Foreword
This is the first record produced by the Every Story Matters team at the UK Covid-19 Inquiry. It brings together the experiences shared with the Inquiry relating to its investigation into healthcare systems and has been submitted by the team to the Chair of the Inquiry, Baroness Hallett.
Baroness Hallett made it clear from the outset that she wanted
to hear from as many people as possible, particularly those who had suffered hardship and loss, as set out in the Inquiry’s Terms of Reference. So we created Every Story Matters to help us hear from people in a way which suited them – in writing, online or on paper, at an Every Story Matters event around the country, by video conference, using sign language or on the telephone. Stories are powerful and personal and they bring to life the human impact of the pandemic.
By launching Every Story Matters, the Inquiry gave people the opportunity to share their experience with us, to have someone listen to them, to have their experience recorded and to contribute to the Inquiry. Our contributors will provide Baroness Hallett with the kind of information she needs before reaching her conclusions and making recommendations. In that way, they can help ensure the UK is better prepared for the next pandemic and that the response to it is more effective.
When we started listening to the people of the UK about their experiences of the pandemic, we knew the experiences would be varied. For many people the impacts of those years, and the years since, were far reaching. In some cases they were and are extremely painful, and for some almost too painful to talk about. For many people the pandemic was devastating and many are still dealing with the consequences be they bereavement, long term medical conditions, or other kinds of loss and hardship. We also heard that some people want to move on and not talk about the pandemic anymore. Sometimes we heard more positive things, where people had formed new connections, had learned something or had their lives changed in some way for the better.
Every Story Matters has been designed to protect people’s identity, avoid re-traumatisation as much as possible and provide them with choice about how to contribute. Collecting and analysing stories in this way is unique for a research project; Every Story Matters is not a survey nor a comparative exercise. It cannot be representative of the entire experience of the UK nor was it designed to be, but it has enabled us to identify themes amongst people’s experiences and cases that do not fit into any particular group.
In this record we cover thousands of experiences that demonstrate the impact of the pandemic on patients, their loved ones, healthcare systems and settings, and key workers within them. There are thousands more experiences that do not feature in this record. All experiences shared with us will flow into future Every Story Matters records. As these records are tailored to the different modules, we use people’s stories where they can add most insight to the areas under ,investigation. We continue to encourage people to share their experiences with us, because it is their stories that can support and strengthen the Inquiry’s recommendations and help reduce the harms of a future pandemic. Please check the Inquiry website for the latest information and timings.
We have been enormously supported by individuals, groups and organisations which have given us feedback and ideas and helped us to hear from a wide range of people. We are very grateful to them and we acknowledge many of them on the next page.
Delivering Every Story Matters has touched all those involved. These are stories that will stay with all those who hear or read them for the rest of their lives.
The Every Story Matters Team
Acknowledgements
The Every Story Matters team would like to express its sincere appreciation to all the organisations listed below for helping us capture and understand the voice and healthcare experiences of members of their communities. Your help was invaluable to us helping ensure that we reached into as many communities as possible. Thank you for arranging opportunities for the Every Story Matters team to hear the experiences of those you work with either in person in your communities, at your conferences, or online.
- Association of Anaesthetists
- British Geriatrics Society
- Carers UK
- Clinically Vulnerable Families
- Covid-19 Bereaved Families for Justice Cymru
- Covid19 Families UK and Marie Curie
- Disability Action Northern Ireland, and the ONSIDE Project (supported by Disability Action Northern Ireland)
- Eden Carers Carlisle
- Enniskillen Long Covid Support Group
- Foyle Deaf Association
- Healthwatch Cumbria
- Long Covid Kids
- Long Covid Scotland
- Long Covid Support
- Long Covid SOS
- Mencap
- Muslim Women’s Council
- People First Independent Advocacy
- PIMS-Hub
- Race Alliance Wales
- Royal College of Midwives
- Royal College of Nurses
- Royal National Institute of Blind People (RNIB)
- Scottish Covid Bereaved
- Sewing2gether All Nations (Refugee community organisation)
- Self-Directed Support Scotland
- Trades Union Congress
- UNISON
To the Bereaved, Children and Young Peoples’, Equalities, Wales, Scotland and Northern Ireland forums, and Long Covid Advisory groups, we truly value your insights, support and challenge on our work. Your input really was instrumental in helping us shape this record.
Last but not least, we would like to convey our deepest gratitude to all the bereaved families, friends and loved ones for sharing their experiences with us.
Overview
How stories were collated and analysed
Every story shared with the Inquiry is analysed and will contribute to one or more themed documents like this one. These records are submitted from Every Story Matters to the Inquiry as evidence. This means the Inquiry’s findings and recommendations will be informed by the experiences of those impacted by the pandemic.
People shared their experiences with the Inquiry in different ways. The stories that described experiences of healthcare during the pandemic have been brought together and analysed to highlight key themes. The approaches used to explore stories relevant to this module include:
- Analysing 32,681 stories submitted online to the Inquiry, using a mix of natural language processing and researchers reviewing and cataloguing what people have shared.
- Researchers drawing together themes from 604 research interviews with those who were involved with healthcare during the pandemic in different ways including patients, loved ones and healthcare workers.
- Researchers drawing together themes from Every Story Matters listening events with the public and community groups in towns and cities across England, Scotland, Wales and Northern Ireland, including among those who experienced specific pandemic impacts. More information about the organisations the Inquiry worked with to organise these listening events is included in the acknowledgements section.
More details about how people’s stories were brought together and analysed in this report are included in the appendix. This document reflects different experiences without trying to reconcile them, as we recognise that everyone’s experience is unique.
Throughout the report, we have referred to people who shared their stories with Every Story Matters as ‘contributors’. This is because they have had an important role in adding to the Inquiry’s evidence and to the official record of the pandemic. Where appropriate, we have also described more about them (for example, different types of staff working in healthcare) or the reason they shared their story (for example as patients or loved ones) to help explain the context.
Some stories are explored in more depth through quotes and case studies. These have been selected to highlight specific experiences and the impact they had on people. The quotes and case studies help ground the report in what people shared with the Inquiry in their own words. Contributions have been anonymised. We have used pseudonyms for case studies which have been drawn from the research interviews. Experiences shared by other methods do not have pseudonyms.
In giving voice to the experiences of the general public, some of the stories and themes included in this report include descriptions of death, near death experiences, and significant physical and psychological harm. These have the potential to be upsetting and readers are encouraged to take steps to support their wellbeing as they do so. This might involve taking breaks, considering which chapters feel more or less tolerable to read, and going to colleagues, friends, family or supportive others for help. Readers who experience ongoing distress related to reading this report are encouraged to consult with their healthcare provider to discuss options for support. A list of supportive services are also provided on the UK Covid-19 Inquiry website.
The stories people shared about healthcare during the pandemic
People told us about the many life-changing impacts the pandemic had on them as patients, loved ones and healthcare workers, and some are still living with these impacts today.
Many people faced problems accessing healthcare during the pandemic, whether in emergency situations, for acute health conditions, or for more routine appointments.
We heard about the devastating loss experienced by those who were bereaved during the pandemic. We heard about lives that have been disrupted and damaged by catching Covid-19, developing and living with Long Covid and delays to receiving treatment for other serious illnesses. Clinically vulnerable and clinically extremely vulnerable people told us about the physical and emotional toll of shielding and the ongoing impact of Covid-19 on their lives.
We also heard about positive things that happened during the pandemic. Healthcare services continued to support many patients and there were examples of good patient care. Healthcare workers reflected on all they did to adapt how they treated and cared for people and the ways they supported patients’ loved ones in uniquely challenging circumstances.
Changes to healthcare during the pandemic
The fear of catching Covid-19 meant many people were reluctant to access healthcare services, particularly early in the pandemic. Fears were strongest about going to hospital but also applied to other in-person healthcare settings. Many patients and their loved ones were scared they might be separated because of visiting policies.
| “ | To be honest, nobody wanted to go to hospital at that stage. Unfortunately, I had no option. I was ambulanced in. I really fought not to go to hospital each time, but it was dangerous, and I needed to be there, and I understood that.”
– Person hospitalised with Covid-19 |
| “ | I didn’t want Dad to go into hospital, my dad didn’t want to go into hospital either. We were both of the same opinion. He didn’t want to go into hospital, he loved being at home, if he’s going to die, he wanted to die at home. We knew if he went into hospital, I would wave goodbye at the door and the chances are I would never see him again and he would die alone in hospital.”
– Bereaved family member |
The fear of catching Covid-19 and public awareness of the pressures on healthcare systems meant there was broad acceptance of the need to reorganise how healthcare was provided during the pandemic. Contributors shared many examples of how challenging these changes were for patients, their loved ones and healthcare workers.
One important change was that many more services were delivered remotely, either online or by phone. Patients, loved ones and clinicians were often unconvinced that symptoms could be properly assessed without a face-to-face consultation.
| “ | I have to send photographs to my doctor’s WhatsApp group. My GP surgery has a WhatsApp telephone number where you send your name, date of birth and the photographs…it’s just not the same.”
– Person living with Long Covid |
There was some confusion about the guidance in place during the pandemic – especially for visiting loved ones or attending appointments with them. We also heard about guidance not being applied consistently and the problems and frustration this caused.
At the time the government guidelines were much more liberal than the rules the hospital actually chose to apply, which was hugely frustrating and had a detrimental impact on my mental health. Other hospitals were far more accommodating, with use of compassion and common sense.
For patients worried about Covid-19 infection, Personal Protective Equipment (“PPE”) was often seen as reassuring because it would reduce the risks they faced. For others, PPE created a barrier that felt unnatural or frightening, adding to their anxiety about being ill during the pandemic. Some healthcare workers agreed that PPE placed an obstacle between them and patients and made providing care more challenging than before the pandemic.
Hospital visits not being allowed or being restricted was frustrating and often frightening for patients. Loved ones found not knowing what was happening incredibly distressing, particularly when patients were very ill or nearing the end of their lives. Similarly, many healthcare workers shared how upsetting they found not being able to communicate in the usual way with loved ones who were distressed.
| “ | 48 hours later, you’re calling them up to tell them that their relative is dying and they don’t believe you and why should they? And they’ve got questions that you can’t answer, and you’ve got answers that they don’t want.”
– Hospital doctor |
Problems accessing healthcare
People found it hard to access healthcare during the pandemic, in some cases with serious and lasting impacts. There were several common problems noticed by patients, loved ones and healthcare workers:
- Many patients shared how hard it was to book GP appointments, leaving them with no way to get routine medical help.
| “ | There was no need to shut down the GP practices and reduce that. I think a lot of people could have still been seen, people who’ve got lumps and bumps or need things removing. I think they could have dealt with that. I think maybe that might have saved a few lives as well.”
– GP patient |
- Non-Covid-19 hospital care was scaled back, leading to long delays for treatment, in some cases for serious illnesses or ongoing health conditions.
| “ | I have several cases in my mind of people who suffered with benign but limiting conditions, that were very easy to fix had they had access to acute healthcare sooner. But, you know, it was very difficult for them to get access to healthcare, to see the person they needed to.”
– Hospital doctor |
- Those who tried to access emergency care were sometimes unable to get help or faced significant delays, even when they or their loved ones were very ill.
| “ | Usually there might be 30 calls waiting at any one time. At peak points in the pandemic there were 900 calls waiting.”
– NHS 111 call handler |
Contributors reflected on how anger and frustration about accessing care increased as the pandemic went on. Many of them blamed these problems for people having to live with pain and other symptoms, reducing their quality of life and leading to worsening health. Some directly linked delays, cancellations or mistakes across healthcare during the pandemic to serious health problems or the death of a loved one.
Patients, loved ones and clinicians were often frustrated that,treating Covid-19 and reducing the spread of the disease was prioritised over other serious healthcare needs. Many contributors argued that more could have been done to avoid the negative impacts on non-Covid patients.
In the lockdown, people were still poorly. Someone was diagnosed with cancer and couldn’t get an appointment. Don’t neglect people with other treatment needs. The chemo treatment was cancelled, the cancer progressed, and they died.
We also heard about the many specific barriers to accessing care – and receiving good care – encountered by people with a disability, those who do not speak English and those without digital technology or reliable internet.
| “ | Understanding information, being deaf, not being able to communicate, lots of things online, and having to use English and write, you know, e-mails and stuff like that and text messages wasn’t really accessible for me.”
– Deaf person |
Some contributors also highlighted how the pandemic worsened existing inequalities.
I witnessed firsthand the impact of Covid-19 on a community that was already disadvantaged by many social disadvantages including poverty. Again, I witnessed that black lives don’t matter. Covid-19 ripped through [where I lived] as Covid-19 has adversely impacted front line workers, people of colour, people on zero hours contracts who would not be furloughed and could not afford to stop working.
| “ | I would say I’m one of the most confident people to ask questions, but even me I sometimes feel a bit embarrassed, ‘Am I asking too much? Or can people understand what I’m trying to explain?’ You know? I knew some people, not only language was a barrier, actually it’s the literacy bit as well. It’s, like, they can’t read, they can’t write, they don’t understand the language. Even when you explained it in Chinese, the medical term was too complicated for them.”
– Person who speaks English as a second language |
Experiences of Covid-19
Some healthcare workers felt motivated to work directly with Covid-19 patients. They wanted to do what they could to help, despite the fear of being directly exposed to the virus. Many healthcare workers were worried about catching Covid-19 themselves and passing it on to their families.
Every day I would go in and see death and every day I would wonder if this is the day I take it home to my small children.
Some shared how they lost colleagues to the disease.
| “ | All three of us who went for training became ill… with Covid-19 symptoms. Another friend and I (all nurses and paramedics) improved but within two weeks our other friend was dead, found by paramedics at home alone after calling for help because at the time people were getting advised not to travel to hospital. She was 29 years old and died alone.”
– Healthcare professional |
Healthcare professionals treating Covid-19 patients told us they did their best despite the huge challenges they faced, sometimes without the equipment and staff resources they needed. This put them under enormous strain and many described feeling stressed and exhausted. They told us their experiences had a negative impact on their mental health. Despite the challenges, those who treated Covid-19 patients also shared how the care they offered improved as the pandemic progressed and more was learned about the disease.
| “ | I know that I see a lot of trauma a lot of the time, but this… was on a different kind of level. It was something that none of us had experienced. And everyone was sort of just winging their way through this situation, that no one really knew how to handle it, but we were trying our best.”
– Paramedic |
Many Covid-19 patients described how afraid they were about being hospitalised unexpectedly with Covid-19 and how confusing it was. Some struggled to remember much about their time in hospital because they were so ill.
One day I woke up in ICU unable to move, speak, eat, drink etc. I was totally reliant on staff go wash me, feed me, etc. I was hooked up to oxygen, had a catheter, wearing a pad, and remains of a tracheostomy in my throat. Apparently, I’d been in an induced coma for two months.
Some patients who were hospitalised with severe Covid-19 told us they are still traumatised by their experiences. We heard how disturbing it was to witness the deaths of other Covid-19 patients, and how this added to fears about the disease.
| “ | A few weeks after, my son’s mental health deteriorated, he was having visions of being back in his hospital ward and the man from the bed next to him in hospital was standing in his room and was angry that he didn’t help him … he is crying in Tesco because the beeping of the tills took him back to the monitors beeping in the hospital.”
– Carer for a patient hospitalised with Covid-19 |
Impact of the pandemic
End-of-life care and bereavement
Many bereaved families, friends and colleagues shared their loss, devastation and anger. They were often not allowed to visit and had little or no contact with their dying loved ones. Some had to say goodbye over the phone or using a tablet. Others had to do so while keeping their distance and wearing full PPE.
Bereaved families and friends had much less involvement in decisions about their loved ones than they usually would. We heard about loved ones struggling to contact healthcare professionals to find out what was going on. This often meant the situation felt out of their control, leaving them scared and helpless. Advocating for their loved ones and their care from afar was much harder than under normal circumstances, and sometimes impossible.
| “ | My husband was taken into hospital and basically written off because of age and other conditions… he was negative for Covid and he was put on a ward where it was rife. We were not allowed to visit, had no idea of what was happening. He passed away and I received a phone call at 3:15am telling me he had gone.”
– Bereaved family member |
| “ | You just couldn’t get through to anybody, you couldn’t talk to anybody, we were all ringing for an update… my father rang daily for her [grandmother] to be released to us… We have everything set up here [at home]. She even had an electric bed, we had wheelchairs and everything for her. We could have helped her.”
– Carer for an elderly family member |
Those bereaved families, friends and colleagues who were able to visit often had to do so in extraordinary and very restricted circumstances, usually when the patient was at the end of their life. Some had to choose who would visit because numbers were limited. Many were not allowed to touch their loved one and had to wear PPE. The restrictions meant some visited alone, without the support of family and friends. The experience was often disorienting and frightening.
We heard a lot about do not attempt cardiopulmonary resuscitation (DNACPR) notices and end-of-life care and how decisions were not always explained to loved ones. Some bereaved families and friends told us they did not know what decisions had been made until after their loved one had passed away, or still did not know.
| “ | The GP asked for a DNACPR to be in place, my dad knew about this and the possible consequences, he wanted to live, he didn’t want one. Then I found out the GP had visited again unannounced with DNACPR request, and they never mentioned it to me.”
– Bereaved family member |
As well as the many challenges bereaved loved ones faced, the stories included examples of healthcare workers offering excellent end-of-life care during the pandemic. Some described how supportive staff were and how much this improved end-of-life care. One common example was health professionals breaking Covid-19 guidance to provide physical comfort to their loved one who was dying.
I remember, one nurse was like, ‘Oh, your dad wanted me to give you a hug, and say, “Here’s a hug.”’ Obviously, she didn’t need to do that...you’re not even meant to be getting that close, but just that kind of humane feeling, and I was just like, oh my God, that is just so refreshing to see in a medical person.
For many, losing loved ones and not being able to say goodbye properly made their loss harder to accept and come to terms with. Some are left with the overwhelming guilt that they should have done more to protect them from Covid-19 or from having to die in healthcare settings alone.
Long covid
Long Covid is a set of long-term health conditions and symptoms some people develop after being infected with the Covid-19 virus. Long Covid had – and continues to have – a dramatic and often devastating impact on people. Many people living with Long Covid told us how they wanted better recognition and more public understanding of the symptoms they continue to experience and the huge impact that it has on their ability to live their lives. Some also emphasised the importance of more research and development focused on treatments for Long Covid.
| “ | We’re left alone now; we don’t know what we can do. They need to recognise Covid is a long term or lifelong condition for some people.”
– Person with Long Covid |
Those living with Long Covid shared the many ongoing health problems they have experienced, with different types and severity of symptoms. These range from continuous aches and pains and brain fog, to debilitating mental exhaustion. Many told us how their lives have been devastated, and how they are now unable to work, socialise and carry out day-to-day tasks.
| “ | “I was unable to return to work or my normal life as it left me very debilitated with chronic fatigue, and dysautonomia1, chronic headaches, brain fog and poor concentration.”– Person living with Long Covid |
Accessing care has often been incredibly challenging for people living with Long Covid. Some shared how they felt their GP was disinterested in their symptoms or did not believe them. In conversations with GPs or other healthcare professionals they often felt dismissed. Sometimes, we heard healthcare professionals would suggest and/or seek to exclude an alternative cause of their symptoms such as issues with their mental health or pre-existing health conditions.
We had GPs refusing to believe in Long Covid here, with many others not getting testing for symptoms.
The experiences shared also highlight inconsistencies in how people with Long Covid have been treated. It has been draining for those with ongoing symptoms who have been passed between different parts of the healthcare system without receiving the care needed, if any – often while very unwell. They described feeling abandoned and helpless, and unsure where to turn.
| “ | Nobody wants to know, I feel invisible. I’m treated as collateral damage. The frustration and anger I feel is incredible; medical gaslighting, lack of support and the way other people treat me, the GP tells me I’m too complex, because I have so many medication reactions.”
– Person living with Long Covid |
Some were referred back to their GP by specialists for further tests or to treat other symptoms, while others were referred to Long Covid clinics or directed towards online courses once these had been set up in some areas of the UK in late 2020. Some people living with Long Covid found clinics and online courses helpful but many received poor care without any tailored support or treatment.
| “ | So, we still feel that we’re being sent to the GP and the GPs don’t know what to do with us, GPs are busy with lots of other things. And even the sympathetic GPs with the best will in the world haven’t got a clue what to do with us. We need something more specialised basically.”
– Person living with Long Covid |
We also heard about healthcare workers who have been, and continue to be, impacted by Long Covid. Some contributors suggested the fact that healthcare professionals have developed Long Covid has reduced the capacity of healthcare services to provide care today.
Shielding
People who were clinically vulnerable and clinically extremely vulnerable told us they were very afraid of Covid-19 and understood why they were asked to shield. However, many shared how hard they found it to follow the shielding advice and the negative impacts this had on them and their families.
I coped by doing other things but if I’d have gone a little bit longer, a few more weeks, I think I would have gone over the edge to be honest with you. I was getting to the stage where I couldn’t cope...and only having [my mother] really to speak to, that was a big thing because my whole life was quite social. I was lonely, and I tried not to let that affect me too much. It was driving me absolutely crazy.
People who shielded shared how doing so frequently led to isolation, loneliness and fear. Their physical and mental health often deteriorated. Some still feel afraid to leave the house – for them, the pandemic is not over.
| “ | Collapse of routine, mental health suffered, physical health suffered. She [her mum] didn’t eat a lot actually, she lost a lot of weight because she wasn’t well…but yes, so she suffered a lot mental health wise and physical health wise from just lack of other people basically more than anything, lack of any kind of interaction.”
– Carer for someone who was clinically extremely vulnerable |
Many were left stuck at home feeling confined, anxious or bored, and in some cases still are. They shared how frustrating it was not being able to exercise and look after their health properly.
| “ | Being told I was so at risk of Covid-19 made me feel out of control of my health and incredibly stressed. I feared I would die if I caught Covid-19. By shielding, the real risk to me was not being able to manage my health condition which I do mainly through exercise.”
– Person who was clinically extremely vulnerable |
Some contributors were more positive about shielding. This was often because they were comfortable at home or were able to keep busy and positive. Being able to develop a routine with meaningful things to do helped them cope.
| “ | With the help of a garden…I was spoilt for things to do. So that probably saved me totally, mental health-wise… it didn’t affect me probably as much, as someone in a housing estate or, high-rise apartments or something, that didn’t have that outside space to go to.”
– Person who was clinically extremely vulnerable |
Some clinically extremely vulnerable people described how they are still shielding because the risks associated with Covid-19 have not gone away for them. They continue to fear mixing with others and have often lost connection to their communities. They want more recognition that the impact of the pandemic is ongoing for those who are clinically extremely vulnerable.
[One] of my friends is older, she’s in her 70s, she’s not come back to church... she really has no social life whatsoever anymore... her biggest challenge is around the fact that she feels that she’s being given this information, that tells her she’s vulnerable, that she needs to protect herself, she needs to stay away from people, she is at risk, and that her risk hasn’t changed, and that Covid-19 is still around. And so, she struggles to reconcile the fact that it feels like the advice has changed, and yet, the risk is still the same... And so, I think there’s a lot of, still, fear wrapped up around all of that for people.
How the healthcare system adapted
As well as the impact on patients and their loved ones, healthcare workers also told us about their experiences during the pandemic. They described the work they did to continue offering care as best they could, with many pointing to the huge changes that were made in healthcare settings.
Many contributors working in healthcare said the pace of change was much faster during the pandemic than they had experienced previously. The stories shared with us highlight some tensions and disagreements among healthcare professionals caused by the challenges of implementing rules. These were often between those working directly with patients and those in management or senior leadership roles. For example, some contributors thought senior leadership often seemed to wait for guidance from the government or NHS Trusts on what to do rather than taking proactive action.
We also heard how some healthcare professionals increasingly questioned the basis for Covid-19 guidance as the pandemic went on. These concerns often focused on whether the guidance was based on evidence of what worked to prevent infection.
Healthcare professionals told us how they found out about guidance through the media and their employers and about differences in how Covid-19 guidance was implemented across different parts of the health service.
Personal protective equipment (PPE)
Healthcare workers across different settings told us they did not have the PPE they needed, especially at the start of the pandemic. The design and fit of some PPE also caused significant problems, making it harder for some to do their jobs and causing discomfort.
| “ | I had friends working in ICU wearing bin bags.”
– Community nurse |
I used to roll it up to my waist, get an apron and use the apron as a belt, and then hang a pen off that as well. So, the sizing wasn’t great and then you’re bigger than you think you are and you crash into a lot of items because you’ve got more width on you.
We heard examples of how PPE that did fit properly physically impacted some staff when they wore it for many hours. This included examples of rashes, skin sensitivity and impression marks from wearing masks for long periods.
PPE also made spoken communication between healthcare professionals and patients more difficult. This was a particular challenge for patients with additional communication needs, including hearing impaired and autistic people who depend on facial expressions for communication.
| “ | You say, ‘I’m deaf,’ and they’re talking to you through a mask, and I’ll say, ‘I’m deaf.’ They’re, like, ‘Oh, no, no, I can’t take my mask off. You might give me Covid-19.’ I’m like, ‘Well, you know, I’ll stand over here, you stand over there. Please take your mask down, I’ll be more than 2 metres away,’ and they still refused. That was really difficult and then you literally can’t see their mouth or their face, so you’ve got no hope of understanding them.”
– Deaf person |
Healthcare workers in different settings had mixed impressions of the clarity of guidance and requirements when it came to testing. They recalled self-isolation guidance being particularly strict at the start of the pandemic, which meant they were unable to work at times when they were well.
Primary care
Those who worked in primary care often shared how adapting to the pandemic had been challenging and made it harder to offer good care to patients. Even so, they reflected on how much they managed to change and how this allowed them to look after many of their patients.
| “ | We did adapt, and I think we did change. I think we did what we had to do. It was dynamic the whole time really, wasn’t it? It was changing all the time, and we did our best, I think, to go and do what we had to do.”
– GP nurse |
Some felt that GPs and community pharmacists were not properly considered and consulted, and that the pandemic response in hospitals was prioritised. They were frustrated at rapidly changing guidelines, with little notice and often a lack of clarity about how GP surgeries or pharmacies were supposed to respond.
We heard about some local GP services collaborating to share ideas and pool staff and resources, and about ‘Covid-19 hubs’ to treat patients and reduce hospital admissions. These approaches were generally seen as positive, giving those working in primary care more confidence in assessing and treating Covid-19.
GPs reflected on how the pandemic caused some new health problems. For example, some thought social distancing had led to greater isolation, in turn contributing to more mental health issues among their patients.
Hospitals
We heard from healthcare workers about how hospitals made changes to manage the expected influx of Covid-19 patients. They told us about the upheaval across different roles in hospitals, not just among clinical staff. While some healthcare workers were positive about the way the response was managed, others said it was insufficiently thought through.
There were enormous changes made. Reallocating areas, reallocating staff, everybody moving from place to place, changing what they were doing.
| “ | Many staff were redeployed to different clinical areas away from where they normally work to assist with the Covid response – these members of staff were “thrown in at the deep end” with little additional training and no choice about where they were sent. This also had an impact on many junior doctors’ training pathways.”
– Hospital doctor |
Planning and delivering care continued to be challenging later in the pandemic. Many contributors shared how making changes to hospital care became more difficult due to staff exhaustion and low morale. Some described a lack of planning as to how to prioritise non-urgent care and treat more patients as pandemic restrictions began to ease.
| “ | There was no advice on how to step back from anything and there was absolutely no help with de-escalation. And it felt, to us, no sense of learning of, ‘Okay, what we did in the first wave’.”
– Hospital doctor |
Emergency and urgent care
There was huge pressure on many emergency departments (EDs) during the pandemic, with challenges linked to the suitability of buildings, staff shortages and periods of increased demand for urgent care. The pressure they were under varied between different EDs and changed at different stages of the pandemic.
Many of those working in emergency care said they were at times unable to maintain infection controls because there were large numbers of patients and not enough space. Some ED staff told us about having to make decisions about prioritising care and transferring patients to intensive care (ICU or ITU), and about how difficult these were because of how serious they could be for patients.
| “ | We were being made to play God in deciding on who went to ITU – who was given a change to live and who wasn’t.”
– Hospital nurse |
Other contributors who worked in EDs said that at times they saw fewer patients than usual because people were too afraid to seek treatment. Reduced demand allowed staff in some EDs to spend more time caring for individual patients than they were able to before the pandemic.
Paramedics told us how much pressure they were under and how much their roles changed. They described waiting outside hospitals in ambulances with unwell patients, often for very long periods. This meant paramedics had to care for patients in ambulances and alert hospital staff to changes in their condition.
We heard from some NHS 111 and 999 call handlers about the pressures of having to deal with large numbers of calls from very anxious and unwell people. They gave examples of the problems caused by ambulance shortages. This was particularly distressing for call handlers.
| “ | They [callers] would phone us, and we’d be like, ‘Yes, but you do need an ambulance,’ so then we’d go through to ambulance, and they’d be like, ‘But we’ve got nothing to send.’ That was distressing.”
– NHS 111 call handler |
The impact on the healthcare workforce
A sense of shared purpose motivated many healthcare professionals during the pandemic. But some said this sense of purpose fell away as the pandemic went on, increasing burnout among staff as waves of the pandemic continued.
| “ | You were helping other people. You actually were providing a service that was valuable. It made you feel proud of what you did.”
– Hospital pharmacist |
I think on a personal level, it just became harder and harder. You got more and more tired. It probably led to a degree of anxiety. Difficult to deal with things. I think those were the challenges.
Staff working across different roles and in different parts of healthcare systems often had to take on huge workloads. This added to their already stressful jobs. Healthcare workers consistently told us how colleagues being off sick or needing to self-isolate added to workload pressures.
We heard how staff were sometimes redeployed to ease the pressure on teams, but contributors said it was challenging to teach the specialist skills and expertise required to work in new areas at pace. For example, nurses who were transferred to work in Covid-19 ICUs shared some of the most challenging frontline experiences.
| “ | I felt disempowered when forced into unfamiliar roles without proper training.”
– Children’s community nurse |
| “ | The ICU nurse was supervising… actually looking after the patient, as you were really only there assisting her, checking drugs etc. But after that… you were main carer with an ICU nurse looking over your shoulder if you were lucky… it changed dramatically from the first couple of days, and then beyond that, it was really you doing it.”
– Hospital nurse |
Many healthcare workers shared the ethical dilemmas they faced around Covid-19 guidance. These were often specific to their role and pandemic experience, but there were some common themes. For example, some healthcare professionals described not following guidance so they could show more compassion for patients, families and colleagues.
One of the most upsetting and stressful experiences for many healthcare workers was dealing with death on a scale they had never encountered before. Some described the damage to their mental health as a result. They often said families not being able to see their dying loved ones was one of the hardest things they had to cope with.
It was like a war zone, overnight 18 people became Covid-19 positive with nowhere to isolate them. They were dropping like flies, it was awful. You can’t underestimate what this did to nursing staff, not being able to offer comfort to patients was soul destroying.
| “ | We became immune to it. It dehumanised us a little bit, I think, at the time. I felt that, and I felt that was difficult to deal with.
– GP practice manager |
When healthcare professionals experienced distressing situations and workload pressures, some were offered, and made use of, emotional support. Peer support within teams was also important to help staff cope with the challenges they faced. However, this was inconsistent, with some healthcare workers not being offered any support with their mental health.
| “ | “I feel that we kept getting told what the hospital were doing for staff and things, but I don’t think they ever asked the staff what would make a difference to being at work. I think it was also the little things, like they would have said being able to park…being able to go for lunch in a chillout space.”
– Hospital doctor |
Some staff were quieter, or had quieter periods, during the pandemic because patients stayed away or because of how care was reorganised. While this usually reduced the immediate pressure and stress they felt, some felt guilty that other healthcare professionals were under greater strain. Those who were less busy also worried about the patients they would usually be seeing and whether they were receiving the care and treatment they needed.
Some contributors described a lasting impact from working in healthcare during the pandemic. They shared how their mental health was now poorer than it had been. We also heard examples of professionals who had faced personal problems like relationship breakdowns that they thought were at least partly due to their experiences in the pandemic. Sadly, some healthcare professionals told us about having to change roles or stop working because of how much their mental health deteriorated during the pandemic.
| “ | I don’t think I’ve come back to 100% of how I normally was. It takes its toll. But it’s almost like having this piece of paper, that’s nice, and flat, and straight, and then you’ve crumpled it and then you try and straighten out that piece of paper again. It’s still creased up, no matter how much you try and straighten it out.”
– Paramedic |
Rebuilding trust in decisions about healthcare
Some contributors shared how their trust in healthcare systems had been shaken by what happened and argued that this was a concern for many across society. This was often less about the care they received from individual healthcare professionals and more about the decisions that were made about organising and providing care.
Trust in services from the public has gone due to how they were treated in the lockdowns.
Many of their reasons for no longer trusting in the decisions made about healthcare have already been highlighted. They were worried about access to healthcare and whether healthcare systems will be able to recover from the pandemic. For many contributors, doing more to preserve and rebuild public trust in healthcare was seen as an important priority – both now and when dealing with future pandemics and emergencies.
Thousands of people shared their experiences about healthcare systems during the pandemic with us. In this report we build on this summary, highlighting in more detail the key themes from the stories we heard.
- Dysautonomia is an umbrella term describing a disorder of the autonomic nervous system, which controls bodily functions including regulating our heart rate, blood pressure, temperature, digestion and breathing. When dysregulation occurs, these functions can be altered, resulting in a range of physical and cognitive symptoms.
Full Report
1. Introduction
This document presents the stories shared with Every Story Matters related to UK healthcare systems during the pandemic.
Background and aims
Every Story Matters is an opportunity for people across the UK to share their experience of the pandemic with the UK Covid-19 Inquiry. Every story shared has been analysed and turned into a themed report. These reports are submitted to the Inquiry as evidence. In doing so, the Inquiry’s findings and recommendations will be informed by the experiences of those impacted by the pandemic.
This document brings together what people told us about their experiences of UK healthcare systems1 during the pandemic.
The UK Covid-19 Inquiry is considering different aspects of the pandemic and how it impacted people. This means that some topics will be covered in other module reports. Therefore, not all experiences shared with Every Story Matters are included in this document. For example, experiences of adult social care and the impact on children and young people will be explored in later modules and included in future Every Story Matters documents.
How people shared their experiences
There are several different ways we have collected people’s stories for Module 3. This includes:
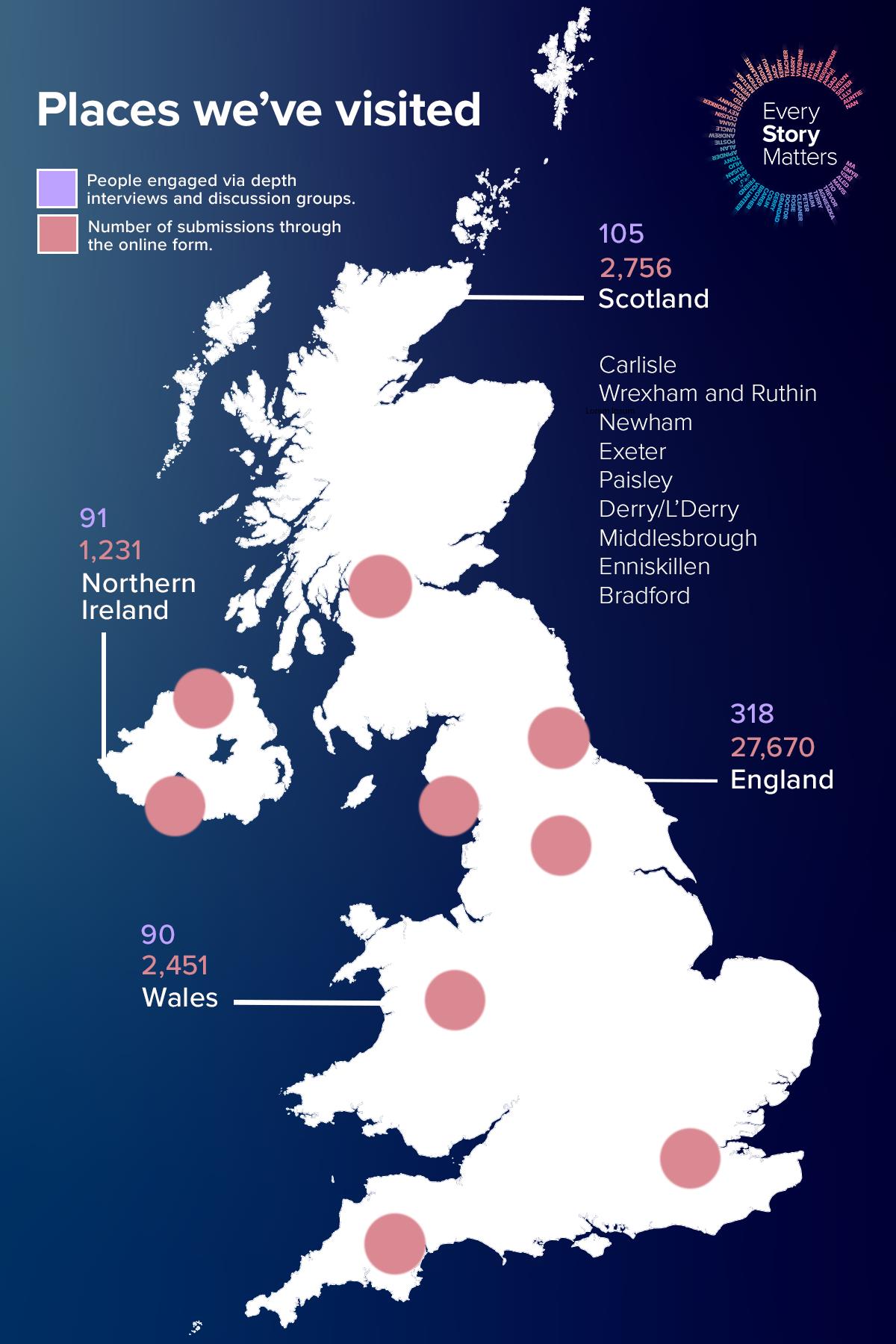
- Members of the public were invited to complete an online form via the Inquiry’s website (paper forms were also offered to contributors and entered into the online form for analysis). This allows them to answer three broad, open-ended questions about their pandemic experience. The form asks other questions to collect background information about them (such as their age, gender and ethnicity). This allows us to hear from a very large number of people about their pandemic experiences. The responses to the online form are submitted anonymously. For Module 3, we analysed 32,681 stories related to UK healthcare systems. This includes 27,670 stories from England, 2,756 from Scotland, 2,451 from Wales and 1,231 from Northern Ireland (contributors were able to select more than one UK nation in the online form, so the total will be higher than the number of responses received). The responses have been analysed through natural language processing (NLP), which uses machine learning to help organise the data in a meaningful way. A combination of algorithmic analysis and human review is then used to further explore the stories.
- The Every Story Matters team travelled to 17 towns and cities across England, Wales, Scotland and Northern Ireland, to give people the opportunity to share their pandemic experience in person in their local communities. Virtual listening sessions were also held where that approach was preferred. We worked with many charities and grassroots community groups (listed in the acknowledgements below) to speak to those impacted by the pandemic in specific ways. This includes bereaved families, people living with Long Covid and PIMS-Ts, clinically vulnerable families, disabled people, refugees, people from ethnic minority backgrounds and healthcare professionals. Short summary reports for each event were written, shared with event participants, and used to inform this document.
- A consortium of social research and community engagement partners were commissioned by Every Story Matters to conduct depth interviews and discussion groups with those most impacted by the pandemic and those less likely to respond in other ways. These interviews and discussion groups focused on the Key Lines of Enquiry (KLOEs) for Module 3. In total, 604 people across England, Scotland, Wales and Northern Ireland contributed in this way between February 2023 and February 2024. This includes 450 depth interviews with:
-
- People directly impacted by Covid-19.
- People indirectly impacted by Covid-19.
- Healthcare professionals and support staff.
- Other professional groups working in the healthcare system.
A further 154 people from communities that are known to experience health inequalities were engaged through community outreach. These community discussion groups and interviews helped ensure the Inquiry heard from people who may not be reached in other ways. The people we spoke to included:
-
- People from an ethnic minority background.
- People with a disability including visual impairment, hearing impairment and those
with a learning disability. - People from more deprived areas in the UK.
All depth interviews and discussion groups were recorded, transcribed, and coded and analysed via human review to identify key themes relevant to the Module 3 KLOEs.
The number of people who shared their stories in each UK nation through the online form, listening events and research interviews and discussion groups is shown below:
Figure 1: Every Story Matters engagement across the UK
For further information on how we listened to people and the methods used to analyse stories, see the appendices.
Notes about the presentation and interpretation of stories
It is important to note the stories collected through Every Story Matters are not representative of all experiences of UK healthcare during the pandemic or of UK public opinion. The pandemic affected everyone in the UK in different ways, and while there are key events and facts, we recognise the importance of everyone’s unique experience of what happened. This report aims to reflect the different experiences shared with us without reconciling the variation or differing accounts.
We have tried to reflect the range of stories we heard, which may mean some stories presented here differ from what other people in the UK experienced, and sometimes contrast with scientific consensus or evidence. Given this, this report seeks to provide balance, nuance, and context around the stories shared with us.
Some stories are explored in more depth through quotes and case studies. These have been selected to highlight the different types of experiences we heard about and the impact these had on people. The quotes and case studies help ground the report in what people shared in their own words. Contributions have been anonymised. We have used pseudonyms for case studies which have been drawn from the depth interview and discussion groups. Case studies based on experiences shared in other ways have been anonymised.
Throughout the report, we refer to people who shared their stories with Every Story Matters as ‘contributors’. Where appropriate, we have also described more about them (for example, different types of staff working in healthcare) or the reason they shared their story (for example as patients or loved ones) to help explain the context and relevance of their experience.
