اس ریکارڈ میں شامل کچھ کہانیوں اور موضوعات میں موت کی تفصیل، قریب قریب موت کے تجربات اور اہم جسمانی اور نفسیاتی نقصانات شامل ہیں۔ یہ پریشان کن ہو سکتے ہیں۔ اگر ایسا ہے تو، قارئین کی حوصلہ افزائی کی جاتی ہے کہ وہ ساتھیوں، دوستوں، خاندان، معاون گروپوں یا صحت کی دیکھ بھال کرنے والے پیشہ ور افراد سے جہاں ضروری ہو مدد لیں۔ UK Covid-19 انکوائری ویب سائٹ پر معاون خدمات کی فہرست فراہم کی گئی ہے۔
پیش لفظ
UK CoVID-19 انکوائری کے لیے یہ دوسرا ایوری سٹوری میٹرز ریکارڈ ہے۔
CoVID-19 ویکسینز کا موضوع، کچھ لوگوں کے لیے، جذباتی طور پر چارج شدہ مسئلہ ہے۔ وہ لوگ تھے جن کے لیے کورونا وائرس ویکسینیشن کا موضوع مرکزی موضوع تھا جسے وہ انکوائری کے ساتھ اٹھانا چاہتے تھے۔
شراکتیں مختلف ہیں اور خلاصہ طور پر، ان میں شامل ہیں:
- وہ لوگ جنہوں نے بے حد راحت محسوس کی کہ وبائی امراض کے دوران تیار اور تقسیم کی گئی ایک ویکسین کا مطلب ہے کہ زندگی ممکنہ طور پر 'معمول' پر واپس آسکتی ہے۔
- وہ لوگ جو اس بارے میں فکر مند رہتے ہیں کہ اسے کتنی جلدی تیار کیا گیا تھا اور وہ اب بھی اس کے فوائد بمقابلہ اس کے خطرات کے بارے میں محتاط، یا حتیٰ کہ شبہات کا شکار ہیں۔
- وہ لوگ جنہوں نے محسوس کیا کہ وبائی مرض کے دوران انہیں ویکسین لینے یا نہ لینے کے بارے میں بہت کم انتخاب دیا گیا تھا اور ویکسین لینے کے لئے سماجی یا کام کے دباؤ کو محسوس کیا گیا تھا۔
- وہ لوگ جو اب بھی خوشی محسوس کرتے ہیں کہ انہوں نے ویکسین نہ لینے کا انتخاب کیا جبکہ دوسروں نے جشن منایا کہ ان کے پاس ہے۔
- وہ لوگ جنہوں نے اس خیال کا اظہار کیا کہ ویکسین اور کسی بھی ممکنہ ضمنی اثرات کے بارے میں کافی معلومات نہیں تھی، اور اب بھی نہیں ہے، اور معلومات کے اس خلا نے افواہوں، سازشی نظریات اور جاری تشویشوں کے لیے جگہ چھوڑ دی ہے۔
- وہ لوگ جو یقین رکھتے ہیں کہ ویکسین لینے سے انہیں چوٹ لگی ہے یا اہم ضمنی اثرات ہوئے ہیں، جن میں سے کچھ جاری ہیں۔
- وہ لوگ جنہوں نے اپنے خدشات کو محسوس کیا ماہرین یا طبی پیشے کی طرف سے مناسب طریقے سے حل نہیں کیا گیا تھا.
لوگ خاندانوں اور دوستوں کے گروپوں میں یہ مختلف خیالات رکھتے تھے اور ویکسین کے بارے میں ان کے تجربات بھی مختلف تھے۔ اس کی وجہ سے بعض اوقات ان کے قریبی لوگوں کے ساتھ تعلقات میں مسائل پیدا ہوتے تھے۔
جن لوگوں نے اپنے تجربات ہمارے ساتھ شیئر کرنے کا انتخاب کیا وہ عام طور پر ویکسین اور علاج کے موضوع پر شدید جذبات، اکثر منفی جذبات سے متاثر ہوتے تھے۔ ہم نے ان لوگوں سے کم کہانیاں اور تجربات سنے جن کا کہنا تھا کہ انہوں نے ویکسین لے لی ہے اور وہ اپنے فیصلے سے خوش ہیں، شاید اس لیے کہ وہ اپنی ویکسین کی کہانیاں شیئر کرنے کے لیے کم حوصلہ افزائی کر رہے تھے۔
ہر کہانی کے معاملات نہ تو سروے ہوتے ہیں اور نہ ہی تقابلی مشق۔ یہ برطانیہ کے پورے تجربے کا نمائندہ نہیں ہو سکتا، اور نہ ہی اسے اس کے لیے ڈیزائن کیا گیا تھا۔ اس کی قدر تجربات کی ایک حد کو سننے میں، ان موضوعات کو حاصل کرنے میں ہے جو ہمارے ساتھ شیئر کیے گئے ہیں، لوگوں کی کہانیوں کو ان کے اپنے الفاظ میں نقل کرنا اور، اہم بات یہ ہے کہ لوگوں کے تجربات انکوائری کے عوامی ریکارڈ کا حصہ ہیں۔
اس لیے ہمیں اس بات پر زور دینا چاہیے کہ یہ ریکارڈ خود انکوائری کے خیالات کی نمائندگی نہیں کرتا ہے۔ بلکہ یہ ان کہانیوں اور تجربات کا عکس ہے جو ایک ایسے موضوع پر ہمارے ساتھ شیئر کیے گئے تھے جو مضبوط اور اکثر منقسم رائے کو جنم دیتے ہیں۔
ہر کہانی کی اہمیت کی ٹیم
اعترافات
ہم سب سے پہلے تمام سوگوار خاندانوں، دوستوں، پیاروں اور ان لوگوں کا تہہ دل سے شکریہ ادا کرنا چاہیں گے جن کی زندگیاں وبائی مرض سے متاثر ہو رہی ہیں۔ انکوائری کے ساتھ اپنے تجربات، یا اپنے پیاروں کی کہانیاں شیئر کرنے کے لیے آپ کا شکریہ۔
ایوری سٹوری میٹرز کی ٹیم نیچے دی گئی تمام تنظیموں کے لیے بھی اپنی مخلصانہ تعریف کا اظہار کرنا چاہے گی جنہوں نے اپنی کمیونٹی کے اراکین کی آواز اور ویکسین کے تجربات کو پکڑنے اور سمجھنے میں ہماری مدد کی۔ آپ کی مدد ہمارے لیے زیادہ سے زیادہ کمیونٹیز تک پہنچنے کے لیے انمول تھی۔ ایوری سٹوری میٹرز ٹیم کے لیے مواقع کا بندوبست کرنے کے لیے آپ کا شکریہ ان لوگوں کے تجربات سننے کے لیے جنہیں آپ اپنی کمیونٹیز میں ذاتی طور پر، اپنی کانفرنسوں میں، یا آن لائن کام کرتے ہیں۔
- عمر برطانیہ
- سوگوار فیملیز فار جسٹس سائمرو
- طبی لحاظ سے کمزور خاندان
- Covid19FamiliesUK
- معذوری ایکشن شمالی آئرلینڈ
- خدمت مراکز بریڈ فورڈ/ نوجوان ان کووڈ
- مینکیپ
- مسلم خواتین کونسل
- ریس الائنس ویلز
- رائل کالج آف مڈوائف
- رائل کالج آف نرسنگ
- رائل نیشنل انسٹی ٹیوٹ آف بلائنڈ پیپل (RNIB)
- سکاٹش کوویڈ سوگوار
- سکاٹش ویکسین انجری گروپ
- سیلف ڈائریکٹڈ سپورٹ سکاٹ لینڈ
- Sewing2gether All Nations (پناہ گزینوں کا سپورٹ گروپ)
- سائن ہیلتھ
- یو کے سی وی فیملی
سوگوار، بچوں اور نوجوانوں کے لیے، مساوات، ویلز، اسکاٹ لینڈ اور شمالی آئرلینڈ کے فورمز، اور لانگ کوویڈ ایڈوائزری گروپ کے لیے، ہم اپنے کام پر آپ کی بصیرت، تعاون اور چیلنج کی واقعی قدر کرتے ہیں۔ آپ کے ان پٹ نے اس ریکارڈ کو تشکیل دینے میں ہماری مدد کی۔
مکمل ریکارڈ
1. تعارف
یہ دستاویز Covid-19 ویکسینز اور علاج سے متعلق ہر کہانی کے معاملات کے ساتھ شیئر کی گئی کہانیاں پیش کرتی ہے۔
پس منظر اور مقاصد
ایوری سٹوری میٹرز یوکے بھر کے لوگوں کے لیے یو کے کوویڈ 19 انکوائری کے ساتھ وبائی مرض کے بارے میں اپنے تجربے کا اشتراک کرنے کا ایک موقع ہے۔ شیئر کی گئی ہر کہانی کا تجزیہ کیا گیا ہے اور حاصل کردہ بصیرت کو متعلقہ ماڈیولز کے لیے تھیمڈ دستاویزات میں تبدیل کر دیا گیا ہے۔ یہ ریکارڈ انکوائری کو بطور ثبوت پیش کیا جاتا ہے۔ ایسا کرنے سے، انکوائری کے نتائج اور سفارشات کو وبائی امراض سے متاثر ہونے والوں کے تجربات سے آگاہ کیا جائے گا۔
یہ دستاویز اس چیز کو اکٹھا کرتی ہے جو تعاون کنندگان نے ہمیں وبائی امراض کے دوران CoVID-19 ویکسینز اور Covid-19 کے علاج کے بارے میں اپنے تجربات کے بارے میں بتایا۔
UK CoVID-19 انکوائری اس وبائی مرض کے مختلف پہلوؤں پر غور کر رہی ہے اور اس نے لوگوں کو کیسے متاثر کیا۔ اس کا مطلب ہے کہ کچھ عنوانات دوسرے ماڈیول ریکارڈز میں شامل ہوں گے۔ لہذا، ہر کہانی کے معاملات کے ساتھ اشتراک کردہ تمام تجربات اس دستاویز میں شامل نہیں ہیں۔ مثال کے طور پر، برطانیہ کے صحت کی دیکھ بھال کے نظام کے تجربات اور بچوں اور نوجوانوں پر اثرات کو دوسرے ماڈیولز میں تلاش کیا جاتا ہے اور انہیں ایوری سٹوری میٹرز کے دیگر ریکارڈز میں شامل کیا جائے گا۔
لوگوں نے اپنے تجربات کا اشتراک کیسے کیا۔
ماڈیول 4 کے لیے ہم نے لوگوں کی کہانیاں جمع کرنے کے کئی مختلف طریقے ہیں۔ اس میں شامل ہیں:
- عوام کے ارکان کو ایک مکمل کرنے کے لیے مدعو کیا گیا تھا۔ انکوائری کی ویب سائٹ کے ذریعے آن لائن فارم (کاغذی فارم بھی شراکت داروں کو پیش کیے گئے اور تجزیہ میں شامل کیے گئے)۔ اس نے ان سے اپنے وبائی تجربے کے بارے میں تین وسیع، کھلے سوالات کے جوابات دینے کو کہا۔ فارم میں ان کے بارے میں پس منظر کی معلومات (جیسے ان کی عمر، جنس اور نسل) جمع کرنے کے لیے دوسرے سوالات پوچھے گئے۔ اس سے ہمیں لوگوں کی ایک بہت بڑی تعداد سے ان کے وبائی تجربات کے بارے میں سننے کا موقع ملا۔ آن لائن فارم کے جوابات گمنام طور پر جمع کرائے گئے تھے۔ ماڈیول 4 کے لیے، ہم نے 34,441 کہانیوں کا تجزیہ کیا۔ اس میں انگلینڈ سے 28,246 کہانیاں، اسکاٹ لینڈ سے 2,756، ویلز سے 3,133 اور شمالی آئرلینڈ سے 1,679 کہانیاں شامل تھیں (مطالعہ کنندگان آن لائن فارم میں ایک سے زیادہ یو کے قوم کو منتخب کرنے کے قابل تھے، لہذا کل موصول ہونے والے جوابات کی تعداد سے زیادہ ہوں گے)۔ جوابات کا تجزیہ 'نیچرل لینگویج پروسیسنگ' (NLP) کے ذریعے کیا گیا، جو ڈیٹا کو بامعنی انداز میں ترتیب دینے میں مدد کرتا ہے۔ الگورتھمک تجزیہ کے ذریعے، جمع کی گئی معلومات کو اصطلاحات یا فقروں کی بنیاد پر 'موضوعات' میں ترتیب دیا جاتا ہے۔ اس کے بعد ان موضوعات کا محققین نے جائزہ لیا تاکہ کہانیوں کو مزید دریافت کیا جا سکے۔
- ایوری سٹوری میٹرز کی ٹیم گئی تھی۔ انگلینڈ، ویلز، سکاٹ لینڈ اور شمالی آئرلینڈ کے 25 قصبے اور شہر لوگوں کو ان کی مقامی کمیونٹیز میں ذاتی طور پر اپنے وبائی تجربے کا اشتراک کرنے کا موقع فراہم کرنا۔ اگر اس نقطہ نظر کو ترجیح دی گئی تو ورچوئل سننے کے سیشن بھی منعقد کیے گئے۔ ہم نے بہت سے خیراتی اداروں اور نچلی سطح کے کمیونٹی گروپس کے ساتھ کام کیا تاکہ وبائی امراض سے متاثر ہونے والوں سے مخصوص طریقوں سے بات کی جا سکے۔ اس میں سوگوار خاندان اور افراد، لانگ کووڈ کے ساتھ رہنے والے افراد، طبی لحاظ سے کمزور خاندان، معذور افراد، ویکسین سے زخمی ہونے والے افراد، نوجوانوں کے گروپ، دیکھ بھال کرنے والے، پناہ گزین، نسلی اقلیتی پس منظر کے لوگ اور صحت کی دیکھ بھال کے پیشہ ور افراد شامل تھے۔ ان گروپوں کے ساتھ واقعات کے لیے مختصر خلاصہ رپورٹیں لکھی گئیں، تقریب کے شرکاء کے ساتھ شیئر کی گئیں اور اس دستاویز کو مطلع کرنے کے لیے استعمال کی گئیں۔
- ایوری سٹوری میٹرز کی طرف سے سماجی تحقیق اور کمیونٹی کے پیشہ ور افراد کا ایک کنسورشیم کام کرنے کے لیے مقرر کیا گیا تھا۔ گہرائی سے انٹرویوز اور بحث گروپ مخصوص گروہوں کے تجربات کو سمجھنے کے لیے، اس بنیاد پر کہ ماڈیول قانونی ٹیم کیا سمجھنا چاہتی ہے۔ اس میں وہ لوگ شامل ہیں جن کی صحت سے متعلق خاص خدشات ہیں جنہوں نے ان کے ویکسین کے فیصلوں کو متاثر کیا ہو (جیسے وہ لوگ جو طبی طور پر کمزور یا طبی لحاظ سے انتہائی کمزور تھے۔1 اور وہ لوگ جو حاملہ تھے یا دودھ پلا رہے تھے جب ویکسین کی پیشکش کی گئی تھی) اور وہ گروپ جہاں CoVID-19 ویکسین کا استعمال نسبتاً کم تھا۔ اس میں عوام کے وہ ارکان بھی شامل تھے جنہوں نے ویکسین کے رول آؤٹ کے تجربات کو سمجھنے کے لیے کم از کم ایک ویکسین حاصل کی تھی۔ ان انٹرویوز اور مباحثے کے گروپوں نے ماڈیول 4 کے لیے کلیدی لائنز آف انکوائری (KLOEs) پر توجہ مرکوز کی، جس کے بارے میں معلومات اس دستاویز کے ضمیمہ میں مل سکتی ہیں۔ مجموعی طور پر، انگلینڈ، سکاٹ لینڈ، ویلز اور شمالی آئرلینڈ میں 228 افراد نے اکتوبر 2023 سے دسمبر 2023 کے درمیان اس طرح تعاون کیا۔ تمام گہرائی والے انٹرویوز اور مباحثے کے گروپس کو ریکارڈ کیا گیا، نقل کیا گیا، کوڈ کیا گیا اور ماڈیول سے متعلقہ کلیدی موضوعات کی شناخت کے لیے تجزیہ کیا گیا۔ 4 KLOEs
ان لوگوں کی تعداد جنہوں نے برطانیہ کے ہر ملک میں اپنی کہانیاں آن لائن فارم، سننے والے واقعات اور تحقیقی انٹرویوز اور مباحثہ گروپوں کے ذریعے شیئر کیں:
شکل 1: ہر کہانی برطانیہ بھر میں مصروفیت کو اہمیت دیتی ہے۔
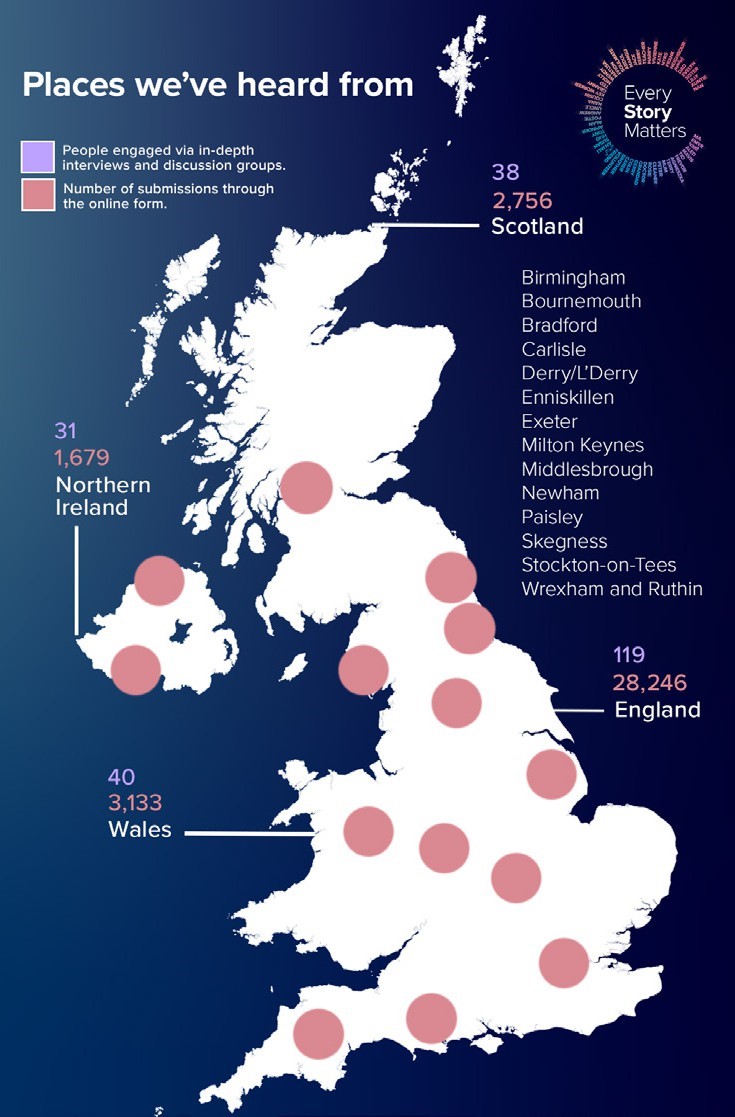
اس بارے میں مزید معلومات کے لیے کہ ہم لوگوں کو کیسے سنتے ہیں اور کہانیوں کا تجزیہ کرنے کے لیے استعمال کیے جانے والے طریقے، ضمیمہ دیکھیں۔
کہانیوں کی پیش کش اور تشریح کے بارے میں نوٹس
یہ نوٹ کرنا ضروری ہے کہ ایوری سٹوری میٹرز کے ذریعے جمع کی گئی کہانیاں وبائی امراض کے دوران کوویڈ 19 ویکسینز کے تمام تجربات کی نمائندہ نہیں ہیں اور نہ ہی برطانیہ کی رائے عامہ کی۔ وبائی مرض نے برطانیہ میں ہر ایک کو مختلف طریقوں سے متاثر کیا، اور جب کہ کہانیوں سے عمومی موضوعات اور نقطہ نظر ابھرتے ہیں، ہم ہر ایک کے منفرد تجربے کی اہمیت کو تسلیم کرتے ہیں۔ اس ریکارڈ کا مقصد مختلف اکاؤنٹس کو ملانے کی کوشش کیے بغیر، ہمارے ساتھ شیئر کیے گئے مختلف تجربات کی عکاسی کرنا ہے۔
ہم نے ان کہانیوں کی عکاسی کرنے کی کوشش کی ہے جو ہم نے سنی ہیں، جس کا مطلب یہ ہو سکتا ہے کہ یہاں پیش کی گئی کچھ کہانیاں اس سے مختلف ہوں جو برطانیہ میں لوگوں نے تجربہ کی ہیں۔
کچھ کہانیوں کو اقتباسات کے ذریعے مزید گہرائی میں تلاش کیا جاتا ہے۔ ان کا انتخاب ان مختلف قسم کے تجربات کو اجاگر کرنے کے لیے کیا گیا ہے جن کے بارے میں ہم نے سنا ہے اور ان کا لوگوں پر کیا اثر پڑا ہے۔ اقتباسات اس بات کو ریکارڈ کرنے میں مدد کرتے ہیں کہ لوگوں نے اپنے الفاظ میں کیا شیئر کیا ہے۔ شراکتیں گمنام کر دی گئی ہیں۔
پورے ریکارڈ کے دوران، ہم ان لوگوں کا حوالہ دیتے ہیں جنہوں نے اپنی کہانیاں ایوری سٹوری میٹرز کے ساتھ 'شراکت کنندگان' کے طور پر شیئر کیں۔ جہاں مناسب ہو، ہم نے ان کے بارے میں مزید بیان بھی کیا ہے (مثال کے طور پر، ان کی نسل یا صحت کی حیثیت) تاکہ ان کے تجربے کے سیاق و سباق اور مطابقت کی وضاحت کی جاسکے۔
2023 اور 2024 کے دوران کہانیاں اکٹھی کی گئیں اور ان کا تجزیہ کیا گیا، اس کا مطلب ہے کہ تجربات ان کے ہونے کے کچھ عرصے بعد یاد رکھے جاتے ہیں۔
ریکارڈ کی ساخت
اس دستاویز کو قارئین کو یہ سمجھنے کی اجازت دینے کے لیے بنایا گیا ہے کہ لوگوں نے CoVID-19 ویکسین کا تجربہ کیسے کیا۔
یہ اس بات کی کھوج سے شروع ہوتا ہے کہ لوگوں نے کوویڈ 19 ویکسین (باب 2) کے بارے میں موصول ہونے والی معلومات کا تجربہ کرنے سے پہلے ان عوامل پر بات کرنے سے پہلے جو لوگوں کو ویکسین حاصل کرنے یا نہ لینے کے فیصلوں سے آگاہ کیا (باب 3)۔ اس کے بعد یہ ان لوگوں کے درمیان ویکسین کے رول آؤٹ کے تجربات کو بیان کرتا ہے جنہوں نے ویکسین حاصل کرنے کا انتخاب کیا (باب 4)، شدید بیماری کے خطرے میں CoVID-19 کے علاج (علاجات) کی دستیابی سے متعلق اثرات کو دیکھنے سے پہلے (باب 5)۔
- ایوری سٹوری میٹرز میں تعاون کرنے والوں میں یہ ہمیشہ ممکن نہیں ہوتا کہ ان لوگوں کی شناخت کی جا سکے جو طبی لحاظ سے کمزور ہیں اور جو طبی لحاظ سے انتہائی کمزور ہیں۔ اس کی وجہ یہ ہے کہ سبھی شراکت داروں نے اپنی کہانیاں شیئر کرتے وقت یہ معلومات فراہم نہیں کیں۔ جہاں ممکن ہو، ہم نے اس بارے میں معلومات شامل کی ہیں کہ آیا تعاون کرنے والے طبی لحاظ سے کمزور ہیں یا طبی لحاظ سے انتہائی کمزور ہیں۔ جب یہ معاملہ نہیں ہے، تو ہم ان تمام لوگوں کے بارے میں بات کرتے ہیں جن سے وبائی امراض کے دوران 'طبی لحاظ سے کمزور' تعاون کرنے والوں کو بچانے کے لیے کہا گیا تھا۔
2. Covid-19 ویکسین کے بارے میں عوامی پیغام رسانی کے تجربات |
 |
یہ باب بیان کرتا ہے کہ تعاون کرنے والوں نے ہمیں وبائی امراض کے دوران کوویڈ 19 ویکسینز کے بارے میں موصول ہونے والی معلومات کے بارے میں کیا بتایا۔ ہم نے حکومت اور NHS کی طرف سے سرکاری رہنمائی کے بارے میں لوگوں کی آراء اکٹھی کیں۔ ہم نے معلومات کے دیگر ذرائع کے بارے میں بھی سنا جو روایتی اور سوشل میڈیا، دوستوں، خاندان، مذہبی ترتیبات اور کمیونٹی گروپس سمیت استعمال کیے گئے تھے۔
تعاون کرنے والوں نے CoVID-19 ویکسینز کے بارے میں پہلی بار کیسے سنا اور انہیں کیا محسوس ہوا۔
بہت کم تعاون کرنے والے بالکل ٹھیک یاد کر سکتے ہیں جب انہوں نے پہلی بار سنا تھا کہ CoVID-19 کے لیے ایک ویکسین تیار کی گئی ہے۔ وہ اکثر اس بات کی عکاسی کرتے تھے کہ برطانیہ میں پہلے لاک ڈاؤن کے بعد سے ویکسین گفتگو کا موضوع رہی ہیں۔ اس کا مطلب تھا کہ ویکسین ایسی چیز تھی جس پر انہوں نے دوستوں یا خاندان کے ساتھ باقاعدگی سے تبادلہ خیال کیا تھا، اور یہ کہ انہوں نے خبروں یا سوشل میڈیا پر دیکھا، سنا یا پڑھا تھا۔
| " | یہ صرف اس کا ایک حصہ تھا - اس کے بارے میں بات کرنے کے لئے اور کچھ نہیں تھا، خبروں میں اور کچھ نہیں تھا۔ کوئی بھی کووڈ ویکسین کے علاوہ کسی چیز کے بارے میں بات نہیں کر رہا تھا"
- ہر کہانی اہم شراکت دار |
CoVID-19 ویکسینز کے بارے میں سب سے زیادہ وابستہ ابتدائی معلومات ٹی وی خبروں پر ان کے بارے میں سننے کے ساتھ۔ صحت کی دیکھ بھال کی ترتیبات میں کام کرنے والے کچھ شراکت داروں نے یہ بھی کہا کہ ان سے ان کے کام کی جگہ پر تبادلہ خیال کیا گیا تھا۔
| " | میں کہوں گا کہ جب میں نے اسے پہلی بار دیکھا، تو یہ خبروں پر تھی… میں اس کے بارے میں کافی خوش تھا، کیونکہ وہ ہمارے لیے یہ تیزی سے تیار کر رہے ہیں تاکہ ہم کوشش کر کے معمول کی زندگی میں واپس جا سکیں۔
- ہر کہانی اہم شراکت دار |
| " | میں نے پہلی بار اس کے بارے میں کام کے ذریعے سنا، اور ایک کلیدی کارکن ہونے کے ناطے، ہم اسے حاصل کرنے کے قابل ہونے کے لیے تیزی سے ٹریک کیے گئے، اور جب میں نے پہلی بار اس کے بارے میں سنا۔ مجھے صحیح تاریخیں یاد نہیں ہیں۔"
- ہر کہانی اہم شراکت دار |
یہ سن کر کہ ایک ویکسین کو استعمال کے لیے منظور کر لیا گیا ہے، بہت سے جذبات کے ساتھ ملا۔ کچھ لوگوں کے لیے راحت اور امید کے مثبت جذبات کا غلبہ ہے۔ اس میں بہت سے وہ لوگ شامل تھے جو طبی لحاظ سے کمزور یا طبی لحاظ سے انتہائی کمزور تھے، کسی کمزور دوست یا خاندان کے رکن کی دیکھ بھال کر رہے تھے، یا جو خود بوڑھے تھے۔ ایک ویکسین کو ان کی زندگیوں کو معمول پر آنے کا پہلا حقیقت پسندانہ موقع پیش کرنے کے لیے دیکھا گیا: بہت سے لوگ وبائی مرض کے شروع ہونے کے بعد سے لوگوں کے ساتھ گھل مل جانے کے بارے میں حفاظت کر رہے تھے یا پھر محتاط تھے۔
| " | جب اس بات کی تصدیق ہوئی کہ ویکسین دستیاب ہے، تو سب سے پہلی چیز جو میں نے محسوس کی، ذاتی طور پر، اس نے مجھے امید دلائی، کیونکہ میں اس وقت مایوس کن صورتحال میں تھا، اور اسی وجہ سے میں اس فہرست میں پہلا ہونا چاہتا تھا۔ ایسا محسوس ہوا جیسے سرنگ کے آخر میں روشنی تھی، یہ بہت اطمینان بخش تھا۔
- طبی لحاظ سے کمزور شراکت دار |
| " | مجھے دمہ ہے اور میرے سسر کو بھی کینسر ہے، لہٰذا جب ہم نے ویکسین کے بارے میں سنا تو یہ ہمارے خاندان کے ہر فرد کے لیے راحت کی سانس تھی۔
- ہر کہانی اہم شراکت دار |
تاہم، دوسروں نے ویکسین کے بارے میں زیادہ ملے جلے یا منفی جذبات کا اظہار کیا۔ ان شراکت داروں نے ویکسین کے بارے میں محتاط یا شکی محسوس کرنے کے بارے میں بات کی۔ اکثر اس کا تعلق اس رفتار سے متعلق خدشات سے ہوتا ہے جس سے ویکسین تیار کی گئی تھیں، جس نے ان کی حفاظت اور تاثیر کے بارے میں سوالات اٹھائے تھے۔
| " | تو، میرے لیے، مجھے ویکسین لگوانے میں کوئی مسئلہ نہیں تھا۔ میرا مسئلہ یہ تھا، 'کیا ویکسین میرے لیے کافی محفوظ تھی؟' اگر یہ میرے لیے محفوظ رہنے کے لیے تمام جانچ پڑتال کر لیتا، کیونکہ میں جانتا ہوں کہ ویکسین کام کرتی ہیں اور وہ مدد کرتی ہیں۔ تو، یہ میرا مخمصہ تھا لیکن اس وقت ویکسین لگائی جا رہی تھی۔ مجھے شک تھا کہ یہ تمام اخلاقی جانچ پڑتال سے گزر چکا ہے اور وہ تمام چیک جو اس کے لیے ضروری تھے کہ میرے لیے محفوظ رہیں۔ لہذا، یہ شروع میں میرا مسئلہ تھا."
