigol |
Teimlai cyfranwyr ei bod yn bwysig i’r llywodraeth, systemau gofal iechyd a’r cyhoedd yn ehangach ddeall bod Covid-19 yn dal i fod yn fygythiad ac yn bryder i bobl sy’n agored i niwed yn glinigol, a dylai hyn gael ei adlewyrchu drwy well defnydd o PPE mewn lleoliadau gofal iechyd, a bod yn fwy hyblyg. a gwasanaethau gofal iechyd ymatebol.
Dysgu ar gyfer y dyfodol: gwarchodDywedodd llawer o gyfranwyr eu bod yn deall pwysigrwydd cysgodi i amddiffyn pobl rhag y firws yn ystod y pandemig. Fodd bynnag, clywsom dro ar ôl tro hefyd fod y canllawiau ar warchod yn rhy gyfyngol. Dywedodd llawer o gyfranwyr wrthym fod angen i ni ddysgu o'r difrod y mae cael ei ynysu wedi'i wneud - ac yn parhau i'w wneud - i iechyd pobl. Roedd yna lawer o alwadau am well cefnogaeth i'r rhai sy'n gwarchod, yn enwedig i amddiffyn a gwella iechyd meddwl a lles emosiynol pobl. Rhannodd rhai cyfranwyr hefyd sut y dylid bod wedi cynnig mwy o help i baratoi pobl oedd yn gwarchod eu hunain. “Roedd gwarchod yn dda, ond roedd angen mwy o gefnogaeth iechyd meddwl i bobl.” Cyfrannwr Mae Pob Stori o Bwys |
12.Profiadau o wasanaethau mamolaeth |
 |
Mae’r bennod hon yn archwilio profiadau menywod a ddefnyddiodd wasanaethau mamolaeth yn ystod pandemig Covid-19. Mae’n rhannu’r hyn a ddywedasant wrthym am y llwybr mamolaeth, gan gynnwys gofal cyn geni, esgor a geni, a gofal ôl-enedigol. Mae hefyd yn amlinellu profiad ehangach menywod o fod yn feichiog yn ystod y pandemig.
Profiadau o feichiogrwydd a gofal cyn geni
Dywedodd llawer o gyfranwyr wrthym pa mor ofnus, ofnus a phryderus yr oeddent yn teimlo ar ddechrau'r pandemig, gan mai ychydig a wyddys am effaith Covid-19 ar fenywod beichiog a’u plentyn heb ei eni. Arweiniodd hyn at rai menywod yn hunan-ynysu, gan eu bod yn poeni am ddal Covid-19 a pha effaith y gallai hyn ei chael ar eu babi
| “ | Achosodd y cyfyngiadau lawer iawn o bryder a phryder i mi, i’r graddau na allwn fwyta, tynnodd yn ôl rhag siarad ag eraill ac roeddwn yn bryderus iawn am roi genedigaeth.”
– Menyw a ddefnyddiodd wasanaethau mamolaeth |
| “ | Am dair wythnos cyn rhoi genedigaeth, arhosodd fy mhartner geni a minnau y tu fewn, i ffwrdd o archfarchnadoedd ac ati i beidio â mentro dal Covid-19.”
– Menyw a ddefnyddiodd wasanaethau mamolaeth |
| “ | Roeddwn i'n hynod baranoiaidd am ddod i gysylltiad â'r firws felly [dw i] dim ond gadael y tŷ am dro mewn mannau agored, roeddwn yn sychu arwynebau, dwylo, yn gwisgo masgiau ac yn ynysu fy hun oddi wrth deulu a ffrindiau yn gyson.”
– Menyw a ddefnyddiodd wasanaethau mamolaeth |
Dywedodd menywod a ddaliodd Covid-19 tra’n feichiog ei fod yn bryderus ac yn straen, gan nad oeddent yn gwybod sut y byddai eu symptomau’n datblygu. Mewn rhai achosion, dywedodd cyfranwyr wrthym y byddai gweithwyr gofal iechyd proffesiynol yn gwirio menywod yn rheolaidd i sicrhau nad oedd eu symptomau'n gwaethygu. Gofynnodd cyfranwyr eraill am gyngor gan ffynonellau eraill (fel GIG 111 i’r rhai sy’n byw yng Nghymru, Lloegr a’r Alban) pan oedd angen.
| “ | Cefais Covid-19 ddwywaith, pan oeddwn yn feichiog. Y tro cyntaf, roeddwn i tua 16 wythnos yn feichiog. Roeddwn yn sâl iawn. Nid oedd yn rhaid i mi fod yn yr ysbyty, ond roeddwn yn sâl iawn gartref. Roedden nhw [y tîm bydwreigiaeth] yn dda iawn ac roedden nhw’n fy ffonio bob dydd i wirio fi.”
– Menyw a ddefnyddiodd wasanaethau mamolaeth |
| “ | Roeddwn yn fyr o wynt un diwrnod ac yna un tro roedd gen i gur pen rhyfedd iawn. Doeddwn i ddim yn deall beth oedd yn digwydd. Fe wnaethon ni ffonio GIG 111 ac fe wnaethon nhw anfon ambiwlans ar unwaith a daethant yn syth, ac roeddwn i’n meddwl ei fod yn anhygoel.”
– Menyw a ddefnyddiodd wasanaethau mamolaeth |
Siaradodd llawer o gyfranwyr am y profiadau cadarnhaol a gawsant gyda gofal cyn geni. Canfuwyd bod eu bydwragedd, meddygon ymgynghorol a staff gofal iechyd eraill yn gymwynasgar ac yn gefnogol ar adeg anodd. Yng nghamau cynnar y pandemig, roedd ymgynghoriadau yn aml yn cael eu cynnal dros y ffôn neu ar-lein. Yn ddiweddarach yn y pandemig, pan gafodd y cyfyngiadau eu lleddfu, dywedodd cyfranwyr wrthym fod ymgynghoriadau wedi'u cynnal wyneb yn wyneb.
| “ | Cynhaliwyd fy sgwrs gychwynnol gyda bydwraig ar alwad fideo, ac roeddwn yn hapus â hynny, ar ôl hynny roedd fy holl apwyntiadau wyneb yn wyneb. Ni fu unrhyw ganslo erioed, [neu] aildrefnu. Cefais yr apwyntiadau drwodd, ac es iddynt. Cefais fy ngweld yn brydlon bob amser.”
– Menyw a ddefnyddiodd wasanaethau mamolaeth |
Rhannodd rhai menywod enghreifftiau o gyflyrau meddygol a oedd yn bodoli eisoes, fel asthma, a oedd yn cymhlethu eu gofal mamolaeth. Dywedodd y cyfranwyr hyn eu bod yn gallu cael mynediad at y driniaeth yr oedd ei hangen arnynt. Roedd hyn yn cynnwys sganiau ac archwiliadau rheolaidd gyda'u bydwraig.
| “ | Roeddwn yn gweld uned asesu beichiogrwydd cynnar oherwydd cefais ychydig o waedu. Roedd yn cael ei arwain gan feddygon ymgynghorol hefyd, oherwydd fy asthma...roeddwn i'n cymryd rhan. Felly, dwi'n meddwl fy mod i wedi cael fy ngweld gan bron pawb."