As well as sharing their experiences, contributors were asked to reflect on what the Inquiry can learn from their experience. Some focused on how specific problems they faced should have been dealt with better. Others shared what they thought had gone well. We heard some broad themes across their reflections, and these are highlighted throughout the report.
It is clear from the stories that some who responded were highly motivated to do so. For this reason, analysis of responses to the online form should not be considered representative of public experiences of the pandemic more broadly. Instead, they reflect the experiences of those that chose to share their story with Every Story Matters.
Structure of the report
This document is structured to allow readers to understand how the pandemic impacted different parts of the healthcare system and particular groups of people.
It starts by exploring experiences in Primary Care (Chapter 2), Hospitals (Chapter 3 and 4), and Emergency and Urgent Care (Chapter 5). The report then looks at impacts related to PPE and Covid-19 testing (Chapter 6), experiences of government and healthcare sector guidance (Chapter 7) and the impact of the pandemic on health care professionals (Chapter 8).
The document then turns to specific experiences of healthcare during the pandemic, including end of life care and bereavement (Chapter 9), Long Covid (Chapter 10), Shielding (Chapter 11) and use of maternity services (Chapter 12).
- We have referred to UK healthcare systems rather than the NHS where possible throughout this report in order to reflect the differences in the healthcare systems across the four nations of the UK.
2. Primary care: experiences of healthcare professionals and patients |
 |
Primary care is usually the first point of contact when people need health advice or treatment, and acts as a ‘front door’ to healthcare systems. Primary care includes general practice, community pharmacy, dental. In this chapter we share the stories we heard from GPs, GP nurses, practice managers, and community pharmacists alongside patient experiences of accessing and using primary care services.
Responding to the pandemic
The early stages of the pandemic were confusing and stressful for GPs, community pharmacists and others in primary care. Contributors working in primary care found it challenging because they wanted to continue to look after their patients, but there was little clarity about how they should respond.
Reflecting on their experience, many contributors said strategic planning for primary care had not been good enough. Some thought government and local healthcare organisations were slow to respond, with minimal advice. These contributors were frustrated because they did not have the support they needed when the pandemic started.
| “ | I think where hospitals had mass plans and emergency plans, within primary care it was very fragmented and disjointed and, ‘Oh, it’s up to you.’ And I get that, but it was tricky to do.”
– GP practice manager |
Contributors felt that emergency planning was more focused on hospitals rather than primary care, because changes could be managed centrally in hospitals.
| “ | I think where hospitals had mass plans and emergency plans, within primary care it was very fragmented and disjointed and, ‘Oh, it’s up to you.’ And I get that, but it was tricky to do.”
– GP practice manager |
However, many GPs told us the independence of GP practices allowed them to change their services quickly and challenge health board suggestions they thought were unhelpful. These contributors said they had been able to develop approaches to service delivery which suited the local context.
| “ | GPs are quite a resourceful, innovative bunch of people. I think that is probably helped by them having their own businesses, they recognise ‘there’s a situation and we need to come up with a solution’.”
– GP |
As time went on, more guidance was shared, but many said this became overwhelming. Primary care staff told us it was impossible to keep up with and act on everything they were being told.
| “ | Official stuff from the health board… was really slow… sometimes that email had 20 attachments to it, which would be sent out at, like, 7 o’clock on a Tuesday night or something ridiculous, when none of us were at work. And you’d go in on a Wednesday morning… and you would be expected to go through, assimilate, organise and act within, quite often, 24 hours or less. It was impossible.”
– GP |
| “ | I probably had on average about 20 different guidelines to read on a daily basis at work. At the end of the day, we were focusing more on reading these guidelines than we were on actually actioning for our patients. It took away a lot of precious clinical time and patient experience.”
– GP nurse |
Some contributors working in primary care said they made use of organisations or individuals that brought together relevant information in one place for GPs. This helped them cope with the constant change and uncertainty, and meant they felt more confident about keeping the public safe.
| “ | [The local NHS Trust] started to do a newsletter which condensed all the different emails down… so it meant we could go to the newsletter and get succinct information… If that had started [earlier], I might not have felt so overwhelmed or worried that I’d missed something.”
– GP practice manager |
| “ | We had obviously emails from the health authority regarding what PPE that we had to wear and things like that for certain procedures… also we have an advanced nurse practitioner who used to coordinate things quite well. I think it was relayed quite well. I think the communication wasn’t bad.”
– GP nurse |
Changes to primary care services
Contributors shared how in these early stages of the pandemic GP services shifted to remote delivery to reduce the risks of spreading Covid-19. This meant that patients – at least at first – were usually restricted to online and telephone consultations.
As the pandemic progressed, GPs continued to adapt and delivered more services face-to-face where possible. Some told us the measures required for infection control meant that even later in the pandemic it was impossible to offer patients the same access to services as pre-pandemic.
| “ | They had to be booked in, they also had to have their temperature checked and that kind of thing, access to services wasn’t as good, for sure. Yes, there was emergency planning training and business continuity, but I don’t know that anybody knew what they were dealing with.”
– GP practice manager |
GP practices that had set up ways to work remotely and telephone triage patients before the pandemic were better placed to respond. Other GP practices did not have these systems in place and had to find temporary ways to move to remote working at the start of the pandemic.
| “ | Most practices were working straightforward appointment systems…other GPs effectively had to set up the system we’d been running for three years overnight.”
– GP |
| “ | There were a few instances when people had never thought that they would need to work from home…they had to come in the car park where they could get reception from the NHS Wi-Fi and they were able to log in on the laptops because you can’t just take your laptop at home and log in.”
– GP |
A common reflection among those working in primary care was the importance of informal networks in supporting the pandemic response. These networks were developed to tackle the many challenges of delivering care to local communities. Contributors working in primary care often joined WhatsApp and Facebook groups where they could share information and advice with others making similar changes to providing care. These groups acted as sources of support when they were finding their work challenging or were unsure on the best way to adapt services.
| “ | We’re all trying to interpret the same information, and when specifications are open to interpretation that’s a problem…we were able to do through WhatsApp groups that we set up so we could ask each other questions and share that information.”
– GP practice manager |
Alara’s storyAlara is a GP working in a busy urban practice where patients often dropped in when they needed an appointment or to pick up prescriptions. This all changed at the start of the pandemic. “Suddenly, the med centre, which was very convenient and very easy to drop into, the doors were closed. It was all large notices on the door and everything by telephone. And we had to quickly adapt to a new way of working.” Working with other local practices, Alara’s practice developed an online consultation portal, where patients could submit and upload photographs as well as answer the set questions. Patients were then seen via telephone consultations. “The threshold for seeing somebody face-to-face was much, much higher, and anybody who was coming was screened as they arrived and had their temperature taken. And every patient contact, we would put on level 2 PPE, except for the time when we were working in the Covid-19 centres, where patients with potentially Covid-19 symptoms, we had level 3 PPE, and it felt to be a much safer environment.” |
Some contributors also joined webinars and virtual meetings with colleagues from other healthcare services. This allowed them to discuss service changes and work out what different approaches would look like. These sessions allowed for thinking to be shared quickly and helped GP practices adapt.
Some GP practices told us they offered face-to-face consultations as much as possible. This often involved moving to pre-booked appointments to manage patient numbers and minimise infection risks. Some described how they set up ‘emergency response rooms’ with higher-grade PPE accessible to staff, allowing patients with Covid-19 symptoms to be treated immediately. Other GPs changed the types of care they offered to patients in response to patient fears of attending hospital.
| “ | Me and another GP were taking on most of the risk by seeing 10% of patients face-to-face and the remaining via telephone. She was also visiting patients a lot more often, particularly the elderly to provide antibiotic IVs who didn’t want to go into hospital.”
– GP |
Community pharmacists we heard from reflected how people turned to them for support when they could not get in touch with their GP or other healthcare services. This meant some community pharmacies were overwhelmed with patients who needed help, with long queues and many more phone calls than they were used to before the pandemic.
| “ | Because doctors shut down, oh, my God, it became hysteria. We had days [where] there was 80 or 90 people queuing [outside the pharmacy].”
– Community pharmacist |
| “ | The phone calls, where we used to get, say, 50 phone calls in a day, the phone calls increased to 150. The phone did not stop. One [of] our pharmacies is based in a medical centre, but we were still operating so lots of people came to us instead.”
– Community pharmacist |
Some pharmacists told us they were also overwhelmed by the demand for medicines to be delivered to people’s homes during the pandemic, creating significant extra pressure. Some were supported by their local authority or volunteers to keep up with demand. Many shared how they still have more deliveries now than before the pandemic.
| “ | Before we had 10 deliveries a day. The deliveries went up from that to 50-60 deliveries a day. The council did help, and there were three or four delivery people that used to come, and volunteers who wanted to help… [Deliveries are] still up, and we now keep a driver.”
– Community pharmacist |
Patient views on the changes to primary care services
Patients were broadly supportive and understanding of the changes to primary care during the pandemic and were aware of the pressures GPs were under. Contributors were also very appreciative of community pharmacy services, and the efforts made to deliver medicines.
However, many patients were frustrated, especially about how long they had to wait for GP appointments. These contributors argued GP surgeries closing did not make sense when there was a huge need for their services. We heard many examples of not being able to access the care they needed, which often left them feeling worried and disappointed.
| “ | It almost felt like keeping people away from the practices, a ‘get on with it’ kind of approach rather than a helping approach, which I don’t blame them for because it must have been awful.”
– GP patient |
| “ | It was difficult to speak to a GP, even on the phone dealing with respiratory issues, initially and over the first 2 years.”
– GP patient |
| “ | There was no need to shut down the GP practices and reduce that. I think a lot of people could have still been seen, people who’ve got lumps and bumps or need things removing. I think they could have dealt with that. I think maybe that might have saved a few lives as well.”
– GP patient |
Many patients also said they were very glad when face-to-face consultations were offered again, especially for older patients. However, some felt the Covid-19 safety measures used caused other issues, describing patients waiting outside or having assessments outdoors.
| “ | I was initially refused to be seen by my GP and the only way my condition was assessed was that I was sent into the surgery car park where a nurse carries out the examination in full view of the public walking by.”
– GP patient |
Another area of frustration for many contributors was how many of the changes to primary care made during the pandemic appeared to be permanent.
| “ | GP appointments have been changed forever – now we get a phone call or video consultation as opposed to being examined in person.”
– GP patient |
The challenges of remote consultations
Patients and clinicians reflected on the significant challenges and concerns they had with GP practices closing and moving to remote appointments. Some patients shared how helpful remote appointments were during the pandemic, as they were often the only form of advice and support they could access. However, many others were unhappy as they were unconvinced their symptoms could be assessed properly unless they saw someone in person.
Some also told us they found it hard to describe their symptoms over the phone or online. Across the stories shared with us, there were many examples of serious problems being missed during remote consultations, often with severe consequences for people’s health.
| “ | My aunt had skin cancer removal delayed and was very frightened. The GP did a phone appointment and made a judgement that it was nothing serious by looking at a photo. He was wrong.”
– GP patient |
Many contributors were very worried about older relatives being referred to online or telephone services. They described serious challenges their relatives encountered.
| “ | During the first lockdown in 2020 mother (aged 75) was experiencing difficulties with her breathing. She became frustrated with her GP at the lack of face-to-face appointments. Over several months she had telephone appointments and was prescribed various different inhalers and steroids for asthma which did not work. She felt that if the doctor saw her in person and listened to her chest it would help ascertain the… instead of ineffective guesswork. Her breathing became progressively worse until one day, in early 2021, my dad had no option but to call 999 and she was taken to hospital.”
– Family member of patient |
Anna’s storyDuring the lockdown Anna’s grandmother started to show early signs of dementia. Her local GP practice had moved to remote services and, after several attempts to secure an appointment, a telephone assessment was offered. Although Anna felt this wasn’t ideal, she was grateful the appointment would be the following week. Unfortunately, shortly before the appointment, Anna tested positive for Covid-19 and had to isolate at home. This meant she couldn’t attend her grandmother’s appointment with her. Afterwards, Anna called her grandmother to ask how it went and what the GP had said. Her grandmother was unable to remember what she had been asked or what she had been told – and Anna was unable to find out. “This became a very stressful and worrying time. As she couldn’t remember, I called the GP practice myself to see if they could give me any clue on if it was dementia and what to do next. I was declined on the basis of patient confidentiality and could not get any information.” Anna’s grandmother was also supported by a wellbeing clinic for older patients, but this service halted during the pandemic. This meant her condition was not monitored for most of the pandemic. When the clinic restarted, she was assessed by a nurse who recognised symptoms of dementia and referred her to hospital for a brain scan, dementia assessment and consultation. At this point she was finally diagnosed with having severe Alzheimer’s. “My grandmother will now never regain any of that memory and mental capacity she lost. This could have been delayed if action was taken at the initial GP appointment. Although I understand the risks and precautions that were needed during lockdown, I feel like this was a major flaw and has cost my grandmother and our family a lot of health and relationship damage.” |
The move to remote consultations was very difficult for d/Deaf and hearing impaired people, those who spoke no English or English as a second language, those with a learning disability, and those with autism. They faced problems understanding information and communicating effectively, which acted as a barrier to accessing healthcare.
| “ | Understanding information, being deaf, not being able to communicate, lots of things online, and having to use English and write, you know, e-mails and stuff like that and text messages wasn’t really accessible for me.”
– d/Deaf person |
Phone consultations were mostly inaccessible, with translators often not available. As a result, some told us they had to rely on family members or volunteers who knew sign language to help with these calls.
| “ | They [the doctors] said they’d call my house, but I’d already said, ‘I’m deaf, you know, I’m not going to be able to take a phone call’. There must be another way, send me an email, send me a text,’ and they ignored it. They phoned my house and said, ‘Oh, this is an emergency, you need to go to A&E’. During the first phone call I’d phoned them via an interpreting service, but they hadn’t phone me back via the interpreting service.”
– d/Deaf person |
Phone consultations were also challenging for contributors who did not speak English as their first language. Many preferred meetings in person because they could use translators more easily.
| “ | Face-to-face is good, no telephone, no, I don’t like the telephone. Because face to face is good for confidence, I have more confidence, more talking. What is the problem? It’s good face-to-face and to bring an interpreter.”
– Refugee |
We heard how some autistic people found the sudden change to telephone consultations uncomfortable and distressing. They were used to face-to-face consultations, and the impersonal nature of telephone appointments was very disruptive.
| “ | He had to have that familiarity with that member of staff. He didn’t like change. And my other son was the same, and they still are. But they used to just give numbers out for you to ring, so that you’d have somebody to talk to. And I was like, ‘You can’t do that when they’re autistic.’ You’ve got to stick to the people that they know because they feel comfortable.”
– Parent of an Autistic person |
Learning for the future: fair access and tackling inequalitiesOne common theme in contributors’ reflections was how to ensure patients can access the care they need during a crisis, and particularly the importance of understanding and addressing inequalities in access to care. The changes during the pandemic were seen to worsen many existing barriers to accessing care, particularly where patients or carers had no access to technology or had problems with travel because of Covid-19 restrictions. Many contributors said plans need to be in place to address healthcare inequalities during crises, to provide consistent and fair support to all patients. Contributors felt additional support– such as interpreters and translated materials – was lacking during the pandemic. This made it hard or impossible for some people to access important information about their healthcare, and to receive the care they needed. In turn, this meant some people were even more marginalised and isolated. These contributors wanted specific plans to support disabled people, tailored to their access and healthcare needs, and recognising the additional barriers they already face and how these worsen during a pandemic. “More guidance for smaller GP practices and opticians who just didn’t know what they could or could not do, delaying treatments which could have saved my sight.” – Every Story Matters contributor |
Healthcare professionals working in primary care also reflected on the impact of the move to remote consultations. They told us how difficult it was to assess patients without seeing them in person, often describing remote consultations as risky and worrying. These contributors said they lost valuable insights they would usually gain from in-person appointments. Others shared specific technological barriers, such as IT systems that were not adequate for remote consultations. As a result, many GPs said they were concerned about patient safety.
| “ | You can gain an awful lot more when you see a person face-to-face, so we felt that we were working with a much higher risk. Not a much higher risk for [being infected with] Covid-19 if we weren’t seeing the patients, obviously, but for our clinical diagnosis, particularly with mental health patients because we didn’t have video capability.”
– GP |
| “ | They were having what felt like high-risk situations over the phone, patients were refusing to come in or go to hospital during some of those calls. People were behaving differently to what they normally would have.”
– GP |
Healthcare professionals shared how the usual approach to caring for patients with long term conditions, such as diabetes, changed with the move to remote care. Telephone consultations, for example, required new skills.
Anvi’s storyAnvi works as a GP nurse. At the start of the pandemic, her practice stopped all face-to-face consultations immediately. They moved most appointments to telephone consultations. Anvi was responsible for managing chronic conditions within the GP practice. This includes patients with diabetes and respiratory diseases. She quickly organised telephone consultations to train people with diabetes how to administer insulin and monitor their glucose levels at home. For those with respiratory diseases, she explained how to monitor peak flows. Training patients to self-manage and carrying out check-ups and consultations over the phone were new skills for Anvi. She initially struggled but over time she improved and was more confident. “I wasn’t doing it very well particularly at the beginning, so getting used to that. Trying to know the patients. I found you lost a lot in the consultation then from that… but I learned to do it better.” |
How the primary care workforce adapted to the pandemic
Staff shortages were a huge challenge during the pandemic. The initial challenge was deciding which appointments to cancel and who to prioritise for treatment. Contributors told us about the increased workload and pressure on staff who were working.
| “ | A lot of people were off…I think I found that the hardest thing through the whole two years; it was to cover for other people all the time. We were always one person down, it seemed, and that’s continued really.”
– GP nurse |
To address staff shortages, surgeries had to change how they worked. Some partnered with other GPs locally to share staff. This often started informally but became more formal as the pandemic progressed and became particularly important as staff absences increased.
| “ | We had to buddy up with all our practices so that we could cross-cover and things like that… any time we had a lot of absence among our staff, clerical or clinical staff, we always could cover it.”
– GP |
Other contributors described how their working patterns changed to ensure services could continue.
| “ | During the pandemic the surgery partners were very supportive to its staff. As administrators, we changed our hours of work, to starting from 6am, finishing at 10pm and working all weekend. Splitting our hours allowed us to continue to support the surgery, whilst keeping our jobs and distancing in the workplace.”
– GP surgery staff member |
For community pharmacists, managing patients and the public was challenging. We heard from some community pharmacists about the impact of social distancing restrictions. They could only allow up to two people into the pharmacy at a time, and their interactions with patients became very short and matter of fact as they did not want people interacting longer than needed. This was a big change from how they usually spoke with patients.
| “ | I had to change my whole way of working. I would be a very touchy-feely pharmacist. It was a community. People would come in for cups of tea, if they had bad news…there was coffee in the back of the shop. There were biscuits there. It was a family, and that just changed overnight. We couldn’t have them in the shop unless they needed something.”
– Community pharmacist |
There were also examples of restrictions on the number of people in pharmacies causing anger and conflict in queues outside. This was difficult for pharmacy staff to deal with as they were not experienced in managing conflict and crowds.
| “ | The problem was you couldn’t let too many people into the shop because you had to space people out. The pharmacies are only a certain size, so you could only allow two people in at a time, do the prescription, and then have them out the door as quick as you could. There could be 80 or 90 people in the queue. People could be and were really abusive. Abusive to staff and people who, at the time, were just working.”
– Community pharmacist |
Covid-19 hubs and care in the community
We heard from some contributors about ‘Covid-19 hubs’ being set up to help manage cases. Covid-19 hubs were specialist teams drawn from those working in primary care, who would see patients with suspected Covid-19 symptoms to assess and treat them.
Contributors said the Covid-19 hubs intended to reduce the burden on hospitals by supporting and treating Covid-19 patients in local areas, through a mix of face-to-face and remote appointments. Some GPs with experience of Covid-19 hubs told us they worried about how well they were able to judge patient conditions without seeing them in person.
| “ | Our main role really was to not send all those people to hospital… you go home after some days and always think oh gosh did I make the right call about that little child or that person. I couldn’t see them. It was just on the basis of a telephone call.”
– GP |
A few contributors shared how they thought Covid-19 hubs offered useful training and support on treating patients with Covid-19. They saw this as positive, and it gave them more confidence in assessing and treating Covid-19.
| “ | We had regular meetings with the respiratory consultants from the hospital as part of the Covid hub. Again, the guidance from them about what risk factors to look at and when to send someone in… there was lots of learning.”
– GP practice manager |
Other GPs said they challenged advice from local health boards to form Covid-19 hubs because they did not think it would help them treat patients. One GP who shared their story with us was unhappy with the idea of a Covid-19 hub because they thought there would be too many staff absences for it to work.
Contributors working in primary care told us about other initiatives to care for people in the community. For example, making pulse oximeters and blood pressure machines available so patients could assess themselves. Some GPs also said they prescribed more antibiotics than they would normally do during the pandemic to help stop health conditions becoming more serious.
Making hospital referrals
For patients with serious or persistent health conditions that needed hospital treatment, the role of GPs in securing access to hospital services is crucial. Many contributors told us the impact of the pandemic on hospital services meant that it was difficult to secure appointments for patients. This led to frustration among contributors – clinicians and patients alike – and meant we heard about many serious health problems that went untreated, often for long periods.
| “ | Patients would be referred to secondary care, [but] they wouldn’t see anybody…even telephone consultations were very few and far between, really. Patients would ring us then, obviously irate because their problems weren’t being dealt with [but] this was the reason why they were referred to secondary care, because we’d reached our limit, really, as to what we could do to help them.”
– GP nurse |
| “ | In terms of secondary care, so hospital care, no, none of that was something that was discussed with GPs, or GPs were involved in developing protocols or anything like that, certainly I wasn’t, and I doubt any of my colleagues have been either.”
– GP |
Contributors described how delayed treatments led to conditions worsening, and to growing waiting lists.
| “ | People were being told to stay home, but healthcare is so vital that you cannot just do the bare minimum. There are now huge backlogs. Provision needed to have continued.”
– GP |
| “ | I started working in a cancer service and there were twice the number of referrals because people had not been to their GP so instead of being diagnosed early it was later stages and the pressure was enormous.”
– Healthcare professional |
Patients who shared their story with us were often very frustrated with the delays to accessing hospital care. Many had to live with worrying health problems that had not been properly assessed or where they were not receiving the right treatment. They often went back to their GPs repeatedly to try to get the care they needed.
Every Story Matters contributor’s storyAn Every Story Matters contributor’s mother was due to see a respiratory consultant in the first week of the first lockdown, but the face-to-face appointment was cancelled, and a telephone appointment was offered instead. The consultant had never seen his mother previously and prescribed her inhalers following the appointment. A month later she was rushed to hospital in a serious condition, but when she was discharged after two days, there was no diagnosis and no tests had been proposed. “I kept phoning her GP, respiratory team etc and [reporting her condition via measurements but they told me] “no that can’t be right, the machine must be broken”, and still no one would see her… this went on for months and months.” Tired of the situation as he knew his mother was very unwell, the contributor decided to complain to his mother’s GP and speak to the Patient Liaison Service at his hospital. Eventually, after some further persistence from the contributor, she received all the tests she needed and was sadly diagnosed with Stage 4 emphysema. This had a devastating impact on the contributor, their mother and their family as they were shocked and upset by the diagnosis. |
Some patients shared how they paid for private treatment because of these delays. They were often very angry they felt forced into this, and in some cases struggled to afford to do so.
| “ | I managed to save my business when restrictions were lifted only to fall foul of the difficulty getting a GP appointment when I started to have mobility problems which turned out to be serious enough to lose my business all over again. I was let down by the NHS waiting times and was forced to pay for private care to avoid paralysis.”
– GP patient |
Learning for the future: primary care during the pandemicThe pandemic shifted ways of working and brought changes to primary care, making it possible to deliver some appointments remotely. Many of those who work in primary care reflected on the successes of this and said lessons should be learned for improving care in future. However, there were also real concerns among some patients, carers and support workers about how the shift to remote care created additional barriers for vulnerable people and those from some communities. “We’ve tried to even make it the norm going forward to change the way we deliver services. But that does require us to change – you need to be, I’d not say retrain, but have different people doing new skills. So, much more developing telephone consultations, working with phoning patients, but also for patients to change; I wouldn’t say less dependence, but look to use – utilise the services closer to home.” – Pharmacist “We are entering a new era of GP, with the increasing demand driving the need for change whereby not every problem does actually need a face-to-face review and can be dealt with remotely. Changes were needed to bring general practice up to date with technology and utilising remote services, it just happened far faster than anticipated.” – Every Story Matters contributor Some contributors argued that the focus on hospitals meant that primary care received less support during the pandemic. They wanted better planning for patients to continue accessing both primary and secondary care. “I think we need a national plan for primary care in a pandemic. I think there wasn’t, that wasn’t there.” – GP |
3. Hospitals: experiences of healthcare professionals |
 |
This chapter shares what healthcare professionals told us about hospital care during the pandemic. It outlines the experiences of those who provided care for Covid-19 patients and other patients, as well as the experiences of hospital support staff.
Preparedness and pandemic response
Contributors’ experiences of the pandemic response varied considerably based on which part of the hospital they worked in, their specific role, and how close they were to decision making.
Senior hospital staff were more involved in emergency planning and made decisions about how the hospital would respond. They received frequent updates (sometimes daily) with guidance from the government and healthcare systems about infection control measures as well as action plans.
To respond to the challenges of the pandemic, some hospitals reorganised and reshaped spaces to assess patients and reduce the spread of Covid-19. Reorganisation also involved significant changes to how hospitals were staffed and how services were managed and delivered.
While some healthcare workers were positive about the way the pandemic response was managed, others said it was insufficiently thought through.
| “ | I think all the clinical staff, the way everything had to be changed and organised, in our hospital was done extraordinarily well. There were enormous changes made. Reallocating areas, reallocating staff, everybody moving from place to place, changing what they were doing.”
– Hospital nurse |
| “ | Many staff were redeployed to different clinical areas away from where they normally work to assist with the Covid response – these members of staff were “thrown in at the deep end” with little additional training and no choice about where they were sent. This also had an impact on many junior doctors’ training pathways.”
– Hospital doctor |
More junior hospital staff described frequent and rapid changes to how they worked. At times, these changes were happening daily and were not always explained as part of emergency planning. Some of these contributors thought what they were asked to do did not always make sense, particularly as things were not implemented consistently across the hospital.
In the early days of the pandemic, contributors shared how infection control and Covid-19 treatment were prioritised, and the public largely stayed away from hospital. A lack of consistency within and between hospital settings caused some frustration among healthcare professionals who shared their story with us. Other contributors mentioned challenges because of limited space and poor ventilation in specific areas within hospitals. These factors made it harder to maintain social distancing, and this increased anxiety among hospital staff.
Planning patient care and treatment in hospitals continued to be challenging later in the pandemic. When Covid-19 restrictions were lifted, hospitals had to balance providing care to more non-Covid patients with reducing the spread of Covid-19.
Returning to ‘business as usual’ demanded sometimes as much effort to move staff, resources and equipment as the initial response to the pandemic. We heard many examples of how wards and units had to be re-opened, and equipment purchased or moved. Staff told us how they tried to return to some normality in delivering healthcare services and helping patients as the pandemic continued, but there were many practical challenges. Contributors said patients often did not receive the usual level of care. Healthcare professionals felt disappointed and guilty about not being able to provide the level of care they wanted.
Sarah’s storySarah specialises in dietetic care for gastric and oesophageal patients within a regional cancer specialist unit. The hospital she was based in had a small Intensive Care Unit (ICU), that was selected as a regional unit for intensive care beds. From March 2020 to June 2022 the specialist cancer centre had to move at least four times so care for cancer patients could continue. Sarah reflected on the logistical challenges of this. These included finding appropriate surgical space and availability for their patients, who were immunosuppressed, and the continual re-planning, or moving patients, equipment and staff at short notice. “Every time there was a change in circumstances where we were like, ‘Right, we’ll restart surgeries’, we were like, ‘Right, how do we do that?’ and within two days we would have moved a full unit a mile across the city and have those set up.” Sarah and her team found it challenging to provide care during these periods of having to stop and move. Many of the skilled nursing staff they relied on had been redeployed to Covid-19 wards because of their specialisms. She felt that treatment, service planning and care delivery were poorer because of these problems. “A lot of them didn’t get the ultimate and optimal pathways they should have been on because of Covid-19. Therefore, that’s led to detrimental impact on their, not just quality of life, but overall lifespan…which has an impact on us, personally, because you just feel like you haven’t been able to deliver the service that you would have hoped.” |
In the early days of the pandemic, contributors reflected on how there was a shared sense of purpose across hospitals. Many described how cooperation became strained during the later stages as different wards and specialisms tried to get their services running again. Some contributors described a lack of planning for when the pandemic restrictions ended. They said there was no ‘exit strategy’ from the strict conditions of the initial Covid-19 response. In their view, there should have been more planning and guidance to support non-urgent services reopening more quickly.
| “ | There was no advice on how to step back from anything and there was absolutely no help with de-escalation. And it felt, to us, no sense of learning of, ‘Okay, what we did in the first wave’.”
– Hospital doctor |
Hospitals faced further challenges returning to normal delivery of health services. One problem was that many staff had left, having been redeployed elsewhere, or were too burnt out to work. For example, one doctor managing surgical theatres described that nursing staff had been deployed to intensive care (Intensive Care Unit or Intensive Therapy Unit) during the pandemic. They found that once theatres could begin operating again, there were not enough nurses to staff them. Those who did come back were distressed and exhausted from working in the ICU.
Learning for the future: planning and preparation across healthcareMany contributors said that planning for healthcare in the event of a pandemic was poor, and the speed of the response to the emergency was too slow. They described the huge and often harmful impact this had, with many lives lost or damaged and incredible strain on the healthcare workforce. They wanted better planning for future pandemics and ensure that the same mistakes are not made again. “It’s by having more emergency protocols in place, then it helps stop the wastage of time and resource and finances. I know from even just our small [team], we have had significant learning just to pool the resources across the region and optimise the simple things. We have those in place now, should we ever need something like that again.” – Allied healthcare professional “At a national level, forward planning issues need addressing. Vulnerable persons to be flagged earlier and better supported. Supply chains in emergency need to be strengthened. NHS should be supported and strengthened, no matter what the cost.” – Every Story Matters contributor Some contributors reflected on how to respond to the rapidly evolving pandemic when so little was known about Covid-19 at the start. Their focus was less on the initial response, and more on how learning about the virus, how it spread and how to treat it should have been embedded faster and communicated better as the pandemic went on. “You’d see the fifteenth iteration of a document that was barely any different in terms of the advice on PPE and protection of staff and all that a year later and you’d be thinking, ‘Yes, but this feels like this just needs to be completely started again. Okay, what did we learn from the first wave, now what should we be doing? This document should look completely different, and it doesn’t.” – Hospital doctor However, many were concerned that the continuing pressure on healthcare systems meant there was no way the lessons learned could be put into practice. This was a particular concern for contributors who work in healthcare, but also for some patients and the public. “It’s only a matter of time before we’re challenged… but it remains the case that the environment in [healthcare] is unfit for practice. It is a risk to both patients and staff; that has not altered at all, and that is a bitter disappointment… I think we’ve not really learned those lessons, and we need to realise that the science takes a while to catch up and they’ve done tremendous things but it’s those first days and weeks where there is a big threat to society and to staff, NHS workers.” – A&E doctor |
Managing the spread of Covid-19
We heard how hospitals changed the way they worked to care for Covid-19 patients and reduce the spread of the disease. Some contributors reflected that the early ways of working were particularly strict because of fear of Covid-19 and uncertainty about how the disease spread and what happened to people who caught it.
| “ | At the beginning, we offered a limited service, we were asking wards to ring down with what they wanted and scanning charts and things through to us, and then we were taking things and leaving them outside wards. We weren’t actually going on to the wards so we weren’t really giving them an adequate service but I think a lot of that was through scaremongering as well. I think everybody was so scared with what was going on, and because we didn’t actually know anything at the beginning.”
– Hospital pharmacist |
Hospitals often had strict zones for treating different types of patients, particularly keeping those with Covid-19 separate from others. Contributors shared how some hospitals labelled particular wards, bays, and areas as ‘hot’ and ‘cold’, or ‘dirty’ and ‘clean’ to signal which areas had Covid-19 patients and which did not. Some had ICUs specifically for Covid- 19 patients.
The Covid-19 areas usually had stricter PPE and visiting rules. There were examples in the stories we heard of hospitals putting in place zoning and one-way systems for moving patients within the hospital and across different wards to limit contact and reduce Covid-19 transmission.
| “ | I was then informed by my line manager that our ward might become a Covid-19 hot ward. Nobody really understood what that would mean but we were instructed to measure the distance between our hospital beds, to see how many patients could be nursed within our bays and maintain that two metre distance. We were told we would have to wear protective equipment at all times, but nobody really knew what that would look like.”
– Hospital nurse |
As hospitals admitted more Covid-19 patients, we heard how designated wards were made larger, or sometimes moved to allow more space.
| “ | The hospital decided they needed more Covid-19 beds. So, we were all put up to the sixth level, which is a cardiology ward. It was such a shame because all the staff there were shunned out to other places. So that was sad. That caused a wee bit of conflict. Twice we did it.”
– Hospital healthcare assistant |
Once areas designated for Covid-19 patients reached capacity, other hospitals, buildings or wards were sometimes converted to manage the numbers of Covid-19 patients. Many of the stories describe how disruptive this reorganisation was for those involved. Decisions about these kinds of changes were often hard for staff to understand, and staff and patients were sometimes frustrated by what was happening. Changes were disorienting and also presented staffing challenges.
| “ | And then, once that filled up, we had to then move up to another ward. So, in the end we ended up covering 2 floors of our hospital. And I think that was maybe the maximum of 40. I think about 40 patients at our worst. But that’s a lot of nurses to cover a lot of patients 24/7.”
– Hospital nurse |
There were also examples of some services, for example outpatient clinics, being moved away from hospitals completely to reduce the number of people needing to come to hospitals and support with social distancing.
| “ | We stopped having outpatients coming to the department. We were issuing prescriptions for them to go to community pharmacies, which I didn’t totally agree with.”
– Hospital pharmacist |
Treating Covid-19 patients
There were many examples of hospitals creating new teams to treat Covid-19 patients. This meant that many staff were reallocated to provide cover, often looking after patients outside their normal expertise. Some hospital staff were moved to work with Covid-19 patients by managers while others volunteered to do so. Some healthcare professionals described wanting to support the pandemic response by doing whatever they could to help people with the disease. Others shared how they wanted to reduce pressure on staff who had the expertise to treat Covid-19.
Caring directly for Covid-19 patients came with significant challenges and pressures. Hospital staff were worried about the added risks for them and their families in terms of catching and spreading the disease. Many were fearful about what they would experience when treating Covid-19 patients, and particularly the deaths they would witness.
| “ | I didn’t want to go to the field hospital. I was frightened of going to the field hospital because the field hospital we were going to have here, it wasn’t going to be where people were going to recover. It was going to be for end-of-life, so it was all going to be palliative, and it was just basically somewhere where they were going to put people. But thankfully, that was the worst possible scenario, and it never came to that.”
– Hospital pharmacist |
Some doctors and nurses who volunteered or were transferred from other roles acted as an extra pair of hands, rather than directly treating patients. Some contributors found these roles challenging, while others were pleased to help in any way they could.
| “ | Working, you know just as extra hands, lifting patients, caring for patients, doing some medicines and things.”
– Hospital doctor |
| “ | Most of the consultants were involved in doing the job of intubating and stabilising the patients. Then, more of the trainees would be involved in caring for them over the next week or two.”
– Hospital doctor |
Learning for the future: nightingale hospitalsNightingale hospitals were temporary hospitals set up during the pandemic as part of the response to the pandemic. Some contributors reflected on what can be learned from the huge efforts made to put Nightingale hospitals in place to increase intensive care capacity. Many contributors understood why this was done, but said they were underused or simply not needed. Contributors reflected on how better planning could ensure these resources are used more effectively if a similar challenge is faced in future. For example, suggestions included focusing resources on where they were needed most in healthcare systems or building extra hospital capacity but not for intensive care patients. “Instead of setting up largely unused Nightingale hospitals, resources should have been diverted to where they were most needed, that is the NHS on the ground.” – Every Story Matters contributor “We set up huge Nightingale hospitals with ICU capabilities which were underused, likely due to lack of highly trained staff or ICU need. A bit of lateral thinking could have meant these being used for less intensive care such as care of the elderly, rehab beds or Covid+ intermediate care beds, freeing up hospital beds for patients that needed them.” – Every Story Matters contributor |
We heard from some redeployed staff about how difficult and stressful it was for them, and how they had to learn quickly, often without enough training or support.
| “ | I and several others experienced ICU physiotherapists volunteered to spend the days on ICU to help the nursing staff in rolling and doing chest physiotherapy as required. When it came to being redeployed, we were actually redeployed as ICU nurses – this had not been communicated to us prior to starting our shifts – and all the jobs that that entails. We had no training – as there were too many patients – and were asked to do 12.5-hour shifts. We undertook all of this willingly as we knew that this was a challenging time.”
– Hospital physiotherapist |
| “ | My role changed abruptly when I was redeployed to work on a busy surgical ward including Covid-19 positive patients. I’d not worked on a hospital ward for over 20 years, so felt like a duck out of water, it was a steep learning curve to work in an area so stressful with little support. Redeployed nurses were needed to fill the gaps when other staff members were needed elsewhere.”
– Hospital nurse |
For example, being redeployed to other parts of the healthcare system was a common experience among community healthcare professionals who shared their stories with us. This often involved moving to work in Covid-19 wards and other support roles in hospitals. Working with new colleagues, performing tasks they had little experience of and adjusting to Covid-19 guidelines for delivering care was incredibly difficult for these contributors. This caused huge stress and anxiety, with some sharing how they did not feel equipped for the roles they were asked to do but were given no choice.
Kirat’s storyBefore the pandemic Kirat worked as a paediatric dietician, supporting children with complex needs who are tube-fed. She mainly worked with schools and also in a specialist clinic with children with autism to ensure they received the right nutrition. A few weeks into the pandemic, Kirat was moved to a new service which cared for elderly patients who had caught Covid-19. This involved being trained in how to move and feed older patients. Kirat felt the training was well organised but did not prepare her for how different the role would be from her usual role as a paediatric dietician. “I was trained to look after elderly care patients in terms of manual handling and feeding them. Because I’m a dietician, they thought, oh, yes, you know, that’s a good role. If somebody needs to be fed, a dietician could do that.” She described it as working in a ‘war’ and felt she was given little choice in whether she took on the role. This new job also meant she had to travel further to get to the hospital which made it difficult to pick up her children from school. “We didn’t get any choices when it came to, ‘Right, you are relocating to a different site and we need you to move to the hospital now, because the dieticians need support.’ Which was actually quite a bit further away from me, it was more stressful, and it’s just not what I’d signed up for, that’s not the job that I applied for.” |
Robert’s storyRobert is a liver disease and transplant consultant who was redeployed to support and treat Covid-19 patients in a Covid-19 ICU. Robert discussed how it was personally and logistically challenging to work in a new role during the pandemic, while also trying to maintain his liver disease/transplant service for non-Covid-19 patients. Working in a Covid-19 ICU meant that he was required to work longer hours. This included working 12 or 13-hour day shifts for four to five days, as well as some night shifts. “On a personal level responding to that…working areas you weren’t comfortable in, [you’re] working different hours, [there is] impact on the family. Then there was also the service that I looked after and how we had to try and keep that going to some extent even though we were doing all these other things. That was very challenging.” Robert’s normal work was treating people with serious liver disease who often die. This meant he felt more prepared for patient deaths than some of his colleagues who had been redeployed to the Covid-19 ICU. “The work itself wasn’t particularly challenging. Performing the role wasn’t particularly challenging. I think the things that were challenging were seeing nursing staff in particular struggling. They really had a hard time. Seeing them upset. There were lots of nurses in tears regularly. Also seeing fellow colleagues and a number of doctors really struggling. Those moments were hard, but I’m used to a speciality where we have a fair number of patients who die.” |
We also heard similar experiences from children’s community nurses at listening events.
Stories from children’s community nursesSeveral children’s community nurses at an Every Story Matters listening event recalled being redeployed to adult services during the pandemic. They expressed feeling a deep sense of concern over inadequate training for their new roles. “There was a sense of backlash from colleagues or managers; it was difficult, especially for those not comfortable with the new roles.” This lack of preparation left them feeling stressed and apprehensive, raising concerns about patient safety due to their unfamiliarity with the work. They emphasised the need for comprehensive training and support when healthcare workers are assigned to unfamiliar areas, especially given the potential impact on patient wellbeing and the anxiety it caused them. “Some nurses felt they couldn’t fulfil their roles properly, potentially endangering patients.” |
Nurses who were transferred to work in Covid-19 ICU wards shared distressing and harrowing frontline experiences with us. For example, some told us there were not enough experienced staff to supervise them. They had to quickly gain hands-on experience, often when dealing with very ill and dying patients. Redeployed nurses might start by observing an ICU-experienced nurse and helping check medication but quickly became the main person looking after Covid-19 patients. These nurses often felt a deep sense of worry and anxiety and did not feel prepared to treat patients. This left some with feelings of guilt and regret.
| “ | There was a big demand for people who had some ICU training, a big demand for ICU nurses which just could not keep up with the demand that we had at the time. It meant that the number of staff that we had, with the appropriate skill set to do the stuff that really needed to be done, was having to be done by much fewer people than you would normally expect.”
– Healthcare professional working in a Nightingale hospital |
| “ | The ICU nurse was supervising… actually looking after the patient, as you were really only there assisting her, checking drugs etc. But after that… you were main carer with an ICU nurse looking over your shoulder if you were lucky… it changed dramatically from the first couple of days, and then beyond that, it was really you doing it.”