- ہر کہانی اہم شراکت دار |
| " | مجھے لگتا ہے کہ یہ کہنا مناسب ہے کہ جس رفتار سے یہ باہر آیا اس نے کچھ لوگوں کے ساتھ تھوڑا سا نرمی چھوڑی۔ اسے بہت تیزی سے نافذ کیا گیا تھا، جہاں دیگر ویکسینز کو مارکیٹ میں آنے میں کئی سال لگے ہیں۔ تو قدرتی طور پر تھوڑا سا میرے خیال میں عام خوف تھا۔
- ہر کہانی اہم شراکت دار |
CoVID-19 ویکسینز کے بارے میں سرکاری رہنمائی
تعاون کنندگان نے CoVID-19 ویکسینز کے بارے میں سرکاری رہنمائی کے بارے میں سوچا کہ انہوں نے خبروں میں، سرکاری بریفنگ میں یا براہ راست NHS سے حاصل کی (صحت کی دیکھ بھال کرنے والے پیشہ ور افراد کے ساتھ ملاقاتوں میں، آن لائن، NHS ایپ کے ذریعے، وغیرہ)۔ لوگوں کو ویکسین لینے کی دعوت دینے والے خطوط اور پیغامات کو بھی سرکاری معلومات کے طور پر دیکھا گیا۔
کوویڈ 19 ویکسین کے بارے میں سرکاری رہنمائی کی وضاحت کے بارے میں رائے ملے جلے تھے۔ عام طور پر، شراکت داروں نے محسوس کیا کہ بعض گروہوں کی ترجیح اور ویکسین حاصل کرنے کے عمل کے بارے میں رہنمائی واضح تھی۔ تاہم، کچھ لوگوں نے محسوس کیا کہ ویکسین کی حفاظت اور تاثیر کے بارے میں رہنمائی مبہم تھی۔ تعاون کرنے والوں نے فرض کیا کہ جس نے بھی ویکسین حاصل کی ہے اس کے CoVID-19 کا شکار ہونے کا بہت امکان نہیں ہوگا (دوسری بیماریوں کے لیے کچھ ویکسین کے ان کے تجربات کی بنیاد پر)۔ جب وہ یا کوئی ایسا شخص جانتا تھا جس نے بعد میں کووِڈ 19 کو ویکسین لگائی تھی تو اس نے ان کے لیے سوالات اٹھائے کہ آیا یہ ویکسین کام کرتی ہیں۔ اس الجھن کو محسوس نہیں کیا گیا کہ Covid-19 ویکسینز پر دستیاب سرکاری رہنمائی کے ذریعے اس کا ازالہ کیا گیا ہے۔
| " | جو کچھ مجھے یاد ہے، میرے خیال میں یہ بالکل واضح تھا۔ آپ کو آپ کا خط مل گیا، یہ ساری خبروں میں تھی کہ وہ آپ کو کیا کرنے کو کہہ رہے تھے۔ مشورہ یقینی طور پر وہاں تھا۔
- ہر کہانی اہم شراکت دار |
| " | میں نے انجکشن لگایا تھا اور پھر بھی مجھے COVID ہو گیا۔ میں نے محسوس کیا کہ ایک بار مجھے اپنا انجکشن لگ گیا تو میں COVID نہیں پکڑ سکوں گا، میں یہی سوچ رہا تھا، لیکن ایسا کیوں ہوا کہ میں نے انجکشن لگایا اور پھر بھی مجھے COVID تھا؟ تو مجھے لگتا ہے کہ انجکشن کام نہیں کر رہا تھا۔
- ہر کہانی اہم شراکت دار |
شراکت دار اس بارے میں بھی فکر مند تھے کہ سرکاری رہنمائی میں ویکسین کے ممکنہ منفی ضمنی اثرات کیسے بتائے گئے۔ خاص طور پر یہ ان لوگوں کے لیے اہم تھا جو پہلے سے موجود صحت کی حالتوں میں مبتلا ہیں جو یہ جاننا چاہتے تھے کہ ویکسین ان کی حالت کے ساتھ کیسے تعامل کر سکتی ہے اور کیا اس سے انہیں منفی اثرات کا خطرہ بڑھ جاتا ہے۔
| " | ایک باخبر فیصلہ کرنے اور باخبر رضامندی دینے کے لیے تمام حقائق کو دستیاب کرایا جانا چاہیے تھا، بشمول jabs کے ممکنہ ضمنی اثرات۔"
- ہر کہانی اہم شراکت دار |
| " | اس کے اثرات کے بارے میں بہت زیادہ تحقیق نہیں ہوئی تھی جو طبی طور پر اس حوالے سے ہو سکتی ہے کہ آیا آپ کی صحت کی حالت جاری ہے۔ میں ویکسینیشن کے طویل مدتی اثرات اور کیا ہو سکتا ہے اس کے بارے میں تھوڑا محتاط تھا۔
- ایک طویل مدتی صحت کی حالت کے ساتھ شخص |
شراکت داروں نے یہ بھی ظاہر کیا کہ استعمال کی جانے والی زبان اور سرکاری رہنمائی میں شامل تصورات اکثر فقرے بھرے ہوتے تھے اور اس میں طبی زبان بھی شامل تھی۔ اس نے کچھ لوگوں کے لیے رہنمائی کو سمجھنا مشکل بنا دیا، اور انھوں نے اس کے نتیجے میں باخبر فیصلہ کرنے سے قاصر ہونے کے بارے میں بات کی۔ الجھن کا ایک مخصوص علاقہ عوام کے لیے دستیاب مختلف قسم کی ویکسین کے ارد گرد تھا۔
| " | میں یہ نہیں کہوں گا کہ اتنی معلومات موجود تھیں جو میں سمجھتا ہوں - لیکن مجھے لگتا ہے کہ وہاں کافی معلومات موجود ہیں کہ، اگر کوئی اسے سمجھتا ہے تو وہ مجھے بہتر طریقے سے سمجھا سکتا ہے، شاید میں اسے تب سمجھ سکتا۔"
- ہر کہانی اہم شراکت دار |
| " | مجھے دو ویکسین کے درمیان فرق سمجھ نہیں آیا، فائزر ایک اور دوسری۔ مجھے یاد ہے کہ ہمارے ایک دوست کو ایک مل گیا تھا، اور دوسرے کو دوسرا مل گیا تھا، اور میں اس طرح تھا، 'آپ کو کیسے معلوم کہ کون سا حاصل کرنا ہے؟' تو یہ ایک اور چیز ہے جس کے بارے میں میں نے محسوس کیا کہ انہوں نے واقعی وضاحت نہیں کی۔
- ہر کہانی اہم شراکت دار |
کچھ تعاون کرنے والے ایسے تھے جنہوں نے ان کے لیے قابل رسائی فارمیٹ میں معلومات حاصل کرنے میں مشکل محسوس کرنے کی وضاحت کی۔ اس میں وہ لوگ شامل تھے جو بصارت سے محروم ہیں یا وہ لوگ جن کے لیے انگریزی ان کی پہلی زبان نہیں تھی۔
| " | میرے خیال میں اگر آپ انگریزی سمجھتے ہیں، تو یہ ٹھیک تھا، لیکن اگر میں اپنی وسیع برادری کے بارے میں سوچتا ہوں، تو ان میں سے کچھ ضروری طور پر انگریزی کو اتنی اچھی طرح سے نہیں سمجھتے، اور یہ ان کے لیے مشکل تھا، اور مجھے یہ معلومات حاصل نہیں ہوئیں۔ ایک مختلف فارمیٹ میں… اچھا ہوتا اگر وہ اس معلومات کو ان لوگوں کے لیے دستیاب کرنے کا موقع تلاش کرتے جو انگریزی نہیں بولتے، کمیونٹی لنک لیڈر، امام، یا اس جیسی کوئی چیز تلاش کرتے۔
- ہر کہانی اہم شراکت دار |
| " | میری بیٹی نے انٹرنیٹ سے بہت ساری معلومات حاصل کرنے میں ہماری مدد کی، لیکن ہم مایوس تھے کہ ہمارے پاس قابل رسائی فارمیٹس میں معلومات نہیں تھیں۔ بہت ساری بصری تصاویر تھیں جنہیں معاون ٹیکنالوجی نہیں پڑھ سکتی۔
- بینائی سے محروم شخص |
| " | مستقبل میں ہمیں بہت زیادہ واضح پیغام رسانی کی ضرورت ہے، خاص طور پر پسماندہ کمیونٹیز کے لیے۔ لوگ طبی پیشوں پر بھروسہ کرتے ہوئے تھک جاتے ہیں اور مختلف کمیونٹیز میں زبان کی مختلف رکاوٹیں ہوتی ہیں۔ کمیونٹیز کے مارے جانے کا یہ احساس تھا، خاندان کے لوگ کہہ رہے تھے کہ 'وہ یہاں ہمیں لینے آئے ہیں، ویکسین نہیں لگوائیں'۔ لوگوں کو ان کی اپنی زبان میں یقین دلانے کے لیے بہت کم کام کیا گیا، بہت سے نوجوانوں نے اس کا ترجمہ کرنے کا بوجھ اٹھایا۔
- ہر کہانی اہم شراکت دار |
ایسے لوگ بھی تھے جنہوں نے محسوس کیا کہ سرکاری رہنمائی نے ان کے مذہبی عقائد سے متعلق خدشات کو دور نہیں کیا۔ مثال کے طور پر، کچھ مسلمان شراکت داروں نے اس بارے میں بات کی کہ ویکسین حلال ہیں یا نہیں اس بارے میں معلومات حاصل کرنا مشکل ہے۔
| " | مجھے لفظی طور پر اپنے NHS ساتھی کو فون کرنا پڑا، کیونکہ میں اس وقت NHS کے لیے کام کر رہا تھا۔ میں نے اپنے ساتھی کو فون کیا اور میں نے کہا، 'دیکھو، میں ہر ویکسینیشن کے اجزاء جاننا چاہتا ہوں، کیونکہ اجزاء میں کیا ہے اس پر منحصر ہے، اگر وہاں جانوروں کی چربی یا اس جیسی چیزیں موجود ہیں، تو ہم اسے نہیں لے سکتے۔ . یہ سبزی خوروں یا سبزی خوروں کے لیے موزوں ہونا چاہیے۔' اور پھر وہ واپس چلے گئے اور انہوں نے کہا کہ یہ ٹھیک ہے۔ اس عقیدے کے تمام لوگ، آپ یہ ویکسینیشن لے سکیں گے۔' تو، میں ایک فرد تھا جس نے یہ سوال کیا۔ یہ معلومات آسانی سے دستیاب نہیں تھیں۔"
- ایک مسلمان عقیدے کا فرد |
تاہم، بہت سے لوگوں نے وبائی امراض کے دوران حکومت کو درپیش چیلنجوں کا اعتراف کیا۔ انہوں نے حکومت کو ویکسین کے بارے میں جو کچھ معلوم تھا اس کی بنیاد پر وہ اس وقت جو کچھ کر سکتی تھی وہ کر رہی تھی۔
| " | ویکسین زندگی بچانے والی مداخلت تھی، اور، میرا اندازہ ہے کہ، ہماری زندگی میں، یہ ان جھلکیوں میں سے ایک ہوگی جس کا ہم نے مشاہدہ کیا ہے۔ انہوں نے میرے سمیت سینکڑوں لوگوں کو بچایا۔ مجھے خوشی ہے کہ میں یہ ویکسین لینے میں کامیاب ہوگیا۔ عمل واقعی اچھا تھا۔ میرا اندازہ ہے کہ حکومت نے جتنا وہ کر سکتے تھے، کیا کیونکہ کچھ بھی کامل نہیں ہے۔
- ہر کہانی اہم شراکت دار |
| " | میرے خیال میں، سچ پوچھیں تو، ان کو اس وجہ سے خراج تحسین پیش کرتا ہوں جس طرح انہوں نے اسے سنبھالا۔ دن کے اختتام پر، یہ ایک وبائی بیماری تھی، وہاں لوگ واقعی جدوجہد کر رہے تھے، ہم لاک ڈاؤن میں تھے، اور وہ اپنی ہر ممکن کوشش کر رہے تھے جو وہ کر سکتے تھے۔ وہ صرف انسان ہیں۔"
- ہر کہانی اہم شراکت دار |
حاملہ یا دودھ پلانے والے لوگوں کے لئے سرکاری رہنمائی کی مطابقت
دسمبر 2020 کے آغاز میں، ویکسینیشن اور حفاظتی ٹیکوں کی مشترکہ کمیٹی (JCVI) کی طرف سے مشورہ یہ تھا کہ چونکہ حمل میں کووِڈ-19 ویکسین کی حفاظت کے بارے میں کوئی ڈیٹا نہیں تھا، اس لیے حاملہ خواتین کو کووِڈ-19 ویکسین کی پیشکش نہیں کی جانی چاہیے۔ 30 دسمبر 2020 کو، تازہ ترین JCVI مشورہ یہ تھا کہ حاملہ خواتین کو ویکسینیشن کی پیشکش کی جا سکتی ہے جہاں انہیں CoVID-19 کی وجہ سے نمائش یا سنگین پیچیدگیوں کا خاص طور پر زیادہ خطرہ ہو۔ اپریل 2021 میں، JCVI نے اپنے مشورے کو دوبارہ اپ ڈیٹ کیا، یہ مشورہ دینے کے لیے کہ حاملہ خواتین کو CoVID-19 ویکسین کی پیشکش کی جائے کیونکہ حمل کے سلسلے میں CoVID-19 ویکسین میں سے کسی کے ساتھ حفاظتی خدشات کی نشاندہی نہیں کی گئی تھی۔
حمل کے دوران ویکسینیشن کے بارے میں سرکاری رہنمائی کی بدلتی ہوئی نوعیت بہت سی خواتین کے لیے الجھن کا باعث تھی جن سے ہم نے بات کی۔ کچھ جو وبائی امراض کے دوران حاملہ تھے انہوں نے سوال کیا کہ مشورہ کیوں تبدیل ہوا کیوں کہ انہوں نے اس کی وضاحت کے لئے ثبوت یا دستیاب معلومات میں کوئی تبدیلی نہیں دیکھی۔ ان لوگوں کے لیے جنہوں نے اس طرح محسوس کیا بدلتی رہنمائی نے ان کے لیے اضافی تناؤ اور اضطراب کا باعث بنا جو پہلے ہی پریشان کن وقت تھا۔
| " | مجھے یاد ہے کہ وہ خاص طور پر کہتے تھے، 'جو کوئی حاملہ ہو یا حاملہ ہونے کی کوشش کر رہا ہو اسے ویکسین نہیں لگوانی چاہیے۔' اس پر ایک پوری آزمائش تھی اور مجھے یاد ہے کہ یہ بہت ضروری تھا کہ آپ کو ویکسین نہیں لگنی چاہیے۔ ہم حاملہ ہونے کی کوشش کر رہے تھے اور پھر جب میں حاملہ ہو گئی تو ظاہر ہے کہ میرے پاس ویکسین نہیں تھی، دائیوں نے اس بات کی تصدیق کی کہ مجھے نہیں لینا چاہیے، اس وقت اس کی سفارش نہیں کی گئی تھی۔ اور پھر اچانک میرے حمل کے آدھے راستے میں حالات میں تبدیلی آئی اور حاملہ لوگوں کو ویکسین کی اجازت دی گئی جس کے بارے میں میں نے سوچا کہ یہ بہت، بہت عجیب اور بہت پریشان کن ہے۔"
- وہ عورت جو حاملہ تھی جب اسے ویکسین دی گئی۔ |
جن خواتین سے ہم نے بات کی ان میں بنیادی تشویش یہ تھی کہ ویکسین ان کے اسقاط حمل کا سبب بن سکتی ہے یا ان کے پیدا ہونے والے بچے کو نقصان پہنچا سکتی ہے۔ انہوں نے ہمیں بتایا کہ کس طرح سرکاری رہنمائی نے ان خدشات کو دور کرنے کے لئے کافی کام نہیں کیا، جو اس احساس سے پیچیدہ تھے کہ صحت کے پیشہ ور افراد کو بھی یقین نہیں تھا کہ کیا مشورہ دیا جائے۔ کچھ لوگوں کے لیے، اس غیر یقینی صورتحال نے انہیں یہ فیصلہ کرنے پر مجبور کیا کہ وہ اس وقت تک ویکسین نہ لگائیں جب تک کہ وہ جنم نہ لے لیں۔
| " | میں اس وقت حاملہ تھی اس لیے کہ انہوں نے کہا تھا کہ جب تک آپ حاملہ ہیں اسے حاصل نہ کریں اور پھر فیصلہ بہت جلد کیا گیا کہ وہ کہہ سکتے ہیں، اس نے مجھے گھبرا دیا۔ کیونکہ یہ صرف فیصلے میں تبدیلی تھی، جیسے، راتوں رات۔ تو، میرے دماغ میں میں نے مسلسل سوچا، 'اچھا انہوں نے پہلے کیوں نہیں کہا؟' اور پھر میں نے فیصلہ کیا، کیونکہ میرا اسقاط حمل ہو گیا تھا اور میں اپنے جسم میں ایسی کوئی چیز نہیں چاہتا تھا جو اس حمل کو نقصان پہنچا سکے۔ اس لیے میں نے فیصلہ کیا کہ جب میں حاملہ تھی ویکسین نہیں لگوانی۔ مجھے اس کے بعد مل گیا۔"
- وہ عورت جو حاملہ تھی جب اسے ویکسین دی گئی۔ |
| " | ہم اپنی فارمیسیوں، GPs کے پاس نہیں جا سکتے تھے، اور 'ٹھیک ہے، ٹھیک ہے، یہ بالکل کیا ہے؟' کیونکہ ہمارے پاس واقعی یہ آپشن نہیں تھا۔ اور مجھے نہیں لگتا کہ صحت کے بہت سے پیشہ ور بھی جانتے تھے۔
- وہ عورت جو حاملہ تھی جب اسے ویکسین دی گئی۔ |
ہم نے جن خواتین سے بات کی تھی ان میں سے کچھ نے بھی اسی طرح کے خدشات کا اظہار کیا تھا جو ویکسین کی پیشکش کے وقت دودھ پلا رہی تھیں۔ ان تعاون کنندگان نے اس بارے میں فکر مند ہونے کے بارے میں بات کی کہ یہ ویکسین اس بچے کو کیسے متاثر کر سکتی ہے جو وہ دودھ پلا رہے تھے: کیا یہ ان کے بچے کو بیمار کر دے گا، یا یہ انہیں CoVID-19 کے خلاف تحفظ فراہم کرے گا؟ ایک بار پھر، یہ محسوس کیا گیا کہ سرکاری مشورے نے اس پوزیشن میں رہنے والوں کے لیے وضاحت فراہم نہیں کی۔
| " | میرا سب سے بڑا سوال یہ تھا کہ میں دودھ پلا رہا تھا، تو کیا یہ میرے بچے پر اثر انداز ہونے والا ہے… کیا یہ میری چھاتی کے دودھ میں جانے والا ہے، کیا یہ میرے نوزائیدہ بچے کو متاثر کرنے والا ہے، کیا یہ کچھ کرنے والا ہے، کیا یہ مجھے بنا دے گا؟ بیمار؟"
- وہ عورت جو دودھ پلا رہی تھی جب ویکسین پیش کی گئی۔ |
میڈیا میں CoVID-19 ویکسین کے بارے میں معلومات
تعاون کنندگان نے وبائی امراض کے دوران میڈیا میں CoVID-19 ویکسینز کے بارے میں مختلف قسم کی معلومات دیکھنے کو بیان کیا۔ اس میں ویکسین کی ترقی اور جانچ کے بارے میں معلومات اور اس کے شروع ہونے کے بعد رول آؤٹ کی پیشرفت کے بارے میں باقاعدہ اپ ڈیٹس شامل ہیں۔
کوویڈ 19 ویکسین کے بارے میں میڈیا میں آنے والی معلومات پر ملا جلا خیالات تھے۔ کچھ شراکت داروں نے محسوس کیا کہ دستیاب معلومات کا مقصد ویکسین لینے سے وابستہ خطرات اور فوائد کے بارے میں متوازن بحث فراہم کرنے کے بجائے اپٹیک کی حوصلہ افزائی کرنا ہے۔ اس کی وجہ سے وہ روایتی میڈیا کے ذریعے دستیاب معلومات پر عدم اعتماد کرتے ہیں اور کہیں اور سے معلومات حاصل کرتے ہیں۔
| " | میں نے جو دیکھا، شاید حکومت کی طرف سے، لیکن خبروں اور آن لائن میں صرف یہ تھا، 'یہ حاصل کریں، آپ کو یہ حاصل کرنے کی ضرورت ہے، آپ کو یہ ویکسین لینا ہوگی۔' واقعی بس اتنا ہی تھا، ایسا لگتا تھا جیسے یہ آپ پر زبردستی کیا جا رہا ہو!"