– Menyw a ddefnyddiodd wasanaethau mamolaeth |
Trwy gydol gwahanol gamau'r pandemig, rhannodd menywod beichiog sut roedd yn rhaid iddynt ymweld ag ysbytai i gael sganiau a gwiriadau yn unig. Yn gyffredinol, nid oedd partneriaid neu aelodau eraill o'r teulu yn cael mynychu gyda nhw. Roedd mynychu apwyntiadau ac ymgynghoriadau yn brofiad unig a brawychus, yn enwedig yn gynnar yn y pandemig. Disgrifiodd merched a oedd wedi rhoi genedigaeth o'r blaen pa mor rhyfedd oedd y profiad o gymharu.
| “ | Roedd eich sganiau'n wahanol iawn, roedd yn rhaid i'ch partner, fy ngŵr aros y tu allan nes i chi ddod i mewn i'r ystafell. Roedd popeth ar ei ben ei hun i raddau helaeth iawn…y sganiau, roedd yn rhaid i chi aros y tu allan, roedd gennych swnyn, yna roedd yn rhaid dod i fyny pan oedd yn amser mynd i'r ystafell a chael y sgan. Roedd pawb o leiaf yn gwisgo masgiau. ”
– Menyw a ddefnyddiodd wasanaethau mamolaeth |
Roedd cael mynediad at ofal yn unig yn ychwanegu at deimladau o bryder ac yn peri gofid i rai merched. Er enghraifft, disgrifiodd un cyfrannwr a oedd wedi colli ei golwg yr heriau o beidio â chael partner yn bresennol i’w chynnal.
| “ | Roedd mynd trwy wasanaethau mamolaeth a rhoi genedigaeth pan oedd y GIG yn chwalu o'm cwmpas gyda haenau ychwanegol o golli golwg yn anodd. Roedd yr holl wybodaeth yn seiliedig ar bapur, doeddwn i ddim yn gallu gweld y sonogram a doedd gen i ddim partner yno i egluro pethau i mi, roeddwn i'n llawn pryder. Ni roddwyd cyfrif am fy nam ar fy ngolwg, roeddent yn canolbwyntio ar lywio gofal yn covid – nid oedd darllen llythyrau i mi yn flaenoriaeth.”
– Menyw a ddefnyddiodd wasanaethau mamolaeth |
Gorfod roedd rhyngweithio â gweithwyr gofal iechyd proffesiynol yn unig hefyd yn anodd i fenywod os oedd problem iechyd bosibl gyda'u plentyn.
| “ | Es i apwyntiad bydwraig arferol, ond roedd hi'n poeni am y babi a dywedodd na allai glywed curiad y galon. Dywedodd fod angen ambiwlans brys arnaf neu i wneud fy ffordd i'r ysbyty yn gyflym. Gyrrasom yn gyflym i [y] ysbyty lle roedden nhw'n fy nisgwyl i. Wrth y drysau dywedwyd wrthyf mai fi oedd yr unig un a ganiateir i mewn….roeddem yn meddwl [y] Roedd y babi wedi marw ar 32 wythnos o feichiogrwydd, ond roedd yn rhaid i mi fynd i mewn ar fy mhen fy hun. Roedd hwn yn un o eiliadau mwyaf brawychus fy mywyd cyfan. Yn y cyfamser [fy mhartner] gorfod aros y tu allan i’r ysbyty i aros i gael gwybod a oedd ei faban yn fyw ai peidio.”
– Menyw a ddefnyddiodd wasanaethau mamolaeth |
Stori GwenMae Gwen yn byw gyda'i gŵr a'i phlentyn. Roedd hi'n feichiog yn ystod y pandemig. Ar ôl i Gwen fynd am ei sgan 12 wythnos cafodd lawer o waedu, a oedd yn cael ei ystyried i ddechrau fel camesgoriad, ond yn y pen draw cafodd ddiagnosis o hematoma (gwaedu neu gasglu gwaed y tu allan i'r pibellau gwaed). Pan dderbyniwyd Gwen i'r ysbyty ar gyfer arsylwi a phrofion, nid oedd ei gŵr yn cael aros gyda hi nac aros dros nos. Roedd hwn yn gyfnod emosiynol ac annifyr i Gwen, ac roedd hi’n teimlo’n unig iawn heb gefnogaeth ei gŵr nac aelodau eraill o’r teulu. “Cafodd ganiatâd i ddod i mewn yn fyr tra roedden nhw’n fy nghyfaddef i, tra roedden nhw’n gwneud yr asesiad cychwynnol, ac yna roedd yn rhaid iddo fynd i aros y tu allan, ac roeddwn i, i mi, yn teimlo’n unig iawn.” Arhosodd bydwraig ar y ward ar ei thraed gyda Gwen yn sgwrsio am y rhan fwyaf o'r nos a rhoi gwybod iddi hefyd pan oedd yn amser iddi orffwys. Y diwrnod wedyn, derbyniodd Gwen ganlyniadau’r prawf a oedd yn cadarnhau nad camesgoriad oedd y gwaedu, ac roedd hi’n gallu mynd adref. Er ei bod yn ddiolchgar am y gofal a’r cymorth a gafodd, byddai wedi hoffi mwy o hyblygrwydd i’w phartner fod yno a’i chefnogi. “Dim ond at ddrws y ward yr oedd fy ngŵr yn gallu fy ngherdded a dyna ni. Ac i fod yn deg, eisteddodd y fydwraig gyda ni drwy'r nos fwy neu lai ar y ward. Dim ond ychydig o gleifion oedd ganddyn nhw, ond yn amlwg menywod oedd yn aros i roi genedigaeth.” |
Clywsom gan lawer o gyfranwyr nad oedd canllawiau ynghylch cael pobl gyda nhw yn ystod apwyntiadau yn cael eu dehongli’n gyson, ac roedd hyn yn teimlo’n annheg. Ar gyfer rhai apwyntiadau dywedodd menywod beichiog wrthym y gallent gael partner yn bresennol, tra na allent ar adegau eraill. Achosodd peidio â bod yn glir a allai rhywun fynd gyda nhw straen a dryswch pellach i rai menywod.
| “ | Dywedodd un fydwraig, 'Byddwn wedi gadael i chi ddod i mewn [i bartner y cyfrannwr], pam na fyddent yn gadael i chi ddod i mewn?' Felly, mae'n, math o, pwy bynnag oedd yno efallai. Dydw i ddim yn gwybod.”
– Menyw a ddefnyddiodd wasanaethau mamolaeth |
Dywedodd y cyfranwyr hyn y dylai fod mwy o gysondeb o ran sut y cymhwyswyd y canllawiau, ond hefyd mwy o hyblygrwydd i bobl yr oedd angen cymorth arnynt.
| “ | [Roedd yn] anodd iawn, ingol iawn, oherwydd dim ond un person a ganiatawyd i chi, neu ni chawsoch neb ddod i mewn, gyda'ch apwyntiadau. Roeddwn yn 20, newydd ddarganfod fy mod yn feichiog. Yn amlwg, yn ofnus iawn, ac nid oedd unrhyw ryddid o gwbl, yn unman. A oedd yn wirioneddol, yn anodd iawn. Byddai hynny'n gwneud fy iechyd meddwl yn llawer gwaeth. Achosodd straen i mi, a oedd wedyn, yn amlwg, yn achosi straen i’r babi. Roeddwn yn sâl iawn drwy gydol fy meichiogrwydd. Sydd wir wedi cychwyn o’r straen.”
– Menyw a ddefnyddiodd wasanaethau mamolaeth |
Roedd absenoldeb dosbarthiadau cyn-geni a chynenedigol yn gynnar yn y pandemig yn gwneud i fenywod deimlo'n fwy ynysig. Roedd llawer o gyfranwyr yn rhannu bod cyfyngiadau cloi yn golygu nad oeddent wedi gallu datblygu rhwydwaith cymorth o bobl a oedd yn mynd trwy brofiad tebyg. Roedd hyn yn arbennig o anodd a thrallodus yng nghamau cynnar y pandemig, pan ddaeth dosbarthiadau cyn geni i ben a heb symud ar-lein eto.
| “ | Doedd gen i ddim dosbarthiadau cyn-geni o gwbl, a gwn yn ddiweddarach eu bod yn gwneud dosbarthiadau. Ni chynygiwyd dim o hono i mi. Rwy'n teimlo eto bod rhan o fy meichiogrwydd wedi'i ddwyn oddi wrthyf."
– Menyw a ddefnyddiodd wasanaethau mamolaeth |
| “ | Roeddwn i eisiau mynd i ddosbarth cyn geni, ond es i ddim gan nad oedden nhw ar gael o gwbl.”
– Menyw a ddefnyddiodd wasanaethau mamolaeth |
Rhannodd rhai merched sut roedd peidio â mynychu dosbarthiadau cyn-geni yn golygu nad oeddent yn gallu ffurfio cyfeillgarwch newydd a allai eu cefnogi yn ystod mamolaeth gynnar. Dywedasant fod hyn wedi cyfrannu at brofiadau diweddarach o unigrwydd ac iselder ôl-enedigol (a amlinellir ymhellach yn ddiweddarach yn y bennod hon).