– Hospital nurse |
Providing care to Covid-19 patients was similar to work some had undertaken before the pandemic. For example, one healthcare assistant told us their responsibilities included taking blood pressure, temperature, and blood sugar measurements as well as providing personal hygiene care. Some in clinical roles shared how the routine of completing daily rounds, assessing, admitting, and caring for patients was much the same.
| “ | There were a lot of resources coming out on a regular basis which were [also frequently] updated… with regards to… what things are… found to be effective, and what things are not particularly effective with regards to treating COVID patients. I think the thing that really helped was we would face a particular challenge for a day or 2 or 3, and then someone in the medical community somewhere would have figured out some solution… a few weeks later.”
– Nightingale healthcare professional |
We heard how the ways that Covid-19 patients were cared for and treated changed as new guidance and evidence emerged and the virus was better understood.
A few hospital staff shared how there was early uncertainty about what treatment was best for Covid-19 patients: to intubate patients and put them on a ventilator, or to provide patients with a Continuous Positive Airway Pressure (CPAP), a ventilation breathing support machine that uses mild air pressure to keep breathing airways open while the patient sleeps. As new evidence emerged, they increasingly turned towards using CPAP face masks as the preferred treatment.
| “ | And it remains a controversial topic. What’s the best way to treat these patients? Should you persevere with the CPAP for as long as you can or intubate them? Despite trials that have been conducted in the last couple of years, it’s not resolved.”
– Hospital doctor |
Healthcare professionals told us they did their best to care for Covid-19 patients in very difficult circumstances, and sometimes without the resources they needed.
Emma’s storyEmma was a nurse in a Nightingale ICU for Covid-19 patients. During the height of the first wave, Emma remembered having to work through difficult circumstances, such as having a limited number of ventilators and not enough staff. “Running from one place to another, looking for equipment, ‘Does this patient no longer need equipment? Can we take it from that patient and give it to this patient?’ You could be running around the whole hospital looking for additional resources, like respiratory resources, so I know it was very stressful.” She and her colleagues in the Nightingale ICU had to make Covid-19 treatment decisions and end-of-life care decisions quickly because of these staffing and resource constraints. This sometimes happened without input from families, as loved ones were not always reachable by phone. As she was in a senior position, Emma found it incredibly stressful being responsible for these decisions. She described many of her colleagues leaving ICU due to the stress they experienced. Despite these challenges, Emma said she felt a sense of camaraderie with her fellow healthcare professionals. “Although it was stressful, the vibe was very much, ‘We’re all in this together, we’re all doing our best with what we have.’ And from what you would be told by the government about resources, about them trying to get you personal protective equipment, trying to get us more ventilators, because the whole world was suffering in the same way, we didn’t feel like we were being let down by our employers or our own government.” However, Emma also experienced frustration as she and her colleagues wanted to provide the best level of care possible for all patients, but they were unable to do this. They did not always have enough respiratory resources. Emma said that many treatment decisions were made on the basis of who would have the best chance of survival. “These very quick decisions often had to be made just so that we can decide where the resources could go, because you could have somebody that was already at the end of their life with their terminal cancer in one ambulance and then in the next ambulance you could have, I don’t know, a 60 year old man who does gardening every weekend and still plays with his grandchildren.” |
In some cases, healthcare professionals who had health conditions or vulnerabilities told us how they were given remote-working roles, some that did not involve in-person patient care.
| “ | I wasn’t allowed to go out for a number of months because I suffer from a condition where it could have been life-threatening. So, I was told to just go home, so I worked from home.”
– Hospital nurse |
| “ | Of course there were health conditions among other medical staff as well, so they had to be redeployed. Some of them were deemed, by occupational health, to not be fit enough to work in a direct patient care responsibility, so they were given slightly different roles.”
– Hospital doctor |
For some healthcare professionals, the possibility of developing severe symptoms or dying from Covid-19 infection was too much of a risk. Some healthcare workers from ethnic minority backgrounds were very worried about the emerging evidence about vulnerabilities to the virus and did not feel comfortable working.
Stories from children’s community nursesDuring an Every Story Matters listening event, healthcare professionals from ethnic minority backgrounds recalled their own heightened concerns about personal safety and the risk of Covid-19 after learning that people from Black and Asian ethnic backgrounds were more at risk from Covid-19 infection. “Being forced into all that, I told her [manager] look. I’m Asian. Recent studies have shown Asians and Black people are hugely affected in terms of deaths, and if you’re breastfeeding, can’t get the vaccine, and she wasn’t taking any of it into consideration.” They felt that their employers did little to help protect them, and it even led to one leaving the healthcare profession out of fear for their safety. |
End-of-life care for Covid-19 patients
Hospital staff told us that seeing so many deaths among Covid-19 patients was very distressing.
| “ | You are going to deal with death and dying and it’s a very important part of the job, and it’s a job that you need to do well, in terms of care, caring for families as well as caring for patients.”
– Hospital doctor |
Contributors described how distressed they were about patients dying alone without their loved ones. Across the stories shared with us, this was seen as one of the toughest aspects of working as a healthcare professional during the pandemic.
| “ | The fact that people were in ITU, and they were alone was horrible because you could just see it in their eyes. You could see it in the eyes of the staff, the nurses, the doctors. At the height, it was a really horrible place to be… that was probably the thing that will stick with me the most, is that so many people died on their own, or so many people died on their own with only one family member around them, which was horrific.”
– Hospital porter |
They also reflected on how hospital staff being there at the end offered comfort to some dying patients’ loved ones.
| “ | [Their loved ones] were very thankful, because you were there when they weren’t, which helped a lot with them. They had peace of mind that they knew they were in good hands.”
– Hospital healthcare assistant |
Contributors shared examples of making sure at least one family member could say goodbye to a dying patient, even where this was not strictly permitted according to the rules at the time. Many healthcare professionals felt incredibly relieved when restrictions eased and loved ones were allowed to visit their dying relatives.
| “ | But if there was somebody that we were thinking was not going to make it… then special procedures were put into place… if there was somebody that we expected would be passing away in the next few hours or that same day, lots of extra effort was made to try and get a singular loved one in to say goodbye, hold their hand, things like that.”
– Nightingale healthcare professional |
Some ICU staff discussed trying not to burden patients with unnecessary and uncomfortable treatments that were unlikely to help them. One described how they tried to ensure that dying Covid-19 patients were not recommended CPAP face masks unnecessarily as they did not want their last days to be spent not being able to drink, eat, or talk.
| “ | We couldn’t burden the patient with painful, distressing, and what would be, ultimately, futile treatment.”
– Hospital doctor |
Other contributors across hospital healthcare roles highlighted the importance of treating dying Covid-19 patients with the dignity and respect they deserved and emphasised that it was a privilege to handle end-of-life care.
| “ | It is very important work, and you feel extremely privileged to be providing this work as well…I don’t feel good about it. On the other hand, I feel extremely privileged about it, and it is a duty for me to do so.”
– Hospital doctor |
The stories we heard described how both senior and junior staff had to make decisions about end-of-life care. At some hospitals, contributors told us only experienced senior doctors made decisions about end-of-life care for Covid-19 patients. They described not wanting to burden junior staff, especially those who did not have the experience and confidence to make those decisions.
| “ | We shouldn’t burden middle-grade staff, junior staff… we shouldn’t, and we mustn’t, and we didn’t burden them with these decisions. These were decisions which we have the experience to make.”
– Hospital doctor |
At other hospitals, we were told that a range of healthcare professionals of different seniority levels and expertise were involved in making end-of-life care decisions. Many contributors shared how making these decisions was stressful – particularly for those who were not used to doing so.
| “ | But, particularly for very young doctors who are on the ward or people who have been, sort of, accelerated through medical school to quickly go and work they didn’t have the confidence to know if what they were doing was the right thing or not. And they were surrounded by people dying, more than one patient in a day and often uncomfortable and looking distressed when they died. If you don’t have that confidence, that certainty and it’s all a bit new to you and you’re surrounded by chaos and suffering and death then I think it’s much more stressful.”
– Hospital doctor |
We heard how care decisions for Covid-19 patients were made based on medical history, underlying health conditions, and previous quality of life. Contributors who treated very ill Covid-19 patients discussed how unusual and challenging it was to have to make decisions about end-of-life care for so many patients at once.
They said they used all the information they had about a patient to make these decisions as best they could. This included what was known about them, such as their age and whether they had underlying conditions which may have made it more likely they would survive or see the most benefit from particular treatments, like ventilation. Some hospital staff, particularly doctors, said they were able to draw on existing knowledge about how to manage and make these kinds of decisions. This was based on similar experiences in intensive care or in areas like respiratory medicine.
| “ | We very quickly knew for whom we should be going straight to end-of-life care. A 90-year-old patient who has been sick for some days, whose heart rate was very high, whose blood pressure was precipitously low, whose chest X-ray was severely infected by the inflammatory condition, infective and inflammatory condition, which was Covid-19. They were end-of-life. We don’t go on age alone with anything, by the way, but it’s age and comorbidity with being 95 years of age comes other illnesses, comes frailty.”
– Hospital doctor |
| “ | So, if I had a 70-year-old or 75-year-old man or woman with Covid -19 who was failing a CPAP and I had to either put them on a ventilator or not put them on a ventilator, I can have a discussion with them… And some people would say, ‘I want to try it’, and some people would say, ‘I don’t want to try it’, and then of those two groups some did live, some died.”
– Hospital doctor |
We heard examples of Covid-19 patients who were admitted to the hospital being given a DNACPR notice. This meant they would not be resuscitated. One contributor shared how senior doctors would try to explain the circumstances for making a DNACPR decision to families over the phone.
| “ | Patients where [they] had a red form put in, which was a DNACPR, do not resuscitate, but they had Covid-19, but they also were in with other conditions. It was in their best interest that there wouldn’t be a call [for resuscitation] put out for them, so you had to, like they’ve had to be done over telephone calls and video calls to families.”
– Hospital healthcare assistant |
Contributors told us how end-of-life care sometimes involved hospital staff being with dying patients when their loved ones could not.
| “ | Nobody wants anybody to die on their own, and as nurses you try really hard to make sure that that doesn’t happen if family members can’t be there, you’re there. You just are. You just do it.”
– Hospital nurse |
For example, one healthcare assistant discussed holding a dying patient’s hands as their family looked on through a window. As well as being with patients at their time of death, hospital staff saw providing personal care and spending time with patients as an important part of their end-of-life care responsibilities.
| “ | It was combing their hair… creaming their bodies, showing them that love… changing their bed sheets, making them listen to their favourite music, giving some patients a bath, you know, pampering them.”
– Hospital healthcare assistant |
Some hospital staff told us about how attached they became to Covid-19 patients they were caring for. They would mourn the loss of their patients, particularly those they had grown close to through providing daily care.
Supporting bereaved families
Some hospital staff told us how hard it was to support bereaved families who were not able to visit when their loved one died. These families found not being there in person very painful and difficult to come to terms with.
| “ | And then I did, on occasions, have patients’ relatives that would ring me up and say, ‘Is my relative really dead? How do I know they’re dead? The ward rang me and told me, but I wasn’t allowed to come in and view the body.’”
– Hospital chaplain |
Many contributors shared how they had to make phone calls to patients’ loved ones to either discuss end-of-life care or let them know that their loved ones had passed away. Before the pandemic, these conversations would usually have happened in person. The healthcare professionals who made these calls often felt they could not offer the right support or convey enough compassion or comfort to bereaved families over the phone or via video calls. Contributors described feeling frustrated, upset and lost as they could not provide loved ones with the answers and explanations they sought.
| “ | It’s not just that physical of work, work, work; it is more the mental and emotional side of what we, what you’re dealing with. Patients’ [loved ones] crying down the phone to you and I’d [have] no answers [for] them, and you’re just going, ‘Look, we’re trying our best. We’re trying to do what we can’, but you know that’s someone else’s mum, dad, aunt, uncle, daughter, son.”
– Allied healthcare professional |
| “ | Talking to somebody on the phone and explaining to them what is going to happen, how it is going to happen, was extremely difficult and the sheer number was overwhelming to much of the staff who were much more involved in providing the care.”
– Hospital doctor |
Conversations with bereaved families were not part of some healthcare professionals’ normal roles. For other staff who shared their story with us, dealing with death and bereavement was more familiar, and this continued during the pandemic. This was particularly the case for contributors who worked in wards like the ICU that see patient deaths more often.
Ravi’s storyRavi was an anaesthetist and consultant in a Covid-19 ITU ward. As a consultant, one of Ravi’s main responsibilities was communicating with the families of Covid-19 patients over the phone. Ravi found it incredibly challenging to have conversations about end-of-life care, patient death, and bereavement every day, particularly when he had to tell families about a death knowing that the pandemic restrictions meant they might not have anyone with them to provide comfort and support. For Ravi, it was emotionally exhausting and draining to call bereaved families one after the other. He described this as one of the most ‘horrific’ things he has had to do. “To have those conversations over the phone with people you’ve never spoken to before when you don’t know who’s in the room on the receiving end, when sometimes the person on the receiving end is on their own and you’re aware that they have no one to give them a hug when you put down the phone, when the last time they saw their relative they were well, they were just getting taken into hospital for checks. Now 48 hours later, you’re calling them up to tell them their relative is dying and they don’t believe you and why should they? And they’ve got questions that you can’t answer, and you’ve got answers that they don’t want. It’s very hard and they can’t visit.” Ravi also got to know patients in the ITU and their families from caring and treating them, often over several weeks. This meant that he often became personally invested in the ITU patients. Even though dealing with their deaths was challenging for Ravi, he tried to make his patients’ passing as dignified as possible. He looked for opportunities for patients reaching the end of their lives to have one last conversation with their loved ones. “We’re trying to get quality for families, and so, even if, you know, I can wake a patient up for 2 hours so they can have a chance to have a coherent conversation with their loved ones, that’s a win, because that’s precious. And, you know, if they’re going to die, if we can make that passing as dignified and as not horrible as it can be, knowing it’s going to be horrible, and if we can take just some of the edges off it, it’s still going to be bad.” |
We also heard how hard and stressful it was to talk with, and comfort, those who believed they may have passed on Covid-19, and therefore felt responsible for the death of their loved ones. The loved ones were often very distressed and felt guilty that there was nothing they could do.
| “ | We had a patient…[where the] daughter who worked in the health centre [caught] Covid-19 and then spread it to him and he died from Covid-19. So, in that scenario that was quite distressing for that family because the worry had been that it would be cancer that would kill that patient, whereas he actually succumbed to Covid-19.”
– Hospital nurse |
Supporting patients with non-Covid health conditions
While many of the stories shared with us by hospital staff focused on supporting Covid-19 patients, hospitals continued to care for other patients too. Those who provided care outside Covid-19 wards shared many stories about challenges they faced during the pandemic.
Demand for hospital care for non-Covid-19 patients varied. Contributors described how people were afraid to attend hospitals. This meant some hospital staff saw fewer non-Covid 19 patients, particularly early on in the pandemic.
Later in the pandemic, contributors shared how they saw a backlog in patients needing care across many specialisms. This included children, cancer patients, and patients with other serious diseases and ongoing health conditions. Hospital staff said the backlog was a result of both services being reduced or closed (as discussed below), and patients being reluctant to access care.
However, some hospital staff shared how they continued to see patients throughout the pandemic. For example, those who work in obstetrics and gynaecology mentioned that their workload was largely normal. One contributor, a sexual health nurse, told us she saw an increase in patients seeking treatment and care during the pandemic.
| “ | The workload I had in sexual health was a lot more because people didn’t stop having sex. They didn’t stop having sexually transmitted infections. They didn’t stop needing family planning advice and contraception… I suppose there were more people at home. There was an increase in domestic violence and things like that as well, which we deal with as well. Sexual assault. So, our workload did increase, but we had less staff to deal with it.”
– Sexual health nurse |
Contributors told us how non-Covid-19 care was scaled back, with serious consequences for many patients, including deaths they thought were avoidable. Many of the stories shared by hospital doctors describe how patients’ medical conditions worsened because hospital care was not available. Some contributors felt that this de-prioritisation of non-Covid-19 healthcare was a result of too much emphasis on the pandemic and Covid-19 restrictions.
Learning for the future: balancing risks and continuing to offer careA common theme in contributors’ reflections on healthcare during the pandemic was that more emphasis should have been placed on other physical and mental health risks. Many contributors thought more should have been done to consider these non-Covid-19 health risks when decisions were made about Covid-19 guidelines and restrictions. “They got focused on one aspect and lost sight of those people who were not going to get a cancer diagnosis, not going to get treatment, not going to get cardiac surgery. There are lots of people that are going to die and have died because of the impact of Covid-19.” – Allied healthcare professional “We must never repeat the message that, ‘If you don’t have Covid-19, we’re not interested in you’. The message has to be healthcare carries on as per normal and if it’s too risky to leave the home, well we crack on and we carry on doing the clinics and we use the telephone and we use video and whatever we’ve got. We don’t just abandon people.” – Hospital doctor We repeatedly heard how more should have been done to continue routine medical care and prevent serious illness and avoidable deaths. This was often seen as something that should have been possible with the right plans and precautions in place. “If you think of the departments, you know, outpatients, that were closed… I still think there was room to keep some services running with precautions, yes, at a much lower patient flow but I do question, you know, there were a lot of people out of the hospital setting that possibly could’ve been utilised in other ways to keep referrals going.” – GP “People were being told to stay home, but healthcare is so vital that you cannot just do the bare minimum. There are now huge backlogs. Provision needed to have continued. There was a resource issue and there is now a backlog because people were told not to come forward and now there is a backlog of cancelled appointments.” – GP |
We heard how ward space and ICU beds were often prioritised for treating Covid-19 patients, leaving fewer resources for treating non-Covid-19 patients. Some healthcare professionals highlighted the shortage of intensive care beds for non-Covid-19 patients. As a result, some contributors gave examples of very unwell patients not getting the care they would normally.
| “ | A big thing that we provide is looking after people with liver disease around the country and also transplantation. Transplantation needs intensive care beds… and we really lacked that resource.”
– Hospital doctor |
| “ | I think professionally it was just very, very hard to not be able to do the job to the standard that we want to do it. We set very high standards for ourselves as professionals, and by and large we do everything possible to meet those standards, but it was physically impossible to do that because of resource constraints at the time.”
– Hospital doctor |
Many healthcare professionals reflected on how concerned they were about letting down patients who needed non-urgent care. The closure of some services did not make sense to some hospital doctors, particularly as the pandemic went on. They argued the needs of their patients were ignored or deprioritised when they should not have been.
Contributors told us how there were also fewer elective operations in hospitals. In some cases, they said elective and even normal non-Covid-19 urgent operations shut down entirely. They told us how they believed this led to some non-Covid-19 patients dying because they did not have the life-saving operations or other urgent treatments that they needed. Healthcare professionals who shared these stories were angry and frustrated and thought these deaths could have been avoided.
| “ | People turning up with diseases, cancers for example, that were more advanced than they otherwise would have been, often with life-changing consequences because they’d been unable to get a face-to-face appointment. And not just cancers, but also really debilitating diseases. I have several cases in my mind of people who suffered with benign but limiting conditions, that were very easy to fix had they had access to acute healthcare sooner. But, you know, it was very difficult for them to get access to healthcare, to see the person they needed to.”
– Hospital doctor |
We heard many stories about the lasting impact of this for patients. For example, one contributor described additional palliative care needs for cancer patients whose treatment plans had been disrupted. The delays to treatment have also worsened outcomes for patients with other conditions.
| “ | I’m now back seeing patients with MS and other rarer brain diseases, and what’s really clear is how significantly damaged they are by the pandemic, by neglect, so it’s only just emerging. We’re still seeing people in clinics now who haven’t been seen for 3 or 4 years face-to-face, and they’ve been neglected and they’re more disabled as a result, they’re more depressed, they’re more isolated and their problems haven’t been addressed.”
– Hospital doctor |
Discussions about end-of-life care and bereavement were no less emotional for non-Covid-19 patients and their loved ones. As with Covid-19 patients, contributors found communicating sensitive and emotional information particularly uncomfortable to do over the phone.
| “ | Some doctors are very good at having that discussion and some doctors are absolutely terrible and I think for some patients the feedback from the patients to the team was they found that quite shocking. So, messages to patients or patients’ relatives were being delivered by staff that were probably not very well trained in doing those discussions.”
– Hospital nurse |
Some contributors shared how they had to tell loved ones their relative had passed away, or were at the end of their life because healthcare professionals suggested non-Covid-19 services were closed. These very challenging conversations sometimes involved patients who were at the end of their lives.
| “ | I remember having to try to tell him and his equally elderly brother over the telephone, that we were not going to be doing an operation, and therefore he would definitely die. And this was probably in March 2020 when we really had zero visitors at all, and so that was incredibly hard. And then he was in a side room, so leaving that room and knowing that probably nobody would be with him in the moment that he died, and so he wouldn’t have that human comfort.”
– Hospital doctor |
Another contributor shared their experience of having to tell a patient with a bowel perforation over the phone that they were going to die because they could not be offered an operation. This was because the operation was moderately high risk and was assessed as riskier due to Covid-19.
| “ | At the time the evidence was suggesting that doing operations on people wasn’t particularly safe, particularly if they had Covid. It meant that people who in any other time would be offered an operation, an emergency operation to fix something catastrophically wrong with them such as bowel perforation, which normally we would go ahead with without thinking twice about, we offered far fewer of those operations. And in doing so, knew that people were going to die as a result, and that was obviously very hard.”
– Hospital doctor |
The experiences of non-clinical hospital staff
Contributors told us how the pandemic had a huge impact on hospital support staff, both practically and emotionally. Non-clinical hospital support staff, such as porters and catering staff, provide essential services to enable patient care. Some contributors who worked in these roles were largely able to carry on as they would, but others experienced significant changes. For example, some said they had to focus on certain aspects of their role and prioritise tasks differently while others had to work in new ways to maintain social distancing.
| “ | There was a special ward, I can’t remember which one it was, and when we delivered food there, there was a barrier, right, and we had to push the trolley through the barrier and not go in there… the staff had to wear something like spacesuits to prevent them from getting Covid. And also, we had to wash our hands more regularly, we had to wear masks all the time, no excuse… we just had to be really careful about hygiene and physical contact with others.”
– Hospital catering staff |
Contributors told us about how the upheaval caused by the pandemic was experienced across different roles in hospitals, not just among clinical staff. For example, hospital chaplains who shared their story with us described how they supported Covid-19 patients by being with them, holding their hands, talking and reading with them, and praying at their bedsides. At some hospitals, the chaplains were not allowed to walk the wards and had to be requested to visit by the patient or their family, or by a member of staff. One hospital chaplain also mentioned organising phone calls between Covid-19 patients and their loved ones.
Hospital porters also discussed how they had to learn different disposal methods for materials coming from Covid-19 patients than from non-Covid-19 patients.
| “ | The linen all changed, the refuse all changed, so if anything was from an infected ward, rather than going into a normal domestic waste bag, it would go into an orange bag or a tiger stripe bag, so it would be incinerated as opposed to landfilled.”
– Hospital porter |
Some contributors told us that where possible, desk-based roles were moved to be remote. This was so fewer people were in hospitals to support social distancing. In some cases, offices were repurposed into care settings.
| “ | And one of the days, we went into work, and we basically got told, ‘Pack your bags and go home,’ and everyone worked from home. So there was no notification, nothing. It was basically, ‘Pack your bags, go home,’ and then obviously everyone packed their bags, they went home. People were asking whether they could go to the office to pick up other items. You’re not allowed back into the office.”
– Hospital administration staff |
Administrative and IT support staff told us they experienced a change in focus within their role. They had to ensure that systems were operating to support social distancing and minimise patients coming to the hospital unless it was absolutely necessary.
| “ | We contacted a local taxi company to basically deliver medication to patients. Literally within two days, we within our team had made an ad hoc home delivery. Contacted patients, told them, ‘You cannot come up to the hospital,’ and I would say 90 per cent didn’t want to come up anyway. ‘Your medication will be delivered by taxi. The taxi will not know your name, they will not know the medication, they will literally be delivering it.’ …they went, ‘Yes, we’ll take it,’ because they weren’t getting any work.”
– Hospital administration staff |
In the early stages of the pandemic, the uncertainty meant support staff told us they had to do their best to help clinical staff without knowing what was most useful or the best way to manage their service in the pandemic context. One contributor who worked in a hospital laboratory said they had to adapt their services to consider Covid-19 contamination in samples even though they were not offering Covid-19 tests.
| “ | We weren’t testing for Covid-19, but there may be Covid-infected samples. Throat swabs for anything would be classed as an infective test. Even if we were just checking for MRSA or checking that they’ve got strep throat, that would have to be done under containment-level conditions because it could be post Covid-19. Right at the beginning, we didn’t know anything. We didn’t know whether it shed in urine. Didn’t know whether it populated blood, so all of our testing was done through Cat 3. Of course, we couldn’t because that’s just 2 rooms.”
– Hospital laboratory technician |
Some support staff shared how they increased their hours and responsibilities during the pandemic to manage the heavier workload. For some, this was viewed as a positive because not only were they helping out, but their skill set was also being broadened.
| “ | I just thought maybe helping them out, because I know they were busy… and it’s just helping the NHS. So, I thought it was a good deed and I thought, well, okay, I might as well just do it.”
– Hospital catering staff |
There were others who described their new roles as more challenging, particularly where redeployments meant that they were working closer to frontline services than they were used to.
| “ | They weren’t trained to be on the front line, to be in critical care, to see patients that were that ill. So, they were coming back with mental health issues and breakdowns, and going off sick, and sickness levels were quite high. The impact was massive.”
– Hospital management support |
Even though they were not providing medical care, some hospital support staff told us how they tried to connect with patients and their families. Hospital cleaners and catering staff interacted with patients and their families as they were carrying out their day-to-day tasks. They could see how difficult it was for families separated from their loved ones and so tried to do what they could to connect with patients and families, although this was often upsetting.
| “ | It was just so nice to do that…you’ve probably got a lot more time than some nurses, because we’re the ones that are in their rooms and mopping away and chatting away to them and making them cups of tea. You get to know them a wee bit…it just makes it that wee bit sadder, because you think, they’ve already been robbed.”
– Hospital cleaner |
For some contributors, offering support to patients included end-of-life care and for bereavement. These experiences were challenging and emotional and have stuck with them.
| “ | I was cleaning her room and I remember; she took her mask off to me. She was only like 24, 25…I’ll never forget her, and she says, ‘I thought Covid-19 wasn’t a real thing’, she went, ‘But honestly, it’s killing me…’ [Weeps] it makes me quite emotional, actually, it was sad.”
– Hospital cleaner |
4. Hospitals: experiences of patients |
 |
This chapter brings together what hospital patients told us about their experiences of accessing and using hospital care during the pandemic. It includes the stories of those who were admitted with serious Covid-19 symptoms.
Problems accessing hospital care
Problems with accessing hospital care were a huge concern to both patients and healthcare professionals. Wards were shut, care was prioritised, and appointments were cancelled, delayed and often moved online.
The changes to hospital services had a damaging and lasting impact on many patients. They shared examples of not being able to access the care they needed, across all types of non-Covid and planned care.
| “ | Everything was shut down, they were overrun with patients…they stopped everything, people died because of not getting their appointments, and not getting their treatment, and not going and getting checked for more lumps, like myself.”
– Hospital patient |
As well as overall problems with access, some people faced specific barriers. For example, some contributors with sight loss struggled to navigate hospitals that were unfamiliar and changing. Some could not find relocated clinics, and faced barriers handling routine tasks like queuing and signing in. The changes in hospitals introduced additional challenges like following social distancing markers, recognising and using sanitation stations, and identifying healthcare professionals dressed in PPE.
| “ | We attended Moorfields [eye hospital] for our glaucoma, during that time they moved the clinics, so the challenge was finding where they were. The queuing and signing in was challenging.”
– Person with sight loss |
This was made more difficult by not enough staff being available to offer support, which left contributors incredibly hurt and frustrated at the system.
Contributors described many problems and delays with care and treatment for long-term conditions and non-urgent health needs. Examples included hormones not being monitored for a long-term condition, tonsillitis being untreated, and patients in pain waiting for knee operations – among many others.
| “ | The precautionary hospital ward closures in 2020 and 2021 has significantly degraded my quality of life and mental health…now I have little to no hope of making a full recovery any more, since my overall health has declined due to my inability to exercise and the intolerable side-effects of the prescribed medication to manage my pain while I still wait for the postponed operation that I was going to be having in the spring of 2020.”
– Hospital patient |
Many blamed delays and problems with their care on steps taken to reduce the spread of Covid-19 in hospitals. These included social distancing guidance that led to reduced hospital capacity, along with the impact of staff shortages. Many told us about how distressing it was to wait for long periods, often while feeling unwell, or worried about their condition worsening. Some shared how they thought these delays were still affecting hospitals after the pandemic.
| “ | The impact of Covid-19 on the hospitals is awful, and noticeable, really noticeable, they are really struggling, they’re overrun, they’re understaffed.”
– Carer |
Some contributors were unsure the issues they saw with their care in hospital were solely because of the pandemic. They thought there were wider problems in healthcare systems that the pandemic worsened rather than caused. Some described their care as poor before, during, and after the pandemic.
| “ | The NHS was on its knees even before the pandemic, I would wait 12 weeks for an appointment even then. During the pandemic it was all phone appointments. Now it’s still diabolical. Lockdown and the pandemic is just an excuse.”
– Hospital patient |
| “ | We felt disappointed with that department just in general even before the pandemic and there were a lot of complaints…no one was happy there; it was completely slated”
– Hospital patient |
We heard how these problems left patients and their loved ones extremely worried about serious conditions that were untreated. Others were concerned about the unknown risks without the diagnosis they needed.
| “ | Due to staff shortages, they were saying, you know, ‘We can’t operate until it’s life or death,’ really.”
– Hospital patient |
| “ | As my operation was delayed by 8 weeks, I spent that time in hospital, unable to have family visits as we were in lockdown; and pinned to my hospital ward as we weren’t allowed to circulate round the hospital due to Covid-19 procedures. I felt many times that this Government wanted me to die rather than look out for me.”
– Hospital patient |
Sylvia and her husband’s storySylvia and her family faced numerous challenges during the pandemic, including cancelled hospital appointments and delays to treatment. Having undergone a knee replacement 18 months before the pandemic, Sylvia found that all of her follow-up appointments were cancelled. This left her with no post-surgical care. As a result, she now experiences pain in her knee, which she believes is a direct consequence of these missed appointments. In addition, her husband was facing his own healthcare needs. “My husband’s treatment for a basal skin cancer was delayed by more than 18 months due to the hospital backlog caused by Covid-19.” The uncertainty and anxiety around his delayed care added to the already overwhelming stress of the pandemic. Sylvia was extremely worried about his cancer getting worse during the wait, and what this would mean for his chances of recovery. As a nurse herself, Sylvia understood the immense pressure healthcare systems were under. However, experiencing cancelled appointments and delayed treatments on a personal level brought the reality of the situation into sharp focus. She felt angry and let down by the government and the healthcare system, arguing that appointments should never have been cancelled in the first place. “Political statements caused and continue to cause my family a lot of distress.” |
Those who experienced delays wanted to know whether more could have been done to allow them to access hospital care more quickly. They felt their health problems were disregarded to prioritise caring for those with Covid-19.
| “ | I went into hospital with sepsis, and I was still really weak. The whole experience with that, I believe, was because there were a lot of ill people in the hospital already with Covid-19. So, for me, without it, there were no hospital beds available. To be left out in an ambulance and being put on antibiotics in a drip and things like that, it was not a nice experience at all.”
– Hospital patient |
Many contributors shared experiences of witnessing older people become increasingly unwell and not receiving timely or adequate care. They believed these delays in care were avoidable and contributed to preventable deaths.
| “ | Whilst it’s very sad that so many people died of Covid-19, it’s equally sad that many of the elderly have died sooner than they would have done due to treatment being withdrawn or delayed because of Covid-19.”
– Hospital patient |
Some contributors directly blamed healthcare systems leadership and the government for the perceived decline in the health of people they knew. They believed that by neglecting to prioritise certain health issues, individuals were left to become sicker or, in some cases, die.
| “ | When Covid-19 occurred in March 2020, my husband was receiving treatment for pancreatic cancer. He had just finished 12 folfirinox treatments and was due to start radiotherapy. Due to the government’s mantra save the NHS, normal cancer services stopped and my husband undertook radiotherapy on his own…why was his end-of-life care not protected and enshrined? Nobody should die in pain from cancer. This was due to the restrictions brought in by Covid-19 and the government’s zealous to save the NHS.”
– Bereaved family member |
Pressure on hospital staff
Many contributors thought staff were trying their best but were clearly under pressure. They often reflected on the emotional toll of the pandemic on hospital staff. They could see that many were struggling with the burden and stress brought about by the pandemic.
| “ | Every time I visit the renal unit now, or speak to anybody, it’s always they’re short of staff…and a lot of it is the knock-on effect of actually having to deal with Covid, because a lot of the nurses themselves have had mental health issues because of what they had to experience.”
– Patient hospitalised with Covid-19 |
Despite the pressures, many contributors were positive about individual healthcare professionals and said they received the care they needed. Some shared how the overall standard of care they received remained high even in tough circumstances. Staff were often described as being attentive, caring, and warm despite all the pressures on them.
| “ | From A&E staff to the ward, to the surgeon, to the theatre staff, they were just all amazing at what they do… even though it was Covid they were going above and beyond what they were supposed to do.”
– Hospital patient |
| “ | The hospital staff who took care of me could not have been kinder and more compassionate, despite the difficult circumstances they were in.”
– Hospital patient |
Others described how hospital staff went out of their way to help them during their treatment, including working overtime to ensure that the patients’ needs were met when there was a shortage of staff.
| “ | Thankfully a lovely nurse from his practice visited him on the evening of the fifth day and was so upset by his treatment she worked overtime to improve things.”
– Carer |
Some contributors had fewer positive experiences with hospital staff, which they attributed to the pressure they were working under. They shared how staff could be worried and distracted and did not always communicate clearly or politely.
| “ | I don’t know the level of care that she got was up to standard…they were quite rude to her and dismissive of how she was feeling and I’ve got no way to challenge that, I’ve got no way to, kind of, support her on that.”
– Family member of a hospital patient |
| “ | At some point, the male consultant came. I’ll never forget this man. He said to me, ‘I understand you’re struggling with the CPAP.’ I said, ‘Yes.’ He said, ‘Well, if you can’t manage with that, you’ll have to be ventilated and then it’s 50/50 if you’ll live or die [harsh tone],’ just literally like that and then went.”
– Hospital patient |
Other stories shared by those receiving ongoing care for long term conditions described a shift in how staff they knew came across.
| “ | I had a pre-existing condition. Every time I visited the hospital, I saw exhausted, demoralised, and burnt-out staff working in a broken system. Nothing like how they used to be. Tempers were certainly frayed during that time, and I still worry about the long-term impact this all had on their mental health and the quality of care they can provide.”
– Hospital patient |
| “ | The impact of Covid-19 on the hospitals is awful, and noticeable, really noticeable, they are really struggling, they’re overrun, they’re understaffed.”
– Hospital patient |
There were a small number of stories from people with sight loss who shared other challenges that they faced, including examples of hostility from healthcare workers when they unintentionally failed to follow guidance.
Emily’s storyEmily, a 35-year-old blind woman, had to visit the hospital for a routine check-up during the pandemic. On arriving at hospital, she was immediately confronted by a staff member who shouted at her for not following the one-way system and not using the hand sanitiser station. This was despite her having a visible stick to help with navigation. Emily tried to explain that she was blind and could not see the signs. However, the staff member seemed to ignore her explanation and continued to berate her loudly in front of other patients and visitors. Emily felt a wave of embarrassment and frustration wash over her as she tried to navigate the unfamiliar hospital layout without any assistance. “I felt humiliated. The staff treated me like I was stupid or deliberately being difficult, when I simply couldn’t see the signs.” The experience left Emily feeling deeply hurt. “I felt like I was being punished for something I had no control over.” |
Patients who were treated for Covid-19 in hospitals
Many of the stories shared with us by Covid-19 patients described the fear they felt about being admitted to hospital, including that they would not see their loved ones again.
| “ | I went into hospital via ambulance on 19th January – 10 days after losing my mum – after testing positive and asked the paramedics if I was going to die. So many people didn’t leave hospital after getting it.”
– Patient hospitalised with Covid-19 |
Some contributors shared how they did not realise how ill they were, or that their symptoms were related to Covid-19. There were also examples of patients going to hospital to be treated for other conditions but testing positive for Covid-19 and having to stay.
| “ | The biggest surprise to me was I didn’t think I was going to get admitted, so I went to A&E in what I was wearing. The thing that I told everybody when I came back out is make sure if you’re, you think you might have it or whatever, have a bag with water, phone charger, anything. I had nothing.”
– Patient hospitalised with Covid-19 |
For some Covid-19 patients, this meant an abrupt and disorienting transition from their regular lives to being hospital patients. Some people woke up in a hospital with no memory of how they got there. It was only later that they realised their health had deteriorated rapidly and they had to be rushed to hospital.
Some Covid-19 patients told us they struggled to recall their time in hospital because they were so ill. They described being in and out of consciousness or, in some cases, being in a coma for days or weeks. This left them unable to speak much about the details of their experience, particularly the treatments they received, as it often felt like a blur.
| “ | One day I woke up in ICU unable to move, speak, eat, drink etc. I was totally reliant on staff to wash me, feed me, etc. I was hooked up to oxygen, had a catheter, wearing a pad, and remains of a tracheostomy in my throat. Apparently, I’d been in an induced coma for 2 months.”
– Patient hospitalised with Covid-19 |
| “ | I was admitted to hospital. I don’t know how long before they put me into – I was in intensive care. I was on a ventilator. So, I was in an induced coma for… a lot of the time that I was there. I can’t remember if they said it was about five weeks.”
– Patient hospitalised with Covid-19 |
For others, their lasting memory was being on a ventilator. These contributors described the discomfort and fear they experienced because they could not breathe on their own. They said they felt confused, vulnerable and very afraid.
| “ | I had the mask on for quite some time. Some masks were easier to tolerate than others. Some just used to feel really awful. I hated it, some of them. Yes, so that was very, very difficult because – yes, some of them – I don’t know. It was like you had to breathe with it, and then when you stopped breathing with it, I’d get into a panic mode, and everything would start – bells would start ringing, and [laughing] I’d be like, I can’t breathe, I can’t breathe.”
– Patient hospitalised with Covid-19 |
Many patients hospitalised with Covid-19 were in crowded wards, separated from other patients only by curtains. They described the constant noise and lights of the hospital, with staff checking on them throughout the night. Some found it very difficult to sleep.
| “ | It’s got some of the elements of torture, like the lights are on constantly, the level of noise…squeaky shoes, the staff would talk in normal volume. At one point, they were smashing up boxes during the middle of the night. Again, I know most of the patients were unconscious, but it did definitely affect my sleep quality and things.”
– Patient hospitalised with Covid-19 |
Some of those who were very ill with Covid-19 were offered experimental drugs or to take part in clinical trials, particularly in the later stages of the pandemic. These contributors described how doctors spoke to them about their options, as well as getting their consent before treatments began. Some felt privileged that they had contributed to the understanding of the virus and were given the opportunity to try something which might have helped save their life.
| “ | I think they gave me a trial drug as well which I’ve found out since, and that’s one thing that did help me.”
– Patient hospitalised with Covid-19 |
| “ | Yes, it was very frightening to be honest with you because you don’t know what’s happening next. I think they gave me a trial drug as well which I’ve found out since, and that’s one thing that did help me.”
– Patient hospitalised with Covid-19 |
Being treated next to others who were very ill sometimes meant patients watched as others died from Covid-19. Contributors told us how moving and terrifying this was, and how it served as a reminder of how deadly the virus is.
| “ | I’ve seen something that wasn’t really nice. It was a young man, and they had to give him compressions, whilst they were doing the compressions, I think it really triggered me… I started to have a panic attack.”
– Patient hospitalised with Covid-19 |
As they were getting better, Covid-19 patients told us they wanted to get out of hospital as quickly as possible. Some were worried they were taking up a bed that someone who was more ill may need. Others described how much they missed their home and family, and how desperate they were to leave and continue their recovery.
| “ | I was just so tired. It was more an exhaustion from the fact of the panic and whatnot that had originally taken place because I couldn’t breathe. Once that stabilised and such like, it was more a case of once I started feeling better, I wanted to go home because I was, like, kind of, ‘Why am I taking up a bed when there’s people that actually need it?’ But obviously they wanted to carry on monitoring me.”
– Patient hospitalised with Covid-19 |
Some of those who were hospitalised with Covid-19 told us they are still traumatised by their experience, even years later. They described the guilt they felt having survived while others that were treated did not. Others shared how they have flashbacks and panic attacks reliving their experience.
| “ | It still affects me on a daily basis. I do believe I have PTSD, but this has not been formally diagnosed. If someone mentions Covid-19 I mentally go straight back to the ward and the poorly patients immediately, the noise, smell, voices, feelings.”
– Patient hospitalised with Covid-19 |
| “ | A few weeks after my son’s mental health deteriorated, he was having visions of being back in his hospital ward and the man from the bed next to him in hospital was standing in his room and was angry that he didn’t help him…he is crying in Tesco because the beeping of the tills took him back to the monitors beeping in the hospital.”
– Carer for a patient hospitalised with Covid-19 |
Communication in hospital settings during the pandemic
Video and phone calls were important to allow patients to communicate with loved ones. These calls provided reassurance to family and friends, and helped patients stay connected to the outside world.
| “ | What was done well during the pandemic: The use of iPads to provide tangible links to family members in the ICU Ward in the early weeks of the 1st Lockdown, this made a huge impact on our family’s wellbeing in challenging times and I can’t thank the staff enough. It kept us connected when I didn’t think it possible.”