- وہ شخص جس نے ویکسین نہ لینے کا انتخاب کیا۔ |
| " | مین اسٹریم میڈیا بہت زیادہ پوزیشن میں تھا، آپ جانتے ہیں، 'ٹھیک ہے، یہ بہت اچھا ہے۔ یہ ہے'، اور کیا نہیں۔ تاہم، اس وقت یوٹیوب پر مختلف کہانیاں تھیں۔ مین اسٹریم میڈیا پر آپ کو کبھی منفی نہیں ملا، سب کچھ مثبت تھا اور اب بھی مثبت ہے۔ تاہم، اگر آپ نے قدرے گہرائی میں دیکھا اور آپ اس پر یقین کرنا چاہتے ہیں جو آپ نے ان دوسرے چینلز پر دیکھا، یہ اتنا مثبت نہیں تھا۔
- وہ شخص جس نے ویکسین نہ لینے کا انتخاب کیا۔ |
تاہم، دوسروں نے روایتی ذرائع ابلاغ کے ذریعے فراہم کی جانے والی باقاعدہ اپ ڈیٹس کو ویکسین کی ترقی میں سرفہرست رہنے کا ایک مفید طریقہ پایا۔ دوسروں نے ویکسینز اور وبائی مرض کے بارے میں معلومات کی مقدار اور بحث سے مغلوب ہونے کا ذکر کیا ، جس کی وجہ سے وہ 'سوئچ آف' ہوئے اور 'فرار ہونے' کی کوشش کی۔
| " | جہاں بھی آپ گئے وہاں نشانیاں تھیں، ہر چینل، ہر آؤٹ لیٹ جس کا آپ تصور کر سکتے ہیں، یہ سب کچھ اس CoVID-19 ویکسین کے بارے میں تھا۔ کوئی سانس نہیں تھا، مجھے یہ احساس کیسے یاد ہے. کافی وقت ہو گیا ہے لیکن مجھے صرف یاد ہے کہ میں کوویڈ کی معلومات پر بمباری محسوس کر رہا ہوں، درحقیقت یہ اتنا برا تھا کہ مجھے خبروں کو بند کرنا یاد ہے، میں نے مزید نہیں سنا کیونکہ میرے پاس کافی تھا۔
- ہر کہانی اہم شراکت دار |
سوشل میڈیا پر کوویڈ 19 ویکسین کے بارے میں معلومات
تعاون کنندگان نے فیس بک، انسٹاگرام، ٹک ٹاک، ٹویٹر، اسنیپ چیٹ، یوٹیوب اور واٹس ایپ سمیت سوشل میڈیا پلیٹ فارمز کی ایک رینج میں کوویڈ 19 ویکسینز کے بارے میں معلومات دیکھ کر یاد کیا۔ اکثر انہوں نے محسوس کیا کہ سوشل میڈیا پر شیئر کی جانے والی معلومات کا لہجہ بنیادی طور پر منفی تھا، خاص طور پر جب رول آؤٹ جاری تھا۔ تعاون کرنے والوں نے ان لوگوں کے بارے میں کہانیوں کی بڑھتی ہوئی تعداد کو یاد کیا جنہوں نے شدید منفی ردعمل کا سامنا کیا تھا یا جو ویکسین کے بعد مر گئے تھے۔ بہت سے لوگوں نے اس بات کی عکاسی کی کہ ان کہانیوں کی وجہ سے ویکسین کے ارد گرد خوف اور شکوک کا ماحول پیدا ہوا۔ بدلے میں، انہوں نے محسوس کیا کہ اس نے ویکسین کے بارے میں افواہوں کو تیز کرنے کی اجازت دی۔
| " | سوشل میڈیا پر، آپ نے خوفناک کہانیاں سنی ہیں، اور مجھے ایسا لگتا ہے کہ آپ شاید ہمیشہ اس قسم کی باتیں سنتے رہیں گے۔ مجھے یاد ہے کہ ان میں سے ایک کے بارے میں کچھ تھا کہ وہ کسی نہ کسی مقام پر خون کے لوتھڑے سے جڑے ہوئے تھے۔ مجھے لگتا ہے کہ یہ جان کر کہ میں اب کیا کرتا ہوں، مجھے ایسا لگتا ہے جیسے یہ تناسب سے مکمل طور پر اڑا ہوا تھا۔
- ہر کہانی اہم شراکت دار |
ان منفی تجربات نے کچھ لوگوں کو یہ محسوس کرنے پر مجبور کیا کہ آن لائن ویکسین کے بارے میں بہت زیادہ غلط یا معلومات موجود ہیں۔ ہم نے بہت سے لوگوں سے سنا جنہوں نے کہا کہ انہیں سوشل میڈیا پر جو کچھ دیکھا اس پر بھروسہ نہیں کیا۔ تاہم، یہاں تک کہ ان لوگوں میں سے کچھ جو سوشل میڈیا پر بھروسہ نہیں کرتے تھے سوچا کہ جو پیغامات انہوں نے دیکھے ہیں اس نے ویکسین کے بارے میں ان کے تاثرات کو متاثر کیا ہے، اور ممکنہ طور پر ان کے فیصلوں کو شکل دی ہے کہ آیا اسے وصول کیا جائے یا نہیں۔
| " | میں جانتا ہوں کہ سوشل میڈیا پر موجود چیزیں واقعی قابل بھروسہ نہیں تھیں لیکن مجھے لگتا ہے کہ میں نے اسے دیکھا تھا تب اس نے میرے دماغ میں بہت بڑا کردار ادا کیا جب میں یہ سوچ رہا تھا کہ آیا میں حاصل کرنا چاہتا ہوں یا نہیں۔ [ایک ویکسین]"
- وہ شخص جس نے ویکسین نہ لینے کا انتخاب کیا۔ |
ان مظاہر کے باوجود، کچھ ایسے تھے جنہوں نے محسوس کیا کہ سوشل میڈیا نے انہیں کوویڈ 19 ویکسینز کے منفی تجربات کے بارے میں براہ راست اس طرح سے سننے کی اجازت دی جو دوسرے ذرائع سے ممکن نہیں تھا۔. ان شراکت داروں کا خیال تھا کہ ویکسین کے منفی تجربات کو روایتی میڈیا آؤٹ لیٹس اور حکومت نے کم رپورٹ کیا ہے، اور اس لیے ان کہانیوں کو سننے کے لیے سوشل میڈیا پر انحصار کیا۔
| " | مجھے یاد ہے کہ وہ واحد جگہ تھی جہاں میں نے بری سچی کہانیاں دیکھی تھیں، سوشل میڈیا پر، یہ خبریں واقعی ویکسین کے بارے میں ایسی کوئی بری رپورٹ نہیں کر رہی تھیں جو مجھے یاد ہے۔"
- ہر کہانی اہم شراکت دار |
Covid-19 ویکسینز کے بارے میں معلومات کے دیگر ذرائع
تعاون کرنے والے اکثر کووڈ-19 ویکسینز کے بارے میں روایتی اور سوشل میڈیا کے ذریعے دستیاب سرکاری رہنمائی اور معلومات سے ہٹ کر ذرائع سے معلومات مانگتے ہیں۔ اس میں صحت کی دیکھ بھال کے پیشہ ور افراد، دوست اور خاندان کے افراد شامل تھے۔
صحت کی دیکھ بھال کے پیشہ ور افراد
صحت کی دیکھ بھال کرنے والے پیشہ ور افراد کوویڈ 19 ویکسین کے بارے میں معلومات کا ایک اہم ذریعہ تھے، خاص طور پر ان لوگوں کے لیے جو طبی لحاظ سے کمزور، طبی لحاظ سے انتہائی کمزور، حاملہ یا دودھ پلانے والے تھے۔ ان شراکت داروں نے بھروسہ کیا کہ ڈاکٹروں، نرسوں اور دائیوں کا مشورہ ویکسین کے طبی علم اور ان سے منسلک خطرات اور فوائد پر مبنی تھا۔ انہوں نے یہ بھی محسوس کیا کہ فراہم کردہ مشورہ ان کے مطابق تھا کیونکہ یہ لوگ اپنی ذاتی طبی تاریخ کو سمجھتے تھے۔
| " | میرے مشیر نے مجھے اپنے بارے میں معلومات بھیجیں۔ [صحت کی حالت]. کچھ ایسی چیزیں تھیں جو عوام کے لیے بڑے پیمانے پر شائع کی گئی تھیں… اور مجھے مزید مخصوص معلومات دی گئیں۔ اس نے اسے ان لوگوں کے لئے تھوڑا سا توڑ دیا جن کے پاس ہے۔ [حالت] اور اس کے امکانات۔ اس نے تمام محاورات کو تھوڑا سا دور کیا اور تھوڑا سا احمقوں کی رہنمائی کی کہ اس کا ہمارے لئے کیا مطلب ہے۔
- طبی لحاظ سے کمزور شراکت دار |
تاہم تمام شراکت داروں کو ان کے صحت کی دیکھ بھال کرنے والے پیشہ ور افراد سے موزوں مشورے نہیں ملے۔ کچھ لوگوں نے اس بارے میں بہت محدود معلومات حاصل کرنے کا بیان کیا کہ CoVID-19 ویکسین ان کی صحت کی مخصوص حالت (حالات) یا حمل کے لیے کیا معنی رکھتی ہیں۔
| " | مجھے بہت واضح طور پر یاد ہے کہ بہت زیادہ معلومات دستیاب نہیں تھی، مجھے فون کرنا پڑا اور پیچھا کرنا پڑا اور مزید معلومات حاصل کرنے کی کوشش کرنی پڑی۔ تو میں اپنے حصے کے لیے جانتا ہوں، میں ہی کام کر رہا تھا۔ آپ جی پی سے بالکل نہیں مل سکے۔"
- ہر کہانی اہم شراکت دار |
مزید وسیع طور پر، وہ تعاون کنندگان جو طبی طور پر کمزور نہیں تھے یا CoVID-19 سے زیادہ خطرے میں تھے، انہوں نے ہمیں بتایا کہ ان کے صحت کی دیکھ بھال فراہم کرنے والے سے دستیاب مدد محدود تھی۔ بہت سے لوگوں نے کہا کہ وہ اپنے جی پی سے ویکسین کے بارے میں معلومات حاصل کرنے کی قدر کریں گے تاکہ وہ اپنے فیصلے سے آگاہ کر سکیں۔ کچھ لوگوں نے ویکسینیشن مراکز میں معلومات حاصل کرنے کی وضاحت کی، جس کا خیرمقدم کیا گیا تھا لیکن خیال کیا جاتا تھا کہ یہ بہت دیر سے آیا ہے۔
| " | آپ واقعی اس کے بارے میں جی پی سے براہ راست بات نہیں کر سکتے تھے… یہ مددگار ثابت ہوسکتا ہے، لیکن وہاں تک رسائی محدود تھی، یہ اتنی قابل رسائی نہیں تھی۔
- ہر کہانی اہم شراکت دار |
| " | مجھے یاد ہے کہ مجھے اپنی پہلی کووِڈ ویکسین کے لیے جانا تھا، مجھے ایک کتابچہ دیا گیا تھا، اور سوچ رہا تھا، 'یہ پہلی بار ہے جب میں نے اس میں سے کچھ معلومات دیکھی ہیں، اور درحقیقت مجھے ایسا محسوس نہیں ہوتا کہ میرے پاس واقعی ہضم ہونے کا وقت ہے۔ مکمل طور پر اس کا کیا مطلب ہے، اور مجھے ایک سیکنڈ میں جا کر اپنا انجکشن لگانا ہے۔' مناسب معلومات، ایسا محسوس ہوا کہ یہ بہت دیر سے آیا ہے۔"
- وہ عورت جو دودھ پلا رہی تھی جب ویکسین پیش کی گئی۔ |
دوست اور خاندان
جن لوگوں سے ہم نے بات کی ان میں سے بہت سے دوستوں اور کنبہ کے ساتھ CoVID-19 ویکسین پر تبادلہ خیال کرنے کا ذکر کرتے ہیں۔ تعاون کنندگان نے بتایا کہ انہوں نے معلومات کا اشتراک کرنے، ویکسین کی بہتر تفہیم حاصل کرنے اور فیصلہ سازی کے عمل کے ذریعے بات کرنے کے لیے دوسروں سے کیسے بات کی۔
| " | یہ دوستوں، خاندان اور ساتھیوں کا مرکب تھا، کیونکہ ہر ایک کی رائے مختلف تھی، اور ہر ایک کی کہانیاں مختلف تھیں۔ آپ نے ایسے لوگوں کی کہانیاں سنی ہیں جو دراصل CoVID-19 کے ساتھ مر رہے ہیں، اس نے آپ کو سوچنے پر مجبور کیا، ٹھیک ہے، شاید ویکسین لگانا اچھا ہے، اور پھر آپ کے پاس ایسے لوگ تھے جنہوں نے کہا کہ ویکسین نے کسی ایسے شخص کو مارا ہے جسے وہ جانتے تھے۔
- ہر کہانی اہم شراکت دار |
اہل خانہ اور دوستوں کے ساتھ جو صحت کی دیکھ بھال کے پیشہ ور تھے اکثر مشورہ کے لیے ان سے رجوع کرتے تھے۔ ان افراد کو اپنے نیٹ ورکس میں موجود لوگوں سے یقین دلایا جو سائنس اور ویکسین کیسے تیار کی جاتی ہیں کے بارے میں زیادہ سمجھتے ہیں۔
| " | سازشیں بہت ہوئیں اور اب بھی ہیں۔ لہذا، اس وقت کے درمیان، خاص طور پر جب آپ الگ تھلگ ہوتے ہیں، آپ کو واٹس ایپ پیغامات مل رہے ہوتے ہیں اور آپ کو دنیا بھر سے مختلف ویڈیوز کے لنکس مل رہے ہوتے ہیں، نام نہاد محققین وغیرہ۔ بعض اوقات آپ کو معلوم نہیں ہوتا تھا کہ کس چیز پر یقین کرنا ہے۔ . لہذا، اگر آپ کے پاس کوئی ایسا شخص ہے جو حقیقت میں اس علاقے میں کام کر رہا ہے، چیزوں کو اپنی آنکھوں سے دیکھ رہا ہے اور آپ کو اپنا تجربہ بتا سکتا ہے، تو یہ وہ چیز تھی جس پر آپ نے بھی بھروسہ کیا۔
- ہر کہانی اہم شراکت دار |
ہم نے ایسے لوگوں کی مثالیں بھی سنی ہیں جو ایسے ہی حالات میں ان لوگوں کے ساتھ ویکسین پر گفتگو کرتے ہیں، بشمول حاملہ یا دودھ پلانے والے یا طبی لحاظ سے کمزور۔
| " | جب میں حاملہ تھی اور دودھ پلا رہی تھی، میرے بہت سے قریبی دوست تھے جو اسی حالت میں تھے، اس لیے ہم نے اس کے بارے میں کافی حد تک بات کی۔ یہ اصل میں ایک اچھی حمایت تھی. بہت ساری معلومات کی عدم موجودگی میں اور کسی ایسے شخص کے ساتھ آمنے سامنے بیٹھنے کے قابل ہونے کی عدم موجودگی میں جسے آپ جانتے ہیں، یہ بات چیت کرنے کے قابل ہونا اچھا لگا۔ صرف کسی ایسے شخص کے ساتھ بحث کرنے کے لئے جس نے ایسا محسوس کیا کیونکہ وہ ایک ہی کشتی میں تھے۔
- وہ عورت جو دودھ پلا رہی تھی جب ویکسین پیش کی گئی۔ |
| " | میں ایسے لوگوں کے ساتھ فیس بک گروپ پر ہوں۔ [صحت کی حالت] اس لیے وہاں کافی بحث ہوئی کیونکہ ہم میں سے بہت سے لوگ کمزور فہرست میں شامل تھے۔
- طبی لحاظ سے کمزور شراکت دار |
کچھ لوگوں نے محسوس کیا کہ دوستوں یا کنبہ کے ساتھ ان کی بات چیت سے انہیں یہ فیصلہ کرنے میں مدد نہیں ملی کہ آیا ویکسین لگائی جائے۔ ان شراکت داروں نے افراد اور مختلف نسلوں کے درمیان تناؤ اور ویکسین کے حق میں اور اس کے خلاف خاندان کے افراد کے دباؤ کے بارے میں بات کی۔
| " | ہاں میرے خاندان میں، پرانی نسل میں، میں نے پایا کہ وہ آپ کو ایک خودغرض شخص کے طور پر دیکھتے ہیں اگر آپ یہ نہیں چاہتے تھے۔"
- ہر کہانی اہم شراکت دار |
| " | مجھے اپنے والد کا دباؤ تھا، وہ بہت پڑھے لکھے آدمی ہیں۔ وہ وہ شخص ہے جس کے پاس میں ہمیشہ مالیات سے لے کر صحت تک ہر طرح کے بارے میں مشورہ اور رہنمائی کے لیے جاتا ہوں۔ اور یہ ایک حقیقی دباؤ تھا کیونکہ اس نے کہا، 'آپ کو یہ نہیں ہونا چاہیے، کیونکہ اس کے بارے میں بات ہو رہی ہے کہ اس سے زرخیزی متاثر ہوتی ہے اور آپ مزید بچے چاہتے ہیں۔' لہذا، ہم نے اس پر تبادلہ خیال کیا، لیکن اس نے ضروری طور پر مدد نہیں کی. مزید، اس نے خوف میں اضافہ کیا۔
- وہ عورت جو دودھ پلا رہی تھی جب ویکسین پیش کی گئی۔ |
مذہبی عقائد رکھنے والے بعض اوقات اپنی عقیدہ برادری کے ذریعے ویکسین کے بارے میں سننے کو بیان کرتے ہیں۔ کچھ نے اس معلومات پر بھروسہ کیا جو دوسرے ذرائع سے شیئر کی گئی تھی۔
| " | میں یہوواہ کا گواہ ہوں، اور ہمارا پوری دنیا کا معاشرہ پوری ویکسین کے اجراء سے بہت زیادہ منسلک ہے۔ انہوں نے کافی تحقیق کی اور ہمیں ایک تنظیم کے طور پر ویکسین کی معلومات سے آگاہ کیا۔
- یہوواہ کے گواہ |
| " | مسلمانوں کے نقطہ نظر سے کچھ خدشات ضرور تھے۔ مجھے ایمانداری سے یاد نہیں ہے کہ وہ کیا تھے۔ لیکن مجھے یاد ہے کہ مسلم کونسل، میرے خیال میں انہوں نے یہ کہنے کے لیے کچھ جاری کیا تھا کہ 'دراصل آپ کو زندگی کو طول دینے کے لیے جو بھی ضروری قدم اٹھانے کی ضرورت ہے، اور یہ آپ کے ہاتھ میں ہے اور اس لیے آپ کو اس میں سرگرم رہنا ہوگا'۔
- ایک مسلمان عقیدے کا فرد |
| " | مختلف جگہوں سے کافی معلومات آرہی تھیں۔ میں واقعی میں میڈیا میں موجود کسی بھی چیز پر بھروسہ نہیں کرتا تھا، لیکن میری ایمانی برادری، ویکسین کے ارد گرد میری عقیدہ برادری کی طرف سے اپ ڈیٹس موجود تھیں۔ انہوں نے اس پر کافی تحقیق کی تھی۔ اور مجھے اس پر بھروسہ تھا۔"
- ہر کہانی اہم شراکت دار |
ذاتی تحقیق
جن لوگوں سے ہم نے بات کی ان میں سے کچھ نے کہا کہ انہوں نے ویکسین لینے یا نہ لینے کے اپنے فیصلے سے آگاہ کرنے کے لیے اپنی تحقیق کی ہے۔ ہم نے بہت سے ذرائع سے مشورہ کرنے والے شراکت داروں کی مثالیں سنی ہیں، جن میں سائنسی جرائد جیسے دی لانسیٹ اور برٹش میڈیکل جرنل، طبی مطالعات اور کووِڈ-19 ویکسینز کے لیے کلینیکل ٹرائلز کا ڈیٹا، بلاگز اور سوشل میڈیا پیجز، نیوز آرٹیکلز، اور دیگر شامل ہیں۔ انٹرنیٹ کی تلاش.