Esgor a genedigaeth
Roedd profiadau merched adeg esgor a geni yn amrywio yn dibynnu ar ba bryd yr oeddent yn feichiog yn ystod y pandemig.
Cyfranwyr a oedd yn agos at eu dyddiad dyledus o gwmpas y cloi cyntaf yn aml yn disgrifio hwn fel cyfnod ansicr a brawychus iawn. Nid oedd yn eglur iddynt sut y byddent yn derbyn gofal yn ystod y cyfnod esgor a geni. Rhannodd menywod beichiog enghreifftiau o wybodaeth anghyson am sut y byddai esgor a genedigaeth yn cael eu rheoli, a ychwanegodd at ddryswch.
| “ | Roedd hynny'n eitha brawychus...roeddwn i'n fam am y tro cyntaf…byddech chi'n clywed sïon, byddai pobl yn dweud eu bod [partneriaid ac aelodau o'r teulu] ni allant fynd i mewn o gwbl neu ni allant fynd i mewn nes bod y babi yn dod allan.”
– Menyw a ddefnyddiodd wasanaethau mamolaeth |
Wrth i'r pandemig fynd rhagddo ac wrth i nifer y bobl yn yr ysbyty gyda Covid-19 ddechrau cynyddu, roedd yn amlwg bod ysbytai dan straen. Roedd hyn yn golygu bod rhai menywod yn dewis cael genedigaeth gartref oherwydd eu bod yn poeni am ddal Covid-19. Roedd y cyfranwyr hyn hefyd yn poeni am ychwanegu at y straen ar systemau gofal iechyd trwy fynd i'r ysbyty. Fodd bynnag, canfu rhai fod bydwragedd yn amharod iawn i awgrymu genedigaeth gartref.
Stori EileenMae Eileen yn 31 oed ac mae ganddi dri o blant. Mae hi'n byw mewn ardal wledig, yn agos at ei theulu. Roedd hi'n feichiog gyda'i thrydydd plentyn ym mis Ebrill 2020 pan oedd y DU yn ei chloi am y tro cyntaf. Roedd Eileen yn awyddus i gael genedigaeth gartref yn ystod y pandemig, a chyn hynny roedd hi wedi dewis y math hwn o enedigaeth ar gyfer ei hail blentyn. Ar ôl ei chyfarfodydd cychwynnol gyda'i bydwraig, gofynnodd am enedigaeth gartref, ond canfu ei bod wedi'i chyfarfod ag amharodrwydd gan nad oedd gweithwyr gofal iechyd proffesiynol yn siŵr beth oedd yn cael ei ganiatáu o dan y canllawiau. “Rydw i wir i mewn i hunaneirioli pan mae'n dod i feichiogrwydd. [roedd yn rhaid i mi ateb] llawer o gwestiynau.” Teimlai fod yn rhaid iddi eirioli’n gryf iawn drosti’i hun i gael mynediad at enedigaeth gartref gyda’r gweithwyr gofal iechyd proffesiynol perthnasol, a chafodd sawl trafodaeth am sut y byddai’r tîm genedigaethau cartref yn gweithio iddi, a sut y byddai canllawiau a PPE yn cael eu defnyddio. Yn y diwedd, cytunodd y tîm genedigaethau cartref i eni'r babi gartref, a llwyddodd Eileen i gael ei phartner a'i mam yn bresennol ar yr enedigaeth. “Dim ond llawer o gwestiynu ac, fel, cael eich gohirio a hoffi, 'Fe ddown yn ôl atoch chi.' Dyna oedd hi’n bennaf ac yna gorfod mynd ar drywydd pethau.” |
Dywedodd menywod a ddewisodd roi genedigaeth yn yr ysbyty wrthym yn aml am y profiadau cadarnhaol a gawsant, er gwaethaf yr amgylchiadau heriol. Canfu llawer o gyfranwyr fod bydwragedd, meddygon a gweithwyr gofal iechyd proffesiynol eraill yn gymwynasgar ac yn gefnogol trwy gydol y cyfnod esgor a geni. Roeddent yn ddiolchgar am y gofal a gawsant yn ystod cyfnod anodd i'r gwasanaeth iechyd.
| “ | Roedd fy mydwraig yn hollol anhygoel, roedden nhw'n wych. Felly, ie, yn gyffredinol, byddwn yn dweud ei fod yn mynd fel [wel] fel y gallai.”
– Menyw a ddefnyddiodd wasanaethau mamolaeth |
Fodd bynnag, roedd rhai menywod a ddefnyddiodd wasanaethau mamolaeth yn rhannu problemau a wynebwyd ganddynt yn ystod genedigaeth. Er enghraifft, soniodd un cyfrannwr pan aethant i’r ysbyty i roi genedigaeth, y dywedwyd wrthynt fod y ward famolaeth ar gau oherwydd prinder staff. Roeddent yn tybio bod hyn oherwydd y pandemig. Er eu bod yn cael eu gweld gan fydwragedd a meddygon, roedd hyn yn eu poeni i ddechrau gan na allent ddilyn eu hoffterau ar gyfer rhoi genedigaeth.
Dywedodd menyw arall wrthym nad oedd yn cael ei gwirio yn y ward famolaeth yn iawn, a bod hyn yn golygu aros am amser hir heb gael ei gweld gan unrhyw un. Pan ddarganfu gweithwyr gofal iechyd proffesiynol gymhlethdodau gyda'r enedigaeth - a oedd yn bygwth bywyd ei phlentyn - roedd hyn yn peri straen ac yn peri pryder mawr iddi. Teimlai'r cyfrannwr ei bod wedi cael ei siomi a'i bod yn hynod siomedig gyda'r gofal a gafodd.
Pryder cyffredin oedd yr anghysondeb ynghylch bod partneriaid geni neu aelodau eraill o'r teulu yn bresennol yn yr enedigaeth. Roedd y rhain yn debyg i'r pryderon am ofal cyn geni. Dywedodd llawer o fenywod wrthym ei bod yn annheg ac yn ofidus nad oeddent yn cael cael partner geni gyda nhw.
Dywedodd y rhai a oedd wedi'u gwahanu oddi wrth eu partneriaid yn ystod y cyfnod esgor a genedigaeth yn aml nad oedd ganddynt y cymorth emosiynol yr oedd ei angen arnynt. Roedd rhai cyfranwyr yn drist nad oedd eu partner wedi cymryd cymaint o ran ag y dylent fod. Disgrifiodd eraill broblemau yn ystod yr enedigaeth a phrofiadau anodd oherwydd eu bod angen yr help y byddai eu partner wedi ei gynnig.
| “ | Rhoddais enedigaeth gartref gyda fy nhîm (Rhagfyr 2020), ond yn anffodus, cefais gymhlethdodau a bu’n rhaid i mi gael fy nerbyn i’r ysbyty y noson honno am 1am…roedd yn rhaid i fy mhartner eistedd y tu allan i’r ward am 3-4 awr drwy’r nos. Gadawyd fy mabi mewn crud wrth fy ymyl, ond oherwydd rhoi genedigaeth nid oeddwn yn gallu eistedd i fyny a symud o gwmpas heb boen eithafol. Roeddwn i mewn trallod. Y rheolau ynghylch dim partneriaid mewn ysbytai oedd y peth mwyaf niweidiol a grëwyd yn ystod y pandemig. ”
– Menyw a ddefnyddiodd wasanaethau mamolaeth |
| “ | Roeddwn mewn esgor dwys ar fy mhen fy hun am lawer o'r amser gyda chefnogaeth wych gan fy mydwraig, ond nid oedd yr un peth [fel cael ei phartner yn bresennol].”
– Menyw a ddefnyddiodd wasanaethau mamolaeth |
Rhoddodd rhai merched enghreifftiau o bobl yn cael gwybod am reolau gwahanol mewn amgylchiadau tebyg iddynt. Roedd hyn yn rhwystredig ac yn ychwanegu ymhellach at ymdeimlad o annhegwch.
| “ | Nid oedd fy mhartner yn cael dod i mewn eto roedd teuluoedd a oedd yn derbyn gofal mewn ymddiriedolaethau eraill wedi cael profiadau gwahanol, roedd rhai o’n ffrindiau’n feichiog ar yr un pryd â ni yn cael mynd i mewn i bob apwyntiad a oedd yn rhwystredig iawn.”