– Carer for a patient hospitalised with Covid-19 |
However, contributors told us that using technology was challenging for some patients. While staff members were sometimes able to assist, it was not always possible for patients to organise calls or find healthcare staff who were able to help.
| “ | My cousin had to really push to get my mum and my sister to FaceTime. You know, it wasn’t an easy. But this is end-of-life care you’re giving. I can understand, you know, if you’ve got 100 patients in there, you don’t have the time to FaceTime everybody, but even if you limit it to a 5-minute FaceTime, but it wasn’t straightforward at all.”
– Carer for a patient hospitalised with Covid-19 |
Some who shared their story with us also worried about making decisions about their health without advice and support from loved ones. Hospital staff often spoke to their loved ones if patients were unable to discuss their care, but this did not always happen.
| “ | [My husband] wasn’t allowed to come, so you miss that support, especially when you’re not thinking right because of brain fog and other different things, [you’ve got] somebody else listening to what the doctor’s telling you both and understanding if you’re not well.”
– Hospital patient |
Being discharged from hospital
Whatever their reason for being admitted, many patients shared with us how relieved they were to survive their hospital stay. Some contributors contrasted this with the fear they felt when they arrived in hospital.
| “ | The only contact with the outside world for much of the day was overhearing conversations staff were having about how Covid-19 was and its effect – a terrifying experience. The goal of everyone on the ward was to get out of hospital and get home. Many had high blood pressure because they were anxious to get home.”
– Patient hospitalised with Covid-19 |
Some contributors said they received less follow-up care than they were expecting after discharge. They often linked this to capacity and staffing issues within the hospitals. This left some feeling neglected, and that they had been left to manage their conditions on their own. This was a significant cause of distress and anxiety.
| “ | I was discharged home and left to deal with my diagnosis with no added support arranged. No follow up appointments with respiratory or cardiology were advised. From discharge, I continued to remain unwell, and after much chasing and aggravation I finally managed to obtain access to my GP – at which point further appointments followed and tests undertaken.”
– Patient hospitalised with Covid-19 |
Some contributors were angry about discharges happening too soon, particularly when they thought older people were put at risk. Contributors described how they felt they or a loved one were sent home from hospital to make space for someone else.
Many of the stories describe older and vulnerable people being discharged to care homes, and this was seen as a particularly contentious issue. Some contributors told us they were very angry that the risks of discharging people to care homes were not properly considered. This was seen as putting vulnerable people at risk and blamed by contributors for deaths they saw as avoidable.
| “ | In 2019 my son then aged 32 suffered a massive brain haemorrhage due to a tumour and was left extremely disabled and had to move to a nursing home. During the pandemic we were aware that hospitals were discharging patients who were infected with Covid-19 back to nursing homes and this was a very worrying time for us. The disregard by hospitals in discharging infected people to care homes should be investigated thoroughly and was extremely poor and dangerous practice.”
– Carer |
Learning for the future: communication with patients, families and carersMany contributors emphasised how lessons needed to be learned about loved ones visiting hospitals or attending appointments with patients, particularly those who needed additional support. There was a repeated concern about inconsistency and unfairness across the experiences shared with us. This unfairness led to resentment and frustration. We heard many examples of the damaging impact on patients who were left unsupported, sometimes as they were dying. Contributors wanted a more consistent, compassionate approach to visits and being with loved ones. “Everyone should’ve been doing the same thing, and they probably were supposed to be, but they weren’t. They weren’t. Everybody should’ve been doing the same protocols, and the same policies should’ve been implemented across the board so that there was no misunderstanding, and that way everyone knew that they should’ve been doing the same thing.” Allied healthcare professional Other contributors told us they understood the need to restrict visitors to reduce the spread of Covid-19. Where these kinds of restrictions have to be in place, they still wanted lessons to be learned about how to prioritise human connection because of how important that is. Ensuring families can still speak to and advocate for their loved ones was a consistent priority. “The staff in hospital were incredible. But that doesn’t make up for the lack of your nearest and dearest at crucial, life changing times. The impact of the restrictions will last for generations. Next time, we need to be better prepared, and we need to ensure that even when restrictions are in place, we’re human and we allow others to also be human and have connections with those they need most in their most difficult times.” Every Story Matters contributor Linked to this, many of the lessons learned highlight the need for much better communication between professionals and families who were separated from their loved ones. We heard many examples of poor communication that added to the distress families felt. The way this was managed also put many staff under enormous pressure. Contributors often said this was particularly important for the most vulnerable or unwell patients who were unable to use technology to communicate with their loved ones. “When a ban on visiting is in place, a much better system of communication with the hospital must be established. Using the normal ward telephone number to try and speak to staff about your relative was a persistent frustration. It was constantly engaged because every relative was using it alongside all of the usual phone calls that are made to the ward.” Every Story Matters contributor “I think one of the worst things was in the beginning when families weren’t able to come in and say goodbye. How that could have been managed any better, I don’t really know because it was safety for them, it was safety for everybody really, but there was a great deal of pain generally in that, not just staff, but obviously for the families themselves. But there was pain for staff as well, because they knew it was important for people to be able to say goodbye to their loved ones.” Hospital chaplain |
5. Emergency and urgent care |
 |
Emergency departments (referred to as EDs or A&Es in this chapter) are the way people with more serious cases of Covid-19 were assessed and treated. Patients with other urgent healthcare problems also continued to need help throughout the pandemic. This chapter shares stories about emergency and urgent care, including the experiences of those working in hospital emergency departments, paramedics and other ambulance staff. It also highlights the experiences of those handling urgent calls via NHS 111 and 999. It ends by describing patient experiences of emergency care.
Experiences of staff in emergency departments
Contributors who worked in EDs shared what it felt like to treat patients with urgent healthcare needs. Some described rising fear about what they would have to deal with during the first wave of infections. They saw themselves as the ‘front door’ for accessing urgent healthcare during a national emergency.
| “ | Part of the thing with emergency medicine is you never really know what’s going to come in through the doors…so, we’re used to the unknown and having to deal with whatever happens, and prioritising people that are in need rather than people that can wait.”
– A&E doctor |
Those working in EDs often said they were used to being flexible and adapting in crisis situations. Longer serving staff had experiences from past incidents and epidemics to draw on. Some contributors reflected that what they had seen and learned before helped them deal with the pandemic.
| “ | We’re trained in infectious disease management; we’re trained in how to protect ourselves from contracting things. In particular [my] last dedicated training was for Ebola.”
– A&E doctor |
Although working in a crisis was familiar, the experiences shared by ED doctors, nurses and paramedics highlight how different and overwhelming the pandemic was for them. The unfamiliar challenges and an ongoing heavy workload put many under significant strain. Many contributors shared how intense and demanding it was to provide healthcare to those who needed urgent help.
| “ | I worked as an NHS nurse in an A&E department for all of Covid-19. It was very challenging and very difficult throughout the whole experience to see so many people so ill.”
– A&E nurse |
| “ | My shift pattern in my job which was in A&E had changed…so every day I would go in and see death and every day I would wonder if this is the day I take it home to my small children.”
– Healthcare professional |
Emergency care workers reflected that patients dying was something they were used to experiencing before the pandemic. However, they found the contrast with normal end-of-life care painful, particularly when families could not see their loved ones.
| “ | I was a registered nurse on the frontline working in A&E during the pandemic…The hardest thing was not being able to allow relatives to be with their loved ones whilst they were dying.”
– A&E nurse |
Changes to emergency and urgent care during the pandemic
Each ED had a different experience during the pandemic, with some contributors describing being overwhelmed at times and others much quieter than usual. ED staff experiences depended on their role and how their hospital managed patients who needed urgent help, including those with likely or confirmed Covid-19. Contributors said that the numbers and types of patients requiring emergency care changed as the pandemic went on, and they had to continue to adapt. This meant there was no single, shared experience among those who worked in emergency and urgent care.
Contributors described huge pressure on many EDs during the pandemic. Many said they were incredibly busy during peaks in Covid-19 infections. Some ED nursing staff said they were not always able to provide the care they wanted to patients. They told us how upsetting and emotionally draining this was, adding to the physical demands of their role. This was particularly hard early on in the pandemic and during peaks of Covid-19 infections.
| “ | It was very sad that in a normal setting these patients might have had…more put to them to try and help them get better. With the number of patients coming our way, we couldn’t cater, and we couldn’t provide the full care for everyone. So, it was really difficult.”
– A&E nurse |
Every Story Matters contributor’s storyAn Every Story Matters contributor worked as a nurse in an emergency Covid-19 admissions ward during the pandemic. While she had 35 years’ experience, she suffered from post-traumatic stress because of her experiences caring for patients during the pandemic. Many people sadly died in the ward where she worked. She shared how she had to deal with relatives who were desperate to see their dying loved ones but were not allowed to. Jane tried to help people as best she could, but it was incredibly difficult. She used her personal phone to allow people to say goodbye before the hospital provided iPads. “[I was] double body bagging deceased patients and cutting locks of hair off them for their relatives.” There were also challenges with transferring very ill patients who needed to be in intensive care. This meant she and her team had to make decisions about who should be given an ITU bed so they could receive more treatment, and who stayed on their ward. “We were being made to play God in deciding on who went to ITU – who was given a chance to live and who wasn’t.” She also shared how difficult the pressure was for her colleagues. This made her own experience even harder. “Nursing staff crying when arriving for shift because they were so scared of being there…seeing junior doctors crying and looking scared and just not knowing what to do.” The contributor was unwell with Covid-19 and ended up being a patient in the ward where she worked. She then developed severe Long Covid symptoms including liver and pancreatic failure and has still not been able to fully recover. |
For some working in EDs, the initial and later waves of Covid-19 cases were manageable. They often pointed to worse experiences in other hospitals, or among colleagues working in intensive care.
| “ | [EDs] were occasionally dealing with really unwell Covid-19 patients, but actually the processes that were put in place for those patients often meant that they were whisked away to intensive care quite quickly.”
– A&E doctor |
| “ | Our intensive care colleagues…bore the brunt of what happened next with the patients if they were that ill. But for us at the front door, receiving patients from the community through into secondary care, I think we could just use the expertise that we’ve had for all these years and apply it.”
– A&E doctor |
Contributors described how EDs initially prepared for treating a large wave of Covid-19 patients. In the early weeks of the pandemic, the focus for EDs was on preparing for the expected wave of Covid-19 cases. We heard how many hospitals moved quickly to isolate potential Covid-19 patients, either in separate areas within their department or in separate buildings.
| “ | We’re a big hospital so we’ve got two sites across the city. The respiratory team looked after Covid mainly, so we didn’t see a lot of patients that came in just with Covid-19 – they tended to go to the respiratory team directly.”
– A&E doctor |
Contributors shared experiences of new shift patterns, physical changes to the layout of buildings, and new pathways for treating patients.
| “ | Changes were made to what they were doing, how they worked, everyone learning to don and doff PPE, isolating some patients, splitting the staff between zones.”
– A&E doctor |
Some ED doctors told us the planning assumption was that ICUs would reach capacity and be unable to take patients who would normally be transferred out of EDs into ITUs. This was a worrying and difficult time for ED staff who shared their experiences with us.
| “ | We thought we were going to have to be intubating patients. Putting them to sleep in our own department and then transferring them up to ICU or possibly having a number of ventilated patients in our department at times.”
– A&E doctor |
However, many contributors did not remember a clear plan at the start of the pandemic for how their services should be changed to deal with Covid-19. Very little was known about the disease, how to treat it, and how many people individual hospitals would have to care for. Instead, they often shared how they had to learn to adapt as the situation changed. Some contributors told us that this type of ongoing crisis response was more familiar because ED staff are trained and used to dealing with emergencies.
| “ | The plan wouldn’t be like an official plan, it would be more, ‘make your triage time quicker to get people in and safe,’ or it would be as soon as we get in, do all the transfers to the ward, don’t do anything else, then we’ll reassess. And it was more of a – depending on who was in charge – a military operation almost.”
– A&E nurse |
| “ | Continual management planning isn’t really part of the emergency department structure. We just go from crisis to crisis.”
– A&E doctor |
One contributor reflected on Covid-19 being an unknown disease, and how difficult that made the early stages of the pandemic. They shared how staff in emergency medicine are generalists, and often rely on others on shift or in wider teams to know how to diagnose and treat unusual cases. When it came to dealing with Covid-19, no one knew what was best, with one contributor describing ED teams as initially “desperate for knowledge”.
Many contributors said EDs found it harder to implement infection controls and that this was made worse by unsuitable buildings and a lack of space. Some who worked in EDs contrasted their problems with infection control with the stricter, more protective measures in place in other parts of the hospital. They said this approach to infection control caused resentment and frustration among staff.
| “ | In the emergency department, we were very much left and told, ‘Social distancing doesn’t apply in the emergency department’. It’s acceptable for us to be on top of each other. When the wards seemed to be cared for greatly, we seemed to be left by the wayside.”
– A&E nurse |
ED doctors and nurses often described how staff working in wards elsewhere in the hospital had a different and safer experience of the pandemic. Some ED staff thought they were forgotten about or ignored despite being on the front line of the healthcare response.
| “ | From speaking to colleagues in other [A&E departments] across the country, it was all very, very much the same. What was good for them wasn’t good for us.”
– A&E doctor |
Contributors working in some EDs shared how they saw fewer patients during the first lockdown, compared to later on in the pandemic. They believed this was because people were initially too afraid to seek treatment.
| “ | [Normally] we could have up to 400 patients through per day, and I think we were lucky if we were hitting 100 to 150.”
– A&E nurse |
Many contributors thought this climate of fear meant people arriving in EDs early in the pandemic were more ill than they would be normally. ED staff described how some people avoided or had not been able to access care from their GP. They then ended up calling an ambulance or arriving in A&E reluctantly, because their condition had worsened, or they felt they had no other choice.
Reduced demand allowed contributors working in some EDs to focus on patient care, which felt unusual. As well as being able to offer better care, reduced workload pressures allowed some contributors to build relationships as a team and improve morale. They saw this as important given the broader pressures they faced and the fear they felt.
| “ | It allowed us as a team in the [department] to get to know each other really, really well and to really build that teamwork and professional friendships, which was brilliant. Anybody who did come into the [department] certainly got a really, really good service.”
– A&E doctor |
Martha’s storyMartha worked as a senior doctor in the ED of hospital throughout the pandemic. While they had to adapt their services, she looks back on the pandemic as a time when her work was more focused. Fewer patients attended her department, partly because those with Covid-19 were treated by other teams in the hospital. “We didn’t have many Covid patients actually come through because they changed the flow through the hospital. So, they would go straight to either intensive care or to another area. So, the numbers in the emergency department were really low.” Martha shared how, before the pandemic, EDs often dealt with many people who were not ill enough to be there and should be seen by their GP instead. These people stayed away when the strictest Covid-19 restrictions were in place. This meant she and her colleagues only dealt with patients who really needed their help. “We saw a lot less patients, people that were there should have been there and it was a lot less stressful…we were dealing with people with something wrong with them, not just trying to avoid getting an appointment with their GP. So, our workload went down incredibly during the pandemic.” She also reflected that there was better co-operation between EDs and other parts of the health service, including specialities like mental health and maternity services. They also had extra help from junior doctors who were reassigned from parts of the hospital that were not seeing patients. “I mean, it’s all turned around now…but during the pandemic we could just do the job that we were meant to do.” |
Despite the benefits for individual patients, some contributors who worked in EDs described how concerned they were about the ‘missing’ patients who should have been seeking help. They were worried about what was happening to people who should have been receiving urgent treatment but were not. We heard how other EDs became busier as restrictions eased and more patients needed treatment for Covid-19 and other urgent health problems.
| “ | People were scared, they were obeying what the government was saying, but it was to their detriment. It’s like saying EDs are busy, stay away. That’s all well and good for the people who are time-wasters, it’s not for the people who are sick.”
– A&E doctor |
Some contributors described how early in the pandemic there was more co-operation between EDs and other parts of the healthcare system than there was before the pandemic, including around patient referrals. Later in the pandemic, contributors often said the pressures on EDs were amplified because other hospital departments were also under strain and therefore less able to offer support.
| “ | What I’d deem turf warfare between us and various specialties just resumed…we had a hope that it would be a big reset, and it’s largely gone back to the old ways – which is a bitter disappointment.”
– A&E doctor |
As with other parts of the healthcare system, contributors working in EDs said there were problems with staffing levels as testing and isolating became more common. They shared how this was particularly hard in EDs given the increasing demand for emergency and urgent care at the same time.
| “ | There was a lot of staff sicknesses so with short staffing obviously, you’re kind of juggling a really high workload and definitely a high equity of patients that you just can’t manage.”
– A&E nurse |
Many ED contributors shared the challenges of having to make decisions about prioritising care and transferring patients to ITU. In some hospitals ITUs were at or near capacity, and contributors shared how this had a knock-on impact on EDs. Where contributors were treating large numbers of Covid-19 patients, some shared how hard it was to deal with the lack of ITU capacity. They had to make decisions about who to prioritise in the ED, and who would be transferred to ITU.
Dami’s storyDami was a staff nurse in an ED during the pandemic. He described the early stages of the pandemic as chaotic, with constantly changing rules and processes. Dami felt some pride that he and his team did what they could, despite the huge challenges and the significant impact on their own mental health. “There was always work to do. So, the mindset was just crack on, like get on with it. You’d have like a meeting in the morning to say what’s changed and you’d just crack back on, get on with it. And anyone that’s upset, you literally just get on with it.” During peaks of cases, Dami and his colleagues faced very tough decisions about the care offered to Covid-19 patients. He said he thought he had blocked out some of the worst examples because it was too traumatic to think about. “I wouldn’t necessarily be proud of…the decisions that had to be made at the time because of lack of equipment or staffing.” One of the most challenging situations was when unwell people had already been ventilated and needed to be transferred from the ED to the ITU. This involved difficult discussions between staff over who to transfer in the context of very limited resources. Dami felt the focus was often on available equipment rather than what was right for that individual person, and that the presence of a DNR affected these decisions. “…that person at the time is ventilated, they don’t have a voice. And ventilation at the time was the only treatment.” |
Ambulances were often left queuing outside hospitals for very long periods because EDs were admitting fewer patients to avoid overcrowding and to maintain social distancing. This meant paramedics had to care for patients in ambulances and alert hospital staff to changes in people’s conditions. Many contributors said this led to delays in treatment, and difficult decisions when patients who were waiting became more unwell.
| “ | If there were lots of ambulances and someone became really critically [ill] and needed to come into the department…I needed to move the dying patient into a corridor. That’s a really terrible decision and that wouldn’t be allowed to be done today, but physically, when you’ve got no room, what can you do?”
– A&E nurse |
Contributors told us that approaches to treating Covid-19 in EDs changed as the pandemic went on, as they shared their experiences and the impact on patients. For example, rather than intubating patients in the ED or transferring them to ITU, patients were often given non-invasive respiratory support using CPAP, a ventilation breathing support machine that uses mild air pressure to keep breathing airways open while the patient sleeps. This change was seen as positive by those who mentioned it, and something that allowed them to offer more effective treatment for Covid-19 in EDs.
| “ | Right at the very start, it was decided this patient is getting intubated, going up to intensive care. Through the months, they realised, no, these patients are going to survive and have a better chance getting put on to this thing called CPAP. So, it did improve outcomes. It’s a shame to think that the people right at the start were given the wrong [care] – you just didn’t know.”
– A&E nurse |
| “ | I think there was some issues with anxiety around CPAP and treatments initially, but they were mainly around the respiratory treatment for patients. We never really saw desperately ill patients apart from the ones that were end-of-life.”
– A&E doctor |
Experiences of paramedics
Paramedics shared the pressure they were under, and how their roles changed. Working as part of a crucial frontline service, many highlighted how demanding it was attending emergencies and treating patients with urgent health needs.
For some paramedics, there were parts of their role that felt familiar. This included treating people with potential Covid-19 symptoms in a similar way to how they treated patients with respiratory illnesses before the pandemic.
| “ | We go to conditions that are similar to Covid all the time, and the way it was treated was no different to any other respiratory illness really. I can’t think of any specific protocols or anything like that.”
– Paramedic |
Yet paramedics described the huge strain they faced at different stages of the pandemic. For many, their working patterns changed. They often described moving to different and longer shifts and said that working extended hours for months on end was draining. Some said they were paired together with colleagues that they had not worked with before because of how working patterns changed. This brought further uncertainty and change in already challenging circumstances.
| “ | [I led] a team of 57 all delivering the highest standard of response and care to those affected. Initially we…were poorly protected, ill advised, and worked hours that were inhumane. But we did it without question…we were all exhausted, debilitated and internally scared.”
– Paramedic |
Some paramedics told us the requirement to use PPE was challenging given the need to act quickly in emergencies. For other contributors, however, there was a recognition of the importance of PPE for respiratory problems, including where Covid-19 was not confirmed.
| “ | We’d have people coming out screaming at us to hurry up, but then we’d have to don up our PPE first before we could go in…then it could be somebody in the house that they were doing CPR on, but you wouldn’t know if they had Covid-19 or not straight away.”
– Paramedic |
| “ | Everybody was kind of treated as Covid-19 positive regardless of their results. You know, you might have been into their home and somebody’s said, ‘Oh, I’ve done a lateral flow there and it was negative,’ but with anybody with any respiratory condition, we weren’t taking the chances.”
– Paramedic |
Some paramedics told us they experienced peaks and troughs in how busy they were during the pandemic, with intense periods that left many feeling exhausted, but also times when there were fewer calls to attend, particularly during national lockdowns.
| “ | We had these really intense periods of working and then these big lulls where we were sat around…everyone’s clapping with pots and pans and we’re, sort of, thinking, ‘This is probably the easiest period I’ve ever had in the ambulance service.’”
– Paramedic |
We heard from many paramedics about how pressures in hospitals, particularly around admissions, meant they were forced to care for patients in ambulances. These contributors shared stories about how they did this often for many hours and without breaks. As well as being difficult for patients, it was challenging for paramedics to look after very unwell people in ambulances. They said the waits for hospital admissions added further pressure to already stretched ambulance services.
| “ | There was an increased strain in the relationship between hospital staff and ambulance staff. Due to hospitals not wanting to off load patients into their department, we would be sitting outside during cold and hot weathers with full PPE and no breaks.”
– Paramedic |
| “ | Because hospitals were having to put in their protective measures because they had to think of their own staff and the patients, that led to longer times for getting patients outside booked in and their treatment started… a call suddenly, instead of lasting an hour or 2 hours, it was becoming a 3 hour, 4 hour… a crew could have gone out and maybe spent 8 hours just on one call between treating the patient, bringing them into hospital and having to wait.”
– Ambulance services manager |
Paramedics said they were the only option for patients to access care. Like the stories we heard from patients (discussed later in this chapter), some paramedics gave examples of GPs not wanting to treat patients with suspected Covid-19. Instead, GPs told patients to call for an ambulance. This included examples of patients who did not need emergency or urgent care.
| “ | We would regularly be sent out to see patients at home that were not housebound, who had been told to stay away from their surgery and await a visit from a paramedic. On one occasion a GP agreed to visit only after I had assessed the patient and determined that the acute illness wasn’t a result of Covid-19. We were used like canaries.”
– Paramedic |
| “ | The GPs would send ambulances around to homes because they did not want to be affected by it.”
– Healthcare professional |
Many contributors shared how this meant paramedics were increasingly exhausted as the pandemic went on. Sickness absence due to Covid-19 was also common.
| “ | There was a period where heaps of people were off and you’d rock up to work and look at the board to see what ambulance you’re on and who you’re crewed with, and that morning half of the board would just be light spots, because those people have called in sick with Covid, or their flatmate’s got Covid, partner’s got Covid, so they can’t come in.”
– Paramedic |
Some paramedics said that staffing pressures led to ambulances only being sent to the most serious calls. This was particularly problematic when demand for emergency and urgent care increased later in the pandemic.
Tyler’s storyTyler had retrained as a paramedic later in life, so had only been fully qualified for a short time when the pandemic started. He worked on the frontline throughout, responding to emergency calls. “We were working lots of hours, there was a lot of sickness and we’d become exhausted because we didn’t know what was going on, we didn’t know what to expect, but also every house we went to, we didn’t know who had Covid-19, who didn’t, how we caught it.” Overall, his experience as a paramedic was very challenging. He struggled with his mental health, and with feeling isolated from his colleagues. Other paramedics he worked with had similar problems, and he sadly lost one of his colleagues. “I was drained, constantly drained, very emotional as well…what didn’t help was a month into the pandemic, one of my colleagues actually took their own life, which had a massive impact then on us in the station as a whole.” As the pandemic continued, there were significant challenges with staffing because people were off ill with Covid-19, and because crews were spending longer waiting for patients to be admitted to EDs. At times they were only attending the most serious and urgent calls. “You’re actually taking over the role of the hospital being the bed outside…it was just getting to the point where we were only going to red calls because that’s how many we were getting.” The staffing pressures meant armed forces and firefighters were drafted in to help crew ambulances. While Tyler understood why this happened, it also meant he was effectively covering the work that would usually be done by two paramedics. This added to the pressure he faced, and he developed anxiety as a result. “So, the army came in to help us and the fire service…making us even more exhausted because you’re then doing everything with a person who doesn’t know what they’re doing.” |
Experiences of NHS 111 and 999 call handlers
Contributors who worked as call handlers for NHS 111 and 999 during the pandemic described the pressures of speaking to unwell and often distressed people.
Call handlers told us they had to deal with large numbers of calls from very anxious and unwell people, and they were not always able to offer help particularly during peaks in Covid-19 infections.
| “ | Usually there might be 30 calls waiting at any one time. At peak points in the pandemic there were 900 calls waiting.”
– NHS 111 call handler |
| “ | We had thousands of calls stacking, we were worried ourselves as we had to test regularly, we would only get a reduced rate of pay so the financial strain was also evident.”
– NHS 111 call handler |
Some call handlers shared how hard it was to speak to patients who had waited for a long time. Dealing with people who urgently needed help was overwhelming for some contributors, particularly when they could not offer the care and advice people wanted. They gave examples of people who said they desperately needed an ambulance, but their symptoms were not urgent enough for one to be sent. This was particularly challenging for call handlers who felt that they could not escape from the pandemic outside of work.
| “ | I would work 8, 10 sometimes 12-hour shifts and then come home to the news where I would have to watch how many people died, became hospitalised or the impact it was having on the whole world. But no training could have ever taught a person how to deal with the calls I had to take on a daily basis.”
– NHS 111 call handler |
Contributors working as call handlers described how there were changes to their usual script, requiring them to screen every patient for possible Covid-19 symptoms. Many of the calls were Covid-related in any case, with people worried about symptoms and what they should do or were from people who wanted an update following earlier calls.
| “ | People [were] more panicked, fearful, exasperated, often calling back because they’d not had any follow up or help.”
– NHS 111 call handler |
Mehreen’s storyMehreen had been working as an NHS 111 call handler for several years. At the start of the pandemic, she started to receive regular email updates with new information and changes to their call scripts. Sometimes, these changes would be put in place in the middle of her shift, which meant Mehreen, and her colleagues were constantly adjusting to the changing advice and guidance. Often, the local area managers would walk around the call centre checking call handlers had seen the latest advice and guidance. “I think that our local managers, like my direct line manager that I would’ve seen in person, they were great. They were always walking round the call centre, ‘Have you seen this update? Do you know that this has changed?” Mehreen found working in the pandemic very intense, she would often come to work early in the morning and answer calls constantly. Social distancing meant it was not possible to sit near to her colleagues, which left her feeling lonely. As the pandemic progressed the pressure on Mehreen increased, with call handlers taking difficult and emotional calls throughout the day. She would often comfort colleagues after an upsetting call. “You’d know when someone had taken a difficult call because I remember one of my friends took a call where she said it sounded as though the person was taking her last breath before they passed through to the ambulance service.” She felt good emotional support was in place in her call centre, with access to a text therapy number. Her line managers would also check in and ask people to take breaks when needed. For Mehreen, the most distressing calls were those where people had already phoned 999 and been told no ambulances were available. “They would phone us, and we’d be like, ‘Yes, but you do need an ambulance,’ so then we’d go through to ambulance, and they’d be like, ‘But we’ve got nothing to send.’ That was distressing.” Over time, the intensity and emotional impact of working in the call centre affected Mehreen. She would sometimes cry on her drive home as she felt so sad and overwhelmed. “I pulled over on the way home into a layby and had a cry because it was so hard. I found that I had to – you know where you…music was the outlet, and I would play music in the car as loud as possible all the way home to try and leave what I’d dealt with on the phones behind.” |
As well as peaks of calls related to Covid-19, contributors who worked as call handlers for NHS 111 or 999 recalled many calls focused on other health problems, including the mental health impact of the pandemic. One contributor shared how they took numerous calls focused on mental health, particularly in the evenings.
| “ | There were increased suicidal calls and calls involving mental health which the training had not really prepared me for.”
– 999 call handler |
The call handlers we heard from said that when they dealt with a difficult call, some level of peer support was usually available. However, this was often harder to access because of social distancing. This meant call handlers might be offered support via a breakout room or simply be sent home.
Given the pressures call handlers faced, some contributors shared how more structured emotional support was put in place where they worked. In one call centre, this support included having free access to a meditation app, access to counselling, and managers that were on the ground and saw them every shift. Other contributors mentioned how supportive their line managers were.
| “ | My direct line manager, they were great. Absolutely no qualms so if you’d had a difficult call, they would say, ‘Go and have a cup of tea. Go and have a sit down, five minutes.’ They really looked after the staff, they know what it’s like to get that beep in your ear and to not know what the call is going to be about.”
– NHS 111 call handler |
We also heard from call handlers who felt unsupported during the pandemic. In some call centres, contributors said they were not allowed to take leave even when they had anxiety or other mental health problems. Some criticised senior managers as not caring enough about the impact on call handlers.
| “ | I just felt I was running on empty…it just felt [like] you were a call handler, you were a number, and you were expected to be at work, you know. It didn’t matter what was going on I didn’t feel supported at all by my work…not from higher ups. I just felt that the support wasn’t there.”
– NHS 111 call handler |
Call centres were adapted to reduce the risk of Covid-19 infection. Contributors gave examples of the steps taken to reduce the spread of Covid-19 in call centres, including lower desk occupancy, social distancing measures, providing cleaning materials and recording where staff worked to enable tracing and reduce the spread of the virus.
| “ | They kicked in a lot of safety things very, very quickly, there was a large gap between us all, and masks, and everything got brought in straightaway.”
– 999 call handler |
In some call centres there were not enough staff to deal with calls. As with other services that saw high demand during the pandemic, staffing levels were a challenge. Call centre staff were often off sick or self-isolating and this reduced the size of teams working which worsened the already reduced capacity because of social distancing guidance. This meant call handlers who were working sometimes did not get breaks between calls, increasing stress and exhaustion.
Contributors gave examples of some successful recruitment drives, particularly bringing in people from industries such as tourism where they had lost their jobs during the pandemic.
| “ | We recruited a lot of people during that time. Strangely enough, a lot of people from tourism. Even at the best of times, it is a stressful job. With a worldwide pandemic going on, call pressure being unrelenting, it can be even more stressful. So yes, there were a lot of people joined, but a lot of people have also left.”
– 999 call handler |
Patient experiences of emergency and urgent care
Accessing emergency care was often harder during the pandemic, even when people were very ill. A lack of help in emergency or urgent situations was a common experience, as were long delays even when treatment was offered.
These problems had a significant and tragic impact on patients. The stories shared with us by clinicians and patients include examples of delays in accessing emergency care at each stage: people waiting longer than they normally would to ask for help; it taking time to find a service willing to assess them and offer care; ambulances being slow to arrive; and hospital admissions taking several hours, leaving patients waiting in ambulances.
| “ | By December 2020 there were no ambulances, no GPs, no room in A&E and we were literally turning up to people’s homes to deliver oximeters being begged for help. Patients were dying before we could get there or completely in the dark about just how ill they were. Desperate family members begging us for help when we arrived expecting us to be able to help.”
– Paramedic |
Patients shared many experiences of them or a loved one being very unwell and calling their GP, NHS 111 or 999 to seek help, but facing delays or not receiving care. Some contributors either gave up or had to wait until their symptoms became very severe before trying again. There were similar experiences among those who had suspected or confirmed Covid-19 and those who had other urgent medical problems.
| “ | One night I was sick over and over again. At 1am I called 999 and they said they would send an ambulance. By 6am it still had not arrived and I got back into bed, pregnant and exhausted. At 11am someone phoned to ask if I still needed the ambulance and that other cases were more “urgent”. They advised me to contact my GP. I did and the GP refused to see me saying I should contact 999 again. At this point I gave up. There was no help.”
– Person who called 999 |
In the early days of the pandemic, some contributors said it was unclear how suspected cases of Covid-19 were being dealt with. They thought health services were cautious about providing care given the risks, and this meant delays and problems for patients. Being referred between services continued to be a problem for many contributors who tried to access emergency care throughout the pandemic.
| “ | A very close friend had been showing Covid-19 symptoms for more than 2 weeks in early March 2020. He phoned the GP and NHS 111 several times but was told to just stay at home and isolate. He lived alone but I kept in touch…one day I couldn’t get an answer on the phone. Another close friend decided to go into his house, and he found him almost incoherent and dehydrated, so called an ambulance. The paramedics refused to go up the stairs to help him, it was left to his friend to get him down the stairs and into the ambulance.”
– Friend of person who needed care |
Some patients also reflected on how scared people were to ask for help, even in emergency situations. Many contributors told us that their fear of hospitals and not wanting to overwhelm healthcare systems meant they or others they knew delayed or avoided seeking urgent care, sometimes with terrible consequences.
| “ | My father-in-law was unwell in May 2020 and had some vomiting episodes and a subsequent chest infection from aspiration. My mother-in-law rang me in tears – she had not phoned their GP or NHS 111 because the news had been full of reports of the NHS being overwhelmed, but my father-in-law was by then quite unwell.”
– Family member of someone who needed care |
Henry’s storyHenry caught Covid-19 in August 2020. After feeling slightly ill for two weeks he went back to work. After a few days he started to have terrible difficulties breathing and he felt very unwell. He contacted his GP, who asked him to contact 119 to discuss his specific symptoms. 119 said that he should speak to his GP again as they could not make a referral to a Covid clinic. Henry went back and forth between his GP and the 119 service before he was referred to a local Covid-19 hub. However, he did not hear from the hub, and when he contacted them they said they had no record of his referral. At this point Henry’s symptoms got worse. Eventually he rang NHS 111 to try and get help, but the person he spoke to told him to call an ambulance if his symptoms were bad enough. “I was desperate for help, chest pains, struggling to breathe and mostly bedbound.” Henry felt he could not contact 999 because there had been so much in the news about people not calling an ambulance unless it was a serious emergency. He worried he would be wasting NHS staff time, particularly when none of the healthcare professionals he spoke to had considered his symptoms as an emergency. Eventually, Henry went back to his GP who referred him to a respiratory clinic. Once assessed by the clinic, he was advised to go straight to A&E. “I was taken through straight away and hooked up to a heart monitor. Lots of tests later, I was told that my blood pressure was so high that I was days away from heart failure. It took two months to be seen by someone, that should not have taken so long.” |
When ambulances were sent, long hospital waiting times caused significant problems and put patients at risk. As paramedics shared, emergency patients often had to wait in an ambulance for several hours before being admitted to hospital. Patients and carers gave many examples of these difficult experiences. Some contributors blamed the delays in being admitted to hospital for patients becoming seriously ill or dying.
| “ | I got rushed into hospital and because the hospital was so busy at the time, I can remember getting told that I was outside in an ambulance for over… six hours and I was on a drip and really unwell because the hospital was just so full of ill people during the time. They [the ambulance] took me there, I was [there until] three in the morning, actually trying to get me a bed.”
– A&E patient |
| “ | My dad suffered a slow and painful death. He didn’t have Covid-19 but was left unattended in an ambulance at A&E rather than having his vital signs recorded. By the time he was discovered, it was too late, he ended up suffering a cardiac arrest on his way for a CT scan. This was August 2020.”
– Bereaved family member |
We also heard examples of how people felt discriminated against when trying to access emergency care. For example, some contributors from an ethnic minority background felt they were deprioritised by ambulance services due to their race and ethnicity, and discrimination played a part in deciding who was prioritised for treatment.
| “ | I would say, white people were being treated quicker and faster, you know. They were Black, were left for hours in, like, emergency care, or even told to go home.”
– Person from a Black ethnic background |
We also heard examples of family members facing discrimination when trying to find out information about their loved ones in emergency situations.
Priya’s storyPriya’s uncle was rushed to hospital after suffering a brain haemorrhage, around 20 family members arrived, anxious for updates on his condition. Understanding the Covid-19 restrictions, the family spoke with the receptionist and agreed that only four of them would stay in the waiting room while the others went home. For the next six hours, as Priya’s uncle underwent surgery, the four family members took turns approaching the reception desk every two hours for updates. The receptionist on duty was accommodating and understanding of their situation. However, when the shifts changed, Priya and her sister encountered a stark difference in treatment. As they walked towards the reception desk, a white receptionist looked at Priya and her aunt, turned to her colleague, and said something inaudible. When Priya and her sister reached the counter, the other receptionist refused to speak to them, deferring to her colleague. The receptionist then spoke to Priya and her family in a condescending and discriminatory way. Priya was shocked and outraged by how they were treated, as she and her family had been co-operative and respected the hospital’s policies. “I think that’s where we felt a bit of racism, with the second receptionist who came on shift.” Priya couldn’t help but notice the clear contrast in the receptionist’s attitude towards a white family in the waiting room, who seemed to be able to approach the desk more frequently without any problems. The discrimination and lack of empathy from the white receptionist added additional distress to an already traumatic situation. “The only thing I would say is just treat everyone equally. Doesn’t matter where they come from, doesn’t matter how they look, doesn’t matter what language they speak. Just, I think, everybody should be treated equally.” |
Despite the problems around delays and other difficult experiences, some contributors shared more positive experiences of emergency care. For example, ambulances arriving when needed, and receiving a high level of care from paramedics.
| “ | My husband rang for an ambulance, and it arrived within 6 minutes. The paramedics were lovely. As my heartbeat was irregular and I’d also injured my face when I fell, it was decided that I should go to hospital. The staff in A&E were kind, friendly and professional, despite the ongoing pandemic restrictions.”
– A&E patient |
| “ | I became ill in October 2020 could not get a [GP] appointment had a telephone call and issued with antibiotics. Got worse eventually after no help from local surgery [my] husband rang for help. Paramedics arrived very quickly, then ambulance arrived and got taken to local hospital. From there within hour transferred to main hospital with sepsis. Operated on straight away and my life was saved.”
– Hospital patient |
2. 119 was a freephone line that was used in the pandemic to handle Covid-19 specific cases and to take pressure off NHS 111.
6. PPE and testing in healthcare settings |
 |
This chapter brings together experiences of personal protective equipment (PPE) during the pandemic and Covid-19 testing across healthcare staff during the pandemic. Both PPE and testing play an important role in infection prevention and control. This chapter starts by describing healthcare professionals’ experiences of the availability, quality and fit of PPE. It then discusses the impact of PPE on patient care, before sharing experiences of Covid-19 testing among healthcare professionals.
Availability of PPE
PPE includes protective items or clothing used to prevent the spread and infection of Covid-19. This includes face masks, gowns, eye protection and gloves.
One of the most difficult challenges healthcare professionals working in hospitals shared with us was not having enough good quality PPE, particularly at the start of the pandemic. Contributors said there was often a discrepancy between the amount and quality of PPE they had, and the PPE that was recommended for their safety at the time. Some said they simply did not have the right protection and felt abandoned by the government.
Many told us about their frustration and fear, and how they felt their safety was not being taken seriously. This was a common experience amongst staff across many different roles, but particularly at the front line of the pandemic response.
| “ | [We] were arguing the whole time along with all of our colleagues up and down the country that we need better levels of PPE…if it was a virus along the lines of Ebola or something like that, that I think all of us would’ve been wiped out. There’s just no way that this level of PPE is suitable…The way that leaves you feeling is being I suppose a bit expendable.”
– Hospital doctor |
While contributors told us that the availability of PPE generally improved as the pandemic progressed, some described problems continuing for longer. They shared stories of ongoing challenges with PPE supplies or changing supplies that meant they had to be fitted repeatedly for different types of PPE.
This was incredibly worrying for staff caring directly for patients with Covid-19. Many contributors were angry about the risks they were made to take. Some made a direct link between poor quality PPE and they or their colleagues being infected with Covid-19.
| “ | There was a lot of anger amongst the hospital staff, of all grades. Much of this was caused by the sporadic supplies of PPE and the lack of information about whether we would have enough to keep us safe for the duration of the pandemic.”
– Healthcare professional |
Contributors from ethnic minority backgrounds also highlighted their concerns around safety, and their fears that a lack of PPE would have a disproportionate impact on them and people from their community. For some, this added to the anxiety and stress they felt about working in healthcare.
| “ | When we started hearing about people of colour dying, we were out here with nothing to protect us. I didn’t want to work, let alone be a nurse.”
– Hospital nurse from an ethnic minority background |
| “ | In the beginning I was refused PPE by my NHS employer – I was not allowed to wear a face mask nor could I use any of own, despite having direct contact with patients coming to the ward. I believe many people of colour were put in situations that threatened there life. In the end I had a break down because of the stress it caused me.”