| " | میں اپنی بہت سی تحقیق کر رہا تھا، اس لیے میں معلومات کی تلاش میں تھا، میں کمپنیوں میں جا رہا تھا، کون سی کمپنی اس پر کام کر رہی تھی، اور میں اس کے بارے میں سب کچھ پڑھ رہا تھا۔
- ہر کہانی اہم شراکت دار |
3. فیصلہ کرنا کہ Covid-19 ویکسین لینا ہے یا نہیں۔ |
 |
یہ باب ان عوامل کی کھوج کرتا ہے جنہوں نے تعاون کرنے والوں کے فیصلوں سے آگاہ کیا کہ آیا Covid-19 ویکسین لینا ہے یا نہیں۔ اس میں انہوں نے ہمیں بتایا کہ وہ اپنے فیصلوں پر کیسے پہنچے، بشمول ان لوگوں کے تجربات جنہوں نے ویکسین لینے کا انتخاب کیا، اور جنہوں نے نہیں کیا۔
Covid-19 ویکسین لینے یا نہ لینے کا فیصلہ
بہت سے تعاون کرنے والوں نے ہمیں بتایا کہ ان کا فیصلہ CoVID-19 ویکسین لینے یا نہ لینے کا نسبتاً سیدھا تھا۔ ان شراکت داروں نے کہا کہ انہوں نے اپنا فیصلہ بہت جلد کیا۔
| " | میں نے واقعی میں اسے حاصل نہ کرنے پر کبھی غور نہیں کیا تھا۔ تو ہاں۔ میں ہمیشہ سے یہ سوچ رکھتا تھا کہ جب یہ مجھے پیش کیا جائے گا، جب میں اسے لینے کے قابل ہو جاؤں گا تو میں جا کر اسے لے جاؤں گا۔
- ہر کہانی اہم شراکت دار |
| " | میں نے کبھی بھی ویکسین نہیں لگائی جب کوئی ویکسینیشن پیش کی گئی تھی۔ یا ایسی چیز کے طور پر سمجھا گیا جو میرے اور میری فلاح و بہبود کے لئے فائدہ مند ہوگا۔ لیکن، آپ جانتے ہیں، میں بالکل دور سے سوچتا ہوں، لفظی طور پر جب میں نے سوچنا شروع کیا، 'کیا یہ وہ چیز تھی جو میں چاہتا تھا؟' میں اصرار اور اٹل تھا، کہ نہیں، میں نے ایسا نہیں کیا… مجھے لگتا ہے کہ یہ صرف ان میں سے ایک ہے، آپ کچھ سنتے ہیں، اور آپ کا فوری، فطری جواب ہے، 'ہاں، میں یہ کرنا چاہتا ہوں'، 'نہیں میں نہیں کرتا' t' اور میرا فطری جواب تھا 'میں یہ نہیں چاہتا۔
- وہ شخص جس نے ویکسین نہ لینے کا انتخاب کیا۔ |
تاہم، ہم نے تعاون کرنے والوں سے بھی سنا جنہیں اپنا فیصلہ مشکل معلوم ہوا۔ ان شراکت داروں نے بیان کیا کہ وہ اپنے حتمی فیصلے پر آنے سے پہلے متعدد مسابقتی عوامل کا وزن کرتے ہوئے مختلف پوزیشنوں کے درمیان کس طرح آگے پیچھے ہوتے ہیں۔ یہ معاملہ ان دونوں کے لیے تھا جنہوں نے CoVID-19 ویکسین لینے کا انتخاب کیا اور جنہوں نے نہیں کیا۔
| " | جس سے بہت سے لوگ مر رہے تھے۔ [COVID-19] اور پھر یہ اس کی پیش رفت تھی، 'ہاں، ہمیں ایک ویکسین مل گئی ہے،' جسے میں نے لاجواب سمجھا۔ لیکن اس کے بعد یہ چھوٹی چھوٹی چیزیں تھیں کہ میں نے سوچا، 'ٹھیک ہے، انہیں اتنی جلدی کیسے مل گئی، اور کیا اس کے لیے آزمائشیں تھیں؟' اور یہ وہ وقت تھا جب میں نے چیزوں پر سوال کرنا شروع کیے، اپنے دماغ میں سوچنا شروع کر دیا، 'یہ اتنی جلدی کیسے ہو گیا؟
- ہر کہانی اہم شراکت دار |
ذیل میں بیان کردہ عوامل وہ ہیں جن کی اطلاع کووڈ-19 ویکسین کی پہلی خوراک کے بارے میں فیصلوں کو مطلع کرنے میں اہم بتائی گئی ہے۔ یہ عوامل اکثر ویکسین کی بعد کی خوراکوں کے بارے میں فیصلوں کو مطلع کرنے میں بھی اہم ہوتے تھے، حالانکہ Covid-19 ویکسین کی بعد میں خوراک لینے یا نہ لینے کا فیصلہ کرتے وقت ایک چھوٹی تعداد نے دوسرے عوامل پر غور کیا۔
تعاون کنندگان نے Covid-19 ویکسین حاصل کرنے کا انتخاب کیوں کیا۔
ایسا نہ کرنے کی کوئی مضبوط وجہ نہیں۔
ہم نے کئی شراکت داروں سے سنا جنہوں نے کہا کہ انہوں نے CoVID-19 ویکسین حاصل کرنے کی بنیادی وجہ یہ تھی کہ انہوں نے ایسا نہ کرنے کی کوئی مضبوط وجہ نہیں دیکھی۔ یہ تعاون کنندگان اکثر حکومت اور NHS کے مشورے پر بھروسہ کرنے کی وضاحت کرتے ہیں، یہ فرض کرتے ہوئے کہ کوئی بھی ایسی چیز کی سفارش نہیں کرے گا جو غیر محفوظ ہو۔ ان شراکت داروں کے لیے ان کا فیصلہ نسبتاً سیدھا تھا: جب انھیں ایک ویکسین پیش کی گئی تو انھوں نے اسے لے لیا۔
| " | یہ کبھی بھی میرے ذہن میں نہیں آیا کہ ویکسینیشن نہ ہو۔ جب بھی میں نے کسی کو اس کے بارے میں کوئی منفی بات کہتے ہوئے سنا تو میں ہمیشہ حیران ہوتا تھا، اور حیران اور حیران رہ جاتا تھا۔
- ہر کہانی اہم شراکت دار |
اپنے آپ کو اور دوسروں کو سنگین بیماری یا موت سے بچانے کے لیے
بہت سے تعاون کرنے والوں نے ہمیں بتایا کہ انہوں نے CoVID-19 ویکسین حاصل کرنے کا انتخاب کرنے کی ایک اہم وجہ یہ تھی کہ انہیں یقین تھا کہ اس سے ان کی اور ان کے پیاروں کی حفاظت میں مدد ملے گی۔ یہ تعاون کرنے والے پریشان تھے کہ کیا ہوگا اگر وہ یا کوئی پیارا CoVID-19 سے شدید بیمار ہو جائے اور ویکسینز کو اپنے آپ کو اور دوسروں کو سنگین بیماری یا موت سے بچانے کا بہترین طریقہ سمجھا۔ یہ اکثر ان لوگوں کے لیے اہم ہوتا ہے جن کے دوستوں یا خاندان کے افراد خطرے میں پڑنے والے گروپس میں ہوتے ہیں (جیسے بوڑھے رشتہ دار، نوزائیدہ بچے، یا دوسرے کمزور لوگ) یا جو خود CoVID-19 کی شدید بیماری کا زیادہ خطرہ رکھتے تھے۔
| " | "مجھے لینا پڑا [ویکسین] بزرگ رشتہ داروں کے لیے، میں انہیں محفوظ رکھنا چاہتا تھا۔ تو، 100% میں نے اسے لینے کا فیصلہ کیا۔
- ہر کہانی اہم شراکت دار |
| " | میں نے پہلے ہی ویکسینیشن کے بغیر اس کا تجربہ کیا تھا، اور کسی ایسے شخص کو کھو دیا تھا جو تھا۔ مجھے واقعی عزیز ہے، اور ایسا کوئی طریقہ نہیں تھا کہ میں اپنے بیٹے کو رکھنا چاہتا ہوں۔ اس کے ذریعے. میں نے صرف وہی کیا جو مجھے کرنا تھا۔"
- طبی لحاظ سے کمزور شخص |
کام کی جگہ کی ضروریات
وبائی امراض کے دوران صحت اور سماجی نگہداشت میں کام کرنے والے شراکت داروں نے اکثر کہا کہ کوویڈ 19 ویکسین حاصل کرنے کے ان کے فیصلے کو کام کی جگہ پر ویکسین کی ضروریات کے ذریعہ مطلع کیا گیا تھا۔ اس کے بارے میں رائے منقسم تھی: کچھ لوگوں کا خیال تھا کہ ویکسین لینا ضروری ہے کیونکہ ان کا خیال تھا کہ اس سے ان کی اور ان لوگوں کی حفاظت میں مدد ملے گی جن کی وہ دیکھ بھال کرتے ہیں۔
| " | میں ایک کیئر ہوم میں کام کر رہا تھا، اور یہ میرے لیے محفوظ تھا، اور میں ان کے لیے بھی محفوظ تھا۔ لہذا یہ میری تشویش تھی، کہ کم از کم میں اپنے کام کی جگہ پر محفوظ طریقے سے کام کر سکتا ہوں، اور میں گھر واپس جاؤں گا، میں آرام محسوس کروں گا، اور میں محفوظ ہوں۔"
- نگہداشت ہوم ورکر |
| " | ہاں میں نے اسے لینے کا فیصلہ کیا۔ میں ان مریضوں کے ساتھ کام کر رہا تھا جو بہت بیمار تھے کیونکہ مجھے ایک یونٹ میں منتقل کر دیا گیا تھا جہاں میرے مریض وینٹیلیشن پر تھے، اس لیے مجھے یہ ہونا پڑا – میں انہیں خطرے میں ڈالنے کا متحمل نہیں تھا۔
- وبائی امراض کے دوران فرنٹ لائن کارکن |
تاہم، دوسروں نے استدلال کیا کہ صحت اور سماجی نگہداشت میں کام کرنے والوں کو اپنی ملازمت سے ویکسین لینے کے لیے دباؤ میں نہیں ڈالا جانا چاہیے تھا۔ ان شراکت داروں نے اکثر ویکسین کے نئے تیار ہونے کے نتیجے میں ان پر طویل مدتی ڈیٹا کی کمی کی طرف اشارہ کیا، اور سوچا کہ لوگوں کو ویکسین حاصل کرنے کے بارے میں اپنے فیصلے کرنے کے لیے آزاد ہونا چاہیے۔ ہم نے یہ کچھ صحت اور سماجی نگہداشت کے عملے سے سنا ہے بلکہ کام کی جگہ پر ویکسینیشن کی ضروریات پر غور کرنے والے دوسرے معاونین سے بھی سنا ہے۔
| " | میں نے ایماندار ہونے کا دباؤ محسوس کیا۔ مجھے کوئی خط یا ٹیکسٹ میسج نہیں ملا۔ میرے خیال میں میرے ایک مینیجر کا فون بند تھا۔ یہ صرف دباؤ تھا۔ یہ ایک اچھا احساس نہیں ہے - اور مجھے نہیں لگتا کہ آپ کو بہت سے معاملات میں ایسا محسوس ہوگا جب اس کا تعلق عام طور پر آپ کی صحت کے ساتھ ہے، کیونکہ آپ یہ فیصلے خود کرتے ہیں نا؟ آپ کے پاس عام طور پر کوئی اور شامل نہیں ہوتا ہے۔"
- وبائی امراض کے دوران فرنٹ لائن کارکن |
| " | عملے کے تقریباً 1,000 ارکان ایسے تھے جو ویکسین نہیں لگانا چاہتے تھے، تاہم سروس نے زبردستی کے رویے کا استعمال کرتے ہوئے، عملے پر دباؤ ڈال کر، انہیں آرام کے دنوں میں فون کرکے، ای میلز بھیج کر اور بعض صورتوں میں غنڈہ گردی کی گئی کیونکہ انہوں نے ویکسین نہ کروانے کا انتخاب کیا۔ ان کے جسموں میں کوئی ایسی چیز ڈالیں جو طویل مدتی حفاظتی ڈیٹا کے بغیر ابھی تک آزمائش میں تھی۔ یہ سراسر خوفناک رویہ تھا جس کا بہت سے عملے پر نقصان دہ اثر پڑا۔ میں نے 18 سال سے زیادہ کا عہد کیا تھا، اپنی صلاحیت کے مطابق اپنا کام کیا تھا، مجھے کبھی کوئی شکایت نہیں تھی، تاہم اگر میں نے یہ تجربہ اپنے جسم میں نہیں ڈالا تو مجھے نوکری سے نکال دیا جائے گا۔
- وبائی امراض کے دوران فرنٹ لائن کارکن |
لاک ڈاؤن ختم کرنا
ہم نے کچھ شراکت داروں سے سنا جنہوں نے کہا کہ ان کا خیال ہے کہ ویکسین لاک ڈاؤن کی پابندیوں کو ختم کر دیں گی اور ان کی زندگیوں کو پہلے کی طرح واپس آنے کا موقع فراہم کرے گی۔ ہم نے اکثر یہ ان لوگوں سے سنا ہے جو جوان، تندرست اور صحت مند تھے، اور کووڈ-19 کو اپنی صحت کے لیے اتنا بڑا خطرہ نہیں سمجھتے تھے جتنا کہ یہ دوسروں کے لیے ہو سکتا ہے، جیسے کہ طبی لحاظ سے کمزور لوگ۔
| " | میں نے صرف سوچا کہ جتنی جلدی ہر کسی کو ویکسین لگائی جائے گی، اتنی ہی جلدی ہم دوبارہ کام شروع کر سکتے ہیں، کھیلنا اور سفر کرنا شروع کر سکتے ہیں اور، آپ جانتے ہیں، باقی سب کچھ۔"
- ہر کہانی اہم شراکت دار |
بہت سے لوگوں کے لیے، سفر اور سماجی کاری پر رکھی گئی پابندیوں سے محدود نہ رہنے کی خواہش ان کے کووِڈ 19 ویکسین حاصل کرنے کے فیصلے کا ایک اہم عنصر تھی۔ اس گروپ کے لیے، ویکسینیشن ختم کرنے کا ایک ذریعہ بن گیا، اور انھوں نے اسے ایک ایسی چیز کے طور پر قبول کر لیا جس کی انھیں سفر کرنے یا سماجی زندگی گزارنے کے لیے کرنے کی ضرورت تھی۔
| " | زیادہ انتخاب نہیں تھا۔ انہوں نے کہا کہ آپ یونیورسٹی نہیں جا سکتے، آپ چھٹی کے دن نائٹ کلبوں، شراب خانوں میں نہیں جا سکتے۔ اگر آپ کے پاس ویکسین نہیں تھی تو انہوں نے آپ سے سب کچھ چھین لیا۔ اگر آپ اپنی زندگی واپس لینا چاہتے ہیں تو آپ کو اسے لینا پڑا۔"
- ہر کہانی اہم شراکت دار |
اتھارٹی کے اعدادوشمار کے فیصلے پر بھروسہ کریں۔
جیسا کہ پہلے زیر بحث آیا، کچھ تعاون کرنے والوں کے لیے سائنسدانوں اور صحت کی دیکھ بھال کرنے والے پیشہ ور افراد کے مشورے نے CoVID-19 ویکسین حاصل کرنے کے ان کے فیصلے سے آگاہ کرنے میں اہم کردار ادا کیا۔ ان شراکت داروں نے ان گروپوں کی فراہم کردہ رہنمائی پر بھروسہ کیا، جن کے بارے میں خیال کیا جاتا تھا کہ وہ رائے کی بجائے سائنسی شواہد کی بنیاد پر ویکسین کے بارے میں فیصلے کر رہے ہیں۔
| " | مجھے اس کا نام کبھی یاد نہیں رہا، لیکن میں نے آکسفورڈ کی اکیڈمک کے ساتھ ایک ڈاکومنٹری دیکھی، وہ خاتون اکیڈمک جو اس ویکسین کو اکٹھا کرنے میں دوسروں کے ساتھ اہم کردار ادا کر رہی تھی، اور دستاویزی فلم کے اختتام تک میں جان گئی تھی کہ اگر مجھے پیشکش کی گئی تو میں اسے لے لوں گی۔ یہ اس نے تمام سوالات کے جوابات دیئے۔‘‘
- وہ شخص جس نے ویکسین لینے کا انتخاب کیا۔ |
| " | آپ کے ساتھ رشتہ استوار کرتے ہیں۔ [آپ کے ہیلتھ کیئر پروفیشنلز] اور یہ اعتماد پر مبنی رشتہ ہے، اور میرا تعلق واقعی لاجواب تھا۔ وہ بہت پیارے تھے اس لیے میں نے ان پر پورے دل سے بھروسہ کیا۔ تو، ہاں میں نے سنا… اور اس سے میرے لیے فرق پڑا۔ اس کا اثر میرے فیصلے پر پڑا۔"
- طبی لحاظ سے کمزور شخص |
وہ لوگ جن کے دوست یا خاندان کے طور پر صحت کی دیکھ بھال کے پیشہ ور افراد تھے اکثر CoVID-19 ویکسین کے بارے میں مشورے کے لیے ان سے رجوع کرتے تھے، سائنس پر ان کے اعتماد کو اپنے پیارے پر اعتماد سے تقویت ملتی ہے۔
| " | میری بہن ایک دندان ساز ہے، تو وہ [کوویڈ 19 کی ویکسین تھی] اور اس نے کہا 'مجھے کچھ نہیں ہوا' تم جانتے ہو۔ وہ ایک دن بازو میں درد تھا۔ میرا بیٹا میڈیکل کا طالب علم تھا، […] تو اسے بھی کرنا پڑا۔ لہذا، یہ لوگ، میرے قریبی خاندان کے افراد، کیونکہ انہوں نے یہ کیا اور کچھ نہیں ہوا، وہ ٹھیک تھے، اور وہ حوصلہ افزا تھے، کیونکہ وہ صحت کی خدمت میں تھے۔"
- فرنٹ لائن کارکنوں کے رشتہ دار |
معاشرتی دباؤ
دوسروں نے احساس کو بیان کیا۔ معاشرے کی طرف سے ویکسینیشن کے لیے زیادہ عام دباؤ. کچھ لوگوں کے لیے، اس نے انہیں ویکسین لینے پر مجبور کیا۔ اس طرح محسوس کرنے والوں نے اس طریقے پر غصے کا اظہار کیا جس میں کوویڈ 19 ویکسین کے بارے میں معلومات عوام تک پہنچائی گئیں۔
| " | اس قسم کے بیرونی دباؤ کی وجہ سے میرے پاس پہلا اور بوسٹر تھا۔ آپ جانتے ہیں، آپ کو یہ کرنا ہے۔ آپ کو سب کی حفاظت کرنی ہے۔ NHS کی حفاظت کریں۔ اپنے خاندان کی حفاظت کریں۔ اپنے ساتھیوں کی حفاظت کریں۔ […] تو مجھے لگتا ہے کہ میں نے دباؤ محسوس کیا۔ میں نے ویکسینیشن کروانے کے لیے دباؤ محسوس کیا۔ میں اسے حاصل کرنے سے خوفزدہ تھا کیونکہ میں نہیں جانتا تھا کہ اصل مضمرات اور اس کا مجھ پر، میری بیٹی پر کیا اثر پڑے گا، اور میں اس ساری صورت حال کے بارے میں کافی ناراض تھا۔
- وہ عورت جو دودھ پلا رہی تھی جب ویکسین پیش کی گئی۔ |
کیوں تعاون کنندگان ویکسین حاصل کرنے میں ہچکچا رہے تھے، یا ایسا نہ کرنے کا انتخاب کیا تھا۔
CoVID-19 ویکسینز کی حفاظت پر اعتماد کا فقدان
بہت سے تعاون کنندگان کے لیے حفاظتی خدشات ایک اہم عنصر تھے جو CoVID-19 ویکسین حاصل کرنے سے ہچکچا رہے تھے یا جنہوں نے ایسا نہ کرنے کا انتخاب کیا۔ جن لوگوں نے اس کا تذکرہ کیا وہ اکثر اس رفتار کے بارے میں بات کرتے تھے جس سے ویکسین تیار کی گئی تھیں: اس سے یہ سوالات اٹھتے ہیں کہ آیا ترقی کا عمل صحیح طریقے سے ہوا ہے۔
| " | سوچنے کا کچھ عنصر تھا کہ آیا یہ محفوظ ہے، اس رفتار کی وجہ سے جس سے اسے تیار کیا گیا تھا، تو میں نے یہی سوچا۔ میرا ابتدائی ردعمل تھا، واہ، یہ جلدی ہے۔ دوسرا فوری ردعمل، اگر یہ اتنا تیز ہے، تو کیا یہ محفوظ ہے؟"
- ہر کہانی اہم شراکت دار |
حفاظتی خدشات ان لوگوں کے لیے خاص اہمیت کے حامل تھے جن سے ہم نے طویل مدتی صحت کی حالتوں یا نسلی اقلیتی پس منظر کے لوگوں سے سنا ہے۔ ان شراکت داروں کو تشویش ہے کہ ویکسین کو تیز رفتاری سے تیار کرنے کی کوشش میں، ان جیسے لوگوں پر مناسب جانچ نہیں ہوئی ہے۔ انہیں خدشہ تھا کہ اس کا مطلب یہ ہوگا کہ انہیں ویکسین کے منفی ردعمل کا زیادہ خطرہ ہے۔
| " | میں نے کوویڈ ویکسین نہ لگانے کا انتخاب کیا۔ […] مجھے خودکار قوت مدافعت کی بیماری ہے اور ویکسین کے ٹرائلز میں آٹو امیون بیماری میں مبتلا کوئی لوگ نہیں تھے۔
- طبی لحاظ سے کمزور شخص |
| " | میں جاننا چاہتا تھا کہ کیا ویکسین کا تجربہ آبادی کے لحاظ سے کیا گیا ہے کیونکہ ویکسین ایک بڑی چیز ہے، چاہے وہ کووڈ کے لیے ہوں یا نہیں۔ ہم آپ کے اندر اس چیز کو انجیکشن لگانے کے بارے میں بات کر رہے ہیں۔ یہ صحت کا ایک متنازعہ علاقہ ہے۔ میں اس بارے میں فکر مند تھا کہ ویکسین کا تجربہ اکثریتی غیر نسلی اقلیتوں پر کیا گیا ہے یا بہت کم، اگر بالکل، نسلی اقلیتوں پر تجربہ کیا گیا ہے اور ان کے نتائج کیا ہیں۔ عام حالات میں آپ اس معلومات کو آسانی سے تلاش کر سکتے تھے… لیکن وہ معلومات دستیاب نہیں تھی۔ بجا طور پر، یہ ایک نئی دوا تھی اس لیے اس کے ساتھ زیادہ تجربہ نہیں تھا، لیکن پھر بھی، جو بھی تجربہ یا افادیت جسے وہ کہتے ہیں، انہوں نے اس وقت استعمال کیا، کیا اس میں سیاہ فام اور اقلیتی نسلی گروہوں کی بڑی تعداد شامل تھی؟ یا سیاہ افریقی-کیریبین یا ایشیائی گروپس، ہمیں اس بات کی ضمانت دینے کے لیے کہ اس میں تھوڑا سا زیادہ سکون ہے؟