– Menyw a ddefnyddiodd wasanaethau mamolaeth |
Dywedodd menywod a roddodd enedigaeth yn yr ysbyty yn ddiweddarach yn y pandemig fod eu partneriaid geni fel arfer yn cael bod yn bresennol. Roedd hyn yn galonogol i'r cyfranwyr hyn gan ei fod yn caniatáu iddynt rannu eu profiad.
| “ | Ar y dechrau, roedden nhw'n llym yn ei gylch ac yn dweud, fel, doedd neb yn gallu dod i mewn. Ond wedyn, erbyn y diwedd, yn amlwg pan gafodd ei eni roedd pawb jest yno. Rwy'n meddwl amdano nawr. Roedd pawb yn yr ystafell.”
– Menyw a ddefnyddiodd wasanaethau mamolaeth |
Roedd hefyd yn aneglur i rai cyfranwyr a allai partneriaid aros dros nos neu a allent aros y tu hwnt i oriau ymweld. Er enghraifft, rhannodd un fenyw sut y dywedwyd wrthi na allai ei phartner aros dros nos gan fydwraig, ond dywedodd un arall y gallai aros oherwydd bod ganddynt efeilliaid.
| “ | Tua thridiau ar ôl bod yn yr ysbyty, dywedodd un o'r bydwragedd, 'Rwy'n synnu nad yw eich gŵr yn aros ac yn eich helpu gyda'r nos.' Ac roeddwn yn union, fel, 'Wel, nid yw'n cael, fel, oriau ymweld, ydych chi'n gwybod yr oriau ymweld?' A dyma hi'n mynd, 'O, wel, i efeilliaid, mae'r gŵr yn cael aros yn y nos, achos mae gen ti ddau fabi. Dau faban, dau oedolyn.' A doedd neb wedi dweud hynny wrthym ni, doedd neb wedi dweud ei fod yn cael aros.”
– Menyw a ddefnyddiodd wasanaethau mamolaeth |
Disgrifiodd menywod eraill mai dim ond am gyfnod byr y gallai eu partneriaid aros gyda nhw. Fel arfer dywedwyd wrthynt fod yn rhaid i'w partner adael oherwydd ei fod wedi mynd heibio'r amser ymweld â'r ysbyty. Dywedodd rhai cyfranwyr wrthym fod hyn yn eu gwneud yn grac oherwydd nad oeddent yn meddwl ei fod yn deg.
| “ | Doeddwn i ddim yn deall pam na allai aros gyda mi oherwydd cafodd y babi ei eni am 10:10 yn y nos, roedd wedi mynd heibio oriau ymweld, felly roedd yn rhaid iddo fynd. Roeddwn i'n meddwl bod hynny'n rhyfedd iawn. Roedden ni'n eistedd yn ein stafell fach ar ein pennau ein hunain. Felly pam y byddai'n rhaid iddo fynd?"
– Menyw a ddefnyddiodd wasanaethau mamolaeth |
| “ | Dim ond sefyllfa chwerthinllyd oedd hi. Ac yna dywedasant, felly cefais hi am 12 o'r gloch, beth bynnag oedd hi, hanner awr wedi 12 y prynhawn. Ac yna dywedasant, 'Dim ond tan 8 o'r gloch y gallai aros gyda mi oherwydd dyna pryd y daeth yr amseroedd ymweld i ben.”
– Menyw a ddefnyddiodd wasanaethau mamolaeth |
Cwestiynodd rhai menywod y mesurau sydd ar waith i leihau lledaeniad Covid-19. Roedd y cyfranwyr hyn o'r farn nad oedd y canllawiau'n gwneud synnwyr a'u bod yn ddiangen. Awgrymodd eraill fod rheolau Covid-19 yn cael eu dehongli'n wahanol yn dibynnu ar y gweithwyr gofal iechyd proffesiynol. Creodd hyn ymdeimlad o annhegwch i rai merched a rannodd eu stori gyda ni.
| “ | Roeddech chi'n gwisgo'r mwgwd o amgylch yr ysbyty, i fyny i'r ward, ond yna unwaith roeddech chi ar y ward, roeddech chi'n cael ei dynnu i ffwrdd ... doedd dim ohono erioed yn gwneud synnwyr, ac yna roedd yr un peth pryd bynnag roeddech chi i lawr y grisiau, pryd bynnag Roeddwn i i mewn i esgor; roedd yn rhaid i chi ei wisgo tra roedden nhw'n eich archwilio chi."
– Menyw a ddefnyddiodd wasanaethau mamolaeth |
Gofal ôl-enedigol
Yng nghamau cynnar y pandemig, clywsom sut daeth rhai archwiliadau ôl-enedigol yn 'ymweliadau carreg drws', gyda bydwragedd ac ymwelwyr iechyd yn cynnal asesiadau wrth y drws ffrynt. Disgrifiodd rhai cyfranwyr pa mor rhyfedd oedd hyn.
| “ | Stopiodd neu barhaodd yr ymweliadau ychydig, a daethant, mewn gwirionedd, yn debyg i ymweliadau carreg drws. Felly, roedd yn rhaid i ni ddod â phethau fel y glorian i mewn i'r cyntedd a phwyso fy merch ac yna rhoi'r glorian yn ôl ar y grisiau ac ni ddaeth yr ymwelwyr iechyd i mewn. Roedd hynny'n rhyfedd iawn.”
– Menyw a ddefnyddiodd wasanaethau mamolaeth |
Profodd cyfranwyr eraill ofal ôl-enedigol dros y ffôn, a oedd yn aml yn ddefnyddiol ac yn gefnogol iddynt. Roeddent yn teimlo bod gweithwyr gofal iechyd proffesiynol yn cymryd yr amser i ddarllen eu nodiadau a deall eu hanes meddygol. Fodd bynnag, rhannodd ychydig o fenywod sut nad oedd cymorth o bell yn gweithio'n dda ar gyfer bwydo ar y fron yn gynnar yn y pandemig.
| “ | Roeddwn yn ceisio bwydo fy mabi ar y fron a chefais ychydig o anawsterau bwydo ar y fron bryd hynny, felly nid oedd y gefnogaeth yno mewn gwirionedd oherwydd nid oedd unrhyw un i ddod i allu, yn gorfforol, i weld beth sy'n digwydd. Felly roedd hynny’n dipyn o straen, a dweud y gwir, roedd hwnnw’n gyfnod eithaf dirdynnol, i beidio â chael yr hyn y byddech chi’n ei alw’n gefnogaeth arferol neu jyst, chi’n gwybod…eich rhieni.”
– Menyw a ddefnyddiodd wasanaethau mamolaeth |
| “ | Mae cymorth bwydo ar y fron yn wasanaeth hanfodol; mae ymweliadau iechyd yn wasanaeth hanfodol. Ni all rhwygo’r llyfr rheolau yn enw rheoli heintiau byth ddigwydd eto.”
– Menyw a ddefnyddiodd wasanaethau mamolaeth |
Dywedodd rhai merched a roddodd enedigaeth yn gynharach yn y pandemig wrthym na welsant ymwelydd iechyd neu fydwraig am sawl mis ar ôl yr enedigaeth. Achosodd hyn bryder i lawer o fenywod a oedd eisoes yn teimlo'n ynysig fel mamau newydd. Roedd hyn yn arbennig o heriol gan nad oedd cymorth ar gael gan aelodau o'r teulu neu ffrindiau oherwydd cyfyngiadau pandemig.
| “ | Ni welais fydwraig na neb nac ymwelydd iechyd – tua 5 mis oed oedd y babi. Roeddwn i’n meddwl y gallai rhywbeth fod yn ddifrifol o’i le ac fel mam am y tro cyntaf, fyddwn i ddim yn gwybod chwaith.”
– Menyw a ddefnyddiodd wasanaethau mamolaeth |
| “ | Ar ôl genedigaeth, gofal dilynol cyfyngedig oedd gen i a dim ond pan wnes i sgrechian y gwelais ymwelydd iechyd [gweld nhw].”