– Healthcare professional from an ethnic minority background |
Many contributors working in primary care also shared problems with PPE supply at the start of the pandemic. They said it was difficult and slow to get hold of the right type of PPE to the level of quality they needed. There was also a strong view among many contributors that hospitals were prioritised over other healthcare settings.
| “ | At the very beginning that was when we needed the best PPE, and we had nothing…the PPE came later on. The initial response was not adequate. This meant there was more staff sickness, early exposure. It took its toll mentally. The receptionists did not have PPE and they were facing patients, and they got the sickest.”
– GP |
Many contributors working in primary care described how the PPE supply improved over time, and they were later able to access PPE more easily.
| “ | I think initially, a little bit slow but it wasn’t for long; we certainly had sufficient [PPE] fairly quickly after an initial delay.”
– GP nurse |
Community health staff said that some basic supplies were available during the early weeks of the pandemic. However, many contributors shared the views of primary care staff that PPE was prioritised for hospitals, leaving community staff without the equipment needed.
| “ | We always had gloves and aprons anyway…it took us a long time to get the visors, actually, because the visors were being given to hospital staff, and I think it wasn’t until about Easter time before we got the visors in the community.”
– Allied healthcare professional |
Contributors told us about hospitals sharing PPE with community teams to help support care being delivered safely. However, the approach to this seemed to vary in different places and depended on decisions made locally.
| “ | In the inpatient service, we had immediate access. When community services started to restart, it was a little bit more challenging. If we knew a patient absolutely needed to be seen in community, there were times where we would offer the community service teams access to some of our PPE… I certainly know community services had a lot more challenges in terms of being able to get PPE. I don’t think it was as great a challenge for inpatient services.”
– Allied healthcare professional |
We heard about how sourcing PPE initially seemed chaotic to some staff, and how they had to find supplies in other ways. Where healthcare settings did not have enough PPE, contributors shared how they increased orders through regular suppliers. Some also shared how they looked for unused PPE from other organisations locally. The stories include examples of receiving masks from car garages or gowns from vets. Staff said they used their networks to find different routes to access PPE, doing their best to find what they could.
| “ | Regards to PPE equipment, I think it was at the very beginning [that there] was the shortage, but it was the schools and communities that were making visors and stuff. It was really amazing how quickly and how much they wanted to help. I think there’s still, within the hospital, some of the stuff that people made. It was an influx of people willing to do anything, just to make sure that we were able to protect ourselves and help protect patients. It was really, it was inspiring to see what the community was doing for us, and it made us know that they were trying to help in any way they could.”
– Hospital nurse |
Healthcare professionals were grateful for any donations and good will from the community. This community support was often described as crucial, with GP practices sometimes using donated PPE while they waited for central supplies.
We also heard about GP practices buying their own PPE through private suppliers to ensure they were sufficiently stocked. There were examples of alert systems being set up to monitor the use of PPE and to flag when more was needed. Some of those working in primary care shared that PPE supply had been fairly chaotic based on their experience in the early months of the pandemic.
| “ | The surge of requirements for PPE and all of that was a bit crazy and there was a lot of storage of things and things being bought from vets and God knows where to try and get masks and FFP3 masks fitted first off. I think maybe if it had been thought about a bit more rather than reactive all the time, it might’ve been better handled.”
– GP practice manager |
Even where GPs were able to source PPE, this could cause different problems. For example, one contributor working in primary care shared how they started to run out of storage space. Eventually they ended up with a supply of PPE that was no longer required. They donated it to other organisations such as care homes.
| “ | We found ourselves constantly having to contact the health board asking if we could return them, which we couldn’t, so we would be having to liaise with other surgeries to see if they could use the PPE. We ended up giving a lot of PPE to local care homes.”
– GP practice manager |
Healthcare professionals shared problems they experienced with PPE quality in hospitals and primary care. Contributors told us the quality of PPE was poor, even if it had been supplied to them relatively quickly. Contributors thought it was easier to find lower quality PPE. Many felt they had been put at risk from Covid-19 in a way that they should not have been.
| “ | The provision of PPE to GPs was poor. Or poor in terms of quality, I think we were provided with our flimsy plastic aprons and our paper masks fairly rapidly…the lack of acceptance that there’s significant evidence that a decent quality mask makes a lot of difference if you’re in contact with patients with Covid-19. And that it’s taken so long, that it took so long for that to be rolled out.”
– GP |
Contributors who worked in hospitals shared stories of PPE that would break or had holes. They also gave examples of PPE with stickers that showed it was out of date. Some described having to reuse PPE that had been washed. They did not trust that this PPE would protect them.
| “ | Being told that the yellow plastic jumpsuit that you’re wearing is going to be washed and reused, and the goggles that you’re wearing are going to be washed and reused, it felt second-hand. Because you could see yourself sweating and just the infection control of it, who’s washing it? Where’s it going? And then you’re wearing someone else’s. A lot of the equipment felt very cheap as well, especially the goggles that would break.”
– Hospital nurse |
Although some contributors spoke positively about the quality of PPE they had available to them. For example, a specialist in a regional cancer unit described a few initial problems but then felt they were provided with an adequate supply of good quality PPE.
Fit and comfort of PPE
Contributors working in healthcare during the pandemic felt that the design and fit of some PPE caused significant problems. These problems were often linked to new or unfamiliar types of PPE.
| “ | I used to do some shifts in the labour ward…if we had to go into [an operating] theatre with somebody… we had to wear the big blue gowns, double gloves, the hat, [the fitted] mask. You had to be fitted for your own mask and things, so once you were in that theatre, you were in. You couldn’t go out, you couldn’t get a drink because obviously, you couldn’t take your mask off, and that was absolutely horrific. That was the worst feeling, to have to wear all that [for] the full length of the emergency c-section. That was absolutely horrific, and that was every shift.”
– Hospital healthcare assistant |
Healthcare professionals shared many examples of PPE that did not fit them properly and had to be adapted. For example, a few female healthcare professionals highlighted how PPE often did not fit and seemed to be designed to fit men.
| “ | [PPE was] ordered in sizes primarily fitting the average male, not the average NHS worker, I was often so swamped in my PPE that it was uncomfortable and restrictive.”
– Healthcare professional |
Having to make adaptations or adjustments reduced confidence in how well the PPE worked to protect them, as well as making it more difficult for them to carry out tasks they needed to do.
| “ | I used to roll it up to my waist, get an apron and use the apron as a belt, and then hang a pen off that as well. So, the sizing wasn’t great and then you’re bigger than you think you are and you crash into a lot of items because you’ve got more width on you.”
– Hospital nurse |
Even for familiar or standard equipment, staff having to wear PPE for long periods led to problems with fit and comfort and negative physical impacts on staff.
| “ | Just the day-to-day things that we do – and you tend to neglect yourself, as in a drink or going to the toilet because you had to take all your PPE off and that was exhausting. Then you’d have to come back and put it all on. So that was hard…[and] that was over two years.”
– Hospital healthcare assistant |
Other physical impacts include examples of rashes, skin sensitivity, and marks from wearing masks for long periods. One contributor shared how they replaced FFP3 masks (a type of face mask that is worn over the nose and mouth to protect the wearer from inhaling hazardous substances) with ventilator hoods because regular masks gave them pressure sores.
Problems with discomfort were not only because of poor fit. Contributors shared examples of problems with PPE being made from uncomfortable materials and having to use PPE in hot environments.
| “ | I hated the masks; I hated the gowns. You were sweating, it was so bad. The wards were, our wards are regulated by steam generators, the heaters, and they put them on in the summer and all that. We were dripping with sweat with all this PPE on and trying to get the patients washed and showered, and that wasn’t a good experience, to be honest.”
– Hospital healthcare assistant |
There were mixed views on the training available for the use of PPE. Some contributors described how PPE was not always used properly (and was therefore less effective) because staff were not properly trained. The lack of access to training also contributed to staffing pressures in healthcare settings where staff were unable to work until the training was completed. Contributors gave examples of those who most needed the training being least able to take time away from patient care to complete it.
| “ | You had a situation whereby office staff, who are free to go for the training for the FFP3 masks, were all fitted. They could safely wear these masks. The people in the shop floor in A&E couldn’t leave. Legally, they weren’t officially allowed to wear the protective equipment because they hadn’t been trained in case we got infected and sued the organisation for not training us properly.”
– Hospital doctor |
| “ | Wearing PPE, being completely honest. So, one of the initial challenges, I think of the pandemic, was that we hadn’t had any training in putting on. I certainly had had some training at some point, but it was a long time ago. And, I think, the majority of my colleagues probably didn’t have any training on correctly putting on level 3 suits and masks. And, as you probably well know, the biggest issue, the biggest concern with putting PPE on is taking it off in the correct order.”
– Paramedic |
Julie’s storyJulie worked as a doctor during the pandemic in both hospital and hospice settings. Wearing PPE was very difficult for her, causing allergic reactions and physical discomfort. “The big thing for me with the introduction of wearing face masks and all the hand hygiene – I suffer from a lot of allergies and eczema, and it transpired that I was allergic to the nickel, the metal in the surgical masks, so I’d have a lot of facial reactions that were very painful. The FFP3 masks, I couldn’t wear because they also had metal in. I’m allergic to latex and the foam, so even wearing the visors, the foam at the top of the visors, I’d start to get very itchy and uncomfortable.” PPE made it hard for her to do her job properly. It also reduced her quality of life. Severe eczema flare-ups led to raw and weeping sores and poor sleep. This made coping with the pressures of work all the more challenging. In the end, Julie found she could not carry on working in the hospital. “I spent ages trying to find ways within which I could wear PPE without it being harmful to myself, and there came a point where actually it just became too difficult. I stepped back from covering the inpatient unit and mainly covered the community where you didn’t need to – you weren’t visiting patients so frequently, so there wasn’t the same intensity with adhering to the PPE, but then I felt very guilty for letting down colleagues.” |
Some contributors had better experiences of PPE, particularly those working in higher risk healthcare settings. For example, one contributor who worked in ICU was more positive about fit and comfort. They mentioned the extent of fit testing (a process of ensuring PPE is fitted in the correct way to prevent the spread of infection and ensure the safety of healthcare professionals) they went through to ensure their masks protected them as much as possible. This was followed up and repeated in the case of stock changes.
| “ | I had no problem, whatsoever. At the very start, we had a few issues with just our initial masks, but that was resolved literally within a week or two, and then we had a continuous supply, so we never had specific issues.”
– Allied healthcare professional |
Impact of PPE on patient care and treatment
The use of PPE was one of the most obvious differences in healthcare settings compared to before the pandemic. For some patients, seeing healthcare professionals in PPE was welcome. They felt reassured and better protected from Covid-19 risks.
| “ | They [the hospital staff] were all very careful [wearing PPE] and wiping things down, and I felt safe. I felt very comfortable with the care that they were taking to care for me, protect me.”
– Hospital patient |
On the other hand, some patients shared how seeing healthcare professionals in PPE was disconcerting and even frightening. This was more of an issue at the beginning of the pandemic when patients did not know what to expect, particularly in hospitals. For some contributors, seeing healthcare professionals in PPE for the first time brought home the reality of the pandemic.
| “ | So, it was definitely not what I was used to in a hospital, especially given that 3 months prior I’d had my baby in the hospital, and it was a lovely experience. It was really scary because you’ve never seen hospitals like that. I think it was the point where the scary-looking PPE was coming in as well.”
– Hospital patient |
Some contributors thought PPE created additional barriers between healthcare professionals and patients, and that this made providing care more challenging. Masks concealed facial expressions or emotions, reducing personal connection. This was seen by some contributors as adding to already heightened anxiety during the early stages of the pandemic.
| “ | They ushered us all into one room and everyone was walking round with face masks…it didn’t feel like a care environment; it felt one step apart because the mask, for being so small, hid such a valuable piece of your face, whether you were smiling, whether you were trying to comfort someone or whatever.”
– Hospital patient |
As well as reducing personal connection, PPE made spoken communication between healthcare professionals and patients more challenging. This was a particular challenge for patients who have additional communication needs, including d/Deaf and hearing impaired and some autistic people who depend on facial expressions to aid communication.
| “ | The other element of wearing the PPE, was it was very difficult then to deliver some of our services, because we’re a stroke service. So, some of our patients would have communication impairments after a stroke, or older people would be quite deaf, and they found that really difficult… especially if they were aphasic (a difficulty with language or speech usually caused by damaged to the brain)after their stroke, then they didn’t really understand what you were saying, and they couldn’t see your expressions, and things like that.”
– Allied healthcare professional |
| “ | I had a nervous suicidal breakdown […] My disability makes it impossible for me to communicate unless I see full faces. I still feel traumatised if I see someone in one [a mask].”
– Autistic person |
People who were d/Deaf or hearing impaired gave many examples of asking healthcare staff to remove masks for lip-reading, but this was refused because of concerns about spreading Covid-19. This left these patients in difficult situations, struggling to understand what they were being told.
| “ | You say, ‘I’m deaf,’ and they’re talking to you through a mask, and I’ll say, ‘I’m deaf.’ They’re, like, ‘Oh, no, no, I can’t take my mask off. You might give me Covid-19.’ I’m like, ‘Well, you know, I’ll stand over here, you stand over there. Please take your mask down, I’ll be more than 2 metres away,’ and they still refused. That was really difficult and then you literally can’t see their mouth or their face, so you’ve got no hope of understanding them.”
– d/Deaf person |
In life-threatening situations, some contributors felt that putting on full PPE meant precious time was lost. This meant contributors did not always feel that following the PPE guidance was the best thing to do – or that it always made sense.
| “ | We were also a bit suspicious that the guidance changed from FFP3 masks and stuff you’d use for a high-consequence aerosol disease [to regular face masks]. We had one weekend of using those guidelines… [and as] if by magic, within three days, it’s, ‘Oh, you just need a face mask,’ and we all went, ‘Oh, well, that’s interesting,’ but we went with it.”
– Hospital doctor |
PPE also presented healthcare professionals with ethical dilemmas. For example, one contributor discussed having to choose whether to quickly resuscitate a Covid-19 patient without PPE and increasing the risk of being exposed to the virus or wait to resuscitate the patient once everyone was wearing PPE.
Jack’s storyJack works as a consultant surgeon, caring for NHS and private patients. During the pandemic, one of his patients went into cardiac arrest. Jack’s instincts led him to start resuscitating the patient, but his colleagues pulled him away because he did not have the right type of PPE on. “I started resuscitating him and I got taken off him because everybody said, ‘No, you’ve got to put your PPE on.’ And I hadn’t and I’d just done it so instinctively and automatically and then the, sort of, complete fear afterwards.” Once this was brought to Jack’s attention, he felt anxious and panicked as he was worried that he had directly exposed himself to Covid-19. He was worried for his own health but also the health of his family, as he didn’t want to bring the virus home. Jack also felt guilty about the need to safely put on and take off PPE in an emergency, as he realised the more time they spent putting on PPE was less time for the team to try and resuscitate the patient, which meant a lower chance of survival. “The knowledge that the time it takes you to safely don and doff PPE meant that that poor man wasn’t being resuscitated for quite a long period of time while we were all putting our PPE on. You know, and it’s just that you are truly stuck between a rock and a hard place and that yes you know. I think you can never capture the reality of no normal person will ever understand, in the nicest possible way, what was involved.” |
When it came to wearing PPE themselves, patients and visitors usually described mask-wearing being strictly enforced during the pandemic, with few exceptions. Some contributors said they had to wear additional PPE such as gowns, overshoes, and gloves.
Some patients reflected on the challenges they encountered wearing a mask, particularly in the face of strict enforcement by healthcare professionals. They mentioned that they struggled to breathe while wearing them, which caused problems for some health conditions. These contributors said they felt under pressure to wear a mask constantly, particularly from staff members.
| “ | Yes, I had to wear my mask… but I was in the middle of being sick, in the hospital, myself, when a mask wasn’t a priority. But they would be, every time they come in, ‘Put your mask back on.’ I just felt very judged because I was trying so hard to put a mask on, and then I couldn’t.”
– Hospital patient |
There were some examples of people needing their own masks in order to visit loved ones in hospitals. At times, some hospitals had no PPE available for visitors.
| “ | I had PPE for my everyday work in my work bag…when I got to the ward, they were so relieved that I had PPE as they had just completely run out. They were all reusing PPE and stated that they would have had to turn me away had I not had any. Had I not turned up wearing PPE it would not have been possible for anyone to care for Nan as the hospital had absolutely none left.”
– Healthcare professional |
Learning for the future: PPEThe need to have enough good quality PPE available for future pandemics was a common reflection shared by many contributors. We heard how problems with PPE meant many healthcare professionals did not have what they needed to be protected, leaving them feeling frightened and undervalued. This was something many patients and carers said needed to be learned from too. Contributors wanted better systems in place to strengthen PPE supply chains and ensure stockpiles were in place for future pandemics. They also wanted fairer access to PPE across healthcare, and not just for staff in hospitals on the front line of the response. “Just having emergency supplies, like PPE, things like that. If we have another pandemic, worldwide leaders should all have some sort of emergency planning system in place for these things.” – Healthcare systems managerial support “I think working in healthcare we assumed wrongly that provision had already been made with stockpiles of PPE should a pandemic strike. The speed at which we required this distribution to localities repeatedly failed and the products themselves were often of inadequate quality. I would like to think that more rigorous testing and procurement of appropriate suppliers is now in place and that the logistics of supply/demand are covered should we need them again.” – Every Story Matters contributor Many of those working in healthcare wanted to see clearer guidance on using PPE for future pandemics, making sure this was tailored to specific settings. “You were getting so many policies and guidance out that just contradicted each other. So we were being told at one point we didn’t have to wear masks outside of work, but then we were told that we still had to wear them inside of work. It’s like we understand that we’re in a hospital setting and that people on wards still had to wear masks and that’s fine, but if we’re in an office setting… They didn’t specify which areas exactly.” – Healthcare systems managerial support |
Experiences of Covid-19 testing among healthcare professionals
Covid-19 testing refers to the availability and use of polymerase chain reaction (PCR) tests and lateral flow tests.
For many of the healthcare staff we heard from, testing was not an important part of their experience. They instead tended to focus on other changes to how they worked and provided care to patients.
Many contributors who worked in healthcare settings had good access to Covid-19 testing, but some said that they did not have enough, particularly early in the pandemic. Some staff were frustrated by this early lack of testing, or by limited support from management around testing. For example, one contributor found it difficult to access testing locally. They also felt that managers were not encouraging staff to test because of acute staffing shortages.
| “ | It definitely wasn’t being encouraged as well because there was a message of, ‘we don’t want you to be ill.’ There was definitely a lot of pressure to work…I tested positive, and I remember telling the team leader at the time and she was fuming. She opened the door, I told her, and she slammed the door…She was just angry that another person was ill.”
– A&E nurse |
Some contributors working in primary care reported that it was challenging to get access to PCR tests at the start of the pandemic. They felt those working in general practice should have been given access to testing for asymptomatic cases sooner. However, as the pandemic progressed access to testing improved – this included both PCR tests and lateral flow tests.
| “ | We had access to them, so that was quite reassuring. There was never any doubt on whether we’d be able to test our staff to see if they were fit for work.”
– GP practice manager |
As Covid-19 testing became more available, being able to test made some staff feel more comfortable and confident about the risks of infection. They thought this reduced the chances that they were working closely with someone who might pass on Covid-19. This was particularly important to some contributors in busy settings, including emergency medicine.
| “ | It gave us the confidence to know that the ones standing with us are unlikely to have Covid-19. We were still adhering to face masks and due to this very day, of course, and so I am confident that the staff were taking the steps necessary. But the lateral flow test availability was a good step in that direction.”
– A&E doctor |
Contributors had mixed views on the clarity of guidance and requirements for testing. Some healthcare professionals said they received regular communication and found it easy to follow the guidance within their settings. Others found guidance more ambiguous and open to interpretation.
| “ | I do remember when the testing came in and to be honest, that was quite up in the air because, you know, we got given the lateral flows and some people were saying, ‘You have to do them weekly and report the test,’ and some people were saying it’s if you’re symptomatic… And then I did lateral flows off my own back for myself and my family, obviously because I had a duty care, but nobody ever asked me, in my work, if I was doing them or the outcome of them.”
– GP practice manager |
We heard about differences in how frequently testing was required in different settings across healthcare. While some contributors were required to test at regular intervals (e.g. weekly, or before every shift), for others it was more ad hoc.
Contributors who worked in healthcare also shared how testing requirements changed over time. This included moving from testing being required only if staff had symptoms to testing regularly regardless of symptoms. They said this shift happened when at-home lateral flow tests became more readily available.
| “ | It was that phase of going from no available testing to some available testing – well, to limited available testing, who is going to get this, up to what are you going to be doing?”
– Palliative care staff |
Contributors working in healthcare settings recalled self-isolation guidance being particularly strict at the start of the pandemic. They shared examples of needing to self-isolate while waiting for test results and also being required to self-isolate if they had contact with someone infected with Covid-19.
Fear of having to self-isolate led some contributors who worked in healthcare to not comply with testing guidance, particularly if they were not experiencing any Covid-19 symptoms.
| “ | I maybe didn’t do it as often as I should have done. One of my concerns, and this sounds really selfish, and I hope this doesn’t come across wrong, [was that] I didn’t want to know that I had it, because I guess I just didn’t want to miss work. If I had felt rough or crap at any point, yes, I would have taken it and not gone in if I was positive.”
– Hospital porter |
7. Experiences of government and healthcare sector guidance |
 |
This chapter outlines views on guidance throughout the pandemic in healthcare settings. This includes how they were communicated to, and implemented by, healthcare professionals and the practical and ethical challenges of working within the guidance. It also covers the views of patients.
Communicating and implementing Covid-19 guidance
Healthcare professionals told us that they received general information about Covid-19 rules and regulations from the news and media, often at the same time as members of the public.
These contributors often felt apprehensive about the restrictions and guidelines, and felt they were ‘going into the unknown’. They heard about more specific rules and policies related to their professional roles through emails and briefings with senior leadership at work.
WhatsApp groups were a common way for sharing information about specific policies like quarantine procedures, staff sickness policies, changes to patient care, and PPE rules and processes.
| “ | National policies, those sorts of things are obviously from media and news channels and what have you. Within the trust, various WhatsApp groups were used as a quick way of circulating policy, legislation changes made within the organisation amongst various committees and senior management and execs.”
– Hospital doctor |
| “ | Yes, we had regular updates. So, the Chief Executive had regular updates. We had email comms as well, so written comms as well as verbal comms, and then information sort of filtered down as well. I don’t think there was a point where I didn’t really know what was going on. I think we were always aware.”
– Clinical scientist |
Many healthcare professionals reflected on how overwhelming the information was during the pandemic and how much of a burden it was to keep up with the changing rules, regulations and guidance.
| “ | I would say communication increased massively. There was a higher presence of senior executives and management. There were structures where there would be morning meetings, and they’re still continuing now, from my understanding. There have been benefits from that communication side, but it was more being told what to do rather than discussing what to do.”
– Healthcare systems managerial support |
However, some contributors working in healthcare settings felt ‘out of the loop’, as their organisation did not communicate with them regularly. This made these healthcare professionals feel excluded and unclear on the latest ways of working.
Contributors working in primary care tended to have discussions about guidance with colleagues. They said changes were the responsibility of individual GP practices, and they had some flexibility to tailor what they did. Some of these contributors gave examples of making decisions by talking things through within a practice and by speaking to other GP surgeries.
| “ | It was communicated really on a word-of-mouth basis for a lot of things. Our local area would have had a GP group, and they would have been on webinars and discussed how they should best move forward. It was pretty much left to themselves how they wanted to move forward with their practices. Then my GPs would have maybe come back from the meetings and said, ‘Look, everybody else is getting a room set aside, so we’ll do that too.’ So, it wasn’t like there was a lot of advice that seemed to come from the health board for the day-to-day practicalities.”
– GP practice manager |
Contributors working in hospitals said changes to guidelines were often communicated via email, with a more top-down system. They said some information was shared through colleagues.
| “ | The hospital services you always heard about what was happening by email, but GPs and stuff it was second hand and even sometimes some of the hospital stuff was second hand news as well. So yes, it was hard trying to keep up with the changes, what was happening, what policies had been put in place to help more people, PPE equipment, all the changes that went on through there as well.”
– Clinical scientist |
Many healthcare professionals reflected on how fast paced decision-making was. There was a sense of needing to respond to an emergency, which was very different from how changes normally happen in healthcare.
For some contributors this new sense of urgency and pace was positive. They tended to be those who said they previously found working in the healthcare system slow and frustrating. However, during the pandemic many of the usual barriers to change disappeared and contributors found it was possible to do things differently.
| “ | I would say for the first time ever, things moved really fast in the NHS. There was this ability to make decisions and to make changes really quickly, whereas that’s not normal practice in the NHS. Things are often, you know, there’s lots of bureaucracy, for reasons, and there’s lots of layers that you have to go through. Things take lots of time, whereas in the pandemic the ability to make change quickly was unbelievable.”
– NHS managerial support |
Many contributors told us how implementing guidance at pace was challenging. Healthcare professionals and managers shared the speed at which they had to consider different viewpoints and the potential impact on different services and their patients.
Some contributors working in healthcare settings gave examples of having to consider how their colleagues felt about their decisions. Many contributors described fear and anxiety about Covid-19, and this made people working in healthcare very cautious about the risks. There were often different perspectives on how best to implement guidelines and policies.
| “ | Challenging, because not everybody had the same views. During the pandemic, I would say dealing with different levels of anxiety and worry from different groups was a huge challenge. You have some people who are absolutely fine and coping really well, just let’s carry on, to people who really couldn’t cope, but all having to be on the same journey. I think there was a little bit of challenge in keeping everything going, and that was tough.”
– Healthcare systems managerial support |
Changes to Covid-19 guidance
We heard how changes to Covid-19 guidance created confusion among healthcare professionals. Many contributors found it difficult to cope with how often guidance changed, and how inconsistent it seemed. This was a common concern across different healthcare settings.
Contributors gave examples of guidance that would contradict previous guidance, and this was often challenging for those who were trying to make and embed changes in services. Some contributors felt this added to a sense of chaos and uncertainty across the healthcare system. They thought this reduced confidence in the basis for the rules and led to some frustration as the pandemic went on.
| “ | It was very chaotic in terms of rules changing all of the time and your knowledge base coming from the news as opposed to standard guidance that you’d expect from textbooks. And obviously, it was not written yet.”
– Hospital nurse |
| “ | It was like you didn’t know what update you were reading half the time, or the letters came that you would have to contact vulnerable patients or whatever group. You’d be thinking, well, I don’t know. I don’t even know where to start with this, and then there are so many different clinical systems. The guidance wasn’t even clear then, so it was confusing, it wasn’t clear.”
– GP practice manager |
Some contributors who worked different shifts, or on weekends, shared examples of coming back to work to find the guidance and protocols had changed. This included guidance for wearing PPE, transferring patients, and clinical procedures.
| “ | I could turn up one weekend and all the procedures that were in place the week before had all completely changed, and the week after I came back, they’d all completely changed again.”
– Hospital nurse |
| “ | Things changing every day was more just about how Covid-19 was being managed. How you should see your patients. Should you offer face-to-face? Should you be wearing a mask for certain patients? Could you be doing aerosol generating procedures in practice when you can’t ventilate a room? Things like that.”
– GP nurse |
The stories shared with us highlight some tensions and disagreements among healthcare professionals because of the challenges of implementing rules. These were often between those working directly with patients and those in management or senior leadership roles. For example, some contributors thought senior leadership often seemed to wait for guidance from the government on what to do rather than taking proactive action.
| “ | It felt like the senior leadership of the hospital was waiting for instructions and the hospitals that did better used their initiative and were autonomous and just thought, ‘What’s the best thing to do?’”
– Hospital doctor |
On the other hand, there were also examples of healthcare professionals taking initiative without consulting others and facing push back on their decisions.
| “ | We locally decided here’s how we’ll staff for the first wave, here’s how we will scale up, here’s how we will scale down. And then, about 6 months later, there came a, ‘Here’s what we did for this, how would we do it again?’ And the board response was, ‘Well, we didn’t ask you to do that.’”
– Hospital nurse |
Other healthcare professionals felt that colleagues used the guidelines and regulations for their own benefit. These contributors mentioned examples of colleagues taking time off when in close contact with Covid-19 too often or seeking to be furloughed. This created tensions in teams and organisations, including between those delivering direct care and managers or team leads, and between those working face-to-face with patients and those working remotely.
| “ | Certain specialities interpreted their national guidance to suit them… especially with some very similar procedures, one group happy to do so, battled on all the way through, another group very unhappy, refused to do it.”
– Hospital doctor |
| “ | For me as a lead chaplain, I suppose I wasn’t off any time, and maybe that was a frustration because when there were lots of people who were able to work from home… whereas some of us were coming to work as normal every day, and still being available every day.”
– Hospital chaplain |
Some contributors said they increasingly questioned the Covid-19 guidance and how it applied in healthcare settings later in the pandemic. For example, some of these concerns focused on whether the guidance was based on evidence.
| “ | Very reactionary and it came down to someone’s opinion rather than evidence, I think. It was just down to what that strategic planner thought should happen, rather than evidence of what is going to work for this.”
– GP |
For example, one contributor suggested that a change in Covid-19 isolation policy was only made to increase the availability of the healthcare workforce, by decreasing the number of days healthcare professionals had to isolate.
| “ | From my point of view, ‘Is it changing because the science is changing and it’s scientifically proven that this is the best choice, or is this decision being made because there are 50,000 vacancies in the hospital at the moment?’ We felt, definitely for those butts on the front-line that it was being changed just to get butts back to work.”
– Nurse who worked in a Nightingale hospital |
Following guidance and ethical dilemmas
Many healthcare professionals told us about difficult ethical dilemmas they faced around Covid-19 guidance. These dilemmas were often specific to their individual experience, but there were some common themes across the stories shared with us.
For example, some healthcare professionals described not following guidance so they could show more compassion for patients, families and colleagues. They often felt a duty to provide care that was human and compassionate, and felt conflicted about balancing this with following guidelines rigidly.
One contributor shared how they and their colleagues did not follow official guidance, instead letting dying patients stay in the emergency department longer so their loved ones could say goodbye.
| “ | They weren’t sending the patients to the ward. They can stay here with their family and die in the emergency department and their family can stay with them and never mind the four hours. That’s happening.’ And I think the nurse in charge got told off.”
– A&E nurse |
Another mentioned how a call from a care home came in asking for ambulances to be sent to take dying elderly patients to the hospital. However, transportation to the hospital by ambulance was not in line with protocols during that time. The contributor, with the ambulance staff’s agreement, provided the ambulance.
A few other healthcare professionals also described not following PPE guidance when caring for patients. For these contributors, some of the guidelines restricted the type and level of care they could provide, which they felt was wrong. One contributor described choosing not to wear all the required PPE, with the patients’ permission, when treating women having complicated births. They let the patients choose if they wanted staff to take off their PPE or keep it on. They offered the choice to not wear full PPE to remove the barrier created between patients and healthcare practitioners and increase human connection.
| “ | The first thing I did, I would say to the woman, ‘I am very uncomfortable having this conversation about what you’re going through with wearing a mask and being unable to touch you.’ So, the first thing we did, very often, was to remove our masks and ignore the restrictions because human contact when someone’s going through loss and extreme change seemed to trump the rules. That’s the kind of area I specialise in, extremely premature birth and babies with abnormalities. We obviously gave women and their families the choice… I can’t think of a case where they didn’t prefer just to have a normal interaction and take whatever risk there was.”
– Hospital nurse |
Patient perceptions of rules and regulations in healthcare settings
Contributors often focused on hospitals when discussing Covid-19 regulations. For hospitals, there was confusion among many patients about visitor policies, PPE requirements, and testing protocols. This confusion caused uncertainty and anxiety for many hospital patients.
Patients often talked about “rumours” they heard about rules and regulations. For example, one contributor thought that wearing a mask was mandatory, only to discover that a significant number of other patients were not wearing them. Another turned up expecting to be tested for Covid-19 on arrival, only to find out that testing was not routinely carried out. This added to stress during an already challenging time.
| “ | We were also devastated to discover, via the media, that some hospital trusts were permitting visits to patients who were on Covid-19 wards, as long as appropriate PPE was worn. I desperately requested the same, to see my mum but was categorically denied the privilege. Their trust would not allow it. No one was getting to see her.”
– Bereaved family member |
| “ | If you were staying there, they didn’t expect the patients to sit in the beds, 24 hours, sleep with masks on, blah, blah, blah so once you were up on to the ward, you were allowed to take the mask off. But you had to wear one – it was so inconsistent.; it was like one person told you this, one person told you that. Then you just had to kind of, I don’t know, hope for the best that you were doing the right thing.”
– Woman who used maternity services |
Stories from people with a learning disabilityIn the listening events with people with a learning disability, they told us it was hard to adapt to the changing world during the pandemic. “You had to stay in your room and keep to yourself. There was no option to understand what it was.” – Person with a learning disability The lack of clear and easy-to-understand guidelines about lockdowns, PPE and service changes or closures left many feeling confused and unsure. This lack of accessible information made it particularly difficult for them to understand the changing rules and regulations, leading to feelings of anxiety, isolation, and exclusion. They recommended that in the future, governments and health services should involve people with learning disabilities in creating accessible guidelines and contribute to decision-making. “I would’ve had all people with learning disabilities involved in decision making and be able to think about what to do and do it better.” – Person with a learning disability |
Some patients described rules not being applied consistently by healthcare professionals, although contributors sometimes welcomed this flexibility. For example, one patient with anxiety was allowed in the wards to see where she would have her operation in advance despite that not being allowed according to the rules.
Some contributors also gave examples of patients being allowed to see relatives in hospital even when this was not allowed by the rules. They were often grateful when this happened.
| “ | My daughter in law’s father unexpectedly had a severe stroke, and he didn’t survive, but he was in the intensive care neurological department in Newcastle. And officially, they were only allowed 2 at his bedside as he died, but actually the staff bent the rules and allowed more which they were very grateful for.”
– Bereaved family member |
On the other hand, many contributors also said rules being applied inconsistently caused problems and uncertainty. For example, one patient described how healthcare professionals allowed a family member to be with her in hospital, but later in the day another staff member made them leave. The next day a third healthcare professional allowed them back again.
When this happened, patients found the mixed messages hard to understand and frustrating. This was particularly difficult when the inconsistency had an impact on their experience of patient care or meant they were not able to see loved ones.
| “ | At the time the government guidelines were much more liberal than the rules the hospital actually chose to apply, which was hugely frustrating and had a detrimental impact on my mental health. Other hospitals were far more accommodating, with use of compassion and common sense.”
– Hospital patient |
Contributors also discussed how guidelines and regulations differed across healthcare settings. There was a feeling that rules could apply in one hospital or GP practice and be different in another.
A few patients gave examples of healthcare professionals who seemed to pay little attention to some guidelines and processes which they found confusing. For example, one patient said they filled in forms about whether they had isolated before their operation, only to have nobody to ask for the forms to ensure they had followed the procedure.
| “ | Every time I went in, I had to do my temperature and write whether I’ve isolated in the last 10 days, and no one ever checked the sheet once I’d gone in anyway. I kept all the sheets myself. No one took it in to look at it. So, I just felt that there were so many tick box jobs going on where I just thought, ‘Well, what’s the point of this?’”
– Bereaved family member |
In another example, a patient explained how some of the doctors and nurses that looked after them were not wearing masks, despite it being required at the time.
Gbemi’s storyGbemi had to spend several days in hospital due to complications with her pregnancy. During her stay, the policies and rules seemed to change daily without clear communication or rationale from staff. Gbemi’s husband was only allowed to visit during specific hours, but these hours varied from day to day. On one occasion, he arrived at noon and was required to stay in the room until 8 pm without leaving, even to get food. If he left the room for any reason, he would not be allowed back in. However, on other days, he was permitted to leave the room, and the visiting times were either shorter or longer. Gbemi felt that these rules failed to consider the practical needs of patients and their families, such as getting meals or taking breaks. “It felt like they just plucked these rules out of the air and thought, ‘Oh this is alright, this is what’ll minimise it.” The lack of clear communication from the hospital staff only added to the confusion. No one took the time to explain the rationale behind the visitation rules or the reasons for the changes. This left Gbemi and her husband feeling frustrated and anxious, not knowing what to expect from one day to the next. Gbemi noticed that the enforcement of these rules was inconsistent among the hospital staff. Some nurses were more lenient, allowing brief visits from family members, while others strictly adhered to the rules. This inconsistency further compounded the stress and frustration of being in the hospital during a pandemic. At times, Gbemi felt the staff’s communication could be rude, with little consideration of the impact on patients and families. Although Gbemi understood the pressure healthcare workers were under, she believed that the hospital could have handled the situation better. “I felt sorry for them because working in the public sector myself I know how bad it is and I knew how swamped they were, but the rules just didn’t make sense.” |
Rules about hospital visits were very frustrating and upsetting for patients and their loved ones. During the pandemic hospital visits were restricted to reduce the number of people going to hospital and the spread of Covid-19. Many contributors were frustrated that patients were expected to attend hospitals alone in the early stages of the pandemic. The number of visitors and visiting times continued to be restricted as the pandemic progressed.
| “ | It was horrible. I wasn’t allowed my sister in, it wasn’t, my girlfriend wasn’t allowed to be there. So, I was sitting there waiting, and you’re in your own room and waiting there for someone to start cutting your neck open. It was hard enough to be facing the operation, but then you’re facing it on your own.”
– Person who was clinically vulnerable |
Having to attend hospital alone without the support of relatives and friends was very difficult for patients who were already afraid. The possibility they could die alone was particularly distressing for patients with life-threatening conditions. Family members and friends also shared the fear and anxiety they felt, and how their loved ones struggled with having to go into hospital alone.
| “ | We could not contact him because the wards wouldn’t pick up the phone. Dad was not well enough to use his phone, it goes against our human rights charter to treat anyone like that, you know.”
– Bereaved family member |
| “ | My husband was taken into hospital and basically written off. because of age and other conditions…he was negative for Covid-19 and he was put on a ward where it was rife. We were not allowed to visit, had no idea of what was happening. He passed away and I received a phone call at 3:15 am telling me he had gone.”
– Bereaved family member |
8. Impact of the pandemic on the healthcare workforce |
 |
This chapter shares stories of the impact the pandemic had on the healthcare workforce. It focuses on how the pandemic affected healthcare workers’ mental health and workload, the availability of support, and access to professional development and training. It finishes by sharing some examples of the lasting impact on staff.
Patient deaths and supporting bereaved families
The pandemic resulted in large numbers of patient deaths, both among Covid-19 patients and those with other health conditions. Experiencing so many deaths had a huge emotional impact on many in the healthcare workforce who shared their stories with us.
| “ | I know that I see a lot of trauma a lot of the time, but this…was on a different kind of level. It was something that none of us had experienced. And everyone was sort of just winging their way through this situation, that no one really knew how to handle it, but we were trying our best.”
– Paramedic |
Many healthcare professionals lost family and close friends during the pandemic.
| “ | He took a wee turn in the house, and he had to go to A&E, and they were going to let him go home, and I had said, ‘Look, Daddy, the ward that I work in, they have a side room for you. You don’t have to wait to get your appointments for these tests. The doctor’s going to take you, and he’ll do the tests, the scans that you need, and you’ll just go and you’ll stay in the side room for a few days.’ So, he then agreed. He was in a side room. Four days later he tested positive for Covid-19, he never recovered fully; he never recovered, but the doctor then came to me and says, ‘We need to have this conversation about end-of-life care.’”
– Healthcare assistant |
Many contributors working in healthcare gave examples of how they treated and supported patients at the end of their lives and their loved ones in very difficult and stressful circumstances. Staff in these roles were often under huge pressure with overwhelming workloads. They often struggled to describe what they had seen and the impact that this had on them.
Marion’s storyMarion worked as a healthcare assistant during the pandemic, and she was new to the role. Her job involved monitoring patients and communicating with them and their loved ones. This meant that during the pandemic she would have to tell people that their loved one had died. Working in healthcare and being faced with patient’s passing away and grief among bereaved family and friends was new for Marion. The numbers of patients at the end of their lives made communicating with loved ones particularly difficult, as did restrictions on visitors. There were times when she would arrive at a patient’s room to learn that they had died that day, and it was not clear who should be told or how to reach them. “I think it felt difficult because for me with it being my first time working in healthcare, it was my first-time experiencing being a healthcare worker faced with a patient death. But I think it was compounded by the fact there was a sense of helplessness for anyone who was there.” Some of the most upsetting and difficult situations were when Marion had to tell people the person they were coming to visit had died. Due to restrictions on visitors, these people were often alone. She found it hard to know what to do to help people. “They were only allowed one visitor at a time. And so, I actually found the hardest thing was talking to them and hearing all their upset when their loved one who had died, they’d maybe not been able to say goodbye. They were trying to process this, but they didn’t have anyone else with them. So, that was all really hard emotionally to kind of take on, absorb and process.” |
It was particularly upsetting and distressing to watch the dramatic deterioration of Covid-19 patients who had otherwise been well before the pandemic. For some contributors, their fear of Covid-19 increased once they saw younger, healthier people dying.
| “ | Initially I didn’t have a big fear of it, and then we started to see younger deaths where you couldn’t quite apply the logic of chronic disease or anything else as an impact on their poor outcome. That became a lot more difficult.”
– A&E doctor |
Healthcare professionals who dealt with death shared how they responded in different ways. Contributors who had more experience often compared what happened during the pandemic with patient deaths they had seen previously. Some felt this experience helped them cope.
| “ | I’m really glad I’ve had the life experience I’ve had…because I think as a younger person, I couldn’t have coped with the stuff we were seeing and the amount of death and…trying to explain to the relatives of people who couldn’t come in that they weren’t going to come out.”