- ایک سیاہ فام نسلی پس منظر سے تعلق رکھنے والا شخص |
عام طور پر، ویکسین کی سمجھی جانے والی حفاظت اور تاثیر کے بارے میں طویل مدتی ڈیٹا کی کمی بہت سے تعاون کنندگان کے لیے اہم تھی جنہوں نے ویکسین حاصل نہ کرنے کا انتخاب کیا۔ انہوں نے بتایا کہ کس طرح CoVID-19 ویکسینز ان دیگر ویکسینز سے مختلف ہیں جو انہیں پہلے موصول ہوئی تھیں: وہ ویکسین برسوں سے موجود تھیں اور ان کی حفاظت اور تاثیر پر طویل مدتی ثبوت موجود تھے۔ یہ CoVID-19 ویکسینز کا معاملہ نہیں تھا۔ ان شراکت داروں نے غصے کے احساس کو بیان کیا کہ ان خدشات کو ویکسین کے بارے میں حکومتی رہنمائی میں واضح طور پر دور نہیں کیا گیا تھا۔
| " | مجھے کوئی خاص تشویش نہیں تھی، جیسے، 'یہ اس کا سبب بن سکتا ہے، یہ X، Y یا Z بیماری، یا خرابی، یا جو کچھ بھی، یا، آپ جانتے ہیں، بانجھ پن کا سبب بن سکتا ہے۔' میں نے کسی خاص چیز کے بارے میں نہیں سوچا۔ میں نے صرف سوچا کہ اس کے کچھ منفی اثرات ہوسکتے ہیں، آپ جانتے ہیں، طویل مدتی۔ ہم واقعی مکمل طور پر نہیں جانتے کیونکہ یہ بالکل نیا ہے۔
- وہ شخص جس نے ویکسین نہ لینے کا انتخاب کیا۔ |
CoVID-19 ویکسین کی تاثیر میں اعتماد کا فقدان
بہت سے تعاون کرنے والوں کے لیے، یہ سن کر کہ جن لوگوں کو Covid-19 کی ویکسین ملی ہے وہ اب بھی Covid-19 کا معاہدہ کر سکتے ہیں اس بارے میں سوالات اٹھائے گئے کہ آیا ویکسین کام کرتی ہیں یا نہیں۔ ان شراکت داروں نے فرض کیا کہ Covid-19 کی ویکسین لوگوں کو CoVID-19 کا شکار ہونے سے روکنے کے لیے بنائی گئی ہیں (دوسری بیماریوں کے لیے ویکسین کے ان کے تجربات کی بنیاد پر)۔ جب انہوں نے سوچا کہ ایسا نہیں ہے (مثال کے طور پر جب دوستوں یا کنبہ کے افراد جنہوں نے بعد میں ایک ویکسین حاصل کی تھی کوویڈ 19 کا معاہدہ کیا تھا) اس سے کوویڈ 19 ویکسین پر عدم اعتماد کا احساس پیدا ہوا جس نے ان کے نہ لینے کے فیصلے کو متاثر کیا۔
| " | یہ تھا، اس قسم کی، جس پر نیچے آیا۔ میں نے صرف سوچا، 'جانے اور ویکسین کروانے کا کیا فائدہ ہے جب میں اس کے بعد بھی کوویڈ حاصل کر سکتا ہوں؟'
- ہر کہانی اہم شراکت دار |
ضروری نہیں سمجھا جاتا
کچھ تعاون کنندگان نے محسوس کیا کہ CoVID-19 سے ان کے شدید بیماری کا خطرہ کم ہے اور اس لیے انہوں نے یہ سمجھا کہ ویکسین ان سے متعلق نہیں تھیں۔ یہ نظریہ ان لوگوں میں زیادہ عام تھا جنہیں ویکسین پیش کیے جانے سے پہلے کووِڈ 19 ہو گیا تھا اور وہ بیمار نہیں ہوئے تھے یا صرف ہلکی علامات کا شکار تھے۔ انہوں نے محسوس کیا کہ انہیں کسی ایسی چیز سے تحفظ کی ضرورت نہیں ہے جس کا وہ پہلے ہی تجربہ کر چکے ہیں، کیونکہ اب ان کے پاس قدرتی استثنیٰ ہے، اور انہیں شدید تکلیف نہیں ہوئی۔
| " | میں اس کے بالکل خلاف تھا۔ […] زیادہ تر صحت کے لحاظ سے۔ ضمنی اثرات کیا ہیں؟ طویل مدتی ضمنی اثرات کیا ہیں؟ اور پھر، کیونکہ مجھے کووِڈ تھا اور مجھے کوئی علامات نہیں تھیں اور مجھے زیادہ خطرہ نہیں تھا۔ میں پہلے ہی اس سے گزر چکا تھا۔ میں نے مثبت تجربہ کیا، تاہم، کچھ نہیں ہوا۔ […] اور میرے خاندان میں سب کو مل گیا۔ ہم میں سے تقریباً 18 تھے اور ہم سب کو ایک ہی وقت میں کووڈ تھا۔ اور پھر ہم نے محسوس کیا کہ یہ غیر ضروری تھا۔ یہ واقعی ایک بری سردی تھی۔"
- ہر کہانی اہم شراکت دار |
جن لوگوں سے ہم نے سنا ان میں سے کچھ نے ہمیں بتایا کہ انہوں نے ویکسین نہ لینے کا انتخاب کیا کیونکہ وہ سمجھتے تھے کہ ان کے مدافعتی نظام کو قدرتی طور پر وائرس سے نمٹنے کے قابل ہونا چاہیے، خاص طور پر اگر وہ خود کو فٹ اور صحت مند رکھیں۔ یہ افراد اکثر CoVID-19 کے دوسرے اصولوں پر عمل کرتے تھے (جیسے چہرے کے ماسک پہننا) اور ویکسین کے بارے میں معلومات پر بھروسہ کرتے تھے۔ تاہم، انھوں نے یہ ضروری نہیں سمجھا کہ انھیں ویکسین لگائی جائے۔
| " | میں جوان ہوں، میں فٹ اور صحت مند ہوں، اور ظاہر ہے کہ اگر مجھے یہ مل گیا تو میں شاید اس سے لڑنے کے قابل ہو جاؤں گا۔"
- وہ شخص جس نے ویکسین نہ لینے کا انتخاب کیا۔ |
امتیازی سلوک اور نسل پرستی کے موجودہ اور تاریخی تجربات
کچھ معاونین نے اشتراک کیا کہ کس طرح امتیازی سلوک اور نسل پرستی کے حالیہ تجربات Covid-19 ویکسین حاصل نہ کرنے کے اپنے فیصلے سے آگاہ کرنے میں اہم تھے۔ ان تجربات پر اکثر نسلی اقلیتی پس منظر سے تعلق رکھنے والے شراکت داروں کے ذریعے تبادلہ خیال کیا جاتا تھا۔ شراکت داروں نے بتایا کہ کس طرح امتیازی سلوک اور نسل پرستی کے پچھلے تجربات نے انہیں حکومت اور صحت کے نظام پر زیادہ وسیع پیمانے پر عدم اعتماد کا باعث بنا، جس کے نتیجے میں وہ CoVID-19 ویکسینز کے بارے میں خوف اور بے چینی محسوس کرنے لگے۔ مخصوص نسلی اقلیتی گروہوں کے لیے ویکسین کے خطرات اور مضر اثرات کے بارے میں معلومات کی کمی نے ان کے خدشات کو بڑھا دیا۔
| " | میں سیاہ فام ہوں… اس کا مطلب ہے کہ میری کمیونٹی کا میری زندگی کے کسی بھی پہلو میں، میری کمیونٹی کی زندگی کا خیال نہیں رکھا جاتا ہے۔ وہ بیرل کے نیچے ہیں، اگر بیرل میں بھی ہوں۔ اور اس لیے، میں کسی پر بھروسہ نہیں کرتا کہ مجھے کوئی حقیقی مخصوص معلومات فراہم کرے کہ اس کا مجھ پر کیا اثر پڑے گا۔ وہاں اب بھی کوئی بھروسہ نہیں ہے۔"
- ایک سیاہ فام نسلی پس منظر سے تعلق رکھنے والا شخص |
| " | میں کسی ایسے شخص کے طور پر لکھتا ہوں جو سیاہ فام ہے اور جس کی زندگی CoVID-19 سے براہ راست متاثر ہوئی ہے۔ […] سیاہ فام لوگوں کی ایک بڑی تعداد نے طبی اسٹیبلشمنٹ کے موروثی عدم اعتماد کی وجہ سے جاب لینے سے انکار کردیا۔
- ایک سیاہ فام نسلی پس منظر سے تعلق رکھنے والا شخص |
طبی سائنس میں نسل پرستی کا تصور یہ بتانے میں بھی اہم تھا کہ نسلی اقلیتی پس منظر سے تعلق رکھنے والے افراد نے ویکسین کو کس طرح سمجھا۔ کچھ تعاون کرنے والوں نے محسوس کیا کہ سیاہ فام کمیونٹیز کی ایک تاریخی میراث پر تجربہ کیا جا رہا ہے، جس کی وجہ سے عدم اعتماد کے جذبات موجود ہیں۔
| " | ہم نے آس پاس کے سوالات پوچھے، جیسے کہ یہ کتنا قابل اعتماد ہے، کس پر اس کا تجربہ کیا گیا ہے۔ کیونکہ اس بارے میں یہ غلط فہمی ہے، آپ جانتے ہیں، نسلی اقلیتوں کو ہمیشہ ویکسینیشن کے لیے استعمال کیا جاتا ہے اور اگر ہم زندہ رہے تو سفید فام کمیونٹی محفوظ ہے اور ان پر ویکسین لگائی جائے گی۔ اور یہ سیاہ فام برادریوں کے ساتھ ہوا ہے، اور اسی لیے غلامی کی تجارت اور وہ سب کچھ، وہ تمام ویکسینیشن استعمال کیے گئے تھے۔ […] لہذا، میں چاہتا تھا کہ اس خوف کو دور کیا جائے اور اس کا تدارک کیا جائے، اس لیے میں نے اس مہم میں صرف اس بات کو سمجھنے کے لیے حصہ لیا۔ میں نے کہا کہ، آپ جانتے ہیں، 'میں یہ جاننا چاہتا ہوں کہ کیا ہمیں گنی پگ کے طور پر استعمال کیا جا رہا ہے یا کیا حقیقی طور پر آپ مطمئن ہیں کہ یہ ویکسین جائز ہے اور یہ کام کرتی ہے اور آپ کے پاس کیا ہے۔'
- ایشیائی نسلی پس منظر سے تعلق رکھنے والا شخص |
اتھارٹی میں عدم اعتماد
جن لوگوں سے ہم نے بات کی ان میں سے چند ایک نے ہمیں بتایا کہ کس طرح CoVID-19 ویکسین کے بارے میں بیانیہ کچھ ہے جو لوگوں کو 'بس کرنا تھا' نے ان کے ایسا کرنے کی خواہش کم کردی۔ اس گروپ نے عام طور پر حکومت پر عدم اعتماد کو بیان کیا، اور یہ نہیں سوچا کہ انہیں ایسا کچھ کرنے کے لیے مجبور محسوس کرنا چاہیے جو وہ نہیں کرنا چاہتے تھے۔
| " | میں 70 سال کا ہوں اور میں نے کسی بھی ویکسین سے انکار کیا۔ کسی بھی حکومت کو یہ حق نہیں ہے کہ وہ اپنے شہریوں کو تجرباتی طریقہ کار پر مجبور کرنے کی کوشش کرے۔
- وہ شخص جس نے ویکسین نہ لینے کا انتخاب کیا۔ |
| " | میں نے صرف سوچا، 'مجھے یہ نہیں بتایا جا رہا ہے کہ میں کیا کر سکتا ہوں اور کیا نہیں کر سکتا کہ آیا میں نے ویکسینیشن کروا لی ہے۔' کیونکہ، اصل میں، دن کے اختتام پر، یہ میرا جسم ہے، اور مجھے آزادانہ طور پر انتخاب کرنے کی اجازت ہونی چاہیے کہ آیا میں اسے لوں، جو ظاہر ہے کہ میں کرنے کے قابل تھا۔ لیکن میں نے اپنی صحت کے بارے میں جو فیصلہ کیا ہے اس کی وجہ سے مجھے اپنی زندگی پر پابندیاں نہیں لگنی چاہئیں۔ اور مجھے لگتا ہے کہ جب بات اس مقام پر پہنچی تو میں بالکل ایسا ہی تھا، 'بالکل، میں اس کے ساتھ مشغول نہیں ہوں۔' اور میں نے واقعی اپنے اردگرد کے لوگوں کی خوشی کے لیے بہت کچھ کیا۔
- وہ شخص جس نے ویکسین نہ لینے کا انتخاب کیا۔ |
طب کے بارے میں ذاتی رویہ
کچھ شراکت داروں نے عام طور پر طبی مداخلتوں کے بارے میں محتاط رہنے کے بارے میں بات کی، بشمول ویکسینیشن، جس کی وجہ سے انہوں نے کوویڈ 19 ویکسین حاصل نہ کرنے کا انتخاب کیا۔ ان میں سے بہت سے افراد نے ابتدائی طور پر فیصلہ کر لیا کہ وہ ویکسین نہیں لگائیں گے کیونکہ وہ 'اپنے جسم میں کچھ ڈالنا' پسند نہیں کرتے تھے۔
| " | میں کوئی بھی دوا اس کی ضرورت کے بغیر نہیں لیتا اور اس کے بارے میں سب کچھ جانتا ہوں، میں یقینی طور پر ایک واحد والدین کے طور پر بغیر ٹیسٹ شدہ ویکسین سے اپنی جان کو خطرے میں نہیں ڈالوں گا، یہ میرے بچوں کے بہترین مفاد میں نہیں ہوگا۔"
- وہ شخص جس نے ویکسین نہ لینے کا انتخاب کیا۔ |
وہ عوامل جو کووڈ-19 ویکسین کی بعد کی خوراکوں کے بارے میں فیصلوں سے آگاہ کرتے ہیں۔
CoVID-19 ویکسین کی ابتدائی خوراک کے بارے میں لوگوں کے فیصلے عام طور پر بعد کی خوراکوں کے بارے میں ان کے فیصلوں پر لاگو ہوتے ہیں۔ تاہم، چند لوگوں نے مزید خوراکیں لینے کے بارے میں فیصلے کرتے وقت مختلف عوامل پر غور کرنے کے بارے میں بات کی۔
اس گروپ میں سے کچھ لوگ وقت کے ساتھ ساتھ کووِڈ 19 کی وجہ سے شدید بیماری یا موت کے خطرات کے بارے میں کم فکر مند ہو گئے۔ ہو سکتا ہے کہ انہوں نے CoVID-19 ویکسین کی اپنی پہلی یا دوسری خوراک لینے کا انتخاب کیا ہو لیکن پھر بعد کی خوراکوں کے لیے اسے نہ لینے کا فیصلہ کیا۔ اکثر اس کی وجہ یہ تھی کہ انہوں نے محسوس کیا کہ ویکسینیشن کے فوائد خطرات سے زیادہ نہیں ہیں۔
| " | مجھے لگتا ہے بس، [2021 میں] یہ صرف ایک خوفناک چیز تھی. میرا بچہ ابھی بہت چھوٹا تھا اور ہم فکر مند تھے کہ اگر ہمارے پاس یہ نہ ہوا تو کچھ برا ہو سکتا ہے۔ میں بیمار ہو سکتا ہوں، میں واقعی خراب ہو سکتا ہوں، یا مر جاؤں گا۔ جبکہ 2022 میں، میں اس کے بارے میں ایک طرح سے زیادہ جانتا تھا اور مجھے کوویڈ تھا اور میں ٹھیک تھا، اور میں نے سوچا، 'دراصل، میں ویکسین کے راستے پر نہیں جاؤں گا'، کیونکہ میں اس وقت حاملہ تھی۔ نقطہ۔"
- ہر کہانی اہم شراکت دار |
کچھ نے بتایا کہ کس طرح CoVID-19 ویکسین کی پہلی خوراک کے منفی تجربات نے بعد میں خوراک نہ لینے کے اپنے فیصلے سے آگاہ کیا۔ ان شراکت داروں کو اکثر اپنی ابتدائی خوراک پر زیادہ شدید منفی ردعمل کا سامنا کرنا پڑا تھا جس کی وجہ سے وہ ہچکچاتے تھے اور بعض اوقات دوسری خوراک لینے سے ڈرتے تھے۔
| " | مجھے پہلی ویکسینیشن پر شدید ردعمل ہوا جو ایک جھٹکا تھا کیونکہ میں نہیں جانتا تھا کہ میں ایک اہم خطرہ تھا۔ علامات ان سے بدتر تھیں جن کا میں نے کوویڈ 19 کے ساتھ تجربہ کیا تھا۔ شدید بخار اور سردی لگ رہی ہے جس میں خوفناک سر درد ہے (ایک درد شقیقہ سے بھی بدتر)، میں کھڑا نہیں ہو سکتا تھا… میرے پاس دوسری خوراک اور اضافہ تھا لیکن میں زیادہ لینے سے گریزاں ہوں۔
- ہر کہانی اہم شراکت دار |
4. ویکسین کے اجراء کے تجربات |
 |
یہ باب ویکسین کے اجراء کے تجربات کو اکٹھا کرتا ہے۔ یہ اس بات کی وضاحت سے شروع ہوتا ہے کہ تعاون کنندگان نے ویکسین کی اہلیت اور ویکسینیشن اور امیونائزیشن کی مشترکہ کمیٹی کی طرف سے دی گئی ترجیحات کے بارے میں کیا سمجھا۔ اس کے بعد یہ خاص طور پر ویکسین کے رول آؤٹ کے تجربات پر بات کرنے کے لیے آگے بڑھتا ہے، بشمول بکنگ اپوائنٹمنٹ، ویکسین وصول کرنا، اور ایسا کرنے کے فوراً بعد کوئی بھی تجربہ۔
ویکسین اور امیونائزیشن کی مشترکہ کمیٹی کی جانب سے ویکسین کی اہلیت اور ترجیحات کے بارے میں سفارشات کو سمجھنا۔
بہت سے لوگوں نے محسوس کیا کہ CoVID-19 ویکسین کی ترجیح کے لیے جو طریقہ اختیار کیا گیا ہے وہ منصفانہ اور معقول تھا۔ تعاون کرنے والے اکثر اس بات کی عکاسی کرتے ہیں کہ محدود تعداد میں ویکسین دستیاب ہیں اور اس بات پر متفق ہیں کہ جن لوگوں کو CoVID-19 سے سب سے زیادہ خطرہ ہے انہیں دوسروں پر ترجیح دی جانی چاہیے۔
| " | میں ذاتی طور پر سوچتا ہوں کہ جس طرح سے انہوں نے اسے رول آؤٹ کیا وہ بہت، بہت اچھا تھا۔ ترجیح ان لوگوں کو دی گئی جن کی بالکل ضرورت تھی […] تو انہوں نے 85 سے شروع کیا، اور پھر 80، پھر 70، اور پھر باقی نے اس کے بعد کیا۔ لیکن یہ یکے بعد دیگرے تھا۔"
- ہر کہانی اہم شراکت دار |
| " | مجھے لگتا ہے کہ انہیں یہ حق مل گیا، ترجیح۔ میں نے سوچا کہ یہ ایک سمجھدار نقطہ نظر تھا، وہ حصہ۔
- ہر کہانی اہم شراکت دار |
کچھ طبی لحاظ سے کمزور اور طبی لحاظ سے انتہائی کمزور شراکت داروں نے سوال کیا کہ ان کے گھر کے دیگر افراد اسی وقت ویکسین کے لیے اہل کیوں نہیں تھے۔ ان شراکت داروں نے استدلال کیا کہ طبی طور پر کمزور لوگوں کے گھریلو رابطوں کو ویکسین کرنے سے یہ ان کے ارد گرد ایک 'حفاظتی بلبلہ' بنائے گا اور ان کے کوویڈ 19 کو پکڑنے کے امکانات کو مزید کم کرے گا۔ طبی لحاظ سے انتہائی کمزور شراکت داروں نے شدید مدافعتی دباؤ والے لوگوں کے گھریلو رابطوں کو ترجیح دینے کے حوالے سے رہنمائی میں تبدیلی کو سراہا جو بعد میں رول آؤٹ میں آیا۔
| " | مجھے ایسا لگتا ہے جیسے رول آؤٹ نے زیادہ احساس پیدا کیا ہو گا کہ اگر آپ کے گھر میں کوئی کمزور فرد ہوتا تو اس گھر کے ہر فرد کو جھنجھوڑ دیا جاتا۔ کیونکہ دوسری صورت میں آپ اب بھی لوگوں کے بیمار ہونے کا خطرہ چلا سکتے ہیں۔
- طبی لحاظ سے کمزور شراکت دار |
چند تعاون کنندگان فکر مند تھے کہ طبی لحاظ سے کمزور اور طبی لحاظ سے انتہائی کمزور لوگوں کو ترجیح دینے سے وہ اضافی خطرے میں پڑ سکتے ہیں۔ ان شراکت داروں نے ممکنہ ویکسین کے ضمنی اثرات اور طویل مدتی اثرات کی طرف اشارہ کیا۔
| " | میں سمجھتا ہوں، لیکن یہ بھی، آپ شاید اسے کسی اور نقطہ نظر سے دیکھ سکتے ہیں کہ، 'اوہ ٹھیک ہے۔ آپ سب سے پہلے سب سے زیادہ کمزور شخص کو ویکسین کر رہے ہیں اور اگر کچھ غلط ہونے جا رہا ہے، تو آپ جانتے ہیں، ان کے لیے اس پر قابو پانا اور اس سے صحت یاب ہونا مشکل ہو جائے گا۔"
- ہر کہانی اہم شراکت دار |
کچھ طبی طور پر کمزور اور طبی لحاظ سے انتہائی کمزور شراکت داروں نے بتایا کہ جب انہیں پیش کیا گیا تو وہ ویکسین لینے سے قاصر ہیں۔ کچھ نے ایوشیلڈ وصول کرنے کے لیے ادائیگی کرنے کا انتخاب کیا تھا۔2 ایک متبادل کے طور پر.