– Menyw a ddefnyddiodd wasanaethau mamolaeth |
Yn ddiweddarach yn y pandemig, roedd bydwragedd ac ymwelwyr iechyd yn fwy cyffredin yn ymweld â phobl yn bersonol wrth wisgo PPE. Roedd y cyfranwyr a gafodd yr ymweliadau wyneb yn wyneb hyn yn galonogol ac yn gadarnhaol ynghylch y cymorth a gynigiwyd iddynt.
| “ | Roedd gen i fydwraig yn dod allan bob tro ... ac roedd hi'n wych. Daeth i mewn gyda mwgwd ymlaen, ei menig ymlaen, a'r ffedog blastig. Ac fe wnaethon nhw bopeth yn iawn, oherwydd yn amlwg maen nhw'n pwyso'r babi, roedd eu clorian i gyd wedi'u glanhau cyn ac ar ôl iddynt eu defnyddio. Roedden nhw'n wych.”
– Menyw a ddefnyddiodd wasanaethau mamolaeth |
| “ | Roedd yr ymwelydd iechyd yn dda iawn i mi. Roeddwn i'n hoffi ei chael hi i ddod i'r tŷ a gweld y babi. Hefyd, y fydwraig a gefais, hi oedd fy mydwraig cyn-geni ar gyfer y beichiogrwydd, ac yna fe arhosodd wedi’i neilltuo i chi am ryw bythefnos ar ôl i’ch babi gael ei eni, ac yna cewch eich trosglwyddo i’r ymwelydd iechyd.”
– Menyw a ddefnyddiodd wasanaethau mamolaeth |
Clywsom gan rai menywod am y ffordd yr oeddent yn teimlo nad oedd eu profiad mamolaeth cyffredinol yr hyn y dylai fod. Roedd hyn yn wir hyd yn oed ymhlith rhai a oedd yn gadarnhaol am eu gofal. Teimlai cyfranwyr fod yr ymdeimlad hwn o golli allan yn dod yn fwy amlwg pan oedd ganddynt amser i fyfyrio ar eu profiadau ar ôl yr enedigaeth.
| “ | Roeddwn i'n teimlo nad oedd neb hyd yn oed wedi siarad â mi am fy adferiad corfforol, hyd yn oed yn yr archwiliad postpartum 6-8 wythnos. Roedd popeth yn teimlo'n wag, ac rwy'n meddwl ei fod wedi newid fy marn o gael ail blentyn yn fawr oherwydd rwyf wedi cael fy nharo gymaint gan y profiad. Nid wyf byth eisiau ailadrodd hynny byth eto. Covid-19 oedd 100% y rheswm dros fy nhrwma ac mae’r gwasanaethau iechyd, er eu bod yn wych, o safbwynt mamolaeth, yn teimlo’n brin o ofal digonol.”
– Menyw a ddefnyddiodd wasanaethau mamolaeth |
Rhannodd mamau sut roedd y misoedd ôl-enedigol yn hynod heriol iddynt yn ystod y pandemig. Fel y dangosir gan brofiadau sydd eisoes wedi’u cynnwys yn y bennod hon, roedd menywod yn aml yn rhannu eu bod wedi colli cyfleoedd i ddatblygu cyfeillgarwch a rhwydweithiau cymorth, yn enwedig heb unrhyw ddosbarthiadau cyn geni. Ar ôl yr enedigaeth, adroddwyd teimladau o unigrwydd, unigedd ac, mewn rhai achosion, iselder ôl-enedigol. Dywedodd rhai cyfranwyr eu bod yn cael trafferth cael mynediad at gymorth iechyd meddwl ôl-enedigol.
| “ | Cefais fy atal rhag cael absenoldeb mamolaeth arferol, gan gymdeithasu â mamau newydd [a] adeiladu rhwydwaith cymorth lleol.”
– Menyw a ddefnyddiodd wasanaethau mamolaeth |
| “ | Nid oedd unrhyw wasanaethau plant, fel, nid oeddem yn gallu mynd i unrhyw grwpiau neu unrhyw beth, neu hyd yn oed fynd allan o'r tŷ, felly rydych chi'n unig yn y pen draw. Mae bod yn fam yn unig fel y mae, ond gwnaeth hynny 10 gwaith yn waeth.”
– Menyw a ddefnyddiodd wasanaethau mamolaeth |
Amlygodd mamau newydd hefyd eu pryderon nad yw eu plentyn yn datblygu sgiliau cymdeithasol ac yn rhyngweithio â phlant ifanc eraill.
| “ | Ni allwn gael mynediad at unrhyw gymorth yn y gymuned na chymdeithasu fy mabi am fisoedd a misoedd.”
– Menyw a ddefnyddiodd wasanaethau mamolaeth |
| “ | Roedd absenoldeb mamolaeth yn anodd, nid oedd unrhyw ddosbarthiadau na grwpiau cymorth i ymuno â nhw i helpu i ddatblygu fy un bach [neu] helpwch fi i ddod o hyd i ffrindiau gyda babanod eraill [o] oedran tebyg.”
– Menyw a ddefnyddiodd wasanaethau mamolaeth |
Disgrifiodd menywod eraill sut roedd contractio Covid-19 wedi parhau i achosi pryder iddynt, gan nad oeddent yn siŵr pa effaith y byddai’n ei chael ar eu plant yn y dyfodol.
| “ | Nid wyf yn deall yr effaith y mae'n ei chael ar blant neu fabanod o hyd, oherwydd rwy'n dal i boeni, fel, yn amlwg, dim ond dwy flwydd oed ydyw. Rwy’n dal i boeni amdano’n cael Covid-19 a beth sy’n mynd i ddigwydd amdano, os yw’n mynd yn sâl iawn.”
– Menyw a ddefnyddiodd wasanaethau mamolaeth |
| “ | Rwy'n meddwl bod cael babi ifanc hefyd yn ei wneud yn fwy brawychus, heb wybod pa fath o effaith y gallai ei gael arnynt. Felly, rwy’n meddwl mai sut yr effeithiodd arnaf yn bendant oedd y gor-wyliadwriaeth, y pryder, dim ond am ei fod yn anhysbys, a dim ond poeni am ei ddal.”
– Menyw a ddefnyddiodd wasanaethau mamolaeth |
13. Atodiad |
Cwmpas dros dro Modiwl 3
Defnyddiwyd cwmpas dros dro Modiwl 3 i arwain sut yr oeddem yn gwrando ar bobl ac yn dadansoddi eu straeon. Amlinellir cwmpas y modiwl isod a gellir ei ganfod hefyd ar y Gwefan Ymholiad Covid-19 y DU.
Bydd y modiwl hwn yn ystyried effaith pandemig Covid-19 ar systemau gofal iechyd yng Nghymru, Lloegr, yr Alban a Gogledd Iwerddon. Bydd hyn yn cynnwys ystyried canlyniadau gofal iechyd y ffordd yr ymatebodd y llywodraethau a'r cyhoedd i'r pandemig. Bydd yn archwilio gallu systemau gofal iechyd i ymateb i bandemig a sut esblygodd hyn yn ystod pandemig Covid-19. Bydd yn ystyried y sectorau a gwasanaethau gofal iechyd sylfaenol, eilaidd a thrydyddol a phrofiad pobl o ofal iechyd yn ystod y pandemig, gan gynnwys drwy gyfrifon enghreifftiol. Bydd hefyd yn archwilio anghydraddoldebau sy'n gysylltiedig â gofal iechyd (megis mewn perthynas â chyfraddau marwolaeth, PPE ac ocsimetrau), gan roi ystyriaeth fanwl bellach mewn modiwl dynodedig ar wahân.
Yn benodol, bydd y modiwl hwn yn archwilio:
- Effaith Covid-19 ar brofiad pobl o ofal iechyd.
- Gwneud penderfyniadau craidd ac arweinyddiaeth o fewn systemau gofal iechyd yn ystod y pandemig.
- Lefelau staffio a chapasiti gofal critigol, sefydlu a defnyddio ysbytai Nightingale a'r defnydd o ysbytai preifat, 111, 999 a gwasanaethau ambiwlans, meddygfeydd ac ysbytai a chydweithrediad trawsadrannol rhwng gwasanaethau.