– A&E doctor |
But many contributors said they experienced damaging impacts on their mental health and wellbeing. Some shared how helpless they felt in the face of so many lives being lost. Adding to this, they were often afraid because they knew their jobs put them at greater risk of infection.
| “ | Lots of anxiety…I started smoking again due to the stress… I really struggled…I was tearful a lot. It almost felt quite manic trying to keep up…I had work-based counselling to help me deal with the emotional stresses”
– Healthcare professional |
Other contributors described detaching from the awful things they saw. Many told us they found it impossible to acknowledge and deal with their feelings at the time because of ongoing work pressures. Some shared how they still struggle to come to terms with what they saw.
| “ | We became immune to it. It dehumanised us a little bit, I think, at the time. I felt that, and I felt that was difficult to deal with.”
– GP practice manager |
| “ | We had patients that we saw regularly that had died from it, yes. That was shocking because it was so sad, because you build such a good relationship with your patients – and then to hear that one of them has gone because of Covid wasn’t nice… It’s just the feeling that you’ll never forget, just the shock of seeing that many people die…the shock and the disbelief and how bad that virus was.”
– GP nurse |
Some contributors described how their role required a level of directness with relatives that was hard for them emotionally. Some had to develop new ways of supporting dying patients and their families, which was outside their usual roles.
| “ | The job had just become so cold. And it wasn’t intentional, it had to be that way. You know, you couldn’t bend the rules, because people’s lives were in danger. So sometimes…you had to be quite blunt with them and that’s what upset me.”
– Paramedic |
| “ | We became more experienced in bereavement than we used to … I think our role basically increased, doing the bereavement counselling. But it’s not an easy role…I’d rather the bereavement counsellor do that.”
– GP |
Many contributors said families not being able to see their dying loved ones was one of the hardest things they had to cope with. Some tried their best to care for patients when their family were unable to visit them.
Patients not being with their families was very difficult for staff to deal with mentally and physically. Many shared how they took this away from work, finding it hard to separate these experiences from their personal lives.
| “ | It was like a war zone, overnight 18 people became Covid-19 positive with nowhere to isolate them. They were dropping like flies, it was awful. You can’t underestimate what this did to nursing staff, not being able to offer comfort to patients was soul destroying.”
– Nurse living with Long Covid |
Some contributors discussed how they, and their colleagues, mental and physical health was impacted. Contributors shared how difficult it was when a colleague passed away, they grieved them deeply even if they did not know them personally. There was a sense of unfairness that some healthcare workers died, and a concern for the devastating impact on their loved ones.
| “ | Just having to lose colleagues as well. We had colleagues who were extremely sick, some who passed away. It just changes morale, really. It makes everyone feel really upset. People feel like, why has this happened? It’s just something we’ll never really understand, to be honest.”
– GP nurse |
| “ | We lost a colleague to suicide towards the end of the pandemic. We will never know why they took their own life, but we know the pandemic had a significant impact on their mental health.”
– Healthcare professional |
One hospital porter shared how they lost a close friend and colleague who they felt likely died from catching Covid-19 while working at the hospital. Despite this, the hospital did not provide any support to the bereaved family. This led to the hospital porter questioning whether the risks of the job were worth it.
| “ | At that time, to be honest, I was thinking, like, do I want to be here? He caught it from the hospital, from the work he was doing…he got infected from there, but no one from the hospital had given any bit of support to his family, and that was the saddest part…they expect you to do so much, but after someone has just lost their life, you aren’t giving his family anything. A little bit of support or showing a bit of sympathy. Nothing.”
– Hospital porter |
The impact of adapting to the pandemic
The changes and pressures of the pandemic meant some healthcare professionals struggled to cope. Many contributors described a working life without routine and predictability. Some told us that a lack of clarity and transparency about the pandemic and their work made things worse, increasing stress and anxiety for many.
| “ | I like routine, I like being in control, I think as surgeons we all like being in control, it’s just the nature of the beast. And so to have two small children, a husband who is also a surgeon, also on an emergency rota, and literally waiting on a Sunday night for the week’s timetable to come out was just incredibly stressful. And it added additional unnecessary stress onto what was already obviously professionally incredibly stressful.”
– Surgeon |
Not all those who shared their experiences with us faced this constant pressure throughout the pandemic. However, some contributors referred to their workload as consistently overwhelming, and said it was impossible to deal with. We heard examples of staff that had to pick up extra work with no recognition, worked in teams that were short-staffed and under constant pressure, and were not able to take annual leave or breaks.
| “ | You get to a point where you’re doing extra shifts and you’re tired, and you’re thinking, oh, I’ve got a weekend off. What happened constantly, though, because people would keep going off, you were always getting contacted, ‘Any chance you could come in and do an extra shift?’ so effectively you were never off.”
– Hospital doctor |
| “ | It was really hard. I think you were rushed off your feet. Your breaks were reduced. You were hungry, you were tired. Then when you got home at night and knowing you’ve got to go and do it again, and you just, it’s kind of, it was a dread you felt, thinking, what am I walking into tomorrow? We’re like a wee family, so I think we did, well, as best we could when you were feeling low, just to try and keep others going”
– Hospital nurse |
Increased workloads and dealing with changes in their roles meant some healthcare staff neglected their own mental and physical health to prioritise patients. Many contributors shared how hard it was to look after themselves when they were overstretched and taking on extra shifts to cover gaps in care. It was often incredibly challenging to both look after their own wellbeing and provide the care patients needed.
| “ | You didn’t have time for having mental health issues, you just needed to get on with it because you were doing a job and you were, you felt like you were fighting for your own life every day.”
– A&E doctor |
To deal with the workload pressures, contributors told us how additional roles were created, staff from other teams volunteered to help, and bank and agency staff were used, often to cover staff sickness. Being paid extra for overtime, night shifts, or emergency shifts encouraged some staff to take on extra work, because they felt they were being properly recognised.
| “ | I know that we had a few pharmacists as a backup in case. Say someone called in and said they had symptoms or whatnot, then there was a group that were kind of on standby in a way. We knew which days they were free and weren’t free. We would try and bear that in mind, but thankfully we didn’t need to use that too much.”
– Hospital pharmacist |
However, in some cases, the staff brought in had little or no relevant experience and could do little to help. Where this happened, it often added to pressures on staff with the right skills, as they had to informally upskill these staff on the job. An example was recruiting firefighters to make up ambulance crews due to a shortage of ambulance workers and paramedics. The use of agency staff could also be unpredictable due to uncertainty about their skillset.
| “ | At one point we were offered a member of agency staff, but you would never really know what skills that agency staff would come with.”
– Hospital nurse |
Some contributors shared how it was also more difficult to find appropriate staff members with the suitable experience to cover absence when working in areas of speciality.
| “ | Some days you were short, you would try and get staff from other wards, but when you work in a speciality area, ward nurses aren’t able to help because they don’t understand the equipment or monitoring that we are used to. You can’t put them in a position. Then they’re also going to the wards, they were so short that they couldn’t come and help us anyway. You just, you had to do what you could.”
– Hospital nurse |
Healthcare professionals often shared how people catching Covid-19 had a big impact on their teams, as team members would not be able to work for days or weeks. This meant the size of teams, rotas and working hours changed quickly. This resulted in longer working hours for some.
| “ | There was a lack of staff because everybody was getting the virus themselves. So others ended up doing double shifts continuously because if they’re not there, there’s nobody there. Yes, so staffing was really lessened. Everybody was going off sick, so staffing was the hardest thing as well.”
– Allied healthcare professional |
The increase in workload due to staff absence led to even greater expectations being placed on remaining staff and fewer options to relieve the pressure.
| “ | There were definitely a lot of people off sick, people within the service that were shielding, so they instantly got, you know, pulled out and then the sickness started and the service was running with the bare minimum, you could definitely see a huge difference. It was really hard. Things were building up. It did become quite scary because, you know, there could’ve been points where there could’ve been nobody left but we just got on with it, there was no answer to it, there was nothing we could do.”
– Paramedic |
| “ | It was very challenging. It was challenging because we had to sometimes do a job where it was a 3, 4, or 5-person job, and one person had to take that role. Like I said to you, we were running, and it was so intense because they were short staffed, there were so many people going off ill, so many people going off with Covid-19. So, the intensity was on us, and it was, like, we had to take on that role as well.”
– Hospital healthcare assistant |
To respond to the unusually high levels of staff absence, approaches to staffing had to be changed. For example, some contributors talked about more flexibility being built into rotas. They said rotas were constantly changed due to staff having suspected Covid-19 symptoms or because they were unable to work for other reasons. This often happened at short notice.
Joe’s storyJoe worked as a practice manager for a GP. His practice shared buildings and facilities with four other practices. Before the pandemic, they had worked together where needed. His job involved co-ordinating services, organising GP and other healthcare staff, and being the point of call for emails coming into the practice. This meant he was directly involved in reorganising how they provided care during the pandemic, and also managed staffing. Joe’s practice faced problems with staff sickness throughout the pandemic. For Joe this was a major challenge and he had to spend considerable time making sure they could find enough cover. Each month they would have at least two members of the team off sick. This had a big impact on their small team. “It was just really bad. Every month I was reporting maybe 50, 60 sick days among staff. On average we might get two sick days a month – it was horrendous.” Joe had to cancel patient appointments, reorganise services and prioritise the patients who could receive care. He also supported colleagues facing mental health difficulties. This included one colleague who was off work for three months with anxiety. The pandemic was a very stressful time for Joe. He found it overwhelming managing patient and colleague expectations. “I had to manage a lot of people’s feelings and fears at work. Between that and staff sickness, you hadn’t time and the impact on my role, I was doing everybody else’s job bar the GP’s job really, because you just had to.” |
Many contributors shared how staff became increasingly exhausted and found it hard to deal with ongoing changes as the pandemic went on. Healthcare professionals told us that their routines and working patterns continued to change as the pandemic progressed. Many started to see more patients face-to-face, while also continuing with online appointments. Some of those who were relatively quiet during the early stages of the pandemic described working more hours, including extra shifts and more weekends.
| “ | We had to work 12-15 hour shifts regularly instead of the 6-hour shifts.”
– Allied healthcare professional |
Some contributors reflected on how staff responded differently to these ongoing pressures. There were some who were described as stepping up to fill gaps, and others who were seen by some as not doing enough. For example, some members of staff refused to work outside the area of speciality they were licensed for (as advised by the General Medical Council). The perception that some staff were not taking on the work they should, led to disappointment and resentment both between and within teams.
| “ | And there were some people who really stepped up. There’s a guy who was a relatively junior manager and he was really impressive taking control of the difficult situation, other people not so much. And there were many people who disappointingly used it to shirk responsibilities.”
– Hospital doctor |
| “ | We had two or three members of staff who decided they didn’t want to work in the hospital anymore, and just went on long-term sick because they didn’t want to take anything home to their families. That caused quite a bit of resentment within the department because obviously some people were having full pay for staying at home, whereas everybody else was going to work and working as a team.”
– Hospital pharmacist |
Staff motivation
Contributors often described how they felt a sense of purpose working in healthcare settings during the pandemic. Many said they were fortunate they were still able to go to work and do something meaningful. Their roles were important during a national health emergency.
| “ | You were helping other people. You actually were providing a service that was valuable. It made you feel proud of what you did.”
– Hospital pharmacist |
Many healthcare professionals found having a clarity of purpose at work helped to distract them from other worries and concerns, including the impact of the pandemic on them and their families. Some were even more positive about the structure and purpose their work during the pandemic gave them.
| “ | At Easter I was meant to have 4 days off, and they called me back after 2 days, and I was actually very happy to go because it’s quite tedious being at home with nothing to do either.”
– Hospital doctor |
Spending time with colleagues was also valuable for many healthcare professionals. As well as offering peer support in their roles, many found the social interaction available to them in healthcare settings helped them to cope. They knew not everyone was able to see people during the pandemic and did not take this for granted.
Some staff who were signed off from work or working from home during the pandemic spoke about how they felt they had let their team down. They found this particularly difficult because they knew their skills and expertise were needed.
| “ | Those first couple of weeks after the decision was made to work from home, I was devastated…I felt like I had let them down. I also in a way felt a little bit left out of, you know, this was the biggest thing to happen to health in my career, and I was going to be sidelined from it”
– A&E doctor |
However, some contributors thought that working collaboratively together across different parts of healthcare did not last. The stresses of the pandemic were described by many contributors as leading to increasingly tense working relationships. Some of this happened within individual healthcare settings or teams.
| “ | So I think, at the beginning, there was a nice, sort of, pulling together of everybody. And that was, sort of, nice and there was a lot of goodwill. I think that burnt out at the 3- or 4-month stage. But to start with, there was a lot of nice comradery.”
– Hospital doctor |
| “ | I think people were very focussed on one enemy, everybody pulled together and other things didn’t matter anymore, it was more about family. It shows that human beings are much better when they’ve got a common purpose and one thing they can focus on. And then as it went on, and became more fragmented, I think we went back to our more normal behaviours, and then it felt a bit of a letdown”
– Hospital doctor |
Some healthcare workers shared how it became more and more difficult to deal with the different waves of Covid-19. Staff were increasingly exhausted and struggling, but still working because they had to cover for colleagues who were unwell or self-isolating. Some contributors had growing frustrations that staff were not being properly recognised and compensated, particularly given the personal risks they took during the pandemic.
| “ | By the second year, the infrastructure, the staffing, the burnout was such that it really suffered. We were all so exhausted and I’ve never really met such a group of well-meaning humans as these…and yet, to see how little reserve was left and…there’s always someone sick and, you know, it’s really hard to be that person yourself as well, so no one goes off sick until they’re [an] absolute mess which is pretty awful too.”
– Hospital doctor |
Contributors largely felt supported by the public, particularly in the early stages of the pandemic. They shared examples of being treated with kindness and often felt held up as ‘heroes’. Many said patients and their families were understanding when things were taking longer than usual or when care moved to remote appointments. There was some fear too, with people worried about catching Covid-19 from those who worked in healthcare settings.
| “ | I think the general public were very supportive of healthcare workers, but also, I think they were very wary of you as well. Obviously, we didn’t go out in uniforms or anything but if you were – you could show your card to pop in the supermarket if you needed to jump the queue or something. Only if I was in a rush to get to work, I’d do that anyway, but nobody seemed to mind; they knew you needed to get to work and I think members of the public were very, very supportive.”
– Hospital pharmacist |
Some contributors reflected on the differences between how the public perceived the healthcare workforce and their own experiences of the pandemic.
| “ | That was the expectation of working there, like you should feel proud, you’re on the front line, you’re a soldier, you’re a hero…when in reality you wouldn’t say what’s going on behind closed doors. And I wouldn’t be necessarily proud of everything that I’d done, or the decisions that had to be made at the time because of lack of equipment or staffing or whatever.”
– Hospital nurse |
Helen’s storyHelen worked as a paramedic during the pandemic. She lives with her three children, close to her extended family. Helen shared how she felt her work was often misunderstood by the public and that these misunderstandings were worse during the pandemic. She said patients expected too much from paramedics and the medical and other help they could offer. For example, patients often expected paramedics to be able to treat them at home so they did not have to go to hospital. Many of the patients and families she came across during the pandemic were impatient, angry, and aggressive with her. She thought this was because of how scared they were. “The expectation on us, as healthcare workers, was unreal. And it’s almost like we were supposed to be superhuman, and not fall ill, know the answers to everything, encourage everyone, while we were feeling terrified ourselves.” While Helen appreciated being clapped for on Thursday nights, over time she grew to resent it. She did not feel that same warmth and appreciation in her interactions with patients. She also did not feel rewarded by her employer or the government for all the personal risks she was taking. “I had to try and get this balance in my mind, that the public don’t quite get what we do. So, they know that we are medical, they know that we can help to some degree, but they don’t quite know the details of our job… they expect you to be able to give them some kind of reassurance, some kind of treatment…because a lot of people we go to in general may not want to go to hospital. They said, I just want to be checked over, I can’t get through to my GP, or I can’t whatever. It’s like, that’s not what we’re here for. This is for if you’re in an accident, or if there’s an emergency going on. This is not an emergency.” |
Healthcare professionals faced the same personal challenges everyone in society did, and this added further pressure and stress. In the many of the stories they shared with us, the impact on their lives outside work were hugely important to their experience of the pandemic. For example, school closures placed huge pressure on those with children as they took on more responsibility for education, juggling this with work commitments. Others described taking on care for loved ones who were vulnerable or shielding.
| “ | The mental anguish, you tell yourself you have to park it, you have to get on for your family, for your children, everyone looks to you because you’re in healthcare, you have to hold it all together. I did feel for the children … you still have that guilt, but they [staff] were short, so I had to go in.”
– Children’s community nurse |
These pressures often added to problems with their mental health and wellbeing. One challenge that some contributors highlighted was how hard it was to have a clear distinction between their personal and work lives. For example, many were dealing with difficult and complex patient needs from home for the first time.
| “ | Working from home and dealing with clients with domestic abuse, substance abuse, dementia, it was so varied, it was difficult. It was difficult having these conversations at home where my daughter could overhear, and she wouldn’t understand why someone was crying/shouting at me.”
– Healthcare professional |
Training and skills
Across healthcare services in the UK there are statutory and mandatory training courses that healthcare professionals complete to ensure their knowledge and skills remain up to date. For example, healthcare professionals receive training on topics such as health, safety and welfare, infection prevention and control, moving and handling patients, resuscitation and safeguarding.
We heard how mandatory training stopped or relaxed in many healthcare settings to prioritise the Covid-19 response. There was an understanding among senior staff that compliance was not possible, particularly as staff were overworked. Training was not as much of a priority as the pandemic response – and this was welcomed by staff who were under strain.
| “ | Just having the mental capacity and the time to do those things was just absolutely not on the agenda…I suppose executive teams [knew] that that was the case. It was not on anyone’s agenda in that sort of firefighting time.”
– Hospital HR professional |
One contributor shared how mandatory training on resuscitation had not been run for two years and was only offered again in 2022. Others suggested that refresher training around things like infection control had not been delivered for several years.
| “ | Normally I would go to training in the evenings, and that was all stopped and there was none of that on, and there hasn’t really been much of that on now for three years.”
– GP nurse |
| “ | In the pandemic I think… a lot of that mandatory training and ensuring that the health and safety of employees was maintained, basically went out of the window.”
– Hospital laboratory staff |
However, other contributors shared how some mandatory training did continue. For some participants, including nurses, training was transferred online. For some professionals, their mandatory training was already available online, which meant there was no change to delivery.
| “ | The only mandatory training then was…all PPE and infection control, and that went on for over a year, maybe a year-and-a-half. That was the only training that was given, and from that, there was a lot of training that now has gone to e-learning. So, you complete the presentation online rather than face-to-face. It’s just slides that you look through online and you get a certificate at the end.”
– Healthcare assistant |
| “ | Yes, we did it all, and we’ve got very good online systems, so we were able – so online training…we obviously kept up with all the mandatory training, it didn’t slip…it was online already. The only one that’s usually face-to-face is the resuscitation, we’re back to face-to-face with that now, but we were able to do that online during the pandemic.”
– GP practice manager |
Much of the usual professional and personal development also stopped during the pandemic, with some expressing a potential impact on the safety of patients. Examples included training on administrative skills, customer service and one-off educational courses (i.e. those delivered by drug companies and representatives on hospital visits).
| “ | We would’ve had things like practice-based learning – those were gone for 2 years. New medical students didn’t get tutorials…we’d talk about clinical decisions informally, but doctors couldn’t be in the same room just in case one of them contracted Covid without knowing. Education took a back seat.”
– GP |
Contributors highlighted some gaps in training as everything moved online. For example, some junior staff missed out on core training due to working on a Covid-19 ward for a year without being rotated to other wards. One contributor shared that there was no training for student paramedics for similar reasons.
There were examples of cancelled training affecting progression. Some contributors were also worried that a lack of training for junior staff might reduce patient safety in future.
| “ | I remember vividly there were some courses I was expecting to attend, which I’d been waiting for 2 or 3 years. It was cancelled and then ultimately it was rescheduled for about a year, a year-and-a-half later. That may potentially have impacted my career progression.”
– Hospital doctor |
| “ | So, we were not allowed to teach any medical students that time. I think 1 or 2 batches came without being examined and I can tell you, as a patient, I would not like to be treated by any of them… just because it was a Covid period, identified as a medical emergency, you lower the bar so much that every person jumps over it. The doctors who have come around that time, they are unsafe to work with.”
– Hospital doctor |
There were different views among healthcare professionals about how good online training was. Some contributors felt online training was more accessible and easier to fit around a busy work schedule. Staff were also able to access recorded training at a later stage if they were unable to attend.
| “ | Some education became more accessible: there were big strategic meetings run by the local medical committee which were excellent – hundreds of GPs attended and there were updates on e.g. the vaccination…due to the time pressure the meetings became online – some were kept in person there has been this cultural change and greater accessibility to training and development, there was a lot more choice.”
– GP |
However, other contributors were more negative about online training during the pandemic. Some said that trainers had to be dynamic in the way training was delivered to encourage engagement, and that this did not always happen in a virtual setting.
They described how limited online training was for some topics, particularly those focused on more practical elements of healthcare. Examples included providing hands-on care to patients as well as interpersonal skills. For example, violence and aggression training usually involves contact between participants.
In-person training also offers benefits like being able to network and have informal conversations with colleagues. Some contributors said this was much more difficult to replicate online.
Carys’ storyCarys is a Nurse Prescriber at a GP practice. When the pandemic started, her practice quickly implemented a telephone triage system for people requesting appointments to minimise face-to-face contact and exposure to Covid-19. She was also responsible for prescribing medication over the phone. “It was challenging because we had no sort of training or preparation in how to deal with it. Whereas, usually patients would come into the surgery, and we would see them face-to-face, we had to adapt to being able to triage, which was something that most of us had never done before. GPs probably had done it, but we as nurses obviously hadn’t, so it was a difficult time to be able to manage people’s conditions. A lot of things could go amiss, because you can tell a lot by seeing a patient, and just speaking over the telephone, you can’t actually make that assessment.” She recalls preparation for this change in her role being very basic and ultimately, she had to adapt and learn on the job. GPs provided high-level guidance about being precise with the questions she asked, making note of red flags, and directing patients to 999 if the condition worsened. She was not provided with a template of questions to use. Carys emphasised the risk involved in assessing patients remotely and also acknowledged that she noticed herself improving over time. “So just assessing and adapting, like I say, to triage over the telephone, which I had no previous experience of, no training. You just had to get on with it, basically, so I felt there was a lot of support lacking at the time. Obviously the more we did it, the more we learnt from it, and the better we got at it.” |
Support for healthcare professionals
When healthcare professionals experienced distressing situations and workload pressures, contributors said there was often some support in place. For example, one contributor discussed how their employer had created ‘support hubs’ which encouraged people to take breaks throughout the day.
| “ | All of a sudden, we got two or three more of these admin slots, and they called them wellbeing slots actually. And I think it was designed just to give us a bit of downtime, a bit of a breather, and because everything was taking so long with patients to give us a bit of a time to catch up on notes and things like that.”
– Allied healthcare professional |
Healthcare workers gave examples of how the uncertainty and pressure worsened pre-existing mental health conditions, and increased anxiety and depression. Some contributors were able to access emotional and mental health support through their employers. This support was provided in a variety of ways, from online apps to telephone helplines or a set number of in person sessions with a therapist. Overall, contributors who accessed this support found it helpful.
| “ | We have a department in the Pharmaceutical Society where, if you need support, you can ring this number and somebody’s there to talk to you, even now. So, we do have that support line, because a lot of pharmacists are still under stress, working under stress even now, so those pharmacists who cannot cope but do have to work, they don’t want to leave, then they will speak to the support team.”
– Hospital pharmacist |
| “ | Mostly virtual but that was the case of most support available. I do think that was done relatively well, it did feel like there was support available and I think quite a few did access it.”
– Hospital nurse |
| “ | Lots of anxiety…I started smoking again due to the stress…I really struggled…I was tearful a lot. It almost felt quite manic trying to keep up with the latest rules as to what was happening, what we were allowed to do and what we couldn’t. I did go through a period where I had work-based counselling to help me deal with the emotional stresses.”
– GP practice manager |
Support from colleagues was considered particularly valuable during the pandemic.
| “ | We had a wee support group with all the other nurses who were trying to talk to one another and share our experiences. A couple of nurses gave up nursing because they’ve witnessed such horrible sights, so I think it was important to talk about it, of what we’d seen, just sharing experiences.”
– GP nurse |
However, support was not consistent, with some healthcare professionals not receiving the emotional and mental health support they needed. Others said that they were not aware what support was available, describing how communication could get lost in high-pressure environments.
| “ | I know there was support for staff if they required it, I didn’t know where you would access that if I indeed needed it.”
– Hospital nurse |
A few contributors felt that support was put in place without considering what would help staff the most. This caused frustration amongst these staff.
| “ | I feel that we kept getting told what the hospital were doing for staff and things, but I don’t think they ever asked the staff what would make a difference to being at work. I think it was also the little things, like they would have said being able to park…being able to go for lunch in a chillout space.”
– Hospital doctor |
Some other contributors said the support they received during the pandemic was dependent on their line manager and the culture of the organisations they worked in.
| “ | My line manager, she’s the best one I’ve ever had. Encouraging, understanding, supportive, yes. So, further on up the line, yes, everybody seemed to be doing what they could to support everybody.”
– Clinical scientist |
We heard some specific examples of line managers working from home for much of the pandemic. This led to contributors feeling unsupported with day-to-day tasks and issues.
| “ | My manager was working from home, so she couldn’t really support me and my colleagues that were working. She wanted to work from home herself. I used to find it irritating and unsupportive from my manager…really, we should have all just carried on doing our role like we were.”
– Allied healthcare professional |
Lasting impact of the pandemic
Many contributors shared how detrimental the pandemic was to their mental health. Some felt they had moved on, but healthcare professionals often told us they were still processing what had happened to them. These contributors reflected on their traumatic memories of delivering care during the pandemic.
| “ | I don’t think I’ve come back to 100% of how I normally was. It takes its toll. But it’s almost like having this piece of paper, that’s nice, and flat, and straight, and then you’ve crumpled it and then you try and straighten out that piece of paper again. It’s still creased up, no matter how much you try and straighten it out.”
– Paramedic |
| “ | It had a big impact actually…we couldn’t resolve a lot of issues. Our particular hospital had a big problem with the number of deaths that we were having, which was sometimes about 80 a day, and because we’re like quite a small flagship hospital really, we couldn’t store the bodies. We had to bring in a massive, big freezer unit, which was just humongous, just to put these bodies in. I’ve never, ever seen anything like that. Just to like go up and see the bodies lined up in the corridor was quite – yes, it was emotional. It was like quite devastating to just see, it continues to have an impact on me.”
– Hospital nurse |
We heard some examples of professionals who had faced difficulties in their lives such as drinking too much or going through divorce. Some of these contributors thought their experiences were at least partly due to the pandemic.
| “ | Healthwise, it’s certainly because of the onset of my drinking [which started in the pandemic] that my health hasn’t been too good. I’ve got a fatty liver which alcohol has a knock-on effect with a lot of things.”
– GP |
| “ | We started a journey of separation and coming to a divorce now. Would that have happened without the pandemic? I don’t know, to be honest. I might not have had the bravery to do it.”
– GP practice manager |
Sadly, some healthcare professionals told us about experiencing psychological crisis during the pandemic, which they were continuing to recover from.
| “ | Working in a Covid-19 ICU, I had a complete breakdown at work. I didn’t see it coming. My colleagues said that they did actually see it coming. I was getting very anxious and almost angry, like, well I was considered one of the most experienced nurses in the Unit, so any of the big cases that were coming through I worked on, I loved looking after, when there was a lot going on I liked being there and getting organised. But all of a sudden, I went into this complete downward spiral, and it happened over about 2 weeks, I think, and got to the point where I just burst into tears on the Unit. I just cried and cried and cried.”
– A&E nurse |
Learning for the future: support for professionalsWhile there were different experiences across the workforce, many healthcare professionals told us about the immense pressure they were under during the pandemic. This had a damaging impact on many, and particularly on their mental health. They argued lessons needed to be learned about supporting and valuing healthcare professionals. Some wanted the government and healthcare systems to do more to support and reward staff, recognising the lasting impact of a crisis like the pandemic. Others wanted the public to appreciate the pressures healthcare professionals are still facing. “Appreciate the staff, the different healthcare professionals, not just when you need them. Appreciate what they can do, because from where I’m standing, the NHS is actually falling apart, and it needs support. Staff are drained. They’ve got nothing to give, and there needs to be a solution.” Pharmacist “It was just the attitude that changed when people became more demanding and I think they put off things in the pandemic and they wanted to be seen, and they wanted to be seen now… [they are] certainly less sympathetic that you were there doing your job in a time of risk, really.” GP nurse Some contributors argued that there should be better support for mental health and wellbeing for healthcare staff in future pandemics. Some contributors argued for more robust mental health support within healthcare, particularly during heightened demand. They recommended prioritising mental health resources, offering counselling services, and creating a supportive environment to address the immense emotional toll faced by healthcare workers in different roles. “I think more publicised support could have [been] offered for the mental health aftermath of the impact of Covid on ICU nurses. I have had counselling through the RCN, but only because I came upon it on social media. We are still suffering.” Every Story Matters contributor “I am still saddened that the NHS does not offer free counselling to staff who have an element of PTSD from the pandemic. We have to pay privately to get any support, however, my colleagues and I are often priced out as private mental health support is very expensive.” Every Story Matters contributor “The NHS needed more mental health support at the time. ‘Front line workers’ got special treatment in departments like A&E and critical care, but the wards within the hospital were also fighting the same battle. We were given fruit baskets and cereal bars when we should have been having regular debriefs and therapy.” Every Story Matters contributor |
9. Experiences of end-of-life care and bereavement |
 |
This chapter outlines experiences of bereavement and healthcare during the pandemic. It includes the experiences of bereaved families, covering how challenging it was to communicate with healthcare professionals and not being able to visit dying loved ones or visits being restricted. It also shares experiences of how end-of-life care was managed, including DNACPR notices.
Families’ experiences of end-of-life care
Bereaved families, friends and colleagues shared how their traumatic experiences of their loved ones dying in hospital during the pandemic mean that they feel deep sadness – and often guilt or anger – that is hard to move beyond.
| “ | I lost my father in November 2021 from Covid-19. He was 65 years old. He had six children, five grandchildren, with a further two joining our family since he left us. He died within six days of a hospital admission. I am still haunted by the thought of hospitals and the fear and pain he must have felt.”
– Bereaved family member |
| “ | We’ve lost faith and trust in the healthcare system. We need to have our voices heard…I’m living with guilt for things we could have done to prevent their [parents’] deaths.”
– Bereaved family member |
Not being able to spend time with their loved one and say goodbye properly means it is much more difficult to come to terms with their loss. They shared the pain and anxiety they felt at not being able to offer comfort, support and advocacy because of pandemic restrictions. Many bereaved families and friends told us how distressing it still is to think of their loved ones not understanding why their family and friends were not with them.
| “ | I cannot move beyond my trauma, I cannot move through this grief…my father died from the effects of isolation, from the heartbreak of not being able to see his wife and family, from the lack of care and love he should have so rightfully received.”
– Bereaved family member |
| “ | I felt awful, absolutely heartbroken because I knew, as much as she probably was poorly, more of that was suffering with not seeing us. I could tell it was more of that, so it was heartbreaking to know that she was there…we were here, me and my daughter and my aunties… It just felt like, ‘We’re not going to see her again.’’
– Bereaved family member |
We heard how many bereaved families and friends thought their loved one felt abandoned in hospital. They shared examples of healthcare professionals not responding to patients despite them calling for help. Bereaved people are understandably angry, shocked and disappointed that their loved ones did not receive the care they needed in their final days.
| “ | There’s been about 6 or 7 instances where he texted us to say goodbye. We would try and phone or text back but, you know, his texts, because he couldn’t hold his phone very well, were often a little bit confusing to us. The other thing was he was so weak at times, he couldn’t pick up his phone…he’s bedridden, he can’t move…he can’t access any forms of communication and they [healthcare professionals] were so busy when often he would press the bell, and nobody would come.”
– Bereaved family member |
There were also bereaved families and friends who described their loved one receiving poor care and said they believed this had contributed to their death. Although they often recognised the pressures on healthcare professionals, they wanted better care for their loved ones. Some contributors said they felt guilty that they were not able to advocate more on their behalf. This made it more difficult for bereaved families and friends to come to terms with their loss.
| “ | We lost my dad for 36 hours [in the hospital]; he was taken here and there and left for hours alone parked in an ambulance with no food or water.”
– Bereaved family member |
| “ | I held her [grandmother’s] hand and she said, ‘I thought you had left me, and I was so scared.’ I said, ‘we’ve been trying to get you home.’ She came home on the Wednesday, and she died on the Sunday. She had literally been left. She was covered in bedsores, on her feet, on her bum. She obviously hadn’t been eating. She obviously hadn’t been drinking. It was horrendous.”
– Bereaved family member |
| “ | They moved him to a Covid-19 ward, on day 4 he didn’t see anybody all day. His catheter was blocked, he had no help, ringing me in tears to tell me the nurse said they didn’t have saline to wash him out. I rang at midnight and the nurse said, ‘what do you want me to do about it?’.”
– Bereaved family member |
The stories shared with us by bereaved loved ones also include examples of healthcare professionals offering excellent and innovative end-of-life care during the pandemic. These families described how supportive staff were and how much this improved their loved ones’ end-of-life care. One common example was health professionals breaking Covid-19 guidance to provide physical comfort while the patient was dying.
| “ | I remember, one nurse was like, ‘Oh, your dad wanted me to give you a hug, and say, “Here’s a hug.”‘ Obviously, she didn’t need to do that…You’re not even meant to be getting that close, but just that kind of humane feeling, and I was just like, oh my God, that is just so refreshing to see in a medical person.”
– Bereaved family member |
| “ | I got a phone call to say she didn’t have long and did I want to video call again. Of course, I did, and this time Dad spoke to her via the phone against the laptop. I was on the call for a long time and could see the care she was getting from the amazing nursing staff.”
– Bereaved family member |
Other contributors shared how healthcare professionals were very caring towards bereaved loved ones and reflected on how traumatic it was for staff caring for patients coming to the end of their lives.
| “ | The nurse looked at me, could only see her eyes above the mask, and asked if I was ok and I said, ‘are you ok? You’re looking after them and spending the last 30 mins of their life with them.’ My concern was for nurses who have to experience that trauma and carry on with it.”
– Bereaved family member |
Communication during end-of-life care
Many of the bereaved people we heard from said they did not receive clear explanations from healthcare professionals about what was happening at the end of their loved ones’ lives. This has made their difficult experience of loss even more stressful and upsetting.
| “ | We were terrified not knowing what was happening. I do feel like we could have been informed more throughout the whole process of what was happening.”
– Bereaved family member |
These experiences were more common early in the pandemic, when many said they were unable to find out what was happening with their family members. This lack of communication also meant they were not involved in decisions about their care.
| Stories from bereaved people
Bereaved people at an Every Story Matters listening event spoke about problems communicating with healthcare professionals caring for their loved ones. They described many difficulties trying to contact their loved ones or find out what was happening to them. This included delays receiving updates about their loved one’s condition, treatment plans and decisions. This left bereaved families feeling anxious and uninformed. “The communication and everything was terrible. Shortly before my daddy died we were getting good reports then suddenly they said it was time to get the family together.” Bereaved family member These bereaved families wanted more transparent communication and to be more involved in the care process. “We weren’t allowed to provide any insight to help with their care. If we’d been allowed to visit my daddy we would have known he was not fit to be sent home. Had we been able to visit my mummy we would have been able to pick up on things before it was too late.” Bereaved family member |
Some contributors described how hard it was to contact healthcare professionals when they wanted to send personal supplies or share final messages with their loved ones.
Phillipa and Alice’s storyPhillipa told us about the heartbreaking circumstances around the death of her beloved 95-year-old grandmother Alice. Alice had lived with Phillipa for five years before the pandemic The two women shared an incredibly close bond – Philippa told us that Alice was not just her grandmother, but one of her best friends and inspirations. When the pandemic hit, Phillipa and Alice shielded together. One day Alice fell, severely cutting her leg. Despite Phillipa’s efforts to stop the bleeding, an ambulance was called, and Alice was taken to hospital against Phillipa’s wishes. She had wanted to care for her grandmother at home given the risks of going to hospital at the time. For the next four weeks Phillipa felt that Alice became lost in the overcrowded, understaffed hospital. Phillipa and other family members called daily to find out what was happening to Alice and to try and get her home. In the meantime, Alice contracted Covid-19 in the hospital. When Alice was finally allowed to come home, Phillipa was shocked at her condition – she had lost weight and was covered in bedsores. Alice passed away just a few days later. Phillipa is haunted by the loneliness, fear and pain Alice must have experienced. She feels the hospital neglected and ultimately killed her grandmother. “I’m just so annoyed that somebody thought they had the right to keep my grandmother, my own flesh and blood, away from us. We couldn’t go and see her, and we couldn’t find her. She felt as if we had left her, as if we had just abandoned her.” The damage to Phillipa’s mental and physical health has been profound. She struggles with feeling low in mood, anxious about leaving the house and hopeless. “It’s left me with a terrible grudge, chip on my shoulder…that somebody can take the most precious things in your life, your loved ones, and keep them, as if they have the right to make that decision. I was lucky, I got my nan home, but they killed her…I know Covid-19 was bad, but they put Covid-19 down as her death and her death wasn’t Covid-19. Her death was the hospital that killed her.” |
Many bereaved families and friends said they had no contact, or contact by video call only, with loved ones and thought more could have been done to help them say goodbye. Many stories described how only one person), or only immediate family could speak to a dying patient on the phone or via a video call. This meant other relatives did not have conversations with their loved ones. Bereaved families told us they thought this could have been managed better. They often shared how more family members being able to speak to their loved ones would have helped them grieve.
| “ | ‘Oh it’s only immediate family. Only immediate family.’ But this is end-of-life care you’re giving. I can understand if you’ve got 100 patients in there, you don’t have the time to FaceTime everybody, but it’s end-of-life care. Even if you limit it to a 5-minute FaceTime, you should be able to find the time for that, but it wasn’t straightforward at all.”
– Bereaved family member |
Bereaved families and friends thought that video calls should have happened consistently. Some wanted more compassion from healthcare professionals and greater flexibility in guidelines to enable this to happen.
| “ | [My dad] was in hospital for 7 days and then I had a telephone call from the ward saying he was not able to tolerate the CPAP machine anymore. I was able to speak to him on the phone, but they did not have tablets to make video calls, so I was unable to see him even on a video. He died later that evening on the 11th April with no family around him.”
– Bereaved family member |
| “ | I know [my uncle’s] daughter was allowed to FaceTime but that was awful, and it reached a point where I didn’t even go to the funeral because I was so upset, and I couldn’t get the closure I needed. I know my mum was really upset with me, but I said, ‘I can’t go to the funeral. I just can’t do it…’”
– Bereaved family member |
| “ | My mother was lying on a bed with something out of space standing by her [staff in PPE], she was being told to wave to her family on an iPad, she waved like a child and the zoom call ended. The doctor told her she’s not going to wake up again, so she waved so hard to say goodbye to her family. I couldn’t believe the doctors told her that, that she wouldn’t wake up after the ventilator. We watched our mother on an iPad on a ventilator dying.”
– Bereaved family member |
Many bereaved families and friends shared how worried they were about their loved ones being isolated and confused. Some shared stories about patients not being able to use technology to stay in touch.
Visiting to say goodbye
Bereaved people found it deeply distressing and heartbreaking when they could not visit their loved ones. The stories shared highlight how guidance for hospital visits were inconsistent and changed during the pandemic. They varied from hospital to hospital, between hospital departments, and were applied differently by staff. Contributors often felt the guidance in place lacked compassion and should have been implemented with greater sensitivity and flexibility.
| “ | When someone is known to be dying, it feels inhumane and callous, for both the dying person and their family, to be forbidden to visit. The death of a family member is an exceptional moment in life. It is my sincere hope that there will be procedures in place to allow visiting in any future situations.”
– Bereaved family member |
| “ | I think older people not seeing their wives, etc – all of that, I think that was horrendous, and I think there was a way round that. Get them [visitors] tested and let them go in. I think that was one of the big mistakes, personally from my point of view.”
– Friend of Covid-19 patient |
In some cases, families reported being allowed to visit as an exception or as the restrictions on visiting eased.
| “ | I saw my mum the day before she died, and the hospital let me in to see her because she was in a room on her own…I got the impression that they were making an exception because of the circumstances my mum was in.”
– Bereaved family member |
Often, only one person was allowed to visit, or numbers were severely restricted. Those who shared these experiences told us how unthinkable it was to have to decide who should visit. In some cases, this led to conflict and divisions within families.
| “ | Unfortunately, my husband took a turn for the worse. We were called to the hospital as there was nothing more they could do. I have 4 children who wanted to see their dad but that was not allowed. Only my eldest son could be with me, which was upsetting they had to say their goodbyes by an iPad in the car park in the hospital.”
– Bereaved family member |
| “ | They were basically telling us, ‘He’s not going to survive.’ And then, we were told that only one of us was allowed to go see him because they only had one designated visitor. So that was really difficult, because who does it?”
– Bereaved family member |
Some of the stories described how people had to wear PPE to visit dying loved ones. We heard about the heartbreak of not being able to physically touch those they were visiting. Contributors also reported older parents with dementia being afraid because their relatives were wearing PPE.
| “ | My daughter and I were allowed to go and see him [husband], after going through several steps to put on PPE equipment. We were told that although he was unconscious, he probably could hear us, and we talked to him, but it broke my heart that I couldn’t hold him in my arms. I could hold his hand and stroke his face, but it wasn’t the same having to wear gloves.”
– Bereaved family member |
| “ | My father, a dementia care patient…was frightened, and he was terrified, he thought he was in a mental home. I mean, from his perception, all he could see was people walking around like space suits, you know? And no-one could explain to him because his mind was already at the stage where rational thought wasn’t there anymore.”