| " | میں نے سیکھا کہ مدافعتی قوت کے شکار لوگ اکثر ویکسین کے لیے اچھا یا بالکل بھی جواب نہیں دیتے۔ ایک ویکسین کے بعد میرے پاس کوئی اینٹی باڈیز نہیں تھیں اور 2 ویکسین کے بعد بہت کم مقدار تھی۔ جب تیسری بنیادی خوراک دی گئی تھی تب تک میرا اینٹی باڈی ردعمل کافی کم ہو چکا تھا اور مجھے تیسری بنیادی خوراک مل رہی تھی، صفر کے نقطہ آغاز کے ساتھ… میں نے ایوشیلڈ کے لیے بہت زیادہ فلایا ہوا (اور VAT سمیت) نجی نشان پر ادائیگی ختم کر دی۔ قیمت میں اضافہ، جس نے مجھے اس کی تاثیر کے آخر میں چند ماہ کی آزادی خریدی۔
- طبی لحاظ سے کمزور شراکت دار |
کچھ شراکت داروں نے محسوس کیا کہ دوسروں کو ویکسین حاصل کرنے کے لیے اعلی ترجیحی گروپوں میں شامل کیا جانا چاہیے تھا۔ اس میں کچھ ایسے بھی شامل تھے جو والدین تھے یا اسکولوں میں کام کرتے تھے اور محسوس کرتے تھے کہ بچوں کو ٹیکے لگانے سے تعلیمی ماحول میں منتقلی کم ہو جائے گی۔ دوسرے جو کلیدی کارکن تھے (مثال کے طور پر جیلوں یا سپر مارکیٹوں میں کام کرنے والے) یا جو بلا معاوضہ دیکھ بھال کرنے والے تھے انہوں نے بیان کیا کہ وہ کیسے محسوس کرتے ہیں کہ ان کے عہدے پر لوگوں کو ترجیح دی جانی چاہیے تھی۔
| " | یہ مایوس کن تھا کہ اساتذہ کو کلیدی کارکن نہیں سمجھا جاتا تھا اور یہ کہ میرا بہت سے عملہ اپنے بچوں کی دیکھ بھال کرنے کے ساتھ ساتھ آن لائن سیکھنے کا ایک مکمل پروگرام پیش کرنے کے ساتھ ساتھ کام کر رہا تھا… اس کے علاوہ، میرے عملے کو بہت کم قدر محسوس ہوئی جب وہ شروع میں اہل نہیں تھے۔ ویکسین کے لیے۔"
- وبائی امراض کے دوران اسکول ٹیچر |
| " | دیکھ بھال کرنے والوں کے طور پر، ہمیں ان لوگوں کے ساتھ ہی ٹیکہ کیوں نہیں لگایا گیا جن کی ہم دیکھ بھال کر رہے ہیں؟ یہ پاگل تھا، میری ماں کو ٹیکہ لگایا جا رہا تھا، وہ گھر آئے، یہ مضحکہ خیز تھا۔ کیا وہ صرف ایک ہی وقت میں مجھے نہیں کر سکتے تھے اور پھر ہمیں معلوم ہوتا کہ اس کی دیکھ بھال کی جا رہی تھی، اس میں کوئی جوڑ اپ سوچ نہیں تھی۔
- دیکھ بھال کرنے والا |
| " | میں ایک جیل میں کام کرتا ہوں اور ہمارے پاس کوئی مدد اور ابتدائی ویکسین تک رسائی نہیں تھی! یہ مجھے حیران کر دیتا ہے کہ معاشرے کے ایک پورے طبقے کو صرف نظر انداز کیا گیا تھا اور میرے جیل ونگ میں 88 آدمی تھے، 2-3 عملہ اس بات پر منحصر تھا کہ کتنے لوگ بیمار تھے اور مایوس، خوفزدہ قیدیوں اور عملے کو سنبھالنا پڑا۔ بہت کم جگہ پر بہت سے پرانے قیدیوں کے ہونے کے باوجود ہم 'کیئر سیٹنگ' کے طور پر اہل نہیں تھے اور اس وجہ سے مجھے کووڈ پازیٹو قیدیوں کی دیکھ بھال کرنی پڑتی تھی جن کے پاس PPE تھا اور ان کے پاس اپنی کوویڈ ویکسین نہیں تھی۔ اس وقت میری عمر 36 سال تھی اس لیے مجھے اہل ہونے کے لیے طویل انتظار کرنا پڑا۔
- وبائی امراض کے دوران جیل کا کارکن |
ویکسین کے اجراء کے تجربات
ویکسین کے لیے مدعو کیا جا رہا ہے اور ملاقات کا وقت بک کرایا جا رہا ہے۔
تعاون کنندگان نے مختلف طریقے بیان کیے جن میں انہیں CoVID-19 ویکسین کی پہلی خوراک لینے کے لیے مدعو کیا گیا تھا۔ بہت سے لوگوں نے NHS کی طرف سے ایک خط یا ٹیکسٹ پیغام کے ذریعے اس وجود کو یاد کیا۔ کچھ نے کہا کہ ان سے ان کے جی پی نے براہ راست رابطہ کیا تھا، جبکہ دوسروں نے میڈیا یا آن لائن میں ایسی معلومات دیکھی تھیں جن میں کہا گیا تھا کہ ان کی عمر کے لوگ اب بک کرنے کے اہل ہیں۔
زیادہ تر معاملات میں، اس مواصلت نے موصول ہونے والوں کو مطلع کیا کہ اب وہ اپوائنٹمنٹ بُک کر سکتے ہیں اور انہیں ایسا کرنے کے طریقہ کی تفصیلات بتائی ہیں۔ کچھ لوگوں نے کہا کہ ان کے لیے ملاقات کا وقت پہلے ہی بک کر لیا گیا تھا۔
| " | میرے خیال میں مجھے خط موصول ہوا، اور ایک پیغام بھی، میرے خیال میں۔ یہ بالکل واضح تھا، یہ اس کے قریب تھا جہاں میں رہ رہا تھا اور یہ صرف ایک ہفتہ پہلے کی بات ہے۔ مجھے بالکل یاد نہیں ہے، لیکن یہ کافی آسان تھا، یہ کوئی مسئلہ نہیں تھا۔
- ہر کہانی اہم شراکت دار |
| " | مجھے لگتا ہے کہ اس نے اچھا کام کیا۔ مجھے فون پر اپنا ملا، میں نے نمبر پر کال کی اور انہوں نے مجھے وقت، تاریخ اور مقام کے لیے آپشنز دیے اور میں نے اسے بک کر لیا۔
- ہر کہانی اہم شراکت دار |
تعاون کرنے والوں کو عام طور پر ویکسین کی بکنگ کا عمل سیدھا سا لگتا ہے۔ بہت سے لوگوں نے سرکاری ویب سائٹ یا NHS ایپ کے ذریعے آن لائن بک کروانے کی اطلاع دی۔ کچھ نے براہ راست اپنی جی پی سرجری کے ساتھ بک کروایا۔
اپوائنٹمنٹ کی دستیابی کو عام طور پر اچھا قرار دیا جاتا تھا، صرف چند شراکت داروں نے ان کے لیے کام کرنے والی تاریخ، وقت اور مقام پر ملاقات تلاش کرنے میں دشواریوں کا ذکر کیا۔ زیادہ دیہی علاقوں میں رہنے والے کچھ لوگوں نے گھر کے قریب ویکسین لینے کا اختیار حاصل کرنے کو ترجیح دی ہوگی۔
| " | اوہ، یہ مردہ سادہ ہاں تھا. آپ ویب سائٹ پر گئے، آپ نے اپنا مقام چن لیا، اور اس نے آپ کو تین جگہیں دیں جہاں سے آپ اسے حاصل کر سکتے ہیں، ویسے بھی میرے لیے۔
- ہر کہانی اہم شراکت دار |
| " | ہمارے پاس زیادہ انتخاب نہیں تھا…میرے خیال میں چونکہ ہم ایک مضافاتی علاقے میں ہیں، آس پاس کئی چھوٹی برادریاں ہیں، اس لیے ہر ایک کو اس ایک مرکز میں جانا پڑا۔ ہمارے علاقے میں صرف ایک مرکز تھا۔
- ہر کہانی اہم شراکت دار |
بہت کم تعداد میں لوگ تھے جنہوں نے بکنگ کے عمل کو زیادہ مشکل قرار دیا۔ ان میں وہ لوگ شامل تھے جن کے بوڑھے رشتہ دار یا خاندان کے افراد محدود انگریزی بولتے تھے، یا وہ لوگ جو بصارت سے محروم تھے۔
| " | میرے لیے یہ آسان تھا کیونکہ میں جانتا ہوں کہ کمپیوٹر کیسے کام کرنا ہے۔ لیکن مجھے یاد ہے کہ میرے نانا اور دادا کے لیے یہ آسان نہیں تھا۔
- ہر کہانی اہم شراکت دار |
| " | وہ لوگ جو بنگلہ دیش سے آتے ہیں، جو کچھ عرصے سے یہاں رہ رہے ہیں لیکن جو ابھی تک انگریزی اتنی اچھی طرح سے نہیں سیکھ سکے ہیں، انہیں ٹیکنالوجی تک رسائی حاصل کرنے میں مشکلات کا سامنا ہے۔ انہیں کسی پر بھروسہ کرنا پڑتا ہے۔"
- بنگلہ دیشی پس منظر سے تعلق رکھنے والا شخص |
| " | ویکسین کی تقرری کا عمل اسکرین ریڈرز کے لیے مکمل طور پر ناقابل رسائی تھا کیونکہ اس میں ایک عمل کے لیے نقشہ اور دوسرے کے لیے کیلنڈر استعمال کیا گیا تھا۔
- بصارت سے محروم شخص |
کچھ لوگ یہ جاننا چاہتے تھے کہ اپوائنٹمنٹ بک کرتے وقت وہ کس قسم کی ویکسین حاصل کریں گے۔ یہ عام طور پر دوسروں کے مقابلے میں کچھ ویکسین کے ساتھ منسلک ضمنی اثرات کے بارے میں خدشات سے منسلک تھا. ان تعاون کنندگان نے اس بات کی عکاسی کی کہ AstraZeneca ویکسین کے حوالے سے رہنمائی میں تبدیلی کے بعد یہ معلومات آن لائن بکنگ سسٹم پر دستیاب کرائی گئیں۔
| " | جس دن میں اپنی ویکسینیشن کے لیے گیا تھا، مجھے نہیں معلوم تھا کہ میں کون سا ٹیکہ لگاؤں گا، اور میرے لیے یہ معلوم کرنے کا کوئی طریقہ نہیں تھا۔ کچھ دیگر کی پیچیدگیوں کے ساتھ، اور یہ جانتے ہوئے کہ دودھ پلانے اور ویکسین کے بارے میں کوئی معلومات نہیں ہے، میں یہ سوچ کر اپنی ویکسینیشن کروانے گیا، 'مجھے یہ نہیں ہو گا جب تک کہ میں Pfizer حاصل نہ کر سکوں۔ میں اس کلینک کے بغیر چھوڑ کر خوش ہوں، اور یہی میرا موقف ہوگا۔'
- وہ عورت جو دودھ پلا رہی تھی جب ویکسین پیش کی گئی۔ |
کچھ شراکت داروں نے ملاقات کا وقت بک کرنے کے بجائے واک ان کلینک کا استعمال کیا۔ ان شراکت داروں کے لیے یہ اکثر ویکسین حاصل کرنے کا موقع پیش کرتا ہے اس سے پہلے کہ وہ دوسری صورت میں کرتے، یا سرکاری طور پر اہل ہونے سے پہلے۔ مثال کے طور پر، ہم نے کچھ نوجوان لوگوں سے سنا جو جلدی سے ویکسین لینے کے خواہشمند تھے تاکہ وہ سفر اور سماجی تعلقات پر واپس آ سکیں۔ دوسروں نے کہا کہ انہوں نے آسانی کے لیے واک اِن کلینک کا استعمال کیا ہے۔
| " | مجھے یاد ہے کہ جب ویکسین پہلی بار ریلیز ہوئی تھیں اور ٹائم سلاٹ دستیاب ہوں گے اور ہر کوئی ملاقات کا وقت بک کرنے کے لیے جلدی کرے گا اور اگر آپ کے ساتھیوں میں سے کسی کو پتہ چلا کہ وہاں کوئی سینٹر ہے جس کے پاس فالتو ہے، تو وہ یہ کہہ کر پیغام بھیجیں گے کہ 'یار، بک کرو یہاں میں جلدی سے وہاں جا کر نیچے جاؤ۔ جگہ ہے، فالتو ویکسین ہے۔"
- ہر کہانی اہم شراکت دار |
| " | میں اس کے لیے واک اِن سینٹر گیا، یہ آسان ہے نا؟ میں لفظی طور پر کام پر اپنے دوپہر کے کھانے کے اوقات میں کر سکتا تھا کیونکہ یہ اسی شہر میں تھا لہذا میں نے ابھی جا کر ایسا کیا۔ میں تقریباً دس منٹ میں اندر اور باہر تھا۔
- ہر کہانی اہم شراکت دار |
CoVID-19 ویکسین کی پہلی خوراک وصول کرنا
تعاون کرنے والے عام طور پر CoVID-19 ویکسین کی پہلی خوراک حاصل کرنے کے اپنے تجربے کے بارے میں مثبت تھے۔ ویکسینیشن مراکز کو اچھی طرح سے منظم اور اچھی طرح سے ترتیب دیا گیا تھا، اور عملے کو دوستانہ اور خوش آمدید کے طور پر دیکھا گیا تھا۔ شراکت داروں نے اس عمل کو سمجھنے میں آسان پایا اور بہت سے لوگوں کے لیے یہ نسبتاً تیز تھا۔
| " | نظام صرف حیرت انگیز تھا. ہم میں سے سینکڑوں ایک قطار میں تھے اور یہ سب طریقہ کار اور اتنا موثر تھا، یہ ناقابل یقین تھا کہ وہ اتنی اچھی چیز کو کیسے ترتیب دے سکتے ہیں۔ ایسا ہی محسوس ہوا۔ ہمیں ویکسینیشن دی گئی اور ہم سے کہا گیا کہ ہم جانے سے پہلے تقریباً 15 منٹ بیٹھ جائیں اگر ہمارے کوئی مضر اثرات ہوں تو۔ اور ایک بار جب ہم گھر پہنچے تو، ہمارے پاس ایک نمبر تھا کہ اگر کچھ غلط ہو جائے، لیکن میرے معاملے میں کچھ بھی غلط نہیں ہوا. میں بالکل ٹھیک تھا۔"
- ہر کہانی اہم شراکت دار |
| " | جب میں مرکز پہنچا تو یہ سب بہت اچھی طرح سے منظم تھا اور رضاکار اور عملہ، نرسیں، ڈاکٹر، وہ سب اتنے مددگار اور خوش مزاج تھے جو کہ واقعی اچھا تھا۔ واقعی عذاب کا کوئی احساس نہیں تھا۔ ایسا ہی تھا، آپ سب اس ویکسینیشن کے لیے یہاں موجود ہیں اور ہم اسے جاری رکھیں گے۔ اور مجھے لگتا ہے کہ یہ کافی تھا، اچھی طرح سے یہ ویکسین حاصل کرنے کے لئے ایک چیز کے لئے ایک راحت تھا. لیکن میرے خیال میں یہ کافی پر امید بھی تھا۔
- ہر کہانی اہم شراکت دار |
| " | یہ حیرت انگیز تھا کہ وہ تمام ویکسینیشن مراکز کیسے قائم کیے گئے تھے اور وہ کتنے منظم تھے۔ ایسا محسوس ہوا جیسے ہم سب مل کر کام کر رہے ہیں اس کے اوپر جانے کے لیے۔
- ہر کہانی اہم شراکت دار |
سماجی دوری کے اقدامات کے استعمال کا مطلب یہ تھا کہ بہت سے لوگوں نے کہا کہ جب انہیں پہلی ویکسین ملی تو وہ خود کو محفوظ محسوس کرتے ہیں۔
| " | سب کچھ واقعی اچھی طرح سے چل رہا تھا، ان کے پاس بہت سارے رضاکار تھے جو مدد کر رہے تھے، ہر کوئی واقعی اچھی جگہ پر تھا اور مجھے لگتا ہے کہ انہوں نے سب کو ماسک پہننے کی ترغیب دی، مجھے پورا یقین ہے کہ اس وقت ہر ایک نے ماسک پہنا تھا، میں نہیں کرتا۔ کسی کو دیکھنا یاد رکھیں جس نے نہیں دیکھا۔ ہاں، یہ محفوظ محسوس ہوا۔"
- وہ عورت جو حاملہ تھی جب اسے ویکسین دی گئی۔ |
| " | ہر ایک نے دو میٹر کے اصول کا مشاہدہ کیا، وہ چہرے کے ماسک پہنے ہوئے تھے، دروازے کھلے تھے۔ ہر چیز اچھی طرح سے ہوادار تھی۔"
- ہر کہانی اہم شراکت دار |
معذور افراد نے بعض اوقات ویکسینیشن مراکز تک رسائی میں رکاوٹوں کا سامنا کرنے کی وضاحت کی۔. مثالوں میں وہ مقامی مراکز شامل تھے جن کے پاس پارکنگ یا وہیل چیئر تک رسائی غیر فعال نہیں تھی، یا جہاں d/deaf لوگوں کے لیے ترجمان دستیاب نہیں تھے اور عملے میں بہرے سے آگاہی کی کمی تھی۔ ان معاملات میں، متاثرہ افراد نے مشورہ دیا کہ ان کے تقرری خط میں سہولیات کی رسائی کے بارے میں معلومات حاصل کرنا مفید ہوتا۔
| " | میں فارمیسی ویکسینیشن سروس تک رسائی حاصل نہیں کر سکا کیونکہ میں نقل و حرکت سے محروم ہوں اور کار پارکنگ کی ضمانت نہیں ہے… تمام معذوری کے قابل رسائی ویکسینیشن مراکز مہینوں کے لیے مکمل طور پر بک کیے گئے تھے!
- معذور شراکت دار |
| " | جب میں ویکسین سنٹر پہنچا تو میں ہر ایک کے اندر ہونے کے بارے میں بہت بے چین تھا۔ ایک ماسک، مجھے اپنی بیٹی کو اپنے ساتھ لے جانا پڑا، اور اسے ترجمانی کرنی پڑی کیونکہ ہمیں کوئی بھی ترجمان نہیں مل سکا۔ مجھے واقعی اپنے بچوں کو میرے لیے تشریح کرنے کے لیے استعمال نہیں کرنا چاہیے تھا۔ یہ بالکل مناسب نہیں ہے۔‘‘
- بہرے معاون |
کچھ تعاون کنندگان جو بلا معاوضہ دیکھ بھال کرنے والے تھے انہوں نے ویکسین سنٹر تلاش کرنے میں درپیش چیلنجوں کا بیان کیا جو اس شخص کی ضروریات کو پورا کر سکے جس کی وہ دیکھ بھال کرتے ہیں۔
| " | جب لوگ سپیکٹرم پر ہوتے ہیں، تو وہ ویکسینیشن کے لیے صرف عام جگہوں پر نہیں جا سکتے۔ مجھے حاصل کرنے کے لیے میلوں میل کا سفر طے کرنا پڑا [میرا بیٹا] ویکسین لگائی گئی، وہ لوگوں کو اسپیکٹرم پر بالکل بھی سہولت نہیں دیتے… اس لیے وہ نہیں ہیں، آپ جانتے ہیں، لوگوں کو فعال کر رہے ہیں، [کے ساتھ] اس قسم کی معذوری کو ٹیکہ لگایا جانا ہے۔"
- دیکھ بھال کرنے والا |
زیادہ دیہی علاقوں میں رہنے والوں کے لیے رسائی بھی ایک مسئلہ تھی، کچھ لوگ بغیر گاڑی کے ویکسین مراکز تک پہنچنے کے چیلنجوں کی عکاسی کرتے ہیں۔
| " | جب ویکسینیشن شروع کرنے کا وقت آیا، تو ہم نے محسوس کیا کہ ہمارا چھوٹا، الگ تھلگ گاؤں ہمارے خلاف کھیلا گیا، ہمیں زیادہ سے زیادہ لوگوں کے ساتھ رابطے میں آنے والے ویکسینیشن سینٹر تک جانے کے لیے لمبا سفر کرنا پڑے گا یا ایک سے زیادہ بسوں کا سفر کرنا پڑے گا۔"
- ہر کہانی اہم شراکت دار |
تاہم، رسائی کی ضروریات کے حامل کچھ شراکت داروں نے ویکسینیشن مراکز تک رسائی میں آسانی اور معذوری کے حامل افراد کے لیے جگہ پائی۔
| " | میں نے اسے قابل رسائی پایا، ہاں۔ ان کے پاس ایک ریمپ اور سب کچھ تھا، ان کے پاس ویٹنگ ایریا تھا، انہوں نے کچھ گیزبوس لگائے تاکہ لوگوں کو ان کی ویکسین لگنے کے بعد دس منٹ یا اس سے زیادہ کے لیے بیٹھ سکیں۔ ان کے پاس تمام انتظامات تھے۔
- معذور شراکت دار |
کچھ جو دودھ پلا رہے تھے جب انہیں پہلی ویکسین ملی تو انہوں نے مخصوص مثبت تجربات کا ذکر کیا۔ تعاون کرنے والوں نے دودھ پلانے کے لیے کمرہ فراہم کیے جانے کی مثالیں دیں، اور دوسروں کو قطار میں تیزی سے گزرنے کی اجازت دی گئی۔ کچھ نے بتایا کہ وہ دودھ پلانے کے دوران ویکسین لینے کے بارے میں خوفزدہ تھے لیکن کہا کہ عملے نے ان کے خدشات کو حساس طریقے سے نپٹایا، انہیں اضافی معلومات فراہم کیں۔
اگرچہ پہلی ویکسین حاصل کرنے کے تجربات عام طور پر بہت مثبت تھے، کچھ شراکت داروں نے بے چینی محسوس کرنے کا بیان کیا۔ انہوں نے محسوس کیا کہ ویکسینیشن مراکز غیر ذاتی یا طبی ہیں اور انہیں ایسا محسوس کرایا گیا ہے جیسے وہ 'کنویئر بیلٹ' پر ہیں۔
| " | یہ بہت ٹھنڈا تھا، یہ بہت طبی تھا، یہ بہت منظم تھا، آپ جانتے ہیں؟ آپ کو فرش پر ایک جگہ پر کھڑا ہونا پڑا اور وہاں کیمرے اور سیکورٹی گارڈز تھے۔ یہ ایک apocalyptic فلم سے باہر کی طرح محسوس ہوا۔ یہ ایک حقیقی، جیسے، ڈسٹوپین تھا، اگر یہ لفظ ہے تو، میرے خیال میں ایک ڈسٹوپین تجربہ ہے۔ لیکن اس کے بارے میں کچھ بھی نہیں بدلا جا سکتا تھا کیونکہ اس وقت حالات ایسے ہی تھے۔
- ہر کہانی اہم شراکت دار |
| " | میرا ایک ہسپتال میں تھا۔ یہ تقریباً ایک پوسٹ اپوکیلیپٹک فلم کی طرح تھا کیونکہ یہ اندر تھا، آپ کے پاس یہ لمبی راہداری تھی، راہداری کے دونوں طرف لوگوں کی لائنیں تھیں، اور پھر لوگوں کی کھیپ کو اندر بلایا گیا، وہ ایک سائیڈ روم میں چلے گئے۔ مجھے لگتا ہے کہ اس نے حقیقت میں مجھے ویکسین لگوانے کے بجائے صرف ترتیب سے زیادہ گھبراہٹ میں ڈال دیا۔
- ہر کہانی اہم شراکت دار |
CoVID-19 ویکسین کی پہلی خوراک حاصل کرنے کے بعد کے تجربات
تعاون کرنے والے اپنی پہلی ویکسینیشن کے بعد اکثر پرجوش یا پر امید تھے۔ کچھ لوگوں کے لیے، ویکسین کو ترقی کی علامت سمجھا جاتا تھا۔
| " | میں نے تھوڑا سا پرامید محسوس کیا کہ شاید ہم ایک طرح سے کہیں پہنچ رہے ہیں، کہ ہم دوبارہ زندگی میں جانے اور دوستوں اور کنبہ والوں کو دیکھنے کے قابل ہو جائیں گے۔ مجھے یاد ہے کہ [مقام] سے نکلنا تھا اور مجھے لگتا ہے کہ ان کے پاس ایک بڑا بل بورڈ تھا جہاں وہ ہر روز لگائی جانے والی ویکسین کی تعداد کو اپ ڈیٹ کر رہے تھے۔ مجھے صرف یہ سوچنا یاد ہے - ہاں، کافی پرامید، یہی تھا - کہ ہم نے کچھ ترقی کی ہو گی، میرا اندازہ ہے۔"
- ہر کہانی اہم شراکت دار |
| " | یہ میرے تمام خاندان کے لیے ایک بہت بڑی راحت تھی کہ یہ کیا گیا، خاص طور پر جب میں گھر میں دیکھ بھال کرنے والے تھے، جو ظاہر ہے کہ دوسرے لوگوں کے گھروں میں چلے گئے تھے۔
- ہر کہانی اہم شراکت دار |
| " | ویکسینیشن پروگرام حیرت انگیز تھا - ٹیکہ لگوانے میں جو راحت ہے وہ ناقابل بیان ہے، جب میرے شوہر کو ویکسین لگائی گئی تو میں رو پڑی۔
- ہر کہانی اہم شراکت دار |
تاہم، جیسا کہ پچھلے باب میں بیان کیا گیا ہے، کچھ نے اپنی پہلی ویکسین کے بعد ندامت یا خوف کے احساس کا ذکر کیا۔ اکثر ایسا اس لیے ہوتا تھا کہ انھوں نے سماجی دباؤ کے وسیع تر احساس سے ویکسین لینے کے لیے 'مجبور' محسوس کیا تھا یا اس لیے کہ یہ ان کے کام کی جگہ یا سفر یا سماجی تعلقات کے لیے ضروری تھا۔
| " | مجھے صرف یہ سوچنا یاد ہے، 'میں نے کیوں پریشان کیا؟' لیکن میں چھٹی پر جانے کے لیے اس پر نشان لگانا چاہتا تھا۔ مجھے یہ کہنا یاد ہے، 'اس کے بعد، مجھے مزید کچھ نہیں مل رہا ہے۔
- ہر کہانی اہم شراکت دار |
تعاون کرنے والے اکثر بتاتے ہیں کہ انہیں ویکسینیشن کے نتیجے میں معمولی ضمنی اثرات کا سامنا کرنا پڑا۔ عام طور پر، اس میں ہلکی علامات شامل ہیں جیسے بازو میں زخم یا بخار یا درد، نزلہ یا فلو ویکسین کے اثرات کی طرح۔
| " | اس کے علاوہ، موسم میں تھوڑا سا محسوس ہو رہا ہے، بازو میں بہت درد ہے، میرا مطلب ہے کہ مجھے ہمیشہ ہی رہتا ہے، اور حمل کے دوران بھی آپ کو فلو کا جھٹکا لگتا ہے، لیکن مجھے یاد ہے کہ یہ درد کی ایک اور سطح ہے، میں بہت زیادہ درد میں تھا۔ درد."