- Darpariaeth a thriniaeth gofal iechyd i gleifion â Covid-19, ymateb systemau gofal iechyd i dreialon clinigol ac ymchwil yn ystod y pandemig. Dyraniad staff ac adnoddau. Yr effaith ar y rhai sydd angen gofal am resymau heblaw Covid-19. Ansawdd y driniaeth ar gyfer cleifion Covid-19 a chleifion nad ydynt yn Covid-19, oedi mewn triniaeth, rhestrau aros a phobl nad ydynt yn ceisio neu'n derbyn triniaeth. Gofal lliniarol. Rhyddhau cleifion o'r ysbyty.
- Gwneud penderfyniadau ynghylch natur y gofal iechyd sydd i’w ddarparu i gleifion â Covid-19, ei waethygu a darparu dadebru cardio-pwlmonaidd, gan gynnwys defnyddio cyfarwyddiadau dadebru cardio-pwlmonaidd peidiwch â cheisio (DNACPRs).
- Effaith y pandemig ar feddygon, nyrsys a staff gofal iechyd eraill, gan gynnwys ar y rhai dan hyfforddiant a grwpiau penodol o weithwyr gofal iechyd (er enghraifft drwy gyfeirio at gefndir ethnig). Argaeledd staff gofal iechyd. Gordal y GIG ar gyfer staff gofal iechyd nad ydynt yn dod o’r DU a’r penderfyniad i ddileu’r gordal.
- Atal lledaeniad Covid-19 o fewn lleoliadau gofal iechyd, gan gynnwys rheoli heintiau, digonolrwydd PPE a rheolau ynghylch ymweld â'r rhai sydd yn yr ysbyty.
- Cyfathrebu â chleifion â Covid-19 a'u hanwyliaid am gyflwr a thriniaeth cleifion, gan gynnwys trafodaethau am DNACPRs.
- Marwolaethau a achosir gan bandemig Covid-19, o ran niferoedd, dosbarthiad a chofnodi marwolaethau, gan gynnwys yr effaith ar grwpiau penodol o weithwyr gofal iechyd, er enghraifft drwy gyfeirio at gefndir lleiafrifoedd ethnig a lleoliad daearyddol.
- Gwarchod a’r effaith ar y rhai sy’n agored i niwed yn glinigol (gan gynnwys y rhai y cyfeirir atynt fel rhai “hynod o agored i niwed yn glinigol”).
- Nodweddu ac adnabod Cyflwr Ôl-Covid (gan gynnwys y cyflwr y cyfeirir ato fel Long Covid) a'i ddiagnosis a thriniaeth.
Sut roedd pobl yn rhannu eu stori gyda ni
Mae tair ffordd wahanol i ni gasglu straeon pobl ar gyfer Modiwl 3:
Ffurflen ar-lein
Gwahoddwyd aelodau'r cyhoedd i gwblhau a ffurflen ar-lein drwy wefan yr Ymchwiliad (cynigiwyd ffurflenni papur hefyd i gyfranwyr a'u hychwanegu drwy'r ffurflen ar-lein i'w dadansoddi). Mae hyn yn caniatáu iddynt ateb tri chwestiwn eang, penagored am eu profiad pandemig. Y cwestiynau hyn oedd:
o Dywedwch wrthym am eich profiad
o Dywedwch wrthym am yr effaith arnoch chi a'r bobl o'ch cwmpas
o Dywedwch wrthym beth rydych chi'n meddwl y gellid ei ddysgu
Mae'r ffurflen yn gofyn cwestiynau demograffig eraill i gasglu gwybodaeth gefndir amdanynt (fel eu hoedran, rhyw ac ethnigrwydd). Mae'r ymatebion i'r ffurflen ar-lein yn cael eu cyflwyno'n ddienw.
Ar gyfer Modiwl 3, dadansoddwyd 32,681 o straeon yn ymwneud â systemau gofal iechyd y DU. Mae hyn yn cynnwys 27,670 o straeon o Loegr, 2,756 o’r Alban, 2,451 o Gymru a 1,231 o Ogledd Iwerddon (roedd cyfranwyr yn gallu dewis mwy nag un wlad yn y DU ar-lein, felly bydd y cyfanswm yn uwch na nifer yr ymatebion a dderbyniwyd).
Dadansoddwyd yr ymatebion trwy brosesu iaith naturiol (NLP), sy'n defnyddio dysgu peirianyddol i helpu i drefnu'r data mewn ffordd ystyrlon. Yna defnyddir cyfuniad o ddadansoddiad algorithmig ac adolygiad dynol i archwilio'r straeon ymhellach.
Mae dadansoddiad NLP yn nodi patrymau iaith ailadroddus o fewn data testun rhydd. Yna mae’n grwpio’r data hwn yn ‘bynciau’ yn seiliedig ar dermau neu ymadroddion a gysylltir yn gyffredin â’r pwnc hwnnw (er enghraifft, gallai’r iaith a ddefnyddir mewn brawddeg am bryder fod yn debyg iawn i’r iaith a ddefnyddir wrth siarad am iselder, sy’n cael ei grwpio i bwnc ar iechyd meddwl). Fe'i gelwir yn ymagwedd 'o'r gwaelod i fyny' at ddadansoddeg testun gan ei fod yn mynd at y data heb unrhyw ragdybiaethau am y testunau sydd ynddo, yn hytrach mae'n caniatáu i bynciau ddod i'r amlwg yn naturiol yn seiliedig ar gynnwys y testun.
Dewiswyd straeon i'w cynnwys yn y model testun mewn dwy ffordd. Yn gyntaf, cymerwyd yr holl ymatebion i bob cwestiwn o'r ffurflen ar-lein a dilëwyd data gwag. Yn ail, cafodd ymatebion eu hidlo ar sail eu perthnasedd i Fodiwl 3.
Ystyriwyd bod straeon yn berthnasol os oedd y rhai a’u rhannodd wedi dewis unrhyw un o’r ymatebion isod i’r cwestiwn ‘Beth hoffech chi ddweud wrthym amdano?’:
o Bod â Covid-19.
o Byw gyda Covid Hir.
o Colli rhywun oherwydd Covid-19.
o Beichiogrwydd neu gael babi, gan gynnwys cymhlethdodau neu golled.
o Lles cyffredinol.
o Iechyd meddwl, er enghraifft, teimlo'n drist, yn ddig, yn bryderus neu dan straen.
o Gwasanaethau iechyd, er enghraifft y GIG neu HSCNI, gan gynnwys meddygfeydd.
o Rhywbeth positif a brofwyd gennych.
Ar ôl nodi straeon perthnasol, cynhaliwyd model testun ar gyfer pob un o’r tri chwestiwn penagored a gynhwyswyd yn y ffurflen ar-lein. O hyn fe wnaethom nodi cyfanswm o 233 o bynciau ar draws yr holl ymatebion i C1, 213 yn C2, a 147 yn Ch3. Gan y gallai cyfranwyr ddewis ymatebion lluosog i'r cwestiwn 'Beth hoffech chi ddweud wrthym amdano?' roedd yn bosibl bod y straeon a ddewiswyd i'w cynnwys yn cynnwys gwybodaeth nad oedd yn berthnasol i Fodiwl 3. Am y rheswm hwn, yn dilyn y modelu testun cychwynnol adolygodd y tîm ymchwil yn Ipsos yr holl bynciau o ran perthnasedd a thynnu pynciau nad oeddent yn berthnasol i Fodiwl 3 o gam olaf y dadansoddi . Roedd hyn yn dileu cyfanswm o 143 o bynciau yn C1, 140 o bynciau yn C2, ac 86 o bynciau yn C3, gan adael cyfanswm o 90, 73, a 61 o bynciau fesul cwestiwn yn y drefn honno.
Yn dilyn dileu pynciau nad oeddent yn berthnasol i Fodiwl 3, cynhaliwyd dadansoddiad ffactor ystadegol i fapio perthnasoedd rhwng pynciau a'u grwpio yn seiliedig ar y rhai sy'n digwydd yn aml gyda'i gilydd neu o fewn tair brawddeg i'w gilydd. Er enghraifft, cafodd pynciau am olchi dwylo, PPE, a gwisgo masgiau eu grwpio'n awtomatig i ffactor sy'n atal trosglwyddo. Cynhyrchodd y dadansoddiad ffactorau 17 ffactor trosfwaol ar draws y 90 o bynciau perthnasol yn Ch1, 13 ffactor yn Ch2, a 15 ffactor yn Ch3.