– Bereaved family member |
Experiences of DNACPR notices
Do not attempt cardiopulmonary resuscitation (DNACPR) notices are medical recommendations written by a doctor. They recommend that healthcare professionals should not attempt cardiopulmonary resuscitation if a patient stops breathing or their heart stops beating. These are sometimes called DNR (do not resuscitate) or DNAR (do not attempt resuscitation). This is different to a treatment escalation plan, which is put in place to help record and communicate the goals of treatment when someone is coming towards the end of their life.
We heard how some patients discussed DNACPR notices themselves, but others relied on those closest to them. This highlighted the importance of loved ones being involved early in discussions about DNACPR notices. Difficulties getting through to the relevant healthcare professionals made this more challenging. Some bereaved families and friends were frightened and worried about what would happen if they could not advocate for their loved one.
| “ | It was the most frightening time for myself and my family as we all thought I was going to die considering my serious respiratory issues. I feel that the hospital could have liaised more with my son and daughter especially regarding the DNR as I was not well enough to make such a momentous decision at that time.”
– Patient hospitalised with Covid-19 |
We heard how some people only discovered that a DNACPR notice had been put in place after their loved one died, or after they were discharged from hospital.
| “ | We didn’t know he had a DNR…and my mum had power of attorney…The only reason we know is because when he was discharged, it was in his pack. But the fact that we weren’t involved in the decision and knowing that dad’s got Alzheimer’s. It kind of felt like they were throwing away old people. It was like they’re not a priority because they’re old.”
– Carer of a Covid-19 patient |
| “ | My mummy’s first consultant [in hospital] incorrectly put my dad’s notes [from his Covid-19 admission] to hers and put on a DNACPR – we were not informed of this, we weren’t asked to clarify her medical history, we were completely oblivious, totally unaware of the consequences on her treatment.”
– Bereaved family member |
Bereaved families shared how they believe that old age or existing health conditions led to healthcare professionals putting a DNACPR notice in place.
| “ | A consultant called to say he [husband with dementia and Covid] was really ill [after a fall in hospital], I couldn’t understand why, he was physically strong, the consultant said, ‘you can argue if you like I’ve made a decision’, he has since apologised to me. I asked if the dementia diagnosis affected the decision [DNACPR] and he didn’t give a reply.”
– Bereaved family member |
Recommending DNACPRs without discussing them with loved ones was seen as particularly inappropriate where patients had limited capacity. This included where relatives had lasting power of attorney. These experiences were more common among relatives of older and disabled people.
| “ | I got a voice message from the registrar telling me mum had sepsis and they put a DNR on her. I said I have power of attorney, but they said we need to see a copy of this before discussing anything. I then had to get in touch with solicitor, which was shut, to get a copy printed. I went to hospital and made them remove the DNR and said you can’t do this without my consent, but they said we can, because she is over the age of 60. They talked about her quality of life, she has a very good quality of life, she has grandkids! How do you decide who lives and who dies?”
– Bereaved family member |
| “ | On another stay in hospital, despite being deaf, not having any hearing aid in or with her and being unable to speak due to being a stroke survivor, a DNR was put in place without any communication with her or any family member present. I clearly said NO over the phone and it was totally ignored.”
– Carer |
Some loved ones felt pressured to agree with the DNACPR decision. They pointed to the media coverage of Covid-19, and the fear this created. At the time the media emphasised how dangerous Covid-19 was for some types of people, and how much pressure healthcare systems were under. Some contributors shared how this meant patients often had little hope of recovering from the disease, particularly if they were older or had pre-existing health conditions. Some families said their loved ones agreed to DNACPRs when they believe that they should not have done.
| “ | Part of you wishes that, if it wasn’t Covid-19, and that happened [grandfather became ill], would he have done that [agreed to DNR]? Would he have said, ‘I don’t want to be brought back’? But if it was just, he was ill, at 69, then the hospital would have done everything they could. They wouldn’t say, ‘Oh, we’re withholding any treatment.’ They’d keep fighting.”
– Bereaved family member |
| “ | You were pushed into it [signing a DNACPR notice]. I think it was because he was a certain age and had certain health conditions, they decided it. Don’t get me wrong, he probably would have wanted a DNR anyway, but he was pushed into it by doctors and nurses, 100%.”
– Bereaved family member |
DNACPR decisions were made differently depending on circumstances. Slower decision-making offered more time for patients and relatives to process the decision and what it meant. Examples of this usually happened at home or with the help of GPs. When this happened, some bereaved families told us they found they were better able to cope with their loss as time had been taken to consider the decision fully.
| “ | We knew that from the offset [a decision on DNR had already been taken]. So, then when he was hospitalised, the doctor said, ‘Look, do you need to put a DNR in place, or whatever.’ So, we did because that’s what he wanted.”
– Bereaved family member |
| “ | We believe that’s what grandma would have wanted because she had dementia at that point, but she’s always said, ‘I’ve had my life, I’ve had a good innings, and when I go…’ she just wants to go. She doesn’t want to hang around. So, we talked about that.”
– Bereaved family member |
Some contributors blamed technical language for confusion about what DNACPR notices meant for them and their loved ones. This increased misunderstandings and could result in unanswered questions about how these were applied.
Noor’s storyDuring the pandemic, Noor’s father was admitted to hospital because of his existing health conditions. While he was there, Noor and her family received an unexpected and rushed call from a doctor about DNACPR. The conversation caused great confusion and stress. The greatest shock was how quickly things progressed – from him being admitted to a DNACPR being discussed. The medical language used to describe her father’s situation added to the confusion. Noor felt it contributed to her mother having a poorly informed conversation about applying DNACPR to Noor’s father. This was something she wanted to change quickly. She also felt the way healthcare professionals explained things made it difficult to understand how they had come to recommend a DNACPR. “Someone must have spouted, like, do you want a DNR on your husband, and my mum was like, yes. But then she must have rung me or my brother, and I remember her telling us. ‘Oh, they called me and said, ‘Do you want a DNR?’ so I said yes.’ We were like, ‘Do you even know what a DNR is?’ and she was like, ‘No, I don’t know, but I just said yes because I assumed it was some sort of treatment. We had to get straight back on the phone.” Noor found the experience of DNACPR decision-making extremely difficult. It was particularly upsetting to be asked repeatedly about whether her father should be resuscitated if the occasion arose. This happened each of the five times he was transferred to a different ward. Her father was also asked each time. While recognising the pressures on hospital staff at the time, she felt discussions were handled very insensitively. She is still afraid when her father is admitted to hospital now. “We’ve explicitly said we do not want a DNR five times. It just takes one person to make that slip-up that could have cost someone’s life. I just thought to myself, imagine if we weren’t, like, on top of it. Can you imagine? So now, I’m just scared every time dad goes in.” |
Despite the challenges, many relatives told us they continued to play an important role in end-of-life care decisions during the pandemic. The pressure on services made families feel like their role as an advocate was especially important.
This need for advocacy was particularly important when it came to discussions about DNACPR notices. Many contributors with dying loved ones said they wanted to remain involved in healthcare decisions about their care, particularly for those who were vulnerable and less able to advocate for themselves. Some bereaved families were concerned that their other treatment options should have been considered before DNACPR notices were applied.
Learning for the future: bereavement and end-of-life careWe heard from many bereaved people who wanted lessons to be learned from the harm that was done when their loved ones died during the pandemic. Many called for more empathy and compassion for those who were vulnerable in hospitals and other healthcare settings. They wanted more recognition of and consultation with families and other carers, and better support and communication to reflect this. “There should have been better communication with families about their loved ones and we should have had the chance to say goodbye.” Every Story Matters contributor “A more strategic approach to recognising and very explicitly thinking about these areas of care, palliative end of life, bereavement but [also] visiting for families.” Palliative care staff Some contributors said that preventing loved ones from visiting dying patients simply should not have happened. Many argued for a different approach in the future that allowed visits during end-of-life care, or for people to die at home with their loved ones. This would offer more compassion to patients and their families. “Please think about vulnerable people in hospitals and care homes. If this happens again, please think about the family. We needed them and they needed us. We were denied that.” Bereaved family member “At least one family member should have been allowed to sit with a dying relative (in PPE), no one should die alone in the 21st century.” Every Story Matters contributor “Looking at the handling of the process of ending of the patient’s life in such a situation, taking into account the lasting effect on close relatives, (which may lead later to a need for treatment), perhaps having a trained person who makes that difficult phone call and meets the family at the hospital, is available to be with them at the crucial moment and offers support afterwards.” Every Story Matters contributor Contributors also wanted a more compassionate protocol for discussing DNACPR notices with patients and their loved ones. They wanted to see more open communication with family and other carers, especially for patients who had limited capacity to make their own decisions. They also wanted more support after difficult decisions were made. |
10. Long Covid |
 |
This chapter shares the stories of people living with Long Covid. Long Covid is a set of long-term health conditions and symptoms some people develop after being infected with the Covid-19 virus. The chapter begins by exploring people’s health before and after contracting Covid-19. It then moves on to sharing people’s experiences of diagnosis and trying to access health services, necessary support and advice, as well as the ongoing impact of Long Covid.
People’s lives and wellbeing before and after contracting Covid-19
Contributors with Long Covid often started their stories by comparing their health before and after catching Covid-19. Many described their lives before the pandemic as healthy and active. They frequently worked full time and had busy social lives. Developing Long Covid meant many had to completely re-evaluate their lives, their identity and their future plans. For some, this meant a complete change in identity and how they imagined their life could be in the future.
| “ | It’s a big identity crisis; my mum and I were fit, active people, I was meant to be beginning pro-ballet as a career, to go from that to being in bed all the time is massive, at a young age difficult as you are finding out who you are. I’m 18 and still don’t know who I am, four years later. It’s an identity I don’t want.”
– Young person living with Long Covid |
| “ | I managed a bar, about 60 staff…I used to run regularly, marathons, half marathons. I was a really keen runner. But now since Covid-19 I can barely get around the park.”
– Person living with Long Covid |
Other contributors said they had poor health before catching Covid-19. This included pre-existing health conditions such as asthma, obesity and migraines. In some cases, when contributors developed Long Covid, their pre-existing conditions made it more difficult to identify the cause of their symptoms.
Generally, contributors said their experience of Long Covid started after they knew they had caught Covid-19. This usually began with Covid-19 symptoms lasting much longer than expected. Symptoms would then change and develop as time went on. For those who developed Long Covid early on in the pandemic, this was a difficult and frightening time as little was known about the disease. Other people were not aware of ever catching Covid-19. They felt confused, unsure and frustrated about their health.
| “ | As far [as] I know, I never had Covid-19, I have never been diagnosed with it. However, I firmly believe I must have had it. Since February [2021] I haven’t been right health-wise, and I do have underlying health issues anyway, but I now have breathing issues [and other ongoing health issues].
– Person living with Long Covid |
Long Covid symptoms and the severity of those symptoms changed over time. Contributors described a variety of symptoms related to Long Covid, including:
- Difficulties breathing and low oxygen levels.
- Continuous sore throat and cough.
- Regular infections.
- Reduced mobility.
- Headaches and poor eyesight.
- Continuous aches and pains.
- Fatigue, confusion and ‘brain fog’.
| “ | Just sitting here, I would start wheezing and be unable to breathe. I had to buy an oximeter to keep on my finger and my oxygen levels were 85 and I looked it up on the NHS website and it said, ‘Call an ambulance if it gets below 95.’…I would get random infections on my fingers; I’ve become allergic to things that I was never allergic to before. Both my ears are completely compacted.”
– Person living with Long Covid |
| “ | My eyes have been a big thing. I’ve felt a lot of pain in my eyes that I never had before. I find it very difficult to see. I would get styes in my eyes that I never would’ve had before.”
– Person living with Long Covid |
Many shared how the type and severity of their symptoms kept changing. Some contributors said Long Covid could feel like a ‘moving target’ that was difficult to predict. This was often very damaging for their mental health, with many feelings exhausted, frustrated and demoralised. It often made it difficult to get out of bed or even or carry out simple day-to-day activities.
| “ | I had cracking pain and different things like that, and it would be peaks and troughs… it just kept being like that, so I would say for at least 9 months, I couldn’t do anything. I could barely get out of my bed. Then I started to have more longer spells of being better and I’d think I was over it again and I’d be out of my bed. I’m back at work…doing much better but I’ve got to pace myself…because I could go right back.”
– Person living with Long Covid |
Pathways to diagnosis and treatment of Long Covid
Contributors found it difficult to understand what was happening to their health as very little was known about the condition at the start of the pandemic. Many looked for information and support, often starting with online searches or by calling NHS 111 or its equivalent. Others spoke to their GP or other healthcare services to try and work out the reasons for their symptoms and find treatment. Early in the pandemic, contributors living with Long Covid said it was challenging to find any information, advice or treatment guidance.
This was all incredibly stressful for people with Long Covid. Many told us how they were panicked and anxious because they did not know what was happening and could not get the help they needed.
| “ | I spoke to my GP and at the same time I was in contact with the community mental health…that’s where we sort of discussed Long Covid because of the fatigue issues. But there wasn’t a lot available at the time.”
– Person living with Long Covid |
Some contributors with Long Covid shared how they felt their GPs were uninterested in their symptoms or did not believe them. When this happened, contributors often felt abandoned and helpless, and unsure where to turn.
| “ | We had GPs refusing to believe in Long Covid, with many others not getting testing for symptoms.”
– Person living with Long Covid |
Frustration with healthcare professionals was also reflected in listening events.
Stories from people with Long CovidContributors at Every Story Matters listening events shared how they experienced a significant gap in medical understanding, research, and treatment, leading to frustration, disappointment, and anger. “It was like I had 50 different diagnoses, but 50 things left undiagnosed with no treatments, cure or help.” Person living with Long Covid They reported dismissive attitudes from healthcare professionals. One contributor, after months of bed rest and isolation, received only a cursory check of their vital signs before being dismissed by their GP. “After 6/7 months of bed rest and no socialising we finally got a GP appointment, and he gave me a once over of my vitals and said he doesn’t know anything about Long Covid, signed me off and that was it.” Person living with Long Covid |
By contrast, those who received help from their GP appreciated the care they received.
| “ | I was so fortunate, my GP listened, they actually cared, which sounds silly because that’s their job. I can’t believe GPs are still telling people there’s no such thing as Long Covid.”
– Person living with Long Covid |
Across the stories shared, the issue of diagnosis and support seems to have improved slowly as the pandemic progressed. However, many have continued to find treatment, support and advice very poor, with little or no help available for them.
| “ | I’ve been passed around specialties, from pillar to post, waiting two years for cardiology, I do not know where to turn.”
– Person living with Long Covid |
Many contributors with Long Covid told us they found it difficult to get a diagnosis and were frustrated and exasperated by the process. Contributors were usually diagnosed with Long Covid after a process of elimination. They would often have to go through a series of tests and assessments to rule out other health conditions. Although this is standard clinical practice for most health conditions, it added to the anxiety, stress and worry they felt. It could also contribute to further feelings of exhaustion, and worsen symptoms, as contributors navigated through the healthcare system and made their case for treatment to healthcare professionals.
Those who shared their stories often waited for a long time with serious health issues that no one could explain to them. Some described how healthcare professionals repeatedly dismissed their illness, further compounding their distress.
| “ | When I left the GP, I was destroyed, I got home and couldn’t speak. I’ve been rejected from haematology, cardiology, infectious diseases, the list goes on. My husband said, ‘I don’t know why you go through the GP or NHS’.”
– Person living with Long Covid |
| “ | I was unwell for a while, so I called [NHS] 111 for advice, and they said for me to go to hospital, I went and after some tests I was admitted to hospital to have further tests…after the tests were complete and [they] still had no idea of the cause…I was then sent home as an outpatient awaiting more referrals.”
– Person living with Long Covid |
Other contributors were referred to experts in specific health conditions. For example, those with continuous aches and pains were sometimes referred to pain management clinics, and some patients reporting brain fog were referred to neurologists.
| “ | I was referred to the respiratory team and I was referred to the cardiologist at that particular time, I had like bouts where they thought it was like pox syndrome.”
– Person living with Long Covid |
The stories highlight inconsistencies in how people living with Long Covid have been treated. Some were referred back to their GP for further tests or to treat other symptoms, while others were referred to Long Covid clinics or directed towards online courses (once these had been set up). This caused further frustration, with some contributors telling us about having to attend multiple consultations and speak repeatedly to their GP and other clinicians.
| “ | So, we still feel that we’re being sent to the GP and the GPs don’t know what to do with us, GPs are busy with lots of other things. And even the sympathetic GPs with the best will in the world haven’t got a clue what to do with us. We need something more specialised basically.”
– Person living with Long Covid |
| “ | I started accessing a new GP, who at least listened and validated my experience, and made appropriate referrals, including neurology, cardiology, Long Covid clinics, fatigue services etc.”
– Person living with Long Covid |
Referrals to specialist Long Covid clinics usually happened through their GP after other causes were ruled out. Later in the pandemic, some people with Long Covid were referred to these specialist clinics by other healthcare professionals, such as those working in mental health and physiotherapy.
Gareth’s storyGareth is 40 years old and lives on his own, close to his family. At the start of the pandemic Gareth was in relatively good health and helped older people in his community to deal with the pandemic restrictions by delivering shopping or helping people to book shopping online, as well as other general odd jobs people needed help with. In 2020 Gareth started to have severe stomach problems. He initially went to his GP and was referred to several specialists for consultations and tests. Testing was not available to Gareth at this early point in the pandemic and as he did not present with the typical symptoms of Covid-19 (e.g., cough, fever, loss of taste and smell or breathing difficulties) he continued to have tests for other health conditions. “All of a sudden [I was unwell] and I didn’t have the typical cough, those symptoms. I had a lot of symptoms in my stomach, and it was more gut related…we didn’t know what it was, because it wasn’t tested it [and it] wasn’t as widespread. Because I wasn’t displaying the typical symptoms I was back and forward to my GP and eventually had to stay in hospital, I still never got a test.” Eventually, Gareth’s symptoms progressed to include severe migraines, muscle pains, fatigue and asthma and he was admitted to hospital. It was at this point that a diagnosis of Long Covid was suggested by the doctors at the hospital, as they had ruled out other conditions. Over the past couple of years Gareth’s health has repeatedly improved and then deteriorated again. This has had a negative impact on his mental health. “I’ll start feeling better and the next thing I would be down [with the symptoms] again. I would just be in tears when that happens.” |
Some people became so frustrated with the care on offer that they paid for private healthcare services to get a Long Covid diagnosis.
| “ | We went private and a week later saw the hospital who confirmed she thought it was Long Covid but did not know how to treat [it].”
– Person living with Long Covid |
The significant financial burden on people living with Long Covid was also discussed at listening events.
| “ | I encountered obstacles in accessing specialised care despite being able to afford private treatment. The lack of co-ordination between NHS and private services was not only frustrating but also financially draining. It required immense patience and personal resources to navigate this complex system.”
– Person living with Long Covid |
| “ | I sought care from a private GP specialising in Long Covid, who has been invaluable.”
– Person living with Long Covid |
| “ | We have to pay through the nose for private…it’s a two-tier health system.”
– Person living with Long Covid |
Other pandemic changes to healthcare often made it harder to access care for Long Covid, adding further frustration. For example, some experiences highlight the difficulties faced in using a telephone or online consultation to communicate their symptoms and the impact this had on them. Contributors were frustrated that telephone or online appointments did not provide care to the same standard as seeing a healthcare professional face-to-face.
| “ | It’s so hard to see a GP now…I have to send photographs to my doctor’s WhatsApp group. My GP surgery has a WhatsApp telephone number where you send your name, date of birth and the photographs…it’s just not the same.”
– Person living with Long Covid |
| “ | I managed to see healthcare professionals, through virtual consultations. They instructed me to monitor my own vital signs like pulse and blood pressure and even guided me through examining my own throat. But I found this mode of consultation inadequate; there’s no substitute for a physical examination by a professional. I was diagnosed with Long Covid. While this diagnosis was a relief, it also taught me a crucial lesson: virtual consultations have their limitations.”
– Person living with Long Covid |
People living with Long Covid experiencing fatigue, brain fog and headaches told us they found it particularly difficult to access care. These contributors told us they struggled to navigate changes, such as using telephone menus or online tools to screen symptoms.
Some healthcare professionals working in primary care were also concerned about the lack of focus on Long Covid compared to other priorities. They felt better guidance was needed on how to diagnose and treat or refer patients to other sources of help like Long Covid clinics.
| “ | Everything was about the vaccine, but we wouldn’t get updated advice on spirometry (a common breathing test to diagnose and monitor certain lung conditions), we wouldn’t get updated advice on how to refer someone to a Long Covid clinic. The vaccines took precedent over everything.”
– GP nurse |
Long Covid healthcare services
Contributors told us the main support offered for Long Covid symptoms was being referred to a Long Covid clinic. Through the Long Covid clinics people would have their symptoms assessed and were offered tools, advice and guidance to help understand and manage their condition.
Those who were referred to Long Covid clinics shared how they were able to access support for a set time – anywhere between six and twelve weeks. Some told us they were provided with a template diary to help track symptoms and periods when they felt fatigued. They were also able to access specialist physiotherapy services and other specialist healthcare advice. For example, some contributors living with Long Covid who had breathing difficulties were shown techniques to control and manage breathing, and how to adjust daily activities to avoid losing their breath too quickly.
| “ | They provided a diary to note your symptoms and they can do stuff if you’ve got breathing difficulties which is good.”
– Person living with Long Covid |
| “ | I accessed the Long Covid service for physio. I accessed ordinary physio, and they sent me to the Long Covid service since they said, ‘They’ll know better what’s going on with you.’…they gave me very small amounts of exercises rather than big exercises. So that’s the one thing that was helpful…got rid of all the joint problems that I had.”
– Person living with Long Covid |
Some contributors said Long Covid clinics helped them find out about how fit they were, and better understand where they need to improve. For example, one contributor shared how they were asked to stand up and down from a chair as many times as they could in a minute, and they were surprised at how difficult they found it. Those contributors who were more positive about Long Covid clinics said they helped them understand how the condition worked and why it was affecting their body in particular ways.
| “ | I attended a Long Covid clinic where the girl there explained that, you know, the Covid-19 stays in your body, but it attacks different parts of your body.”
– Person living with Long Covid |
However, many contributors told us about negative experiences of Long Covid clinics, with little tailored help and poor care. Those who accessed support earlier in the pandemic described Long Covid clinics as a ‘signposting service’ and were disappointed with what they were offered.
Phoebe’s storyPhoebe is 50 years old. She worked in finance but had to take a break due to challenges with her mental health. Phoebe was previously diagnosed with bipolar disorder, anxiety and depression, she also has type 2 diabetes. At the beginning of March 2020, Phoebe developed a skin condition, and other symptoms such as fatigue, brain fog and issues with her breathing and stomach. These were diagnosed as Long Covid. Her GP referred her to an online Long Covid course which helped her manage her symptoms. Through this course, Phoebe was referred to a six-week Long Covid clinic. “I’d been on the course, I got access, very early access to the Long Covid clinic. Now, this was [the] beginning of last year.” Phoebe found some parts of the clinic useful, particularly in understanding how Long Covid ‘attacks’ different parts of the body to cause a variety of symptoms. The healthcare professionals at the clinic also offered advice on how to best manage her breathing and suggested Phoebe keep a diary to track her fatigue. However, Phoebe felt disappointed by the Long Covid clinic. It seemed to mainly be for signposting patients to other healthcare services and support organisations. She had expected to be offered more tailored treatment that would help her with her skin condition. “If you’ve got breathing difficulties, they can do stuff with the Long Covid clinic. Anything else, forget it. And they’re not really geared up to really support people, because it’s all about signposting you to other services. And because my mental health services are covered anyway, they couldn’t help me with that.” |
We heard examples of other problems with Long Covid clinics, with contributors highlighting issues including delayed tests, tests not being carried out, and miscommunication about patient histories.
| “ | My local Long Covid clinic was a disgrace, absolutely unprofessional advice and management, for example saying testing was urgent and then not being ordered, starting my second consultation as if I was a new patient, so none of the initial referrals had been done.”
– Person living with Long Covid |
Others were frustrated that the clinics focused on how to manage symptoms, rather than testing different treatments that might ease or even end their symptoms. For these contributors, the clinics were ‘not fit for purpose’. They suggested the healthcare system should focus on research and development of treatments for Long Covid. Some said the clinics had only added to the distress of living with Long Covid.
| “ | The Long Covid clinic just provides support for the new disability, not treatment.”
– Person living with Long Covid |
| “ | Long Covid clinics that are not fit for purpose adds to the frustration, trauma and uncertainty for me – invest the money used in those clinics into meaningful trials and research.”
– Person living with Long Covid |
| “ | With other activists, I have been calling for proper clinics to be set up to do in depth, thorough, research level testing and saving of samples for future research, with adequate diagnostics.”
– Person living with Long Covid |
Contributors shared differences in Long Covid services available to people across the UK and globally. For example, there was a perception among some contributors that England was ahead of Scotland, Wales and Northern Ireland in terms of setting up Long Covid clinics and developing support for patients.
| “ | In Wales in particular, the Long Covid services have been a bit of an after-thought. There isn’t a really good Long Covid clinic like you’ve got in England, you know? You’ve got the one consultant in Cardiff doing her best. She had to start that service for Long Covid in her own time, it wasn’t an official service at all, and she hasn’t really been supported with it either.”
– Person living with Long Covid |
Similarly, contributors felt the UK had been slow to provide support and treatment for Long Covid compared to other countries such as America and Canada.
| “ | I would just say the fact that it’s taken Scotland…we’re a good few years behind because you look things up, over the world really, and you were hearing from America and they had clinics, and England had clinics, and we had nothing. And that is me now, 2 years later, just getting told about this Long Covid clinic.”
– Person living with Long Covid |
Support and advice for managing Long Covid
Initially there was very little support and advice available, but many contributors said this had since improved.
| “ | The first months of Long Covid saw me having no support or information.”
– Person living with Long Covid |
In the early stages of the pandemic contributors searched online for information and used social media to find people who were experiencing similar symptoms. People used platforms such as Facebook, Instagram and Twitter/X to post questions, find groups and read information.
| “ | When I got online and started finding the Long Covid groups, there were other people having similar experiences to me, so I didn’t feel like it was just me going nuts, which is how it felt.”
– Person living with Long Covid |
These peer groups were a source of support and reassurance for people during an uncertain, isolating and worrying time. Contributors were able to connect online to share advice with and offer support to people who were in a similar situation.
| “ | I found the groups probably I think in June… by the end of June I started to get a bit more involved because everything else was gone in my life and at that time I wasn’t really well enough. I could chat a bit online and then, over time, there were times where I joined a Zoom chat and met some of the people. That was amazing. It was like group therapy for all of us.”
– Person living with Long Covid |
As time went on, these groups and networks were a vital source of reassurance and support for people with Long Covid. As time progressed other forms of support and advice from charities and other organisations also improved. Contributors often told us that support tailored to particular health conditions such as asthma or heart and lung health was helpful.
The impact of Long Covid on healthcare professionals
A few contributors who worked as healthcare professionals shared their experience of catching Covid-19 at work and the devastating impact Long Covid subsequently had on them. Others described the impact this had on their family.
| “ | My husband ended up in the hospital but lucky enough he was out in about 4 or 5 days, but he still suffers from Long Covid and that was because I had taken it home from the ward.”
– Healthcare professional and carer |
We heard from some healthcare professionals about how Long Covid had affected colleagues and led to staffing pressures. Colleagues being off sick long term made it more difficult for healthcare services to operate at full capacity and provide care to patients.
| “ | Within the people I was responsible [for] there were a number of people who have had Long Covid symptoms…there’s probably about 5 people who had what I would say a significant period of altered physical ability. Maybe more than that, maybe about 10.”
– Hospital doctor |
| “ | A lot of Long Covid amongst my colleagues, chronic fatigue, Long Covid symptoms, breathlessness, which is all physical as well. It probably didn’t help that they were burnt out at the time they then got Covid-19 as well.”
– GP |
Some healthcare professionals shared how their long-term sick leave because of Long Covid had resulted in problems and conflict with their employer. They said there was a lack of understanding or recognition of Long Covid as an ongoing health condition in the healthcare system.
| “ | To this day, even with an incident form my employers they still deny I got it at work…wrote an email to [the] CEO of my Trust saying I felt completely abandoned, that my employers didn’t want to know.”
– Person living with Long Covid |
A few healthcare professionals also told us that organisations were not properly measuring the impact of Long Covid on the healthcare system. They felt that more needed to be done to understand the impact Long Covid will have on the healthcare workforce.
| “ | In terms of monitoring NHS staff with Long Covid, I am counted when I am off sick, but not when on a phased return – so there is no log of how long staff have been affected without returning to their original job role and hours, so how can you monitor the true impact of covid on NHS workers?”
– Healthcare professional living with Long Covid |
Ongoing impact of Long Covid
Long Covid continues to have a dramatic and damaging impact on many people’s lives. Contributors living with Long Covid told us they continue to face difficulties breathing. This makes it hard to move around easily and carry out day-to-day tasks. Contributors also described other severe impacts, such as significant loss of mobility.
| “ | I am now a wheelchair user due to neuropathy in my lower left leg/foot, fatigue and breathlessness caused by Long Covid.”
– Person living with Long Covid |
| “ | I was unable to return to work or my normal life as it left me very debilitated with chronic fatigue and dysautonomia (a condition that affects the nervous system), chronic headaches, brain fog and poor concentration.”
– Person living with Long Covid |
Contributors described how they are no longer able to work and the impact of losing their income. People living with Long Covid wanted to resume their normal lives once they had started to feel better, but found they were not able to do so.
| “ | I’m out of breath all the time. I still get fatigue, I still get the brain fog, and this is two years on, so work is really, really difficult.”
– Person living with Long Covid |
| “ | I went back to work, I should not have gone back to work so soon…I went back, I think, about 5 or 6 weeks after I came out of hospital…maybe that has caused the progression to be [better] much slower, I don’t know.”
– Person living with Long Covid |
Some contributors with Long Covid also described their experiences of feeling lonely and isolated, and how the condition made it difficult to maintain friendships. They described how other people were alarmed by their health and could find it distressing.
| “ | My breathing, if it gets difficult, it sounds terrible. People around me panic, because it sounds as though I’m really struggling to breathe. I just can’t get enough air into the lungs. So, if I walk up a hill, or I carry something up the stairs, then I am going to be very breathless…It doesn’t hurt, it doesn’t distress me, because I know, in a minute, it’ll be fine. But, for people around me, it can be quite distressing.”
– Person living with Long Covid |
Stories from people with Long CovidContributors at an Every Story Matters listening event spoke about the lasting effects of Long Covid, particularly on their energy levels and mental health. They stated that it impacted their wellbeing and ability to perform their roles effectively. “I can live with the headache, but it’s the tiredness that is so hard. I go home after work, and I fall asleep straight away.” They shared their experience of feeling constantly tired, with their energy “completely ripped” after contracting Covid-19. Healthcare staff spoke about the persistent headaches and overwhelming fatigue they experienced, impacting their ability to spend quality time with their family. They expressed feeling like a different person, overwhelming sadness and a lack of motivation. “Life should not be like this; I don’t know what’s wrong with me. I have three kids, all grown up. I am not the same anymore. I want to cry; I am not sure why I am so down, not sure why I am not the same man.” |
Long Covid has drastically limited what many contributors can do day-to-day. This has been a life-changing and traumatic experience for many who shared their story with us and their families.
| “ | I’m really good in the mornings…at 1 o’clock, I can feel the fatigue coming on. It’s like an oncoming storm, and it’s like a storm in my head, that’s what it does to my head. I can feel everything going wrong, it starts to [go] fuzzy, and I start to get a bit of a headache. Then I will feel tired…part of the problem is, it isn’t regular as clockwork. So, some days I can go a bit longer, other days, I can start to feel it at 11 o’clock in the morning.”
– Person living with Long Covid |
| “ | Life has been hell and torment, the effects on my family have been horrific. Before I was happy, healthy, in the best health of my life, then well before lockdown we got infected, well before testing or anyone believed it was in this country.”
– Person living with Long Covid |
Many contributors with Long Covid said they feel like they have been forgotten by the healthcare system and wider society, and that no one cares any more. They want recognition for their health condition and for the wider public to understand the challenges they and their families face.
| “ | Nobody wants to know, I feel invisible. I’m treated as collateral damage. The frustration and anger I feel is incredible; medical gaslighting, lack of support and the way other people treat me.”
– Person living with Long Covid |
They also emphasised their frustration and anger that Long Covid is spoken about as something that happened in the past.
| “ | Docs and scientists refer to Covid-19 as a thing of the past; this is frustrating and angering.”
– Person living with Long Covid |
Learning for the future: Long CovidPeople living with Long Covid reflected on what they thought needs to be learned from their experiences. Many want more recognition, research into, and understanding of Long Covid and related post-Covid-19 conditions. We were told that treating these post-Covid conditions needs to be better embedded into the healthcare system, including GPs being more responsive and understanding, and better care being available. “The NHS urgently needs funding, more staff and more training and resources for supporting and treating people with Long Covid. Access to Long Covid clinics needs to be extremely swift, and there needs to be much more support in terms of helping Long Covid patients to access the knowledge and resources out there that might help them to recover.” Every Story Matters contributor Ensuring Long Covid diagnosis and treatment happens more quickly was a priority for many. This was described as crucial because of how debilitating Long Covid is for people, and because of the ongoing physical and mental decline experienced by many with the condition. “Further research into Long Covid and cardiovascular complications could help with rapid diagnosis and treatment, also sharing good practice and patient findings between consultants and doctors across England and Wales/whole of UK and other countries too to get the best patient care pathways set up early on, so patients get treated quickly before a physical and mental decline, and a financial effect on families.” Every Story Matters contributor Many living with Long Covid wanted more to be done to raise awareness and understanding. For example, they called for targeted efforts to educate both the public and healthcare professionals about Long Covid through public health messaging, and for more funding for research for post-Covid conditions. As well as being the right thing to do to support and treat those already living with Long Covid, this was seen as crucial to prevent more post-Covid healthcare needs developing in future. “Be honest to the public about Long Covid so that we can look after, support and educate ourselves and each other. Invest in research and provide treatment. Acknowledge the risks of long-term consequences of Long Covid (cardiac pathology, dementia, cancer, etc) of chronic inflammation, immune dysregulation, gastrointestinal dysfunction, etc. Provide care now. Treating Long Covid is cheaper than the chronic ill health which results.” Every Story Matters contributor |
11. Shielding |
 |
This chapter outlines the experiences of people who were shielding during the pandemic, and the healthcare professionals caring for clinically vulnerable and clinically extremely vulnerable patients . It covers communication about shielding, the impact of shielding on mental and physical health, and experiences of accessing healthcare when shielding.
Communication about shielding
Many contributors who were clinically vulnerable and clinically extremely vulnerable told us how frightened they were at the start of the pandemic. They were often worried about contracting Covid-19 and how it would impact them and their families. Early in the pandemic, some avoided all contact with people outside of their immediate family because they were anxious about catching the virus. Some did this before there was any official advice, aware of the risks associated with their health conditions.
| “ | You didn’t know what way it was going to go or how bad it was going to be, especially the early part. Everywhere was closing down, it was very, very scary.”
– Person who is clinically vulnerable/clinically extremely vulnerable |
3. Please note it is not possible to differentiate between people who are clinically vulnerable or extremely clinically vulnerable in the stories collected by Every Story Matters. Therefore, all quotes are attributed as ‘Person who is clinically vulnerable/clinically extremely vulnerable.
| “ | I have damaged lungs & kidneys, so any form of respiratory illness would be dangerous. Do not go outside. I was in the same situation as everyone, nobody knew what to expect.”
– Person who is clinically vulnerable/clinically extremely vulnerable |
Contributors who were told to shield usually received a letter from their GP. This explained that they were at higher risk if they caught the virus. Contributors often expected this news, with many accepting that shielding was necessary for them. Many could see the benefits of shielding if this kept them safe.
| “ | Well, I knew it was for my own protection, you know, so I didn’t object. It was restrictive but I knew that I was in a situation where if I got the disease, it would be a lot worse. So, I didn’t mind.”
– Person who was clinically vulnerable/clinically extremely vulnerable |
Other contributors said they were surprised by how restrictive the shielding rules were and found them difficult to accept. Some were very worried about catching Covid-19, but also how they would cope with the restrictions.
| “ | It was hard to receive that letter and be told you can’t go out. Yes, I was just reading through the details here, and it says, ‘Get out in the garden or sit on the doorstep if you can.’ So, we weren’t allowed to even go out for a walk. So, that was hard.”
– Person who was clinically vulnerable/clinically extremely vulnerable |
| “ | I was told not to even go outside to my own bin because it was deemed too dangerous. This was incredibly scary, being told that I was likely to become seriously ill or die if I were to be exposed to Covid-19. Every time the government lifted restrictions [clinically vulnerable] people were advised to continue shielding because the risk for us had not lessened.”
– Person who was clinically vulnerable/clinically extremely vulnerable |
Those who were clinically vulnerable were sometimes confused about the guidelines, and some contacted their GP for clarification on what they were required to do. GPs said this confusion was more of a problem at the start of the pandemic, as the classification of ‘clinically vulnerable’ was not clear and changed over time. Some GPs found it difficult to advise patients because the risks for different conditions were not well understood.
| “ | So [clinically vulnerable] people [were calling] asking what they should do, were they meant to be shielding, were they meant to be changing their medicine, how were they going to get their medicines and that sort of thing…we were getting very limited information as to who was high risk…if there had been a bit more communication as to who was thought to be high risk it would have made it a bit simpler.”
– GP |
Some GPs also gave examples of clinically vulnerable and clinically extremely vulnerable patients who did not follow the guidelines because they found them too restrictive.
| “ | We had people who were supposedly on shielding lists coming into the surgery and telling us they were going away to their best friends for afternoon tea and things, and you’re like, ‘You’re supposed to be shielding…You’re not even supposed to go to the supermarket, what the hell do you think you’re doing going to somebody else’s house? Nobody’s allowed to go to somebody else’s house.’”
– GP |
Some contributors with additional needs said they found it difficult to access information from their GPs in the right format for them. This meant they did not understand what having to shield meant in practice, making them feel less safe and more isolated.
| “ | I asked for support from social services and my GP, and there was none available, everybody was isolated and you’re leaving the vulnerable and pushing them to one side and you feel rejected, I didn’t feel safe at all.”
– Person with sight loss |
Impact of shielding on mental and physical health
Contributors told us how shielding often led to, and continues to contribute toward, feelings of isolation, loneliness, anxiety and fear. Shielding has many harmful impacts on people’s physical and mental health. Some described how the fear of catching Covid-19 continued and was draining. Many felt constantly on edge and fearful, needing to be aware of who they interacted with and how they could protect themselves.
| “ | I was petrified, because I knew at the time that if I caught it that I was going to have to go to hospital. I was very afraid of it, so you know, there was blue gloves everywhere, you were washing hands constantly…you’re putting the gel on your hands.”
– Person who was clinically vulnerable/clinically extremely vulnerable |
| “ | I was so scared of catching Covid-19 and dying; so many people died. I have this very rare eye cancer…I was so scared of getting Covid-19. I didn’t leave [my town] except for one time, which was an appointment for my diabetes.”
– Person with sight loss |
We heard many stories about how shielding completely disrupted people’s usual routines and made them feel that their normal life had stopped. They told us they could no longer spend time with friends and family, even when others were able to. They shared how they could no longer exercise, and how their hobbies often stopped. Many said they were unable to work or worked alone.
As well as being afraid, the disruption meant contributors who shielded often experienced overwhelming boredom and isolation. Many of the stories shared how people’s physical and mental health deteriorated quickly throughout the pandemic.
| “ | Collapse of routine, mental health suffered, physical health suffered. She [her mum] didn’t eat a lot actually, she lost a lot of weight because she wasn’t well…but yes, so she suffered a lot mental health wise and physical health wise from just lack of other people basically more than anything, lack of any kind of interaction.”
– Carer for someone who was clinically vulnerable/clinically extremely vulnerable |
| “ | I coped by doing other things but if I’d have gone a little bit longer, a few more weeks, I think I would have gone over the edge to be honest with you. I was getting to the stage where I couldn’t cope… and only having [my mother] really to speak to, that was a big thing because my whole life was quite social. I was lonely, and I tried not to let that affect me too much. It was driving me absolutely crazy.”
– Person who was clinically vulnerable/clinically extremely vulnerable |
Many clinically vulnerable and clinically extremely vulnerable contributors found it particularly difficult when they were not allowed to join friends and family as lockdowns eased later in the pandemic. This was incredibly upsetting for older people or people living on their own.
| “ | My sisters were able to go places together and do things, and my daughter and her children and stuff, they were all able to…and I just had to watch them, so we became more isolated as the time went on and you had less people to talk to. And it got to the stage then where…you ended up getting into bed and you didn’t want to come out, even on the most beautiful day of the year, because I had nothing to get up for.”
– Person who was clinically vulnerable/clinically extremely vulnerable |
Some contributors who had shielded were able to keep in contact with their families through video calls using platforms like WhatsApp and FaceTime. This helped them feel more connected to their loved ones and reduced feelings of loneliness and isolation.
We heard examples of people who were shielding joining household ‘bubbles’ later in the pandemic. The return of more social contact was a huge relief for these contributors and greatly helped to improve some people’s mental health.
| “ | I would say that [one] positive was being allowed to bubble with another family. That was life-changing. I remember that enabled me to go to stay with my friends at Christmas, who were on the doorstep when I couldn’t see my family. I just remember, I wept when I got my hug for the first time after a long time.”