- وہ عورت جو حاملہ تھی جب اسے ویکسین دی گئی۔ |
| " | مجھے ابھی حسب معمول، ایک قدرے زخم بازو ملا اور بس۔ کوئی سائیڈ ایفیکٹ نہیں ہے۔"
- ہر کہانی اہم شراکت دار |
کچھ معاملات میں تعاون کرنے والوں نے ویکسینیشن کے بعد مزید شدید منفی ردعمل کا سامنا کرنے کے بارے میں بات کی۔ ایک چھوٹی سی تعداد نے ہمیں بتایا کہ وہ تجربہ کر چکے ہیں، اور یہ تجربہ کرتے رہتے ہیں۔ دوسروں نے خاندان، دوستوں یا دوسرے لوگوں کی مثالیں دیں جنہیں وہ جانتے تھے جنہوں نے ایسا کیا تھا۔
| " | ویکسین کی چوٹیں بہت حقیقی ہیں - میں جمنے کے مسائل کے پہلے ہاتھ کے تجربے سے کہتا ہوں جس نے مجھے 10 خوفناک دنوں تک ہسپتال میں رکھا جب مجھے یقین نہیں تھا کہ میں زندہ رہوں گا یا نہیں۔"
- ہر کہانی اہم شراکت دار |
| " | میرا ایک اور دوست ہے جو شدید زخمی ٹیکے لگا رہا ہے، ڈاکٹروں نے اس کا اعتراف کیا ہے۔ ویکسین لگوانے کے بعد اسے کیمسٹ میں anaphylactic جھٹکا لگا، وہ 28 سال کی ہے اور اب اس کی زندگی نہیں ہے۔ وہ کام نہیں کر سکتی وہ ٹھیک نہیں ہے۔‘‘
- ہر کہانی اہم شراکت دار |
شدید منفی ردعمل کا سامنا کرنے والے کچھ لوگوں نے بتایا کہ وہ کتنے مایوس اور غصے میں تھے کہ ان پر اور ان کی صحت پر پڑنے والے اثرات کو تسلیم کرنے اور ان سے نمٹنے کے لیے کتنا کم کیا گیا۔ انہوں نے محسوس کیا کہ ویکسین کی چوٹوں کو اکثر انڈر پلے، برخاست اور نظر انداز کیا جاتا ہے۔ ان تعاون کنندگان نے طبی پیشہ ور افراد کی مثالیں دیں جو انہیں سنجیدگی سے لینے یا انہیں وہ دیکھ بھال فراہم کرنے میں ناکام رہے جس کی انہیں ضرورت تھی۔
| " | میں ویکسین سے زخمی ہو گیا ہوں۔ تمام ڈاکٹروں نے یہ کیا ہے کہ مجھے دوا دو، بس، وہ تسلیم نہیں کرتے کہ یہ ویکسین کی چوٹ ہے۔ ایسا لگتا ہے کہ جب میں جی پی سے بات کرتا ہوں تو میں خالی دیوار سے بات کر رہا ہوں۔"
- ہر کہانی اہم شراکت دار |
وہ لوگ جنہوں نے ذاتی طور پر یا دوسروں کے ذریعے ویکسین کی چوٹ کا تجربہ کیا وہ اکثر جسمانی اثرات، بلکہ ان کی نفسیاتی اور سماجی بہبود پر پڑنے والے اثرات پر بھی بات کرتے تھے۔ بعض نے مثالیں دیں کہ ان کی صحت پر منفی اثرات کس طرح مالی مشکلات کا شکار ہوئے۔
| " | مجھے اس منفی واقعے سے نہ صرف جسمانی بلکہ ذہنی طور پر بھی بہت نقصان پہنچا ہے۔ ویکسین کی چوٹ کے ساتھ ایک بہت بڑا بدنما داغ ہے جو متاثرہ افراد کے ساتھ انتہائی غیر منصفانہ ہے۔ کوئی بھی اس کے بارے میں سننا نہیں چاہتا، کچھ لوگ میری بیماری کی وضاحت کرنے کی کوئی اور وجہ ڈھونڈنے کی کوشش کرتے ہیں۔
- ہر کہانی اہم شراکت دار |
| " | میری ویکسین کی چوٹ کا نتیجہ بنیادی طور پر جسمانی تھا، کمزور علامات کے ساتھ جس کی وجہ سے میں ایک طویل مدت تک کام کرنے سے قاصر رہا۔ اس نے نہ صرف میری فلاح و بہبود کو متاثر کیا بلکہ اس نازک وقت کے دوران میری ملازمت کے کھو جانے اور مدد کی کمی کی وجہ سے ایک اہم مالی اثر بھی پڑا۔"
- ہر کہانی اہم شراکت دار |
Covid-19 ویکسینز کی بعد میں خوراک حاصل کرنے کے تجربات
تعاون کرنے والے جنہوں نے بعد میں کووِڈ-19 ویکسین کی خوراکیں حاصل کیں، انھوں نے عام طور پر ہمیں بتایا کہ ان کے تجربات ان کی پہلی خوراک سے ملتے جلتے تھے۔ بہت سے لوگوں نے اپنی دوسری خوراک اسی وقت بک کی تھی جب انہوں نے اپنی پہلی خوراک بک کی تھی اور اسے حاصل کرنے کے لیے اسی جگہ پر حاضر ہوئے تھے۔
| " | واقعی بالکل اسی طرح. میں نے انہیں اسی جگہ پر کیا تھا، اسی طرح کے ردعمل۔
- ہر کہانی اہم شراکت دار |
چند لوگوں کے لیے، پہلی خوراک حاصل کرنے کے ان کے تجربات نے انھیں بعد میں کوئی خوراک لینے پر مجبور کیا۔ عام طور پر، اس کی وجہ یہ تھی کہ انہوں نے اپنی پہلی ویکسین کے بعد پریشان کن ضمنی اثرات کا تجربہ کیا تھا۔
| " | میں نے کتنا بیمار محسوس کیا، اس نے واقعی مجھے ایک اور رکھنے پر مجبور کر دیا۔
- ہر کہانی اہم شراکت دار |
2. ایوشیلڈ ایک 'پری ایکسپوژر پروفیلیکسس' علاج ہے، مطلب یہ ہے کہ یہ کووڈ-19 کو انفیکشن لگنے کے خطرے سے پہلے روکا جائے۔ ماخذ: ادویات اور صحت کی دیکھ بھال کی مصنوعات کی ریگولیٹری ایجنسی
5. طبی لحاظ سے کمزور اور طبی لحاظ سے انتہائی کمزور شراکت داروں کے درمیان CoVID-19 کے علاج کی اہلیت کے بارے میں آگاہی اور سمجھ |
 |
یہ باب طبی طور پر کمزور اور طبی لحاظ سے انتہائی کمزور شراکت داروں کے درمیان CoVID-19 کے علاج کے لیے اہلیت کے معیار کے بارے میں آگاہی اور تفہیم کی تلاش کرتا ہے۔ کووڈ-19 کے علاج کے بارے میں آگاہی اور ان علاجوں کے لیے اہلیت کے معیار کو سمجھنے کے لیے آگے بڑھنے سے پہلے، یہ ان افراد کی کووڈ-19 سے شدید بیماری کے ان کے ذاتی خطرے کے بارے میں تفہیم کو بیان کرنے سے شروع ہوتا ہے۔
طبی لحاظ سے کمزور شراکت داروں کے درمیان CoVID-19 سے سنگین بیماری کے ذاتی خطرے کے تصورات
طبی طور پر کمزور اور طبی لحاظ سے انتہائی کمزور شراکت داروں کو عام طور پر CoVID-19 کو اپنی صحت کے لیے ایک اہم خطرہ سمجھا جاتا ہے۔ انہوں نے CoVID-19 کے معاہدے کے بارے میں خوفزدہ ہونے اور اس سے ان پر اور ان کے خاندانوں پر کیا اثر پڑے گا کے بارے میں بتایا۔ بہت سے لوگ مرنے کے بارے میں فکر مند ہیں اگر وہ وائرس پکڑ لیتے ہیں۔ اس وجہ سے، زیادہ تر نے حفاظت کے لیے رہنمائی کی پیروی کی جب تک کہ وہ اپنی پہلی ویکسین حاصل نہ کر لیں۔
| " | میں نے اپنی صحت کے ساتھ ایک مشکل زندگی گزاری ہے، اور میں مختلف مقامات پر کافی خراب رہا ہوں۔ لیکن میں عام طور پر صرف اس کے ساتھ مل گیا ہے. جب کووڈ ہوا، اگر میں ایماندار ہوں، تو میں نے کبھی نہیں سوچا تھا کہ میں موت سے اتنا خوفزدہ ہوں گا جتنا میں اس وقت تھا، اگر یہ سمجھ میں آتا ہے۔ میں نے کبھی نہیں سوچا تھا کہ باہر کی دنیا میں جانا خوفناک ہوگا۔ لیکن جب کوویڈ مارا گیا، یہ دنوں میں بدل گیا۔ تو ایک دن میں کام پر ہوں، اور اگلے دن ہمیں اپنے آپ کو گھر کے اندر بند کرنا پڑا… چیزوں کو اس طرح بدلنے کے لیے، اس طرح سے اپنی زندگی کے لیے خوفزدہ ہونا، یہ واقعی خوفناک تھا۔
- طبی لحاظ سے کمزور شراکت دار |
| " | میں کمزور ہوں کیونکہ مجھے صحت کے کچھ نسبتاً سنگین مسائل ہیں۔ میں پریشان تھا، میں فکر مند تھا، لیکن میں نے صرف سوچا کہ 'مجھے کسی بھی ممکنہ مسائل کو کم کرنے کے لیے کچھ عملی اقدامات کرنے کی ضرورت ہے'۔ جب میں ڈھال بنا رہا تھا، میں سیر کے لیے جا رہا تھا اور میں ماسک پہنوں گا۔ تھوڑا سا شدید لگتا ہے، لیکن آپ کو کبھی معلوم نہیں ہے؟…میں جا کر اپنے پڑوسیوں کو نہیں دیکھ سکتا تھا، مجھے ان سے دور سے یا فون پر بات کرنی پڑتی تھی، اور میں ان کے ساتھ کافی دوستانہ ہوں۔ اس نے نہ صرف میری صحت بلکہ میری ذہنی صحت کو متاثر کیا۔
- طبی لحاظ سے کمزور شراکت دار |
CoVID-19 کے علاج تک رسائی کے لیے اہلیت کے معیار کے بارے میں آگاہی اور سمجھ
وبائی مرض کے جواب میں کووڈ-19 سے شدید بیمار ہونے کے سب سے زیادہ خطرہ والے لوگوں کے لیے علاج کی ایک رینج دستیاب کرائی گئی۔ جو دستیاب ہیں ان میں نرماتریلویر پلس ریتوناویر (پاکسلوویڈ)، سوٹروویماب (Xevudy)، molnupiravir (Lagevrio)، اور remdesivir (Veklury) شامل ہیں۔ ان علاجوں اور ادویات کا مقصد سنگین بیماری کے خطرے میں مبتلا افراد کو ان کی CoVID-19 علامات کو منظم کرنے اور شدید بیمار ہونے کے خطرے کو کم کرنے میں مدد کرنا تھا۔
طبی لحاظ سے کمزور لوگوں میں سے کچھ جن سے ہم نے سنا وہ کووڈ 19 کے لیے صحت کے نظام کے ذریعے بنائے گئے علاج سے واقف تھے۔ انہوں نے عام طور پر NHS ویب سائٹ یا چیف میڈیکل آفیسر کی طرف سے بھیجے گئے مواصلات کے ذریعے علاج کے بارے میں سنا تھا۔ دوسروں نے ان علاجوں کے بارے میں مقامی سپورٹ گروپس کے ذریعے سننے کا ذکر کیا جن کی حالت ان لوگوں کے لیے تھی جہاں CoVID-19 کے علاج کے بارے میں معلومات پر تبادلہ خیال کیا گیا تھا۔ وہ سمجھ گئے کہ یہ وہ علاج ہیں جو ان جیسے لوگوں کے لیے دستیاب ہیں، جن کو CoVID-19 سے شدید بیمار ہونے کا زیادہ خطرہ تھا۔
| " | مجھے میرے خیال میں چیف میڈیکل آفیسر یا محکمہ صحت کے کسی قسم کے خطوط اور ای میلز ملے ہیں جن میں مجھے ان کے بارے میں بتایا گیا ہے… اور میرے خیال میں میرے خیال میں لوگ [صحت کی حالت] فیس بک گروپ ان پر بحث کر رہے تھے۔
- طبی لحاظ سے کمزور شراکت دار |
| " | میں نے ان کے بارے میں سنا لیکن مجھے ان میں سے کسی کی پیشکش نہیں کی گئی۔ میں نے سنا ہے کہ اگر ہم اس سے متاثر ہو جاتے ہیں، تو اس سے زیادہ تکلیف نہ ہونے میں ہماری مدد کے لیے ایک علاج دستیاب تھا۔ لیکن میں نے کبھی اس کا معاہدہ نہیں کیا لہذا مجھے کبھی بھی کوئی علاج نہیں کرنا پڑا۔ لہذا میں ان کے بارے میں بہت کچھ نہیں جانتا تھا لیکن میں جانتا تھا کہ اگر ہمیں اس کی ضرورت ہو تو ہمارے لئے وہاں علاج موجود ہیں۔
- طبی لحاظ سے کمزور شراکت دار |
علاج تک رسائی کے تجربات ملے جلے تھے۔ کچھ لوگوں نے علاج تک رسائی آسان اور سیدھی پائی۔ ان شراکت داروں نے NHS 111 پر کال کرنے یا مثبت ٹیسٹ کے بعد ٹیسٹ اینڈ ٹریس کے ذریعے رابطہ کرنے کا ذکر کیا۔ ان بات چیت کے دوران ان سے کئی سوالات پوچھے گئے تاکہ یہ معلوم کیا جا سکے کہ آیا وہ علاج کے اہل ہیں یا نہیں۔ اہل سمجھے جانے والوں کو یا تو علاج کروانے کے لیے ہسپتال میں داخل کرایا گیا یا گھر پر لے جانے کے لیے علاج فراہم کیا گیا۔ انہوں نے اکثر محسوس کیا کہ ان علاجوں سے ان کی علامات کی شدت کو کم کرنے میں مدد ملی اور وہ ان کے موصول ہونے پر شکر گزار تھے۔
| " | جیسا کہ ذکر کیا گیا ہے، مجھے چیف میڈیکل آفیسر کی طرف سے اپ ڈیٹس کے ساتھ باقاعدہ خطوط موصول ہوئے… ان خطوط میں سے ایک مجھے کووڈ پکڑے جانے کے فوراً بعد پہنچا جس میں مشورہ دیا گیا تھا کہ مجھے اینٹی وائرل علاج کے لیے سمجھا جا سکتا ہے… مثبت آنے پر مجھے ٹیسٹ اینڈ پروٹیکٹ نے مشورہ دینے کے لیے مجھ سے رابطہ کیا تھا۔ علاج کے لیے اہل ہو سکتے ہیں اور پوچھیں کہ کیا میں دلچسپی رکھتا ہوں۔ مجھے اپنی Covid علامات اور اپنی طبی تاریخ کے بارے میں تفصیلات سے متعلق ایک سوالنامے سے گزرنا پڑا۔ جس شخص سے میں بات کر رہا تھا اس نے اتفاق کیا کہ میں علاج کے لیے اہل ہوں، لیکن میری طبی تاریخ کی وجہ سے وہ میرے علاج سے قبل اپنے ہسپتال کے مشیر سے کووِڈ اور ممکنہ علاج پر بات کرنا چاہتا تھا۔ مجھے مشورہ دیا گیا کہ جب بحث ہو جائے تو مجھے اگلی صبح ایک اور فون کال موصول ہو گی۔ مجھے اگلے دن جلد بلایا گیا تاکہ میرے لیے دوائیں لینے کے انتظامات کیے جا سکیں… انہوں نے مجھے فوری طور پر ہسپتال منتقل کرنے کا انتظام کیا اور میں خوش قسمت تھا کہ میں IV کی شکل میں اینٹی باڈی علاج حاصل کر سکا۔
- طبی لحاظ سے کمزور شراکت دار |
دوسروں نے علاج تک رسائی کے چیلنجوں کا سامنا کرنے کی وضاحت کی۔ ان شراکت داروں نے اس بارے میں الجھن کا اظہار کیا کہ کون علاج کے لیے اہل تھا اور کون نہیں تھا۔ کچھ لوگوں نے وبائی امراض کے دوران NHS اور چیف میڈیکل آفیسر سے موصول ہونے والی معلومات کی بنیاد پر خود کو اہل سمجھا۔ تاہم، جب انہوں نے NHS سے رابطہ کیا یا ٹیسٹ اینڈ ٹریس سے بات کی تو انہیں بتایا گیا کہ وہ علاج کے اہل نہیں ہیں۔ جن لوگوں نے اس کا تجربہ کیا وہ غصے اور مایوسی کا شکار ہوئے لیکن ان کے انفیکشن کے بڑھنے کے ساتھ ان کے ساتھ کیا ہو سکتا ہے اس کے بارے میں خوفزدہ بھی ہوئے۔
| " | جب مجھے معلوم ہوا کہ سانس کے مریض اینٹی وائرل ادویات کے اہل نہیں ہیں تو میں بہت زیادہ مایوس اور مایوس ہوا۔ انہیں متعدد خطوط بھیجے گئے تھے جن میں کہا گیا تھا کہ وہ حفاظت کریں لیکن ان کو اتنا بیمار نہیں سمجھا گیا کہ وہ اینٹی وائرل وارنٹ دیں۔ ہمارے تمام دوست کسی نہ کسی طرح کے معمولات سے لطف اندوز ہونے کے لیے واپس آ گئے تھے لیکن پھر بھی ہم اس خوف سے بہت زیادہ گھل مل جانے سے ڈرتے تھے کہ کووِڈ کا اثر کمزور شخص پر پڑے گا۔ میں نے متعدد سیاست دانوں کو خط لکھا… ان سے کہا کہ وہ سینے کی بیماری والے لوگوں کے لیے اینٹی وائرل کے لیے لڑیں۔ یہ بیکار تھا۔ اس کے باوجود برطانیہ کے دوسرے حصوں میں کچھ لوگ اینٹی وائرل علاج کے حقدار ہیں۔ یہ ایک لاٹری کی طرح لگتا ہے."
- طبی لحاظ سے کمزور کنٹریبیوٹر کے فیملی ممبر |
کچھ نے تشخیص کی رفتار پر تشویش کا اظہار کیا، اس کے ساتھ بعض اوقات 48 گھنٹے سے زیادہ وقت لگتا ہے جس کے اندر وہ سمجھتے تھے کہ علاج شروع ہونا چاہیے۔
| " | میرے شوہر کو مئی 2021 تک ہمارا فلیٹ بالکل بھی نہ چھوڑنے کے بعد CoVID-19 ہو گیا۔ ہم نے NHS 111 اور دیگر متعدد فون نمبروں پر کال کی مسلسل یہ جاننے کی کوشش کی کہ ہم یہ کیسے جان سکتے ہیں کہ انہیں کب پتہ چلے گا کہ وہ ہسپتال میں داخل ہوں گے، لیکن کب۔ اس نے کہا کہ اسے سانس لینے میں تکلیف نہیں ہو رہی ہے ہم نے کچھ نہیں سنا۔ تین دن کے بعد اسے ایک کال موصول ہوئی جس میں کہا گیا تھا کہ ہمارے مقامی ہسپتال میں ایک ڈاکٹر اس کی معلومات کا جائزہ لے رہا ہے – یہ پہلے ہی اس کے مثبت ٹیسٹ کے 48 گھنٹے بعد اور کھڑکی کے باہر اینٹی وائرل علاج شروع کرنے کی سفارش کی گئی تھی۔
- طبی لحاظ سے انتہائی کمزور کنٹریبیوٹر کے فیملی ممبر |
NHS میں مستقل مزاجی کی کمی کی وجہ سے مایوسی کے جذبات میں اضافہ ہوا۔ کچھ شراکت داروں نے NHS کے عملے کی طرف سے متضاد مشورے دیئے جانے کا ذکر کیا، یا ان لوگوں کے بارے میں سنا جن کی حالت ان کی حالت میں تھی جنہیں کسی اور جگہ علاج کرایا گیا تھا لیکن انہیں بتایا گیا تھا کہ وہ اس کے اہل نہیں ہیں۔
| " | نرسیں پریشان اور الجھن میں تھیں کہ وہ مجھے اینٹی وائرل علاج نہیں دے سکتیں، جو انہیں پریشان دیکھ کر اچھا نہیں لگا۔ میرا [صحت کی حالت] جیسے ہی میں کوویڈ پکڑا گیا ٹیم کو یقینی طور پر مزید شامل ہونے اور بہتر طور پر آگاہ کرنے کی ضرورت تھی۔
- طبی لحاظ سے کمزور شراکت دار |
| " | ہمیں اب طبی لحاظ سے کمزور لوگوں کے ارد گرد موجود کل افراتفری کو دیکھنے کی ضرورت ہے جب وہ کوویڈ پکڑتے ہیں تو اینٹی وائرل علاج تک رسائی حاصل کرنے کی کوشش کرتے ہیں۔ اس گروپ کے اندر خوفناک کہانیاں سنائی جاتی ہیں جب وائرس پکڑتے وقت اپنے جی پی سے رابطہ کرنے کے لیے، جو کچھ نہیں جانتا، این ایچ ایس 111، جو ان سے جی پی کو فون کرنے کے لیے، یا بے نقاب مریضوں اور طبی عملے کے ساتھ اے اینڈ ای ڈیپارٹمنٹ میں جانے کو کہتے ہیں۔
- طبی لحاظ سے کمزور شراکت دار |
کچھ لوگوں نے علاج کے لیے رابطہ کرنے کا ذکر کیا حالانکہ انہیں یقین تھا کہ وہ اہل نہیں ہیں۔
| " | جب CoVID-19 سے متاثرہ لوگوں کے علاج کے لیے اینٹی وائرل ادویات دستیاب ہوئیں تو مجھے ایک ای میل موصول ہوئی جس میں مجھے متنبہ کیا گیا تھا کہ اگر میں انفیکشن کا شکار ہوں تو میں اس علاج کے لیے اہل ہوں، حالانکہ صرف اس صورت میں جب جلد علاج کیا جائے، اور یہ کہ جلد پتہ لگانے میں مدد کے لیے، مجھے ایک PCR کٹ بھیجی جائے گی۔ اگر مجھے انفیکشن کا شبہ ہو تو استعمال کرنا۔ میں حیران تھا کیونکہ میں کسی بھی خطرے والے گروپ میں نہیں ہوں اور مجھے کبھی بھی حفاظت کرنے کا مشورہ نہیں دیا گیا تھا۔ میں نے کٹ وصول کی اور اسے ایک طرف رکھ دیا۔ جب میں متاثر ہوا، میں نے مشورہ پر عمل کیا اور نمونہ جمع کرایا۔ پھر مجھے اینٹی وائرل علاج شروع کرنے کے لیے ایک فون کال موصول ہوئی۔ ایجنٹ نے مشورہ دیا کہ مجھے اعضاء کا عطیہ کرنے کے طور پر ریکارڈ کیا گیا ہے، جو کہ ایسا نہیں ہے۔ ہم نے اتفاق کیا کہ مجھے اس فہرست میں غلط طریقے سے شامل کیا گیا ہے اور ہم نے اینٹی وائرل علاج کے ساتھ آگے نہیں بڑھایا۔"
- ہر کہانی اہم شراکت دار |
3. ایوری سٹوری میٹرز میں تعاون کرنے والوں میں ان لوگوں کی شناخت کرنا ہمیشہ ممکن نہیں ہوتا جو طبی لحاظ سے کمزور ہیں اور جو طبی لحاظ سے انتہائی کمزور ہیں۔ اس کی وجہ یہ ہے کہ سبھی شراکت داروں نے اپنی کہانیاں شیئر کرتے وقت یہ معلومات فراہم نہیں کیں۔ جہاں ممکن ہو، ہم نے اس بارے میں معلومات شامل کی ہیں کہ آیا تعاون کرنے والے طبی لحاظ سے کمزور ہیں یا طبی لحاظ سے انتہائی کمزور ہیں۔ جب یہ معاملہ نہیں ہے، تو ہم ان تمام لوگوں کے بارے میں بات کرتے ہیں جن سے وبائی امراض کے دوران 'طبی لحاظ سے کمزور' تعاون کرنے والوں کو بچانے کے لیے کہا گیا تھا۔
6. ضمیمہ |
ماڈیول 4 عارضی دائرہ کار
ماڈیول 4 کا عارضی دائرہ کار اس رہنمائی کے لیے استعمال کیا گیا کہ ہم لوگوں کو کس طرح سنتے ہیں اور ان کی کہانیوں کا تجزیہ کرتے ہیں۔ ماڈیول کی گنجائش ذیل میں بیان کی گئی ہے اور یہ UK Covid-19 انکوائری ویب سائٹ پر بھی پایا جا سکتا ہے۔ یہاں.