Yn dilyn modelu testunau a dadansoddi ffactorau, cynhyrchwyd ffrâm god yn seiliedig ar y pynciau hynny sy'n berthnasol i Fodiwl 3. Roedd hyn yn cynnwys adolygiad dynol o'r geiriau a'r ymadroddion mwyaf cyffredin, yn y set ddata lawn ac o fewn pob pwnc, i nodi geiriau allweddol a phatrymau y gellid eu defnyddio. defnyddio i grwpio straeon yn bynciau ac is-bynciau priodol. Wrth wneud hynny, rhoddodd hyn fesuriad llawer mwy cywir i'r tîm ymchwil o faint ac elfennau'r pynciau, er mwyn llywio'r dull dadansoddi.
Gan fod mwy o bobl wedi rhannu eu stori gyda'r Ymchwiliad rhwng y modelu testun a'r paru allweddeiriau, darparwyd set ychwanegol o straeon i Ipsos ar gyfer y cam dadansoddi olaf hwn. At ei gilydd, cynhwyswyd 32,681 o straeon ar y pwynt hwn, ac nid oedd y rhain bellach yn cael eu hidlo gan y cwestiwn 'Beth hoffech chi ddweud wrthym amdano?'. Cymerwyd y penderfyniad hwn i sicrhau bod yr holl straeon perthnasol yn cael eu dal, yn seiliedig ar y geiriau a ddefnyddiwyd gan bobl.
Yna adolygodd ymchwilwyr y gwahanol bynciau sy'n berthnasol i Fodiwl 3 i archwilio'r straeon. Daethpwyd â’r rhain ynghyd â straeon a rannwyd gyda’r Ymchwiliad mewn ffyrdd eraill (a ddisgrifir isod) i’w cynnwys yn yr adroddiad hwn.
Mae’r diagram isod yn dangos y themâu sydd wedi’u cynnwys yn y ffurflen ar-lein a’r nifer o weithiau y soniodd cyfrannwr am bob thema yn eu hymateb. Mae maint pob bloc yn cynrychioli nifer yr ymatebion sy'n gysylltiedig â'r thema. Sylwch y gallai cyfranwyr fod wedi crybwyll themâu lluosog yn eu hymateb ac y gallant felly gael eu cyfrif nifer o weithiau.
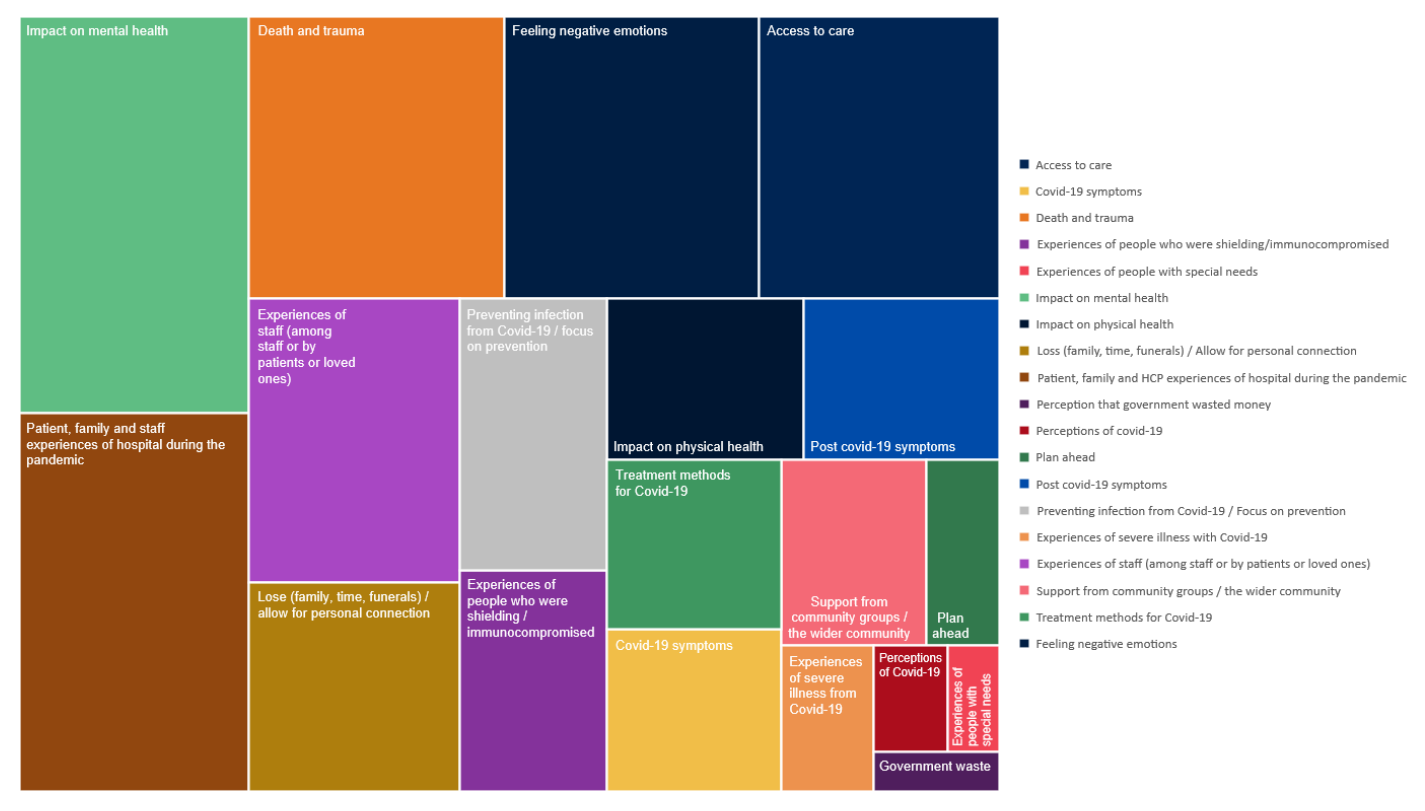
Digwyddiadau gwrando
Tîm Mae Pob Stori yn Bwysig teithio i 17 o drefi a dinasoedd ar draws Cymru, Lloegr, yr Alban a Gogledd Iwerddon, i roi cyfle i bobl rannu eu profiad pandemig yn bersonol yn eu cymunedau lleol. Cynhaliwyd digwyddiadau gwrando yn y lleoliadau canlynol:
- Carlisle
- Wrecsam a Rhuthun
- Newham
- Caerwysg
- Paisley
- Derry / Londonderry
- Middlesborough
- Enniskillen
o Bradford
Cynhaliwyd sesiynau gwrando rhithwir hefyd lle'r oedd y dull hwnnw'n cael ei ffafrio. Buom yn gweithio gyda llawer o elusennau a grwpiau cymunedol ar lawr gwlad i siarad â’r rhai yr effeithiwyd arnynt gan y pandemig mewn ffyrdd penodol. Mae hyn yn cynnwys teuluoedd mewn profedigaeth, pobl sy'n byw gyda Covid Hir a Syndrom Aml-system Llidiol Pediatrig (PIMS-Ts), teuluoedd sy'n agored i niwed yn glinigol, pobl anabl, ffoaduriaid, pobl o gefndiroedd lleiafrifoedd ethnig a gweithwyr gofal iechyd proffesiynol. Ysgrifennwyd adroddiadau cryno ar gyfer pob digwyddiad, eu rhannu â chyfranogwyr y digwyddiad, a'u defnyddio i lywio'r ddogfen hon.
Gwrando wedi'i dargedu
Comisiynwyd consortiwm o bartneriaid ymchwil cymdeithasol ac ymgysylltu cymunedol gan Every Story Matters i gynnal cyfweliadau manwl a grwpiau trafod gyda'r rhai yr effeithir arnynt fwyaf gan y pandemig a'r rhai sy'n llai tebygol o ymateb mewn ffyrdd eraill. Roedd y cyfweliadau a’r grwpiau trafod hyn yn canolbwyntio ar y Prif Linellau Ymholi (KLOEs) ar gyfer Modiwl 3. I gyd, cyfrannodd 604 o bobl ledled Lloegr (318), yr Alban (105), Cymru (90) a Gogledd Iwerddon (91) fel hyn rhwng Chwefror 2023 a Chwefror 2024. Mae hyn yn cynnwys 450 o gyfweliadau manwl gyda:
- Pobl yr effeithir yn uniongyrchol arnynt gan Covid-19.