– Person who was clinically vulnerable/clinically extremely vulnerable |
Some contributors with pre-existing health conditions said these got worse because of shielding.
| “ | Being told I was so at risk of Covid-19 made me feel out of control of my health and incredibly stressed. I feared I would die if I caught Covid-19. By shielding, the real risk to me was not being able to manage my health condition which I do mainly through exercise.”
– Person who was clinically vulnerable/clinically extremely vulnerable |
| “ | [My] fatty liver disease came up [during] the pandemic and again, that was probably because you were in the house, no exercise, you were eating more.”
– Person who was clinically vulnerable/clinically extremely vulnerable |
Some contributors were more positive about shielding, often because they were comfortable at home, or were able to keep busy and positive. These contributors were worried about catching Covid-19 and did not want to take risks with their health. They often had good housing, access to a garden or had a pet to keep them company. Many were able to stay in contact with family remotely or continued working in jobs they enjoyed. Being able to develop a routine with meaningful things to do reduced feelings of boredom or isolation and helped them stay positive.
| “ | With the help of a garden…I was spoilt for things to do. So that probably saved me totally, mental health-wise…it didn’t affect me probably as much, as someone in a housing estate or, high-rise apartments or something, that didn’t have that outside space to go to.”
– Person who was clinically vulnerable/clinically extremely vulnerable |
| “ | No one around me as I shielded alone, I felt safe and looked after by the process. [I] felt a little lonely at times, but as I was working from home, I had lots of video calls daily and even sent my mum and dad a video device so we could have meals together over the video link.”
– Person who was clinically vulnerable/clinically extremely vulnerable |
Practical challenges of shielding
Many contributors who shielded described being fearful about leaving home but also being desperate to work out how they would get the essential supplies they needed. This often focused on food, but medicines were also important too. They asked family, friends or neighbours to help or visit the shops for them.
| “ | When the advice [guidelines] became clear, we were virtually kept as prisoners in our own homes. We struggled to get shopping slots and had to rely on family who did not live close by, and we lost our support network at what was a most difficult period in our lives.”
– Person who was clinically vulnerable/clinically extremely vulnerable |
| “ | This was the most frightening time for me, as I had no one, no idea how I would get help, being alone, with getting food, medicines etc, especially as I live in the countryside… One friend was… a regional manager for Tesco and it was her efforts that got me on their priority list. I ended up in tears when I rang them, and the relief was immeasurable. After a month, I was able to get food.”
– Person who was clinically vulnerable/clinically extremely vulnerable |
Experiences of accessing healthcare
Experiences of accessing healthcare services were mixed but some contributors who shielded said they had good access to healthcare and medicines, and they were grateful for the help they received. Contributors told us that most of their GP appointments went ahead online or over the telephone. In the early stages of the pandemic, they often felt telephone or video calls were safer and reduced the risk of catching Covid-19.
Those contributors who had regular check-ups with their GPs generally said that the quality of the care they received through remote appointments was good. Contributors with long term health conditions described how helpful their GPs were during this time. We heard examples of healthcare professionals going the extra mile to support them.
| “ | My GP practice did their best to keep me safe whilst ensuring I could still see them for necessary procedures such as monitoring blood tests.”
– Person who was clinically vulnerable/clinically extremely vulnerable |
| “ | I found that anytime I contacted them [GP] about anything…because you do get things [that] go on with your arthritis and your diabetes…they would’ve asked me to send in a photograph of my joints or monitored me on the phone…they were very good. The doctor was on the phone constantly checking with me. Absolutely no hassle, I actually thought they were really on the ball.”
– Person who was clinically vulnerable/clinically extremely vulnerable |
Leila’s storyLeila was diagnosed with cancer and psoriatic arthritis before the pandemic. She had been told to shield during the pandemic as her health conditions required her to take immunosuppressant drugs. Due to the urgency of the cancer treatment, Leila had not asked for further treatment for her arthritis. However, after an operation, she found herself struggling to manage the pain and swelling and contacted her GP in late 2021. Getting the initial GP appointment was difficult, but she was eventually offered a blood test and referred to a consultant. From this point on, Leila was very impressed with the support she received. She was offered appointments with consultants to ensure she was not in pain and that her condition was monitored. “In my experience with the NHS, I’ve had every appointment that I should have had… Even though there was a crisis going on, somehow they were able to give me those services.” Sometimes treatments had to be managed remotely, which could be daunting – for example, she needed to switch from tablets to an injection – but she overcame her fears with support from the hospital team. “The training for the injections was done on the phone, and I was a bit worried because I thought, ‘Oh gosh, I don’t know how I’m going to be able to do this.’ But actually, it was straightforward, and the nurse took me through it, you know, on the other side of the phone, and it was successful. And that’s one that would [not?] work for everybody now, but for me it was great, because I don’t have to bother with [travelling].” |
Contributors who shielded told us they were usually able to access medicines via a local pharmacy. They or their family organised for prescriptions to be delivered, or for family and friends to pick up their prescriptions.
| “ | Getting prescriptions and stuff were not a problem…it was a repeat [prescription] for my medication…I had to ring and then 24 hours later it was ready for pick-up. So, the wife would go and pick it up.”
– Person who was clinically vulnerable/clinically extremely vulnerable |
When people who were shielding had to have an in-person appointment, they reported receiving Covid-19 home testing kits in the post beforehand. However, for some, getting to medical appointments was difficult. For example, one contributor shared that they had vertigo during the pandemic and decided not to go to an in-person appointment with their GP. They felt it was too difficult to organise their transport to get there.
| “ | It was just getting there and getting back again because I don’t think I was able to drive, I’ve got vertigo, so I would have had to get a taxi or an Uber or something and then that made me think, ‘Do I really want to get into a taxi, go all the way there, maybe not, and then come back again?’…so eventually I just…let it go and just coped with it the best way I could.”
– Person who was clinically vulnerable/clinically extremely vulnerable |
Other contributors told us they found it harder to access care and had frustrations about remote appointments. Among those who shielded, experiences of primary care during the pandemic were similar to other patients. They said booking a GP appointment could be difficult due to high demand. For example, one contributor called their GP practice every day for two weeks before they were able to see a doctor.
| “ | You have to phone up on the day at 8:30 in the morning, along with everybody else, and join the lengthy calls to wait in queue to get an appointment. And, often, you’d get through and all the appointments had gone…so, it’s been challenging to even get access to the GPs.”
– Person who was clinically vulnerable/clinically extremely vulnerable |
Many primary care appointments were also delayed or cancelled. Some contributors who shielded had problems with accessing care, or said it was harder for healthcare professionals to assess their health condition without being examined in person.
When contributors were able to see a healthcare professional in person, they reported wearing PPE. They also felt reassured by how much PPE healthcare professionals wore when visiting their GP or hospital.
| “ | In a way, I think I felt safer in the surgery and in hospital, where [wearing PPE] was enforced and everybody was doing it, than in shops.”
– Person who was clinically vulnerable/clinically extremely vulnerable |
Other contributors said they disliked wearing PPE to their appointments. They felt it was restrictive or made it difficult to communicate with healthcare professionals.
| “ | It just felt…a little bit claustrophobic. I wasn’t able to breathe properly with the best will in the world. Masks do make you feel restricted.”
– Person who was clinically vulnerable/clinically extremely vulnerable |
Some contributors reflected on what their experience of shielding meant for their long-term health. They suggested that as society started to open back up, many people have moved on. They felt the public did not appreciate the ongoing threat Covid-19 still poses to people who are clinically vulnerable. Some are still limiting their social interactions and what they felt comfortable doing outside of their own homes. They wanted more support for people in their situation in the future.
| “ | [One] of my friends is older, she’s in her 70s, she’s not come back to church… she really has no social life whatsoever anymore…her biggest challenge is around the fact that she feels that she’s being given this information, that tells her she’s vulnerable, that she needs to protect herself, she needs to stay away from people, she is at risk, and that her risk hasn’t changed, and that Covid-19 is still around. And so she struggles to reconcile the fact that it feels like the advice has changed, and yet, the risk is still the same…And so, I think there’s a lot of, still, fear wrapped up around all of that for people.”
– Person who was clinically vulnerable/clinically extremely vulnerable |
Contributors felt it was important for government, healthcare systems and the wider public to understand that Covid-19 is still a threat and concern to people who are clinically vulnerable, and this should be reflected by better use of PPE in healthcare settings, and more flexible and responsive healthcare services.
Learning for the future: shieldingMany contributors said they understood the importance of shielding to protect people from the virus during the pandemic. However, we also heard repeatedly that the guidance on shielding was too restrictive. Many contributors told us that we need to learn from the damage being isolated did – and continues to do – to people’s health. There were many calls for better support for those shielding, particularly to protect and improve people’s mental health and emotional wellbeing. Some contributors also shared how more help should have been offered to prepare people who were shielding. “Shielding was good, but there needed to be more mental health support for people.” Every Story Matters contributor |
12.Experiences of maternity services |
 |
This chapter explores the experiences of women who used maternity services during the Covid-19 pandemic. It shares what they told us about the maternity pathway, including antenatal care, labour and birth, and postnatal care. It also outlines women’s broader experience of being pregnant during the pandemic.
Experiences of pregnancy and antenatal care
Many contributors told us how scared, fearful and anxious they felt at the start of the pandemic, as little was known about the impact of Covid-19 on pregnant women and their unborn child. This led some women to self-isolate, as they were worried about catching Covid-19 and what impact this may have on their baby
| “ | The restrictions caused me a huge amount of anxiety and worry, to the extent I could not eat, withdrew from speaking to others and was deeply worried about giving birth.”
– Woman who used maternity services |
| “ | For three weeks prior to giving birth, my birth partner and I remained indoors, away from supermarkets etc to not risk catching Covid-19.”
– Woman who used maternity services |
| “ | I was extremely paranoid about coming into contact with the virus so [I] only left the house for walks in open spaces, I was constantly wiping down surfaces, hands, wearing masks and isolating myself from family and friends.”
– Woman who used maternity services |
Women who caught Covid-19 while pregnant said it was worrying and stressful, as they did not know how their symptoms would develop. In some cases, contributors told us that healthcare professionals would check in on women regularly to ensure their symptoms did not worsen. Other contributors sought advice from other sources (such as NHS 111 for those living in England, Scotland and Wales) when needed.
| “ | I had Covid-19 twice, when I was pregnant. The first time, I was about 16 weeks pregnant. I was really sick. I didn’t have to be hospitalised, but I was really unwell at home. They [the midwifery team] were really good and they called me every day to check on me.”
– Woman who used maternity services |
| “ | I was really breathless one day and then one time I had a really weird headache. I didn’t understand what was going on. We called NHS 111 and they sent out an ambulance immediately and they came straight away, which I thought was amazing.”
– Woman who used maternity services |
Many contributors spoke about the positive experiences they had with antenatal care. They found their midwives, consultants and other healthcare staff were helpful and supportive in what was a difficult time. In the early phases of the pandemic, consultations were often carried out by telephone or online. Later in the pandemic, when restrictions were eased, contributors told us consultations took place face-to-face.
| “ | My initial conversation with a midwife was done on a video call, and I was happy with that, after that all of my appointments were face-to-face. There were never any cancellations, [or] rescheduling. I got the appointments through, and I went to them. I was always seen promptly.”
– Woman who used maternity services |
Some women shared examples of pre-existing medical conditions, such as asthma, which complicated their maternity care. These contributors said they were able to access the treatment they needed. This included regular scans and check-ups with their midwife.
| “ | I was seeing an early pregnancy assessment unit because I had some slight bleeding. It was consultant-led as well, because of my asthma…I had all of that involvement. So, I think I’ve been seen by pretty much everyone.”
– Woman who used maternity services |
Throughout the different stages of the pandemic, pregnant women shared how they had to visit hospitals for scans and checks alone. Partners or other family members were generally not allowed to attend with them. Attending appointments and consultations was a lonely and frightening experience, particularly early in the pandemic. Women who had given birth before described how strange the experience was in comparison.
| “ | Your scans were very different, your partner, my husband had to wait outside until you actually entered the room. Everything was very much alone…the scans, you had to wait outside, you got a buzzer, then had to come up when it was time to go in the room and have the scan. At least everybody was wearing masks.”
– Woman who used maternity services |
Accessing care alone added to feelings of anxiety and was upsetting for some women. For example, one contributor who had sight loss described the challenges of not having a partner present to support her.
| “ | Going through maternity services and giving birth when the NHS was crashing around me with added layers of having sight loss was hard. All information was paper based, I couldn’t see the sonogram and didn’t have a partner there to explain things to me, I was full of anxiety. My sight loss wasn’t accounted for, they were focussed on navigating care in covid – reading out letters to me wasn’t a priority.”
– Woman who used maternity services |
Having to interact with healthcare professionals alone was also difficult for women if there was a potential health issue with their child.
| “ | I went to a routine midwife appointment, but she was worried about the baby and said she couldn’t hear a heartbeat. She said I needed an emergency ambulance or to make my way to hospital quickly. We drove quickly to [the] hospital where they were expecting me. At the doors I was told I was the only one allowed in….we thought [the] baby had died at 32 weeks gestation, yet I had to go in alone. This was one of the scariest moments of my entire life. Meanwhile [my partner] had to wait outside the hospital waiting to be told if his baby was alive or not.”
– Woman who used maternity services |
Gwen’s storyGwen lives with her husband and child. She was pregnant during the pandemic. After Gwen went for her 12-week scan she had a lot of bleeding, which was initially thought to be a miscarriage, but was eventually diagnosed as a haematoma (bleeding or the collection of blood outside the blood vessels). When Gwen was admitted to hospital for observation and tests, her husband was not allowed to wait with her or to stay overnight. This was an emotional and upsetting time for Gwen, and she felt very alone without the support of her husband or other family members. “He was allowed in briefly while they admitted me, while they did the initial assessment, and then he had to go and wait outside, which, to me, I felt very alone.” A midwife on the ward stayed up with Gwen chatting for most of the night and also let her know when it was time for her to get some rest. The next day, Gwen received the test results which confirmed that the bleeding was not a miscarriage, and she was able to go home. Although she was grateful for the care and support she received, she would have liked more flexibility for her partner to be there and support her. “My husband was only able to walk me to the ward door and that was it. And to be fair, the midwife sat with us all night pretty much on the ward. They only had a few patients, but it was obviously women that were waiting to give birth.” |
We heard from many contributors that guidelines around having people with them during appointments were not interpreted consistently, and this felt unfair. For some appointments pregnant women told us they could have a partner present, while at other times they could not. Not being clear about whether someone could go with them caused further stress and confusion for some women.
| “ | One midwife said, ‘I would have let you in [to the contributor’s partner], why wouldn’t they let you in?’ So, it’s, kind of, whoever was there maybe. I don’t know.”
– Woman who used maternity services |
These contributors said there should have been more consistency in how the guidelines were applied, but also more flexibility for people who needed support.
| “ | [It was] very difficult, very stressful, because you were only allowed one person, or you weren’t allowed anybody in, with your appointments. I was 20, I had just found out I was pregnant. Obviously, very scared, and there was no leeway at all, anywhere. Which was really, really difficult. That would make my mental health a whole lot worse. It caused stress for me, which then, obviously, caused stress for the baby. I ended up really ill all through my pregnancy. Which truly started from the stress.”
– Woman who used maternity services |
The absence of prenatal and antenatal classes early in the pandemic made women feel more isolated. Many contributors shared that lockdown restrictions meant they had not been able to develop a support network of people going through a similar experience. This was particularly difficult and upsetting in the early stages of the pandemic, when antenatal classes stopped and had not yet moved online.
| “ | I had no prenatal classes whatsoever, and I know later on they did do classes. There was none of that offered to me. I just feel again like that part of my pregnancy was stolen from me.”
– Woman who used maternity services |
| “ | I wanted to go to an antenatal class, but I didn’t go as they weren’t available at all.”
– Woman who used maternity services |
Some women shared how not attending antenatal classes meant they were unable to form new friendships that could support them during early motherhood. They said this contributed to later experiences of loneliness and postnatal depression (outlined further later in this chapter).
Labour and birth
Women’s experiences at labour and birth varied depending on when they were pregnant during the pandemic.
Contributors who were close to their due date around the first lockdown often described this as a very uncertain and frightening time. It was unclear to them how they would be cared for during labour and birth. Pregnant women shared examples of conflicting information about how labour and birth would be managed, which added to confusion.
| “ | That was quite scary…I was a first-time mum…you’d hear rumours, people would say they [partners and family members] can’t go in at all or they can’t go in until the baby’s coming out.”
– Woman who used maternity services |
As the pandemic progressed and the numbers of people hospitalised with Covid-19 started to rise, it was clear hospitals were under stress. This meant some women chose to have a home birth because they were worried about catching Covid-19. These contributors were also worried about adding to the strain on healthcare systems by going to hospital. However, some found that suggesting a home birth was met with reluctance from midwives.
Eileen’s storyEileen is 31 years old and has three children. She lives in a rural area, close to her family. She was pregnant with her third child in April 2020 when the UK was in its first lockdown. Eileen was keen to have a home birth during the pandemic, and she had previously chosen this type of birth for her second child. After her initial meetings with her midwife, she requested a home birth, but found she was met with reluctance as healthcare professionals were not sure what was allowed under the guidance. “I’m really into self-advocating when it comes to pregnancy. [I had to answer] a lot of questions.” She felt she had to advocate very strongly for herself to access a home birth with the relevant health care professionals, and had several discussions about how the home births team would work for her, and how guidance and PPE would be used. Eventually, the home births team agreed to deliver the baby at home, and Eileen was able to have her partner and mother present at the birth. “Just a lot of questioning and, like, being put on hold and like, ‘We’ll get back to you.’ It was mostly that and then having to chase things up.” |
Women who chose to give birth in hospital often told us about the positive experiences they had, despite the challenging circumstances. Many contributors found midwives, doctors and other healthcare professionals were helpful and supportive throughout labour and birth. They were grateful for the care they received during a difficult time for the health service.
| “ | My midwife was absolutely incredible, they were brilliant. So, yes, overall, I would say it went as [well] as it possibly could.”
– Woman who used maternity services |
However, some women who used maternity services shared problems they faced during birth. For example, one contributor mentioned that when they went to hospital to give birth, they were told the maternity ward was closed due to staff shortages. They assumed this was because of the pandemic. Although they were seen by midwives and doctors, this initially worried them as they could not follow their preferences for giving birth.
Another woman told us she was not checked into the maternity ward properly, and this meant waiting for a long time without being seen by anyone. When healthcare professionals eventually discovered complications with the birth – which were life threatening to her child – this was deeply stressful and worrying for her. The contributor felt she had been let down and was extremely disappointed with the care she received.
A common concern was the inconsistency around birthing partners or other family members being present at the birth. These were similar to the concerns about antenatal care. Many women told us it was unfair and distressing that they were not allowed to have a birthing partner with them.
Those who were separated from their partners during labour and birth often said they did not have the emotional support they needed. Some contributors were sad their partner had not been as involved as they should have been. Others described problems during the birth and difficult experiences because they needed the help their partner would have offered.
| “ | I gave birth at home with my team (December 2020), but unfortunately, I had complications and had to be admitted to hospital that evening at 1am…my partner had to sit outside the ward for 3-4 hours through the night. My baby was left in a cot next to me, but due to giving birth I was unable to sit up and move around without extreme pain. I was distraught. The rules about no partners in hospitals was the most damaging thing created during the pandemic.”
– Woman who used maternity services |
| “ | I was in intense labour on my own for much of the time with some brilliant support from my midwife, but it wasn’t the same [as having her partner present].”
– Woman who used maternity services |
Some women gave examples of people being told different rules in similar circumstances to them. This was frustrating and further added to a sense of unfairness.
| “ | My partner was not allowed in yet families being cared for in other trusts had different experiences, some of our friends pregnant at the same time as us were allowed in to every appointment which was really frustrating.”
– Woman who used maternity services |
Women who gave birth in hospital later in the pandemic said their birthing partners were usually allowed to be present. These contributors found this reassuring as it allowed them to share their experience.
| “ | At first, they were strict about it and saying, like, no one could come in. But then, by the end, obviously when he was born everyone was just in there. I’m thinking about it now. Everyone was in the room.”
– Woman who used maternity services |
It was also unclear to some contributors whether partners could stay overnight or whether they could stay past visiting hours. For example, one woman shared how she had been told her partner could not stay overnight by a midwife, but then another said he could stay because they had twins.
| “ | About three days after being in hospital, one of the midwives just said, ‘I’m surprised your husband doesn’t stay and help you out at night.’ And I was just, like, ‘Well, he’s not allowed, like, visiting hours, you know the visiting hours?’ And she went, ‘Oh, well, for twins, the husband’s allowed to stay at night, because you’ve got two babies. Two babies, two adults.’ And no one had told us that, no one had said that he was allowed to stay.”
– Woman who used maternity services |
Other women described their partners only being able to stay with them for a short time. They were usually told their partner had to leave because it was past hospital visiting time. Some contributors told us this made them angry because they did not think it was fair.
| “ | I didn’t understand why he couldn’t stay with me because the baby was born at 10:10 at night, it was past visiting hours, so he had to go. I just thought that was really strange. We were just sitting in our little room bit on our own. So why would he have to go?”
– Woman who used maternity services |
| “ | It was just a ridiculous situation. And then they said, so I had her at 12 o’clock, whatever it was, half past 12 in the afternoon. And then they said, ‘He could only stay with me until 8 o’clock because that’s when the visiting times stopped.”
– Woman who used maternity services |
Some women questioned the measures in place to reduce the spread of Covid-19. These contributors considered that the guidelines did not make sense and were unnecessary. Others suggested Covid-19 rules were interpreted differently depending on the healthcare professionals. This created a sense of unfairness for some women who shared their story with us.
| “ | You wore the mask round the hospital, up on to the ward, but then once you were on the ward, you were allowed to take it off…none of it ever made sense, and then it was the same whenever you were downstairs, whenever I was in for labour; you had to wear it while they were examining you.”
– Woman who used maternity services |
Postnatal care
In the early stages of the pandemic, we heard how some postnatal check-ups became ‘doorstep visits’, with midwives and health visitors carrying out assessments at the front door. Some contributors described how strange this was.
| “ | The visits stopped or continued a little bit, and they became, actually, like doorstep visits. So, we had to bring things in like the weighing scales into the passage and weigh my daughter and then hand the scales back onto the steps and the health visitors didn’t come in. That was really bizarre.”
– Woman who used maternity services |
Other contributors experienced postnatal care over the phone, which they often found helpful and supportive. They felt healthcare professionals took the time to read their notes and understand their medical history. However, a few women shared how remote support did not work well for breastfeeding early in the pandemic.
| “ | I was trying to breastfeed my baby and had a few breastfeeding difficulties at that time, so the support wasn’t really there because there wasn’t anybody to, sort of, come and be able, physically be able, to see what’s happening. So that was quite stressful, actually, that was quite a stressful time, to not have what you would call normal support or just, you know…your parents.”
– Woman who used maternity services |
| “ | Breastfeeding support is an essential service; health visiting is an essential service. Ripping up the rule book in the name of infection control can never happen again.”
– Woman who used maternity services |
Some women who gave birth earlier in the pandemic told us they did not see a health visitor or midwife for several months after the birth. This caused anxiety for many women who already felt isolated as new mothers. This was particularly challenging as help was not available from family members or friends due to pandemic restrictions.
| “ | I didn’t see a midwife or anyone or a health visitor – the baby was about 5 months old. I thought something could be seriously wrong and as a first-time mum, I wouldn’t know either.”
– Woman who used maternity services |
| “ | After birth I had limited follow up care and only saw a health visitor when I screamed to [see them].”
– Woman who used maternity services |
Later in the pandemic, midwives and health visitors were more commonly visiting people in person while wearing PPE. Contributors who had these face-to-face visits found them reassuring and were positive about the support they were offered.
| “ | I had a midwife come out every single time…and she was great. She came in with a mask on, her gloves on, and the plastic apron. And they did everything properly, because obviously they weigh the baby, they had their scales all cleaned before and after they used them. They were great.”
– Woman who used maternity services |
| “ | I did find the health visitor really good. I liked to have her come to the house and to see the baby. Also, the midwife that I had, she was my antenatal midwife for the pregnancy, and then she stayed assigned to you for two weeks or so after your baby’s born, and then you get handed over to the health visitor.”
– Woman who used maternity services |
We heard from some women about how they felt their overall maternity experience was not what it should have been. This was the case even among some who were positive about their care. Contributors felt that this sense of missing out became more apparent when they had time to reflect on their experiences after the birth.
| “ | I felt like nobody even talked to me about my physical recovery, even at the 6–8-week postpartum checkup. Everything just felt hollow, and I think it really changed my views of having a second child because I’ve been so traumatised by the experience. I never want to repeat that ever again. Covid-19 was 100% the reason for my trauma and the health services, even though they’re fantastic, from the maternity perspective, felt short of adequate care.”
– Woman who used maternity services |
Mothers shared how they found the postpartum months extremely challenging during the pandemic. As shown by experiences already included in this chapter, women often shared that they had missed opportunities to develop friendships and support networks, particularly with no antenatal classes running. After the birth, they reported feelings of loneliness, isolation and, in some cases, postnatal depression. Some contributors said they struggled to access postpartum mental health support.
| “ | I was prevented from having a normal maternity leave, socialising with new mums [and] building a local support network.”
– Woman who used maternity services |
| “ | There were no child services, like, we weren’t able to go to any groups or anything, or even get out of the house, so you end up just being lonely. Motherhood is lonely as it is, but that made it 10 times worse.”
– Woman who used maternity services |
New mothers also highlighted their worries about their child not developing social skills and interacting with other young children.
| “ | I could not access any support in the community or socialise my baby for months and months.”
– Woman who used maternity services |
| “ | Maternity leave was hard, there was no classes or support groups to join to help develop my little one [or] help me find friends with other babies [of] a similar age.”
– Woman who used maternity services |
Other women described how contracting Covid-19 had continued to cause them worry, as they were unsure what impact it would have on their children in the future.
| “ | I still don’t really understand the effect it has on kids or babies, because I’m still worrying, like, obviously, he’s only two years old. I still worry about him getting Covid-19 and what’s going to happen about him, if he gets really ill.”
– Woman who used maternity services |
| “ | I think having a young baby as well made it all the more…scary, not knowing what sort of impact it might have on them. So, I think how it affected me definitely was the hypervigilance, worry, just about it being an unknown, and just worried about catching it.”
– Woman who used maternity services |
13. Appendix |
Module 3 provisional scope
The provisional scope of Module 3 was used to guide how we listened to people and analysed their stories. The scope for the module is outlined below and can also be found on the UK Covid-19 Inquiry website.
This module will consider the impact of the Covid-19 pandemic on healthcare systems in England, Wales, Scotland and Northern Ireland. This will include consideration of the healthcare consequences of how the governments and the public responded to the pandemic. It will examine the capacity of healthcare systems to respond to a pandemic and how this evolved during the Covid-19 pandemic. It will consider the primary, secondary and tertiary healthcare sectors and services and people’s experience of healthcare during the pandemic, including through illustrative accounts. It will also examine healthcare-related inequalities (such as in relation to death rates, PPE and oximeters), with further detailed consideration in a separate designated module.
In particular, this module will examine:
- The impact of Covid-19 on people’s experience of healthcare.
- Core decision-making and leadership within healthcare systems during the pandemic.
- Staffing levels and critical care capacity, the establishment and use of Nightingale hospitals and the use of private hospitals, 111, 999 and ambulance services, GP surgeries and hospitals and cross-sectional co-operation between services.
- Healthcare provision and treatment for patients with Covid-19, healthcare systems’ response to clinical trials and research during the pandemic. The allocation of staff and resources. The impact on those requiring care for reasons other than Covid-19. Quality of treatment for Covid-19 and non-Covid-19 patients, delays in treatment, waiting lists and people not seeking or receiving treatment. Palliative care. The discharge of patients from hospital.
- Decision-making about the nature of healthcare to be provided for patients with Covid-19, its escalation and the provision of cardiopulmonary resuscitation, including the use of do not attempt cardiopulmonary resuscitation instructions (DNACPRs).
- The impact of the pandemic on doctors, nurses and other healthcare staff, including on those in training and specific groups of healthcare workers (for example by reference to ethnic background). Availability of healthcare staff. The NHS surcharge for non-UK healthcare staff and the decision to remove the surcharge.
- Preventing the spread of Covid-19 within healthcare settings, including infection control, the adequacy of PPE and rules about visiting those in hospital.
- Communication with patients with Covid-19 and their loved ones about patients’ condition and treatment, including discussions about DNACPRs.
- Deaths caused by the Covid-19 pandemic, in terms of the numbers, classification and recording of deaths, including the impact on specific groups of healthcare workers, for example by reference to ethnic minority background and geographical location.
- Shielding and the impact on the clinically vulnerable (including those referred to as “clinically extremely vulnerable”).
- Characterisation and identification of Post-Covid Condition (including the condition referred to as Long Covid) and its diagnosis and treatment.
How people shared their story with us
There are three different ways we collected people’s stories for Module 3:
Online form
Members of the public were invited to complete an online form via the Inquiry’s website (paper forms were also offered to contributors and added via the online form for analysis). This allows them to answer three broad, open-ended questions about their pandemic experience. These questions were:
o Tell us about your experience
o Tell us about the effect on you and people around you
o Tell us what you think could be learned
The form asks other demographic questions to collect background information about them (such as their age, gender and ethnicity). The responses to the online form are submitted anonymously.
For Module 3, we analysed 32,681 stories related to UK healthcare systems. This includes 27,670 stories from England, 2,756 from Scotland, 2,451 from Wales and 1,231 from Northern Ireland (contributors were able to select more than one UK nation in the online form, so the total will be higher than the number of responses received).
The responses were analysed through natural language processing (NLP), which uses machine learning to help organise the data in a meaningful way. A combination of algorithmic analysis and human review is then used to further explore the stories.
The NLP analysis identifies repeated language patterns within free-text data. It then groups this data into ‘topics’ based on terms or phrases commonly associated with that topic (for example, the language used in a sentence about anxiety might be very similar to that used when talking about depression, which is grouped into a topic on mental health). It is known as a ‘bottom-up’ approach to text analytics since it approaches the data with no preconceptions about the topics it contains, rather it allows topics to emerge naturally based on the contents of the text.
Stories were selected for inclusion in the topic model in two ways. First all responses to each question were taken from the online form and blank data was removed. Second, responses were filtered based on their relevance to Module 3.
Stories were considered relevant if those who shared them had selected any of the below responses at the question ‘What would you like to tell us about?’:
o Having Covid-19.
o Living with Long Covid.
o Losing someone because of Covid-19.
o Pregnancy or having a baby, including complications or loss.
o General wellbeing.
o Mental health, for example, feeling sad, angry, anxious, or stressed.
o Health services, for example the NHS or HSCNI, including GP surgeries.
o Something positive that you experienced.
Following the identification of relevant stories, a topic model was run for each of the three open-ended questions included in the online form. From this we identified a total of 233 topics across all responses to Q1, 213 at Q2, and 147 at Q3. Since contributors could select multiple responses at the question ‘What would you like to tell us about?’ it was possible that the stories selected for inclusion contained information not relevant to Module 3. For this reason, following the initial topic modelling the research team at Ipsos reviewed all topics for relevance and removed topics not relevant to Module 3 from the final stage of analysis. This removed a total of 143 topics at Q1, 140 topics at Q2, and 86 topics at Q3, leaving a total of 90, 73, and 61 topics per question respectively.
Following the removal of topics not relevant to Module 3 a statistical factor analysis was conducted to map relationships between topics and group them based on those commonly occurring together or within three sentences of each other. For example, topics about hand washing, PPE, and mask wearing were automatically grouped into a factor about preventing transmission. The factor analysis produced 17 overarching factors across the 90 topics relevant at Q1, 13 factors at Q2, and 15 factors at Q3.
Following the topic modelling and factor analysis a codeframe was generated based on those topics relevant to Module 3. This involved human review of the most common words and phrases, both in the full dataset and within each topic, to identify keywords and patterns that could be used to group stories into appropriate topics and sub-topics. In doing so, this provided the research team with a much more accurate quantification of the size and elements of topics, to inform the approach to analysis.
Since more people had shared their story with the Inquiry between the topic modelling and the keyword matching, an additional set of stories were provided to Ipsos for this latter stage of analysis. In total, 32,681 stories were included at this point, and these were no longer filtered by the question ‘What would you like to tell us about?’. This decision was taken to ensure all relevant stories were captured, based on the words people used.
Researchers then reviewed the different topics relevant to Module 3 to explore the stories. These were brought together with stories shared with the Inquiry in other ways (described below) to include in this report.
The diagram below shows the themes included in the online form and the number of times each theme was mentioned by a contributor in their response. The size of each block represents the volume of responses related to the theme. Note that contributors may have mentioned multiple themes within their response and may therefore be counted a number of times.
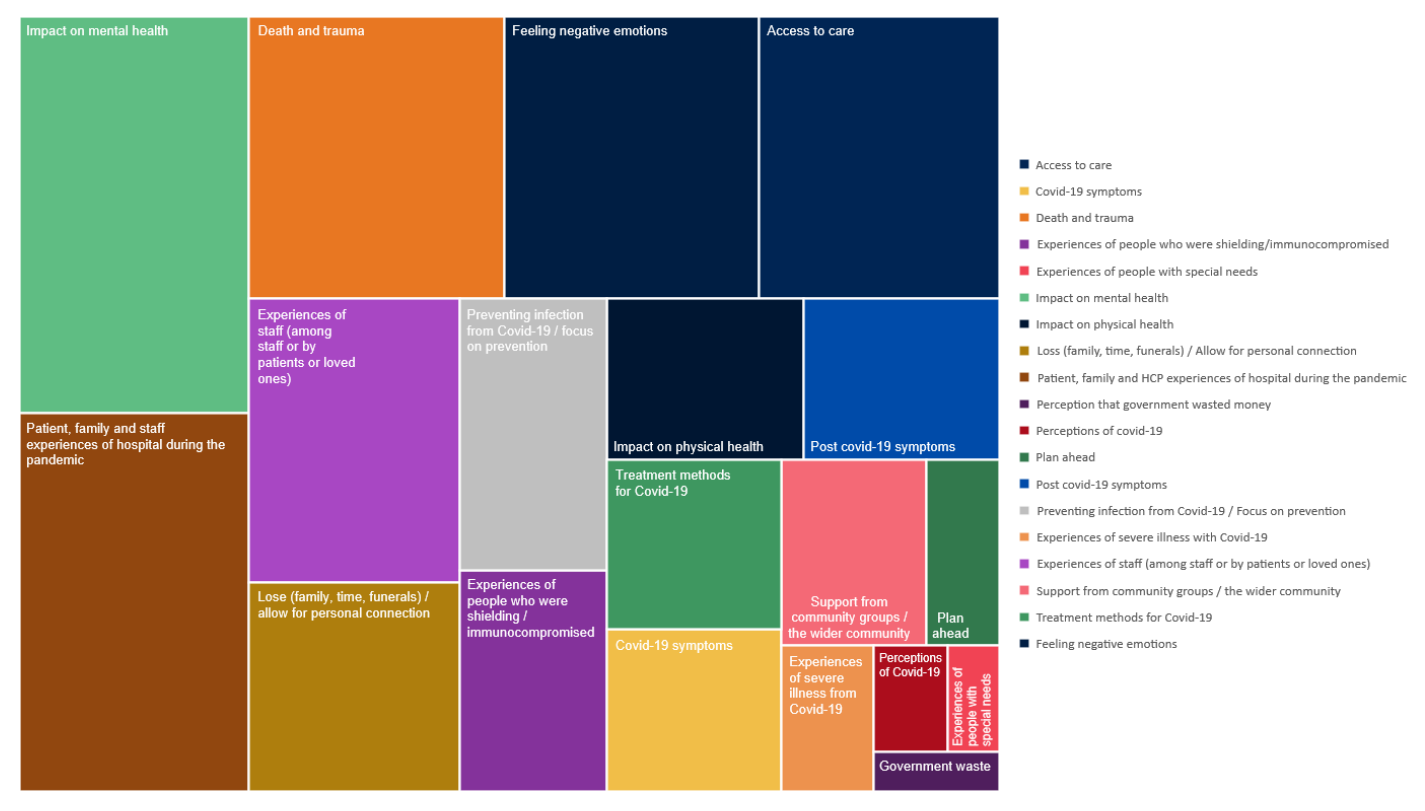
Listening events
The Every Story Matters team travelled to 17 towns and cities across England, Wales, Scotland and Northern Ireland, to give people the opportunity to share their pandemic experience in person in their local communities. Listening events were held in the following locations:
- Carlisle
- Wrexham and Ruthin
- Newham
- Exeter
- Paisley
- Derry / Londonderry
- Middlesborough
- Enniskillen
o Bradford
Virtual listening sessions were also held where that approach was preferred. We worked with many charities and grassroots community groups to speak to those impacted by the pandemic in specific ways. This includes bereaved families, people living with Long Covid and Paediatric Inflammatory Multisystem Syndrome (PIMS-Ts), clinically vulnerable families, disabled people, refugees, people from ethnic minority backgrounds and healthcare professionals. Short summary reports for each event were written, shared with event participants, and used to inform this document.
Targeted listening
A consortium of social research and community engagement partners were commissioned by Every Story Matters to conduct depth interviews and discussion groups with those most impacted by the pandemic and those less likely to respond in other ways. These interviews and discussion groups focused on the Key Lines of Enquiry (KLOEs) for Module 3. In total, 604 people across England (318), Scotland (105), Wales (90) and Northern Ireland (91) contributed in this way between February 2023 and February 2024. This includes 450 depth interviews with:
- People directly impacted by Covid-19.
- People indirectly impacted by Covid-19.
- Healthcare professionals and support staff.
- Other professional groups working in the healthcare system.
A further 154 people from communities that are known to experience health inequalities were engaged through community outreach. These community discussion groups and interviews helped ensure the Inquiry heard from people who may not be reached in other ways. The people we spoke to included:
- People from an ethnic minority background.
- People with a disability including visual impairment, hearing impairment and those with a learning disability.
- People experiencing deprivation.
All depth interviews and discussion groups were recorded, transcribed, and coded and analysed via human review to identify key themes relevant to the Module 3 Key Lines of Enquiry (KLOEs).
The tables below outline the number of interviews across the healthcare system and with people experiencing health inequalities.
| Participant type | Interviews completed |
|---|---|
| Direct impact of Covid-19 (service users) 4 | 72 |
| Indirect impact of Covid-19 (service users) 5 | 140 |
| Healthcare workers and support staff | 223 |
| Other professional roles | 15 |
| Total | 450 |
- This group includes bereaved family and friends, patients hospitalised with Covid-19, people living with Long Covid and several other experiences as outlined in Table 3 below.
- This group includes people who used healthcare services during the pandemic, those who were shielding and several other experiences as outlined in Table 3 below.
| Participant type | People engaged |
|---|---|
| People from an ethnic minority background | 60 |
| People with a disability including visual impairment, hearing impairment and those with a learning disability | 15 |
| People experiencing social and economic deprivation | 79 |
| Total | 154 |
People were asked to take part in targeted research based on the scope of Module 3 and specific experiences they had during the pandemic of interest to the Inquiry. The table below outlines the experiences they were asked to tell us about, although experiences discussed in the interviews covered a range of different things that happened to them during the pandemic related to healthcare
| Type of contributor | Interviews completed |
|---|---|
| People directly impacted by Covid-19 | |
| Bereaved individual/families | 12 |
| Patients hospitalised with Covid-19 | 9 |
| Patients who had cancelled OR postponed appointments/operations/treatments | 19 |
| Long Covid patients | 9 |
| People who decided not to seek treatment or attend in-person appointments | 11 |
| Individuals/ family members who were involved in discussions and decisions about DNACPR | 12 |
| People indirectly impacted by Covid-19 | |
| People who used inpatient hospital services | 19 |
| People who used maternity services | 17 |
| People who used community hospital services | 8 |
| People who used mental health hospital services (excluded from analysis as adult mental health services do not form part of Module 3’s investigation) | 7 |
| People who used GP services | 24 |
| People who used emergency ambulance services | 7 |
| People who used NHS 111 | 7 |
| People whose relatives/loved ones were in hospital | 8 |
| People who were told to shield / clinically vulnerable or clinically extremely vulnerable | 14 |
| People who used outpatient hospital services | 8 |
| People who used A&E services | 16 |
| Dental service users (excluded from analysis as dentistry does not form part of Module 3’s investigation) | 3 |
| Healthcare professionals and support staff | |
| Hospital doctors (NHS Acute general) | 21 |
| Hospital doctor (A&E in particular) | 10 |
| Hospital doctors (Private) | 4 |
| Hospital nurses (Acute including A&E) | 10 |
| Hospital healthcare assistants | 7 |
| Hospital porters | 7 |
| Hospital chaplains | 7 |
| Hospital cleaning staff | 7 |
| Hospital catering staff | 7 |
| Palliative care staff | 10 |
| GPs (including locums) | 21 |
| GP nurses | 15 |
| GP practice managers | 7 |
| Dentists (excluded from analysis as dentistry does not form part of Module 3’s investigation) | 6 |
| Pharmacists and pharmacist technicians | 8 |
| Paramedics and ambulance staff | 20 |
| Allied healthcare professionals (Acute hospitals and community) | 24 |
| NHS 111 call handlers | 4 |
| 999 call handlers | 4 |
| Hospital laboratory staff (known as Clinical Scientists) | 4 |
| Nightingale staff | 5 |
| NHS admin and managerial support | 17 |
| Other professional groups working in the healthcare system | |
| Army personnel | 2 |
| Healthcare workers in secure mental health hospital/facilities (excluded from analysis as dentistry does not form part of Module 3’s investigation) | 7 |
| Regulatory staff (e.g. CQC in England or Healthcare Inspectorate Wales) | 6 |
| Total | 450 |