یہ ماڈیول CoVID-19 ویکسینز کی ترقی اور انگلینڈ، ویلز، اسکاٹ لینڈ اور شمالی آئرلینڈ میں ویکسین رول آؤٹ پروگرام کے نفاذ سے متعلق متعدد مسائل پر غور کرے گا اور سفارشات پیش کرے گا۔ موجودہ اور نئی دوائیوں کے ذریعے CoVID-19 کے علاج سے متعلق مسائل کا متوازی طور پر جائزہ لیا جائے گا۔ سیکھے گئے اسباق اور اگلی وبائی بیماری کے لیے تیاری پر توجہ دی جائے گی۔
غیر مساوی ویکسین اپٹیک سے متعلق موضوعاتی مسائل کا جائزہ لیا جائے گا، جس میں ان گروپوں کی شناخت کو شامل کیا جائے گا جو غیر مساوی اپٹیک کا موضوع تھے، اس طرح کے غیر مساوی اپٹیک کی ممکنہ وجوہات، اور حکومتی ردعمل۔
یہ ماڈیول ویکسین کی حفاظت اور یوکے ویکسین ڈیمیج پیمنٹ اسکیم کے تحت مالی ازالے کے لیے موجودہ نظام سے متعلق حالیہ عوامی تشویش کے مسائل کو حل کرے گا۔
خاص طور پر، یہ ماڈیول جانچے گا:
- وبائی مرض کے دوران ویکسین کی ترقی، حصول، تیاری اور منظوری، بشمول برطانیہ بھر میں فیصلہ سازی کی تاثیر، خاص طور پر یو کے ویکسین ٹاسک فورس کا کردار۔ ہم ان اختراعی طریقوں سے کیا سبق سیکھ سکتے ہیں جو مستقبل میں وبائی امراض کی تیاری کے لیے وبائی امراض کے دوران کامیابی کے ساتھ متعارف کروائے گئے تھے؟
- وبائی امراض کے دوران نئے علاج معالجے کے استعمال کو قابل بنانے کے لیے کی گئی ترقی، آزمائشیں اور اقدامات۔
- انگلینڈ، ویلز، سکاٹ لینڈ، اور شمالی آئرلینڈ میں ویکسین کی ترسیل، بشمول رول آؤٹ کے طریقہ کار جیسے:
زمینی اور عوامی پیغام رسانی: ویکسینیشن اور حفاظتی ٹیکوں کی مشترکہ کمیٹی کی اہلیت/ترجیحات اور پالیسی سازوں کی طرف سے لیے گئے فیصلے؛ ترجیحی فیصلوں کی اخلاقیات اور خاص گروپوں پر اثرات جیسے کہ وہ لوگ جو کموربیڈیٹیز میں مبتلا ہیں۔ تعیناتی کی شرط کے طور پر ویکسین، خاص طور پر ٹرانسمیشن کو محدود کرنے میں اس کی تاثیر اور ویکسین کی ہچکچاہٹ پر اثر۔ - ویکسین لینے میں رکاوٹیں، بشمول ویکسین کے اعتماد اور رسائی کے مسائل اور ویکسین کے استعمال سے متعلق عدم مساوات کے لیے حکومت کی منصوبہ بندی کی تاثیر، بروقت، اور کافییت۔
- ویکسین کی حفاظت کے مسائل بشمول پوسٹ مارکیٹنگ کی نگرانی، جیسے یلو کارڈ کی نگرانی اور رپورٹنگ کا نظام اور تجویز کردہ
CoVID-19 ویکسینز اور قلبی مسائل کے درمیان ارتباط۔ - کیا یو کے ویکسین ڈیمیج پیمنٹ اسکیم میں کوئی اصلاحات ضروری ہیں۔
براہ کرم نوٹ کریں کہ ماڈیول 4 کے لیے ہدف شدہ تحقیق کلیدی خطوط انکوائری (KLOEs) 3 اور 4 پر مرکوز ہے۔
کس طرح لوگوں نے اپنی کہانی ہمارے ساتھ شیئر کی۔
ماڈیول 4 کے لیے لوگوں کی کہانیاں جمع کرنے کے تین مختلف طریقے ہیں:
آن لائن فارم
عوام کے ارکان کو ایک مکمل کرنے کے لیے مدعو کیا گیا تھا۔ انکوائری کی ویب سائٹ کے ذریعے آن لائن فارم (کاغذی فارم بھی شراکت داروں کو پیش کیے گئے اور تجزیہ کے لیے آن لائن فارم کے ذریعے شامل کیے گئے)۔ اس نے ان سے اپنے وبائی تجربے کے بارے میں تین وسیع، کھلے سوالات کے جوابات دینے کو کہا۔ یہ سوالات تھے:
- ہمیں اپنے تجربے کے بارے میں بتائیں
- ہمیں اپنے اور اپنے آس پاس کے لوگوں پر اثرات کے بارے میں بتائیں
- ہمیں بتائیں کہ آپ کے خیال میں کیا سیکھا جا سکتا ہے۔
فارم نے ان کے بارے میں پس منظر کی معلومات (جیسے ان کی عمر، جنس اور نسل) جمع کرنے کے لیے دیگر آبادیاتی سوالات پوچھے۔ آن لائن فارم کے جوابات گمنام طور پر جمع کرائے جاتے ہیں۔
اس کی نوعیت کے مطابق، جن لوگوں نے آن لائن فارم میں تعاون کیا وہ وہ تھے جنہوں نے ایسا کرنے کا انتخاب کیا، اور انہوں نے صرف وہی شیئر کیا جس میں وہ آرام سے تھے۔
ماڈیول 4 کے لیے، ہم نے CoVID-19 ویکسینز سے متعلق 34,441 کہانیوں کا تجزیہ کیا۔ اس میں انگلینڈ سے 28,246 کہانیاں، سکاٹ لینڈ سے 2,756، ویلز سے 3,133 اور شمالی آئرلینڈ سے 1,679 کہانیاں شامل ہیں (مطالعہ کنندگان آن لائن فارم میں ایک سے زیادہ یو کے قوم کو منتخب کرنے کے قابل تھے، اس لیے کل موصول ہونے والے جوابات کی تعداد سے زیادہ ہوں گے)۔
جوابات کا تجزیہ نیچرل لینگویج پروسیسنگ (NLP) کے ذریعے کیا گیا، جو ڈیٹا کو بامعنی انداز میں ترتیب دینے میں مدد کے لیے مشین لرننگ کا استعمال کرتا ہے۔ الگورتھمک تجزیہ اور انسانی جائزے کا مجموعہ پھر کہانیوں کو مزید دریافت کرنے کے لیے استعمال کیا جاتا ہے۔
NLP تجزیہ فری ٹیکسٹ ڈیٹا کے اندر زبان کے بار بار نمونوں کی نشاندہی کرتا ہے۔ اس کے بعد یہ اس ڈیٹا کو 'موضوعات' میں گروپ کرتا ہے جو عام طور پر اس موضوع سے وابستہ اصطلاحات یا فقروں کی بنیاد پر ہوتا ہے۔ مثال کے طور پر، اضطراب کے بارے میں ایک جملے میں استعمال ہونے والی زبان ڈپریشن کے بارے میں بات کرتے وقت استعمال ہونے والی زبان سے بہت ملتی جلتی ہو سکتی ہے، جسے ذہنی صحت کے موضوع میں گروپ کیا گیا ہے۔ اسے ٹیکسٹ اینالیٹکس کے لیے 'باٹم اپ' اپروچ کے طور پر جانا جاتا ہے کیونکہ یہ ڈیٹا تک پہنچتا ہے جس میں اس میں موجود موضوعات کے بارے میں کوئی پیشگی تصورات نہیں ہوتے، بلکہ یہ متن کے مواد کی بنیاد پر موضوعات کو ابھرنے کی اجازت دیتا ہے۔
کہانیوں کو موضوع کے ماڈل میں شامل کرنے کے لیے دو طریقوں سے منتخب کیا گیا تھا۔ سب سے پہلے، ہر سوال کے تمام جوابات آن لائن فارم سے لیے گئے اور خالی ڈیٹا ہٹا دیا گیا۔ دوم، جوابات کو ماڈیول 4 سے ان کی مطابقت کی بنیاد پر فلٹر کیا گیا تھا۔
کہانیوں کو متعلقہ سمجھا جاتا تھا اگر ان کا اشتراک کرنے والوں نے سوال 'آپ ہمیں کس کے بارے میں بتانا چاہیں گے؟' پر نیچے دیئے گئے جوابات میں سے کسی کو منتخب کیا تھا:
- کوویڈ ٹیسٹنگ اور ویکسینیشن
- سرکاری سرکاری معلومات، مثال کے طور پر، گھر میں الگ تھلگ رہنے کے بارے میں مشورہ
- کچھ مثبت جس کا آپ نے تجربہ کیا۔
متعلقہ کہانیوں کی شناخت کے بعد، آن لائن فارم میں شامل تین کھلے سوالات میں سے ہر ایک کے لیے ایک ٹاپک ماڈل چلایا گیا۔ اس سے ہم نے Q1 کے تمام جوابات میں کل 110 عنوانات کی نشاندہی کی، Q2 میں 129، اور Q3 میں 132۔ چونکہ تعاون کنندگان سوال کے متعدد جوابات منتخب کر سکتے ہیں 'آپ ہمیں کس بارے میں بتانا چاہیں گے؟' یہ ممکن تھا کہ شامل کرنے کے لیے منتخب کردہ کہانیوں میں ایسی معلومات شامل ہوں جو ماڈیول 4 سے متعلق نہ ہوں۔ اس وجہ سے، ابتدائی موضوع کی ماڈلنگ کے بعد، Ipsos کی تحقیقی ٹیم نے تمام موضوعات کا مطابقت کے لیے جائزہ لیا اور ماڈیول 4 سے متعلق نہ ہونے والے موضوعات کو آخری مرحلے سے ہٹا دیا گیا۔ تجزیہ اس نے Q1 میں کل 28 عنوانات، Q2 میں 49 عنوانات، اور Q3 میں 73 عنوانات کو ہٹا دیا، جس سے فی سوال بالترتیب 82، 80، اور 59 عنوانات رہ گئے۔
ماڈیول 4 سے متعلق نہ ہونے والے عنوانات کو ہٹانے کے بعد ایک شماریاتی عنصر کا تجزیہ کیا گیا تاکہ موضوعات کے درمیان تعلقات کو نقشہ بنایا جا سکے اور ان کی بنیاد پر ان کو گروپ کیا جائے جو عام طور پر ایک دوسرے کے ساتھ یا ایک دوسرے کے تین جملوں کے اندر ہوتے ہیں۔ مثال کے طور پر، سائنسی شواہد، صحت عامہ اور اعداد و شمار اور اعداد و شمار کے عنوانات کو خود بخود حکومتی ڈیٹا کے بارے میں ایک عنصر میں گروپ کیا گیا تھا۔ عنصر کے تجزیے نے Q1 میں متعلقہ 82 موضوعات پر 16 اہم عوامل، Q2 میں 19 عوامل، اور Q3 میں 19 عوامل پیدا کیے۔
موضوع کی ماڈلنگ اور فیکٹر تجزیہ کے بعد ماڈیول 4 سے متعلقہ موضوعات کی بنیاد پر ایک کوڈ فریم تیار کیا گیا تھا۔ اس میں کلیدی الفاظ اور نمونوں کی شناخت کرنے کے لیے، مکمل ڈیٹا سیٹ اور ہر موضوع کے اندر، سب سے زیادہ عام الفاظ اور فقروں کا انسانی جائزہ شامل تھا۔ کہانیوں کو مناسب عنوانات اور ذیلی عنوانات میں گروپ کرنے کے لیے استعمال کیا جاتا ہے۔ ایسا کرنے سے، اس نے تحقیقی ٹیم کو عنوانات کے سائز اور عناصر کی بہت زیادہ درست مقدار فراہم کی، تاکہ تجزیہ کے نقطہ نظر سے آگاہ کیا جا سکے۔
چونکہ زیادہ لوگوں نے موضوع کی ماڈلنگ اور مطلوبہ الفاظ کی مماثلت کے درمیان انکوائری کے ساتھ اپنی کہانی شیئر کی تھی، اس لیے تجزیہ کے اس آخری مرحلے کے لیے Ipsos کو کہانیوں کا ایک اضافی سیٹ فراہم کیا گیا تھا۔ مجموعی طور پر، اس مقام پر 34,441 کہانیاں شامل کی گئی تھیں، اور یہ سوال 'آپ ہمیں کس کے بارے میں بتانا چاہیں گے؟' سے اب فلٹر نہیں کیے گئے تھے۔ یہ فیصلہ اس بات کو یقینی بنانے کے لیے لیا گیا کہ لوگوں کے استعمال کردہ الفاظ کی بنیاد پر تمام متعلقہ کہانیوں کو پکڑ لیا جائے۔
اس کے بعد محققین نے کہانیوں کو دریافت کرنے کے لیے ماڈیول 4 سے متعلقہ مختلف موضوعات کا جائزہ لیا۔ ان کو اس ریکارڈ میں شامل کرنے کے لیے دوسرے طریقوں سے انکوائری کے ساتھ شیئر کی گئی کہانیوں کے ساتھ لایا گیا تھا (ذیل میں بیان کیا گیا ہے)۔
ذیل کا خاکہ آن لائن فارم میں شامل تھیمز کو دکھاتا ہے اور ان کے جواب میں ایک شراکت دار کے ذریعہ ہر تھیم کا کتنی بار ذکر کیا گیا تھا۔ ہر بلاک کا سائز تھیم سے متعلق جوابات کے حجم کی نمائندگی کرتا ہے۔ نوٹ کریں کہ شراکت داروں نے اپنے جواب میں متعدد موضوعات کا تذکرہ کیا ہو سکتا ہے اور اس وجہ سے انہیں کئی بار شمار کیا جا سکتا ہے۔
شکل 2: آن لائن فارم تھیمز
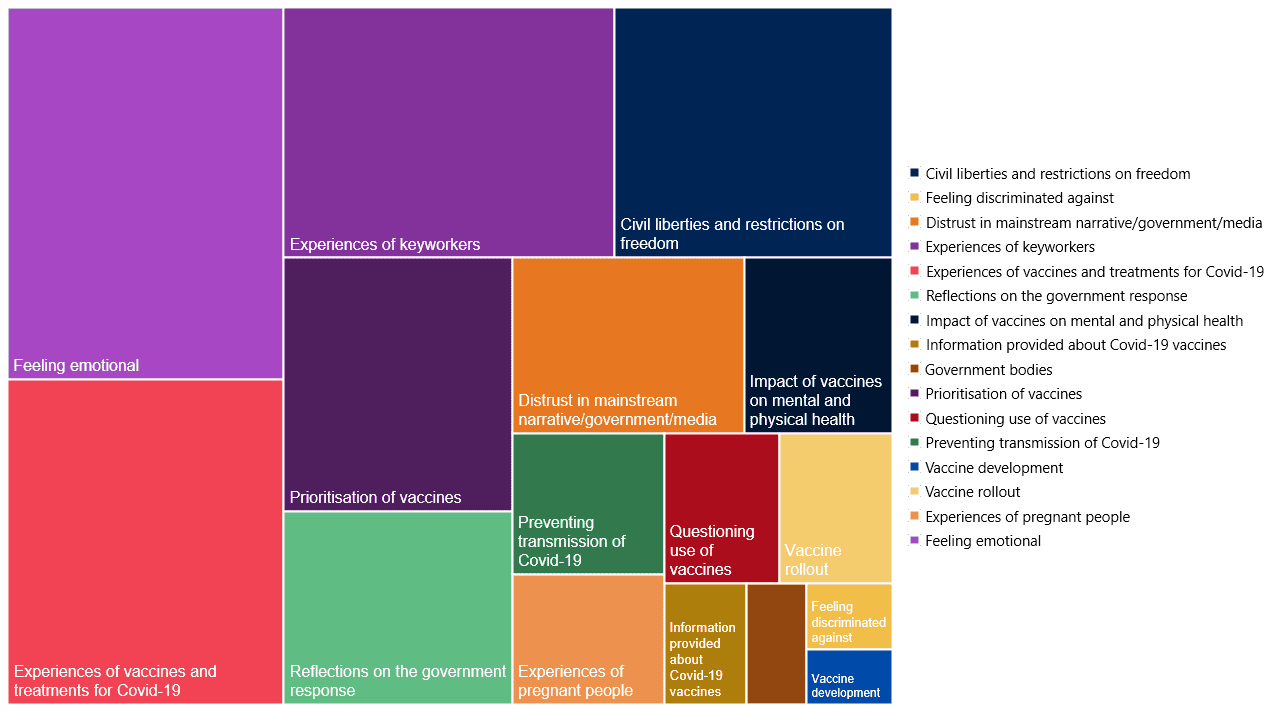
سننے والے واقعات
ایوری سٹوری میٹرز ٹیم انگلینڈ، ویلز، سکاٹ لینڈ اور شمالی آئرلینڈ کے 25 قصبوں اور شہروں کا سفر کیا، لوگوں کو ان کی مقامی کمیونٹیز میں ذاتی طور پر اپنے وبائی تجربے کا اشتراک کرنے کا موقع فراہم کرنا۔ سننے کی تقریبات درج ذیل مقامات پر منعقد کی گئیں۔
- کارلیسیل
- Wrexham اور Ruthin
- نیوہم
- ایکسیٹر
- پیسلے
- ڈیری / لندنڈیری
- مڈلزبرو
- اینسکیلن
- بریڈ فورڈ
- سکیگنیس
- اسٹاکٹن آن ٹیز
- برمنگھم
- ملٹن کینز
- بورن ماؤتھ
ورچوئل سننے کے سیشن بھی منعقد کیے گئے جہاں اس نقطہ نظر کو ترجیح دی گئی۔ ہم نے بہت سے خیراتی اداروں اور نچلی سطح کے کمیونٹی گروپس کے ساتھ کام کیا تاکہ وبائی امراض سے متاثر ہونے والوں سے مخصوص طریقوں سے بات کی جا سکے۔ اس میں سوگوار خاندان، لانگ کوویڈ اور پیڈیاٹرک انفلامیٹری ملٹی سسٹم سنڈروم (PIMS-Ts) کے ساتھ رہنے والے لوگ، طبی لحاظ سے کمزور لوگ اور ان کے خاندان، معذور افراد، پناہ گزین، نسلی اقلیتی پس منظر کے لوگ اور صحت کی دیکھ بھال کے پیشہ ور افراد شامل ہیں۔ ہر ایونٹ کے لیے مختصر خلاصہ رپورٹیں لکھی جاتی تھیں، ایونٹ کے شرکاء کے ساتھ شیئر کی جاتی تھیں، اور اس دستاویز کو مطلع کرنے کے لیے استعمال کی جاتی تھیں۔
ٹارگٹڈ سننا
سماجی تحقیق اور کمیونٹی کے پیشہ ور افراد کے کنسورشیم کو ایوری سٹوری میٹرز نے گہرائی سے انٹرویوز اور ڈسکشن گروپس کرنے کے لیے کمیشن بنایا تھا۔ مخصوص گروہوں کے تجربات کو سمجھنے کے لیے، یعنی وہ لوگ جن کی صحت سے متعلق خاص خدشات ہیں جنہوں نے ان کے ویکسین کے فیصلوں کو متاثر کیا ہو (بشمول طبی طور پر کمزور اور طبی لحاظ سے انتہائی کمزور افراد اور وہ لوگ جو حاملہ تھے یا دودھ پلا رہے تھے جب انہیں ویکسین پیش کی گئی تھی) اور وہ گروپ جہاں موجود تھے۔ CoVID-19 ویکسینز کا استعمال نسبتاً کم تھا (بشمول سیاہ افریقی، سیاہ کیریبین، پاکستانی، اور بنگلہ دیشی گروپوں کے ساتھ ساتھ دوسرے طریقوں سے جواب دینے کے امکانات کم ہیں۔ ان انٹرویوز اور ڈسکشن گروپس نے ماڈیول 4 کے لیے کلیدی لائنز آف انکوائری (KLOEs) پر توجہ دی۔ اکتوبر 2023 اور دسمبر 2023۔ اس میں 121 گہرائی سے انٹرویوز شامل ہیں:
- وہ لوگ جو قوت مدافعت کا شکار ہیں/طبی طور پر کمزور ہیں اور وہ وبائی امراض کے دوران حفاظت کر رہے تھے۔
- وہ لوگ جو حاملہ تھے یا دودھ پلا رہے تھے اس وقت جب انہیں ویکسین لگائی گئی تھی۔
- سیاہ افریقی، سیاہ کیریبین، پاکستانی اور بنگلہ دیشی گروہوں کے لوگ۔
- وہ لوگ جنہوں نے CoVID-19 ویکسین حاصل نہ کرنے کا انتخاب کیا۔
تمام گہرائی والے انٹرویوز اور ڈسکشن گروپس تربیت یافتہ محققین کے ذریعہ کئے گئے تھے جنہوں نے ڈسکشن گائیڈ کی پیروی کی۔ جہاں ضرورت ہو، محققین شراکت داروں سے ان کے تجربے کے بارے میں مزید معلومات حاصل کریں گے۔ ہر انٹرویو 30 منٹ تک جاری رہا اور تمام فوکس گروپ 90 منٹ تک جاری رہے۔ ماڈیول 4 کی لائنز آف انکوائری (KLOEs) سے متعلقہ کلیدی موضوعات کی نشاندہی کرنے کے لیے انٹرویوز اور ڈسکشن گائیڈز ریکارڈ کیے گئے، نقل کیے گئے، اور کوڈ کیے گئے اور انسانی جائزے کے ذریعے تجزیہ کیے گئے۔
نیچے دی گئی جدولیں صحت کی دیکھ بھال کے نظام میں اور صحت کی عدم مساوات کا سامنا کرنے والے لوگوں کے انٹرویوز کی تعداد کا خاکہ پیش کرتی ہیں۔
| شریک کی قسم | انٹرویوز مکمل |
|---|---|
| عام لوگ جنھیں کم از کم ایک خوراک ملی تھی۔ | 18 مباحثہ گروپوں میں 107 شرکاء |
| وہ لوگ جنہوں نے CoVID-19 ویکسین حاصل نہ کرنے کا انتخاب کیا۔ | 20 |
| وہ لوگ جو حاملہ تھے یا دودھ پلا رہے تھے جب ویکسین کی پیشکش کی گئی تھی۔ | 30 |
| وہ لوگ جو مدافعتی طور پر کمزور/طبی طور پر کمزور ہیں۔ | 30 |
| نسلی اقلیتی پس منظر سے تعلق رکھنے والے لوگ | 41 |
| کل | 228 |