- Pobl yr effeithir arnynt yn anuniongyrchol gan Covid-19.
- Gweithwyr gofal iechyd proffesiynol a staff cymorth.
- Grwpiau proffesiynol eraill sy'n gweithio yn y system gofal iechyd.
Ymgysylltwyd â 154 o bobl eraill o gymunedau y gwyddys eu bod yn profi anghydraddoldebau iechyd drwy allgymorth cymunedol. Helpodd y grwpiau trafod cymunedol a chyfweliadau hyn i sicrhau bod yr Ymchwiliad yn clywed gan bobl na fyddai'n bosibl eu cyrraedd mewn ffyrdd eraill. Roedd y bobl y siaradom â nhw yn cynnwys:
- Pobl o gefndir ethnig lleiafrifol.
- Pobl ag anabledd gan gynnwys nam ar y golwg, nam ar y clyw a'r rhai ag anabledd dysgu.
- Pobl sy'n profi amddifadedd.
Cafodd yr holl gyfweliadau manwl a grwpiau trafod eu recordio, eu trawsgrifio, eu codio a'u dadansoddi trwy adolygiad dynol i nodi themâu allweddol sy'n berthnasol i Lwybrau Ymholi Allweddol Modiwl 3 (KLOEs).
Mae'r tablau isod yn amlinellu nifer y cyfweliadau ar draws y system gofal iechyd a chyda phobl sy'n profi anghydraddoldebau iechyd.
| Math o gyfranogwr | Cwblhawyd y cyfweliadau |
|---|---|
| Effaith uniongyrchol Covid-19 (defnyddwyr gwasanaeth) 4 | 72 |
| Effaith anuniongyrchol Covid-19 (defnyddwyr gwasanaeth) 5 | 140 |
| Gweithwyr gofal iechyd a staff cymorth | 223 |
| Rolau proffesiynol eraill | 15 |
| Cyfanswm | 450 |
- Mae’r grŵp hwn yn cynnwys teulu a ffrindiau mewn profedigaeth, cleifion yn yr ysbyty gyda Covid-19, pobl sy’n byw gyda Long Covid a sawl profiad arall fel yr amlinellir yn Nhabl 3 isod.
- Mae'r grŵp hwn yn cynnwys pobl a ddefnyddiodd wasanaethau gofal iechyd yn ystod y pandemig, y rhai a oedd yn gwarchod a sawl profiad arall fel yr amlinellir yn Nhabl 3 isod.
| Math o gyfranogwr | Pobl yn ymgysylltu |
|---|---|
| Pobl o gefndir ethnig lleiafrifol | 60 |
| Pobl ag anabledd gan gynnwys nam ar y golwg, nam ar y clyw a'r rhai ag anabledd dysgu | 15 |
| Pobl sy’n profi amddifadedd cymdeithasol ac economaidd | 79 |
| Cyfanswm | 154 |
Gofynnwyd i bobl gymryd rhan mewn ymchwil wedi'i thargedu yn seiliedig ar gwmpas Modiwl 3 a phrofiadau penodol a gawsant yn ystod y pandemig o ddiddordeb i'r Ymchwiliad. Mae’r tabl isod yn amlinellu’r profiadau y gofynnwyd iddynt ddweud wrthym amdanynt, er bod y profiadau a drafodwyd yn y cyfweliadau yn cwmpasu ystod o wahanol bethau a ddigwyddodd iddynt yn ystod y pandemig yn ymwneud â gofal iechyd
| Math o gyfrannwr | Cwblhawyd y cyfweliadau |
|---|---|
| Pobl y mae Covid-19 yn effeithio'n uniongyrchol arnynt | |
| Unigolyn/teuluoedd mewn profedigaeth | 12 |
| Cleifion yn yr ysbyty gyda Covid-19 | 9 |
| Cleifion a oedd wedi canslo NEU wedi gohirio apwyntiadau/llawdriniaethau/triniaethau | 19 |
| Cleifion Covid hir | 9 |
| Pobl a benderfynodd beidio â cheisio triniaeth neu fynychu apwyntiadau personol | 11 |
| Unigolion/aelodau o'r teulu a gymerodd ran mewn trafodaethau a phenderfyniadau am DNACPR | 12 |
| Pobl yr effeithir arnynt yn anuniongyrchol gan Covid-19 | |
| Pobl oedd yn defnyddio gwasanaethau ysbyty cleifion mewnol | 19 |
| Pobl oedd yn defnyddio gwasanaethau mamolaeth | 17 |
| Pobl a ddefnyddiodd wasanaethau ysbyty cymunedol | 8 |
| Nid yw pobl a ddefnyddiodd wasanaethau ysbyty iechyd meddwl (wedi’u heithrio o ddadansoddiad gan nad yw gwasanaethau iechyd meddwl oedolion yn rhan o ymchwiliad Modiwl 3) | 7 |
| Pobl oedd yn defnyddio gwasanaethau meddyg teulu | 24 |
| Pobl oedd yn defnyddio gwasanaethau ambiwlans brys | 7 |
| Pobl a ddefnyddiodd GIG 111 | 7 |
| Pobl yr oedd eu perthnasau/anwyliaid yn yr ysbyty | 8 |
| Pobl y dywedwyd wrthynt am warchod / yn glinigol agored i niwed neu'n hynod agored i niwed yn glinigol | 14 |
| Pobl a ddefnyddiodd wasanaethau ysbyty cleifion allanol | 8 |
| Pobl oedd yn defnyddio gwasanaethau damweiniau ac achosion brys | 16 |
| Defnyddwyr gwasanaethau deintyddol (wedi'u heithrio o ddadansoddiad gan nad yw deintyddiaeth yn rhan o ymchwiliad Modiwl 3) | 3 |
| Gweithwyr gofal iechyd proffesiynol a staff cymorth | |
| Meddygon ysbyty (cyffredinol llym y GIG) | 21 |
| Meddyg ysbyty (A&E yn arbennig) | 10 |
| Meddygon ysbyty (Preifat) | 4 |
| Nyrsys ysbyty (Aciwt gan gynnwys Damweiniau ac Achosion Brys) | 10 |
| Cynorthwywyr gofal iechyd ysbytai | 7 |
| Porthorion ysbyty | 7 |
| Caplaniaid ysbytai | 7 |
| Staff glanhau ysbytai | 7 |
| Staff arlwyo ysbytai | 7 |
| Staff gofal lliniarol | 10 |
| meddygon teulu (gan gynnwys locwm) | 21 |
| nyrsys meddyg teulu | 15 |
| rheolwyr practisau meddygon teulu | 7 |
| Deintyddion (wedi'u heithrio o ddadansoddiad gan nad yw deintyddiaeth yn rhan o ymchwiliad Modiwl 3) | 6 |
| Fferyllwyr a thechnegwyr fferyllol | 8 |
| Parafeddygon a staff ambiwlans | 20 |
| Gweithwyr gofal iechyd proffesiynol perthynol (ysbytai acíwt a chymuned) | 24 |
| Trinwyr galwadau GIG 111 | 4 |
| 999 trinwyr galwadau | 4 |
| Staff labordy ysbytai (a elwir yn Wyddonwyr Clinigol) | 4 |
| Staff Nightingale | 5 |
| Cefnogaeth weinyddol a rheolaethol y GIG | 17 |
| Grwpiau proffesiynol eraill sy'n gweithio yn y system gofal iechyd | |
| Personél y fyddin | 2 |
| Gweithwyr gofal iechyd mewn ysbyty/cyfleusterau iechyd meddwl diogel (wedi'u heithrio o ddadansoddiad gan nad yw deintyddiaeth yn rhan o ymchwiliad Modiwl 3) | 7 |
| Staff rheoleiddio (e.e. CQC yn Lloegr neu Arolygiaeth Gofal Iechyd Cymru) | 6 |
| Cyfanswm | 450 |